
1
Last updated on September 26, 2023
Cognitive Vitality Reports® are reports written by neuroscientists at the Alzheimer’s Drug
Discovery Foundation (ADDF). These scientific reports include analysis of drugs, drugs-in-
development, drug targets, supplements, nutraceuticals, food/drink, non-pharmacologic
interventions, and risk factors. Neuroscientists evaluate the potential benefit (or harm) for brain
health, as well as for age-related health concerns that can affect brain health (e.g.,
cardiovascular diseases, cancers, diabetes/metabolic syndrome). In addition, these reports
include evaluation of safety data, from clinical trials if available, and from preclinical models.
Melatonin
Evidence Summary
Melatonin may improve sleep onset, blood pressure, lipid profile, metabolic profile, and antioxidant
defenses. It is not recommended for dementia patients due to risks of falls and other adverse events.
Neuroprotective Benefit: A meta-analysis reported melatonin improved cognitive function in
mild AD patients. But melatonin and other sleep medications increase risks of falls and other
adverse events and are not recommended for dementia patients.
Aging and related health concerns: Aside from its effect on sleep onset, melatonin treatment
has shown benefits in preventing delirium, reducing blood pressure, reducing cholesterol and
triglycerides, and improving metabolic and antioxidant biomarkers.
Safety: Melatonin is considered safe for most healthy adults but a few contraindications are
known and long-term use has not been extensively studied. The use of melatonin is not
recommended for elderly patients with dementia due to increased risks of falls.
2
Last updated on September 26, 2023
Availability: OTC in the US; Rx
in EU, UK, and other countries.
Dose: As a sleep-aid, melatonin is
often taken orally in doses of 1-5
mg per day before bed.
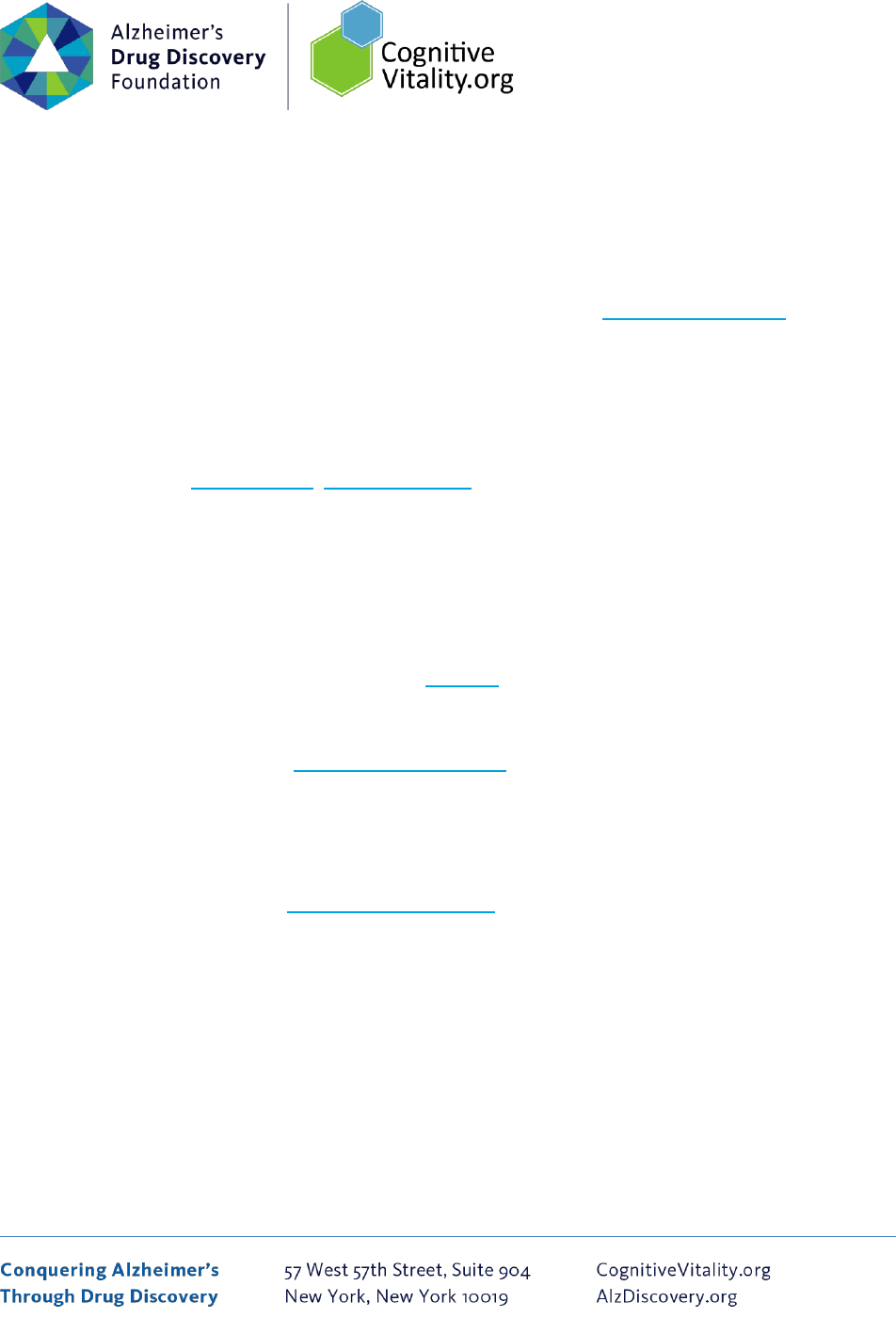
Chemical formula: C
13
H
16
N
2
O
2
MW: 232.2783
Source: PubChem
Common brand: Circadin®
(prolonged release form)
Half-life: ~45 minutes;
prolonged release forms have
elimination terminal half-life
of 3.5-4.0 hours
BBB: penetrant
Clinical trials: Meta-analyses
of randomized controlled trials
have examined the effects of
melatonin in thousands of
patients with various
conditions.
Observational studies: Small
studies have examined the
relationship between melatonin
levels and aging/dementia.
What is it?
In humans and other animals, melatonin is a hormone produced by the pineal gland located in the brain.
It acts in various ways throughout the body and regulates sleep-wake cycles, also known as circadian
rhythms. As we age, we produce less melatonin, which is thought to account for disrupted and
disordered sleep in older adults. Melatonin is commonly used to treat sleep disorders such as insomnia.
Melatonin treatment is also effective in alleviating symptoms of jet lag after travel across time zones
[Miyamoto et al., 2009].
In the US, melatonin is available as a dietary supplement. In Europe, a sustained-release form of
melatonin is licensed as a medicine for short-term treatment of primary insomnia in adults aged 55
years and older. Melatonin treatment has also been tested extensively in various conditions, including
metabolic diseases, liver conditions, surgery patients, cancer patients, prevention of delirium, and
others. Several melatonin receptor agonists have also been developed and are marketed for insomnia
and other conditions (described in the Sources & Dosing section).

