
Medical Assistance Division
Managed Care Policy Manual
THIS PAGE INTENTIONALLY LEFT BLANK
Contents
1. General Provisions...................................................................................................... 1
1.1. General Information .................................................................................................... 1
2. Provider Network ........................................................................................................ 2
2.1. Service Termination and Provider Closure .................................................................. 2
2.2. MCO-Initiated Provider Network Closures and Reductions ......................................... 3
2.3. Provider Monitoring ..................................................................................................... 4
2.4. Requirements for Provider Enrollment ........................................................................ 4
2.5. Institutional Type Providers ......................................................................................... 8
2.6. Providers Whose Services are Based on Orders and Referrals ................................ 10
2.7. Rendering Providers ................................................................................................. 11
2.8. Using the Web to Verify Attending, Ordering, Referring, Rendering or Prescribing
Providers .................................................................................................................. 14
2.9. Exclusions ................................................................................................................ 17
2.10. General Information on the Requirements based on Procedure Codes .................... 18
2.11. Appendices ............................................................................................................... 23
2.11.1. Notification of Change in Services – Notification of Transition ...................................24
2.11.2. Transition Plans Narrative .........................................................................................25
2.11.3. Transition Plan A ......................................................................................................27
2.11.4. Transition Plan B ......................................................................................................29
2.11.5. Definitions .................................................................................................................31
3. Member Education .................................................................................................... 32
3.1. Policies and Procedures ........................................................................................... 32
3.2. Member Handbook ................................................................................................... 33
3.3. Provider Directories .................................................................................................. 35
3.4. Member Identification Card ....................................................................................... 35
3.5. Member Advisory Board ........................................................................................... 35
4. Care Coordination ..................................................................................................... 37
4.1. General Information .................................................................................................. 37
4.2. Care Coordination Functions .................................................................................... 37
4.3. Health Risk Assessment ........................................................................................... 40
4.4. Comprehensive Needs Assessment ......................................................................... 42
4.5. Community Benefit Service Questionnaire ................................................................ 47
4.6. CNA Reassessments ................................................................................................ 48
4.7. Comprehensive Care Plan Requirements ................................................................. 49
4.8. Staffing Requirements and Delegations .................................................................... 54
4.9. Engagement of Members .......................................................................................... 57
4.10. MCO Care Coordination with 1915(c) HCBS Waivers: Developmental Disabilities
(DD), Mia Via, and Medically Fragile (MF) Waivers ................................................... 58
4.11. Overview of Medicaid 1915(c) HCBS Waiver Programs ............................................ 59
4.12. MCO Care Coordination Activities and the 1915(c) HCBS Waivers Service Plan (ISP
or SSP) ..................................................................................................................... 61
4.13. MCO Care Coordination Activities for MF EPSDT (Non-Waiver) Members Case
Managed by the MFW Case Management Agency ................................................... 63
4.14. Transitions from the HSD Non-Medicaid Brain Injury Services Fund to a Centennial
Care MCO ................................................................................................................ 64
4.15. Appendix ................................................................................................................... 66
4.15.1. Health Risk Assessment ........................................................................................... 66
5. Transitions of Care.................................................................................................... 68
5.1. General Information .................................................................................................. 68
5.2. Transitions of Care.................................................................................................... 69
5.3. Transitions of Care Requirements ............................................................................. 70
5.4. Transition of Care Requirements for Pregnant Women ............................................. 71
5.5. Transfer from the Health Insurance Exchange .......................................................... 72
5.6. Transitions of Care for Members Moving from a Higher LOC to a Lower LOC .......... 72
5.7. Transitions of Members Turning 21 Years of Age ..................................................... 73
5.8. Transition for Members changing MCOs while Hospitalized ...................................... 74
5.9. Transition for Members Changing MCOs during Major Organ and Tissue
Transplantation Services .......................................................................................... 75
5.10. Transition for Members Changing MCOs while receiving Outpatient Treatment for
Significant Medical Conditions .................................................................................. 75
5.11. MCO Requirements for Members Transitioning between MCOs ............................... 76
5.12 Transitions of Care for Justice Involved Members ..................................................... 77
5.13 Transitions of Care for Substance Exposed infants ................................................... 78
6. Nursing Facilities (NFs) ............................................................................................. 80
6.1. General Information .................................................................................................. 80
6.2. NF Procedures for Requests for Prior Approval ........................................................ 80
6.3. Pre-Admission Screening and Resident Review (PASRR) ........................................ 80
6.4. Level of Care Packet for Nursing Facilities ................................................................ 83
6.5. Denial of Requests for NF LOC Determinations ........................................................ 85
6.6. Reserve Bed Days .................................................................................................... 86
6.7. Initial Determination, Redetermination, and Pending Medicaid Eligibility ................... 87
6.8. Care Plan and Emergency Preparedness ................................................................. 88
6.9. Retroactive Medicaid Eligibility .................................................................................. 89
6.10. Re-Admission Reviews ............................................................................................. 89
6.11. Current/Retrospective Reviews ................................................................................. 90
6.12. Transfer from Another NF ......................................................................................... 90
6.13. Changes in the LOC ................................................................................................. 91
6.14. Discharge Status ...................................................................................................... 91
6.15. Re-Review, Reconsideration, Appeal, Administrative Hearing .................................. 92
6.16. Communication Forms .............................................................................................. 94
6.17. External Audits of NF LOC Determinations ............................................................... 94
6.18. MCO Internal Audits of NF LOC Determinations ....................................................... 94
6.19. RESERVED ............................................................................................................. 94
7. Community Benefits .................................................................................................. 95
7.1. General Information .................................................................................................. 95
7.2. Definitions ................................................................................................................. 96
7.3. Nursing Facility Level of Care ................................................................................... 98
7.4. Continuous NF LOC for Certain Eligible Members .................................................... 98
7.5. External Audits of NF LOC Determinations ............................................................... 99
7.6. MCO Internal Audits of NF LOC Determinations ....................................................... 99
7.7. Registration for the CB for NOME Members ........................................................... 100
7.8. Allocation Process .................................................................................................. 102
7.9. Eligibility .................................................................................................................. 104
7.10. Closing/Inactivating an Allocation ............................................................................ 105
7.11. Registrant Notice Requirements ............................................................................. 105
7.12. Undeliverable Notice ............................................................................................... 106
8. Agency-Based Community Benefits (ABCB) ........................................................... 107
8.1. General Information ................................................................................................ 107
8.2. Definitions ............................................................................................................... 109
8.3. ABCB Services Requirements ................................................................................ 111
8.4. ABCB Covered Services ......................................................................................... 112
8.5. Adult Day Health Services ...................................................................................... 112
8.6. Assisted Living Facility (ALF) .................................................................................. 115
8.7. Behavior Support Consultation (BSC) ..................................................................... 122
8.8. Community Transition Services (CTS) .................................................................... 126
8.9. Emergency Response Services (ERS).................................................................... 128
8.10. Employment Supports ............................................................................................. 131
8.11. Environmental Modifications ................................................................................... 136
8.12. Home Health Aide (HH Aide) .................................................................................. 139
8.13. Nutritional Counseling ............................................................................................. 142
8.14. Personal Care Services (PCS) ................................................................................ 146
8.15. Private Duty Nursing (PDN) for Adults .................................................................... 176
8.16. Nursing Respite Services ........................................................................................ 182
8.17. Respite Services ..................................................................................................... 185
8.18. Skilled Maintenance Therapies ............................................................................... 190
8.19. Occupational Therapy (OT) for Adults ..................................................................... 191
8.20. Physical Therapy (PT) for Adults............................................................................. 195
8.21. Speech Language Therapy (SLT) for Adults ........................................................... 200
9. Self-Directed Community Benefits (SDCB) ............................................................. 207
9.1. Purpose .................................................................................................................. 207
9.2. Guiding Principles ................................................................................................... 208
9.3. Philosophy of Self Direction .................................................................................... 208
9.4. Definitions ............................................................................................................... 209
9.5. SDCB Member Rights ............................................................................................. 212
9.6. SDCB Member Responsibilities .............................................................................. 212
9.7. SDCB Supports ...................................................................................................... 216
9.8. Planning and Budgeting for SDCB Covered Services ............................................. 226
9.9. SDCB Qualifications for all SDCB Employees, Independent Providers, Provider
Agencies and Vendors ............................................................................................ 229
9.10. SDCB Covered Services ......................................................................................... 231
9.11. Self-Directed Non-Covered Services ...................................................................... 264
9.12. SDCB Budget and Care Plan Approval Process ..................................................... 264
9.13. Initial SDCB Budget Determination Process ........................................................... 265
9.14. Initial SDCB Care Plan Approval Process ............................................................... 265
9.15. Annual SDCB Budget Determination and Approval Process ................................... 266
9.16. Annual SDCB Care Plan Development and Approval Process ................................ 267
9.17. SDCB Budget and Care Plan Approval Process for Individuals Who Transitioned from
the MI VIA Waiver Program .................................................................................... 267
9.18. Denials, Revisions and Reconsiderations of the SDCB Care Plan .......................... 268
9.19. SDCB Care Plan Review Criteria ............................................................................ 270
9.20. Implementation of the SDCB Care Plan .................................................................. 270
9.21. Transitions, Terminations, and Reinstatement Processes ....................................... 276
9.22. Appendices ............................................................................................................. 279
9.22.1. SDCB Range of Rates Chart .................................................................................. 280
9.22.2. SDCB Vendor Credentialing Requirements ............................................................ 283
9.22.3 Employee Credentialing Requirements Grid ............................................................ 290
9.22.4. Vendor Toolkit: Invoices .......................................................................................... 291
9.22.5. Employee Toolkit: Timesheets ................................................................................ 294
10. RESERVED ............................................................................................................ 297
11. Marketing ................................................................................................................ 298
11.1. General Information ................................................................................................ 298
12. Patient-Centered Initiatives ..................................................................................... 304
12.1. Broad Standards ..................................................................................................... 304
13. ABP Medically Frail and ABP Exempt ..................................................................... 306
13.1. General Information ................................................................................................ 306
13.2. Determination of Medically Frail Diagnosis ............................................................. 306
13.3. ABP Exempt Approval ............................................................................................ 307
13.4. Appendices ............................................................................................................. 307
13.4.1. ABP Benefit Chart .................................................................................................. 308
13.4.2. Alternative Benefit Plan-Exempt Medically Frail Conditions List .............................. 320
13.4.3. Chronic SUD Criteria Checklist .............................................................................. 323
13.4.4. SMI Criteria Checklist ............................................................................................ 324
13.4.5. SMI-SED Criteria .................................................................................................... 325
14. School-Based Health Centers ................................................................................. 329
14.1. General Information ................................................................................................ 329
14.2. Initial Certification Process ...................................................................................... 331
14.3. Recertification Process ........................................................................................... 332
14.4. Adolescent Confidential Services and Suppression of Explanation of Benefits (EOBs)
............................................................................................................................... 335
15. Indian Health Services, Tribal Health Providers, and Urban Indian Providers (I/T/U)
337
15.1. FQHC/Tribal 638 Claims Processing (Alamo and Pine Hill) .................................... 337
16. Fair Hearings .......................................................................................................... 338
16.1. Administrative Hearings .......................................................................................... 338
16.2. The Member’s HSD Administrative Hearing ............................................................ 339
16.3. Appendices ............................................................................................................. 349
16.3.1. MCO Checklist – Acknowledgement of Receipt of a Member-Filed Grievance ........ 350
16.3.2. MCO Checklist for Member Grievance Final Letter ................................................. 352
16.3.3. MCO Checklist for Notice of Action Letter to Member ............................................. 353
16.3.4. MCO Checklist for Notice of Action Letter to Member Regarding VAS .................... 357
16.3.5. MCO Checklist for the Acknowledgements of Member Appeals .............................. 358
16.3.6. MCO Checklist for Letter Informing the Member of a Delay for an Appeal Decision 361
16.3.7. MCO Checklist for the MCO Member Appeal Final Decision Letter ......................... 362
17. Managed Care Reporting ........................................................................................ 365
17.1. General Information ................................................................................................ 365
17.2. General Requirements ............................................................................................ 365
17.3. MCO Reporting and Intake ..................................................................................... 365
17.4. Report Rejection ..................................................................................................... 366
17.5. MCO Report Resubmission .................................................................................... 366
17.6. Report Revisions .................................................................................................... 367
17.7. System Availability Reporting .................................................................................. 368
17.8. Appendices ............................................................................................................. 368
17.8.1. Centennial Care MCO Reports ............................................................................... 369
17.8.2. Systems Availability Incident or Event Report ......................................................... 374
18. Quality .................................................................................................................... 375
18.1. Performance Improvement Projects (PIPs) ............................................................. 375
18.2. Provider Satisfaction Survey ................................................................................... 375
18.3. Critical Incident Reporting ....................................................................................... 376
18.4. Appendix ................................................................................................................. 377
18.4.1. Centennial Care Reporting Survey Template .......................................................... 378
19. Program Integrity .................................................................................................... 382
19.1. General Information ................................................................................................ 382
19.2. Fraud, Waste and Abuse Requirements ................................................................. 382
19.3. Suspension of Medicaid Payments for Credible Allegations of Fraud ...................... 386
19.4. Adverse Action Reporting ....................................................................................... 387
19.5. Recipient Explanation of Medical Benefits .............................................................. 388
19.6. Fraud, Waste and Abuse Compliance Plan ............................................................. 388
20. Pharmacy ............................................................................................................... 389
20.1. General Information ................................................................................................ 389
21. Manual Acronyms ................................................................................................... 403
THIS PAGE INTENTIONALLY LEFT BLANK

Section 1: General Provisions
Revision dates: August 15, 2014; March 3, 2015
Effective dates: January 1, 2014
1 | P a g e
1. General Provisions
1.1. General Information
The purpose for the Managed Care Policy Manual (the Manual) is to provide a reference for the policies
established by the New Mexico Human Services Division (HSD) for the administration of the Medicaid
managed care program and to provide direction to the managed care organizations (MCOs) and other
entities providing services under managed care.
The Manual was developed by the Medical Assistance Division (MAD) of HSD to assist MCOs in the
administration of the managed care program. These policies establish general operating procedures to
assist in the day to day management of the managed care program. This Manual should be used as a
reference and a general guide. It is a resource for interpreting the Medicaid Managed Care Services
Agreement (the Agreement) and New Mexico Administrative Code (NMAC) rules pertaining to managed
care.
The provisions of the Manual reflect the general operating policies and essential procedures of the
managed care program, are not all inclusive, and may be amended or revoked at any time by the HSD.
These policies may be amended and will be reviewed on a periodic basis to determine if changes are
necessary. The Manual will be updated on a regular basis, and HSD reserves the right to change, modify,
or supersede any of these policies and procedures with or without notice at any time.
As policies are revised throughout the year, they will be incorporated into the Manual. The Manual may
be viewed or downloaded from MAD’s home page website at www.hsd.state.nm.us. A summary list of
the policy revisions will also be posted on line each year.
If there is a conflict between the Manual and the Agreement or NMAC rules, the Agreement and NMAC
rules will control. The Manual is intended to provide guidance; it is not intended to, nor does it create,
any rights that are not contained in the Agreement or NMAC rules.
The Manual will be issued and maintained by HSD. It is the responsibility of all members and entities
affiliated with Medicaid managed care in New Mexico to review and be familiar with the Manual and
any amendments.
If you have any questions about the application of any policy, you should contact the Medical Assistance
Division at 505-827-3100.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
2 | P a g e
2. Provider Network
2.1. Service Termination and Provider Closure
Anticipated changes in the MCO provider network shall be reported to the MAD and Behavioral Health
Services Division (BHSD) Contract Managers in writing within 30 calendar days prior to the change, or as
soon as the MCO knows of the anticipated change. Unexpected changes shall be reported within five
calendar days of the MCO’s knowledge about the change.
Anticipated Changes
Notification
30 Calendar Days
Narrative
10 Calendar Days from date of Notification
Transition Plan A (Overall)
15 Calendar Days from date of Notification
(if change is significant)
Transition Plan B (Member-Specific)
15 Calendar Days from date of Notification
(if change is significant)
Unanticipated Changes
Notification
5 Calendar Days
Narrative
10 Calendar Days from date of Notification
Transition Plan A (Overall)
15 Calendar Days from date of Notification
(if change is significant)
Transition Plan B (Member-Specific)
15 Calendar Days from date of Notification
(if change is significant)
The MCO is required to submit a Notification, Narrative, Transition Plan A, and Transition Plan B as
appropriate, to its Contract Manager on anticipated changes to the network. Refer to the appendices
included in this section for HSD templates. The Manager for either the Behavioral Health (BH) Unit or
the Long-Term Services and Supports (LTSS) Unit shall be copied on any network change related to
either BH or LTSS. Notification is expected whenever a provider informs the MCO, or when the MCO
learns through means other than provider notification, of its intent to change or terminate a service(s).
Notification is also expected if a service provider becomes incapable of performing a contracted service.
In all instances, the MCO is expected to report how the changes will affect the service delivery system,
which may result in the need for members to transition from one service provider to another.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
3 | P a g e
In both expected and unexpected changes in the network, the MCO shall assess the significance of the
change or closure within 10 calendar days of confirmation by the provider. If the MCO determines the
change will not have a significant impact on the system, the Narrative template must be submitted
within 10 calendar days from the date of notification of change or closure to the Contract Manager. In
the Narrative, the MCO must explain all factors considered in making a determination that the change
will not significantly impact the system and provide assurances that all members will be transitioned to
new providers (if applicable). If the MCO determines the change or closure will significantly impact the
delivery system, the MCO is required to submit Transition Plan A (Overall) and Transition Plan B
(Client-Specific) to the Contract Manager within 15 calendar days of the official Notification and
Narrative to HSD. In the event HSD determines a network change is significant, the MCO will be required
to submit all transition information as requested.
Transition information will be submitted on the templates provided by HSD with all columns completed.
The Narrative will be submitted in text format. Updates will be submitted every other week after the
initial submission. A final update will be submitted when all members are transitioned. The Notification,
Narrative, and Transition Plan A will be submitted via email to the HSD Contract Manager. Transition
Plan B will be submitted by fax or via a secure website as determined by the MCO and HSD. The HSD
Contract Manager will review and approve the official Notification, Narrative, and Transition Plan A and
will monitor and provide feedback on Transition Plan B.
If the submitted transition plan documents are incomplete, with the exception of Plan B, HSD will reject
the reporting and monetary penalties may apply per Section 7.3.3.6.5 of the Medicaid Managed Care
Services Agreement.
2.2. MCO-Initiated Provider Network Closures and Reductions
The MCOs will submit a written request to HSD regarding a significant change in the MCO’s provider
network to include either closure or reduction of providers. A significant change is defined as:
• Affecting more than 100 members statewide;
• Affecting more than 100 members in urban area;
• Affecting more than 50 members in rural area;
• Affecting more than 25 members in frontier area; and/or

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
4 | P a g e
• Limits or removes members’ choice of providers, (e.g., closure of BH network, in rural and frontier
areas).
The request must be submitted at least 60 calendar days prior to the MCO’s intended action.
• The request must include a completed Notification form and provide justification for the closure or
reduction of the specific provider network.
• The MCO must submit a current Geographical Access (Geo/Access) report demonstrating member
access and include the accessibility overview, map, and analysis of the provider network.
• HSD will review and provide the MCO with a written approval or denial within 10 business days.
• At HSD’s discretion, the MCOs may be required to submit all transition plan documents.
2.3. Provider Monitoring
HSD/MAD monitors provider access and network adequacy in a variety of ways and through various
reports. The following methods are utilized to monitor MCO provider access and network adequacy:
• Provider Satisfaction Survey;
• Member Satisfaction Survey;
• Secret Shopper Survey;
• Consumer Assessment of Healthcare Providers and Systems (CAHPS) results;
• External Quality Review Organization (EQRO) Reviews;
• MCO Call Center Reports;
• Member Grievances & Appeals Report;
• Primary Care Physician/ Primary Care Provider (PCP) Report;
• Geo/Access Report;
• Network Adequacy Report; and
• Ad Hoc Reports.
2.4. Requirements for Provider Enrollment
In considering provider enrollment, it is important for the MCO to understand there are many instances
when claims cannot be paid, if the billing provider, rendering, referring, ordering, or attending physician
or other practitioner is not enrolled and active with a status of 60 or 70. All managed care network
providers, including network providers of an MCO subcontractor, must be enrolled through a Provider

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
5 | P a g e
Participation Agreement (PPA) with the State Medicaid Agency. MAD may require that some
“non-network” providers enroll based on the number of services rendered to New Mexico Medicaid
recipients or other criteria.
Each MCO must submit a monthly listing of its network providers including the network providers of its
subcontractors. This list is due by the tenth day of each month, reflecting the network providers for the
previous month, and must include the following:
• Provider Name;
• Provider National Provider Identifier (NPI);
• Provider Taxpayer Identification Number (Social Security Number [SSN] or Federal Employer
Identification Number);
• Provider Location Address; and
• If provider receives direct reimbursement from MCO or is employed by a provider receiving the
payment.
The Patient Protection and Affordable Care Act (PPACA) Title 42, Part 455 of the Code of Federal
Regulations requires attending, ordering, referring, rendering, and prescribing providers to be enrolled
in the Medicaid program in order to meet PPACA program integrity requirements designed to ensure all
attended, prescribed, ordered, referred, or rendered services, items, and admissions for Medicaid
beneficiaries originate from properly-licensed providers who have not been excluded from Medicare or
Medicaid. A provider who is enrolled through a PPA with MAD only as a fee-for-service (FFS) provider,
only as a managed care provider, or who is enrolled as both FFS and managed care is considered to be
“enrolled with Medicaid” for these purposes.
Therefore, the expectation is that most services and items will only be paid by the Medicaid program if
the individual provider who attends, prescribes, orders, refers, or renders a service or item is identified
on the claim and is enrolled in the Medicaid program. Otherwise, the claim will be denied in accordance
with Federal requirements.
This requirement now applies to both the Medicaid FFS program and to the Medicaid MCOs. Even with
the implementation of these requirements, FFS and the MCOs will still be required to continue
implementing more changes in the near future, such as:
• Including prescribing providers on pharmacy claims.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
6 | P a g e
• Ensuring we are meeting Centers for Medicare & Medicaid Services (CMS) expectations for Indian
Health Services (IHS) and Federally Qualified Health Centers (FQHCs), which may have changed since
the previous CMS review.
• Working towards including rendering providers on more BH services and home- and
community-based services (HCBS) developmentally disabled (DD) waiver services. (We may also
begin enrolling opticians, hearing aid testers, and other individuals who provide services within a
health care business entity. We are expanding our type and specialty listings to accommodate this
action.
• The MCOs should allow certified-nurse practitioners, clinical nurse specialists and certified nurse-
midwives who have been granted parity with physician privileges at health facilities to admit,
discharge, and authorize continued patient care.
Under these requirements, it is possible that some practitioners will need to enroll in the Medicaid
program; otherwise, the recipient may have to change individual providers in order for their services
to be ordered, referred, prescribed, or attended by a Medicaid enrolled provider.
There are also some providers who are members of groups, agencies, and other facilities who have
not enrolled individually as a member of the group, agency, or facility. To a lesser extent, there may
be some individual providers who have not enrolled in the Medicaid program because they do not
bill Medicaid, but who, never-the-less, order or prescribe services for the recipient that will be billed
to Medicaid by other providers as a result of the order or prescription.
• MAD has developed, and made available on the Conduent New Mexico Medicaid Web Portal at
https://nmmedicaid.portal.conduent.com/webportal/providerSearch a look-up tool to help
providers obtain the NPI of a rendering, prescribing, ordering, referring, or attending provider. The
instructions for using this web portal tool and contact information for the Conduent Provider
Relations staff, are included in this document.
Providers should use this tool to determine if any services they are providing to Medicaid recipients
are based on prescriptions, orders, or referrals from a provider who is not enrolled in the Medicaid
or managed care program.
Providers should also use this tool to determine if any provider or practitioner on their staff needs to
be enrolled and to immediately begin the enrollment process if necessary.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
7 | P a g e
• MAD allows provider enrollment as a Medicaid provider solely for the purpose of establishing
appropriate enrollment for the services they order, refer, or prescribe without having to commit to
seeing all Medicaid patients or even any Medicaid patients.
While discriminatory practices towards recipients are not allowed by State and Federal rules, a
provider can still choose to limit his or her practice and participation in the Medicaid program in
ways that are not discriminatory. Such limitations could include treating emergency situations only,
only seeing recipients who are dually eligible for Medicare, limiting the number of patients or
recipients seen, or to only see existing recipients without taking new patients.
This information may be useful to a provider who is hesitant to enroll in the Medicaid program.
Hospital, Residential, Nursing Facility (NF), HH, and Hospice Claims
The essential requirements are:
• The attending provider must be reported on the Universal Billing (UB) format claim for the
following:
o Inpatient hospital claims;
o Hospice claims; and
o Home health agency (HHA) claims (referring or ordering provider in the attending field).
• NF and intermediate care facilities for individuals with intellectual disabilities (ICF-IID) claims
(referring or ordering provider in attending field;
• Residential facility claims (accredited residential treatment center [ARTC], RTC, and Group Homes)
(referring or ordering provider in the attending field);
• The rendering provider must be reported at the claim header level or on all lines on an outpatient
hospital claim;
• A referring or ordering provider must be reported on an outpatient hospital claim when the service
is the result of a referral; and/or
• If any of these providers submit claims on the CMS 1500 format, such as the physician component
that corresponds to an inpatient or outpatient hospital claim, the requirements for rendering
provider on the CMS 1500 format must be followed.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
8 | P a g e
Referring or Ordering Providers on Claims
The essential requirements are:
• When the service provided is the result of a referral from another practitioner, that provider should
be reported as the Referring or Ordering provider.
• In most instances, the MCO will not know if the service was based on a referral or not; therefore, in
most instances, a referral cannot be required. Instead the provider must be relied upon to follow
the instructions. However, there are certain types of providers whose services are performed only
upon an order or referral from another provider such as independent laboratories, radiology
facilities, suppliers of medical equipment, medical supplies, and oxygen. So it is possible to make the
Referring or Ordering provider mandatory under these circumstances as indicated in this document.
Rendering Providers on Claims
The essential requirements are:
• The rendering provider must be identified for most services.
• Exceptions and special circumstances are described in this document.
2.5. Institutional Type Providers
Specific Provider Reporting Requirements
• HHA Claims; NF Claims: the ordering provider’s NPI must be indicated in the attending provider NPI
field.
• Hospice Claims, Residential Provider claims (ARTC, RTC, and Group Homes): the attending
provider’s NPI is required.
• Hospital Inpatient Claims (including specialty hospitals): the attending provider’s NPI is required.
See below for requirements for outpatient hospital claims.
• Hospital Outpatient claims (Including specialty hospitals): the rendering provider’s NPI must be
reported on hospital outpatient claims. It may either be reported at the header level (if a single
provider is the rendering provider) or at the line level (if there are different rendering providers for
each service or line). Or they may always choose to report at the line level.
In many hospitals, the rendering provider may be a resident, an intern, or a supervised nurse,
technician, or other individual who cannot enroll as a provider in their own right. In these situations,

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
9 | P a g e
the provider overseeing the services for the recipient may be considered the rendering provider and
reported as such.
Even though one may think of a lab code or radiology code, or some other service codes on the
claim as not being performed by the provider, but rather by a lab or radiology technician, the
provider overseeing the service for the recipient is still to be reported as the rendering provider on
that line.
Correct Placement of Information on Claims
Attending Physicians for Inpatient Hospitals, Hospice Providers, Ordering Physicians or HHAs NFs, ICF-
IID, and Residential Facilities
Paper UB format claim: Report the names and NPI in form locator 76 (Attending Provider Name
and Identifiers)
Electronic 837 I claim: Report the names and NPI in loop 2310A
Data Element NM 101 Attending Provider = “71”
Data Element NM 103 Attending Provider Last Name
Data Element NM 104 Attending Provider First Name
Data Element NM 108 Identification Code Qualifier “XX”
Data Element NM 109 Attending Physician Primary Identifier NPI
Referring or Ordering Physicians (or other Providers), Reported when Applicable
Paper UB format: Report the NPI and name of the referring or other provider in Field
Locator 78 (Other Physician’s Name and Identifier)
Electronic 837I The following loop, segment, and element places are used to report the referring provider’s NPI and
name, depending on whether reporting is being done at the header or line level
Referring Provider – 2310F (Header)/2420D (Line), Data Element NM101 = “DN”
Referring Provider Last Name – 2310F (Header)/2420D (Line), Data Element NM103
Referring Provider First Name – 2310F (Header)/2420D (Line), NM104
Referring Provider’s NPI – 2310F (Header)/2420D (Line), NM108 = “XX”
Referring Provider’s NPI – 2310F (Header)/2420D (Line), NM109
Referring or ordering providers are to be reported on claims when the service or item is the result of a
referral or an order.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
10 | P a g e
Rendering providers must be reported on claims for professional services such as reading or interpreting
the results of an anatomical laboratory service or radiological images. Rendering providers may either
be reported at the header level (if a single provider is the rendering provider) or at the line level.
The rendering, referring, or ordering provider may be a resident, intern, supervised nurse, technician, or
other individual not typically enrolled as a provider in their own right. In these situations, the supervising
provider may be considered the rendering provider, referring, or ordering provider, as appropriate, and
reported as such.
2.6. Providers Whose Services are Based on Orders and Referrals
Specific Provider Reporting Requirements
For the Medicaid program, MAD does not distinguish between an ordering and referring provider;
information may be placed in either the ordering or referring provider fields.
The following providers should always have an ordering or referring provider for their services or items:
• Clinical diagnostic laboratories including clinical labs, diagnostic labs for physical tests and
measurements, clinical labs with radiology, and other diagnostic laboratories.
• Hearing aid dealers, IV infusion services, opticians and other eyeglass dispensers, and medical supply
and durable medical equipment (DME) companies.
• Occupational therapists, orthotists, physical therapists, prosthetists, speech and language
pathologists, and rehabilitation centers.
• Radiology and radiation treatment facilities.
MAD recognizes that some therapists can self-refer; that is, upon seeing and evaluating a recipient,
they may refer the recipient to themselves for treatment. When this occurs, the therapist must
report himself or herself as the referring provider, as well as the rendering provider.
Sometimes the referring, ordering, or prescribing provider may be a resident, intern, or supervised
nurse, technician, or other qualified individual who cannot enroll as a provider in their own right. In
these situations, the supervising provider may be considered the rendering provider and reported as
such.
When a laboratory, radiology, or diagnostic test is for or includes a professional component for
reading or interpretation of the results, the rendering provider must be provided in addition to the
referring or ordering provider.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
11 | P a g e
Correct Placement of Information
Referring or Ordering Physicians (or other Provider), Reported when Applicable
Paper CMS 1500 format: Report the NPI of the referring or ordering provider in Field Locator 17b
(Other Physician’s Name and Identifier)
Electronic 837P: The following loop, segment, and element places are used to report the
referring provider’s NPI and name, depending on whether reporting is
being done at the header or line level
Referring Provider – 2310A (Header)/2420F (Line), Data Element NM101 = “DN”
Referring Provider Last Name – 2310A (Header)/2420F (Line), Data Element NM103
Referring Provider First Name – 2310A (Header)/2420F (Line), NM104
Referring Provider’s NPI – 2310A (Header)/2420F (Line), NM108 = “XX”
Referring Provider’s NPI – 2310A (Header)/2420F (Line), NM109
Rendering Physician or Other Provider - Report on all Professional Services
Paper CMS 1500: Report the NPI of the rendering provider in Field Locator 24 J lower line
Rendering Provider ID number
Electronic 837P: The following loop, segment and element places are used to
report the rendering provider’s NPI and name, depending on whether
reporting is being done at the header or line level
Rendering Provider – 2310B (Header)/2420A (Line), Data Element NM101 = “82”
Rendering Provider Last Name - 2310B (Header)/2420A (Line), Data Element M103
Rendering Provider First Name – 2310B (Header)/2420A (Line), NM104
Rendering Provider’s NPI – 2310B (Header)/2420A (Line), NM108 = “XX”
Rendering Provider’s NPI – 2310B (Header)/2420A (Line), NM109
2.7. Rendering Providers
Rendering providers must be reported on professional services. There is a new requirement for
rendering providers that they must also be reported on laboratory, radiology, injections, supplies, items,
and all other services reported on a CMS 1500 format claim.
Even though one may think of a lab code, a radiology code, or other service codes on the claim as not
being performed by the physician or physician extender, but rather by a lab or radiology technician, or
an injection or other treatment as being performed by a nurse or other staff, the provider overseeing

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
12 | P a g e
the primary service for the recipient is still to be reported as the rendering provider for these types of
services.
Rendering providers may either be reported at the header level (if a single provider is the rendering
provider) or at the line level.
In many hospitals, the rendering provider may be a resident, an intern, or a supervised nurse,
technician, or other individual not typically enrolled as a provider in their own right. In these situations,
the supervising provider may be considered the rendering provider and reported as such.
Referring or ordering providers are to be reported when the service is a result of a referral or an order. It
may also be reported at the header level on a claim or at the line lever.
Specific Provider Reporting Requirements
Multidisciplinary Team Services
MAD is still working on issues with BH Agencies, Certified Mental Health (MH) Centers, BH Core Service
Agencies, Opioid Treatment Centers, Health Homes, and Case Management Agencies, regarding
reporting rendering providers on any service which is rendered by a multidisciplinary team. For these
providers, for services that are not provided by a multidisciplinary team, the provider must report
rendering providers and proceed with enrolling all practitioners on their staffs.
If the rendering provider is a resident, intern, supervised nurse, technician, or other qualified individual
who cannot enroll as a provider in their own right, the supervising provider may be considered the
rendering provider and reported as such.
Referring and Ordering Providers:
In addition to a rendering provider, the referring or ordering provider may also be reported. For the
Medicaid program, MAD does not distinguish between an ordering and referring provide and the
information may be placed in either the ordering or referring provider fields. These instructions are for
using the referring provider fields.
If the referring, ordering, or prescribing provider is a resident, an intern, a supervised nurse, technician,
or other qualified individual who cannot enroll as a provider in their own right, the supervising provider
may be considered the rendering provider and reported as such.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
13 | P a g e
Correct Placement of Information
Rendering Physician or Other Provider - Report on all Professional Services
Paper CMS 1500: Report the NPI of the rendering provider in Field Locator 24 J lower line
Rendering Provider ID number.
Electronic 837P: The following loop, segment, and element places are used to
report the rendering provider’s NPI and name, depending on whether
reporting is being done at the header or line level.
Rendering Provider – 2310B (Header)/2420A (Line), Data Element NM101 = “82”
Rendering Provider Last Name 2310B (Header)/2420A (Line), Data Element NM103
Rendering Provider First Name – 2310B (Header)/2420A (Line), NM104
Rendering Provider’s NPI – 2310B (Header)/2420A (Line), NM108 = “XX”
Rendering Provider’s NPI – 2310B (Header)/2420A (Line), NM109
Rendering Dentist or Other Provider, Report on Dental Services
Paper ADA form: Report the NPI of the rendering provider in Block 54.
Electronic 837D: The following loop, segment and element places are used to report the
rendering provider’s NPI and name, depending on whether reporting is
being done at the header or line level.
Rendering Provider – 2310B (Header)/2420A (Line), Data Element NM101 = “82”
Rendering Provider Last Name - 2310B (Header)/2420A (Line), Data Element NM103
Rendering Provider First Name – 2310B (Header)/2420A (Line), NM104
Rendering Provider’s NPI – 2310B (Header)/2420A (Line), NM108 = “XX”
Rendering Provider’s NPI – 2310B (Header)/2420A (Line), NM109
Referring or Ordering Physicians or Other Provider) - Reported When Applicable
Paper CMS 1500 format: Report the NPI of the referring or ordering provider in Field Locator 17b
(Other Physician’s Name and Identifier).
Electronic 837P: The following loop, segment and element places are used to report the
referring provider’s NPI and name, depending on whether reporting is
being done at the header or line level.
Referring Provider – 2310A (Header)/2420F (Line), Data Element NM101 = “DN”
Referring Provider Last Name – 2310A (Header)/2420F (Line), Data Element NM103
Referring Provider First Name – 2310A (Header)/2420F (Line), NM104

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
14 | P a g e
Referring Provider’s NPI – 2310A (Header)/2420F (Line), NM108 = “XX”
Referring Provider’s NPI – 2310A (Header)/2420F (Line), NM109
Referring or Ordering Dentist On Dental Claims - Reported When Applicable
Paper ADA: Form does not have this field. Cannot be reported.
Electronic 837: The following loop, segment and element places are used to report the
referring provider’s NPI and name, depending on whether reporting is
being done at the header or line level.
Referring Provider – 2310A (Header)/2420F (Line), Data Element NM101 = “DN”
Referring Provider Last Name – 2310A (Header)/2420F (Line), Data Element NM103
Referring Provider First Name – 2310A (Header)/2420F (Line), NM104
Referring Provider’s NPI – 2310A (Header)/2420F (Line), NM108 = “XX”
Referring Provider’s NPI – 2310A (Header)/2420F (Line), NM109
2.8. Using the Web to Verify Attending, Ordering, Referring, Rendering or Prescribing Providers
It is ultimately the responsibility of the Medicaid provider billing the service to obtain the NPI of the
prescribing, referring, ordering, attending, or rendering provider and to confirm the provider’s active
enrollment in the Medicaid program. Each Medicaid provider will need to develop its own internal
processes to ensure the enrollment requirement is met or the provider risks the claim being denied.
A provider may look up the NPI of a provider participating in the Medicaid program on the Conduent
New Mexico Medicaid web portal and may also determine if the attending, ordering, referring,
rendering, or prescribing provider is enrolled in the Medicaid FFS or managed care program as required.
1.
From the main ‘Provider Information’ section of the portal
https://nmmedicaid.portal.conduent.com/static/ProviderInformation.htm
2.
Click on the ‘Provider Search’ link on the left side of the screen (highlighted in yellow below.) It can
also be accessed directly by going to the URL:
https://nmmedicaid.portal.conduent.com/webportal/providerSearch

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
15 | P a g e
3. Then search by NPI, organization name, or provider name.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
16 | P a g e
4. You will get results such as those below.
5. To be considered to meet the Medicaid FFS or managed care enrollment requirements, a provider
must either be “active” as a status 60 or “MCO” as a status 70 on the date of service on the claim.
6. If you do not get any results, re-check the information entered.
7. If you do not find the ordering, referring, or prescribing provider listed, and the individual provider
works for the Indian Health Services or a tribal health care facility, an FQHC, or is a resident at
University of New Mexico Hospital (UNMH), you can look up the organization using the provider
name search field and use the NPI of that entity on the claim.
You can search for an organization by putting part of the organization’s name in the search field. The
NPI of an organization such as those listed above may be entered as the prescriber or referring
provider.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
17 | P a g e
2.9. Exclusions
At this time, reporting the rendering, referring, ordering, or attending providers on a claim are not
required for the following provider types. However, to the extent that an MCO may already be requiring
such information, there is no need for the MCO to discontinue the requirement.
Provider Type
Description
221
Indian Health Services Hospital or Tribal Compact facility –
specialty required, multiple specialties allowed
313
Clinic FQHC, Medical
314
Clinic, Rural Health Medical, freestanding
315
Clinic, Rural Health Medical, hospital-based
343
Methadone Clinic
346
Lodging, Meals
363
Community Benefit Provider (enrolled for MCOs only)
401
Ambulance, Air
402
Ambulance, Ground
403
Handivan
404
Taxi, or MCO General Transportation Contractor (Non-Capitated)
462
Case Management Agency (specialty required)
This may change in the future as we work with CMS and providers.
HSD is not addressing value-added services (VAS) at this time. If an MCO feels it is appropriate to notify
providers of VAS that a rendering or referring provider or ordering provider is required, an MCO may do
so. For example, a physician applying a dental fluoride varnish would reasonably be expected to be
identified as a rendering provider; however, this is not stated on any FFS list.
When Medicare or a Medicare Advantage program has paid the claim, and the claim is being evaluated
for co-insurance, deductible or co-payment, rendering, referring, ordering, or attending providers on a
claim are not required. However, for any other claim with a prior payment, such as from an insurance
company or a health maintenance organization plan, there is no exemption. The provider must add the
information to the claim.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
18 | P a g e
If MAD does not enroll certain providers of services that are in managed care, such as Support Brokers,
there is no requirement for them to be actively enrolled in Medicaid. If a provider is enrolled or
identified with a provider type in the 900 series of provider types, which are only applicable to managed
care (such as a traditional healer), there is no current requirement that rendering, referring, ordering,
attending providers be reported.
Medicaid is not requiring changes for pharmacy claims at this time. MAD is working on system changes
within the State system to meet the Federal requirements for prescriber, but more work is needed.
MCOs do not need to remove any requirements on pharmacy claims they may already have in place.
School-based health clinics are not exempt from the requirements. Neither are out of state,
out-of-network providers, or single case agreement providers exempt from the rule.
2.10. General Information on the Requirements based on Procedure Codes
Each procedure code in the Omnicaid System has an indicator on it that indicates if a rendering provider
is required (with an S), a referring provider is required (with an R), or whether both are required (with a
B) or if nothing is required (with an N).
A list of codes with the indicators is periodically provided to each MCO which includes most codes on
the Rendering Provider Required by Procedure Code List.
However, there are some important considerations in using that list:
1. Referring Requirements for Laboratories, Radiology Facilities, Suppliers of Prosthetics and
Orthotics, Oxygen, DME, and Medical Supplies
The indicator on the procedure code list is not applicable to services billed by laboratories, radiology
facilities, prosthesis and orthosis suppliers, oxygen suppliers, durable medical equipment and
medical supply suppliers.
For these providers there is always an expectation that the services were ordered and therefore the
ordering provider must be indicated.
Therefore, for example, the indicator on a lab code that says a rendering provider is required does
not apply to these providers, not even the free-standing laboratory. Rather, the requirement that
there should always be a referring provider is applicable.
For a laboratory or radiology facility, a rendering provider would only be required when a
professional interpretation billed (typically using modifier 26).

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
19 | P a g e
For claim processing and encounter purposes MAD does not make a distinction between referring or
ordering providers. Either will meet the requirements when a referring provider is required.
2. Rendering Provider Requirements
The Rendering Provider Required by Procedure Code List described above may be used to determine
when a rendering provider is required. However, there are other aspects to be considered, such as
the billing provider type.
The following provider types are always exempt from reporting a rendering provider. This may
change in the future, but until individuals working within these providers are always enrolled, we
cannot enforce a rendering provider requirements:
Provider Type
Description
218
Treatment Foster Care Services
221
Indian Health Services Hospital or Tribal Compact facility
324
Nursing, Private Duty
334
Optician
336
Orthotist
337
Prosthetist
338
Prosthetist & Orthotist
343
Methadone Clinic
344
HCBS or Mi Via Self-Directed Waivers
346
Lodging, Meals
363
Community Benefit Provider
405
Birthing Centers
412
Hearing Aid Supplier
414
Medical Supply Company
415
IV Infusion Services
416
Pharmacy
417
Pharmacy, Rural Health Clinic (RHC)
441
Developmental Delay Services
447
Renal Dialysis Facility
462
Case Management Agency

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
20 | P a g e
For clarity, MAD has prepared a list of all FFS provider types for which a rendering provider may be
required (Rendering Provider Required by Provider Type List). If the provider is on this list, and the
procedure code is on the Rendering Provider Required by Procedure Code List, a rendering provider
should be reported.
The rendering provider cannot be the same as the billing provider if the billing provider is a group.
• A billing group provider number cannot be used as the rendering provider on the claim. There may
be various ways of enforcing this.
However, MAD has always designated whether a provider is a group practice or an individual. Most
individual health professionals can belong to a group practice or practice individually. When it is
possible for a provider ID to be either a “group” (G) or an “individual” (I), MAD is careful when
processing an application to designate the provider as either G or I.
This information is used when validating a rendering provider entered on a claim. Assume there is a
professional group such as Scrooge and Marley Pediatricians with a G indicator and there is an
individual within the group “Dr. Jacob Marley” with an I indicator.
If the billing provider Scrooge and Marley Pediatricians also enters their group NPI number in the
rendering provider field, the Medicaid Management Information Systems (MMIS) will detect the
rendering provider is the same as the billing group and deny the claim.
If the billing provider is an individual, Dr. Bob Cratchit, for example, and the NPI appears as both the
billing provider and the rendering provider, the MMIS will recognize that the billing provider is an
individual and therefore may certainly use the individual NPI in the rendering provider field. (This is
done by using by-pass logic in the edit.)
In the MMIS, the billing provider is propagated to the lines of the claim.
• This principle remains exactly the same for dental individual providers and dental group practices.
Not all providers can be designated as a G and having many employees does not make a provider a
group. The G distinction is largely for professional providers and the groups they form. Institutional
providers such as hospitals are considered I, not as group, as is a hospice or an HHA – that is, they
only function as individual entities.
The only exception is the FQHC because it is a clinic and a clinic is considered a group practice.
Depending on how the MCO processes Comprehensive Outpatient Rehabilitation Facility claims,
such as if they use the UB format, there is a requirement for rendering providers to be identified for
them.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
21 | P a g e
• One of the major new requirements for Medicaid is the rendering provider must be reported for
outpatient hospital services billed on the outpatient hospital claim.
• Behavioral Health Codes Exempted from Reporting Rendering Provider
It is anticipated that many of the BH codes listed below will, at some point, require a rendering
provider. Until there has been further communications with the providers, MAD will not require a
rendering provider for the following. A chart showing the rendering provider requirements for BH
services will be periodically updated and sent to the MCOs.
Note that for clarity, MAD will periodically send the MCOs lists of all codes that do and do not require a
rendering provider. Also, a transportation provider never has to identify a rendering provider.
Note that if a MCO is already requiring rendering providers for these codes, there is no need for a MCO
to stop doing so.
Also, please do not use this list to try to determine which codes are a benefit of the program. That is a
different issue. We do not necessarily cover all the codes described above.
3. Attending Provider Requirements by Provider Type
The following providers require an attending provider. A rendering provider is never required unless
the provider is not the facility, but rather a practitioner billing on the CMS 1500 form such as for
skilled nursing facility (SNF) rehabilitation services, for example.
Provider Type
Description
201
Hospital, General Acute Inpatient
202
Hospital, Rehabilitation Unit in a General Acute Hospital Inpatient
203
Hospital, Rehabilitation or Other Specialty Hospitals- such as LTAC hospitals - Inpatient
204
Hospital, Psychiatric Unit in a General Acute Hospital Inpatient
205
Hospital, Psychiatric Free-Standing Inpatient
211
NF, Private for NF Stays
212
NF, State for NF Stays
213
Hospital, Swing-Bed for NF Stays
216
ARTC, Joint Commission accredited for Residential Facility Stays
217
RTC, not Joint Commission accredited for Residential Facility Stays
219
RTC Group Home, not Joint Commission accredited for Residential Facility Stays

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
22 | P a g e
The attending provider cannot be the same as the billing provider and must be an individual
provider. The MMIS has edits that enforce this requirement.
4. The Referring Provider by Provider Type
The requirements for referring providers on some claims is covered in number 1, above. A referring
provider is required from the following unless otherwise exempted in this document (such as when
we say that Medicare cross overs are exempt from the requirement).
Provider Type
Description
351
Lab, Clinical Freestanding
352
Radiology Facility
353
Laboratory, Clinical with Radiology
354
Diagnostic Laboratory (physical measurements)
414
Medical Supply Company
415
IV Infusion Services
416
Pharmacy when billing on a CMS 1500 format
417
Pharmacy, RHC when billing on a CMS 1500 format
451
Occupational Therapy (OT) (may self-refer)
452
Occupational Therapist Licensed, not certified (may self-refer)
453
Physical Therapy (PT) (may self-refer)
454
Physical Therapist, Licensed, not certified (may self-refer)
Additional circumstances for which a referring provider is required are as follows:
Provider Type
Description
324
Nursing, Private Duty - referring is required when not being billed by an HHA
334
Optician - a referring provider must be indicated for glasses but not for repairs
Other providers are to report a referring provider when there is one, but generally unless the MCO
specifically requires a referring provider for a service, it is not known whether the service was due to
a referral.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
23 | P a g e
However, the following procedure codes would seem to logically have a referring provider so it must
be reported for them:
Description
Procedure Code
Requirement
Office Consultation
99241
R-Referring
Office Consultation
99242
R-Referring
Office Consultation
99243
R-Referring
Office Consultation
99244
R-Referring
Office Consultation
99245
R-Referring
At this time, CMS rules allow Medicaid to accept the referring provider can be an institution and not
necessarily an individual. This is generally allowed when the referring provider is with a type of
institution such as UNMH, an IHS facility, or tribal facility where interns, residents, and non-enrolled
staff might be practicing. MCOs must also allow for this.
2.11. Appendices
2.11.1 Notification of Change in Services – Notification of Transition
2.11.2 MCO Notification to HSD of Change or Closure- Narrative for Provider/Facility
2.11.3 Transition Plan A- Overall Transition Plan Information- MCO Transition Plan for Provider/Facility
2.11.4 Transition Plan B- Member Specific Information for Provider
2.11.5 Definitions

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
24 | P a g e
2.11.1. Notification of Change in Services – Notification of Transition
MCO NOTIFICATION TO HSD- NOTICE OF CHANGE IN SERVICES ☐
MCO NOTIFICATION TO HSD- NOTICE OF TRANSITION ☐
*Expected Change ☐ *Unexpected Change ☐
Date:
Date MCO Notified of Closure:
Anticipated Date of Closure:
Name of Provider or Facility:
Type of Provider Individual:
☐Group:
☐Agency: ☐
Facility: ☐
Full contract termination? Yes ☐ No ☐
Addresses of all locations (include county and region type):
Type(s) of Service(s):
Satellite location terminating? Yes ☐ No ☐
Address of location terming (include county and region type):
Type(s) of Service(s) at location:
Terminating Services only? Yes ☐ No ☐
Type(s) of Service(s):
Total Number of Members Affected: <21 >21
Transition Plans Required? Yes ☐ No ☐
Narrative Due Date: (Due 10 calendar days after Notification):
The below items should be filled in only if transition plans are required.
Transition Plans A & B Due Date:
(Due 15 calendar days after Notification)
Name of MCO Staff and/or Care Coordinator Responsible for Transition:
*Notification of unexpected change is due within five business days of confirmed change. Notification of expected change is due
30 days prior to the confirmed change.

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
25 | P a g e
2.11.2. Transition Plans Narrative
MCO Notification to HSD of Change or Closure
Narrative For
(Provider/Facility Name)
Date:
MCO Staff and/or Care Coordinator:
Describe the reason(s) and/or circumstances and any contributing factors to the change or closure:
How the change affects delivery of, or access to, covered services (describe how the change impacts the
system as whole and at the community level):

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
26 | P a g e
The MCO’s plan for maintaining access and the quality of Member care:
Please explain all factors considered in making the determination that the change will not significantly
impact the system and provide assurances that all Members will be transitioned to new providers (if
applicable).
Transition issues identified

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
27 | P a g e
2.11.3. Transition Plan A
Overall Transition Plan Information
MCO Transition Plan For
(Provider Name) (Date)
MCO task
assignment
Comments
Begin
Date
End Date
1. Preplanning
MCO receives communication of
contract, location, service closure.
Closing program sends a formal
letter to MCO advising of closing.
List of affected members sent to
MCO.
List of special problems expected or
associated with transition.
MCO letter to affected members
offering assistance (as needed).
2. Network Operations
Contracting department to complete
Table A Provider Information.
3. Transition planning
Meeting with program or director.
Complete plan to ensure program is
appropriately referring and
transitioning affected members.
Progress updates of transition
program.
Template for Records Retention
Completed and attached.
4. Communication to HSD
Submit notification.
Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
28 | P a g e
MCO task
assignment
Comments
Begin
Date
End Date
Submit narrative.
Submit Transition Plan A.
Submit Transition Plan B.
Bi-weekly updates of transition plans
and narrative from MCO to state
agency contact person.
5. Care Coordination
Identify Care Coordinators to be
contact point for members seeking
assistance.
Care Coordinator review of
community resources.
Care coordination and MCO
Clinical/UM Department tasks.
Compile weekly report of care
coordination.
Meeting with MCO and program
transition team to coordinate efforts,
if applicable.
Other requirements as needed
depending on circumstances of
closing.
Transition plan finalized.
MCO certifies the transition of all members has taken place and is finalized.
Signature:
Date: __________________

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
29 | P a g e
2.11.4. Transition Plan B

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
30 | P a g e

Section 2: Provider Network
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
31 | P a g e
2.11.5. Definitions
• Certified Nurse Midwife (CNM) means a registered nurse pursuant to the Nursing Practice Act who
is licensed by the board of nursing for advanced practice and licensed by the Department of Health
as a nurse-midwife.
• Certified Nurse Practitioner (CNP) means a registered nurse who is licensed by the
board for advanced practice as a certified nurse practitioner and whose name and
pertinent information are entered on the list of certified nurse practitioners maintained by
the board.
• Clinical Nurse Specialist (CNS) means a registered nurse who is licensed by the board
for advanced practice as a clinical nurse specialist and whose name and pertinent
information are entered on the list of clinical nurse specialists maintained by the board.

Section 3: Member Education
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
32 | P a g e
3. Member Education
3.1. Policies and Procedures
The MCO shall maintain policies and procedures governing the development and distribution of
educational material for members. Policies shall address how members and potential members receive
information, the means of dissemination and the content comprehension level, and languages of this
information. The MCO shall have written policies and procedures regarding the utilization of information
on race, ethnicity, and primary language spoken by its membership.
All written member materials shall meet the material guidelines established in the Agreement and
defined in Section 11 Marketing of this Manual. All materials distributed shall include a language block
informing the member that the document contains important information and directs the member to
call the MCO to request the document in an alternative language or to have it orally translated at no
expense to the member. The language block shall be printed, at a minimum, in the non-English
languages meeting the requirement of Subsection A of 8.308.8.10 NMAC.
MCOs shall provide members the option of receiving materials via mail, email, or website in accordance
with 42 CFR 438.10. Member materials and enrollee information may not be provided electronically to
the enrollee unless all of the following are met:
• The information is provided electronically after obtaining the enrollee’s consent to receive the
information electronically;
• The format is readily accessible;
• The information is placed in a location on the MCO’s website that is prominent and readily accessible;
• The information is provided in an electronic form that can be electronically retained and printed;
• The information is consistent with the content and language requirements of Section 42 CFR 438.10;
and
• The enrollee is informed the information is available in paper form without charge upon request and
the MCO provides it upon request within 5 business days.
The MCO shall provide written notice to members of any material changes previously sent at least 30
calendar days before effective date of the change.

Section 3: Member Education
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
33 | P a g e
3.2. Member Handbook
The MCO member handbook must include a table of contents and, at a minimum, comply with the
following:
• MCO demographic information, including the organization’s hotline telephone number and hours of
operation;
• Information on how to obtain services such as after-hours and emergency services, including the
911 telephone system or its local equivalent, and Nurse Advice line;
• Member bill of rights and member responsibilities, including any restrictions on the member’s
freedom of choice among network providers;
• Information pertaining to coordination of care by and with PCPs (within the MCO), as well as
information pertaining to transition of care (between the MCOs);
• How to obtain care in emergency and urgent conditions and that prior authorization is not required
for emergency services;
• The amount, duration, and scope of mandatory benefits;
• Information on accessing BH or other specialty services, including a discussion of the member’s
rights to self-refer to in-plan and out-of-plan family planning providers, a female member’s right to
self-refer to a women’s health specialist within the network for covered care, and that members
may self-refer for BH services and are not required to visit their PCP first;
• Limitations to the receipt of care from out-of-network providers;
• A list of services for which prior authorization or a referral is required and the method of obtaining
both;
• Information on Utilization Management (UM) Services;
• A policy on referrals for specialty care and other benefits not furnished by the member’s PCP;
• Information on how to obtain pharmacy services;
• Information regarding Grievances, Appeals, and Fair Hearing procedures and timeframes including
all pertinent information provided in 42 CFR 438.00 through 438.424;
• Information on the member’s right to terminate enrollment and the process for voluntarily
dis-enrolling from the plan;
• Information on the MCO switch process;
• Information on how members change their demographic information.

Section 3: Member Education
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
34 | P a g e
• Information regarding advance directives including advance directives for BH;
• Information regarding how to obtain a second opinion;
• Information on cost sharing, if any;
• How to obtain information, upon request, determined by HSD as essential during the member’s
initial contact with the MCO, which may include a request for information (RFI) regarding the MCO’s
structure, operation, and physician’s or senior staff’s incentive plans;
• Value-added benefits which are not covered by the Agreement and how the member may access
those benefits;
• Information regarding the birthing option program;
• Language that clearly explains that a Native American member may self-refer to an IHS or a tribal
health care facility for services;
• Information on how to report fraud, waste and abuse;
• Information on member’s privacy rights;
• Information on the circumstance/situations under which a member may be billed for services or
assessed charges or fees; specifically that the provider may not bill a member or assess charges or
fees except: if a Member self-refers to a specialist or other provider within the network without
following contractor procedures (e.g., without obtaining prior authorization) and the contractor
denies payment to the provider, the provider may bill the member, if a provider fails to follow the
contractor’s procedures, which results in non-payment, the provider may not bill the member, and if
a provider bills the member for non-covered services or for self-referrals, he or she shall inform the
member and obtain prior agreement from the member regarding the cost of the procedure and the
payment terms at time of service;
• Information on how to access services when out of state;
• Include information about Care Coordination, including the role of Care Coordinators; and
• Information on the centennial rewards program and how a member accesses the program and earns
rewards.

Section 3: Member Education
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
35 | P a g e
3.3. Provider Directories
The MCO may choose to maintain regionalized, printed, or printable provider directories by Northern,
Southern, and Central regions of the State; however, each regionalized provider directory must include
telephone numbers for crisis lines, Member Services line, all out of state providers and Bernalillo
County providers. Information on how to access these regionalized provider directories online or how
to request a copy should be indicated on the MCO’s website and in the Member Handbook.
Online provider directories must be comprehensive and inclusive of all providers in all regions, as well as
telephone numbers for crisis lines, Member Services line, and all out of state providers.
3.4. Member Identification Card
The member ID card shall be durable (e.g., plastic or other durable paper stock but not regular paper
stock), shall comply with all State and Federal requirements and, at a minimum, shall include:
• The MCO’s name and issuer identifier, with the company logo;
• Phone numbers for information and/or authorizations, including for physical health (PH), BH, and
Long-Term Care (LTC) services;
• Descriptions of procedures to be followed for emergency or special services;
• The member’s identification number;
• The member’s name (first, last, and middle initial);
• The member’s date of birth;
• The member’s enrollment effective date;
• The member’s PCP;
• Whether the member is enrolled in the Alternative Benefit Plan;
• The member’s State-issued Medicaid identification number. This number is the ten-digit number
supplied to the MCO in the nightly batch of member information sent from HSD; and
• All applicable co-payment amounts.
3.5. Member Advisory Board
The MCO shall convene and facilitate a Member Advisory Board and adhere to all requirements below.
Member Advisory Board members shall serve to advise the MCO on issues concerning service delivery
and quality of all Covered Services (e.g., BH, PH and LTC), Member rights and responsibilities, resolution

Section 3: Member Education
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
36 | P a g e
of Member Grievances and Appeals and the needs of groups represented by Member Advisory Board
members as they pertain to Medicaid.
The Member Advisory Board shall consist of members (with representation of all Medicaid populations
enrolled in the MCO), family members, and providers. The MCO shall have an equitable representation
of its members in terms of race, gender, special populations, and New Mexico’s geographic areas.
The MCO’s Member Advisory Board shall keep a written record of all attempts to invite and include its
members in its meetings. The Member Advisory Board roster and minutes shall be made available to
HSD 10 calendar days following the meeting date.
The MCO shall hold quarterly, centrally-located Member Advisory Board meetings throughout the term
of the Agreement. The MCO shall advise HSD 10 calendar days in advance of meetings to be held.
In addition to the quarterly meetings, the MCO shall hold at least two additional statewide Member
Advisory Board meetings each contract year that focus on member issues to ensure members’ issues
and concerns are heard and addressed. Attendance rosters and minutes for these two statewide
meetings shall be made available to HSD within 10 calendar days following the meeting date.
The MCO shall ensure all Member Advisory Board members actively participate in deliberations and that
no one Board member dominates proceedings in order to foster an inclusive meeting environment.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
37 | P a g e
4. Care Coordination
4.1. General Information
The MCO, through implementation of its policies and procedures, will develop a comprehensive program
for continuous monitoring of the effectiveness of its care coordination processes. The policies and
procedures will include the staff responsible for the monitoring, how the monitoring will be done, as
well as the frequency of the oversight. Care Coordination strategies will be analyzed for effectiveness
and appropriate changes made. Any issues or concerns will be addressed immediately.
4.2. Care Coordination Functions
The following primary care coordination functions are requirements for care coordination that must be
performed by staff employed by the MCO.
• Conducting Health Risk Assessments (HRAs) for members newly enrolled in Centennial Care or
members who have had a change in condition and who are not currently identified for Care
Coordination Level 2 or 3 services;
• Conducting Comprehensive Needs Assessments (CNAs) initially, semi-annually or annually;
• Administer the Community Benefit Service Questionnaire (CBSQ) as applicable (see Section
4.5 CBSQ);
• Semi-annual or quarterly in-person visits with the member;
• Quarterly or monthly telephone contact with the member;
• Comprehensive Care Plan (CCP) development and updates; and
• Targeted Health Education, including disease management, based on the member’s individual
diagnosis (as determined by the CNA).
MCOs may delegate care coordination functions in the following instances:
• MCOs that own and operate patient-centered medical homes (PCMHs) as part of their provider
network may delegate to such PCMHs, provided the PCMH Care Coordinator is employed by the
MCO;
• MCOs may delegate all primary care coordination functions to a designated Section 2703 Health
Home, provided the Health Home is determined ready by the Health Home Steering Committee to
perform such functions;

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
38 | P a g e
• MCOs may fully delegate care coordination to providers/health systems in a value-based purchasing
(VBP) arrangement that outlines a payment arrangement for the full delegation of Care
Coordination and other requirements associated with improving quality and health outcomes;
and/or
• MCOs may delegate the HRA, CNA, care coordination touch points with high need members,
coordination of referrals, linking Members to community services, and locating and engaging with
Unreachable and Difficult to Engage Members as part of the Shared Function Model with entities or
individuals for a mutually-agreed upon reimbursement rate.
The MCOs may not delegate the NF level of care (LOC) assessment and may not delegate care
coordination for members who are in the SDCB model.
The MCO, through its care coordination monitoring of MCO staff and care coordination delegates, will
ensure, at a minimum:
• The care coordination tools and protocols are consistently and objectively applied and outcomes are
continuously measured (frequency and methodology stated in the policies and procedures such as
inter-rater reliability) to determine effectiveness and appropriateness of processes.
• Competencies will be evaluated in the following areas, but not limited to:
o LOC assessments and reassessments occur on schedule in compliance with the Agreement and
are submitted to the lead or supervising Care Coordinator;
o CNAs and reassessments, as applicable, occur on schedule in compliance with the contract;
o Care plans are developed and updated on schedule in compliance with the Agreement;
o Care plans reflect needs identified in the CNA and reassessment process;
o Care plan goals are member-centric, and agreed-upon by the member;
o Care plans are appropriate and adequate to address the member’s needs including the need for
all Community Benefit (CB) services;
o Services are delivered as described in the care plan and authorized by the MCO;
o Services are appropriate to address the member’s needs; including culturally responsive
treatments and supports to Native American children and youth in CYFD Protective Services (PS)
custody;
o Services are delivered;
o Service utilization is appropriate;
o Service gaps are identified and addressed;

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
39 | P a g e
o Minimum Care Coordinator contacts are conducted;
o Care Coordinator-to-member ratios are appropriate;
o Service limits are monitored (as described in the policies and procedures) and appropriate
action is taken if a member is nearing or exceeds a service limit; and
o CBSQ is administered as appropriate.
• The MCO, or its delegate, will use an electronic case management system that includes the
functionality to ensure compliance with all requirements specified in the 1115(a) Waiver, Federal
and State statutes, regulations, the Agreement and the MCO’s policies and procedures. The
functionality will include but not be limited to the ability to:
o Capture and track enrollment dates, date of development of the care plan, date of authorization
of the care plan, date of initial service delivery for each service in the care plan, date of each LOC
and needs reassessment, date of each update to the care plan, and dates regarding transition
from an institutional facility to the community;
o Capture care coordination level assignments and track compliance with minimum care
coordination contacts as specified in the Agreement;
o Notify the Care Coordinator of eligibility end date, date for annual LOC reassessment, date of
comprehensive needs reassessment, and date to update the care plan;
o Capture and track eligibility/enrollment information, LOC assessments and reassessments, and
needs assessments and reassessments;
o Capture and monitor the care plan;
o Track requested and approved service authorizations, including Covered Services and VAS, as
applicable;
o Document all referrals received by the Care Coordinator on behalf of the member for Covered
Services and VAS, as applicable, needed in order to ensure the member’s health, safety and
welfare, and to delay or prevent the need for more expensive institutional placement. Include
notes regarding how such a referral was handled by the Care Coordinator, including any
additional follow up;
o Establish a schedule of services for each member identifying the time that each service is
needed and the amount, frequency, duration and scope of each service;
o Track service delivery against authorized services and providers;
o Track actions taken by the Care Coordinator to immediately address service gaps;

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
40 | P a g e
o Document case notes relevant to the provision of care coordination; and
o Allow HSD or its designee to have remote access to case files.
4.3. Health Risk Assessment
The MCO or its delegate shall conduct HSD standardized HRAs on all members who are newly enrolled in
Centennial Care for the purpose of: introducing the MCO to the member, obtaining basic health and
demographic information about the member, and confirming the need for a CNA to determine if the
member should be assigned to care coordination level 2 or level 3. The MCO may assign a member for
care coordination without completion of a CNA, provided they obtain HSD approval in advance of the
level assignment.
The standardized HRA (Section 4.15.1.) will be completed for each new Centennial Care member within
30 calendar days of the member’s enrollment in the MCO. Additionally, an HRA will be completed upon
a change in the member’s health condition if the member is not in care coordination level 2 or level 3.
The HRA may be conducted by telephone, in person, or as otherwise approved by HSD; HRA information
must be obtained from the member or the AR and must be documented in the member’s file. The MCO
shall ensure its staff, subcontractors, or vendor(s) conducting the HRA are adequately trained to
effectively conduct the HSD standardized HRA.
The MCO or its delegate will make reasonable efforts to contact members to conduct an HRA and
provide information about care coordination. Such efforts shall include, but not be limited to, engaging
community supports such as Community Health Workers (CHWs), Community Health Representatives
(CHRs), Core Service Agencies (CSAs), 1915 (c) HCBS Waiver Case Managers and Consultants, New
Mexico Brain Injury Resource Center, and Centers for Independent Living. For CYFD protective services
(PS) and/or juvenile justice services (JJS) involved children/youth, the MCO or its delegate will
collaborate with the assigned CYFD permanency placement worker (PPW), juvenile probation officer
(JPO), and community behavioral health clinician (CBHC) for physical and behavioral health services. The
MCO or its delegate shall document at least three attempts to contact a member which includes at least
one attempt to contact the member at the most recently reported phone number. The three attempts
shall be followed by a letter sent to the member's most recently reported address that provides
information about care coordination and how to obtain an HRA. Documentation of the three attempts
shall be included in the member’s file. Such attempts shall occur on not less than three different
calendar days, at different hours of the day, including day and evening hours and after business hours.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
41 | P a g e
After these attempts have been made and documented, and if the member has not been engaged, the
member is categorized as “Unreachable” and is not assigned to care coordination level 2 or level 3. The
MCO will conduct quarterly claims mining for these members and will renew attempts to reach the
member if claims indicate a possible need for care coordination.
If the MCO has made three documented attempts to contact and has reached the member at least once,
but the member fails to engage with the completion of the HRA or CNA, the member is categorized as
“Difficult to Engage” (DTE) and is not assigned a care coordination level 2 or level 3. If the member is
categorized as a care coordination level 2 or level 3 based on the most recent CNA but fails to engage in
two consecutive contract required touch points (telephonic or in person), the member is then
categorized as DTE, with appropriate documentation in the member’s file. The MCO will perform
quarterly claims mining for these Members and will renew attempts to reach Members if claims mining
indicates a possible need for care coordination.
The HSD standardized HRA includes the following information:
• Member demographics
o Member name, address, telephone number, date of birth;
o Member Medicaid number;
o Names and relationship of person(s) completing form (other than member);
o Emergency contact and telephone number;
o HRA date; and
o Assessment Method and Type.
• Member Health Information
o Language preference, translation needs, and special preferences (cultural, religious, physical);
o Main health concern;
o Current or past PH and BH conditions or diagnoses, including brain injury;
o Pending PH or BH procedures;
o Most recent physical examination and/or recent medical appointment;
o Emergency room visits, including reason, number of visits and dates of visit(s);
o Number of hospital stays in past 6 months, and any readmissions;
o Indication of a 1915(c) waiver LOC assessment;
o Number of medications;
o Living situation;

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
42 | P a g e
o Assistance with two or more activities of daily living (ADL) and type of need;
o Interest in and need for LTC services;
o Advance directives preference and interest in receiving information; and
o Interest in receiving care coordination.
The MCO or its delegate shall provide the following information to every member during his or her HRA:
• The purpose of care coordination;
• The care coordination levels (CCLs);
• Notification of the member’s right to request a higher CCL;
• For Native American members, the right to have a Native American Care Coordinator;
• Requirement for an in-person CNA for the purpose of providing services associated with CCL2 or
CCL3; and
• Specific next steps for the member.
Within seven calendar days of completion of the HRA, all members shall be informed of the need for a
CNA. MCOs may request to add additional questions to the HRA to meet the requirements of regulatory
and accrediting bodies by submitting the additional questions and the reason(s) for inclusion for State
approval. Requests must be sent for approval to HSD/MAD through the MCO’s Contract Manager to the
attention of the Quality Bureau Care Coordination Unit (CCU).
The HRA and the CNA may be performed concurrently.
4.4. Comprehensive Needs Assessment
A CNA is conducted for Medicaid members eligible for managed care who are identified through the
HRA as having significant health conditions and risk indicators signifying the potential need for CCL2 or
CCL3. The MCO shall schedule a CNA within 14 calendar days of completion of the HRA and complete
the CNA within 30 calendar days of completion of the HRA unless the member is in a model approved
for delegated care coordination functions with other State-approved guidelines.
Members who are identified as not needing a CNA shall be monitored by the MCO care coordination
unit quarterly through predictive modeling software and available utilization and claims data to
determine if the member had a change in health status and is in need of an HRA or CNA.
For members who reside in a NF, rather than conduct a CNA, the MCO shall ensure the Minimum Data
Set (MDS) is completed and collect supplemental information related to BH needs and the member's
interest in receiving CB services.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
43 | P a g e
For members who have indicators that may warrant a NF LOC, the MCO Care Coordinator shall conduct
an in person, in home CNA at the member’s primary residence. The MCO shall use the New Mexico
Medicaid NF LOC Criteria and Instructions to determine NF LOC for members.
The CNA is the sole responsibility of the MCO Care Coordinator unless delegated to another entity via a
Shared or Full Delegation Model.
CNAs must be performed through the utilization of an assessment tool that has been approved by HSD
for assessing the member’s medical/PH, BH, LTC, and social needs. The assessment tool may include the
identification of targeted needs related to improving health, functional outcomes, or quality of life
outcomes (e.g., related to targeted health education, pharmacy management, or increasing and/or
maintaining functional abilities, including provision of covered services). Any changes to the assessment
tool must be approved by HSD 30 calendar days prior to use by the MCO or its delegate.
The CNA must be conducted in the member’s primary place of residence or facility for members
reintegrating back into the community. The MCO or its delegate will involve collateral respondents
when scheduling the CNA, including family members, caregivers, CHRs, CHWs, and/or other significant
social support individuals, with the consent of the member. For CYFD PS and/or JJS involved
children/youth, the MCO or its delegate will collaborate with the assigned CYFD permanency placement
worker (PPW), juvenile probation officer (JPO), and community behavioral health clinician (CBHC) for all
medically necessary services including behavioral health services. The MCO or its delegate must
evaluate the need for translation, including signing or communication boards when scheduling the CNA.
CNAs must be conducted face-to-face with the member and collateral parties in the home, unless an
exception has been granted by HSD. Home setting is defined as the primary residence for the member in
the community where there is an identifiable address, and the member is residing for an established
period of time for shelter, safety, physical assistance, recovery, legal requirements, or treatment
services.
The CNA may be conducted without requesting an exception from the State under the following
conditions:
• If the member is homeless, or in a transition home or youth shelter and the assessment can be
conducted in a private setting at a location, mutually agreeable to the member, such as a church
meal site program, community non-profit organization center, community MH agency, food bank
site, etc.;
• If the member is currently part of the jail-involved population preparing for release; or

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
44 | P a g e
• If the Member is in a Health Home or being served by a provider approved for a Full Care
Coordination Delegation Model.
Other requests for exceptions to the CNA face-to-face or in the member’s home setting requirements
must be made directly to HSD by the MCO using the following process:
• Complete the Centennial Care CNA Exception Request form (MAD 601);
• Alternate locations must be submitted to HSD for review and should be assessed for privacy to
ensure the member’s Protected Health Information (PHI) is not jeopardized;
• Send the completed MAD 601 by secure email to: HSD-QB-CCU-CNA@state.nm.us;
• HSD will review the request and respond to the specific MCO requestor within two business days;
• If an exception is approved, it shall only be valid for six months, or until the next CNA is needed,
whichever comes first; and
• Requests will not be reviewed or approved if submitted:
o Via unsecure email;
o To an email address other than HSD-QB-CCU-CNA@state.nm.us; and
o Via any format other than the MAD 601 Form.
All efforts must be made to negotiate with and educate the member about the importance of
participating in the completion of a CNA. The MCO or its delegate must provide documentation of
further negotiations with the member and/or legal representatives when refusal by the member is
articulated.
CNAs are considered to be best practice and valid when conducted in the home setting. The home
setting must be evaluated for health, welfare, and safety of the member. The CNA, when conducted
with the member in his/her home, includes determination of: any structural problems for member’s
mobility access; need for safety enhancements, such as smoke detectors, fire extinguishers, ramps,
guard rails, and bathroom equipment; fall prevention concerns such as throw rugs; doorway access for
wheelchairs; plumbing and electricity issues; nutritional concerns such as no food resources or
food/beverage items identified as being beyond expiration dates; and other structural damages such as
mold, broken windows, entry doors without locks, broken flooring. Additional areas of considerations
include assessing for rodent/pest infestation, fire hazards due to electrical wiring issues and
clutter/hoarding, as well as outdoor hazards due to overgrown weeds and undergrowth of yards/trees.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
45 | P a g e
The practice of conducting in home CNAs further allows for observation of the existence of other parties
living in the home and possibly presenting support or risk to the member.
When a member, currently categorized as a CCL2 or a CCL3, refuses to participate with a CNA, the MCO
will make every effort to discuss the benefits of the needs assessment with the member, emphasizing
this assessment makes the determination of useful resources to meet the member’s needs, such as the
CB for personal care assistance, special home environment modifications and adaptive equipment. The
MCO will ensure the member signs the HSD-approved care coordination declination form and maintain
the signed form in the member’s file. If the member refuses to sign the care coordination declination
form, the MCO shall document such refusal in the member’s record. The MCO will perform quarterly
claims mining for these members and will renew attempts to reach the member if claims mining
indicates a possible need for care coordination. The member who has refused care coordination will not
be assigned to care coordination level 2 or level 3. In documented refusal circumstances, the MCO will
submit a proposal to the member outlining a basic care plan with minimum services outlined and
suspend any requests for increased services/personal care hours until a CNA and NF LOC is conducted
and completed.
At a minimum, the CNA shall:
• Assess PH and BH needs, including but not limited to: current diagnoses; history of significant PH
and BH events, including hospitalizations and emergency room visits; complete placement history
for children and youth in CYFD PS custody; medications; allergies; providers involved in member’s
care; DME; brief substance abuse screening questionnaire, as approved by HSD/BHSD and history;
family medical and BH (MH and substance use/abuse) history; cognitive capacities, (including
evaluation of alertness, orientation, history of head/brain injury); health-related lifestyle (smoking,
food intake/nutrition, sleep patterns, exercise, continence); and functional abilities, including ADLs
(mobility, grooming, bathing, eating, dressing, and medications) and instrumental activities of daily
living (IADLs)(i.e., money management, meal preparation, housekeeping/cleaning, emergency
awareness and preparedness, and grocery shopping).
• Assess LTC needs including but not limited to: environmental safety including items such as smoke
detectors; pests/infestation; trip and fall dangers; and adaptive needs such as ramps or other
mobility assistance. If the member is eligible for the CB, the MCO shall assess for all CB services.
• Include a risk assessment, using a tool and protocol approved by HSD, as applicable. A risk
agreement that shall be signed by the member or his/her representative that shall include:

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
46 | P a g e
identified risks to the member; the consequences of such risks; strategies to mitigate the identified
risks; and the member’s decision regarding his/her acceptance of risk.
• Assess disease management needs, including: identification of disease state; need for targeted
intervention and education; and development of appropriate intervention strategies.
• Determine a social profile including, but not limited to: living arrangements; natural and social
support systems which are available to assist the member; Individualized Planning Meeting Plans for
children and youth in CYFD PS custody; demographics; transportation; employment; financial
resources and challenges (other insurance, food, utilities, housing expenses); Medicare services;
other community services being accessed, such as senior companion services, meals-on-wheels,
etc.; living environment (related to health and safety); Individualized Education Plan; and
Individualized Service Plans for Developmental Disabilities, Medically Fragile (MF), or Mi Via Waiver
Program recipients, (if applicable). A copy of the HCBS Waiver Prior Authorization or budget is not
required to be obtained by the Care Coordinator.
• Identify possible suicidal and/or homicidal thinking, planning/intent and lethality risk, history of
aggressive and/or violent behaviors, history of running away and wandering for both adults and
children.
• Identify cultural information, including language and translation needs and utilization of ceremonial
or natural healing techniques.
• Ask the member for a self-assessment regarding their viewpoint of their condition(s) and service
needs.
• In the event the member is a minor under the age of 18, or is a youth in CYFD PS custody, identify
the parent or legal guardian participating in and/or responding for the minor during assessment.
• For members on the DD, Mi Via, or MF Waivers (categories of eligibility [COEs] 095 and 096) and as
applicable to the member’s living arrangement, identify the parent, family member or legal guardian
participating in and/or responding for the member during the assessment.
• In the event the member is receiving the Alternative Benefit Plan (ABP) and meets the definition and
criteria of Medically Frail or is otherwise ABP Exempt, notify the member that he/she may be
exempt, explain the difference in benefits and facilitate his/her transition to the ABP Exempt benefit
package at the member’s choice.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
47 | P a g e
4.5. Community Benefit Service Questionnaire
As part of the CNA process, MCO Care Coordinators must administer the CBSQ. The CBSQ/CBMA will be
administered as part of the CNA, at the beginning of the CNA. The CBSQ assists the Care Coordinator in
discussing all available CB services with the member, and the Community Benefit Member Agreement
(CBMA) elicits the member’s participation in identifying risks. The CBMA is not used to document the
member’s refusal to complete a CBSQ.
The completed CBSQ and the CBMA are considered part of the member’s CNA. The MCOs must ensure
all Care Coordinators are trained in administering these documents. The MCOs must have a process in
place to monitor that CBSQs and CBMAs are completed correctly and in accordance with Section 4.5 of
the Managed Care Policy Manual.
The CBSQ/CBMA will be administered as part of the CNA, at the beginning of the CNA, for the following
members:
• Allocated members receiving their first CNA, including members who are in the process of
community reintegration from a NF and members who lost their full Medicaid Category of Eligibility
(COE) and are being allocated for continuity of care.
• Annually for members with a current NF LOC (see note about CCL3 members below).
• Full Medicaid members without a NF LOC who request CB services.
• Full Medicaid members without a NF LOC who have not requested CB services but appear to meet
NF LOC criteria prior to or during the CNA. MCOs must attempt to determine this through claims
data or other information obtained prior to the member’s CNA including the functional needs
identified in the HRA.
The CBSQ/CBMA will not be administered for the following members:
• Members who have not previously met a NF LOC and who are not requesting CB at the time of the
CNA.
• Members who may meet a NF LOC for a short period of time due to a clinical episode
(e.g., pregnancy).
• Members not being assessed for a NF LOC.
• Members on the DD, Mi Via, or MF Waivers (categories of eligibility [COEs] 095 and 096).

