
ACGME Program Requirements for
Graduate Medical Education
in Internal Medicine
Definitions
For more information, see the ACGME Glossary of Terms.
Core Requirements: Statements that define structure, resource, or process elements
essential to every graduate medical educational program.
Detail Requirements: Statements that describe a specific structure, resource, or
process, for achieving compliance with a Core Requirement. Programs and
sponsoring institutions in substantial compliance with the Outcome Requirements may
utilize alternative or innovative approaches to meet Core Requirements.
Outcome Requirements: Statements that specify expected measurable or observable
attributes (knowledge, abilities, skills, or attitudes) of residents or fellows at key stages
of their graduate medical education.
Osteopathic Recognition
For programs with or applying for Osteopathic Recognition, the Osteopathic Recognition
Requirements also apply (www.acgme.org/OsteopathicRecognition).
Revision Information
ACGME-approved Focused Revision: February 7, 2022; effective July 1, 2022
Updated to include revised Common Program Requirements, effective July 1, 2023
Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 2 of 64
Contents
Introduction ................................................................................................................................. 3
Int.A. Definition of Graduate Medical Education ............................................................................ 3
Int.B. Definition of Specialty ........................................................................................................... 3
Int.C. Length of Educational Program ............................................................................................ 4
I. Oversight .............................................................................................................................. 5
I.A. Sponsoring Institution ............................................................................................................ 5
I.B. Participating Sites ................................................................................................................... 5
I.C. Workforce Recruitment and Retention ................................................................................. 6
I.D. Resources ................................................................................................................................ 6
I.E. Other Learners and Health Care Personnel ......................................................................... 8
II. Personnel ............................................................................................................................. 9
II.A. Program Director ..................................................................................................................... 9
II.B. Faculty .................................................................................................................................... 15
II.C. Program Coordinator ............................................................................................................ 22
II.D. Other Program Personnel .................................................................................................... 25
III. Resident Appointments .................................................................................................... 25
III.A. Eligibility Requirements ....................................................................................................... 25
III.B. Resident Complement .......................................................................................................... 26
III.C. Resident Transfers ................................................................................................................ 26
IV. Educational Program ......................................................................................................... 26
IV.A. Educational Components ..................................................................................................... 27
IV.B. ACGME Competencies ......................................................................................................... 28
IV.C. Curriculum Organization and Resident Experiences ........................................................ 34
IV.D. Scholarship ............................................................................................................................ 40
V. Evaluation ........................................................................................................................... 42
V.A. Resident Evaluation .............................................................................................................. 42
V.B. Faculty Evaluation ................................................................................................................ 45
V.C. Program Evaluation and Improvement ............................................................................... 46
VI. The Learning and Working Environment ........................................................................ 49
VI.A. Patient Safety, Quality Improvement, Supervision, and Accountability ......................... 50
VI.B. Professionalism..................................................................................................................... 53
VI.C. Well-Being .............................................................................................................................. 55
VI.D. Fatigue Mitigation ................................................................................................................. 57
VI.E. Clinical Responsibilities, Teamwork, and Transitions of Care ........................................ 58
VI.F. Clinical Experience and Education ..................................................................................... 59
Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 3 of 64
ACGME Program Requirements for Graduate Medical Education
in Internal Medicine
Common Program Requirements (Residency) are in BOLD
Where applicable, text in italics describes the underlying philosophy of the requirements in that
section. These philosophic statements are not program requirements and are therefore not
citable.
Introduction
Int.A. Definition of Graduate Medical Education
Graduate medical education is the crucial step of professional
development between medical school and autonomous clinical practice. It
is in this vital phase of the continuum of medical education that residents
learn to provide optimal patient care under the supervision of faculty
members who not only instruct, but serve as role models of excellence,
compassion, cultural sensitivity, professionalism, and scholarship.
Graduate medical education transforms medical students into physician
scholars who care for the patient, patient’s family, and a diverse
community; create and integrate new knowledge into practice; and educate
future generations of physicians to serve the public. Practice patterns
established during graduate medical education persist many years later.
Graduate medical education has as a core tenet the graded authority and
responsibility for patient care. The care of patients is undertaken with
appropriate faculty supervision and conditional independence, allowing
residents to attain the knowledge, skills, attitudes, judgment, and empathy
required for autonomous practice. Graduate medical education develops
physicians who focus on excellence in delivery of safe, equitable,
affordable, quality care; and the health of the populations they serve.
Graduate medical education values the strength that a diverse group of
physicians brings to medical care, and the importance of inclusive and
psychologically safe learning environments.
Graduate medical education occurs in clinical settings that establish the
foundation for practice-based and lifelong learning. The professional
development of the physician, begun in medical school, continues through
faculty modeling of the effacement of self-interest in a humanistic
environment that emphasizes joy in curiosity, problem-solving, academic
rigor, and discovery. This transformation is often physically, emotionally,
and intellectually demanding and occurs in a variety of clinical learning
environments committed to graduate medical education and the well-being
of patients, residents, fellows, faculty members, students, and all members
of the health care team.
Int.B. Definition of Specialty

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 4 of 64
Internists are specialists who care for adult patients through comprehensive,
clinical problem solving. They integrate the history, physical examination, and all
available data to deliver, direct, and coordinate care across varied clinical
settings, both in person and remotely through telemedicine. Internists are
diagnosticians who manage the care of patients who present with
undifferentiated, complex illnesses, and comorbidities; promote health and health
equity in communities; collaborate with colleagues; and lead, mentor, and serve
multidisciplinary teams. Internists integrate care across organ systems and
disease processes throughout the adult lifespan. They are expert
communicators, creative and adaptable to the changing needs of patients and
the health care environment. They advocate for their patients within the health
care system to achieve the patient’s and family’s care goals. Internists embrace
lifelong learning and the privilege and responsibility of educating patients,
populations, and other health professionals. The discipline is characterized by a
compassionate, cognitive, scholarly, relationship-oriented approach to
comprehensive patient care.
The successful, fulfilled internist maintains this core function and these core
values. Internists find meaning and purpose in caring for individual patients with
increased efficiency through well-functioning teams, and are equipped and
trained to manage change effectively and lead those teams. They understand
and manage the business of medicine to optimize cost-conscious care for their
patients. They apply data management science to population and patient
applications and help solve the clinical problems of their patients and their
community. Internists communicate fluently and are able to educate and clearly
explain complex data and concepts to all audiences, especially patients. They
collaborate with patients to implement health care ethics in all aspects of their
care. Internists display emotional intelligence in their relationships with
colleagues, team members, and patients, maximizing both their own and their
teams’ well-being. They are dedicated professionals who have the knowledge,
skills, and attitudes to effectively use all available resources, and bring
intellectual curiosity and human warmth to their patients and community.
Specialty-Specific Background and Intent: The Review Committee developed this definition
to clearly articulate the core functions and values of internal medicine and describe what is
needed to move the specialty forward through program requirements. They express what
the Review Committee aspires to see in the graduates of internal medicine residency
programs, faculty members, and the broader internal medicine community.
Int.C. Length of Educational Program
An accredited residency program in internal medicine must provide 36 months of
supervised graduate medical education.
(Core)
Specialty-Specific Background and Intent: While internal medicine residency must be
completed within a 36-month supervised educational framework (barring remediation and
extended leaves), the requirements were written to be flexible and allow program directors
the opportunity to create more individualized educational experiences for residents who have
achieved, or are on a trajectory to achieve, competence in the foundational areas of internal
medicine. This was a guiding principle for the revision process. The requirements for the

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 5 of 64
foundational areas of internal medicine and individualized educational experiences are
located in Section IV.C.: Curriculum Organization and Resident Experiences.
I. Oversight
I.A. Sponsoring Institution
The Sponsoring Institution is the organization or entity that assumes the
ultimate financial and academic responsibility for a program of graduate
medical education, consistent with the ACGME Institutional Requirements.
When the Sponsoring Institution is not a rotation site for the program, the
most commonly utilized site of clinical activity for the program is the
primary clinical site.
Background and Intent: Participating sites will reflect the health care needs of the
community and the educational needs of the residents. A wide variety of organizations
may provide a robust educational experience and, thus, Sponsoring Institutions and
participating sites may encompass inpatient and outpatient settings including, but not
limited to a university, a medical school, a teaching hospital, a nursing home, a school
of public health, a health department, a public health agency, an organized health care
delivery system, a medical examiner’s office, an educational consortium, a teaching
health center, a physician group practice, federally qualified health center, or an
educational foundation.
I.A.1. The program must be sponsored by one ACGME-accredited
Sponsoring Institution.
(Core)
I.B. Participating Sites
A participating site is an organization providing educational experiences or
educational assignments/rotations for residents.
I.B.1. The program, with approval of its Sponsoring Institution, must
designate a primary clinical site.
(Core)
I.B.1.a) The program, in partnership with its Sponsoring Institution, must
ensure that there is a reporting relationship between the internal
medicine subspecialty programs and the residency program
director.
(Core)
I.B.2. There must be a program letter of agreement (PLA) between the
program and each participating site that governs the relationship
between the program and the participating site providing a required
assignment.
(Core)
I.B.2.a) The PLA must:
I.B.2.a).(1) be renewed at least every 10 years; and,
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 6 of 64
I.B.2.a).(2) be approved by the designated institutional official
(DIO).
(Core)
I.B.3. The program must monitor the clinical learning and working
environment at all participating sites.
(Core)
I.B.3.a) At each participating site there must be one faculty member,
designated by the program director as the site director, who
is accountable for resident education at that site, in
collaboration with the program director.
(Core)
Background and Intent: While all residency programs must be sponsored by a single
ACGME-accredited Sponsoring Institution, many programs will utilize other clinical
settings to provide required or elective training experiences. At times it is appropriate
to utilize community sites that are not owned by or affiliated with the Sponsoring
Institution. Some of these sites may be remote for geographic, transportation, or
communication issues. When utilizing such sites, the program must ensure the quality
of the educational experience.
Suggested elements to be considered in PLAs will be found in the Guide to the
Common Program Requirements. These include:
• Identifying the faculty members who will assume educational and supervisory
responsibility for residents
• Specifying the responsibilities for teaching, supervision, and formal evaluation
of residents
• Specifying the duration and content of the educational experience
• Stating the policies and procedures that will govern resident education during
the assignment
I.B.4. The program director must submit any additions or deletions of
participating sites routinely providing an educational experience,
required for all residents, of one month full time equivalent (FTE) or
more through the ACGME’s Accreditation Data System (ADS).
(Core)
I.C. Workforce Recruitment and Retention
The program, in partnership with its Sponsoring Institution, must engage in
practices that focus on mission-driven, ongoing, systematic recruitment
and retention of a diverse and inclusive workforce of residents, fellows (if
present), faculty members, senior administrative GME staff members, and
other relevant members of its academic community.
(Core)
Background and Intent: It is expected that the Sponsoring Institution has, and
programs implement, policies and procedures related to recruitment and retention of
individuals underrepresented in medicine and medical leadership in accordance with
the Sponsoring Institution’s mission and aims.
I.D. Resources

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 7 of 64
I.D.1. The program, in partnership with its Sponsoring Institution, must
ensure the availability of adequate resources for resident education.
(Core)
I.D.1.a) The program, in partnership with its Sponsoring institution, must:
I.D.1.a).(1) provide the broad range of facilities and clinical support
services necessary to provide comprehensive and timely
care of adult patients;
(Core)
I.D.1.a).(2) ensure that the program has adequate space available,
including meeting rooms, classrooms, examination rooms,
computers, visual and other educational aids, and office
space;
(Core)
I.D.1.a).(3) ensure that appropriate in-person or remote/virtual
consultations, including those done using
telecommunication technology, are available in settings in
which residents work;
(Core)
I.D.1.a).(4) provide access to an electronic health record; and,
(Core)
Specialty-Specific Background and Intent: An electronic health record (EHR) can include
electronic notes, orders, and lab reporting. Such a system also facilitates data reporting
regarding the care provided to a patient or a panel of patients. It may also include systems for
enhancing the quality and safety of patient care. An EHR does not have to be present at all
participating sites and does not have to include every element of patient care information.
However, a system that simply reports laboratory or imaging results does not meet the
definition of an EHR.
I.D.1.a).(5) provide residents with access to training using simulation
to support resident education and patient safety.
(Core)
Specialty-Specific Background and Intent: The Review Committee does not expect each
program to own a simulator or to have a simulation center. “Simulation” is used broadly to
mean learning about patient care in settings that do not include actual patients. This could
include objective structured clinical examinations (OSCEs), standardized patients, patient
simulators, or electronic simulation of resuscitation, procedures, and other clinical scenarios.
I.D.1.b) The program must provide residents with a patient population
representative of both the broad spectrum of clinical disorders and
medical conditions managed by internists, and of the community
being served.
(Core)
I.D.2. The program, in partnership with its Sponsoring Institution, must
ensure healthy and safe learning and working environments that
promote resident well-being and provide for:
I.D.2.a) access to food while on duty;
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 8 of 64
I.D.2.b) safe, quiet, clean, and private sleep/rest facilities available
and accessible for residents with proximity appropriate for
safe patient care;
(Core)
Background and Intent: Care of patients within a hospital or health system occurs
continually through the day and night. Such care requires that residents function at
their peak abilities, which requires the work environment to provide them with the
ability to meet their basic needs within proximity of their clinical responsibilities.
Access to food and rest are examples of these basic needs, which must be met while
residents are working. Residents should have access to refrigeration where food may
be stored. Food should be available when residents are required to be in the hospital
overnight. Rest facilities are necessary, even when overnight call is not required, to
accommodate the fatigued resident.
I.D.2.c) clean and private facilities for lactation that have refrigeration
capabilities, with proximity appropriate for safe patient care;
(Core)
Background and Intent: Sites must provide private and clean locations where residents
may lactate and store the milk within a refrigerator. These locations should be in close
proximity to clinical responsibilities. It would be helpful to have additional support
within these locations that may assist the resident with the continued care of patients,
such as a computer and a phone. While space is important, the time required for
lactation is also critical for the well-being of the resident and the resident's family, as
outlined in VI.C.1.c).(1).
I.D.2.d) security and safety measures appropriate to the participating
site; and,
(Core)
I.D.2.e)
accommodations for residents with disabilities consistent
with the Sponsoring Institution’s policy.
(Core)
I.D.3. Residents must have ready access to specialty-specific and other
appropriate reference material in print or electronic format. This
must include access to electronic medical literature databases with
full text capabilities.
(Core)
I.E. Other Learners and Health Care Personnel
The presence of other learners and other health care personnel, including
but not limited to residents from other programs, subspecialty fellows, and
advanced practice providers, must not negatively impact the appointed
residents’ education.
(Core)
Background and Intent: The clinical learning environment has become increasingly
complex and often includes care providers, students, and post-graduate residents and
fellows from multiple disciplines. The presence of these practitioners and their
learners enriches the learning environment. Programs have a responsibility to monitor
the learning environment to ensure that residents’ education is not compromised by
the presence of other providers and learners.

