
Accreditation Council for Graduate Medical Education
2014-2015 Annual Report Building Momentum

We improve health care
and population health by
assessing and advancing
the quality of resident
physicians’ education through
accreditiation.
We imagine a world
characterized by:
• a structured approach to
evaluating the competency
of all residents and fellows;
• motivated physician role
models leading all GME
programs;
• high-quality, supervised,
humanistic clinical
educational experience,
with customized formative
feedback;
• residents and fellows
ahieving specialty-specific
proficiency prior to
graduation; and
• residents and fellows
prepared to become
Virtuous Physicians who
place the needs and well-
being of patients first.
• Honesty and Integrity
• Excellence and Innovation
• Accountability and
Transparency
• Fairness and Equity
• Stewardship and Service
• Engagement of
Stakeholders
• Foster innovation and
improvement in the
learning environment
• Increase the accreditation
emphasis on educational
outcomes
• Increase efficiency
and reduce burden in
accreditation
• Improve communication
and collaboration with key
external stakeholders
• Customer Focus
• Integrity/Ethics
• Results Focus
• Teamwork
VisionMission Values
Strategic
Priorities
Core Staff
Values
About the Accreditation Council
for Graduate Medical Education
and ACGME International
The Accreditation Council for Graduate Medical Education (ACGME)
is a private, non-profit organization that reviews and accredits
graduate medical education (residency and fellowship) programs,
and the institutions that sponsor them, in the United States.
The ACGME was established in 1981 from a consensus in the
academic medical community for an independent accrediting
organization. Its mission is to improve health care and population
health by assessing and advancing the quality of resident physicians’
education through accreditation. Accreditation is achieved through
a peer-review process overseen by volunteer physicians making
up 30 Review Committees that annually evaluate the specialty and
subspecialty programs and Institutions in their respective disciplines
for adherence to established Common, Program, and Institutional
Requirements. One Recognition Committee, the Osteopathic
Principles Committee, confers Osteopathic Recognition upon
any ACGME-accredited program providing requisite training in
Osteopathic Principles and Practice.
The ACGME’s member organizations are the American Board of
Medical Specialties, American Hospital Association, American
Medical Association, Association of American Medical Colleges,
the Council of Medical Specialty Societies, the American
Osteopathic Association, and the American Association of
Colleges of Osteopathic Medicine.
ACGME International (ACGME-I), an LLC of the parent organization
ACGME, arose consequent to petitioning by governments and
institutions that the ACGME extend its accreditation model
internationally. It is funded through contracts with individual
ministries of health or institutions. The ACGME-I mission, though
similar to that of the ACGME, focuses on improving the quality of
health care specific to each individual country’s need.

Year In ReviewIntroduction Features
Statistics
& Financials Lists
01
02
03
06
14 23
07
16 27
09
12
17
19
2109
13
29
30
32
39
Message from the CEO
Message from the Chair
of the Board of Directors
Department of
Accreditation Services
Department of
Field Activities
Department of Education
Journal of Graduate
Medical Education
Council of Review
Committee Residents
Milestones Department
Reaches Early Milestones
in the Next Accreditation
System
Statistical Highlights
2015 ACGME Awards
Timeline: The Next
Accreditation System
ACGME International
Making an Impact
Board of Directors
Review/Recognition
Committees and Accredited
Specialties
ACGME Staff Listing
Record Setting Attendance
at the 2015 Annual
Educational Conference
2014 Financial Report
Clinical Learning Environment
Review Program
Council of Review
Committee Chairs
Review/Recognition
Committee Members
www.acgme.org | 2014-2015 ACGME Annual Report

2014-2015 ACGME Annual Report
1
Academic Year 2014-2015 was a
productive one for the ACGME,
and one in which projects
that spanned years came to
fruition. The fulllment of the
Outcome Project, rst outlined
in the Journal of the American
Medical Association in 1978,
manifested in successful
creation and implementation
of the Milestone Project. Every accredited specialty
and subspecialty now has articulated in behavioral
terms the key elements of the six domains of clinical
competency that should be evaluated in each
resident or fellow in the discipline, and has described
observable developmental steps, called Milestones,
in each key element. The momentum generated by
this effort is profound. For the rst time, across each
specialty, there is agreement about the core skills
and competencies that are important and shared
by all physicians in that discipline. Specialties now
have the opportunity to evaluate the effectiveness of
their educational effort at a national level, and tools
to introduce new “competencies” as their disciplines
evolve. Programs will be able to compare the progress
of their residents and fellows over time to national
cohorts in the same discipline.
Whether at the specialty society level, or the program
level, interest in excellence in educational outcomes
and effective evaluation has been energized. This
concentration on effective achievement of outcomes
in our graduates has re-invigorated the graduate
medical education (GME) effort in the United States,
and we hope to demonstrate the salutary benets of
this effort in the effectiveness of our graduates in their
service to the public.
The Next Accreditation System (NAS) was fully
instituted across all specialties in 2014-2015 with
the successful implementation across the Phase II
specialties. Extensive training and preparation of the
Review Committees was completed, and accreditation
decisions were rendered for all programs. The next
step in implementation and renement of the NAS
is to accelerate the accreditation process, moving
it earlier in the academic year, to permit earlier
dissemination of national data back to programs to
facilitate continuous quality improvement efforts.
The Clinical Learning Environment Review (CLER)
Program, envisioned in 2010 during the deliberations
of a national committee formed to advise the ACGME
on patient safety, completed its rst cycle of evaluation
of the principle training site of nearly 300 institutions
sponsoring residency and fellowship programs.
The ndings, now being compiled, will guide the
nation’s efforts toward enhancing the clinical learning
environment for GME. Our goals are enhancement
of the safety and quality of clinical care rendered
both today in the teaching environment, as well as
tomorrow in the future practice of our graduates,
and removal of health care disparities while ensuring
the modeling of professionalism and effacement of
self-interest among our faculty, staff members, and
graduates. The ACGME’s efforts in enhancement of
the clinical learning environment have been joined
by other organizations with similar goals. A national
alliance, the National Coalition for the Improvement
of the Clinical Learning Environment (N-CICLE), has
emerged, providing an opportunity for the efforts of
the ACGME to be multiplied, and positive changes
accelerated, through shared efforts.
A single accreditation system for all GME came
to fruition in 2014-2015. After more than 15 years
of intermittent discussion, and three years of
concentrated efforts in the latest round of negotiations,
the American Osteopathic Association (AOA) and the
American Association of Colleges of Osteopathic
Medicine (AACOM) joined the ACGME as Member
Organizations after a unanimous afrmative vote by
the ACGME’s ve allopathic Member Organizations
to approve the bylaws changes required to make
this a reality. For the rst time in nearly 125 years,
allopathic and osteopathic medicine have formally
come together to oversee the education of the
entire physician cohort being prepared to serve the
American Public.
As the backdrop to these important advances,
the ACGME Board of Directors approved a new
strategic plan for the organization. The result of a
two-year in-depth scenario planning process, the six
strategic directions and 15 strategies are designed to
prepare the ACGME to support and ensure that the
physicians of the future are well prepared, to uphold
the ACGME’s responsibilities as a Public Trust, and
to fulll our professional responsibility to prepare the
next generation of physicians to serve the American
Public.
These efforts and many others are outlined in the
pages of this report. The successes achieved are the
result of the more than 300 volunteer physicians and
members of the public who serve on the ACGME’s
31 Review/Recognition Committees and the Board
of Directors, the nearly 200 dedicated professionals
who make up the administration and staff of the
ACGME, and the more than 300 individuals from
the profession and beyond who participated in the
ACGME’s strategic planning process. The efforts of
these individuals are a microcosm of the efforts of
the more than 150,000 physician faculty members,
tens of thousands of nurses and other professionals,
administrators, and more than 120,000 residents
and fellows in ACGME-accredited programs who are
teaching, learning, and caring for the American Public
each and every day.
Respectfully submitted,
Thomas J. Nasca, MD, MACP
Chief Executive Ofcer
Message from the CEO
INTRODUCTION

2014-2015 ACGME Annual Report
2
The ACGME and graduate
medical education (GME)
as a whole have been on a
remarkable and accelerating
path of change. With the full
implementation of the Next
Accreditation System, the
promulgation and application
of the Milestones, the
development and roll-out of the Clinical Learning
Environment Review (CLER) Program, and the
critically important work of coming together with
the American Osteopathic Association (AOA)
and the Association of American Colleges of
Osteopathic Medicine (AACOM)—establishing
a single system of accreditation—the medical
profession and society’s expectations of it have
entered a time of great transition.
Even as we execute these changes within the GME
community, there is an array of corresponding
and at times confounding changes in the
greater environment that impacts us. Among
these changes are: Medicaid expansion; federal
scrutiny of GME funding; workforce shortages
across all domains; and growing demands
on our faculty. All of these have vast potential
consequences for residency and fellowship
programs and GME.
This is one of the most amazing times in human
and medical history. Fortunately for us, we have
the great privilege of witnessing and contributing
to the management of this incredible change.
Advances in the clinical applications of molecular
medicine alone promise to offer more therapies
and cures to disease and human suffering than
could have been imagined just two decades ago.
The progress of information systems and clinical
informatics increasingly enables the harvesting
of benets from decades of investment through
deployment of predictive medicine applications
while improving the safety of health care.
Greater transparency in the practice of medicine
and in medical education is a large part of this
evolution. The Milestones provide tangible
evidence of clinical competence in learners.
CLER forces evaluation of care and patient safety
while facilitating improvement and attention to
problem areas. We are changing the way we do
what we do, and in doing so, are helping doctors
become better doctors, while providing patients
with better care.
On the international stage we see tremendous
growth coupled with a desire and dedication to
the standards and principles of better outcomes,
greater patient safety, and improved care overall
no matter where we are on the globe. What this
says about the work and mission of the ACGME
and ACGME International, and about its stewards,
is nothing short of remarkable.
The momentous history-changing agreement
among the ACGME, AOA, and AACOM only
further conrms this is not just a moment in
history, but an evolution. We welcome our newest
members with open arms, and celebrate this
exciting development: the establishment of a
single accreditation system for all of GME.
The momentum from all of these efforts both
domestically and internationally is driving toward
a broad embrasure of the highest achievable
standards in medicine.
Graduates of accredited programs are the leaders
of tomorrow, and along with their interprofessional
teammates, will build systems that ensure the
care provided by attending physicians and
learners alike is safe, timely, effective, efcient,
equitable, and patient-centered. If we do this
and do this well, we will build a great future for
graduate medical education.
Mr. John Duval
Chair, Board of Directors
This is one of the
most amazing times in
human and medical history.
Message from the Chair of the Board of Directors

2014-2015 ACGME Annual Report
3
Institutional Accreditation in
Transition to the Next Accreditation System
The academic year and the transition to the Next
Accreditation System (NAS) for ACGME-accredited
Sponsoring Institutions began with implementation
of revised Institutional Requirements that became
effective on July1, 2014. The revision represented
an overall simplication and reorganization
of the previous version of the Requirements.
However, several new requirements—including
implementation of an Annual Institutional Review
of a Sponsoring Institution’s own performance
with regard to its educational mission; the
introduction of a Special Review process by the
Graduate Medical Education Committee (GMEC);
and an expectation for oversight of the programs’
Annual Program Evaluations—emphasize quality
improvement, a cornerstone of the NAS. A new
section focused on the Resident Learning and
Working Environment reects concern for how
residents and fellows are integrated into the setting
in which patient care is provided.
Until recently, institutional compliance for smaller
institutions with only one accredited specialty
program was assessed by the specialty-specic
Review Committee concurrent with the program
site visit. In the NAS, and with the maturation
of the institutional review process, the ACGME
Board delegated responsibility for all institutional
accreditation decisions to the Institutional Review
Committee (IRC).
In 2014-2015, the IRC approved 28 new Sponsoring
Institutions. It also conducted full reviews of
institutions which had received Initial Accreditation
under the prior accreditation system, and continued
to monitor some Sponsoring Institutions through
review of progress reports.
The IRC plans to begin NAS review of annual
institutional data in 2015-2016. The Committee
continues to work closely with ACGME leadership,
and with the Department of Data Analysis and
Applications in particular, to identify the data
elements it will review annually for all Sponsoring
Institutions. In 2015-2016, the IRC will collaborate
with the Department of Field Activities to develop
the process for the institutional self-study and the
10-year accreditation site visits that will begin in
approximately two years.
Reflections on Year One of the
Next Accreditation System
July 1, 2014 marked the dawn of the rst round
of accreditation decisions under the NAS for
Phase II specialties. A time of both excitement
and unease, anticipation of great success
was offset by concerns related to the greater
unknown, specically, the shift in the approach
from an episodic (1-5-year) to an annual program
accreditation review.
The rst set of annual accreditation data for Phase
II programs was summarized and reported to the
respective Review Committees in Fall 2014. The
outcome data included information corresponding
to the 2013-2014 academic year, Resident and
Faculty Survey results, Board pass rates, Case
Log data (as applicable), and scholarly activity. A
visualization software program was used by the
executive directors to compare the data against
decision rules the Review Committees developed
to guide the work of the NAS.
Under the previous accreditation model, Review
Committees focused equally on high functioning
programs and those deemed underperforming
(e.g., those with continued areas of non-
compliance in critical areas as identied by
the Review Committee). The new model allows
Review Committee staff to use Committee-
determined criteria to identify high functioning
programs for Continued Accreditation, thereby
allowing the Committees to focus attention on the
underperforming programs.
Department of Accreditation Services
YEAR IN REVIEW
In 2014-2015, the IRC approved
28 new Sponsoring Institutions
The 2014-2015 year was especially momentous for the Department of Accreditation Services (DAS). The Next Accreditation System was fully implemented
for all core specialties while department staff also prepared for review of new institutional and program as well as Osteopathic Recognition applications
as part of the historical transition to a single accreditation system for all graduate medical education (GME). The scope of some of these activities are
addressed in the following vignettes.

2014-2015 ACGME Annual Report
4
In the new system, the Committees review
programs by examining annual program data
submitted via the Accreditation Data System (ADS)
in comparison to the Program Requirements, and
by carefully evaluating responses to previous
citations.
In the rst round of reviews, a number of
programs received Continued Accreditation with
citations or areas for improvement (AFI). AFIs
are new in the NAS, and unlike citations, do not
require programs to provide a response in ADS.
The expectation is that AFIs will be monitored
locally (by the program director and GMEC) so
as to avoid future citations. Although AFIs do not
require a formal response, the Review Committee
is able to track them to determine if they have
been resolved.
Upon conclusion of the rst year of the NAS for
Phase II specialties, some Committee members
said they missed the days when they reviewed
high-functioning programs, identied best
practices, and provided commendations to their
peers. Overall, the benets of the NAS were
widely recognized and it was found to be an
efcient and effective system. Further, the Review
Committees’ initial unease was assuaged by their
ability to provide critical feedback to programs
earlier to assist them in achieving substantial
compliance with the Requirements.
Department Emphasizes Outreach and
Communication
Individuals in the DAS communicate daily with
the programs and institutions accredited by
the ACGME to answer questions and respond
to concerns. On a regular basis, they also
leave the ofce and go into the community to
provide educational opportunities for program
coordinators, program directors, and designated
institutional ofcials (DIOs). In 2014-2015, a time
of great change, the Review Committee Executive
Directors and the Senior Vice Presidents for the
DAS sections (Hospital-based, Institutional,
Medical, Osteopathic, and Surgical) participated
in meetings and workshops across the country
for coordinators in specic specialties, regional
coordinator groups such as GME Action,
program director meetings, program director
workshops, and various gatherings of DIOs. The
Executive Directors, often in conjunction with the
Review Committee Chairs, allot time during these
sessions for scheduled one-on-one meetings
with program representatives to answer specic
questions and concerns about their programs.
2014-2015 was particularly busy for DAS staff
because of the implementation of the NAS, as
well as the approaching transition to a single
accreditation system for all of GME. In addition to
making presentations to all of the groups noted
above representing currently accredited programs
and institutions, staff members were also meeting
with and educating osteopathic colleagues about
the ACGME and the accreditation processes. To
that end, presentations were made at the ACGME
Annual Educational Conference, the Osteopathic
Medical Education Conference, the combined
American Academy of Colleges of Osteopathic
Medicine/Association of Osteopathic Directors
and Medical Educators Conference, several
statewide osteopathic GME meetings, and for a
number of program director groups and specialty
college meetings. The Department also produced
more than 20 specialty-specic and general
webinars regarding the transition to a single GME
accreditation system.
Introducing a Unique Subspecialty to the
ACGME Accreditation Process
At the time Clinical Informatics was approved
as a new subspecialty for certication by the
American Board of Medical Specialties and
for accreditation by the ACGME in 2012, there
were over 30 programs afliated with medical
schools, and over 1400 self-identied physician
informaticians. The eld met the denition of
clinical “by providing clinical decision support
and information systems…” but was different
enough from other clinical programs that a new
paradigm was used to review the specialty.
After developing the Program Requirements,
soliciting feedback, and incorporating revisions,
the rst applications for new clinical informatics
programs were received for accreditation review
in 2014. These programs are reviewed by the
nine Review Committees representing the
specialties with the most practitioners today
(anesthesiology, diagnostic radiology, emergency
medicine, family medicine, internal medicine,
medical genetics, pathology, pediatrics, and
preventive medicine) and predicted to most likely
sponsor future programs. Review Committees
are familiar with many subspecialties and their
Program Requirements, but because of the
initial need to learn more about this area and
provide for a consistent background, an Advisory
Group was formed to pre-review programs.
The informaticians comprising this group’s
Overall, the benefits of the NAS
were widely recognized and it
was found to be an efficient and
effective system
continued on next page

