New Zealand Data sheet
Page 1 of 14
1 CIRCADIN
®
Melatonin 2 mg Prolonged Release Tablets
2 QUALITATIVE AND QUANTITATIVE COMPOSITION
The active ingredient in CIRCADIN prolonged release tablets is a melatonin NOT of
plant or animal origin.
Excipient with known effect: lactose monohydrate.
For the full list of excipients, see section 6.1 List of excipients.
3 PHARMACEUTICAL FORM
CIRCADIN 2 mg prolonged release tablets: White to off-white, round, biconvex tablets.
4 CLINICAL PARTICULARS
4.1 Therapeutic indications
Monotherapy for the short term treatment of primary insomnia characterized by poor
quality of sleep in patients who are aged 55 or over.
4.2 Dose and method of administration
Oral use. Tablets should be swallowed whole.
The recommended dose is 2 mg once daily, 1 - 2 hours before bedtime and after food.
This dosage may be continued for up to thirteen weeks.
Paediatric Use
CIRCADIN is not recommended for use in children and adolescents below 18 years
of age due to insufficient data on safety and efficacy.
Renal Insufficiency
The effect of any stage of renal insufficiency on melatonin pharmacokinetics has not
been studied. Caution should be used when melatonin is administered to such
patients.
Hepatic Impairment
There is no experience of the use of CIRCADIN in patients with liver impairment.
Published data demonstrates markedly elevated endogenous melatonin levels during
daytime hours due to decreased clearance in patients with hepatic impairment.
Therefore, CIRCADIN is not recommended for use in patients with hepatic impairment.
New Zealand Data sheet
Page 2 of 14
4.3 Contraindications
CIRCADIN prolonged release tablets are contraindicated in patients with a known
hypersensitivity to any ingredient of the product (see section 2 QUALITATIVE AND
QUANTITATIVE COMPOSITION and section 6.1 List of excipients).
4.4 Special warnings and precautions for use
Drowsiness
CIRCADIN may cause drowsiness. Therefore the product should be used with caution
if the effects of drowsiness are likely to be associated with a risk to safety.
Autoimmune Diseases
No clinical data exist concerning the use of CIRCADIN in individuals with autoimmune
diseases. Therefore CIRCADIN is not recommended for use in patients with
autoimmune diseases.
Excipients
The tablets contain lactose. Patients with rare hereditary problems of galactose
intolerance, the LAPP lactase deficiency or glucose-galactose malabsorption should
not take this medicine.
Paediatric Use
CIRCADIN is not recommended for use in children and adolescents below 18 years
of age due to insufficient data on safety and efficacy.
Use in the Elderly
Melatonin metabolism is known to decline with age. Across a range of doses, higher
AUC and C
max
levels have been reported in older subjects compared to younger
subjects, reflecting the lower metabolism of melatonin in the elderly.
4.5 Interaction with other medicines and other forms of interaction
Pharmacokinetic Interactions
Hepatic Enzymes
Melatonin has been observed to induce CYP3A in vitro at supra-therapeutic
concentrations. The clinical relevance of the finding is unknown. If induction occurs,
plasma concentrations of concomitantly administered medicines can be reduced.
Melatonin does not appear to induce CYP1A enzymes in vitro at supra-therapeutic
concentrations. Therefore, interactions between melatonin and other active
substances as a consequence of melatonin’s effect on CYP1A enzymes are not likely
to be significant.
Melatonin’s metabolism is mainly mediated by CYP1A enzymes. Therefore,
interactions between melatonin and other active substances as a consequence of their
effect on CYP1A enzymes is possible:
New Zealand Data sheet
Page 3 of 14
Quinolones
CYP1A2 inhibitors such as quinolones may give rise to increased melatonin exposure.
Carbamazepine and Rifampicin
CYP1A2 inducers such as carbamazepine and rifampicin may give rise to reduced
plasma concentrations of melatonin.