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 9 of 64
II. Personnel
II.A. Program Director
II.A.1. There must be one faculty member appointed as program director
with authority and accountability for the overall program, including
compliance with all applicable program requirements.
(Core)
II.A.1.a) The Sponsoring Institution’s GMEC must approve a change in
program director and must verify the program director’s
licensure and clinical appointment.
(Core)
Background and Intent: While the ACGME recognizes the value of input from
numerous individuals in the management of a residency, a single individual must be
designated as program director and have overall responsibility for the program. The
program director’s nomination is reviewed and approved by the GMEC.
II.A.1.b) The program must demonstrate retention of the program
director for a length of time adequate to maintain continuity
of leadership and program stability.
(Core)
Background and Intent: The success of residency programs is generally enhanced by
continuity in the program director position. The professional activities required of a
program director are unique and complex and take time to master. All programs are
encouraged to undertake succession planning to facilitate program stability when
there is necessary turnover in the program director position.
II.A.2. The program director and, as applicable, the program’s leadership
team, must be provided with support adequate for administration of
the program based upon its size and configuration.
(Core)
II.A.2.a) At a minimum, the program director must be provided with the
dedicated time and support specified below for administration of
the program:
(Core)
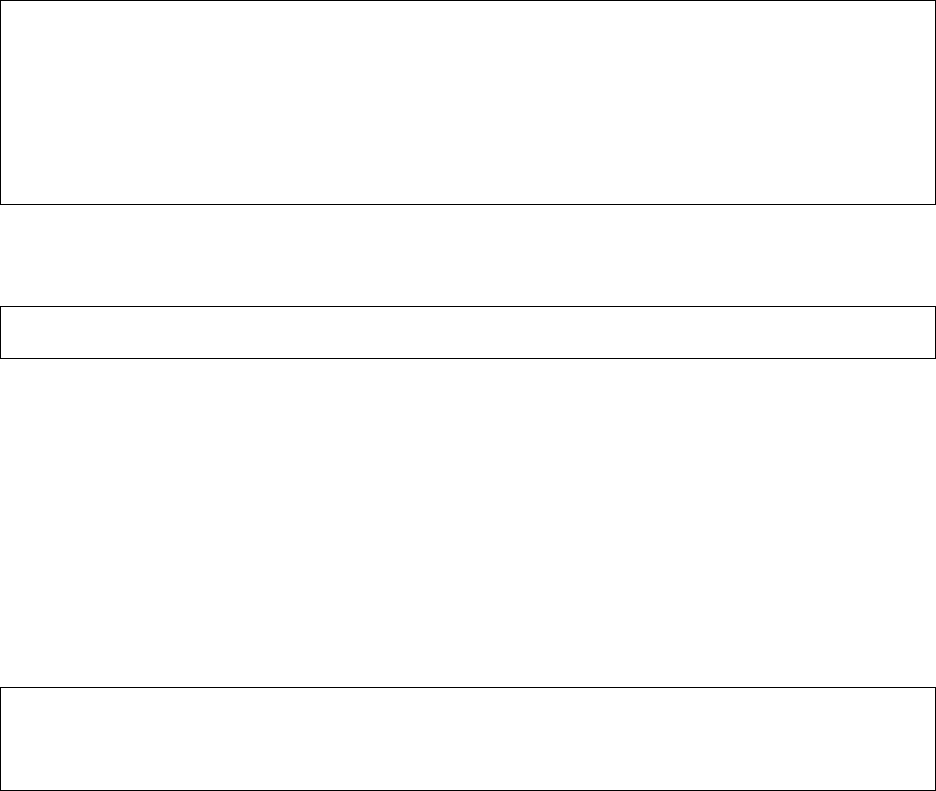
Number of Approved
Resident Positions
Minimum Support
Required (FTE)
<7
0.2
7-10
0.4
>10
0.5
II.A.2.b) Programs with more than 15 residents must appoint an associate
program director(s). The associate program director(s) must be
provided with support equal to a dedicated minimum time for
administration of the program as follows:
(Core)
Number of Approved
Resident Positions
Minimum Support
Required (FTE)
<15
0

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 10 of 64
Number of Approved
Resident Positions
Minimum Support
Required (FTE)
16-20
0.1
21-25
0.2
26-30
0.3
31-35
0.4
36-40
0.5
41-45
0.6
46-50
0.7
51-55
0.8
56-60
0.9
61-65
1.0
66-70
1.1
71-75
1.2
76-80
1.3
81-85
1.4
86-90
1.5
91-95
1.6
96-100
1.7
101-105
1.8
106-110
1.9
111-115
2.0
116-120
2.1
121-125
2.2
126-130
2.3
131-135
2.4
136-140
2.5
141-145
2.6
146-150
2.7
151-155
2.8
156-160
2.9
161-165
3.0
166-170
3.1
171-175
3.2
176-180
3.3
181-185
3.4
186-190
3.5
191-195
3.6
196-200
3.7
201-205
3.8
206-210
3.9
211-215
4.0
216-220
4.1
221-225
4.2
226-230
4.3
Background and Intent: To achieve successful graduate medical education, individuals

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 11 of 64
serving as education and administrative leaders of residency programs, as well as
those significantly engaged in the education, supervision, evaluation, and mentoring of
residents, must have sufficient dedicated professional time to perform the vital
activities required to sustain an accredited program.
The ultimate outcome of graduate medical education is excellence in resident
education and patient care.
The program director and, as applicable, the program leadership team, devote a
portion of their professional effort to the oversight and management of the residency
program, as defined in II.A.4.-II.A.4.a).(12). Both provision of support for the time
required for the leadership effort and flexibility regarding how this support is provided
are important. Programs, in partnership with their Sponsoring Institutions, may provide
support for this time in a variety of ways. Examples of support may include, but are not
limited to, salary support, supplemental compensation, educational value units, or
relief of time from other professional duties.
Program directors and, as applicable, members of the program leadership team, who
are new to the role may need to devote additional time to program oversight and
management initially as they learn and become proficient in administering the
program. It is suggested that during this initial period the support described above be
increased as needed.
In addition, it is important to remember that the dedicated time and support
requirement for ACGME activities is a minimum, recognizing that, depending on the
unique needs of the program, additional support may be warranted. The need to
ensure adequate resources, including adequate support and dedicated time for the
program director, is also addressed in Institutional Requirement II.B.1. The amount of
support and dedicated time needed for individual programs will vary based on a
number of factors and may exceed the minimum specified in the applicable
specialty/subspecialty-specific Program Requirements. It is expected that the
Sponsoring Institution, in partnership with its accredited programs, will ensure support
for program directors to fulfill their program responsibilities effectively.
Specialty-Specific Background and Intent: For instance, a program with an approved
complement of 36 residents is required to have 50% FTE support for the program director
and 50 percent FTE support for the associate program director(s). The Review Committee
decided not to specify how the support should be distributed among associate program
directors to allow programs, in partnership with their sponsoring institution, to allocate the
support as they see fit. Further, the program could redistribute the FTE back to the program
director; for example, in this instance, the associate program director(s) could receive 25
percent FTE support and the program director could receive 75 percent FTE support (50
percent plus the remaining 25 percent from the associate program director FTE support).
II.A.3. Qualifications of the program director:
II.A.3.a) must include specialty expertise and at least three years of
documented educational and/or administrative experience, or
qualifications acceptable to the Review Committee;
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 12 of 64
Background and Intent: Leading a program requires knowledge and skills that are
established during residency and subsequently further developed. The time period
from completion of residency until assuming the role of program director allows the
individual to cultivate leadership abilities while becoming professionally established.
The three-year period is intended for the individual's professional maturation.
The broad allowance for educational and/or administrative experience recognizes that
strong leaders arise through diverse pathways. These areas of expertise are important
when identifying and appointing a program director. The choice of a program director
should be informed by the mission of the program and the needs of the community.
In certain circumstances, the program and Sponsoring Institution may propose and the
Review Committee may accept a candidate for program director who fulfills these
goals but does not meet the three-year minimum.
II.A.3.b) must include current certification in the specialty for which
they are the program director by the American Board of
Internal Medicine (ABIM) or by the American Osteopathic
Board of Internal Medicine (AOBIM), or specialty qualifications
that are acceptable to the Review Committee;
(Core)
II.A.3.b).(1) The Review Committee only accepts current certification in
internal medicine from the ABIM or AOBIM.
(Core)
II.A.3.c) must include ongoing clinical activity.
(Core)
Background and Intent: A program director is a role model for faculty members and
residents. The program director must participate in clinical activity consistent with the
specialty. This activity will allow the program director to role model the Core
Competencies for the faculty members and residents.
II.A.3.d) must have experience working as part of an interdisciplinary, inter-
professional team to create an educational environment that
promotes high-quality care, patient safety, and resident well-being.
(Core)
II.A.4. Program Director Responsibilities
The program director must have responsibility, authority, and
accountability for: administration and operations; teaching and
scholarly activity; resident recruitment and selection, evaluation,
and promotion of residents, and disciplinary action; supervision of
residents; and resident education in the context of patient care.
(Core)
II.A.4.a) The program director must:
II.A.4.a).(1) be a role model of professionalism;
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 13 of 64
Background and Intent: The program director, as the leader of the program, must serve
as a role model to residents in addition to fulfilling the technical aspects of the role. As
residents are expected to demonstrate compassion, integrity, and respect for others,
they must be able to look to the program director as an exemplar. It is of utmost
importance, therefore, that the program director model outstanding professionalism,
high quality patient care, educational excellence, and a scholarly approach to work.
The program director creates an environment where respectful discussion is welcome,
with the goal of continued improvement of the educational experience.
II.A.4.a).(2) design and conduct the program in a fashion
consistent with the needs of the community, the
mission(s) of the Sponsoring Institution, and the
mission(s) of the program;
(Core)
Background and Intent: The mission of institutions participating in graduate medical
education is to improve the health of the public. Each community has health needs that
vary based upon location and demographics. Programs must understand the structural
and social determinants of health of the populations they serve and incorporate them
in the design and implementation of the program curriculum, with the ultimate goal of
addressing these needs and eliminating health disparities.
II.A.4.a).(3) administer and maintain a learning environment
conducive to educating the residents in each of the
ACGME Competency domains;
(Core)
Background and Intent: The program director may establish a leadership team to
assist in the accomplishment of program goals. Residency programs can be highly
complex. In a complex organization, the leader typically has the ability to delegate
authority to others, yet remains accountable. The leadership team may include
physician and non-physician personnel with varying levels of education, training, and
experience.
II.A.4.a).(4) have the authority to approve or remove physicians
and non-physicians as faculty members at all
participating sites, including the designation of core
faculty members, and must develop and oversee a
process to evaluate candidates prior to approval;
(Core)
Background and Intent: The provision of optimal and safe patient care requires a team
approach. The education of residents by non-physician educators may enable the
resident to better manage patient care and provides valuable advancement of the
residents’ knowledge. Furthermore, other individuals contribute to the education of
residents in the basic science of the specialty or in research methodology. If the
program director determines that the contribution of a non-physician individual is
significant to the education of the residents, the program director may designate the
individual as a program faculty member or a program core faculty member.
II.A.4.a).(5) have the authority to remove residents from
supervising interactions and/or learning environments
that do not meet the standards of the program;
(Core)
Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 14 of 64
Background and Intent: The program director has the responsibility to ensure that all
who educate residents effectively role model the Core Competencies. Working with a
resident is a privilege that is earned through effective teaching and professional role
modeling. This privilege may be removed by the program director when the standards
of the clinical learning environment are not met.
There may be faculty in a department who are not part of the educational program, and
the program director controls who is teaching the residents.
II.A.4.a).(6) submit accurate and complete information required
and requested by the DIO, GMEC, and ACGME;
(Core)
Background and Intent: This includes providing information in the form and format
requested by the ACGME and obtaining requisite sign-off by the DIO.
II.A.4.a).(7) provide a learning and working environment in which
residents have the opportunity to raise concerns,
report mistreatment, and provide feedback in a
confidential manner as appropriate, without fear of
intimidation or retaliation;
(Core)
II.A.4.a).(8) ensure the program’s compliance with the Sponsoring
Institution’s policies and procedures related to
grievances and due process, including when action is
taken to suspend or dismiss, or not to promote or
renew the appointment of a resident;
(Core)
Background and Intent: A program does not operate independently of its Sponsoring
Institution. It is expected that the program director will be aware of the Sponsoring
Institution’s policies and procedures, and will ensure they are followed by the
program’s leadership, faculty members, support personnel, and residents.
II.A.4.a).(9) ensure the program’s compliance with the Sponsoring
Institution’s policies and procedures on employment
and non-discrimination;
(Core)
II.A.4.a).(9).(a) Residents must not be required to sign a non-
competition guarantee or restrictive covenant.
(Core)
II.A.4.a).(10) document verification of education for all residents
within 30 days of completion of or departure from the
program;
(Core)
II.A.4.a).(11) provide verification of an individual resident’s
education upon the resident’s request, within 30 days;
and,
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 15 of 64
Background and Intent: Primary verification of graduate medical education is
important to credentialing of physicians for further training and practice. Such
verification must be accurate and timely. Sponsoring Institution and program policies
for record retention are important to facilitate timely documentation of residents who
have previously completed the program. Residents who leave the program prior to
completion also require timely documentation of their summative evaluation.
II.A.4.a).(12) provide applicants who are offered an interview with
information related to their eligibility for the relevant
specialty board examination(s).
(Core)
II.B. Faculty
Faculty members are a foundational element of graduate medical education
– faculty members teach residents how to care for patients. Faculty
members provide an important bridge allowing residents to grow and
become practice-ready, ensuring that patients receive the highest quality of
care. They are role models for future generations of physicians by
demonstrating compassion, commitment to excellence in teaching and
patient care, professionalism, and a dedication to lifelong learning. Faculty
members experience the pride and joy of fostering the growth and
development of future colleagues. The care they provide is enhanced by
the opportunity to teach and model exemplary behavior. By employing a
scholarly approach to patient care, faculty members, through the graduate
medical education system, improve the health of the individual and the
population.
Faculty members ensure that patients receive the level of care expected
from a specialist in the field. They recognize and respond to the needs of
the patients, residents, community, and institution. Faculty members
provide appropriate levels of supervision to promote patient safety. Faculty
members create an effective learning environment by acting in a
professional manner and attending to the well-being of the residents and
themselves.
Background and Intent: “Faculty” refers to the entire teaching force responsible for
educating residents. The term “faculty,” including “core faculty,” does not imply or
require an academic appointment.
II.B.1. There must be a sufficient number of faculty members with
competence to instruct and supervise all residents.
(Core)
II.B.1.a) Faculty members with credentials appropriate to the care setting
must supervise all clinical experiences.
(Core)
II.B.1.a).(1) There must be physicians with certification in internal
medicine by the ABIM or AOBIM to teach and supervise
internal medicine residents while they are on internal
medicine inpatient and outpatient rotations.
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 16 of 64
Specialty-Specific Background and Intent: The Review Committee believes the best role
models for internal medicine residents are internal medicine physicians with certification in
internal medicine from the ABIM or AOBIM. Providing such faculty members ensures
specialty-specific educators with significant experience managing and providing
comprehensive patient care to complex patients. However, the Review Committee recognizes
there are circumstances and clinical settings in which a non-internist who has been approved
by the program director would be an appropriate supervisor. Examples include but are not
limited to the following:
• On inpatient medicine ward rotations, it is appropriate for an ABFM- or AOBFP- certified
physician with extensive experience in caring for inpatient adults to teach and supervise
internal medicine residents, provided they are approved by the site director and the
program director. Working as an adult hospitalist for at least three years would be one
way to demonstrate such extensive experience.
• On inpatient medicine rotations in the critical care setting, it would be appropriate for a
non-internist who has been approved by the program director and the medical intensive
care unit director to teach and supervise internal medicine residents. For example, it
would be appropriate for emergency medicine physicians with certification in internal
medicine-critical care medicine to supervise internal medicine residents on critical care
medicine rotations. It is also appropriate for physicians with certification in critical care
from other disciplines to teach and supervise in limited circumstances, such as evening or
weekend cross-coverage.
• On outpatient medicine rotations/experiences, it is appropriate for a non-internist with
documented expertise (e.g., a family medicine physician with extensive
outpatient/ambulatory experience or procedural proficiency) to teach and supervise
internal medicine residents provided the non-internist is approved by the site director and
the program director.
II.B.1.a).(2) Physicians certified by the ABIM or the AOBIM in the
relevant subspecialty must be available to teach and
supervise internal medicine residents while they are on
internal medicine subspecialty rotations.
(Core)
II.B.1.a).(3) Physicians certified by an ABMS or AOA board in the
relevant subspecialty should be available to teach and
supervise internal medicine residents while they are on
multidisciplinary subspecialty rotations.
(Core)
Specialty-Specific Background and Intent: For example, it would be appropriate for a faculty
member certified in geriatric medicine by the ABIM, AOBIM, American Board of Family
Medicine, or American Osteopathic Board of Family Medicine to teach and supervise internal
medicine residents on geriatric medicine rotations.
II.B.1.a).(4) Physicians certified by an ABMS or AOA board in the
relevant specialty should be available to teach and
supervise internal medicine residents while they are having
non-internal medicine experiences.
(Core)
Specialty-Specific Background and Intent: For example, it would be appropriate for a faculty
member certified in neurology by the American Board of Psychiatry and Neurology or the