2014-2015 ACGME Annual Report
5
membership volunteered many hours to learn the
ACGME review process and develop a special
form to use in review of the informatics-specic
section of the application. The completed pre-
reviews were subsequently sent to the Review
Committees for full review. As the Review
Committees gain experience and familiarity with
clinical informatics, it is anticipated that the need
for pre-reviews will eventually decrease. Ten
programs were accredited in this rst year, with
more to follow as clinical informatics grows and
adds a new expertise to the scope of GME.
ACGME Osteopathic Accreditation Section in
Place
Osteopathic Accreditation is new for the
ACGME. This section of the DAS was developed
in association with the transition to a single
accreditation system for all GME. Since the
agreement among the ACGME, American
Osteopathic Association (AOA), and American
Association of Colleges of Osteopathic Medicine
(AACOM) was announced on February 26, 2014,
the process of this transition has moved at a fast
pace. The Memorandum of Understanding (MOU)
approved by all three organizations gives AOA-
approved institutions and programs a specic
window of time during which they may apply for
and obtain ACGME accreditation. Institutions
began applying for accreditation on April 1, 2015,
and programs could submit applications beginning
July 1, 2015.
The February 2015 meeting of the ACGME Board
of Directors was historic, with the addition of
osteopathic representatives to the Board’s
membership (four representatives were added,
with two nominated by the AOA and two by
AACOM).
New Board Members:
• Karen J. Nichols, DO (nominated by AOA)
• David Forstein, DO (nominated by AOA)
• Gary Slick, DO (nominated by AACOM)
• Clinton Adams, DO (nominated by AACOM)
Two additional osteopathic directors (one each
from the AOA and AACOM) will be added in 2018
and 2020 (eight will be the total members added
by the 2020 conclusion of the MOU). Osteopathic
members also joined each Review Committee for
specialties that were found in both the ACGME-
accredited and AOA-approved arenas.
Two new committees—the Review Committee
for Osteopathic Neuromusculoskeletal Medicine
[(ONMM; a new specialty for the ACGME) that
reviews and approves new ONMM programs],
and the Osteopathic Principals Committee (OPC)
that reviews and approves ACGME-accredited
programs for Osteopathic Recognition—
have been formed. The OPC and the Review
Committee for ONMM each met for the rst time
in Fall 2014, and have since developed, vetted,
and implemented Requirements for Osteopathic
Recognition and accreditation in ONMM. The
timeline for both committees to create these new
requirements was unprecedentedly short, and the
committee members and ACGME staff members
who supported them (notably Kathy Malloy and
Tiffany Moss) were instrumental in this success.
Both sets of Requirements were approved at
the February meeting of the Board, and both
committees now meet on a regular schedule.
Milestones for Osteopathic Recognition and for
ONMM are in development, and it is anticipated
they will be ready for approval in September 2015.
The Osteopathic Accreditation section’s
responsibilities include stafng the ONMM and
Osteopathic Principles committees and working
collaboratively with all ACGME departments. The
staff includes a senior vice president, Osteopathic
Accreditation (Dr. Lorenzo Pence), an executive
director, Osteopathic Accreditation (Tiffany
Moss), and an executive assistant (Julia Weigle).
The ACGME and AOA celebrate the end of
Academic Year 2014-2015 with much to report
on the transition to a single GME accreditation
system, including decisions from most Review
Committees that would allow AOA-boarded
physicians to be approved as program directors
if other program director requirements are met.
The AOA has 1,247 approved programs and
fellowships, 163 of which are dually accredited by
the ACGME, and 1,084 of which can now move
forward with the application process for ACGME
accreditation. The 2015-2016 year will be an
exciting one, as institutions and programs move
forward pursuing ACGME accreditation and
Osteopathic Recognition.

2014-2015 ACGME Annual Report
6
2014-2015 was an important year for the Department of Field Activities and the accreditation eld representatives. Major efforts included the second year
of site visits in the Next Accreditation System (NAS), and the design and development of the site visit components of the ACGME self-study, as well as
related to the transition to a single accreditation system for graduate medical education (GME).
Department of Field Activities
The Department coordinated all aspects of
program and institutional accreditation site visits,
including scheduling and logistics, site visit
reporting, quality improvement, and eld staff
professional development.
2014-2015 marked the second year of site visits in
the NAS, and eld representatives conducted 212
site visits for programs with full accreditation. The
majority, 168 were “data-prompted” visits that
were scheduled because the review of the annual
data suggested a possible problem for further
exploration through a site visit. An additional
44 were scheduled at the request of the Review
Committees for concerns not arising directly out
of the annual data.
Accreditation eld representatives also conducted
site visits for new program applications, programs
transitioning at the end of the period of Initial
Accreditation, and Sponsoring Institutions, visits
to assess the merits of a complaint, and visits for
international programs for ACGME-I.
The Department developed new site visit
protocols for site visits of osteopathic programs
with pre-accreditation status in the transition
to a single GME accreditation system, as well
as a voluntary non-accreditation site visit for
programs with an ACGME self-study scheduled
between April 2015 and January 2017, and for the
subsequent 10-year site visit for these programs.
By June 30, 2015, a total of 253 programs in Phase
I of the NAS had volunteered for a voluntary self-
study pilot visit.
2014-2015 also saw collaboration with the
Department of Accreditation Services to continue
to rene the protocols for data-prompted site
visits. Renements aim to enhance the utility of
the information for the Review Committees, with a
special focus on exploring and diagnosing areas
of potential concern identied during the review
of the annual data.
Professional development for eld representatives
in 2014-2015 focused on aspects of new site visit
types, including data-prompted visits in the NAS,
the self-study pilot visits, and visits to osteopathic
programs.
An ongoing focal area for professional
development related to the new role of the eld
representatives in offering suggestions or ideas
for innovative practices found in the medical
education literature or through other programs
and institutions successful in creating an effective
working and learning environment.

2014-2015 ACGME Annual Report
7
The Department of Education serves the ACGME mission to meet the needs of over 9,600 programs and 700 Sponsoring Institutions that prepare over
120,000 residents and fellows to embark on the path of mastery to effectively meet the health and health care needs of the public. The department
accomplishes this mission through dissemination of knowledge and furthering skill development, often acting as a facilitating body serving and collaborating
with other departments within the ACGME and with appropriate outside organizational and individual collaborators.
Department of Education
The department’s division of Educational
Activities, led by Director Debra Dooley and
staffed by Educational Project Manager Jessalynn
Watanabe; Continuing Medical Education
Administrator Laura Barbo; Registration
Specialist Andrea Rio, MA; Educational
Administrator Lauren Wojnarowski; and
Educational Project Associate Victoria Shaffer,
designs, develops, produces, and evaluates the
ACGME’s educational activities, including the
ACGME Annual Educational Conference, various
ACGME workshops and workshop series, the
Baldwin Lecture Series, the ACGME Webinar
Series, some of the CLER Program’s educational
initiatives, and more.
The 2015 Annual Educational Conference was a
phenomenal success on multiple levels, reecting
years of vision, development, and collaborative
efforts (see article, p.16).
ACGME Webinar Series
The ACGME Webinar Series began during
2013-2014 with presentations specic to the
implementation of the Next Accreditation System
for program directors, designated institutional
ofcials (DIOs), and coordinators, and has
reached an audience of 17,212 participants to
date. These highly evaluated sessions were
developed by ACGME Senior Vice Presidents
Mary Lieh-Lai, MD; Louis Ling, MD; Ingrid
Philibert, PhD; John Potts, MD; and Kevin Weiss,
MD, and were delivered in collaboration with the
Executive Directors and physician leaders of the
Review Committees. In 2014-2015, the Webinar
Series expanded to other topics of interest,
including the transition to a single accreditation
system for all graduate medical education (GME),
the Milestones, and the CLER program.
Workshops
Ten Basics of Accreditation for New Program
Coordinators workshops were delivered with
a total registration of 280. These workshops
provide new coordinators with the opportunity
to meet their specialty’s Review Committee staff
members and other members of the ACGME’s
senior staff and administration, while learning the
nuts and bolts of ACGME accreditation.
The Baldwin Seminar Series, named after Senior
Scholar in Residence DeWitt C. Baldwin Jr., MD,
is a series of didactic seminars held throughout
the year at the ACGME ofces. The goal of the
Baldwin Series is to develop an educational
interchange between colleagues that will
stimulate creative, innovative thinking on topics
pertinent to GME. Speakers are drawn from
across the country, and in 2014-2015 included
ACGME Accreditation Field Representative Serge
Martinez, MD, JD; Liselotte Dyrbye, MD, MHPS,
FACP; ACGME Board member Kenneth Ludmerer,
MD; F. Daniel Duffy, MD; Frederic W. Hafferty,
PhD; and Robert Englander, MD, MPH. Subjects
covered included burnout, the history and future
of residency education, the Hidden Curriculum,
and Entrustable Professional Activities.
The Developing Faculty Competencies in
Assessment Workshop was designed by Senior
Vice President, Milestone Development and
Evaluation Eric Holmboe, MD, MACP. This six-day
interactive workshop, limited to 30 participants,
was given twice in 2014. The program was highly
rated and successful, and more sessions are
scheduled for 2015-2016.
CLER Conversations is a two-day workshop
developed by Senior Vice President, Institutional
Accreditation Kevin Weiss, MD and Vice President,
CLER Program Robin Wagner, RN, MHSA. This
innovative, interactive workshop bring teams of
senior executive leaders of teaching hospitals
and medical centers of ACGME Sponsoring
Institutions to join in a facilitated discussion
focused on strategic planning. The program
was successfully piloted in 2014-2015, and two
workshops are planned for 2015-2016.

2014-2015 ACGME Annual Report
8
The department convened a Joint Steering
Committee composed of three members of the
allopathic community and six members of the
osteopathic community to assess the educational
needs of and design educational activities for
osteopathic institutions and programs entering
the ACGME accreditation process in the transition
to a single GME accreditation system. Starting
with comprehensive interviews of Osteopathic
Post-doctoral Training Institutes (OPTIs), the
team developed educational activities at the
major educational meetings of the American
Osteopathic Association, Association of
American Colleges of Osteopathic Medicine, and
the ACGME, and created a series of specialty-
specific webinars for all specialties entering the
single accreditation system.
Future planned activity includes the development
of an advanced coordinator training that would
go beyond the basics of accreditation, as well
as new educational initiatives with the CLER and
Milestones teams.
Office of Resident Services
The Ofce of Resident Services works closely
with residents, program directors, DIOs, and the
Review Committees to help them navigate the
concerns and complaints process and provide
essential ACGME support. Senior Associate
Amy Beane also staffs the Council of Review
Committee Residents (CRCR), made up of the
resident members of each of the Review and
Recognition Committees. The CRCR (see article,
p.13) advises the ACGME and Board of Directors
on issues of concern important to the ACGME,
providing the resident/fellow perspective.
Senior Scholars in Residence
The Senior Scholars in Residence, led by Senior
Scholar Dr. Baldwin, continues its stellar work
of discovery and dissemination. During 2014-
2015, Paul Rockey, MD; Joanne Schwartzberg,
MD; and Nicholas Yaghmour, MPP conducted
research and provided vital insight in a number
of important areas, including resident well-being,
interprofessional team-based training, physician
workforce issues, and health policy.
A longitudinal survey asking questions related to
resident well-being conducted by the team and
led by Mr. Yaghmour has yielded responses from
approximately 20,000 residents per year since
2013.
Leadership Skills Training Programs for
Chief Residents
Robert Doughty, MD, PhD, the senior scholar
for Experiential Learning and Leadership
Development, has conducted multi-day, multi-
specialty leadership training programs for 2,000
chief residents from all specialties since 2010.
Nine workshops were conducted in 2014-2015, all
lled to capacity and evaluated extremely highly.
For the rst time the ACGME conducted two chief
resident workshops internationally, one in Abu
Dhabi and one in Singapore. Both were delivered
by Dr. Timothy P. Brigham and Dr. Doughty
and were eye opening experiences for both
the ACGME-I facilitators and the international
participants. It is expected that the sessions
will be offered again in 2015-2016. A pilot test
continues to train facilitators for these Leadership
Skills Training Programs for Chief Residents,
resulting in nine “apprentice” facilitators working
in 2014-2015.
As the department looks forward to 2015-2016,
continued program growth development is on the
horizon.
A Distance Learning Director has been identied.
Anne Gravel Sullivan, PhD will lead the ACGME’s
distance learning activities. She brings a special
blend of content expertise and understanding
of the ACGME to this position that makes
her uniquely qualied to lead these efforts.
Dr. Sullivan will continue to also serve as the
Executive Director for the Review Committees for
Anesthesiology and the Transitional Year as she
begins her new responsibilities.
In conjunction with the leadership of the
ACGME-I, the Department of Education will build
a systematized and coordinated educational
arm to meet the needs of its international
colleagues. Included in this effort is the creation
of an ACGME-I Conference to be conducted in
Singapore in 2017.
Drs. Brigham and Doughty with participants from the Leadership Skills
Training Program for Chief Residents conducted in Abu Dhabi.

