UnitedHealthcare Vision
UnitedHealthcare Insurance Company of New York
Certificate of Coverage
For
the Plan V2134
of
Columbia University
Group Number: 712790
Effective Date: January 1, 2023
VCOC.18.NY 1
Certificate of Coverage
UnitedHealthcare Insurance Company of New York
What Is the Certificate of Coverage?
This Certificate of Coverage (Certificate) is part of the Policy that is a legal document between
UnitedHealthcare Insurance Company of New York and the Group. The Certificate describes Covered
Vision Care Services, subject to the terms, conditions, exclusions and limitations of the Policy. We issue
the Policy based on the Group's Application and payment of the required Policy Charges.
In addition to this Certificate, the Policy includes:
• The Schedule of Covered Vision Care Services.
• The Group's Application.
• Riders.
• Amendments.
You can review the Policy at the Group's office during regular business hours.
Can This Certificate Change?
We may, from time to time, change this Certificate by attaching legal documents called Riders and/or
Amendments that may change certain provisions of this Certificate. When this happens we will send you
a new Certificate, Rider or Amendment.
Other Information You Should Have
We have the right to change, interpret, withdraw or add Benefits, or to end the Policy, as permitted by
law, without your approval.
On its effective date, this Certificate replaces and overrules any Certificate that we may have previously
issued to you. This Certificate will in turn be overruled by any Certificate we issue to you in the future.
The Policy will take effect on the date shown in the Policy. Coverage under the Policy starts at 12:01 a.m.
and ends at 12:00 midnight in the time zone of the Group's location. The Policy will remain in effect as
long as the Policy Charges are paid when they are due, subject to Section 4: When Coverage Ends.
We are delivering the Policy in New York. The Policy is governed by ERISA unless the Group is not an
employee health and welfare plan as defined by ERISA. To the extent that state law applies, New York
law governs the Policy.
VCOC.18.NY 2
Introduction to Your Certificate
This Certificate and the other Policy documents describe your Benefits, as well as your rights and
responsibilities, under the Policy.
What Are Defined Terms?
Certain capitalized words have special meanings. We have defined these words in Section 8: Defined
Terms.
When we use the words "we," "us," and "our" in this document, we are referring to UnitedHealthcare
Insurance Company of New York. When we use the words "you" and "your," we are referring to people
who are Covered Persons, as that term is defined in Section 8: Defined Terms.
How Do You Use This Document?
Read your entire Certificate and any attached Riders and/or Amendments. You may not have all of the
information you need by reading just one section. Keep your Certificate and Schedule of Covered Vision
Care Services and any attachments in a safe place for your future reference.
Review the Benefit limitations of this Certificate by reading the attached Schedule of Covered Vision Care
Services along with Section 1: Covered Vision Care Services and Section 2: Exclusions and Limitations.
Read Section 7: General Legal Provisions to understand how this Certificate and your Benefits work. Call
us if you have questions about the limits of the coverage available to you.
If there is a conflict between this Certificate and any summaries provided to you by the Group, this
Certificate controls.
Please be aware that your Vision Provider is not responsible for knowing or communicating your Benefits.
How Do You Contact Us?
Call us at 1-800-638-3120. Throughout the document you will find statements that encourage you to
contact us for more information.
VCOC.18.NY 3
Your Responsibilities
Enrollment and Required Contributions
Benefits are available to you if you are enrolled for coverage under the Policy. Your enrollment options,
and the corresponding dates that coverage begins, are listed in Section 3: When Coverage Begins. To be
enrolled and receive Benefits, both of the following apply:
• Your enrollment must be in accordance with the requirements of the Policy issued to your Group,
including the eligibility requirements.
• You must qualify as a Subscriber or a Dependent as those terms are defined in Section 8: Defined
Terms.
Your Group may require you to make certain payments to them, in order for you to remain enrolled under
the Policy. If you have questions about this, contact your Group.
Be Aware the Policy Does Not Pay for All Vision Care Services
The Policy does not pay for all vision care services. Benefits are limited to Covered Vision Care Services.
The Schedule of Covered Vision Care Services will tell you the portion you must pay for Covered Vision
Care Services.
Decide What Services You Should Receive
Care decisions are between you and your Vision Provider. We do not make decisions about the kind of
care you should or should not receive.
Choose Your Vision Provider
It is your responsibility to select the vision care professionals who will deliver your care. We arrange for
Vision Providers and facilities to participate in a Network. Our credentialing process confirms public
information about the professionals' licenses and other credentials, but does not assure the quality of their
services. These professionals and facilities are independent practitioners that are solely responsible for
the care they deliver.
Pay Your Share
You must meet any applicable Deductible and pay a Co-payment and/or Co-insurance for most Covered
Vision Care Services. These payments are due at the time of service or when billed by the Vision
Provider. Any applicable Deductible, Co-payment and Co-insurance amounts are listed in the Schedule of
Covered Vision Care Services. You must also pay any amount that exceeds your Benefits.
Pay the Cost of Excluded Services
You must pay the cost of all excluded services and items. Review Section 2: Exclusions and Limitations
to become familiar with the Policy's exclusions.
VCOC.18.NY 4
File Claims with Complete and Accurate Information
When you receive Covered Vision Care Services from an out-of-Network Vision Provider, you are
responsible for requesting payment from us. You must file the claim in a format that contains all of the
information we require, as described in Section 5: How to File a Claim.
VCOC.18.NY 5
Our Responsibilities
Determine Benefits
We make administrative decisions regarding whether the Policy will pay for any portion of the cost of a
vision care service you intend to receive or have received. Our decisions are for payment purposes only.
We do not make decisions about the kind of care you should or should not receive.
We have the final authority to do the following:
• Interpret Benefits and the other terms, limitations and exclusions set out in this Certificate, the
Schedule of Covered Vision Care Services and any Riders and/or Amendments.
• Make factual determinations relating to Benefits.
We may assign this authority to other persons or entities that may provide administrative services for the
Policy, such as claims processing. The identity of the service providers and the nature of their services
may be changed from time to time as we determine. In order to receive Benefits, you must cooperate with
those service providers.
Pay for Our Portion of the Cost of Covered Vision Care Services
We pay Benefits for Covered Vision Care Services as described in Section 1: Covered Vision Care
Services and in the Schedule of Vision Care Services, unless the service is excluded in Section 2:
Exclusions and Limitations. This means we only pay our portion of the cost of Covered Vision Care
Services. It also means that not all of the vision care services you receive may be paid for (in full or in
part) by the Policy.
Pay Network Providers
It is the responsibility of Network Vision Providers and facilities to file for payment from us. When you
receive Covered Vision Care Services from Network providers, you do not have to submit a claim to us.
Pay for Covered Vision Care Services Provided by Out-of-Network
Providers
In accordance with any state prompt pay requirements, we pay Benefits after we receive your request for
payment that includes all required information. See Section 5: How to File a Claim. Your cost sharing may
be more when you see an out-of-Network Vision Provider.
VCOC.18.NY 6
Certificate of Coverage Table of Contents
Section 1: Covered Vision Care Services 7................................................
Section 2: Exclusions and Limitations 10 ..................................................
Section 3: When Coverage Begins 11 .........................................................
Section 4: When Coverage Ends 14............................................................
Section 5: How to File a Claim 16 ................................................................
Section 6: Questions, Complaints and Appeals 18...................................
Section 7: General Legal Provisions 20 ......................................................
Section 8: Defined Terms 25........................................................................
VCOC.18.NY 7
Section 1: Covered Vision Care Services
When Are Benefits Available for Covered Vision Care Services?
Benefits are available only when all of the following are true:
• The vision care service, including materials as shown in the Schedule of Covered Vision Care
Services.
• You receive Covered Vision Care Services while the Policy is in effect.
• You receive Covered Vision Care Services prior to the date that any of the individual termination
conditions listed in Section 4: When Coverage Ends occurs.
• The person who receives Covered Vision Care Services is a Covered Person and meets all
eligibility requirements specified in the Policy.
This section describes Covered Vision Care Services for which Benefits are available. Please refer to the
attached Schedule of Covered Vision Care Services for details about:
• The amount you must pay for these Covered Vision Care Services (including any Co-payment).
• Any limit that applies to these Covered Vision Care Services (including frequency and dollar limits
on services and materials).
1. Routine Vision Examination
A routine vision exam of the eyes and according to the standards of care in your area, including:
A. A patient history that includes reasons for the exam, patient medical/eye history, and current
medications;
B. Visual acuity with each eye and both eyes, far and near, with and without glasses or contact lenses
(for example, 20/20 and 20/40);
C. Cover test at 20 feet and 16 inches (checks how the eyes work together as a team);
D. Ocular motility (how the eyes move) near point convergence (how well eyes move together for near
vision tasks, such as reading), and depth perception (3D Vision);
E. Pupil reaction to light and focusing;
F. Exam of the eye lids, lashes, and outside of the eye;
G. Refraction (when applicable) - to determine power of corrective lenses for distance and near vision;
Retinoscopy (when applicable): Objective refraction to determine lens power of corrective lenses.
Subjective refraction to determine lens power of corrective lenses;
H. Photometry/Binocular testing - far and near: how well eyes work as a team;
I. Tonometry, when indicated: test pressure in eye (glaucoma check);
J. Ophthalmoscopic exam of the internal eye;
K. Visual field testing;
L. Biomicroscopy;
M. Color vision testing;
VCOC.18.NY 8
N. Diagnosis/prognosis;
O. Dilation (when indicated) - Examine the internal structures of the eye; and
P. Specific recommendations.
Post exam procedures will be performed only when materials are required.
Or in lieu of a complete exam, Retinoscopy (when applicable) - objective refraction to determine lens
power of corrective lenses and subjective refraction to determine lens power of corrective lenses.
2. Eyeglass Lenses
Lenses that are mounted in an eyeglass frame and worn on the face to correct visual acuity limitations.
3. Eyeglass Frame
A structure that contains eyeglass lenses, holding the lenses in front of the eyes and supported by the
bridge of the nose.
4. Optional Lens Extras
Special lens stock or modifications to lenses that do not correct visual acuity problems. Optional Lens
Extras include options such as, but not limited to, lens tints, polycarbonate lenses, high-index lenses,
ultraviolet coating, scratch-resistant coating, edge coating, and photochromic.
5. Contact Lenses
Lenses worn on the surface of the eye to correct visual acuity limitations.
6. Necessary Contact Lenses
This benefit is available where a Vision Provider has determined a need for and has prescribed the
service. Such determination will be made by the Vision Provider and not by us.