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 17 of 64
American Osteopathic Board of Neurology and Psychiatry to teach and supervise internal
medicine residents on neurology rotations.
II.B.2. Faculty members must:
II.B.2.a) be role models of professionalism;
(Core)
II.B.2.b) demonstrate commitment to the delivery of safe, equitable,
high-quality, cost-effective, patient-centered care;
(Core)
Background and Intent: Patients have the right to expect quality, cost-effective care
with patient safety at its core. The foundation for meeting this expectation is formed
during residency and fellowship. Faculty members model these goals and continually
strive for improvement in care and cost, embracing a commitment to the patient and
the community they serve.
II.B.2.c) demonstrate a strong interest in the education of residents,
including devoting sufficient time to the educational program
to fulfill their supervisory and teaching responsibilities;
(Core)
II.B.2.d) administer and maintain an educational environment
conducive to educating residents;
(Core)
II.B.2.e) regularly participate in organized clinical discussions,
rounds, journal clubs, and conferences; and,
(Core)
II.B.2.f) pursue faculty development designed to enhance their skills
at least annually:
(Core)
Background and Intent: Faculty development is intended to describe structured
programming developed for the purpose of enhancing transference of knowledge, skill,
and behavior from the educator to the learner. Faculty development may occur in a
variety of configurations (lecture, workshop, etc.) using internal and/or external
resources. Programming is typically needs-based (individual or group) and may be
specific to the institution or the program. Faculty development programming is to be
reported for the residency program faculty in the aggregate.
II.B.2.f).(1) as educators and evaluators;
(Detail)
II.B.2.f).(2) in quality improvement, eliminating health inequities,
and patient safety;
(Detail)
II.B.2.f).(3) in fostering their own and their residents’ well-being;
and,
(Detail)
II.B.2.f).(4) in patient care based on their practice-based learning
and improvement efforts.
(Detail)
Background and Intent: Practice-based learning serves as the foundation for the
practice of medicine. Through a systematic analysis of one’s practice and review of the

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 18 of 64
literature, one is able to make adjustments that improve patient outcomes and care.
Thoughtful consideration to practice-based analysis improves quality of care, as well
as patient safety. This allows faculty members to serve as role models for residents in
practice-based learning.
II.B.2.g) There must be a subspecialty education coordinator (SEC) in
each of the subspecialties of internal medicine and in the
multidisciplinary subspecialty of geriatric medicine.
(Core)
Specialty-Specific Background and Intent: An SEC is necessary in each of the following
subspecialties of internal medicine: cardiovascular disease; critical care medicine;
endocrinology, diabetes, and metabolism; gastroenterology; hematology; infectious disease;
nephrology; medical oncology; pulmonary disease; and rheumatology.
II.B.2.g).(1) Each SEC must be accountable to the program director for
coordination of all educational experiences in the
subspecialty area.
(Core)
II.B.2.g).(2) Each SEC must be certified in the relevant subspecialty by
the ABIM or the AOBIM, except that the geriatric medicine
SEC must be certified in the subspecialty by the relevant
ABMS member board or AOA certifying board.
(Core)
Specialty-Specific Background and Intent: SECs are responsible for developing the
educational content and curriculum for the subspecialty area. An associate program director
or core faculty member can also function as an SEC with adequate additional administrative
resources. Double-boarded SECs can act as education coordinators for two specialties (e.g.,
hematology-medical oncology and pulmonary disease-critical care medicine). The SEC for
geriatric medicine can be certified by the ABIM, the AOBIM, the American Board of Family
Medicine, or the American Osteopathic Board of Family Medicine. The Review Committee
encourages programs that cannot identify an SEC for a particular subspecialty area to
consider the option of sharing one with a program that does have one. The SEC can be
remotely located and associated with multiple residency programs.
II.B.2.h) There must be faculty members with expertise in the analysis and
interpretation of practice data, data management science and
clinical decision support systems, and managing emerging health
issues.
(Core)
Specialty-Specific Background and Intent: Advances in technology are likely to significantly
impact and redefine patient care, and this requirement is intended to ensure that residents
are provided with access to faculty members with knowledge, skills, or experience in the
analysis and interpretation of practice data, and who are able to analyze and evaluate the
validity of decisions from advanced data management and clinical decision support systems.
Faculty members with expertise in this area can be physicians or non-physicians, core or
non-core faculty members. Institutions may already have such experts assisting programs in
meeting the Common Program Requirement to systematically analyze practice data to
improve patient care [IV.B.1.d).(1).(d)]. The Review Committee encourages programs that
cannot identify an existing internal candidate with expertise in this area to consider the option

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 19 of 64
of sharing one with a program that does. The faculty member can be remotely located and
associated with multiple residency programs.
II.B.2.i) Faculty members must have experience working in
interdisciplinary, interprofessional team-based health care delivery
models.
(Core)
Specialty-Specific Background and Intent: The Review Committee believes that
interdisciplinary, interprofessional, team-based care is the foundation of care delivery.
Individuals working within such teams are essential to resident education.
II.B.3. Faculty Qualifications
II.B.3.a) Faculty members must have appropriate qualifications in
their field and hold appropriate institutional appointments.
(Core)
II.B.3.b) Physician faculty members must:
II.B.3.b).(1) have current certification in the specialty by the
American Board of Internal Medicine or the American
Osteopathic Board of Internal Medicine, or possess
qualifications judged acceptable to the Review
Committee.
(Core)
II.B.4. Core Faculty
Core faculty members must have a significant role in the education
and supervision of residents and must devote a significant portion
of their entire effort to resident education and/or administration, and
must, as a component of their activities, teach, evaluate, and
provide formative feedback to residents.
(Core)
Background and Intent: Core faculty members are critical to the success of resident
education. They support the program leadership in developing, implementing, and
assessing curriculum, mentoring residents, and assessing residents’ progress toward
achievement of competence in and the autonomous practice of the specialty. Core
faculty members should be selected for their broad knowledge of and involvement in
the program, permitting them to effectively evaluate the program. Core faculty
members may also be selected for their specific expertise and unique contribution to
the program. Core faculty members are engaged in a broad range of activities, which
may vary across programs and specialties. Core faculty members provide clinical
teaching and supervision of residents, and also participate in non-clinical activities
related to resident education and program administration. Examples of these non-
clinical activities include, but are not limited to, interviewing and selecting resident
applicants, providing didactic instruction, mentoring residents, simulation exercises,
completing the annual ACGME Faculty Survey, and participating on the program’s
Clinical Competency Committee, Program Evaluation Committee, and other GME
committees.

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 20 of 64
II.B.4.a) Core faculty members must complete the annual ACGME
Faculty Survey.
(Core)
II.B.4.b) In addition to the program director and associate program
director(s), programs must have the minimum number of ABIM- or
AOBIM-certified core faculty members based on the number of
approved resident positions, as follows.
(Core)
II.B.4.c) At a minimum, the required core faculty members, in aggregate
and excluding program leadership, must be provided with support
equal to an average dedicated minimum of 0.1 FTE for
educational and administrative responsibilities that do not involve
direct patient care.
(Core)
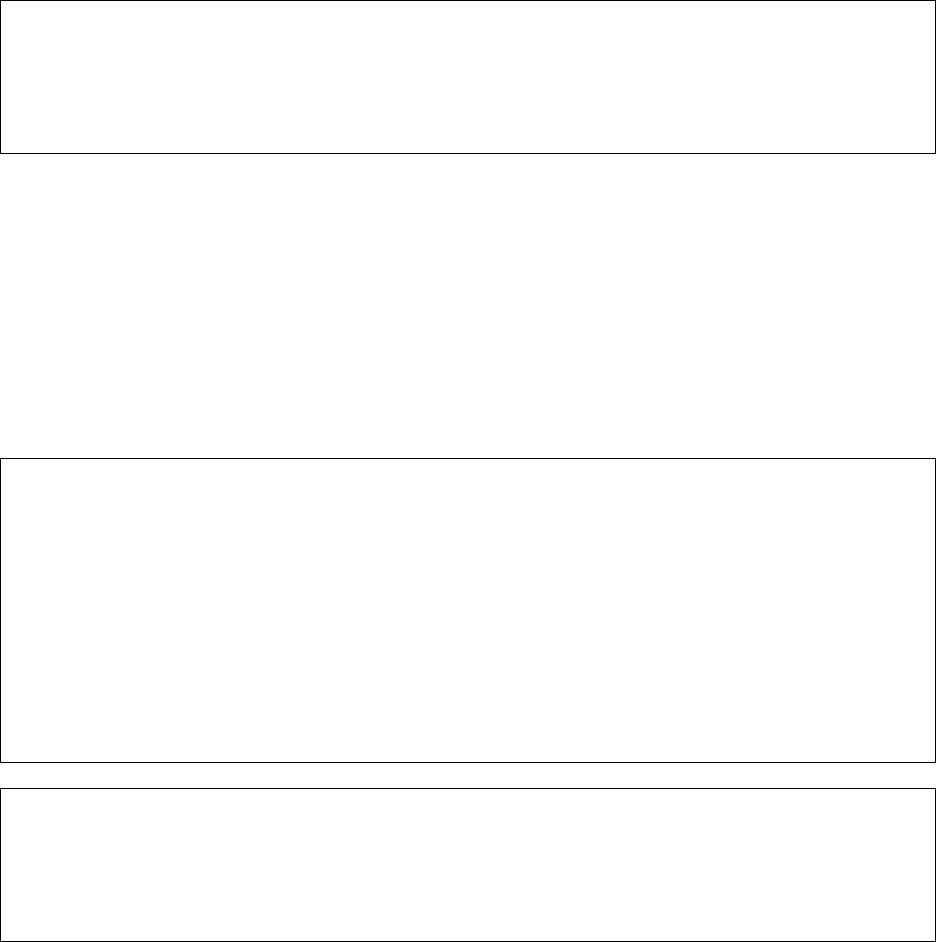
Number of Approved
Resident Positions
Minimum Number of
ABIM- or AOBIM-
certified Core Faculty
Members
<30
3
30-39
4
40-49
5
50-59
6
60-69
7
70-79
8
80-89
9
90-99
10
100-109
11
110-119
12
120-129
13
130-139
14
140-149
15
150-159
16
160-169
17
170-179
18
180-189
19
190-199
20
200-209
21
Specialty-Specific Background and Intent: The Review Committee specified the minimum
required number of ABIM- or AOBIM-certified internal medicine core faculty, but did not
specify how the aggregate FTE support should be distributed to allow programs, in
partnership with their sponsoring institution, to allocate the support as they see fit. For
instance, a program with an approved complement of 36 residents is required to have a
minimum of four ABIM- or AOBIM-certified core faculty members and a minimum aggregate
FTE of 40 percent. The program could choose to operationalize this as four ABIM- or AOBIM-
certified faculty members each with 10 percent FTE support, but it could also have eight
members each with five percent FTE support, or one member with twenty percent FTE and
four members with five percent each.

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 21 of 64
The duties of the program director, associate program director(s), and internal medicine core
faculty members are separate and distinct. As such, the minimum required internal medicine
core faculty members are in addition to the program director and the associate program
director(s). One individual cannot “count” as both an associate program director and internal
medicine core faculty member.
The requirement related to support for core internal medicine faculty members is intended to
ensure these faculty members have sufficient protected time to meet the following
educational responsibilities:
• Membership on the Clinical Competency Committee
• Participation in the annual program review as Chair or member of the Program
Evaluation Committee
• Implementation and analysis of the outcome of action plans developed by the
Program Evaluation Committee
• Significant participation in recruitment and selection, including efforts related to the
program’s commitment to diversity
• Advising, mentoring, and coaching residents (co-creating, implementing, and
monitoring individualized learning plans)
• Designing and overseeing remediation plans
• Supporting/overseeing residents in the development/assessment of quality
improvement/patient safety projects
• Supporting/overseeing residents in the conduct of their scholarly work, including the
dissemination of such work through presentations, posters/abstracts, and peer-
reviewed publications
• Significant participation in educational activities (didactics, lab, or simulation)
• Overseeing faculty development for the program’s faculty members
• Designing and implementing simulation and/or standardized patients for teaching and
assessment
• Developing, implementing, and assessing one or more of the major components of the
curriculum, such as patient safety, quality, health disparities, or core didactics
• Designing and implementing the program’s assessment strategies, making certain
there are robust methods used to assess each competency, and ensuring they
provide meaningful information by which the Clinical Competency Committee can
judge resident performance on the Milestones
• Leading the program’s efforts related to resident and faculty member well-being
Each core faculty member does not need to participate in every listed educational
responsibility.
Background and Intent: Provision of support for the time required for the core faculty
members’ responsibilities related to resident education and/or administration of the
program, as well as flexibility regarding how this support is provided, are important.
Programs, in partnership with their Sponsoring Institutions, may provide support for
this time in a variety of ways. Examples of support may include, but are not limited to,
salary support, supplemental compensation, educational value units, or relief of time
from other professional duties.
It is important to remember that the dedicated time and support requirement is a
minimum, recognizing that, depending on the unique needs of the program, additional

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 22 of 64
support may be warranted. The need to ensure adequate resources, including
adequate support and dedicated time for the core faculty members, is also addressed
in Institutional Requirement II.B.2. The amount of support and dedicated time needed
for individual programs will vary based on a number of factors and may exceed the
minimum specified in the applicable specialty-/ subspecialty-specific Program
Requirements.
II.B.5. Associate Program Directors
Associate program directors assist the program director in the
administrative and clinical oversight of the educational program.
II.B.5.a) Associate program directors must:
II.B.5.a).(1) have current certification from the ABIM or AOBIM in either
internal medicine or a subspecialty of internal medicine;
(Core)
II.B.5.a).(2) report directly to the program director;
(Core)
II.B.5.a).(3) participate in academic societies and in educational
programs designed to enhance their educational and
administrative skills; and,
(Core)
II.B.5.a).(4) take an active role in curriculum development, resident
teaching and evaluation, continuous program
improvement, and faculty development.
(Core)
II.C. Program Coordinator
II.C.1. There must be a program coordinator.
(Core)
II.C.2. The program coordinator must be provided with dedicated time and
support adequate for administration of the program based upon its
size and configuration.
(Core)
II.C.2.a) At a minimum, the program coordinator must be provided with the
dedicated time and support specified below for administration of
the program. Additional administrative support must be provided
based on the program size as follows:
(Core
)
Number of Approved
Resident Positions
Minimum FTE Required
for Coordinator Support
Additional Aggregate FTE
Required for Administration
of the Program
<7
0.5
0
7-10
0.5
0.2
10-15
0.5
0.3
16-20
0.5
0.4
21-25
0.5
0.5
26-30
0.5
0.6

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 23 of 64
Number of Approved
Resident Positions
Minimum FTE Required
for Coordinator Support
Additional Aggregate FTE
Required for Administration
of the Program
31-35
0.5
0.7
36-40
0.5
0.8
41-45
0.5
0.9
46-50
0.5
1.0
51-55
0.5
1.1
56-60
0.5
1.2
61-65
0.5
1.3
66-70
0.5
1.4
71-75
0.5
1.5
76-80
0.5
1.6
81-85
0.5
1.7
86-90
0.5
1.8
91-95
0.5
1.9
96-100
0.5
2.0
101-105
0.5
2.1
106-110
0.5
2.2
111-115
0.5
2.3
116-120
0.5
2.4
121-125
0.5
2.5
126-130
0.5
2.6
131-135
0.5
2.7
136-140
0.5
2.8
141-145
0.5
2.9
146-150
0.5
3.0
151-155
0.5
3.1
156-160
0.5
3.2
161-165
0.5
3.3
166-170
0.5
3.4
171-175
0.5
3.5
176-180
0.5
3.6
181-185
0.5
3.7
186-190
0.5
3.8
191-195
0.5
3.9
196-200
0.5
4.0
201-205
0.5
4.1
206-210
0.5
4.2
211-215
0.5
4.3
216-220
0.5
4.4
221-225
0.5
4.5
226-230
0.5
4.6
Background and Intent: The requirement does not address the source of funding
required to provide the specified salary support.