Fluvoxamine
Caution should be exercised in patients on fluvoxamine, which increases melatonin
levels (17-fold higher AUC and 12-fold higher serum C
max
) by inhibiting its metabolism
by hepatic cytochrome P450 (CYP) isozymes CYP1A2 and CYP2C19. The
combination should be avoided.
5- or 8-methoxypsoralen
Caution should be exercised in patients on 5- or 8-methoxypsoralen (5 and 8-MOP),
which increases melatonin levels by inhibiting its metabolism.
Cimetidine
Coadministration of CIRCADIN with cimetidine resulted in a 1.7 fold increase in
exposure to melatonin with no change in the exposure to cimetidine.
Caution should be exercised in patients on cimetidine, a CYP2D inhibitor which
increases plasma melatonin levels by inhibiting its metabolism.
Cigarette Smoking
Cigarette smoking may decrease melatonin levels due to induction of CYP1A2.
Oestrogens
Caution should be exercised in patients on oestrogens (e.g. contraceptives or
hormone replacement therapy), which increase melatonin levels by inhibiting its
metabolism by CYP1A1 and CYP1A2.
Other
There is a large amount of data in the literature regarding the effect of adrenergic
agonists/antagonists, opiate agonists/antagonists, antidepressant medicinal products,
prostaglandin inhibitors, benzodiazepines, tryptophan and alcohol, on endogenous
melatonin secretion. Whether or not these active substances interfere with the
dynamic or kinetic effects of CIRCADIN or vice versa has not been studied.
Pharmacodynamic Interactions
Alcohol
Alcohol should not be taken with CIRCADIN, because it reduces the effectiveness of
CIRCADIN on sleep. The prolonged release characteristics of CIRCADIN may be
altered by alcohol, resulting in immediate release of melatonin.
New Zealand Data sheet
Page 4 of 14
Hypnotics
CIRCADIN may enhance the sedative properties of benzodiazepines and
non-benzodiazepine hypnotics, such as zalepon, zolpidem and zopiclone. In a clinical
trial, there was clear evidence for a transitory pharmacodynamic interaction between
CIRCADIN and zolpidem one hour following co-dosing. Concomitant administration
resulted in increased impairment of attention, memory and co-ordination compared to
zolpidem alone.
Thioridazine and Imipramine
CIRCADIN has been co-administered in studies with thioridazine and imipramine,
active substances which affect the central nervous system. No clinically significant
pharmacokinetic interactions were found in each case. However, CIRCADIN
co-administration resulted in increased feelings of tranquility and difficulty in
performing tasks compared to imipramine alone, and increased feelings of “muzzy-
headedness” compared to thioridazine alone.
Effects on Laboratory Tests
No information is available on the effect of melatonin on laboratory tests.
4.6 Fertility, pregnancy and lactation
Effects on Fertility
No significant effects on fertility or reproductive performance were observed in rats
given oral melatonin prior to mating through to early gestation at doses over 900-fold
the recommended clinical dose, based on body surface area.
Use in Pregnancy
Category B3.
No significant effects on embryofoetal development were observed in rats given oral
melatonin during the period of organogenesis at doses over 900 - fold the
recommended clinical dose, based on body surface area.
No clinical data on exposed pregnancies are available. In view of the lack of clinical
data, use in pregnant women and by women intended to become pregnant is not
recommended.
Use in Lactation
Maternal transfer of exogenous melatonin to the fetus via the placenta or milk has
been demonstrated in several animal species including rats, hamsters, goats,
monkeys and cows. A slight reduction in post-natal growth, viability and development
was found in rats given oral melatonin during gestation through weaning at doses over
900 - fold the recommended clinical dose, based on body surface area; the no-effect
dose was over 250 - fold the clinical dose.