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
48 | P a g e
• Members in a NF (unless in the process of being allocated through community reintegration or
member has a COE (i.e., Supplemental Security Income [SSI]) that deems them eligible to reintegrate
without a waiver allocation).
• Members who decline assessment for NF LOC or refuse CB services. The MCO Care Coordinator
must document the refusal in the member’s record.
• Members who decline care coordination. The declination form must be on file with the MCO. If a
member refuses to sign the care coordination declination form, the contractor shall document such
refusal in the member’s record.
CCL3 members:
• For all members with CCL3 and a NF LOC, the CBSQ/CBMA must be administered at least annually or
more frequently as determined by the Care Coordinator.
• For members with CCL3 but without a NF LOC, follow the criteria above.
In any circumstances not covered by the criteria, the Care Coordinator should use his/her judgment and
consult with his/her supervisor as necessary to determine appropriate use of the CBSQ. Care
Coordinators should use the CBSQ as a tool to guide the discussion with the member and/or the
member’s representative to inform them of the availability of CB services.
HSD will audit CBSQ and CBMA completion to ensure that these requirements are met.
4.6. CNA Reassessments
The CNA shall be conducted at least annually for level 2 care coordination and semi-annually for level 3
care coordination, to determine if the care plan is appropriate for the member and if a higher or lower
LOC coordination may be needed.
Additional CNAs may also be conducted, as the Care Coordinator deems necessary, as requested by the
member, provider, family member or legal representative, or as a result of a change in health status
and/or social support situation including changes in placement for children in CYFD PS custody.
Specific indicators warranting a need for conducting a new CNA may include but are not limited to:
significant changes in member’s medical and/or BH condition (decline or improvements in health
status); changes in setting of care (SOC), such as hospitalization, rehabilitation and/or short-term NF
admission (long-term NF stay(s) require administration of the MDS): residential treatment facility
admission; changes in the member’s family or natural/social support system (such as, sudden illness
and/or convalescence or death of a family caregiver); living arrangement disruption (loss of residence,

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
49 | P a g e
eviction, fire/flooding, move to another family home); involvement of Adult Protective Services (APS),
Child Protective Services, Juvenile Justice Services, Behavioral Health Services and/or other New Mexico
Children, Youth & Family Department (CYFD) interventions; and changes in the amount of caregiver
services requested and requested amount exceeds the range of hours corresponding with member’s
existing assessment score. These events may at times not require a new CNA be completed. If a new
CNA is not conducted, the member’s record should clearly establish why the triggering event did not
result in the MCO conducting a new CNA. The decision can be made via telephone contact or face to
face visit with the member.
4.7. Comprehensive Care Plan Requirements
This policy is in conjunction with all elements described in the CCP Requirements outlined in the
Agreement, which defines the processes for development, implementation and management of a care
plan for all members in levels 2 and 3 of care coordination. The MCO- or HSD-approved designee is
responsible for ensuring a CCP is initiated upon enrollment and must oversee the Care Coordinator who
is responsible for coordinating all services in the CCP.
• CCP Scope and Process. The MCO- or HSD-approved designee must establish a process to ensure
coordination of care for members that includes:
o Coordination of the member’s PH, BH, and long-term health care needs through the
development of the CCP;
o Collaboration with the member, member’s friends and family (at member’s request), member’s
PCP, specialists, BH providers, other providers, communities, and interdisciplinary team experts
including the Individualized Planning Meeting Team for children and youth in CYFD PS custody,
as needed when developing the care plan, including documentation of all attempts to engage
providers and other individuals identified in the development of the care plan;
o With the member’s consent to share information, the care plan should be shared and utilized by
those involved in providing care to the member (e.g., BH providers should be aware and take
into consideration the member’s PH care issues when working with the member); and
o Verification of all decisions made regarding the member’s needs and services, and ensures all
information is documented in a written, CCP.
• CCP Development and Management:

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
50 | P a g e
o The CCP is in a language the member and/or family member can understand. The member shall
lead the person-centered planning process to ensure the CCP is member-centric and agreed
upon by the member;
o The member may designate his/her representative to have a participatory role, as needed, and
as defined by the member, unless the representative has decision making authority, under law;
and
o The MCO or HSD approved designee shall develop the CCP within 14 business days of
completion of the CNA unless the member is in a health home and/or using the Treat First
model of care.
o The Care Coordinator shall:
▪ Ensure the member or member’s legal representative understands, reviews, signs and dates
the CCP.
▪ Provide a copy of the completed CCP to the member, member’s legal representative as
applicable or other providers authorized to deliver care to the member in a format that is
easily readable (e.g., 12 font).
▪ With the member’s and/or parent, legal guardian and/or CYFD worker's (if in CYFD Custody)
consent, confirm family, providers, or any other relevant parties are included in the
treatment and planning of the member’s CCP.
▪ Ensure timelines for the development and implementation and/or update the CCP are met.
▪ Facilitate treatment and coordinate with providers to assist the member and his or her
family and CYFD lead worker (if in CYFD custody) with navigating the system including
scheduling appointments, arranging transportation, or advocating for the member as
needed.
▪ Verify services have been initiated and/or continue to be provided as identified in the CCP
and ensure services continue to meet the member’s needs.
▪ With member’s consent, maintain appropriate, constant communication with community
and natural supports to monitor and support their ongoing participation in the member's
care.
▪ Identify, address, and evaluate service gaps to determine their cause and minimize any gaps
going forward and ensuring back-up plans are implemented and effectively working;

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
51 | P a g e
including strategies for solving conflicts or disagreements, and provide clear
conflict-of-interest guidelines for all planning participants.
▪ Identify and list specific risk factors and changes to member’s risk, address those changes
and update the member’s risk agreement and CCP as necessary to include measures to
minimize the identified risks.
▪ Inform each member of his or her Medicaid eligibility status and end date and assist the
member with the process for eligibility redetermination.
▪ For children and youth in CYFD PS custody, inform Native American children and youth and
their permanency placement worker (PPW) of opportunities to receive culturally responsive
treatments, interventions and supports, including those that are non-medicalized.
▪ Educate members with identified disease management needs by providing specific disease
management interventions and strategies.
▪ Educate the member about his or her ability to have an Advance Directive and ensure the
member’s decision is well documented in the member’s file.
▪ Educate member about non-Medicaid services available as appropriate (e.g., Adult
Substance Abuse Residential Treatment, Detoxification, Home Delivered Meals, and Infant
MH).
▪ Reflect cultural considerations of the member and conduct the CCP process in a manner
that is accessible to individuals with disabilities and persons who are limited English
proficient.
o Required Elements of a CCP include the following:
▪ Pertinent member demographics and enrollment data.
▪ Ensure implementation of interventions and the dates by which the interventions must
occur and identify specific agencies or organizations with which treatment must be
coordinated, including non-Medicaid providers.
▪ Covered medical diagnosis, past treatment, previous or pending surgeries (as applicable),
medications and allergies.
▪ Member’s current status, including present levels of function in physical, BH cognitive,
social, and educational domains.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
52 | P a g e
▪ Member or family, foster family or extended kinship barriers to receiving treatment, such as
a member or family member’s inability to travel to an appointment or for children and
youth in CYFD PS custody who lack access to services in the child’s home community.
▪ Identify the member or family’s, foster family’s, and/or extended kinship/guardian’s
strengths, resources, priorities, and concerns related to achieving mutual recommendations
made in caring for the member.
▪ Services recommended achieve the identified objectives, including provider(s) or person(s)
responsible and timeframes for meeting the member’s desired outcomes.
▪ Identify services provided by natural supports that are scheduled to be enhancers and
back-up (including emergency purposes) to services that are authorized by the MCO.
▪ An interdisciplinary team, with member’s consent, including but not limited to: the Care
Coordinator; social worker; registered nurse (RN); medical director; PCP; and others must be
identified to develop, implement and update the CCP as needed and coordinate with the
Individualized Planning Team for each child or youth in CYFD PS custody.
▪ Reflect the setting in which the individual resides is chosen by the member, and is
integrated in and supports full access of members receiving HCBS, to the greater
community, including opportunities to seek employment and work in competitive
integrated settings, engage in community life, control personal resources, and receive
services in the community to the same degree of access as individuals not receiving
Medicaid HCBS.
▪ Reflect the member’s strengths and preferences.
▪ Identify goals and desired outcomes that reflect the least restrictive, community-based
services and supports (paid and unpaid) that will assist the member to achieve identified
goals, and include who will provide the services and supports.
▪ Identify goals and preferences related to relationships, community participation,
employment, income and savings, health care and wellness, education and others.
▪ Include services and, the purpose or control of which the member elects to self-direct.
▪ Prevent the provision of unnecessary or inappropriate services and supports.
o CCP Revisions
▪ The CCP will be revised when the member experiences one of the following circumstances:

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
53 | P a g e
• Risk of significant harm: within one business day of the MCO receiving notification, the
care coordination team will convene, in person or by teleconference; and if necessary
the care plan will be modified accordingly within 72 hours;
• Major medical change;
• The loss of a primary caregiver or other significant person;
• A serious accident, illness, injury or hospitalization that disrupts the implementation of
the CCP;
• Serious or sudden change in behavior;
• Change in living situation, including out-of-home placements, removal from the home
by CYFD or changes in CYFD placements, and subsequent discharges;
• Proposed change in services or providers (e.g. CB);
• It has been confirmed by APS or CYFD that the member is a victim of abuse, neglect, or
exploitation;
• Any team member requests a meeting to propose changes to the CCP;
• Criminal justice involvement on the part of the member (e.g., arrest, incarceration,
release, probation, parole); or
• As requested by HSD.
▪ Within five business days of completing a reassessment of a member’s needs, the Care
Coordinator shall update the member’s CCP as appropriate, and the MCO or HSD approved
designee shall authorize and initiate services in the updated CCP.
o Ongoing Care Coordination
▪ This policy along with all elements described in Ongoing Care Coordination outlined in the
Agreement, defines how the MCO or HSD approved designee shall perform real time and
ongoing care coordination to ensure all members receive the appropriate care.
▪ Ongoing care coordination functions shall include all elements defined in the Agreement
including the following:
• Identify gaps and address the needs of the member, including develop and/or update
the care plan as needed.
• Ensure when a member’s LOC coordination increases or decreases that continuity of
care is always maintained.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
54 | P a g e
• Maintain a single point of contact for the member to ensure coordination of all services
and monitoring of treatment.
• Maintain face-to-face and telephonic meetings with the member to ensure appropriate
support of the member’s goals and foster independence.
• Coordinate and provide access to specialists, as needed; relevant long-term specialty
providers, relevant emergency resources, relevant rehabilitation therapy services,
relevant non-Medicaid services, etc.
• Education regarding service delivery through Medicare and/or Medicaid.
• Measure and evaluate outcomes designated in the CCP and monitor progress to ensure
covered services are being received and assist in resolution of identified problems.
• Achieve coordination of physical, BH, and LTC services.
• Maintain consistent communication and contact with member’s PCP, specialists, and
other individuals involved in the member’s care. The MCO shall maintain consistent
communication and contact with the assigned CYFD permanency placement worker
(PPW) for protective services involved children and youth, juvenile probation officer
(JPO) for juvenile justice involved youth, and community behavioral health clinician
(CBHC) for CYFD involved children and youth.
• Maintain and monitor the member’s CB and provide assistance with complex services.
• Consider member and provider input to identify opportunities for improvement.
• Collaborate and/or cooperate with representatives of the Independent Consumer
Support System.
4.8. Staffing Requirements and Delegations
The MCO may utilize a care coordination team approach to perform care coordination activities, with
the MCO’s care coordination team consisting of the member’s primary Care Coordinator and other
individuals with relevant expertise and experience appropriate to address the needs of members. While
the MCO may subcontract the HRA activities, the MCO shall ensure its staff, subcontractor(s), or
vendor(s) conducting the HRA are adequately trained to effectively conduct the HSD standardized HRA.
CNAs must be performed by primary Care Coordinators employed by the MCO or its delegate. The MCO
may delegate some care coordination functions to local resources, such as: PCMHs, FQHCs, CHWs, CHRs,

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
55 | P a g e
school-based health centers [SBHCs], Correctional Facilities, CSAs, Paramedicine programs, county
entities, Centers for Independent Living, and Tribal entities. The MCO will implement policies and
procedures that will define and specify the qualifications, experience, and training of each member of
the MCO care coordination team and its delegated Care Coordinators to ensure specific functions are
performed by a qualified Care Coordinator.
Maximum caseload per Care Coordinator, are established by HSD and shall not be exceeded by the
MCO. As the MCO transitions more care coordination functions to the provider level, it will collaborate
with HSD to adjust care coordination caseload requirements. Caseload to Care Coordinator ratios are as
follows:
• CCL2:
o Members not residing in a NF 1:75; and
o Members residing in a NF 1:125.
• CCL3:
o Members not residing in a NF 1:50; and
o Members residing in a NF 1:125.
• Care coordination for members who participate in the self-directed CB:
o CCL2 is 1:75; and
o CCL3 is 1:50.
MCOs or its delegate shall submit, upon request by HSD, a Care Coordination Staffing Plan, which at a
minimum shall specify:
• The number of Care Coordinators, care coordination supervisors, other care coordination team
members the MCO plans to employ;
• The ratio of Care Coordinators to members;
• The MCO’s plans to maintain ratios as outlined by care coordination level and the explanation of the
methodology used for determining such ratios;
• How the MCO will ensure such ratios are sufficient to fulfill the Agreement requirements;
• The roles and responsibilities for each member of the care coordination team;
• A strategy that encourages the use of Native American Care Coordinators and limits duplication of
services between Indian Health Services, Tribal Health Providers, and Urban Indian Providers (I/T/U)
and non-I/T/U providers;

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
56 | P a g e
• How ratios are adjusted to accommodate travel requirements for those Care Coordinators serving
members in rural/frontier areas of the State and/or for those members that require extraordinary
efforts from the assigned Care Coordinator; and
• How the MCO will use Care Coordinators to meet the needs of New Mexico’s unique population.
The MCO or its delegate shall ensure members have a telephone number for direct contact with their
Care Coordinator and/or a member of their care coordination team, (without being routed through
several contact points), during normal business hours (8:00 a.m. – 5:00 p.m. Mountain Standard Time).
When the member’s Care Coordinator or a member of the member’s care coordination team is not
available, the call shall be answered/facilitated by another qualified staff person in the MCO’s or its
delegate’s care coordination unit. Calls requiring immediate attention shall be “warm” transferred
directly to another Care Coordinator, not letting the call go to voice mail. After normal business hours,
calls requiring immediate attention by Care Coordinator shall be handled by the member services line,
as stipulated by Section 4.15.1 of the Agreement.
When Native American members request a Native American Care Coordinator, the MCO must employ or
contract with a Native American Care Coordinator or contract with a CHR to serve as the Care
Coordinator.
The MCO or its delegate must accommodate the member’s requests to change to a different Care
Coordinator if desired and if there is an alternative Care Coordinator available. Such availability may take
into consideration the MCO’s or its delegate’s need to efficiently deliver care coordination in accordance
with the requirements in the Agreement. In ensuring quality and continuity of care the MCO or its
delegate shall make efforts to minimize the number of changes in a member’s Care Coordinator. The
MCO or its delegate may need to initiate change in the following circumstances:
• Assigned Care Coordinator is no longer employed by the MCO or its delegate;
• There is a conflict of interest preventing neutral support for the member;
• Care Coordinator is on temporary leave from employment; or
• Caseload of the assigned Care Coordinator must be adjusted due to its size or intensity.
The MCO or its delegate shall develop policies and procedures regarding notice to members of Care
Coordinator changes initiated by either the MCO or its delegate, or the member, including notice of
planned Care Coordinator changes initiated by the MCO or its delegate.
The MCO or its delegate shall ensure continuity of care when Care Coordinator changes are made. The
MCO or its delegate shall demonstrate use of best practices by encouraging newly assigned Care

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
57 | P a g e
Coordinators to attend a face-to-face transition visit with the member and the out-going Care
Coordinator, when possible, and include documentation of such transition in the member’s file.
Initial training shall be provided by the MCO or its delegate to newly hired Care Coordinators and
ongoing training provided at least annually to all Care Coordinators. Involvement of New Mexico Tribes
as training instructors should be utilized where appropriate.
4.9. Engagement of Members
HSD recognizes there may be a select few managed care members who present challenges to the service
delivery system due to the complexity of their needs. This policy is designed for members who
demonstrate inappropriate behaviors and/or frequent contact of State and MCO staff, and/or have been
unresponsive to traditional care coordination efforts and noncompliant with recommended BH services.
This group of “high health risk/high resource utilization” (HHR/HRU) is different than other populations
and individuals in the care system because denying or delaying care to them has significant immediate
negative consequences to their health and safety. The risk to the individual can be documented in
assessments, contact notes, and care plans. Responding to the challenges presented by this category of
members requires monitoring of attempted delivery of care, documenting interactions, and thresholds
of behavior or conditions that escalate events to a higher level of response and identifying appropriate
teams to design and implement responses. Consistent, well-crafted responses to concerns are essential
when providing care or addressing resistance to care. This will minimize excessive use of State, MCO, and
provider resources, as well as minimizing risk to the individual’s health and safety.
The following protocol is to be utilized across MCOs, agency providers, and State employees and
programs for each recipient identified as part of the HHR/HRU population. The expected result is a more
efficient use of resources to achieve an optimal outcome for the individual. This is intended to free time
and energy to manage all complex individuals in the care system and to achieve optimal levels of health
and safety for all individuals.
Intervention Procedures/Policies: Care delivery literature recommends the use of behavioral contractual
agreements with members so all parties agree on appropriate responses in a non-compliant care
situation. The State may partner with MCOs to make this intervention consistent for all MCOs and all
individuals identified as HHR/HRU.
At the threshold of risk agreed upon by the MCO, a meeting is arranged with the individual and
appropriate recipients of the care team. For CYFD involved clients, include the CYFD community

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
58 | P a g e
behavioral health clinician (CBHC) and the child’s PPW. This team must include the Care Coordinator, a
management level staff of the MCO and a high-level clinical staff member of the MCO. The member may
request one or two people to be in attendance. The intention of the meeting with the participant is to:
• Establish/discuss optimal outcome for health and safety;
• Identify the issues interfering with optimal health and safety outcomes;
• Clarify roles for each member of the team;
• Clarify rules of engagement (who can call whom and when, etc.) and program regulations;
• Assign tasks to each team member with timeline;
• Sign agreement that documents the discussion and assignment of tasks and holds each member
accountable;
• Schedule 2nd meeting within two weeks. Second meeting is a final meeting. Review tasks.
Discuss/establish consequences of any failure to deliver on tasks. Sign contract/care plan. (Includes
updates weekly and addressing ongoing/emergent issues at a bi-monthly meeting.)
• Schedule updates between participants, MCO staff on a regular basis; and
• Ensure maintenance of documentation is with MCO, participant, and natural supports.
When HHR/HRU recipients are identified, the MCOs will designate one point of contact and communicate
that point of contact to HSD/MAD and other involved individuals. If the identified recipient calls
HSD/MAD or other agencies, the individual will be referred back to the MCO point of contact.
If the process outlined above does not provide resolution, the MCOs will utilize their complex case team
and complex case rounds protocol.
4.10. MCO Care Coordination with 1915(c) HCBS Waivers: Developmental Disabilities (DD), Mia Via, and
Medically Fragile (MF) Waivers
The MCOs provide acute and ancillary medical and BH services to the 1915 (c) HCBS recipients/MCO
members. The MCO is responsible for ensuring a CCP is initiated upon enrollment and assigning a Care
Coordinator for coordinating all services in the MCO CCP. The MCOs are required to perform all care
coordination functions described in this Manual section including but not limited to: capturing the
member’s medical, BH, and ancillary needs; explaining to the member, family, and/or guardian, the
Medicaid benefits that are available from the MCO, and how the MCO care coordinator can assist with
coordinating services with the case manager or consultant; developing a CCP; and completing all

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
59 | P a g e
required touch points identified by the member’s current care coordination level. Exceptions to care
coordination functions are specifically described below for members receiving 1915(c) HCBS waiver
services.
4.11. Overview of Medicaid 1915(c) HCBS Waiver Programs
• Developmental Disabilities Waiver (DDW) Program
The DDW provides an array of HCBS to help individuals with developmental and/or intellectual
disabilities to remain in their homes and communities as opposed to institutional care, become
more independent, and reach their personal goals. The DDW serves individuals who meet an
Intermediate Care Facility for Individuals with Intellectual Disabilities (ICF-IID) LOC. DDW individuals
have a Medicaid Category of Eligibility (COE) 096.
The DDW provides the following HCBS: behavior support consultation; case management;
community integrated employment services; customized community supports; customized IHS;
crisis support; environmental modification; independent living transition service; intensive medical
living supports; living supports; non-medical transportation; nutritional counseling; personal support
technology; preliminary risk screening and consultation related to inappropriate sexual behavior;
adult nursing; respite; socialization and sexuality education; supplemental dental care; and skilled
therapies. DDW services are supplementary to early periodic screening, diagnostic, and treatment
(EPSDT) benefits for recipients under the age of 21.
DDW services and budgets are outlined in the recipient's Individual Service Plan (ISP). The ISP is
developed through a person-centered planning process which allows recipients to select services
that will help them achieve personally defined outcomes in the most integrated community setting.
The ISP is created by the DDW recipient with the assistance of their DDW case manager and the
DDW Interdisciplinary team (IDT). The DDW case manager provides information, support, guidance,
and assistance to recipients during the Medicaid eligibility process and afterwards during the ISP
development. The IDT serves to help the recipient identify supports, services and goods that meet
their need for DDW services and are specific to the recipient’s qualifying condition.
• Mi Via Self-Directed Waiver Program
Mi Via is the State of New Mexico’s self-directed waiver program serving individuals who meet an
ICF-IID LOC. Medicaid members served through the Mi Via waiver are referred to as “participants”.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
60 | P a g e
Mi Via participants are identified with either COE 095 Medically Fragile or COE 096 Developmental
Disability and a Setting of Care (SOC) of “MIV”. The goal of Mi Via is to provide home and
community-based alternatives that facilitate greater participant choice and control over the types of
services and supports they receive. It is important to distinguish that Mi Via is a self-directed waiver
program that is operated separately from the Centennial Care Self-Directed Community Benefit
(SDCB) Program.
Mi Via provides the following services: consultant/support guide services; behavior support
consultation; community direct support; customized community supports; in-home living supports;
emergency response network; Employment Supports services; environmental modification services;
Home Health Aide; homemaker/direct support services; nutritional counseling; personal plan
facilitation; private duty nursing for adults; respite; skilled therapies for adults; specialized therapies;
related goods; and non-medical transportation. Mi Via services are supplementary to EPSDT benefits
for participants under the age of 21 years old.
Mi Via waiver services and budget are outlined in the participant's Service and Support Plan (SSP).
The SSPs are developed through a person-centered planning process which allows participants to
select services that will help them achieve personally defined outcomes in the most integrated
community setting. The SSP is created by the Mi Via participant with the assistance of their
consultant. Consultants provide information, support, guidance, and assistance to participants
during the Medicaid eligibility process and afterwards during SSP development. Consultants serve to
help the participant identify supports, services, and goods that meet their need for Mi Via waiver
services and are specific to the participant’s qualifying condition. The level of support a consultant
provides is unique to the individual participant and their ability to self-direct in the Mi Via program.
• Medically Fragile Waiver (MFW) Program
The MFW serves individuals who have been diagnosed with an MF condition defined as a life
threatening, chronic condition which results in a prolonged dependency on skilled nursing care at
home. MFW individuals have a Medicaid COE 095. MFW recipients meet an ICF/IID LOC, as well as
established MF parameters.
The MFW provides the following HCBS: RN case management; private duty nursing (RN, licensed
practical nurse [LPN]); home health aide; behavior support consultation; respite care; nutritional
counseling; skilled therapies (physical, occupational, and speech) for adults; environmental

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
61 | P a g e
modifications; and specialized medical equipment. MFW services are supplementary to EPSDT
benefits for recipients under the age of 21.
The UNM Health Sciences Center, Center for Development and Disability has a Medically Fragile
Case Management Program (MFCMP) that currently provides RN/case management services to both
MF waiver and non-waiver (EPSDT) MF persons statewide. Case managers from the UNM/MFCMP
assess the recipient for MF parameters, compile the MFW LOC forms, and submit the MFW LOC
packet to the Medicaid Third Party Assessor (TPA) for an ICF/IID LOC determination. Case Managers
also create the MFW recipient’s ISP that includes services and budget amounts determined by the
LOC.
4.12. MCO Care Coordination Activities and the 1915(c) HCBS Waivers Service Plan (ISP or SSP)
• Members who transition from Community Benefits to a 1915 (c) HCBS Waiver
o Coordination between the MCO and 1915 (c) Waiver program must be coordinated to avoid
gaps in home and community-based services (i.e. Community Benefits and 1915 (c) Waiver)
during the transition.
o The MCO Care Coordinator shall work proactively with the member and member’s 1915 (c)
case manager/consultant to coordinate the transition dates for the member to move
seamlessly from Community Benefits to the 1915 (c) waiver service plan.
• Members in the DD Waiver program
o The MCO Care Coordinator shall request a copy of the approved DDW LOC packet,
consisting of the Intermediate Care Facility for Individuals with Intellectual Disabilities
(ICF/IID) abstract (MAD 378 form) and related waiver assessments from the Medicaid TPA
for the purpose of obtaining a complete, comprehensive picture of the recipient and their
needs.
o A Client Information Update (CIU) form/MAD 054 is faxed to the TPA to request the LOC
packet.
o The MCO Care Coordinator cannot make changes to the member’s DDW ISP and Budget.
o The MCO will not complete a NF LOC on members enrolled in the DD 1915 (c) waiver, unless
the member is transitioning from the community to a nursing facility for long-term care
permanent placement. The MCO shall inform the member’s DDW case manager in the event
of a NF long-term permanent placement.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
62 | P a g e
o The MCO will utilize the DDW LOC and CIA information obtained from the Medicaid TPA to
complete certain portions of the CNA prior to initiating a visit with the member.
o The MCO Care Coordinator shall have knowledge that while the MCO is responsible for
annual CNA visits, the DD waiver case manager assists the member with the DD waiver LOC
assessment process and ISP and Budget development. The MCO Care Coordinator shall
utilize only the PH and BH portion of the MCO’s CCP for members who are receiving HCBS
through the DD waiver.
• MCO members in the Mi Via Self-Directed Waiver Program
o The MCO Care Coordinator shall request a copy of the approved Mi Via LOC packet,
consisting of the abstract (MAD 378 form) and related assessments from the TPA for the
purpose of obtaining a complete, comprehensive picture of the participant and their needs.
o A CIU/MAD 054 form is faxed to the Medicaid TPA to request the LOC abstract and CIA.
o The MCO Care Coordinator cannot make changes to the member’s Mi Via SSP and Budget.
o The MCO will not complete a NF LOC on members enrolled in the Mi Via 1915 (c) Waiver,
unless the member is transitioning from the community to a nursing facility for long-term
care permanent placement. The MCO shall inform the member’s Mi Via consultant in the
event of a NF long-term permanent placement.
o The MCO Care Coordinator will utilize the LOC and CIA information obtained from the
Medicaid TPA to complete certain portions of the CNA prior to initiating a visit with the
member.
o The MCO Care Coordinator shall have knowledge that while the MCO is responsible for the
annual CNA visits, the consultant assists the participant with the annual Mi Via waiver LOC
assessment process (which requires the TPA to conduct an in-home assessment of
long-term HCBS needs). The MCO and consultant are encouraged to coordinate the CNA
visits and LOC in-home assessment at the same time in order to reduce the burden to the
participant/member and the participant’s family.
o The MCO Care Coordinator shall utilize only the PH and BH portion of the MCO’s CCP for
members who are receiving HCBS through the Mi Via waiver.
• MCO Members in the MFW Program
o The MCO Care Coordinator shall request a copy of the approved MFW LOC packet and ISP
packet from the MFW case management agency prior to the completion of the CNA. The

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
63 | P a g e
MCO will utilize the LOC and ISP information to complete as much of the CNA as possible
prior to the visit.
o The MCO shall ensure the MFW ISP serves as the CCP for the MF member.
o The MCO shall work with the MFW case management agency to coordinate MFW LOC
assessments and/or CNA visits at the same time in order to reduce the burden on these
families.
o The MCO will not complete an NF LOC on members enrolled in the MF 1915(c) Waiver,
unless the member is transitioning from the community to a nursing facility for long-term
care permanent placement. The MCO shall inform the member’s MFW case manager in the
event of a NF long-term permanent placement.
o Not be required to conduct a monthly/quarterly face-to-face or telephonic contact for the
MF members. The MFW case management agency will conduct monthly visits and provide
the MCO with copies of the visit notes. The MCO will review the visit notes monthly and
update the CNA as needed.
o Conduct the required annual in person visit and CNA for MF members.
o Utilize the MFW ISP as the CCP for the MFW recipient.
4.13. MCO Care Coordination Activities for MF EPSDT (Non-Waiver) Members Case Managed by the MFW
Case Management Agency
The MCOs are contracted with the MFW case management agency to continue to provide RN/case
management services for those individuals (non-waiver) who meet the MF criteria. The same MF
parameters are utilized for non-waiver members.
For MF EPSDT (non-waiver) clients, the MCO Care Coordinator shall:
• Request a copy of the approved MF ISP from the MFW case management agency prior to the
completion of the CNA. The MCO will utilize the information in the ISP to complete as much of the
CNA as possible prior to the annual visit.
• Not complete a NF LOC assessment on MF EPSDT members.
• Ensure the MF ISP serves as the CCP for the MF member.
• Work with the MFW case management agency to coordinate the CNA in-person visits at the same
time in order to reduce the burden on these MF members and families.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
64 | P a g e
• Not be required to conduct a monthly/quarterly face-to-face or telephonic contact for the MF
members. The MFW case management agency will conduct monthly visits or phone conference calls
with the MCO Care Coordinator and provide the MCO with copies of the visit notes. The MCO will
review the visit notes monthly and update the CCP as needed.
• Conduct the required annual in-person visit and CNA for MF members.
4.14. Transitions from the HSD Non-Medicaid Brain Injury Services Fund to a Centennial Care MCO
The HSD Brain Injury Services Fund (BISF) offers short-term non-Medicaid services to individuals with a
confirmed diagnosis of brain injury, either traumatic brain injury (TBI) or other acquired brain injury.
The MCO shall implement policies and procedures for ensuring members with brain injury transition
from the BISF into benefits and services that are covered under the MCO. The MCO will follow all care
coordination requirements as applicable. The MCO may contact the HSD BISF service coordination
contractor to verify the status of a member’s BISF eligibility. Upon enrollment with the MCO, all BISF
service coordination requirements transfer to the MCO. At a minimum, the following must be
addressed:
• The MCO shall maintain ongoing communication, enlist the involvement of, and coordinate with
BISF service coordinators to affect the full transition of the member’s care from the BISF to the
MCO.
o The HRA shall include questions about specific health diagnoses, including brain injury.
o For members who identify as having brain injury during the HRA, opportunity shall be given to
reschedule the HRA when natural supports and advocates, including a BISF service coordinator
can be presented. During any HRA, information shall be requested by the reviewer about the
member’s specific needs and what services were assessed as needed through the BISF or its
currently contracted providers.
o An HRA containing information about a self-reported brain injury shall trigger the scheduling of
a CNA to include the person with the brain injury, any natural supports or advocates, and the
BISF service coordinator or BISF life skills coach, as applicable.
o All parties are to ensure a Release of Information has been signed by the member to affect the
participation of the BISF service coordinator and/or other identified advocates in the member’s
transition.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
65 | P a g e
o The MCO Care Coordinator is to acquire a copy of the BISF participant’s BISF assessment and
Independent Living Plan (ILP) from the BISF service coordinator to ensure their inclusion in the
member’s file. These efforts are intended to preserve the history of brain injury and ensure that
care needs are related to the brain injury diagnosis.
• The MCO shall receive brain injury training by the HSD including: general brain injury information;
available state and community resources; and communication strategies. Other topics may include:
how to conduct assessments that capture the needs of brain injury; and how to develop a CCP that
considers the needs of members with brain injury. Training by the MCO shall be required for any
new care coordination staff within three months of employment, with renewed training to occur on
a two-year schedule.

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
66 | P a g e
4.15. Appendix
4.15.1. Health Risk Assessment

Section 4: Care Coordination
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
67 | P a g e

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
68 | P a g e
5. Transitions of Care
5.1. General Information
In managed care, HSD will continue its commitment to providing the necessary supports to assist
members as they transition under various circumstances.
The MCOs must identify and facilitate coordination of care for all members during various transitions
including but not limited to:
• Transition from an NF to the community;
• Transition for member(s) with special circumstances;
• Transition for member(s) moving from a higher LOC to a lower LOC;
• Transition for member(s) turning 21 years of age;
• Transition for member(s) changing MCOs while hospitalized;
• Transition for member(s) changing MCOs during major organ and tissue transplantation services;
• Transition for member(s) changing MCOs while receiving outpatient treatment for significant
medical conditions;
• Transition for member(s) changing MCOs;
• Transition for member(s) previously in FFS;
• Transition for member(s) moving from a residential placement or institutional facility (including
psychiatric hospitals) to a community placement;
• Transition for children entering or returning home from a foster care placement;
• Transition for member(s) released from incarceration or detention facilities;
• Transition for member(s) moving from an out-of-state placement to an in-state placement;
• Transition from RTC to TFC, group home or foster care.
• Transition for member(s) discharging from a hospital;
• Transition for member(s) discharging from out-of-home placements (ARTC, RTC, Group Home,
Therapeutic Foster Care [TFC]) and crisis centers related to BH treatment; and/or
• Transition for member(s) who are preparing to receive out-of-state treatment.

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
69 | P a g e
5.2. Transitions of Care
The MCOs shall develop and implement methods for identifying and facilitating care coordination for all
members involved in various transition scenarios. Such methods shall include, at a minimum:
• The CNA;
• Preadmission Screening and Resident Review (PASRR);
• MDS;
• Provider referrals to or from hospitals and RTCs;
• Ombudsman;
• Family member;
• Change in medical status;
• Member self-referral;
• Community Reintegration Allocation received;
• A recommendation from the Individualized Planning Meeting Plan for a child or youth in CYFD PS
custody;
• State Agency Referral; and/or
• Incarceration or detention facility referral.
If a member is a candidate for transitioning to the community, the Care Coordinator shall facilitate the
development of and implementation of a transition plan which must be labeled “Transition of Care Plan”
and may be a stand-alone document or included in the CCP. If included as a part of the CCP, the
“Transition of Care Plan” must be clearly labeled for MCO tracking and HSD auditing. The transition of
care plan shall remain in place for a minimum of 60 calendar days from the date of the decision to
pursue transition or until the transition has occurred and a new CCP is in place. The transition of care
plan shall address the member’s transitional needs including but not limited to:
• PH and BH needs;
• CB needs;
• Continuation of Medicaid eligibility;
• Selection of providers in the community;
• Housing needs;
• Financial needs;
• Interpersonal skills (the social skills people use to interact effectively with other people, including
the ability to convey one’s needs); and

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
70 | P a g e
• Safety.
The Care Coordinator shall conduct an additional assessment within 75 calendar days after the transition
to determine if the transition was successful and to identify any remaining needs resulting in a new CCP
or modifications to an existing CCP.
If the member has an existing full Medicaid category of assistance, other than Institutional Care, an
allocation is not needed to reintegrate into the community. The reintegration process can be completed
and CBs can be provided with the full Medicaid category.
If the member is Not Otherwise Medicaid Eligible (NOME), and in an NF and wishes to receive services in
the community, a Community Reintegration (CRI) allocation must be requested by contacting the Aging
and Long-Term Services Department, Aging and Disability Resource Center (ALTSD/ADRC), prior to
discharge (see Section 7: Community Benefits). The Care Coordinator must assist the member in gaining
eligibility for a CB category of assistance, and ensure services are authorized and in place for a safe and
seamless discharge.
5.3. Transitions of Care Requirements
The MCO shall establish policies and procedures to ensure all members are contacted in a timely
manner and are appropriately assessed using HSD prescribed time frames, processes and tools, to
identify needs.
The MCO shall coordinate with the discharge planning teams at hospitals and institutions (e.g., NFs,
jails/prisons, juvenile detention centers and CYFD secure facilities, RTCs, psychiatric hospitals, behavioral
health facilities) to address at a minimum:
• Need for HCBS;
• Follow up appointments;
• Therapies and treatments;
• Medications; and/or
• DME.
The MCO shall notify the assigned CYFD permanency placement worker (PPW) for protective services
(PS) involved children and youth and juvenile probation officer (JPO) for juvenile justice-involved youth,
and community behavioral health clinician (CBHC) within 30 Business Days prior to transition in care for
CYFD-involved children/youth. Precipitous discharge from these placements is prohibited.

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
71 | P a g e
The MCO shall perform an in-home assessment for members who are transitioning from an inpatient
hospital or NF stay within three calendar days after the transition. The assessment will address at a
minimum:
• Safety in home environment;
• PH needs;
• BH needs;
• Housing needs;
• Continuation of Medicaid eligibility;
• Financial needs;
• CNA if one is not in place; and
• CB needs and services in place.
The MCO shall contact the member monthly for three months to ensure continuity of care has occurred
and the member’s needs are met. The MCO shall not transition members to another provider for
continuing services unless the current provider is not a contract provider. The MCO shall facilitate a
seamless transition to new services and/or providers, without any disruption in services as outlined in
the CCP.
For members who are preparing to receive out-of-state treatment, the MCO shall ensure daily updates
are provided to the member and/or AR about the status of the out-of-state provider agreement and
authorized treatment plan until treatment begins.
The MCO shall maintain active communication with the member and/or AR once out-of-state treatment
begins, including weekends and holidays, for the duration of the treatment. The MCO shall resume care
coordination activities pursuant to 4.4 of the Agreement following treatment completion and member’s
return to New Mexico.
5.4. Transition of Care Requirements for Pregnant Women
In the event a member enrolling with an MCO is in her second or third trimester of pregnancy and is
receiving medically necessary covered prenatal care services prior to enrollment in the MCO, the MCO
shall be responsible for providing continued access to the prenatal care provider (whether contract or
non-contract provider) through the postpartum period, without any form of prior approval.
In the event a member enrolled with an MCO is in her first trimester of pregnancy and is receiving
medically necessary covered prenatal care services prior to enrollment, the MCO shall be responsible for

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
72 | P a g e
the costs related to the continuation of such medically necessary prenatal care services. This includes
the delivery, without any form of prior approval and without regard to whether such services are being
provided by a contract or non-contract provider. This coverage is required for up to 60 calendar days
from the member’s enrollment or until the member may be reasonably transferred to a contract
provider without disruption in care, whichever is less.
If the member is receiving services from a contract provider, the MCO shall be responsible for the costs
of continuation of medically necessary covered prenatal services from that provider, without any form
of prior approval, through the postpartum period.
If the member is receiving services from a non-contract provider, the MCO shall be responsible for the
costs of continuation of medically necessary covered prenatal services, without any form of prior
approval, until such time as the MCO can reasonably transfer the member to a contract provider
without impeding service delivery that might be harmful to the member’s health in accordance with
Section 4.4.16.3 of the Agreement.
5.5. Transfer from the Health Insurance Exchange
The MCO must minimize disruption of care and ensure uninterrupted access to medically necessary
services for individuals transitioning between Medicaid and qualified MCO coverage on the Health
Insurance Exchange.
At a minimum, the MCO shall establish transition guidelines for the following individuals:
• Pregnant women;
• Individuals with significant health care needs or complex medical conditions;
• Individuals receiving ongoing services or who are hospitalized at the time of transition; and
• Individuals who received prior authorization for services from its qualified MCO.
The MCO is expected to coordinate services and provide phase-in and phase-out time periods for each
of these individuals, and to maintain written policies, procedures, and documentation to address
coverage transitions.
5.6. Transitions of Care for Members Moving from a Higher LOC to a Lower LOC
The MCO shall develop and implement policies and procedures for ensuring that members transition
successfully from higher levels of care (e.g., acute inpatient, residential treatment centers, social
detoxification programs, treatment foster care, etc.) to the most appropriate lower LOC. Transitions

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
73 | P a g e
from inpatient and BH residential treatment facilities for both children and adults must be addressed. At
a minimum, the following must be addressed:
• Maintain on-going communication, enlist the involvement of and coordinate with state-run facilities
to monitor and support their participation in the member’s care.
• Care Coordinators must be knowledgeable of non-Medicaid BH and PH programs/services,
statewide, available to its members in order to facilitate referrals, coordinate care, and ensure
transition to community-based services.
• Ensure members receive follow-up care within seven calendar days of discharge from a higher LOC
to a lower LOC but receive follow up care no longer than 30 calendar days following other
discharges.
5.7. Transitions of Members Turning 21 Years of Age
All members, including those who are under the care of EPSDT, must be transitioned to other services
on their 21st birthday. The Care Coordinator must initiate a transition plan by the age of 20 years, which
is ongoing until the member leaves the EPSDT program. The transition plan must be labeled “Transition
of Care Plan” and may be a stand-alone document or included in the CCP. If included as part of the CCP,
the “Transition of Care Plan” must be clearly labeled for MCO tracking and HSD auditing. The transition
plan must:
• Establish a plan that is age appropriate and addresses the transition needs of the member:
o Health condition management;
o Developmental and functional independence;
o Education;
o Social and emotional health;
o Continuity of behavioral health services, if requested;
o Guardianship; and
o Transportation.
• Ensure members and, when authorized, family members, guardians and PCPs are part of the
development and implementation of the transition plan. The MCO shall also ensure that the
assigned CYFD permanency placement worker (PPW) and/or youth transition specialist for
Protective Services (PS) involved children and youth, juvenile probation officer (JPO) or transition
coordinator for juvenile justice involved youth, and community behavioral health clinician (CBHC)

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
74 | P a g e
for CYFD involved children/youth are part of the development and implementation of the transition
plan for CYFD involved children/youth.
• Document the transition plan in the medical record.
• Provide the member, and when authorized, family members and guardian with a copy of the
transition plan.
• Establish a timeline for completing all services the member should receive through EPSDT prior to
his or her 21st birthday.
• Review and update the plan and timeline with the member, and when authorized, the guardian and
family prior to official transition to adult provider.
• Advise the member’s PCP of the discharge and ensure coordination of the services with the adult
PCP.
5.8. Transition for Members changing MCOs while Hospitalized
The MCO will make provisions for the smooth transition of care for members who are hospitalized on
the day of an enrollment change. The provisions must include policies for the following:
• Authorization of treatment by the receiving MCO on an individualized basis. The receiving MCO
must address contracting for continued treatment with the institution on a negotiated fee basis, as
appropriate.
• Notification to the hospital and attending physician of the transition by the relinquishing MCO. The
relinquishing MCO must notify the hospital and attending physician of the pending transition prior
to the date of the transition and instruct the providers to contact the receiving MCO for
authorization of continued services. If the relinquishing MCO fails to provide notification to the
hospital and the attending physician relative to the transitioning member, the relinquishing MCO
will be responsible for coverage of services rendered to the hospitalized member for up to 30
calendar days. This includes, but is not limited to, elective surgeries for which the relinquishing MCO
issued prior authorization.
• Coordination with providers regarding activities relevant to concurrent review and discharge planning must
be addressed by the receiving MCO, along with the mechanism for notification regarding pending discharge.
• Transfer of care to a physician and/or hospital affiliated with the receiving MCO. Transfers from an
out-of-network provider to one of the receiving MCO providers cannot be made if harmful to the

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
75 | P a g e
member's health and must be determined medically appropriate. The transfer may not be initiated
without approval from the relinquishing MCO PCP, or the receiving MCO Medical Director.
Note: Members in Critical Care Units, Intensive Care Units, and Neonatal Intensive Care Units require
close consultation between the attending physician and the receiving MCO physician. If a member is
admitted to an inpatient facility while still assigned to the relinquishing MCO, and discharged after
transition to the receiving MCO, both must work together to coordinate discharge activities.
The relinquishing MCO will be responsible for coordination with the receiving MCO regarding each
specific prior authorized service. For members known to be transitioning, the relinquishing MCO will not
authorize hospital services such as elective surgeries scheduled less than 15 calendar days prior to
enrollment with the receiving MCO. If authorized to be provided during this time frame, the service for
the transitioning member will be the financial responsibility of the MCO who authorized the service.
5.9. Transition for Members Changing MCOs during Major Organ and Tissue Transplantation Services
If there is a change in MCO enrollment, both the relinquishing and receiving MCOs will be responsible
for coordination of care and coverage for members awaiting major organ or tissue transplantation from
the time of transplantation evaluation and determination through follow-up care after the
transplantation surgery. If a member changes MCO enrollment while undergoing transplantation at a
contracted transplant center, the relinquishing MCO is responsible for contracted components or
modules of the service up to and including completion of the service modules that the member is
receiving at the time of the change. The receiving MCO is responsible for the remainder of the module
components of the transplantation service.
If a member changes to a different MCO while undergoing transplantation at a transplant center that is
not a contracted provider, each MCO is responsible for its respective dates of service (DOS). If the
relinquishing MCO has negotiated a special rate, it is the responsibility of the receiving MCO to
coordinate the continuation of the special rate with the respective transplant center.
5.10. Transition for Members Changing MCOs while receiving Outpatient Treatment for Significant Medical
Conditions
MCOs must have protocols for ongoing care of active and/or chronic "high risk" (e.g., outpatient
chemotherapy, home dialysis, etc.) members and pregnant members during the transition period. The
receiving MCO must have protocols to address the timely transition of the member from the
relinquishing PCP to the receiving PCP, in order to maintain continuity of care.

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
76 | P a g e
The receiving MCO must address methods to continue the member's care, such as contracting on a
negotiated rate basis with the member's current provider(s) and/or assisting members and providing
instructions regarding their transfer to providers affiliated with the receiving MCO.
Receiving MCOs are also responsible for coordinating the transition of pregnant women to maintain
continuity of care. Pregnant women who transition to a new MCO within the last trimester of their
expected date of delivery must be allowed the option of continuing to receive services from their
established physician and anticipated delivery site.
5.11. MCO Requirements for Members Transitioning between MCOs
For any member transitioning from one MCO to another the following must occur.
• The relinquishing MCO must provide relevant information regarding members who transition to a
receiving MCO.
• The MCO must also provide protocols for the transfer of pertinent medical records, as discussed in
this policy, and the timely notification of members, subcontractors, or other providers, as
appropriate during times of transition.
• The receiving MCO must provide new members with their handbook and emergency numbers
within 10 calendar days of transition for acute care members and within 12 calendar days of
transition for all other members (allows for care coordination on-site visit).
• If a member is referred to and approved for enrollment, the relinquishing MCO must coordinate the
transition with the receiving MCO to ensure applicable protocols are followed for any special
circumstances of the member, and that continuity and quality of care is maintained during and after
the transition.
• The relinquishing MCO that fails to notify the receiving MCO of transitioning members with special
circumstances, or fails to send the transition notification, will be responsible for covering the
member's care resulting from the lack of notification, for up to 30 calendar days.
• The MCO shall ensure that any member entering the MCO has access to services consistent with the
access they previously had and is permitted to retain their current provider for a period of time, if
that provider is not contracted with the MCO.

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
77 | P a g e
5.12 Transitions of Care for Justice Involved Members
The MCO shall develop and implement policies and procedures for ensuring that members released
from incarceration or detention facilities transition successfully back into the community. At a minimum,
MCOs must:
• Initiate an HSD approved Transition of Care (TOC) assessment with the member prior to member’s
release or within three (3) business days of notification of member’s release.
• Develop a TOC plan, derived from the TOC assessment, with member and/or member’s
representative’s participation, that addresses, at a minimum:
• Physical and Behavioral Health needs;
• Community Benefit needs;
• Selection of Providers in the community;
• Housing needs;
• Financial needs;
• Continuation of Medicaid eligibility
• Interpersonal skills; and
• Safety
The Transition of Care plan shall remain in place for a minimum of sixty (60) calendar days from the
member’s release or sixty (60) calendar days from notification of member’s release.
• Conduct a Health Risk Assessment (HRA) within three (3) business days of member’s release or
three (3) business days of notification of member’s release unless the member has had one within
the past thirty (30) calendar days.
• Complete a Comprehensive Needs Assessment (CNA), within thirty (30) business days of member’s
release or within thirty (30) business days of notification of member’s release, if warranted by the
completed HRA, to determine if the member should be assigned to Care Coordination level two (2)
or level three (3).
• If the member is leveled at CCL2 or CCL3, follow all contract requirements for ongoing care
coordination including development of a Comprehensive Care Plan and required touchpoints
pursuant to the Medicaid Managed Care Services Agreement 4.4.
• Contact the member monthly for three (3) months after member’s release to ensure continuity of
care has occurred and that the member’s needs have been met.
• Conduct an additional assessment within seventy-five (75) calendar days of member’s release to
determine if the transition was successful and identify any remaining or ongoing needs.

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
78 | P a g e
5.13 Transitions of Care for Substance Exposed infants
The MCO shall develop and implement policies and procedures to ensure care coordinators assist in
addressing the needs of pregnant mothers and fathers with opioid use disorders and their infants. Once
the member is referred to the MCO by DOH or a hospital, the MCO care coordinator will be responsible
for assessing, referring, and coordinating support services identified in the Plan of Care. MCO care
coordinators are responsible for collaborating and coordinating care for the infant, affected
mother/father and family and caregivers in accordance with the Children, Youth and Families
Department (CYFD).
At a minimum, MCOs are responsible for:
• Providing annual training for care coordination staff on the Comprehensive Addiction and
Recovery Act (CARA) Plan of Care (POC) to address the needs of both the pregnant women with
opioid use disorders and their substance-exposed newborns. Training to include the difference
between CYFD notification and CYFD referral or report;
• Coordinating care with the CYFD case worker, in cases where a child protective services case is
determined necessary;
• Ensuring care coordination staff communicate and collaborate with hospital staff on
implementation of the POC;
• Obtaining a copy of the POC from the hospital discharge planner;
• Ensuring MCO care coordination staff introduce support service providers identified in the POC
to the infant and mothers including family and caregivers;
• Conducting a Health Risk Assessment (HRA) with the substance abuse-exposed infant, parent or
caregiver within three (3) Business Days of referral to the MCO;
• Completing a Comprehensive Needs Assessment (CNA), within thirty (30) Business Days of HRA
completion to determine if the member(s) should be assigned to Care Coordination level two
(CCL2) or level three (CCL3);
• Following all contract requirements for ongoing care coordination for member(s) leveled at CCL2
or CCL3, including development of a Comprehensive Care Plan (CCP) and required touchpoints
pursuant to section 4.4 of the Medicaid Managed Care Services Agreement and sections 5.2 and
5.3 of the Managed Care Policy Manual; including but not limited to home visitation programs,
early intervention services and recovery supports. MCOs should refer to contract requirements
detailed in sections 4.4.6 and 4.4.7 that include, but are not limited to, high risk pregnancy and

Section 5: Transitions of Care
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
79 | P a g e
co-morbid health conditions as CCL2 and medically complex and/or untreated substance abuse
dependency as CCL3; and
• Notifying CYFD if the mother and/or family/caregiver(s) are Unable to be Reached, Difficult to
Engage, Refuse Care Coordination, or are non-compliant with the POC and the CCP.

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
80 | P a g e
6. Nursing Facilities (NFs)
6.1. General Information
This policy establishes guidelines for the MCOs regarding NFs. The NF LOC Criteria and instructions can
be found on the HSD website.
6.2. NF Procedures for Requests for Prior Approval
All requests for prior approval shall contain appropriate documentation and must be completed for each
resident for every situation requiring prior approval. All requests for prior authorization are submitted to
the resident’s MCO by fax.
6.3. Pre-Admission Screening and Resident Review (PASRR)
Federal law requires NFs to perform PASRR screens for mental illness, ID, and related conditions. There
are procedures and information that are applicable to all situations requiring prior approval.
• Purpose of PASRR is as follows:
o To determine whether a resident requires a specific level of nursing care;
o To determine if there is suspicion of serious mental illness (SMI) or intellectual disability/related
condition (ID/RC);
o To assess persons suspected of having serious SMI or ID/RC;
o To assess whether specialized services for SMI or ID/RC are needed; and,
o To prevent inappropriate placement in a NF by determining whether the resident is more
appropriately served in a specialized program for those with SMI or ID/RC.
• Organization of the PASRR: PASRR is divided into two levels: Level I Screen and Level II Evaluation.
o Level I Screen: A Level I Screen must be completed prior to admission on every NF applicant. If,
during the Level I Screen, it is determined that the individual is suspected of having either SMI or
ID/RC, a Level II Evaluation or PASRR waiver must occur prior to admission. A Level I Screen must
also be done if there has been a significant change in the physical or mental condition of a
resident who is suspected of having, or previously determined to have SMI or ID/RC. “Significant
change” for PASRR purposes can be tied to the already existing regulatory definition for
significant change that prompts an alteration in a resident’s MDS. Significant change referrals
must be made to the PASRR Unit no later than 21 business days after the occurrence of the
significant change. The PASRR Unit is required to review the completed Level I Screen packet
within seven to nine business days of receipt of the completed packet from the NF. Notification

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
81 | P a g e
of the review decision must be submitted to the NF by phone or in writing within that time
period.
o Level II Evaluation: If the Level I Screen identifies a resident who is diagnosed with or suspected
of having SMI or ID/RC, a Level II Evaluation or a PASRR waiver must be completed prior to the
admission of the resident. The Level II Evaluation includes a comprehensive evaluation of the
needs of the resident.
• PASRR Waiver:
o If an individual falls within one of the following categories, a complete Level II Evaluation may
not be performed. A PASRR Waiver is granted on a case-by-case basis.
▪ The resident has a primary diagnosis of dementia.
▪ The resident is being discharged from an acute care hospital for the purpose of convalescent
care medically prescribed for recovery, not to exceed 30 business days.
▪ The resident is suspected of having SMI or ID/RC but is certified to be terminally ill with a life
expectancy of six months or less and is in need of continuous nursing care and/or medical
supervision and treatment due to a physical condition.
▪ The severity of the resident’s medical condition and medical treatment needs are so
extensive that specialized SMI or ID/RC services are not likely to be beneficial.
▪ The resident who is suspected of having SMI or ID/RC and is admitted directly to an NF from
a home for very brief and finite stay (up to 14 days) for the purpose of providing respite to
in-home caregivers.
▪ If APS directly admits an individual to an NF because the individual is in harm’s way, the
PASRR Unit is required to complete the Level II assessment within 10 business days.
• Level I Screen Process
o An NF is required to submit copies of the Level I Screen for each resident with the MDS to the
MCO/Utilization Review (UR) Contractor. The Screen and other necessary documentation must
be sent with the MDS to avoid delays in the review process.
o The MCO/UR Contractor logs in the date on the recipient screen when the MDS, Level I Screen,
and other documentation is received.
o The MCO/UR Contractor scans the Level I Screen. If the resident passes the Screen, the MCO/UR
Contractor determines the NF LOC. If the resident fails the Screen, no further NF LOC action is to
be taken by the MCO/UR Contractor. The MDS Screen, and other documentation, must be
submitted to the PASRR Unit for a Level II determination.

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
82 | P a g e
o The MCO/UR Contractor then sends a notice to the NF that the MDS and other documentation
have been sent to the PASRR Unit for a Level II Evaluation determination.
• Level II Evaluation Process: There are two types of Level II PASRR reviews.
o SMI PASRR II screens are completed by the BHSD contractor for residents living in an NF or
individuals being admitted from a hospital or home to an NF.
▪ The PASRR Unit sends the documents to the BHSD contractor to complete an evaluation and
makes the Level II determination on the review portion of the MDS and the NF LOC
determination, then returns to the PASRR Unit. The PASRR Unit sends the NF LOC
determination and MDS to the NF. The NF then sends the MCO/UR Contractor the MDS and
other documentation with the NF LOC determination if a waiver was not granted.
▪ Within 24 hours of the MCO/UR Contractor receiving the NF LOC determination from the NF
determined by the BHSD contractor, the MCO/UR Contractor transmits the NF LOC
determination via the appropriate interface file.
▪ If a subsequent specified review or significant change review is required, the review portion
of the MDS must be completed by the PASRR Unit. All subsequent reviews follow the
process above by the PASRR Unit instead of the MCO/UR Contractor.
▪ If a subsequent specified review or significant change review is not required, the MDS is
returned to the MCO/UR Contractor for an NF LOC determination.
o ID and RC PASRR II screens are completed by the PASRR Unit for residents living in an NF or
individuals being admitted from a hospital or from home to an NF.
▪ The PASRR Unit completes an evaluation and makes the Level II determination on the
review portion of the MDS and returns the MDS to the NF. The NF then sends the MCO/UR
Contractor the MDS and other documentation for an NF LOC determination if a waiver was
not granted.
▪ All subsequent PASRR Level II reviews are performed by the PASRR Unit unless waived by
the PASRR Unit.
▪ All subsequent NF LOC determinations are made by the MCO/UR contractor.
• PASRR and re-admission from a hospital: The NF contacts the PASRR Unit if the hospitalization of a
resident results in a change in the Level I Screen. If an individual is hospitalized from the NF, the
hospital will complete a new Level I screen prior to discharge.

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
83 | P a g e
• PASRR and Medicaid eligibility pending: If a resident is in a “Pending Medicaid” status at the time of
MDS submission and the resident fails the Level I Screen, the MDS is forwarded to the PASRR Unit as
notification while the following actions occur:
o The NF LOC determination is made by the MCO/UR Contractor.
o The MCO/UR Contractor transmits the NF LOC determination via the appropriate interface
within 24 hours of making the NF LOC determination. The information is processed by the
appropriate Income Support Division (ISD) office once received. The MCO also sends the NF
notification form to the NF with the NF LOC effective dates and prior authorization information.
o Once eligibility is established, the ISD office notifies the NF and the MCO.
o The NF must notify the PASRR Unit of the status of the resident’s eligibility.
o The MDS, which includes the Medicaid number and the certified length of stay, is completed by
the PASRR Unit.
o Upon completion, the MDS is submitted to the MCO/UR Contractor.
6.4. Level of Care Packet for Nursing Facilities
• PASRR
• NF LOC Notification Form - used for all prior approval reviews
o All requests for prior approval will be submitted on the NF LOC Notification Form.
o The NF should document what type of review is being requested at the top of the NF LOC
Notification Form:
▪ Initial;
▪ Continued Stay;
▪ Medicaid Pending;
▪ Transfer;
▪ Re-admit;
▪ Re-Review;
▪ Reconsideration; and/or
▪ All other required fields must be completed.
• MDS
o An MDS and all other appropriate documentation must be completed for each resident for
every situation requiring prior approval.

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
84 | P a g e
o All locator fields must be clearly marked on the MDS.
o When the resident goes from Medicare co-pay to Medicaid, the NF submits an Internal MDS
that begins the UR process for the resident.
o Appropriate documentation must accompany the MDS. Generally, appropriate documentation
includes a valid order and must:
▪ Be signed by a physician, nurse practitioner, clinical nurse specialist, or physician assistant;
▪ Be dated; and
▪ Indicate the LOC – either high NF (HNF) or low NF (LNF).
The NF must submit the initial NF LOC packet to the MCO no later than 30 calendar days after
admission, which includes all of the above documentation and the physician’s order. The MCO may
assign unexcused late days if the NF submits the LOC packet later than 30 calendar days. Please refer to
the Current/Retrospective Reviews Section above for more information about assignment of late days.
Once an order is signed and dated, it cannot be changed. If a change is required, a new order must be
written, signed, and dated by the physician, nurse practitioner or physician assistant.
Verbal or telephone orders are permitted. The order must be taken by an RN or LPN who must also sign
and date the order. It must be clearly indicated the order is a telephone or verbal order with the name
of the physician, nurse practitioner or physician assistant who gave the order and LOC. The date of the
call or verbal communication is the date of the order.
The MCO approves the documentation and makes a LOC determination following the New Mexico
Medicaid NF LOC Instructions and Criteria within five business days of receiving a completed packet. The
MCO shall review the documentation provided to determine the appropriate NF LOC and transmits the
determination via the appropriate interface file within 24 hours of making the NF LOC determination. A
packet that requests LNF but meets HNF criteria shall be upgraded to HNF; a packet that requests HNF
but only meets LNF criteria shall be downgraded to LNF. A new doctor’s order is not required.
When required documentation is missing, an RFI sheet will be generated by the MCO and sent to the NF.
If the required documentation is not provided to the MCO within 14 business days of the request, it will
be technically denied. The MCO will make three attempts during the 14-business day period to contact
the NF to obtain the information. The MCO will transmit a technical denial via the ASPEN interface file
within 24 hours of no response from the NF. Please see Current/Retrospective Reviews for more
information on assignment of late days.
Note: A formal RFI to the NF to justify the HNF request is not required when reviewing and processing
HNF requests that clearly do not meet HNF criteria but do meet LNF criteria or vice versa. In the event a

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
85 | P a g e
determination is upgraded or downgraded from the physician’s order the MCO shall assign the LOC and
provide the NF with technical assistance to educate the NF on determination criteria.
The MCO faxes the NF notification form with authorization and date spans to the NF.
Short-term skilled stays:
For short-term stays (90 days or less) the MCO will provide ISD with NF LOC determination dates but will
only issue a prior authorization to the NF for the authorized bed days, if appropriate and after eligibility
has been established.
The updated NF LOC criteria published on 01/ 01/2019 includes General Eligibility Requirements under
Section V. This section explains the minimum requirements for LOC and includes information on when
the MCO should not assign a LOC, but rather issue a skilled nursing authorization.
Not appropriate for NF care: The member’s needs are too complex or inappropriate for NF, such that:
• The member requires acute level of care for adequate diagnosis, monitoring and treatment or
requires inpatient based acute rehabilitation services.
▪ Members who reside in a NF long-term and have a clinical episode which
requires hospitalization, should be evaluated for skilled nursing services once
readmitted to the facility to determine if the member requires acute therapy
related to the hospitalization.
▪ Members who reside in a NF long-term and have a clinical episode which does
not require hospitalization, but may indicate a change in LOC, should be
evaluated for HNF.
▪ Members who do not reside in the NF but have been hospitalized and require
inpatient based acute rehabilitation services should be evaluated for skilled
nursing services.
6.5. Denial of Requests for NF LOC Determinations
If the NF LOC criteria is not met and the request for initial NF placement or Medicaid pending is denied,
the MCO will send the referring party and the applicant a denial letter within five business days of
receipt of a completed packet, with the reason for denial as determined by the MCO. The requesting
provider then has the opportunity to request a Re-review and/or Reconsideration of the MCO’s decision
per the timelines indicated in section 6.15. If no reconsideration is requested, the MCO will transmit the
determination via the ASPEN interface file within 24 hours of making the NF LOC determination. The

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
86 | P a g e
applicant will receive a Notice of Case Action from the ISD office, which explains the right to request an
administrative hearing.
Providers who disagree with the initial review decision must request a Re-review of the decision(s)
before requesting a Reconsideration. Please see section 6.15 for timelines and requirements.
If the NF LOC criteria is not met for an existing resident, the MCO will send the referring NF and the
member a denial letter with information regarding the right to appeal to the MCO before requesting an
administrative hearing. The MCO will not transmit the denial via the ASPEN until a final appeal decision
has been made or until after the allowed time to request an appeal has lapsed, whichever is later.
6.6. Reserve Bed Days
Medicaid pays to hold or reserve a bed for a resident in an NF to allow for the residents to make a brief
home visit, for acclimation to a new environment or for hospitalization according to the limits and
conditions outlined below.
• Medicaid covers six reserve bed days per calendar year for every LTC resident for hospitalization
without prior approval. Medicaid covers three reserve bed days per calendar year for a brief home
visit without prior approval.
• Medicaid covers an additional six reserve bed days per calendar year with prior approval to enable
residents to adjust to a new environment, as part of the discharge plan.
o Resident’s discharge plan must clearly state the objectives, including how the home visits or
visits to alternative placement relate to discharge implementation.
o The prior approval request must include the resident’s name, Medicaid number, requested
approval dates, copy of the discharge plan, name and address for individuals who will care for
the resident during the visit or placement and a written physician order for trial placement.
Requests for additional discharge reserve bed days must be submitted by the NF to the MCO that the
resident is enrolled with for prior approval. The NF follows the written process of the MCO for
submission of the request, and receipt of documentation of the approval. The written process of the
MCOs must also indicate if any documentation or procedures are required of the NF to assure payment
of claims for approved discharge reserve bed days.