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 24 of 64
Each program requires a lead administrative person, frequently referred to as a
program coordinator, administrator, or as otherwise titled by the institution. This
person will frequently manage the day-to-day operations of the program and serve as
an important liaison and facilitator between the learners, faculty and other staff
members, and the ACGME. Individuals serving in this role are recognized as program
coordinators by the ACGME.
The program coordinator is a key member of the leadership team and is critical to the
success of the program. As such, the program coordinator must possess skills in
leadership and personnel management appropriate to the complexity of the program.
Program coordinators are expected to develop in-depth knowledge of the ACGME and
Program Requirements, including policies and procedures. Program coordinators
assist the program director in meeting accreditation requirements, educational
programming, and support of residents.
Programs, in partnership with their Sponsoring Institutions, should encourage the
professional development of their program coordinators and avail them of
opportunities for both professional and personal growth. Programs with fewer
residents may not require a full-time coordinator; one coordinator may support more
than one program.
The minimum required dedicated time and support specified in II.C.2.a) is inclusive of
activities directly related to administration of the accredited program. It is understood
that coordinators often have additional responsibilities, beyond those directly related
to program administration, including, but not limited to, departmental administrative
responsibilities, medical school clerkships, planning lectures that are not solely
intended for the accredited program, and mandatory reporting for entities other than
the ACGME. Assignment of these other responsibilities will necessitate consideration
of allocation of additional support so as not to preclude the coordinator from devoting
the time specified above solely to administrative activities that support the accredited
program.
In addition, it is important to remember that the dedicated time and support
requirement for ACGME activities is a minimum, recognizing that, depending on the
unique needs of the program, additional support may be warranted. The need to
ensure adequate resources, including adequate support and dedicated time for the
program coordinator, is also addressed in Institutional Requirement II.B.4. The amount
of support and dedicated time needed for individual programs will vary based on a
number of factors and may exceed the minimum specified in the applicable
specialty/subspecialty-specific Program Requirements. It is expected that the
Sponsoring Institution, in partnership with its accredited programs, will ensure support
for program coordinators to fulfill their program responsibilities effectively.
Specialty-Specific Background and Intent: For instance, a program with an approved
complement of 36 residents is required to have 130 percent FTE for coordinator support. The
Review Committee decided not to specify how the support should be distributed to allow
programs, in partnership with their Sponsoring Institution, to allocate the support as they see
fit.

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 25 of 64
II.D. Other Program Personnel
The program, in partnership with its Sponsoring Institution, must jointly
ensure the availability of necessary personnel for the effective
administration of the program.
(Core)
Background and Intent: Multiple personnel may be required to effectively administer a
program. These may include staff members with clerical skills, project managers,
education experts, and staff members to maintain electronic communication for the
program. These personnel may support more than one program in more than one
discipline.
III. Resident Appointments
III.A. Eligibility Requirements
III.A.1. An applicant must meet one of the following qualifications to be
eligible for appointment to an ACGME-accredited program:
(Core)
III.A.1.a) graduation from a medical school in the United States or
Canada, accredited by the Liaison Committee on Medical
Education (LCME) or graduation from a college of
osteopathic medicine in the United States, accredited by the
American Osteopathic Association Commission on
Osteopathic College Accreditation (AOACOCA); or,
(Core)
III.A.1.b) graduation from a medical school outside of the United
States or Canada, and meeting one of the following additional
qualifications:
(Core)
III.A.1.b).(1) holding a currently valid certificate from the
Educational Commission for Foreign Medical
Graduates (ECFMG) prior to appointment; or,
(Core)
III.A.1.b).(2) holding a full and unrestricted license to practice
medicine in the United States licensing jurisdiction in
which the ACGME-accredited program is located.
(Core)
III.A.2. All prerequisite post-graduate clinical education required for initial
entry or transfer into ACGME-accredited residency programs must
be completed in ACGME-accredited residency programs, AOA-
approved residency programs, Royal College of Physicians and
Surgeons of Canada (RCPSC)-accredited or College of Family
Physicians of Canada (CFPC)-accredited residency programs
located in Canada, or in residency programs with ACGME
International (ACGME-I) Advanced Specialty Accreditation.
(Core)
III.A.2.a) Residency programs must receive verification of each
resident’s level of competency in the required clinical field
using ACGME, CanMEDS, or ACGME-I Milestones evaluations
from the prior training program upon matriculation.
(Core)
Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 26 of 64
Background and Intent: Programs with ACGME-I Foundational Accreditation or from
institutions with ACGME-I accreditation do not qualify unless the program has also
achieved ACGME-I Advanced Specialty Accreditation. To ensure entrants into ACGME-
accredited programs from ACGME-I programs have attained the prerequisite
milestones for this training, they must be from programs that have ACGME-I Advanced
Specialty Accreditation.
III.B. Resident Complement
The program director must not appoint more residents than approved by
the Review Committee.
(Core)
III.B.1.a) There must be a sufficient number of residents to allow peer-to-
peer interaction and learning.
(Core)
III.B.1.a).(1) The program should offer a minimum of nine positions.
(Detail)
Specialty-Specific Background and Intent: The Review Committee believes that peer-to-peer
interactions and learning are extremely important components of residency education and
has set the minimum number of residents to nine. While three residents per educational year
is suggested, it is not required as long as there is relative balance per level. To ensure that
resident education is not compromised by having too few residents, the number of residents
in a program will be monitored at each review, particularly for those programs with significant
decreases in complement. However, this requirement is categorized as a “detail” as there
may be programs that have specific circumstances that allow them to function with a smaller
resident complement. This categorization allows the establishment of residency education
programs in rural and medically underserved areas and populations when the Review
Committee determines that the program has sufficient resources to ensure substantial
compliance with accreditation requirements.
Background and Intent: Programs are required to request approval of all complement
changes, whether temporary or permanent, by the Review Committee through ADS.
Permanent increases require prior approval from the Review Committee and temporary
increases may also require approval. Specialty-specific instructions for requesting a
complement increase are found in the “Documents and Resources” page of the
applicable specialty section of the ACGME website.
III.C. Resident Transfers
The program must obtain verification of previous educational experiences
and a summative competency-based performance evaluation prior to
acceptance of a transferring resident, and Milestones evaluations upon
matriculation.
(Core)
IV. Educational Program

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 27 of 64
The ACGME accreditation system is designed to encourage excellence and
innovation in graduate medical education regardless of the organizational
affiliation, size, or location of the program.
The educational program must support the development of knowledgeable, skillful
physicians who provide compassionate care.
It is recognized that programs may place different emphasis on research,
leadership, public health, etc. It is expected that the program aims will reflect the
nuanced program-specific goals for it and its graduates; for example, it is
expected that a program aiming to prepare physician-scientists will have a
different curriculum from one focusing on community health.
IV.A. Educational Components
The curriculum must contain the following educational components:
IV.A.1. a set of program aims consistent with the Sponsoring Institution’s
mission, the needs of the community it serves, and the desired
distinctive capabilities of its graduates, which must be made
available to program applicants, residents, and faculty members;
(Core)
IV.A.2. competency-based goals and objectives for each educational
experience designed to promote progress on a trajectory to
autonomous practice. These must be distributed, reviewed, and
available to residents and faculty members;
(Core)
Background and Intent: The trajectory to autonomous practice is documented by
Milestones evaluations. Milestones are considered formative and should be used to
identify learning needs. Milestones data may lead to focused or general curricular
revision in any given program or to individualized learning plans for any specific
resident.
IV.A.3. delineation of resident responsibilities for patient care, progressive
responsibility for patient management, and graded supervision;
(Core)
Background and Intent: These responsibilities may generally be described by PGY
level and specifically by Milestones progress as determined by the Clinical
Competency Committee. This approach encourages the transition to competency-
based education. An advanced learner may be granted more responsibility
independent of PGY level and a learner needing more time to accomplish a certain task
may do so in a focused rather than global manner.
IV.A.4. a broad range of structured didactic activities; and,
(Core)
IV.A.4.a) Residents must be provided with protected time to participate
in core didactic activities.
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 28 of 64
Background and Intent: It is intended that residents will participate in structured
didactic activities. It is recognized that there may be circumstances in which this is not
possible. Programs should define core didactic activities for which time is protected
and the circumstances in which residents may be excused from these didactic
activities. Didactic activities may include, but are not limited to, lectures, conferences,
courses, labs, asynchronous learning, simulations, drills, case discussions, grand
rounds, didactic teaching, and education in critical appraisal of medical evidence.
IV.A.5. formal educational activities that promote patient safety-related
goals, tools, and techniques.
(Core)
IV.B. ACGME Competencies
Background and Intent: The Competencies provide a conceptual framework describing
the required domains for a trusted physician to enter autonomous practice. These
Competencies are core to the practice of all physicians, although the specifics are
further defined by each specialty. The developmental trajectories in each of the
Competencies are articulated through the Milestones for each specialty.
IV.B.1. The program must integrate the following ACGME Competencies
into the curriculum:
IV.B.1.a) Professionalism
Residents must demonstrate a commitment to
professionalism and an adherence to ethical principles.
(Core)
IV.B.1.a).(1) Residents must demonstrate competence in:
IV.B.1.a).(1).(a) compassion, integrity, and respect for others;
(Core)
IV.B.1.a).(1).(b) responsiveness to patient needs that
supersedes self-interest;
(Core)
IV.B.1.a).(1).(c) cultural humility;
(Core)
IV.B.1.a).(1).(d) respect for patient privacy and autonomy;
(Core)
IV.B.1.a).(1).(e) accountability to patients, society, and the
profession;
(Core)
IV.B.1.a).(1).(f) respect and responsiveness to diverse patient
populations, including but not limited to
diversity in gender, age, culture, race, religion,
disabilities, national origin, socioeconomic
status, and sexual orientation;
(Core)
IV.B.1.a).(1).(g) ability to recognize and develop a plan for one’s
own personal and professional well-being; and,
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 29 of 64
IV.B.1.a).(1).(h) appropriately disclosing and addressing
conflict or duality of interest.
(Core)
Background and Intent: This includes the recognition that under certain
circumstances, the interests of the patient may be best served by transitioning care to
another practitioner. Examples include fatigue, conflict or duality of interest, not
connecting well with a patient, or when another physician would be better for the
situation based on skill set or knowledge base.
IV.B.1.b) Patient Care and Procedural Skills
Background and Intent: Quality patient care is safe, effective, timely, efficient, patient-
centered, equitable, and designed to improve population health, while reducing per
capita costs. In addition, there should be a focus on improving the clinician’s well-
being as a means to improve patient care and reduce burnout among residents,
fellows, and practicing physicians.
IV.B.1.b).(1) Residents must be able to provide patient care that is
patient- and family-centered, compassionate,
equitable, appropriate, and effective for the treatment
of health problems and the promotion of health.
(Core)
IV.B.1.b).(1).(a) Residents must demonstrate the ability to manage
the care of patients:
IV.B.1.b).(1).(a).(i) using clinical skills of interviewing and
physical examination;
(Core)
IV.B.1.b).(1).(a).(ii) in a variety of roles within a health system
with progressive responsibility, including
serving as the direct provider, a member, or
leader of an interprofessional team of
providers; as a consultant to other
physicians; and as a teacher to the patient,
the patient’s family, and other health care
workers;
(Core)
IV.B.1.b).(1).(a).(iii) including the prevention, counseling,
detection, diagnosis, and treatment of adult
diseases;
(Core)
IV.B.1.b).(1).(a).(iv) in a variety of health care settings, including
the inpatient ward, critical care units, and
various ambulatory settings;
(Core)
Specialty-Specific Background and Intent: Emerging models of care and needs of populations
served by programs will result in residents having educational experiences in novel or non-
traditional settings. Examples of non-traditional educational settings include rotations on

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 30 of 64
mobile buses that travel to areas of increased need, and “pop-up” health clinics within
community centers.
IV.B.1.b).(1).(a).(v) for whom they have limited or no physical
contact, through the use of telemedicine;
(Core)
IV.B.1.b).(1).(a).(vi) in the subspecialties of internal medicine;
(Core)
IV.B.1.b).(1).(a).(vii) using population-based data;
(Core)
Specialty-Specific Background and Intent: Understanding population health within the context
of prevention is an important competency for the physician practicing medicine in the future.
Residents need experience using, understanding, and analyzing population health data so
that they can develop health care plans to improve health outcomes for their patients. For
instance, residents may be provided experience in analyzing and interpreting data from health
registries, and understanding the local impact of infectious and non-infectious epidemics
(e.g., obesity or opioid) and pandemics, and the important role social determinants of health
have when developing and applying health care and preventive care decisions.
IV.B.1.b).(1).(a).(viii) using critical thinking and evidence-based
tools.
(Core)
IV.B.1.b).(2) Residents must be able to perform all medical,
diagnostic, and surgical procedures considered
essential for the area of practice.
(Core)
IV.B.1.b).(2).(a) Residents must demonstrate the ability to:
IV.B.1.b).(2).(a).(i) use and/or perform point-of-care laboratory,
diagnostic, and/or imaging studies relevant
to the care of the patient;
(Core)
Specialty-Specific Background and Intent: The Review Committee intentionally did not identify
specific laboratory, diagnostic, and/or imaging studies that residents must perform because it
believes that scientific advances will be constant and ongoing, and whatever is codified in the
requirements quickly becomes outdated. Additionally, the decision to not specifically denote
studies in the requirements aligns with the Committee’s overall position that residents should
perform and develop expertise with those procedures appropriate to their future practice
needs, as noted in the requirement below. However, the Committee acknowledges that
offering point-of-care ultrasonography to residents who believe this will be relevant for their
future career practice may be one way to meet the above-mentioned requirement.
IV.B.1.b).(2).(a).(ii) perform diagnostic and therapeutic
procedures relevant to their specific career
paths; and,
(Core)
IV.B.1.b).(2).(a).(iii) treat their patients’ conditions with practices
that are patient-centered, safe, scientifically