Endogenous melatonin has been detected in human breast milk, thus exogenous
melatonin is likely excreted into human milk. The effects of melatonin on the nursing

New Zealand Data sheet
Page 5 of 14
infant have not been established. Therefore, breast-feeding is not recommended in
women under treatment with melatonin.
4.7 Effects on ability to drive and use machines
CIRCADIN has negligible influence on the ability to drive and use machines.
Nevertheless, patients should avoid engaging in hazardous activities (such as driving
or operating machinery) after taking CIRCADIN.
4.8 Undesirable effects
In clinical trials (in which a total of 1931 patients were taking CIRCADIN and 1642
patients were taking placebo), 48.8% of patients receiving CIRCADIN reported an
adverse reaction compared with 37.8% taking placebo. Comparing the rate of patients
with adverse reactions per 100 patient weeks, the rate was higher for placebo than
CIRCADIN (5.743 – placebo vs. 3.013 CIRCADIN). The most common adverse
reactions were headache, nasopharyngitis, back pain, and arthralgia, which were
common, by MedDRA definition, in both the CIRCADIN and placebo treated groups.
In the CIRCADIN group, there were 72 cases (2.9% of the safety population) of
adverse events leading to discontinuation of the patient. In the placebo group there
were 62 cases (4.0% of the safety population) of adverse events leading to
discontinuation of the patient.
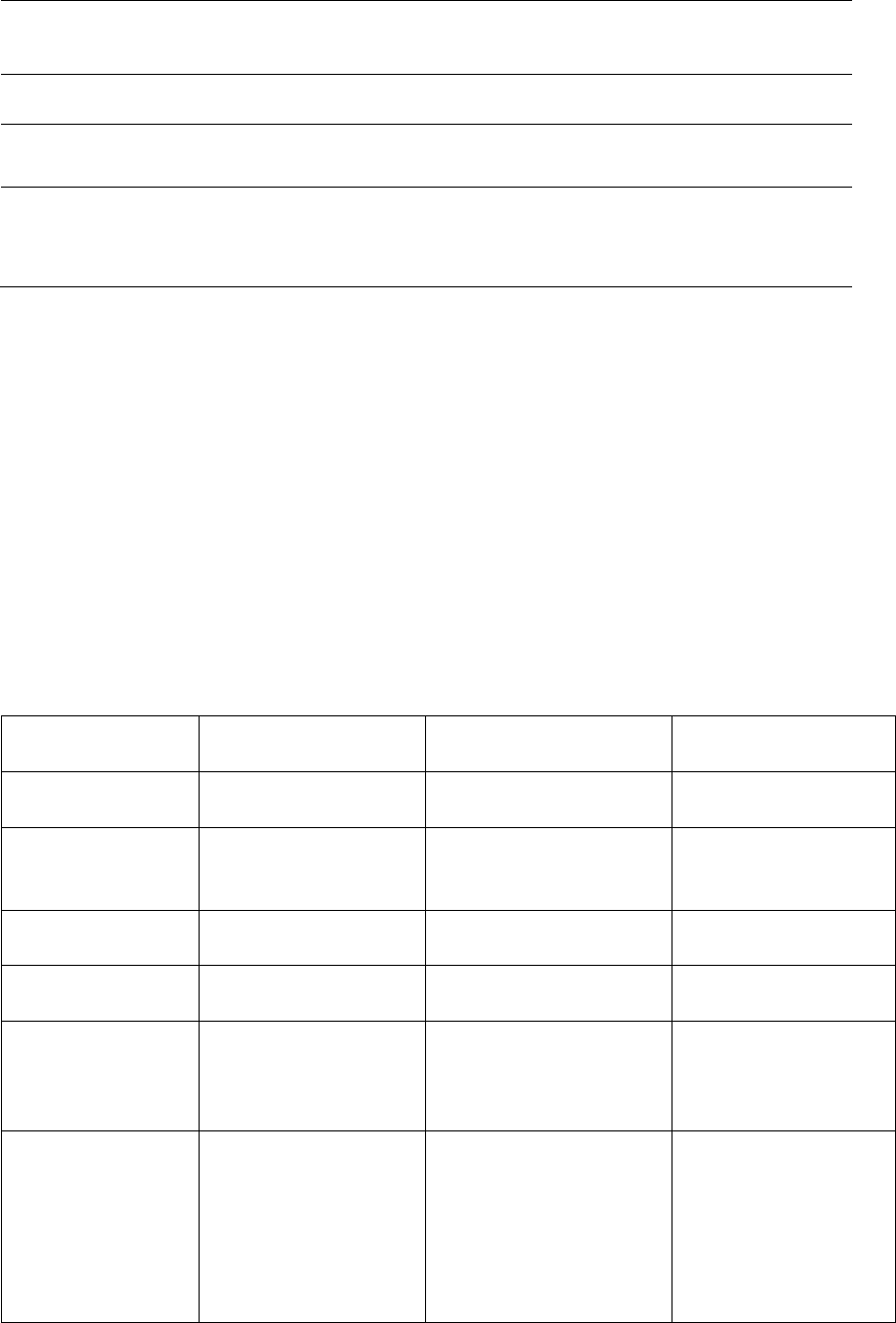
Overall Adverse Experience for adverse events occurring with a frequency ≥ 1%
Body System/Adverse Experience
Circadin %
(N=1931)