Contact lenses are necessary if the Covered Person has:
A. Keratoconus;
B. Anisometropia;
C. Irregular corneal/astigmatism;
D. Aphakia;
E. Facial deformity;
F. Corneal deformity;
G. Pathological myopia;
H. Aniseikonia;
I. Aniridia;
J. Post-traumatic disorders;
K. Post-cataract surgery without intraocular lens; or
VCOC.18.NY 9
L. Visual acuity in the better eye of less than 20/70 with visual correction by eyeglasses but better
than 20/70 with visual correction by contact lenses.
7. Contact Lens Fitting & Evaluation
A contact lens evaluation and fitting includes examination and measurement of the eyes and adjacent
structures to determine the contact lens size, design and power to achieve and maintain eye health,
comfort and vision.
8. Virtual Visits
Virtual visits for Covered Vision Care Services through live audio and video technology. Virtual visits
provide a Routine Vision Examination for the patient by a distant Vision Provider.
Network Benefits are available only when services are delivered through a Designated Virtual Network
Vision Provider. You can find a Designated Virtual Network Vision Provider by contacting us at
www.myuhcvision.com or by calling us at 1-800-638-3120.
Please Note: Not all Routine Examinations or other services can be provided through virtual visits. The
Designated Virtual Network Vision Provider will identify any patients for which services by in-person
Vision Provider is needed.
Benefits do not include email, fax and standard telephone calls.
VCOC.18.NY 10
Section 2: Exclusions and Limitations
We Do Not Pay Benefits for Exclusions
We will not pay Benefits for any of the services, treatments, and materials described in this section, even
if it is recommended or prescribed by a Physician or Vision Provider.
The services, treatments, and materials listed in this section are not Covered Vision Care Services,
except as may be specifically provided for in Section 1: Covered Vision Care Services or through a Rider
to the Policy.
Where Are Benefit Limitations Shown?
When Benefits are limited within any of the Covered Vision Care Service categories described in Section
1: Covered Vision Care Services, those limits are stated in the corresponding Covered Vision Care
Service category in the Schedule of Covered Vision Care Services. Please review all limits carefully, as
we will not pay Benefits for any of the services, treatments, items or supplies that exceed these Benefit
limits.
The following Services and materials are excluded from coverage under the Policy:
A. Non-prescription items (e.g. Plano lenses) other than those listed in the Schedule(s) of Covered
Vision Care Services.
B. Services that the Covered Person, without cost, obtains from any governmental organization or
program.
C. Services for which the Covered Person is proved compensated under Workers' Compensation
Law, or other similar employer liability law.
D. Medical or surgical treatment for eye disease, which requires the services of a Physician.
E. Replacement or repair of lenses and/or frame that have been lost or broken.
F. Optional Lens Extras not listed in the Schedule of Covered Vision Care Services.
G. Technological devices such as smart phones and tablets used as Optical Low Vision Aids.
H. Missed appointment charges.
I. Applicable sales tax charged on Services.
J. Services that are not specifically covered by the Policy.
K. Procedures that are considered to be Experimental, Investigational or Unproven. The fact that an
Experimental, Investigational or Unproven Service, treatment, device or pharmacological regimen
is the only available treatment for a particular condition will not result in Benefits if the procedure is
considered to be Experimental, Investigational or Unproven in the treatment of that particular
condition.
L. Any Vision Service rendered by the Policyholder.
M. Intraocular lenses.
VCOC.18.NY 11
Section 3: When Coverage Begins
How Do You Enroll?
Eligible Persons must complete an enrollment form given to them by the Group. The Group will submit the
completed forms to us, along with any required Premium. We will not provide Benefits for vision care
services that you receive before your effective date of coverage.
Who Is Eligible for Coverage?
The Group determines who is eligible to enroll and who qualifies as a Dependent.
Eligible Person
Eligible Person usually refers to an employee or member of the Group who meets the eligibility rules.
When an Eligible Person enrolls, we refer to that person as a Subscriber. For a complete definition of
Eligible Person, Group and Subscriber, see Section 8: Defined Terms.
If both spouses are Eligible Persons of the Group, each may enroll as a Subscriber or be covered as an
Enrolled Dependent of the other, but not both.
Dependent
Dependent generally refers to the Subscriber's spouse and children. When a Dependent enrolls, we refer
to that person as an Enrolled Dependent. For a complete definition of Dependent and Enrolled
Dependent, see Section 8: Defined Terms.
Dependents of an Eligible Person may not enroll unless the Eligible Person is also covered under the
Policy.
If both parents of a Dependent child are enrolled as a Subscriber, only one parent may enroll the child as
a Dependent.
When Do You Enroll and When Does Coverage Begin?
Except as described below, Eligible Persons may not enroll themselves or their Dependents.
Initial Enrollment Period
When the Group purchases coverage under the Policy from us, the Initial Enrollment Period is the first
period of time when Eligible Persons can enroll themselves and their Dependents.
Coverage begins on the date shown in the Policy. We must receive the completed enrollment form and
any required Premium within 31 days of the date the Eligible Person becomes eligible.
Open Enrollment Period
The Group sets the Open Enrollment Period. During the Open Enrollment Period, Eligible Persons can
enroll themselves and their Dependents.
Coverage begins on the date identified by the Group. We must receive the completed enrollment form
and any required Premium within 31 days of the date the Eligible Person becomes eligible.
VCOC.18.NY 12
New Eligible Persons
Coverage for a new Eligible Person and his or her Dependents begins on the date agreed to by the
Group. We must receive the completed enrollment form and any required Premium within 31 days of the
date the new Eligible Person first becomes eligible.
Adding New Dependents
Subscribers may enroll Dependents who join their family because of any of the following events:
• Birth.
All vision benefits applicable for children, including the Necessary care or treatment of medically
diagnosed congenital defects or birth abnormalities, will apply with respect to your newborn child from the
moment of birth.
• Legal adoption and Placement for adoption.
All vision benefits applicable to children will apply to your adopted child, including a newborn child, from
the moment of placement in your residence.
In the case of a newborn child, coverage begins at the moment of birth if you have entered into a written
agreement to adopt such child.
• Marriage.
• Legal guardianship.
• Court or administrative order.
• Registering a Domestic Partner.
Coverage for the Dependent begins on the date of the event. We must receive the completed enrollment
form and any required Premium within 31 days of the event.
Special Enrollment Period
An Eligible Person and/or Dependent may also be able to enroll during a special enrollment period. A
special enrollment period is not available to an Eligible Person and his or her Dependents if coverage
under the prior plan ended for cause, or because premiums were not paid on a timely basis.
An Eligible Person and/or Dependent does not need to elect COBRA continuation coverage to preserve
special enrollment rights. Special enrollment is available to an Eligible Person and/or Dependent even if
COBRA is not elected.
A special enrollment period applies to an Eligible Person and any Dependents when one of the following
events occurs:
• Birth.
• Legal adoption.
• Placement for adoption.
• Marriage.
• Registering a Domestic Partner.
A special enrollment period also applies for an Eligible Person and/or Dependent who did not enroll
during the Initial Enrollment Period or Open Enrollment Period if any of the following are true:
VCOC.18.NY 13
• The Eligible Person previously declined coverage under the Policy, but the Eligible Person and/or
Dependent becomes eligible for a premium assistance subsidy under Medicaid or Children's Health
Insurance Program (CHIP). Coverage will begin only if we receive the completed enrollment form
and any required Premium within 60 days of the date of determination of subsidy eligibility.
• The Eligible Person and/or Dependent had existing vision coverage under another plan at the time
they had an opportunity to enroll during the Initial Enrollment Period or Open Enrollment Period and
coverage under the prior plan ended because of any of the following:
▪ Loss of eligibility (including legal separation, divorce or death).
▪ The employer stopped paying the contributions. This is true even if the Eligible Person
and/or Dependent continues to receive coverage under the prior plan and to pay the
amounts previously paid by the employer.
▪ In the case of COBRA continuation coverage, the coverage ended.
▪ The plan no longer offers benefits to a class of individuals that includes the Eligible Person
and/or Dependent.
▪ The Eligible Person and/or Dependent loses eligibility under Medicaid or Children's Health
Insurance Program (CHIP). Coverage will begin only if we receive the completed enrollment
form and any required Premium within 60 days of the date coverage ended.
When an event takes place (for example, a birth, marriage or determination of eligibility for state subsidy),
coverage begins on the date of the event. We must receive the completed enrollment form and any
required Premium within 31 days of the event unless otherwise noted above.
For an Eligible Person and/or Dependent who did not enroll during the Initial Enrollment Period or Open
Enrollment Period because they had existing health coverage under another plan, coverage begins on
the day following the day coverage under the prior plan ends. Except as otherwise noted above, coverage
will begin only if we receive the completed enrollment form and any required Premium within 31 days of
the date coverage under the prior plan ended.
VCOC.18.NY 14
Section 4: When Coverage Ends
General Information about When Coverage Ends
As permitted by law, we may end the Policy and/or all similar benefit plans at any time for the reasons
explained in the Policy.
Your right to Benefits automatically ends on the date that coverage ends. When your coverage ends, we
will still pay claims for Covered Vision Care Services that you received before the date your coverage
ended. However, once your coverage ends, we will not pay claims for any vision care services received
after that date.
Unless otherwise stated, an Enrolled Dependent's coverage ends on the date the Subscriber's coverage
ends.
What Events End Your Coverage?
Coverage ends on the earliest of the dates specified below, with a 30 day notice:
• The Entire Policy Ends
Your coverage ends on the date the Policy ends. In this event, the Group is responsible for
notifying you that your coverage has ended.
• You Are No Longer Eligible
Your coverage ends on the date you are no longer eligible to be a Subscriber or Enrolled
Dependent. Please refer to Section 8: Defined Terms for definitions of the terms "Eligible Person,"
"Subscriber," "Dependent" and "Enrolled Dependent."
• We Receive Notice to End Coverage
The Group is responsible for providing the required notice to us to end your coverage. Your
coverage ends on the date we receive the required notice from the Group to end your coverage, or
on the date requested in the notice, if later.
• Subscriber Retires or Is Pensioned
The Group is responsible for providing the required notice to us to end your coverage. Your
coverage ends the date the Subscriber is retired or receiving benefits under the Group's pension or
retirement plan.
This provision applies unless there is specific coverage classification for retired or pensioned
persons in the Group's Application, and only if the Subscriber continues to meet any applicable
eligibility requirements. The Group can provide you with specific information about what coverage
is available for retirees.