3
Last updated on September 26, 2023
Neuroprotective Benefit: A meta-analysis reported melatonin improved cognitive function in mild AD
patients. But melatonin and other sleep medications increase risks of falls and other adverse events and
are not recommended for dementia patients.
Types of evidence:
• 8 meta-analyses or systematic reviews of clinical trials testing melatonin treatment
• 1 meta-analysis of animal studies
• Numerous observational studies examining melatonin levels/production
• 2 reviews/guidelines from the US Department of Health & Human Services and the American
Academy of Sleep Medicine
• Numerous preclinical studies on possible mechanisms of action.
Human research to suggest prevention of dementia, prevention of decline, or improved cognitive
function:
A 2021 meta-analyses of up to 11 randomized controlled trials in healthy people reported that
melatonin treatment (ranging from 0.1 mg to 80 mg daily) during the daytime did not slow reaction time
scores or reduce memory function, but significantly decreased accuracy on attention tasks (standardized
mean difference=-0.74; p<0.00001)[Sumsuzzman et al., 2021]. A subgroup analysis showed that
melatonin treatment at noon significantly reduced memory (p<0.00001), while melatonin treatment in
the afternoon did not. Subgroup analyses regarding reaction time demonstrated that a melatonin dose
of 5 mg did not affect reaction time, while doses of 10 mg or higher slowed reaction time (p<0.00001
and 0.0002, respectively). In general, melatonin treatment is recommended at night, before bedtime.
Thus, it is not unusual for melatonin treatment during the day to cause fatigue and sleepiness,
contributing to reduced cognitive performance.
In a double-blind randomized controlled trial enrolling 26 healthy older adults, 1 mg of melatonin daily
for 4 weeks improved feelings of restedness and verbal fluency scores [Peck et al., 2004]. A single-blind
placebo-controlled trial of 50 healthy young men showed that a single oral dose of 3 mg melatonin
enhanced recognition memory of objects encoded under stress, but not of objects encoded in the
absence of stress [Rimmele et al., 2009]. In another randomized controlled trial of 10 healthy
volunteers, application of melatonin cream did not result in significant effects on cognitive parameters
[Scheuer et al., 2016].
4
Last updated on September 26, 2023
Human research to suggest benefits to patients with dementia:
Elderly people with Alzheimer’s disease typically exhibit sleep disturbance, including shorter sleep
duration, fragmented sleep, and a disrupted circadian rhythm. These disturbances in sleep and circadian
rhythm are associated with cognitive decline and memory impairment [Srinivasan et al., 2010]. People
with Alzheimer’s disease and other dementias often experience “sundowning”, which refers to
increased confusion occurring from dusk through the night, with symptoms including disorganized
thinking, reduced attention to external stimuli, agitation, and emotional disturbances. Several studies
have shown that melatonin levels in the cerebral spinal fluid are lower in Alzheimer’s patients compared
to age-matched control subjects, and an impairment in melatonin production at night correlates with
cognitive impairment [Liu et al., 1999; Magri et al., 1997].
Numerous meta-analyses and systematic reviews have evaluated whether melatonin treatment benefits
patients with dementia, with some positive findings, but overall the results are mixed and inconclusive.
A 2015 meta-analysis of 7 studies including 520 patients with dementia concluded that melatonin
therapy improved sleep efficacy and extended total sleep time. However, there was no evidence that
these improvements impacted cognitive function [Xu, 2015]. A smaller 2016 meta-analysis of patients
with Alzheimer’s and other dementias (including 176-279 patients, depending on the outcome measure
of interest) also concluded that melatonin did not improve cognitive scores (MMSE and ADAS-Cog) or
the majority of measures of sleep [Trotti and Karroum, 2016].
A more recent 2021 meta-analysis and systematic review of up to 9 randomized controlled trials in
people with Alzheimer’s disease reported that melatonin treatment (0.15 to 6 mg before bed) for over
12 weeks improved cognitive function, as measured by the Mini-Mental State Examination (MMSE;
mean difference=1.82, p<0.0001)[Sumsuzzman et al., 2021]. Melatonin treatment significantly improved
global cognition in people with mild Alzheimer’s disease (MMSE at or above 20; mean difference-1.89;
p<0.0001), but not in people with moderate Alzheimer’s disease (MMSE above 10, below 20; p=0.98).
When examining the duration of melatonin treatment, long-term treatment over 12 weeks significantly
improved global cognitive function (mean difference=1.82; p<0.0001), but short-term treatment failed
to improve cognitive function (p=0.33).
A 2020 Cochrane meta-analysis of 4 types of sleep medications for dementia patients reported that
there was low-certainty evidence that melatonin treatment (2-10 mg/night) may have little or no effect