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 31 of 64
based, effective, timely, and cost-effective.
(Core)
IV.B.1.c) Medical Knowledge
Residents must demonstrate knowledge of established and
evolving biomedical, clinical, epidemiological, and social-
behavioral sciences, including scientific inquiry, as well as
the application of this knowledge to patient care.
(Core)
IV.B.1.c).(1) Residents must demonstrate a level of expertise in the
knowledge of the broad spectrum of clinical disorders seen
by an internist, including:
(Core)
IV.B.1.c).(1).(a) the core content of general internal medicine, which
includes the internal medicine subspecialties, the
multidisciplinary subspecialties of geriatric
medicine, hospice and palliative medicine and
addiction medicine, and neurology.
(Core)
IV.B.1.c).(2) Residents must demonstrate sufficient knowledge in the
following areas:
IV.B.1.c).(2).(a) evaluation of patients with an undiagnosed and
undifferentiated presentation;
(Core)
IV.B.1.c).(2).(b) pharmacotherapeutic and non-
pharmacotherapeutic treatment of the broad
spectrum of medical conditions and clinical
disorders managed by internists;
(Core)
IV.B.1.c).(2).(c) provision of preventive care;
(Core)
IV.B.1.c).(2).(d) interpretation of clinical tests and images;
(Core)
IV.B.1.c).(2).(e) recognition and initial management of urgent
medical problems; and,
(Core)
IV.B.1.c).(2).(f) application of technology appropriate for the clinical
context, including evolving techniques.
(Core)
Specialty-Specific Background and Intent: Advances in technology will likely continue to make
substantive changes in patient diagnosis and management. This requirement ensures that
residents will be able to gain experience and become familiar with emerging technologies,
such as intensive care units managed remotely or the use of personalized or precision
medicine.
IV.B.1.d) Practice-based Learning and Improvement
Residents must demonstrate the ability to investigate and
evaluate their care of patients, to appraise and assimilate
Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 32 of 64
scientific evidence, and to continuously improve patient care
based on constant self-evaluation and lifelong learning.
(Core)
IV.B.1.d).(1) Residents must demonstrate competence in:
IV.B.1.d).(1).(a) identifying strengths, deficiencies, and limits in
one’s knowledge and expertise;
(Core)
IV.B.1.d).(1).(b) setting learning and improvement goals;
(Core)
IV.B.1.d).(1).(c) identifying and performing appropriate learning
activities;
(Core)
IV.B.1.d).(1).(d) systematically analyzing practice using quality
improvement methods, including activities
aimed at reducing health care disparities, and
implementing changes with the goal of practice
improvement;
(Core)
IV.B.1.d).(1).(e) incorporating feedback and formative
evaluation into daily practice; and,
(Core)
IV.B.1.d).(1).(f) locating, appraising, and assimilating evidence
from scientific studies related to their patients’
health problems.
(Core)
IV.B.1.e) Interpersonal and Communication Skills
Residents must demonstrate interpersonal and
communication skills that result in the effective exchange of
information and collaboration with patients, their families,
and health professionals.
(Core)
IV.B.1.e).(1) Residents must demonstrate competence in:
IV.B.1.e).(1).(a) communicating effectively with patients and
patients’ families, as appropriate, across a
broad range of socioeconomic circumstances,
cultural backgrounds, and language
capabilities, learning to engage interpretive
services as required to provide appropriate care
to each patient;
(Core)
IV.B.1.e).(1).(b) communicating effectively with physicians,
other health professionals, and health-related
agencies;
(Core)
IV.B.1.e).(1).(c) working effectively as a member or leader of a
health care team or other professional group;
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 33 of 64
IV.B.1.e).(1).(d) educating patients, patients’ families, students,
other residents, and other health professionals;
(Core)
IV.B.1.e).(1).(e) acting in a consultative role to other physicians
and health professionals;
(Core)
IV.B.1.e).(1).(f) maintaining comprehensive, timely, and legible
health care records, if applicable.
(Core)
IV.B.1.e).(2) Residents must learn to communicate with patients
and patients’ families to partner with them to assess
their care goals, including, when appropriate, end-of-
life goals.
(Core)
IV.B.1.f) Systems-based Practice
Residents must demonstrate an awareness of and
responsiveness to the larger context and system of health
care, including the structural and social determinants of
health, as well as the ability to call effectively on other
resources to provide optimal health care.
(Core)
Background and Intent: Medical practice occurs in the context of an increasingly
complex clinical care environment where optimal patient care requires attention to
compliance with external and internal administrative and regulatory requirements.
IV.B.1.f).(1) Residents must demonstrate competence in:
IV.B.1.f).(1).(a) working effectively in various health care
delivery settings and systems relevant to their
clinical specialty;
(Core)
IV.B.1.f).(1).(b) coordinating patient care across the health care
continuum and beyond as relevant to their
clinical specialty;
(Core)
Background and Intent: Every patient deserves to be treated as a whole person.
Therefore it is recognized that any one component of the health care system does not
meet the totality of the patient's needs. An appropriate transition plan requires
coordination and forethought by an interdisciplinary team. The patient benefits from
proper care and the system benefits from proper use of resources.
IV.B.1.f).(1).(c) advocating for quality patient care and optimal
patient care systems;
(Core)
IV.B.1.f).(1).(d) participating in identifying system errors and
implementing potential systems solutions;
(Core)
IV.B.1.f).(1).(e) incorporating considerations of value, equity,
cost awareness, delivery and payment, and

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 34 of 64
risk-benefit analysis in patient and/or
population-based care as appropriate;
(Core)
IV.B.1.f).(1).(f) understanding health care finances and its
impact on individual patients’ health decisions;
and,
(Core)
IV.B.1.f).(1).(g) using tools and techniques that promote patient
safety and disclosure of patient safety events
(real or simulated).
(Detail)
IV.B.1.f).(2) Residents must learn to advocate for patients within
the health care system to achieve the patient's and
patient’s family's care goals, including, when
appropriate, end-of-life goals.
(Core)
IV.C. Curriculum Organization and Resident Experiences
IV.C.1. The curriculum must be structured to optimize resident educational
experiences, the length of the experiences, and the supervisory
continuity. These educational experiences include an appropriate
blend of supervised patient care responsibilities, clinical teaching,
and didactic educational events.
(Core)
IV.C.1.a) Rotations must be of sufficient length to provide longitudinal
relationships with faculty members to allow for meaningful
assessment and feedback.
(Core)
IV.C.1.b) Rotations must be structured to allow residents to function as part
of effective interprofessional teams that work together towards the
shared goals of patient safety and quality improvement.
(Core)
IV.C.1.c) Rotations must be structured to minimize conflicting inpatient and
outpatient responsibilities.
(Core)
Background and Intent: In some specialties, frequent rotational transitions, inadequate
continuity of faculty member supervision, and dispersed patient locations within the
hospital have adversely affected optimal resident education and effective team-based
care. The need for patient care continuity varies from specialty to specialty and by
clinical situation, and may be addressed by the individual Review Committee.
Specialty-Specific Background and Intent: The Review Committee encourages programs to
think of ways to balance the inherent conflicts between inpatient and outpatient
responsibilities, including using an effective hand-off process. For example, programs may
want to consider schedules that allow members of the interprofessional health care team to
provide coverage for the inpatient service when residents are in continuity clinics.
Alternatively, programs may consider creating schedules that either provide more continuity
clinic experiences or an exclusive continuity clinic experience when residents are not on
inpatient rotations to allow them to have less or no clinic during inpatient rotations.

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 35 of 64
IV.C.2. The program must provide instruction and experience in pain
management if applicable for the specialty, including recognition of
the signs of substance use disorder.
(Core)
IV.C.3. The educational program for all residents must include:
(Core)
IV.C.3.a) at least 30 months of clinical experiences;
(Core)
IV.C.3.b) a longitudinal team-based continuity experience for the duration of
the program;
(Core)
IV.C.3.c) foundational experience in internal medicine, including:
IV.C.3.c).(1) at least 10 months of clinical experiences in the outpatient
setting;
(Core)
Specialty-Specific Background and Intent: Clinical experiences in the following settings may
be used to fulfill this requirement: general internal medicine continuity clinics; internal
medicine subspecialty clinics (e.g., HIV clinic); non-medicine clinics (e.g., dermatology or
physical medicine and rehabilitation clinic); walk-in clinics; neighborhood health clinics; home
care visit programs; urgent care clinics; and ambulatory block rotations.
Time devoted to the longitudinal continuity experience can count towards the minimum
required 10 months of foundational experiences in the outpatient setting. For the purposes of
this calculation, a month is equivalent to four weeks, 20 days, or 40 half-days. For example,
40 half-day continuity clinic sessions would equal one month of outpatient experience.
IV.C.3.c).(2) at least 10 months of clinical experiences in the inpatient
and critical care settings;
(Core)
IV.C.3.c).(2).(a) Critical care experiences must be a minimum of two
months and a maximum of six months and must not
occur solely in the PGY-1.
(Core)
IV.C.3.c).(3) clinical experiences in each of the internal medicine
subspecialties; and,
(Core)
Specialty-Specific Background and Intent: Clinical experiences in the each of the
subspecialties can be used to fulfill either the minimum required number of months in the
inpatient or outpatient setting, depending on the setting the experience is provided. For
instance, a month rotation on a hematology-oncology service would count towards meeting
the inpatient minimums whereas a month in an oncology clinic would count towards
outpatient.
IV.C.3.c).(4) clinical experiences in geriatric medicine, hospice and
palliative medicine, addiction medicine, emergency
medicine, and neurology.
(Core)
IV.C.3.d) at least six months of individualized educational experiences to
participate in opportunities relevant to their future practice or to

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 36 of 64
further skill/competency development in the foundational areas.
(Core)
Specialty-Specific Background and Intent: The Review Committee views these four
components of internal medicine residency (at least 30 months of clinical experience,
longitudinal continuity experience, foundational internal medicine experience, and at least six
months of individualized experience) as distinct but overlapping. For example, the longitudinal
continuity experience could be obtained through discrete blocks or interspersed among other
clinical experiences. Time in an outpatient clinic may be part of the continuity experience or
may be part of a subspecialty experience, or both, and it would count towards the minimum
for both foundational outpatient experience and the 30 months of clinical experience.
Additional time in that clinic may be part of a resident’s individualized learning experiences,
which would also count towards the 30-month minimum. The six months of individualized
learning experiences may be all clinical experiences that would count towards the 30-month
minimum, or they may include non-clinical experiences.
The requirements acknowledge that in addition to providing residents with broad foundational
educational experiences in ambulatory and hospital-based internal medicine, programs must
ensure residents have educational experiences that take into account their future plans and
the different paces and trajectories at and on which residents will learn and demonstrate
competence in the foundational areas.
Individualized educational experiences will be determined by the program director and take
into account demonstrated competence in the foundational areas noted above, resources,
program aims, and the residents’ future practice plans. Although six months can be devoted
to individualized experiences, some residents may require more time to achieve competence
in the foundational educational areas, which may result in less time for individualized
educational experiences. Some residents may need to devote the entirety of residency to
achieve competence in the foundational areas. The converse may be possible. Programs
may have the opportunity to allocate more than six months of individualized educational
opportunities for residents who have achieved or are on target to achieve competence in the
foundational areas. These opportunities may include more ambulatory/outpatient experiences
for residents interested in practicing in an outpatient setting after residency, more inpatient
experiences for those interested in hospitalist medicine careers, or more experiences in a
subspecialty for those interested in subspecializing. Individualized educational experiences
may be integrated throughout the 36 months of the educational program and do not need to
be consecutive.
The Review Committee is interested in programs pursuing innovations in internal medicine
training. Additional information on the development of the Program Requirements and the
Review Committee’s interest in exploring innovative proposals that will guide future versions
of the Program Requirements can be found on the Internal Medicine section of the ACGME
website.
IV.C.4. While on inpatient rotations:
IV.C.4.a) residents' responsibilities must be limited to patients for whom the
teaching team has diagnostic and therapeutic responsibility;
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 37 of 64
IV.C.4.b) programs must monitor and limit the number of resident-attending
relationships to ensure that communication and education is not
compromised;
(Core)
IV.C.4.c) non-physician faculty members must not supervise internal
medicine residents on inpatient rotations;
(Core)
Specialty-Specific Background and Intent: While it is important for residents to acquire
experience in leading and participating in interprofessional, interdisciplinary health care
teams, the overall supervision of all clinical care provided by residents is the responsibility of
the members of the physician faculty. A physician faculty member may delegate an
appropriately qualified non-physician to assist a resident in discrete activities, such as
performing procedures.
IV.C.4.d) residents from other specialties must not supervise internal
medicine residents on any internal medicine inpatient rotation;
(Core)
IV.C.4.e) the resident team and each attending physician must have the
responsibility to make management rounds on their patients and
communicate effectively with each other at a frequency
appropriate to the changing care needs of the patients;
(Core)
IV.C.4.f) residents must write all orders for patients
under their care, with
appropriate supervision by the attending physician;
(Core)
IV.C.4.f).(1) In those circumstances when another attending physician
or consultant writes an order on a resident's patient, the
attending or consultant must communicate the action to the
resident in a timely manner.
(Core)
IV.C.4.g) PGY-1 residents must not be assigned more than five new
patients per admitting day;
(Core)
IV.C.4.g).(1) an additional two patients may be assigned if they are in-
house transfers from the medical services.
(Core)
IV.C.4.h) PGY-1 residents must not be assigned more than eight new
patients in a 48-hour period;
(Core)
IV.C.4.i) PGY-1 residents must not be responsible for the ongoing care of
more than 10 patients;
(Core)
IV.C.4.j) when supervising more than one PGY-1 resident, the PGY-2 or
PGY-3 supervising resident must not be responsible for the
supervision or admission of more than 10 new patients and four
transfer patients per admitting day or more than 16 new patients in
a 48-hour period;
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 38 of 64
IV.C.4.k) when supervising one PGY-1 resident, the PGY-2 or PGY-3
supervising resident must not be responsible for the ongoing care
of more than 14 patients; and,
(Core)
IV.C.4.l) when supervising more than one PGY-1 resident, the PGY-2 or
PGY-3 supervising resident must not be responsible for the
ongoing care of more than 20 patients.
(Core)
Specialty-Specific Background and Intent: The Review Committee cannot prescriptively and
explicitly assign patient census limits for every possible educational scenario or circumstance
given the variability in these settings and the complexity and acuity of the patients. Instead,
the committee asks program and institutional leadership teams to proactively and regularly
monitor the census, complexity, and acuity of patients assigned to resident-comprised health
care teams, and the structure and composition of the team, particularly the knowledge, skills,
and abilities of the team members, to determine the appropriate patient team size for the
situation. Although the Review Committee limits the number of new patients PGY-2 and PGY-
3 residents can be assigned per admitting day (Program Requirements IV.C.4. j)-l)), programs
can exercise flexibility and deviate from these limits for PGY-3 residents who have significant
experience in the inpatient setting and are interested in hospitalist medicine careers in the
future. The leadership team will need to carefully review institutional patient safety outcome
data when determining patient census team limits in such scenarios. The census limits noted
above apply to all inpatient experiences during the 36 months of supervised graduate medical
education regardless of whether an inpatient rotation is part of the foundational educational
experiences in internal medicine or part of the individualized experiences.
IV.C.5. While on outpatient rotations:
IV.C.5.a) residents must have clinical experiences in chronic disease
management, preventive health, patient counseling, and common
acute ambulatory problems; and,
(Core)
IV.C.5.b) residents must have a longitudinal, team-based, continuity
experience for the duration of the educational program through
which they develop a long-term therapeutic relationship with a
panel of patients.
(Core)
Specialty-Specific Background and Intent: The Review Committee believes that residents can
only achieve a long-term therapeutic relationship with a panel of patients if the continuity clinic
experience takes place for the entirety of the educational program. This will allow patients to
understand that the resident is “their” primary care doctor, and residents to see the continuity
clinic patients as “their” patients. While new patients will be added to the panel (and others
will leave) throughout the course of the program, the Review Committee suggests that
residents will remain in the same clinic throughout the 36 months to maintain continuity of
care for their patient panel.
The committee believes this requirement can be best met through assigning residents to a
general internal medicine clinic. However, to allow for residents to pursue post-residency
interests during residency, programs may assign residents to subspecialty or specialized
continuity clinics (e.g., an HIV clinic) if these assignments achieve the desired outcome noted
in the requirement: that residents develop a long-term therapeutic relationship with a panel of
patients.