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
87 | P a g e
6.7. Initial Determination, Redetermination, and Pending Medicaid Eligibility
• Initial Determination: All services furnished by Medicaid NF providers must be medically necessary.
The procedures described in the NF Procedures for Requests for Prior Approval Section above,
should be referred to when preparing documents for all initial reviews. Documents must be
completed and submitted within 30 calendar days of admission.
Initial length of stays:
o Initial HNF is not to exceed thirty (30) days; however, a shorter length of stay can be
assigned based on the needs of the resident;
o Initial LNF cannot exceed ninety (90) days; however, a shorter length of stay can be assigned
based on the needs of the resident.
• Redetermination: The medical documentation must be faxed and received by the MCO a minimum
of 60 calendar days prior to the start date of the new certification period for LNF and 30 calendar
days prior for HNF.
Continued stay length of stays:
o HNF continued stay reviews can be certified by the MCO for up to 90 days based on the
medical needs and stability of the resident.
o LNF continued stay reviews can be certified by the MCO up to 365 days based on the
medical needs and stability of the resident.
Prior approval reviews are required for all requests for the continued stay of a resident in a NF.
These reviews are based on the medical necessity of NF services being continually provided to the
resident. The medical necessity decision is made during the continued stay review. Thirty days
before the expiration of the current certification, a request for continued stay must be received by
the MCO.
• Pending Medicaid Eligibility: Prior approval reviews can be done when the service is furnished
before the determination of the effective date of the resident’s financial eligibility for Medicaid. If
the resident is applying for Medicaid, both financial and medical eligibility at the same time, please
write “Medicaid Pending” in the type of request box on the Notification form. Note: A resident on
SSI is not considered Medicaid Pending.
o When an individual is admitted to a NF pending Medicaid financial eligibility, the NF submits
a completed Minimum Data Set (MDS) with required documentation and a Physician’s,
Nurse Practitioner’s or Physician Assistant’s order for LOC. The Notification Form - Section I.

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
88 | P a g e
Nursing Facility Prior Authorization Request - should have “MEDICAID PENDING” selected
for Type of Request (Choose an item from the drop-down menu).
o The MCO will review the information submitted and determine the NF LOC.
o The MCO will issue NF LOC, if appropriate but will only issue a prior authorization to the NF
for the authorized bed days, and after eligibility is established.
o The MCO will review the information submitted and determine the NF LOC.
o The Prior Authorization form will be completed by the MCO and sent to the NF.
o The MCO will transmit the NF LOC determination via the ASPEN interface within 24 hours of
making the determination.
6.8. Care Plan and Emergency Preparedness
Care Plan
The NF must develop a care plan, per 42 CFR 483.21, for each resident within 48 hours of admission, to
include instructions needed to provide effective and person-centered care that meets professional
standards of quality of care. The care plan must include all specialized or rehabilitation services the NF
will provide as a result of PASRR recommendations.
Emergency Preparedness
The NF must be in compliance with 42 CFR 483.73 including, but not limited to:
• Self-Assessment and Planning:
o Develop an emergency plan based on a risk assessment;
o Perform risk assessment using an “all-hazards” approach, focusing on capacities and capabilities;
and
o Update emergency plan at least annually.
• Policies and Procedures:
o Develop and implement policies and procedures based on the emergency plan and risk
assessment;
o Policies and procedures must address a range of issues including subsistence needs, evacuation
plans, procedures for sheltering in place, tracking patients and staff during an emergency; and
o Review and update policies and procedures at least annually.
• Communication Plan
o Develop a communication plan that complies with both Federal and State laws;

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
89 | P a g e
o Coordinate patient care within the facility, across health care providers, and with State and local
public health departments and emergency management systems;
o Review and update plan annually; and
o Share information from the emergency plan with residents, family members or representatives,
and the member’s MCO.
• Training and Testing Requirements
o Develop and maintain training and testing programs, including initial training in policies and
procedures;
o Demonstrate knowledge of emergency procedures and provide training at least annually; and
o Conduct drills and exercises to test the emergency plan.
6.9. Retroactive Medicaid Eligibility
Written requests for prior approval based on a resident’s retroactive financial eligibility must be
reviewed by the MCO within 30 calendar days of the date of the eligibility determination. The NF must
submit all appropriate medical documentation to the MCO for the NF LOC determination. The MCO will
transmit the determination via the ASPEN interface file within 24 hours of making the NF LOC
determination. Requests for retroactive eligibility will not be accepted after 180 days of the Medicaid
eligibility determination date. Please see NMAC 8.281.600.13.
6.10. Re-Admission Reviews
When the resident leaves the NF for three or more midnights for an inpatient hospital stay, a
readmission review is required.
The NF must submit a re-admit MCO approval request form within 30 calendar days together with the
following accompanying documentation – the hospital discharge summary and/or resident’s admission
note back to the NF.
• When the resident is re-admitted to the NF and has more than 30 calendar days left on his/her
certification, days will be assigned from the re-admit date. The NF sends the notification form to the
MCO along with supporting documentation.
• If the resident has less than 30 calendar days left on his/her certification, the NF will not submit a
re-admit notification form. Instead the NF should submit a re-determination (annual or continued
stay) request on the notification form along with supporting documentation.

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
90 | P a g e
6.11. Current/Retrospective Reviews
Medical documentation for initial, redetermination, re-admit and changes in LOC reviews can be
reviewed retrospectively if requested by the NF.
A request for a current or a retrospective review for initial (including Medicaid pending),
redetermination or re-admit reviews will be considered; however, the below outlines the procedure for
unexcused and excused assignment of late days by the MCO.
Unexcused late reviews
Starting July 1, 2014, the NF may lose payment for each day that the NF LOC review is submitted late.
Excused Late Reviews
Prior authorization forms not submitted timely due to reasons beyond the control of the NF must be
submitted to the MCO with a detailed written explanation and documentation that supports the request
for an excusable late review. Reimbursement and retrospective reviews:
• If the reason for the delay in documentation submission was within the control of the NF, the
effective date for reimbursement is the date the packet was received by the MCO.
• Medicaid will not reimburse NFs for DOS not covered by the MCO prior authorization form. In
addition, the Medicaid member and his/her family member(s)cannot be billed for the services
provided by the NF. The NF will not discharge the resident due to assignment of late days by the
MCO.
6.12. Transfer from Another NF
If a resident transfers from one NF to another NF, the following procedures apply:
• The receiving NF must notify the MCO by telephone that a transfer to its NF is to occur. The
receiving NF will provide the MCO with the date of the transfer. Without this information, claims
submitted by the receiving NF will not be paid by the MCO.
o If there are more than 30 calendar days on the resident’s current authorization, the MCO will fax
the receiving NF the completed notification form which will include the prior authorization and
date span.
o If there are less than 30 calendar days remaining on the resident’s current authorization, the
receiving NF shall request a continued stay on the notification form to the MCO. The MCO shall
make a new NF LOC determination; the days remaining on the current certification will be added

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
91 | P a g e
to the continued stay. Please write “Transfer” in the type of request box on the notification
form.
• The NF receiving the resident receives the status of resident’s reserve bed days from the MCO
through the notification form. This includes the number of days used during a calendar year and the
reason for the use of these days. This information is placed in the resident’s NF records.
6.13. Changes in the LOC
All changes in LOC require a new notification form that should be submitted within 30 calendar days of
the change in LOC. If a prior authorization form is being submitted for a change in LOC, please write
“LOC Change” in the type of request box on the notification form. The NF must provide a signed and
dated order from the physician, nurse practitioner or physician assistant as well as any documentation
to support the LOC request (see New Mexico NF LOC Instructions and Criteria). The date the LOC change
occurred must be clearly stated.
6.14. Discharge Status
Discharge status occurs when a resident no longer meets the LOC that qualifies for NF placement, but
there is no option for community placement at that time. Individuals are often already residing in an NF
at the time of initial application for Medicaid. In addition, Medicaid eligible individuals residing in an NF
may clinically improve to the point that they no longer meet an NF LOC. Such individuals may lack the
personal or family resources to provide for their own ongoing care in the community if discharged from
the NF. Community-based health care and support services may be limited or unavailable. Residents
may be at risk for failure to thrive outside the supportive structured environment of the NF. Physically
discharging the resident under such circumstances may put the resident’s health at risk.
To accommodate this health care issue, the New Mexico Medicaid program allows for temporary
continuation of coverage at LNF level of reimbursement while the NF and the MCO actively address the
development of community placement on an ongoing basis to meet the resident’s lower level of need.
The temporary continuation of coverage while discharge planning is taking place for a resident is termed
“Discharge Status;” however, Discharge Status does not mean the resident is being discharged from the
facility. Families and residents should not be told the resident is being discharged from the facility. The
MCO Care Coordinator, family, resident, and NF will work together to develop a transition plan to safely
transition the resident to an alternate SOC per Section 5 of this Manual.

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
92 | P a g e
• Initial Discharge Status is authorized at LNF for a maximum of 90 calendar days, based upon the
MCO physician determination.
• Continued Stay Discharge Status is authorized at LNF for not less than 180 calendar days and up to
365 calendar days. Submission of a continued stay on a prior authorization form for a resident in
Discharge Status must acknowledge the resident’s Discharge Status and document the facility staff’s
and MCO Care Coordinator’s ongoing attempts to find and develop appropriate community
placement options for the resident. The facility should document why the resident must remain in
an NF environment if the resident is at risk for failure to thrive upon discharge to a community
placement. Failure to submit sufficient documentation specifying the facility’s discharge planning
efforts could result in the denial of prior authorization. The resident’s inability to afford assisted
living services may be a consideration in discharge planning.
6.15. Re-Review, Reconsideration, Appeal, Administrative Hearing
• Re-review: The Re-review must be requested within ten (10) calendar days after the date on
the written notification of the MCO decision or action. Requests for a Re-review must be
submitted in writing directly to the MCO. The MCO completes and submits a written Re-review
decision to the NF within six (6) business days from receipt and will include the decision and
information on the Reconsideration process. Providers who do not meet the ten (10) calendar
days for a Re-review may request a Reconsideration.
• Reconsideration: Providers who disagree with a Re-Review NF LOC determination can request
reconsideration. Members who disagree with a NF LOC determination may request the provider
to pursue reconsideration on his or her behalf. Requests for reconsideration must be in writing
and received by the MCO within thirty (30) calendar days after the date on the Re-Review
decision notice. The MCO completes and submits a written Reconsideration decision to the NF
within ten (10) business days of receipt and will include the decision and information on the
MCO Appeals and HSD Administrative Hearing process, as appropriate. The provider or eligible
recipient may file a written request for Reconsideration up to 14 calendar days past the 30-
calendar day limit if the MCO finds there was “good cause” for failure to file a timely request.
The provider or the eligible recipient is responsible for providing written documentation
supporting “good cause” for failure to file a timely request. “Good cause” includes a death in the
family, disabling personal illness, other significant emergency or executional circumstance.

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
93 | P a g e
o The request for reconsideration must include the following:
▪ Statement that reconsideration is requested;
▪ Reference to the challenged decision or action;
▪ Basis for the challenge;
▪ Copies of any document(s) pertinent to the challenged decision or action; and
▪ Copies of claim form(s) if the challenge involves a claim for payment which is denied
due to a decision.
Individuals employed with the MCO, who were not participants in the initial decision, conduct
the Reconsideration review.
The MCO reviews the information and findings upon which the initial action was based, and any
additional information submitted to, or otherwise obtained by, the MCO. The information can
include the following:
• case records and other applicable documents submitted to the MCO by the provider
when the request for services was initially submitted;
• findings of the reviewer resulting in the initial decision;
• complete record of the service(s) provided, including hospital or medical records;
and
• additional documents submitted by the provider to support a Reconsideration
review.
The MCO performs the Reconsideration and furnishes the Reconsideration decision within ten
(10) business days of receipt of the Reconsideration request.
The MCO gives the provider and the eligible recipient written notice of the reconsideration
determination. If the decision is adverse to the eligible recipient the notice includes information
on the eligible recipient’s right to an MCO appeal, HSD Administrative Fair Hearings, timeframes
to file an appeal or fair hearing, and how to request continuation of benefits, as applicable.
• Appeal: If a reconsideration determination is adverse to the member, the member may request an
appeal with his or her MCO in accordance with 8.308.15 NMAC.
• State Administrative Fair Hearing: After the parties have exhausted the MCO appeals process, the
parties may request an administrative hearing according to State administrative rule 8.352.2 NMAC.
The MCO/UR Contractor is responsible for the development of the Summary of Evidence (SOE) to

Section 6: Nursing Facilities
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
94 | P a g e
ISD and for the testimony of the NF LOC denial during the fair hearing, including denied NF LOCs for
Medicaid Pending residents.
6.16. Communication Forms
The MCO shall use the approved HSD forms at https://www.hsd.state.nm.us/providers/nursing-facility-
level-of-care.aspx for the updated forms for communication and notification with the NFs.
6.17. External Audits of NF LOC Determinations
HSD or its designee will audit a sample of each MCO’s NF LOC determinations to ensure the LOC criteria
are being appropriately applied by the MCOs. Each MCO will submit a universe of NF LOC
determinations to HSD or its designee for review. HSD or its designee will meet with the MCO to discuss
audit findings.
6.18. MCO Internal Audits of NF LOC Determinations
Each MCO will conduct internal random sample audits of both facility and CB NF LOC determinations
based on HSD NF LOC instructions and tool guidelines each quarter. The audit will include, at a
minimum: accuracy, timeliness, training documentation of reviewers, and consistency of reviewers. The
results and findings will be reported to HSD by the 7th day of the month following the end of the quarter
along with any Quality Performance Improvement Plan via DMZ (NF LOC reviews folder). The naming
convention for the results and findings file is MCO, quarter, year, internal audit results. For example, if
the MCO is submitting first quarter reviews, the file shall be named “MCO-name.Q1.18.internal audit
results.”
6.19. RESERVED

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
95 | P a g e
7. Community Benefits
7.1. General Information
Community Benefits (CBs) are services that provide assistance to individuals who require LTSS so they
may remain in the family residence, in their own home, or in community residences. This program
serves as an alternative to placement in a NF. CB do not provide 24-hour care and are intended as a
supplement to an individual’s natural supports. CB services are available to members meeting a NF LOC.
The member’s MCO shall provide the CB services as determined appropriate by the CNA. Members
eligible for CBs have the option of selecting either the Agency-Based Community Benefit (ABCB) or
SDCB.
Two eligibility components must be met prior to receiving CB services: financial eligibility, determined by
the HSD/ISD and medical eligibility, determined by an MCO through a NF LOC assessment conducted as
part of the CNA. Additionally, if an individual is under the age of 65 and has not been deemed disabled
by the Social Security Administration (SSA), they must be evaluated by MAD’s Disability Determination
Unit (DDU) to establish their disability meets SSA guidelines. See NMAC 8.290.400.10(A).
Members who have a Full Medicaid COE may be eligible for CB if they meet an NF LOC and indicate they
have a need for CB. These individuals should request a CNA from their MCO to be assessed for CB. These
individuals do not need an allocation to access CB (see Section 5 Transitions of Care). Individuals up to
age 21 may be eligible for the EPSDT program, which provides personal care services (PCS). If a Medicaid
enrolled minor indicates he or she has a need for CB and meets an NF LOC, an allocation is not needed
to access CB services.

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
96 | P a g e
7.2. Definitions
1. Active Registration: A registration is active if there is an open category of registration on the Central
Registry.
2. Activity of Daily Living (ADL): Tasks that are essential for self-care, such as bathing, feeding oneself,
dressing, toileting and transferring.
3. Agency Based Community Benefits (ABCB): The CB services offered through a provider agency to a
member who does not wish to self-direct his or her CB services.
4. Allocation: The opportunity given to a registrant who is NOME to apply for CBs.
5. Allocation Packet: The documents sent by HSD/MAD/LTSSB to a registrant that includes the Letter
of Interest (LOI), Primary Freedom of Choice (PFOC), Withdrawal Form, Medicaid Application for
Assistance, and a self-addressed stamped envelope.
6. Central Registry: A database that maintains a list of individuals who are interested in receiving CBs
and may be eligible for an allocation.
7. Community Benefits (CB): HCBS that provide LTSS to eligible members that allow them to remain in
the family residence, in their own home, or in community residences such as an Assisted Living
Facility.
8. HSD 100: “Medicaid Application for Assistance” that is used to apply for CBs and is available online
or at a local HSD/ISD office.
9. Inactive Registration: A registration is inactivated/closed under certain circumstances (see
Section 7.10 of this Manual, Closing/Inactivating an Allocation).
10. Letter of Interest (LOI): The letter that is sent to a registrant informing him or her that an allocation
is available and that he or she may apply for CBs.
11. Notice of Allocation (NOA): The letter that is sent to a registrant informing him or her that the PFOC
was received at HSD/MAD/LTSSB and informs him or her of the next steps in the allocation process.
The date of the NOA is the allocation date.
12. Nursing Facility Level of Care (NF LOC): The member's functional level is such that two or more ADLs
cannot be accomplished without consistent, ongoing, daily provision, of some or all of the following
levels of service: skilled, intermediate or assistance. A member must meet an NF LOC to be eligible
for CB services.

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
97 | P a g e
13. Primary Freedom of Choice (PFOC): The form included in the Allocation Packet that allows a
registrant to confirm his or her interest in pursuing the opportunity to apply for CB services.
14. Self-Directed Community Benefits (SDCB): CB services offered to a member who is able to and who
chooses to self-direct his or her CB services.
15. Withdrawal Form: The form that is contained in the Allocation Packet that allows a registrant to
withdraw his or her request to apply for CB services.

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
98 | P a g e
7.3. Nursing Facility Level of Care
NF LOC determinations for CB members:
All individuals receiving CB services must meet NF LOC eligibility requirements initially and annually
thereafter, unless eligible for continuous NF LOC.
Members who have a full Medicaid COE do not need an allocation to access CB. The member must
contact his/her MCO Care Coordinator to request an NF LOC evaluation to determine if medical
eligibility can be established. The Care Coordinator must schedule a CNA, to be completed in the
member’s home. The CNA must be scheduled within 30 calendar days of the member’s request for CB
services.
Once medical eligibility is established, the member must be reevaluated for NF LOC eligibility annually.
The MCO Care Coordinator must begin the NF LOC evaluation process (i.e., schedule the CNA) 120
calendar days prior to the existing NF LOC expiration date. The MCO must send 120 and 60 calendar day
reminder letters to the member. If the member has not complied with the CNA process and there are
only 30 calendar days left before the NF LOC expiration date, the MCO will send a Notice of Action to
the member explaining that CB services will expire in 30 calendar days due to member not complying
with the NF LOC evaluation process. The NOA must advise the member that if CB services are desired,
the CNA process must be completed. The notice must include member appeal and fair hearing rights.
Individuals requesting CB services who are not eligible for a full Medicaid COE, must place their name on
the Central Registry as described later in this section of the Manual.
7.4. Continuous NF LOC for Certain Eligible Members
CB members who meet the following criteria may be eligible for a continuous NF LOC. The MCO is
required to complete the CNA as outlined in Section 4 of the Manual.
• The member must have had an approved NF LOC for the prior three years.
• The approved NF LOC must be related to the member’s primary diagnosis.
• A continuous NF LOC status must be approved initially and annually by the MCO Medical Director
and documented in the member’s file.
• The member’s PCP must annually complete and sign a form that documents the member’s ongoing
ADL deficits related to the member’s primary diagnosis. The MCO must maintain this form in the
member’s file.

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
99 | P a g e
• The MCOs will be required to regularly report to HSD the number of members with approved
continuing NF LOC status and other related information.
Conditions that may warrant a continuous NF LOC include, but are not limited to:
• Cerebral Palsy;
• Chronic Obstructive Pulmonary Disease (end stage);
• Cystic Fibrosis;
• Dementias (such as Alzheimer’s, Multi-Infarct, Lewy Body);
• Developmental Disability (such as microcephaly and severe chromosomal abnormalities);
• Neurodegenerative Diseases (such as ALS, muscular dystrophy, multiple sclerosis,);
• Paralysis secondary to Cerebral Vascular Accident;
• Parkinson’s Disease;
• Paraplegia;
• Quadriplegia;
• Spina Bifida;
• Paralysis secondary to severe spinal cord injury; or
• Ventilator Dependent.
7.5. External Audits of NF LOC Determinations
HSD or its designee will audit a sample of each MCO’s NF LOC determinations to ensure the LOC criteria
are being appropriately applied by the MCOs. Each MCO will submit a universe of NF LOC
determinations to HSD or its designee for review. HSD or its designee will meet with the MCO to discuss
audit findings.
7.6. MCO Internal Audits of NF LOC Determinations
Each MCO will conduct internal random sample audits of both facility and CB NF LOC determinations
based on HSD NF LOC instructions and tool guidelines each quarter. The audit will include, at a
minimum: accuracy, timeliness, training documentation of reviewers, and consistency of reviewers. The
results and findings will be reported to HSD by the 7th day of the month following the end of the quarter
along with any Quality Performance Improvement Plan via DMZ (NF LOC reviews folder). The naming
convention for the results and findings file is MCO, quarter, year, internal audit results. For example, if

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
100 | P a g e
the MCO is submitting first quarter reviews, the file shall be named “MCO-name.Q1.18.internal audit
results.”
7.7. Registration for the CB for NOME Members
The ALTSD/ADRC (referred to as ADRC from this point forward) manages the Centennial Care Central
Registry by enrolling individuals, completing the pre-assessment, assigning the category of registration,
and sending Exception requests to HSD/MAD/LTSSB. Any individual has the right to place his or her
name on the Central Registry if: it has been determined the individual is not currently Medicaid eligible,
or current Medicaid shows a termination date, or the individual has applied for Medicaid and received a
denial.
At the time of registration, if the individual has a Medicaid COE entitling the individual to full Medicaid
benefits, the ADRC shall refer the individual to his or her MCO.
Any individual has the right to register for multiple waivers at the same time. Individuals may place their
name on the Central Registry by calling or appearing in person at the ADRC. An individual must be a
resident of the state of New Mexico in order to be registered. Residency is determined based on the
State’s eligibility rule for Medicaid. It is the individual’s responsibility to inform the ADRC of any changes
in address and/or telephone number so the Central Registry can be updated. Individuals are also
encouraged to contact the ADRC if they have significant changes in their health condition or living
situation. These circumstances may affect their type of registration.
Individuals should note that the Central Registry records information such as: the applicant’s
demographic information, the date of registration, and the applicant’s specific LTC needs. Individuals are
also required to complete a pre-assessment which aids the ADRC staff in directing the applicant to the
appropriate category of registration: Community Reintegration, Expedite, and Regular. The registration
types are defined as follows:
• Community Reintegration – provides individuals the opportunity to move out of an NF and back
into the community for a registrant who is residing in an NF at the time of registration. In order to
be eligible for CRI, the registrant must have resided in an NF for 90 consecutive days. Within the 90
consecutive days, the registrant may have been hospitalized and returned to the NF for the
remainder of the 90 days. If the 90-day stay was confined to only a hospital stay and the client was
never in a NF this does not qualify them for a CRI, they would have to be evaluated under another
allocation type such as Regular or Exception. The individual participating in the community

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
101 | P a g e
reintegration process must be capable of comprehending the decisions being made or have a
primary caregiver or legal guardian that understands the options. The individual must not require
ABCB services 24 hours per day in his or her home. The intent of CRI is to assist the individual to
become integrated into his/her community and be as independent as possible. The MCO must be
able to ensure a reasonable level of health and safety for the member while ABCB services are being
provided. ABCB services must be cost-effective and must not exceed the average annual per capita
costs of NF services as determined by HSD.
CRI registration for the ABCB can be completed by calling the ADRC. Once a continuous 90-day stay
is confirmed by the HSD/MAD/LTSSB and funding is available, a community re-integration allocation
is granted. The HSD/MAD/LTSSB sends the allocation packet to the registrant/representative. The
allocation paperwork must be returned to the HSD/MAD/LTSSB within 45 calendar days or the
allocation will be closed, and the registrant will need to re-register for placement on the Central
Registry and wait for another allocation. If an extension is needed to complete the packet,
HSD/MAD/LTSSB must be notified to grant the extension (see “The Allocation Process: Timelines for
the Allocation Packet”).
Once the PFOC and HSD 100 are received by HSD/MAD/LTSSB, the allocation is processed (see “The
Allocation Process: Processing PFOCs”). Once the allocation has been granted, it is the MCO’s
responsibility to ensure services are authorized and in place prior to discharge to ensure a safe and
appropriate discharge.
The MCO must contact the registrant within five business days of receipt of the PFOC to schedule an
initial assessment to determine medical eligibility. The assessor explains the CRI process to the
registrant/representative. If the registrant/representative wishes to remain in the institution, the
Withdrawal Form must be completed, signed and mailed to HSD/MAD/LTSSB. If the
registrant/representative wishes to proceed with the eligibility process, the MCO proceeds with the
medical eligibility process.
• Expedite (EXP) – a registrant who has an urgent need for care. To be eligible, the registrant must:
o Be pre-assessed by the ADRC to require total assistance in at least three categories of ADLs; and
o Score a minimum of 48 points on the ADRC pre-assessment.
• Regular (REG) – a registrant who does not meet the criteria for any of the other registration types,
based upon the ADRC pre-assessment.

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
102 | P a g e
Individuals may request an Exception to their category of registration and request an Expedited
allocation to the ADRC, under extreme circumstances. The ADRC will send the request to the
HSD/MAD/LTSSB who will consider issuing an Expedited allocation. The following are examples of
circumstances that may warrant an Exception request for an Expedited allocation:
o To ensure continuity of care, an individual was receiving CBs under a full Medicaid category of
assistance and his or her full Medicaid eligibility terminated. An individual must inform the ADRC
that he or she has lost full Medicaid and was receiving CBs. The request must be made to ADRC
within six months of termination of the full Medicaid category of assistance;
o An individual who was in an NF for 90 consecutive calendar days and was not registered for a
CRI allocation prior to discharge. The request must be made to ADRC within 30 calendar days
after discharge from the NF;
o An individual is residing in a Medicaid approved Assisted Living Facility, has been paying out of
pocket, and can no longer afford the private pay;
o An individual who has been diagnosed as having Acquired Immunodeficiency Syndrome (AIDS)
or Aids-Related Complex (ARC);
o An individual who no longer qualifies for the MFW and is ventilator dependent; or
o In rare cases, an individual with an extreme health and safety risk.
7.8. Allocation Process
The ADRC manages the Central Registry by enrolling individuals, completing the pre-assessment, and
sending Exception requests to HSD/MAD. The HSD/MAD/LTSSB manages the allocation process by
mailing Allocation Packets to registrants and forwarding completed allocation paperwork to HSD/ISD
and to the MCO. In order to facilitate the allocation process, the ADRC shall:
• Maintain accurate registrant information in the Central Registry, including coding of category of
registration for each registrant; and
• Change a registrant’s category of registration, if the ADRC obtains information that justifies the
change (e.g., a registrant leaves an NF before the 90-day requirement is met).
When the HSD/MAD Director determines a regular allocation should be released, the allocation process
begins by sending the Allocation Packet to the registrant. The registrant is notified there is an allocation
available and is asked to respond by returning a completed PFOC and HSD 100, or a Withdrawal Form.
The Allocation Packet contains the following:

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
103 | P a g e
• LOI;
• PFOC;
• Withdrawal Form;
• HSD 100 “Medicaid Application for Assistance”;
• CBs Informational Brochure; and
• Business Reply envelope addressed to HSD/MAD/LTSSB.
Timeframes for the Allocation Packet:
• The registrant has 45 calendar days to return either a completed PFOC and HSD 100, or a
Withdrawal Form to HSD/MAD/LTSSB.
• The registrant may request a one-time extension to return the PFOC and HSD 100, or Withdrawal
Form by contacting the HSD/MAD/LTSSB, and if requested, it shall be granted for up to 30 calendar
days. Any additional time (extensions) requested by the registrant must be made directly to
HSD/MAD/LTSSB for approval.
• If there is no response to the Allocation Packet either after the original 45 calendar days or after the
expiration of any granted extensions, HSD/MAD/LTSSB shall send a closure letter to the registrant’s
mailing address on file.
Processing PFOCs:
Once HSD/MAD/LTSSB receives the PFOC and the HSD 100, HSD/MAD/LTSSB will review the documents
to ensure they are complete and signed by the registrant.
• If the PFOC is not complete and/or signed, the PFOC will be returned to the registrant, identifying
the information required, and providing the registrant up to 30 calendar days to complete and
return the form. Failure to return the PFOC within the 30-calendar days will result in closure upon
the 45th day, as described herein.
• If the PFOC and HSD 100 are completed and signed, HSD/MAD/LTSSB will process them by sending:
o A NOA letter to the registrant;
o A copy of the NOA, PFOC, and HSD 100 to the HSD/ISD Eligibility system; and
o A copy of the PFOC to the registrant’s MCO.

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
104 | P a g e
7.9. Eligibility
Once the PFOC and HSD 100 have been distributed to HSD/ISD and the MCO, HSD/MAD/LTSSB’s
“Processing PFOCs” is complete. HSD/MAD/LTSSB is unable to assist with medical or financial eligibility.
Registrants must meet two types of eligibility, initially and annually, to receive and continue receiving
CBs:
• Medical Eligibility: The medical eligibility determination is completed by the MCO. In order to be
medically eligible, the registrant must meet an NF LOC. In addition, the CNA must indicate that the
registrant has a need for CBs.
o The MCOs must have established procedures for their call centers to resolve issues and address
inquiries from those who are allocated, but not yet fully enrolled with the MCO, because the
NFLOC determination has not yet been completed. The MCO must be able to identify these
individuals in their systems within two (2) business days of receipt of the PFOC or 112 trigger
and be able to address questions and concerns from these future members who are newly
allocated and may be enrolled in the MCO when eligibility is complete.
o The NF LOC shall be determined and transmitted to ASPEN within 40 calendar days from the
MCO’s receipt of the PFOC.
o The MCO shall submit the NF LOC determination to HSD/ISD, via the interface file, within 5
business days of the NF LOC determination so it can be used by HSD/ISD to complete the
eligibility process.
o If there is an existing NF LOC determination, the MCO shall submit the NF LOC effective dates to
HSD/ISD, via the interface file, within 5 business days of the MCO’s receipt of the PFOC so it can
be used by HSD/ISD to complete the eligibility process. A new NF LOC does not need to be
determined by the MCO, unless there are less than 120 calendar days remaining on the existing
NF LOC.
o The MCO shall submit the NF LOC effective dates and applicable SOC of ADB (Agency Directed
Services) to the Omnicaid system, via the interface file, within 5 business days of receiving the
member’s initial enrollment on the Enrollment Roster file.
o If an individual is under the age of 65 and has not been deemed disabled by the Social Security
Administration (SSA), they must be evaluated by MAD’s Disability Determination Unit to
establish whether they meet the disability criteria according to SSA guidelines. Current medical
records regarding the individual’s disability must be provided to ISD.

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
105 | P a g e
• Financial Eligibility: In order to be financially eligible, income and assets must be below the
Institutional Care Medicaid (ICM)/Waiver maximum allowable amount. In addition, all other
financial and non-financial eligibility requirements must be met as determined by HSD/ISD.
Once eligibility is approved by HSD/ISD, the registrant’s ABCB services will be provided based on the CNA
conducted by the member’s MCO. Although the COE for the CB Waiver is approved, CB services will not
begin until the CCP is in place. CB services are not approved retroactively.
The member must participate in the ABCB service delivery model for a minimum of 120 calendar days
before the member requests a switch to the SDCB service delivery model. A member must contact their
MCO Care Coordinator to discuss the switch from ABCB to SDCB. The CB services are described in
Sections 8 and 9 of the Manual.
7.10. Closing/Inactivating an Allocation
An allocation will be inactivated by HSD/MAD/LTSSB if one of the following occurs:
• The registrant returns a signed Withdrawal Form;
• The registrant does not return the PFOC within the required timeframes;
• The ADRC or HSD/MAD/LTSSB is informed the registrant intends to remain in the NF;
• The ADRC or HSD/MAD/LTSSB is informed the registrant is no longer a resident of the State of New
Mexico;
• The ADRC or HSD/MAD/LTSSB has been notified the registrant has expired;
• The Allocation Packet is returned as undeliverable and no other contact information is available; or
• The registrant has a full Medicaid category of eligibility (COE) and has access to CB services through
their MCO.
7.11. Registrant Notice Requirements
The registrant is notified by letter in the following circumstances:
• New registration (mailed by the ADRC);
• When the State is unable to contact the registrant by telephone;
• When an allocation becomes available for the registrant (Allocation Packet);
• When an allocation is complete (NOA);
• When a registration is closed/inactivated for any reason other than a completed allocation; and

Section 7: Community Benefits
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
106 | P a g e
• When the State has been notified that the registrant is deceased, a letter will not be sent to the
registrant or the registrant’s representative.
7.12. Undeliverable Notice
It is the registrant’s responsibility to inform the ADRC of any change in address and/or telephone
number. If a letter is returned to the State as undeliverable, HSD/MAD/LTSSB shall review the
registrant’s record to determine an alternate address and attempt to call the registrant or the
registrant’s representative to verify a correct mailing address. If HSD/MAD/LTSSB cannot obtain the
registrant’s address, the registrant’s Central Registry record will be inactivated due to the inability to
contact the registrant. HSD/MAD/LTSSB shall document the reason the registration has closed, the
specific attempts made to contact the registrant, and the date(s) of attempts, in the registrant’s journal
notes in the Central Registry.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
107 | P a g e
8. Agency-Based Community Benefits (ABCB)
8.1. General Information
The ABCB is intended to provide a community-based alternative to institutional care.
Members selecting the Agency-Based model have the choice of the consumer delegated or consumer
directed models for PCS.
HCBS shall meet the following requirements:
• Are integrated and support full access of members receiving Medicaid HCBS to the greater
community, including opportunities to seek employment, and work in competitive integrated
settings, engage in community life, control personal resources, and receive services in the
community, to the same degree of access as individuals not receiving Medicaid HCBS;
• Are selected by the member from among setting options including non-disability specific settings.
The setting options are identified and documented in the person-centered care plan and are based
on the member’s needs and preferences;
• Ensure a member’s rights of privacy, dignity and respect, and freedom from coercion and restraint;
• Optimize, but do not regiment, member’s initiative, autonomy, and independence in making life
choices, including but not limited to, daily activities, physical environment, and with whom to
interact; and
• Facilitate member choice regarding services and supports, and who provides them.
HSD will take the following factors into account when determining whether a setting may have the
effect of isolating members receiving Medicaid HCBS from the broader community of members not
receiving HCBS:
o Due to the design or model of service provision in the setting, members have limited, if any,
opportunities for interaction in and with the broader community, including with individuals
not receiving Medicaid funded HCBS. Opportunities as well as identified supports to provide
access to and participation in the broader community, should be reflected in both the
member’s person-centered care plans and policies and practices of the provider setting in
accordance with 42 CFR 441.301(c)(1)(3) and (4)(vi)(F), 42 CFR 441.530(a)(1)(vi)(F) and
441.540, and 42 CFR 441.710(a)(1)(vi)(F) and 441.725;
o The setting restricts member choice to receive services or to engage in activities outside of
the setting; or

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
108 | P a g e
o The setting is physically located separate and apart from the broader community and does
not facilitate member opportunity to access the broader community and participate in
community services, consistent with the member’s person-centered care plan.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
109 | P a g e
8.2. Definitions
1. Adult: Individuals who are 21 years of age or older.
2. Allocation: Funding becomes available to serve additional individuals on the 1115 waiver who are
NOME.
3. Annual: The 12-month period covered by a Comprehensive Care Plan, except where otherwise
stated.
4. Adult Protective Services Division (APS): APS Division of the Aging and Long-Term Services
Department.
5. Care Coordinator (CC): The individual responsible for coordinating a member’s services in the
managed care program.
6. Child: An individual under 21 years of age.
7. Community Re-integration: Provides individuals the opportunity to move out of a SNF into a
community placement, after a 90-day continuous stay.
8. Comprehensive Care Plan (CCP): means a comprehensive plan of services that meets the
member’s physical, behavioral and long-term needs.
9. Electronic Visit Verification (EVV): EVV is a computer-based system that electronically verifies the
occurrence of authorized personal care service visits by electronically documenting the precise time
and location where a service delivery visit begins and ends.
10. Face-to-Face: Being in the physical presence of the individual who is receiving services.
11. Human Services Department (HSD): Designated by CMS as the Medicaid administering agency in
New Mexico. HSD is also responsible for operating the ABCB Services for populations that meet the
NF LOC.
12. Interdisciplinary Team (IDT): IDT, consisting of the member, the legal AR, the family, service
providers and other people invited by the member and the legal authority representative, if
applicable.
13. Immediate Family Member: Father (includes natural or adoptive father, father-in-law, stepparent),
mother (includes natural or adoptive mother, mother-in-law, stepparent), brother (includes
half-brother, step-brother), sister (includes half-sister, step-sister), son or daughter, step-son or step
daughter, adoptive son or daughter, natural grandfather, and natural grandmother and spouse
relationship to the individual.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
110 | P a g e
14. Incident Report: Required form for documenting all reportable incidents of abuse, neglect,
exploitation, death, expected and unexpected, environmental hazard, law enforcement intervention
and emergency services.
15. Medical Assistance Division (MAD): The MAD, New Mexico Human Services Department.
16. Natural Supports: Supports not paid for with Medicaid funds that assist the individual to attain the
goals as identified on the Comprehensive Care Plan. Individuals who provide natural supports are
not paid staff members of a service provider, but they may be planned, facilitated, or coordinated in
partnership with a provider.
17. Nursing Facility Level of Care (NF LOC): The member’s functional level is such that two or more ADL
cannot be accomplished without consistent, ongoing, daily provision, of some or all of the following
levels of service: skilled, intermediate or assisted. A member must meet an NF LOC to be eligible for
NF placement and CB services.
18. Parent: Natural or adoptive mother or father, or step-mother, step-father.
19. Person-Centered Care Plan (PCCP): A procedural plan that describes the provision of specified
activities and oversight on a routine basis in order to safeguard the health of the member.
20. Primary Caregiver: The person who takes primary responsibility for someone who cannot care-fully
for himself or herself. The primary caregiver may be a family member, a trained professional or
another individual.
21. Relatives: Immediate family members such as the parent of an adult, a sibling, grandparent, aunt,
uncle, etc. but not the parent of a minor child or a spouse.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
111 | P a g e
8.3. ABCB Services Requirements
These requirements apply to the services provided through the Medicaid 1115 Waiver for members who
meet the eligibility criteria for HCBS, ABCB. These requirements clarify, interpret, and further enforce
8.308.12 NMAC, Managed Care Program, Community Benefit.
• ABCB providers must meet all Federal requirements for HCBS providers, including the Final HCBS
Settings Rule. All ABCB providers must be enrolled as an active Medicaid approved provider
type 363 (Community Benefit Provider) and have HSD/MAD approval to provide that service. All
incomplete applications submitted to the HSD/MAD Long-Term Services and Supports Bureau
(LTSSB) shall be rejected and not considered for review until a complete application is
submitted.
The requirements address each service covered by the ABCB. Members served through this program will
expect to receive services that meet these requirements. Centennial Care MCOs must contract with an
active ABCB Medicaid approved provider type 363 that has approval from HSD/MAD to provide that
service before rendering CBs to members. Eligible ABCB providers are those that have been approved
and certified by the HSD/MAD/LTSSB, per 8.308.2.9 NMAC Managed Care Program, Provider Network.
Each MCO must ensure that it has an adequate statewide provider network for all ABCB Services.
These requirements define the services offered as approved by CMS. The ABCB services are supplement
to the member’s natural supports and are not intended to replace family supports. The ABCB is not a
24-hour service. The services are designed to increase independence and achieve personal goals while
providing care and support to enable individuals to live as active members of the community while
ensuring their health and safety. The purpose of this program is to provide assistance to individuals that
require LTSS so they may remain in the family residence, in their own home, or in community
residences. This program serves as an alternative to placement in an NF. The ABCB services are
implemented in accordance with the Person-Centered Care Plan (PCCP) and/or Comprehensive Care
Plan (CCP) as developed by the member and the MCO Care Coordinator. The PCCP must revolve around
the ABCB member and reflect his/her chosen lifestyle, cultural, functional, and social needs for
successful community living.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
112 | P a g e
8.4. ABCB Covered Services
All ABCB services are subject to the approval of the MCO/UR. Below is a list of ABCB covered services for
members in ABCB, followed by detailed service descriptions:
• Adult Day Health;
• Assisted Living;
• Behavior Support Consultation;
• Community Transition Services;
• Emergency Response;
• Employment Supports;
• Environmental Modifications;
• Home Health Aide;
• Nutritional Counseling;
• Personal Care – Consumer Directed;
• Personal Care – Consumer Delegated;
• Private Duty Nursing (PDN);
• Nursing Respite;
• Respite; and
• Skilled Maintenance Therapy Services.
o Occupational Therapy for Adults
o Physical Therapy for Adults
o Speech Therapy for Adults
8.5. Adult Day Health Services
Adult Day Health Services provide structured therapeutic, social and rehabilitative services designed to
meet the specific needs and interests of ABCB members as determined by the PCCP incorporated into
the CCP. Adult Day Health settings must be integrated and support full access of members receiving
Medicaid HCBS to the greater community, engage in community life, control personal resources, and
receive services in the community, to the same degree of access as individuals not receiving Medicaid
HCBS. The services are generally provided for two or more hours per day on a regularly scheduled basis,
for one or more days per week, by a licensed Adult Day Care Center, that offers health and social

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
113 | P a g e
services to assist members to achieve optimal functioning. Meals provided as part of this service shall
not constitute a “full nutritional regime” (3 meals per day). Transportation to and from the Adult Day
Care Center must be coordinated by the Adult Day Care provider.
PDN services and Skilled Maintenance Therapies (physical, occupational, and speech) may be provided
in conjunction with Adult Day Health services, by the Adult Day Care provider or by another qualified
provider. PDN and therapy services must be provided by licensed nurses and therapists. The PDN and
Skilled Maintenance Therapies must be provided in a private setting at the facility.
Scope of Services/Requirements:
• The health, safety, and welfare of the member must be the primary concern of all activities and
services provided. Provider staff must supervise all activities. Activities provided by the Adult Day
Care Center are included in the negotiated rate with the MCO and are not billed separately. Specific
services may include the following:
o Coordination of transportation to and from the Adult Day Care center;
o Activities that promote personal growth;
o Activities that enhance the member’s self-esteem by providing opportunities to learn new skills
and adaptive behaviors;
o Supervision of self-administrated medication as determined by the New Mexico Nurse Practice
Act;
o Activities that improve capacity for independent functioning;
o Activities that provide for group interaction in social and instructional programs and therapeutic
activities;
o Personal Care Services (PCS);
o Meals that do not constitute a “full nutritional regime” of three (3) meals per day;
o Intergenerational experiences;
o Involvement in the greater community; and
o Providing access to community resources as needed.
• Activities shall be planned by the member, family, caregivers, volunteers, staff and other interested
individuals and groups. The provider must ensure safe and healthy conditions for activities inside or
outside the facility.
Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
114 | P a g e
• An IDT meeting for each member will occur at least quarterly to review ongoing progress of direct
services and activities. The PCCP will be adjusted as necessary to meet the needs of the member at
the quarterly meeting or at other times as needed. A PCCP will be developed with identified goals
and measurable objectives. It will be attached to or incorporated into the CCP.
• All activities must be supervised by provider staff. Members must never be left unattended. Adult
Day Care Center staff must be physically present with the member(s) at all times.
• Activities must be designed to meet the needs of the member and enhance the member’s
self-esteem by providing opportunities to:
o Learn new skills and adaptive behaviors;
o Improve or maintain the capacity for independent functioning; and
o Provide for group interaction in social and instruction programs and therapeutic activities.
Provider Requirements/Qualifications:
• Adult day health services may be provided by eligible adult day care agencies.
• Adult Day Care Centers must maintain (no gaps in licensure) a full permanent license by Department
of Health (DOH) as an adult day care facility pursuant to 7 NMAC 13.2. Adult day health facilities must
meet all requirements and regulations set forth by DOH as an adult day care facility pursuant to 7
NMAC 13.2. Provisional licenses will not be accepted.
• Adult Day Care Centers must comply with the provisions of Title II and III of the American’s with
Disabilities Act (ADA) of 1990, P.L. 101-336 (42 U.S.C. Section 12101, et seq.).
• In order to be approved and certified by the HSD/MAD/LTSSB Adult Day Care Centers must be
operating with a permanent license. All incomplete applications submitted to the HSD/MAD/LTSSB
shall be rejected and not considered for review until a complete application is submitted.
• Adult Day Care Centers must comply with all applicable cities, county or state regulations governing
transportation services, if providing transportation services to its members.
• Adult Day Care Centers must comply with the HSD/MAD requirements including but not limited to:
OSHA training requirements; incident management reporting; criminal background check (CBC); labor
laws, etc.
• Adult Day Care Centers must make appropriate provisions to meet the needs of adults who require
special services as indicated in the member’s Care Plans.
• The MCO will provide a copy of the CCP to the Adult Day Care Services Provider.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
115 | P a g e
• A written Adult Day Health Services PCCP will include the assessment of the special needs, the
interventions to meet those needs, and evaluation of the plan, with changes as needed. The PCCP will
be provided to the MCO Care Coordinator and must be incorporated into the member’s CCP.
• The provider must be culturally sensitive to the needs and preferences of the member.
Communicating in a language other than English may be required.
Reimbursement
Billing is on an hourly basis and is accrued to the nearest quarter of an hour. Training on
member-specific issues is reimbursable and included in the MCO negotiated hourly rate. General
training requirements are an administrative cost and not billable. Reimbursement for adult day health
services will be based on the negotiated rate with the MCO. Providers of this service have the
responsibility to review the prior authorizations issued from the MCO to ensure the information on the
prior authorization for their services is correct. If the provider identifies an error, they will contact the
MCO immediately to have the error corrected.
Limits or Exclusions
The member must attend the Adult Day Care Center for a minimum of two hours per day for one or
more days per week and the frequency (number of days per week) of attendance at the center must be
included in the individual’s PCCP and the CCP.
8.6. Assisted Living Facility (ALF)
Assisted living facilities offer residential services that provide a homelike environment which may be in a
group setting with individualized services designed to respond to the member’s needs as identified by
the member, provider and the Care Coordinator. A PCCP is developed with the member that needs
services in the ALF and incorporated in the CCP. Assisted living services include assistance with Activities
of Daily Living (ADLs) (i.e., ability to perform tasks that are essential for self-care, such as bathing,
feeding oneself, dressing, toileting, and transferring) and assistance with Instrumental Activities of Daily
Living (IADLs) (i.e., ability to care for household and social tasks to meet individual needs within the
community). Assisted living is based on the following fundamental principles of practice:
• Offering quality care that is personalized for the member’s needs;
• Fostering independence for each member;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
116 | P a g e
• Treating each member with dignity and respect;
• Promoting the individuality of each member;
• Allowing each member choice in care and lifestyle;
• Protecting each member’s right to privacy;
• Nurturing the spirit of each member;
• Involving family and friends in care planning and implementation;
• Providing a safe residential environment; and
• Providing safe community outings or activities.
Scope of Services/Requirements:
• Core services provide assistance to the member in meeting a broad range of activities of daily living.
Specific services may include the following:
o Personal Hygiene;
o Dressing;
o Eating;
o Socialization;
o Opportunities for individual and group interaction;
o Housekeeping;
o Laundry;
o Transportation;
o Meal preparation and dining;
o 24-hour, on-site response capability to meet scheduled or unpredictable member needs;
o Capacity to provide on-going supervision of the ABCB member within a 24-hour period;
o Coordination of access to services not provided directly;
o Participation in the IDT meetings for development of the PCCP;
o Implementation of the PCCP to meet the member’s needs, evaluation for effectiveness, and
adaptation as needs change;
o Services provided to a resident at an ALF are pursuant to the PCCP, developed by the member,
provider and the MCO Care Coordinator; and/or

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
117 | P a g e
o Other direct services (not listed above as core services) that provide assistance to the member
in meeting a broad range of ADLs. Direct services may be provided by the ALF or may be
provided by another ABCB active, Medicaid approved type 363 provider with HSD/MAD
approval to provide that service. These direct care providers must be identified on the
member’s PCCP, that is separate from the CCP, and might include:
▪ PDN services for Adults (see the Scope of Services/Requirements for PDN); and/or
▪ Skilled Maintenance Therapies for Adults (see the Scope of Services/Requirements for
Skilled Maintenance Therapies).
Provider Requirements/Qualifications:
• Assisted Living Services must be provided by an active, Medicaid approved provider type 363
Assisted Living Facility (ALF).
• ALF must maintain (no gaps in licensure) a full permanent license by Licensing and Certification
Bureau, Division of Health Improvement/Department of Health. Provisional licenses will not be
accepted.
• ALF must comply with the provisions of Title II and III of the ADA of 1990, P.L. 101-336 (42 U.S.C.
Section 12101, et seq.).
• The ALF must be located in the State of New Mexico.
• In order to be approved and certified by the HSD/MAD/LTSSB, ALF must be holding and operating
with a fully approved permanent license. All incomplete applications submitted to the
HSD/MAD/LTSSB shall be rejected and not considered for review until a complete application is
submitted.
• Assisted Living providers must ensure that personnel providing direct services (directly employed by
the ALF or through a contract for services) meet all requirements established by HSD/MAD for direct
services such as, PDN, and skilled maintenance therapies (see Provider Requirements/Qualifications
for each separate service).
• Assisted Living providers are required to maintain staffing ratios and patterns that will meet the
member’s needs as identified in the PCCP and the CCP.
• Assisted Living providers will develop a PCCP for each member based on the assessment of the
needs of the member and include strategies to meet those needs. The PCCP must be evaluated for

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
118 | P a g e
effectiveness and revised as the needs of the member change. The PCCP is separate and
incorporated into the CCP.
• Assisted Living providers will develop a written agreement with each ABCB member residing in their
ALF. This agreement will detail all aspects of care to be provided including identified risk factors.
Members shall be afforded the same protections from eviction as all tenants under landlord law of
state, county, city or other designated entity. It will also include the financial agreement regarding
the cost of room and board and the funding sources. A copy of this agreement and any later revisions
must be forwarded to the MCO Care Coordinator and must be maintained in the member’s file with
the MCO. The original is maintained in the member’s file at the assisted living residence.
• Assisted Living providers must meet all requirements set forth by the Licensing and Certification
Bureau/Department of Health. This would include the definition of a homelike environment
described below:
o Providers must meet the minimum, applicable qualifications set forth by the Licensing and
Certification Bureau of the Department of Health and HSD/MAD, including but not limited to:
labor/staffing rules and regulations; criminal background checks; employee abuse registry;
incident management reporting; OSHA training requirements, etc.
o Definition of Homelike Environment: A homelike environment must possess the following
structural features prior to the placement of the ABCB member. Meeting these
requirements is the financial responsibility of the Assisted Living provider:
• A minimum of 220 square feet of living space, including kitchen space for newly
constructed units. Rehabilitated units must provide a minimum of 160 square feet
of living space;
• A minimum of 100 square feet of floor space in each single bedroom. Closet and
locker areas shall not be counted as part of the available floor space. Members must
have access to a separate common living area, kitchen and bathroom that are all
accessible for persons with a disability;
• A minimum of 80 square feet of floor space per member in a semi-private bedroom
(sharing a bedroom is the member’s choice only). Closet and locker areas shall not
be counted as part of the available floor space. Members must have access to a
separate common living area, kitchen and bathroom that are all accessible for
persons with a disability;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
119 | P a g e
• Kitchens must be furnished with a sink, a refrigerator, at least a two-burner stove
top or 1.5 cubic foot microwave oven;
• Each unit must be equipped with an emergency response system;
• Common living areas must be smoke free;
• Floor plans must be submitted to the HSD/MAD along with the Medicaid Provider
Participation Application or renewal; and
• In addition, CMS requires residential settings located in the community to provide
members with the following:
o Private or semi-private bedrooms including decisions associated with sharing
a bedroom; Full access to typical facilities in a home such as a kitchen with
cooking facilities, small dining areas; All members must be given an option to
receive HCBS in more than one residential setting appropriate to their needs;
Private or semi-private bathrooms that include provisions for privacy;
Common living areas and shared common space for interaction between
members, their guests, and other residents; Members must have access to
food storage or food pantry area at all times; Members must have the
freedom and support to control their own schedules regarding their day to
day activities including having visitors of their own choosing at any time,
when and what to eat, in their home and in the community; and Members
will be treated with respect, choose to wear their own clothing, have private
space for their personal items, have privacy to visit with friends, family, be
able to use a telephone with privacy, choose how and when to spend their
free time, have easy access to resources and activities of their choosing in
the community.
▪ In provider owned or controlled residential settings, the following additional conditions will
be provided to members: Privacy in sleeping or living unit; Units have lockable entrance
doors, with members and appropriate staff having keys to doors; Members share units only
at the member’s choice and have a choice of roommates in that setting; Members have
freedom to furnish and decorate sleeping or living units as specified in the lease or
agreement; and the setting is physically accessible to the member.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
120 | P a g e
▪ Any modification of the above conditions must be supported by a specific need and justified
and documented in the PCCP to address the following:
• Identify a specific and individualized assessed need;
• Document the positive interventions and supports used prior to any modifications to
the PCCP;
• Document less intrusive methods of meeting the need that have been tried but did not
work;
• Include a clear description of the condition that is directly proportionate to the specific
assessed need;
• Include regular collection and review of data to measure the ongoing effectiveness of
the modification;
• Include established time limits for periodic reviews to determine if the modification is
still necessary or can be terminated;
• Include the informed consent of the member; and
• Include an assurance that interventions and supports will cause no harm to the
member.
Reimbursement
Billing for Assisted Living services is based on a daily rate which includes core services such as personal
care. Reimbursement for Assisted Living services will be based on the negotiated rate with the MCO.
Providers of service have the responsibility to review the prior authorizations issued from the MCO to
ensure the information on the prior authorization for their services is correct. If the provider identifies
an error, they must contact the MCO immediately to have the error corrected. An ALF may not bill the
MCO for services that the prior authorization does not cover.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
121 | P a g e
Limits or Exclusions
Assisted Living services includes core services, such as, but not limited to: personal care, transportation
and meal preparation. These services cannot be billed separately. ALF services do not include the
following ABCB services:
• Personal care services (billed separately);
• Respite;
• Environmental Modifications; and
• Emergency Response or Adult Day Health.
The Assisted Living provider is responsible for all of these services in the ALF. Therefore, billing for these
services in addition to the Assisted Living services would constitute duplication of services. Assisted
Living services require a prior authorization from a Centennial Care MCO and will not be approved
retro-actively.
• Room and Board
o The ABCB does not reimburse for room and board costs for the member (such as rent, groceries,
etc.);
o Room and board rates billed to the ABCB members must be reported to the HSD/MAD along
with the Medicaid Provider Participation Agreement (PPA) application and renewal prior to the
provision of assisted living services by the provider agency. Any subsequent changes to those
rates must also be forwarded to the HSD/MAD when they occur;
o The provider must comply with all state and Federal guidelines regarding the establishment of
room and board rates to the ABCB services recipients; and
o Training on member specific issues is reimbursable and is included in the daily rate negotiated
with the MCO.
• Non-Billable Activities
o Assisted Living providers will not bill the MCO for Room and Board;
o General training requirements are an administrative cost and are not billable; and
o The Provider will not bill when a member is hospitalized or in an institutional care setting.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
122 | P a g e
8.7. Behavior Support Consultation (BSC)
A Behavior Support Consultant is a licensed professional as specified by applicable State laws and
standards. BSC services assist the member and his or her family as well as the direct support
professionals (DSP). BSC services for the member include:
• Assessments;
• Evaluations;
• Treatments;
• Interventions; and
• Follow-up services and assistance with challenging behaviors and coping skill development.
Services for the parents, family members, and DSPs include training in dealing with challenging
behaviors and assistance with coping skill development at home and in the community.
Scope of Services/Requirements:
BSC services are initiated when the MCO Care Coordinator identifies and recommends the service be
provided to the member/member’s representative and/or family member(s). The Care Coordinator is
responsible for including recommended units of BSC services into the CCP. Strategies, support plans,
goals and outcomes will be developed based on the identified strengths, concerns and priorities in the
PCCP.
BSC services include:
o Providing assessments, evaluations, development of treatment plans and interventions, training,
monitoring of the member/member representative, and planning modification as needed for
therapeutic purposes within the professional scope of practice of the BSC;
o Designing, modifying and monitoring the use of related activities for the member/member
representative and/or family member(s) that is supportive of the PCCP;
o Training families and DSPs in relevant settings as needed for successful implementation of
therapeutic activities, strategies, and treatments;
o Consulting with the IDT member(s), guardians, family, or support staff;
o Consulting and collaborating with the member’s PCP and/or other therapists and/or medical
personnel for the purposes of evaluation of the member developing, modifying or monitoring
BSC services for the member;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
123 | P a g e
o Observing the member/member representative in all relevant settings in order to monitor the
member’s status as it relates to therapeutic goals or implementation of BSC services and
professional recommendations; and
o Services may be provided in a clinic, home, or community setting.
Comprehensive Assessment Guidelines:
o The BSC must perform an initial comprehensive assessment for each member to give the
appropriate behavior support recommendations, taking into consideration the overall array of
services received by the member. A comprehensive assessment must be done at least annually
and when clinically indicated.
Attendance at the IDT Meeting:
o The BSC is responsible for attending and participating, either in person or by conference call in
IDT meetings convened for service planning;
o If unable to attend the IDT meeting, the BSC is expected in advance of the meeting to submit
recommended updates to the strategies, support plans, and goals and objectives. The BSC and
MCO Care Coordinator will follow up after the IDT meeting to update the BSC on specific issues;
and
o The BSC must document in the member’s clinical file the date, time, and any changes to
strategies, support plans, and goals and objectives as a result of the IDT meeting.
• Discharge Planning Documentation Requirements Include:
o Reason for discontinuing services (such as failure to participate, request from member/member
representative, goal completion, and/or failure to progress);
o Written discharge plan shall be provided to the member/member representative and the MCO
Care Coordinator by the BSC;
o Strategies developed with member/member representative that can support the maintenance
of behavioral support activities;
o Family and direct support professional training that is completed in accordance with the written
discharge plan; and
o Discharge summary is to be maintained in the member’s clinical file maintained by the BSC and
a copy is to be sent to the MCO Care Coordinator and distributed to the member/member
representative.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
124 | P a g e
Other Documentation Requirements:
o Documentation must be completed in accordance with applicable HSD/MAD and Federal
guidelines;
o All documents are identified by title of document, member name, and date of documentation.
Each entry will be signed with appropriate credential(s) and name of person making entry;
o Verified Electronic Signatures may be used. BSC name and credential(s) typed on a document is
not acceptable;
o All documentation will be signed and dated by the BSC providing services;
o A copy of the annual evaluation and updated treatment plan will be provided to the MCO Care
Coordinator within 10 business days following the IDT meeting. The treatment plan must
include intervention strategies, as well as frequency and duration of care. The goals and
objectives must be measurable;
o BSC progress/summary notes will include date of service, beginning/end time of service,
location of service, description of service provided, member/family/DSP response to service,
and plan for future service;
o The summary will include the number and types of treatment provided and will describe the
progress toward BSC goals using the parameters identified in the initial and annual treatment
plan and/or evaluation;
o Any modifications that need to be included in the PCCP must be coordinated with the MCO Care
Coordinator;
o Complications that delay, interrupt, or extend the duration of the program will be documented
in the member’s medical record and in communications to the physician/health care provider as
indicated;
o Each member will have an individual clinical file maintained by the provider; and
o Review physician/health care provider orders at least annually and as appropriate and
recommend revisions to the PCCP and CCP based on evaluation findings.
Agency Provider Requirements/Qualifications:
o BSC services must be provided by an active, Medicaid approved provider type 363 BSC provider.
o Employees of a provider agency who offer BSC services shall meet all the requirements under
this section of the policy.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
125 | P a g e
o The BSC agency must be able to demonstrate that all employees providing BSC, upon
employment and thereafter, maintain (no gaps in licensure) a full permanent license through
the appropriate board of licensure. Below identifies acceptable licensure for a BSC worker:
▪ Master’s degree from an accredited school for psychology, social work, counseling or
guidance program and maintain current permanent license as required by New Mexico State
Law.
▪ Acceptable licensure includes:
• New Mexico Licensed Psychologist or Psychologist Associate.
• New Mexico Licensed Independent Social Worker (LISW).
• New Mexico Licensed Master Social Worker (LMSW).
• New Mexico Licensed Professional Clinical Counselor (LPCC).
• New Mexico Licensed Marriage and Family Therapist (LMFT).
• New Mexico Licensed Mental Health Counselor (LMHC).
o Maintain a culturally sensitive attentiveness to the needs and preferences of members and their
families based upon culture and language. Communicating in a language other than English may
be required.
Individual Provider Requirements/Qualifications:
o BSC services must be provided by an active, Medicaid approved provider type 363 BSC provider.
o An individual providing BSC services must maintain a full permanent license through DOH and
shall meet all the requirements under this section of the policy. Provisional license is not
acceptable.
o Must meet all other requirements listed under Agency Provider Qualifications/Requirements.
Reimbursement:
BSC providers are responsible for providing clinical documentation that identifies the provider’s role
in all components of the provision of care, including assessment information, care planning,
intervention, communications, and care coordination and evaluation. There must be justification in
each member’s clinical record supporting medical necessity for the care and for the approved LOC
that will also include frequency and duration of the care. All services must be reflected in the PCCP
that is coordinated with the member/member’s representative and other caregivers as applicable.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
126 | P a g e
All services provided, claimed, and billed must have documented justification supporting medical
necessity and authorized by the MCO.
Billing is on an hourly basis and is accrued to the nearest quarter hour. Training on member specific
issues are reimbursable and included in the negotiated rate. Payment for BSC services through the
MCO is considered payment in full. Reimbursement for BSC services will be based on the MCO
negotiated rate. BSC providers have the responsibility to review and ensure the information on the
prior authorization for their services is current and correct. If the provider identifies an error, they
will contact the MCO immediately to have the error corrected.
Limits or Exclusions
HSD/MAD does not consider the following to be professional BSC duties and will not authorize
payment for:
o Performing specific errands for the member/member’s representative or family that is not
program specific;
o Friendly visiting;
o Financial brokerage services, handling of member’s finances or preparation of legal documents;
o Time spent on paperwork or travel that is administrative for the provider;
o Transportation of member/member’s representative;
o Pick up and/or delivery of commodities; and
o Other non-Medicaid reimbursable activities.
8.8. Community Transition Services (CTS)
CTS are non-recurring set-up expenses for adults 21 years old and older who are transitioning from an
SNF/NF to a living arrangement in the community where the person is directly responsible for his or her
own on-going living expenses.
This service is not intended to cover the household costs of the member’s natural supports.
Allowable expenses are those necessary to enable a member to establish a basic household. CTS are
furnished only when the member is unable to meet the expenses to initially establish his/her household
or when the services cannot be obtained from other sources. CTS may not be used to furnish or
establish living arrangements owned or leased by a service provider, except an ALF. Deposits to an ALF

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
127 | P a g e
are limited to $500.00. Services must be reasonable and necessary as determined by the MCO and
authorized in the transition and/or discharge plan.
Scope of Services/Requirements:
CTS must be reasonable and necessary as determined through the transition plan development process
and must be clearly identified in the discharge plan. Allowable expenses are those necessary to enable a
person to establish a basic household that do not constitute room and board and may include:
• Security deposits that are required to obtain a lease on an apartment or home. Monthly rental or
mortgage expenses are not covered; therefore, the member should have sufficient resources to pay
for the first month’s rent or mortgage as well as ongoing rent or mortgage costs;
• Essential household furnishings required to occupy and use a community domicile, including
furniture, window coverings, food preparation items, and bed/bath linens;
• Set-up fees or deposits for utility or service access, including telephone, electricity, heating and
water;
• Services necessary for the individual’s health and safety such as but not limited to, pest eradication
and one-time cleaning prior to occupancy;
• Moving expenses; and/or
• Fees to obtain a copy of birth certificate, identification card or driver’s license.
The Community Transition Agency (CTA) must be able to provide at least two of the following core
services:
o Information and referral;
o Independent living skills training;
o Peer counseling; and
o Individual and systems advocacy;
Provider Requirements/Qualifications:
The CTS may be provided directly by the MCO or contracted out to an active, Medicaid approved
provider type 363 CTA. The CTA is defined as an agency that provides CTS to individuals who are
transitioning from a SNF/NF to a home and community-based residence.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
128 | P a g e
Reimbursement
Reimbursement for CTS will be based on the negotiated rate with the MCO. Training on member
specific issues is reimbursable and included in the negotiated rate, general training requirements are an
administrative cost and are not billable.
CTS Providers have the responsibility to review the prior authorizations issued from the MCO to ensure
that the information on the prior authorization for their services is correct. If the provider identifies an
error, they must contact the MCO immediately to have the error corrected.
Limits or Exclusions
CTS do not include monthly rental or mortgage expense, food, regular utility charges, household
appliances or items that are intended for purely diversional/recreational purposes.
Additional exclusions: music systems, cable/internet, TV, VCR, DVD, MP3 player, telephone equipment,
computer, exercise equipment, personal hygiene items, decorative items, experimental or prohibited
treatments and memberships. CTS are limited to $3,500.00 per person every five years. In order to be
eligible for this service, the person must have an SNF/NF stay of at least 90 days prior to transition to the
community.
The Care Coordinator must explain this service to the member prior to discharge as part of the
community reintegration process. The member should request this service prior to discharging from the
Nursing Facility. If the member discharges from the NF to the community against medical advice (AMA)
or without MCO acknowledgement, this benefit may not be available.
Payment for a deposit to an ALF is limited to $500.00.
8.9. Emergency Response Services (ERS)
(ERS) are provided through an electronic monitoring system to secure help in the event of an
emergency. This service is to be used by ABCB members whose safety is at risk. The member may use a
portable “help” button to allow for mobility in his/her home environment. The monitoring system has a
24-hour, seven day a week monitoring capability. The system is connected to the member’s phone and
programmed to send a signal to a response center once the “help” button is activated. This response
system helps ensure that the appropriate service agency responds to alarm calls. (ERS) are provided
pursuant to the CCP.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
129 | P a g e
Scope of Services/Requirements:
Services provided by the emergency response service provider include:
o Installation, testing and maintenance of equipment;
o Training on the use of the equipment to members/caregivers and first responders;
o 24-hour monitoring for alarms;
o Monthly systems check, or more frequently if electrical outages, severe weather systems, etc.
warrant more frequent checks;
o Reports of member emergencies to the Care Coordinator and changes in the member’s
condition that may affect service delivery;
• The response center must be staffed by trained professionals; and
• Emergency Response Service categories consist of emergency response, emergency response high
need.
Provider Requirements/Qualifications:
• ERS services must be provided by an active, Medicaid approved provider type 363 ERS provider;
• In order to be approved and certified by the HSD/MAD/LTSSB, ERS providers must meet all provider
requirements/qualifications under this section. All incomplete applications submitted to the
HSD/MAD/LTSSB shall be rejected and not considered for review until a complete application is
submitted;
• The ERS provider must have emergency monitoring capability 24 hours a day, seven days a week;
• The ERS provider must be able to demonstrate it has professional trained staff to answer and
manage the response center;
• The ERS provider must be able to demonstrate it is:
o Equipped to provide verifiable data using technology capable of producing a printed record of:
▪ The type of alarm code (test, accidental or emergency);
▪ The unit subscriber number;
▪ The date; and
▪ The time of the activated alarm in seconds.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
130 | P a g e
o Emergency Response Service providers must comply with all laws, rules and regulations of the
New Mexico state corporation commission for telecommunications and security systems, if
applicable.
• Provider agencies must establish and maintain financial reporting and accounting for each member.
• Emergency Response Service providers must provide the member with information regarding
services rendered, limits of service, and information regarding agency service contracts. This
information will also include whom to contact if a problem arises, liability for payment of damages
over normal wear, and notification when change of service occurs.
• The provider agency will have security bonding.
• Emergency Response Service providers must report emergencies and changes in the member’s
condition that may affect service delivery to the MCO Care Coordinator within 24 hours.
• Emergency Response Service providers must complete quarterly reports for each member served.
The original report must be maintained in the member’s file and a copy must be submitted to the
MCO Care Coordinator on a quarterly basis.
Reimbursement
• Reimbursement for (ERS) will be based on the negotiated rate with the MCOs. Providers of service
have the responsibility to review and ensure that the information on the prior authorization for their
services is correct. If the provider identifies an error, they will contact the MCO immediately to have
the error corrected.
• A monthly fee charged can be billed to the MCO for each calendar month the member is authorized
for use of the service.
• A fee for special equipment (e.g., aa bracelet rather than a necklace) must be medically necessary
and must be substantiated and authorized by the MCO. This is designated as Emergency Response
High Need. The reason(s) for high need (ERS) must be documented in the CCP.
• All rates are based on the negotiated rate with the MCO.
Limits or Exclusions: None