Fraud or Intentional Misrepresentation of a Material Fact
We will provide at least 30 days advance required notice to the Subscriber that coverage will end on the
date we identify in the notice because you committed an act, practice, or omission that constituted fraud,
or an intentional misrepresentation of a material fact. Examples include knowingly providing incorrect
information relating to another person's eligibility or status as a Dependent. You may appeal this decision
during the notice period. The notice will contain information on how to appeal the decision.
VCOC.18.NY 15
If we find that you have performed an act, practice, or omission that constitutes fraud, or have made an
intentional misrepresentation of material fact we have the right to demand that you pay back all Benefits
we paid to you, or paid in your name, during the time you were incorrectly covered under the Policy.
Coverage for a Disabled Dependent Child
Any unmarried dependent Child, regardless of age, who is incapable of self-sustaining employment by
reason of mental illness, developmental disability, mental retardation (as defined in the Mental Hygiene
Law), or physical handicap and who became so incapable prior to attainment of the age at which the
Child's coverage would otherwise terminate and who is chiefly dependent upon You for support and
maintenance, will remain covered while Your insurance remains in force and Your Child remains in such
condition. You have 31 days from the date of Your Child's attainment of the termination age to submit an
application to request that the Child be included in Your coverage and proof of the Child's incapacity. We
have the right to check whether a Child is and continues to qualify under this section.
We have the right to request and be furnished with such proof as may be needed to determine eligibility
status of a prospective or Covered Subscriber and all other prospective or Covered Members as they
pertain to eligibility for coverage under this Policy at any time.
Continuation of Coverage
If your coverage ends under the Policy, you may have the right to elect continuation coverage (coverage
that continues on in some form) in accordance with federal law.
Continuation coverage under COBRA (the federal Consolidated Omnibus Budget Reconciliation Act) is
available only to Groups that are subject to the terms of COBRA. Contact your plan administrator to find
out if your Group is subject to the provisions of COBRA.
If you chose continuation coverage under a prior plan which was then replaced by coverage under the
Policy, continuation coverage will end as scheduled under the prior plan or in accordance with federal or
state law, whichever is earlier.
We are not the Group's designated "plan administrator" as that term is used in federal law, and we do not
assume any responsibilities of a "plan administrator" according to federal law.
We are not obligated to provide continuation coverage to you if the Group or its plan administrator fails to
perform its responsibilities under federal law. Examples of the responsibilities of the Group or its plan
administrator are:
• Notifying you in a timely manner of the right to elect continuation coverage.
• Notifying us in a timely manner of your election of continuation coverage.
VCOC.18.NY 16
Section 5: How to File a Claim
How Are Covered Vision Care Services from Network Providers Paid?
We pay Network providers directly for your Covered Vision Care Services. If a Network provider bills you
for any Covered Vision Care Service, contact us. However, you are required to meet any applicable
Deductible and to pay any required Co-payments and/or Co-insurance to a Network provider. You will
also be responsible for any charges that are not covered by the Policy to your Vision Provider.
How Are Covered Vision Care Services from an Out-of-Network
Provider Paid?
When you receive Covered Vision Care Services from an out-of-Network provider you will be required to
pay all billed charges to your Vision Provider. You are also responsible for requesting payment from us.
You must file the claim in a format that contains all of the information we require, as described below.
You should submit a request for payment of Benefits within 90 days after the date of service. If you don't
provide this information to us within one year of the date of service, Benefits for that vision care service
will be denied or reduced, as determined by us. This time limit does not apply if you are legally
incapacitated.
Required Information
When you request payment of Benefits from us, you must provide us with all of the following information:
• The Subscriber's name and address.
• The patient's name and age.
• Your identification number.
• The name and address of the provider of the service(s).
• An itemized bill from your provider that includes a description of each charge.
The above information should be filed with us at Claims Department, PO Box 30978, Salt Lake City, UT
84130 or by fax to 248-733-6060. If you would like to use a claim form, you may access a form on the
Internet at www.myuhcvision.com or call us at 1-800-638-3120 and a claim form will be provided to you.
Payment of Benefits
If you provide written authorization to allow this, all or a portion of Benefits due to a provider may be paid
directly to the provider instead of being paid to the Subscriber. We will not reimburse third parties that
have purchased or been assigned benefits by Physicians or other Vision Providers.
Benefits will be paid to you unless either of the following is true:
• The Vision Provider notifies us that your signature is on file, assigning benefits directly to that
provider.
• You make a written request at the time you submit your claim.
Payment of Benefits under the Policy shall be in cash or cash equivalents, or in a form of other
consideration that we determine to be adequate. Where Benefits are payable directly to a provider, such
adequate consideration includes the forgiveness in whole or in part of the amount the provider owes us,
VCOC.18.NY 17
or to other plans for which we make payments where we have taken an assignment of the other plans'
recovery rights for value.
Obtaining Services
To find a Network Vision Provider, you may access a listing of Network Vision Providers on the Internet at
www.myuhcvision.com. You may also call the UnitedHealthcare Provider Locator Service at 1-800-839-
3242.
You also may obtain Vision Care Services from an out-of-Network Vision Provider. However, the amount
of Benefits may be reduced.
Foreign Services
Foreign Services will be treated as Out-of-Network Benefits under this Policy. Payments will be made in
U.S. currency and dispersed to the U.S. address of the Subscriber. We make no guarantee on value of
payment and will not protect against currency risk. Currency valuations for payment liability will be based
on exchange rates published on the date the Vision Care Services were rendered.
VCOC.18.NY 18
Section 6: Questions, Complaints and Appeals
To resolve a question, complaint, or appeal, just follow these steps:
What if You Have a Question?
Contact Customer Service at 1-800-638-3120. Representatives are available to take your call during
regular business hours, Monday through Friday.
What if You Have a Complaint?
Contact Customer Service at 1-800-638-3120. Representatives are available to take your call during
regular business hours, Monday through Friday.
If you would rather send your complaint to us in writing, the representative can provide you with the
address.
If the representative cannot resolve the issue over the phone, he/she can help you prepare and submit a
written complaint. We will notify you of our decision regarding your complaint within 60 days of receiving
it.
How Do You Appeal a Claim Decision?
How to Request an Appeal
If you disagree with either claim determination or a rescission of coverage determination, you can contact
us in writing to request an appeal.
Your request for an appeal should include:
• The patient's name and Policy number.
• The date(s) of vision service(s).
• The provider's name.
• The reason you believe the claim should be paid.
• Any documentation or other written information to support your request for claim payment.
Your appeal request must be submitted to us within 180 days after you receive claim denial.
Appeal Process
A qualified individual who was not involved in the decision being appealed will be chosen to decide the
appeal. If your appeal is related to clinical matters, the review will be done in consultation with a vision
care professional with expertise in the field, who was not involved in the prior determination. We may
consult with, or ask vision experts to take part in the appeal process. You consent to this referral and the
sharing of needed vision claim information. Upon request and free of charge, you have the right to
reasonable access to and copies of all documents, records and other information related to your claim for
Benefits. If any new or additional evidence is relied upon or generated by us during the determination of
the appeal, we will provide it to you free of charge and in advance of the due date of the response to the
adverse benefit determination.
VCOC.18.NY 19
Appeals Determinations
You will be provided written or electronic notification of the decision on your appeal as follows:
• For appeals of Benefits, the appeal will take place and you will be notified of the decision within 30
days from receipt of a request for appeal of a denied request for Benefits.
Please note that our decision is based only on whether or not Benefits are available under the Policy for
the proposed treatment or procedure.
VCOC.18.NY 20
Section 7: General Legal Provisions
What Is Your Relationship with Us?
It is important for you to understand our role with respect to the Group's Policy and how it may affect you.
We help finance or administer the Group's Policy in which you are enrolled. We do not provide vision
services or make treatment decisions. This means:
• We communicate to you decisions about whether the Group's Policy will cover or pay for the vision
care that you may receive. The Policy pays for Covered Vision Care Services, which are more fully
described in this Certificate.
• The Policy may not pay for all vision services or materials you or your Vision Provider may believe
are needed. If the Policy does not pay, you will be responsible for the cost.
We may use individually identifiable information about you to identify for you (and you alone) procedures,
products or services that you may find valuable. We will use individually identifiable information about you
as permitted or required by law, including in our operations and in our research. We will use de-identified
data for commercial purposes including research.
Please refer to our Notice of Privacy Practices for details.
What Is Our Relationship with Providers and Groups?
The relationships between us and Network Vision Providers and Groups are solely contractual
relationships between independent contractors. Network Vision Providers and Groups are not our agents
or employees. Neither we nor any of our employees are agents or employees of Network Vision Providers
or the Groups.
We do not provide vision care services or materials. We arrange for vision providers to participate in a
Network and we pay Benefits. Network Vision Providers are independent practitioners who run their own
offices and facilities. Our credentialing process confirms public information about the providers' licenses
and other credentials. It does not assure the quality of the services provided. They are not our employees
nor do we have any other relationship with Network vision providers such as principal-agent or joint
venture. We are not responsible for any act or omission of any vision provider.
We are not considered to be an employer for any purpose with respect to the administration or provision
of benefits under the Group's Policy. We are not responsible for fulfilling any duties or obligations of an
employer with respect to the Group's Policy.
The Group is solely responsible for all of the following:
• Enrollment and classification changes (including classification changes resulting in your enrollment
or the termination of your coverage).
• The timely payment of the Policy Charge to us.
• Notifying you of when the Policy ends.
When the Group purchases the Policy to provide coverage under a benefit plan governed by the
Employee Retirement Income Security Act ("ERISA"), 29 U.S.C. §1001 et seq., we are not the plan
administrator or named fiduciary of the benefit plan, as those terms are used in ERISA. If you have
questions about your welfare benefit plan, you should contact the Group. If you have any questions about
this statement or about your rights under ERISA, contact the nearest area office of the Employee Benefits
Security Administration, U. S. Department of Labor.
VCOC.18.NY 21
What Is Your Relationship with Providers and Groups?
The relationship between you and any vision provider is that of provider and patient.
You are responsible for all of the following:
• Choosing your own Vision Provider.
• Paying, directly to your Vision Provider, any amount identified as a member responsibility, including
Co-payments, Co-insurance, any Deductible and any amount that exceeds your Benefits.
• Paying, directly to your Vision Provider, the cost of any non-Covered Vision Care Service.