Placebo %
(N=1642)
Gastrointestinal disorders
Abdominal Pain
1.1
0.7
Abdominal Pain Upper
1.0
1.2
Constipation
1.2
0.9
Diarrhoea
3.1
1.8
Nausea
1.8
1.7
Vomiting
1.5
0.9
General Disorders and administration site conditions
Asthenia
1.9
1.2
Infections and infestations
Influenza
1.5
0.9
Lower respiratory tract infection
1.9
1.2
Nasopharyngitis
Pharyngitis
Upper respiratory tract infection
Urinary tract infection
4.0
1.9
2.9
2.1
3.0
1.2
1.2
0.7
Musculoskeletal and connective tissue disorder
Arthralgia
Back Pain
Muscle cramp
Neck pain
Pain in extremity
3.5
3.8
1.1
1.1
1.6
1.8
1.5
0.6
0.6
1.1
Nervous system disorders
Dizziness
1.6
1.2
New Zealand Data sheet
Page 6 of 14
Body System/Adverse Experience
Circadin %
(N=1931)
Placebo %
(N=1642)
Headache
5.7
6.2
Migraine
1.1
1.2
Psychiatric disorders
Anxiety
1.0
1.2
Respiratory, thoracic and mediastinal disorders
Cough
2.2
1.3
Pharyngolaryngeal pain
1.5
0.9
Rhinitis
1.1
0.9
The adverse reactions in the table below were reported in clinical trials and were
defined as possibly, probably or definitely related to treatment. A total of 9.5% of
subjects receiving CIRCADIN reported an adverse reaction compared with 7.4% of
subjects taking placebo. Only those adverse events occurring in subjects at an
equivalent or greater rate than placebo have been included.
Within each frequency grouping, undesirable effects are presented in order of
decreasing seriousness.
Very common (≥ 1/10); Common (≥ 1/100 to <1/10); Uncommon (≥ 1/1,000 to <1/100);
Rare (≥ 1/10,000 to <1/1,000); Very rare (<1/10,000), Not known (cannot be
established from the available data).