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
131 | P a g e
8.10. Employment Supports
Employment Supports include job development, job seeking, and job coaching supports after available
vocational rehabilitation supports have been exhausted. The job coach provides training, skill
development, and employer consultation that a member may require while learning to perform specific
work tasks on the job; co-worker training; job site analysis; situational and/or vocational assessments
and profiles; education of the eligible member and co-workers on rights and responsibilities; and
benefits counseling.
The service must be tied to a specific goal specified in the member’s CCP. Job development is a service
provided to eligible members by skilled staff.
The service has five components: 1) job identification and development activities; 2) employer
negotiations; 3) job restructuring; 4) job sampling; and 5) job placement.
Employment Supports will be provided by staff at current or potential work sites. When employment
supports are provided at a work site where persons without disabilities are employed, payment is made
only for the adaptations; supervision and training required by eligible members receiving services as a
result of their disabilities but does not include payment for the supervisory activities rendered as a
normal part of the business setting.
Scope of Services
Employment Supports facilitates competitive work in integrated work settings for individuals with
disabilities (i.e., psychiatric, mental retardation, learning disabilities, and TBI) for whom competitive
employment has not traditionally occurred, and who, because of the nature and severity of their
disability, need ongoing support services in order to perform their job. Employment Supports settings
must be integrated and support full access of members receiving Medicaid HCBS to the greater
community, including opportunities to seek employment, and work in competitive integrated settings,
engage in community life, control personal resources, and provide access to services in the community,
to the same degree of access as individuals not receiving Medicaid HCBS. Employment Supports
provides assistance such as job coaches, transportation, assistive technology, specialized job training,
and individually tailored supervision.
• Basic components of employment supports should seek to achieve the following outcomes:
o Opportunity to earn equitable wages and other employment-related benefits;
o Development of new skills;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
132 | P a g e
o Increased community participation;
o Enhanced self-esteem;
o Increased consumer empowerment; and
o Quality of life.
The types of employment supports used depend on the needs of the member. The following are the
basic components of employment supports:
o Paid Employment - Wages are a major outcome of employment supports. Work performed
must be compensated with the same benefits and wages as other workers in similar jobs
receive. This includes sick leave, vacation time, health benefits, bonuses, training opportunities,
and other benefits.
o Integrated Work Sites - Integration is one of the essential features of Employment Supports.
Members with disabilities should have the same opportunities to participate in all activities in
which other employees participate and to work alongside other employees who do not have
disabilities.
Members who are interested in pursuing work should discuss this with their MCO Care Coordinator and
ensure it is a goal within their CCP. Members should not receive Employment Supports services through
the ABCB program without first exhausting available vocational rehabilitation services. DVR services are
considered unavailable if the member is placed on the DVR waitlist.
Employment Supports does not include sheltered work or other similar types of vocational services
furnished in specialized facilities (Federal guidelines). The employment setting needs to be in an
integrated setting.
Provider Requirements/Qualifications:
• The employment supports services must be provided by an active, Medicaid approved provider type
363, Employment Supports provider;
• The employment supports provider must adhere to all rules and regulations regarding employment
supports in this section of the policy and any applicable city, county or state regulations governing
employment supports;
• The employment supports provider must be able to demonstrate it has a functioning, physical office
located in New Mexico, where staff and members can go to obtain information or assistance;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
133 | P a g e
• In order to be approved and certified by the HSD/MAD/LTSSB, Employment support providers must
meet all requirements in this section of the policy. All incomplete applications submitted to the
HSD/MAD/LTSSB shall be rejected and not considered for review until a complete application is
submitted;
• Provider Records: The provider adheres to the Department of Labor wage laws and maintains
required certificates and documentation. These documents are subject to review by the HSD/MAD.
Each member’s earnings and benefits shall be monitored by the provider in accordance with the Fair
Labor Standards Act. Each member’s earnings and benefits shall be reviewed at least semi-annually
by the Employment Supports provider to ensure the appropriateness of pay rates and benefits;
• The Provider shall maintain a confidential case file for each member and will include the following
items:
o Quarterly progress reports;
o Vocational assessment or profile; and
▪ Vocational assessments or profile is an objective analysis of a person’s interests, skills,
needs, career goals, preferences, concerns, in areas that can pertain to an employment
outcome and can ultimately be compared to the requirements and attributes of a potential
job in order to determine the degree of compatibility as well as identification of training
needs. A vocational assessment must be of a quality and content acceptable to the Division
of Vocational Rehabilitation (DVR) or HSD/MAD;
o Career development plan as incorporated in the Comprehensive Care Plan:
▪ A career development plan consists of the vocational assessment and the Work/Learn
Action Plan that specifies steps necessary towards a successful employment outcome and
identifies the people who will complete specific tasks including the individual, as well and a
review and reporting mechanism for mutual accountability.
Provider Reporting Requirements/Qualifications:
The Employment Supports provider shall submit the following to the MCO Care Coordinator;
o Quarterly Progress Reports based upon the Care Plan cycle;
o Vocational Assessment; and
o Written updates, at least every six months, to the Work/Learn Action Plan.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
134 | P a g e
Training Requirements
Providers shall retain staff trained to establish Career Development Plans. Training will be provided by
the provider necessary to ensure that employees are able to demonstrate competency in skills listed
under this policy.
• Staffing Requirements (Individual to Staff Ratio)
The provider shall ensure adequate staffing to assure health, safety, and promote positive work
behavior and growth. The amount of staff contact time shall be adequate to meet the member’s needs
and outcomes as indicated in the CCP and may vary according to purpose (e.g., job development, job
training, job stabilization, career enhancement). For Employment Supports, the staff to individual ratio is
1:1 unless otherwise specified in the CCP. For Individual Employment Supports, a minimum of 1
one-hour face-to face visit per month is required.
Staffing Requirements and Restrictions
Providers may not employ or sub-contract direct care personnel who are an immediate family member
or spouse of the member served to work in the setting in which the member is served.
• Qualification and Competencies for Employment Supports Staff: Qualifications and competencies for
staff providing job coaching/consultation services shall, at a minimum, be able to:
o Provide supports to the member as contained in the work/learn action plan and incorporated
into the CCP to achieve his or her outcomes and goals;
o Employ job-coaching techniques and to help the member learn to accomplish job tasks to the
employer’s specifications;
o Increase the member’s capacity to engage in meaningful and productive interpersonal
interactions with co-workers, supervisors and customers;
o Identify and strengthen natural supports that are available to the member at the job site and
fade paid supports in response to increased natural supports;
o Identify specific information about the member’s interests, preferences and abilities;
o Effectively communicate with the employer about how to support the member to succeed in
their employment, including any special precautions and considerations of the member’s
disability, medications, or other special concerns;
o Monitor and evaluate the effectiveness of the service and provide documentation that
demonstrates this information was effectively communicated to the MCO Care Coordinator and
the IDT members through progress notes, quarterly reports, and participation in IDT meetings;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
135 | P a g e
o Address behavioral, medical or other significant needs identified in the work/learn action
plan/CCP that require intensive one-on-one staff support;
o Communicate effectively with the member including communication through the use of
adaptive equipment if applicable, at the work site;
o Document information that pertains to the CCP, progress notes, outcomes, and health and
safety issues/concerns and any and all other required documentation by HSD/MAD;
o Adhere to relevant state policies/standards and provider policies and procedures that directly
impact services to the member;
o Model behavior, instruct and monitor any workplace requirements to the member;
o Adhere to professionally acceptable business attire and appearance, and interact and
communicate through a business-like, respectful manner; and
o Adherence to the rules of the specific workplace, including dress, confidentiality, safety rules,
and other areas required by the employer.
Supervision
• In a group employment setting (a setting where up to six individuals work in an integrated setting
with staff supports on site), the Employment Supports provider determines the job site and is
responsible for the day-to-day supervision of the members and for follow-up services. For individual
placements, the employer is responsible for the provision of general supervision consistent with his
or her role as employer. When necessary and appropriate, the Employment Support provider may
supplement these services.
Reimbursement
Employment Supports providers must maintain appropriate record keeping of services provided,
personnel and training documentation, and fiscal accountability as indicated in the Medicaid PPA. Billing
is on an hourly basis and is accrued and rounded to the nearest quarter of an hour. Reimbursements for
employment support services will be based on the negotiated rate with the MCOs. Providers of service
have the responsibility to review and ensure the information on the prior authorization for their services
is correct. If the provider identifies an error, they will contact the MCO immediately to have the error
corrected.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
136 | P a g e
Limits or Exclusions
Payment shall not be made for incentive payments, subsidies, or unrelated vocational training expenses
such as: incentive payments made to an employer to encourage or subsidize the employer's
participation in an employment supports program, payments that are passed through to users of
employment supports programs, or payments for training that is not directly related to a member’s
employment supports program. Federal financial participation cannot be claimed to defray expenses
associated with starting up or operating a business.
8.11. Environmental Modifications
Environmental modification services include the purchase and/or installation of equipment and/or
making physical adaptations to an eligible member’s residence that are necessary to ensure the health,
welfare, and safety of the member or enhance the member’s level of independence.
Scope of Services
Environmental modifications are physical adaptations and environmental control systems excluding
DME. Environmental modifications need to be identified in the member’s CCP. Adaptations include the
installation of ramps and hand rails; widening of doorways/hallways; installation of specialized electric
and plumbing systems to accommodate medical equipment and supplies; lifts/elevators; modification of
bathroom facilities (roll-in showers, sink, bathtub, and toilet modifications, water faucet controls,
lowering counters, floor urinals and bidet adaptations and plumbing); turnaround space adaptations;
specialized accessibility/safety adaptations/additions; trapeze and mobility tracks for home ceilings;
automatic door openers/doorbells; voice-activated, light-activated, motion-activated, and electronic
devices; fire safety adaptations; air filtering devices; heating/cooling adaptations; glass substitute for
windows and doors; modified switches, outlets or environmental controls for home devices; and alarm
and alert systems and/or signaling devices.
Environmental modifications are managed by professional staff available to provide technical assistance
and oversight to environmental modification projects. These modifications shall exclude those
adaptations, improvements or repairs to the existing home that do not directly affect accessibility.
Environmental modifications exclude such things as carpeting, roof repair, furnace replacement,
remodeling bare rooms, and other general household repairs.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
137 | P a g e
Provider Requirements/Qualifications:
• The environmental modifications must be provided by an active, Medicaid approved provider type
363, environmental modifications provider.
• The environmental modification provider must comply with all New Mexico State laws, rules and
regulations, including applicable building codes and the Construction Industries Licensing Act, NMSA
1978, Section 60-13-3.
• The environmental modification provider must maintain a valid New Mexico regulation and licensing
department, construction industries division GB02 class or higher construction license pursuant to
the Construction Industries Licensing Act NMSA 1978, Section 60-13-3.
• The environmental modification provider must provide a one-year warranty from the completion
date on all parts and labor. The environmental modification provider must have a working
knowledge of environmental modifications and be familiar with the needs of persons with
functional limitations in relation to environmental modifications.
• The environmental modification provider must ensure proper design criteria as addressed in
planning and design of the adaptation. The environmental modification provider is responsible for
all adaptions being made to member’s home, including but not limited to: oversight of construction
and all administrative and technical oversight of projects.
• The environmental modification provider must provide consultation to family members, waiver
providers and MCOs concerning environmental modification projects to the member’s residence
and complete a final inspection of the environmental modification project to ensure that the
adaptations meet the approved plan submitted for environmental adaptation. The MCO Care
Coordinator will also complete a final inspection to ensure the environmental modification provider
has completed the project according to authorization before final payment is made to the
environmental modification provider.
• Environmental modification providers who receive authorization from an MCO for a member project
must complete the authorized job and retain full control of the authorized project. Portions of the
authorized project may be contracted out; however, the environmental modification provider
retains full responsibility for the entire project.
• The environmental modification provider must establish and maintain financial reporting and
accounting for each member.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
138 | P a g e
o The environmental modification provider will submit the following information and
documentation to the MCO:
▪ Environmental modification evaluation;
▪ Service Cost Estimate. Photographs of the proposed modifications. The estimated start date
of the work on the proposed modification; (equipment, materials, supplies, labor, travel, per
diem, report writing time, and completion date of modification);
▪ Letter of Acceptance of service cost estimate signed by the member;
▪ Letter of Permission from property owner. If the property owner is someone other than the
member, the letter must be signed by the property owner and the member;
▪ The construction letter of understanding. If the property owner is someone other than the
member, the letter must be signed by the property owner and the member;
▪ Documentation demonstrating compliance with the ADA.
• The Provider must submit the following to the MCO Care Coordinator, after the completion of work:
o Letter of approval of work completed signed by the member; and
o Photographs of the completed modifications.
• The MCO must submit the Care Coordinator Individual Assessment of Need to the provider.
Reimbursement
Environmental modification provider agencies must maintain appropriate record keeping of services
provided, and fiscal accountability as indicated in the Medicaid PPA. Billing is based on a project basis,
one unit per environmental modification project. Reimbursement for environmental modification
services will be based on the authorized environmental modification project with the MCOs. Providers
of service have the responsibility to review and ensure the information on the prior authorization for
their services is correct. If the provider identifies an error, they will contact the MCO immediately to
have the error corrected.
The MCO Care Coordinator or other designee must visit the member’s home to ensure the
environmental authorized project reasonably appears to have been completed before final payment is
made to the environmental modification provider.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
139 | P a g e
Limits or Exclusions
Environmental modification services are limited to $5,000.00 every five years. Administrative Costs of
the provider for environmental modification services will not exceed 15% of the total cost of the
environmental modification project for each project managed by the MCO.
No duplicate adaptations, modifications or improvements shall be approved regardless of the payment
source. For example, if the client has a safe and usable ramp, a replacement ramp shall not be
approved.
This service cannot be used to fund new construction including apartment buildings and Assisted Living
facilities.
8.12. Home Health Aide (HH Aide)
HH Aide services provide total care or assist an eligible member in all ADLs. Total care is defined as: the
provision of bathing (bed, sponge, tub, or shower), shampoo (sink, tub, or bed), care of nails and skin,
oral hygiene, toileting and elimination, safe transfer techniques and ambulation, normal range of
motion and positioning, adequate oral nutrition and fluid intake.
Scope of Services/Requirements:
The HH Aide services assist the eligible member in a manner that promotes an improved quality of life
and a safe environment for the eligible member. HH Aide services can be provided outside the eligible
member's home. State Plan HH Aide services are intermittent and provided primarily on a short-term
basis; whereas, HH Aide services within the ABCB are provided hourly, for eligible ABCB members who
need this service on a long-term basis. HH Aides may provide basic non-invasive nursing assistant skills
within the scope of their practice. HH Aides perform procedures as an extension of nursing and therapy
services such as; bowel and bladder care, ostomy site care, personal care, walking and exercise,
household services essential to health care at home, assisting with medications that are normally
self-administered, reporting changes in patient conditions and needs, and completing appropriate
records.
HH aide services must be provided under the supervision of an RN or other appropriate professional
staff. The agency must make a supervisory visit to member's residence at least every two weeks to
observe and determine whether goals are being met.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
140 | P a g e
All supervisory visits/contacts must be documented in the member’s HH Aide clinical file on a
standardized form that reflects the following:
o Service received;
o Member’s status;
o Contact with family members; and
o Review of HH Aide PCCP with appropriate modification annually and as needed.
Provider Requirements/Qualifications:
• HH Aide services must be provided by an active, Medicaid approved provider type 363, Home Health
Agency (HHA);
• The HHA must maintain (no gaps in license) full permanent license by the New Mexico Licensing and
Certification Bureau, Division of Health Improvement; DOH as an HHA;
• In order to be approved and certified by the HSD/MAD/LTSSB, the HHA must be holding and
operating with a fully approved permanent license. All incomplete applications submitted to the
HSD/MAD/LTSSB shall be rejected and not considered for review until a complete packet is
submitted;
• The HHA nursing supervisor(s) must have at least one year of supervisory experience. The nursing
supervisor will supervise the RN, LPN and HH Aide;
• The HHA staff will be culturally sensitive to the needs and preferences of members and households.
Arrangement of written or spoken communication in another language may need to be considered;
• The HHA will document and report any noncompliance with the CCP to the MCO Care Coordinator;
• All physician orders that change the member’s service needs must be conveyed to the MCO Care
Coordinator for coordination with service providers and modification to CCP if necessary;
o The HHA will document in the member’s clinical file that the supervision of the HH Aide
occurs at least once every two weeks. Supervisory forms must be developed and
implemented specifically for this task;
o The HHA and MCO Care Coordinator must have documented monthly contact that reflects
the discussion and review of services and ongoing coordination of care;
o The HHA nursing supervisor, direct care RN and LPN shall train families, DSP and all relevant
individuals in all relevant settings as needed for successful implementation of therapeutic

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
141 | P a g e
activities, strategies, treatments, use of equipment and technologies or other areas of
concern; and
o It is expected the HHA will consult with IDT members, guardians, family, and DSPs as
needed.
• Qualifications for employed HH Aides:
o HHA Certificate from an approved community-based program following the HHA training
Federal regulations 42 CFR 484.36 or the State Regulation 7 NMAC 28.2;
o HH Aide training at the licensed HHA which follows the Federal HH Aide training regulation in 42
CFR 484.36 or the State Regulation 7 NMAC 28.2;
o A CNA must have successfully completed the employing HH Agency’s written and practical
competency standards and have met the qualifications for a HH Aide. Documentation will be
maintained in personnel file;
o A HH Aide who was not trained at the employing HHA must successfully complete the employing
HHA’s written and practical competency standards before providing direct care services to an
ABCB member. Documentation will be maintained in personnel file; or
o The HH Aide will be supervised by the HH Agency nursing supervisor or designee at least once
every two weeks in the member’s home; and
o The HH Aide will be culturally sensitive to the needs and preferences of the members and their
families. Based upon the individual language needs or preferences, the HH Aide may be
requested to communicate in a language other than English.
Reimbursement
The HHA must maintain appropriate record keeping of services provided by personnel and training
documentation, and fiscal accountability as indicated in the Medicaid PPA. Billing is on an hourly basis
and is accrued and rounded to the nearest quarter of an hour. Reimbursement for HH Aide services will
be based on the negotiated rate with the MCOs. HHAs have the responsibility to review and ensure that
the information on the prior authorization for their services is correct. If the provider identifies an error,
they will contact the MCO immediately to have the error corrected.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
142 | P a g e
8.13. Nutritional Counseling
Nutritional Counseling services are designed to meet the unique food and nutritional needs of ABCB
members. These services are available to assist members living in a community setting to maintain (or
improve and maintain) their health and/or functional status and remain in their setting of choice. This
does not include oral-motor skill development services, such as those provided by a speech pathologist.
Nutritional assessment is defined as the evaluation of the nutritional needs of the ABCB member based
upon appropriate biochemical, anthropometric, physical and dietary data to determine nutrient needs
and includes recommending appropriate nutritional intake.
Nutritional counseling is defined as advising and helping an ABCB member obtain appropriate nutritional
intake by integrating information from the nutritional assessment with information on food, other
sources of nutrients, and meal preparation consistent with cultural background and socioeconomic
status.
Nutritional Counseling services may be in addition to and cannot duplicate nutritional or dietary services
allowed in the member’s Medicaid state plan benefit, or another funding source.
Scope of Services/Requirements:
Services can be initiated where they are indicated and authorized in the member’s PCCP/CCP. A PCCP
will be developed by the Nutritional Counseling provider with identified goals and measurable objectives
and will be attached to or incorporated into the CCP. The MCO should agree to the arrangements for
record-keeping, and the frequency and duration of services with the provider agency or individual
provider.
Nutritional Counseling services include:
• Assessment of nutritional needs;
• Development and/or revision of the member’s nutritional plan; and
• Counseling and nutritional intervention and observation and technical assistance related to
implementation of the nutritional plan.
The services allow for consultation with appropriate professionals, attendance at/participation in
Interdisciplinary Team meetings, liaison with the member’s representative/family/caregivers, and
monitoring of the nutritional plan.
Services are person-centered and must be culturally sensitive to the needs and preferences of the
member and their household based upon language and cultural traditions.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
143 | P a g e
The staff: client ratio is 1:1 with the member and/or the member’s representative for the period of time
in which the member is receiving Nutritional Counseling services. All services should be provided face-
to-face. They may be provided at the member’s residence or an appropriate community location.
Agency Provider Requirements/Qualifications:
• Nutritional counseling services must be provided by an active, Medicaid approved provider type 363
Nutritional Counseling provider.
• The agency must have on staff or employ a full-time licensed dietitian or a licensed nutritionist who
maintains (no gaps in licensure) a full permanent license through the New Mexico Regulation and
Licensing Department; Nutrition and Dietetics Practice Act, NMSA 1978, Section 61-7A et.seq.
Provisional permits are not acceptable.
• In order to be approved and certified by the HSD/MAD/LTSSB, Nutritional Counseling providers must
be operating with a fully approved permanent license. All incomplete applications submitted to the
HSD/MAD/LTSSB shall be rejected and not considered for review until a complete application is
submitted.
• Licensed nutrition associates will work under the supervision of a licensed dietitian or licensed
nutritionist. The provider agency must ensure that the supervision requirements for licensed
nutrition associates specified in the New Mexico Regulation and Licensing Department; Nutrition
and Dietetics Practice Act, NMSA 1978, Section 61-7A et.seq. are met.
• All licensed practitioners providing nutritional assessment and counseling services will operate
within their professional scope of practice.
• Provider agencies must comply with the HSD/MAD requirements including but not limited to: OSHA
training requirements, Incident Management reporting, Criminal Background checks, Labor Laws,
etc.
• Provider personnel must be proficient in the member’s primary language or have access to an
interpreter (family member, friend, or caregiver). Professional interpretation service fees are the
responsibility of the agency.
• Provider agencies must employ and maintain a sufficient pool of appropriately licensed and trained
personnel to provide scheduled services to all ABCB members.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
144 | P a g e
Individual Provider Requirements/Qualifications:
• Nutritional counseling services must be provided by an active, eligible, Medicaid approved
provider type 363 Nutritional Counseling provider.
• The individual must maintain a full permanent dietitian license or a nutritionist license (no gaps
in licensure) through the New Mexico Regulation and Licensing Department; Nutrition and
Dietetics Practice Act, NMSA 1978, Section 61-7A et.seq. Provisional licenses are not
acceptable.
• The individual may employ licensed nutrition associates who work under their supervision as a
licensed dietitian or licensed nutritionist. The provider must ensure that the supervision
requirements for licensed nutrition associates specified in the New Mexico Regulation and
Licensing Department; Nutrition and Dietetics Practice Act, NMSA 1978, Section 61-7A et.seq.
are met.
• All licensed practitioners providing nutritional assessment and counseling services will operate
within their professional scope of practice.
• The individual provider must comply with HSD/MAD requirements including but not limited to:
OSHA training requirements, Incident Management reporting, Criminal Background checks,
Labor Laws, etc.
• All personnel must be proficient in the member’s primary language or have access to an
interpreter (family member, friend, or caregiver). Professional interpretation service fees are
the responsibility of the agency.
• The individual provider must employ and maintain a sufficient pool of appropriately licensed
and trained personnel, sufficient to provide scheduled services to all ABCB members on their
caseload.
• Nutritional Counseling services must abide by all federal, state, HSD policies and procedures
regarding billable and non-billable items.
Reimbursement
Nutritional Counseling provider agencies and individual providers must maintain appropriate record-
keeping of services provided, personnel and training documentation, and fiscal accountability as
indicated in the Medicaid Provider Participation Agreement (PPA). All services must be reflected on a

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
145 | P a g e
PCCP that is coordinated by the Care Coordinator and authorized by the MCO. Reimbursement for
Nutritional Counseling services will be based on the negotiated rate with the MCO. Billing is on an
hourly basis and is accrued and rounded to the nearest quarter of an hour. Payment for Nutritional
Counseling services through the MCO is considered payment in full. Providers of service have the
responsibility to review the prior authorizations issued from the MCO to ensure that the information on
the prior authorization for their service is correct. If the provider identifies an error, they must contact
the MCO immediately to have the error corrected.
Billable Nutritional Counseling services include:
• Attendance and/or telephone conference calls to participate in Interdisciplinary Team
meetings; and
• Training on member-specific issues is included in the negotiated rate.
Limits or Exclusions
HSD does not consider the following to be Nutritional Counseling services and will not authorize
payment for the following non-billable activities:
o General training requirements are an administrative cost and not billable;
o Performing specific errands for the individual and/or family that are not program
specific;
o Friendly visiting;
o Financial brokerage services, handling of member finances, or, preparation of legal
documents;
o Time spent on paperwork or travel that is administrative for the provider;
o Transportation of members;
o Pick up and/or delivery of commodities; and
o Other non-Medicaid reimbursable activities.
Nutritional Counseling services are provided with the understanding that the MCO is the payer of last
resort. ABCB services should not be requested or authorized until all other third party and community
resources have been explored and/or exhausted. If services are available for reimbursement through
third party liability or other payment sources, these sources must be accessed before Community
Benefit services are delivered.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
146 | P a g e
8.14. Personal Care Services (PCS)
Scope of Services
PCS have been established by HSD/MAD or Medicaid to assist individuals 21 years of age or older who
are eligible for full Medicaid coverage and meet the NF LOC criteria. This policy describes PCS for
consumers who meet NF LOC because of disability or functional limitation and need assistance with
certain ADLs and IADLs.
• The MCO determines medical LOC for PCS eligibility upon initial application and at least annually
thereafter. Medicaid-eligible individuals may contact the MCO to apply for PCS.
• The goals of PCS are to avoid institutionalization and to maintain the consumer’s functional level
and independence. Although a consumer’s assessment for the amount and types of services may
vary, PCS are not provided 24 hours a day.
• PCS is a Medicaid service, not a Medicaid category of assistance, and services are delivered pursuant
to an Individual Plan of Care (IPoC). PCS includes a range of ADL and IADL services to consumers who
meet NF LOC because of a disability or functional limitation(s). Consumers will be assessed for
services at least annually, or more frequently, as appropriate. PCS will not include those services for
a task the individual is already receiving from other sources such as tasks provided by natural
supports. Natural supports are friends, family, and the community (through individuals, clubs, and
organizations) that are able and consistently available to provide supports and services to the
consumer. The CNA is conducted pursuant to the managed care service agreement. The CNA is
performed by the MCO and determines the amount and type of services needed to supplement the
services a consumer is already receiving including those services provided by natural supports. PCS
must be related to the individual’s functional level to perform ADLs and IADLs as indicated in the
CNA.
• PCS providers will use the HSD approved EVV system to record date and time for provided PCS. PCS
agencies are responsible for establishing employment policies and providing oversight of employees
to ensure the required use of EVV as mandated in the 21st Century Cures Act.
Eligible Population
To be eligible for PCS, a member must meet all of the following criteria:
• Be a recipient of a full benefit Medicaid category of assistance and, not be receiving other Medicaid
HCBS waiver benefits, Medicaid NF, ICF/IID Medicaid, PACE, or APS attendant care program, at the

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
147 | P a g e
time PCS are furnished; an individual residing in an NF or ICF/IID Medicaid is eligible to apply for PCS
to facilitate NF discharge; recipients of community transition goods or services may also receive PCS;
all individuals must meet the Medicaid eligibility requirements to receive PCS; the MCO, Medicaid or
its alternative designee must conduct an assessment (CNA) or evaluation to determine if the
transfer to PCS is appropriate and if the PCS would be able to meet the needs of that individual;
• Be age 21 or older;
• Be determined to have met NF LOC by the MCO; and
• Comply with all Medicaid and PCS regulations and procedures.
LOC Determination
To be eligible for PCS, a consumer must meet the LOC required in an NF. The MCO makes initial LOC
determination and subsequent determinations at least annually thereafter.
• The MCO approves the consumer’s LOC for a maximum of one year (12 consecutive months); a new
LOC determination must be made at least annually to ensure the consumer continues to meet
medical eligibility criteria for PCS; each LOC determination must be based on the consumer’s current
medical condition and need of service(s), and may not be based on prior year LOC determinations;
the approved NF LOC has a start date and an end date of no more than 12 consecutive months,
which is the NF LOC span.
• Any individual applying for PCS who has an existing approved NF LOC determination in another
program (i.e., NF) will not need an additional LOC determination until his/her next annual
assessment.
• A PCS agency that does not agree with the LOC determination made by the MCO or Medicaid’s
designee may work with the consumer’s physician or physician designee to request a re-review or
reconsideration from the MCO.
• A member that does not agree with the LOC determination made by the MCO may file a grievance
or appeal with the MCO. The MCO grievance or appeal process must be exhausted before the
consumer may request a fair hearing with HSD pursuant to 8.352.2 NMAC, Recipient Hearings.
• The MCO shall review the LOC determination upon a referral from the PCS agency, the consumer, or
the consumer's legal representative when a change in the consumer's health condition is identified
and make a new determination, if appropriate.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
148 | P a g e
Service Delivery Models – Consumer-Delegated PCS and Consumer-Directed PCS
• Consumers eligible for PCS have the option of choosing the consumer-delegated or the
consumer-directed personal care model. In both models, the consumer may select a family member
(except the spouse), a friend, neighbor, or other person as the attendant. The MCO’s Care
Coordinator is responsible for explaining both models to each consumer, initially, and annually
thereafter.
o In the consumer-delegated model, the consumer chooses the PCS agency to perform all
employer-related tasks and the agency is responsible for ensuring all service delivery to the
consumer.
o The consumer-directed model allows the consumer to oversee his/her own service care delivery
and requires that the consumer work with a PCS agency acting as a fiscal intermediary agency to
processing all financial paperwork to be submitted to the MCO.
Consumer’s Responsibilities
Consumers receiving PCS have certain responsibilities depending on the service delivery model they
choose.
• The consumer’s or legal representative’s responsibilities under the consumer-delegated model
include:
o Allowing the MCO to complete assessment visits and other contacts necessary to avoid a lapse
in services;
o Allowing the PCS provider to complete monthly home supervisory visits;
o Participating in the CNA process, at least annually, in the consumer’s primary place of residence;
o Participating in the development and review of the IPoC;
o Maintaining proof of current vehicle insurance (as mandated by the laws of the State of
New Mexico) if the attendant will transport the consumer in the consumer’s vehicle for support
services that have been allocated to the consumer; and
o Complying with all Medicaid rules, regulations, and PC service requirements; failure to comply
may result in discontinuation of PCS.
• The consumer’s or legal representative’s responsibilities under the consumer-directed model
include:

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
149 | P a g e
o Interviewing, hiring, training, terminating, and scheduling personal care attendants; this
includes, but is not limited to:
▪ Verifying the attendant possesses a current and valid State driver’s license if there are any
driving-related activities listed on the IPoC; a copy of the current driver’s license must be
maintained in the attendant’s personnel file at all times; if no driving-related activities are
listed on the IPoC, a copy of a valid State identification is kept in the attendant’s personnel
file at all times;
▪ Verifying the attendant has proof of current liability vehicle insurance if the consumer is to
be transported in the attendant’s vehicle at any time; a copy of the current proof of
insurance must be maintained in the attendant’s personnel file at all times;
▪ Identifying training needs; this includes training his/her own attendant(s) or arranging for
training for the attendant(s);
o Developing a list of attendants who can be contacted when an unforeseen event occurs that
prevents the consumer’s regularly scheduled attendant from providing services; making
arrangements with attendants to ensure coverage and notifying the agency when arrangements
are changed;
o Verifying services have been rendered by completing, dating, signing, and submitting
documentation to the agency for payroll; a consumer or his/her legal representative is
responsible for ensuring the submission of accurate timesheets/logs; payment shall not be
issued without appropriate documentation;
o Notifying the agency, within one business day, of the date of hire or the date of termination of
his/her attendant and ensure all relevant employment paperwork and other applicable
paperwork is completed and submitted; this may include, but is not limited to: employment
application, verification from the employee abuse registry, criminal history screening, doctor’s
release to work, photo identification, proof of eligibility to work in the United States, copy of a
State driver’s license and proof of insurance;
o Notifying and submitting a report of an incident to the PCS agency within 24 hours of such
incident, so the PCS agency can submit an incident report on behalf of the consumer; the
consumer or his/her legal representative is responsible for completing the incident report;
o Ensuring the individual selected for hire has submitted a request for a nationwide caregiver
criminal history screening, pursuant to 7.1.9 NMAC and in accordance with NMSA 1978, Section

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
150 | P a g e
29-17-2 et seq. of the Caregivers Criminal History Screening Act, within 20 calendar days of the
individual beginning employment; the consumer must work with the selected agency to
complete all paperwork required for submitting to the nationwide caregiver criminal history
screening; the consumer may conditionally (temporarily) employ the individual contingent upon
the receipt of written notice that the individual has submitted to a nationwide caregiver criminal
history screening; a consumer may not continue employing an attendant who does not
successfully pass a nationwide criminal history screening. The agency is responsible for the cost
of the first criminal history screening and the member and/or caregiver is responsible for any
additional caregiver history screenings and the associated costs thereafter if the caregiver’s
termination of employment is a result of termination on behalf of the member for an
unjustifiable reason not related to the agencies standard employment conditions. If the
caregiver quits or termination is a result of the caregiver failing to meet standard employment
conditions outlined by the agency, the agency will be responsible for the criminal history
screening for the next hired caregiver.
o Obtaining a signed agreement from the attendant, in which the attendant agrees that he/she
will not provide PCS while under the influence of drugs or alcohol and acknowledges that if
he/she is under the influence of drugs or alcohol while providing PCS he/she will be immediately
terminated; a copy of the signed agreement must be provided to the PCS;
o Ensuring if the attendant is the consumer’s legal representative and is the individual selected for
hire, prior approval has been obtained from Medicaid or its designee; any PCS provided by the
consumer’s legal representative must be justified, in writing, by the PCS agency and consumer
and submitted for approval to the consumer’s MCO prior to employment; the justification must
demonstrate the lack of other qualified attendants in the applicable area and indicate how
timesheets will be verified to ensure services were provided; documentation of written approval
by the consumer’s MCO must be maintained in the consumer’s file; the consumer is responsible
for immediately informing the agency if the consumer has appointed or obtained a legal
representative any time during the plan year;
o Signing an agreement accepting responsibility for all aspects of care and training including
mandatory training in cardiopulmonary resuscitation (CPR), first aid for all attendants,
competency testing, tuberculosis (TB) testing, Hepatitis B immunizations, or waiving the
provision of such training and accepting the consequences of such a waiver;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
151 | P a g e
o Verifying prior to employment, and annually thereafter, that attendants are not on the
employee abuse registry by researching the Consolidated Online Registry (COR) pursuant to
8.11.6 NMAC and in accordance with the Employee Abuse Registry Act, NMSA, Section 27-7A-1
et. seq.;
o Allowing the MCO to complete assessment visits and other contacts necessary to avoid a lapse
in services;
o Allowing the PCS provider to maintain at least a minimum of quarterly in-person contact;
o Participating in the CNA process, at least annually, in the consumer’s primary place of residence;
o Participating in the development and review of the IPoC;
o Maintaining proof of current vehicle insurance (as mandated by the laws of the State of New
Mexico) if the attendant will transport the consumer in the consumer’s vehicle for support
services that have been allocated to the consumer; and
o Complying with all Medicaid rules, regulations, and PCS requirements.
• Consumers may have a personal representative assist him/her to give instruction to the personal
care attendant or to provide information to the MCO during assessments of the consumer's natural
supports and service needs. A personal representative is not the same as a legal representative but
may be the same person. A personal representative must have the following qualifications: be at
least 18 years of age, have a personal relationship with the consumer and understand the
consumer's natural supports and service support needs, and know the consumer’s daily schedule
and routine (to include medications, medical, and functional status, likes and dislikes, strengths and
weaknesses). A personal representative does not make decisions for the consumer unless he/she is
also a legal representative, but may assist the consumer in communicating, as appropriate. A
personal representative may not be a personal care attendant, unless he/she is also the legal
representative and has obtained written approval from the MCO pursuant to these PCS regulations.
A person’s status as a personal representative must be properly documented with the PCS agency.
Agency Provider Requirements:
• Eligible PCS Agencies: PCS agencies electing to participate in providing PCS must obtain agency
certification.
• PCS agency certification: A PCS agency providing either the consumer-directed, the
consumer-delegated, or both models, must comply with the requirements of this section. PCS

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
152 | P a g e
agencies must be certified by Medicaid or its designee. A PCS agency may only serve members in the
counties that are approved by HSD. An agency listing, by county, is maintained by Medicaid or its
designee. All certified PCS agencies are required to select a county in which to establish and
maintain an official office for conducting of business with published phone number and hours of
operation; the PCS agency must provide services in all areas of the county in which the main office is
located. Upon HSD approval, the PCS agency may elect to serve any county within 100 miles of the
main office. The PCS agency may elect to establish branch office(s) within 100 miles of the main
office. The PCS agency must provide PCS services to all areas of all selected counties.
• To be certified by Medicaid or its designee, agencies must meet the following conditions and submit
for approval, a packet, to Medicaid’s fiscal agent or its designee, containing the following:
o A completed Medicaid PPA (also known as the MAD 335);
o Copies of successfully passed nationwide caregivers criminal history screenings on employees
who meet the definition of “caregiver” and “care provider” pursuant to 7.1.9 NMAC and in
accordance with NMSA 1978, Section 29-17-2 et seq., of the Caregivers Criminal History
Screening Act; A copy of a current and valid business license or documentation of non-profit
status; if certified, a copy of the business license or documentation of non-profit status must be
kept current and submitted annually;
o Proof of liability and workers’ compensation insurance (if certified, proof of liability and
workers’ compensation insurance must be submitted annually to HSD and the MCO); and
o A copy of written policies and procedures that address:
▪ Medicaid’s PCS provider rules and regulations;
▪ Personnel policies; and
▪ Office details that include but are not limited to:
• Contact information, mailing address, physical location if different from mailing
address, and hours of operation for the main office and branch offices if any;
designation of counties served by the office;
• Meeting all ADA requirements; and
• If PCS agencies have branch offices, the branch office must have a qualified onsite
administrator to handle day-to-day operations and receive direction and supervision
from the main/central office;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
153 | P a g e
o Quality improvement (QI) to ensure adequate and effective operation, including documentation
of quarterly activity that addresses, but is not limited to:
▪ Service delivery;
▪ Operational activities;
▪ Critical incident and significant events management practices;
▪ QI action plan;
▪ Documentation of QI activities;
o Agency operations to furnish services as consumer-directed or consumer-delegated, or both;
o A copy of a current and valid home health license, issued by the DOH, Division of Health
Improvement, licensing, and certification (pursuant to 7.28.2 NMAC) may be submitted in lieu of
the requirements; if certified, a copy of a current and valid home health license must be
submitted annually along with proof of liability and workers’ compensation insurance; and
o Upon request, for approval to provide the consumer-delegated model of service, a copy of the
agency’s written competency test for attendants approved by Medicaid or its designee; an
agency may select to purchase a competency test or it may develop its own test; the test must
address at least the following:
▪ Communication skills;
▪ Patient/member rights, including respect for cultural diversity;
▪ Recording of information for patient/client records;
▪ Nutrition and meal preparation;
▪ Housekeeping skills;
▪ Care of the ill and disabled, including the special needs populations;
▪ Emergency response (including CPR and first aid);
▪ Universal precautions and basic infection control; home safety including oxygen and fire
safety;
▪ Incident management and reporting; and
▪ Confidentiality.
After the packet is received, reviewed, and approved in writing by Medicaid or its designee, the agency
will be contacted to complete the rest of the certification process; this will require the agency to attend
a mandatory Medicaid or its designee’s provider training session prior to the delivery of PCS.
An agency will not be certified as a personal care agency if:

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
154 | P a g e
▪ It is owned in full or in part by a professional authorized to complete the CNA or other
similar assessment tool subsequently approved by Medicaid under PCS or the agency would
have any other actual or potential conflict of interest; and
▪ A conflict of interest is presumed between people who are related within the third degree
of blood or consanguinity or when there is a financial relationship between:
• Persons who are related within the third degree of consanguinity (by blood) or affinity
(by marriage) including a person’s spouse, children, parents (first degree by blood);
siblings, half-siblings, grandchildren or grandparents (second degree by blood and
uncles, aunts, nephews, nieces, great grandparents, and great grandchildren (third
degree by blood); step-mother, step-father, mother-in-law, father-in-law (first degree by
marriage); step-brother, step-sister, brothers-in-law, sisters-in-law, step grandchildren,
grandparents (second degree by marriage); step-uncles, step-aunts, step-nephews,
step-nieces, step-great grandparents, step-great grandchildren (third degree by
marriage); and
• Persons or entities with an ongoing financial relationship with each other including a
personal care provider whose principals have a financial interest in an entity or financial
relationship with a person who is authorized to complete a CNA or other similar
assessment tool or authorized to carry out any of the MCO’s responsibilities; a financial
relationship is presumed between spouses.
• Approved PCS agency responsibilities: A personal care agency electing to provide PCS under either
the consumer-directed model or the consumer-delegated model, or both, is responsible for:
o Furnishing services to Medicaid consumers that comply with all specified Medicaid participation
requirements outlined in 8.302.1 NMAC, General Provider Policies and 8.308.2.9 NMAC,
Provider Network Policies;
o Verifying every month that all consumers are eligible for full Medicaid coverage and PCS prior to
furnishing services pursuant to Subsection A of 8.302.1.11 NMAC, provider responsibilities and
requirements; PCS agencies must document the date and method of eligibility verification;
possession of a Medicaid card does not guarantee a consumer’s financial eligibility because the
card itself does not include financial eligibility, dates or other limitations on the consumer’s
financial eligibility; PCS agencies must notify consumers who are not financially eligible that
he/she cannot authorize employment for his/her attendant(s) until financial eligibility is

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
155 | P a g e
resumed; PCS agencies and consumers cannot bill Medicaid or its designee for PCS services
rendered to the consumer if he/she is not eligible for PCS services;
o Using the HSD-approved EVV system;
o Maintaining appropriate recordkeeping of services provided and fiscal accountability as required
by the PPA;
o Maintaining records, as required by the PPA and as outlined in 8.302.1 NMAC, General Provider
Policies, that are sufficient to fully disclose the extent and nature of the services furnished to the
consumers;
o The PCS agency will, unless exempted by MAD or its designee, use an electronic system
attendants will use to check in and check out at the end of each period of service delivery; the
system must produce records that can be audited to determine the time of services provided,
the type of services provided, and verification by the consumer or the consumer’s legal
representative; failure by a PCS agency to maintain a proper record for audit under this system
will subject the PCS agency to recovery by Medicaid of any insufficiently documented claims;
o Passing random and targeted audits, conducted by Medicaid or its designee, that ensure
agencies are billing appropriately for services rendered; Medicaid or its designee will seek
recoupment of funds from agencies when audits show inappropriate billing or inappropriate
documentation for services;
o Providing either the consumer-directed or the consumer-delegated models, or both models;
o Furnishing to their consumers, upon request, information regarding each model; if the
consumer chooses a model an agency does not offer, the agency must refer the consumer to
the MCO for a list of agencies that offer the chosen model; the MCO is required to explain each
model in detail to each consumer annually;
o Ensuring each consumer receiving PCS services has a current IPoC on file;
o Performing the necessary nationwide caregiver criminal history screening, pursuant to 7.1.9
NMAC and in accordance with NMSA 1978, Section 29-17-2 et seq. of the Caregivers Criminal
History Screening Act, on all potential personal care attendants; nationwide caregiver criminal
history screenings must be performed by an agency certified to conduct such checks; the
agency, and the consumer, as applicable, ensures the paperwork is submitted within the first 20
calendar days of hire; consumers under the consumer-directed model or agencies under the
consumer-delegated model may conditionally (temporarily) employ an attendant until such

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
156 | P a g e
check has been returned from the certified agency; if the attendant does not then successfully
pass the nationwide caregiver criminal history screening, the agency under consumer-delegated
or the consumer under consumer-directed may not continue employment of the attendant. The
agency is responsible for the cost of the first criminal history screening and the member and/or
caregiver is responsible for any additional caregiver history screenings and the associated costs
thereafter if the caregiver’s termination of employment is a result of termination on behalf of
the member for an unjustifiable reason not related to the agencies standard employment
conditions. If the caregiver quits or termination is a result of the caregiver failing to meet
standard employment conditions outlined by the agency, the agency will be responsible for the
criminal history screening for the next hired caregiver;
o Producing reports or documentation as required by Medicaid or its designee;
o Verifying consumers will not be receiving services through the following programs while they
are receiving PCS: Medicaid HCBS through the DD or MF waivers; Medicaid certified NF, ICF/IID,
PACE, or APS attendant care program; recipients of community transition goods or services may
receive Planning Center Online (PCO) services; all individuals must meet the Medicaid and LOC
eligibility requirements to receive PCS; the MCO must conduct an assessment or evaluation to
determine if the transfer is appropriate and if PCS would be able to meet the needs of that
individual; if an agency is authorized to provide services by the MCO in error, the MCO will bear
the cost of the error;
o Processing all claims for PCS in accordance with the billing specifications from the MCO;
payment shall not be issued without appropriate documentation;
o Making a referral to an appropriate social service, legal, or state agency, or the MCO for
assistance, if the agency questions whether the consumer is able to direct his/her own care or is
non-compliant with Medicaid rules and regulations; and
o Immediately reporting abuse, neglect, or exploitation pursuant to NMSA 1978, Section 27-7-30
and in accordance with the Adult Protective Services Act, by fax, within 24 hours of the incident
being reported to the agency; reportable incidents may include but are not limited to abuse,
neglect and exploitation as defined below:
▪ Abuse is defined as the willful infliction of injury, unreasonable confinement, intimidation, or
punishment with resulting physical harm, pain or mental anguish to a consumer;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
157 | P a g e
▪ Neglect is defined as the failure to provide goods and services necessary to avoid physical
harm, mental anguish, or mental illness to a consumer;
▪ Exploitation is defined as the deliberate misplacement or wrongful, temporary or permanent
use of a consumer’s belongings or money without the voluntary and informed consent of the
consumer; and
o Submit written incident reports to Medicaid or its designee, and the MCO, on behalf of the
consumer, within 24 hours of the incident being reported to the PCS agency; the PCS agency
must provide the consumer with an appropriate form for completion; reportable incidents may
include, but are not limited to:
▪ Death of the consumer:
• Unexpected death is defined as any death of an individual caused by an accident, or an
unknown or unanticipated cause; and/or
• Natural/expected death is defined as any death of an individual caused by a long-term
illness, a diagnosed chronic medical condition, or other natural/expected conditions
resulting in death;
▪ Other reportable incidents:
• Environmental hazard is defined as an unsafe condition that creates an immediate threat
to life or health of a consumer;
• Law enforcement intervention is defined as the arrest or detention of a person by a law
enforcement agency, involvement of law enforcement in an incident or event, or
placement of a person in a correctional facility;
• Emergency services refers to admission to a hospital or psychiatric facility or the
provision of emergency services that results in medical care that is not anticipated for
this consumer and that would not routinely be provided by a PCP; and/or
• Any reports made to APS.
o Informing the consumer and his/her attendant of the responsibilities of the agency;
o Developing an IPoC based on the assessment, services authorization, task list, and consideration
of natural supports provided by the MCO;
o Providing an informed consent form to consumers if the agency chooses not to provide
transportation services as part of support services;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
158 | P a g e
o Identifying a consumer with an improved or declining health condition or whose needs have
changed (i.e. more or less natural supports) and believe the consumer is in need of more or
fewer services should send written notification to the MCO for an LOC determination and
additional assessment of need of services; and
o Maintaining documentation in the consumer's file regarding legal and personal representatives,
as applicable.
• For agencies providing PCS under the consumer-directed model, the responsibilities include:
o Providing services through an agency with choice model or as a fiscal employer agent, and
complying with all applicable state and Federal employment laws as applicable to the provision
of such services;
▪ Agency with choice, in which the agency is the legal employer of the personal care
attendant and the consumer is the managing employer and the agency maintains at least
quarterly in-person contact with the consumer;
▪ Fiscal employer agent (FEA) in which the consumer is the legal employer of record (EOR)
and the managing employer; and the agency maintains at least quarterly in-person contact
with the consumer;
o Obtaining from the consumer or his/her legal representative a signed agreement in which the
attendant agrees that he/she will not provide PCS while under the influence of drugs or alcohol
and acknowledges that if he/she is under the influence of drugs or alcohol while providing PCS
he/she will be immediately terminated; the agency must maintain a copy of the signed
agreement in the attendant’s personnel file, for the consumer;
o Obtaining a signed agreement from each consumer accepting responsibility for all aspects of
care and training, including mandatory training in CPR, first aid for all attendants, competency
testing, TB testing, Hepatitis B immunizations, or a waiver of providing such training, and
accepting the consequences thereof; supervisory visits are not included in the
consumer-directed option; however; the agency must maintain at least quarterly in-person
contact with the consumer; a copy of the signed agreement must be maintained in the
consumer’s file;
o Encouraging the care giver to complete mental health first aid training and providing
information on where the training can be obtained;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
159 | P a g e
o Verifying, if the consumer has selected the consumer’s legal representative as the attendant,
that the consumer has obtained prior approval from Medicaid or its designee; any PCS provided
by the consumer’s legal representative must be justified, in writing, by the agency and
consumer, and submitted for approval to the MCO prior to employment; the justification must
demonstrate the unavailability of other qualified attendants in the applicable area, and indicate
how timesheets will be verified to ensure that services were provided; documentation of
written approval by the MCO must be maintained in the consumer’s file; the agency must
inform the consumer that if the consumer selects a legal representative during the plan year,
the consumer must notify the agency immediately, and the agency must ensure appropriate
documentation is maintained in the consumer’s file;
o Establishing and explaining to the consumer necessary payroll documentation for
reimbursement of PCS;
o Performing payroll activities for the attendants, such as, but not limited to, state and Federal
income tax and social security withholding and making payroll liability payments;
o Arranging for unemployment coverage and workers’ compensation insurance;
o Informing the consumer of available resources for necessary training, if requested by the
consumer, in the following areas: hiring, recruiting, training, supervision of attendants,
advertising, and interviewing techniques;
o Making a referral to an appropriate social service agency, legal agency(s) or Medicaid designee
for assistance, if the agency questions the ability of the consumer to direct his/her own care;
and
o Maintaining a consumer file, and an attendant personnel file for the consumer, for a minimum
of six years.
• For agencies providing PCS under the consumer-delegated model, the responsibilities include, but
are not limited to the following:
o Employing, terminating, and scheduling qualified attendants; and/or
o Conducting or arranging for training of all attendants for a minimum of 12 hours annually; initial
training must be completed within the first three months of employment and must include:
▪ An overview of PCS;
▪ Living with a disability or chronic illness in the community;
▪ CPR, first aid training;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
160 | P a g e
▪ A written competency test with a minimum passing score of at least 80%; expenses for all
training are to be incurred by the agency; other training may take place throughout the year
as determined by the agency; the agency must maintain in the attendant’s file: copies of all
training certifications; CPR and first aid certifications must be current;
▪ Documentation of all training must include at least: name of trainee, title of the training,
source, number of hours, and date of training;
▪ Documentation of competency testing must include at least the following: name of
individual being evaluated, date and method used to determine competency, and a copy of
the attendant’s graded competency test indicating a passing score of at least 80%; special
accommodations must be made for attendants who are not able to read or write, or who
speak, read, or write only language(s) other than English;
o Developing and maintaining a procedure to ensure trained, qualified attendants are available as
backup for regularly scheduled attendants, and for emergency situations; complete instructions
regarding the consumer’s care and a list of attendant responsibilities must be available in each
consumer’s home;
o Informing the attendant of the risks of Hepatitis B infection per current DOH or the Centers for
Disease Control and Prevention (CDC) recommendation, and offering Hepatitis B immunization
at the time of employment at no cost to the attendant; attendants are not considered to be at
risk for Hepatitis B since only non-medical services are performed; therefore attendants may
refuse the vaccine; documentation of the immunization, prior immunization, or refusal of
immunization must be in the attendant’s personnel file;
o Obtaining a copy of the attendant’s current and valid State driver’s license or other current and
valid State photo identification if the consumer is to be transported by the attendant; obtaining
a copy of the attendant’s current and valid driver’s license and current motor vehicle insurance
policy; maintaining copies of these documents in the attendant’s personnel file;
o Complying with Federal and state labor laws;
o Preparing all documentation necessary for payroll;
o Complying with Medicaid participation requirements outlined in 8.302.1 NMAC, General
Provider Policies;
o Maintaining records sufficient to fully disclose the extent, duration, and nature of services
furnished to the consumers as outlined in 8.302.1 NMAC, General Provider Policies;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
161 | P a g e
o Obtaining from the attendant a signed agreement, in which the attendant agrees that he/she
will not provide PCS while under the influence of drugs or alcohol and acknowledges that if
he/she is under the influence of drugs or alcohol while providing PCS, he/she will be
immediately terminated;
o Ensuring, if the consumer has elected the consumer’s legal representative as his/her attendant,
the agency has obtained prior approval from Medicaid or its designee; all PCS provided by the
consumer’s legal representative must be justified in writing by the agency and consumer and
submitted for approval to the MCO prior to employment; the justification must demonstrate the
unavailability of other qualified attendants in the applicable area and include a plan for
oversight by the agency to assure service delivery; documentation of approval by the MCO must
be maintained in the consumer’s file; the agency must inform the consumer that if the
consumer is appointed or selects a legal representative any time during the plan year, they must
notify the agency immediately;
o Establishing and explaining to all their consumers and all attendants the necessary
documentation needed for reimbursement of PCS;
o Performing payroll activities for the attendants;
o Providing workers’ compensation insurance for attendants; and/or
o Conducting face-to-face supervisory visits in the consumer’s residence at least monthly (12 per
service plan year); each visit must be documented in the consumer’s file indicating:
▪ Date of visit;
▪ Time of visit to include length of visit;
▪ Name and title of person conducting supervisory visit;
▪ Individuals present during visit;
▪ Review of IPoC;
▪ Identification of health and safety issues and quality of care provided by attendant, and
▪ Signature of consumer or consumer's legal representative;
o Maintaining an accessible and responsive 24-hour communication system for consumers to use
in emergency situations to contact the agency;
o Following current recommendations of DOH and CDC, as appropriate, for preventing the
transmission of TB; and

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
162 | P a g e
o Verifying initially prior to employment, and annually thereafter, that attendants are not on the
employee abuse registry by researching COR pursuant to 8.11.6 NMAC and in accordance with
the Employee Abuse Registry Act, NMSA 1978, Section 27-7A-1 et seq.
• Personal Care Attendant Responsibilities: Personal care attendants providing PCS for consumers
electing either consumer-directed or consumer delegated must comply with the following
responsibilities and requirements. They include:
o Being hired by the consumer (consumer-directed model) or the PCS agency
(consumer-delegated model);
o Not being the spouse of a consumer, pursuant to 42 CFR Section 440.167;
o Providing the consumer (consumer-directed), or the PCS agency (consumer-delegated), with
proof and copies of their current valid state driver’s license or current valid state photo
identification, and if the attendant will be transporting the consumer, current valid driver’s
license and current motor vehicle insurance policy;
o Being 18 years of age or older;
o Ensuring, if the attendant is the consumer’s legal representative, and is the selected individual
for hire, prior approval has been obtained from the MCO; any PCS provided by the consumer’s
legal representative must be justified, in writing, by the PCS agency, and consumer, having been
submitted for written approval to the MCO prior to employment; the justification must
demonstrate the unavailability of other qualified attendants in the applicable area and indicate
how timesheets will be verified to ensure services were provided; documentation of approval by
the MCO must be maintained in the consumer’s file; and submit appropriate documentation of
time worked and services performed ensuring that he/she has signed his/her time
sheet/log/check list verifying the services provided to the consumer;
o Successfully passing a nationwide caregiver criminal history screening, pursuant to 7.1.9 NMAC
and in accordance with NMSA 1978, Section 29-17-2 et seq., of the Caregivers Criminal History
Screening Act, performed by an agency certified to conduct such checks; attendants are
required to submit to a criminal history screening within the first 20 calendar days of hire; an
attendant may be conditionally hired by the agency contingent upon the receipt of written
notice from the certified agency of the results of the nationwide criminal history screening;
attendants who do not successfully pass a nationwide criminal history screening are not eligible
for further PCS employment. The agency is responsible for the cost of the first criminal history

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
163 | P a g e
screening and the member and/or caregiver is responsible for any additional caregiver history
screenings and the associated costs thereafter if the caregiver’s termination of employment is a
result of termination on behalf of the member for an unjustifiable reason not related to the
agencies standard employment conditions. If the caregiver quits or termination is a result of the
caregiver failing to meet standard employment conditions outlined by the agency, the agency
will be responsible for the criminal history screening for the next hired caregiver;
o Ensuring while employed as an attendant he/she will not be under the influence of drugs or
alcohol while performing PCS; the attendant must complete and sign an agreement with the
agency or consumer in which the attendant acknowledges that if he/she is under the influence
of drugs or alcohol while providing PCS he/she will be immediately terminated;
o May not be the consumer's representative, unless he/she is also the legal representative;
o If the attendant is a member of the consumer’s family, he/she may not be paid for services that
would have otherwise been provided to the consumer; if the attendant is a member of the
consumer’s household, he/she may not be paid for household services, support services
(shopping and errands), or meal preparation that are routinely provided as part of the
household division of chores, unless those services are specific to the consumer (i.e., cleaning
consumer’s room, linens, clothing, and special diets);
o An attendant may not act as the consumer’s legal representative, in matters regarding medical
treatment, financial or budgetary decision making, unless the attendant has documentation
authorizing the attendant to act in a legal capacity on behalf of the consumer;
o Following current recommendations of DOH and CDC, as appropriate for preventing the
transmission of TB;
o For consumer-delegated care only, completing 12 hours of training yearly; the attendant must
obtain certification of CPR, and first aid training within the first three months of employment,
and the attendant must maintain certification throughout the entire duration of providing PCS;
additional training will be based on the consumer’s needs as listed in the IPoC; attendants must
successfully pass a written personal care attendant competency test with at least 80% correct
within the first three months of employment; and
o Use the EVV system to document when and where PCS were provided to the member.
• Coverage Criteria: PCS have been established to assist individuals 21 years of age or older who are
eligible for full Medicaid benefits and meet the NF LOC criteria. PCS are defined as those tasks

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
164 | P a g e
necessary to avoid institutionalization and maintain the consumer’s functional level and
independence. PCS are for consumers who meet NF LOC because of disability or functional
limitation and need assistance with certain ADLs and IADLs. PCS are allocated for a reasonable
accommodation of tasks to be performed by a personal care attendant, but do not provide 24 hours
per day services. A CNA is conducted pursuant to this policy, assessments for services, to determine
the amount and type of services needed to supplement the services a consumer is already receiving
including those services provided by natural supports. PCS are not provided 24 hours a day and
allocation of time and services must be directly related to an individual’s functional level to perform
ADLs and IADLs as indicated in the CNA.
o PCS are usually furnished in the consumer’s residence, except as otherwise indicated, and
during the hours specified in the consumer’s IPoC. Services may be furnished outside the
residence only when appropriate and necessary and when not available through other existing
benefits and programs, such as HH or other State plan or LTC services. If a consumer is receiving
hospice care, is a resident in an ALF, shelter home, or room and board facility, the MCO will
perform a CNA and ensure the PCS does not duplicate the services that are already being
provided. If ADL or IADL services are part of the hospice or ALF, shelter home, or room and
board facility, as indicated by the contract or admission agreement signed by the consumer, PCS
cannot duplicate those services. Regulations for assisted living facilities may be found at 7.8.2
NMAC, Assisted Living Facilities for Adults.
o PCS are not furnished to an individual who is an inpatient or resident of a hospital, NF, ICF/IID,
MH facility, correctional facility, other institutional settings, except for recipients of community
transition goods or services.
o All consumers, regardless of living arrangements, will be assessed for natural supports. PCS are
not intended to replace natural supports. Service hours will be allocated, as appropriate, to
supplement the natural supports available to a consumer. Consumers that reside with other
adult household members, that are not receiving PCS or are not disabled, will be presumed to
have household services in the common/shared areas provided by the other adult residents,
whether or not the adult residents are the selected personal care attendant. Personal care
attendants that live with the consumer will not be paid to deliver household services, support
services (shopping and errands), or meal preparation that are routinely provided as part of the

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
165 | P a g e
household division of chores, unless those services are specific to the consumer (i.e., cleaning
consumer’s room, linens, clothing, and special diets). If a consumer’s living situation changes:
▪ Such that there is no longer a shared living space with another consumer, he/she will be
re-assessed for services that were allocated between multiple consumers in a shared
household; or
▪ Such that he/she begins sharing a living space with another consumer(s), all consumers in
the new shared living space will be re-assessed to determine the allocation of services
shared by all consumers residing in the household.
• Covered Services: PCS are provided as described in 8.308.12.13 NMAC. PCS will not include those
services for tasks the individual does not need or is already receiving from other sources including
tasks provided by natural supports. PCS must be related to the individual’s functional level to
perform ADLs and IADLs as indicated in the CNA conducted pursuant to this policy, assessments for
services, mobility assistance, either physical assistance or verbal prompting and cueing, may be
provided during the administration of any PCS task by the attendant. Mobility assistance includes
assistance with ambulation, transferring, or repositioning, which is defined as moving around inside
or outside the residence or consumer’s living area with or without assistive devices(s) such as
walkers, canes, and wheelchairs, or changing position to prevent skin breakdown.
o Certain PCS are provided only when the consumer has the ability to self-administer. Ability to
self-administer is defined as the ability to identify and communicate medication name, dosage,
frequency and reason for the medication. A consumer who does not meet this definition of
ability to self-administer is not eligible for these services.
o When two or more consumers living in the same residence, including assisted living facilities,
shelter homes, and other similar living arrangements, are receiving PCS, they will be assessed
both individually and jointly to determine services that are shared. Consumers sharing living
space will be assessed for services identified in Paragraphs (5) and (7) of Subsection I of
8.308.12.13 NMAC: assess each consumer individually to determine if the consumer requires
unique assistance with the service; and jointly with other household members to determine
shared living space and common needs of the household; services will be allocated based on
common needs, not based on individual needs, unless as assessed by the MCO, an individual
need for the service(s) is indicated; common needs may include meals that can be prepared for
several individuals; shopping/errands that can be completed at the same time; laundry that can

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
166 | P a g e
be completed for more than one individual at the same time; dusting and vacuuming of shared
living spaces; these PCS are based on the assessment of combined needs in the household
without replacing natural and unpaid supports identified during the assessment. Description of
PCS refers to 8.308.12.13 NMAC.
• Assessments for Services: After the consumer is determined medically eligible for PCS, the MCO
determines, allocates, and authorizes PCS based on a functional assessment, which is part of the
CNA process. Although a consumer’s assessment for the amount and types of services may vary, PCS
are not provided 24 hours a day. An individual’s PCS are directly related to their functional level to
perform ADLs and IADLs as indicated by the CNA. The CNA is performed when a consumer enters
the program, at least annually or at the discretion of the MCO.
o The CNA determines the type of covered services needed by the consumer. The amount of time
allocated to each type of covered service is determined by applying and recording the
individual’s functional level to perform ADLs and IADLs. PCS are allocated for a reasonable
accommodation of tasks to be performed by a personal care attendant. A CNA determines the
amount and type of PCS needed to supplement and not duplicate the services a consumer is
already receiving including those services provided by natural supports. In the event that the
consumer’s functional needs exceed the average allocation of time allotted to perform a
particular service task per the recommendation of a medical professional, the MCO may
consider authorization of additional time based on the consumer’s verified medical and clinical
need.
o The CNA is conducted by the MCO and discussed with the consumer in the consumer’s primary
place of residence. It serves to document the current health condition and functional needs of
the consumer. It is to include no duplication of services a consumer is already receiving,
including those services provided by natural supports, and shall not be based on a prior
assessment of the consumer's health condition, functional needs, or existing services.
o Any relevant sections of the CNA and the personal care service allocation tool is sent to the PCS
agency by the MCO to allow the PCS agency to develop the IPoC.
o The CNA must be performed by the MCO upon a consumer’s initial approval for medical NF LOC
eligibility to receive PCS and at least annually thereafter, based on their assigned care
coordination level or at the MCO’s discretion. The annual CNA is completed prior to the
expiration of the current NF LOC period and determines the type and amount of services for the

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
167 | P a g e
subsequent NF LOC period. The type and amount of PCS as determined by the CNA shall not be
effective prior to the start of the applicable NF LOC period. An interim assessment may be
conducted if:
▪ There is a change in the consumer’s condition (either improved or declined);
▪ There is a change in the consumer’s natural supports or living conditions; and/or
▪ The consumer requests and interim assessment.
o The MCO must explain each service delivery model at least annually to consumers enrolled in
ABCB.
o The MCO will issue a prior authorization to the PCS agency. A PCS authorization cannot extend
beyond the LOC period and must be provided to the PCS agency prior to the prior authorization
effective date and may not be applied retroactively.
o A PCS consumer who disagrees with the authorized number of hours may utilize the MCO
grievance and appeal process when enrolled in managed care. The consumer must exhaust the
appeals process with the MCO before a fair hearing can be requested pursuant to 8.352.2
NMAC, Recipient Hearings. Upon notification of the resolution of the appeal or grievance, a
member may request a fair hearing with the State. The MCO may schedule a pre-hearing
conference with the consumer to explain how the PCS regulations were applied to the
authorized service time and attempt to resolve issues prior to the fair hearing.
o Continuation of benefits: A member may continue PCS benefits while an MCO grievance and
appeal or State fair hearing decision is pending, pursuant to 8.352.2 NMAC, Recipient Hearings,
if the member requests continuation of benefits within 10 calendar days of the date of the
Notice of Action.
o The member shall be responsible for repayment of the cost of the services furnished while the
MCO grievance and appeal process or the State’s fair hearing process was pending, to the extent
the services were furnished solely because of this requirement to provide continuation of
benefits during the MCO grievance and appeal or state fair hearing process. The MCO may
recover these costs from the member, not the provider.
• IPOC: An IPoC is developed, and PCS are identified, with the appropriate assessment (CNA) for
allocating PCS. The PCS agency develops an IPoC using an MCO authorization.
The PCS agency, with the consumer’s consent, may use the authorized allocation of hours in an
individualized schedule. The individualized schedule of services allows the consumer and PCS agency

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
168 | P a g e
flexibility while maintaining a focus on the consumer’s health and safety. The IPoC will clearly
document the consumer’s consent to the schedule. The PCS agency and consumer will develop the
schedule for the number of days-per-week and hours-per-day to complete the needed ADL and IADL
assistance. The PCS agency shall establish the appropriate monitoring protocols to ensure this
flexible schedule does not adversely affect the consumer’s health and safety.
Should the MCO determine, based on care coordination, IPoC reviews, or other quality oversight
that the IPoC does not adequately meet the consumer’s needs or has created a health and/or safety
concern, the MCO will communicate a request to the PCS Agency that the IPoC will need to be
adjusted to ensure the consumer’s care needs are met. The PCS agency will follow the standard IPoC
process utilizing the PCS Allocation Tool and will resubmit the IPoC for re-review within seven
calendar days from receipt of request by the MCO.
o The PCS agency must:
▪ Develop the IPoC with a specific description of the attendant’s responsibilities, including
tasks to be performed by the attendant and any special instructions related to maintaining
the health and safety of the consumer;
▪ Ensure the consumer has participated in the development of the plan and the IPoC is
reviewed and signed by the consumer or the consumer’s legal representative; a consumers’
signature on the IPoC indicates the consumer understands what services have been
identified and that services will be provided on a weekly basis for a maximum of one year; if
a consumer is unable to sign the IPoC and the consumer does not have a legal
representative, a thumbprint or personal mark (i.e., an “X”) will suffice; if signed by a legal
representative, Medicaid or its designee and the agency must have documentation in the
consumer’s file verifying the individual is the consumer’s legal representative;
▪ Maintain an approved IPoC for PCS for a maximum of one year (12 consecutive months), a
new IPoC must be developed at least annually, to ensure the consumer’s current needs are
being met; a consumer’s previous year IPoC is not used or considered in developing a new
IPoC and allocating services; a new IPoC must be developed independently at least every
year based on the consumer’s current medical condition; the tasks and number of hours in
the IPoC must match the authorized tasks and number of hours on the authorization;
▪ Submit the IPoC to the MCO for review if the IPoC varies from the PCS Allocation Tool;
Provide the consumer with a copy of their approved IPoC;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
169 | P a g e
▪ Obtain an approved task list and/or CNA;
▪ Obtain written verification the consumer, or the consumer’s legal representative,
understands if the consumer does not utilize services, for two months, the full amount of
allocated services on the IPoC, that these circumstances will be documented in the
consumer’s file; and
▪ Submit a personal care transfer/closure form (MAD 062 or other approved transfer/closure
form) to the MCO for a consumer who has passed away or who has not received services for
90 consecutive days.
• PCS are to be delivered only in the State of New Mexico. However, consumers who require PCS out
of the state may request an exception and must obtain written approval from the MCO for out of
state delivery of service prior to leaving the state. The following must be submitted for
consideration when requesting medically necessary out of state services:
o A letter from the consumer or the consumer’s legal representative requesting an out of state
exception and reasons for the request; the letter must include:
▪ The consumer’s name and SSN;
▪ How time sheets/logs/check-off list will be transmitted and payroll checks issued to the
attendant;
▪ Date the consumer will be leaving the state, including the date of the medical procedure or
other medical event, the anticipated date of return;
▪ Where the consumer will be housed after the medical procedure;
o A letter or documentation from the physician, surgeon, physician assistant, nurse practitioner,
or clinical nurse specialist verifying the date of the medical procedure; and
o A copy of the consumer’s approved IPoC and a proposed adjusted revision of services to be
provided during the time the consumer is out-of-state; support services and household services
will not be approved unless justified; if the consumer has been approved for services under
self-administered medications, a statement from the physician, physician assistant, nurse
practitioner, or clinical nurse specialist must be included indicating the consumer will continue
to have the ability to self-administer for the duration of time he/she is out-of-state.
▪ Utilization Review (UR): All PCS require prior LOC approval by the MCO; therefore,
retroactive services are not authorized. All PCS are subject to UR for medical necessity and

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
170 | P a g e
program compliance. The MCO will perform UR for medical necessity. The MCO makes final
authorization of PCS using:
▪ The HSD-approved LOC criteria; and
▪ The CNA.
• PCS Agency Transfer Process: A consumer requesting to transfer services from one PCS agency to
another Medicaid-approved PCS agency may request a transfer form (MAD 062) or other approved
transfer/closure form) from his/her MCO. Transfers may only be initiated by the consumer, his/her
legal representative, or by a PCS agency on behalf of a consumer or his/her legal representative.
Transfer requests shall not be requested by the personal care attendant. Transfer approvals are
determined by the MCO and should be initiated by the consumer through the consumer’s assigned
Care Coordinator.
The following outlines the process for PCS Agency Transfers:
o The consumer must inform his/her MCO of the desire to transfer to another PCS agency;
o The consumer must complete a MAD 062 or an approved transfer form to include: the
consumer’s signature; the date of the signature of the receiving PCS agency; and the justification
for the transfer;
o The MCO will process the transfer request within 15 business days after receipt of the transfer
request;
o If approved, the MCO works with both the agency from which the consumer is currently
receiving services (originating agency) and the agency to which the consumer would like to
transfer (receiving agency) to complete the transfer;
o Originating agencies are responsible for continued provision of services until the transfer is
complete;
o Upon approval of the request, the MCO will issue a new prior authorization to the receiving
agency and make the transfer date effective 10 business days from the date of processing the
transfer. The prior authorization will include: a new prior authorization number and new DOS
and units remaining for the remainder of the IPoC year;
o The MCO will notify the consumer as well as the receiving PCS agency and issue an ending
authorization to the originating agency; and
The following outlines the MCO review process for PCS agency transfers:

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
171 | P a g e
o When the MCO receives a request for a transfer from a consumer or PCS agency on behalf of a
consumer or his/her legal representative, the consumer’s Care Coordinator will interview the
consumer to determine if the request is consumer-driven;
o The Care Coordinator will ask the consumer or his/her legal guardian for specific reasons for the
transfer, including but not limited to: Will you be taking your caregiver with you? If the
consumer is taking his/her caregiver, the Care Coordinator should ask why the consumer is
requesting a transfer;
o The Care Coordinator will contact the originating and the receiving agency to investigate the
reasons given by the consumer and/or legal representative. In addition, the Care Coordinator
will ensure the consumer has notified both agencies;
o If, during the review process, the MCO determines the originating and/or receiving agency is not
compliant with the applicable Medicaid regulations, the MCO shall conduct an audit of the
agency and, if necessary, provide additional training or impose a corrective action plan (CAP).
For example, if the receiving agency has engaged in solicitation, or if the originating agency is
not sending back-up caregivers or the caregivers are not showing up on the scheduled days or
for the hours care is planned for, these issues need to be addressed by the MCO and corrected
by the agencies;
o If, during the course of the review process, the Care Coordinator finds that the consumer has
requested three transfers within a six-month period, the Care Coordinator shall meet with the
consumer and/or legal guardian to try to determine the reason for such requests and consider
whether to approve or deny the transfer;
o The consumer and/or legal guardian will not be allowed to hire an individual to be his/her
attendant who has not passed a nationwide criminal history screening or an attendant that has
been terminated from another agency for fraudulent activities or other misconduct. The Care
Coordinator will educate the consumer about the Medicaid PCS policies;
o When reviewing a transfer request, the MCO should take into consideration whether the
consumer can speak and read English. If the consumer does not speak or read English, the MCO
shall provide a translator to ensure the consumer’s options have been explained and the
consumer fully understands his/her options, and the service model selected is available to the
consumer;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
172 | P a g e
o The Care Coordinator should ensure the location of the agency or provider is convenient to the
consumer;
o A consumer who does not agree with the MCO’s decision shall utilize the MCO grievance and
appeal process;
o Upon receiving notification of the resolution of the appeal or grievance by the MCO, a consumer
may request a fair hearing pursuant to 8.352.2 NMAC, Recipient Hearings;
o The originating agency is responsible for the continuance of PCS while the hearing is pending, if
continuation of benefits is requested timely by the consumer and approved by the MCO;
All requests for change of service model (from/to, directed/delegated) must be approved by the MCO
prior to the receiving agency providing services to the consumer; and
A transfer requested by a consumer may be denied by the MCO for the following reasons:
o The consumer is requesting more hours/services;
o The consumer’s attendant or family member is requesting the transfer;
o The consumer has requested three or more transfers within a six-month period;
o The consumer wants his/her legal guardian, spouse or attorney-in-fact to be his/her attendant;
o The consumer wants an individual to be his/her attendant who has not successfully passed a
nationwide criminal history screening;
o The consumer wants an attendant who has been terminated from another agency for
fraudulent activities or other misconduct;
o The attendant does not want to complete the mandated trainings under the
consumer-delegated model;
o The consumer does not wish to comply with the Medicaid or PCS regulations and procedures;
and
o There is reason to believe that solicitation has occurred as defined in this policy in the,
Solicitation/Advertising Section in this Manual.
• Consumer Closure: The transfer/closure form may also be used by a consumer or PCS agency to
initiate closure of PCS for a member who has gone 90 consecutive days or more without PCS. The
PCS agency will submit the transfer/closure form to the MCO and the MCO will call and verify with
the consumer that PCS are no longer needed or wanted. After verification is received the MCO will
provide an end authorization to the PCS agency.
• Consumer Discharge: A consumer may be discharged from a PCS agency.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
173 | P a g e
• PCS Agency Discharge: The PCS agency may discharge a consumer for a justifiable reason, as
explained below. Prior to initiating discharge, the PCS agency must send a notice to the MCO for
approval. Once approved by the MCO, the PCS agency may initiate the discharge process with a 30-
day written notice to the consumer. The notice must include the consumer’s right to request an
appeal with the MCO and that he/she must exhaust the grievance and appeal process with the MCO
before a fair hearing can be filed with HSD pursuant to 8.352.2 NMAC, Recipient Hearings. The
notice must include the justifiable reason for the agency’s decision to discharge.
o A justifiable reason for discharge may include:
▪ Staffing problems (i.e., excessive request for change in attendants, such as three or more
during within 30 calendar days);
▪ A consumer demonstrates a pattern of verbal or physical abuse toward attendants or
agency personnel, including the use of vulgar or explicit (i.e., sexual) language, sexual
harassment, excessive use of force, use of verbal threats or physical threats, or intimidating
behavior; the agency or attendant must have documentation demonstrating the pattern of
abuse; the agency may also discharge a consumer if the life or safety of an attendant or
agency’s staff member is believed is in immediate danger;
▪ A consumer or family member demonstrates a pattern of uncooperative behavior including
not complying with agency or Medicaid regulations; not allowing the PCS agency to enter
the home to provide services; and continued requests to provide services not approved on
the IPoC;
▪ Illegal use of narcotics or alcohol abuse;
▪ Fraudulent submission of timesheets; or
▪ Living conditions or environment that may pose a health or safety risk or cause harm to the
personal care attendant, employee of an agency, MCO, or other Medicaid designee.
o The MCO must provide the consumer with a current list of Medicaid-approved personal care
agencies that service the county in which the consumer resides. The PCS agency must assist the
consumer in the discharge process, cooperate with the MCO, and continue services throughout
the discharge. If the consumer does not select another PCS agency within the 30-day time
frame, the current PCS agency must inform the MCO’s Care Coordinator and the consumer that
a lapse in services will occur until the consumer selects an agency.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
174 | P a g e
o A consumer has a right to appeal the PCS agency’s decision to suspend services. The consumer
must exhaust the MCO grievance and appeal process prior to requesting a fair hearing with HSD
as outlined in 8.352.2 NMAC, Recipient Hearings.
o Discharge by the state: Medicaid or its designee reserves the right to discontinue the
consumer’s receipt of PCS due to the consumer’s non-compliance with Medicaid regulations
and/or PCS requirements. The discontinuation of PCS does not affect the consumer’s Medicaid
eligibility. The consumer may be discharged for a justifiable reason by means of a 30-day written
notice to the consumer. The notice will include the duration of discharge, which may be
permanent, the consumer’s right to request a fair hearing, pursuant to 8.352.2 NMAC, Recipient
Hearings, and the justifiable reason for the discharge. A justifiable reason for discharge may
include:
o Staffing problems (i.e., unjustified excessive requests for change in attendants, such as three or
more during a 30-day period), excessive requests for transfers to other agencies or excessive
agency discharges;
o A consumer who demonstrates a pattern of verbal or physical abuse toward attendants, agency
personnel, or state staff or contractors, including use of vulgar or explicit sexual language, verbal
or sexual harassment, excessive use of force, demonstrates intimidating behavior, verbal or
physical threats toward attendants, agency personnel, or state staff or contractors;
o A consumer or family member who demonstrates a pattern of uncooperative behavior
including, noncompliance with agency, Medicaid program requirements or regulations or
procedures;
o Illegal use of narcotics, or alcohol abuse;
o Fraudulent submission of timesheets;
o Unsafe or unhealthy living conditions or environment; and/or
o PCS agencies and the MCO are responsible for documenting and reporting any incidents
involving a consumer to Medicaid or its designee.
Reimbursement
A Medicaid-approved PCS agency will process billings in accordance with the MCO billing instructions.
Reimbursement for PCS will be based on the negotiated rate with the MCO.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
175 | P a g e
The agency’s billed charge must be the usual and customary charge for services. “Usual and customary
charge” refers to the amount an individual provider charges the general public in the majority of cases
for a specific service and level of service.
PCS Provider Voluntary Disenrollment
A Medicaid-approved PCS agency may choose to discontinue provision of services by disenrollment.
Once approved by Medicaid or its designee, the PCS agency may initiate the disenrollment process to
assist consumers to transfer to another Medicaid approved PCS agency. The PCS agency must continue
to provide services until consumers have completed the transfer process and the agency has received
approval from Medicaid or its designee to discontinue services. Prior to disenrollment, the PCS agency
must send a notice to Medicaid or its designee for approval. The notice must include:
• Consumer notification letter;
• List of all the Medicaid approved personal care agencies serving the county in which the consumer
resides; and
• List of all consumers currently being served by the agency and the MCO in which they are enrolled.
Solicitation/Advertising
For the purposes of this section, solicitation shall be defined as any communication regarding PCS
services from an agency’s employees, affiliated providers, agents or contractors to a Medicaid member
who is not a current client that can reasonably be interpreted as intended to influence the recipient to
become a client of that entity. Individualized personal solicitation of existing or potential consumers by
an agency for their business is strictly prohibited.
• Prohibited solicitation includes, but is not limited to, the following:
o Contacting a consumer who is receiving services through another PCS or any another Medicaid
program;
o Contacting a potential consumer to discuss the benefits of its agency, including door-to-door,
telephone, mail and email solicitation;
o Offering a consumer/attendant a finder fee, higher wage, kick back, or bribe consisting of
anything of value to the consumer to obtain transfers to its agency; see 8.351.2 NMAC,
Sanctions and Remedies;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
176 | P a g e
o Directly or indirectly engaging in door-to-door, telephone, or other cold-call marketing activities
by the entity’s employees, affiliated providers, agents or contractors;
o Making false promises;
o Misinterpretation or misrepresentation of Medicaid rules, regulations or eligibility;
o Misrepresenting itself as having affiliation with another entity; and/or
o Distributing PCS-related marketing materials.
• Penalties for engaging in solicitation prohibitions: Agencies found to be conducting such activity will
be subject to sanctions and remedies as provided in 8.351.2 NMAC and applicable provisions of the
PPA.
• An agency wishing to advertise for PCS provision must first get prior written approval from Medicaid
or its designee before conducting any such activity. Advertising and community outreach materials
means materials that are produced in any medium, on behalf of a PCS agency and can reasonably be
interpreted as advertising to potential clients. Only approved advertising materials may be used to
conduct any type of community outreach. Advertising or community outreach materials must not
misrepresent the agency as having affiliation with another entity or use proprietary titles, such as
“Medicaid PCS”. Any PCS agency conducting any such activity without prior written approval from
Medicaid or its designee will be subject to sanctions and remedies as provided in 8.351.2 NMAC and
applicable provisions of the PPA.
Sanctions and Remedies
Any agency or contractor that is not compliant with the applicable Medicaid regulations is subject to
sanctions and remedies as provided in 8.351.2 NMAC.
8.15. Private Duty Nursing (PDN) for Adults
PDN services provide members who are 21 years of age and older with intermittent or extended direct
nursing care in the member’s home. All services provided under PDN require the skills of a licensed RN
or a LPN under a written physician’s order in accordance with the New Mexico Nurse Practice Act, Code
of Federal Regulation for Skilled Nursing. PDN services are planned in collaboration with the physician,
the member, and the MCO Care Coordinator. All services provided under PDN are pursuant to a
physician’s order and in conjunction with the MCO. The private duty nurse will develop and implement a
PCCP/Treatment (CMS form 485) that is separate from the CCP developed by the MCO. Members do not

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
177 | P a g e
have to be homebound in order to receive this service. PDN and Medicare/Medicaid skilled nursing may
not be provided at the same time. PDN services offered through the ABCB program will vary in scope
and duration from Medicare and Medicaid skilled nursing. PDN services will be offered to members who
are 21 years of age and older receiving the CB service as the provider of last resort in accordance with
the State Medicaid Plan, State Medicaid Manual, Part 4, Section 4310 and Section 4442.1. A copy of the
written referral will be maintained in the member’s file by the PDN provider and shared with the MCO
Care Coordinator. Children (individuals under the age of 21) receive this service through the EPSDT.
PDN services are provided with the understanding that the MCO is the payer of last resort. PDN services
should not be requested or authorized until all other third party and community resources have been
explored and/or exhausted. If services are available for reimbursement through third party liability or
other payment sources, these sources must be accessed before ABCB services are delivered.
Scope of Services/Requirements:
Specific services may include the following:
• Obtaining pertinent medical history;
• Observing and assessing the member’s condition;
• Administration of medications including: oral, parenteral, gastrostomy, jejunostomy, inhalation,
rectal and topical routes;
• Providing wound care, suture removal and dressing changes;
• Monitoring feeding tubes (i.e., gastrostomy, naso-gastric, or jejunostomy including patency),
including signs of possible infection;
• Monitoring bladder program and providing care, including ostomy and indwelling catheter insertion
and removal;
• Monitoring aspiration precautions;
• Monitoring administration of oxygen, ventilator management, and member’s response;
• Monitoring infection control methods;
• Monitoring seizure protocols;
• Collecting specimens (blood, urine, stool, or sputum) and obtaining cultures as ordered by the
member’s primary physician;
• Alerting the member’s physician to any change in health status;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
178 | P a g e
• Monitoring nutritional status of the member and reporting any changes to the physician and
nutritionist if available;
• Maintaining member intake and output flow sheets as ordered by the physician;
• Performing physical assessments including monitoring of vital signs and the member’s medical
condition as warranted;
• Providing education and training to the member’s appropriate family member(s) and primary
caregiver(s) regarding care needs and treatments etc. The goal for education and training is to
encourage self-sufficiency in delivery of care by the family or primary caregiver;
• Providing staff supervision of appropriate activities, procedures and treatment;
• Developing the PCCP/treatment in collaboration with the member, and the MCO Care Coordinator.
The plan will identify and address the member’s specific needs in accordance with the physician’s
orders. Develop and implement the PCCP/treatment (CMS form 485) on the basis of the member
assessment and evaluation;
• Analyzing and interpreting member’s needs on the basis of medical history, pertinent precautions,
limitations, and evaluative findings;
• Developing interventions to assist the member to achieve and promote health to meet the
member’s needs;
• Developing individualized service goals, identifying short-and long-term goals that are measurable
and objective; and/or
• Documenting dates and types of treatments performed, as well as member’s response to
treatment and progress toward all goals.
Requirements include the following:
• The private duty nurse must perform a comprehensive assessment/evaluation for each member
and coordinate with the MCO Care Coordinator to determine appropriate services annually at a
minimum or at each visit;
• PDN services listed in the PCCP are to be within the scope of the New Mexico Nurse Practice Act,
are provided subsequent to obtaining a physician’s order and under the supervision of a RN.
Physician’s orders will contain the following:
o The task to be performed;
o How frequently the task is to be performed;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
179 | P a g e
o The duration that the order is applicable; and
o Any individualized instructions. Additionally, a physician’s order will be obtained for the
revision of any PDN service and annually with the PCCP renewal, if PDN are to continue.
• The PDN supervisor will provide clinical supervision in the member’s home at a minimum of once
each quarter. Supervision of PDN services must be documented in the member’s clinical record;
• All services must be under the order of the member’s PCP. The order will be obtained by an RN
working for the agency that provides PDN services, and will be shared with the MCO Care
Coordinator;
• The PCCP/Treatment (Form CMS-485) will be provided to the MCO Care Coordinator. Within 48
hours of any changes ordered by the physician, the provider agency will inform the MCO Care
Coordinator of physician ordered changes and the agency’s ability or inability to provide PDN in
accordance with the Care Plan. The provider agency will provide the MCO Care Coordinator with a
copy of revised orders;
• Submitting initial and quarterly progress reports to the MCO. Copies of quarterly progress reports
sent to the MCO will be maintained in the member file and will include an assessment of the
member’s current status, health and safety issues and the progress goals as listed on the
PCCP/Treatment;
• Reports must be current and available upon request of HSD/MAD;
• Reviewing and revising the PDN PCCP/Treatment making appropriate treatment modifications as
necessary and coordinate with the MCO Care Coordinator of the changes that may need to be
identified and/or changed on the CCP;
• Document complications that delay, interrupt, or extend the duration of the services in the
member’s medical record as well as communication with the member’s physician;
• Reviewing physician’s request for treatment. If appropriate, recommend revisions to the Care Plan
to the MCO Care Coordinator by requesting a conference; and
• Providing member and/or caregiver education regarding services. Document the date and time this
occurred in the member’s clinical file.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
180 | P a g e
Provider Requirements/Qualifications:
• PDN services must be provided by an active, Medicaid approved provider type 363, PDN provider;
• PDN providers must maintain (no gap in license) a full permanent license through the New Mexico
Board of Nursing;
• PDN services may also be furnished through a licensed HH Agency, licensed RHC or certified FQHC
who meet all requirements/qualifications in this section of the policy and are approved by the
HSD/MAD/LTSSB as a provider type 363, PDN provider;
• PDN providers must comply with provision of the Nurse Practice Act and all city, state and federal
rules/regulations;
• In order to be approved and certified by the HSD/MAD LTSSB, PDN providers must be operating
with a full permanent license. All incomplete applications submitted to the HSD/MAD/LTSSB shall
be rejected and not considered for review until a complete application is submitted. Provisional
licenses will not be accepted; and
• PDN providers must comply with all applicable State and Federal rules and regulations under the
Nurse Practice Act and program standards determined by HSD/MAD including but not limited to
CBCs, OSHA training requirements, incident management system reporting, labor laws, etc.
Staffing Requirements:
o An RN or LPN is considered a qualified private duty nurse when the following criteria are met:
▪ Must have current (no gaps in license) licensure as required by the state of New Mexico;
provisional licenses are not acceptable;
▪ Nursing experience preferably with disabled and elderly individuals. This includes settings
such as HH, hospital, NF facility, or other types of clinics and institutions;
▪ Nursing services must be furnished through a licensed HH Agency, licensed RHC or certified
FQHC;
▪ RNs who supervise must have at least one year of supervisory experience. Supervision of
LPNs must be provided by an RN and shall be in accordance with the New Mexico Nursing
Practice Act. The supervision of all personnel is the responsibility of the agency’s
Administrator and Director;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
181 | P a g e
▪ Be culturally sensitive to the needs and preferences of members and their households
based upon language. Communicating in a language other than English may be required;
and
▪ Hepatitis B vaccine will be offered by the provider agency upon employment at no cost to
the employee per the Federal OSHA requirements. Record of prior Hepatitis B
immunization, acceptance or denial by the employee will be maintained in the employee’s
personnel record.
Reimbursement
PDN providers are responsible for providing clinical documentation that identifies his or her role in all
components of the provision of nursing services, including assessment information, care planning,
intervention, communications, and evaluation. There must be justification in each member’s clinical
record supporting medical necessity for the care and for the level or intensity (frequency and duration)
of the care. All services must be reflected on a CCP that is coordinated with the member/member’s
representative, other caregivers as applicable, and authorized by the MCO. All services provided,
claimed, and billed must have documented justification supporting medical necessity and must be
covered by the ABCB program. Billing is on an hourly basis and is accrued and rounded to the nearest
quarter of an hour. Reimbursement for PDN for adults will be based on the negotiated rate with the
MCO. Providers have the responsibility to review and ensure the information on the prior authorization
for their services is correct. If the provider identifies an error, they will contact the MCO immediately to
have the error corrected.
• Payment for PDN services is through the MCO and is considered payment in full.
• PDN services must abide by all Federal, state, HSD, policies and procedures regarding billable and
non-billable items.
• PDN providers must ensure all insurance records are maintained correctly.
• Billable hours are as follows:
o Face-to-face activities that are described above in the scope of service for PDN;
o Attendance and/or telephone conference call to participant in IDT meetings;
o Development of the PCCP/Treatment, not to exceed four hours annually; and
o Training on member specific issues is reimbursable and included in the negotiated rate; general
training requirements are an administrative cost and not billable.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
182 | P a g e
Limits or Exclusions
• HSD/MAD does not consider the following to be professional PDN services and will not authorize
payment for the following non-billable activities:
o Performing specific errands for the member and/or family that are not program specific;
o Friendly visiting;
o Financial brokerage services, handling of member finances, or preparation of legal documents;
o Time spent on paperwork or travel that is administrative for the provider;
o Transportation of members;
o Pick up and/or delivery of commodities; and
o Other non-Medicaid reimbursable activities.
8.16. Nursing Respite Services
Nursing respite services provide the member’s primary caregiver with a limited leave of absence to
prevent burnout and provide temporary relief to meet a family crisis, emergency or caregiver’s illness as
determined in the CCP. A primary caregiver is the individual who has been identified in the PCCP and
who assists the member on a frequent basis (i.e., daily or at a minimum weekly). It is not necessary for
the primary caregiver to reside with the member in order to receive nursing respite services. Nursing
respite services may be provided in the member’s home, in the nursing respite provider’s home, and in
the community. Nursing respite services may be provided by an RN, or an LPN. Nursing respite services
are limited to a total maximum of 300 hours per PCCP year. Nursing respite services must not be
provided by a member of the member’s household or by any relative approved as the employed, paid
caregiver.
Scope of Services/Requirements:
Specific services may include the following:
• Assistance with routine ADLs such as bathing, eating, meal preparation, dressing, and hygiene;
• Assistance with routine IADLs such as general housekeeping;
• Assistance with PCS or PDN services, based on the member’s needs;
• Assistance with the enhancement of self-help skills;
• Assistance with providing opportunities for leisure, play and other recreational activities.;
Requirements include the following:

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
183 | P a g e
• Nursing Respite services are available to any member of any age;
• Nursing Respite services are determined by the MCO Care Coordinator and documented on the CCP;
• Scheduling of hours for use of nursing respite services is the responsibility of the nursing respite
provider and the Care Coordinator; and
• Nursing respite services provided by a PDN provider requires a physician’s order that includes the
scope and duration of service(s). A new physician’s order will be obtained annually with the CCP
renewal or when there is a revision in the service. The order must be obtained by the agency
providing PDN and shared with the MCO Care Coordinator. The provider agency may require
advanced notice from the member/family for provision of services and will notify members of their
advanced notice requirement. The provider of nursing respite services must maintain a cumulative
record of utilization of respite care, to include time used.
Provider Requirements/Qualifications:
The provider agency of nursing respite services must meet all requirements, certifications, and training
standards set forth by the HSD/MAD to provide PDN services, as described in this section of the policy.
• Nursing respite services must be provided by an active, Medicaid approved provider type 363
Nursing Respite provider.
• Nursing respite providers must maintain (no gap in license) a full permanent license through
the New Mexico Board of Nursing. Provisional licenses will not be accepted.
o Nursing respite services may also be furnished through a licensed HH Agency, licensed
RHC or certified FQHC who meet all requirements/qualifications in this section of the
policy and are approved by the HSD/MAD/LTSSB as a provider type 363 nursing respite
provider.
• Nursing respite providers must comply with provisions of the Nurse Practice Act and the state
rules/regulations.
• In order to be approved and certified by the HSD/MAD/LTSSB, Nursing respite providers must
be holding and operating with a full permanent license (no gaps in license). All incomplete
applications submitted to the HSD/MAD/LTSSB shall be rejected and not considered for review
until a complete application is submitted.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
184 | P a g e
• Nursing respite providers must comply with all applicable State and Federal rules and
regulations under the nurse practice Act and program standards determined by HSD/MAD
including but not limited to CBCs, OSHA training requirements, incident management system
reporting, labor laws, etc.;
• Nursing respite providers must have a functioning office located in New Mexico where staff and
members can go to obtain information and/or assistance.
• The provider agency of nursing respite services must meet all requirements, certifications, and
training standards set forth by the HSD/MAD to provide PDN services, as described in this
section of the policy.
Staffing Requirements:
o An RN or LPN is considered a qualified respite nurse when the following criteria are met:
▪ Must be holding and maintaining a current (no gaps in licensure) permanent license as
required by the state of New Mexico;
▪ Nursing experience preferably with disabled and elderly individuals. This includes settings
such as HH, hospital, NF facility, or other types of clinics and institutions;
▪ RNs who supervise must have at least one year of supervisory experience. Supervision of
RNs and LPNs must be provided by a qualified RN on a quarterly basis and shall be in
accordance with the New Mexico Nursing Practice Act. The supervision of all personnel is
the responsibility of the agency’s Administrator and Director;
▪ Be culturally sensitive to the needs and preferences of members and their households
based upon language. Communicating in a language other than English may be required;
and
Hepatitis B vaccine will be offered by the provider agency upon employment at no cost to the employee
per the Federal OSHA requirements. Record of prior Hepatitis B immunization, acceptance or denial by
the employee will be maintained in the employee’s personnel record.
Supervision of nursing respite employees must be documented by the nursing respite supervisor. The
supervisor must be a staff member of the nursing respite provider agency and provide in-service training
to the personnel providing the care.
Nursing respite providers must maintain a current roster that is updated quarterly of nurse respite
providers to provide services as requested by the member or family.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
185 | P a g e
Nursing respite service providers must immediately notify the MCO Care Coordinator if there is a change
in the member’s condition, if the member refuses care or if the agency is unable to comply with the care
delivery as agreed upon in the CCP.
Reimbursement
Reimbursement is on an hourly basis and is accrued to the nearest quarter of an hour. Training on
member specific issues is reimbursable and included in the negotiated rate, general training
requirements are an administrative cost and not billable.
Reimbursement for nursing respite services will be based on the negotiated rate with the MCO.
Providers of service have the responsibility to review and ensure the information on the prior
authorization for their services is correct. If the provider identifies an error, they must contact the MCO
immediately to have the error corrected.
Limits or Exclusions
The member cannot schedule his or her own nursing respite with the nursing respite staff. The member
may receive a maximum of 300 total hours of nursing respite hours annually per CCP year provided
there is a primary caregiver. Additional hours may be requested if an eligible member’s health and
safety needs exceed the specified amount.
8.17. Respite Services
Respite services provide the member’s primary caregiver with a limited leave of absence to prevent
burnout, to reduce stress and provide temporary relief to meet a family crisis, emergency or caregiver’s
illness as determined in the CCP. A primary caregiver is the individual who has been identified in the CCP
and who assists the member on an intermittent basis (i.e., daily or as needed). Respite services provide a
temporary relief to the primary caregiver during times when he/she would normally provide unpaid
care. If a caregiver needs a break during the time when he/she provides paid care, the agency must
provide a substitute caregiver. Respite services may be provided in the member’s home, in the respite
provider’s home and/or in the community. Respite services are limited to a total maximum of 300 hours
per CCP year. Respite services does not cover or provide skilled care. If a member requires skilled care,
that care must be provided by a PDN or a nursing respite provider approved as a provider type 363,
nursing respite provider. Respite services must not be provided by a member of the member’s

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
186 | P a g e
household or by any relative approved as the paid caregiver. Respite services are provided pursuant to
the CCP, developed and authorized by the member and the MCO Care Coordinator. Additional hours
may be requested if an eligible member’s health and safety needs exceed the specified amount.
Scope of Services/Requirements:
Specific respite services may include the following:
• Household Activities – The following household activities are considered necessary to maintain a
clean and safe environment and to support the member living in their home. These activities are
limited to maintenance of the member’s individual living area (i.e., kitchen, living room, bedroom,
and bathroom). For example, the respite staff would not clean the entire home if the member only
occupies three rooms in a house of six rooms. In this case, the respite caregiver would clean the
three rooms only. The respite services will assist the member in performing these activities
independently or semi-independently when appropriate. These duties are performed as indicated in
the CCP:
o Sweeping, mopping or vacuuming of carpets, hardwood floors, or linoleum;
o Dusting of furniture;
o Changing of linens;
o Doing laundry (member’s clothing and linens only);
o Cleaning bathrooms (tub and/or shower area, sink, and toilet); and/or
o Cleaning of kitchen and dining area after preparation and serving meals by the respite staff for
member, such as washing dishes, putting dishes away; cleaning counter tops, dining table where
the member ate, and sweeping the floor, etc.
• Meal Preparation – A tentative schedule for preparation of meals will be identified in the CCP as
determined by the assessment. The respite staff will assist the member in independent or
semi-independent meal preparation, including dietary restrictions per physician order.
• Personal Care – The CCP may include the following tasks to be performed by the respite provider:
o Bathing – Giving a sponge bath/bed bath/tub bath/shower, including transfer in/out;
o Dressing – Putting on, fastening, removing clothing; including prosthesis;
o Grooming – Shampooing, combing or brushing hair, applying makeup, trimming beard or
mustache, braiding hair, shaving under arms or legs as requested by the member;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
187 | P a g e
o Oral care – Brushing teeth, cleaning dentures/partials (includes use of floss, swabs, or
mouthwash). Members whose swallowing reflex is not intact, are an exception and may require
specialized oral care beyond the scope of this service as identified by a physician’s order;
o Nail care – Cleaning or filing to trim and or do cuticle care. Members with diabetes are an
exception and may require specialized nail care beyond the scope of this service as identified by
a physician’s order;
o Perineal Care – Cleansing of the perineal area and changing of sanitary napkins;
o Toileting – Transferring on/off toilet, bedside commode and/or bedpan; cleaning perinea area,
changing adult briefs/pads, readjusting clothing;
o Bowel Care – Evacuation and ostomy care, including irrigations, changing and cleaning of bags,
and ostomy site skin care. Members requiring the assistance of bowel care must be determined
medically stable by his or her physician, and are able to communicate their bowel care verbally
or in writing. A physician must prescribe a bowel program for the member. An RN is required to
provide whatever additional training the respite staff needs to ensure the respite staff is
competent to implement the member’s bowel program. The respite staff must demonstrate
competency to the nurse that he or she is able to properly implement the bowel program
according to the physician’s order(s);
o Bladder Care – Elimination, catheter care, including the changing and cleaning of catheter bag.
Members requiring the assistance of a bladder care must be determined medically stable by his
or her physician, and are able to communicate their bladder care verbally or in writing. A
physician must prescribe a bladder program for the member. An RN is required to provide
whatever additional training the homemaker staff needs to ensure the respite staff is
competent to implement the member’s bladder program. The respite staff must demonstrate
competency to the nurse that he or she is able to properly implement the bladder program
according to the physician’s order(s);
o Mobility Assistance – Assistance in ambulation, transfer and toileting, defined as follows:
▪ Ambulation – Moving around inside and/or outside the home or member’s living
area with or without assistive device(s) such as walkers, canes and wheelchairs;
▪ Transferring – Moving to/from one location/position to another with or without
assistive device(s); and/or
▪ Toileting – Transferring on or off toilet.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
188 | P a g e
o Skin Care – Observation of skin condition for maintaining good skin integrity and prevention of
skin infection, irritation, ulceration or pressure sores;
o Assisting with Self-Administered Medication – Prompting and reminding only in accordance with
the New Mexico Nursing Practice Act. Getting a glass of water or juice as requested if member is
not able to do that for himself/herself, handing the member a daily medication box or
medication bottle. For the Nurse Practice Act, refer to the PDN services in this policy;
o Eating – Assistance with eating as determined in the Care Plan. Individuals requiring tube
feeding or J-tube feedings or who are at risk for aspiration are an exception and require
specialized care as prescribed by physician;
o Range of motion exercises as described in a Therapeutic Plan developed by therapists and
taught to the caregiver and caregiver supervisor by a physical therapist or occupational
therapist;
o Support Services – Support services provide additional assistance to members in order to
promote independence and enhance his or her ability to remain in a clean and safe
environment. The following support services will be identified in the assessment of the IADLs
and are provided as determined in the Care Plan;
o Shopping and/or completing errands for the member, with or without the member;
o Accompanying or assisting with non-medical transportation.;
o Respite services are available to any member of any age; and
o Respite services are determined by the MCO Care Coordinator and documented on the CCP.
Provider Requirements/Qualifications:
• Respite services must be provided by an active, Medicaid approved provider type 363 Respite
provider.
• In order to be approved and certified by the HSD/MAD/LTSSB, respite providers must be able to
demonstrate all requirements in this section are met. All incomplete applications submitted to the
HSD/MAD/LTSSB shall be rejected and not considered for review until a complete application is
submitted;
• The respite staff must possess a current New Mexico driver’s license and a motor vehicle insurance
policy if the member is to be transported by the respite staff. Release of liability forms must be
completed and on file in the member and/or employee’s file. Respite provider agencies are not

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
189 | P a g e
required to provide transportation services. The MCO Care Coordinator assesses the member’s
formal and informal support system and determine if other individuals and/or other Medicaid
agencies can provide assistance with shopping and transportation services.
o Respite agencies may be licensed by the DOH as an HH agency pursuant to 7.28.2.1 NMAC et
seq. and must meet all requirements in this section of the policy to be approved as a Medicaid
provider type 363 respite provider;
o Respite agencies must comply with DOH abuse registry screening laws regulations in accordance
with the DOH Act, NMSA 1978, section 90706(E) and the Employee Abuse Registry Act, NMSA
1978, Sections 24-27-1 to 24-27-8;
o Respite agencies must provide incident management and review on an annual basis. Maintain
documentation in the employee’s personnel file as required by HSD/MAD;
▪ Respite agencies must ensure written notification to the MCO Care Coordinator and provide
the MCO with a copy of the incident report.
o Respite agencies must comply with all requirements set forth in the Medicaid PPA;
o Respite agencies must have available and maintain a roster of trained and qualified respite
employee(s) for back-up or regular scheduling and emergencies. For members whose health and
welfare will be at risk due to absence, there should be a backup plan that ensures the member’s
health and safety;
o Respite agencies must have available in the member’s home a current copy of the CCP and any
additional materials/instructions related to the member’s care; and
o Training of the bowel and bladder care must be taught by an RN with a current license to
practice in the State of New Mexico. Upon completion the respite staff must demonstrate
competencies to perform individualized bowel and bladder programs. No respite staff will
provide bowel and bladder services prior to completion of the initial training;
o Respite supervisors must provide specific instructions to assigned respite staff on each member
prior to providing services to the member. It is the responsibility of the respite agency to ensure
that respite caregivers are appropriately trained.
Reimbursement
Respite provider agencies must maintain appropriate record keeping of services provided to personnel
and training documentation, and fiscal accountability as indicated in the Medicaid PPA. Billing is on an

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
190 | P a g e
hourly basis and is accrued and rounded to the nearest quarter of an hour. Reimbursement for respite
services will be based on the negotiated rate with the MCO. Providers of respite services have the
responsibility to review and ensure the information on the prior authorization for their services is
correct. If the provider identifies an error, they will contact the MCO immediately to have the error
corrected.
ABCB respite provider agencies will use the state mandated EVV system as required by the 21st Century
Cures Act.
Limits or Exclusions
Respite services may not be provided to the member by his or her spouse. Respite services cannot be
included in the CCP in combination with Assisted Living. Respite services are limited to a total maximum
of 300 hours per CCP year. Additional hours may be requested if an eligible member’s health and safety
needs exceed the specified amount. Respite providers do not provide skilled services.
Scheduling of hours for use of respite services will be the responsibility of the member or their
representative. The provider agency may require advanced notice from the member/family for provision
of services and will notify members of their advanced notice requirement. The provider of respite
services must maintain a cumulative record of utilization of respite care, to include time used.
The member may receive a maximum of 300 hours annually unless additional hours are approved by the
MCO.
Under no circumstances may a respite staff act on behalf of a member as their representative in matters
regarding medical treatment, financial, legal or budgetary decision-making, and/or manage a member’s
finances. An immediate referral must be made to the MCO in order to determine if the member should
be referred to an appropriate social service or legal services agency(s) for assistance in these areas.
8.18. Skilled Maintenance Therapies
Skilled maintenance therapies include Occupational Therapy (OT), Physical Therapy (PT) and speech and
language therapy (SLT) for individuals 21 years and older. These services are an extension of therapy
services provided for acute and temporary conditions that are provided with the expectation that the
individual will improve significantly in a reasonable and generally predictable period of time. Skilled
maintenance therapy services are provided to adults with a focus on maintenance, community
integration, socialization and exercise, or enhance support and normalization of family relationships.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
191 | P a g e
Limits or Exclusions
A signed therapy referral for treatment must be obtained from the member’s primary care physician.
The referral will include frequency, estimated duration of therapy, and treatment/procedures to be
rendered.
8.19. Occupational Therapy (OT) for Adults
OT is a skilled therapy service for individuals 21 years and older provided by a licensed occupational
therapist. OT services promote/maintain fine motor skills, coordination, sensory integration, and/or
facilitate the use of adaptive equipment or other assistive technology. A signed OT referral for
treatment must be obtained from the member’s PCP in accordance with State laws and applicable
regulations. A copy of the written referral will be maintained in the member’s file by the occupational
therapist and shared with the MCO. The OT provider must develop a PCCP with the member and share
with the MCO Care Coordinator, which will be incorporated into the CCP. Children (under the age of 21)
receive this service through EPSDT.
OT services should not be requested or authorized until all other third party and community resources
have been explored and/or exhausted. If services are available for reimbursement through third party
liability or other payment sources, these sources must be accessed before ABCB services are delivered.
Scope of Services/Requirements:
• Teaching daily living skills;
• Developing perceptional motor skills and sensory integrative functioning;
• Designing, fabricating or modifying of assistive technology or adaptive devices;
• Providing assistive technology services;
• Designing, fabricating or applying of selected orthotic or prosthetic devices or selecting adaptive
equipment;
• Using specifically designed crafts and exercise to enhance functional performance;
• Training regarding OT activities;
• Consulting or collaborating with other service providers or family members, as directed by the
member;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
192 | P a g e
• Training of all relevant staff, family, primary caregiver, etc., in the implementation of the therapy
plan and follow up; and
• The occupational therapist must perform a comprehensive assessment evaluation for each member
to determine appropriate therapy, develop a PCCP and coordinate services with the MCO Care
Coordinator. Services may include the following:
o Obtaining pertinent medical history;
o Assessing the member for specific needs in gross/fine motor skills pertinent to OT;
o Adapting the member’s environment in order to meet his/her needs;
o Evaluating, administrating and interpreting tests;
o Assessing, interpretation and summary of objective evaluation findings, identification of
functional problems, and determining treatment goals that is objective and measurable with a
statement on potential to achieve goals;
o Administering a technically complete and correct program, using skilled techniques, that
provides for flexibility to member response;
o Establishing individualized service goals and formulate a treatment plan/PCCP on the basis of
the member’s evaluation;
▪ Analyze and interpret member’s needs on the basis of medical history, pertinent
precautions, limitations, and evaluative findings. Identify short- and long-term goals that are
measurable, objective, and related to functional mobility as determined by medical history
and evaluative findings;
▪ Formulate a treatment plan/PCCP to achieve the goals identified. The treatment plan should
include frequency, estimated duration of therapy, treatment/procedures to be rendered,
member’s response to treatment, and progress toward therapy goals with dates and time of
service;
▪ Review physician’s request for treatment, and if appropriate, recommend revisions on the
basis of evaluative findings;
▪ Implement and administer appropriate treatment;
o Providing the member or caregiver education and documenting in the member’s medical
record;
Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
193 | P a g e
o Preparing discharge summary and include the number and types of treatment provided. The
member disposition at discharge including functional, sensory/perceptual, and physical and
status of all levels and follow-up recommendations as indicated;
• The staff: client rate is 1:1 for the period of time in which a specific member is receiving therapy
services; and/or
• Occupational Therapy services may be provided at:
o A community-based center, i.e. therapy center;
o The member’s home; and/or
o Any other location in which the member engages in day-to-day activities.
Provider Requirements/Qualifications:
o Occupational therapy services must be provided by an active, Medicaid approved provider type
363 Occupational therapy provider.
o Occupational therapists must comply with provisions of the Occupational Therapy Act and all
other city, state and federal rules and regulations.
o Occupational therapists must maintain (no gaps in licensure) a full permanent Occupational
therapist license from the New Mexico Regulation & Licensing Department. Provisional licenses
will not be accepted.
o In order to be approved and certified by the HSD/MAD/LTSSB, Occupational Therapists must
operate with a fully approved permanent license. All incomplete applications submitted to
HSD/MAD/LTSSB shall be rejected and not considered for review until a complete application is
submitted.
o OT experience preferably in in-home care and general acute care;
o Must have access to all required diagnostic and therapeutic materials to provide services;
o Must be proficient in the member’s primary language or have access to an interpreter (family
member, friend, or caregiver). Professional interpretation service fees are the responsibility of
the agency;
o Must be culturally sensitive to the needs and preferences of members and their households
based upon language. Communicating in a language other than English may be required;
o Certified Occupational Therapy Assistants (COTA) may perform OT procedures and related tasks
pursuant to a PCCP written by the supervising licensed occupational therapist. A COTA must be

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
194 | P a g e
supervised by a licensed occupational therapist. All related tasks and procedures performed by a
COTA must be within a COTA scope of service following all Federal and state requirements
applicable to COTA services;
o Provider agencies must adhere to the HSD/MAD requirements including but not limited to:
OSHA training requirements, incident management reporting, CBC, labor laws, etc.;
o Provider agencies will establish and maintain financial reporting and accounting for each
member;
o All services must be under the order of the member’s PCP. The order will be obtained by the
skilled therapist, and shared with the MCO Care Coordinator;
o Therapy reports must be current and available upon request of HSD/MAD; and
o OT providers must ensure all insurance records are maintained correctly in the member’s clinical
file.
Reimbursement
Providers are responsible for providing clinical documentation that identifies their role in all
components of the provision of OT, including assessment information, care planning, intervention,
communications, care coordination, and evaluation. There must be justification in each member’s
clinical record supporting medical necessity for the care and for the level or intensity (frequency and
duration) of the care. All services must be reflected on a Care Plan that is coordinated with the
member/member’s representative, other caregivers as applicable, and authorized by the MCO. All
services provided, claimed, and billed must have documented justification supporting medical necessity.
Reimbursement is on a per hour basis and rounded to the nearest quarter hour.
• Payment for OT services is based on the negotiated rate through the MCO and is considered
payment in full. Providers of service have the responsibility to review and ensure the information on
the prior authorization for their services is correct. If the provider identifies an error, they must
contact the MCO immediately to have the error corrected.
• OT providers must abide by all Federal, State, HSD policies and procedures regarding billable and
non-billable items.
• Billable hours are as follows:
o Face-to-face activities described in the Scope of Service;
o Maximum of eight hours for an initial comprehensive individual assessment;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
195 | P a g e
o Maximum of eight hours to develop an initial comprehensive therapy plan;
▪ Attendance and/or telephone conference call to participate in IDT meetings;
▪ Annual maximum of six hours to complete progress reports and/or to revise annual plan;
▪ Annual maximum of eight hours to arrange assistive technology development;
▪ Training on member specific issues is reimbursable, general training requirements are an
administrative cost and not billable.
Limits or Exclusions
• HSD does not consider the following to be professional OT services and will not authorize payment
for the following non-billable activities:
o Performing specific errands for the member and/or family that are not program specific;
o Friendly visiting;
o Financial brokerage services, handling of member finances, or, preparation of legal documents;
o Time spent on paperwork or travel that is administrative for the provider;
o Transportation of members;
o Pick up and/or delivery of commodities; and
o Other non-Medicaid reimbursable activities.
8.20. Physical Therapy (PT) for Adults
PT is a skilled therapy service for members 21 years and older provided by licensed Physical therapist. PT
services promote/maintain gross/fine motor skills, facilitate independent functioning and/or prevent
progressive disabilities. A signed PT referral for treatment must be obtained from the member’s PCP in
accordance with State laws and applicable regulations. A copy of the written referral will be maintained
in the member’s file by the physical therapist and shared with the MCO Care Coordinator. Children
(under the age of 21) receive this service through EPSDT.
PT services should not be requested or authorized until all other third party and community resources
have been explored and/or exhausted. If services are available for reimbursement through third party
liability or other payment sources, these sources must be accessed before ABCB services are delivered.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
196 | P a g e
Scope of Services/Requirements:
• Providing professional assessment(s) of the individual for specific needs in gross/fine motor skills;
• Developing, implementing, modifying and monitoring PT treatments and interventions for the
member;
• Designing, modifying or monitoring use of related environmental modifications;
• Designing, modifying and monitoring use of related activities supportive to the Care Plan goals and
objectives;
• Consulting or collaborating with other service providers or family members, as directed by the
member or Care Coordinator;
• Using of equipment and technologies or any other aspect of the member’s PT services;
• Training regarding PT activities;
• Training of all relevant staff, family, primary caregiver, etc., in the implementation of the therapy
plan and follow up.
• The physical therapist must perform a comprehensive assessment evaluation and develop a PCCP
for each member to determine appropriate therapy and coordinate services with the MCO Care
Coordinator. Services may include the following:
o Obtaining pertinent medical history;
o Assessing of the member on physical strengths and deficits including, but limited to:
▪ Range of motion for all joints;
▪ Muscle strength, gait pattern, sensation, balance, coordination, and perception;
▪ Skin integrity and respiratory status;
o Functional level of motor developmental level;
o Adapting the member’s environment in order to meet his/her needs;
o Evaluating, including the administration and interpreting tests and measurements within the
scope of the therapist;
o Assessing interpretation and summary of objective evaluation findings, identification of
functional problems, and determining treatment goals that are objective and measurable with a
statement on potential to achieve goals;
o Administering a technically complete and correct program, using skilled techniques, that
provides for flexibility to member response;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
197 | P a g e
o Establishing individualized service goals and formulate a treatment plan on the basis of the
member evaluation;
o Analyze and interpret member’s needs on the basis of medical history, pertinent precautions,
limitations, and evaluative findings;
o Identify short- and long-term goals that are measurable, objective, and related to functional
mobility as determined by medical history and evaluative findings. Formulate a treatment
plan/PCCP to achieve the goals identified. The Treatment Plan should include frequency,
estimated duration of therapy, treatment/procedures to be rendered, member’s response to
treatment, and progress toward therapy goals with dates and time of service;
o Review physician’s request for treatment, and if appropriate, recommend revisions on the basis
of evaluative findings;
o Implement and administer appropriate treatment;
o Providing the member or caregiver education and documenting in the member’s medical
record; and
o Preparing discharge summary and include the number and types of treatment provided. The
member disposition at discharge including functional mobility level and follow-up
recommendations as indicated.
• The staff to client ratio is 1:1 for the period of time in which a specific member is receiving therapy
services; and/or
o Therapy services may be provided at:
▪ A community-based center (i.e., therapy center);
▪ The member’s home; and/or
▪ Any other location in which the member engages in day-to-day activities.
Provider Requirements/Qualifications:
o Physical therapy services must be provided by an active, Medicaid approved provider type 363
Physical therapist provider.
o Physical therapists must comply with all provisions and city, state and federal rules regarding
physical therapy.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
198 | P a g e
o Physical therapists must maintain (no gaps in licensure) a full permanent physical therapist
license from the New Mexico Regulation & Licensing Department. Provisional licenses will not
be accepted.
o In order to be approved and certified by the HSD/MAD/LTSSB, Physical Therapists must be
holding and operating with a fully approved permanent license. All incomplete applications
submitted to HSD/MAD/LTSSB shall be rejected and not considered for review until a complete
application is submitted.
• Staffing Requirements:
▪ PT experience preferably in in-home care and general acute care;
▪ Must have access to all required diagnostic and therapeutic materials to provide services;
▪ Must be proficient in the member’s primary language or have access to an interpreter
(family member, friend, or caregiver). Professional interpretation service fees are the
responsibility of the agency;
▪ Must be culturally sensitive to the needs and preferences of members and their households
based upon language. Communicating in a language other than English may be required;
and
▪ Certified Physical Therapy Assistants (PTA) may perform PT procedures and related tasks
pursuant to a PCCP written by the supervising licensed physical therapist. A PTA must be
supervised by a licensed physical therapist. All related tasks and procedures performed by a
PTA must be within a PTA scope of service following all Federal and state requirements
applicable to PTA services.
• Administrative Requirements:
o Provider agencies must adhere to HSD/MAD requirements including but not limited to: OSHA
training requirements, incident management reporting, CBC, labor laws, etc.;
o All services must be under the order of member’s PCP. The order will be obtained by the skilled
therapist, and shared with the MCO Care Coordinator; and
o Therapy reports must be current and available upon request of HSD/MAD.
Reimbursement
Reimbursement for PT services will be based on the negotiated rate with the MCO. Providers of service
have the responsibility to review and ensure that the information on the prior authorization for their
Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
199 | P a g e
services is correct. If the provider identifies an error, they must contact the MCO immediately to have
the error corrected.
PT services are provided with the understanding the MCO is the payer of last resort. PT services should
not be requested or authorized until all other third party and community resources have been explored
and/or exhausted. If services are available for reimbursement through third party liability or other
payment sources, these sources must be accessed before ABCB services are delivered.
Each provider of PT services is responsible to provide clinical documentation that identifies his or her
role in all components of the provision of PT, including assessment information, care planning,
intervention, communications, care coordination, and evaluation. There must be justification in each
member’s clinical record supporting medical necessity for the care and for the level or intensity
(frequency and duration) of the care. All services must be reflected on a Care Plan that is coordinated
with the member/member representative, other caregivers as applicable, and authorized by the MCO.
All services provided, claimed, and billed must have documented justification supporting medical
necessity.
• PT services must abide by all Federal, State, HSD policies and procedures regarding billable and
non-billable items; and
• PT providers must ensure all insurance records are maintained correctly.
Billable hours are as follows:
o Face-to-face activities described in the Scope of Service;
o Maximum of eight hours for an initial comprehensive individual assessment;
o Maximum of eight hours to develop an initial comprehensive therapy plan;
▪ Attendance and/or telephone conference call to participate in IDT meetings;
▪ Annual maximum of six hours to complete progress reports and/or to revise annual plan;
▪ Annual maximum of eight hours to arrange assistive technology development;
• Reimbursement is on a unit rate per hour and rounded to the nearest quarter hour;
• Training on member specific issues is reimbursable, general training requirements are
an administrative cost and not billable;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
200 | P a g e
Limits or Exclusions
• HSD does not consider the following to be professional PT services and will not authorize payment
for the following non-billable activities:
o Performing specific errands for the individual and/or family that are not program specific;
o Friendly visiting;
o Financial brokerage services, handling of member finances, or, preparation of legal documents;
o Time spent on paperwork or travel that is administrative for the provider;
o Transportation of members;
o Pick up and/or delivery of commodities; and
o Other non-Medicaid reimbursable activities.
8.21. Speech Language Therapy (SLT) for Adults
SLT is a skilled therapy service for individuals 21 years and older provided by a licensed speech and
language pathologist. SLT services preserve abilities for independent function in communication; to
facilitate oral motor and swallowing function, to facilitate use of assistive technology, and to prevent
progressive disabilities. A signed speech therapy referral for treatment must be obtained from the
member’s PCP in accordance with State laws and applicable regulations. A copy of the written referral
will be maintained in the member’s file by the speech language therapist and shared with the MCO Care
Coordinator. Children (under age 21) receive this service through EPSDT.
SLT services should not be requested or authorized until all other third party and community resources
have been explored and/or exhausted. If services are available for reimbursement through third party
liability or other payment sources, these sources must be accessed before ABCB services are delivered.
Scope of Services/Requirements:
Specific services may include the following:
• Identification of communicative or oropharyngeal disorders and delays in the development of
communication skills;
• Prevention of communicative or oropharyngeal disorders and delays in the development of
communication skills;
• Use of specifically designed equipment, tools, and exercises to enhance functional performance;
• Design, fabrication or modification of assistive technology or adaptive devices;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
201 | P a g e
• Provision of assistive technology services;
• Evaluation, including administering and interpreting tests;
• Adapting the member’s environment in order to meet his/her needs;
• Implementation of the maintenance therapy plan;
• Training of all relevant staff, family, primary caregiver, etc., in the implementation of the therapy
plan and follow up;
• Consulting or collaborating with other service providers or family members; and
• Development of eating or swallowing plans and monitoring their effectiveness.
• The speech language therapist must perform a comprehensive assessment evaluation for each
member to determine appropriate therapy and coordinate services with the MCO Care Coordinator.
Services may include the following:
o Obtaining pertinent medical history;
o Assessing for speech language disorders;
o Assessing for swallowing disorders (dysphasia);
o Assessing of communicative functions including underlying processes (i.e., cognitive skills,
memory, attention, perception, and auditory processing, includes ability to convey or receive a
message effectively and independently, regardless of the mode);
o Assessing of oral motor function;
o Assessing for the use of prosthetic/adaptive devices;
o Assessing of resonance and nasal airflow;
o Assessing of orofacial myofunctional patterns;
o Assessing interpretation and summary of objective evaluation findings, identification of
functional problems, and determining treatment goals that are objective and measurable with a
statement on potential to achieve goals;
o Administering a technically complete and correct program, using skilled techniques, that
provides for flexibility to member response;
o Establishing individualized service goals and formulate a treatment plan on the basis of the
member evaluation;
o Analyze and interpret member’s needs on the basis of medical history, pertinent precautions,
limitations, and evaluative findings;

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
202 | P a g e
o Identify short- and long-term goals that are measurable, objective, and related to
augmentative/alternative communication and/or device treatment/orientation, orofacial
myofunctional treatment, prosthetic/device treatment/orientation, swallowing function
treatment, voice treatment, central auditory processing treatment, etc.;
o Formulate a treatment plan to achieve the goals identified. The treatment plan should include
frequency, estimated duration of therapy, treatment/procedures to be rendered, member’s
response to treatment, and progress toward therapy goals with dates and time of service;
o Review physician’s request for treatment, and if appropriate, recommend revisions on the basis
of evaluative findings;
o Implement and administer appropriate treatment;
o Providing the member or caregiver education and documenting in the member’s medical
record;
o Preparing discharge summary and include the number and types of treatment provided. The
member disposition at discharge including functional, sensory/perceptual, and physical and
status of all levels and follow-up recommendations as indicated;
o The staff to client rate is 1:1 for the period of time in which a specific member is receiving
therapy services; and
o Therapy services may be provided at:
▪ A community-based center (i.e., therapy center);
▪ The member’s home; and/or
▪ Any other location in which the member engages in day-to-day activities.
Provider Requirements/Qualifications:
SLT services must be provided by an active, Medicaid approved provider type 363 SLT provider.
SLT providers must maintain (no gaps in licensure) a full permanent license by the New Mexico
Regulation & Licensing Department. Provisional licenses will not be accepted.
In order to be approved and certified by the HSD/MAD/LTSSB, SLT providers must be operating with a
fully approved permanent license. All incomplete applications submitted to HSD/MAD/LTSSB shall be
rejected and not considered for review until a complete application is submitted.
• Staffing Requirements:

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
203 | P a g e
o Graduation from an accredited masters or doctoral degree level, and holding the Certificate of
Clinical Competence from the American Speech Language Hearing Association;
o Must have a current licensure by State of New Mexico;
o SLT experience preferably in in-home care and general acute care;
o Must have access to all required diagnostic and therapeutic materials to provide services;
o Must be proficient in the member’s primary language or have access to an interpreter (family
member, friend, or caregiver). Professional interpretation service fees are the responsibility of
the agency; and
o Must be culturally sensitive to the needs and preferences of members and their households
based upon language. Communicating in a language other than English may be required.
• Administrative Requirements:
o Provider agencies must adhere to the HSD/MAD requirements including but not limited to:
OSHA training requirements, incident management reporting, CBC, labor laws, etc.;
o Provider agencies will establish and maintain financial reporting and accounting for each
member;
o All services must be under the order of the member’s PCP. The order will be obtained by the
skilled therapist, and shared with the MCO Care Coordinator; and
o Therapy reports must be current and available upon request of HSD/MAD.
Reimbursement
• SLT providers are responsible for providing clinical documentation that identifies his or her role in all
components of the provision of home care, including assessment information, care planning,
intervention, communications, care coordination, and evaluation. There must be justification in each
member’s clinical record supporting medical necessity for the care and for the level or intensity
(frequency and duration) of the care. All services must be reflected on a Care Plan that is
coordinated with the member/member representative, other caregivers as applicable, and
authorized by the MCO. All services provided, claimed, and billed must have documented
justification supporting medical necessity. Reimbursement is on a per hour basis and rounded to the
nearest quarter hour.
• Payment for SLT services is based on the negotiated rate through the MCO and is considered
payment in full. Providers of service have the responsibility to review and ensure the information

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
204 | P a g e
on the prior authorization for their services is correct. If the provider identifies an error, they must
contact the MCO immediately to have the error corrected.
• SLT services must abide by all Federal, State, HSD policies and procedures regarding billable and
non-billable items.
• Billable hours are as follows:
o Face-to-face activities described in the Scope of Service;
o Maximum of eight hours for an initial comprehensive individual assessment;
o Maximum of eight hours to develop an initial comprehensive therapy plan;
o Attendance and/or telephone conference call to participate in IDT meetings;
o Annual maximum of six hours to complete progress reports and/or to revise annual plan;
o Annual maximum of eight hours to arrange assistive technology development;
o Reimbursement is on a unit rate per hour and rounded to the nearest quarter hour; and
o Training on member specific issues is reimbursable, general training requirements are an
administrative cost and not billable.
Limits or Exclusions
• HSD/MAD does not consider the following to be professional SLT services and will not authorize
payment for the following non-billable activities:
o Performing specific errands for the individual and/or family that are not program specific;
o Friendly visiting;
o Financial brokerage services, handling of member finances, or, preparation of legal documents;
o Time spent on paperwork or travel that is administrative for the provider;
o Transportation of members;
o Pick up and/or delivery of commodities; and
o Other non-Medicaid reimbursable activities.
• SLT providers must ensure all insurance records are maintained correctly.

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
205 | P a g e
Services, Service Codes and Applicable Units of Service
SERVICE TYPE
CODE
UNIT INCREMENTS
1 UNIT =
Adult Day Health
S5100
15 minutes
Assisted Living
T2031
Day
Community Transition Services
T2038
Per service
Emergency Response
S5161
Month
Emergency Response High Need
S5161 U1
Month
Environmental Modifications
S5165
1 unit per project
Behavior Support Consultation
H2019
15 minutes
Behavior Support Consultation, Clinic Based
H2019TT
15 minutes
Employment Supports
H2024
Day
Home Health Aide
S9122
Hour
Nutritional Counseling
S9470
Hour
Personal Care-Consumer Directed
99509
Hour
Personal Care-Consumer Delegated
T1019
15 minutes
Personal Care-Directed training
S5110
15 minutes
Personal Care-Directed-Administrative Fee
G9006
1 unit + 1 month
Personal Care-Directed Advertisement Reimbursement Fee
G9012
1 Advertisement
Private Duty Nursing for Adults – RN
T1002
15 minutes
Private Duty Nursing for Adults – LPN
T1003
15 minutes
Respite RN
T1002 U1
15 minutes
Private Duty Nursing for Adults – LPN
T1003 U1
15 minutes
Respite
99509 U1
Hour
Physical Therapy for Adults
G0151
15 minutes
Occupational Therapy for Adults
G0152
15 minutes
Speech Language Therapy for Adults
G0153
15 minutes

Section 8: Agency-Based Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
206 | P a g e
Personal Care Services (PCS) Consumer Directed Model Code Definitions
Personal Care
Consumer-Directed
99509
Hour
The rate for ongoing attendant services. The rate includes
both the employee’s and the employer’s share of Social
Security withholding and the cost for worker’s
compensation insurance. The maximum number of hours
billable is determined by the authorization issued by the
MCO which must be approved by the MCO Medicaid
Utilization Review Department.
Personal Care
Consumer-Directed
Training
S5110
15 minutes
The rate for training provided to the consumer or their
attendant at the request of the consumer. There is an
annual maximum of eight (8) hours of training allowed per
consumer.
Personal Care
Consumer-Directed
Advertisement
Reimbursement Fee
G9012
1 unit = 1
advertisement
The maximum allowable rate for advertising. Consumers
are reimbursed for up to two (2) advertisements per year if
seeking a new Personal Care Attendant. If the billed
amount exceeds the maximum allowable rate, the billed
amount will be reduced to the maximum allowable
rate. The advertising reimbursement is allowed only for
actual and necessary advertising. Documentation is
required in the case file.
Personal Care
Consumer-Directed
Administrative Fee
G9006
1 unit = 1 month
The rate for fiscal intermediary tasks such as processing
payroll for the consumer’s Personal Care Attendants,
producing reports required by the Medical Assistance
Division, processing claims for Consumer-Directed Personal
Care services (including Income Tax and Social Security
withholding) and submitting billings to the MCO.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
207 | P a g e
9. Self-Directed Community Benefits (SDCB)
9.1. Purpose
The SDCB is intended to provide a community-based alternative to institutional care that facilitates
greater member choice, direction and control over covered services and supports. For this section of the
Manual, the terms “member”, “care plan”, “services” and “providers” refer to SDCB.
HCBS shall meet the following standards:
• Are integrated and support full access of individuals receiving Medicaid HCBS to the greater
community, including opportunities to seek employment, and work in competitive integrated
settings, engage in community life, control personal resources, and receive services in the
community, to the same degree of access as individuals not receiving Medicaid HCBS;
• Are selected by the individual from among setting options including non-disability specific settings.
The setting options are identified and documented in the person-centered service plan and are
based on the individual’s needs and preferences;
• Ensure an individual’s rights of privacy, dignity and respect, and freedom from coercion and
restraint;
• Optimize, but do not regiment, individual initiative, autonomy, and independence in making life
choices, including but not limited to, daily activities, physical environment, and with whom to
interact; and
• Facilitate individual choice regarding services and supports, and who provides them.
CMS will take the following factors into account when determining whether a setting may have the
effect of isolating individuals receiving Medicaid HCBS form the broader community of individuals not
receiving HCBS:
• Due to the design or model of service provision in the setting, individuals have limited, if
any, opportunities for interaction in and with the broader community, including with
individuals not receiving Medicaid funded HCBS. Opportunities as well as identified
supports to provide access to and participation in the broader community, should be
reflected in both the individuals’ person-centered service plans and policies and
practices of the setting in accordance with 42 CFR 441.301(c)(1)(3) and (4)(vi)(F), 42 CFR
441.530(a)(1)(vi)(F) and 441.540, and 42 CFR 441.710(a)(1)(vi)(F) and 441.725;
Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
208 | P a g e
• The setting restricts beneficiary choice to receive services or to engage in activities
outside of the setting; or
• The setting is physically located separate and apart from the broader community and
does not facilitate beneficiary opportunity to access the broader community and
participate in community services, consistent with the beneficiary’s person-centered
service plan.
9.2. Guiding Principles
All members:
• Have value and potential;
• Will be viewed in terms of their abilities;
• Have the right to participate and be fully included in their communities; and
• Have the right to live, work, learn, and receive services and supports to meet their individual needs,
in the most integrated settings possible within their community.
9.3. Philosophy of Self Direction
Self-direction is a tool that leads to self-determination, through which members can have greater
control over their lives and have more freedom to lead a meaningful life in the community. Within the
context of SDCB, self-direction means members choose which covered services they need, as identified
in the most recent CNA. Members also decide when, where and how those SDCB covered services will
be provided and who they want to provide them. Members decide who they want to assist them with
planning and managing their SDCB covered services within a managed care environment. Self-direction
means members have more choice, control, flexibility, freedom and responsibility in directing their CBs.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
209 | P a g e
9.4. Definitions
1. Authorized Representative (AR): The AR is an individual designated to represent and act on the
member’s behalf. The member or AR must provide formal documentation authorizing the named
individual or individuals to access the identified case information for a specified purpose and time
frame. An AR may be an attorney representing a person or household, a person acting under the
authority of a valid power of attorney, a guardian, or any other individual or individuals designated
in writing by the eligible recipient or member.
2. Centers for Medicare and Medicaid Services (CMS): Federal agency within the United States
Department of Health and Human Services that works in partnership with the states to administer
Medicaid. CMS must approve all Medicaid programs.
3. Electronic Visit Verification (EVV): EVV is a computer-based system that electronically verifies the
occurrence of authorized personal care service visits by electronically documenting the precise time
and location where a service delivery visit begins and ends. For SDCB, EVV will be implemented
according to federal requirements and timelines.
4. Employer of Record (EOR): Individual responsible for directing the work of SDCB employees by
recruiting, hiring, training, supervising and terminating employees, and ensuring payment to
employees and vendors.
5. Financial Management Agency (FMA): Contracted with each Centennial Care MCO and helps the
member implement the approved SDCB Care Plan by receiving and processing payment requests for
the member’s employees and vendors, tracking the SDCB expenditures and credentialing the SDCB
employees and vendors.
6. FOCoSonline: The web-based system used by the SDCB FMA for receiving and processing SDCB
payment requests. The FOCoSonline system is also used by members, Care Coordinators, and
Support Brokers to develop and submit SDCB care plan/budget requests for MCO/UR review, and to
monitor utilization and spending throughout the SDCB care plan year.
7. Human Services Department (HSD): Designated by CMS as the Medicaid administering agency in
New Mexico. HSD is also responsible for operating the SDCB HCBS for populations that meet the NF
LOC (disabled & elderly, brain injury, and AIDS).
8. Legally Responsible Individual (LRI): A person who has a duty under State law to care for another
person. This category typically includes: the parent (biological or adoptive) of a minor child; the

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
210 | P a g e
guardian of a minor child who must provide care to the child; or the spouse of a member. Payment
may not be made to a LRI for the provision of personal care or similar services that the LRI would
ordinarily perform or be responsible to perform on behalf of a member. Exceptions to this
prohibition may be made under extraordinary circumstances specified by the State, utilizing
documentation specified by the State and only after approval by the appropriate MCO.
9. MCO/UR: Provides services related to medical eligibility determination and re-determination, and
NF LOC for members. The MCO also performs UM duties, review and approval or denial of each
individual services or related goods requested in the SDCB care plan/budget.
10. Quality Assurance and Quality Improvement (QA/QI): Processes utilized by state and Federal
governments, programs and providers whereby appropriate oversight and monitoring of CB
assurances and other measures provide information about the health and welfare of members and
the delivery of appropriate services. This information is then collected, analyzed and used to
improve services and outcomes and to meet requirements by state and Federal agencies. Quality
plans, systems and processes are designed and implemented to maintain continuous QI.
11. Reconsideration: Members who disagree with an adverse decision made by the MCO/UR may
submit a written request through a Care Coordinator/Support Broker to the MCO/UR for a
reconsideration of the adverse decision. These requests must include new, additional information
that is different from, or expands on, the information submitted with the initial request.
12. SDCB: Is a component of the State’s 1115 Medicaid Managed Care waiver which allows eligible
members meeting NF LOC the option to access SDCB Medicaid funds, using the essential elements
of person-centered planning, individualized budgeting, member protections, and QA/QI. Members
have choices (among the state-determined SDCB services and related goods) in identifying,
accessing and managing the services and related goods needed to meet their personal goals.
13. SDCB Budget: The maximum budget allotment available to an eligible member, determined by
his/her established NF LOC, CNA, and the amount and type of services the member was receiving in
the ABCB. Based on this maximum amount, the eligible member will develop a SDCB care plan to
meet his/her assessed functional, medical and habilitative needs to enable that member to remain
in the community.
14. SDCB Care Plan: A plan that includes approved SDCB services of the SDCB member’s choice; the
projected cost, frequency and duration of services and related goods; the type of provider who will
furnish each service or related good; other services and related goods to be used by the member.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
211 | P a g e
Each SDCB care plan shall include a backup plan which lists who the member will contact if regularly
scheduled employees or service providers are unable to report to work. The SDCB care plan is
mandatory for all SDCB members and must be processed through the FOCoSonline or other state
approved system.
15. SDCB Member: An individual who meets the medical and financial eligibility and is approved to
receive services through the SDCB after receiving services in the ABCB for a minimum of 120
calendar days.
16. Support Broker (SB): An individual who provides support to members and assists the member (or
the member’s family or representative, as appropriate) in arranging for, directing and managing
services and supports as well as developing, implementing and monitoring the SDCB care plan and
budget. Individual Support Brokers work for MCO contracted Support Broker agencies or may be
directly employed by an MCO.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
212 | P a g e
9.5. SDCB Member Rights
SDCB member has the right to:
• Decide where and with whom to live;
• Choose his/her own work or productive activity;
• Choose how to establish community and personal relationships;
• Make decisions regarding his/her own support, based upon informed choice;
• Be respected and supported during the decision-making process and in the decisions made;
• Recruit, hire, train, schedule, supervise and terminate SDCB service providers, as necessary;
• Receive training, resources and information related to SDCB in a format that meets the ADA
requirements;
• Have the right to appeal denial decisions through the MCO appeals and State fair hearing processes;
• Transfer to programs that are not self-directed; and
• Receive culturally competent services.
9.6. SDCB Member Responsibilities
SDCB members have certain responsibilities in order to participate in the program. Failure to comply
with these responsibilities or other program rules and policies can result in an involuntary termination
from the SDCB.
The most basic responsibility of each member is to maintain his/her financial and medical eligibility to
remain in the SDCB. This includes completing the required documentation to determine initial and
annual financial eligibility and participating in the initial and annual CNA conducted by the MCO. The
Care Coordinator and Support Broker may assist with the application and recertification process as
needed.
Ongoing SDCB member responsibilities include:
• Comply with the rules and policies that govern the SDCB;
• Maintain an open and collaborative relationship with the Care Coordinator and Support Broker, and
work together to determine support needs related to the activities of self-direction, develop an
appropriate SDCB care plan/budget request, receive necessary assistance with carrying out the
approved SDCB care plan/budget, and with documenting service delivery;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
213 | P a g e
• Communicate with the Support Broker at least once a month, either in person or by phone, and
meet with the Support Broker in-person at least once every three months. Report concerns or
problems with any part of SDCB to the Support Broker or Care Coordinator;
• Use SDCB funds appropriately by only requesting services and related goods covered by the SDCB
and only purchasing services and related goods after they have been approved by the MCO;
• Comply with the approved SDCB care plan and not spend more than the authorized budget;
• Work with the Care Coordinator by attending scheduled meetings and assessments, in the
member’s home as required, and providing documentation as requested;
• Respond to requests for additional documentation and information from the Care Coordinator,
Support Broker, FMA, and the MCO within the required deadlines;
• Report to the local ISD office, within 10 business days, any change in circumstances, including, but
not limited to, a change in address or hospitalization, which may affect eligibility for the program.
Changes in address or other contact information must also be reported to the Care Coordinator,
Support Broker and the FMA within 10 calendar days;
• Report to the Care Coordinator and Support Broker if hospitalized for more than three consecutive
nights so that a new appropriate LOC or CNA can be conducted; and
• Communicate with SDCB service providers, State contractors and State personnel in a respectful,
non-abusive and non-threatening manner.
Member/employer of record (EOR) Responsibilities: Every member must have an EOR who is
responsible for directing the work of SDCB employees and ensuring accurate and timely employee and
vendor payment requests are sent to the FMA for processing. The EOR must authorize by signing, either
electronically or on paper, all invoices and timesheets for his/her employees and vendors. A member
may be his/her own EOR unless the member is a minor or has a guardianship or conservatorship in place
that precludes the individual from exercising control over financial matters. A designated EOR may not
be an employee of the member. Members may also designate an individual of their choice to serve as
their EOR, subject to the EOR meeting the qualifications specified in the SDCB rules and policies. The
Care Coordinator completes an EOR self-assessment at least annually with the member to determine if
the member requires assistance in fulfilling the EOR responsibilities. If the EOR self-assessment
demonstrates the member is not able to be his/her own EOR, and the member does not designate a
qualified individual to serve as the EOR, the member shall not be allowed to transfer to SDCB until the