• Deciding if any Vision Provider treating you is right for you. This includes Network Vision Providers
you choose and vision providers that they refer.
• Deciding with your Vision Provider what care you should receive.
• Paying all billed charges, directly to your out-of-Network provider.
Your Vision Provider is solely responsible for the quality of the services provided to you.
The relationship between you and the Group is that of employer and employee, Dependent or other
classification as defined in the Policy.
Notice
When we provide written notice regarding administration of the Policy to an authorized representative of
the Group, that notice is deemed notice to all affected Subscribers and their Enrolled Dependents. The
Group is responsible for giving notice to you.
How Do We Use Headings?
The headings, titles and any table of contents contained in the Policy, Certificate or Schedule of Covered
Vision Care Services are for reference purposes only and shall not in any way affect the meaning or
interpretation of the Policy, Certificate or Schedule of Covered Vision Care Services.
Statements by Group or Subscriber
All statements made by the Group or by a Subscriber shall be deemed representations and not
warranties. We will not use any statement made by the Group to void the Policy after it has been in force
for two years.
Who Interprets Benefits and Other Provisions under the Policy?
We have the final authority to do all of the following:
• Interpret Benefits under the Policy.
• Interpret the other terms, conditions, limitations and exclusions set out in the Policy, including this
Certificate, the Schedule of Covered Vision Care Services and any Riders and/or Amendments.
• Make factual determinations related to the Policy and its Benefits.
We may assign this authority to other persons or entities that provide services in regard to the
administration of the Policy.
VCOC.18.NY 22
In certain circumstances, for purposes of overall cost savings or efficiency, we may offer Benefits for
services that would otherwise not be Covered Vision Care Services. The fact that we do so in any
particular case shall not in any way be deemed to require us to do so in other similar cases.
Who Provides Administrative Services?
We provide administrative services or, as we determine, we may arrange for various persons or entities to
provide administrative services, such as claims processing. The identity of the service providers and the
nature of the services they provide may be changed from time to time as we determine. We are not
required to give you prior notice of any such change, nor are we required to obtain your approval. You
must cooperate with those persons or entities in the performance of their responsibilities.
Amendments to the Policy
To the extent permitted by law, we have the right, as we determine and without your approval, to change,
interpret, withdraw or add Benefits or end the Policy.
Any provision of the Policy which, on its effective date, is in conflict with the requirements of state or
federal statutes or regulations (of the jurisdiction in which the Policy is delivered) is amended to conform
to the minimum requirements of such statutes and regulations.
No other change may be made to the Policy unless it is made by an Amendment or Rider which has been
signed by one of our officers and consistent with applicable notice requirements. All of the following
conditions apply:
• Amendments and Riders to the Policy are effective upon the Group's next anniversary date, except
as otherwise permitted by law.
• No agent has the authority to change the Policy or to waive any of its provisions.
• No one has authority to make any oral changes or amendments to the Policy.
How Do We Use Information and Records?
We may use your individually identifiable health information as follows:
• To administer the Policy and pay claims.
• To identify procedures, products, or services that you may find valuable.
• As otherwise permitted or required by law.
We may request additional information from you to decide your claim for Benefits. We will keep this
information confidential. We may also use de-identified data for commercial purposes, including research,
as permitted by law. More detail about how we may use or disclose your information is found in our
Notice of Privacy Practices.
By accepting Benefits under the Policy, you authorize and direct any person or institution that has
provided services to you to furnish us with all information or copies of records relating to the services
provided to you. We have the right to request this information at any reasonable time. This applies to all
Covered Persons, including Enrolled Dependents whether or not they have signed the Subscriber's
enrollment form. We agree that such information and records will be considered confidential.
We have the right to release records concerning vision care services when any of the following apply:
• Needed to put in place and administer the terms of the Policy.
• Needed for review or quality assessment.
VCOC.18.NY 23
• Required by law or regulation.
During and after the term of the Policy, we and our related entities may use and transfer the information
gathered under the Policy in a de-identified format for commercial purposes, including research and
analytic purposes. Please refer to our Notice of Privacy Practices.
For complete listings of your vision records or billing statements you may contact your Vision Provider.
Providers may charge you reasonable fees to cover their costs for providing records or completing
requested forms.
If you request vision forms or records from us, we also may charge you reasonable fees to cover costs for
completing the forms or providing the records.
In some cases, as permitted by law, we will designate other persons or entities to request records or
information from or related to you, and to release those records as needed. Our designees have the
same rights to this information as we have.
Do We Require Examination of Covered Persons?
In the event of a question or dispute regarding your right to Benefits, we may require that a Network
Vision Provider of our choice examine you at our expense.
Is Workers' Compensation Affected?
Benefits provided under the Policy do not substitute for and do not affect any requirements for coverage
by workers' compensation insurance.
When Do We Receive Refunds of Overpayments?
If we pay Benefits for expenses incurred on your account, you, or any other person or organization that
was paid, must make a refund to us if any of the following apply:
• All or some of the expenses were not paid or did not legally have to be paid by you.
• All or some of the payment we made exceeded the Benefits under the Policy.
• All or some of the payment was made in error.
The refund equals the amount we paid in excess of the amount we should have paid under the Policy. If
the refund is due from another person or organization, you agree to help us get the refund when
requested.
If the refund is due from you and you do not promptly refund the full amount, we may recover the
overpayment by reallocating the overpaid amount to pay, in whole or in part, your future Benefits that are
payable under the Policy. If the refund is due from a person or organization other than you, we may
recover the overpayment by reallocating the overpaid amount to pay, in whole or in part; (i) future
Benefits that are payable in connection with services provided to other Covered Persons under the Policy;
or (ii) future Benefits that are payment in connection with services provided to persons under other plans
for which we make payments, pursuant to a transaction in which our overpayment recovery rights are
assigned to such other plans in exchange for such plans' remittance of the amount of the reallocated
payment.
The reductions will equal the amount of the required refund. We may have other rights in addition to the
right to reduce future benefits.
VCOC.18.NY 24
Is There a Limitation of Action?
You cannot bring any legal action against us to recover reimbursement until sixty days after proof of loss
has been filed in accordance with the requirements of the policy. Any legal action against us must be
brought prior to the expiration of two years following the time such proof of loss is required.
What Is the Entire Policy?
The Policy, this Certificate, the Schedule of Covered Vision Care Services, the Group's Application and
any Riders and/or Amendments, make up the entire Policy that is issued to the Group.
VCOC.18.NY 25
Section 8: Defined Terms
Amendment - any attached written description of added or changed provisions to the Policy. It is
effective only when signed by us. It is subject to all conditions, limitations and exclusions of the Policy,
except for those that are specifically amended.
Benefits - your right to payment for Covered Vision Care Services that are available under the Policy.
Co-insurance - the charge, stated as a percentage, that you are required to pay for certain Covered
Vision Care Services.
Co-payment - the charge, stated as a set dollar amount, that you are required to pay for certain Covered
Vision Care Services.
Covered Contact Lens Formulary - a selection of available contact lenses that may be obtained from a
Network Vision Provider on a covered-in-full basis, subject to payment of any applicable Co-payment.
Covered Person - the Subscriber or a Dependent, but this term applies only while the person is enrolled
under the Policy. We use "you" and "your" in this Certificate to refer to a Covered Person.
Covered Vision Care Service(s) - vision care services which we determine to be all of the following:
• Necessary.
• Described as a Covered Vision Care Service in this Certificate under Section 1: Covered Vision
Care Services and in the Schedule of Covered Vision Care Services.
• Not excluded in this Certificate under Section 2: Exclusions and Limitations.
Dependent - the Subscriber's legal spouse or an unmarried child of the Subscriber or the Subscriber's
spouse. All references to the spouse of a Subscriber shall include a Domestic Partner, except for the
purpose of coordinating Benefits with Medicare. As described in Section 3: When Coverage Begins, the
Group determines who is eligible to enroll and who qualifies as a Dependent. The term "child" includes:
• A natural child.
• A stepchild.
• A legally adopted child.
• A child placed for adoption, including during any waiting period prior to the finalization of the
adoption.
• A child for whom legal guardianship has been awarded to the Subscriber or the Subscriber's
spouse.
• A child for whom vision care coverage is required through a Qualified Medical Child Support Order
or other court or administrative order. The Group is responsible for determining if an order meets
the criteria of a Qualified Medical Child Support Order.
The following conditions apply:
• A Dependent includes a child listed above under age 26.
• A Dependent includes an unmarried child age 26 or older who is or becomes disabled and
dependent upon the Subscriber.
A child who meets the requirements set forth above ceases to be eligible as a Dependent on the last day
of the month following the date the child reaches age 26.
VCOC.18.NY 26
The Subscriber must reimburse us for any Benefits paid during a time a child did not satisfy these
conditions.
A Dependent does not include anyone who is also enrolled as a Subscriber. No one can be a Dependent
of more than one Subscriber.
Designated Virtual Network Provider - a provider or facility that has entered into an agreement with us,
or with an organization contracting on our behalf, to deliver Covered Vision Care Services through live
audio and video technology.
Domestic Partner - Coverage is included for domestic partners, who are financially interdependent on
the employee or member.
The applicant must provide the following:
• Registration as a domestic partner or an affidavit of domestic partnership.
• Proof of cohabitation.
• Proof of financial interdependency by evidence of two or more of the following: joint bank account;
joint credit or charge card; joint obligation on a loan; status as authorized signatory on the partner's
bank account, credit card or charge card; joint ownership or holding of investments; joint ownership
of residence; joint ownership of real estate other than residence; listing of both partners as tenants
on lease; shared rental payments; shared household expenses; shared household budget for
purposes of receiving government benefits; joint ownership of major items of personal property;
joint ownership of a motor vehicle; joint responsibility for child care; shared child-care expenses;
execution of wills naming each other as executor and/or beneficiary; designation as beneficiary
under the other's life insurance policy or retirement benefits account; mutual grant of durable power
of attorney; mutual grant of authority to make health care decisions; affidavit by creditor or other
individual able to testify to partners' financial interdependence; other items of sufficient proof to
establish economic interdependency under the circumstances of the particular case.
Eligible Person - an employee of the Group or other person connected to the Group who meets the
eligibility requirements shown in both the Group's Application and the Policy.
Enrolled Dependent - a Dependent who is properly enrolled under the Policy.