2014-2015 ACGME Annual Report
9
Program Concludes First Cycle of Visits—In March 2015, the CLER Program completed the rst cycle of visits to participating sites of Sponsoring
Institutions with three or more core residency programs. This rst cycle included visits to 297 of the nation’s teaching hospitals and medical centers.
The Journal of Graduate Medical Education (JGME) is the ACGME’s peer-reviewed publication. Editorially independent, JGME was inaugurated in 2009
to disseminate scholarship and promote critical inquiry to inform and engage the graduate medical education community. JGME is published quarterly
and is provided to more than 10,000 residency and fellowship program directors, designated institutional ofcials, and members of the ACGME’s Review
Committees and Board of Directors.
Clinical Learning Environment Review
Journal of Graduate Medical Education
With the close of Cycle 1, the CLER Program is in
the process of analyzing the data and drafting a
national report for release later in 2015. The report
will present aggregate, de-identied data that
highlight key ndings across the six focus areas.
Simultaneous with preparing the report, the CLER
Program is exploring opportunities to partner
with other organizations and engage teaching
hospitals and medical centers in targeted efforts
to better integrate graduate medical education in
strategic planning to improve patient safety and
health care quality.
In April 2015, the CLER Program began Cycle 2.
In this next round, the CLER team is conducting
repeat visits to the hospitals and medical centers
visited in Cycle 1 to assess each site’s goals and
priorities resulting from the initial CLER visit and
progress towards those goals. The protocol for
Cycle 2 has been updated to closely align with
the CLER Pathways to Excellence. Cycle 2 also
includes initial visits to the approximately 400
small and single-program Sponsoring Institutions
(those with one or two core residency programs).
The Journal’s rst aim is to be a leading peer-
reviewed journal in graduate medical education.
Evidence of success in meeting this aim includes:
• PubMed/MEDLINE indexing in June 2015
• A steady increase in the rejection rate from
less than 50% during the early phase of the
Journal, to 78% in 2014
• A 30-member Editorial Board under the
direction of an Editor in Chief and three
Deputy Editors. The Editorial Board includes
US members and representatives from
Canada, the Netherlands, the United Kingdom,
the United Arab Emirates, Germany, and
Singapore, as well as residents and fellows.
Members have broad, diverse expertise,
including in the areas of assessment, faculty
development, survey design, qualitative
research, and quality and safety of care.
• Business oversight of the Journal provided
by a subcommittee of the ACGME’s Board of
Directors that includes a chair, Dr. Kenneth
Ludmerer, who is a noted medical historian
and author

2014-2015 ACGME Annual Report
10
The second aim is to promote scholarship and
enhance the quality of research in the eld, with
success in a number of key areas:
• 812 manuscripts were submitted in 2014,
which represents a sizable increase over the
just over 500 manuscripts submitted in 2013.
International submissions have grown to 10%
of all submissions.
• JGME
works with trainees and junior faculty
members, as well as with other authors new
to academic publishing, through workshops,
practical guidance for authors, and pre-
submission review and suggestions on
manuscripts from trainees and new authors.
• Journal-sponsored workshops and lectures
at national and international meetings seek
to enhance authors’ skills, and have drawn
from 50 to more than 100 participants each.
In addition to general topics in scholarly
publishing, sessions in 2014–2015 covered
topics including survey design and use of
different assessment methods in research in
graduate medical education. An international
session on research design and submissions
to scholarly journals was also conducted.
The Journal’s third aim is to disseminate evidence-
based approaches related to educational
curricula and content, assessment, and the
learning environment. Evidence of success in
meeting this aim includes:
• Online content received 204,604 web hits in
2014 compared to 50,857 for 2010, the rst full
year of publication; dissemination of content
through electronic tables of content with direct
links to articles.
• Use of social media, particularly Twitter
(follow @JournalofGME), to raise community
awareness of content and to stimulate
discussion.
• Selected articles relevant to residents/fellows
are made available via an open-access page,
with commentaries by members of the ACGME
Council of Review Committee Residents.
• Online journal clubs with two major
organizations in medical education to expand
JGME outreach to the faculty and resident/
fellow community, with topics of general
interest, such as residents as teachers and
resident well-being.
• New approaches to journal metrics offer
authors and readers information about the use
of content beyond traditional citations.
The fourth JGME aim is to contribute to new
knowledge that enhances the competence
of residency/fellowship graduates and their
effectiveness in providing safe and high-quality
patient care. Evidence of success in meeting this
aim includes:
1. JGME has published early seminal work
on the development and validation of the
educational Milestones, and continues to
publish articles on the validation of the
Milestones and on their use in resident/fellow
assessment, including studies that seek to
develop best practices for Milestone use.
2. Survey tools, research protocols, and other
practical information are made available as
online supplemental data, so these resources
are accessible to educators and researchers.
3. A section in each issue is devoted to updates
on key ACGME initiatives, with these pages
clearly distinguished from peer-reviewed content.
In 2014–2015, this section included updates on
the Clinical Learning Environment Review (CLER)
program, ACGME strategic planning, initiatives in
residency programs already in keeping with the
recommendations in the Institute of Medicine’s
report Graduate Medical Education That Meets
the Nation’s Health Needs, and the ACGME
program self-study.
continued on next page

2014-2015 ACGME Annual Report
11
Journal of Graduate Medical Education
Editorial Board
Gail M. Sullivan, MD, MPH
Editor-in-Chief
University of Connecticut
Anthony R. Artino Jr., PhD
Deputy Editor
Uniformed Services University of the
Health Sciences
Deborah Simpson, PhD
Deputy Editor
Aurora UW Medical Group
Lalena M. Yarris, MD, MCR
Deputy Editor
Oregon Health & Science University
Kathryn M. Andolsek, MD, MPH
Associate Editor
Duke University School of Medicine
Hans Arora, MD, PhD
Resident Member
Cleveland Clinic Foundation
Peter J. Carek, MD, MS
Associate Editor
University of Florida College of Medicine
Katherine C. Chretien, MD, FACP
Associate Editor
Washington DC VA Medical Center,
George Washington University School of Medicine
and Health Sciences
Joseph B. Cofer, MD, FACS
Associate Editor
University of Tennessee College of Medicine
Thomas G. Cooney, MD
Associate Editor
Oregon Health & Science University
Denise Dupras, MD, PhD
Associate Editor
Mayo Clinic, Rochester
Cameron Escovedo, MD
Resident Member
Mattel Children’s Hospital, UCLA
Michael Hann, MD LT MC USN
Resident Member
Naval Medical Center San Diego
Halah Ibrahim, MD, MEHP
Associate Editor
Tawam Hospital, Abu Dhabi, United Arab Emirates
Jonathan Ilgen, MD, MCR
Associate Editor
University of Washington
S. Barry Issenberg, MD, FACP
Associate Editor
University of Miami Miller School of Medicine
Barbara G. Jericho, MD
Associate Editor
University of Illinois Medical Center at Chicago
M. Douglas Jones Jr., MD
Associate Editor
University of Colorado School of Medicine
Dotun Ogunyemi, MD, FACOG, MFM
Associate Editor
Oakland University William Beaumont
School of Medicine
Lawrence Opas, MD
Associate Editor
USC/LAC+USC Healthcare Network
Harm Peters, MD, PhD
Associate Editor
Charité–Universitätsmedizin, Berlin, Germany
Joan Sargeant, PhD
Associate Editor
Dalhousie University, Halifax, NS, Canada
Lori A. Schuh, MD, FAAN
Associate Editor
Spectrum Health
Meredith J. Sorensen, MD, MS
Associate Editor
Dartmouth Hitchcock Medical Center
Prof Dame Lesley Southgate, MB, FRCP, FRGGP
Associate Editor
St. George’s University School of Medicine,
London, United Kingdom
Th. J. (Olle) ten Cate, PhD
Associate Editor
University Medical Center Utrecht, Netherlands
Christopher R. Thomas, MD
Associate Editor
University of Texas Medical Branch at Galveston
Travis Paul Webb, MD
Associate Editor
Medical College of Wisconsin
Max Wohlauer, MD
Resident Member
University of Colorado, Denver
Brian Wong, MD
Associate Editor
Sunnybrook Health Sciences Centre,
University of Toronto, Ontario, Canada

2014-2015 ACGME Annual Report
12
Peter Carek, MD, MS, Chair, Review Committee for Family Medicine
Council of Review Committee Chairs
Historically, the Council of Review Committee
Chairs (CRCC) has been an excellent venue for
Review Committees and their chairs to gather
information from the other committees and
organizations associated with graduate medical
education, receive updates and other data from
the ACGME, and discuss topics relevant to
their work and the work of their Committees.
With the introduction and implementation of
the Next Accreditation System (NAS), the work
of the CRCC has changed. Still
a valuable setting for information
gathering and dissemination, the
CRCC’s meetings now also provide
an extraordinary opportunity to
solve problems associated with the
accreditation process and discuss
quality improvement activities that
pertain to graduate medical education
in all disciplines. Additionally, the
meetings have allowed the chairs
to share valuable “lessons learned”
from colleagues from specialties and
Committees at varying phases of
the transition into the NAS, including
unique challenges, or opportunities
for innovation in the efforts to improve
residency and fellowship education.
This enhancement of CRCC activity served as
a model for the work of the Review Committee
for Family Medicine in the efforts to maintain
the momentum of moving to a more quality
improvement-focused approach to program
review. As such, the communication with
residency and fellowship programs has shifted,
more often addressing issues identied as
areas for improvement than citations. So far
the Committee has found that often, we seek a
better understanding and clarication of program
activities prior to rendering a formal citation. The
Review Committee for Family Medicine is hoping
for a more collegial relationship with programs
in this, the Next Accreditation System. We do
not take lightly the great responsibility we have
in reviewing programs and making accreditation
decisions, and our intent is rmly to work
constantly toward program improvement and
educational innovation.
Members of the Council of Review Committee Chairs, September 2014

2014-2015 ACGME Annual Report
13
Council of Review Committee Residents
Providing the Resident Voice in Advancing
Educational Policy
The Council of Review Committee Residents
(CRCR) promotes the mission of the ACGME by
advising on resident matters, graduate medical
education (GME), and accreditation. In January
2015, the current vice chair, Dinchen Jardine, MD,
MS (ENT), was elected chair and will succeed
Timothy Daskivich, MD, MSHPM (Urology) when
his term of service concludes in September.Over
the last year, the Council has focused its efforts on
the topics of physician wellness and mental health
awareness in the GME learning environment, as
well as on leadership training during residency.
Physicians in training are at high risk for burnout
and depression, and early career physicians have
substantially elevated risk of suicide compared
with those in other professions. In November
2015, the ACGME will host a national symposium
on physician well-being that will bring together
GME leadership, scholars, residents, and
program directors to determine how to change
the training environment to promote wellness
during training and beyond. As an adjunct to
this effort, the CRCR wrote an article, published
in the March issue of the
Journal of Graduate
Medical Education (JGME) (http://www.jgme.org/
doi/pdf/10.4300/JGME-07-01-42) that provides a
trainee-level perspective on the resources that
currently exist and those that are lacking in the
learning environment to address this issue. Using
an appreciative inquiry approach, the CRCR
identied several actionable goals for national
policy: (1) to increase awareness of the high
risk of depression during training and thereby
destigmatize it; (2) to build systems to identify and
treat depression condentially; (3) to formalize
peer and faculty mentorship; (4) to promote a
supportive culture within the profession; and
(5) to support research to learn more about the
issue. The CRCR looks forward to partnering with
ACGME leadership to address this critical issue.
The CRCR also devoted effort over the last
year to envisioning ideal systems for formal
leadership training during residency. Because
health care is increasingly carried out by teams of
providers—physicians, nurses, care coordinators,
pharmacists, social workers, nutritionists,
physical and occupational therapists—physicians
must learn to be co-leaders (and team players) in
the clinical environment. Despite this, there is no
formalized training in leadership that is universally
available for residents. The CRCR wrote an
article for the June 2015 issue of JGME (http://
www.jgme.org/doi/pdf/10.4300/JGME-07-02-31)
that calls for a national leadership curriculum for
residents. The Council hopes that this piece will
spark further discussion on developing critically-
needed leadership training in GME.
The CRCR is delighted to play a role in assisting
the ACGME in its visionary efforts to advance
the GME learning environment. We look forward
to continuing to provide the resident perspective
on salient issues within GME to further the
mission of the organization: to improve health
care and population health by advancing the
quality of resident physicians’ education through
accreditation.
Timothy J. Daskivich, MD, MSHPM, Chair, Council of Review Committee Residents
Members of the Council of Review Committee Residents, September 2014

2014-2015 ACGME Annual Report
14
Engagement
In conjunction with full implementation of the Next
Accreditation System (NAS) for all specialties, all
core specialties, and the majority of subspecialties,
reported Milestones data in Academic Year 2014-
2015. In the mid-year reporting period, a total of 7,498
programs reported on a total of 117,548 residents
and fellows (99.96%). Additionally, at the year-end,
7,628 programs reported on 118,360 residents and
fellows for a 99.98% resident level response rate.
Educational initiatives
The Milestones Department successfully piloted a
week-long interactive faculty development course
in assessment. Developing Faculty Competencies
in Assessment: A Course to Help Achieve the Goals
of Competency-Based Medical Education (CBME),
had three successful sessions during the 2014-2015
pilot year, with two in the fall of 2014 and one in the
spring. In all, 73 faculty members from 55 different
institutions and 15 different specialties participated.
The highly interactive course involves multiple
exercises and small-group learning exercises, as well
as a half-day session at the Northwestern Feinberg
School of Medicine simulation center, which allows
the participants to practice their direct observation
assessment and feedback skills working with
standardized patients and residents. This experience
was routinely the highest rated session of the week.
In addition to the direction of Dr. Eric Holmboe,
senior vice president, Milestone Development and
Evaluation, the course also features other major
educational leaders in the eld facilitating some
of the workshops: Dr. Jennifer Kogan, from the
University of Pennsylvania; Dr. William Iobst from
the Commonwealth Medical College; and Dr. Kelly
Caverzagie from the University of Nebraska. In
Academic Year 2015-2016, the ACGME will offer four
sessions of this course in Chicago, and in October will
also pilot a shortened version, focusing on essential
teaching faculty, in collaboration with Drs. Donald
Brady, Sandy Moutsios, and John McPherson of
Vanderbilt University in Nashville, Tennessee.
The Department also produced its rst publication, a
new guidebook for Clinical Competency Committees
(CCCs), in February 2015. The guidebook provides
information regarding the purpose and structure of
the CCC, how to prepare for and run a CCC meeting,
and post-CCC meeting actions, as well as legal
and other considerations. Clinical Competency
Committees: A Guidebook for Programs can
be found in the Milestones section of the ACGME
website. The Milestones Department will continue to
develop educational resources related to assessment
to help program directors in the coming year.
The Listening Tour
The ACGME, as represented by the gure (next page)
of the Professional Self-Regulatory Assessment
System, fully understands that, ultimately,
effective accreditation is highly dependent on
the effectiveness of the residency and fellowship
programs in producing highly competent physicians;
or, in other words, that as an organization, the
ACGME is only as successful in its work as are
the programs it accredits in producing competent
physicians. During 2014-2015, Drs. Holmboe, Stan
Hamstra, and Laura Edgar attended over 25 society
meetings and met with over 30 institutions and
organizations to discuss the Milestones initiative
and provide faculty development. Perhaps more
importantly, staff of the Milestones Department took
the opportunity to conduct informal focus groups
that included, in aggregate, hundreds of program
directors, designated institutional ofcials (DIOs),
and faculty leaders. These rich sessions enabled
department leadership to learn, directly from
the programs, how the Milestones are impacting
programs, including meaningful successes, but also
in terms of challenges in implementing the changes.
This information will be invaluable in making real-
time adjustments in the Milestones system, and
will help to inform what revisions will be important
in the future. The Milestones Department ascribes
Milestones Department Reaches Early Milestones
in the Next Accreditation System
FEATURES
The past year was momentous for the Milestones Department. New staff members in key functions joined the team, the remaining core residency
disciplines entered the Milestones system, and the department launched a number of new activities and collaborations. This report will touch on four major
themes for the past year: engagement, educational initiatives, listening to our stakeholders, and research.
continued on next page

2014-2015 ACGME Annual Report
15
to a philosophy of service and continuous quality
improvement, in alignment with the ACGME’s
placement of importance on these features in the
model for the NAS. As such, these focus groups
are an invaluable and critical demonstration of the
application of that philosophy, and will continue. The
department also invites feedback and comment,
at any time, through the Milestones mailbox:
milestones@acgme.org.
Research
Ongoing research and evaluation of the Milestones
is critically important. The Milestones Department
also recognizes it cannot and should not do the
research and evaluation alone; the best research
and learning will come from robust collaborations.
To that end the Department launched two important
advisory committees: an analytic group and a
CCC group. The Analytic Advisory Group includes
Drs. John Norcini of FAIMER, Ara Tekian and Rachel
Yudkowsky of the University Illinois Chicago, and
Reed Williams of Indiana University, all highly
regarded measurement experts. The Analytic
Advisory Group is supported by Dr. Hamstra, Senior
Vice President, Applications and Data Analysis
Ms. Rebecca Miller, and Outcomes Assessment
Project Associate Dr. Kenji Yamazaki. The CCC
Advisory Group includes Drs. Kathy Andolsek of
Duke University, Karen Hauer of UCSF, and Jamie
Padmore of Medstar Health, whose expertise and
wisdom has been vital in planning Milestones
research activities.
One the more exciting developments last year was the
initial validity research led by the American Board of
Emergency Medicine (ABEM) in partnership with the
ACGME. The rst Emergency Medicine Milestones
study demonstrated early evidence of validity as an
assessment instrument for competency development.
The Milestones were able to discriminate between
residency years, and an exploratory factor analysis
found the factor structure further supported the
validity of the Emergency Medicine Milestones. The
group that conducted this research also submitted
a paper to Academic Medicine that examines the
relationship between emergency medicine resident
performance on the in-training examination and
performance on the Emergency Medicine Milestones.
The research arm of the Milestones Department is
also currently collaborating on a qualitative study with
Dr. Nate Selden and his team at the Oregon Health
Sciences University (OHSU), investigating the early
experience of residents and program directors with
the Milestones. Data collection should be completed
by early fall, and lessons from this study will inform
similar studies with other specialty disciplines.
The ACGME will also be one of the collaborators
on the Professionals Accelerating Clinical and
Educational Redesign (PACER) national initiative to
improve the quality of ambulatory-based training
and care. This exciting project is being primarily
funded by the Josiah Macy Foundation, with
additional support from the American Boards of
Family Medicine, Internal Medicine, and Pediatrics
and the ACGME. The PACER project builds off
the successful Primary Care Faculty Development
Initiative (PCFDI) pilot interdisciplinary project.
The Milestones team is also developing research
activities with other certication boards and
medical educators around the country. This is a
very exciting time for graduate medical education
and the Milestones team wants to help advance the
research and science around competency-based
medical education.
An Overview of the Professional Self-regulatory Assessment System in United States
(from Holmboe ES, Batalden P.
Achieving the Desired Transformation: Thoughts on Next Steps for Outcomes-Based Medical Education.
Acad Med. 2015 Jun 16. [Epub ahead of print] PMID: 26083400)
The majority of learner assessments occur within
the training institution and program. Milestones
and entrustable professional activities (EPAs) can
serve as the guiding framework and blueprint for
curriculum and assessment. Programs need to
implement a combination of assessment tools
(e.g., direct observation, medical record audit of
clinical performance using validated measures)
to align with the competencies and Milestones.
The figure also highlights the critical importance
of active resident engagement in the assessment
system. Effective group process via the CCC
leads to better decisions and judgments about
learner development. Professional self-regulation,
represented in the United States by the ACGME
(accreditation) and the American Board of Medical
Specialties (certification), are the public-facing
entities of the system, but depend substantially
on the programs for execution of standards. The
bi-directional arrows signify the co-dependent
relationships of all actors in the system.