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
214 | P a g e
member designates a suitable EOR. If the member was already his/her own EOR, and based on the
results of the self-assessment, the Care Coordinator determines that the member requires assistance to
direct his or her services, the Care Coordinator shall inform the member that he or she will need to
designate an EOR to assume the self-direction functions on their behalf. A member’s failure to follow
this direction may be cause for involuntary termination from the SDCB program.
An EOR is responsible for recruiting, hiring, training, supervising and terminating employees, as
necessary. The EOR will establish work schedules and tasks and provide relevant training. The EOR will
keep track of SDCB budget amounts spent on paying employees and for approved services and related
goods. EORs authorize the payment of timesheets and invoices by the FMA. EORs must use the FMA
electronic timesheet system, unless granted an exception by the MCO. EORs must also ensure that their
self-directed personal care and respite providers use the State approved EVV system as required. An EOR
cannot be paid for any services utilized by the member for whom he or she is the EOR and the EOR
cannot be paid for performing the EOR functions. An individual may serve as an EOR for more than one
SDCB member.
The SDCB member/EOR responsibilities include:
• Arranging for the delivery of SDCB services, supports and related goods as approved in the SDCB
care plan;
• Verifying and attesting that employees meet the minimum qualifications for employment as
required by the SDCB;
• Orienting, training, and directing SDCB employees in providing the services that are described and
authorized in the member’s SDCB care plan;
• Establishing a mutually agreeable schedule for employees’ services in writing and providing fair
notice of changes in the employee’s work schedule in the event of unforeseen circumstances or
emergencies;
• Submitting all necessary and required documents to the FMA. Documents must be completed and
provided to the FMA according to the timelines and rules established by the State. Documents
include, but are not limited to, vendor and employee agreements, vendor information forms, CBC
forms, time-sheets, payment request forms (PRFs) and invoices, updated employee information, and
other documentation needed by the FMA to process timely and accurate payment to SDCB
providers;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
215 | P a g e
• Agreeing that SDCB employees may not begin work until all materials necessary for a CBC have been
received by the FMA and the employee has successfully passed the COR background check and the
National Sex Offender Registry;
• Agreeing to select or employ the employee on an interim (temporary) basis until a final CBC has
been successfully completed, for those crimes determined to be disqualifying convictions as stated
in NMSA 1978, Section 29-17-3. The EOR discusses this with the employee and reserves the right to
dismiss the employee based on the results of the CBC;
• Providing fair notice of changes in the employee’s work schedule in the event of unforeseen
circumstances or emergencies;
• Reviewing and approving/denying completed employee timesheets in order to pay employees
according to the FMA predetermined payroll schedule. Net wages are gross earnings calculated
according to the employee’s pay rate, minus payroll deductions for the employee’s share of
applicable State, Federal, and local payroll withholdings;
• Ensuring employees are not signing or sending in their own timesheets;
• Reporting any incidents of abuse, neglect or exploitation by any employee or other service provider
to the Support Broker and/or Care Coordinator;
• Maintaining SDCB employee and service records and documentation in accordance with SDCB rules
and policies, and Federal and state employment rules;
• As the common-law employer, fully cooperating with the New Mexico Department of Workforce
Solutions (DWS) in any investigations or other matters related to his/her SDCB employees;
• Working with the FMA and Care Coordinator on payment issues;
• Fully cooperating with the State’s worker’s compensation carrier. Responsibilities include reporting
claims and providing information to New Mexico Mutual;
• Meeting Federal employer requirements, such as completing and maintaining a Federal I-9 form for
each employee as required by law; and
• When necessary, requesting assistance from the Support Broker and/or Care Coordinator with any
of these SDCB responsibilities.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
216 | P a g e
9.7. SDCB Supports
Important resources of support and direction for members are the MCO, the Support Broker and the
FMA. The MCO determines initial and ongoing medical eligibility, reviews and authorizes the SDCB care
plan/budget, and provides care coordination and support to the member to ensure successful
implementation of the care plan. The Support Broker provides support to the SDCB member (or the
member’s family/representative, as appropriate) in arranging for, directing, and managing SDCB services
and supports as well as developing, implementing, and monitoring the care plan and budget. The FMA
acts as the intermediary between the member and the Medicaid payment system and assists the
member or the EOR with employer-related responsibilities.
MCO
The MCO provides services related to medical eligibility determination and re-determination, and
determines the NF LOC for SDCB members. The MCO also performs UM duties, including review and
approval or denial of each individual care plan. All SDCB members have an MCO Care Coordinator and a
Support Broker. The Care Coordinator and Support Broker assist the member with virtually every aspect
of the SDCB. The Support Broker is instrumental in developing the SDCB care plan and provides an
additional layer of assistance to ensure successful implementation of the SDCB care plan.
Care Coordinator
The Care Coordinator is responsible for managing the member’s acute care, BH care, LTC, and HCBS. In
SDCB, the Care Coordinator is primarily responsible for coordinating all aspects of the member’s care,
determining the SDCB budget, and submitting the care plan to the MCO for review and approval/denial.
Care Coordinator related assistance includes, but is not limited to:
• Understanding SDCB member and EOR roles and responsibilities;
• Identifying resources outside the SDCB, including natural and informal supports, that may assist in
meeting the member’s needs;
• Understanding the array of SDCB covered services, supports, and related goods;
• Determining and assigning the annual budget for the SDCB member, based on the CNA, to address
the home- and community-based needs of the SDCB member in accordance with the requirements
stated in the Agreement and the member’s CB;
• Providing the Support Broker with the current and all historical CNAs including the assessor’s
individual specific health and safety recommendations, and the calculations used to determine the
SDCB budget;
Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
217 | P a g e
• Monitoring utilization of SDCB services and related goods on a regular basis;
• Assisting the EOR, and working with the FMA; on payment issues;
• Conducting employer-related activities such as completing the EOR self-assessment with the
member and informing the FMA of the designated EOR;
• Identifying and resolving issues related to the implementation of the SDCB care plan/budget;
• Assisting the SDCB member with QA activities to ensure implementation of the member’s SDCB care
plan/budget, and utilization of the authorized budget;
• Recognizing and reporting critical incidents, including abuse, neglect, exploitation, emergency
services, law enforcement involvement, and environmental hazards;
• Monitoring the quality of services provided by Support Brokers;
• Assisting the member with Support Broker changes; and
• Working with the member to provide the necessary assistance for successful SDCB implementation.
Support Broker
Support Broker services are direct services intended to educate, guide, and assist the SDCB member to
make informed planning decisions about SDCB services and supports and to assist the member with QA
related to the SDCB care plan. This leads to the development of a Care Plan that is based on the
member’s assessed needs and is in accordance with 8.308.12 NMAC, and the Manual.
Support Broker services help the SDCB member to identify supports, services and related goods that
meet his/her needs as identified in the most recent CNA and are specific to the member’s disability or
qualifying condition and help prevent institutionalization. Support Broker services provide a level of
support to SDCB members that are unique to their individual needs in order to maximize their ability to
self-direct.
• The extent of assistance is based upon the individual member’s needs, and includes, but is not
limited to, providing help and guidance to:
o Educate members on how to use self-directed supports and services and provide information on
program changes or updates;
o Review, monitor and document progress of the member’s care plan;
o Assist in managing budget expenditures and complete and submit care plan revisions;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
218 | P a g e
o Assist with EOR functions including, but not limited to recruiting, hiring and supervising SDCB
providers;
o Assist with developing job descriptions for the SDCB direct support caregivers;
o Assist with completing forms related to SDCB employees;
o Assist with approving timesheets and purchase orders or invoices for related goods, obtaining
quotes for services and related goods as well as identifying and negotiating with vendors;
o Assist with problem solving employee and vendor payment issues with the FMA and other
relevant parties;
o Facilitate resolution of any disputes regarding payment to providers for services rendered;
o Develop the care plan based on the SDCB budget amount determined by the annual CNA;
o Assist in completing all documentation required by the FMA; and
o Assist with EVV functions including device registration and entering location information.
• Support Broker services begin with the enrollment of the member in SDCB and continue throughout
the member’s participation in SDCB. The Support Broker shall:
o Conduct a transition meeting, including the transfer of program information prior to the SDCB
enrollment meeting, for those members transitioning from the ABCB;
o Assist members to transition from/to ABCB/SDCB.
o Provide the SDCB member with information, support and assistance during the annual Medicaid
eligibility processes, including the annual CNA and the annual medical/financial eligibility
processes;
o Assist existing members with annual LOC requirements within 120 calendar days prior to the
expiration of the LOC; and
o Schedule member enrollment meetings within five business days of notification and Support
Broker agency selection. The actual enrollment meeting should be conducted within 30 calendar
days. Enrollment activities include but are not limited to:
▪ Ensure the member has received and reviewed the SDCB Rules and the Manual and provide
responses to their questions and/or concerns;
▪ General overview of the SDCB including key agencies, their responsibilities and contact
information;
▪ Discuss the annual Medicaid eligibility requirements and offer assistance in completing
these requirements as needed;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
219 | P a g e
▪ Discuss and review SDCB member roles and responsibilities;
▪ Discuss and review the EOR roles and responsibilities;
▪ Discuss and review the processes for hiring SDCB employees and contractors and required
paperwork;
▪ Discuss and review the requirements, process and paperwork for hiring LRIs as employees;
▪ Discuss and review the background check and other credentialing requirements for SDCB
employees and vendors;
▪ Referral for accessing training for the FOCoSonline system; and to obtain information on the
FMA;
▪ Discuss and review the EVV system that personal care and respite provider(s) will be
required to use;
o Schedule the date for SDCB care plan meeting within 10 business days of the SDCB enrollment
meeting;
o Provide information on the SDCB care plan including covered services and related goods, and
community resources available;
o Assist the members in utilizing all program assessments including the CNA, to develop each
SDCB care plan;
o Educate members regarding SDCB covered services, supports and related goods;
o Assist member to identify resources outside SDCB that may assist in meeting his/her needs as
identified in the CNA;
o Assist the member with the application for LRI as employee process; submit the application to
the MCO/UR;
o Assist members with the environmental modification process;
o Serve as an advocate for the SDCB member, as needed, to enhance his/her opportunity to be
successful in the SDCB;
o Assist the member with reconsiderations of services or related goods denied by the MCO/UR,
submit documentations as required, and participate in MCO appeals process and State Fair
Hearings as requested by the MCO, SDCB member or state;
o Assist the member with QA activities to ensure implementation of the member’s SDCB care
plan, and utilization of the SDCB annual budget;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
220 | P a g e
o Assist members to transition to another Support Broker agency when requested. Support Broker
transitions should occur within 30 calendar days of SDCB member’s written request, but may
occur sooner based on the needs of the SDCB member. Transition from one Support Broker
agency to another can only occur at the first of the month. Support Broker agency transitions
may not occur if there are less than 120 days remaining in the current LOC;
o Assist members to identify and resolve issues related to the implementation of the SDCB care
plan; and
o Assist the member, employee(s) and EOR in utilizing the EVV system, including but not limited
to:
▪ Registering the device (tablet, computer or mobile device) to be utilized for EVV;
▪ Collaborating with MCO Care Coordination and the member/EOR to resolve any
time entry, timecard, or payment issues;
▪ Understanding and agreeing to all roles and responsibilities of the EVV system;
▪ Training and assisting member/EOR and employee(s) on the EVV system to
include:
• Employee and EOR device enrollment
• Employee initial log in
• Employer Web log in
• Alternate Interactive Voice Response (IVR) phone numbers
• Updating alternate care locations
• Support Brokers must ensure the SDCB care plan for each member is submitted in the appropriate
format as prescribed by the state and MCOs, utilizing the FOCoSonline system. The care plan in
FOCoSonline shall include the following:
o The requested services and supports that are covered by the SDCB, and necessary to address
the needs of the member as determined through the CNA and person-centered planning
process;
o The purpose for the requested services, expected outcomes, and methods for monitoring
progress must be clearly and specifically identified and addressed;
o Clear, specific and accurate calculation of the employee/vendor reimbursement rate including
all local and/or Federal taxes using the calculator in FOCoSonline; and

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
221 | P a g e
o The quality indicators, identified by the member, for the services and supports provided through
the SDCB. SDCB care plan revisions shall be completed and submitted as needed, in the format
as prescribed by the state. No more than one revision is allowed to be submitted at any given
time. The annual SDCB care plan must be submitted to the Care Coordinator and MCO/UR at
least 30 calendar days prior to the expiration of the current SDCB plan so that sufficient time is
afforded for MCO/UR review. A copy of the final approved SDCB care plan and budget
documents must be provided to each SDCB member.
• Support Brokers will contact the SDCB member in person or by telephone at least monthly for a
routine follow-up. Support Brokers will meet in person with the member at least once per quarter. It
is mandatory that a minimum of one visit per SDCB care plan year is to be conducted in the
member’s home. Support Brokers will, at a minimum:
o Review spending patterns;
o Review and document progress of care plan/budget implementation;
o Document the usage and effectiveness of the SDCB backup plan; and
o Document the purchase of related goods.
The quarterly visits are for the following purposes:
o Review and document progress on implementation of the SDCB care plan;
o Review and document any usage and the effectiveness of the 24-hour backup plan and update
the backup plan as necessary;
o Review SDCB care plan and budget spending patterns (over and underutilization);
o Review and document the SDCB member’s access to SDCB related goods requested and
approved in the SDCB care plan;
o Review any incidents or events that have impacted the SDCB member’s health and welfare or
ability to fully access and utilize service(s) as identified and approved in the SDCB care plan; and
o Identify other concerns or challenges as noted by the member/representative/EOR.
Administrative Requirements
Support Broker services may be provided by direct MCO personnel or by Support Broker agencies
subcontracted by the MCO. SDCB members may choose to work with one of their MCO’s contracted
Support Broker agencies that is providing Support Broker services in their region. If an MCO employs

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
222 | P a g e
MCO personnel to provide Support Broker services, the same qualifications and criteria that are used for
Support Broker agencies also apply to the MCO personnel.
The Support Broker agency shall comply with all applicable Federal and State rules, all policies and
procedures governing Support Broker services, all terms of their provider agreement and shall meet all
of the following requirements, as applicable:
• Have a current business license issued by the state, county, or city government as required;
• Maintain financial solvency;
• Ensure all employees providing Support Broker services under this standard attend all
State-required orientation and trainings and demonstrate knowledge of and competence with the
SDCB rules, policies and procedures, philosophy of self-direction, financial management processes
and responsibilities, CNA, person-centered planning and SDCB care plan development, and adhere
to all other training requirements as specified by the State;
• Ensure all employees are trained and competent in the use of the FMA and FOCoSonline system;
• Ensure all employees providing services under this scope of service and all other staff are trained on
how to identify and where to report critical incidents, abuse, neglect and exploitation; and
• Ensure compliance with the Caregivers Criminal History Screening Requirements (7.1.9 NMAC) for all
employees.
The Support Broker agency shall develop a quality management plan to ensure compliance with
regulatory and program requirements and to identify opportunities for continuous QI.
The Support Broker agency shall ensure that SDCB members have access to their Support Broker. This
requirement includes, but is not limited to the following:
• The Support Broker agency must maintain a presence in each region for which they are providing
services;
• The Support Broker agency must maintain a consistent way (for example, phone, pager, email, and
fax) for the SDCB member to contact the Support Broker provider during typical business hours
which are 8:00 a.m. to 5:00 p.m. Monday through Friday;
• The Support Broker agency must maintain a consistent way (for example phone, pager, email, and
fax) for the SDCB member to contact the Support Broker provider during non-business hours: prior
to 8:00 a.m. and after 5:00 p.m. MST on weekdays and on weekends and for emergency purposes;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
223 | P a g e
• The Support Broker agency must provide a location to conduct confidential meetings with SDCB
members when it is not possible to do so in the SDCB member’s home. This location must be
convenient for the SDCB member and compliant with the ADA;
• The Support Broker agency must maintain an operational fax machine at all times;
• The Support Broker agency must maintain an operational email; address, internet access, and the
necessary technology to access SDCB related systems;
• The Support Broker agency shall maintain a current local/state community resource manual;
• The Support Broker agency shall adhere to Medicaid General Provider policies 8.302.1.;
• The Support Broker agency shall ensure the development and implementation of a written
grievance procedure in compliance with 8.349.2.11 NMAC;
• The Support Broker agency shall meet all of the qualifications set forth in 8.304.12 NMAC; and/or
• The Support Broker agency shall maintain HIPAA compliant primary records for each member
including, but not limited to:
o Current and historical SDCB care plan and budget;
o Contact log that documents all communication with the SDCB member;
o Completed/signed quarterly visit form(s);
o MCO/UR documentation of approvals/denials, including SDCB care plan and revision requests;
o MCO/UR correspondence; (requests for additional information, etc.);
o Copy of current and all historical CNAs including the assessor’s individual specific health and
safety recommendations;
o Notifications of medical and financial eligibility;
o SDCB budget utilization reports from the FMA;
o Environmental modification approvals/denials;
o LRI approvals/denials;
o Documentation of SDCB member and employee incident management training;
o Copy of legal guardianship or representative papers and other pertinent legal designations;
o Copy of the approval form for the AR and/or AA; and
o Copies of completed EOR self-assessments.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
224 | P a g e
Support Broker Qualifications
Support Broker agencies shall ensure that all individuals providing Support Broker services meet the
criteria specified in this section. Support Broker providers shall:
• Be at least 18 years of age; and
• Possess a minimum of a Bachelor’s degree in social work, psychology, human services, counseling,
nursing, special education or a closely related field; or
• Have one year of supervised experience working with seniors and/or people living with disabilities;
or
• Have a minimum of six years of direct experience related to the delivery of social services to seniors
and/or people living with disabilities;
• Complete all required SDCB orientation and training courses; and
• Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section 29-17-2 et
seq. and 7.1.9 NMAC and an abuse registry screen pursuant to NMSA 1978, Section 27-7a-1 et seq.
and 8.11.6 NMAC; and the National Sex Offender Registry.
Conflict of Interest
The Support Broker agency may not provide any other direct services for SDCB members that have an
approved SDCB care plan and are actively receiving services in the SDCB. The Support Broker agency may
not employ, as a Support Broker, any immediate family member or guardian of a member in the SDCB
that is served by the Support Broker agency.
Critical Incident Management Responsibilities and Reporting Requirements
All incident reports for the HCBS and BH services population involving abuse, neglect, self-neglect,
exploitation, environmental hazard, law enforcement involvement, and emergency services, must be
reported to the member’s MCO, Support Broker and/or APS.
The Support Broker agency shall provide training to SDCB members related to recognizing and reporting
critical incidents. Critical incidents include: abuse, neglect, exploitation, emergency services, law
enforcement involvement, environmental hazards and member deaths. This SDCB member training shall
also include reporting procedures for SDCB employees, members/member representatives, and other
designated individuals. Please refer to the Critical Incident Management Responsibilities for
requirements.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
225 | P a g e
The Support Broker agency will also maintain documentation that each SDCB member has been trained
on the critical incident reporting process. This member training shall include reporting procedures for
SDCB members, employees, member representative, and/or other designated individuals. The Support
Broker agency shall report incidents of abuse, neglect and/or exploitation as directed by the State.
The Support Broker agency will maintain a critical incident management system to identify, report, and
address critical incidents. The Support Broker is responsible for follow-up and assisting the individual to
help ensure health and safety when a critical incident has occurred.
Financial Management Agent
The FMA is under contract with the MCOs to provide payment for services and related goods which are
approved on the SDCB care plan. The FMA is responsible for providing the following services in the
SDCB:
• Assure SDCB compliance with state and Federal employment and IRS requirements;
• Assist each member/EOR to set up a unique EIN if they intend to hire employees;
• Answer member inquiries, solve related problems, and offer periodic trainings for members and
their representatives on how to handle the SDCB billing and invoicing processes;
• Provide all members with necessary documents, instructions and guidelines;
• Collect all documentation necessary to verify that SDCB providers and vendors have the
qualifications and credentials required by the SDCB rules;
• Collect all documentation necessary to support the member’s specific arrangements with each
employee and vendor, including employment agreement forms and vendor agreement forms;
• Successfully complete criminal history and/or background investigations for prospective SDCB
service providers, pursuant to 7.1.9 NMAC and in accordance with 1978 Section 29-17-1 NMAC of
the Caregivers Criminal History Screening Act and the National Sex Offender Registry;
• Check the Department of Health Employee Abuse Registry, pursuant to 7.1.12 NMAC COR, to
determine whether prospective SDCB service providers or employees of members are included in
the registry. If a prospective SDCB provider or employee is listed in the Abuse Registry, that person
or vendor may not be employed by a SDCB member/EOR;
• Process and pay invoices for services and related goods that are approved in the member’s care
plan, when supported by required documentation;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
226 | P a g e
• Handle all payroll functions on behalf of members who hire direct service employees and other
support personnel, including collecting and processing timesheets of support workers, processing
payroll, withholding, filing and payment of applicable Federal, State and local employment-related
taxes and insurances;
• Track and report on SDCB employee payment disbursements and balances of member funds,
including providing the member and his/her Care Coordinator/Support Broker with a monthly report
of expenditures and budget status; and
• Report any concerns related to the health and safety of a member or that the member is not
following the approved SDCB care plan/budget to the Care Coordinator and/or Support Broker, and
HSD/MAD, as appropriate.
FOCoSonline
In addition to the above functions, the FMA operates FOCoSonline. FOCoSonline is a web-based system
that is used for FMA functions such as housing the SDCB care plan, noting the annual SDCB budget,
tracking the credentialing status of employees and vendors, timesheet submission, payment processing
for employees and vendors, and tracking the SDCB care plan/budget expenditures.
FOCoSonline is also used by SDCB members/EORs, Support Brokers and Care Coordinators to develop
and submit a SDCB care plan for MCO/UR review and approval/denial.
The MCO/UR also uses FOCoSonline to receive SDCB care plan/budget requests and request additional
information from the SDCB member and Care Coordinator/Support Broker, and to indicate what SDCB
services, supports and related goods have been approved or denied.
The FMA will provide SDCB members/EORs, Care Coordinators and Support Brokers with training and
access for FOCoSonline, as well as on-going technical assistance and help with problem solving.
9.8. Planning and Budgeting for SDCB Covered Services
SDCB Care Plan Development Processes
The SDCB care plan development process starts with person-centered planning. In person-centered
planning, the SDCB care plan must revolve around the individual SDCB member and reflect his/her
chosen lifestyle, cultural, functional, and social needs for successful community living. The goal of the
SDCB care plan development process is for the SDCB member to achieve a meaningful life in the
community, as defined by the SDCB member. Upon enrollment in SDCB and choosing his/her Support

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
227 | P a g e
Broker agency, each SDCB member shall receive a SDCB budget amount, which is determined by the
Care Coordinator, based on the results of the NF LOC and the CNA. The SDCB budget amount is entered
into FOCoSonline by the Care Coordinator. The SDCB member will receive information and training from
the Care Coordinator and/or Support Broker about covered SDCB services and the requirements for the
content of the SDCB care plan.
The SDCB member is the leader in the development of the SDCB care plan. The member will take the
lead or be encouraged and supported to take the lead to the best of his/her abilities, to direct the
development of the SDCB care plan. If the member desires, he/she may include family members or
other individuals, including service workers or providers, in the SDCB care plan development process.
The SDCB care plan is entered into FOCoSonline by the Support Broker. The SDCB care plan is developed
one goal at a time. Each goal shall include a clear and complete explanation of the requested service(s)
or good(s) as defined in the service description, how they are related to the member’s condition and why
they are appropriate for the member.
In addition, each goal includes full details about each of the requested service(s) or good(s), including,
but not limited to: amount, frequency, cost or estimated cost, and rate of pay.
The SDCB care plan is developed by the member and the Support Broker. Once the SDCB care plan
request is complete and approved by the SDCB member, the Support Broker notifies the Care
Coordinator, via FOCoSonline, the member’s SDCB care plan is ready for review and submission into
FOCoSonline. After reviewing the SDCB care plan, the Care Coordinator will submit it in FOCoSonline to
the MCO/UR for review and approval or denial using FOCoSonline. Annual SDCB care plans shall be
submitted by the Care Coordinator to the MCO/UR no later than 30 calendar days prior to the end of the
current SDCB care plan/budget year. MCOs must provide the member with a written Notice of Action for
all MCO/UR decisions made in response to SDCB service related requests made by the SDCB member via
FOCoSonline.
SDCB Member’s Employer Authority
The SDCB EOR is the common-law employer of all SDCB service providers. The FMA serves as the
member’s agent in conducting payroll and other employer-related responsibilities that are required by
Federal and State law.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
228 | P a g e
SDCB Member Decision-Making Authority
Members shall have authority to do the following:
• Complete the employer paperwork to be submitted to the FMA;
• Determine the amount paid for SDCB services within the State’s approved limits (Range of Rates,
9.22.1);
• Schedule the provision of SDCB services;
• Specify service provider qualifications of the SDCB member’s choice, consistent with the
qualifications specified in the SDCB rules and the Manual;
• Specify how SDCB services are provided, consistent with the SDCB rules and the Manual;
• Identify potential SDCB service providers and vendors and refer them to the FMA for enrollment;
• Arrange to have potential SDCB service providers paid for the approved SDCB services by ensuring
that all proposed SDCB employees and service providers complete all FMA required paperwork,
including a CBC when necessary. Payment for approved SDCB services and related goods cannot be
made until all necessary and required paperwork is successfully completed and approved by the
FMA;
• Review, approve and submit SDCB provider timesheets to the FMA within established timeframes.
Timesheets must be submitted to the FMA electronically through FOCoSonline. The member’s MCO
shall approve an exception to the online timesheet requirement if the member is unable to submit
timesheets electronically. Failure to submit SDCB provider timesheets within the required
timeframes will result in SDCB providers not being paid in accordance with the employee payroll
schedule;
• Review, approve and submit payment requests, according to the SDCB care plan, for approved SDCB
services and related goods identified in the approved SDCB care plan. The SDCB member/EOR must
submit a PRF to the FMA and an invoice or receipt from a SDCB vendor for any item he/she has an
approved SDCB goal and budget to purchase; and
• Additionally, the SDCB members:
o Cannot/will not be reimbursed directly for any SDCB services, supports and/or related goods;
o Must follow the SDCB care plan as approved by the MCO/UR;
o Shall work with the FMA to have all potential SDCB employees, providers and vendors approved
and enrolled prior to delivery or provision of any SDCB service or good; and

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
229 | P a g e
o Shall be accountable for the use of all SDCB funds.
9.9. SDCB Qualifications for all SDCB Employees, Independent Providers, Provider Agencies and Vendors
In order to be approved as a SDCB employee, an independent provider, a provider agency (excluding
Support Broker agencies, which are covered later in this document) or a vendor, each entity must meet
the general and service specific qualifications found in the SDCB rules and the Manual and submit an
employee agreement packet or vendor agreement packet, specific to the SDCB provider or vendor type,
for approval to the FMA.
SDCB providers must meet all Federal and State requirements for home- and community-based
providers. In order to be an authorized provider for SDCB, and receive payment for delivered services,
the potential provider must complete and sign an employee agreement or vendor agreement and
provide all required credentialing documents. The potential provider’s credentials must be verified by
the member/EOR and the FMA.
General qualifications for SDCB individual employees, independent providers, including non-licensed
homemaker/companion workers and provider agencies who are employed by a SDCB member/EOR to
provide direct services:
• Be at least 18 years of age;
• Be qualified to perform the service and demonstrate capacity to perform required tasks;
• Be able to communicate successfully with the SDCB member;
• Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section 29-17-2 et
seq. and 7.1.9 NMAC and an abuse registry screen pursuant to NMSA 1978, Section 27-7a-1 et seq.
and 8.11.6 NMAC and the National Sex Offender Registry;
• Complete training on critical incident, abuse, neglect, and exploitation reporting;
• Complete member specific training; the evaluation of training needs is determined by the member
or his/her legal representative; the member is also responsible for providing and arranging for
employee training and supervising employee performance; training expenses for paid employees
cannot be paid for with the SDCB member’s annual budget;
• Meet any other service specific qualifications, as specified in the SDCB rules (8.308.12 NMAC); and
• Maintain documentation of services provided per the SDCB rules (8.308.12 NMAC).
General qualifications for SDCB vendors, including those providing professional services:

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
230 | P a g e
• Be qualified to provide the service;
• Possess a valid business license, if applicable;
• If a professional provider, be required to follow the applicable licensing regulations set forth by the
profession; refer to the appropriate New Mexico Board of Licensure for information regarding
applicable licenses;
• If a Support Broker provider, meet all of the qualifications set forth in 8.308.12 NMAC;
• If a currently approved SDCB provider, be in good standing with the appropriate state agency;
• Meet any other service specific qualifications, as specified in the SDCB rules (8.308.12 NMAC); and
• Maintain documentation of services provided per the SDCB rules (8.308.12 NMAC).
General qualifications for LRIs who provide services:
• LRIs (e.g., the parent/guardian biological, legal or adoptive) of a minor child (under age 18) or the
guardian of a minor child, who must provide care to the child, or a spouse of a member, may be
hired and paid for the provision of SDCB-covered services (except Support Broker) under
extraordinary circumstances in order to assure the health and welfare of the member, to avoid
institutionalization and provided that the state is eligible to receive Federal financial participation;
• Extraordinary circumstances include the inability of the parent/legal guardian to find and retain
other qualified, suitable caregivers when the parent/guardian would otherwise be absent from the
home and, thus, the parent/guardian must stay at home to ensure the member’s health and safety.
The member may request that the LRI (parent/guardian or spouse) be allowed to be employed by
the member/EOR and provide services as approved in the member’s current SDCB care plan. The
request must include documentation showing all attempts to employ other available resources in
the member’s community, the challenges the member and/or providers encountered, and why the
member-chosen providers were unable to successfully provide the approved covered service as
approved in the SDCB care plan;
• LRIs may not be paid for any services that they would ordinarily perform in the household for
individuals of the same age who do not have a disability or chronic illness. This includes, but is not
limited to, transportation of minors to and from school, activities and events; and
• Requests to employ an LRI must be submitted in writing to the MCO. The request must be approved
or denied in writing by the appropriate MCO/UR staff member. The approval of an LRI must be
renewed annually, at the same time as the NF LOC and SDCB care plan.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
231 | P a g e
• Services provided by LRIs must:
o Meet the definition of a SDCB covered service and be specified in the member’s approved SDCB
care plan;
o Be provided by a SDCB member’s parent/guardian or spouse who meets the provider
qualifications and training standards specified in the SDCB rules and these service descriptions
and qualifications for that covered service; and
o Be paid at a rate that does not exceed the SDCB Range of Rates (9.22.1) for the specific service
the LRI is approved to provide and be approved by the MCO/UR.
9.10. SDCB Covered Services
All services are subject to the approval of the MCO/UR. Below is a list of SDCB covered services and
related goods for members in SDCB, followed by a detailed service description:
• Behavior Support Consultation Services;
• Customized Community Support;
• Emergency Response;
• Employment Supports;
• Environmental Modifications;
• HH Aide;
• Nutritional Counseling;
• Private Duty Nursing;
• Related Goods;
• Respite;
• Self-Directed Personal Care;
• Skilled Maintenance Therapy Services for Adults;
• Specialized Therapies; and
• Transportation (Non-Medical).
Descriptions for each of the above SDCB covered services are as follows.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
232 | P a g e
Behavior support consultation services
• Definition of Service
Behavior Support Consultation services consist of functional support assessments, treatment plan
development and training and support coordination for a SDCB member related to behaviors that
compromise a member’s quality of life. Behavior support consultation services are provided in an
integrated/natural setting or in a clinical setting.
• Scope of Services:
o Inform and guide the SDCB member, family, employees and/or vendors on understanding the
contributing factors to the SDCB member’s behavior;
o Identify support strategies to enhance functional capacities, adding to the provider’s
competency to predict, prevent and respond to interfering behavior and potentially reducing
interfering behaviors;
o Support effective implementation based on a functional assessment and subsequent SDCB care
plans;
o Collaborate with medical and ancillary therapies to promote coherent psychotherapeutic
medications; and
o Monitor and adapt support strategies based on the response of the SDCB member and his/her
family, employees and/or vendors.
• Behavior Support Consultant Qualifications – Individual:
o Provide a tax identification number;
o Maintain a member file within HIPAA guidelines to include:
▪ Member’s SDCB care plan;
▪ Reports as requested in the SDCB care plan;
▪ Contact notes; and
▪ Training roster(s).
o Have and maintain a current New Mexico license with the appropriate professional field
licensing body; current licensure may be any of the following:
▪ MD;
▪ Licensed clinical psychologist;
▪ Licensed psychologist associate (masters or PhD level);
▪ LISW or LMSW;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
233 | P a g e
▪ LPCC;
▪ Licensed professional counselor (LPC);
▪ Licensed psychiatric nurse;
▪ LMFT; or
▪ Licensed practicing art therapist (LPAT).
• Behavior Support Consultant Qualifications - Provider Agency
o Provide a tax identification number; and current business license issued by State, county or city
government, if required;
o Maintain a member file within HIPAA guidelines to include:
▪ Member’s SDCB care plan;
▪ Reports as requested in the SDCB care plan;
▪ Contact notes; and
▪ Training roster(s).
o Ensure therapists have and maintain a current New Mexico license with the appropriate
professional field licensing body; current licensure may be any of the following:
▪ MD;
▪ Licensed clinical psychologist;
▪ Licensed psychologist associate (masters or PhD level);
▪ LISW or LMSW;
▪ LPCC;
▪ LPC;
▪ MSN/RNSC;
▪ LMFT; or
▪ LPAT.
Customized Community Supports
• Definition of Service
o Customized community support services are designed to offer the SDCB member flexible
supports that are related to the member’s qualifying condition or disability. Customized
community supports may include participation in congregate community day programs and
centers that offer functional meaningful activities that assist with acquisition, retention, or

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
234 | P a g e
improvement in self-help, socialization and adaptive skills. Customized community supports may
include adult day habilitation, adult day health and other day support models. Customized
community supports are provided in community day program facilities and centers and can take
place in non-institutional and non-residential settings.
o Customized community supports settings must be integrated and support full access of
individuals receiving Centennial Care CBs to the greater community, including opportunities to
seek employment, and work in competitive integrated settings, engage in community life,
control personal resources, and receive services in the community, with the same degree of
access as individuals not receiving Medicaid HCBS.
o These services are provided at least four or more hours per day one or more days per week as
specified in the member’s SDCB care plan. Customized community supports cannot duplicate
any other SDCB service.
• Scope of Services
o Customized Community Support services include, but are not limited to the following:
▪ Provide supports in congregate and community day programs that assist with the
acquisition, retention or improvement in self-help, socialization and adaptive skills;
▪ Adult day health services;
▪ Adult day habilitation services; and
▪ Other day support model services.
o Customized Community Supports Qualifications - Provider Agency:
▪ Possess a current business license, if applicable;
▪ Meet financial solvency;
▪ Adhere to training requirements;
▪ Maintain member records for each member within HIPAA compliance;
▪ Develop and adhere to a records management policy;
▪ Develop and adhere to QA rules and requirements;
▪ Adult day health provider agencies must be licensed by New Mexico DOH as an adult day
care facility pursuant to 7.13.2 NMAC; and
▪ Ensure all assigned staff meets the following qualifications:
• Be at least 18 years of age;
• Have at least one year of experience working with people with disabilities;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
235 | P a g e
• Be qualified to perform the service and demonstrate capacity to perform required tasks;
• Be able to communicate successfully with the member/member representative;
• Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section
29-17-2 et seq. and 7.1.9 NMAC and an abuse registry screen pursuant to NMSA 1978,
Section 27-7a-1 et seq. and 8.11.6 NMAC;
• Complete training on critical incident, abuse, neglect, and exploitation reporting;
• Complete member specific training; the evaluation of training needs is determined by
the member or his/her legal representative; member is also responsible for providing
and arranging for provider training and supervising provider performance; training
expenses for paid providers cannot be paid for with the SDCB member’s budget; and
• Meet any other service qualifications, as specified in the SDCB rules.
Emergency Response
• Definition of Service:
o Emergency Response Services provide an electronic device that enables a member to secure help
in an emergency at home and thereby avoid institutionalization. The member may also wear a
portable “help” button to allow for mobility. The system is connected to the member’s phone
and programmed to signal a response center when a “help” button is activated. The response
center is staffed by trained professionals.
• Scope of Services:
o Testing and maintaining equipment;
o Training SDCB members, caregivers and first responders on the use of the equipment;
o 24-hour monitoring for alarms;
o Checking systems monthly or more frequently if warranted (e.g., electrical outages, severe
weather); and
o Reporting member’s condition that may affect service delivery; and
o Initial set-up and installation of Emergency Response Service devices is not a covered service; see
the service description for environmental modification for allowance of the initial set-up and
installation.
• Emergency Response Qualifications – Vendor/Agency

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
236 | P a g e
o Comply with all laws, rules and regulations of the New Mexico State Corporation Commission
for Telecommunications and Security Systems; and
o Comply with all laws, rules and regulations from the Federal Communications Commission for
telecommunications.
Employment Supports
• Definition of Service:
o Employment support services provide support to the member in achieving and maintaining
employment in jobs of his/her choice in his/her community. The member must exhaust all
available vocational rehabilitation supports prior to requesting Employment Supports on his/her
SDCB care plan Employment Supports cannot duplicate any other SDCB service. Employment
Supports include two types of services: job coaching and job-development. The specific
employment support service to be provided must be clearly described in the member’s care
plan and must address specific employment-related activities;
o Employment Supports will be provided by staff at current or potential work sites. If member is
self-employed, Employment Supports may be provided in a setting other than a formal work
site. When employment support services are provided at a work site where persons without
disabilities are employed, payment is made only for the adaptations, supervision and training
required by members receiving SDCB services as a result of their disabilities, but does not
include payment for the supervisory activities rendered as a normal part of the business setting.
Employment Supports settings must be integrated in, and support full access for individuals
receiving Medicaid HCBS to the greater community, including opportunities to seek
employment, and work in competitive integrated settings, engage in community life, control
personal resources, and receive services in the community, to the same degree of access as
individuals not receiving Centennial Care CBs; and
o Providers will maintain a confidential case file for each individual that documents activities,
progress and scope of work outlined in the member’s SDCB care plan. Documentation is
maintained in the file of each member receiving this service to demonstrate that the service is
not available under a program funded under section 110 of the Rehabilitation Act of 1973 or
Individuals with Disabilities Education Act (IDEA).
• Employment Supports include the following services:

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
237 | P a g e
o Job coaching is a service provided to members when the services are not otherwise available for
the member under a program funded under the Rehabilitation Act of 1973, the Division of
Vocational Rehabilitation (DVR) or through the New Mexico Department of Education. Job
coaching services are available 365 days a year, 24 hours a day. Services are driven by the
member’s SDCB care plan, budget and job. Medicaid funds are not used to pay the member. Job
coaches will adhere to the specific supports and expectations negotiated with the member and
employer prior to service delivery; and
o Job development services are provided to members when the services are not otherwise
available for the member under a program funded under the Rehabilitation Act of 1973, the
DVR or through the New Mexico Department of Education. Job development is a service
provided to members by skilled staff. The service has five components: job identification and
development activities; employer negotiations; job restructuring; job sampling; and job
placement.
• Scope of job coach services:
Job coach services will include, but are not limited to the following:
o Provide support to members as contained in the SDCB care plan as to achieve his/her outcomes;
o Teach vocational skills in a workplace setting;
o Employ job-coaching techniques and help members learn to accomplish job tasks to the
employer’s specifications;
o Increase the member’s capacity to engage in meaningful and productive interpersonal
interactions with co-workers, supervisors and customers;
o Identify and strengthen natural supports that are available to the member at the job site and
decrease paid supports in response to increased natural supports;
o Identify specific information about the member’s employment interests, preferences and
abilities;
o Effectively communicate with the employer about how to support the member to succeed
including any special precautions and considerations of the member’s disability, medications, or
other special concerns;
o Monitor and evaluate the effectiveness of the service and provide reports or documentation to
the member as requested in the SDCB care plan;
o Address behavioral, medical or other significant needs identified in the SDCB care plan;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
238 | P a g e
o Follow any individual specific therapeutic recommendations including speech, occupational
and/or PT, behavioral support, special diets and other therapeutic routines that are noted in the
SDCB care plan;
o Communicate effectively with the member including communication through the use of
adaptive equipment as well as the member’s communication dictionary, if applicable, at the
work site;
o Monitor the health and safety of the member;
o Model behavior, instruct and monitor any workplace requirements to the member;
o Adhere to professionally acceptable business attire and appearance, and communicate
professionally and in a respectful manner; and
o Adherence to rules of the specific workplace, including dress, confidentiality, safety rules and
other areas required by the employer.
• Scope of job development services:
o Identify potential employers and jobs in the area that provide work opportunities consistent
with the member’s preferences, interests and choice;
o Negotiate job functions, hours and supervision in the member’s best interest;
o Conduct satisfaction surveys as requested by the member;
o Broker relationships between the employer and the member in order to develop and maintain
job success;
o Identify potential employers and jobs in the area that provide work opportunities consistent
with the member’s preferences, interests and choices;
o Conduct job task analysis to ensure appropriate job match(es);
o Assess barriers to member skill development on the job and provide or obtain appropriate
accommodations tailored to the SDCB member’s ability to master task;
o Interact professionally in individual and group contacts, on the phone, in writing with various
levels of the company, including human resources and management;
o Assist the employer with ADA issues, Work Opportunity Tax Credit eligibility, requests for
reasonable accommodations, disability awareness training and workplace modification or make
referrals to appropriate agencies;
o Utilize, refer, and communicate with the DVR concerning job placement and referral activities
consistent with industry and SDCB standards;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
239 | P a g e
o Utilize DWS Navigators and One-Stop Career Centers, Business Leadership Network (BLN),
Chamber of Commerce, Job Accommodation Network (JAN), Small Business Development
Centers, Retired Executive, Businesses, community agencies, and the New Mexico Employment
Institute to achieve employment outcomes;
o Maintain on-going communication with various levels of the employer company to assure
satisfaction to both the member and the company;
o During the time of service delivery, ensure the member’s earnings and benefits are in
accordance with Fair Labor Standards Act. Each member’s earnings and benefits will be
reviewed at least semi-annually during the SDCB care plan year to ensure the appropriateness of
pay rates and benefits;
o Conduct a vocational assessment or profile as deemed necessary upon request of the member;
o Provide a career development plan as deemed necessary or upon the request of the member;
o Develop specific supports and expectations at the work site that are appropriate to the setting
and negotiated with the employer prior to and during employment;
o Verify and ensure that members receive job benefits and services such as paid time off, health
insurance, retirement, awards, raises, performance reviews and training consistent with those in
a similar job category; and
o Provide career and skill development for advancement and integration in work-related activities
or events.
• Job Coach Qualifications – Individual Provider:
o Be at least 18 years of age;
o Be qualified to perform the service and demonstrate capacity to perform required tasks;
o Be able to communicate successfully with the member;
o Experience as a job coach for at least one year;
o Experience for at least one year using job and task analyses;
o Trained on ADA;
o Trained on the purpose, function and general practices of the DVR;
o Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section 29-17-2
et seq. and 7.1.9 NMAC and an abuse registry screen pursuant to NMSA 1978, Section 27-7a-1
et seq. and 8.11.6 NMAC;
o Complete training on critical incident, abuse, neglect, and exploitation reporting;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
240 | P a g e
o Complete member specific training; the evaluation of training needs is determined by the
member or his/her legal representative; member is also responsible for providing and arranging
for provider training and supervising provider performance; training expenses for paid providers
cannot be paid for with the member’s annual budget; and
o Meet any other service qualifications, as specified in the SDCB rules.
• Job Developer Qualifications – Individual Provider:
o Be at least 18 years of age;
o Pass CBC and abuse registry screen;
o Experience as a job developer for at least one year;
o Experience for at least one year developing and using job task and analyses;
o Experience for at least one year working with the DVR, an independent living center or
organization that provides Employment Supports or services for people with disabilities;
o Trained on the purposes, functions and general practices entities such as:
▪ DWS Navigators;
▪ One-Stop Career Centers;
▪ BLN;
▪ Chamber of Commerce;
▪ JAN;
▪ Small Business Development Centers;
▪ Retired Executives; and
▪ New Mexico Employment Institute.
o Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section 29-17-2
et seq. and 7.1.9 NMAC and an abuse registry screen pursuant to NMSA 1978, Section 27-7a-1
et seq. and 8.11.6 NMAC;
o Complete training on critical incident, abuse, neglect, and exploitation reporting;
o Complete member specific training; the evaluation of training needs is determined by the
member or his/her legal representative; member is also responsible for providing and arranging
for provider training and supervising provider performance; training expenses for paid providers
cannot be paid for with the SDCB member’s annual budget; and
o Meet any other service qualifications, as specified in the SDCB rules.
• Job Coach and/or Job Developer Qualifications – Provider Agency:

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
241 | P a g e
o Possess a current business license, if applicable;
o Meet financial solvency;
o Adhere to training requirements;
o Maintain individual records for each member within HIPAA compliance. The agency will
maintain a confidential case file for each member that documents activities, progress and scope
of work outlined in the member’s SDCB care plan;
o Develop and adhere to a records management policy;
o Develop and adhere to QA rules and requirements;
o Ensure job coaches have the following qualifications:
▪ Be at least 18 years of age;
▪ Be qualified to perform the service and demonstrate capacity to perform required tasks;
▪ Be able to communicate successfully with the member;
▪ Experience as a job coach for at least one year;
▪ Experience for at least one year using job and task analyses;
▪ Trained on ADA;
▪ Trained on the purpose, function and general practices of the DVR;
▪ Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section
29-17-2 et seq. and 7.1.9 NMAC and an abuse registry screen pursuant to NMSA 1978,
Section 27-7a-1 et seq. and 8.11.6 NMAC;
▪ Complete training on critical incident, abuse, neglect, and exploitation reporting;
▪ Complete member specific training; the evaluation of training needs is determined by the
member or his/her legal representative; member is also responsible for providing and
arranging for provider training and supervising provider performance; training expenses for
paid providers cannot be paid for with the member’s annual budget; and
▪ Meet any other service qualifications, as specified in the SDCB rules.
• Ensure job developers have the following qualifications:
o Be at least 18 years of age;
o Experience as a job developer for at least one year;
o Experience for at least one year developing and using job task and analyses;
o Experience for at least one year working with the DVR, an independent living center or
organization that provides Employment Supports or services for people with disabilities; and

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
242 | P a g e
o Trained on the purposes, functions and general practices entities such as:
▪ DWS Navigators;
▪ One-Stop Career Centers;
▪ BLN;
▪ Chamber of Commerce;
▪ JAN;
▪ Small Business Development Centers;
▪ Retired Executives;
▪ New Mexico employment institute;
▪ Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section
29-17-2 et seq. and 7.1.9 NMAC and an abuse registry screen pursuant to NMSA 1978,
Section 27-7;
▪ a-1 et seq. and 8.11.6 NMAC;
▪ Complete training on critical incident, abuse, neglect, and exploitation reporting;
▪ Complete SDCB member specific training; the evaluation of training needs is determined by
the SDCB member or his/her legal representative; SDCB member is also responsible for
providing and arranging for provider training and supervising provider performance; training
expenses for paid SDCB providers cannot be paid for with the SDCB member’s annual
budget; and
▪ Meet any other service qualifications, as specified in the SDCB rules.
Environmental modification
• Definition of Service:
Environmental modification services include the purchase and/or installation of equipment and/or
making physical adaptations to a SDCB member's residence that are necessary to ensure the health,
welfare, and safety of the SDCB member or enhance the SDCB member’s level of independence. All
approved services shall be provided in accordance with applicable Federal, State, and local building
codes.
The environmental modification provider must ensure proper design criteria is addressed in the
planning and design of the adaptation, provide or secure licensed contractor(s) or approved
vendor(s) to provide construction services, provide administrative and technical oversight of

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
243 | P a g e
construction projects, provide consultation to family members, providers and contractors
concerning environmental modification projects to the SDCB member's residence, and inspect the
final environmental modification project to ensure that the adaptations meet the approved plan
submitted to the SDCB member’s Care Coordinator for environmental adaptation.
Environmental modifications are managed by professional staff available to provide technical
assistance and oversight to environmental modification projects. All services shall be provided in
accordance with applicable Federal, State, and local building codes.
• Scope of Services:
o Environmental adaptations include the following:
▪ Installation of ramps and grab-bars;
▪ Widening of doorways/hallways;
▪ Installation of specialized electric and plumbing systems to accommodate medical
equipment and supplies;
▪ Installation of lifts/elevators;
▪ Modification of bathroom facilities (roll-in showers, sink, bathtub, and toilet modifications,
water faucet controls, floor urinals, and bidet adaptations and plumbing);
▪ Turnaround space adaptations;
▪ Installation of specialized accessibility/safety adaptations/additions;
▪ Installation of Trapeze and mobility tracks for home ceilings;
▪ Installation of Automatic door openers/doorbells;
▪ Installation of Voice-activated, light-activated, motion- activated and electronic devices;
▪ Installation of Fire safety adaptations;
▪ Installation of Air filtering devices;
▪ Installation of heating/cooling adaptations;
▪ Installation of glass substitute for windows and doors;
▪ Installation of modified switches, outlets or environmental controls for home devices; and
▪ Installation of alarm and alert systems, emergency response systems, and/or signaling
devices.
o Environmental modification Qualifications – Individual Contractor and Agency Contractor:
▪ Current business license;
▪ Appropriate plumbing, electrician, contractor license; and/or

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
244 | P a g e
▪ Appropriate technical certification or other license to perform the modification.
o The environmental modification provider must:
▪ Provide a one-year warranty from the completion date on all parts and labor;
▪ Have a working knowledge of environmental modifications and be familiar with the needs of
persons with functional limitations in relation to environmental modifications;
▪ Provide consultation to family members, providers and MCOs concerning environmental
modification projects to the SDCB member’s individual’s residence, and inspect the final
environmental modification project prior to the member/EOR requesting the final payment
to ensure that the adaptations meet the approved plan as submitted and approved for
environmental adaptation; and
▪ Provider must establish and maintain financial reporting and accounting for each member.
o The environmental modification provider will submit the environmental modification Service
Cost Quote Packet containing the following information and documentation to the MCO:
▪ Environmental modification evaluation;
▪ Service Cost Estimate;
▪ Photographs of the proposed modifications;
▪ The estimated start date of the work on the proposed modification; (equipment, materials,
supplies, labor, travel, per diem, report writing time, and completion date of modification);
▪ Letter of Acceptance of Service Cost Estimate signed by the SDCB member/EOR;
▪ Letter of Permission from property owner. If the property owner is someone other than the
member, the letter must be signed by the property owner and the member;
▪ The Construction Letter of Understanding. If the property owner is someone other than the
member, the letter must be signed by the property owner and the member; and
▪ Documentation demonstrating compliance with the ADA.
o The environmental modification provider must submit the following to the MCO, after the
completion of work:
▪ Letter of Approval of Work completed signed by the SDCB member/EOR; and
▪ Photographs of the completed modifications.
o The MCO must submit a Care Coordinator Individual Assessment of Need to the provider.
o Reimbursement:

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
245 | P a g e
Environmental modification providers must maintain appropriate record keeping of services
provided, and fiscal accountability as indicated in the Medicaid PPA. Billing is on a project basis,
one unit per environmental modification project. Reimbursement for environmental
modification services will be based on the negotiated rate with the SDCB member/EOR;
Environmental modification services are limited to $5,000.00 every five years, beginning from
the first date of service. Additional services may be requested if the member’s health and safety
needs exceed the specified limit. The $5,000.00, five-year time limit applies across all CB
packages where environmental modifications are a covered service. Example: an ABCB member
receives an environmental modification of $2,300.00 leaving a $2,700.00 available balance for
future environmental modification. Six months later the ABCB member transitions to the SDCB,
the member now has $2,700.00 available for environmental modifications; and
Environmental modifications exclude those adaptations or improvements to the home that are
of general utility and are not of direct medical or remedial benefit to the member, such as
carpeting, fences, roof repair, storage sheds or other outbuildings, furnace replacement,
insulation, and other general household repairs. Adaptations that add to the total square
footage of the home are also excluded from this benefit except when necessary to complete an
adaptation related to the member’s medical condition.
Home Health Aide
• Definition of Service:
HH Aide services provide total care or assist a member in all activities of daily living. HH Aide
services assist the member in a manner that will promote and improve the member’s quality of life
and provide a safe environment for the member. HH aide services can be provided outside the
member’s home;
State plan HH Aide services are intermittent and are provided primarily on a short-term basis;
whereas, in SDCB, HH Aide services are hourly services for members who need this service on a
long-term basis; and
HH Aides may provide basic non-invasive nursing assistant skills within the scope of their practice.
HH Aides do not administer medication(s), adjust oxygen levels, perform any intravenous
procedures or perform sterile procedures. HH Aide services are not duplicative of self-directed PCS.
• Scope of Services:

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
246 | P a g e
o Provide personal hygiene (e.g. sponge bathing, showering, bed shampooing, shaving, oral
hygiene dressing);
o While under the supervision of a licensed physical therapist or licensed nurse (RN or LPN), assist
with ambulation, transfer and range of motion exercises;
o Assist with menu planning, meal/snack preparation and assist member with eating as necessary;
o As ordered by a physician and under supervision of a licensed nurse (RN or LPN), he/she will
assist with bowel and bladder elimination with activities such as: catheter care, colostomy care,
enemas, insertion of non-prescribed suppository, prosthesis care and vital signs;
o Provide homemaking services (e.g. laundry, linen change, cleaning);
o Pick up medication(s);
o Assist or prompt member in self-administration of medication(s);
o Observe general condition of member and report changes to supervisor;
o Document SDCB member’s status and services furnished, infection control procedures; and
o Recognize emergencies and adhere to emergency procedures.
• HH Aide Qualifications – Agency Provider:
o Licensed in New Mexico as an HH agency, RHC or FQHC;
o Possess current business license;
o Meet financial solvency;
o Adhere to training requirements;
o Maintain individual records for each SDCB member within HIPAA compliance;
o Develop and adhere to records management policy;
o Develop and adhere to QA policies and processes;
o Supervision must be performed by an RN. Such supervision must occur at least once every 60
calendar days in the member's home and shall be in accordance with the New Mexico Nurse
Practice Act and be specific to the member's SDCB care plan. Contact must be made with family
members during supervision; and
o Ensure all assigned staff meets the following qualifications:
▪ Be at least 18 years of age;
▪ Be qualified to perform the service and demonstrate capacity to perform required tasks;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
247 | P a g e
▪ Have successfully completed a HH aide training program, as described in 42 CFR 484.36(a)(1)
and (2); or have successfully completed a HH aide training program pursuant to 7.28.2.30
NMAC. Copies of CNA certificates must be maintained in the personnel file of the HH aide;
▪ Be able to communicate successfully with the member;
▪ Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section
29-17-2 et seq. and 7.1.9 NMAC and an abuse registry screen pursuant to NMSA 1978,
Section 27-7a-1 et seq. and 8.11.6 NMAC;
▪ Complete training on critical incident, abuse, neglect, and exploitation reporting; and
▪ Meet any other service qualifications, as specified in the SDCB rules.
Nutritional Counseling
• Definition of Service:
o Nutritional Counseling services are designed to meet the unique food and nutritional needs of
SDCB members. This does not include oral-motor skill development services, such as those
provided by a speech pathologist.
• Scope of Services:
o Assessment of nutritional needs;
o Development and/or revision of the SDCB member’s nutritional plan; and
o Counseling and nutritional intervention and observation and technical assistance related to
implementation of the nutritional plan.
• Nutritional Counseling Qualifications - Individual Provider:
o Be licensed per the New Mexico Regulation and Licensing Department; Nutrition and Dietetics
Practice Act, NMSA 1978, Section 61-7A et. seq.
• Nutritional Counseling Qualifications - Agency Provider:
o Current business license; and provide a tax identification number;
o Rendering providers are Licensed per the New Mexico Regulation and Licensing Department;
Nutrition and Dietetics Practice Act, NMSA 1978, Section 61-7A et. seq.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
248 | P a g e
Private Duty Nursing for Adults
• Definition of Service:
o Private duty nursing for adult services includes activities, procedures, and treatment for a
member’s physical condition, physical illness or chronic disability. Children (individuals under
the age of 21) receive this service through the State plan EPSDT.
• Scope of Services:
o Private duty nursing services for adults may include performance, assistance and education with
the following tasks:
▪ Medication management, administration and teaching;
▪ Aspiration precautions;
▪ Feeding tube management, gastrostomy and jejunostomy;
▪ Skin care;
▪ Weight management;
▪ Urinary catheter management;
▪ Bowel and bladder care; wound care; health education and screening;
▪ Infection control;
▪ Environmental management for safety;
▪ Nutrition management;
▪ Oxygen management;
▪ Seizure management and precautions;
▪ Anxiety reduction;
▪ Staff supervision; and
▪ Behavior and self-care assistance.
o Private Duty Nursing Qualifications – Agency:
▪ Licensed in New Mexico as a HH Agency, RHC or FQHC agency;
▪ Possess current business license;
▪ Meet financial solvency;
▪ Adhere to training requirements;
▪ Maintain individual records for each member within HIPAA compliance;
▪ Develop and adhere to a records management policy;
▪ Develop and adhere to QA policies and processes;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
249 | P a g e
▪ Ensure all assigned staff meet the following qualifications;
▪ Licensed by the New Mexico State Board of Nursing as a RN or LPN;
▪ Demonstrate capacity to perform required tasks;
▪ Be able to communicate successfully with the member;
▪ Complete training on critical incident, abuse, neglect, and exploitation reporting;
▪ Individual RN/LPN providers must be licensed by the New Mexico State board of nursing as
an RN or LPN; and
▪ Meet any other service qualifications, as specified in the SDCB rules.
o Private Duty Nursing Qualifications – Individual:
▪ Provide a tax identification number;
▪ Individual RN/LPN providers must be licensed by the New Mexico State Board of Nursing as
an RN or LPN;
▪ Demonstrate capacity to perform required tasks;
▪ Be able to communicate successfully with the SDCB member;
▪ Complete training on critical incident, abuse, neglect, and exploitation reporting; and
▪ Meet any other service qualifications, as specified in the SDCB rules.
Related Goods
• Definition of Service:
Related Goods are services, goods, and equipment, including supplies, fees or memberships (such as
for conferences or classes), which support the SDCB member to remain in the community, decrease
the need for other Medicaid services and reduce the risk for institutionalization. Related goods must
promote personal safety and health, accommodate the SDCB member in managing his/her
household and/or facilitate ADLs. The related goods must not be available through another source
including the Medicaid State Plan and/or Medicare, and the SDCB member must not have the
personal funds needed to purchase the goods; and
Related goods must be documented in the SDCB care plan in a manner that clearly describes how
the related good will advance the desired outcomes in the SDCB member’s care plan. Related goods
must be linked to the SDCB member’s identified needs and are intended for the sole use of the SDCB
member, and one caregiver, if appropriate. All related goods must be approved by the MCO/UR. The
cost and type of related good is subject to approval by the MCO/UR. SDCB members are not

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
250 | P a g e
guaranteed the exact type and model of related good that is requested. The Support Broker and/or
the Care Coordinator can work with the SDCB member to find other (including less costly)
alternatives. Items that are purchased with SDCB funds cannot be returned for store credit, cash or
gift cards. Experimental or prohibited treatments and related goods are excluded. For members who
enter the SDCB program after January 1, 2019, related goods are limited to a total maximum of
$2,000.00 annually.
• Scope of Services:
Related goods must address a specific, assessed need identified in the member’s CNA (including
improving and maintaining the member’s opportunities for full membership in the community) and
must directly relate to the member’s qualifying condition or disability. Related goods must explicitly
address the member’s clinical, functional, medical or habilitative needs;
Related goods must meet all of the following requirements:
o Are related to a need or goal identified in the approved care plan;
o Are for the purpose of increasing independence or substituting for human assistance, to the
extent the expenditures would otherwise be made for that human assistance;
o Promote opportunities for community living and inclusion;
o Are able to be accommodated within the member’s budget without compromising the
member’s health or safety; and
o Are provided to, or directed exclusively toward, the benefit of the member.
Medicaid does not pay for the purchase of related goods or services that a household not including
a person with a disability would be expected to pay for as a routine household or personal expense.
Examples include, but are not limited to:
o Goods or services that are considered primarily recreational or diversional;
o Cell phones and cell phone service for members who are minors (these are items that LRI such
as a parent/guardian, or spouse would ordinarily purchase for household members of the same
age who do not have a disability or chronic illness);
o Cell phone services including fees for data and GPS in excess of $100.00 per month or more than
one cell phone per SDCB member;
o Cell phone services that include more than one cell phone or cell phone line per member; cell
phone service, including data, is limited to the cost of $100.00 per month;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
251 | P a g e
o Room and board, meaning shelter expenses (including property-related costs such as home and
property maintenance, insurance policies, utilities and all deposits; and all food items other than
nutritional supplements as approved in the SDCB care plan);
o Purchase of usual and customary furniture/home furnishings,
o Regularly scheduled upkeep, maintenance and repairs of a home, addition of fences, insulation,
construction of storage sheds or other outbuildings, except upkeep and maintenance of
modifications or alterations to a home which are an accommodation directly related to the
member’s qualifying condition or disability;
o Regularly scheduled upkeep, maintenance and repairs of a vehicle or van, or tire purchase or
replacement, except upkeep and maintenance of modifications or alterations to a vehicle or
van, which is an accommodation directly related to the member’s qualifying condition or
disability.
o Purchase, lease, or rental of a vehicle, including recreational vehicles;
o Memberships/fees related to religious activities/events;
o Purchase of animals and the costs of maintaining animals, including the purchase of food,
veterinary visits, grooming and boarding but with the exception of training and certification for
service dogs;
o Purchase of insurance policies, such as automobile, health, life, burial, renter’s, home-owner,
service warrantees or other such policies, including the purchase of cell phone insurance;
o Personal goods or items not related to the member’s qualifying condition or disability, including
clothing and personal hygiene products and accessories;
o Moving expenses including but not limited to the cost of moving truck rental, gas/mileage,
labor, storage, moving equipment and supplies;
o Vacation expenses, including means of transport, guided tours, meals, tips, lodging or similar
recreational expenses including fuel, mileage or driver time reimbursement for vacation travel
by an automobile;
o Costs associated with conferences or classes, including airfare, lodging, mileage/gas, or meals;
o Training expenses for employees;
o Professional housecleaning or yard maintenance;
o Formal academic degrees or certification-seeking education, educational services covered by
IDEA, or vocational training provided by the public education department, DVR; and

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
252 | P a g e
o For electronics such as cell phones, computers (including desktop, laptop, and tablets),
monitors, printers and fax machines, copiers, and other electronic equipment, no more than
one of each type of item may be purchased at one time, and member electronics may not be
replaced more frequently than once every three years.
• Related Goods Qualifications - Vendor Agency Provider:
o Valid tax identification for the state and Federal governments.
Respite
• Definition of Service:
o Respite is to be used to give the primary caregiver a break on an episodic basis in the event of an
emergency or to prevent burnout. Respite provides a temporary relief to the primary caregiver
of a SDCB member during times when the caregiver would normally provide unpaid care.
Respite services can be provided in the SDCB member’s home, the provider’s home, in
community setting of the family’s choice (e.g., community center, swimming pool and park, or
at a center in which other individuals are provided care); and
o Respite services may be provided by eligible individual respite providers; RN or LPN; or respite
provider agencies.
• Scope of Services:
Respite services include, but are not limited to the following:
o For members meeting NF LOC, respite services are limited to a maximum of 300 hours annually
per care plan year provided there is a primary caregiver. The 300-hour respite service applies
across all CB packages where respite is a covered service. Additional hours may be requested if
an eligible beneficiary’s health and safety needs exceed the specified limit;
o Assist with routine ADLs;
o Enhance self-help skills, leisure time skills and community and social awareness;
o Provide opportunities for leisure, play and other recreational activities;
o Provide opportunities for community and neighborhood integration and involvement;
o Provide opportunities for the SDCB member to make his/her own choices with regards to daily
activities;
o Respite services do not include the cost of room and board;
o Cannot be used for purposes of day-care;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
253 | P a g e
o Cannot be provided to school age children during school hours; and
o Respite must be documented through the EVV system.
• Respite Qualifications – Individual Provider:
o Be at least 18 years of age;
o Be qualified to perform the service and demonstrate capacity to perform required tasks;
o Be able to communicate successfully with the SDCB member;
o Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section 29-17-2
et seq. and 7.1.9 NMAC and an abuse registry screen pursuant to NMSA 1978, Section 27-7a-1
et seq. and 8.11.6 NMAC;
o Complete training on critical incident, abuse, neglect, and exploitation reporting;
o Complete member specific training; the evaluation of training needs is determined by the
member or his/her legal representative; member is also responsible for providing and arranging
for provider training and supervising provider performance; training expenses for paid providers
cannot be paid for with the SDCB member’s annual budget;
o Meet any other service qualifications, as specified in the SDCB rules and the Manual; and
o Individual RN/LPN providers must be licensed by the New Mexico State Board of Nursing as an
RN or LPN.
• Respite Qualifications - Provider Agency:
o Possess a current business license, if applicable;
o Meet financial solvency;
o Adhere to training requirements;
o Maintain individual records for each SDCB member within HIPAA compliance;
o Develop and adhere to a records management policy;
o Develop and adhere to QA rules and requirements; and
o Ensure all assigned staff meet the following qualifications:
▪ Be at least 18 years of age;
▪ Be qualified to perform the service and demonstrate capacity to perform required tasks;
▪ Be able to communicate successfully with the SDCB member;
▪ Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section
29-17-2 et seq. and 7.1.9 NMAC and an abuse registry screen pursuant to NMSA 1978,
Section 27-7a-1 et seq. and 8.11.6 NMAC;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
254 | P a g e
▪ Complete training on critical incident, abuse, neglect, and exploitation reporting;
▪ Complete SDCB member specific training; the evaluation of training needs is determined by
the SDCB member or his/her legal representative; member is also responsible for providing
and arranging for provider training and supervising provider performance; training expenses
for paid providers cannot be paid for with the SDCB member’s SDCB annual budget;
▪ Individual RN/LPN providers must be licensed by the New Mexico State Board of Nursing as
an RN or LPN; and
▪ Meet any other service qualifications, as specified in the SDCB rules and the Manual.
Self-Directed Personal Care
• Definition of Service:
Self-directed PCS are provided on a continuing basis to assist the member with accomplishing tasks
he/she would normally do for him/herself if he/she did not have a disability. Self-directed PCS are
provided in the member’s home and in the community, depending on the member’s needs. The
member/EOR identifies the self-directed personal care worker’s training needs. If the SDCB
member/EOR is unable to do the training him/herself, the SDCB member/EOR arranges for the
needed training;
Services are not intended to replace supports available from a primary caregiver or natural supports.
Although a member’s assessment for the amount and types of services may vary, Self-directed PCS
are not provided 24 hours a day. Allocation of time and services must be directly related to an
individual’s functional level to perform ADLs and IADLs as indicated in the CNA; and this service is
not available for members under age 21 because PCS are covered under the Medicaid State Plan as
expanded EPSDT benefits for members under age 21.
• Scope of Services:
o Self-directed PCS include but are not limited to the following:
▪ Assist the member with ADLs;
▪ Perform general household tasks, not including services such as yard maintenance;
▪ Provide companionship to acquire, maintain or improve social interaction skills in the
community; and
▪ Attend trainings as designated by the member in the care plan.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
255 | P a g e
o Self-Directed Personal Care Qualifications – Individual Provider:
▪ Be at least 18 years of age;
▪ Be qualified to perform the service and demonstrate capacity to perform required tasks;
▪ Be able to communicate successfully with the member;
▪ Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section
29-17-2 et seq. and 7.1.9 NMAC and an abuse registry screen pursuant to NMSA 1978,
Section 27-7a-1 et seq. and 8.11.6 NMAC and the National Sex Offender Registry;
▪ Complete training on critical incident, abuse, neglect, and exploitation reporting;
▪ Complete member specific training; the evaluation of training needs is determined by the
member or his/her legal representative; member is also responsible for providing and
arranging for provider training and supervising provider performance; training expenses for
paid providers cannot be paid for with the member’s annual budget;
▪ Use the State-approved EVV system to record location of services and time worked; and
▪ Meet any other service qualifications, as specified in the SDCB rules.
o Self-Directed Personal Care Qualifications – Agency Provider:
▪ HHAs must hold an HHA license;
▪ Possess a current business license, if applicable;
▪ Meet financial solvency;
▪ Adhere to training requirements;
▪ Maintain individual records for each SDCB member within HIPAA compliance;
▪ Develop and adhere to a records management policy;
▪ Develop and adhere to QA rules and requirements; and
▪ Ensure all assigned staff meet the following qualifications:
• Be at least 18 years of age;
• Be qualified to perform the service and demonstrate capacity to perform required tasks;
• Be able to communicate successfully with the member;
• Pass a nationwide caregiver criminal history screening pursuant to NMSA 1978, Section
29-17-2 et seq. and 7.1.9 NMAC and an abuse registry screening pursuant to NMSA
1978, Section 27-7a-1 et seq. and 8.11.6 NMAC and the National Sex Offender Registry;
• Complete training on critical incident, abuse, neglect, and exploitation reporting;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
256 | P a g e
• Complete member specific training; the evaluation of training needs is determined by
the member or his/her legal representative; member is also responsible for providing
and arranging for employee training and supervising employee performance; training
expenses for paid employees cannot be paid for with the member’s annual budget;
▪ Ensure employees use the State-approved EVV system to record location of services and
time worked; and
• Meet any other service qualifications, as specified in the SDCB rules and the Manual.
Skilled Maintenance Therapies Services
• Definition of Service:
Skilled maintenance therapies are provided when Medicaid State Plan skilled therapy services are
exhausted. Adult members in SDCB access therapy services under the Medicaid State Plan for acute
and temporary conditions that are expected to improve significantly in a reasonable and generally
predictable period of time. A signed therapy referral for treatment must be obtained from the
member’s PCP. The referral will include frequency, estimated duration of therapy, and
treatment/procedures to be rendered. Therapy services provided to adults in SDCB are to focus on
health maintenance, improving functional independence, community integration, socialization,
exercise or to enhance supports and normalization of family relationships.
o PT is the diagnosis and management of movement dysfunction and the enhancement of physical
and functional abilities;
o OT is the diagnosis, assessment and management of functional limitations intended to assist
adults to regain, maintain, develop and build skills that are important for independence,
functioning and health; and
o SLT services preserve speech fluency, voice, verbal, written language, auditory comprehension,
cognition, swallowing dysfunction, oral pharyngeal or laryngeal and sensor motor competencies.
Speech language pathology is also used when a SDCB member requires the use of an
augmentative communication device. Based upon therapy goals, services may be delivered in an
integrated natural setting, clinical setting or in a group.
• Scope of Services
o PT:
• Diagnostic activities to determine the dysfunction of physical and functional activities;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
257 | P a g e
• Activities to increase, maintain or reduce the loss of functional skills;
• Treat specific condition(s) clinically related to a member’s qualifying condition or
disability;
• Activities to support the member’s health and safety needs; and
• Identify, implement and train on therapeutic strategies to support the member, family
and/or staff in the home setting or other environments as addressed in the SDCB care
plan.
o OT:
• Diagnostic activities to determine skills assessment and treatment;
• Write treatment program to improve one’s ability to perform daily tasks;
• Comprehensive home, employment and/or volunteer sites evaluations with adaptation
recommendations;
• Provide guidance to family members and caregivers;
• Make assistive technology recommendations and provide usage training for members,
family and staff; and
• Identify, implement and train on therapeutic strategies to support the SDCB member,
family and/or staff in the home setting or other environments as addressed in the SDCB
care plan.
o Speech and Language Pathology:
• Improve or maintain the member’s capacity for successful communication or to lessen
the effects of the member’s loss of communication skills;
• Consultation on usage and training on augmentative communication devices;
• Activities to improve or maintain the member’s ability to eat food, drink liquid and
manage oral secretions with minimal risk of aspiration or other injuries or illness related
to swallowing disorders; and
• Activities to identify, implement, and train on therapeutic strategies to support the
member, his/her family and/or staff consistent with the member’s Care Plan.
o Therapy Qualifications – Individual Therapist Provider:
• Provide a tax identification number; and
• Maintain a case file within HIPAA guidelines for the member to include:

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
258 | P a g e
o Member’s SDCB care plan;
o Reports as requested in the care plan;
o Contact notes;
o Training roster(s); and
o Assessments for environmental modification requests.
▪ Licensures:
• Physical therapists will be licensed as per the New Mexico Regulation and Licensing
Department; Physical Therapy Act NMSA 1978, Section 61-12-1.1 et. seq;
• Occupational therapists will be licensed as per the New Mexico Regulation and Licensing
Department; Occupational Therapy Act NMSA 1978, Section 61-12A- 1et.seq.; and
• Speech and Language Pathologists will be licensed as per the New Mexico Regulation
and Licensing Department; Occupational Therapy Act NMSA 1978, Section
61-14B- 1et.seq.
o Therapy Qualifications – Provider Agency:
• Current business license;
• Provide tax identification number;
• Ensure physical therapists maintain a case file within HIPAA guidelines for the member
to include:
o Member’s SDCB care plan;
o Reports as requested in the SDCB care plan;
o Contact notes;
o Training roster(s); and
o Environmental modification requests.
• Ensure therapists has appropriate license for service:
o Physical therapists will be licensed as per the New Mexico Regulation and Licensing
Department; Physical Therapy Act NMSA 1978, Section 61-12-1.1 et. seq.;
o Occupational therapists will be licensed as per the New Mexico Regulation;
o Licensing Department; Occupational Therapy Act NMSA 1978, Section
61-12A- 1et.seq.; and