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 39 of 64
IV.C.5.b).(1) Residents must serve as the primary physician for a panel
of patients, with responsibility for chronic disease
management, management of acute health problems, and
preventive health care for their patients.
(Core)
IV.C.5.b).(2) Residents must participate in the coordination of care of
patients across health care settings and between
outpatient visits.
(Core)
IV.C.5.b).(3) Residents must be supervised and taught by faculty
members with whom they have developed a longitudinal
relationship.
(Core)
IV.C.5.b).(4) Faculty members must maintain a ratio of residents or
other learners to faculty preceptors not to exceed four to
one;
(Detail)
IV.C.5.b).(4).(a) Faculty members must not have other patient care
responsibilities while supervising more than two
residents or other learners.
(Detail)
IV.C.6. Required Didactic Experiences
IV.C.6.a) The educational program must include didactic instruction based
upon the core knowledge content of internal medicine.
(Core)
IV.C.6.a).(1) Residents must participate in diverse teaching conferences
or didactic sessions, including those dedicated to quality
improvement.
(Core)
IV.C.6.a).(2) The program must ensure that residents have the
opportunity to review all knowledge content from
conferences they could not attend.
(Core)
Specialty-Specific Background and Intent: Core knowledge content presented during
conferences will need to be made available for residents who missed the conference due to
clinical responsibilities. This can include repeating the conference, recording and making it
available electronically, or making the content provided during the conference available
electronically.
IV.C.6.a).(3) Residents’ educational experience must include didactic
sessions in which residents interact with other residents
and faculty members.
(Core)
IV.C.6.a).(3).(a) The frequency of these sessions must be sufficient
for peer-to-peer and peer-to-faculty member
interaction.
(Core)
IV.C.6.a).(4) Residents must be provided a patient or case-based
approach to clinical teaching:
Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 40 of 64
IV.C.6.a).(4).(a) on all inpatient, outpatient, telemedicine, and
consultative services;
(Core)
IV.C.6.a).(4).(b) with a frequency and duration sufficient to ensure a
meaningful and continuous teaching relationship
between the assigned teaching faculty member and
the resident; and,
(Core)
IV.C.6.a).(4).(c) that includes interactions between resident and the
teaching faculty member, bedside teaching,
discussion of pathophysiology, and the application
of current evidence in diagnostic and therapeutic
decisions.
(Core)
IV.D. Scholarship
Medicine is both an art and a science. The physician is a humanistic
scientist who cares for patients. This requires the ability to think critically,
evaluate the literature, appropriately assimilate new knowledge, and
practice lifelong learning. The program and faculty must create an
environment that fosters the acquisition of such skills through resident
participation in scholarly activities. Scholarly activities may include
discovery, integration, application, and teaching.
The ACGME recognizes the diversity of residencies and anticipates that
programs prepare physicians for a variety of roles, including clinicians,
scientists, and educators. It is expected that the program’s scholarship will
reflect its mission(s) and aims, and the needs of the community it serves.
For example, some programs may concentrate their scholarly activity on
quality improvement, population health, and/or teaching, while other
programs might choose to utilize more classic forms of biomedical
research as the focus for scholarship.
IV.D.1. Program Responsibilities
IV.D.1.a) The program must demonstrate evidence of scholarly
activities consistent with its mission(s) and aims.
(Core)
IV.D.1.b) The program, in partnership with its Sponsoring Institution,
must allocate adequate resources to facilitate resident and
faculty involvement in scholarly activities.
(Core)
IV.D.1.c) The program must advance residents’ knowledge and
practice of the scholarly approach to evidence-based patient
care.
(Core)
IV.D.2. Faculty Scholarly Activity

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 41 of 64
IV.D.2.a) Among their scholarly activity, programs must demonstrate
accomplishments in at least three of the following domains:
(Core)
• Research in basic science, education, translational
science, patient care, or population health
• Peer-reviewed grants
• Quality improvement and/or patient safety initiatives
• Systematic reviews, meta-analyses, review articles,
chapters in medical textbooks, or case reports
• Creation of curricula, evaluation tools, didactic
educational activities, or electronic educational
materials
• Contribution to professional committees, educational
organizations, or editorial boards
• Innovations in education
IV.D.2.b) The program must demonstrate dissemination of scholarly
activity within and external to the program by the following
methods:
Background and Intent: For the purposes of education, metrics of scholarly activity
represent one of the surrogates for the program’s effectiveness in the creation of an
environment of inquiry that advances the residents’ scholarly approach to patient care.
The Review Committee will evaluate the dissemination of scholarship for the program
as a whole, not for individual faculty members, for a five-year interval, for both core
and non-core faculty members, with the goal of assessing the effectiveness of the
creation of such an environment. The ACGME recognizes that there may be differences
in scholarship requirements between different specialties and between residencies and
fellowships in the same specialty.
IV.D.2.b).(1) faculty participation in grand rounds, posters,
workshops, quality improvement presentations,
podium presentations, grant leadership, non-peer-
reviewed print/electronic resources, articles or
publications, book chapters, textbooks, webinars,
service on professional committees, or serving as a
journal reviewer, journal editorial board member, or
editor;
(Outcome)
IV.D.3. Resident Scholarly Activity
IV.D.3.a) Residents must participate in scholarship.
(Core)
IV.D.3.a).(1) A program’s graduates must demonstrate dissemination of
scholarship within or external to the program by any of the
following methods:
(Core)
IV.D.3.a).(1).(a) presenting in grand rounds, poster sessions,
leading conference presentations (journal club,

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 42 of 64
morbidity and mortality, case conferences);
workshops; quality improvement presentations;
podium presentations; grant leadership; non-peer-
reviewed print/electronic resources; articles or
publications; book chapters; textbooks; webinars;
service on professional committees; or serving as a
journal reviewer, journal editorial board member, or
editor.
(Core)
V. Evaluation
V.A. Resident Evaluation
V.A.1. Feedback and Evaluation
Background and Intent: Feedback is ongoing information provided regarding aspects
of one’s performance, knowledge, or understanding. The faculty empower residents to
provide much of that feedback themselves in a spirit of continuous learning and self-
reflection. Feedback from faculty members in the context of routine clinical care
should be frequent, and need not always be formally documented.
Formative and summative evaluation have distinct definitions. Formative evaluation is
monitoring resident learning and providing ongoing feedback that can be used by
residents to improve their learning in the context of provision of patient care or other
educational opportunities. More specifically, formative evaluations help:
• residents identify their strengths and weaknesses and target areas that need
work
• program directors and faculty members recognize where residents are
struggling and address problems immediately
Summative evaluation is evaluating a resident’s learning by comparing the residents
against the goals and objectives of the rotation and program, respectively. Summative
evaluation is utilized to make decisions about promotion to the next level of training, or
program completion.
End-of-rotation and end-of-year evaluations have both summative and formative
components. Information from a summative evaluation can be used formatively when
residents or faculty members use it to guide their efforts and activities in subsequent
rotations and to successfully complete the residency program.
Feedback, formative evaluation, and summative evaluation compare intentions with
accomplishments, enabling the transformation of a neophyte physician to one with
growing expertise.
V.A.1.a) Faculty members must directly observe, evaluate, and
frequently provide feedback on resident performance during
each rotation or similar educational assignment.
(Core)
Background and Intent: Faculty members should provide feedback frequently
throughout the course of each rotation. Residents require feedback from faculty

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 43 of 64
members to reinforce well-performed duties and tasks, as well as to correct
deficiencies. This feedback will allow for the development of the learner as they strive
to achieve the Milestones. More frequent feedback is strongly encouraged for
residents who have deficiencies that may result in a poor final rotation evaluation.
V.A.1.b) Evaluation must be documented at the completion of the
assignment.
(Core)
V.A.1.b).(1) For block rotations of greater than three months in
duration, evaluation must be documented at least
every three months.
(Core)
V.A.1.b).(2) Longitudinal experiences, such as continuity clinic in
the context of other clinical responsibilities, must be
evaluated at least every three months and at
completion.
(Core)
V.A.1.c) The program must provide an objective performance
evaluation based on the Competencies and the specialty-
specific Milestones, and must:
(Core)
V.A.1.c).(1) use multiple evaluators (e.g., faculty members, peers,
patients, self, and other professional staff members);
and,
(Core)
V.A.1.c).(2) provide that information to the Clinical Competency
Committee for its synthesis of progressive resident
performance and improvement toward unsupervised
practice.
(Core)
V.A.1.d) The program director or their designee, with input from the
Clinical Competency Committee, must:
V.A.1.d).(1) meet with and review with each resident their
documented semi-annual evaluation of performance,
including progress along the specialty-specific
Milestones;
(Core)
V.A.1.d).(2) assist residents in developing individualized learning
plans to capitalize on their strengths and identify areas
for growth; and,
(Core)
V.A.1.d).(3) develop plans for residents failing to progress,
following institutional policies and procedures.
(Core)
Background and Intent: Learning is an active process that requires effort from the
teacher and the learner. Faculty members evaluate a resident's performance at least at
the end of each rotation. The program director or their designee will review those
evaluations, including their progress on the Milestones, at a minimum of every six
months. Residents should be encouraged to reflect upon the evaluation, using the
information to reinforce well-performed tasks or knowledge or to modify deficiencies in

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 44 of 64
knowledge or practice. Working together with the faculty members, residents should
develop an individualized learning plan.
Residents who are experiencing difficulties with achieving progress along the
Milestones may require intervention to address specific deficiencies. Such
intervention, documented in an individual remediation plan developed by the program
director or a faculty mentor and the resident, will take a variety of forms based on the
specific learning needs of the resident. However, the ACGME recognizes that there are
situations which require more significant intervention that may alter the time course of
resident progression. To ensure due process, it is essential that the program director
follow institutional policies and procedures.
V.A.1.e) At least annually, there must be a summative evaluation of
each resident that includes their readiness to progress to the
next year of the program, if applicable.
(Core)
V.A.1.f) The evaluations of a resident’s performance must be
accessible for review by the resident.
(Core)
V.A.1.g) The program must assess residents’ skills in data gathering and
analysis, physical examination, clinical reasoning, patient
management, and procedures in all clinical settings.
(Core)
V.A.2. Final Evaluation
V.A.2.a) The program director must provide a final evaluation for each
resident upon completion of the program.
(Core)
V.A.2.a).(1) The specialty-specific Milestones, and when applicable
the specialty-specific Case Logs, must be used as
tools to ensure residents are able to engage in
autonomous practice upon completion of the program.
(Core)
V.A.2.a).(2) The final evaluation must:
V.A.2.a).(2).(a) become part of the resident’s permanent record
maintained by the institution, and must be
accessible for review by the resident in
accordance with institutional policy;
(Core)
V.A.2.a).(2).(b) verify that the resident has demonstrated the
knowledge, skills, and behaviors necessary to
enter autonomous practice; and,
(Core)
V.A.2.a).(2).(c) be shared with the resident upon completion of
the program.
(Core)
V.A.3. A Clinical Competency Committee must be appointed by the
program director.
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 45 of 64
V.A.3.a) At a minimum, the Clinical Competency Committee must
include three members of the program faculty, at least one of
whom is a core faculty member.
(Core)
V.A.3.a).(1) Additional members must be faculty members from
the same program or other programs, or other health
professionals who have extensive contact and
experience with the program’s residents.
(Core)
Background and Intent: The requirements regarding the Clinical Competency
Committee do not preclude or limit a program director’s participation on the Clinical
Competency Committee. The intent is to leave flexibility for each program to decide the
best structure for its own circumstances, but a program should consider: its program
director’s other roles as resident advocate, advisor, and confidante; the impact of the
program director’s presence on the other Clinical Competency Committee members’
discussions and decisions; the size of the program faculty; and other program-relevant
factors. Inclusivity is an important consideration in the appointment of Clinical
Competency Committee members, allowing for diverse participation to ensure fair
evaluation. The program director has final responsibility for resident evaluation and
promotion decisions.
The program faculty may include more than the physician faculty members, such as
other physicians and non-physicians who teach and evaluate the program’s residents.
There may be additional members of the Clinical Competency Committee. Chief
residents who have completed core residency programs in their specialty may be
members of the Clinical Competency Committee.
V.A.3.b) The Clinical Competency Committee must:
V.A.3.b).(1) review all resident evaluations at least semi-annually;
(Core)
V.A.3.b).(2) determine each resident’s progress on achievement of
the specialty-specific Milestones; and,
(Core)
V.A.3.b).(3) meet prior to the residents’ semi-annual evaluations
and advise the program director regarding each
resident’s progress.
(Core)
V.B. Faculty Evaluation
V.B.1. The program must have a process to evaluate each faculty
member’s performance as it relates to the educational program at
least annually.
(Core)
Background and Intent: The program director is responsible for the educational
program and all educators. While the term “faculty” may be applied to physicians
within a given institution for other reasons, it is applied to residency program faculty
members only through approval by a program director. The development of the faculty
improves the education, clinical, and research aspects of a program. Faculty members
have a strong commitment to the resident and desire to provide optimal education and

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 46 of 64
work opportunities. Faculty members must be provided feedback on their contribution
to the mission of the program. All faculty members who interact with residents desire
feedback on their education, clinical care, and research. If a faculty member does not
interact with residents, feedback is not required. With regard to the diverse operating
environments and configurations, the residency program director may need to work
with others to determine the effectiveness of the program’s faculty performance with
regard to their role in the educational program. All teaching faculty members should
have their educational efforts evaluated by the residents in a confidential and
anonymous manner. Other aspects for the feedback may include research or clinical
productivity, review of patient outcomes, or peer review of scholarly activity. The
process should reflect the local environment and identify the necessary information.
The feedback from the various sources should be summarized and provided to the
faculty on an annual basis by a member of the leadership team of the program.
V.B.1.a) This evaluation must include a review of the faculty member’s
clinical teaching abilities, engagement with the educational
program, participation in faculty development related to their
skills as an educator, clinical performance, professionalism,
and scholarly activities.
(Core)
V.B.1.b) This evaluation must include written, anonymous, and
confidential evaluations by the residents.
(Core)
V.B.2. Faculty members must receive feedback on their evaluations at least
annually.
(Core)
V.B.3. Results of the faculty educational evaluations should be
incorporated into program-wide faculty development plans.
(Core)
Background and Intent: The quality of the faculty’s teaching and clinical care is a
determinant of the quality of the program and the quality of the residents’ future
clinical care. Therefore, the program has the responsibility to evaluate and improve the
program faculty members’ teaching, scholarship, professionalism, and quality care.
This section mandates annual review of the program’s faculty members for this
purpose, and can be used as input into the Annual Program Evaluation.
V.C. Program Evaluation and Improvement
V.C.1. The program director must appoint the Program Evaluation
Committee to conduct and document the Annual Program
Evaluation as part of the program’s continuous improvement
process.
(Core)
V.C.1.a) The Program Evaluation Committee must be composed of at
least two program faculty members, at least one of whom is a
core faculty member, and at least one resident.
(Core)
V.C.1.b) Program Evaluation Committee responsibilities must include:
V.C.1.b).(1) review of the program’s self-determined goals and
progress toward meeting them;
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 47 of 64
V.C.1.b).(2) guiding ongoing program improvement, including
development of new goals, based upon outcomes;
and,
(Core)
V.C.1.b).(3) review of the current operating environment to identify
strengths, challenges, opportunities, and threats as
related to the program’s mission and aims.
(Core)
Background and Intent: To achieve its mission and educate and train quality
physicians, a program must evaluate its performance and plan for improvement in the
Annual Program Evaluation. Performance of residents and faculty members is a
reflection of program quality, and can use metrics that reflect the goals that a program
has set for itself. The Program Evaluation Committee utilizes outcome parameters and
other data to assess the program’s progress toward achievement of its goals and aims.
The Program Evaluation Committee advises the program director through program
oversight.
V.C.1.c) The Program Evaluation Committee should consider the
outcomes from prior Annual Program Evaluation(s),
aggregate resident and faculty written evaluations of the
program, and other relevant data in its assessment of the
program.
(Core)
Background and Intent: Other data to be considered for assessment include:
• Curriculum
• ACGME letters of notification, including citations, Areas for Improvement, and
comments
• Quality and safety of patient care
• Aggregate resident and faculty well-being; recruitment and retention; workforce
diversity, including graduate medical education staff and other relevant
academic community members; engagement in quality improvement and patient
safety; and scholarly activity
• ACGME Resident and Faculty Survey results
• Aggregate resident Milestones evaluations, and achievement on in-training
examinations (where applicable), board pass and certification rates, and
graduate performance.
• Aggregate faculty evaluation and professional development
V.C.1.d) The Program Evaluation Committee must evaluate the
program’s mission and aims, strengths, areas for
improvement, and threats.
(Core)
V.C.1.e) The Annual Program Evaluation, including the action plan,
must be distributed to and discussed with the residents and
the members of the teaching faculty, and be submitted to the
DIO.
(Core)
V.C.2. The program must complete a Self-Study and submit it to the DIO.
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 48 of 64
Background and Intent: Outcomes of the documented Annual Program Evaluation can
be integrated into the accreditation Self-Study process. The accreditation Self-Study is
an objective, comprehensive evaluation of the residency program, with the aim of
improving it. Underlying the accreditation Self-Study is this longitudinal evaluation of
the program and its learning environment, facilitated through sequential Annual
Program Evaluations that focus on the required components, with an emphasis on
program strengths and self-identified areas for improvement. Details regarding the
timing and expectations for the accreditation Self-Study are provided in the ACGME
Manual of Policies and Procedures. Additionally, a description of the
accreditation
Self-Study process is available on the ACGME website.
V.C.3. One goal of ACGME-accredited education is to educate physicians
who seek and achieve board certification. One measure of the
effectiveness of the educational program is the ultimate pass rate.
The program director should encourage all eligible program
graduates to take the certifying examination offered by the
applicable American Board of Medical Specialties (ABMS) member
board or American Osteopathic Association (AOA) certifying board.
V.C.3.a) For specialties in which the ABMS member board and/or AOA
certifying board offer(s) an annual written exam, in the
preceding three years, the program’s aggregate pass rate of
those taking the examination for the first time must be higher
than the bottom fifth percentile of programs in that specialty.
(Outcome)
V.C.3.b) For specialties in which the ABMS member board and/or AOA
certifying board offer(s) a biennial written exam, in the
preceding six years, the program’s aggregate pass rate of
those taking the examination for the first time must be higher
than the bottom fifth percentile of programs in that specialty.
(Outcome)
V.C.3.c) For specialties in which the ABMS member board and/or AOA
certifying board offer(s) an annual oral exam, in the preceding
three years, the program’s aggregate pass rate of those
taking the examination for the first time must be higher than
the bottom fifth percentile of programs in that specialty.
(Outcome)
V.C.3.d) For specialties in which the ABMS member board and/or AOA
certifying board offer(s) a biennial oral exam, in the preceding
six years, the program’s aggregate pass rate of those taking
the examination for the first time must be higher than the
bottom fifth percentile of programs in that specialty.
(Outcome)
V.C.3.e) For each of the exams referenced in V.C.3.a)-d), any program
whose graduates over the time period specified in the
requirement have achieved an 80 percent pass rate will have