2014-2015 ACGME Annual Report
16
The 2015 ACGME Annual Educational Conference
(AEC) achieved a signicant milestone that was
only dreamed of a decade ago. 3472 participants
attended the conference, held in San Diego,
California, marking the rst time the AEC exceeded
3,000 registrants, and representing the largest
graduate medical educational conference in the
world to date.
This is signicant for several reasons:
1. In 2005, conference attendance was 802. The
2015 gathering reached over four times as many
graduate medical education (GME) professionals
with essential accreditation information, high
quality GME research and scholarship, and the
opportunity to network with and learn from peers
from around the world.
2. It marks a signicant expansion of the
nature of the event and the type of educational
experiences and opportunities offered during
the conference. The 2005 AEC was limited
to large group presentations given mainly by
ACGME staff members and administrators,
primarily on accreditation-specic topics. Since
2008, the conference planning team widened
the tent to include an array of courses using
a variety of educational methodologies with
faculty members drawn, yes from the staff
and administration, but also from outside
experts and the GME community at-large, and
with content expanded beyond accreditation
to include the total spectrum of GME to meet
the needs of program directors, designated
institutional ofcials, coordinators, residents
and fellows, and others, both domestically and
internationally.
3. The expansion in scope allowed another
signicant dimension to emerge – the AEC has
become a gathering place for the worldwide
GME community, increasing collegiality,
collaboration, and community, and enabling
the participants to share knowledge and
experience. The opportunity to meet and learn
from fellow travelers on the GME road has
been cited time and again as a vitally important
reason participants return to this conference
year after year.
Record-Setting Attendance at
2015 Annual Educational Conference
Total AEC attendance,
2004-present
Year Attendance
2004 712
2005 802
2006 1003
2007 1160
2008 1209
2009 1380
2010 1622
2011 1753
2012 2251
2013 2941
2014 2869
2015 3472
Total Accreditation versus General (GME research/educational)
AEC presentations, 2005-present
Year Accreditation General
Total
Sessions
2005 43 24 67
2006 42 16 58
2007 35 17 52
2008 38 22 60
2009 41 41 82
2010 37 52 89
2011 37 54 91
2012 35 79 114
2013 42 76 118
2014
76
(includes
NAS)
57 133
2015 52 81 132
Total number presentations selected for AEC from
those submitted for consideration
Year
Selected
Presentations
Total
Presentations
2009 36 82
2010 41 89
2011 45 91
2012 60 114
2013 63 118
2014 91 133
2015 73 132

2014-2015 ACGME Annual Report
17
ACGME Awards
Parker J. Palmer Courage to Teach Award
Presented to up to 10 program directors who
have fostered innovation and improvement in their
residency programs and served as exemplary
role models for residents.
Anthony Arnold, MD
Ophthalmology
Jules Stein Eye Institute, UCLA School of Medicine
Bashar Attar, MD, PhD
Gastroenterology
John H. Stroger Hospital of Cook County
Samuel Borden, MD
Medicine-Pediatrics
Baystate Medical Center
Kalli Doyle, MD
Pediatrics
William Beaumont School of Medicine
Karl Golnik, MD, MEd
Ophthalmology
University of Cincinnati
E. Gormley, MD
Urology
Dartmouth-Hitchcock Medical Center
Kevin Means, MD
Physical Medicine and Rehabilitation
University of Arkansas for Medical Sciences College of
Medicine
Matthew Short, MD
Transitional Year
Madigan Healthcare System
Christopher Varley, MD
Child and Adolescent Psychiatry
University of Washington
Kenneth Zukerman, MD
Hematology and Oncology
University of South Florida and H. Lee Moffitt Cancer
Center
Parker J. Palmer Courage to Lead Award
Presented each year to up to three designated
institutional ofcials who have demonstrated
strong leadership and astute resource
management, and who have also encouraged
innovation and improvement in residency
programs and their sponsoring institutions.
Roseanne Berger, MD
University at Buffalo
Thomas Blackwell, MD
University of Texas Medical Branch at Galveston
Miriam Bar-on, MD
University of Nevada School of Medicine
Each year the ACGME recognizes notable program directors, designated institutional ofcials, residents, and coordinators for their outstanding work and
contributions to graduate medical education through its Awards Program. Below are the 2015 awardees who were honored at a luncheon reception during
the 2015 ACGME Annual Educational Conference held February 6-March 1, 2015 in San Diego, California.
Parker J. Palmer Courage to Teach Award Winners
Parker J. Palmer Courage to Lead Award Winners

2014-2015 ACGME Annual Report
18
David C. Leach, MD Award
Presented to up to ve residents who have
fostered innovation and improvement in their
residency programs, advanced humanism in
medicine, and increased efciency and emphasis
on educational outcomes.
Prathit Kulkarni, MD
Pediatrics
Baylor College of Medicine, Houston
Kenneth Remy, MD
Surgery
Erlanger Medical Center
GME Program Coordinator Excellence Award
Presented to up to ve program coordinators in
recognition of their in-depth understanding of the
accreditation process, excellent communication
and interpersonal skills, and projects to improve
residency programs.
Alicia Crispin
Family Medicine
Grand Rapids Medical Education Partners/Michigan
State University
Denise Mussehl
Anesthesiology
University of Wisconsin School of Medicine and Public
Health
Cynthia Neal
Family Medicine
Long Beach Memorial Medical Center
Mary Rich
Endocrinology, Diabetes and Metabolism Coordinator
University of Cincinnati Medical Center College of
Medicine
GME Institutional Coordinator Excellence
Award
Presented to one institutional coordinator upon
whom everyone depends to know graduate
medical education and what the process is for
internal review. The ACGME depends on this
person to wear many hats, including those of
administrator, counselor, enforcer, coordinator,
organizer, and scheduler.
Paul Johnson
Ichan School of Medicine at Mount Sinai
GME Program and Institutional Coordinator Excellence Award Winners
David C. Leach, MD Award Winners

19
Swing, SR. ACGME Launches
Outcomes Assessment Project.
JAMA. 1998. 279(18);1492.
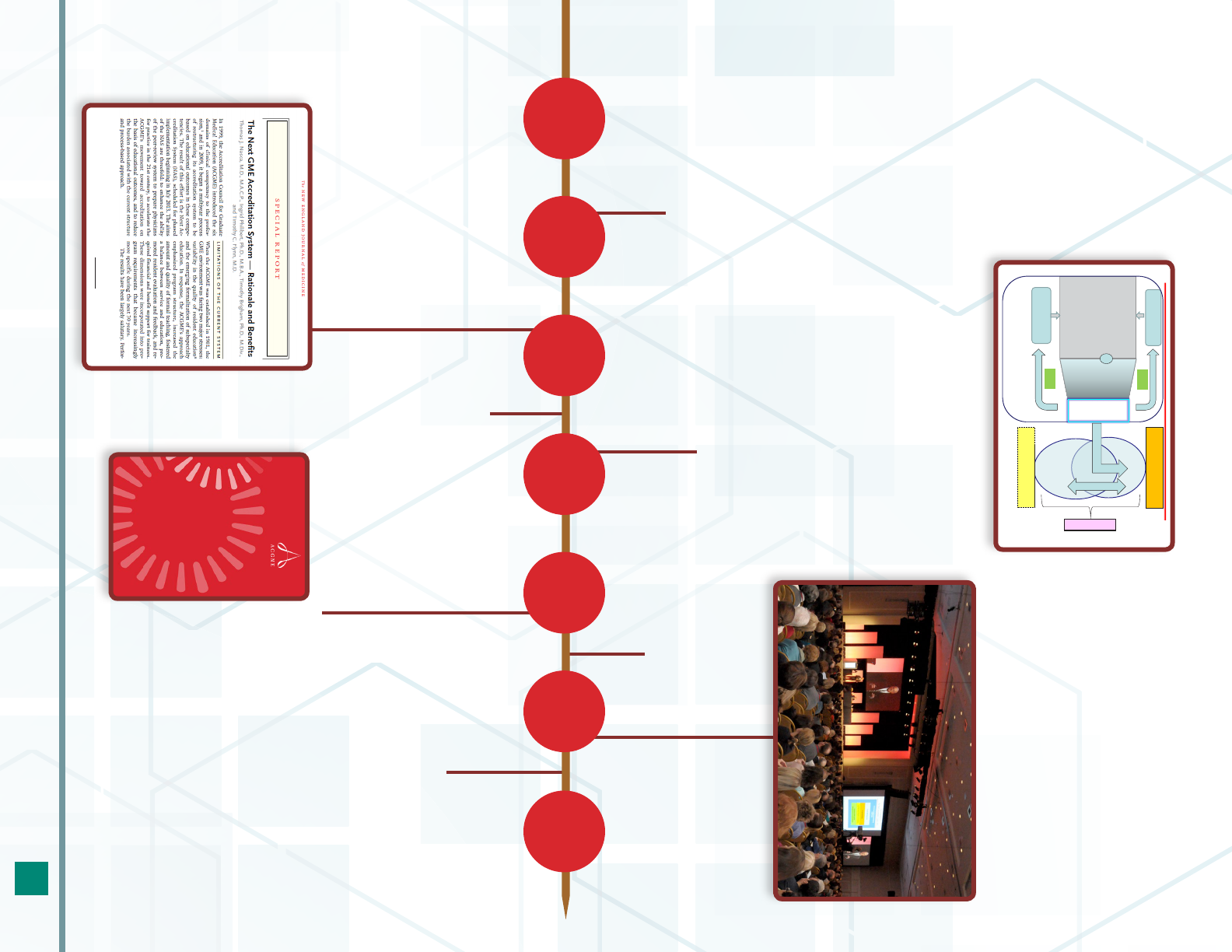
Intellectual Foundation of NAS
Educational Innovations Project (EIP)
© 2012 Accreditation Council for Graduate Medical Education (ACGME)
EIP Initiated by Henry Schultz, MD, Roger Bush, MD, T.J. Nasca, MD
and RRC-IM in 2001-2002. Completed in 2012.
Nasca, T.J., Day, S.H., Amis, E.S., for the ACGME Duty Hour Task Force.
Sounding Board: The New Recommendations on Duty Hours from the ACGME Task Force.
New England Journal of Medicine. 362 (25): e3(1-6). 2010. June 23, 2010.
“Task Force on Patient Safety and Professionalism”
The New
Accreditation
Model
Foster innovation and
improvement in the
learning environment
Increase the
accreditation emphasis ON
educational outcomes
Increase efficiency
and reduce burden
in accreditation
Improve communication
and collaboration with key
internal and external
stakeholders
1998 1999 2002 2005 2007 20092008
The Next Accreditation System
1998
Launch of the Outcome Project
2009
Task Force on
Patient Safety and
Professionalism convened
2001-2002
“Intellectual Foundation of the Next Accreditation
System” // Educational Innovations Projects initiated
by H. Schultz, MD, R. Bush, MD, T. Nasca, MD, and the
Review Committee for Internal Medicine
2005
ACGME Board Executive Committee
endorses “four strategic priorities”
designed to enable the emergence of a
new model of accreditation
2008
Institute of Medicine releases
Resident Duty Hours:
Enhancing Sleep, Supervision,
and Safety report
1999
ACGME/ABMS Competencies
introduced
2007
Thomas J. Nasca, MD, MACP
named CEO of ACGME
TIMELINE:
2014-2015 ACGME Annual Report
20
1
Nasca, T.J., Philibert, I., Brigham, T.P., Flynn, T.C.
The Next GME Accreditation System: Rationale and Benefits.
New England Journal of Medicine. Published Electronically, February 22, 2012. In Print, March 15, 2012.
DOI:10.1056/nejmsr1200117 www.nejm.org
.
NEJM. 2012.366;11:1051-1056.
Clinical Learning
Environment Review (CLER)
CLER Pathways
to Excellence
Expectations for an optimal clinical
learning environment to achieve safe
and high quality patient care
2014 Accreditation Council for Graduate Medical Education
Assessments within
Program:
• Direct observations
• Audit and
performance data
• Multi-source FB
• Simulation
• Exams
“Data”
Synthesis:
Committee
Residents
Faculty, PDs
and others
Milestones and EPAs
as Guiding Framework and Blueprint
Accreditation
Unit of Analysis:
Program
Certification and
Credentialing
Unit of Analysis:
Individual
J
U
D
G
M
E
N
T
D
FB
FB
P
U
B
L
I
C
MILESTONES
RESEARCH
2016201520142013201220112010
2011
• ACGME Board of
Directors approves phased
implementation of the Next
Accreditation System (NAS)
• Policy change revisions
relating to NAS initiated
• Revised Duty Hour
Requirements in effect
2014-2015
NAS fully implemented
for all specialties
2015
Spring 2015: Pilot for 10-year accreditation
site visit/self-studies begins
2012-2013
Milestones process and
reporting structure formalized
and operationalized across all
disciplines; Working Groups
convene to develop Milestones
2013
• July 1, 2013: NAS Policy
Changes in Effect
• July 1, 2013: Phase I
implemented with 7 specialties
(Diagnostic Radiology, Emergency
Medicine, Internal Medicine,
Pediatrics, Neurological Surgery,
Orthopaedic Surgery, Urology) and
their subspecialties
• Milestones reporting/rst data
collection for Phase I
2015-2016
Transitional implementation
to NAS for institutions
2012
• Public announcement of
the Next Accreditation System
• Clinical Learning
Environment Review Program
launched
2014
• February 2014: CLER
Pathways to Excellence
launched
• July 1, 2014: Phase
II implemented for
remaining specialties and
subspecialties

2014-2015 ACGME Annual Report
21
The ACGME-I Mission
ACGME International (ACGME-I) was developed
after multiple countries reached out to the
ACGME for accreditation information and
assistance. There was an expressed need for
physicians to be trained to better serve individual
international communities. The ACGME’s highly
structured system of education and accreditation
demonstrated unique appeal as compared to
alternative models. This endeavor was rst
sparked by Singapore in 2009 and has been
expanded to other countries across the globe. The
mission—though similar to that of the ACGME—
focuses on improving the quality of health care
specific to each individual country’s need
.
It is important to clarify that the ACGME-I does
not serve individuals from other countries who
wish to enter into a residency in the United States.
One of the major expectations of countries
and institutions that seek ACGME-I services
is to prevent brain drain and to cultivate a local
environment that encourages a physician to
stay in one’s own country. Though the emphasis
for the ACGME-I is to create quality residency
programs abroad, an absence of subspecialists
internationally has created a desire by many
ACGME-I graduates to add an accredited
fellowship year in the US. Some domestic
Review Committees have dened such graduates
as “exceptional candidates” for fellowship
consideration. Notably, such individuals do not
become eligible to sit for an American Board of
Medical Specialties certifying examination.
The relationship with the ACGME
Organizationally, ACGME-I is an LLC of the parent
organization ACGME. As such, it is nancially
self-sufcient. The ACGME-I is funded through
contracts with individual ministries of health or
institutions. The ACGME-I reports to the ACGME
Board of Directors through its Finance Committee
(see Financial Reports, p.26).
The ACGME-I does rely on certain tools and
resources housed within the ACGME. For example,
data collection through the Accreditation Data
System, site visits by professional staff, reliance
upon the Education Department related to areas
such as the Milestones, and other features all
utilize the services and personnel of the ACGME.
The ACGME-I Requirements and Review
Process
While the system is similar to that of the ACGME,
the ACGME-I accreditation requirements for
both institutions and programs are necessarily
distinct. Accreditation is rst granted to an
institution; programs must be sponsored by such
an accredited institution. Both institutions and
programs are held to accreditation requirements.
The ACGME-I accreditation process reects
a similarity to the ACGME system of recent
design (prior to the implementation of the Next
Accreditation System), typied by review cycle
lengths of three years or fewer between site
visits; program information forms; and other
processes designed to assist programs as they
adopt ACGME-I requirements particular to a
specialty/subspecialty. Undoubtedly, there will
be future iterations of international requirements
reective of growth and change, just as domestic
requirements have evolved under the Next
Accreditation System.
A substantial component of international
accreditation, just as with domestic norms, is the
presence of volunteerism and peer standards-
setting. International members of the Review
Committee do a superlative job of representing
the patients’, residents’, educators’, and
countries’ needs as unique to their environment.
The organization especially thanks Drs. Margaret
Blott; Sally Ho; Abdulatif al Khal; Halah Ibrahim;
and Colin Song; and notes with sadness the
passing of Dr. Vijayan Appasamy, a charter
member of the Review Committee-International.
ACGME International Making an Impact
ACGME-I BY THE NUMBERS - 2014-2015
3.5 new FTE ACGME-I staff members
6 new country inquiries/discussions
7 newly-accredited programs
10 countries visited one or more times
during 2014-2015
38 accredited specialties
64 site visits
99 accredited programs
~2000 residents in accredited programs