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
259 | P a g e
o Speech and Language Pathologists will be licensed as per the New Mexico
Regulation and Licensing Department; Occupational Therapy Act NMSA 1978,
Section 61-14B- 1et.seq.
Specialized Therapies Services
• Definition of Service:
Specialized therapies are non-experimental therapies or techniques that have been proven effective
for certain conditions. Services must be related to the member’s disability or condition and ensure
the member’s health and welfare in the community. The service will supplement to (not replace) the
member’s natural supports and other community services for which the member may be eligible.
Experimental or investigational procedures, technologies or therapies and those services covered in
Medicaid State Plans are excluded. For members who enter the SDCB program on or after January 1,
2019, specialized therapies are limited to a total maximum of $2,000.00 annually.
Only the specific specialized therapy services outlined below are covered through the SDCB.
• Scope of Services:
o Acupuncture is a distinct system of primary health care;
The goal of acupuncture is to prevent, cure or correct any disease, illness, injury, pain or other
physical or mental condition by controlling and regulating the flow and balance of energy, form
and function to restore and maintain PH and increased mental clarity. Acupuncture may provide
effective pain control, decreased symptoms of stress, improved circulation and a stronger
immune system, as well as other benefits. See Acupuncture and Oriental Medicine Practitioners
16.2.1 NMAC.
o Biofeedback uses visual, auditory or other monitors to provide SDCB members physiological
information of which they are normally unaware. This technique enables a member to learn
how to change physiological, psychological and behavioral responses for the purposes of
improving emotional, behavioral and cognitive health performance. Biofeedback may assist in
strengthening or gaining conscious control over the above processes in order to self-regulate.
Biofeedback is also useful for muscle re- education of specific muscle groups or for treating
pathological muscle abnormalities of spasticity, incapacitating muscle spasm or weakness;
o Chiropractic care is designed to locate and remove interference with the transmissions or
expression of nerve forces in the human body by the correction of misalignments or

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
260 | P a g e
subluxations of the vertebral column and pelvis. Chiropractic care restores and maintains health
for treatment of human disease primarily by, but not limited to adjustment and manipulation of
the human structure. Chiropractic therapy may positively affect neurological function, improve
certain reflexes and sensations, and increase range of motion and lead to improved general
health. See Chiropractic Practitioners 16.4.1 NMAC;
o Cognitive rehabilitation therapy is designed to improve cognitive functioning with the following
activities: reinforcing, strengthening, or re-establishing previously learned patterns of behavior;
establishing new patterns of cognitive activity; or compensatory mechanisms of impaired
neurological systems. Treatments may be focused on improving a particular cognitive domain
such as attention, memory, language, or executive functions. Alternatively, treatments may be
skill-based, aimed at improving performance of activities of daily living. The overall goal is to
restore function in a cognitive domain or set of domains or to teach compensatory strategies to
overcome specific cognitive problems;
o Hippotherapy is a physical, occupational and SLT treatment strategy that utilizes equine
movement as part of an integrated intervention program to achieve functional outcomes.
Hippotherapy applies multidimensional movement of a horse for members with movement
dysfunction and may increase mobility and rage of motion, decrease contractures and aid in
normalizing muscle tone. Hippotherapy requires that the member use cognitive functioning
especially for sequencing and memory. Members with attention deficits and behavior problems
are redirecting attention and behaviors by focusing on the activity. Hippotherapy involves
therapeutic exercise, neuromuscular education, kinetic activities, therapeutic activities, sensory
integration activities and individual speech therapy. The activities may also help improve
respiratory function and assist with improved breathing and speech production. Hippotherapy
must be performed by a physical therapist, occupational therapist, or speech therapist licensed
by the New Mexico Regulation and Licensing Department;
o Massage therapy is the assessment and treatment of soft tissues and their dysfunction for
therapeutic purposes primarily for comfort and relief of pain. It includes gliding, kneading,
percussion, compression, vibration, friction, nerve strokes, stretching the tissue and exercising
range of motion and may include the use of oils, salt glows, hot or cold packs or hydrotherapy.
Massage increases the circulation, helps loosen contracted, shortened muscles and can
stimulate weak muscles to improve posture and movement, improves range of motion and

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
261 | P a g e
reduces spasticity. Massage therapy may increase, or help sustain, a member’s ability to be
more independent in the performance of activities of daily living; thereby, decreasing
dependency upon others to perform or assist with basic daily activities. See Massage Therapists
16.7.1 NMAC;
o Naprapathy focuses on the evaluation and treatment of neuro-musculoskeletal conditions and is
a system for restoring functionality and reducing pain in muscles and joints. The therapy uses
manipulation and mobilization of the spine and joints and muscle treatments such as stretching
and massage. Based on the concept that constricted connective tissue (ligaments, muscles and
tendons) interfere with nerve, blood and lymph flow, Naprapathy uses manipulation of
connective tissue to open these channels of body function. See Naprapathic Practitioners 16.6.1
NMAC; and
o Native American healing therapies encompass a wide variety of culturally-appropriate therapies
that support members in their communities by addressing their physical, emotional and spiritual
health. Treatments may include prayer, dance, ceremony and song, plant medicines and foods,
participation in sweat lodges, and the use of meaningful symbols of healing, such as the
medicine wheel and/or other sacred objects.
• Specialized Therapy Qualifications – Individual Provider:
o Current New Mexico state license as applicable:
▪ Acupuncture and Oriental medicine license;
▪ Biofeedback – license in a healthcare profession whose scope of practice includes
biofeedback, and appropriate specialized training and clinical experience and supervision;
▪ Chiropractic Physician license;
▪ Cognitive rehabilitation therapy – license in a health care profession whose scope of
practice includes cognitive rehabilitation therapy, and appropriate specialized training and
clinical experience and supervision;
▪ Hippotherapy – licensed occupational therapist, physical therapist, or speech therapist;
▪ Massage therapy license; and
▪ Naprapathic physician license.
o Native American Healers – individuals who are recognized as healers within their communities.
This form of therapy may be provided by community-recognized medicine men and women and
others as healers, mentors and advisors to SDCB members.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
262 | P a g e
• Specialized Therapy Qualifications - Provider Agency:
o Current business license;
o Tax identification number; and
o Group practice/vendor staff must hold current New Mexico licensure and training in their
respective discipline as follows:
▪ Acupuncture and Oriental Medicine license;
▪ Biofeedback – license in a healthcare profession whose scope of practice includes
biofeedback, and appropriate specialized training and clinical experience and supervision;
▪ Chiropractic Physician license;
▪ Cognitive rehabilitation therapy – license in a health care profession whose scope of
practice includes cognitive rehabilitation therapy, and appropriate specialized training and
clinical experience and supervision;
▪ Hippotherapy – license in a health care profession whose scope of practice includes
Hippotherapy and appropriate specialized training and experience;
▪ Massage therapy license; and
▪ Naprapathic physician license.
Start-Up Goods
• Definition of Service:
Start-up goods are available to a member who is transitioning from the ABCB to the SDCB for the
first time. Start-up goods are limited to one time. Start-up goods help the member in self-directing
his or her services. Examples of start-up goods include, but are not limited to a computer, fax
machine, and printer. All start-up goods must be approved by the MCO. The cost and type of related
good is subject to approval by the MCO. Start-up goods must be purchased during the member’s
first budget period. Start-up goods are limited to $2,000.00.
Transportation (Non-Medical)
• Definition of Service:
Transportation services are offered in order to enable SDCB members to gain access to and from
community services, activities and resources, as specified by the SDCB care plan. Transportation
services are intended for access to the member’s local area, within a 75-mile radius of the SDCB
member’s home. Transportation services under SDCB are non-medical in nature, whereas

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
263 | P a g e
transportation services provided under the Medicaid State Plan are to transport members to
medically necessary physical and BH services. Transportation for the purpose of picking up
pharmacy prescriptions is allowed. Transportation for the purpose of vacation is not covered
through the SDCB;
Non-medical transportation services for minors is not a covered service;
Non-medical transportation may be reimbursed:
o To the driver by the mile; and/or
o Through the purchase of a bus pass or local taxi.
Payments are made to the member’s individual transportation employee or vendor or to a public or
private transportation service vendor. Payments cannot be made to the SDCB member. Whenever
possible, natural supports should provide this service without charge. For members who enter the
SDCB program on or after January 1, 2019, SDCB non-medical transportation is limited to a total
maximum of $1,000.00 annually.
• Scope of Services:
The service will be provided as specified in the member’s SDCB care plan. SDCB non-medical
transportation services cannot be used instead of, or to replace, medical transportation services
available under the Medicaid State Plan; and
Payment is allowable for transportation to and from specific locations/sites that provide specific
services that are approved in the member’s care plan goals.
• Transportation Qualifications - Individual Provider:
o Be at least 18 years of age;
o Possess a valid New Mexico driver’s license;
o Be free of physical or mental impairment that would adversely affect driving performance;
o No driving while intoxicated convictions within the previous two years;
o No chargeable (at fault) accidents within the previous two years;
o Have current CPR/First Aid certification;
o Complete training on critical incident, abuse, neglect, and exploitation reporting; and
o Possess and maintain current insurance policy and registration.
• Transportation Qualifications – Provider Agency:
o Current business license;
o Valid tax identification number;

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
264 | P a g e
o Have a current basic First Aid kit in the vehicle;
o Each vehicle will contain a current insurance policy and registration; and
o Ensure drivers meet individual qualifications:
▪ Be at least 18 years of age;
▪ Possess a valid New Mexico driver’s license;
▪ Be free of physical or mental impairment that would adversely affect driving performance
▪ No driving while intoxicated convictions within the previous two years;
▪ No chargeable (at fault) accidents within the previous two years;
▪ Have current CPR/First Aid certification;
▪ Complete training on critical incident, abuse, neglect, and exploitation reporting;
▪ Trained on New Mexico Department of Health Improvement (DHI) Critical Incident
Reporting and Procedures; and
▪ Possess current insurance policy and registration.
9.11. Self-Directed Non-Covered Services
When a member requests a non-covered service or good, the Support Broker and/or Care Coordinator
shall work with the member to find other (including less costly) alternatives. Services and goods that are
not covered by the SDCB program include, but are not limited to:
• The SDCB Program is the payer of last resort; and
• Any service or good, the provision of which would violate Federal or State statutes, rules or
guidance. This includes services that are recreational or diversional, which are not deemed eligible
SDCB services by CMS. Recreational and diversional in nature is defined as inherently and
characteristically related to activities done for enjoyment. This includes, but is not limited to tickets
for movies, theatrical and musical performances, sporting events, zoos or museums.
9.12. SDCB Budget and Care Plan Approval Process
The Care Coordinator adds the member to FOCoSonline when the member has expressed a desire to
transfer to SDCB by signing the SDCB statement. Once the member selects the Support Broker agency
he/she wishes to work with, the Care Coordinator informs the Support Broker agency of the selection.
After the Support Broker meets with the member and an anticipated transfer date is agreed upon, the

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
265 | P a g e
Support Broker creates a Working Plan shell with the anticipated SDCB care plan dates. Once the
Working Plan shell is created, the Care Coordinator shall enter the SDCB budget amount in FOCoSonline.
9.13. Initial SDCB Budget Determination Process
The SDCB budget is determined by the Care Coordinator and is based on two factors: the needs
identified in the CNA, and the amount and type of services the member has been receiving in the ABCB.
Both of these evaluations are used to assign the SDCB budget amount for development of the SDCB care
plan. The Care Coordinator shall provide the Support Broker with the SDCB budget amount.
The member must receive his/her HCBS in the ABCB for a minimum of 120 calendar days before
transferring to the SDCB. The initial 12-month SDCB budget shall be pro-rated based on the number of
months already completed in the ABCB. The SDCB member may request a new CNA if the SDCB member
thinks his/her needs were not adequately addressed in the initial CNA.
9.14. Initial SDCB Care Plan Approval Process
Once the Care Plan is developed, the Support Broker, in cooperation with the member, shall inform the
Care Coordinator that the Care Plan is ready for review. Once the Care Coordinator reviews the Care
Plan, the Care Coordinator shall formally submit the care plan in FOCoSonline to the MCO for review and
approval/denial decisions. The member’s Care Plan must be reviewed, and each individual requested
goal approved or denied by the MCO and written notification must be sent to the member before any
services may be utilized and related goods may be purchased. If, during the process of reviewing the
Care Plan and all subsequent Care Plan revisions, the MCO is unable to make a decision on a goal, due to
insufficient information, the MCO shall initiate an RFI via FOCoSonline. The MCO shall provide written
notification to the member and the Support Broker, specifying what is needed by the MCO to satisfy the
RFI. It is the member’s responsibility to provide a timely and complete response to the RFI. The Support
Broker/Care Coordinator may assist the member in obtaining the requested documents to fulfill the RFI.
The member/Support Broker must provide the RFI response to the Care Coordinator within 15 calendar
days from the date of the RFI letter. After review of the RFI response the Care Coordinator shall submit
the RFI response to the MCO for approval/denial decision. If the requested information is not received
by the Care Coordinator within 15 calendar days from the date of the RFI letter, the service or good shall
be denied by the MCO.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
266 | P a g e
If the Care Coordinator or MCO identify an administrative error on the submitted SDCB care plan a
“Request for Administrative Action” (RFA) shall be sent to the Support Broker. The RFA shall specify what
is needed to correct the administrative error. The Support Broker must respond to the RFA within five
calendar days from the date of the RFA notification. If the RFA is not addressed by the Support Broker or
Care Coordinator within five calendar days from the date of the RFA letter, the service or good shall be
denied by the MCO/UR
The MCO will notify the member, Care Coordinator, and Support Broker in writing when a determination
has been made on the Care Plan. The determination may be a full approval, a partial approval, or a full
denial. The MCO shall indicate which goal(s) of the Care Plan have been approved or denied in
FOCoSonline. Written notifications will include steps for the SDCB member/legal representative to
follow if the member disagrees with a denial decision.
The FMA will utilize the approved care plan/budget to process payment for the approved amount of
SDCB services and related goods.
The member’s Care Plan must be approved before SDCB services can begin. The MCO will not issue
payment for any services, supports and/or related goods which are provided or purchased prior to the
approval of the Care Plan, or before the provider is linked to the Care Plan.
At the earliest opportunity, the Care Plan and the NF LOC shall be aligned to start/end on the same day.
This may entail truncating the existing SDCB care plan to align with the annual NF LOC or truncating the
existing NF LOC to align with the annual SDCB care plan.
9.15. Annual SDCB Budget Determination and Approval Process
Approximately 90 calendar days prior to the expiration of the existing SDCB care plan/budget, the Care
Coordinator shall conduct the annual CNA. The Care Coordinator shall assign the budget based on the
assessed needs identified in the CNA. The budget is determined annually, and the budget amount may
differ from year to year. The budget shall not be higher than the cost of care for persons served in a
private NF, unless the member transitioned into SDCB with their prior approved self-directed budget.
Unused budget amounts from a previous year cannot be carried over to the new SDCB care plan year.
Approximately 90 days prior to the expiration of the existing care plan/budget, the Support Broker shall
open the new Working Plan shell in FOCoSonline, with the begin and end dates for the upcoming SDCB
Care Plan. Upon the annual SDCB budget determination, the Care Coordinator shall enter the SDCB

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
267 | P a g e
budget amount in FOCoSonline, allowing the member and Support Broker to begin developing the
upcoming year’s Care Plan.
9.16. Annual SDCB Care Plan Development and Approval Process
At a minimum, the Care Plan must be developed and submitted to the MCO for review annually, and no
less than 30 calendar days prior to the expiration of the existing care plan/budget. This 30 calendar day
timeframe allows enough time for the Care Coordinator and MCO to make an informed and accurate
determination of all requested services before the existing care plan/budget expires. The MCO will
notify the member, Care Coordinator, and Support Broker in writing when a determination has been
made on the Care Plan request. The determination may be a full approval, a partial approval, or a full
denial. The MCO shall indicate which goal(s) of the Care Plan have been approved or denied in
FOCoSonline and a letter shall be sent to the member including written instructions for the
member/legal representative to follow if the member disagrees with the denial decision(s).
9.17. SDCB Budget and Care Plan Approval Process for Individuals Who Transitioned from the MI VIA
Waiver Program
Prior to 1/1/2014, the Mi Via TPA approved many Mi Via employees/vendors at a reimbursement rate
which was above the maximum Mi Via rate for a particular Mi Via service. The higher reimbursement
rates are to continue to be approved in SDCB so long as the specific EOR and SDCB provider relationship
does not encounter a break in service. If, for any reason, the relationship ends and a new
employee/vendor is hired, the SDCB reimbursement rate for the new provider shall not exceed the
current approved SDCB range of rates (9.22.1) for any SDCB covered service. When the aforementioned
situation occurs, the budget may be reduced by the corresponding amount, if the SDCB member has no
other legitimate SDCB need(s).
Although Related Goods are not a covered service in ABCB, the need for “continuity of care” exists for
Related Goods. When redetermining the annual SDCB budget for SDCB members who transitioned from
the Mi Via waiver program, the MCO CC/UM shall allow the currently approved related good(s) and
previously approved reimbursement rate to be requested and approved, as deemed appropriate, for
each ongoing year of the SDCB care plan/budget.
At each annual assessment and budget determination, the Care Coordinator shall determine if the
member has underutilized his/her current SDCB care plan/budget. Underutilization is defined as using

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
268 | P a g e
less than 75% of the total budget by the end of quarter three of the member’s current Care Plan year. If
underutilization has occurred, the Care Coordinator shall consider reducing the budget by an amount
which is no more than the approved total for the underutilized service for the upcoming care plan
year/budget. However, if underutilization is due to, for example, a temporary hospital admission, and if
the hospital admission had not occurred, the member would have utilized SDCB services as requested
and approved, the Care Coordinator may not adjust the budget for the upcoming care plan year/budget.
If overutilization of the Care Plan/budget is identified at any time during the care plan/budget year, the
MCO shall not increase the current budget and level of services without identifying the need for a new
CNA, and determining whether all other available resources have been exhausted. Overutilization is
defined as using more than: 1) 50% of the budget by the end of quarter two of the member’s current
care plan year; 2) 75% of the budget by the end of quarter three of the member’s current care plan year;
or 3) 100% of the budget by the end of quarter four of the member’s current Care Plan year.
Underutilization and overutilization of the budget may result in an involuntary termination from the
SDCB to ABCB depending on the situation; please refer to the SDCB involuntary termination policy.
9.18. Denials, Revisions and Reconsiderations of the SDCB Care Plan
• Denials:
The MCO shall send final decisions to the member in writing, including steps for the member/legal
representative to follow if he/she disagrees with the denial decision and wants to pursue a
reconsideration and/or the MCO appeal process. The MCO appeal process must be exhausted prior
to the member requesting a State Fair Hearing.
• Revisions:
The Care Plan may be revised based upon a change in the member’s needs or circumstances
identified in the CNA, such as a change in the member’s health status or condition, or a change in
the member’s natural support system such as the death or disabling condition of a family member
or other individual who was providing services.
If the revision is to provide new or additional services other than those originally included in the
Care Plan, these services must not be able to be acquired through other programs or sources. The
member may be required to document the fact that the services are not available through another
source. The Care Coordinator and/or Support Broker shall assist the member with exploring other
available resources.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
269 | P a g e
The member must provide written documentation of the change in needs or circumstances as
specified in the Manual. The member submits the documentation to the Care Coordinator/Support
Broker. In FOCoSonline, the member or the member’s legal representative and the Support Broker
initiate the process to modify the Care Plan by developing a revision in FOCoSonline and forwarding
the completed request for a care plan revision to the Care Coordinator who will submit the revision
to the MCO/UR for review, via FOCoSonline. At the MCO’s discretion, another CNA may be
performed. Per the SDCB rule, if the revision includes a request for additional services, another CNA
must be performed to determine whether the change in needs or circumstances necessitate an
increase to the budget.
The Care Plan may be revised once the original care plan has been submitted and approved. Only
one Care Plan revision may be submitted at a time, for example, a Care Plan revision may not be
submitted if an initial Care Plan or prior Care Plan revision request is under initial review by the
MCO/UR.
Other than for critical health and safety reasons, Care Plan revision requests may not be submitted
to the MCO within the last 60 calendar days prior to the expiration date of the current Care Plan
/budget. This constraint does not apply to environmental modifications requests, as environmental
modification work is not tied to a specific care plan year and the funding is not part of the overall
SDCB budget amount.
Anytime a member exits SDCB and transfers to ABCB, another Medicaid waiver such as the DD
Waiver, or is permanently institutionalized, the Support Broker must develop a close-out budget to
coincide with the last day the member will receive SDCB services. The only time a close-out budget is
not needed is when a member’s Care Plan will expire in the same month as the member’s final
month in SDCB. The close-out budget must be reviewed/approved by the MCO.
• Reconsiderations:
If the Care Plan, or a part of the Care Plan, is not approved, the Care Coordinator and/or Support
Broker assists the member to explore his/her options, including the right to request a
reconsideration of the denial decision. Reconsideration requests must be submitted to the MCO
within 30 calendar days of the date on the denial notice. Reconsideration requests must be made by
the Support Broker through FOCoSonline and additional documentation or additional clarifying
information must be submitted in writing regarding the member’s request for reconsideration of the
denied services or related goods.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
270 | P a g e
9.19. SDCB Care Plan Review Criteria
Services and related goods identified in the member’s requested Care Plan may be considered for
approval if all the following requirements are met:
• The services or related goods must be responsive and directly related to the member’s qualifying
condition or disability;
• The services or related goods must address the member’s clinical, functional, medical or habilitative
needs;
• The services or related goods must accommodate the member in managing his/her household;
• The services or related goods must facilitate ADLs;
• The services or related goods must promote the member’s personal health and safety;
• The services or related goods must afford the member an accommodation for greater
independence;
• The services or related goods must support the member to remain in the community and reduce
his/her risk for institutionalization;
• The services or related goods must be documented in the member’s Care Plan and facilitate the
desired outcomes stated in the member’s Care Plan;
• The service or related good is not prohibited by Federal and State statutes, rules and guidance;
• Each service or good must be listed as an individual line item; when services or related goods must
be “bundled” the Care Plan must document why bundling is necessary and appropriate;
• The proposed Care Plan is within the member’s approved budget;
• The proposed rate for each service is within the SDCB range of rates (9.22.1) for that chosen service;
• The proposed cost for each good is reasonable, appropriate and reflects the lowest available cost for
that chosen good; and
• The estimated cost of the service or good is specifically documented in the member’s Care Plan.
9.20. Implementation of the SDCB Care Plan
• Enrolling SDCB Employees and Vendors:
o Pre-Hire Packet:
▪ Before providing services to a member, most employees and vendors are required to submit
the appropriate State-approved pre-hire packet to the FMA and pass the COR screening. The

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
271 | P a g e
exception to this requirement is when the vendor has a professional license, such as an RN
or Speech Language Pathologist (SLP) that qualifies them to provide the approved service.
The FMA is responsible for maintaining, distributing and processing the pre-hire packets. For
answers to questions about hiring employees or vendors and to obtain the pre-hire packet,
an EOR shall contact the FMA Help Desk at 1-866-916-0310;
▪ Potential SDCB employees are required by New Mexico law through the caregivers’ criminal
history screening act (7.1.9 NMAC) to pass a CBC which begins by screening against the COR.
This COR screening is completed by the FMA, usually within 48 hours, once the complete
and correct pre-hire packet is received by the FMA. Once the COR check is completed, and
the potential SDCB provider has passed the COR check, the EOR will receive an email
notification from the FMA that the potential SDCB employee has passed his/her COR and
CBC and may begin providing SDCB services. If the EOR does not have an email address
listed in FOCoSonline, the FMA Help Desk will contact the EOR, via telephone to let the EOR
know that the potential SDCB employee has passed the COR check. Although an employee
may begin providing services as soon as he/she has passed the COR Background Check,
payment will not be issued until all required paperwork as indicated below is successfully
completed and has been approved by the FMA. If a potential SDCB employee or vendor
does not pass the CBC, as required by New Mexico law, he/she may not continue to provide
services to the SDCB member. The potential SDCB employee or vendor and FMA will be
notified by the Department of Health if he/she does not pass the CBC. The FMA will notify
the SDCB member/EOR when a potential SDCB employee has or has not successfully
completed the COR check and/or CBC; and
▪ No SDCB provider shall exceed 40 hours paid work in one work week per EOR. If an
employee works for more than one EOR, the employee shall not exceed 40 hours paid work
in one work week, per EOR.
o Credentialing Requirements:
▪ The State has set credentialing requirements for credentialing providers of SDCB services,
and these requirements have been approved by CMS. The FMA shall ensure these
requirements are met. These requirements include certain licenses which must be
submitted by the potential SDCB provider to the FMA, and are described in 9.B & 9.C
(Vendor and Employee Credentialing Requirements). Services cannot be provided to a

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
272 | P a g e
member until the SDCB care plan is approved, and there is a credentialed and approved
provider linked to the approved SDCB goal.
o Other Required Documents:
▪ There are other documents that must be correctly completed by the potential SDCB
employee or vendor and submitted to the FMA for review and approval before payment can
be made. Potential SDCB employees and vendors may obtain these documents by
contacting the FMA. It is the member/EOR’s responsibility to ensure all employment
documents are submitted to the FMA.
For potential SDCB employees, the required documents are included in the Employee Packet:
• Employment Agreement;
• Employee Information Form;
• Declaration of Relationship Form;
• Federal W-4; and
• State W-4.
For potential SDCB vendors who are providing services the required documents are included as part of
the Vendor Packet:
• Vendor Agreement;
• Vendor Information Form; and
• Federal W-9.
Vendors who are providing SDCB related goods only (such as a large retailer) do not need to provide the
Vendor Agreement and Federal W-9, however the SDCB member/EOR or vendor must submit the
Vendor Information Form to the FMA before payment is issued.
Direct deposit is provided and strongly recommended for all employees and vendors when possible. The
FMA also offers the service of providing payment through a ComData Card. Please contact the FMA if
interested in using this service. Direct deposit forms can be completed as part of the initial hire
documentation or may be completed and submitted to the FMA at a later date.
• Purchasing Services and Related Goods:
o Timesheets:
▪ ASDCB employee (or EOR) must enter and approve the employee(s)’s timesheet(s) in
FOCoSonline unless he/she is approved for an exception to fax timesheets to the FMA. Upon

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
273 | P a g e
completing the FOCoSonline training, a new user will receive a FOCoSonline Account
Authorization form (via email). Once the new user completes the FOCoSonline Account
Authorization form and faxes it to the FMA Technical Department, the user will receive an
email with his/her password and login instructions;
▪ Timesheets are submitted and processed on a two-week pay schedule according to the
SDCB Payroll Payment Schedule. The payroll workweek starts on Saturday and ends the
following Friday. The payment schedule is available through the FMA and on the MCOs’
websites. Timesheets are due at the end of the two- week pay period and must be received
at the FMA no later than Saturday at 11:59 pm for a SDCB employee to be paid on time and
according to the payment schedule; and
▪ An AR may also complete the training and gain access to FOCoSonline. If an AR has access,
they will be able to view payments and monitor SDCB budget spending, however, the AR will
not have authorization to perform the functions of the EOR and approve timesheets. To
designate an AR, members must complete the AR form, which may be requested through
the FMA or the Support Broker.
▪ Self-Directed Personal Care and Respite providers must utilize the EVV system to clock-in
and out in order to generate a timesheet in FOCoSonline or other state approved system.
o Invoices:
▪ Vendor PRF and invoices may be submitted to the FMA on any day of the week (unlike
timesheets which must be submitted according to the payroll schedule). The processing
time for a PRF/invoice is approximately two weeks. The vendor payment schedule is
available through the FMA. Vendor checks are generated by TeleCheck and are mailed
directly to the EOR (payments are not mailed to the vendor). After the EOR receives the
vendor check, it is recommended that the EOR mail/deliver the check to the vendor as soon
as possible to ensure prompt payment. For phone/internet payments, the EOR must send
the payment to the phone/internet company’s main billing address (with the payment
coupon). It is not recommended that phone/internet payments be attempted through
kiosks or at local phone/internet stores (e.g., T-Mobile or Cricket) since these payments are
frequently rejected by TeleCheck. Uncashed checks may be voided by the FMA after six
months; and

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
274 | P a g e
▪ Although an EOR must submit timesheets online (after completing necessary FOCoSonline
training and paperwork), it is not possible to submit invoices online. PRFs and invoices must
be faxed or sent electronically to the FMA for processing. If a SDCB member/EOR has access
to FOCoSonline, he/she should review his/her payments and monitor them as they are being
processed. In addition, the SDCB member, EOR, or AR may run reports through FOCoSonline
to monitor spending activity.
o Return to Member (RTM) Process:
▪ RTM letters are an effective means used by the FMA to assist in communicating with the
EOR when there are problems in processing SDCB payment. For example, if a timesheet or
invoice is submitted to the FMA and it does not contain the appropriate signatures, the FMA
uses the RTM process to inform the EOR that payment cannot be made. In addition to the
RTM letter which is mailed, the FMA attempts contact with the EOR by phone. If three
unsuccessful phone call attempts to the EOR have been made and the corrected document
still has not been received, the FMA will send an email to the EOR (provided the EOR has an
email address in FOCoSonline) with a copy to the Care Coordinator and Support Broker. If
the EOR does not have an email address in FOCoSonline, the FMA will send an email to the
Care Coordinator and Support Broker and attach a copy of the RTM letter. Since frequent
contact is attempted by the FMA to the EOR, it is extremely important that FOCoSonline
contain the EOR’s correct contact information. If the EOR contact information needs to be
updated, please contact the FMA Help Desk for assistance.
o Employee and Vendor Pay Rates:
▪ Employee and vendor pay rates must be approved in the member’s care plan. Once the
SDCB rate is approved, completed employee agreements and vendor agreements must be
submitted to the FMA in order to indicate the rate of pay. If a potential SDCB employee or
vendor does not submit an employee or vendor agreement, as appropriate, the FMA will
not know the correct rate of pay for the service that the employee or vendor is providing. In
order for the FMA to pay a SDCB employee or vendor, a completed employee agreement or
vendor agreement needs to be submitted to, and approved by, the FMA and the
employee/vendor must be linked to the SDCB goal inside FOCoSonline. If the pay rate for an
approved SDCB employee or vendor needs to be changed, the new rate must be approved
by the MCO via a SDCB care plan revision in FOCoSonline and in the member’s SDCB care

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
275 | P a g e
plan and a new employee agreement or vendor agreement, signed by the EOR, must be
submitted to the FMA at least 15 calendar days before the effective date of the rate change.
If a change to a SDCB employee’s rate of pay is made after the SDCB care plan has started,
the change will not be effective until the beginning of the next pay period.
o Timely Filing Requirements:
▪ New Mexico has a 90 calendar day time limit for filing all Medicaid claims and since the
SDCB is a Medicaid benefit, the same requirements apply. If timesheets or invoices are
submitted more than 90 calendar days after the service has been provided, payment will not
be processed and the timesheet or invoice and PRF will be returned to the EOR/member
through the RTM process.
o SDCB Care Plan Expenditure Safeguards:
▪ The SDCB member holds the primary responsibility for monitoring and ensuring his/her
approved SDCB care plan is spent appropriately; however, the Care Coordinator and Support
Broker must support the SDCB member in this activity. The FMA also assists in ensuring that
funds are spent appropriately through payment of approved services and related goods
according to the approved SDCB care plan and Employee/Vendor Agreements;
▪ The member/EOR is responsible for reviewing his/her monthly spending report which is
available to each member/EOR by the FMA on a monthly basis. The SDCB member/EOR may
also obtain “real-time” information on service usage and spending by directly accessing
FOCoSonline. It is highly recommended that members/EORs obtain access to FOCoSonline so
that they can effectively monitor their care plan/budget and track spending. Monthly
training for FOCoSonline is offered for SDCB members, employees, and EORs. If interested in
training, the SDCB member, employee, or EOR should contact the FMA Help Desk for
assistance;
▪ The Support Broker is required to review the member’s SDCB care plan expenditures during
each quarterly face-to-face contact with the member. The Care Coordinator and/or Support
Broker will provide the member with expenditure information and discuss any concerns. If
the member needs to revise his/her SDCB care plan, the Support Broker shall assist with
drafting the revision and the Care Coordinator will submit it to the MCO/UR for
consideration per established procedures. The Care Coordinator may also initiate a new CNA
as needed; and

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
276 | P a g e
▪ The FMA is responsible for processing payments for approved SDCB services and related
goods. When an invoice or timesheet is received by the FMA, they verify that the particular
service or good is approved in the member’s SDCB Care Plan/budget and payment is
processed according to the approved SDCB Care Plan/budget and employee/vendor
agreement. In regards to internet and phone services (landline or cell), the FMA will pay up
to the approved monthly amount. This helps to ensure that this category of service is not
overspent which could put the member at-risk of losing these services due to possible
non-payment later in the SDCB Care Plan year. If the FMA is unable to make payment as
requested due to lack of funds remaining in the Care Plan, the FMA will send an RTM letter
to the member and make three attempts to contact the member by telephone to inform the
EOR/member of the insufficient funds issue.
9.21. Transitions, Terminations, and Reinstatement Processes
Upon initial eligibility for the CB, the member will be eligible for the ABCB. An ABCB member may choose
to move to SDCB at any time but may not move to SDCB until the first day of the month after 120
calendar days are completed in the ABCB. The member must utilize CB services in the ABCB prior to
transitioning to SDCB. If the member has a short-term admission to an NF, the 120 calendar days does
not start over. The member must always end the current CB model on the last day of the month and
start the new CB model on the first day of the following month. The Care Coordinator must ensure there
is no break in CB services during model switches. Examples of transition for members who enter an NF
include, but are not limited to, the following:
• The member only has a waiver COE (090, 091, 092, 093 or 094) and is institutionalized more than 60
days, the member must apply for IC and submit their name back on the Central Registry. They then
must receive a Community Reintegration allocation. If, when they are discharged, they still have
living arrangements in place, they are not required to complete the 120 days in ABCB again;
• If the member does not have living arrangements in place, the member must go back to ABCB
during the transition and is not mandated to complete another 120 days in ABCB. Meaning, the
member can begin self-directing after all living arrangements have been set up and the member is
successfully in that living arrangement and the SDCB budget, Care Plan and employees are approved
to provide SDCB-covered services; and

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
277 | P a g e
• If the member has a full Medicaid COE (001, 003, 004, etc.) and is institutionalized for more than 60
days and the member does not have living arrangements still in place, the member must go back to
ABCB during the transition and is not mandated to complete another 120 days. Meaning, the
member can begin self-directing after all living arrangement have been set up and the member is
successfully in that living arrangement and the SDCB budget, Care Plan and employees are approved
to provide SDCB-covered services.
Voluntary Termination
• SDCB members may transfer from the SDCB to the ABCB at any time. To the extent possible, the
SDCB member shall provide his/her SDCB provider(s) with 10 business days advance notice
regarding his/her intent to withdraw from the SDCB. All transfers will become effective on the 1st
day of the following month.
Involuntary Termination
• Reasons SDCB members may be involuntarily terminated from the SDCB and offered services
through the ABCB include, but are not limited to, the following circumstances:
o The SDCB member refuses to follow SDCB rules after receiving: focused technical assistance on
multiple occasions; and support from the program staff, Care Coordinator/Support Broker, or
FMA that is supported with documentation of the efforts to assist the SDCB member. Focused
technical assistance is defined as a minimum of three separate occasions where the member
/EOR have received training, education or technical assistance, or a combination of both;
o The SDCB member has immediate risk to his/her health or safety by continued self-direction of
services, e.g., the SDCB member is in imminent risk of death or serious bodily injury related to
participation in the SDCB. Examples include, but are not limited to, the following:
▪ The SDCB member refuses to include and maintain services in his/her SDCB Care Plan that
would address health and safety issues identified in the member’s CNA or challenges the
assessment after repeated and focused technical assistance and support from program
staff, Care Coordinator/Support Broker, or FMA;
▪ The SDCB member is experiencing significant health or safety needs, and, after having been
referred to the State contractor team (that includes the appropriate State program manager
and additional parties as deemed necessary by the State) for technical assistance, refuses to

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
278 | P a g e
incorporate the team’s recommendations into his/her SDCB Care Plan, or the SDCB member
exhibits behaviors which endanger him/her or others;
▪ The SDCB member misuses SDCB funds following repeated and focused technical assistance
and support from the Care Coordinator/Support Broker or FMA, which is supported by
documentation;
▪ The SDCB member expends his/her entire SDCB budget prior to the end of the SDCB Care
Plan year;
▪ The SDCB member commits Medicaid fraud such as, for example, altering SDCB
employee/vendor payment checks;
▪ The final decision to terminate a SDCB member and move him/her to ABCB is made by the
State. The MCO shall submit sufficient documentation to the State for approval of the
involuntary termination request. Upon State approval, the MCO shall notify the member of
the involuntary termination, in writing, and shall include appeal rights per HSD rules. The
MCO must transition the member to the ABCB with no break in services. The transition must
be completed within 90 calendar days of the date of HSD approval. SDCB involuntary
terminations may become effective any time during the month;
▪ Requests to be reinstated back to SDCB may be made one time during a 12-month period.
The member must make the request to his/her MCO in writing. All members shall be
required to participate in SDCB training prior to their reinstatement;
▪ A SDCB member who voluntarily terminated his/her participation in SDCB may request to
move back from ABCB to SDCB any time during a 12-year month period. The final decision to
allow the reinstatement to SDCB is at the discretion of the MCO. The Care Coordinator must
ensure the transition does not cause a break in services; and/or
▪ A SDCB member who was involuntarily terminated from SDCB may request to be reinstated
to SDCB once per 12-month period. The final decision to allow the reinstatement to SDCB is
at the discretion of the State. The MCO shall submit sufficient documentation to the State
for approval of reinstatement to the SDCB. If approved, the Care Coordinator shall work
with the FMA to ensure the issues previously identified as reasons for termination have
been adequately addressed prior to the reinstatement.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
279 | P a g e
9.22. Appendices
9.22.1 SDCB Range of Rates Chart
9.22.2 SDCB Vendor Credentialing Requirements
9.22.3 Employee Credentialing Requirements Grid
9.22.4 Vendor Toolkit
9.22.5 Employee Toolkit

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
280 | P a g e
9.22.1. SDCB Range of Rates Chart
SDCB Service
Billing
Code
Internal
Focos Code
Unit
SDCB Payment
Rate
Self-Directed Personal Care
99509
99509
Hour
minimum wage
- $14.60
HH Aide
S9122
S9122
Hour
$16.32
Employment Supports (includes Job Coach)
T2019
T2019
15 min.
$2.15 - $6.93
Job Developer (Per job that is developed for member)
T2019
T2019JD
Each
$100-$700
Customized Community Supports (adult day hab.)
S5100
S5100
15 min.
$1.36-$8.82
PT
G0151
G0151
15 min.
$13.51 - $24.22
OT
G0152
G0152
15 min.
$12.74 - $23.71
Speech/Language Pathology
G0153
G0153
15 min.
$16.06 - $24.22
Behavior Support Consultation
H2019
H2019
15 min.
$12.24 - $20.65
Private Duty Nursing – Adults- RN
T1002
T1002
15 min.
$10.90
Private Duty Nursing – Adults- LPN
T1003
T1003
15 min
$6.79
Nutritional Counseling
S9470
S9470
Hour
$42.83
Acupuncture
97810
97810
15 min.
$12.50-$25.00
Biofeedback
90901
90901
Visit
$50.00-$100.00
Chiropractic
98940
98940
Visit
$50.00-$100.00
Cognitive Rehabilitation Therapy
97532
97532
15 min.
$12.50-$25.00
Hippotherapy
S8940
S8940
Visit
$50.00-$100.00
Massage Therapy
97124
97124
15 min.
$12.50-$25.00
Naprapathy
S8990
S8990
Visit
$50.00-$100.00
Native American Healers
S9445
S9445
Session
As approved by MCO
Respite Standard (not provided by RN, LPN or HHA)
T1005
T1005SD
15 min.
$3.38
Respite RN
T1005
T1005RN
15 min.
$10.90
Respite LPN
T1005
T1005LPN
15 min.
$6.79
Respite HH Aide
T1005
T1005HHA
15 min.
$4.08
Emergency Response (monthly fee)
S5161
S5161
Each
$36.71-$40.79
Emergency Response (testing and maintenance)
S5160
S5160
Each
As approved by MCO

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
281 | P a g e
SDCB Service
Billing
Code
Internal
Focos Code
Unit
SDCB Payment
Rate
Environmental Modifications
S5165
S5165
Each
As approved by MCO
(maximum of $5,000
every 5 years)
Transportation Mile
T2049
T2049
Per Mile
$0.34-$.40
Transportation Commercial Carrier Pass
T2004
T2004
Each
As approved by MCO
Start Up-Goods Computer
T2028
T2028CR
Each
As approved by MCO
Start Up-Goods Fax Machine
T2028
T2028FX
Each
As approved by MCO
Start Up-Goods Internet Activation
T2028
T2028IA
Each
As approved by MCO
Start Up-Goods Landline Activation
T2028
T2028LA
Each
As approved by MCO
Start Up-Goods Office Supplies
T2028
T2028OS
Each
As approved by MCO
Start Up-Goods Printer
T2028
T2028PR
Each
As approved by MCO
Fees and Memberships
T1999
T1999CP-I
Each
As approved by MCO
Coaching/education for parents, spouse or others
(not available for paid caregivers)
T1999
T1999CE-I
Each
As approved by MCO
Coaching/education for parents, spouse or others
Classes only (not available for paid caregivers)
T1999
T1999CL-I
Each
As approved by MCO
Coaching/education for parents, spouse or others
Conferences and seminars (not available for paid
caregivers)
T1999
T1999CS-I
Each
As approved by MCO
Technology for Safety and Independence
T1999
T1999TS
Each
As approved by MCO
Cell phone service (including data/GPS)
T1999
T1999CELL
Each
$0.00-$100.00
Cell phone and related equipment
T1999
T1999CPEP
Each
As approved by MCO
Cell phone/landline
T1999
T1999CPL
Each
As approved by MCO
Internet service
T1999
T1999IS
Each
As approved by MCO
Landline service
T1999
T1999LS
Each
As approved by MCO
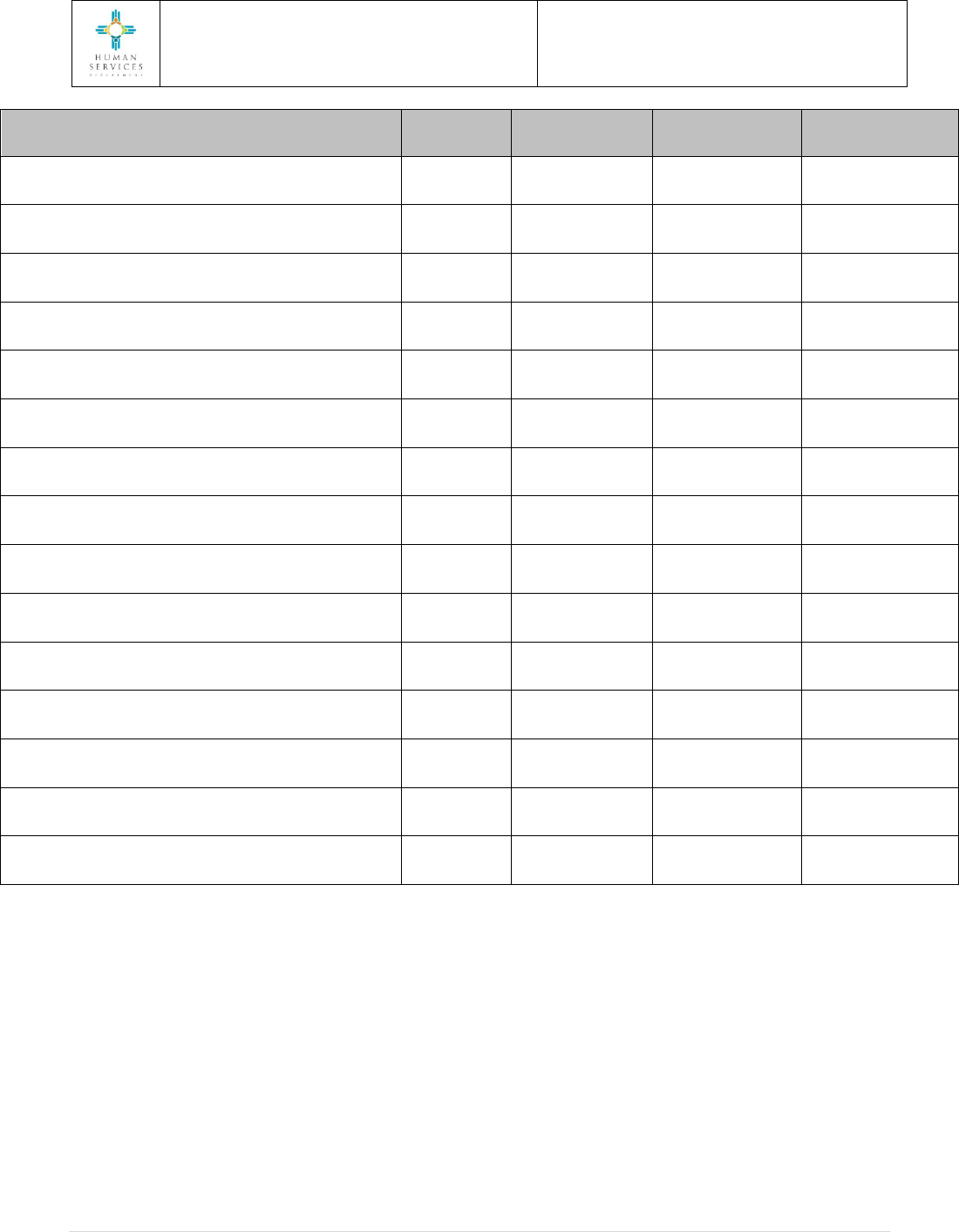
Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
282 | P a g e
SDCB Service
Billing
Code
Internal
Focos Code
Unit
SDCB Payment
Rate
Internet/cell phone
T1999
T1999IC
Each
As approved by MCO
Internet/cell phone/landline
T1999
T1999ICL
Each
As approved by MCO
Internet/landline
T1999
T1999IL
Each
As approved by MCO
Fax machine
T1999
T1999FX
Each
As approved by MCO
Computer
T1999
T1999CR
Each
As approved by MCO
Office supplies
T1999
T1999OS
Each
As approved by MCO
Printer
T1999
T1999PR
Each
As approved by MCO
Health-related equipment and supplies
T1999
T1999HR-I
Each
As approved by MCO
Adaptive equipment and supplies
T1999
T1999AE-I
Each
As approved by MCO
Exercise equipment and related items
T1999
T199EE-I
Each
As approved by MCO
Nutritional supplements
T1999
T1999NS-I
Each
As approved by MCO
OTC medications
T1999
T1999OM-I
Each
As approved by MCO
Household related goods
T1999
T1999HG-I
Each
As approved by MCO
Appliances for independence
T1999
T1999AI-I
Each
As approved by MCO
Adaptive furniture
T1999
T1999AF-I
Each
As approved by MCO

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
283 | P a g e
9.22.2. SDCB Vendor Credentialing Requirements
Requirements for enrolling SDCB Vendors
Before using any Vendor, please call Conduent (1-866-916-0310) to ensure all required vendor paperwork has been processed and the vendor
has been set up on your SDCB Care Plan. If you use a vendor before their paperwork has been processed, they will not be paid for those DOS.
All enrollment requirements (with the exception of the final CBC) must be processed before services can be provided. Services that are provided
prior to enrollment will not be paid by Medicaid or Conduent.
If a vendor provides only related goods (not services), you will only need to complete the Vendor Information Form (you do not need to
complete the entire Vendor Packet). We use the Vendor Information Form to show that you will be using this vendor on your Plan. Since vendors
that provide related goods are usually large companies (for example: CenturyLink, Comcast, Wal-Mart, K-Mart, Best Buy), it is not necessary to
get their signature on the form. If you are not sure whether you are purchasing a “good” or a “service,” please call Conduent for assistance.
Vendors (Independent Contractors and Agencies) that provide Services
Ag = Agency, IC = Independent Contractor
Service Code
Service Code Description
Billing
Method
Vendor Packet
License and/or Additional Requirements
97810
Acupuncture
Allowed Providers: Group Practice or Individual Specialized Therapist
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License
IC: Acupuncture and/or oriental medicine license
H2019
Behavior Support Consultation
Allowed Providers: Individual BSC or BSC Group Practice
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License
IC: Licensed (MD, Clinical Psychologist, Psychologist
Associate, SW, LPCC, LPC, Psychiatric Nurse, New Mexico
LMFT, New Mexico LPAT)
90901
Biofeedback
Allowed Providers: Group Practice or Individual Specialized Therapist
Visit
Agency: Yes
IC: Yes
Agency: Business License
IC: License in Health Care Profession whose scope of
practice includes Biofeedback
98940
Chiropractic
Allowed Providers: Group Practice or Individual Chiropractor
Visit
Agency: Yes
IC: Yes
Agency: Business License
IC: Chiropractic Physician License

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
284 | P a g e
Vendors (Independent Contractors and Agencies) that provide Services
Ag = Agency, IC = Independent Contractor
Service Code
Service Code Description
Billing
Method
Vendor Packet
License and/or Additional Requirements
T1999CE-I
Coaching Education for Parents, Spouse or Other
Allowed Providers: Vendor
Each
Agency: Yes
IC: Yes
Agency: Business License IC: Pre-Hire Packet
T1999CS-I
Coaching Education for Parents/Spouse: Conferences & Seminars ONLY
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999CL-I
Coaching Education for Parents/Spouse: Classes ONLY
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
97532
Cognitive Rehabilitation Therapy
Allowed Providers: Group practice or Individual Specialized Therapist
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License
IC: License in Health Care Profession whose scope of
practice includes Cognitive Rehabilitation Therapy
S5100
Customized Community Support
Allowed Providers: Adult Day Health Agency or Adult Day Habilitation
Agency
Per 15 min
Agency: Yes
Agency: Business License
S5160
Emergency Response Testing and Maintenance
Allowed Providers: Emergency Response Provider (Agency)
Each
Agency: No
Agency: Business License
S5161
Emergency Response Monthly Service Fee
Allowed Providers: Emergency Response Provider (Agency)
Monthly
Agency: No
Agency: Business License
T2019
Employment Supports (includes Job Coach)
Allowed Providers: Supported Employment Provider Agency or
Individual
Each
Agency: Yes
IC: Yes
Agency: Business License IC: Pre-Hire Packet
S5165
Environmental Modifications
Allowed Providers: Individual or Company (Agency)
Each
Agency: Yes
IC: Yes
Agency: Appropriate License IC: Appropriate License
T1999CP-I
Fees and Memberships
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999HR-I
Health-Related Equipment and Supplies
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
285 | P a g e
Vendors (Independent Contractors and Agencies) that provide Services
Ag = Agency, IC = Independent Contractor
Service Code
Service Code Description
Billing
Method
Vendor Packet
License and/or Additional Requirements
T1999AE-I
Adaptive Equipment and Supplies
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999EE-I
Exercise Equipment and Related Items
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999NS-I
Nutritional Supplements
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999OM-I
OTC Medications
Allowed Providers: Vendor
Each
Agency: No
Yes IC: No
VIF is required (goods only)
S8940
Hippotherapy
Allowed Providers: Group Practice or Individual Specialized Therapist
Visit
Agency: Yes
IC: Yes
Agency: Business License
IC: License in Healthcare profession whose scope of
practice includes Hippotherapy.
S9122
Home Health Aide
Allowed Providers: HHA/PCS Agency
Hour
Agency: Yes
Agency: Business License
99509
Self-Directed Personal Care
Allowed Providers: Individual Self-Directed Personal Care Provider or
HHA/PCS Agency
Hourly
Agency: Yes
IC: Yes
Agency: Business License IC: Pre-Hire Packet
T1999HG-I
Household Related Goods and Services Item/Invoice
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999AI-I
Appliances for Independence Item/Invoice
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999AF-I
Adaptive Furniture Item/Invoice
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T2019JD
Job Developer
Allowed Providers: Supported Employment Provider Agency or
Individual
Each
Agency: Yes
IC: Yes
Agency: Business License IC: Pre-Hire Packet
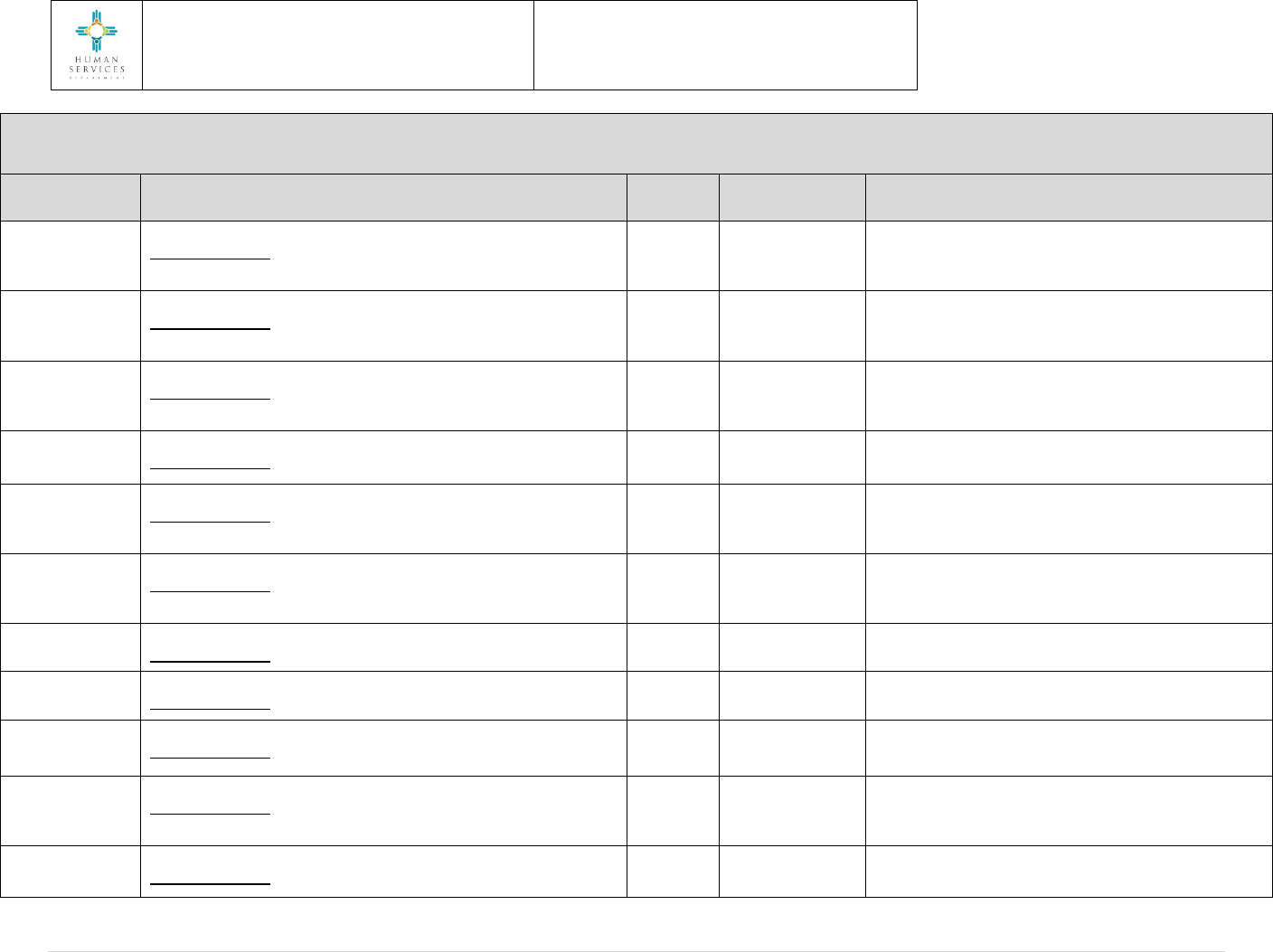
Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
286 | P a g e
Vendors (Independent Contractors and Agencies) that provide Services
Ag = Agency, IC = Independent Contractor
Service Code
Service Code Description
Billing
Method
Vendor Packet
License and/or Additional Requirements
97124
Massage Therapy
Allowed Providers: Group Practice or Individual Specialized Therapist
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License
IC: Massage Therapist License
S8990
Naprapathy
Allowed Providers: Group Practice or Individual Specialized Therapist
Visit
Agency: Yes
IC: Yes
Agency: Business License
IC: Naprapathic Physician License
S9445
Native American Healers
Allowed Providers: Group Practice or Individual Specialized Therapist
Session
IC: Yes
IC: Pre-Hire Packet
S9470
Nutritional Counseling
Allowed Providers: Group Practice or Individual
Hourly
Agency: Yes
IC: Yes
Agency: Business License
IC: Registered Dietician License
G0152
Occupational Therapy
Allowed Providers: Individual Occupational Therapist or Group Practice
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License IC: OT License
G0151
Physical Therapy
Allowed Providers: Group Practice or Individual Physical Therapist
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License IC: PT License
T1003
Private Duty Nursing LPN
Allowed Providers: HHA, RHC, FQHC or Individual
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License IC: LPN License
T1002
Private Duty Nursing RN
Allowed Providers: HHA, RHC, FQHC or Individual
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License IC: RN License
T1005HHA
Respite Home Health Aide
Allowed Providers: Respite Agency
Per 15 min
Agency: Yes
Agency: Business License
T1005SD
Respite Standard
Allowed Providers: Individual Provider (not RN, LPN or HHA) or Respite
Provider Agency
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License IC: Pre-Hire Packet
T1005LPN
Respite LPN
Allowed Providers: Respite Provider Agency or Individual LPN
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License IC: LPN License

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
287 | P a g e
Vendors (Independent Contractors and Agencies) that provide Services
Ag = Agency, IC = Independent Contractor
Service Code
Service Code Description
Billing
Method
Vendor Packet
License and/or Additional Requirements
T1005RN
Respite RN
Allowed Providers: Respite Provider Agency or Individual RN
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License IC: RN License
G0153
Speech/Language Pathology
Allowed Providers: Individual SLP or Group Practice
Per 15 min
Agency: Yes
IC: Yes
Agency: Business License IC: RN License
T2028CR
Start-Up Goods- Computer Purchase
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T2028FX
Start-Up Goods - Fax Machine Purchase
Each
Agency: No
IC: No
VIF is required (goods only)
T2028IA
Start-Up Goods - Internet Activation
Each
Agency: No
IC: No
VIF is required (goods only)
T2028LA
Start-Up Goods - Landline Activation
Each
Agency: No
IC: No
VIF is required (goods only)
T2028OS
Start-Up Goods – Office Supplies (purchased as items)
Each
Agency: No
IC: No
VIF is required (goods only)
T2028PR
Start-Up Goods – Printer Purchase
Each
Agency: No
IC: No
VIF is required (goods only)
T1999TS
Technology for Safety and Independence
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999CR
Computer Purchase (item)
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999PR
Printer Purchase (item)
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999FX
Fax Machine Purchase (item)
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999CPEP
Cell Phone and Related Equipment Purchase (item)
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
288 | P a g e
Vendors (Independent Contractors and Agencies) that provide Services
Ag = Agency, IC = Independent Contractor
Service Code
Service Code Description
Billing
Method
Vendor Packet
License and/or Additional Requirements
T1999IS
Internet Service
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999CELL
Cell Phone Service
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999LS
Landline Service
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999ICL
Internet/Cell Phone/Landline Service (bundled)
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999IC
Internet/Cell Phone Service (bundled)
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999IL
Internet/Landline Service (bundled)
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999CPL
Cell Phone/Landline Service (bundled)
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T1999OS
Office Supplies (purchased as items)
Allowed Providers: Vendor
Each
Agency: No
IC: No
VIF is required (goods only)
T2004
Transportation Commercial Carrier Pass
Allowed Providers: Transportation Commercial Carrier
Each
Agency: No
IC: No
VIF is required (goods only)
T2049
Transportation Mile
Allowed Providers: Transportation Agency or Individual Driver
Per Mile
Agency: Yes
IC: Yes
Agency: Business License
IC: Transportation Appendix, Pre-Hire Packet

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
289 | P a g e
If the vendor has a professional license (such as an RN or therapist), their licensing board has already completed a background check. Provider
agencies are responsible for completing CBC on all their staff. Confirmation of the CBC must be available to the State and Conduent for review as
requested.
Please remember that at the beginning of each SDCB Care Plan year (annual renewal), new Vendor Agreements are required for any vendor
providing services. If Conduent does not receive a Vendor Agreement before your new Plan starts, your vendor will not be set up on your new
Plan and they may be paid late. Please call Conduent (1-866-916-0310) before your new SDCB Care Plan starts to ensure all your SDCB providers
are set up for payment.
The above grid provides an overview of general vendor credentialing requirements. In certain specific cases, additional licensing or other
documentation may be required.
Please contact Conduent (1-866-916-0310) or your Support Broker if you have any questions.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
290 | P a g e
9.22.3 Employee Credentialing Requirements Grid
SELF-DIRECTED
COMMUNITY BENEFIT SERVICE
Service
Code
*Pre-Hire
Packet
**Employee
Packet
Transportation
Appendix
Employment Supports (includes Job Coach)
T2019
Yes
Yes
No
Self-Directed Personal Care
99509
Yes
Yes
No
Respite – Standard
T1005SD
Yes
Yes
No
Transportation Mile
T2049
Yes
Yes
Yes
*Pre-Hire Packet: Division of Health Improvement (DHI) form, copy of identification card, and three
fingerprint cards.
**Employee Packet: Employee Information Form, Employee Agreement, Transportation Appendix (if
performing driving services), Declaration of Relationship, W-4 (Federal and State), I-9 Form, Direct
Deposit Authorization Form (optional).
Helpful Reminders
•
Employer of Record (EOR) documentation must be completed and approved before an employee’s
enrollment can be approved and before an employee can begin work.
•
Employees may not begin working until they have passed their initial COR Background Check (this is
included in the Pre-Hire Packet).
•
Employees cannot be paid until their entire Employee Packet has been successfully processed.
•
In order to drive, an employee must have current vehicle registration and insurance in the
employee’s name.
•
Please remember that Employees must complete a new Employee Agreement for each Plan year. If
Conduent does not receive an Employee Agreement before the beginning of the new Plan, the
employee may not get paid on time.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
291 | P a g e
9.22.4. Vendor Toolkit: Invoices
Toolkit: Invoices
Use these tips for completing Invoices!
Q: What is this toolkit for?
A: This toolkit explains how to make the invoice process work smoothly! Members,
Employers and Vendors can work together to help make sure invoices get processed
and paid on time.
Keys to Getting Paid the Correct Amount, On Time!
Follow these tips to avoid delayed payment of your invoice.
•
Be sure ALL vendor paperwork has been completed and submitted.
•
Effective July 15, 2011, invoices that are received by Conduent (formerly Xerox)
more than 90 days after the service was provided, will not be processed for
payment. According to Medicaid timely-filing requirements, we cannot process any
request for payment that has not been submitted within 90 days from the date the
vendor performed the service. This means that all invoices with a PRF, must be
submitted to Conduent no later than midnight on the 90th
day after services have
taken place. Any invoices with a PRF that are submitted after this time limit will not be
paid by Conduent and will be returned to you. Also, if you need to make corrections to
your invoice and/or PRF, you must complete them within this timeframe (90 days
from the date the service was performed).
•
Follow the CURRENT Vendor Payment Schedule.
Keep a copy of the Vendor Payment Schedule in front of you. If you submit your
invoice and PRF after the deadline on Saturday, your vendor payment may be
delayed.
Note: The deadline for submitting invoices is always on a Saturday by midnight
(before 12:00 am on Sunday).
•
Use your legally registered business name.
For example,
o Smith Industries, LLC is your legally registered business name with State of New
Mexico. This is the name you must use on your invoice and PRF!
o
Bobby Smith is your personal name. Do not use!

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
292 | P a g e
o
Smith Wheelchair Repair is a name you sometimes use to refer to your company
but it is not your legal name. Do not use!
•
Submit invoices and PRFs for monthly service codes after the service is complete.
If the service is monthly, you must wait until after midnight on the last day of the month.
If the service is hourly, you must wait until you have finished working on that day. For
example, if you finish working at 3:00 pm, you cannot submit your invoice and PRF until
3:01 pm on the same day. The general rule is: you cannot enter, submit or sign an invoice
for services not yet rendered.
•
Use correct units on invoices
For example, if the rate for service is in 15 minute increments, you must enter the
invoice charge in 15 minute increments. Do not combine amounts into hourly.
•
Only the vendor can make a correction to an invoice
Corrections to an invoice cannot be handwritten unless the invoice to be corrected is
handwritten. We will not accept invoices if white-out appears to have been used or if
changes appear to have been made by anyone other than the vendor.
•
You can use your own invoice form, but…
Your invoice must include the same level and type of detail shown on the invoice (see
below.) This detail is required for legal and auditing purposes and to ensure you get paid
correctly and on time.
•
Send in the PRF
The PRF must also be submitted (in addition to the invoice). This applies whether it is you
or the Employer who typically sends in the PRF and invoice. (The Employer is responsible
for making sure that the PRF and invoice are sent in.)
•
Fax your invoice.
Only fax your PRF and invoice one time unless you are faxing a corrected invoice. If it is a
corrected invoice, check the box Yes for “Is this a correction to a PRIOR Invoice?” Re-faxing
the same PRF and invoice or forgetting to check the “Corrected” box on the PRF for a
corrected invoice will cause delays in a check being issued. The fax number is
1-866-302-6787. This applies whether it is you or the Employer who typically faxes in the
invoice (the Employer is responsible for making sure the PRF and invoice are faxed in.
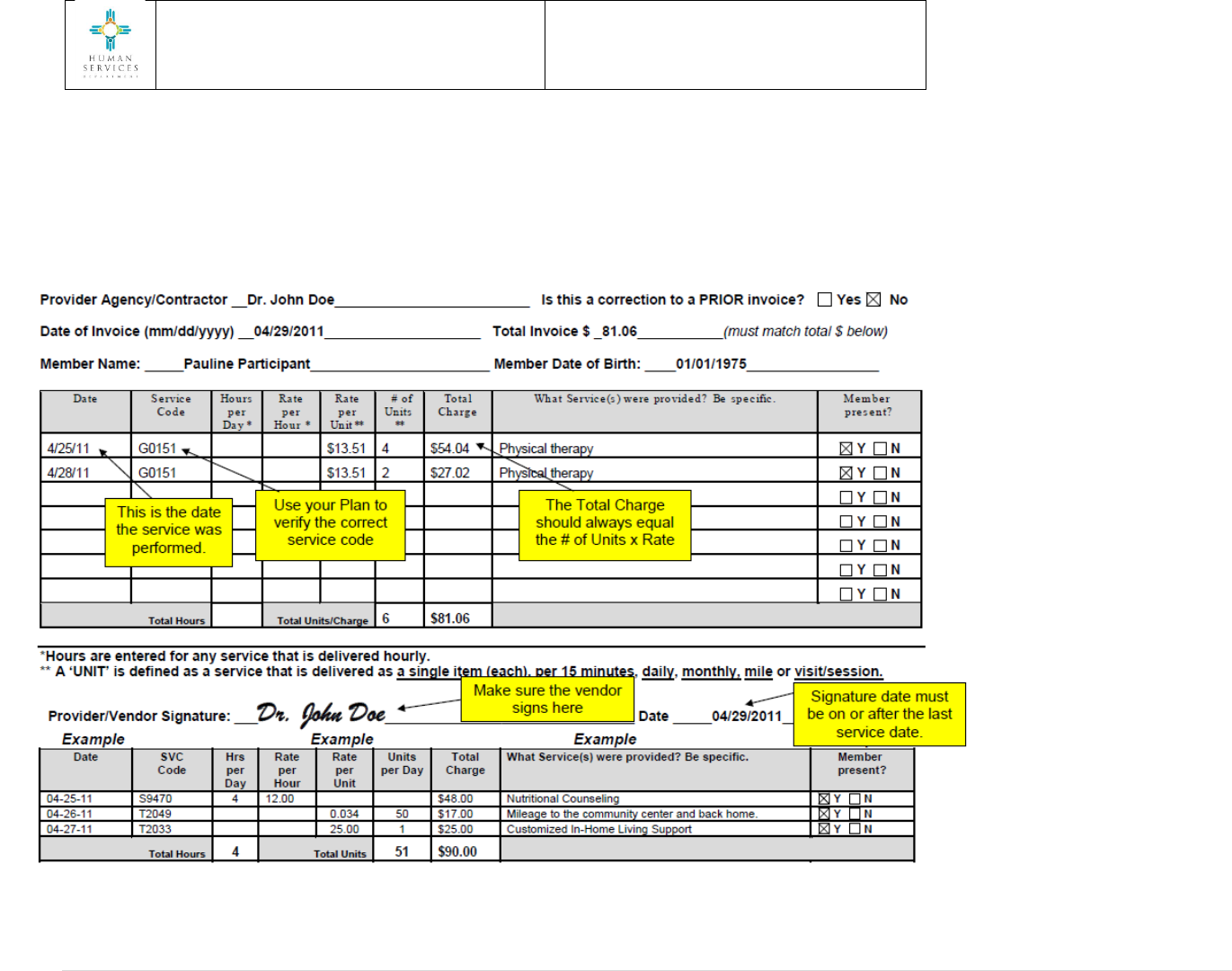
Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
293 | P a g e
Invoice for Non-Timesheet Provider Agency/Contractor
FAX: 1-866-302-6787 MAIL: CONDUENT PO Box 27460, Albuquerque, NM 87125
Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
294 | P a g e
9.22.5. Employee Toolkit: Timesheets
Toolkit: Timesheets
Q: What is this toolkit for?
A: This toolkit explains how to make the timesheet process work smoothly! Members, Employers
and Employees can work together to help make sure timesheets get processed and paid on
time.
TIPS FOR GETTING PAYCHECKS THAT ARE ACCURATE AND ON TIME!
•
Be sure ALL employee paperwork has been completed & submitted.
•
Effective July 15, 2011, timesheets that are received by Conduent (formerly Xerox) more than
90 days after the service was provided will not be processed for payment. According to
Medicaid timely-filing requirements, we cannot process any request for payment that has not
been submitted within 90 days from the date the employee worked. This means that all
timesheets must be submitted to Conduent (via fax or the FOCoSonline system) no later than
Midnight on the 90th
day after services have taken place. Any timesheets that are submitted
after this time limit will not be paid by Conduent and will be returned to you.
Also, if you need to make corrections to your timesheets, you must complete them within this
timeframe (90 days from the date the employee worked).
•
Follow the CURRENT payroll periods.
Keep a copy of the payroll schedule in front of you. Timesheets submitted after Saturday’s
deadline may result in a delayed paycheck. If you would like a copy of the current Payroll
Payment Schedule, please contact the Self-Direction Help Desk (1-866- 916-0310).
Note: For Employers that have been approved by the MCO for online timesheet exceptions, the
deadline for submitting timesheets by fax is always on the Saturday by Midnight (before 12:00
am on Sunday) at the end of the pay period. Online timesheets must be approved in
FOCoSonline by the Employer by 12:00 pm (noon) Tuesday after the end of the pay period.
•
Service dates on all timesheets need to be ON or BEFORE the last day of the timesheet
period.
You cannot enter, submit or sign a timesheet for work not yet performed. For example, if the
pay period ends on Friday, May 20th, you cannot enter time for services you will provide on
Monday, May 23rd
even if the services are generally similar or the same.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
295 | P a g e
•
Services Provided field on the Timesheet.
Enter descriptions of tasks and services provided to the member.
•
Timesheets need to be complete and correct (see example on Page 3 of this toolkit).
•
Both the Employee and the Employer need to sign and date the timesheet.
•
Fax your timesheet if you are on the MCO approved exception list.
Only fax your timesheet one (1) time unless you are faxing a corrected timesheet or if you have
been asked to refax it. If it is a corrected timesheet, check the box Yes for “Is this a correction
to a PRIOR Timesheet?” Not following these guidelines can cause delays in a check being
issued. The fax number is 1-866-302-6787.
•
Use the exact same name on your timesheet as used for your employee paperwork.
For example, if you completed paperwork as William J Smith and you enter Billy Smith on your
timesheet, we won’t know who you are. This will cause a delay in getting paid.