Adverse events related to treatment occurring with a frequency < 1%
System Organ
Class
Uncommon
Rare
Not known
Infections and
Infestations
Herpes zoster
Blood and
Lymphatic
System Disorders
Leukopenia,
Thrombocytopenia
Cardiac Disorders
Angina pectoris
Palpitations
Immune System
Disorders
Hypersensitivity
reaction
Metabolism and
Nutrition
Disorders
Hypertriglyceridaemia
Hypocalcaemia
Hyponatraemia
Psychiatric
Disorders
Irritability,
Nervousness,
Restlessness,
Insomnia, Abnormal
dreams, Anxiety,
Nightmares
Mood altered,
Aggression, Agitation,
Crying, Stress
symptoms,
Disorientation, Early
morning awakening,
Libido increased,

New Zealand Data sheet
Page 7 of 14
System Organ
Class
Uncommon
Rare
Not known
Depressed mood,
Depression
Nervous System
Disorders
Migraine Lethargy
Psychomotor
hyperactivity,
Dizziness,
Somnolence,
Headache
Syncope, Memory
impairment,
Disturbance in
attention, Dreamy
state, Restless legs
syndrome, Poor quality
sleep, Paresthesia
Eye Disorders
Visual acuity reduced,
Vision blurred,
Lacrimation increased
Ear and Labyrinth
Disorders
Vertigo positional,
Vertigo
Vascular
Disorders
Hypertension
Hot flush
Gastrointestinal
Disorders
Abdominal pain,
Abdominal pain
upper, Dyspepsia,
Mouth ulceration,
Dry mouth, Nausea
Gastro-oesophageal
reflux disease,
Gastrointestinal
disorder, oral Mucosal
blistering, Tongue
ulceration,
Gastrointestinal upset,
Vomiting, Bowel
sounds abnormal,
Flatulence, Salivary
hypersecretion,
Halitosis, Abdominal
discomfort, Gastric
disorder, Gastritis
Hepatobiliary
Disorders
Hyperbilirubinaemia
Skin and
Subcutaneous
Tissue Disorders
Dermatitis, Night
sweats, Pruritus,
Rash, Pruritus
generalised, Dry
skin
Eczema, Erythema,
Hand dermatitis,
Psoriasis, Rash
generalised, Rash
pruritic, Nail disorder
Angioedema,
Oedema of mouth,
Tongue oedema
Musculoskeletal
and Connective
Tissue Disorders
Pain in extremity
Arthritis, Muscle
spasm, Neck pain,
Night cramps
Reproductive
System and
Breast Disorders
Menopausal
symptoms
Priapism, Prostatitis
Galactorrhoea
General
Disorders and
Administration
Site Conditions
Asthenia, Chest pain
Fatigue, Pain, Thirst

New Zealand Data sheet
Page 8 of 14
System Organ
Class
Uncommon
Rare
Not known
Renal and
Urinary Disorders
Glycosuria,
Proteinuria
Polyuria, Haematuria,
Nocturia
Investigations
Liver function test
abnormal, Weight
increased
Hepatic enzyme
increased, Blood
electrolytes abnormal,
Laboratory test
abnormal
Post-Marketing Data
Psychiatric Disorders: Nightmares
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicine is
important. It allows continued monitoring of the benefit/risk balance of the medicine.
Healthcare professionals are asked to report any suspected adverse reactions
https://nzphvc.otago.ac.nz/reporting/
4.9 Overdose
In general, the main therapy for all overdoses is supportive and symptomatic care.
Symptoms
No case of overdose has been reported. CIRCADIN has been administered at 5 mg
daily doses in clinical trials over 12 months without significantly changing the nature
of the adverse reactions reported.
Administration of daily doses of up to 300 mg of melatonin without causing clinically
significant adverse reactions have been reported in the literature.
If overdose occurs, drowsiness is to be expected.
Treatment
Clearance of the active substance is expected within 12 hours after ingestion. No
special treatment is required.
For advice on the management of overdose please contact the National Poisons
Centre on 0800 POISON (0800 764766).
5 PHARMACOLOGICAL PROPERTIES
Pharmacotherapeutic group: Melatonin Receptor Agonists, ATC code: N05CH01
Melatonin
Chemical name: N-[2-(5-Methoxyindol-3-yl)ethyl]acetamide. Melatonin is a slightly
off-white, odourless crystalline powder.