2014-2015 ACGME Annual Report
22
Making a Difference
After six years, the ACGME-I has over 100
programs currently or soon to be accredited. The
Journal of Graduate Medical Education
includes
international articles describing improvements in
residency education and patient care. Residents
who experienced GME in their countries both
before and after the implementation of ACGME-I
accreditation note the value of a structured
evaluative system, and of knowing what it is they
need to know as they learn. Faculty members
echo this, expressing a clearer understanding of
what needs to be taught, of a dened approach
to teaching, and of a better educational process
for different types of learners. Medical education
leadership is beginning to see the value of the
Milestones and Clinical Competency Committees
as tools for identifying areas requiring attention
or earlier intervention, so that remediation may
occur more effectively when necessary.
Ultimately, the ACGME-I hopes to dene a
stronger collaboration between domestic
accredited programs and international programs.
Such opportunities are limitless, from rotations
that provide international learning, to identication
of best practices, to teaching and learning that
takes advantage of mobile health technologies.
Collaborative efforts, above all, are intended
to honor both similarities and differences
in countries’ needs, and to tailor education
appropriately.
Continuing to Build
Thus far, the ACGME-I’s success has in large
part been in economically stable countries that
seek a more rigorous medical education system.
But this approach is changing in order to more
fully serve the Mission of improving global health.
In the past year, visits were conducted in Haiti
and Panama, where highly committed medical
education leaders reached out for assistance. The
ACGME-I team witnessed the most fundamental
of pre-requisites for solid medical education: a
dedicated administrative core; an enthusiastic
faculty desirous of improving; residents wanting
to provide the best care; and long lines of patients
needing help. There were clear differences
in the economic resources and technological
sophistication in these two countries, but both
afrmed the need to expand what the ACGME-I
can do. Consequent to these visits, the ACGME-I
is cultivating stakeholders in an effort to dene
how the needs of such countries can be met.
Rather than producing an “all or none” model
for accreditation, a tiered approach to improving
education is being developed. The ACGME-I is
also working with institutions devoted to global
health to identify graduate medical education’s
current status in numerous locations in order to
more fully serve its Mission.
The ACGME-I launched a redesigned website at www.acgme-i.org in January 2015.

2014-2015 ACGME Annual Report
23
2014-2015 Statistical Highlights
STATISTICS AND FINACIALS
Institutions
There are 692 institutions that sponsor graduate medical education
programs. Over 60% sponsor multiple programs, while almost 40%
sponsor single programs.
Sponsoring Institutions
Multiple programs 429 62%
Single programs 263 38%
692 100%
Sponsoring Institutions use 4,858 participating sites to teach residents and
fellows. Over the past decade, the number of teaching sites has nearly
doubled, while ambulatory teaching sites nearly tripled during the same
timeframe.

2014-2015 ACGME Annual Report
24
Specialty
Subspecialty
4,020
4,867
4,060
4,962
4,084
5,181
4,134
5,393
4,171
5,474
Number of Programs
1,500
3,000
4,500
6,000
2010-11 2011-12 2012-13 2013-14 2014-15
Programs
Accredited Programs
During 2014-2015, there were 9,645 accredited programs of which
4,171 were specialty programs and 5,474 were subspecialty programs.
Additionally, there were 193 new programs, which is the smallest annual
increase in new programs in over a decade. The number of programs that
closed or voluntarily withdrew their accreditation was 46.
During the 2014-2015 annual review cycle, Review Committees reviewed
and issued 8,816 accreditation decisions to programs participating in the
Next Accreditation System annual review.Based on review of their annual
indicators, the vast majority of programs (82.8%) did not require an in-depth
review by the Review Committee.The remaining programs were assessed
by Review Committee reviewers with or without a site visit.Most programs
were conferred a status of Continued Accreditation.A small number, 190
programs (2.2%), were granted a status of Continued Accreditation with
Warning or placed on Probationary Accreditation.
Specialty Program: A structured educational experience
in a eld of medical practice following completion of
medical school and, in some cases, prerequisite basic
clinical education designed to conform to the Program
Requirements of a particular specialty; also known as
‘core’ programs.
Subspecialty Program: A structured educational
experience following completion of a prerequisite
specialty program in GME designed to conform to the
Program Requirements of a particular subspecialty.
Accredited Programs

2014-2015 ACGME Annual Report
25
Number of Residents and Fellows
25,000
50,000
75,000
100,000
125,000
2010-2011 2011-2012 2012-2013 2013-2014 2014-2015
66,989
66,056
64,435
63,183
62,260
27,534
27,004
26,974
26,737
26,107
121,599
120,108
117,717
115,293
113,142
24,775
25,373
26,308
27,048
27,076
Note: 'Pipeline programs' are programs within specialties that lead to initial board
certification. Residents entering the pipeline are in Year 1 (e
xcluding preliminary year).
Number of Residents
Continuing in Pipeline
Programs that lead to
Initial Board Certificatio
n
Number of Residents
Entering Pipeline
Programs that lead to
Initial Board Certification
Number of Residents and
Fellows in Preliminary
Positions, Transitional
Year Programs, and
Fellowship Programs
Residents and Fellows
Active Residents and Fellows
There are 121,599 active residents and fellows in 9,645 programs. Of
the total 121,599 residents and fellows in 2014-2015, 23% were entering
pipeline programs, 55% were continuing in pipeline programs, and 22%
were in preliminary positions, transitional year programs, and fellowships.
Active Residents and Fellows by Medical School Type
Of the 121,599 active residents/fellows in ACGME-accredited programs
during Academic Year 2014-2015, the majority, at 65% completed LCME-
accredited medical schools in the U.S. Over a quarter, at 26%, are
international medical school graduates (IMGs).
Medical School Type
Count of
Residents
US-LCME Accredited Medical School 79,142
International Medical School 31,271
Osteopathic Medical School 10,999
Canadian Medical School 178
Medical School Unknown 9
Resident and Fellow Status
In addition to the 121,599 active residents, 42,741 successfully completed
and graduated from their ACGME-accredited programs.
Resident Status
Count of
Residents
Active 121,599
Completed Training 42,741
Left Program
Prior to Successful Completion
2,238
Inactive 1,368
Note: More breakdowns and additional details regarding these data are provided in the
ACGME’s Graduate Medical Education Data Resource Book, which can be found on the
ACGME website, www.acgme.org.
Active Residents and Fellows

2014-2015 ACGME Annual Report
26
ACGME revenue comes primarily from annual
fees charged to all programs accredited during
the academic year, accounting for nearly 87% of
ACGME income. Applications for new programs
accounted for 3.5% of 2014 revenue. Conference
and Workshop revenue and Investment income
accounted for 5.2% and 3.5% of total revenues,
respectively. During 2014, total revenues
amounted to more than $54.9 million. Of this
amount, the ACGME generated just under $51.4
million and the ACGME-I generated just under
$3.6 million.
As a service organization, salary and benet
expenses, as well as travel and meeting costs,
make up over 69% of the ACGME’s annual
expenses. During 2014, total expenses incurred
amounted to $53.6 million. The ACGME incurred
$51.1 million, while the ACGME-I incurred just
under $2.5 million.
Net income for 2014 was just over $1.3 million.
The ACGME’s net gain for 2014 was $247,000,
while the ACGME-I’s net gain was just under $1.1
million.
2014 Financial Reports
The ACGME’s scal year runs from January 1-December 31. These results represent audited results for Fiscal Year 2014.
Program Fees $47,557,370 86.6%
Conferences and Workshops $2,867,728 5.2%
Application Fees $1,918,380 3.5%
Net Investment Income $1,925,463 3.5%
Rent Revenue $449,334 0.8%
Other $218,668 0.4%
Total Revenues $54,936,943 100.0%
2014 Revenue
Personnel $29,932,145 55.8%
Meetings and Travel $7,261,291 13.5%
Depreciation $3,509,259 6.5%
Facilities $3,480,226 6.5%
Professional Services $3,863,255 7.2%
Ofce Supplies and Other $5,559,242 10.4%
Total Expenses $53,605,418 100.0%
2014 Expenses

2014-2015 ACGME Annual Report
27
Clinton Adams, DO
Term began January 2015
Stephen Albanese, MD
Stanley Ashley, MD
Carol Bernstein, MD
Donald Brady, MD
Term began September 2014
David Brown, MD
Term ended September 2014
Baretta Casey, MD
Term ended September 2014
Candice Chen, MD
Federal Government Representative
Term began September 2014
Jordan Cohen, MD
At Large Director
Timothy Daskivich, MD
Chair, Council of Review Committee Residents
Anjali Dogra, MD
Term ended September 2014
John Duval
Chair
David Entwistle
Term began September 2014
Ted Epperly, MD
Norman D. Ferrari III, MD
David Fine, MD
Term ended September 2014
David Forstein, DO
Term began January 2015
Rosemary Gibson
Public Director
Jeffrey Gold, MD
Steven Goldstein
Term began September 2014
Paul Grundy, MD
At Large Director
Diane Hartmann, MD
Term began September 2014
James Hebert, MD
Chair, Council of Review Committee Chairs
Carmen Hooker Odom, M.R.P.
Public Director
Lynne Kirk, MD
Dorothy Lane, MD
Term ended September 2014
Lorrie Langdale, MD
Jo Ellen Linder, MD
Term ended September 2014
Kenneth Ludmerer, MD
At Large Director
William McDade, MD
John B. McWhorter III
Term began September 2014
Travis Meyer, MD
Term began September 2014
Karen Nichols, DO
Term began January 2015
William Pinsky, MD
Peter Rapp
Term ended September 2014
Karen Sanders, MD
Federal Government Representative
Term began September 2014
Henry Schultz, MD
Treasurer
Gary Slick, DO
Term began January 2015
Edwin Zalneraitis, MD
Rowen Zetterman, MD
Vice Chair
ACGME Board of Directors • 2014-2015
LISTS
ACGME Board of Directors, September 2014

2014-2015 ACGME Annual Report
28
Review/Recognition Committees and Accredited Specialties
Review/Recognition Committee Specialized Areas Appointing Organizations
Allergy and Immunology
American Academy of Allergy, Asthma, and Immunology
American College of Allergy, Asthma, and Immunology
Anesthesiology
Adult Cardiothoracic Anesthesiology
Clinical Informatics
Anesthesiology Critical Care Medicine
Hospice and Palliative Medicine
Obstetric Anesthesiology
Pain Medicine
Pediatric Anesthesiology
American Board of Anesthesiology
American Osteopathic Association
Colon and Rectal Surgery
American Board of Colon and Rectal Surgery
American College of Surgeons
Dermatology Dermatopathology Micrographic Surgery and Dermatologic Oncology
American Board of Dermatology
American Osteopathic Association
Diagnostic Radiology
Abdominal Radiology
Clinical Informatics
Endovascular Surgical Neuroradiology
Interventional Radiology
Musculoskeletal Radiology
Neuroradiology
Nuclear Radiology
Pediatric Radiology
Vascular and Interventional Radiology
American Board of Radiology
American College of Radiology
American Osteopathic Association
Emergency Medicine
Clinical Informatics
Emergency Medical Services
Medical Toxicology
Pediatric Emergency Medicine
Sports Medicine
Undersea and Hyperbaric Medicine
American Board of Emergency Medicine
American College of Emergency Physicians
American Osteopathic Association
Family Medicine
Clinical Informatics
Geriatric Medicine
Hospice and Palliative Medicine
Sports Medicine
American Board of Family Practice
American Academy of Family Physicians
American Osteopathic Association
Institutional
ACGME Board of Directors
American Osteopathic Association
Internal Medicine
Adult Congenital Heart Disease
Advanced Heart Failure and Transplant Cardiology
Cardiovascular Disease
Clinical Cardiac Electrophysiology
Clinical Informatics
Critical Care Medicine
Endocrinology, Diabetes, and Metabolism
Gastroenterology
Geriatric Medicine
Hematology
Hematology and Medical Oncology
Hospice and Palliative Medicine
Infectious Disease
Internal Medicine-Pediatrics
Interventional Cardiology
Medical Oncology
Nephrology
Pulmonary Critical Care
Pulmonary Disease
Rheumatology
Sleep Medicine
Transplant Hepatology
American Board of Internal Medicine
American College of Physicians
American Osteopathic Association
Medical Genetics
Clinical Informatics
Medical Biochemical Genetics
Molecular Genetic Pathology
American Board of Medical Genetics
American College of Medical Genetics
Neurological Surgery Endovascular Surgical Neuroradiology
American Board of Neurological Surgery
American College of Surgeons
American Osteopathic Association
Neurology
Brain Injury Medicine
Child Neurology
Clinical Neurophysiology
Endovascular Surgical Neuroradiology
Epilepsy
Neurodevelopmental Disabilities
Neuromuscular Medicine
Pain Medicine
Sleep Medicine
Vascular Neurology
American Board of Psychiatry and Neurology
American Academy of Neurology
American Osteopathic Association
Nuclear Medicine
American Board of Nuclear Medicine
Society of Nuclear Medicine
Obstetrics and Gynecology
Female Pelvic Medicine
and Reconstructive Surgery
American Board of Obstetrics and Gynecology
American College of Obstetricians and Gynecologists
American Osteopathic Association

2014-2015 ACGME Annual Report
29
Review/Recognition Committee Specialized Areas Appointing Organizations
Ophthalmology Ophthalmic Plastic and Reconstructive Surgery
American Board of Ophthalmology
American Academy of Ophthalmology
American Osteopathic Association
Orthopaedic Surgery
Adult Reconstructive Orthopaedic Surgery
Foot and Ankle Orthopaedic Surgery
Hand Surgery
Musculoskeletal Oncology
Orthopaedic Sports Medicine
Orthopaedic Surgery of the Spine
Orthopaedic Trauma
Pediatric Orthopaedic Surgery
American Board of Orthopaedic Surgery
American Academy of Orthopaedic Surgeons
American Osteopathic Association
Osteopathic Neuromusculoskeletal
Medicine
ACGME Board of Directors
American Osteopathic Association
Osteopathic Principles Committee
ACGME Board of Directors
American Osteopathic Association
Otolaryngology Neurotology Pediatric Otolaryngology
American Board of Otolaryngology
American College of Surgeons
American Osteopathic Association
Pathology – Anatomic and Clinical
Blood Banking/Transfusion Medicine
Chemical Pathology
Clinical Informatics
Cytopathology
Dermatopathology
Forensic Pathology
Hematology
Medical Microbiology
Molecular Genetic Pathology
Neuropathology
Pediatric Pathology
Selective Pathology
American Board of Pathology
Pediatrics
Adolescent Medicine
Child Abuse
Clinical Informatics
Developmental-Behavioral Pediatrics
Hospice and Palliative Medicine
Internal Medicine-Pediatrics
Neonatal-Perinatal Medicine
Pediatric Cardiology
Pediatric Critical Care
Pediatric Emergency Medicine
Pediatric Endocrinology
Pediatric Gastroenterology
Pediatric Hematology Oncology
Pediatric Infectious Diseases
Pediatric Nephrology
Pediatric Pulmonology
Pediatric Rheumatology
Pediatric Transplant Hepatology
Sleep Medicine
Sports Medicine
American Board of Pediatrics
American Academy of Pediatrics
American Osteopathic Association
Physical Medicine and Rehabilitation
Brain Injury Medicine
Neuromuscular Medicine
Pain Medicine
Pediatric Rehabilitation Medicine
Spinal Cord Injury Medicine
Sports Medicine
American Board of Physical Medicine and Rehabilitation
American Academy of Physical Medicine and
Rehabilitation
American Osteopathic Association
Plastic Surgery Craniofacial Surgery Hand Surgery
American Board of Plastic Surgery
American College of Surgeons
American Osteopathic Association
Preventive Medicine
Clinical Informatics
Medical Toxicology
Undersea and Hyperbaric Medicine American Board of Preventive Medicine
Psychiatry
Addiction Psychiatry
Brain Injury Medicine
Child Psychiatry
Forensic Psychiatry
Geriatric Psychiatry
Hospice and Palliative Medicine
Psychosomatic Medicine
Sleep Medicine
American Board of Psychiatry and Neurology
American Psychiatric Association
American Osteopathic Association
Radiation Oncology Hospice and Palliative Medicine
American Board of Radiology
American College of Radiology
Surgery
Complex General Surgical Oncology
Surgical Critical Care
Hand Surgery
Pediatric Surgery
Vascular Surgery
American Board of Surgery
American College of Surgeons
American Osteopathic Association
Thoracic Surgery Congenital Cardiac Surgery
American Board of Thoracic Surgery
American College of Surgeons
Urology
Female Pelvic Medicine
and Reconstructive Surgery
Pediatric Urology
American Board of Urology
American College of Surgeons
American Osteopathic Association
Transitional Year
ACGME Board of Directors
American Osteopathic Association
* The American Medical Association’s Council on Medical Education is an appointing organization for all Review Committees except for the Institutional Review Committee, the Transitional Year Review
Committee, the Osteopathic Neuromusculoskeletal Medicine Review Committee, and the Osteopathic Principles Committee.