Experimental or Investigational Service(s) - medical, surgical, diagnostic, psychiatric, mental health,
substance-related and addictive disorders or other health care services, technologies, supplies,
treatments, procedures, drug therapies, medications or devices that, at the time we make a determination
regarding coverage in a particular case, are determined to be any of the following:
• Not approved by the U.S. Food and Drug Administration (FDA) to be lawfully marketed for the
proposed use and not identified in the American Hospital Formulary Service or the United States
Pharmacopoeia Dispensing Information as appropriate for the proposed use.
• Subject to review and approval by any institutional review board for the proposed use. (Devices
which are FDA approved under the Humanitarian Use Device exemption are not Experimental or
Investigational.)
• The subject of an ongoing clinical trial that meets the definition of a Phase I, II or III clinical trial set
forth in the FDA regulations, regardless of whether the trial is actually subject to FDA oversight.
• Not demonstrated through prevailing peer-related professional literature to be safe and effective for
treating or diagnosing the condition or illness for which its use is proposed.
Foreign Services - services provided outside the U.S. and U.S. territories.
Group - the employer, or other defined or otherwise legally established group, to whom the Policy is
issued.
VCOC.18.NY 27
Initial Enrollment Period - the first period of time when Eligible Persons may enroll themselves and their
Dependents under the Policy.
Medicare - Parts A, B, C, and D of the insurance program established by Title XVIII, United States Social
Security Act, as amended by 42 U.S.C. Sections 1394, et seq. and as later amended.
Network - when used to describe a provider of vision care services, this means a provider that has a
participation agreement in effect (either directly or indirectly) with us or with our affiliate to participate in
our Network. This does not include those providers who have agreed to discount their charges for
Covered Vision Care Services. Our affiliates are those entities affiliated with us through common
ownership or control with us or with our ultimate corporate parent, including direct and indirect
subsidiaries.
A provider may enter into an agreement to provide only certain Covered Vision Care Services, but not all
Covered Vision Care Services, or to be a Network provider for only some of our products. In this case, the
provider will be a Network provider for the Covered Vision Care Services and products included in the
participation agreement and an out-of-Network provider for other Covered Vision Care Services and
products. The participation status of providers will change from time to time.
Network Benefits - the description of how Benefits are paid for Covered Vision Care Services provided
by Network Vision Providers. The Schedule of Covered Vision Care Services will tell you if your plan
offers Network Benefits and how Network Benefits apply.
Open Enrollment Period - a period of time, after the Initial Enrollment Period, when Eligible Persons
may enroll themselves and Dependents under the Policy. The Group sets the period of time that is the
Open Enrollment Period.
Out-of-Network Benefits - the description of how Benefits are paid for Covered Vision Care Services
provided by out-of-Network Vision Providers. The Schedule of Covered Vision Care Services will tell you
if your plan offers Out-of-Network Benefits and how Out-of-Network Benefits apply.
Physician - any Doctor of Medicine or Doctor of Osteopathy who is properly licensed and qualified by
law.
Please Note: Any podiatrist, dentist, psychologist, chiropractor, optometrist, or other provider who acts
within the scope of his or her license will be considered on the same basis as a Physician. The fact that
we describe a provider as a Physician does not mean that Benefits for services from that provider are
available to you under the Policy.
Policy - the entire agreement issued to the Group that includes all of the following:
• Group Policy.
• Certificate.
• Schedule of Covered Vision Care Services.
• Group Application.
• Riders.
• Amendments.
These documents make up the entire agreement that is issued to the Group.
Policy Charge - the sum of the Premiums for all Covered Persons enrolled under the Policy.
Premium - the periodic fee required for each Subscriber and each Enrolled Dependent, in accordance
with the terms of the Policy.
VCOC.18.NY 28
Rider - any attached written description of additional Covered Vision Care Services not described in this
Certificate. Covered Vision Care Services provided by a Rider may be subject to payment of additional
Premiums. Riders are effective only when signed by us and are subject to all conditions, limitations and
exclusions of the Policy except for those that are specifically amended in the Rider.
Subscriber - an Eligible Person who is properly enrolled under the Policy. The Subscriber is the person
(who is not a Dependent) on whose behalf the Policy is issued to the Group.
Vision Provider - any optometrist, ophthalmologist, surgeon, or other person who may lawfully provide
services to Covered Persons participating in our vision plans.

VSCH.18.NY 1
Schedule of Covered Vision Care Services
The following Vision Care Services will be covered, subject to a Co-payment, when obtained from
Network Providers.
When obtaining these Vision Care Services from a Network Provider, you will be required to pay a Co-
payment for certain Vision Care Services. The amount of Co-payment that a Network Provider will charge
is as noted in the column "Network Benefit" in the chart below.
When obtaining these Vision Care Services from an out-of-Network Provider, you will be required to pay
all billed charges at the time of service. You may then obtain reimbursement from us. Reimbursement for
out-of-Network Providers will be limited to the amounts noted in the column "Out-of-Network Benefit" in
the chart below.
SERVICE
K, M
FREQUENCY OF
SERVICE
NETWORK BENEFIT
The Amount You Pay
OUT-OF-NETWORK
BENEFIT
The Amount You Pay
Routine Vision
Examination for
Dependent children up
to age 13
Twice every 12 months Co-payment of $10
To a maximum of a $40
allowance
Routine Vision
Examination for
Covered Persons age
13 or older
Once every 12 months
Co-payment of $10
To a maximum of a $40
allowance
Routine Vision
Examination for
diabetics
Twice every 12 months Co-payment of $10
To a maximum of a $40
allowance
Refraction Only in lieu
of Routine Vision
Examination for
Dependent children up
to age 13
Twice every 12 months
To a maximum of a $0
allowance
To a maximum of a $40
allowance
Refraction Only in lieu
of Routine Vision
Examination for
Covered Persons age
13 or older
Once every 12 months
To a maximum of a $0
allowance
To a maximum of a $40
allowance
Retinal Photography
for diabetics
Once every 12 months Co-payment of $0
To a maximum of a $0
allowance
EYEGLASS
FRAME
B1, G
Once every 12 months
Eyeglass Frame
Co-payment of $0
C
to a
maximum of a $130
allowance
To a maximum of a $45
allowance
EYEGLASS
LENSES
B1
Once every 12 months

VSCH.18.NY 2
SERVICE
K, M
FREQUENCY OF
SERVICE
NETWORK BENEFIT
The Amount You Pay
OUT-OF-NETWORK
BENEFIT
The Amount You Pay
Single Vision Lenses*
Co-payment of $0
C
To a maximum of a $40
allowance
Bifocal-lined Lenses
Co-payment of $0
C
To a maximum of a $60
allowance
Trifocal-lined Lenses
Co-payment of $0
C
To a maximum of a $80
allowance
Lenticular Lenses
Co-payment of $0
C
To a maximum of a $80
allowance
OPTIONAL LENS
EXTRAS
F
Once every 12 months
Standard Scratch
Coating
Co-payment of $0
To a maximum of a $0
allowance
Oversize Lenses
80% of retail billed
charge after a Co-
payment of $0
C
toward
Covered Eyeglass
Lenses
To a maximum of a $0
allowance
Blended Bifocal
Lenses
80% of retail billed
charge after a Co-
payment of $0
C
toward
Covered Eyeglass
Lenses
To a maximum of a $0
allowance
Standard Progressive
Lenses
After a Co-payment of
$0
C
toward Covered
Eyeglass Lenses and
the lesser of $55 or
retail billed charge
To a maximum of a $0
allowance
Deluxe Progressive
Lenses
After a Co-payment of
$0
C
toward Covered
Eyeglass Lenses and
the lesser of $100 or
retail billed charge
To a maximum of a $0
allowance
Premium Progressive
Lenses
After a Co-payment of
$0
C
toward Covered
Eyeglass Lenses and
the lesser of $150 or
retail billed charge
To a maximum of a $0
allowance
Platinum Progressive
Lenses
After a Co-payment of
$0
C
toward Covered
Eyeglass Lenses and
the lesser of $200 or
retail billed charge
To a maximum of a $0
allowance

VSCH.18.NY 3
SERVICE
K, M
FREQUENCY OF
SERVICE
NETWORK BENEFIT
The Amount You Pay
OUT-OF-NETWORK
BENEFIT
The Amount You Pay
Aspheric Lenses
80% of retail billed
charge after a Co-
payment of $0
C
toward
Covered Eyeglass
Lenses
To a maximum of a $0
allowance
Digital Single Vision
Lenses
80% of retail billed
charge after a Co-
payment of $0
C
toward
Covered Eyeglass
Lenses
To a maximum of a $0
allowance
Polycarbonate for
Dependent children up
to age 19
Co-payment of $0
To a maximum of a $0
allowance
Cataract Lenses
80% of retail billed
charge after a Co-
payment of $0
C
toward
Covered Eyeglass
Lenses
To a maximum of a $0
allowance
Occupational Double
Segment Lenses
80% of retail billed
charge after a Co-
payment of $0
C
toward
Covered Eyeglass
Lenses
To a maximum of a $0
allowance
CONTACT
LENSES
B1, H
Once every 12 months
Contact Lenses
Formulary
J
Co-payment of $0 for
up to 4 boxes from the
Covered Contact Lens
Formulary
D
. One Co-
payment for Contact
Lens Fitting and
Evaluation and Contact
Lenses combined if
from the Covered
Contact Lens
Formulary
D
to a
maximum of a $130
allowance for Contact
Lenses that are not on
the Formulary
D
.
To a maximum of a
$130 allowance
Necessary Contact
Lenses
Co-payment of $0
To a maximum of a
$210 allowance
B1
You are eligible to select only one of either eyeglasses (Eyeglass Lenses/or Eyeglass Lenses and
Eyeglass Frame) or Contact Lenses. If you select more than one of these Vision Care Services, only one
VSCH.18.NY 4
service will be covered. Once the contact lens option is selected and the lenses are fitted, they may not
be exchanged for eyeglasses.
C
If you purchase Eyeglass Lenses and Eyeglass Frames at the same time from the same Network
Provider, only one Co-payment will apply to those Eyeglass Lenses and Eyeglass Frames together.
D
Coverage for Covered Contact Lens Formulary will not apply at Walmart, Sam's Club, and Costco
locations. Other Network locations may not offer Formulary contact lenses. In those cases, your
allowance for Contact Lenses that are not on the Formulary will apply.
F
Coverage for some Optional Lens Extras, which may include progressive lenses, may be included with
eyeglass packages offered at some Network locations.
G
Some eyeglass frame brands may not be available for purchase as a Covered Vision Service, or may
be subject to additional limitations.
H
Necessary contact lenses are in lieu of Contact Lenses.