5
Last updated on September 26, 2023
on sleep outcomes (total nocturnal sleep time and ratio of daytime to night-time sleep) over 8 to 10
weeks of treatment in people with Alzheimer’s disease and sleep disturbances [McCleery and Sharpley,
2020]. This meta-analysis included up to 5 randomized controlled trials that tested melatonin treatment
against placebo, with a total of 253 participants. Three studies reported cognitive outcomes and a meta-
analysis found that there may be little or no effect of melatonin on cognition assessed with change from
baseline in either MMSE (mean difference=0.09; 95% CI, –0.85 to 1.03) or ADAS-Cog (mean difference=-
1.03; 95% CI, -2.70 to 0.65). Based on the inconsistency across studies and the low sample size, the
evidence was deemed to be of low certainty. Three studies reported outcomes on activities of daily
living (e.g., ADCS-ADL), and the meta-analysis found moderate-certainty evidence that melatonin
probably has little or no effect on activities of daily living (standardized mean difference=-0.04; 95% CI, -
0.34 to 0.26).
A 2022 network meta-analysis of 50 randomized controlled trials in Alzheimer’s disease patients
(including a total of 19,704 patients) compared melatonin treatment against FDA-approved medications
for Alzheimer’s disease (donepezil, galantamine, rivastigmine, memantine, and Namzaric) [Tseng et al.,
2022]. This network meta-analysis found that medium-term (at least 6 months but <1 year) low-dose
melatonin treatment (less than or equal to 3 mg per night) is associated with the highest post-treatment
cognitive score, measured by MMSE (mean difference=1.48; 95% Cis, 0.51 to 2.46), among all
investigated medications. Medium-term high-dose donepezil was associated with the second highest
post-treatment MMSE score. Melatonin treatment was also associated with the highest post-treatment
quality of life compared to other treatments. However, the authors note that future large-scale, long-
term treatment studies are needed to focus on the efficacy of different dosages and treatment
durations of melatonin supplementation.
In 2015, the American Academy of Sleep Medicine recommended against the use of melatonin and
discrete sleep-promoting medications for elderly people with dementia due to increased risks of falls
and other adverse events [Auger et al., 2015]. However, disrupted or fragmented sleep can worsen the
pathology of dementia by impairing clearance of toxic proteins from the brain. A randomized controlled
study suggested that the combined use of light therapy in the morning and melatonin in the evening (5
mg) may be a possible approach in addressing circadian dysregulation in Alzheimer’s patients [Dowling
et al., 2008; Steele et al., 2021]. The benefit to risk ratio of melatonin use needs to be carefully
evaluated with healthcare providers, especially in dementia patients.
6
Last updated on September 26, 2023
Mechanisms of action for neuroprotection identified from laboratory and clinical research:
Results from multiple studies suggest that melatonin can reduce neurodegenerative processes and
improve cognitive function through various mechanisms.
Mouse models of Alzheimer’s disease: In a meta-analysis of 9 studies using mouse models of
Alzheimer’s disease, melatonin treatment ameliorated learning and memory (measured by the Morris
water maze) and reduced Aβ40 and Aβ42 deposition in the cortex [Zhai et al., 2022].
Neurogenesis: Neurogenesis is the growth and proliferation of new neurons in the hippocampus, an
area of the brain responsible for learning and memory. Neurogenesis decreases with age and is reduced
in disorders like depression and Alzheimer’s disease. In animal studies, melatonin supplementation
stimulated the creation of new neurons and promoted cell survival in the hippocampus of aged mice.
However, after 12 months of melatonin treatment, there was no effect in cell proliferation or survival,
indicating that melatonin may delay, but not stop the decline of neurogenesis [Ramirez-Rodriguez,
2012].
Mitochondria function: Mitochondria are organelles that are essential for generating energy in a cell. In
Alzheimer’s disease, mitochondrial dysfunction is an early event and triggers cell degradation and death.
In pre-clinical animal studies, it is suggested that melatonin helps in cell energy production by improving
signaling in the mitochondria [Acuna-Castroviejo, 2001; Dragicevic, 2012]. Melatonin is also an
antioxidant with the ability to scavenge “free radicals” and prevent DNA and protein damage. In animal
studies, melatonin treatment inhibited neuronal damage and counteracted neurodegenerative
conditions like oxidative stress [Feng, 2006].
Circadian rhythm and sleep: Circadian rhythms regulate human sleep-wake patterns through hormonal
release and other bodily functions. Disturbances in sleep-wake cycles have been associated with an
increased risk of dementia [Gehrman, 2005]. Melatonin is a hormone that is directly involved in the
regulation of circadian rhythm that has been shown to decrease with age. Animal studies suggest that
melatonin may significantly improve circadian rhythm dysfunction and sleep impairment. In small
clinical trials, some modest benefits of melatonin in sleep and circadian rhythm have been reported, but
overall, the evidence is limited [Auger et al., 2015].
APOE4 interactions: In a test tube experiment, melatonin treatment in the presence of ApoE4 resulted
in the inhibition of amyloid-β fibril formation, a component of Alzheimer’s pathology. In addition,
7
Last updated on September 26, 2023
melatonin prevented the neurotoxicity mediated by amyloid-β and ApoE4 [Poeggeler, 2001]. However,
no other studies have confirmed this initial finding and no clinical studies in humans have reported that
melatonin may have different effects in APOE4 carriers versus non-carriers.
Aging and related health concerns: Aside from its effect on sleep onset, melatonin treatment has
shown benefits in preventing delirium, reducing blood pressure, reducing cholesterol and triglycerides,
and improving metabolic and antioxidant biomarkers.
Types of evidence:
• 17 meta-analyses or systematic reviews of clinical trials testing melatonin treatment
• Several review articles
• Numerous preclinical studies
Longevity: UNKNOWN
Some evidence from test tube experiments suggests that melatonin may influence the activity of
telomerase, an enzyme responsible for regulating cellular aging [Leon-Blanco, 2003; Rastmanesh,
2011]. However, the impact of this influence on life span in humans still needs to be
researched. Researchers are also exploring whether melatonin and/or light entrainment of circadian
rhythm [Cajochen, 2003] can improve outcomes in critically ill patients [Madrid-Navarro, 2015] and
reduce the need for sedation [Mistraletti, 2015].
Insomnia: PROLONGED-RELEASE MELATONIN MAY IMPROVE SLEEP ONSET LATENCY
Sleep is critically important for long-term health [Hublin, 2007]. Consequences of insomnia can include
reduced productivity, higher health care costs, increased accident risk, and risks of diabetes, obesity,
hypertension, coronary heart disease, and depression [CDC.gov/sleep].
The first-generation drugs for insomnia were barbiturates, including pentobarbital and phenobarbital,
which have a high abuse potential and significant risks of overdose and respiratory suppression
[reviewed in Miyamoto et al., 2009]. The second-generation insomnia drugs were benzodiazepines, such
as lorazepam, triazolam, and estazolam. While benzodiazepines have a lower potential for abuse and
risk of overdose, they are associated with side effects including cognitive impairment, psychomotor
impairment, dependence, tolerance, rebound insomnia, and others. Third-generation drugs were