2014-2015 ACGME Annual Report
30
Review/Recognition Committee Specialized Areas Appointing Organizations
Ophthalmology Ophthalmic Plastic and Reconstructive Surgery
American Board of Ophthalmology
American Academy of Ophthalmology
American Osteopathic Association
Orthopaedic Surgery
Adult Reconstructive Orthopaedic Surgery
Foot and Ankle Orthopaedic Surgery
Hand Surgery
Musculoskeletal Oncology
Orthopaedic Sports Medicine
Orthopaedic Surgery of the Spine
Orthopaedic Trauma
Pediatric Orthopaedic Surgery
American Board of Orthopaedic Surgery
American Academy of Orthopaedic Surgeons
American Osteopathic Association
Osteopathic Neuromusculoskeletal
Medicine
ACGME Board of Directors
American Osteopathic Association
Osteopathic Principles Committee
ACGME Board of Directors
American Osteopathic Association
Otolaryngology Neurotology Pediatric Otolaryngology
American Board of Otolaryngology
American College of Surgeons
American Osteopathic Association
Pathology – Anatomic and Clinical
Blood Banking/Transfusion Medicine
Chemical Pathology
Clinical Informatics
Cytopathology
Dermatopathology
Forensic Pathology
Hematology
Medical Microbiology
Molecular Genetic Pathology
Neuropathology
Pediatric Pathology
Selective Pathology
American Board of Pathology
Pediatrics
Adolescent Medicine
Child Abuse
Clinical Informatics
Developmental-Behavioral Pediatrics
Hospice and Palliative Medicine
Internal Medicine-Pediatrics
Neonatal-Perinatal Medicine
Pediatric Cardiology
Pediatric Critical Care
Pediatric Emergency Medicine
Pediatric Endocrinology
Pediatric Gastroenterology
Pediatric Hematology Oncology
Pediatric Infectious Diseases
Pediatric Nephrology
Pediatric Pulmonology
Pediatric Rheumatology
Pediatric Transplant Hepatology
Sleep Medicine
Sports Medicine
American Board of Pediatrics
American Academy of Pediatrics
American Osteopathic Association
Physical Medicine and Rehabilitation
Brain Injury Medicine
Neuromuscular Medicine
Pain Medicine
Pediatric Rehabilitation Medicine
Spinal Cord Injury Medicine
Sports Medicine
American Board of Physical Medicine and Rehabilitation
American Academy of Physical Medicine and
Rehabilitation
American Osteopathic Association
Plastic Surgery Craniofacial Surgery Hand Surgery
American Board of Plastic Surgery
American College of Surgeons
American Osteopathic Association
Preventive Medicine
Clinical Informatics
Medical Toxicology
Undersea and Hyperbaric Medicine American Board of Preventive Medicine
Psychiatry
Addiction Psychiatry
Brain Injury Medicine
Child Psychiatry
Forensic Psychiatry
Geriatric Psychiatry
Hospice and Palliative Medicine
Psychosomatic Medicine
Sleep Medicine
American Board of Psychiatry and Neurology
American Psychiatric Association
American Osteopathic Association
Radiation Oncology Hospice and Palliative Medicine
American Board of Radiology
American College of Radiology
Surgery
Complex General Surgical Oncology
Surgical Critical Care
Hand Surgery
Pediatric Surgery
Vascular Surgery
American Board of Surgery
American College of Surgeons
American Osteopathic Association
Thoracic Surgery Congenital Cardiac Surgery
American Board of Thoracic Surgery
American College of Surgeons
Urology
Female Pelvic Medicine
and Reconstructive Surgery
Pediatric Urology
American Board of Urology
American College of Surgeons
American Osteopathic Association
Transitional Year
ACGME Board of Directors
American Osteopathic Association
* The American Medical Association’s Council on Medical Education is an appointing organization for all Review Committees except for the Institutional Review Committee, the Transitional Year Review
Committee, the Osteopathic Neuromusculoskeletal Medicine Review Committee, and the Osteopathic Principles Committee.
Review/Recognition Committee Members • 2014-2015
Allergy and Immunology
Amal H. Assa’ad, MD
Cincinnati Children’s Hospital Medical Center
Cincinnati, Ohio
William K. Dolen, MD—Chair
Georgia Regents University
Augusta, Georgia
Mary Beth Fasano, MD
University of Iowa Hospitals and Clinics
Iowa City, Iowa
Anita T. Gewurz, MD
Rush Medical College, Rush University
Chicago, Illinois
David P. Huston, MD
Texas A&M Health Science Center
Houston, Texas
Bruce J. Lanser, MD—Resident
National Jewish Health
Denver, Colorado
Gailen D. Marshall Jr., MD
The University of Mississippi Medical Center
Jackson, Mississippi
Michael R. Nelson, MD
Walter Reed National Medical Center
Bethesda, Maryland
Jay M. Portnoy, MD—Vice Chair
Children’s Mercy Hospital
Kansas City, Missouri
Stephen I. Wasserman, MD—Ex-Officio
American Board of Allergy and Immunology
Philadelphia, Pennsylvania
Anesthesiology
J. Jeffrey Andrews, MD—Ex-Officio
(Term ended September 30, 2014)
American Board of Anesthesiology
San Antonio, Texas
Deborah J. Culley, MD
Brigham and Women’s Hospital
Boston, Massachusetts
Brenda G. Fahy, MD
University of Florida
Gainesville, Florida
Robert Gaiser, MD—Vice Chair
Hospital of the University of Pennsylvania
Philadelphia, Pennsylvania
Linda Jo Mason, MD
Loma Linda University Medical Center
Loma Linda, California
Joel Musee, MD—Resident
Vanderbilt University
Antioch, Tennessee
Andrew Patterson, MD, PhD
Stanford University
Stanford, California
James Ramsay, MD
University of California, San Francisco
San Francisco, California
James P. Rathmell, MD—Ex-Officio
(Term began October 1, 2014)
American Board of Anesthesiology
Boston, Massachusetts
Richard W. Rosenquist, MD
Cleveland Clinic
Cleveland, Ohio
Margaret Wood, MD—Chair
Columbia University
New York, New York
Cynthia A. Wong, MD
Northwestern University
Feinberg School of Medicine
Chicago, Illinois
Colon and Rectal Surgery
Patrice Blair, MPH—Ex-Officio
American College of Surgeons
Chicago, Illinois
Russell W. Farmer, MD—Resident
University of Louisville
Louisville, Kentucky
Tracy L. Hull, MD
The Cleveland Clinic Foundation
Cleveland, Ohio
Matthew G. Mutch, MD
Washington University School of Medicine
St. Louis, Missouri
Bruce A. Orkin, MD—Chair
Rush University
Chicago, Illinois
David J. Schoetz Jr., MD—Ex-Officio
American Board of Colon and Rectal Surgeons
Burlington, Massachusetts
Anthony J. Senagore, MD—Vice Chair
University Hospitals/Parma Medical Center
Parma, Ohio
Michael J. Snyder, MD
University of Texas Medical School
Houston, Texas
Charles B. Whitlow, MD
Ochsner Medical Center
New Orleans, Louisiana
Dermatology
Robert T. Brodell, MD
University of Mississippi
Jackson, Mississippi
C. William Hanke, MD, MPH, FACP
Laser Skin and Surgery Center of Indiana
Carmel, Indiana
Brian R. Hinds, MD—Resident
University of Louisville
Louisville, Kentucky
Thomas D. Horn, MD, MBA—Ex-Officio
American Board of Dermatology
Newton, Massachusetts
Nicole M. Owens, MD—Chair
Skin Specialists of San Antonio
San Antonio, Texas
Amy Susan Paller, MD—Vice Chair
Northwestern University
Chicago, Illinois
James W. Patterson, MD
University of Virginia
Charlottesville, Virginia
Mary Stone, MD
University of Iowa
Iowa City, Iowa
Colonel George W. Turiansky, MD
Uniformed Services University of
the Health Sciences
Bethesda, Maryland
John A. Zitelli, MD
University of Pittsburgh
Pittsburgh, Pennsylvania
continued on next page

2014-2015 ACGME Annual Report
31
Diagnostic Radiology
James C. Anderson, MD—Chair
Oregon Health & Science University
Portland, Oregon
Bradley Carra, MD—Resident
San Antonio Uniformed Services
Health Education Consortium
San Antonio, Texas
Kristen K. DeStigter, MD
University of Vermont/Fletcher Allen Health Care
Burlington, Vermont
Donald Flemming, MD
Penn State Hershey Radiology
Hershey, Pennsylvania
Valerie Jackson, MD—Ex-Officio
American Board of Radiology
Tucson, Arizona
Susan D. John, MD
University of Texas Medical School at Houston
Houston, Texas
Jeanne M. LaBerge, MD
University of California, San Francisco
San Francisco, California
Mary Mahoney, MD
UC Health
Cincinnati, Ohio
Duane G. Mezwa, MD—Vice Chair
Oakland University, William Beaumont Hospitals
Rochester Hills, Michigan
Elizabeth Oates, MD
University of Kentucky
Lexington, Kentucky
Gautham P. Reddy, MD
University of Washington
Seattle, Washington
Kay Vydareny, MD—Ex-Officio
American Board of Radiology
Tucson, Arizona
Emergency Medicine
Brandon R. Allen, MD—Resident
University of Florida
Newberry, Florida
Steven H. Bowman, MD
Stroger Cook County Hospital
Chicago, Illinois
Lance Brown, MD
Loma Linda University
Loma Linda, California
Wallace Carter, MD
New York Presbyterian
Bronxville, New York
Amy Church, MD
Rutgers University
Stockton, New Jersey
Marjorie Geist, PhD—Ex-Officio
American College of Emergency Physicians
Irving, Texas
Diane Gorgas, MD
Ohio State University
Columbus, Ohio
Douglas McGee, DO
Einstein Healthcare Network
Philadelphia, Pennsylvania
Earl J. Reisdorff, MD—Ex-Officio
American Board of Emergency Medicine
East Lansing, Michigan
Philip Shayne, MD—Chair
Emory University
Atlanta, Georgia
Christine Sullivan, MD—Vice Chair
Truman Medical Center
Kansas City, Missouri
Suzanne R. White, MD
Detroit Medical Center
Detroit, Michigan
Family Medicine
Suzanne M. Allen, MD
University of Washington School of Medicine
Boise, Idaho
John R. Bucholtz, DO
Columbus Regional Family Residency Program
Columbus, Georgia
Gary Buckholz, MD
University of California at San Diego
La Jolla, California
Paul A. Callaway, MD—Vice Chair
University of Kansas School of Medicine
Wichita, Kansas
Peter J. Carek, MD, MS—Chair
University of Florida
Gainesville, Florida
Samuel Jones, MD
VCU-Fairfax Family Medicine Residency
Fairfax, Virginia
Stanley Kozakowski, MD—Ex-Officio
American Academy of Family Physicians
Leawood, Kansas
Martha H. Lansing, MD
UMDNJ-Robert Wood Johnson Medical School
New Brunswick, New Jersey
Michael K. Magill, MD
University of Utah School of Medicine
Salt Lake City, Utah
Stacy E. Potts, MD
UMass Memorial Group
Barre, Massachusetts
James Puffer, MD—Ex-Officio
American Board of Family Medicine
Lexington, Kentucky
Nicholas Weida, MD—Resident
Swedish Family Medicine Residency
Seattle, Washington
Institutional Review Committee
Ronald G. Amedee, MD, FACS
Ochsner Health System
New Orleans, Louisiana
James A. Clardy, MD
University of Arkansas for Medical Sciences
Little Rock, Arkansas
Andrew T. Filak, MD
University of Cincinnati College of Medicine
Cincinnati, Ohio
Joseph Jaeger, DrPH
Monmouth Medical Center
Long Branch, New Jersey
Dinchen Jardine, MD LCDR MC USN
—Resident
Naval Medical Center – Portsmouth
Portsmouth, Virginia
Susan Kirk, MD
University of Virginia Health System
Charlottesville, Virginia
Peter M. Nalin, MD
(Term ended January 31, 2015)
Indiana University School of Medicine
Indianapolis, Indiana
Lawrence M. Opas, MD—Chair
University of Southern California/LAC+USC
Medical Center
Los Angeles, California
Rita M. Patel, MD
University of Pittsburgh School of Medicine
Pittsburgh, Pennsylvania
James R. Zaidan, MD, MBA —Vice Chair
Emory University School of Medicine
Atlanta, Georgia