New Zealand Data sheet
Page 9 of 14
Structural formula:
Molecular formula: C
13
H
16
N
2
O
2
Molecular weight: 232.27
CAS number: 73-31-4
pKa: 12.3 – 12.7
Melatonin is very slightly soluble in water and in dilute hydrochloric acid.
5.1 Pharmacodynamic properties
Pharmacological Actions
Melatonin is a naturally occurring hormone produced by the pineal gland and is
structurally related to serotonin. Physiologically, melatonin secretion increases soon
after the onset of darkness, peaks at 2 - 4 am and diminishes during the second half
of the night. Melatonin is associated with the control of circadian rhythms and
entrainment to the light-dark cycle. It is also associated with a hypnotic effect and
increased propensity for sleep.
Mechanism of Action
The activity of melatonin at the MT1 MT2 receptors is believed to contribute to its
sleep-promoting properties via their distinct actions on the circadian clock. The MT1
receptors are thought to inhibit neuronal firing, while the MT2 receptors have been
implicated in the phase-shifting response.
Rationale for Use
Because of the role of melatonin in sleep and circadian rhythm regulation, and the age
related decrease in endogenous melatonin production, melatonin may effectively
improve sleep quality particularly in patients who are over 55 with primary insomnia.
Clinical Trials
Three Phase 3 studies and a sleep laboratory study were considered pivotal. These
studies enrolled patients with primary insomnia who were aged at least 55 years.
Patients suffering from severe neurological, psychiatric or neurosurgical diseases or
New Zealand Data sheet
Page 10 of 14
taking CNS medications including benzodiazepines or other hypnotic agents were
excluded.
The primary assessment tool was the Leeds Sleep Evaluation Questionnaire (LSEQ),
comprising 10 self-rated 100 mm-line analogue questions concerning aspects of sleep
and early morning behaviour. The LSEQ measures ease of getting to sleep (GTS),
quality of sleep (QOS), ease of waking from sleep (AFS) and behaviour following
wakefulness (BFW). The primary outcome variable in the pivotal clinical trials was
QOS, or a combination on QOS and BFW, where a patient had to show a clinically
relevant improvement on both QOS and BFW. Time to onset of sleep and duration of
sleep were measured objectively only in a polysomnography study. Efficacy of
CIRCADIN in combination with other hypnotic agents has not been assessed.
In a polysomnographic (PSG) study (N = 40; 20 CIRCADIN, 20 placebo) with a run-in
of 2 weeks (single-blind with placebo treatment), followed by a treatment period of 3
weeks (double-blind, placebo-controlled, parallel group design) and a 3-week
withdrawal period, time to onset of sleep was shortened significantly by 9 minutes
compared to placebo. A statistically significant difference favouring CIRCADIN was
seen for total duration of time awake prior to sleep onset (approx change from 10 to
11 minutes for CIRCADIN and from 21 to 20 minutes for placebo). There were no
modifications of sleep architecture and no effect on REM sleep duration by CIRCADIN.
Modifications in diurnal functioning did not occur with CIRCADIN 2 mg. CIRCADIN did
not prolong the duration of sleep significantly compared to placebo.
In the outpatient studies patients who failed to meet the inclusion criteria at the end of
the run-in period due to the instability of their disorder (16% of the total population)
were not included in the efficacy analysis.
In an outpatient study (Neurim VII: N = 170; 82 CIRCADIN, 88 placebo) with two week
run in baseline period with placebo, a randomised, double blind, placebo controlled,
parallel group treatment period of 3 weeks and two week withdrawal period with
placebo, the primary efficacy endpoint was Quality of Sleep (QOS). The rate of
patients who showed a clinically significant improvement in both quality of sleep and
morning alertness was 47% in the CIRCADIN group as compared to 27% in the
placebo group. There was a mean difference of approximately 6 mm in quality of sleep
and approximately 9 mm in morning alertness, both favouring CIRCADIN compared
to placebo. Sleep variables gradually returned to baseline with no rebound, no
increase in adverse events and no increase in withdrawal symptoms.