8
Last updated on September 26, 2023
benzodiazepine receptor agonists with non-benzodiazepine chemical structures: zolpidem, zopiclone,
zaleplon, and others. These benzodiazepine receptor agonists were aimed to induce sleep while
reducing the cognitive and motor side effects. However, these agonists still have abuse and dependence
potential. It is worth noting that sleep induced by benzodiazepines and benzodiazepine receptor
agonists is electrophysiologically distinct from naturally occurring sleep [Borbely et al., 1985; Brunner et
al., 1991]. For example, these drugs decrease REM sleep and increase stage 2 sleep. More recently,
direct administration of exogenous melatonin and/or melatonin receptor agonists has garnered interest
and attention.
In a 2023 meta-analysis of 22 randomized controlled trials (total of 4,875 participants) testing melatonin
or ramelteon (melatonin receptor agonist) in adults with insomnia disorder, treatment with prolonged
release melatonin showed efficacy with small to medium effect sizes on subjective sleep onset latency
(weighted difference= -6.30 min; p=0.031) and objective sleep onset latency (weighted difference=-5.05
min; p<0.001)[Maruani et al., 2023]. In a subgroup analysis, prolonged release melatonin was efficacious
in improving objective sleep efficiency in people at or over 55 years old (weighted difference=2.95%;
p<0.001). No significant effects of melatonin treatment (prolonged release or immediate release) were
found on subjective or objective total sleep time or on wakefulness after sleep onset compared to
placebo. Melatonin treatment was also not effective in reducing the number of awakenings or
improving sleep quality compared to placebo. Immediate release melatonin treatment did not
significantly reduce sleep onset latency compared with placebo when administered for 4 weeks or less.
Authors of this meta-analysis noted that a first-line therapy for insomnia is typically cognitive behavioral
treatment (CBT), which has shown larger effects than melatonin treatment. However, in cases where
CBT is not possible or only partially effective, benefits may be derived from the addition of prolonged
release melatonin.
In a 2022 network meta-analysis of 170 trials testing 30 interventions for insomnia disorder in a total of
44,089 adults, benzodiazepines, eszopiclone, zolpidem, and zopiclone were more efficacious than
melatonin, ramelteon, and zaleplon with regards to acute treatment [De Crescenzo et al., 2022].
However, benzodiazepines are associated with poor tolerability, risk of cognitive impairment, delirium,
falls, and motor accidents, and therefore, are not ideal for long-term use [American Geriatrics Society
2015 Beers Criteria update]. Other benzodiazepine receptor agonists have also been associated with
emergency department visits. When considering all outcomes at different time points, lemborexant and
eszopiclone had the best profile in terms of efficacy, acceptability, and tolerability [De Crescenzo et al.,
2022]. Overall, melatonin and the melatonin receptor agonist, ramelteon, had poor efficacy compared
to other classes of insomnia medications. The authors of this meta-analysis emphasize the importance
9
Last updated on September 26, 2023
of considering non-pharmacological treatments for insomnia disorder, as they are supported by high-
quality evidence and recommended as first-line treatment by guidelines [Riemann et al., 2017].
In a 2017 Clinical Practice Guideline for the pharmacologic treatment of chronic insomnia in adults by
the American Academy of Sleep Medicine, melatonin is recommended against for the treatment of sleep
onset or sleep maintenance insomnia [Sateia et al., 2017]. For sleep onset insomnia, eszopiclone,
zaleplon, zolpidem, triazolam, and ramelteon are recommended. For sleep maintenance insomnia,
suvorexant, zolpidem, temazepam, and doxepin are recommended. However, all of these
recommendations are weak recommendations (based on the GRADE process) reflecting a lower degree
of certainty in the outcome and appropriateness of the patient-care strategy for all patients.
Delirium: MAY DECREASE DELIRIUM INCIDENCE AND DURATION BUT FINDINGS ARE MIXED
Delirium is characterized by disturbance in attention, awareness, and cognition. Delirium is a common
complication in hospitalized patients, especially in older patients, and it is associated with a longer
hospital stay, increased risk of functional and cognitive decline, increased dementia risk, and increased
mortality risk [Pereira et al., 2021; Inouye et al., 2023]. Other predisposing factors of delirium include
medical comorbidities (e.g., pre-existing cognitive impairment, atherosclerosis, etc.), medication use,
intraoperative factors (e.g., use of benzodiazepines, highly invasive surgery), postoperative factors (e.g.,
pain), and circadian rhythm disturbance [Barnes et al., 2023]. Sleep deprivation and delirium share
behavioral and biological similarities, including disturbances in the sleep-wake cycle and abnormal
melatonin secretion [Weinhouse et al., 2009; Yoshitaka et al., 2013]. Observational studies have
reported lower plasma melatonin levels in people with delirium compared to those without delirium
[Yoshitaka et al., 2013]. While the causes of delirium are not clearly defined and likely vary across
people, several potential causes are modulated by melatonin, including diurnal sleep disturbance,
melatonin dysregulation, neuroinflammation, oxidative stress, and neurotransmitter dysregulation
[Maldonado, 2013].
In a 2023 meta-analysis of 8 randomized controlled trials in ICU patients, melatonin treatment did not
significantly reduce delirium incidence (RR=0.76; 95% CI, 0.54 to 1.07; p=0.12), based on 6 randomized
controlled trials that included a total of 1,625 patients [Aiello et al., 2023]. However, a sensitivity
analysis that added 4 studies (2 retrospective studies and 2 randomized controlled trials) showed that
melatonin/ramelteon reduced delirium risk (RR=0.67; 95% CI, 0.48 to 0.92; p=0.01). Of secondary
outcomes, there was a trend towards a reduction in the duration of mechanical ventilation (mean
difference, -2.80; p=0.09), but no significant effects in the ICU length of stay (mean difference, -0.26;

10
Last updated on September 26, 2023
p=0.42) or mortality (RR=0.85; p=0.30). The GRADE of evidence suggests a very low certainty of evidence
due to the risk of bias in several studies (ranging from low to high risk). The trial sequential analysis
showed that the sample size required was far from sufficient, with only 1,625 patients enrolled in the
included randomized controlled trials versus the 13,699 patients needed. The authors concluded that
the results are not yet robust, and more studies are needed to validate these findings.
In a 2023 meta-analysis of 4 randomized controlled trials and 2 cohort studies including a total of 2,374
ICU patients, melatonin treatment (3-5 mg) did not reduce the incidence of delirium (OR=0.71; 95% CI,
0.46 to 1.12; p=0.14) [Duan et al., 2023]. However, subgroup analysis showed that melatonin treatment
reduced the incidence of delirium in the cardiovascular care unit (OR=0.52; 95% CI, 0.37 to 0.73;
p=0.0001), but not in the general ICU (OR=1.14; 95% CI, 0.86 to 1.50; p=0.35). There were no significant
melatonin treatment effects on all-cause mortality (OR=0.85; 95% CI, 0.66 to 1.09; p=0.20), length of ICU
stay (mean difference=0.33; p=0.45) or length of hospital stay (mean difference=0.51; p=0.55). The
authors speculate that the preferential benefit of melatonin in the cardiovascular care unit patients may
be related to improved vascular endothelial cell function, anti-vasospasmic effects, anti-apoptotic
effects, improved cerebral perfusion, and reduced microthrombosis.
In a 2023 systematic review and meta-analysis of 11 randomized controlled trials including a total of
1,244 surgery patients, melatonin (3-5 mg or 50 mg/kg per day) or ramelteon treatment (melatonin
agonist; 8 mg per day) resulted in a significantly lower odds of developing postoperative delirium
(OR=0.41; 95% CI, 0.21 to 0.80; p=0.01)[Barnes et al., 2023]. The incidence of delirium ranged from 0-
42% in the intervention groups and 4-92% in the control groups. Because of the lack of reported data,
meta-analyses could not be performed for secondary outcomes or complications. Caveats include the
heterogeneity of the published clinical trials, varied outcome measures across studies, and the highly
variable populations, dosing, and melatonin administration regimens.
In a 2023 meta-analysis of 3 randomized controlled trials and 6 observational studies in a total of 1,211
patients with delirium, melatonin treatment reduced the duration of delirium (-1.72 days, 95% CI, -2.66
to -0.77; p=0.0004) based on 2 randomized controlled trials [Beaucage-Charron et al., 2023]. Melatonin
treatment did not significantly improve hospital length of stay compared to antipsychotics. The authors
noted that the current data is limited for melatonin as the majority of included studies were at high risk
of bias due to limited availability of information regarding study methods. Ongoing studies will likely
provide better insight.