J
If Contact Lenses that are not on the Formulary are prescribed; the member will be responsible for the
Contact Lens Fitting and Evaluation.
K
If you choose to use a promotional offer from a provider your claim may be reimbursed based on the
out-of-Network coverage.
M
Additional detail on your plan can be directed to Customer Service 1-800-638-3120.
*Single vision lens are defined as one single power across their entire surface with a single optical center
and made from CR-39.

I
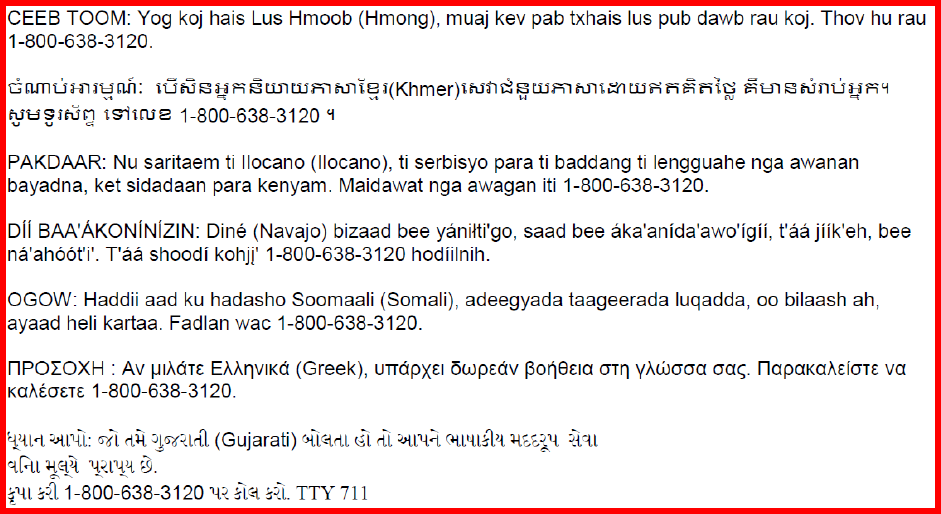
Language Assistance Services
We
1
provide free language services to help you communicate with us. We offer interpreters, letters in
other languages, and letters in other formats like large print. To get help, please call 1-800-638-3120, or
the toll-free member phone number listed on your vision plan ID card, TTY/RTT 711. We are available
Monday through Friday, 8 a.m. to 8 p.m. ET.
ATENCION :
Si
habla espafiol (Spanish
),
hay servicios de asistencia de idiomas, sin cargo, a su
disposici6n. Llame al 1-800-638-3120.
ph&fax
XIN LU'U Y: Neu quy
vi
n6i tieng Viet (Vietnamese), quy
vise
dlJ'Q'C
cung cap dich
Vl,J
trQ'
giup ve ng6n
ngo,
mien
ph
i.
Vui long goi 1-800-638-3120.
gt
~:
"tl-
~
O~(
Korean) ~ N§o~
J...I~
~-9-
'2:!
o~ Ai
r:!
J,.1
1::::ll
A ~ -'f'-li~ Ol§o
~~
-4='
'.?1&
LI
Cr
. 1-800-638-
3120
'ti
O
~
~
2~
o~~
J...l
.2.
.
PAUNAWA: Kung nagsasalita
ka
ng
Tagalog (Tagalog), may makukuha kang mga libreng serbisyo ng
tulong sa wi
ka
. Mangyaring tumawag sa 1-800-638-3120.
BH
VIM
AHVIE : 6ecnnaTHble ycnyrn
nepeBOAa
AOCTynHbl
An51
nlOAe~
, 4e~
POAHO
~
51361K
51Bn5leTC51
PycC
K
l,1~
(Russi
an
).
no3BOH"1Te
no
HOMepy
1-800-638-3120.
ph&fax
ATANSYON :
Si
w pale Kreyol ayisyen (Haitian Creole), ou kapab benefisye sevis
ki
gratis pou ede w nan
lang pa
w.
Tanpri rele nan 1-800-638-3120.
ATTENTION : Si vous parlez frani;:ais (French), des services d'aide linguistique vous sont proposes
gratuitement. Veuillez appeler le
1-800-638-3120.
UWAGA: Jezeli
m6
wisz po polsku (Polish), udost~pnilismy darmowe us!ugi tlumacza. Prosimy zadzwonic
pod numer
1-800-638-3120.
ATEN<;Ao: Se voce fala portugues (Portuguese), contate o serv
ii;:o
de assistencia de idiomas gratuito.
Ligue para 1-800-638-3120.
ATTENZIONE: in caso la lingua parlata sia l'italiano (Italian), sono disponibili servizi
di
assistenza
linguistica gratuiti. Si prega
di
chiamare
ii
numero 1-800-638-3120.
ACHTUNG: Falls Sie Deutsch (German) sprechen, stehen Ihnen kostenlos sprach
li
che
Hilfsdienstleistu ngen zur VerfOgung . Rufen Sie
1-800-638-3120 an.
;
1~$-lJi
: B *~g (Japanese)
~~!~
ti,-Q ~-g-,
~:J!;j
.
O)
~
~g3i:t
i -+t-
t::
'
A~
.:.
'
f1
J
ffl
L
'f.::
t.::
It
*9
0
1-800-638-312
01=;1=3
~
~!(
f
.::
~L\
0
~
.)
J W 1
)-1j
p l :
<\.;,,-
;i
_
.i.:;t,
($"
\......::,
)
#,.
I
.J..l
u~
I.J
.J
..ib
4../
__,;t,
j
..ib
.. l
wl..
.S
,c::.,..,
I (Farsi)
1-800-638-3120 .
..leJ?--/
u-:W
¥TT
~
,n,:r
~:
'l"R
3TT1l
~
(Hindi)
mm
~ en-~
IBc;
'ITTl'.fT
~
~
f.:t
:~
'0
9 ~1 "'~ ~ I ¥TT~
cfiTT1
~
1-800-
638-3120
ph&fax
II
CEEB TOOM: Yog koj hais Lus Hmoob (Hmong), muaj kev pab txhais
lu
s pub dawb rau koj. Thov
hu
rau
1-800-638-3120.
6
runt.:a-n
l~nii:
iu w s tt n s
lifl
wrn
hl"l t
'2
l(
Khmer)t n1t1cl §
wrn
hl"l
\
c-Yl
wrl
n
~
n
i~
~t::rl
s n1nu
ttn'i
~H:1~
l hJ'.:)
tsiHUB
1-800-638-3120 'i
PAKDAAR: Nu saritaem ti llocano (llocano), ti serbisyo para
ti
baddang
ti
lengguahe nga awanan
bayadna, ket sidadaan para kenyam. Maidawat nga awagan iti 1-800-638-3120.
Dif BAA'AKONiNiZIN: D
in
e
(N
avajo) bizaad bee yanHti'go, saad bee aka'an ida'awo'ig ii, t'aa jiik'eh, bee
na'ah66t'i'.
T'aa
shood i kohji' 1-800-638-3120 hodiilnih .
OGOW: Haddii aad ku hadasho Soomaali (Soma
li
), adeegyada taageerada luqadda, oo bilaash ah ,
ayaad heli kartaa. Fadlan wac 1-800-638-3120.
nPOLOXH
: Av
µIMTE
EMriv
I
Kd
(Greek),
UTTCIPXE
I owpEdV
~0~8E
Ia
crrr1
y"Awcrcra
crac;
.
napa
K
aAE
i
OTE
va
KaAtcrnE 1-800-638-3120.
tJ,'.1.l.-J.
:1.,w
-tt:
15'6'L
<i.il.
J_!15'6':/.L
<i.1
(Gujarati)
l>ll'=l
<i.l
~1
<i.L
:/.>U"Y.::J.
Gll
4.
U,1
1-l
l-l
tti"Y.
~AL
0
{Hl
1~"il.
"Y,_:/.
l"Y,_1-l
0.
!s"Y.
L
1;
;[1.
1-800-638-3120
"Y.
:/.
!sl'=l
!s
:U.
.
TTY
7
11
<-
III
Notice of Non-Discrimination
We
1
do not treat members differently because of sex, age, race, color, disability or national origin.
If you think you were treated unfairly because of your sex, age, race, color, disability or national origin,
you can send a complaint to:
Civil Rights Coordinator
UnitedHealthcare Civil Rights Grievance
P.O. Box 30608
Salt Lake City, UTAH 84130
You must send the complaint within 60 days of the incident. We will send you a decision within 30 days. If
you disagree with the decision, you have 15 days to appeal.
If you need help with your complaint, please call 1-800-638-3120 or the toll-free member phone number
listed on your vision plan ID card, TTY/RTT 711. We are available Monday through Friday, 8 a.m. to 8
p.m.
You can also file a complaint with the U.S. Dept. of Health and Human services.
Online: https://ocrportal.hhs.gov/ocr/portal/lobby.jsf
Complaint forms are available at http://www.hhs.gov/ocr/office/file/index.html.
Phone: Toll-free 1-800-368-1019, 800-537-7697 (TDD)
Mail: U.S. Dept. of Health and Human Services. 200 Independence Avenue, SW Room 509F, HHH
Building Washington, D.C. 20201
1
For purposes of the Language Assistance Services and this Non-Discrimination Notice ("Notice"), "we"
refers to the entities listed in Footnote 2 of the Notice of Privacy Practices and Footnote 3 of the Financial
Information Privacy Notice. Please note that not all entities listed are covered by this Notice.
IV
Claims and Appeal Notice
This Notice is provided to you in order to describe our responsibilities under Federal law for making
benefit determinations and your right to appeal adverse benefit determinations. To the extent that state
law provides you with more generous timelines or opportunities for appeal, those rights also apply to you.
Please refer to your benefit documents for information about your rights under state law.
How to Request an Appeal
If you disagree with a claim determination or a rescission of coverage determination, you can contact us
in writing to request an appeal.
Your request for an appeal should include:
• The patient's name and Policy number.
• The date(s) of Vision Service(s).
• The provider's name.
• The reason you believe the claim should be paid.
• Any documentation or other written information to support your request for claim payment.
Your appeal request must be submitted to us within 180 days after you receive the claim denial.