In a second outpatient study (N = 334; 169 CIRCADIN, 165 placebo) with two week
run in baseline period with placebo and a randomised, double blind, placebo
controlled, parallel group treatment period of 3 weeks, the rate of patients who showed
a clinically significant improvement in both quality of sleep and morning alertness was
26% in the CIRCADIN group as compared to 15% in the placebo group. CIRCADIN
shortened patients’ reported time to onset of sleep by 24.3 minutes vs 12.9 minutes
with placebo. In addition, patients’ self-reported quality of sleep, number of
awakenings and morning alertness significantly improved with CIRCADIN compared
to placebo. Quality of life was improved significantly with CIRCADIN 2 mg compared
to placebo.
New Zealand Data sheet
Page 11 of 14
A third study involved more than 600 patients over 55, over 400 of whom were on
CIRCADIN treatment for up to 6 months. Patients given CIRCADIN demonstrated a
difference from placebo in mean change from baseline in subjective sleep latency,
assessed using a sleep diary, of -7.8 minutes after 3 weeks (p = 0.014). Small
differences in sleep latency were generally maintained over 13 weeks of placebo-
controlled treatment.
The percentage of patients showing both remission of insomnia (PSQI of < 6) and a
clinically relevant improvement of 10% in quality of life scores (WHO-5 index)
increased from 16.7% (cf. 10.6% placebo, p = 0.044) at week 3 to 25.8% at week 13
(cf. 15.7% placebo, p = 0.0006).
This study also examined the effect of CIRCADIN on sleep latency in younger subjects
with primary insomnia and low excretion of melatonin. Clinically significant effects on
sleep latency were not demonstrated in these patients.
Long Term Safety
The safety profile both during 3 weeks and during the 26 week periods was
comparable to placebo with no withdrawal and rebound effects.
In an open study where 96 subjects completed 12 months treatment with CIRCADIN
no tolerance, rebound or withdrawal effects were reported.
5.2 Pharmacokinetic properties
The absolute bioavailability of melatonin from CIRCADIN has not been assessed.
Other oral formulations of melatonin have an absolute bioavailability in the region of
15% but this is highly variable with high first-pass metabolism. The relative
bioavailability of melatonin from CIRCADIN is comparable to that of an oral melatonin
solution.
Absorption
Data from other formulations of melatonin indicate that the absorption of orally
ingested melatonin is complete in adults and may be decreased by up to 50% in the
elderly. The kinetics of melatonin is linear over the range of 2 – 8 mg as obtained from
published results using a formulation other than CIRCADIN.
Bioavailability as assessed from other oral formulations of melatonin is in the order of
15%. There is a significant first pass effect with an estimated first pass metabolism of
85% as assess from other oral formulations of melatonin. T
max
occurs after 2.6 hours
in a fed state. The rate of melatonin absorption following CIRCADIN 2 mg oral
administration is affected by food. The presence of food delayed the absorption of the
melatonin resulting in a later T
max
(T
max
= 2.6 h versus T
max
= 1.6 h). C
max
and AUC
levels were not affected by food.
Distribution
The in vitro plasma protein binding of melatonin is approximately 60%. Melatonin is
mainly bound to albumin, alpha
1
-acid glycoprotein and high density lipoprotein. The
binding to the other serum proteins is insignificant. The melatonin binding was
New Zealand Data sheet
Page 12 of 14
constant over the range of the studied concentrations in serum. Literature data
indicates that melatonin is distributed in all body fluids and is accessible at all tissues.
Biotransformation
Experimental data suggest that isoenzymes CYP1A1, CYP1A2 and possibly
CYP2C19 of the cytochrome P450 system are involved in melatonin metabolism. The
principal metabolite is 6-sulphatoxy-melatonin (6-S-MT), which is inactive. The site of
biotransformation is the liver. The excretion of the metabolite is completed within 12
hours after ingestion.