11
Last updated on September 26, 2023
Prior meta-analyses have found that dexmedetomidine, a selective α2-adrenergic receptor agonist, is
effective in reducing the incidence of delirium by about 50%. A 2020 review that explored different
preventive interventions for delirium noted that ramelteon and dexmedetomidine appear to have the
best supporting evidence thus far [Fontaine et al., 2020]. There is a lack of studies comparing
melatonergic agents with dexmedetomidine and other agents thought to prevent delirium.
Dexmedetomidine is associated with a high dropout rate and adverse events such as bradycardia and
hypotension. It is also worth noting that the route of administration for dexmedetomidine (continuous
intravenous infusion) precludes at-home use of dexmedetomidine.
Prevention and management of delirium involve many non-pharmacological interventions, such as
overnight eye masks, ear plugs, early mobilization, limiting the use of sedative drugs, and strategies to
improve the quality of sleep.
Hypertension: REDUCES BLOOD PRESSURE
Hypertension is a major cause of cardiovascular events and deaths, yet proper blood pressure control is
not achieved by many patients. In a 2022 meta-analysis of 4 randomized controlled trials in people with
hypertension or nocturnal hypertension, controlled release melatonin treatment for 3-4 weeks
significantly reduced nocturnal systolic blood pressure by 3.57 mmHg (95% CI, -7.88 to 0.73)[Lee et al.,
2022]. Melatonin treatment also lowered nocturnal and awake diastolic blood pressure, but these
changes were not statistically significant. Immediate release melatonin treatment had a lack of effect on
blood pressure measures, likely due to the short half-life of around 45 minutes. The overall certainty of
the evidence was low for all blood pressure outcomes because there were only a few included studies to
assess publication bias, and most randomized controlled trials had an unclear risk of bias or imprecision
in outcomes. Melatonin treatment may reduce blood pressure by vasodilation (via inhibition of calcium
channels and enhancement of nitric oxide and cGMP production in the endothelium), antioxidation, and
inhibition of the sympathetic nervous system (reduction of noradrenaline).
In a meta-analysis of 5 randomized controlled trials in people with metabolic impairment (metabolic
syndrome, diabetes, coronary heart disease, and NAFLD), melatonin treatment significantly reduced
systolic blood pressure (mean difference=-3.43 mmHg; 95% CI, -5.76 to -1.09; p=0.004) and diastolic
blood pressure (mean difference=-3.33 mmHg; 95% CI, -4.57 to -2.08; p<0.001) compared with control
treatment [Hadi et al., 2019]. Sensitivity analysis indicated that the results were robust and there was no
evidence regarding publication bias.

12
Last updated on September 26, 2023
Cardiovascular disease: MAY PROTECT AGAINST ISCHEMIC-REPURFUSION INJURY
Ischemic-reperfusion injury during coronary artery bypass graft (CABG) is associated with increased
oxidative stress, inflammation, and apoptosis, and it can lead to serious complications such as
arrhythmia and myocardial injury. Numerous studies have examined the efficacies of antioxidant
interventions before or during CABG surgery. In a 2023 meta-analysis of 6 randomized controlled trials
with a total of 342 CABG surgery patients, melatonin treatment (3-20 mg per day) led to a significant
reduction in a cardiac injury marker, cardiac troponin I (weighted mean difference [WMD]=-2.28 ng/ml;
95% CI, -2.87 to -1.69; p<0.01) and high sensitivity CRP levels (WMD=-0.62 mg/L; 95% CI, -0.73 to -0.5;
p<0.01)[Farshidianfar et al., 2023]. There was a non-significant decrease in creatine kinase isozyme
muscle/brain (CK-MB) levels (WMD=-2.87 ng/ml; 95% CI, -5.97 to 0.23; p=0.07) with melatonin
treatment. Melatonin treatment schedules varied from just 2 doses to over 1 month. Based on the
Egger’s test, no publication bias was found.
In a 2021 meta-analysis of 7 randomized controlled trials including a total of 426 patients who
underwent myocardial revascularization, melatonin treatment (orally or i.v. or i.c.) resulted in a higher
left ventricular ejection fraction (LVEF) than placebo treatment (WMD=3.1%; 95% CI, 0.6 to 5.5; p=0.01)
[Dominguez-Rodriguez et al., 2021]. Melatonin-treated patients also had lower levels of troponin
(standardized mean difference=-1.76; 95% CI, -2.85 to -0.67; p=0.002). Because only two randomized
controlled trials reported the myocardial infarct size, a meta-analysis could not be performed on this
measure.
Hyperlipidemia: MAY DECREASE LDL-CHOLESTEROL AND TRIGLYCERIDE LEVELS
Dyslipidemia plays an important role in the development of cardiovascular diseases by increasing
atherosclerosis and altering membrane integrity. Melatonin plays a role in the regulation of lipid
metabolism [Mohammadi-Sartang et al., 2018].
In a 2019 meta-analysis of 12 clinical trials including a total of 641 people with various conditions
(metabolic syndrome, obesity, menopause, chronic kidney disease, diabetes, NAFLD, etc.), melatonin
treatment (0.8 mg to 10 mg per day) for 4-56 weeks reduced LDL-cholesterol (SMD=-0.31 mmol/L, 95%
CI, -0.61 to 0.01; p=0.049) and triglyceride levels (SMD=-0.45 mmol/L; 95% CI, -0.77 to -0.13;
p=0.006)[Loloei et al., 2019]. In a subgroup analysis, melatonin treatment for more than 8 weeks
showed significant lowering of LDL-cholesterol (SMD=-0.48 mmol/L; 95% CI, -0.90 to -0.07; p=0.02), but
not in studies where melatonin treatment was less than 8 weeks. A significant effect of melatonin on