2014-2015 ACGME Annual Report
32
Internal Medicine
Patrick Alguire, MD, FACP—Ex-Officio
American College of Physicians
Philadelphia, Pennsylvania
James A. Arrighi, MD—Chair
Rhode Island Hospital, Brown Medical School
Providence, Rhode Island
Robert L. Benz, MD
Lankenau Medical Center
Wynnewood, Pennsylvania
Christian T. Cable, MD, MHPE
Texas A&M University Health Science Center
Temple, Texas
E. Benjamin Clyburn, MD—Vice Chair
Medical University of South Carolina
Charleston, South Carolina
Ricardo Correa, MD—Resident
National Institute of Health
Rockville, Maryland
Alan C. Dalkin, MD
University of Virginia
Charlottesville, Virginia
Andrew N. Dentino, MD
University of Oklahoma Health Science Center
Oklahoma City, Oklahoma
Sima S. Desai, MD
Oregon Health & Science University
Portland, Oregon
John D. Fisher, MD
Montefiore Medical Center/
Albert Einstein College of Medicine
Bronx, New York
Andrew S. Gersoff, MD
Santa Barbara Cottage Hospital
Santa Barbara, California
Kristin Jacob, MD—Resident
Grand Rapids Medical Education Partners
Grand Rapids, Michigan
Betty Lo, MD
Louisiana State University
Health Sciences Center
New Orleans, Louisiana
Monica L. Lypson, MD
University of Michigan
Ann Arbor, Michigan
Brian F. Mandell, MD
Cleveland Clinic
Cleveland, Ohio
Furman S. McDonald, MD—Ex-Officio
American Board of Internal Medicine
Philadelphia, Pennsylvania
Elaine A. Muchmore, MD
University of California, San Diego
San Diego, California
Susan Murin, MD
University of California, Davis
School of Medicine
Sacramento, California
Victor J. Navarro, MD
Einstein Medical Center/
Einstein Healthcare Network
Philadelphia, Pennsylvania
Andrea Reid, MD
Washington Veterans Affairs Medical Center
Washington, District of Columbia
Ilene M. Rosen, MD, MSCE
University of Pennsylvania School of Medicine
Philadelphia, Pennsylvania
Jacqueline Stocking, RN, MSN, MBA
—Public Member
University of California Davis Health System
Sacramento, California
Jennifer C. Thompson, MD, FACP, FIDSA
Orlando VA Medical Center
Orlando, Florida
Medical Genetics
Hans Christoph Andersson, MD
Tulane University Medical School
New Orleans, Louisiana
Mimi G. Blitzer, PhD, FACMG—Ex-Officio
American Board of Medical Genetics
Bethesda, Maryland
Laurie A. Demmer, MD, MA
Carolinas Medical Center
Charlotte, North Carolina
Katrina M. Dipple, MD
David Geffen School of Medicine, UCLA
Los Angeles, California
Susan D. Klugman, MD
Montefiore Medical Center/
Albert Einstein College of Medicine
Bronx, New York
Austin Larson, MD—Resident
Children’s Hospital Colorado
Aurora, Colorado
Shawn E. McCandless, MD—Vice Chair
University Hospitals Case Medical Center
Cleveland, Ohio
V. Reid Sutton, MD—Chair
Baylor College of Medicine
Houston, Texas
Neurological Surgery
Nicholas M. Barbaro, MD—Vice Chair
Indiana University School of Medicine
Indianapolis, Indiana
H. Hunt Batjer, MD, FACS
UT Southwestern Medical Center
Dallas, Texas
Patrice Blair, MPH—Ex-Officio
American College of Surgeons
Chicago, Illinois
Jeffrey N. Bruce, MD—Ex-Officio
American Board of Neurological Surgery
New York, New York
Kim J. Burchiel, MD, FACS—Chair
Oregon Health & Science University
Portland, Oregon
M. Sean Grady, MD
The Hospital of the University of Pennsylvania
Philadelphia, Pennsylvania
Griffith R. Harsh IV, MD
Stanford University
Stanford, California
Benjamin C. Kennedy, MD—Resident
Columbia University/
New York Presbyterian Hospital
New York, New York
Nelson M. Oyesiku, MD, PhD
Emory University School of Medicine
Atlanta, Georgia
continued on next page

2014-2015 ACGME Annual Report
33
Neurology
Imran I. Ali, MD
University of Toledo Health Science Campus
Toledo, Ohio
Eric R. Anderson, MD—Resident
Emory University
Atlanta, Georgia
David J. Capobianco, MD, FAAN
Mayo Clinic Florida
Jacksonville, Florida
Larry Faulkner, MD—Ex-Officio
American Board of Psychiatry and Neurology
Buffalo Grove, Illinois
Laurie Gutmann, MD
University of Iowa
Iowa City, Iowa
Ralph F. Józefowicz, MD
University of Rochester School of
Medicine and Dentistry
Rochester, New York
Shannon M. Kilgore, MD—Vice Chair
VA Palo Alto Health Care System
Palo Alto, California
Steven L. Lewis, MD—Chair
Rush University Medical Center
Chicago, Illinois
Phillip L. Pearl, MD
Boston Children’s Hospital
Boston, Massachusetts
Catherine M. Rydell, CAE—Ex-Officio
American Academy of Neurology
Minneapolis, Minnesota
Lori A. Schuh, MD, FAAN
Spectrum Health
Grand Rapids, Michigan
Barney J. Stern, MD
University of Maryland School of Medicine
Baltimore, Maryland
Nuclear Medicine
Jon Baldwin, DO—Chair
University of Alabama Birmingham
Medical Center
Hoover, Alabama
Helena Balon, MD
William Beaumont Hospital
Royal Oak, Michigan
Erica Cohen, DO—Resident
Loyola University Medical Center
Maywood, Illinois
Kirk A. Frey, MD
The University of Michigan Hospitals
Ann Arbor, Michigan
Frederick Grant, MD
Children’s Hospital Boston
Boston, Massachusetts
David Lewis, MD—Vice Chair
University of Washington
Seattle, Washington
J. Anthony Parker, MD—Ex-Officio
American Board of Nuclear Medicine
Boston, Massachusetts
George Segall, MD—Ex-Officio
American Board of Nuclear Medicine
St. Louis, Missouri
Barry L. Shulkin, MD, MBA
St. Jude Children’s Research Hospital
Memphis, Tennessee
Obstetrics and Gynecology
Karen E. Adams, MD
Oregon Health & Science University
Portland, Oregon
Jessica L. Bienstock, MD, MPH—Vice Chair
Johns Hopkins University School of Medicine
Baltimore, Maryland
Mary C. Ciotti, MD—Chair
University of Southern California
Los Angeles, California
AnnaMarie Connolly, MD
University of North Carolina at Chapel Hill
Chapel Hill, North Carolina
Amber R. Crowder, MD—Resident
Tripler Army Medical Center
Tripler AMC, Hawaii
Gary N. Frishman, MD
Women & Infants Hospital of Rhode Island
Providence, Rhode Island
Larry C. Gilstrap III, MD—Ex-Officio
American Board of Obstetrics and Gynecology
Dallas, Texas
Robert V. Higgins, MD
Carolinas Medical Center
Charlotte, North Carolina
Kimberly S. Kenton, MD
Northwestern University Feinberg
School of Medicine
Chicago, Illinois
Hal Lawrence, MD—Ex-Officio
American College of
Obstetricians and Gynecologists
Washington, District of Columbia
Lee A. Learman, MD, PhD
Indiana University School of Medicine
Indianapolis, Indiana
Robert S. Schenken, MD
University of Texas Health Science Center at
San Antonio
San Antonio, Texas
Patrice M. Weiss, MD
Carilion Roanoke Memorial Hospital
Roanoke, Virginia
Christopher Zahn, MD
(Term ended April 1, 2015)
Uniformed Services University of the
Health Sciences
Bethesda, Maryland
Ophthalmology
Anthony C. Arnold, MD—Chair
UCLA Medical Center
Los Angeles, California
John G. Clarkson, MD—Ex-Officio
American Board of Ophthalmology
Miami, Florida
Claude L. Cowan Jr., MD
Veterans Affairs Medical Center
Washington, District of Columbia
Andreas K. Lauer, MD
Oregon Health & Science University
Portland, Oregon
Assumpta A. Madu, MD, MBA, PharmD, CPE
Montefiore Medical Center
Bronx, New York
Shahzad Mian, MD
University of Michigan
Ann Arbor, Michigan
Howard D. Pomeranz, MD, PhD
North Shore Long Island Jewish Medical Center
Great Neck, New York
Joel S. Schuman, MD
University of Pittsburgh Medical Center
Pittsburgh, Pennsylvania
Raymond M. Siatkowski, MD—Vice Chair
University of Oklahoma
Oklahoma City, Oklahoma
Brian C. Stagg, MD—Resident
University Health Care
Salt Lake City, Utah
Laura L. Wayman, MD
Vanderbilt Eye Institute
Nashville, Tennessee

2014-2015 ACGME Annual Report
34
Orthopaedic Surgery
R. Dale Blasier, MD, FRCS
Arkansas Children’s Hospital
Little Rock, Arkansas
Lynn A. Crosby, MD
Georgia Regents University
Augusta, Georgia
Jeanne M. Franzone, MD—Resident
Columbia University Medical Center
New York, New York
Shepard R. Hurwitz, MD—Ex-Officio
American Board of Orthopaedic Surgery
Chapel Hill, North Carolina
Paul J. Juliano, MD
The Penn State Milton S. Hershey
Medical Center
Hershey, Pennsylvania
Dawn M. LaPorte, MD
Johns Hopkins University
Baltimore, Maryland
Terry R. Light, MD
Loyola University, Stritch School of Medicine
Maywood, Illinois
J. Lawrence Marsh, MD—Chair
University of Iowa Hospitals
Iowa City, Iowa
Peter M. Murray, MD
Mayo Clinic
Jacksonville, Florida
Theodore W. Parsons III, MD, FACS
Henry Ford Health System
Detroit, Michigan
Terry L. Thompson, MD—Vice Chair
Howard University Hospital
Washington, District of Columbia
Osteopathic
Neuromusculoskeletal Medicine
William Thomas Crow, DO, FAAO
University of North Texas Health Science Center
Fort Worth, Texas
Guy DeFeo, DO
University of New England
Biddeford, Maine
Lisa DeStephano, DO—Chair
Michigan State University College of
Osteopathic Medicine
East Lansing, Michigan
John Leuenberger, DO—Resident
Eastern Maine Medical Center
Bangor, Maine
James Martin, MD
CHRISTUS Santa Rosa Health Care
San Antonio, Texas
Natalie A. Nevins, DO, MSHPE
Western University of Health Sciences/COMP
Pomona, California
Eric Hunter Sharp, DO—Vice Chair
Central Maine Medical Center
Lewiston, Maine
Jim Swartwout, MA—Ex-Officio
American Osteopathic Association
Chicago, Illinois
Osteopathic Principles
Committee
Juan F. Acosta, DO, MS, FACOEP-D, FACEP
OPTI-West/Pacific Northwest University of
Health Sciences
Yakima, Washington
Natasha N. Bray, DO, MSEd, FACOI, FACP
—Vice Chair
Proposed Arkansas College of
Osteopathic Medicine
Fort Smith, Arkansas
Robert A. Cain, DO—Chair
Ohio University Heritage College of
Osteopathic Medicine
Powell, Ohio
Jane Carreiro, DO
University of New England
Kennebunkport, Maine
Millicent Channell, DO, FAAO
Rowan University – School of
Osteopathic Medicine
Philadelphia, Pennsylvania
Alissa Craft, DO, MBA
NYIT – College of Osteopathic Medicine
Old Westbury, New York
John Dougherty, DO, FACOFP, FAOASM,
FAODME, FILM
Kansas City University of Medicine and
Biosciences – College of Osteopathic Medicine
Kansas City, Missouri
Robert Hasty, DO, FACOI, FACP
Campbell University
Buies Creek, North Carolina
Kenneth A. Heiles, DO, FACOFP dist
Proposed Arkansas College of
Osteopathic Medicine
Fort Smith, Arkansas
Bridget McIlwee, DO—Resident
University of North Texas Health Science Center
Fort Worth, Texas
Anthony N. Ottaviani, DO, MPH, MACOI, FCCP
Largo Medical Center-Nova Southeastern
University College of Osteopathic Medicine
Largo, Florida
George Pasquarello, DO, FAAO
East Greenwich Spine & Sport
East Greenwich, Rhode Island
Michael P. Rowane, DO, MS, FAAFP, FAAO
University Hospitals Regional Hospitals
Willoughby Hills, Ohio
Barry Smith, MD
Baylor College of Medicine
Houston, Texas
Karen T. Snider, DO, MS, FAAO
ATSU-KCOM
Kirksville, Missouri
Jim Swartwout, MA—Ex-Officio
American Osteopathic Association
Chicago, Illinois
Penelope Tippy, MD
Southern Illinois University Carbondale
Family Medicine Residency
West Frankfort, Illinois
continued on next page

2014-2015 ACGME Annual Report
35
Otolaryngology
Iram Ahmad, MD—Resident
University of Iowa Hospitals and Clinics
Iowa City, Iowa
Patrice Gabler Blair, MPH —Ex-Officio
American College of Surgeons
Chicago, Illinois
Sukgi S. Choi, MD—Chair
Children’s Hospital Pittsburgh
Pittsburgh, Pennsylvania
Michael Cunningham, MD, FACS—Vice Chair
Children’s Hospital Boston
Boston, Massachusetts
David Brian Hom, MD
University of Cincinnati College of Medicine
Cincinnati, Ohio
Robert H. Miller, MD, MBA—Ex-Officio
American Board of Otolaryngology
Houston, Texas
Lloyd B. Minor, MD
Stanford University School of Medicine
Stanford, California
John Rhee, MD, MPH, FACS
Medical College of Wisconsin
Milwaukee, Wisconsin
David J. Terris, MD, FACS
Georgia Regents University
Augusta, Georgia
Terance T. Tsue, MD
University of Kansas School of Medicine
Kansas City, Kansas
Randal S. Weber, MD
University of Texas MD Anderson Cancer Center
Houston, Texas
D. Bradley Welling, MD, PhD, FACS
Harvard Medical School
Boston, Massachusetts
Pathology
Melissa Austin, MD, MBS—Resident
Walter Reed National Military Medical Center
Bethesda, Maryland
Susan Adela Fuhrman, MD
Riverside Methodist Hospital
Columbus, Ohio
Michael N. Hart, MD
(Term ended January 27, 2015)
University of Wisconsin-Madison
Madison, Wisconsin
Julia C. Iezzoni, MD—Chair
University of Virginia Health System
Charlottesville, Virginia
Rebecca Johnson, MD—Ex-Officio
American Board of Pathology
Tampa, Florida
Karen L. Kaul, MD, PhD
NorthShore University Health System,
Evanston Hospital
Evanston, Illinois
Barbara Sampson, MD—Vice Chair
Office of the Chief Medical Examiner of the
City of New York
New York, New York
James R. Stubbs, MD
Mayo Clinic
Rochester, Minnesota
Steven Swerdlow, MD
UPMC Presbyterian Hospital
Pittsburgh, Pennsylvania
Charles F. Timmons Jr., MD, PhD
University of Texas Southwestern
Dallas, Texas
Pediatrics
Ann E. Burke, MD
Dayton Children’s Medical Center
Dayton, Ohio
Dalya Leviant Chefitz, MD
UMDNJ-Robert Wood Johnson Medical School
New Brunswick, New Jersey
Jerri Curtis, MD
Uniformed Services University of the
Health Sciences
Bethesda, Maryland
Alan H. Friedman, MD
Yale University Department of Pediatrics
Madison, Connecticut
Rani Gereige, MD, MPH, FAAP
(Term began January 1, 2015)
Miami Children’s Hospital
Miami, Florida
Joseph Gilhooly, MD—Chair
Oregon Health & Science University
Portland, Oregon
Maryellen Gusic, MD
(Term ended July 17, 2014)
Indiana University School of Medicine
Indianapolis, Indiana
Richard Hawkins, MD—Ex-Officio
American Medical Association
Chicago, Illinois
David Jaffe, MD
University of California, San Francisco
San Francisco, California
Deepak M. Kamat, MD, PhD, FAAP
Children’s Hospital of Michigan
Detroit, Michigan
Cathy A. Lee-Miller, MD—Resident
University of Colorado
Aurora, Colorado
Gail A. McGuinness, MD—Ex-Officio
American Board of Pediatrics
Chapel Hill, North Carolina
Holly Mulvey, MA—Ex-Officio
American Academy of Pediatrics
Elk Grove Village, Illinois
Victoria Fay Norwood, MD
University of Virginia Health System
Charlottesville, Virginia
Carrie Radabough, MPP—Ex-Officio
American Academy of Pediatrics
Elk Grove Village, Illinois
R. Franklin Trimm, MD—Vice Chair
University of South Alabama Children’s and
Women’s Hospital
Mobile, Alabama
Daniel C. West, MD
University of California, San Francisco
San Francisco, California
Suzanne K. Woods, MD
Duke University Medical Center
Durham, North Carolina