Elimination
Terminal half life (t
½
) is 3.5 - 4 hours. Elimination is by renal excretion of metabolites,
89% as sulphated and glucoronide conjugates of 6-hydroxymeltonin and 2% is
excreted as melatonin (unchanged medicine).
Gender
A 3 - 4-fold increase in C
max
is apparent for women compared to men. A five-fold
variability in C
max
between different members of the same sex has also been observed.
However, no pharmacodynamic differences between males and females were found
despite differences in blood levels.
Elderly
Melatonin metabolism is known to decline with age. Across a range of doses, higher
AUC and Cmax levels have been reported in older subjects compared to younger
subjects, reflecting the lower metabolism of melatonin in the elderly. C
max
levels
around 500 pg/mL in adults (18 - 45) versus 1200 pg/mL in the elderly (55 - 65); AUC
levels around 3,000 pg*h/mL in adults versus 6000 pg*h/mL in the elderly.
Renal Impairment
Melatonin did not accumulate after repeated dosing with CIRCADIN. This finding is
compatible with the short half-life of melatonin in humans.
The levels assessed in the blood of patients at 23:00 (2 hours after administration)
following 1 and 3 weeks of daily administration were 411.4 ± 56.5 and 432.00 ± 83.2
pg/mL respectively, and are similar to those found in healthy volunteers following a
single dose of CIRCADIN 2 mg.
Hepatic Impairment
The liver is the primary site of melatonin metabolism and therefore, hepatic impairment
results in higher endogenous melatonin levels.
Plasma melatonin levels in patients
with cirrhosis were significantly increased during
daylight
hours. Patients had a significantly
decreased total
excretion of 6-
sulfatoxymelatonin compared with controls.

New Zealand Data sheet
Page 13 of 14
5.3 Preclinical safety data
Carcinogenicity
An oral lifetime carcinogenicity study with melatonin in rats showed an increased
incidence of thyroid follicular cell adenomas in males at doses around 700 - fold the
recommended clinical dose, based on body surface area. No neoplastic tissue
histopathology was examined at lower doses and therefore the no-effect dose could
not be determined. These effects were associated with liver enzyme induction in this
species and are unlikely to be relevant to humans.
Genotoxicity
Results from a standard battery of in vitro and in vivo assays showed no evidence of
a genotoxic potential for melatonin.
6 PHARMACEUTICAL PARTICULARS
6.1 List of excipients
CIRCADIN prolonged release tablets contain the excipients: Ammonio methacrylate
copolymer, calcium hydrogen phosphate dihydrate, lactose monohydrate, colloidal
silicon dioxide, purified talc and magnesium stearate.
6.2 Incompatibilities
Not applicable
6.3 Shelf life
36 months
6.4 Special precautions for storage
Store below 25ºC. Protect from light.
6.5 Nature and contents of container
Blister pack, PVC/PVdC/Al
Circadin is available in pack sizes of 7, 21, 30, 42, 60 and 90 tablets.
6.6 Special precautions for disposal
No special requirements for disposal.
7 MEDICINE SCHEDULE
Prescription Medicine

New Zealand Data sheet
Page 14 of 14
8 SPONSOR
Pharmacy Retailing t/a Healthcare Logistics
58 Richard Pearse Drive
Airport Oaks
Mangere
Auckland
New Zealand
9 DATE OF FIRST APPROVAL
16 June 2011
10 DATE OF REVISION OF THE TEXT
12 March 2021
CIRCADIN is a registered trademark of Neurim Pharmaceuticals
SUMMARY TABLE OF CHANGES
Section changed
Summary of new information
3
Pack sizes moved to section 6.5
6.5
Pack size information added with
additional proposed pack sizes.