13
Last updated on September 26, 2023
LDL cholesterol was observed in a subset of trials administering melatonin at doses lower than 8 mg
(SMD-=-0.35 mmol/L; 95% CI, -0.70 to −0.01, p=0.05), but not in the subset of trials administering doses
higher than 8 mg (SMD=-0.25 mmol/L; 95% CI, -0.82 to 0.31, p=0.96). With regards to triglyceride levels,
melatonin treatment durations shorter than 8 weeks significantly decreased triglyceride levels (SMD=-
0.69 mmol/L; 95% CI, -1.08 to −0.29; p<0.001), but longer treatment had no significant effect (SMD=-
0.31 mmol/L; 95% CI, -0.75 to 0.12; p=0.16). A significant effect of melatonin on triglyceride levels was
observed at doses higher than 8 mg daily (SMD=-0.45; 95% CI, -0.89 to −0.01; p=0.049), but not when
doses lower than 8 mg were used (SMD=-0.46; 95% CI, -1.04 to 0.12; p=0.12). No effects of melatonin
treatment were seen on HDL cholesterol. Most of the included studies were of small size, and there was
a high heterogeneity likely due to the wide range of health conditions studied.
In a 2018 meta-analysis of 8 randomized controlled trials of people with various conditions (non-
alcoholic steatohepatitis, metabolic syndrome, schizophrenia, hypercholesterolemia), melatonin
treatment (0.3 to 10 mg daily) for 4-24 weeks significantly reduced triglyceride levels (WMD=-31.54
mg/dL; 95% CI, -50.71 to -12.38; p=0.001) and total cholesterol levels (WMD=-18.48 mg/dL; 95% CI, -
35.33 to -1.63; p=0.032)[Mohammadi-Sartang et al., 2018]. There were no significant effects of
melatonin treatment on LDL-cholesterol (WMD=-2.37 mg/dL; 95% CI, -11.61 to -6.86; p=0.615) or HDL-
cholesterol (WMD=1.28 mg/dL; 95% CI, -0.66 to 3.23; p=0.197). In subgroup analyses, melatonin
treatment significantly decreased triglyceride levels at doses ≥8 mg/day (WMD=−42.82 mg/dL; 95% CI,
−69.61 to −16.04; p=0.002) and when trials lasted ≥8 weeks (WMD=−32.25 mg/dL; 95% CI, -51.21 to
−13.28; p=0.001), but not with lower doses or shorter durations. In addition, a significant decrease of
total cholesterol was found with melatonin doses of ≥8 mg/day (WMD=−39.56 mg/dL; 95% CI, −54.13 to
−25.00; p<0.001) and when baseline total cholesterol levels were ≥200 mg/dL.
Cancer: MAY IMPROVE SURVIVAL AND CANCER THERAPY-RELATED SIDE EFFECTS
Melatonin has been investigated for cancer treatment and prevention. For example, the use of
melatonin as an addition to standard cancer treatments was reported in a meta-analysis to reduce the
risk of mortality by 40% (RR=0.60; 95% CI, 0.54 to 0.73) [Mills, 2005]. In a 2012 meta-analysis, melatonin
improved complete and partial remission and the one-year survival rate in patients with solid tumor
cancers, while concurrently alleviating radio/chemotherapy-related side effects [Wang et al., 2012].
In a 2022 meta-analysis of 19 randomized controlled trials including a total of 2,101 patients with
cancer, melatonin treatment (3-20 mg per night) did not significantly affect sleep quality, quality of life,
fatigue, pain, or severity of stomatitis (inflammation of oral mucosa)[Fan et al., 2022]. However,

14
Last updated on September 26, 2023
melatonin treatment significantly reduced stomatitis rate (RR=0.47; 95% CI, 0.26 to 0.88; p=0.02), except
in people with head and neck cancer (RR=1.09; 95% CI, 0.92 to 1.29; p=0.35). In studies where melatonin
treatment was administered for more than 14 days, melatonin treatment significantly eased depression
(standardized mean difference [SMD]=-0.14; 95% CI, -0.27 to -0.01; p=0.03). Further clinical trials are
needed to determine whether specific dosages or durations may offer benefit in specific types of cancer.
Type 2 diabetes and metabolic diseases: MAY IMPROVE METABOLIC INDICES
In a 2021 meta-analysis of 12 randomized controlled trials enrolling healthy adults and people with
metabolic diseases (diabetes, metabolic syndrome, NAFLD, osteopenia, polycystic ovary syndrome),
melatonin treatment (1-10 mg nightly) for 2-56 weeks significantly reduced fasting insulin levels, and
showed a trend towards reduced insulin resistance measured by HOMA-IR, but did not significantly alter
fasting glucose or hemoglobin A1c (HbA1c) levels compared with placebo [Lauritzen et al., 2021].
In another 2021 meta-analysis of 16 randomized controlled trials enrolling healthy people or those with
metabolic diseases (diabetes, metabolic syndrome, NAFLD, bipolar disorder, schizophrenia), melatonin
treatment (3-10 mg per day) for 4-24 weeks significantly reduced fasting blood glucose (mean
difference=-4.65; 95% CI, -8.06 to -1.23; p<0.01), but not HbA1c or insulin resistance [Delpino et al.,
2021].
In a 2019 meta-analysis of 12 clinical trials including a total of 641 people with various conditions
(metabolic syndrome, obesity, menopause, chronic kidney disease, diabetes, NAFLD, etc.), melatonin
treatment (0.8 mg to 10 mg per day) for 4-56 weeks did not significantly lower body weight, BMI, or
waist circumference [Loloei et al., 2019].
Paradoxically, melatonin may also increase blood sugar in certain situations, and therefore decrease the
effectiveness of medications to lower blood sugar in people with diabetes [WebMD]. Over 100 genetic
variants are associated with type 2 diabetes, including a common variant of the melatonin receptor 1B
gene (MTNR1B). In people with a specific variant (GG) of the MTNR1B gene, melatonin can inhibit insulin
secretion [Tuomi et al., 2016]. Thus, people with this GG variant can have lower insulin and higher
glucose levels in response to melatonin treatment.

15
Last updated on September 26, 2023
Liver disease: POTENTIAL BENEFIT
Nonalcoholic fatty liver disease (NAFLD) is characterized by fat accumulation in hepatocytes, which can
progress to steatohepatitis, fibrosis, cirrhosis, and liver cancer. In a pilot clinical study of patients with
nonalcoholic steatohepatitis, melatonin treatment (5 mg twice daily, orally) for 3 months significantly
improved liver function [Gonciarz et al., 2010]. In a double-blind randomized controlled trial in 45
patients with NAFLD, melatonin treatment (6 mg daily) for 3 months improved liver enzymes (ALT and
AST), the grade of fatty liver, systolic and diastolic blood pressure, and the inflammation biomarker hs-
CRP [Bahrami et al., 2020]. Longer and larger clinical trials are needed to validate these findings.
Oxidative stress: INCREASED ANTIOXIDANT CAPACITY, DECREASED OXIDATIVE STRESS
High oxidative stress is associated with cardiovascular disease, diabetes, metabolic syndrome, and other
age-related conditions. Melatonin can reduce oxidative stress by scavenging free radicals and activating
antioxidant enzymes [Jomova et al., 2023]. In a 2020 meta-analysis of 15 randomized controlled trials in
people with various conditions (cystic fibrosis, obesity, cardiovascular disease, cancer, diabetes, multiple
sclerosis, polycystic ovary syndrome, methadone maintenance, transplant patients) as well as in healthy
people, melatonin treatment (3-100 mg/day) for 14-180 days significantly increased total antioxidant
capacity level (standardized mean difference[SMD]=1.03; 95% CI, 0.24 to 1.81; p=0.011) and reduced
oxidative stress markers including protein carbonyl (SMD=-1.78; 95% CI, -2.97 to -0.58; p=0.004) and
malondialdehyde levels (SMD=-0.94; 95% CI, -1.48 to -0.40; p=0.001) [Ghorbaninejad et al., 2020]. The
effects on total antioxidant capacity was greatest when melatonin doses at or over 20 mg/day were
used and in people under 35 years old. A significant increase in total antioxidant capacity was observed
in studies where the treatment duration was at or over 60 days (SMD=1.31; 95% CI, 0.10 to 2.51;
p=0.033), but not in those with study durations under 60 days. Malondialdehyde levels were also
decreased with melatonin doses below 20 mg/day in people over 35 years old. Subgroup analyses found
that melatonin treatment significantly reduced malondialdehyde in women (SMD=−1.94; 95% CI, −3.68
to −0.19; p=0.029) but not in men. However, the Egger test showed significant evidence of publication
bias for meta-analyses assessing the effect of melatonin on protein carbonyl and malondialdehyde
levels. No effects of melatonin treatment were seen on nitric oxide (modulator of endothelial function)
or antioxidant enzymes: glutathione reductase, superoxide dismutase, or glutathione peroxidase.
However, in studies using melatonin doses at or above 20 mg/day, there was a significant decrease in
nitric oxide levels (SMD=−3.16; 95% CI, −4.26 to −2.07; p<0.001).