2014-2015 ACGME Annual Report
36
Physical Medicine and
Rehabilitation
Anthony E. Chiodo, MD—Vice Chair
University of Michigan
Ann Arbor, Michigan
Salar Deldar, MD—Resident
Monterey Spine & Joint
Monterey, California
Gerard E. Francisco, MD, FAAPMR—Chair
University of Texas
Health Science Center at Houston
Houston, Texas
Susan V. Garstang, MD
VA New Jersey Healthcare System
East Orange, New Jersey
William F. Micheo, MD
University of Puerto Rico School of Medicine
San Juan, Puerto Rico
David W. Pruitt, MD
Cincinnati Children’s Hospital Medical Center
Cincinnati, Ohio
Tom Stautzenbach—Ex-Officio
American Academy of
Physical Medicine and Rehabilitation
Rosemont, Illinois
Anthony M. Tarvestad, JD—Ex-Officio
(Term ended February 1, 2015)
American Board of
Physical Medicine and Rehabilitation
Rochester, Minnesota
Carol Vandenakker-Albanese, MD
UC Davis Health System
Sacramento, California
Plastic Surgery
Michael L. Bentz, MD
University of Wisconsin
Madison, Wisconsin
Patrice Blair, MPH—Ex-Officio
American College of Surgeons
Chicago, Illinois
James Chang, MD—Vice Chair
Stanford University
Stanford, California
Kevin C. Chung, MD
University of Michigan
Ann Arbor, Michigan
Arun K. Gosain, MD
Lurie Children’s Hospital
Chicago, Illinois
Juliana E. Hansen, MD
Oregon Health & Science University
Portland, Oregon
Donald R. Mackay, MD—Chair
Penn State Milton S. Hershey Medical Center
Hershey, Pennsylvania
Aaron Mull, MD—Resident
Washington University
St. Louis, Missouri
R. Barrett Noone, MD—Ex-Officio
American Board of Plastic Surgery
Philadelphia, Pennsylvania
Robert A. Weber Jr., MD
Texas A&M University Health Science Center
Temple, Texas
James E. Zins, MD
The Cleveland Clinic Foundation
Cleveland, Ohio
Preventive Medicine
Beth A. Baker, MD—Chair
Canadian Pacific Railway
Minneapolis, Minnesota
Tina C. Foster, MD, MPH, MS
Dartmouth Hitchcock Medical Center
Lebanon, New Hampshire
William Greaves, MD, MPH—Ex-Officio
American Board of Preventive Medicine
Chicago, Illinois
Kurt Timothy Hegmann, MD, MPH
University of Utah
Salt Lake City, Utah
Robert Johnson, MD, MPH, MBA
Humana Military Healthcare Services
Boerne, Texas
Denece Odland Kesler, MD, MPH, FACOEM
—Vice Chair
University of New Mexico
Albuquerque, New Mexico
Ana E. Nobis, MD, MSPH—Resident
University of Illinois at Chicago
Chicago, Illinois
Col. Samual W. Sauer, MD, MPH
USASAM/NAMI
Pensacola, Florida
Psychiatry
Iqbal Ahmed, MD
Tripler Army Medical Center
Honolulu, Hawaii
Robert J. Boland, MD
Brigham and Women’s Hospital
Boston, Massachusetts
Carlyle H. Chan, MD
Medical College of Wisconsin
Milwaukee, Wisconsin
Josepha A. Cheong, MD
Malcom Randall VA Medical Center
Gainesville, Florida
Steven P. Cuffe, MD
University of Florida College of Medicine
Jacksonville, Florida
Mina Dulcan, MD
Lurie Children’s Hospital
Chicago, Illinois
Larry Faulkner, MD—Ex-Officio
American Board of Psychiatry and Neurology
Buffalo Grove, Illinois
Anne L. Glowinski, MD, MPE
Washington University School of Medicine
St. Louis, Missouri
George A. Keepers, MD—Chair
Oregon Health & Science University
Portland, Oregon
M. Philip Luber, MD
University of Texas Health Science Center
San Antonio, Texas
Gerald A. Maguire, MD
UC Riverside School of Medicine
Riverside, California
Annelle Primm, MD—Ex-Officio
American Psychiatric Association
Arlington, Virginia
Robert J. Ronis, MD
University Hospitals Case Medical Center
Cleveland, Ohio
continued on next page

2014-2015 ACGME Annual Report
37
Psychiatry (continued)
Heather E. W. Schultz, MD—Resident
University of Michigan
Ann Arbor, Michigan
Mark Servis, MD—Vice Chair
University of California, Davis
School of Medicine
Sacramento, California
Andrea Stolar, MD
Baylor College of Medicine
Houston, Texas
Dorothy E. Stubbe, MD
Yale University Child Study Center
New Haven, Connecticut
Richard F. Summers, MD
Perelman School of Medicine,
University of Pennsylvania
Philadelphia, Pennsylvania
Radiation Oncology
Robert J. Amdur, MD—Chair
University of Florida
Gainesville, Florida
Katherine L. Griem, MD—Vice Chair
Rush University Medical Center
Chicago, Illinois
Miranda Kim, MD—Resident
Brigham and Women’s Hospital
Boston, Massachusetts
William Regine, MD
University of Maryland
Baltimore, Maryland
Dennis C. Shrieve, MD, PhD
Huntsman Cancer Hospital
Salt Lake City, Utah
Ann E. Spangler, MD, MACM
University of Texas Southwestern
Dallas, Texas
Paul E. Wallner, DO—Ex-Officio
American Board of Radiology
Bethesda, Maryland
Lynn D. Wilson, MD, MPH
Yale University School of Medicine
New Haven, Connecticut
Surgery
John Armstrong, MD
University of South Florida
Morsani College of Medicine
Tallahassee, Florida
Patrice Blair, MPH—Ex-Officio
American College of Surgeons
Chicago, Illinois
Ronald Dalman, MD
Stanford University School of Medicine
Stanford, California
George M. Fuhrman, MD
Ochsner Clinic Foundation
New Orleans, Louisiana
David N. Herndon, MD
University of Texas Medical Branch
Galveston, Texas
Mark Malangoni, MD—Ex-Officio
The American Board of Surgery
Philadelphia, Pennsylvania
Jeffrey B. Matthews, MD
University of Chicago
Chicago, Illinois
Joseph Mills, MD
Baylor College of Medicine
Houston, Texas
John J. Ricotta, MD
Georgetown University
Washington, District of Columbia
Marshall Z. Schwartz, MD
Drexel University
Philadelphia, Pennsylvania
Steven C. Stain, MD—Chair
Albany Medical College
Albany, New York
Danny M. Takanishi, MD—Vice Chair
University of Hawaii John A. Burns
School of Medicine
Honolulu, Hawaii
Paula M. Termuhlen, MD
University of Minnesota
Duluth, Minnesota
Richard Thirlby, MD
Virginia Mason Medical Center
Seattle, Washington
Thomas F. Tracy, MD
Alpert Medical School, Brown University
Providence, Rhode Island
Jennifer Tseng, MD—Resident
Oregon Health & Science University
Portland, Oregon

2014-2015 ACGME Annual Report
38
Thoracic Surgery
Carl L. Backer, MD—Vice Chair
Northwestern University
Feinberg School of Medicine
Chicago, Illinois
William A. Baumgartner, MD—Ex-Officio
American Board of Thoracic Surgery
Chicago, Illinois
Patrice Blair, MPH—Ex-Officio
American College of Surgeons
Chicago, Illinois
Thomas A. D’Amico, MD
Duke University Medical Center
Durham, North Carolina
Robert S. D. Higgins, MD
Ohio State University
Columbus, Ohio
Jennifer Lawton, MD
Washington University
St. Louis, Missouri
Walter H. Merrill, MD—Chair
Vanderbilt University Medical Center
Nashville, Tennessee
Helen Merritt, DO—Resident
University of Texas Health Science Center
San Antonio, Texas
Ara Vaporciyan, MD
University of Texas MD Anderson Cancer Center
Houston, Texas
Transitional Year
Brian M. Aboff, MD—Chair
Christiana Care Health System
Newark, Delaware
Gerard T. Costello, MD
Ball Memorial Hospital
Muncie, Indiana
Steven R. Craig, MD
Unity Point Health
Des Moines, Iowa
Andrew S. Flotten, MD—Resident
Chesapeake, Virginia
Susan Guralnick, MD
Winthrop University Hospital
Mineola, New York
Julie B. McCausland, MD, MS—Vice Chair
University of Pittsburgh Medical Center
Pittsburgh, Pennsylvania
Paul M. Sherman, MD
Wilford Hall Ambulatory Surgical Center
Lackland Air Force Base, Texas
Robert P. Sticca, MD
University of North Dakota School of
Medicine and Health Sciences
Grand Forks, North Dakota
Matthew Short, MD
Madigan Healthcare System
Tacoma, Washington
Urology
Laurence S. Baskin, MD
University of California, San Francisco
San Francisco, California
Patrice Blair, MPH—Ex-Officio
American College of Surgeons
Chicago, Illinois
Jessica Tooredman Casey, MD
Northwestern University
Indianapolis, Indiana
Elizabeth Ann Gormley, MD—Vice Chair
Dartmouth-Hitchcock Medical Center
Lebanon, New Hampshire
Gerald H. Jordan, MD—Ex-Officio
American Board of Urology
Charlottesville, Virginia
Byron D. Joyner, MD
Seattle Children’s Hospital
Seattle, Washington
Barry A. Kogan, MD
Urologic Institute of Northeastern New York
Albany, New York
Randall B. Meacham, MD—Chair
University of Colorado School of Medicine
Aurora, Colorado
Stephen Y. Nakada, MD, FACS
University of Wisconsin School of
Medicine and Public Health
Madison, Wisconsin
Margaret S. Pearle, MD
University of Texas Southwestern
Dallas, Texas
Chad W. M. Ritenour, MD
Emory University
Atlanta, Georgia
James Brantley Thrasher, MD
University of Kansas Medical Center
Kansas City, Kansas

2014-2015 ACGME Annual Report
39
ACGME Staff Listing
Office of the
Chief Executive Officer
Thomas J. Nasca, MD, MACP
Chief Executive Officer
Douglas Carlson, Esq.
Bethanie Clausen
Melissa Lynn
Tami Walters
Office of the
Chief Executive Officer/
Accreditation Standards
Kathy Malloy
Vice President, Accreditation Standards
Timothy Stephansen
Brenda Treviño
Office of the Chief of Staff/
Department of Education
Timothy P. Brigham, MDiv, PhD
Chief of Staff;
Senior Vice President, Department of Education
DeWitt C. Baldwin Jr., MD
Laura Barbo
Amy Beane
Debra Dooley
Robert A. Doughty, MD, PhD
DeLonda Y. Dowling
Ann Riley
Andrea Rio, MA
Paul H. Rockey, MD, MPH
Joanne G. Schwartzberg, MD
Victoria Shaffer
Jessalynn Watanabe
Lauren Wojnarowski, MA
Nicholas Yaghmour, MPP
Department of Finance and
Operations
John Ogunkeye, MS
Chief Financial Officer;
Senior Vice President, Operations
Juan Aguirre
Sheri Bellar
Patricia Desmond
Soukvilai Grenier
Coralie Janssen
Steven Jarvis
Tom Jurczak, MBA
Annie Leong, CPA
Jose Munoz
Bryan Naraky
Patrick Nasca
Javier Nuno
Daniel Parra
Lauren Reali, MA
Teri Robins, JD, MBA
Josiah Robinson
Patricia Trojnar
Sharon Walker
Department of Applications and
Data Analysis
Rebecca S. Miller, MS
Senior Vice President, Applications and
Data Analysis
Samantha Alvarado
Lauren Byrne, MPH
Raquel Eng
Erle Fajardo
Sidney Fox
Jason Goertz
Tom Hackett
Christine Jessup
Christopher Jordan
Kirsten Kolar
Sudarshan Kondur
Sudhir Kumar
Jean Minick
Stephen Moore
Michael Mroz
Steven Nash
David Pott
Thomas Richter, MA
Raquel Running
Hina Shah
Heidi Sowl
Andrew Turkington
Noelle Volovic
Bassam Wassouf
Quinn White
Department of Communications
Paige Amidon, MBA, MPH
Senior Vice President, Communications
Beata Risner, MA
Maayan S. Schwab, MA
Emily Vasiliou, MA
Rayda D. Young
CLER Program
Kevin B. Weiss, MD
Senior Vice President, Institutional Accreditation
Mark Bixby, MD
Jennifer Buescher, MD, MSPH
Ericka Cannaday
Baretta Casey, MD, MPH, FAAFP
Mary Cleveland
Robin Dibner, MD
Anne Down
Staci Fischer, MD
Constance Haan, MD, MS
Joshual Heller, MA
Scott Holliday, MD
John Hopper, MD
Betsy Kimball, MA
Nancy Koh, PhD
Robin Newton, MD
Morgan Passiment, MS
Carl Patow, MD
Mark Pian, MD
Dale Ray, MD, MMM
Melissa Schori, MD, FACP, MBA

2014-2015 ACGME Annual Report
40
Stephen Smith, MD
Hongling Sun, PhD
Marie Trontell, MD
Robin Wagner, RN, MHSA
Elizabeth Wedemeyer, MD
Milestones Department
Eric Holmboe, MD, MACP, FRCP
Senior Vice President,
Milestone Development and Evaluation
Megan Bluth
Lisa Conforti, MPH
Laura Edgar, EdD, CAE
Stanley Hamstra, PhD
Sydney Roberts
Nicholas Yaghmour, MPP
Kenji Yamazaki, PhD
Department of Field Activities
Ingrid Philibert, PhD, MBA
Senior Vice President, Field Activities
Mark Arner, MD
John H. Beernink, MD
Barbara H. Bush, PhD
Joseph F. Campisano, PhD
Donna A. Caniano, MD
Jim Cichon, MSW
John R. Caughron, MD
John J. Coyle, MD
Sterling M. Ellsworth, MD
Andrea Galla, MA
Joseph Gilhooly, MD
Barbara Heywood, MD
Penny Iverson-Lawrence
Nalini Juthani, MD
Donald E. Kraybill, PhD
David L. Larson, MD
Serge A. Martinez, MD, JD
William T. McKinney, MD
John Musich, MD, MBA
Cathy Nace, MD
Christopher A. Pack, PhD
Margarita Perez
Amanda Plashal
Kristen B. Raines, MD
William Robertson, MD, MBA
Judith D. Rubin, MD, MPH
Laurence M. Russell Jr., MD
Theodore Sanford, MD
Carl L. Stanitski, MD
Li Tang, EdD, MPH
Kenneth G. Torrington, MD
Michael R. Valdez, MD, MPH&TM
John A. Zapp, MD
Department of Accreditation
Services/Institutional
Accreditation
Kevin B. Weiss, MD
Senior Vice President, Institutional Accreditation
Ericka Cannaday
Anne Down
Paul Foster Johnson, MFA
Department of Accreditation
Services/Hospital-Based
Accreditation
Louis Ling, MD
Senior Vice President, Hospital-Based
Accreditation
Erin Berryhill
Kelli Cousins, MFA
Felicia Davis, MHA
Laura Edgar, EdD, CAE
Anne Gravel Sullivan, PhD
Cheryl Gross, MA, CAE
Kate Hatlak, MSEd
Sonia Sangha, MPH
Sara Thomas
Nicole Wright
Department of Accreditation
Services/Medical Accreditation
Mary Lieh-Lai, MD
Senior Vice President, Medical Accreditation
Eileen Anthony, MJ
Luz Barrera
Sandra Benitez
Denise Braun-Hart
Bertha Cervantes
Caroline Fischer, MBA
William Hart
Tiffany Hewitt
Lauren Johnson, MNA
Louise King, MS
Karen Lambert
Kimberly Rucker, MPH
Jerry Vasilias, PhD
Department of Accreditation
Services/Osteopathic
Accreditation
Lorenzo Pence, DO
Senior Vice President, Osteopathic Accreditation
Tiffany Moss, MBA
Julia Weigle
Department of Accreditation
Services/Surgical Accreditation
John R. Potts III, MD
Senior Vice President, Surgical Accreditation
Jenny Campbell, MA
Ericka Cannaday
Pamela Derstine, PhD, MHPE
Jordan Elvord
Donna Lamb, MBA
Jennifer Luna
Susan Mansker
Olivia Orndorff
Catherine Ruiz, MA
June Thiele
Mary Joyce Turner, RHIA, MJ
Deidre Williams
Department of Human Resources
Richard Murphy
Vice President, Human Resources
Lynn Cusack
Colleen Murray
Meredith Weil, MS
Office of the Journal of Graduate
Medical Education
Ingrid Philibert, PhD, MBA
Executive Managing Editor, JGME
Andrea Galla, MA
Jean Mattes, MA
Sarah Moran, MA, MM
Amanda Plashal
ACGME International, LLC
John Ogunkeye, MS
Executive Vice President, ACGME International
Susan Day, MD
Senior Vice President for Medical Affairs,
ACGME International
Lorraine Lewis, EdD, RD
Teri Robins, JD, MBA
Kristin Rohn, JD

2014-2015 ACGME Annual Report
41
NOTES

2014-2015 ACGME Annual Report
42
NOTES

2014-2015 ACGME Annual Report
43
NOTES

“Interest in excellence in educational outcomes
and effective evaluation has been energized.
This concentration on effective achievement of
outcomes in our graduates has re-invigorated the
GME effort in the United States.”
Thomas J. Nasca, MD, MACP, Chief Executive Officer, ACGME

515 North State Street, Suite 2000
Chicago, IL 60654
Telephone: 312.755.5000
Fax: 312.755.7498
www.acgme.org
Accreditation Council for Graduate Medical Education