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 49 of 64
met this requirement, no matter the percentile rank of the
program for pass rate in that specialty.
(Outcome)
Background and Intent: Setting a single standard for pass rate that works across
specialties is not supportable based on the heterogeneity of the psychometrics of
different examinations. By using a percentile rank, the performance of the lower five
percent (fifth percentile) of programs can be identified and set on a path to curricular
and test preparation reform.
There are specialties where there is a very high board pass rate that could leave
successful programs in the bottom five percent (fifth percentile) despite admirable
performance. These high-performing programs should not be cited, and V.C.3.e) is
designed to address this.
V.C.3.f) Programs must report, in ADS, board certification status
annually for the cohort of board-eligible residents that
graduated seven years earlier.
(Core)
Background and Intent: It is essential that residency programs demonstrate knowledge
and skill transfer to their residents. One measure of that is the qualifying or initial
certification exam pass rate. Another important parameter of the success of the
program is the ultimate board certification rate of its graduates. Graduates are eligible
for up to seven years from residency graduation for initial certification. The ACGME
will calculate a rolling three-year average of the ultimate board certification rate at
seven years post-graduation, and the Review Committees will monitor it.
The Review Committees will track the rolling seven-year certification rate as an
indicator of program quality. Programs are encouraged to monitor their graduates’
performance on board certification examinations.
In the future, the ACGME may establish parameters related to ultimate board
certification rates.
VI. The Learning and Working Environment
Residency education must occur in the context of a learning and working
environment that emphasizes the following principles:
• Excellence in the safety and quality of care rendered to patients by residents
today
• Excellence in the safety and quality of care rendered to patients by today’s
residents in their future practice
• Excellence in professionalism through faculty modeling of:
• Appreciation for the privilege of providing care for patients
• Commitment to the well-being of the students, residents, faculty members, and
all members of the health care team
Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 50 of 64
VI.A. Patient Safety, Quality Improvement, Supervision, and Accountability
VI.A.1. Patient Safety and Quality Improvement
VI.A.1.a) Patient Safety
VI.A.1.a).(1) Culture of Safety
A culture of safety requires continuous identification
of vulnerabilities and a willingness to transparently
deal with them. An effective organization has formal
mechanisms to assess the knowledge, skills, and
attitudes of its personnel toward safety in order to
identify areas for improvement.
VI.A.1.a).(1).(a) The program, its faculty, residents, and fellows
must actively participate in patient safety
systems and contribute to a culture of safety.
(Core)
VI.A.1.a).(2) Patient Safety Events
Reporting, investigation, and follow-up of safety
events, near misses, and unsafe conditions are pivotal
mechanisms for improving patient safety, and are
essential for the success of any patient safety
program. Feedback and experiential learning are
essential to developing true competence in the ability
to identify causes and institute sustainable systems-
based changes to ameliorate patient safety
vulnerabilities.
VI.A.1.a).(2).(a) Residents, fellows, faculty members, and other
clinical staff members must:
VI.A.1.a).(2).(a).(i) know their responsibilities in reporting
patient safety events and unsafe
conditions at the clinical site, including
how to report such events; and,
(Core)
VI.A.1.a).(2).(a).(ii) be provided with summary information
of their institution’s patient safety
reports.
(Core)
VI.A.1.a).(2).(b) Residents must participate as team members in
real and/or simulated interprofessional clinical
patient safety and quality improvement
activities, such as root cause analyses or other
activities that include analysis, as well as
formulation and implementation of actions.
(Core)
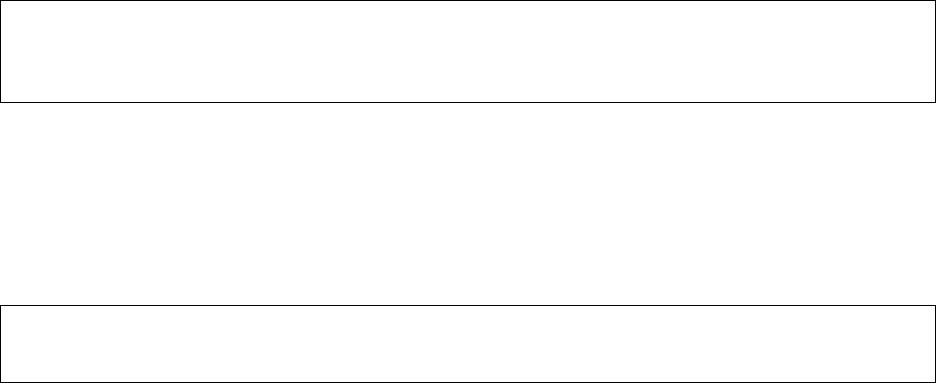
Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 51 of 64
VI.A.1.a).(3) Quality Metrics
Access to data is essential to prioritizing activities for
care improvement and evaluating success of
improvement efforts.
VI.A.1.a).(3).(a) Residents and faculty members must receive
data on quality metrics and benchmarks related
to their patient populations.
(Core)
VI.A.2. Supervision and Accountability
VI.A.2.a) Although the attending physician is ultimately responsible for
the care of the patient, every physician shares in the
responsibility and accountability for their efforts in the
provision of care. Effective programs, in partnership with
their Sponsoring Institutions, define, widely communicate,
and monitor a structured chain of responsibility and
accountability as it relates to the supervision of all patient
care.
Supervision in the setting of graduate medical education
provides safe and effective care to patients; ensures each
resident’s development of the skills, knowledge, and attitudes
required to enter the unsupervised practice of medicine; and
establishes a foundation for continued professional growth.
VI.A.2.a).(1) Residents and faculty members must inform each
patient of their respective roles in that patient’s care
when providing direct patient care.
(Core)
VI.A.2.a).(1).(a) This information must be available to residents,
faculty members, other members of the health
care team, and patients.
(Core)
Background and Intent: Each patient will have an identifiable and appropriately
credentialed and privileged attending physician (or licensed independent practitioner
as specified by the applicable Review Committee) who is responsible and accountable
for the patient’s care.
VI.A.2.a).(2) The program must demonstrate that the appropriate
level of supervision in place for all residents is based
on each resident’s level of training and ability, as well
as patient complexity and acuity. Supervision may be
exercised through a variety of methods, as appropriate
to the situation.
(Core)
Background and Intent: Appropriate supervision is essential for patient safety and
high-quality teaching. Supervision is also contextual. There is tremendous diversity of
resident-patient interactions, training locations, and resident skills and abilities, even
Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 52 of 64
at the same level of the educational program. The degree of supervision for a resident
is expected to evolve progressively as the resident gains more experience, even with
the same patient condition or procedure. The level of supervision for each resident is
commensurate with that resident’s level of independence in practice; this level of
supervision may be enhanced based on factors such as patient safety, complexity,
acuity, urgency, risk of serious safety events, or other pertinent variables.
VI.A.2.b) Levels of Supervision
To promote appropriate resident supervision while providing
for graded authority and responsibility, the program must use
the following classification of supervision:
VI.A.2.b).(1) Direct Supervision:
VI.A.2.b).(1).(a) the supervising physician is physically present
with the resident during the key portions of the
patient interaction; or,
VI.A.2.b).(1).(a).(i) PGY-1 residents must initially be
supervised directly, only as described in
VI.A.2.b).(1).(a).
(Core)
VI.A.2.b).(1).(a).(i).(a) A supervising physician must be
immediately available to be
physically present for PGY-1
residents on inpatient rotations who
have demonstrated the skills
sufficient to progress to indirect
supervision.
(Core)
VI.A.2.b).(1).(b) the supervising physician and/or patient is not
physically present with the resident and the
supervising physician is concurrently
monitoring the patient care through appropriate
telecommunication technology.
VI.A.2.b).(2) Indirect Supervision: the supervising physician is not
providing physical or concurrent visual or audio
supervision but is immediately available to the
resident for guidance and is available to provide
appropriate direct supervision.
VI.A.2.b).(3) Oversight – the supervising physician is available to
provide review of procedures/encounters with
feedback provided after care is delivered.
VI.A.2.c) The program must define when physical presence of a
supervising physician is required.
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 53 of 64
VI.A.2.d) The privilege of progressive authority and responsibility,
conditional independence, and a supervisory role in patient
care delegated to each resident must be assigned by the
program director and faculty members.
(Core)
VI.A.2.d).(1) The program director must evaluate each resident’s
abilities based on specific criteria, guided by the
Milestones.
(Core)
VI.A.2.d).(2) Faculty members functioning as supervising
physicians must delegate portions of care to residents
based on the needs of the patient and the skills of
each resident.
(Core)
VI.A.2.d).(3) Senior residents or fellows should serve in a
supervisory role to junior residents in recognition of
their progress toward independence, based on the
needs of each patient and the skills of the individual
resident or fellow.
(Detail)
VI.A.2.e) Programs must set guidelines for circumstances and events
in which residents must communicate with the supervising
faculty member(s).
(Core)
VI.A.2.e).(1) Each resident must know the limits of their scope of
authority, and the circumstances under which the
resident is permitted to act with conditional
independence.
(Outcome)
Background and Intent: The ACGME Glossary of Terms defines conditional
independence as: Graded, progressive responsibility for patient care with defined
oversight.
VI.A.2.f) Faculty supervision assignments must be of sufficient
duration to assess the knowledge and skills of each resident
and to delegate to the resident the appropriate level of patient
care authority and responsibility.
(Core)
VI.B. Professionalism
VI.B.1. Programs, in partnership with their Sponsoring Institutions, must
educate residents and faculty members concerning the professional
and ethical responsibilities of physicians, including but not limited
to their obligation to be appropriately rested and fit to provide the
care required by their patients.
(Core)
Background and Intent: This requirement emphasizes the professional responsibility
of residents and faculty members to arrive for work adequately rested and ready to
care for patients. It is also the responsibility of residents, faculty members, and other
members of the care team to be observant, to intervene, and/or to escalate their

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 54 of 64
concern about resident and faculty member fitness for work, depending on the
situation, and in accordance with institutional policies. This includes recognition of
impairment, including from illness, fatigue, and substance use, in themselves, their
peers, and other members of the health care team, and the recognition that under
certain circumstances, the best interests of the patient may be served by transitioning
that patient’s care to another qualified and rested practitioner.
VI.B.2. The learning objectives of the program must:
VI.B.2.a) be accomplished without excessive reliance on residents to
fulfill non-physician obligations;
(Core)
Background and Intent: Routine reliance on residents to fulfill non-physician obligations
increases work compression for residents and does not provide an optimal educational
experience. Non-physician obligations are those duties which in most institutions are
performed by nursing and allied health professionals, transport services, or clerical
staff. Examples of such obligations include transport of patients from the wards or units
for procedures elsewhere in the hospital; routine blood drawing for laboratory tests;
routine monitoring of patients when off the ward; and clerical duties, such as
scheduling. While it is understood that residents may be expected to do any of these
things on occasion when the need arises, these activities should not be performed by
residents routinely and must be kept to a minimum to optimize resident education.
VI.B.2.b) ensure manageable patient care responsibilities; and,
(Core)
Background and Intent: The Common Program Requirements do not define
“manageable patient care responsibilities” as this is variable by specialty and PGY
level. Review Committees will provide further detail regarding patient care
responsibilities in the applicable specialty-specific Program Requirements and
accompanying FAQs. However, all programs, regardless of specialty, should carefully
assess how the assignment of patient care responsibilities can affect work
compression, especially at the PGY-1 level.
VI.B.2.c) include efforts to enhance the meaning that each resident
finds in the experience of being a physician, including
protecting time with patients, providing administrative
support, promoting progressive independence and flexibility,
and enhancing professional relationships.
(Core)
VI.B.3. The program director, in partnership with the Sponsoring Institution,
must provide a culture of professionalism that supports patient
safety and personal responsibility.
(Core)
Background and Intent: The accurate reporting of clinical and educational work hours,
patient outcomes, and clinical experience data are the responsibility of the program
leadership, residents, and faculty.
VI.B.4. Residents and faculty members must demonstrate an understanding
of their personal role in the safety and welfare of patients entrusted
Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 55 of 64
to their care, including the ability to report unsafe conditions and
safety events.
(Core)
VI.B.5. Programs, in partnership with their Sponsoring Institutions, must
provide a professional, equitable, respectful, and civil environment
that is psychologically safe and that is free from discrimination,
sexual and other forms of harassment, mistreatment, abuse, or
coercion of students, residents, faculty, and staff.
(Core)
Background and Intent: Psychological safety is defined as an environment of trust and
respect that allows individuals to feel able to ask for help, admit mistakes, raise
concerns, suggest ideas, and challenge ways of working and the ideas of others on the
team, including the ideas of those in authority, without fear of humiliation, and the
knowledge that mistakes will be handled justly and fairly.
The ACGME is unable to adjudicate disputes between individuals, including residents,
faculty members, and staff members. However, information that suggests a pattern of
behavior that violates the requirement above will trigger a careful review and, if
deemed appropriate, action by the Review Committee and/or ACGME, in accordance
with ACGME Policies and Procedures.
VI.B.6. Programs, in partnership with their Sponsoring Institutions, should
have a process for education of residents and faculty regarding
unprofessional behavior and a confidential process for reporting,
investigating, and addressing such concerns.
(Core)
VI.C. Well-Being
Psychological, emotional, and physical well-being are critical in the
development of the competent, caring, and resilient physician and require
proactive attention to life inside and outside of medicine. Well-being
requires that physicians retain the joy in medicine while managing their
own real-life stresses. Self-care and responsibility to support other
members of the health care team are important components of
professionalism; they are also skills that must be modeled, learned, and
nurtured in the context of other aspects of residency training.
Residents and faculty members are at risk for burnout and depression.
Programs, in partnership with their Sponsoring Institutions, have the same
responsibility to address well-being as other aspects of resident
competence. Physicians and all members of the health care team share
responsibility for the well-being of each other. A positive culture in a
clinical learning environment models constructive behaviors, and prepares
residents with the skills and attitudes needed to thrive throughout their
careers.
VI.C.1. The responsibility of the program, in partnership with the
Sponsoring Institution, must include:
VI.C.1.a) attention to scheduling, work intensity, and work
compression that impacts resident well-being;
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 56 of 64
VI.C.1.b) evaluating workplace safety data and addressing the safety of
residents and faculty members;
(Core)
Background and Intent: This requirement emphasizes the responsibility shared by the
Sponsoring Institution and its programs to gather information and utilize systems that
monitor and enhance resident and faculty member safety, including physical safety.
Issues to be addressed include, but are not limited to, monitoring of workplace injuries,
physical or emotional violence, vehicle collisions, and emotional well-being after safety
events.
VI.C.1.c) policies and programs that encourage optimal resident and
faculty member well-being; and,
(Core)
Background and Intent: Well-being includes having time away from work to engage with
family and friends, as well as to attend to personal needs and to one’s own health,
including adequate rest, healthy diet, and regular exercise. The intent of this
requirement is to ensure that residents have the opportunity to access medical and
dental care, including mental health care, at times that are appr
opriate to their individual
circumstances. Residents must be provided with time away from the program as needed
to access care, including appointments scheduled during their working hours.
VI.C.1.c).(1) Residents must be given the opportunity to attend
medical, mental health, and dental care appointments,
including those scheduled during their working hours.
(Core)
VI.C.1.d) education of residents and faculty members in:
VI.C.1.d).(1) identification of the symptoms of burnout, depression,
and substance use disorders, suicidal ideation, or
potential for violence, including means to assist those
who experience these conditions;
(Core)
VI.C.1.d).(2) recognition of these symptoms in themselves and how
to seek appropriate care; and,
(Core)
VI.C.1.d).(3) access to appropriate tools for self-screening.
(Core)
Background and Intent: Programs and Sponsoring Institutions are encouraged to review
materials to create systems for identification of burnout, depression, and substance use
disorders. Materials and more information are available in Learn at ACGME
(
https://dl.acgme.org/pages/well-being-tools-resources).
Individuals experiencing burnout, depression, a substance use disorder, and/or suicidal
ideation are often reluctant to reach out for help due to the stigma associated with these
conditions and may be
concerned that seeking help may have a negative impact on their
career. Recognizing that physicians are at increased risk in these areas, it is essential
that residents and faculty members are able to report their concerns when another
resident or faculty member displays signs of any of these conditions, so that the