16
Last updated on September 26, 2023
In another 2020 meta-analysis of 12 randomized controlled trials in people with various conditions (neck
cancer, diabetes, diabetic hemodialysis, Parkinson’s disease, obesity, polycystic ovary syndrome,
methadone maintenance, orthognathic patients, epileptic children), melatonin treatment (3-250 mg) for
2-12 weeks significantly increased total antioxidant capacity (SMD=0.76; 95% CI, 0.30 to 1.21),
glutathione levels (SMD=0.57; 95% CI, 0.32 to 0.83), and activities of superoxide dismutase (SMD=1.38;
95% CI, 0.13 to 2.62), glutathione peroxidase (SMD=1.36; 95% CI, 0.46 to 2.30), and glutathione
reductase (SMD=1.21; 95% CI, 0.65 to 1.77), while significantly decreasing malondialdehyde levels
(SMD=-0.79; 95% CI, -1.19 to -0.39) [Morvaridzadeh et al., 2020]. Melatonin treatment duration of at
least 10 weeks increased total antioxidant capacity more efficiently than in studies where melatonin
treatment lasted less than 10 weeks. A subgroup analysis by disease type showed that melatonin
treatment reduced malondialdehyde levels in people with metabolic diseases more than in non-
metabolic diseases. Melatonin treatment did not significantly affect nitric oxide or catalase activity.
Melatonin exerts anti-oxidative effects through direct scavenging of reactive oxygen species and
reactive nitrogen species, stimulation of antioxidative enzymes (glutathione reductase, glutathione
peroxidase), and upregulating the endogenous antioxidant, glutathione [reviewed in Leelaviwat et al.,
2022].
Safety: Melatonin is considered safe for most healthy adults but a few contraindications are known and
long-term use has not been extensively studied. The use of melatonin is not recommended for elderly
patients with dementia due to increased risks of falls.
Types of evidence:
• 9 meta-analyses or systematic reviews of clinical trials testing melatonin treatment
• Numerous reviews, guidelines, and observational studies
• Several preclinical studies
General safety:
Evidence reviews by the AHRQ (Agency for Healthcare Research and Quality), the American Academy of
Sleep Medicine and numerous clinical trials suggests that melatonin supplementation is safe for most
healthy people for short-term use (up to 2 years) [McCleery, 2014; Xu, 2015; Schutte-Rodin,
2008]. Although many healthy people have used it for periods longer than 2 years, the risks or benefits

17
Last updated on September 26, 2023
from long-term use have not been well-studied. Melatonin derived from animal pineal glands should be
avoided as it may be contaminated with viruses [Altun, 2007].
Reports of serious adverse effects of melatonin supplementation are rare. Common adverse effects
include nausea, drowsiness, dizziness, hypotension, nightmares, abdominal pain, and decreased blood-
flow leading to lower body temperature (hypothermia) [Buscemi, 2006; Leelaviwat et al.,
2022]. Melatonin is best taken before bed, to align with the circadian rhythm. Melatonin may worsen
symptoms of “orthostatic hypotension”, a blood-pressure condition common in older adults [Ray, 2003].
Melatonin may also be unsafe in people with the following conditions: bleeding disorders, diabetes,
depression, autoimmune diseases, seizure disorders, and transplant recipients [WebMD].
People with dementia:
The American Academy of Sleep Medicine recommends against the use of melatonin and discrete sleep-
promoting medications for elderly patients with dementia due to increased risks of falls and other
adverse events [Auger et al., 2015]. In elderly patients with dementia, melatonin treatment has also
been shown to worsen caregiver ratings of patient mood [Riemersma-van der Lek et al., 2008].
A 2022 network meta-analysis of 50 randomized controlled trials in Alzheimer’s disease patients
(including a total of 19,704 patients) compared melatonin treatment against FDA-approved medications
for Alzheimer’s disease (donepezil, galantamine, rivastigmine, memantine, and Namzaric) and found
that melatonin treatment was associated with a similar drop-out rate and adverse events as compared
with placebo [Tseng et al., 2022].
In a 2020 Cochrane meta-analysis of 9 randomized controlled trials testing pharmacotherapies for sleep
disturbances in Alzheimer’s dementia, 5 trials tested melatonin treatment (2-10 mg per night) and there
was low-certainty evidence that melatonin and placebo groups did not differ in the number of adverse
events per person, in the severity of adverse events, or the likelihood of reporting any adverse event
[McCleery and Sharpley, 2020].
People with or at risk of delirium:
In a 2023 meta-analysis of clinical trials and observational studies examining delirium treatments,
melatonin treatment did not cause adverse events such as falls, nausea, rash, neurologic deterioration,

18
Last updated on September 26, 2023
or oversedation [Beaucage-Charron et al., 2023]. In one of the included studies, one participant
receiving melatonin had increased alanine aminotransferase (ALT) levels but recovered 15 days later.
Drug interactions:
Melatonin may reduce the effects of nifedipine and increase the effects of sedatives (clonazepam,
lorazepam, phenobarbital, zolpidem) and warfarin [Drugs.com, WebMD]. Caffeine and fluvoxamine may
increase the effects of melatonin. On the other hand, melatonin may alleviate the sleep disruption
caused by drugs like beta-blockers and benzodiazepines that alter melatonin production [Wright, 2015;
Stoschitzky, 1999; Scheer, 2012].
Sources and Dosing:
Melatonin is found in small concentrations in foods, such as meats, grains, fruits and vegetables. Since
melatonin regulates sleep cycles in humans it is most commonly marketed as a sleep aid dietary
supplement. It is available over-the-counter in the US as a liquid, tablet, pill, and transdermal patch. In
the EU, UK, Australia, and Canada, melatonin is available with prescription [Grigg-Damberger and
Ianakieva, 2017]. In the UK and Australia, melatonin is approved for the short-term treatment (<13
weeks) of primary insomnia in people over the age of 55 years old. In the UK, melatonin is also
prescribed for treatment of some sleep disorders in children with neurological disorders (2-10 mg
doses).
Melatonin was once derived from bovine pineal glands, which carried the risk of it being contaminated
with viruses [Altun, 2007]. Currently, melatonin supplements are made synthetically so they do not carry
the risk of being contaminated with infectious material. However, over-the-counter melatonin is not
regulated by the FDA, so several organizations offer independent testing of supplement quality to earn
“seals-of-approval.” Quality testing and important facts about supplements are offered by the NIH
Office of Dietary Supplements .
As a sleep-aid, melatonin is often taken orally in doses of 1-5 mg per day before bed. The most effective
dose will vary from person to person and should only be taken as advised by a physician.
Supraphysiological serum levels are expected with melatonin doses over 0.5 mg [Lee et al., 2022].
Length of treatment is also variable depending on the condition it is used to treat, but can range from a
few days (for jet lag) to 9 months (for trouble falling asleep) [WebMD].