Appeal Process
A qualified individual who was not involved in the decision being appealed will be chosen to decide the
appeal. If your appeal is related to clinical matters, the review will be done in consultation with a Vision
care professional with experience in the field, who was not involved in the prior determination. We may
consult with, or ask vision experts to take part in the appeal process. You consent to this referral and the
sharing of needed vision claim information. Upon request and free of charge, you have the right to
reasonable access to and copies of all documents, records and other information related to your claim for
Benefits. If any new or additional evidence is relied upon or generated by us during the determination of
the appeal, we will provide it to you free of charge and in advance of the due date of the response to the
adverse benefit determination.
Appeals Determinations
You will be provided written or electronic notification of the decision on your appeal as follows:
• For appeals of Benefits, the appeal will take place and you will be notified of the decision within 30
days from receipt of a request for appeal of a denied request for Benefits.
Please note that our decision is based only on whether or not Benefits are available under the Policy for
the proposed treatment or procedure.
You may have the right to external review through an Independent Review Organization (IRO) upon the
completion of the internal appeal process. Instructions regarding any such rights, and how to access
those rights, will be provided in our decision letter to you.
V
VISION PLAN NOTICES OF PRIVACY PRACTICES
MEDICAL INFORMATION PRIVACY NOTICE
THIS NOTICE DESCRIBES HOW MEDICAL INFORMATION ABOUT YOU MAY BE USED AND
DISCLOSED AND HOW YOU CAN GET ACCESS TO THIS INFORMATION.
PLEASE REVIEW IT CAREFULLY.
Effective January 1, 2022
We
2
are required by law to protect the privacy of your health information. We are also required to send
you this notice, which explains how we may use information about you and when we can give out or
"disclose" that information to others. You also have rights regarding your health information that are
described in this notice. We are required by law to abide by the terms of this notice.
The terms "information" or "health information" in this notice include any information we maintain that
reasonably can be used to identify you and that relates to your physical or mental health care condition,
the provision of health care to you, or the payment for such health care. We will comply with the
requirements of applicable privacy laws related to notifying you in the event of a breach of your health
information.
We have the right to change our privacy practices and the terms of this notice. If we make a material
change to our privacy practices, we will provide to you, in our next annual distribution, either a revised
notice or information about the material change and how to obtain a revised notice. We will provide you
with this information either by direct mail or electronically, in accordance with applicable law. In all cases,
if we maintain a website for your particular vision plan, we will post the revised notice on your vision plan
website, such as www.myuhcvision.com. We have the right to make any revised or changed notice
effective for information we already have and for information that we receive in the future.
UnitedHealth Group collects and maintains oral, written and electronic information to administer our
business and to provide products, services and information of importance to our enrollees. We maintain
physical, electronic and procedural security safeguards in the handling and maintenance of our enrollee
information, in accordance with applicable state and federal standards, to protect against risks such as
loss, destruction or misuse.
How We Use or Disclose Information
We must use and disclose your health information to provide that information:
• To you or someone who has the legal right to act for you (your personal representative) in order to
administer your rights as described in this notice.
• To the Secretary of the Department of Health and Human Services, if necessary, to make sure
your privacy is protected.
We have the right to use and disclose health information for your treatment, to pay for your health care
and to operate our business. For example, we may use or disclose your health information:
• For Payment of premiums due us, to determine your coverage, and to process claims for health
care services you receive, including for subrogation or coordination of other benefits you may have.
For example, we may tell a doctor whether you are eligible for coverage and what percentage of
the bill may be covered.
• For Treatment. We may use or disclose health information to aid in your treatment or the
coordination of your care. For example, we may disclose information to your physicians or hospitals
to help them provide medical care to you.
VI
• For Health Care Operations. We may use or disclose health information as needed to operate
and manage our business activities related to providing and managing your health care coverage.
For example, we might talk to your physician to suggest a disease management or wellness
program that could help improve your health or we may analyze data to determine how we can
improve our services. We may also de-identify health information in accordance with applicable
laws. After that information is de-identified, the information is no longer subject to this notice and
we may use the information for any lawful purpose.
• To Provide You Information on Health Related Programs or Products such as alternative
medical treatments and programs or about health-related products and services, subject to limits
imposed by law.
• For Plan Sponsors. If your coverage is through an employer sponsored group health plan, we
may share summary health information and enrollment and disenrollment information with the plan
sponsor. In addition, we may share other health information with the plan sponsor for plan
administration if the plan sponsor agrees to special restrictions on its use and disclosure of the
information in accordance with federal law.
• For Underwriting Purposes. We may use or disclose your health information for underwriting
purposes; however, we will not use or disclose your genetic information for such purposes.
• For Reminders. We may use or disclose health information to send you reminders about your
benefits or care, such as appointment reminders with providers who provide medical care to you.
We may use or disclose your health information for the following purposes under limited circumstances:
• As Required by Law. We may disclose information when required to do so by law.
• To Persons Involved With Your Care. We may use or disclose your health information to a
person involved in your care or who helps pay for your care, such as a family member, when you
are incapacitated or in an emergency, or when you agree or fail to object when given the
opportunity. If you are unavailable or unable to object, we will use our best judgment to decide if
the disclosure is in your best interests. Special rules apply regarding when we may disclose health
information to family members and others involved in a deceased individual's care. We may
disclose health information to any persons involved, prior to the death, in the care or payment for
care of a deceased individual, unless we are aware that doing so would be inconsistent with a
preference previously expressed by the deceased.
• For Public Health Activities such as reporting or preventing disease outbreaks to a public health
authority.
• For Reporting Victims of Abuse, Neglect or Domestic Violence to government authorities that
are authorized by law to receive such information, including a social service or protective service
agency.
• For Health Oversight Activities to a health oversight agency for activities authorized by law, such
as licensure, governmental audits and fraud and abuse investigations.
• For Judicial or Administrative Proceedings such as in response to a court order, search warrant
or subpoena.
• For Law Enforcement Purposes. We may disclose your health information to a law enforcement
official for purposes such as providing limited information to locate a missing person or report a
crime.
• To Avoid a Serious Threat to Health or Safety to you, another person, or the public, by, for
example, disclosing information to public health agencies or law enforcement authorities, or in the
event of an emergency or natural disaster.
VII
• For Specialized Government Functions such as military and veteran activities, national security
and intelligence activities, and the protective services for the President and others.
• For Workers' Compensation as authorized by, or to the extent necessary to comply with, state
workers compensation laws that govern job-related injuries or illness.
• For Research Purposes such as research related to the review of certain treatments or the
prevention of disease or disability, if the research study meets privacy law requirements.
• To Provide Information Regarding Decedents. We may disclose information to a coroner or
medical examiner to identify a deceased person, determine a cause of death, or as authorized by
law. We may also disclose information to funeral directors as needed to carry out their duties.
• For Organ Procurement Purposes. We may use or disclose information to entities that handle
procurement, banking or transplantation of organs, eyes or tissue to facilitate donation and
transplantation.
• To Correctional Institutions or Law Enforcement Officials if you are an inmate of a correctional
institution or under the custody of a law enforcement official, but only if needed (1) for the institution
to provide you with health care; (2) to protect your health and safety or the health and safety of
others; or (3) for the safety and security of the correctional institution.
• To Business Associates that perform functions on our behalf or provide us with services if the
information is needed for such functions or services. Our business associates are required, under
contract with us and according to federal law, to protect the privacy of your information and are not
allowed to use or disclose any information other than as shown in our contract as permitted by
federal law.
• Additional Restrictions on Use and Disclosure. Certain federal and state laws may require
special privacy protections that restrict the use and disclosure of certain health information,
including highly confidential information about you. Such laws may protect the following types of
information:
1. Alcohol and Substance Abuse
2. Biometric Information
3. Child or Adult Abuse or Neglect, including Sexual Assault
4. Communicable Diseases
5. Genetic Information
6. HIV/AIDS
7. Mental Health
8. Minors' Information
9. Prescriptions
10. Reproductive Health
11. Sexually Transmitted Diseases
If a use or disclosure of health information described above in this notice is prohibited or materially limited
by other laws that apply to us, it is our intent to meet the requirements of the more stringent law.
Except for uses and disclosures described and limited as stated in this notice, we will use and disclose
your health information only with a written authorization from you. This includes, except for limited
circumstances allowed by federal privacy law, not using or disclosing psychotherapy notes about you,
VIII
selling your health information to others, or using or disclosing your health information for certain
promotional communications that are prohibited marketing communications under federal law, without
your written authorization. Once you give us authorization to release your health information, we cannot
guarantee that the recipient to whom the information is provided will not disclose the information. You
may take back or "revoke" your written authorization at any time in writing, except if we have already
acted based on your authorization. To find out where to mail your written authorization and how to revoke
an authorization, call the phone number listed on your vision plan ID card.
What Are Your Rights
The following are your rights with respect to your health information:
• You have the right to ask to restrict uses or disclosures of your information for treatment,
payment, or health care operations. You also have the right to ask to restrict disclosures to family
members or to others who are involved in your health care or payment for your health care. We
may also have policies on dependent access that authorize your dependents to request certain
restrictions. Please note that while we will try to honor your request and will permit requests
consistent with our policies, we are not required to agree to any restriction.
• You have the right to ask to receive confidential communications of information in a different
manner or at a different place (for example, by sending information to a P.O. Box instead of your
home address). We will accommodate reasonable requests where a disclosure of all or part of your
health information otherwise could endanger you. In certain circumstances, we will accept your
verbal request to receive confidential communications, however; we may also require you confirm
your request in writing. In addition, any requests to change or cancel a previous confidential
communication request must be made in writing. Mail your request to the address listed below.
• You have the right to see and get a copy of certain health information we maintain about you
such as claims and case or medical management records. If we maintain your health information
electronically, you will have the right to request that we send a copy of your health information in an
electronic format to you. You can also request that we provide a copy of your information to a third
party that you identify. In some cases, you may receive a summary of this health information. You
must make a written request to inspect and copy your health information or have your information
sent to a third party. Mail your request to the address listed below. In certain limited circumstances,
we may deny your request to inspect and copy your health information. If we deny your request,
you may have the right to have the denial reviewed. We may charge a reasonable fee for any
copies.
• You have the right to ask to amend certain health information we maintain about you such as
claims and case or medical management records, if you believe the health information about you is
wrong or incomplete. Your request must be in writing and provide the reasons for the requested
amendment. Mail your request to the address listed below. If we deny your request, you may have
a statement of your disagreement added to your health information.
• You have the right to receive an accounting of certain disclosures of your information made by
us during the six years prior to your request. This accounting will not include disclosures of
information made: (i) for treatment, payment, and health care operations purposes; (ii) to you or
according to your authorization; and (iii) to correctional institutions or law enforcement officials; and
(iv) other disclosures for which federal law does not require us to provide an accounting.