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 57 of 64
program director or other designated personnel, such as the department chair, may
assess the situation and intervene as necessary to facilitate access to appropriate care.
Residents and faculty members must know which personnel, in addition to the program
director, have been designated with this responsibility; those personnel and the
program director should be familiar with the institution’s impaired physician policy and
any employee health, employee assistance, and/or wellness/well-being programs within
the institution. In cases of physician impairment, the program director or designated
personnel should follow the policies of their institution for reporting.
VI.C.1.e) providing access to confidential, affordable mental health
assessment, counseling, and treatment, including access to
urgent and emergent care 24 hours a day, seven days a week.
(Core)
Background and Intent: The intent of this requirement is to ensure that residents have
immediate access at all times to a mental health professional (psychiatrist,
psychologist, Licensed Clinical Social Worker, Primary Mental Health Nurse
Practitioner, or Licensed Professional Counselor) for urgent or emergent mental health
issues. In-person, telemedicine, or telephonic means may be utilized to satisfy this
requirement. Care in the Emergency Department may be necessary in some cases, but
not as the primary or sole means to meet the requirement.
The reference to affordable counseling is intended to require that financial cost not be a
barrier to obtaining care.
VI.C.2. There are circumstances in which residents may be unable to attend
work, including but not limited to fatigue, illness, family
emergencies, and medical, parental, or caregiver leave. Each
program must allow an appropriate length of absence for residents
unable to perform their patient care responsibilities.
(Core)
VI.C.2.a) The program must have policies and procedures in place to
ensure coverage of patient care and ensure continuity of
patient care.
(Core)
VI.C.2.b) These policies must be implemented without fear of negative
consequences for the resident who is or was unable to
provide the clinical work.
(Core)
Background and Intent: Residents may need to extend their length of training
depending on length of absence and specialty board eligibility requirements.
Teammates should assist colleagues in need and equitably reintegrate them upon
return.
VI.D. Fatigue Mitigation
VI.D.1. Programs must educate all residents and faculty members in
recognition of the signs of fatigue and sleep deprivation, alertness
management, and fatigue mitigation processes.
(Detail)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 58 of 64
Background and Intent: Providing medical care to patients is physically and mentally
demanding. Night shifts, even for those who have had enough rest, cause fatigue.
Experiencing fatigue in a supervised environment during training prepares residents for
managing fatigue in practice. It is expected that programs adopt fatigue mitigation
processes and ensure that there are no negative consequences and/or stigma for using
fatigue mitigation strategies.
Strategies that may be used include but are not limited to strategic napping; the
judicious use of caffeine; availability of other caregivers; time management to maximize
sleep off-duty; learning to recognize the signs of fatigue, and self-monitoring
performance and/or asking others to monitor performance; remaining active to promote
alertness; maintaining a healthy diet; using relaxation techniques to fall asleep;
maintaining a consistent sleep routine; exercising regularly; increasing sleep time
before and after call; and ensuring sufficient sleep recovery periods.
VI.D.2. The program, in partnership with its Sponsoring Institution, must
ensure adequate sleep facilities and safe transportation options for
residents who may be too fatigued to safely return home.
(Core)
VI.E. Clinical Responsibilities, Teamwork, and Transitions of Care
VI.E.1. Clinical Responsibilities
The clinical responsibilities for each resident must be based on PGY
level, patient safety, resident ability, severity and complexity of
patient illness/condition, and available support services.
(Core)
VI.E.1.a) Programs must ensure that residents’ clinical responsibilities on
inpatient rotations are consistent with the requirements in IV.C.4.
(Core)
Background and Intent: The changing clinical care environment of medicine has meant
that work compression due to high complexity has increased stress on residents.
Faculty members and program directors need to make sure residents function in an
environment that has safe patient care and a sense of resident well-being. It is an
essential responsibility of the program director to monitor resident workload. Workload
should be distributed among the resident team and interdisciplinary teams to minimize
work compression.
VI.E.2. Teamwork
Residents must care for patients in an environment that maximizes
communication and promotes safe, interprofessional, team-based
care in the specialty and larger health system.
(Core)
VI.E.2.a) The program must provide educational experiences that allow
residents to interact with and learn from other health care
professionals, including physicians in other specialties, advanced
practice providers, nurses, social workers, physical therapists,
case managers, language interpreters, and dieticians, in order to

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 59 of 64
achieve effective, interdisciplinary, and interprofessional team-
based care.
(Core)
Specialty-Specific Background and Intent: Physician and non-physicians, core and non-core
faculty members, are part of the different teams that form depending on the health care
situation and on patients’ health status and circumstances. The intent of the requirement is to
ensure that residents will have access to the appropriate health care personnel as defined by
the circumstances, and that interdisciplinary, interprofessional teams will be constituted as
appropriate and as needed.
Background and Intent: Effective programs will have a structure that promotes safe,
interprofessional, team-based care. Optimal patient safety occurs in the setting of a
coordinated interprofessional learning and working environment.
VI.E.3. Transitions of Care
VI.E.3.a) Programs must design clinical assignments to optimize
transitions in patient care, including their safety, frequency,
and structure.
(Core)
VI.E.3.b) Programs, in partnership with their Sponsoring Institutions,
must ensure and monitor effective, structured hand-off
processes to facilitate both continuity of care and patient
safety.
(Core)
VI.E.3.c) Programs must ensure that residents are competent in
communicating with team members in the hand-off process.
(Outcome)
VI.F. Clinical Experience and Education
Programs, in partnership with their Sponsoring Institutions, must design
an effective program structure that is configured to provide residents with
educational and clinical experience opportunities, as well as reasonable
opportunities for rest and personal activities.
Background and Intent: The terms “clinical experience and education,” “clinical and
educational work,” and “clinical and educational work hours” replace the terms “duty
hours,” “duty periods,” and “duty.” These terms are used in response to concerns that
the previous use of the term “duty” in reference to number of hours worked may have
led some to conclude that residents’ duty to “clock out” on time superseded their duty
to their patients.
VI.F.1. Maximum Hours of Clinical and Educational Work per Week
Clinical and educational work hours must be limited to no more than
80 hours per week, averaged over a four-week period, inclusive of all
in-house clinical and educational activities, clinical work done from
home, and all moonlighting.
(Core)

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 60 of 64
Background and Intent: Programs and residents have a shared responsibility to ensure
that the 80-hour maximum weekly limit is not exceeded. While the requirement has been
written with the intent of allowing residents to remain beyond their scheduled work
periods to care for a patient or participate in an educational activity, these additional
hours must be accounted for in the allocated 80 hours when averaged over four weeks.
Work from Home
While the requirement specifies that clinical work done from home must be counted
toward the 80-hour maximum weekly limit, the expectation remains that scheduling be
structured so that residents are able to complete most work on site during scheduled
clinical work hours without requiring them to take work home. The requirements
acknowledge the changing landscape of medicine, including electronic health records,
and the resulting increase in the amount of work residents choose to do from home. The
requirement provides flexibility for residents to do this while ensuring that the time
spent by residents completing clinical work from home is accomplished within the 80-
hour weekly maximum. Types of work from home that must be counted include using an
electronic health record and taking calls from home. Reading done in preparation for t
he
following day’s cases, studying, and research done from home do not count toward the
80 hours. Resident decisions to leave the hospital before their clinical work has been
completed and to finish that work later from home should be made in consultation with
the resident’s supervisor. In such circumstances, residents should be mindful of their
professional responsibility to complete work in a timely manner and to maintain patient
confidentiality.
Residents are to track the time they spend on clinical work from home and to report that
time to the program. Decisions regarding whether to report infrequent phone calls of
very short duration will be left to the individual resident. Programs will need to factor in
time residents are spending on clinical work at home when schedules are developed to
ensure that residents are not working in excess of 80 hours per week, averaged over
four weeks. There is no requirement that programs assume responsibility for
documenting this time. Rather, the program’s responsibility is ensuring that residents
report their time from home and that schedules are structured to ensure that residents
are not working in excess of 80 hours per week, averaged over four weeks.
VI.F.2. Mandatory Time Free of Clinical Work and Education
VI.F.2.a) Residents should have eight hours off between scheduled
clinical work and education periods.
(Detail)
Background and Intent: There may be circumstances when residents choose to stay to
care for their patients or return to the hospital with fewer than eigh
t hours free of clinical
experience and education. This occurs within the context of the 80-hour and the one-
day-off-in-seven requirements. While it is expected that resident schedules will be
structured to ensure that residents are provided with a minimum of eight hours off
between scheduled work periods, it is recognized that residents may choose to remain
beyond their scheduled time, or return to the clinical site during this time-off period, to
care for a patient. The requirement preserves the flexibility for residents to make those
choices. It is also noted that the 80-hour weekly limit (averaged over four weeks) is a
deterrent for scheduling fewer than eight hours off between clinical and education work
Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 61 of 64
periods, as it would be difficult for a program to design a schedule that provides fewer
than eight hours off without violating the 80-hour rule.
VI.F.2.b) Residents must have at least 14 hours free of clinical work
and education after 24 hours of in-house call.
(Core)
Background and Intent: Residents have a responsibility to return to work rested, and
thus are expected to use this time away from work to get adequate rest. In support of
this goal, residents are encouraged to prioritize sleep over other discretionary activities.
VI.F.2.c) Residents must be scheduled for a minimum of one day in
seven free of clinical work and required education (when
averaged over four weeks). At-home call cannot be assigned
on these free days.
(Core)
Background and Intent: The requirement provides flexibility for programs to distribute
days off in a manner that meets program and resident needs. It is strongly
recommended that residents’ preference regarding how their days off are distributed be
considered as schedules are developed. It is desirable that days off be distributed
throughout the month, but some residents may prefer to group their days off to have a
“golden weekend,” meaning a consecutive Saturday and Sunday free from work. The
requirement for one free day in seven should not be interpreted as precluding a golden
weekend. Where feasible, schedules may be designed to provide residents with a
weekend, or two consecutive days, free of work. The applicable Review Committee will
evaluate the number of consecutive days of work and determine whether they meet
educational objectives. Programs are encouraged to distribute days off in a fashion that
optimizes resident well-being, and educational and personal goals. It is noted that a day
off is defined in the ACGME Glossary of Terms as “one (1) continuous 24-hour period
free from all administrative, clinical, and educational activities.”
VI.F.3. Maximum Clinical Work and Education Period Length
VI.F.3.a) Clinical and educational work periods for residents must not
exceed 24 hours of continuous scheduled clinical
assignments.
(Core)
VI.F.3.a).(1) Up to four hours of additional time may be used for
activities related to patient safety, such as providing
effective transitions of care, and/or resident education.
Additional patient care responsibilities must not be
assigned to a resident during this time.
(Core)
Background and Intent: The additional time referenced in VI.F.3.a).(1) should not be
used for the care of new patients. It is essential that the resident continue to function as
a member of the team in an environment where other members of the team can assess
resident fatigue, and that supervision for post-call residents is provided. This 24 hours
and up to an additional four hours must occur within the context of 80-hour weekly limit
,
averaged over four weeks.
VI.F.4. Clinical and Educational Work Hour Exceptions

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 62 of 64
VI.F.4.a) In rare circumstances, after handing off all other
responsibilities, a resident, on their own initiative, may elect
to remain or return to the clinical site in the following
circumstances: to continue to provide care to a single
severely ill or unstable patient; to give humanistic attention to
the needs of a patient or patient’s family; or to attend unique
educational events.
(Detail)
VI.F.4.b) These additional hours of care or education must be counted
toward the 80-hour weekly limit.
(Detail)
Background and Intent: This requirement is intended to provide residents with some
control over their schedules by providing the flexibility to voluntarily remain beyond the
scheduled responsibilities under the circumstances described above. It is important to
note that a resident may remain to attend a conference, or return for a conference later
in the day, only if the decision is made voluntarily. Residents must not be required to
stay. Programs allowing residents to remain or return beyond the scheduled work and
clinical education period must ensure that the decision to remain is initiated by the
resident and that residents are not coerced. This additional time must be counted
toward the 80-hour maximum weekly limit.
VI.F.4.c) A Review Committee may grant rotation-specific exceptions
for up to 10 percent or a maximum of 88 clinical and
educational work hours to individual programs based on a
sound educational rationale.
The Review Committee for Internal Medicine will not consider
requests for exceptions to the 80-hour limit to the resident work
week.
VI.F.5. Moonlighting
VI.F.5.a) Moonlighting must not interfere with the ability of the resident
to achieve the goals and objectives of the educational
program, and must not interfere with the resident’s fitness for
work nor compromise patient safety.
(Core)
VI.F.5.b) Time spent by residents in internal and external moonlighting
(as defined in the ACGME Glossary of Terms) must be
counted toward the 80-hour maximum weekly limit.
(Core)
VI.F.5.c) PGY-1 residents are not permitted to moonlight.
(Core)
Background and Intent: For additional clarification of the expectations related to
moonlighting, please refer to the Common Program Requirement FAQs (available at
http://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements).
VI.F.6. In-House Night Float

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 63 of 64
Night float must occur within the context of the 80-hour and one-
day-off-in-seven requirements.
(Core)
VI.F.6.a) Residents must not be assigned more than two months of night
float during any year of the educational program, or more than
four months of night float during the course of the residency.
(Core)
VI.F.6.b) Residents must not be assigned to more than one month of
consecutive night float rotation.
(Core)
Specialty-Specific Background and Intent: Night float rotations are designed to either
eliminate in-house call or to assist other residents during the night. Residents assigned to
night float are assigned on-site duty during evening/night shifts and are responsible for
admitting or cross-covering patients until morning and will not have daytime assignments or
ongoing primary responsibility for these patients. The Committee has limited the number a
program can assign because it believes too many such rotations can negatively affect
resident well-being and contribute to burnout and fatigue. Overnight shifts occurring during
critical care rotations (in the medical intensive care unit or the critical care unit) do not count
towards night float, but towards the maximum six months of required critical care time.
Overnight emergency medicine assignments do not count towards night float.
VI.F.7. Maximum In-House On-Call Frequency
Residents must be scheduled for in-house call no more frequently
than every third night (when averaged over a four-week period).
(Core)
VI.F.8. At-Home Call
VI.F.8.a) Time spent on patient care activities by residents on at-home
call must count toward the 80-hour maximum weekly limit.
The frequency of at-home call is not subject to the every-
third-night limitation, but must satisfy the requirement for one
day in seven free of clinical work and education, when
averaged over four weeks.
(Core)
VI.F.8.a).(1) At-home call must not be so frequent or taxing as to
preclude rest or reasonable personal time for each
resident.
(Core)
Background and Intent: As noted in VI.F.1., clinical work done from home when a
resident is taking at-home call must count toward the 80-hour maximum weekly limit.
This acknowledges the often significant amount of time residents devote to clinical
activities when taking at-home call, and ensures that taking at-home call does not result
in residents routinely working more than 80 hours per week. At-home call activities that
must be counted include responding to phone calls and other forms of communication,
as well as documentation, such as entering notes in an electronic health record.
Activities such as reading about the next day’s case, studying, or research activities do
not count toward the 80-hour weekly limit.

Internal Medicine
©2023 Accreditation Council for Graduate Medical Education (ACGME) Page 64 of 64
In their evaluation of residency/fellowship programs, Review Committees will look at the
overall impact of at-home call on resident/fellow rest and personal time.