19
Last updated on September 26, 2023
Bioavailability of melatonin can vary depending on whether it is ingested orally or sublingually. With oral
tablets, it is estimated that about 33% is absorbed through the gastrointestinal tract, though
bioavailability varies widely across people [Di et al., 1997]. Melatonin taken sublingually may have
higher bioavailability (50% or higher) and faster effects compared to oral tablets, though it is unlikely to
follow natural physiological trajectories of melatonin levels in the body. There have not been any studies
that directly compared the effectiveness of melatonin delivered orally versus sublingually.
Other formulations/drugs:
Circadin® and other prolonged-release forms of melatonin
Prolonged-release melatonin is designed to mimic the pharmacokinetics of endogenously produced
melatonin. Daily Circadin® (2 mg) consistently improved sleep quality, sleep latency (- 9 min), and next-
morning alertness in middle aged people with insomnia [Luthringer et al., 2009; Lemoine et al., 2012;
Hajak et al., 2015], middle-aged healthy people [Otmani et al., 2008], middle aged and elderly
insomniacs with hypertension [Lemoine et al., 2012], and in perimenopausal women with insomnia
[Dolev, 2011]. In mild to moderate AD patients taking AChE inhibitors and/or mementine, prolonged-
release melatonin (2 mg) improved cognitive performance (IADL and MMSE) in addition to sleep quality
[Wade et al., 2014]. Some of these clinical trials also showed improvement in quality of life with
Circadin® [Dolev, 2011; Lemoine et al., 2012]. Prolonged-release melatonin does not cause negative
effects on daytime psychomotor, driving, or memory performance [Otmani et al., 2008; Luthringer et al.,
2009] and is well-tolerated with no withdrawals or “rebound insomnia” upon discontinuation of the
drug [Lemoine et al., 2007, 2012; Luthringer et al., 2009; Wade et al., 2011, 2014]. Side effects with
Circadin® are not common but include irritability, nervousness, restlessness, and others. Circadin®
should not be taken if you have diabetes, depression, bleeding/clotting disorders, high/low blood
pressure, or epilepsy/seizure disorders. Drugs that may interact with melatonin include antibiotics,
aspirin/acetoaminophen, birth control pills, insulin (and other diabetes medicine), narcotics, antacids
(Prevacid, Prilosec, Zofran), ADHD medication, heart medicine (mexiletine, propranolol, verapamil),
anticoagulant/antiplatelet drugs (Plavix, warfarin), NSAIDs, and steroids (prednisone, etc.). Other safety
information can be found at drugs.com.
Piromelatine® (Neu-P11)
Piromelatine® is a melatonin receptor (MT1/2/3) and serotonin receptor (5HT-1A/D) agonist. Neurim
Pharmaceuticals Ltd has shown positive phase II RCT results for the treatment of primary and comorbid
insomnia [link]. Piromelatine® 20/50 mg treatment for 4 weeks resulted in significant and clinically
meaningful improvements in polysomnographic parameters (Wake After Sleep Onset; WASO), sleep

20
Last updated on September 26, 2023
efficiency, total sleep time, time in NREM sleep, as well as subjective sleep duration/quality.
Piromelatine® is generally safe and well-tolerated, with no negative effects on next-day psychomotor
performance. See full Piromelatine report for details and updates.
Ramelteon (Rozerem®)
Ramelteon, marketed as Rozerem® by Takeda Pharmaceuticals, is a synthetic drug that acts on
melatonin receptors (MT1/2) and is approved for insomnia related to difficulty of sleep onset. Meta-
analyses have shown that Ramelteon is associated with reduced sleep latency (-4.3 min), shorter latency
to persistent sleep (-9.36 min), improved sleep quality and efficiency, and longer total sleep time (+7.26
min) [Liu and Wang, 2012; Kuriyama et al., 2014]. However, no improvement in the percentage of REM
sleep has been observed. Subjective sleep latency is reduced with 4 and 8 mg doses, sleep quality is
increased with the 8 mg dose, and latency to persistent sleep is reduced in all doses studied (4, 8, 16, 32
mg). Side effects include diarrhea, dizziness, drowsiness, fatigue, and tiredness. The occurrence of
somnolence, but not other adverse events reported, was significantly higher in people taking Ramelteon
than placebo [Kuriyama et al., 2014]. Next-day residual effects were not significantly different between
Ramelteon and placebo groups [Liu and Wang, 2012]. Ramelteon should not be taken if you have severe
liver problems, sleep apnea, COPD, or mental or mood problems. Ramelteon interacts with azole
antifungals, donepezil, doxeparin, and fluvoxamine. Other safety information can be found here.
Ramelteon has also been shown to reduce the incidence of delirium. See full Ramelteon report for
details and updates.
Research underway:
There are over 100 clinical studies testing melatonin, based on ClinicalTrials.gov. Aside from studies of
sleep, melatonin is studied in various conditions, including acute/ischemic stroke, concussion, brain
injury, coronary artery bypass grafting surgery, hypertension, cardiovascular diseases, osteoarthritis,
postoperative delirium, autism spectrum disorder, schizophrenia, epilepsy, kidney injury prevention, and
others. One randomized controlled study is testing melatonin (5 mg) on cognition and brain health in
people with mild cognitive impairment (NCT03954899).

21
Last updated on September 26, 2023
Search terms:
PubMed, Google, Cinicaltrials.gov:
• Melatonin, Ramelteon, Rozerem, Piromelatine, MEL, MLT, Pineal, hormone, Circadin, prolonged-
release melatonin, PRM, amyloid, blood pressure, cancer, hypertension, dementia, Alzheimer’s,
aging, mortality, cognitive function, telomere, gait, lifespan, ApoE4, sleep deprivation, delirium, and
USP certified supplements.
Disclaimer: Cognitive Vitality Reports® do not provide, and should not be used for, medical
advice, diagnosis, or treatment. You should consult with your healthcare providers when
making decisions regarding your health. Your use of these reports constitutes your agreement
to the Terms & Conditions.
If you have suggestions for drugs, drugs-in-development, supplements, nutraceuticals, or
food/drink with neuroprotective properties that warrant in-depth reviews by ADDF’s Aging and
Alzheimer’s Prevention Program, please contact INFO@alzdiscovery.org. To view our official
ratings, visit Cognitive Vitality’s Rating page.