• You have the right to a paper copy of this notice. You may ask for a copy of this notice at any
time. Even if you have agreed to receive this notice electronically, you are still entitled to a paper
copy of this notice. You also may get a copy of this notice on your vision plan website, such as
www.myuhcvision.com.
IX
Exercising Your Rights
• Contacting your Vision Plan. If you have any questions about this notice or want information
about exercising your rights, please call the toll-free member phone number on your vision ID card
or you may call us at 1-800-638-3120, or TTY 711.
• Submitting a Written Request. You can mail your written requests to exercise any of your rights,
including modifying or cancelling a confidential communication, requesting copies of your records,
or requesting amendments to your record, to us at the following address:
UnitedHealthcare
Vision HIPAA - Privacy Unit
PO Box 30978
Salt Lake City, UT 84130
• Filing a Complaint. If you believe your privacy rights have been violated, you may file a complaint
with us at the address listed above.
You may also notify the Secretary of the U.S. Department of Health and Human Services of your
complaint. We will not take any action against you for filing a complaint.
2
This Vision Information Notice of Privacy Practices applies to the following health plans that are affiliated
with UnitedHealth Group: UnitedHealthcare Insurance Company and UnitedHealthcare Insurance
Company of New York. This list of vision plans is complete as of the effective date of this notice. For a
current list of vision plans subject to this notice go to www.uhc.com/privacy/entities-fn-v3.
X
FINANCIAL INFORMATION PRIVACY NOTICE
THIS NOTICE DESCRIBES HOW FINANCIAL INFORMATION ABOUT YOU MAY BE USED AND
DISCLOSED.
PLEASE REVIEW IT CAREFULLY.
Effective January 1, 2022
We
3
are committed to maintaining the confidentiality of your personal financial information. For the
purposes of this notice, "personal financial information" means information, other than health information,
about an enrollee or an applicant for health care coverage that identifies the individual, is not generally
publicly available and is collected from the individual or is obtained in connection with providing health
care coverage to the individual.
Information We Collect
Depending upon the product or service you have with us, we may collect personal financial information
about you from the following sources:
• Information we receive from you on applications or other forms, such as name, address, age,
medical information and Social Security number.
• Information about your transactions with us, our affiliates or others, such as premium payment and
claims history.
• Information from a consumer reporting agency.
Disclosure of Information
We do not disclose personal financial information about our enrollees or former enrollees to any third
party, except as required or permitted by law. For example, in the course of our general business
practices, we may, as permitted by law, disclose any of the personal financial information that we collect
about you without your authorization, to the following types of institutions:
▪ To our corporate affiliates, which include financial service providers, such as other insurers,
and non-financial companies, such as data processors.
▪ To nonaffiliated companies for our everyday business purposes, such as to process your
transactions, maintain your account(s), or respond to court orders and legal investigations.
▪ To nonaffiliated companies that perform services for us, including sending promotional
communications on our behalf.
Confidentiality and Security
We maintain physical, electronic and procedural safeguards in accordance with applicable state and
federal standards to protect your personal financial information against risks such as loss, destruction or
misuse. These measures include computer safeguards, secured files and buildings, and restrictions on
who may access your personal financial information.
Questions about this Notice
If you have any questions about this notice, please call the toll-free member phone number on your vision
plan ID card or call us at 1-800-638-3120, or TTY 711.
3
For purposes of this Financial Information Privacy Notice, "we" or "us" refers to the entities listed in
footnote 2, beginning on the first page of the Health Plan Notices of Privacy Practices, plus the following
UnitedHealthcare affiliate: Spectera, Inc. This Financial Information Privacy Notice only applies where
required by law. Specifically, it does not apply to any other UnitedHealth Group health plans in states that
XII
Statement of Employee Retirement Income Security
Act of 1974 (ERISA) Rights
As a participant in the plan, you are entitled to certain rights and protections under the Employee
Retirement Income Security Act of 1974 (ERISA).
Receive Information about Your Plan and Benefits
You are entitled to examine, without charge, at the Plan Administrator's office and at other specified
locations, such as worksites and union halls, all documents governing the plan, including insurance
contracts and collective bargaining agreements, and a copy of the latest annual report (Form 5500
Series), if applicable, filed by the plan with the U.S. Department of Labor and available at the Public
Disclosure Room of the Employee Benefits Security Administration.
You are entitled to get, upon written request to the Plan Administrator, copies of documents governing the
operation of the plan, including insurance contracts and collective bargaining agreements, and copies of
the latest annual report (Form 5500 Series), if applicable and updated Summary Plan Description. The
Plan Administrator may make a reasonable charge for the copies.
Continue Group Health Plan Coverage
You are entitled to continue health care coverage for yourself, spouse or Dependents if there is a loss of
coverage under the plan due to a qualifying event. You or your Dependents may have to pay for such
coverage. The Plan Sponsor is responsible for providing you notice of your Consolidated Omnibus
Budget Reconciliation Act (COBRA) continuation rights. Review the Summary Plan Description and the
documents governing the plan on the rules governing your COBRA continuation coverage rights.
Prudent Actions by Plan Fiduciaries
In addition to creating rights for plan participants, ERISA imposes duties upon the people who are
responsible for the operation of the employee benefit plan. The people who operate your plan, called
"fiduciaries" of the plan, have a duty to do so prudently and in the interest of you and other plan
participants and beneficiaries. No one, including your employer, your union, or any other person may fire
you or otherwise discriminate against you in any way to prevent you from obtaining a welfare benefit or
exercising your rights under ERISA.
Enforce Your Rights
If your claim for a welfare benefit is denied or ignored, in whole or in part, you have a right to know why
this was done, to get copies of documents relating to the decision without charge, and to appeal any
denial, all within certain time schedules. Under ERISA, there are steps you can take to enforce the above
rights. For instance, if you request a copy of plan documents or the latest annual report from the plan and
do not receive them within 30 days, you may file suit in a Federal court. In such a case, the court may
require the Plan Administrator to provide the materials and pay you up to $156 a day (subject to
adjustment based on inflation) until you receive the materials, unless the materials were not sent because
of reasons beyond the control of the Plan Administrator. If you have a claim for Benefits which is denied
or ignored, in whole or in part, you may file suit in a state or Federal court. In addition, if you disagree with
the plan's decision or lack thereof concerning the qualified status of a domestic relations order or a
medical child support order, you may file suit in Federal court. If it should happen that plan fiduciaries
misuse the plan's money, or if you are discriminated against for asserting your rights, you may seek
assistance from the U.S. Department of Labor, or you may file suit in a Federal court. The court will
decide who should pay court costs and legal fees. If you are successful, the court may order the person
XIII
you have sued to pay these costs and fees. If you lose, the court may order you to pay these costs and
fees, for example, if it finds your claim is frivolous.
Assistance with Your Questions
If you have any questions about your plan, you should contact the Plan Administrator. If you have any
questions about this statement or about your rights under ERISA, or if you need assistance in obtaining
documents from the Plan Administrator, you should contact the nearest office of the Employee Benefits
Security Administration, U.S. Department of Labor listed in your telephone directory or the Division of
Technical Assistance and Inquiries, Employee Benefits Security Administration, U.S. Department of
Labor, 200 Constitution Avenue, N.W., Washington, D.C. 20210. You may also get certain publications
about your rights and responsibilities under ERISA by calling the publication hotline of the Employee
Benefits Security Administration.
XIV
ERISA Statement
If the Group is subject to ERISA, the following information applies to you.
Summary Plan Description
Name of Plan: Columbia University Welfare Benefit Plan
Name, Address and Telephone Number of Plan Sponsor and Named Fiduciary:
Columbia University
615 West 131st Street
New York, NY 10027
(212) 851-0649
The Plan Sponsor retains all fiduciary responsibilities with respect to the Plan, except to the extent the
Plan Sponsor has assigned or allocated to other persons or entities one or more fiduciary responsibilities
with respect to the Plan.
Claims Fiduciary: UnitedHealthcare Insurance Company ("UnitedHealthcare," refer to your Certificate of
Coverage for details on the legal entity that provides your coverage) is your Plan's Claims Fiduciary and
has been assigned this responsibility by your Plan Sponsor. Your Claims Fiduciary has the authority to
require eligible individuals to furnish it with information necessary for the proper administration of your
Plan.
Employer Identification Number (EIN): 13-5598093
Plan Number: 515
Plan Year: January 1 through December 31
Type of Plan: Health care coverage plan
Name, Business Address, and Business Telephone Number of Plan Administrator:
Columbia University
615 West 131st Street
New York, NY 10027
(212) 851-0649
Type of Administration of the Plan: Your Plan is fully insured. Benefits are provided under a group
insurance contract entered into between your Plan Sponsor and UnitedHealthcare. Claims for benefits
are sent to UnitedHealthcare. Your employer and UnitedHealthcare share responsibility for administering
the plan.
UnitedHealthcare
2950 Expressway Drive
Suite 240
Islandia, NY 11749-1412
800-357-1371
Person designated as Agent for Service of Legal Process: Plan Administrator
Discretionary Authority of Plan Administrator and Other Plan Fiduciaries: The Plan Administrator
and other Plan fiduciaries shall have discretionary authority to interpret the terms of the Plan and to
determine eligibility for benefits in accordance with the terms of the Plan. Any interpretation or
determination made according to such discretionary authority shall be given deference and be legally
binding on all parties and subject to review by a legal authority only to the extent the decision was
arbitrary and capricious.
XV
Source of Contributions and Funding under the Plan: There are no contributions to the Plan. Any
required employee contributions are used to partially reimburse the Plan Sponsor for Premiums under the
Plan. Benefits under the Plan are funded by the payment of Premium required by the group Policy.
Method of Calculating the Amount of Contribution: Employee-required contributions to the Plan
Sponsor are the employee's share of costs as determined by Plan Sponsor. From time to time, the Plan
Sponsor will determine the required employee contributions for reimbursement to the Plan Sponsor and
distribute a schedule of such required contributions to employees.
Qualified Medical Child Support Orders: The Plan's procedures for handling qualified medical child
support orders are available without charge upon request to the Plan Administrator.
Amendment or Termination of the Plan: Your employer, as the Plan Sponsor, has the right to amend or
terminate this Plan at any time. Note that the insurance contract, which is how benefits under the Plan are
provided, is not necessarily the same as the Plan. As a result, termination of the insurance contract does
not necessarily terminate the Plan.
1446790 - 10/26/2022