Section 9: Self-Directed Community
Benefit
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
296 | P a g e

Section 10: RESERVED
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
297 | P a g e
10. RESERVED

Section 11: Marketing
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
298 | P a g e
11. Marketing
11.1. General Information
This policy establishes guidelines and restrictions for all MCOs awarded a contract and subcontractors of
the MCO, or under contract with HSD to deliver health care services, for marketing and outreach
activities referencing the managed care program.
Definitions
Health Education: Programs, services or promotions designed or intended to advise or inform the
MCO’s enrolled members about issues related to healthy lifestyles, situations that affect or influence
health status, behaviors that affect or influence health status or methods of medical treatment.
Health Educational Materials: Materials designed, intended, or used for health education or outreach to
the MCO’s enrolled members. Health education materials include, but are not limited to:
condition-specific brochures, letters or phone calls, member newsletters, posters and member
handbooks.
Incentives: Items used to encourage behavior changes in the MCO’s enrolled members or health
promotion incentives used to motivate members to adopt a healthy lifestyle and/or obtain specific
health care services. These may include but are not limited to:
• Infant car seats or baby item giveaways;
• Gift cards;
• Manufacturer or coupons for savings on products; or
• Services or any other objects designed or intended to be used in health education or outreach.
Incentives may not be used in conjunction with the distribution of alcohol or tobacco products, or
firearms.
Marketing: Any medium of communication that is written, audio/oral, personal face-to-face, or
electronic, including any promotional activities, intended to increase the MCO’s or subcontractor’s
membership or to “brand” an MCO’s or subcontractor’s name or organization.
Marketing Materials: General audience materials such as general circulation of brochures, flyers,
newspaper, phone book advertisements, websites and/or any other materials designed, intended, or
used for increasing the MCO’s or subcontractor’s membership or establishing a brand. Such marketing
materials may include but are not limited to scripts, provider directories, leaflets, posters, billboards, or

Section 11: Marketing
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
299 | P a g e
any material that is distributed or circulated by the MCOs and subcontractors, including providers
(e.g., personal care providers).
Outreach: Any means of educating or informing the MCO’s enrolled members about health issues. See
also Health Education.
Outreach Materials: Materials designed, intended, or used for health education or outreach purposes
only for the MCO’s enrolled members. See also Health Education.
Event Promotion: Any activity in which any approved marketing materials are given away or displayed
with the intent to provide health education and/or outreach.
Provider: A hospital/hospital staff, physician/physician staff, pharmacy/pharmacist, ancillary service
providers and their staff, personal care/homemaker providers and their staff.
Policy
Marketing is information intended for the general public about the existence of the MCO and its
subcontractors and the availability of the MCO as an enrollment option for people deemed eligible for
services through Centennial Care.
Outreach is communication with enrolled members for the purpose of member retention and improving
the health status of enrolled members. Retention efforts must be directed to currently enrolled
members who are determined to be at risk for attrition or be based on analysis of membership trends
such as decreased utilization of preventative services.
The MCO must submit marketing, outreach, retention activities and materials to HSD for review and
prior approval. In addition, the MCO must provide HSD with an electronic copy of the approved
materials, advertising copy or publication in which the ad will be placed. All member materials must be
mailed to members unless the member requests the material in an alternative format.
• Marketing Material Approval
The MCO shall submit electronic versions of all written materials that will be distributed to members
(referred to as member materials) to HSD’s Communication and Education Bureau’s Marketing
Coordinator and copy the HSD contract manager for review and approval. This includes but is not limited
to member handbooks, provider directories, member newsletters, member identification cards and,
upon request, any other additional, but not required, materials and information provided to members
designed to promote health and/or educate members.
• All member materials must be submitted to HSD in electronic file media, in the format
prescribed by HSD. The MCO shall submit the reading level and the methodology used to

Section 11: Marketing
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
300 | P a g e
measure it concurrent with all submissions of member materials and include a plan that
describes the MCO’s intent for the use of the member materials.
• The HSD Marketing Committee will attempt to approve or deny marketing requests within 15
business days of the receipt of the complete request. The 15 business day timeframe for
approval or denial shall only apply to the specific date of the initial submission. Modifications of
any type would need to be resubmitted, which may delay approval.
• Prior to modifying approved member materials, the MCO shall submit to HSD for prior written
approval a detailed description of the proposed modifications in accordance with this section of
the Manual.
• The use of any material, including those that pertain to incentives, marketing, outreach, and
promotions must have prior approval from the HSD Marketing Committee.
• Materials that have been previously approved, but will be included in a specific activity must
also be included in the MCO’s submission for review and approval by HSD.
• MCOs shall review all material on a regular basis and revise materials as necessary. Any revised
or updated material previously approved must be submitted to HSD for approval.
• HSD Review of MCO Materials
The MCO shall ensure all materials submitted to HSD for review meet the following criteria:
o All materials shall include information that describes what the submission is, its purpose and
what population (if applicable) it will target. This information may be submitted in form of a
cover letter, MCO Contractor plan form, or in the body of an email;
o All materials consisting of two or more pages must be numbered;
o All materials must be 6th grade reading level or lower and each submission must provide the
reading level with and without, proper names, medical terminology, etc.;
o All materials must indicate if a translated version will be made available to the member or how
the member can request a translated version;
o All materials must be submitted timely and at least 30 calendar days prior to use allowing the
HSD Marketing Committee at least 15 business days to review. If an “expedited” review is
needed, please submit and allow at least five business days for review and approval or request
special accommodations for unique circumstances;
o All materials used for any type of Medicaid or managed care training purposes must be
submitted for review and approval before training occurs (i.e., handouts, PowerPoint

Section 11: Marketing
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
301 | P a g e
presentations, etc.). If MCOs are collaborating and conducting one training using the same
PowerPoint presentation, one MCO should be designated to submit the material on behalf of all
MCOs (e.g. Annual Tribal Meetings);
o All materials shall identify the MCO as an HSD/MAD managed care provider and are consistent
with all the requirements for information to members described in the Agreement, regulations
and the Manual;
o All materials shall specify “Such services are funded in part with the State of New Mexico”;
o All related materials should be submitted to HSD for review together, in lieu of separate
submissions;
o All approved materials shall be provided in electronic format to the HSD marketing coordinator
in the English and translated Spanish version (if applicable); and
o Outreach material may not include the words: “free”, “join”, “enroll”, “sign up” or similar
verbiage unless approved by the HSD Marketing Committee. If the MCO intends on using such
language in any of the materials, the request for approval must include how the message is
related to an Outreach goal.
• Events
MCOs may participate in health-related marketing and outreach events. Events must be health-related
or have health education components. MCO participation in these events must be substantive; an
unmanned booth(s) with handouts is not acceptable.
The MCO shall submit to the HSD Marketing Committee all marketing outreach events in which the MCO
participated. Participation includes, but is not limited to, having a manned booth at the event, financially
contributing to the event, and/or having a presence at the event.
• Marketing and Outreach Plan
The MCO shall submit an annual Marketing and Outreach Plan as well as a quarterly report which
outlines the MCO’s activities.
• MCO Health Plan Name and Logos
MCO Name and Logos can be included on event flyers or websites that are produced by hosting
organizations without prior approval. MCO must monitor their MCO name and logo use to prevent
misuse. Small giveaway items such as, but not limited to, pens, pencils, balls, toys, etc. that are only
identified by the addition of the MCO’s logo do not need prior approval from HSD.

Section 11: Marketing
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
302 | P a g e
Any items that include the MCO’s logo as well as any reference to Centennial Care or the State Medicaid
program must be approved by HSD through the Marketing approval process.
• Restrictions
The following restrictions apply to all marketing, outreach and retention activities. The following shall
not be allowed:
o Incentive items such as t-shirts, buttons, balloons, key chains, etc. unless the intent of such a
give-away is outreach in nature (i.e., for educating members about benefits of safety,
immunizations, well-care, or as a “reward/incentive” for member accessing care as part of an
approved incentive program);
o Solicitation of any individual face-to-face, door-to-door or cold call telemarketing, including that
of the MCO’s subcontractors;
o Any reference to competing plans;
o Promotional materials, incentives, or any other activity to influence enrollment in conjunction
with the sale or offering of any private insurance;
o Unsolicited direct mail advertising, including that of the MCO’s subcontractors;
o Marketing of non-covered services;
o Reference to the word “free” for any covered service;
o Use of HSD/MAD logo;
o Inaccurate, misleading, confusing, or negative information about HSD, or statements designed
to recruit potential members, including that of the MCO’s subcontractors;
o Discriminatory marketing practices; and/or
o The MCO may not encourage or persuade the member to select a particular MCO plan or
subcontracted provider when completing specific applications or forms. The MCO or its
subcontractor may not complete any portion of the application forms on behalf of the potential
enrollee. The prohibition covers all situations, whether sponsored by the MCO, its parent
company, or any other entity.
HSD reserves the right to impose additional restrictions at any time.
• Sanctions/Penalties
Any violation of this policy may result in the sanctions as described in 7.3 of the Agreement.

Section 11: Marketing
Revision dates: August 15, 2014; March 3, 2015;
October 1, 2020
Effective dates: January 1, 2014
303 | P a g e
The MCO shall ensure subcontractors are advised that they must comply with this policy. All materials
must be submitted by all subcontractors to the MCO for review and approval based on the MCO specific
policies and procedures for marketing.
Failure of a subcontracted provider to adhere to this policy may result in sanctions/penalties to the
contractor contracted with such a provider.
Subcontractors may only advertise the services they provide and may not make any reference to
HSD/MAD programs, Medicaid or services the MCO provides.
o Temporary Sanctions/Penalties
Any activities or materials found in violation of this policy will be subject to sanction regardless of
previous approval or terms in contractual agreements. The MCO contractor will be placed on
“Moratorium” status and will not be allowed to advertise via the following:
▪ Television advertising;
▪ Internet advertising;
▪ Print advertising;
▪ Radio advertising;
▪ Billboards; and
▪ Bus wraps (including bus stops).
The MCO will monitor its subcontractors found in violation of this policy and impose sanctions for
marketing or advertising of the subcontractor’s services and/or business.
The HSD Marketing Review Committee will review the “Moratorium” status on an annual basis, or at
HSD’s discretion, to determine if the MCO or its subcontractor is deemed compliant.
• References
o 42 CFR 438.104, 42 CFR 438.10, 42 CFR 431.12, 42 CFR 431.307
o HSD/MAD Medicaid Managed Care Services Agreement

Section 12: Patient Centered Initiatives
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
304 | P a g e
12. Patient-Centered Initiatives
12.1. Broad Standards
The MCO shall establish patient-centered initiatives based on the National Committee for Quality
(NCQA), Joint Commission on Accreditation of Healthcare Organizations, (JCAHOJCAHO) or Accreditation
Association for Ambulatory Health Care (AAAHC) PCMH recognition programs.
The MCO shall develop patient-centered, “whole person” models of care that are uniform across payers
and tailored to the diverse needs and capacities of primary care practices, large and small, urban, rural
and frontier. The New Mexico model should be based upon nationally accepted standards.
This model will be a blended model building upon the work already completed by practices that have
achieved certification programs. A blended model will include a pathway toward certification for those
practices that do not currently have the capacity to attain certification.
The New Mexico PCMH program will provide technical assistance, benchmarks, and financial support to
practices in order to move them along the pathway towards national recognition. Payment to
New Mexico PCMH practices is standardized and based on the level of PCMH achievement and
continued evidence of quality care to patients and reduced cost. The New Mexico PCMH will include
State-specific goals tailored to the unique needs of communities and patients.
Core components of the New Mexico PCMH Model include:
• Administrative:
o Adopt a standard model for PCMH that includes national certification by NCQA, AAAHC, and
JCAHO;
o Develop a “Glide Path” to certification that is open to all practices seeking PCMH status;
o Provide technical assistance and hands on training for practices working towards PCMH
certification; and
o Simplify, coordinate and standardize practices across MCOs specifically: claims, prior
authorizations, and other administrative processes.
• Clinical:
o Improved access to care through flexible scheduling, accommodating walk-ins, utilization of
telemedicine, providing after hours and weekend office hours;
o Provider teams collaborate with community health workers, lactation consultants, public health
workers, and other community members;
o Integration/co-location of BH services, MH, and substance use including SBIRT;

Section 12: Patient Centered Initiatives
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
305 | P a g e
o Include school-based health centers and other non-traditional healthcare settings; and
o Engage patients in their own health care decisions, respect for patient values, and culture and
inclusion of patient care givers.
• Coordination of care:
o Develop a care coordination collaborative that operates across payers at the point of care (in
the health care office or other community location);
o Prioritize communities of highest need;
o Address social determinants of health (i.e., housing, food, transportation, etc.);
o Seamless transition between services and providers; and
o Integration of public health services, including but not limited to: Children’s Medical Services
care coordination for children with special health care needs, Women Infants and Children,
sexually transmitted infection (STI) treatment, and contact tracing, etc.
• Data:
o Build provider capacity through support for evidence-based programs;
o Facilitate partnerships with supporting entities such as the Primary Care Association to help
develop tools for providers;
o Facilitate data sharing that provides optimal use of data for improving member outcomes; and
o Commitment to data integration and sharing information to improve collaborative efforts to
improve quality and lower costs, and to improve population health.
• Payment:
o While the MCO is not required to enter into VBP reimbursement arrangements with PCMHs,
the MCOs are expected to implement VBP strategies to promote quality and improve health
care outcomes in alignment with the Centennial Care contractual requirements;
o Align value-based payments with patient health care outcomes and achievement of quality
metrics; and
o Standardize a payment approach for PCMH that includes practices that have not yet attained
certification but are working on improving quality, access, and other core components of
PCMH.
• Specific Actions Related to Policy:
o Support Tribal 638 programs to become FQHCs under 330.

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
306 | P a g e
13. ABP Medically Frail and ABP Exempt
13.1. General Information
This section of the Manual is issued to address the criteria and process for determining whether a
member in the Other Adult Group COE 100 is medically frail. A medically frail member in COE 100 may
choose to continue receiving services under the ABP services package or may choose to become ABP
exempt and receive services under the Medicaid State Plan benefit package.
ABP exempt means an Other Adult Group Medicaid (COE 100) recipient who has been determined as
meeting the definition and criteria of medically frail (as defined in Section 13.2. of the Manual) and has
chosen to receive services under the Medicaid State Plan benefit package instead of the ABP. All COE
100 members are notified of their enrollment in the ABP and of the medically frail exemption
criteria/process on their HSD Medicaid eligibility notice. The eligibility notice also directs ABP recipients
to the HSD/MAD website where they can find the full listing of ABP benefits and a comparison to the
Medicaid State Plan. This section of the Manual explains the detailed criteria that should be used by the
MCO to determine whether COE 100 members meet one of the definitions of medically frail.
13.2. Determination of Medically Frail Diagnosis
Members in COE 100 may self-identify to the MCO by telephone that they may be medically frail and
may do so at any time during their eligibility for COE 100. Members in COE 100 may also be identified as
potentially medically frail by the MCO through the care coordination process.
To determine whether a member qualifies as medically frail, the MCO should reference the Medically
Frail Conditions List. The member must have a documented medical diagnosis from the list of qualifying
conditions. A written statement from a licensed provider attesting to the medical condition will suffice.
The entire medical record is not needed. If obtaining a written statement will cause significant delay, the
MCO may confirm the diagnosis by a licensed provider over the telephone. If the diagnosis is confirmed
by telephone, the MCO should document the discussion occurred and the outcome of that conversation.
The MCO should determine which staff can perform this function. A nurse is not required.
There shall be no end date for a medically frail approval. Upon the member’s self-identification, or
through the MCO’s care coordination process, the MCO shall evaluate and confirm whether the member
qualifies as medically frail. The MCO shall confirm the member’s status and notify the member whether
they meet the criteria for ABP exempt by mail within 10 business days of the member’s
self-identification. If the MCO is unable to obtain a provider’s diagnosis or any requisite follow-up from

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
307 | P a g e
either the member or a provider after making a good faith effort to do so within the necessary
timeframe, the MCO should issue a denial letter to the member.
The ABP member remains enrolled in the ABP until the MCO has confirmed medically frail status and the
member has chosen to receive the ABP exempt benefit package. The MCO shall describe the benefit and
cost-sharing differences between the ABP and the full Medicaid benefit package, if requested by the
member.
13.3. ABP Exempt Approval
If the member chooses the ABP exempt benefit package, the MCO shall make the indication in Omnicaid
using a Disability Type Code of ME (for an SMI, substance use disorder [SUD], or other mental disability)
or PH (for a PH disability) within two business days of receiving a call from a medically frail COE 100
member choosing the ABP Exempt benefit package; and shall mail the ABP Exempt member an approval
letter. The entry in Omnicaid should be made in the Client Detail window in the Client Subsystem and
may be made at any time during the month.
If the member does not meet medically frail criteria, the MCO shall mail the member a denial letter.
Should the member disagree with the MCO’s determination about his/her ABP Exempt status, the
member may file a reconsideration or request a fair hearing through the MCO’s appeals process. If a
member does not have one of the conditions or diagnoses listed on the Medically Frail Conditions List
and the member believes that his/her condition should be considered for inclusion, a request may be
sent to HSD/MAD to include the condition. The HSD/MAD Medical Director will review the request to
determine whether the individual’s condition should be added.
13.4. Appendices
13.4.1 ABP Benefit Chart
13.4.2 Alternative Benefit Plan-Exempt Medically Frail Conditions List
13.4.3 Chronic Substance Use Disorder (SUD) Criteria Checklist
13.4.4 Serious Mental Illness (SMI) Criteria Checklist
13.4.5 SMI-SED Criteria

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
308 | P a g e
13.4.1. ABP Benefit Chart
Medicaid ABP 1-8-2014
Recipient Definitions
Note there are 2 types of ABP recipients. The ABP recipient: The recipient is COE 100, but does not have
a disability indicator of PH or ME. The charts below are only applicable to the ABP recipient category.
ABP Exempt: The recipient is COE 100 but also has a disability indicator of PH or ME, meaning either a
PH or MH disability, or other condition that qualifies the recipient as medically frail.
When an ABP recipient’s condition is evaluated and it is determined they meet the qualifying conditions,
they may choose to become an “ABP Exempt” recipient. The benefit package of an ABP Exempt recipient
changes from the standard ABP recipient to that of the “standard” Medicaid full benefit recipient. That
is, the ABP benefit package ends and the ABP Exempt recipient then has access to the same benefits as a
full standard Medicaid recipient.
The COE of the recipient remains 100 with a PH or ME indicator to distinguish them in the various
computer systems. Because the benefits of an ABP-Exempt recipient become the same as any other
standard full benefit Medicaid recipient, we do not list their benefits in this chart.
The term “ABP recipient” always means an ABP recipient who is not ABP exempt. If the recipient is exempt
(and therefore eligible for the standard Medicaid full benefit services) the recipient is always referred to
as an “ABP Exempt recipient”.
Once the recipient becomes an ABP Exempt recipient, they are not subject to any of the service limits
associated with ABP. They do not retain any of the additional services found only in the ABP (primarily
preventive services). If the ABP Exempt recipient is enrolled in an MCO, the MCO extends the same
benefits and managed care services to the ABP Exempt recipient provided to the full benefit Medicaid
recipient.
An ABP Recipient has the following benefits equivalent to those of standard Medicaid Benefits:
professional services and treatments, including services at FQHC’s and other clinics; inpatient and
outpatient hospital services; equipment and devices; laboratory and radiology; and transportation).
The coverage of the following services or providers of services under the ABP is essentially the same that
for the standard Medicaid full benefit population and, therefore, would be covered by an MCO to the
same extent an MCO covers and provides services to traditional full Medicaid eligible recipients. The list
is intended to be used to communicate the general scope of the services. Not every provider and service
is described:

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
309 | P a g e
• Physician and most practitioner services and visits, including maternity service, surgeries,
anesthesia, podiatry, etc., that are available for traditional full Medicaid eligible recipients;
• BH and substance abuse services, evaluations, assessments, therapies, including all the various
forms of therapy such as Comprehensive Community Support Services that are available for
traditional full Medicaid eligible recipients:
o Specialized BH services for children: the MCO must ensure BH and substance abuse services
provided to EPSDT recipients are available to ABP recipients ages 19 and 20;
o Specialized BH services for adults: The specialized BH services for adults are Intensive
Outpatient, Assertive Community Treatment, and Psychosocial Rehabilitation. These three
services are included in the ABP;
o Services not included in the ABP: The following services are not included in the ABP plan
because they are considered more in the area of supportive waiver-type services and are not
State Plan services: Family Support, Recovery Services, and Respite Services; and
o Electroconvulsive therapy: This is a benefit under ABP, but not as a State Plan service for
standard service.
• Cancer trials, chemotherapy, IV infusions, and reconstructive surgery services that are available for
traditional full Medicaid eligible recipients;
• Dental services as available for traditional full Medicaid eligible recipients. An EPSDT recipient must
have available the increased frequency schedule of oral exams every six months and orthodontia
(when medically necessary) for 19 and 20 year olds per EPSDT rules;
• Diabetes treatment including diabetic shoes;
• Dialysis;
• DME, oxygen, and supplies necessary to use other equipment such as for oxygen equipment,
ventilators and nebulizers, or to assist with treatment such as casts and splints that are applied by
the healthcare practitioner;
• Family planning, sterilization, pregnancy termination, contraceptives;
• Hearing testing or screening as part of a routine health exam. ABP does not cover the hearing aids
and does not typically cover audiologist’s services or any services by a hearing aid dealer, except for
EPSDT children, ages 19 and 20, for whom testing and hearings aids are covered;

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
310 | P a g e
• Hospice services — If the hospice recipient requires NF LOC, the recipient will have to meet the
requirements for receiving NF care;
• Hospital inpatient, outpatient, urgent care, emergency department, outpatient free-standing
psychiatric hospitals, inpatient units in acute care hospitals for rehabilitation or psychiatric, and
rehabilitation specialty hospitals:
o Free-standing psychiatric hospitals are only covered for EPSDT children (therefore, up through
age 20) for FFS recipients. However, MCOs continue to pay for inpatient free-standing
psychiatric hospitals for adults; and
o Inpatient drug rehabilitation services are not an ABP benefit. Acute inpatient services for
“detox” are an ABP covered benefit.
• Immunizations, mammography, colorectal cancer screenings, pap smears, prostate-specific antigen
(PSA) tests, and other age appropriate tests that are available for traditional full Medicaid eligible
recipients;
• Inhalation therapy;
• Lab including diagnostic testing, and colorectal cancer screenings, pap smears, PSA tests, and other
age appropriate tests that are available for traditional full Medicaid eligible recipients;
• Lab genetic testing to specific molecular lab tests such as breast cancer susceptibility gene (BRCA)1
and BRCA2 and similar tests used to determine appropriate treatment, not including random genetic
screening;
• Medication assisted treatment (substance abuse treatment including methadone programs and
suboxone);
• Ob-gyn, prenatal care, deliveries, midwives;
• Orthotics (note foot orthotics including shoes and arch supports are only covered when an integral
part of a leg brace, or are diabetic shoes);
• Podiatry services are available to the same extent as for traditional full Medicaid eligible recipients.
(coverage is similar to Medicare);
• Prescription drug items (but not over the counter [OTC] items, except for prenatal drug items
(examples include vitamins, folic acid, iron), low dose aspirin as preventative for cardiac conditions;
contraception drugs and devices, and items for treating diabetes. OTC items are covered for ages 19
and 20);

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
311 | P a g e
• Prosthetics are available to the same extent as for traditional full Medicaid eligible recipients;
• Radiology including diagnostic imaging and radiation therapy, including mammography and other
age appropriate imagining;
• Reproductive health services are available to the same extent as for traditional full Medicaid eligible
recipients;
• Telemedicine;
• Tobacco cessation counseling that are available for traditional full Medicaid eligible recipients.
MCOs must cover tobacco cessation counseling beyond the Medicaid FFS coverage; and
• Transportation (emergency and non-emergency) including air and ground ambulance, taxi and
handivan.
The following services are not covered under the standard Medicaid benefits or the ABP and are not
required to be covered by the MCO for ABP members unless the MCO chooses to do so as VAS.
• Acupuncture;
• Infertility treatment;
• Naprapathy;
• Temporomandibular joint and crania mandibular joint treatment;
• Weight loss programs; and
• Any other service not covered by the standard Medicaid program unless specifically described as an
added benefit for ABP in this section.
Note also the ABP does not include the following:
• CBs;
• NF care, except as a temporary step down LOC from a hospital prior to being discharged to home;
and
• Mi Via.
However, if an ABP recipient becomes an ABP Exempt recipient, the recipient can access CBs, NF care,
and Mi Via when all the requirements to receive those services are met.
An ABP recipient has the following benefits similar to standard Medicaid recipients but with limitations.
These are services which are benefits for recipients under the standard Medicaid program, but which
have limitations to coverage under the ABP.
Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
312 | P a g e
Service
Limitations for ABP Recipients (COE 100) for Ages
21 and above
For Ages 19 and 20
Limitations do not apply to ABP
recipients (COE 100) who are Ages
19 or 20 because of EPSDT rules.
Recipients Under Age 19 Are Not
Enrolled In ABP
Bariatric surgery
Limited to 1 per lifetime.
Criteria may be applied that considers previous attempts
by the recipient to lose weight, BMI, health status, etc.
Covered under EPSDT if medically
necessary (perhaps unlikely) without the
lifetime limit.
Criteria may be applied that considers
previous attempts by the recipient to lose
weight, BMI, health status, etc.
Cardiac rehabilitation
Limited to 36 hours per cardiac event.
Covered under EPSDT if medically
necessary without the limit on hours.
Chiropractic
Not covered.
Covered under EPSDT if medically
necessary (this very rarely happens).
Drug items that do not
require a prescription
(OTC)
Not covered except for items related to prenatal care;
low dose aspirin for preventing cardiac events; treatment
of diabetes, items used for contraception (foams,
devices, etc.).
Coverage of diabetic test strips, and similar items are
described under medical supplies, below. An MCO may
choose to cover any OTC product when the OTC product
is less expensive than the therapeutically equivalent drug
that would require a prescription (a “legend” drug).
Covered using the same provisions as
for recipient under EPSDT in the
standard Medicaid program.
Glasses and contact
lens
Not covered except for aphasia (following removal of
the lens.) Eye exams and treatment related to eye
diseases and testing for eye diseases are a benefit, but
that the refraction component of the exam (a separate
code) is not a benefit.
Covered using the same provisions as
for children under EPSDT in the
standard Medicaid program.
Hearing aids
Not covered.
Hearing screening is covered, but only when part of a
routine health exam. Typically; additional separate
payment is not made for this part of the exam.
Hearing testing by an audiologist or a hearing aid dealer
is not a benefit.
Covered using the same provisions as
for children under EPSDT in the
standard Medicaid program.
HH services
Limited to 100 visits annually – a visit cannot exceed 4
hours.
An MCO has the option of providing these services through
private duty nursing and nursing registry personnel
Covered under EPSDT without the
limitation on the dollar amount or length
of visits.

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
313 | P a g e
Service
Limitations for ABP Recipients (COE 100) for Ages
21 and above
For Ages 19 and 20
Limitations do not apply to ABP
recipients (COE 100) who are Ages
19 or 20 because of EPSDT rules.
Recipients Under Age 19 Are Not
Enrolled In ABP
Medical foods for
errors of inborn
metabolism, or as a
substitute for other
food for weight gain,
weight loss, or
specialized diets, for
use at home by a
recipient.
Not covered.
Covered using the same provisions as
for children under EPSDT in the
standard Medicaid program.
May be subjected to criteria that
assure medical necessity.
Disposable medical
supplies such as
diapers, under pads,
gauzes, gloves,
dressings,
colostomy supplies,
for use at home by a
recipient.
Not covered.
Except for diabetic supplies (reagents, test strips, needles,
test tapes, alcohol swabs, etc.).
However, supplies necessary to utilize oxygen or DME
such as administer oxygen, use nebulizer, clean tracheas
for ventilator use, or assist in treatments such as casts or
splints are covered.
Medical supplies used on an inpatient basis, applied as
part of a treatment in a practitioner’s office, outpatient
hospital, residential facilities, as a HH service, etc. are
covered though often these items are not paid
separately in addition to the payment for the overall
service.
When separate payment is allowed in these settings, the
items are considered covered.
Covered using the same provisions as
for children under EPSDT in the
standard Medicaid program.
May be subjected to criteria that
assure medical necessity.
Pulmonary
rehabilitation
Limited to 36 hours per year.
Covered under EPSDT without the
limitation on the number of visits.
Rehabilitation
and Habilitation
• PT
• OT
• SLP
Rehabilitative services for short-term physical,
occupational, and speech therapies are covered.
Short-term therapy includes therapy services that
produce significant and demonstrable improvement
within a two-month period from the initial date of
treatment.
Extension of short-term therapy beyond the initial two
months may be extended for one period of up to two
months, dependent on the approval of the MCO’S
medical director, only if such services can be expected to
result in continued significant improvement of the
member’s physical condition within the extension period.
Other than the above one-time extension, therapy
services extending beyond the two-month period from
the initial date of treatment are considered long-term
therapy and are not covered.
Covered under EPSDT without the
limitation on duration.

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
314 | P a g e
Service
Limitations for ABP Recipients (COE 100) for Ages
21 and above
For Ages 19 and 20
Limitations do not apply to ABP
recipients (COE 100) who are Ages
19 or 20 because of EPSDT rules.
Recipients Under Age 19 Are Not
Enrolled In ABP
Extended care
hospitals (LTC
hospitals)
Extended care hospitals are not covered. Sometimes these
are referred to as LTC hospitals (certified as acute care
hospitals but focus on care for more than 25 days).
NF LTC stays are not covered by ABP except as a
temporary step down LOC following discharge from a
hospital prior to being discharged to home.
Covered under EPSDT without the
limitations.
Sleep studies
Not covered.
Covered under EPSDT.
Transplants
Limited to 2 per lifetime.
Covered under EPSDT without the dollar
amount limitation.
ABP benefits that may exceed the standard Medicaid Coverage are listed below. The following services
must be provided to ABP recipients, even though these services may not be covered for standard
Medicaid eligible recipients, but may already be required to be provided through an MCO to a member.
Service
Notes
Preventive care, annual physicals, etc.
Under preventive care, a large range of services are covered as part of or in addition
to the preventative care exam. See extended comments on the preventive services
at the end of this document.
Autism spectrum disorder
There are no age or dollar limits for Applied Behavioral Analysis (ABA) benefits.
Disease management
Electroconvulsive therapy
Educational materials and
counseling for a healthy lifestyle
Nutritional counseling
Skilled nursing
Skilled nursing is generally provided only through a HH agency under the Medicaid
FFS program.
However, an MCO can also provide skilled nursing through private duty nursing.
Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
315 | P a g e
Preventive care services, typical of what is found in a commercial insurance plan, are covered for ABP
recipients. Typically, this includes annual exams with all the components appropriate for the age,
condition, and history of the recipient as recommended by various physician specialty associations and
academies.
Additionally, for recipients who are aged 19 and 20, all of the screening and preventive services
available to this age group under the EPSDT provisions are benefits for both ABP recipients and ABP
Exempt recipients.
The requirements related to ABP include assuring the ABP population’s preventive care benefits include
the recommendations of the United States Preventive Services Task Force (USPSTF). These
recommendations are found at the following website:
https://www.uspreventiveservicestaskforce.org/
ABP coverage of preventive services is not intended to be to only those services on the list. Other
preventive services that are generally found in a commercial insurance plan would be covered. The list is
not intended to describe or replace the preventive screening and services available to EPSDT recipients.
The following list includes items that may need special attention or comment, but we have removed
items from the list that are routinely performed in hospitals at the time of birth (e.g., phenylketonuria
screening), and services for children for which the EPSDT screenings and service components are already
more comprehensive. When the website above is updated with new recommendations, those additions
and charges are considered to be part of the requirement.
Service
USPSTF Recommendations
Application to Medicaid
Abdominal aortic aneurysm
screening: men
One-time screening for abdominal aortic aneurysm by
ultrasonography in men ages 65 to 75 years who have
never smoked.
Technically a new requirement, but Medicaid
would not currently deny a claim for this
service.
Alcohol misuse: screening and
counseling
Clinicians screen adults age 18 years or older for alcohol
misuse and provide persons engaged in risky or
hazardous drinking with brief behavioral counseling
interventions to reduce alcohol misuse.
Technically a new requirement, but
practitioners would already be performing
this function during exams.
The counseling component does not have to
include any providers not currently covered
by the Medicaid program.
Anemia screening: pregnant
women
Routine screening for iron deficiency anemia in
asymptomatic pregnant women.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Aspirin to prevent
cardiovascular disease: men
The use of aspirin for men ages 45 to 79 years when the
potential benefit due to a reduction in myocardial
infarctions outweighs the potential harm due to an
increase in gastrointestinal hemorrhage.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
316 | P a g e
Service
USPSTF Recommendations
Application to Medicaid
Aspirin to prevent
cardiovascular disease: women
The use of aspirin for women ages 55 to 79 years when
the potential benefit of a reduction in ischemic strokes
outweighs the potential harm of an increase in
gastrointestinal hemorrhage.
Covered – already in managed care coverage
requirements or as a standard.
Medicaid recipient State Plan service.
Bacteriuria screening: pregnant
women
Screening for asymptomatic bacteriuria with urine
culture in pregnant women at 12 to 16 weeks' gestation
or at the first prenatal visit, if later.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Blood pressure screening in
adults
Screening for high blood pressure in adults age 18 years
and older.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
BRCA screening, counseling
about
Women whose family history is associated with an
increased risk for deleterious mutations in BRCA1 or
BRCA2 genes be referred for genetic counseling and
evaluation for BRCA testing.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Breast cancer preventive
medication
Clinicians discuss chemoprevention with women at high
risk for breast cancer and at low risk for adverse effects
of chemoprevention. Clinicians should inform patients
of the potential benefits and harms of
chemoprevention.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Breast cancer screening
Screening mammography for women, with or without
clinical breast examination, every 1 to 2 years for
women age 40 years and older.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Breastfeeding counseling
Interventions during pregnancy and after birth to
promote and support breastfeeding.
At this time, based on comparison with
commercial plans MAD interprets this as
instruction or counseling that would occur
during the routine prenatal care and
postpartum care; and possibly assessed for
any issues or lack of success by the
pediatrician treating the newborn.
Cervical cancer screening
Screening for cervical cancer in women ages 21 to 65
years with cytology (Pap smear) every 3 years or, for
women ages 30 to 65 years who want to lengthen the
screening interval, screening with a combination of
cytology and human papillomavirus testing every 5
years.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Chlamydial infection screening:
non-pregnant women
Screening for chlamydial infection in all sexually active
non-pregnant young women age 24 years and younger
and for older non-pregnant women who are at increased
risk.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Chlamydial infection
screening: pregnant women
Screening for chlamydial infection in all pregnant women
age 24 years and younger and for older pregnant women
who are at increased risk.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Cholesterol abnormalities
screening: men 35 and older
Screening men age 35 years and older for lipid disorders.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
317 | P a g e
Service
USPSTF Recommendations
Application to Medicaid
Cholesterol abnormalities
screening: men younger than
35
Screening men ages 20 to 35 years for lipid disorders if
they are at increased risk for coronary heart disease.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Cholesterol abnormalities
screening: women 45 and
older
Screening women age 45 years and older for lipid
disorders if they are at increased risk for coronary heart
disease.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Cholesterol
abnormalities
screening: women
younger than 45
Screening women ages 20 to 45 years for lipid disorders
if they are at increased risk for coronary heart disease.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Colorectal cancer screening
Screening for colorectal cancer using fecal occult blood
testing, sigmoidoscopy, or colonoscopy in adults
beginning at age 50 years and continuing until age 75
years. The risks and benefits of these screening methods
vary.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Depression screening: adults
Screening adults for depression when staff-assisted
depression care supports are in place to assure accurate
diagnosis, effective treatment, and follow-up.
Covered – already in managed care coverage
requirements.
The “depression care supports” component
does not have to include any provider types
not currently covered by the Medicaid
program.
Diabetes screening
Screening for Type 2 Diabetes in asymptomatic adults
with sustained blood pressure (either treated or
untreated) greater than 135/80 mm Hg.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Falls prevention in older
adults: exercise or PT
Exercise or PT to prevent falls in community-dwelling
adults age 65 years and older who are at increased risk
for falls.
At this time and based on comparison with
commercial plans, MAD interprets this as
detection of the issue during routine annual
preventive care exams, and referring as
necessary.
The referrals might be to community
programs, home use of TV and DVD
programs, etc. We do not believe the
requirement is to pay for the exercise class or
PT.
Falls prevention in older
adults: vitamin D
Vitamin D supplementation to prevent falls in
community- dwelling adults age 65 years and older who
are at increased risk for falls.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Folic acid
supplementation
All women planning or capable of pregnancy take a
daily supplement containing 0.4 to 0.8 mg (400 to 800
µg) of folic acid.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
318 | P a g e
Service
USPSTF Recommendations
Application to Medicaid
Healthy diet counseling
Intensive behavioral dietary counseling for adult
patients with hyperlipidemia and other known risk
factors for cardiovascular and diet-related chronic
disease. Intensive counseling can be delivered by
primary care clinicians or by referral to other specialists,
such as nutritionists or dietitians.
Coverage of this benefit exceeds the
coverage currently found in Medicaid rules. It
may include covering additional providers
when there is a referral.
May be performed by a physician, dietician,
or other qualifying practitioner
Hepatitis B screening: pregnant
women
Screening for Hepatitis B virus infection in pregnant
women at their first prenatal visit.
Technically a new, requirement, but good
practitioners would already be performing
this function during exams for high risk
individuals.
Hepatitis C virus infection
screening: adults
Screening for Hepatitis C virus (HCV) infection in
persons at high risk for infection. The USPSTF also
recommends offering one-time screening for HCV
infection to adults born between 1945 and 1965.
Technically a new requirement, but
practitioners would already be performing this
function during exams for high risk individuals.
HIV screening: non-pregnant
adolescents and adults
Clinicians screen for HIV infection in adolescents and
adults ages 15 to 65 years. Younger adolescents and
older adults who are at increased risk should also be
screened.
Technically a new requirement, but
practitioners would already be performing this
function during exams for high risk individuals.
HIV screening:
pregnant women
Clinicians screen all pregnant women for HIV, including
those who present in labor who are untested and
whose HIV status is unknown.
Technically a new requirement, but
practitioners would already be performing this
function during exams for high risk individuals.
Intimate partner violence
screening: women of
childbearing age
Clinicians screen women of childbearing age for
intimate partner violence, such as domestic violence,
and provide or refer women who screen positive to
intervention services. This recommendation applies to
women who do not have signs or symptoms of abuse.
Technically a new requirement, but
practitioners would already be performing
this function during exams for high risk
individuals.
Obesity screening and
counseling: adults
Screening all adults for obesity. Clinicians should offer or
refer patients with a body mass index of 30 kg/m
2
or
higher to intensive, multicomponent behavioral
interventions.
Covered – already in managed care coverage
requirements. May be performed by a
physician, dietician, or other qualifying
practitioner
Osteoporosis screening:
women
Screening for osteoporosis in women age 65 years and
older and in younger women whose fracture risk is
equal to or greater than that of a 65-year-old white
woman who has no additional risk factors.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Rh incompatibility screening:
first pregnancy visit
Rh (D) blood typing and antibody testing for all
pregnant women during their first visit for
pregnancy-related care.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
Rh incompatibility screening:
24–28 weeks' gestation
Repeated Rh (D) antibody testing for all unsensitized
Rh (D)- negative women at 24 to 28 weeks' gestation,
unless the biological father is known to be Rh
(D)-negative.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.
STI counseling
High-intensity behavioral counseling to prevent STIs in all
sexually active adolescents and for adults at increased
risk for STIs.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient State Plan service.

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
319 | P a g e
Service
USPSTF Recommendations
Application to Medicaid
Skin cancer behavioral
counseling
Counseling children, adolescents, and young adults ages
10 to 24 years who have fair skin about minimizing their
exposure to ultraviolet radiation to reduce risk for skin
cancer.
Broader requirement than currently exists as a
standard Medicaid recipient service.
Tobacco use counseling and
interventions: non-pregnant
adults
Clinicians ask all adults about tobacco use and provide
tobacco cessation interventions for those who use
tobacco products.
Broader requirement than currently exists as a
standard Medicaid recipient service.
Tobacco use counseling:
pregnant women
Clinicians ask all pregnant women about tobacco use
and provide augmented, pregnancy-tailored counseling
to those who smoke.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient service.
Syphilis screening:
non-pregnant persons
Clinicians screen persons at increased risk for syphilis
infection.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient service.
Syphilis screening: pregnant
women
Clinicians screen all pregnant women for syphilis
infection.
Covered – already in managed care coverage
requirements or as a standard Medicaid
recipient service.

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
320 | P a g e
13.4.2. Alternative Benefit Plan-Exempt Medically Frail Conditions List
Alternative Benefit Plan-Exempt Medically Frail Conditions List
Effective January 1, 2014; Revised August 15, 2014
In order for a COE 100 (Other Adult Group) Medicaid recipient to be exempt from the Alternative Benefit
Plan (ABP), he/she must have a documented medical diagnosis of one of the conditions or services listed
below.
• Acquired Immune Deficiency Syndrome (AIDS)
• ALS (Lou Gehrig’s Disease)
• Angina Pectoris
• Arteriosclerosis Obliterans
• Artificial Heart Valve
• Ascites
• Blindness
• Cancer (current diagnosis/treatment, within five years)
• Cardiomyopathy
• Chronic Substance Use Disorder – refer to the Substance Use Disorder (SUD) Criteria effective
August 2015 (or subsequent replacement version)
• Cirrhosis of the liver
• Compromised immune system
• Coronary insufficiency
• Coronary occlusion
• Crohn’s disease
• Cystic Fibrosis
• Dermatomayositis
• Diabetes (Insulin Dependent)
• Disability: A physical, intellectual or developmental disability that significantly impairs the ability to
perform one or more ADLs – refer to the NF LOC Supplement effective January 1, 2014 (or
subsequent replacement version)
• Friedreich’s Disease
• Hemophilia

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
321 | P a g e
• Hepatitis C (Active)
• HIV+
• Hodgkin’s Disease
• Huntington’s Chorea
• Hydrocephalus
• Intermittent Claudication
• Juvenile Diabetes
• Kidney failure
• Lead poisoning with cerebral involvement
• Leukemia
• Lupus Erythematosus Disseminate
• Malignant tumor (If treated/occurred within previous five years)
• Metastatic cancer
• Motor or sensory aphasia
• Multiple or Disseminated Sclerosis
• Muscular Atrophy or Dystrophy
• Myasthenia Gravis
• Myotonia
• Open heart surgery
• Organ transplant
• Paraplegia or Quadriplegia
• Parkinson’s Disease
• Peripheral Arteriosclerosis (If treated within previous three years)
• Polyarthritis (Periarteritis Nodosa)
• Polycystic kidney
• Posterolateral Sclerosis
• Renal failure
• Serious Mental Illness – refer to the Serious Mental Illness (SMI) Criteria Checklist effective July 27,
2010 (or subsequent replacement version)
• Sickle Cell Anemia

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
322 | P a g e
• Silicosis
• Splenic Anemia (True Banti’s Syndrome)
• Still’s Disease
• Stroke (CVA)
• Syringomyelia
• Tabes Dorsalis (Locomotor Ataxia)
• Terminal illness requiring hospice care
• Thalassemia (Cooley’s or Mediterranean Anemia)
• Topectomy and Lobotomy
• Wilson’s Disease

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
323 | P a g e
13.4.3. Chronic SUD Criteria Checklist
Sources: SMI Criteria 8_19_2015 approved by the Collaborative document, SED Criteria 8_19_2015
approved by the Collaborative document, and Desk Reference to the Diagnostic Criteria from DSM-5.
HSD - March 2016.
SUD Criteria
DSM-V
ICD-9
DSM-V
ICD-10
Description
Substance-Related and Addictive Disorders
292.9
F12.99
Unspecified Cannabis Abuse Disorder
Substance-Related and Addictive Disorders
303.90
F10.20
Alcohol Use Disorder – Moderate, Severe
Substance-Related and Addictive Disorders
304.00
F11.20
Opioid-Related Disorders – Moderate, Severe
Substance-Related and Addictive Disorders
304.20
F14.20
Stimulant-Related Disorder - Cocaine
Substance-Related and Addictive Disorders
304.30
F12.20
Cannabis- Related Disorder - Moderate, Severe
Substance-Related and Addictive Disorders
304.40
F15.20
Stimulant-Related Disorder – Other or unspecified
stimulant
Substance-Related and Addictive Disorders
304.40
F15.20
Stimulant-Related Disorder –
Amphetamine-type substance
Substance-Related and Addictive Disorders
304.50
F16.20
Hallucinogen-Related Disorder- Other
Hallucinogen Use
Substance-Related and Addictive Disorders
304.60
F16.20
Hallucinogen-Related Disorder – Phencyclidine Use
Disorder –
Substance-Related and Addictive Disorders
304.90
F19.20
Other (or Unknown) Substance-Related and
Addictive Disorders

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
324 | P a g e
13.4.4. SMI Criteria Checklist
Serious Mental Illness (SMI) determination is based on the age of the individual, functional impairment, duration of
the disorder and the diagnosis. Adults must meet all of the following four criteria:
□ 1. Age: Must be an adult 18 years of age or older.
□ 2. Diagnoses: Have one of the diagnoses as defined under the current American
Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. The
diagnosis would need to have been determined within the prior 12 months by an
appropriately credentialed and licensed professional.
• Diagnoses codes and descriptions that are found in
Appendix A and Appendix B of this document are those
providing a primary reason for receiving public system BH
services.
□ 3. Functional Impairment: The disturbance is excessive and causes clinically significant
distress or impairment in social, occupational, or other important areas of
functioning.
□ 4. Duration:
□ The disability must be expected to persist for six months or longer.
Person must meet SMI criteria and at least one of the following in A or B:
□ A. Symptom Severity and Other Risk Factors
□ Significant current danger to self or others or presence of active symptoms
of a SMI.
□ Three or more emergency room visits or at least one
psychiatric hospitalization within the last year.
□ Individuals with substance use disorder that complicates SMI and results in
worsened intoxicated/withdrawal complications, bio medical conditions,
emotional/behavior/cognitive conditions.
□ Person is experiencing trauma symptoms related to sexual assault,
domestic violence or other
traumatic event.
□ B. Co- Occurring Disorders
□ Substance Use Disorder (SUD) diagnosis and
any mental illness that affects functionality.
□ SMI or SUD and potentially life-threatening chronic
medical condition (e.g., diabetes, HIV/AIDS, hepatitis).
□ SMI or SUD and Developmental Disability.

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
325 | P a g e
13.4.5. SMI-SED Criteria
SMI-SED Category
DSM-V
ICD-9
DSM-V
ICD-10
Description
Neurodevelopmental Disorders
299.00
F84.0
Autism Spectrum Disorder
Neurodevelopmental Disorders
307.22
F95.1
Motor Disorder – persistent (chronic) motor or vocal tic
Neurodevelopmental Disorders
307.23
F95.2
Tourette’s Disorder
Neurodevelopmental Disorders
307.3
F98.4
Stereotypic Movement Disorder
Neurodevelopmental Disorders
314.00
F90.0
Attention Deficit/Hyperactivity Disorder (ADHD): Predominantly
Neurodevelopmental Disorders
314.01
F90.1
ADHD: Predominantly
Neurodevelopmental Disorders
314.01
F90.2
ADHD: Combined
Neurodevelopmental Disorders
314.01
F90.8
ADHD: Other Specified
Neurodevelopmental Disorders
314.01
F90.0
ADHD: Unidentified
Schizophrenia Spectrum and other Psychotic Disorders
293.81
F06.2
With delusions
Schizophrenia Spectrum and other Psychotic Disorders
293.82
F06.0
With hallucinations
Schizophrenia Spectrum and other Psychotic Disorders
295.40
F20.81
Schizophreniform Disorder
Schizophrenia Spectrum and other Psychotic Disorders
295.70
F25.0
Bipolar type
Schizophrenia Spectrum and other Psychotic Disorders
295.70
F25.1
Depressive type
Schizophrenia Spectrum and other Psychotic Disorders
295.90
F20.9
Schizophrenia
Schizophrenia Spectrum and other Psychotic Disorders
297.1
F22
Delusional Disorder
Schizophrenia Spectrum and other Psychotic Disorders
298.8
F28
Other Specified Schizophrenia Spectrum and Other Psychotic
Schizophrenia Spectrum and other Psychotic Disorders
293.89
F06.01
Catatonia Associated with Another Mental Disorder
Schizophrenia Spectrum and other Psychotic Disorders
298.9
F29
Unspecified Schizophrenia Spectrum and Other Psychotic
Schizophrenia Spectrum and other Psychotic Disorders
301.22
F21
Schizotypal (Personality) Disorder
Bipolar and Related Disorders
293.83
F06.33
Bipolar and Related Disorders due to another medical condition.
Specify.
Bipolar and Related Disorders
293.83
F06.34
Bipolar and Related Disorders due to another medical
Bipolar and Related Disorders
296.40
F31.9
Unspecified
Bipolar and Related Disorders
296.41
F31.11
Mild
Bipolar and Related Disorders
296.42
F31.12
Moderate
Bipolar and Related Disorders
296.43
F31.13
Severe
Bipolar and Related Disorders
296.44
F31.2
With psychotic features
Bipolar and Related Disorders
296.45
F31.73
In partial remission
Bipolar and Related Disorders
296.46
F31.74
In full remission
Bipolar and Related Disorders
296.50
F31.9
Unspecified
Bipolar and Related Disorders
296.51
F31.31
Mild

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
326 | P a g e
SMI-SED Category
DSM-V
ICD-9
DSM-V
ICD-10
Description
Bipolar and Related Disorders
296.52
F31.32
Moderate
Bipolar and Related Disorders
296.53
F31.4
Severe
Bipolar and Related Disorders
296.54
F31.5
With psychotic features
Bipolar and Related Disorders
296.55
F31.75
In partial remission
Bipolar and Related Disorders
296.56
F31.76
In full remission
Bipolar and Related Disorders
296.89
F31.81
Bipolar II Disorder
Bipolar and Related Disorders
296.80
F31.9
Unspecified Bipolar and related disorder
Depressive Disorders
296.99
F34.8
Disruptive Mood Dysregulation Disorder
Depressive Disorders
293.83
F06.31
Bipolar and Related Disorders due to another medical condition
Depressive Disorders
293.83
F06.32
Bipolar and Related Disorders due to another medical condition
Depressive Disorders
293.83
F06.34
Bipolar and Related Disorders due to another medical condition
Depressive Disorders
296.20
F32.9
Unspecified
Depressive Disorders
296.21
F32.0
Mild
Depressive Disorders
296.22
F32.1
Moderate
Depressive Disorders
296.23
F32.2
Severe
Depressive Disorders
296.24
F32.3
With psychotic features
Depressive Disorders
296.25
F32.4
In partial remission
Depressive Disorders
296.26
F32.5
In full remission
Depressive Disorders
296.30
F33.9
Unspecified
Depressive Disorders
296.31
F33.0
Mild
Depressive Disorders
296.32
F33.1
Moderate
Depressive Disorders
296.33
F33.2
Severe
Depressive Disorders
296.34
F33.3
With psychotic features
Depressive Disorders
296.35
F33.41
In partial remission
Depressive Disorders
296.36
F33.42
In full remission
Depressive Disorders
300.4
F34.1
Persistent Depressive Disorder
Depressive Disorders
311
F32.8
Other Specified Depressive Disorder
Depressive Disorders
311
F32.9
Unspecified Depressive Disorder
Depressive Disorders
625.4
N94.3
Premenstrual Dysphoric Disorder
Anxiety Disorders
293.84
F06.4
Anxiety Disorder due to another medical condition
Anxiety Disorders
300.00
F41.9
Unspecified Anxiety Disorder
Anxiety Disorders
300.01
F41.0
Panic Disorder
Anxiety Disorders
300.02
F41.1
Generalized Anxiety Disorder

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
327 | P a g e
SMI-SED Category
DSM-V
ICD-9
DSM-V
ICD-10
Description
Anxiety Disorders
300.09
F43.9
Other Specified Anxiety Disorder
Anxiety Disorders
300.22
F40.00
Agoraphobia
Anxiety Disorders
300.23
F40.10
Social Anxiety Disorder (Social Phobia)
Anxiety Disorders
309.21
F93.0
Separation Anxiety Disorder
Obsessive-Compulsive Related Disorders
294.8
F06.8
Obsessive-Compulsive Disorder due to another medical
condition
Obsessive-Compulsive Related Disorders
300.3
F42
Obsessive-Compulsive Disorder, Hoarding Disorder, Other
Specified Obsessive-Compulsive
Obsessive-Compulsive Related Disorders
300.7
F45.22
Body Dysmorphic Disorder
Obsessive-Compulsive Related Disorders
312.39
F63.3
Trichotillomania (Hair-Pulling Disorder)
Obsessive-Compulsive Related Disorders
698.4
L98.1
Excoriation (Skin-Picking) Disorder
Trauma-and Stressor Related Disorders
308.3
F43.0
Acute Stress Disorder
Trauma-and Stressor Related Disorders
309.0
F43.21
With depressed mood
Trauma-and Stressor Related Disorders
309.24
F43.22
With anxiety
Trauma-and Stressor Related Disorders
309.28
F43.23
With anxiety and depressed mood
Trauma-and Stressor Related Disorders
309.3
F43.24
With disturbance of conduct
Trauma-and Stressor Related Disorders
309.4
F43.25
With mixed disturbance of emotions
Trauma-and Stressor Related Disorders
309.81
F43.10
Posttraumatic Stress Disorder
Trauma-and Stressor Related Disorders
309.89
F43.8
Other specified trauma and stressor-related
Trauma-and Stressor Related Disorders
309.9
F43.9
Unspecified trauma and stressor-related
Trauma-and Stressor Related Disorders
313.89
F94.1
Trauma and stressor-related Disorder
Trauma-and Stressor Related Disorders
313.89
F94.2
Disinhibited Social Engagement Disorder
Dissociative Disorders
300.12
F44.0
Dissociative Amnesia
Dissociative Disorders
300.13
F44.1
With dissociative fugue
Dissociative Disorders
300.14
F44.81
Dissociative Identity Disorder
Dissociative Disorders
300.15
F44.89
Other Specified Dissociative Disorder
Dissociative Disorders
300.15
F44.9
Unspecified Dissociative Disorder
Dissociative Disorders
300.6
F48.1
Depersonalization/Derealization Disorder
Somatic Symptom and Related Disorders
300.11
F44.4
Conversation Disorder (Functional Neurological Symptom
Disorder. Specify: with weakness or paralysis; or with abnormal
movement; or with swallowing symptoms
Somatic Symptom and Related Disorders
300.11
F44.5
Conversation Disorder (Functional Neurological
Symptom) Disorder. Specify: With attacks of seizures; or with
special sensory
Somatic Symptom and Related Disorders
300.11
F44.6
Conversation Disorder (Functional Neurological Symptom)
Somatic Symptom and Related Disorders
300.11
F44.7
Conversation Disorder (Functional Neurological Symptom)

Section 13: Alternative Benefit
Package
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
328 | P a g e
SMI-SED Category
DSM-V
ICD-9
DSM-V
ICD-10
Description
Somatic Symptom and Related Disorders
300.19
F68.10
Factitious Disorder Imposed on Self, Factitious Disorder Imposed
Somatic Symptom and Related Disorders
300.7
F45.21
Illness Anxiety Disorder
Somatic Symptom and Related Disorders
300.82
F45.1
Somatic Symptom Disorder
Somatic Symptom and Related Disorders
300.89
F45.8
Other Specified Somatic Symptom and
Feeding and Eating Disorders
307.1
F50.01
Anorexia Nervosa – Restricting type
Feeding and Eating Disorders
307.1
F50.02
Anorexia Nervosa – Binge-eating/Purging
Feeding and Eating Disorders
307.50
F50.9
Unspecified Feeding and Eating Disorders
Feeding and Eating Disorders
307.51
F50.2
F50.8
Bulimia Nervosa (F50.2)
Binge-eating Disorder (F50.)
Feeding and Eating Disorders
307.52
F98.3
In children
Feeding and Eating Disorders
307.52
F50.8
In adults
Disruptive, Impulse Control and Conduct
312.33
F63.1
Pyromania
Disruptive, Impulse Control and Conduct
312.34
F63.81
Intermittent Explosive Disorder
Disruptive, Impulse Control and Conduct
312.81
F91.1
Childhood-onset type
Disruptive, Impulse Control and Conduct
312.89
F91.8
Other Specified Disruptive Impulse
Disruptive, Impulse Control and Conduct
312.9
F91.9
Unspecified Disruptive, Impulse Control
Disruptive, Impulse Control and Conduct
Disorders
313.81
F91.3
Oppositional Defiant Disorder –
Specify current severity: Mild
Cyclothymic Disorder
301.13
F34.0
Cyclothymic Disorder
Persistent Depressive Disorder
300.4
F34.1
Persistent Depressive Disorder - Dysthymia
Personality Disorders [For which there is an evidence
based clinical intervention available]
301.83
F60.3
Borderline Personality Disorder
Substance-Related and Addictive Disorders
292.9
F12.99
Unspecified Cannabis Abuse Disorder
Substance-Related and Addictive Disorders
303.90
F10.20
Alcohol Use Disorder – Moderate, Severe
Substance-Related and Addictive Disorders
304.00
F11.20
Opioid-Related Disorders – Moderate
Substance-Related and Addictive Disorders
304.20
F14.20
Stimulant-Related Disorder - Cocaine
Substance-Related and Addictive Disorders
304.30
F12.20
Cannabis- Related Disorder - Moderate
Substance-Related and Addictive Disorders
304.40
F15.20
Stimulant-Related Disorder – Other or
Substance-Related and Addictive Disorders
304.40
F15.20
Stimulant-Related Disorder – Amphetamine
Substance-Related and Addictive Disorders
304.50
F16.20
Hallucinogen-Related Disorder – Other Hallucinogen Use
Substance-Related and Addictive Disorders
304.60
F16.20
Hallucinogen-Related Disorder – Phencyclidine Use Disorder –
Substance-Related and Addictive Disorders
304.90
F19.20
Other (or Unknown) Substance-Related and Addictive Disorders
– moderate, severe
Sources: SMI Criteria 8_19_2015 approved by the Collaborative document, SED Criteria 8_19_2015 approved by
the Collaborative document, and Desk Reference to the Diagnostic Criteria from DSM-5.

Section 14: School-Based Health
Centers
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
329 | P a g e
14. School-Based Health Centers
14.1. General Information
SBHCs are a vital part of the health care delivery system in New Mexico. SBHCs are comprehensive
primary health care centers on or adjacent to school grounds that provide PH and BH services to
students and community members. SBHCs also promote positive health behaviors and health care
literacy by increasing health knowledge and decision-making skills in the students they serve. By offering
a range of health care services in school settings, SBHCs simultaneously increase access to care and
decrease the amount of classroom time missed by students leaving campus for care in traditional
settings. As a result, SBHCs can positively impact academic participation as well as health outcomes.
The HSD/MAD supports SBHCs by providing Medicaid reimbursement through MCOs, to SBHCs and their
medical providers for Medicaid eligible members as appropriate. A working partnership between the
New Mexico Department of Health’s Office of School and Adolescent Health (DOH/OSAH) and HSD/MAD
certify that SBHCs meet State quality standards. HSD/MAD contracts with DOH/OSAH for the provision
of funding, leadership, support and oversight to SBHCs across New Mexico. SBHCs may choose to
contract for those provisions through the New Mexico DOH/OSAH.
This policy uses the following terms which take on a unique application to the SBHC program.
Sponsorship - SBHCs contracting with DOH/OSAH do so under either medical sponsorship (i.e., an FQHC
or medical group) or non-medical sponsorship (i.e., an educational cooperative). A Sponsoring Entity
provides its designated SBHC(s) one or more of the following: funding, staffing, medical oversight,
liability insurance, and billing support; and
SBHC Provider Type - SBHCs may apply for approval for HSD/MAD Certification for Medicaid billing as
either a Provider Type 321 (SBHC) or Provider Type 313 (FQHC):
• Provider Type 313 – FQHC:
o An FQHC that meets the definition of a SBHC according to Social Security Act Section 2110 (c) (9)
and is certified by CMS as a FQHC, meets State requirements of an eligible SBHC provider
according to NMAC 8.302.1.10; and
o FQHC Sponsored SBHCs may also contract with the DOH/OSAH for the provision of funding,
leadership, support and oversight.
• Provider Type 321 – Independent/Non-Medical Entity Sponsored:

Section 14: School-Based Health
Centers
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
330 | P a g e
o This type of SBHC must contract with DOH/OSAH for the provision of funding, leadership,
support, and oversight.
o SBHCs operating under provider type 321 must do so in collaboration with DOH/OSAH and
HSD/MAD. Although the facilities are not licensed as required by the Medicaid General Provider
Policy (NMAC 8.302.1.10) to meet the definition of an “eligible provider,” the sites participate
under a limited scope of services they are also subject to the New Mexico Standards and
Benchmarks for SBHCs and must pass a periodic on-site review conducted by DOH/OSAH.
If a SBHC sponsored by an FQHC is enrolled as a different provider type than an FQHC, the MCO
shall reimburse according to the SBHC provider type.
SBHC Liaison: By January 1
st
of each year the MCO will provide an update to HSD with the name of their
designated SBHC Liaison. The SBHC Liaison is the primary contact and will ensure the following:
• Participate in quarterly MCO SBHC Advisory Committee meetings;
• Conduct SBHC recertification site reviews for medically sponsored SBHCs;
• Receive, facilitate, respond and/or provide referrals to subject matter experts within the
MCO for SBHC education, inquiries and general communications with SBHC
stakeholders; and
• Collaborate with HSD/MAD, DOH/OSAH, contractors, SBHC Sponsors and Site
Coordinators.
DOH/OSAH and HSD/MAD will work collaboratively on program planning, policy development,
interagency coordination, and education related to health care services, including primary care, BH, and
dental services, provided by the SBHC and other SBHC programs.

Section 14: School-Based Health
Centers
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
331 | P a g e
14.2. Initial Certification Process
SBHCs and sponsoring entities interested in becoming certified for the first time must contact
DOH/OSAH to begin the contracting process. To complete an initial onsite review and receive a MAD
Provider Medicaid Eligibility Letter DOH/OSAH will provide interested parties with the following:
• Standards and Benchmarks;
• SBHC Site Review Self-Assessment; and
• Technical assistance as needed
Any SBHC site that experiences a lapse in eligibility, validation or is an additional SBHC to the Sponsoring
Entity is subject to the same process.
• Initial On-Site Review:
o DOH/OSAH will conduct an initial on-site review with the SBHC staff and sponsor to include
discussion of findings, questions, concerns, and recommendations;
• DOH/OSAH will provide HSD/MAD with documentation of the initial on-site review
o HSD/MAD will issue a letter to the SBHCs, sponsor, DOH/OSAH, and the MCOs within 10 to 15
business days after completion of site review indicating whether the SBHC has passed or failed
the review:
• If the SBHC/Sponsor passed, the HSD/MAD letter will include the effective date the SBHC
and Sponsor are eligible to begin billing Medicaid; and
• If the SBHC/Sponsor failed, the HSD/MAD letter will include the reasons and requirements
the SBHC must complete to pass the certification/recertification process. If the
SBHC/Sponsor is not able to correct the noted deficiencies within 10 business days from
receipt of letter, HSD/MAD will send notification to the SBHC/Sponsor requesting a
corrective action plan (CAP).
• The CAP must address each noted deficiency, action steps required to correct the
deficiency, and the desired outcome with a due date;
• The SBHC/Sponsor will have 60 calendar days upon receipt of the notification to
implement the CAP and correct all deficiencies. Evidence of the corrections must be
submitted to HSD/MAD before or on the 60th calendar day;
• HSD/MAD will determine what documentation and in what format is required based on
the CAP and resolution of deficiencies;

Section 14: School-Based Health
Centers
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
332 | P a g e
• HSD/MAD will send a letter of certification/recertification to the SBHC, sponsor,
DOH/OSAH, and the MCOs within five business days of resolution of deficiencies and
completion of the CAP; and
If the CAP is not completed and deficiencies are not resolved, HSD/MAD will collaborate with
DOH/OSAH to determine if certification/recertification is possible and next steps.
• Centennial Care Enrollment:
o SBHCs must obtain an individual NPI from CMS.
o SBHCs must submit a MAD 335 application to Conduent as either provider type 313 or provider
type 321:
• SBHCs with Provider Type 313 must submit a copy of documentation from CMS certifying
the center as an FQHC; and
• SBHCs with Provider Type 321 must submit a copy of the MAD Medicaid Eligibility Letter.
o Upon completion of the successful enrollment with HSD/MAD, SBHCs will finalize agreements
with MCOs:
• SBHCs will also affiliate every rendering provider with the SBHC in the New Mexico Medicaid
System;
• It is the SBHC’s responsibility to contact each MCO; and
• MCOs are required to make best efforts to contract with SBHCs per Section subsection
4.8.13.1 of the Agreement.
14.3. Recertification Process
The HSD/MAD letter of New Mexico Medicaid Eligibility is issued for a period of three years and is
subject to revocation in the event that HSD/MAD becomes aware of loss of appropriate licensure(s) or
significant deviation from the Standards and Benchmarks. Recertification must be conducted prior to
the expiration of the initial certification and every three years after.
• Provider Type 321s with Non-Medical Sponsorship Recertification Process review will be conducted
by the DOH/OSAH Site Review Team no later than six weeks before the expiration of current
certification.
o DOH/OSAH will schedule the site review through the SBHC’s Sponsoring Entity.

Section 14: School-Based Health
Centers
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
333 | P a g e
o DOH/OSAH shall ensure the Sponsoring Entity has access to the most recent copy of the
Standards and Benchmarks, SBHC Site Review Self-Assessment, and the Site Review Guide
within one month of the site review.
o The DOH/OSAH site review will be conducted as outlined in Certification Process above.
• The recertification process for Medically Sponsored SBHCs contracted with DOH/OSAH is the
responsibility of the MCOs.
o In January of each year, no later than the first quarterly meeting of the MCO SBHC Advisory
Committee, HSD/MAD will provide the MCOs with a list of medically sponsored DOH/OSAH
contracted SBHCs with expiring certifications, including recertification due dates, and the MCO
responsible for performing the on-site review.
o The MCO will schedule the on-site review with the Medical Sponsor for no later than six weeks
before the expiration of current certification.
o The review may be conducted remotely for additional SBHC sites. There is no requirement for an
on-site visit for every individual SBHC under the same sponsoring entity.
o In preparation of the on-site review the MCO shall:
▪ Within one month of the site review ensure the Medical Sponsor has access to the most
recent copy of the Standards and Benchmarks, SBHC Site Review Self-Assessment, and the
Site Review Guide.
▪ Instruct the Medical Sponsor and SBHC to prepare to make available hard or electronic
copies of:
• Attestation Statement for Federally Qualified Health Centers (Exhibit 177) or copy of
Acknowledgment of Ability to Comply with New Mexico Standards and Benchmarks
for School-based Health Centers.
• Facility Documentation:
o Facility licenses,
o Evidence of other licensure and/or certification by appropriate jurisdictional
agencies as requested;
o The latest fire inspection report by the fire authority with jurisdiction over the
site;
o Valid license from the New Mexico Board of Pharmacy;
o Current Clinical Laboratory Improvement Amendments (CLIA) certificate;

Section 14: School-Based Health
Centers
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
334 | P a g e
o Evidence of compliance with such standards such as the requirement for “No
Smoking” signs, “Handicap Accessibility” signs, and the posting of appropriate
licenses
• SBHC Policy and Procedure Manual, including the policies and procedures described
in the Standards and Benchmarks;
• Complaint logs, Material Safety Data Sheets (MSDS), pharmacy logs, and laboratory
logs;
• Access to Medical Records;
• Other materials that may be specified by the Site Review Team;
• Staff Documentation:
o Current license, registration or certificate of each staff member for which a
license, registration, or certification is required by the State of New Mexico;
o Health training certificates and logs of all staff;
• Completed SBHC Site Review Self-Assessment for every SBHC;
o Review the completed SBHC Site Review Self-Assessment for completeness and
discrepancies;
o MCO’s should reschedule the onsite review if SBHC Site Review Self-Assessment
is not provided 1 week prior or is incomplete;
o Recertification Onsite Review shall:
▪ Meet with the clinic staff and sponsor representatives in person, to discuss the site review
process;
▪ Conduct a visual review and use the HSD/MAD Electronic Assessment Tool to determine
adherence to the SBHC Standards and Benchmarks;
▪ Medical Record Review of the designated MCOs members shall be conducted per the
HSD/MAD training guidelines; and
▪ Conduct an exit interview with the staff and sponsor to discuss findings, questions,
concerns, and recommendations. Sponsor will sign the Electronic Assessment Tool
Summary and a verbal indication will be given of the certification status.
o After Onsite Review Activities:
▪ The MCO will deliver the site review documentation to HSD/MAD within 10
business days. This documentation includes:

Section 14: School-Based Health
Centers
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
335 | P a g e
o All SBHC Site Review Self-Assessment(s)
o Electronic Assessment Tool- Scoring
o Electronic Assessment Tool- Summary
▪ HSD/MAD will compile the data and make the final determination for
recertification. HSD final determination will be demonstrated by the MAD
Medicaid Eligibility Letter. This letter will be distributed by HSD/MAD directly to
the Sponsoring Entity and MCOs.
▪ If the SBHC/Sponsor failed, HSD/MAD will follow the CAP process as outlined in
the initial certification section.
14.4. Adolescent Confidential Services and Suppression of Explanation of Benefits (EOBs)
SBHC services are subject to Federal and New Mexico state law. There are a number of circumstances in
which an adolescent (an un-emancipated minor) may consent to receive services without parental
consent, including the following:
• Treatment for Sexually Transmitted Diseases:
Under Section 24-1-9 (capacity to consent to examination and treatment for a sexually transmitted
disease), any person regardless of age has the capacity to consent to an examination and treatment
by a licensed physician for any sexually transmitted disease; however, under Section 24-1-9.4,
disclosure of the test results is authorized “to the subject of the test or the subject’s legally AR,
guardian or legal custodian.”
• Pregnancy Examination and Diagnosis:
Under Section 24-1-13 (pregnancy; capacity to consent to examination and diagnosis), any person,
regardless of age, has the capacity to consent to an examination by a licensed physician for
pregnancy.
• Family Planning Services:
Under Section 24-8-5 (prohibition against imposition of standards and requirements as prerequisites
for receipt of requested family planning services) there are no prerequisites for parental consent to
obtain family planning services.
• BH Services:

Section 14: School-Based Health
Centers
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
336 | P a g e
Under Section 32A-6-14 (treatment and habilitation of children; liability), parental consent is not
required to receive “individual psychotherapy, group psychotherapy, guidance, counseling or other
forms of verbal therapy that do not include any aversive stimuli or substantial deprivations.”
MCO contracts require the MCOs to adopt and implement written confidentiality policies and
procedures that conform to state and Federal laws and regulations that:
o Preserve adolescent members’ confidentiality rights; and
o Honor adolescent members’ rights to receive confidential services under HIPAA and other State
and Federal confidentiality provisions.
MCOs are required to adopt and implement policies and procedures unique to SBHCs beyond State and
Federal laws and regulations that:
• Suspend the distribution of EOBs and any other communication, written or electronic, to the
guardian for all confidential services provided at SBHCs. This would include lab and test results,
patient satisfaction surveys, patient portal records, and any other communication that would
result in a breach of confidentiality related to adolescent confidential services.

Section 15: I/T/U
Revision dates: August 15, 2014; March 3, 2015
Effective dates: January 1, 2014
337 | P a g e
15. Indian Health Services, Tribal Health Providers, and Urban Indian Providers (I/T/U)
15.1. FQHC/Tribal 638 Claims Processing (Alamo and Pine Hill)
MCOs must configure their systems to pay claims either off of the COBA (Coordination of Benefits
Agreement) file or paper claims and pay up to the Medicare OMB rate for the applicable year.
For IHS and Tribal 638 facilities when there is a Medicare reimbursement for services that are not
included in the OMB rate, for services billed on a UB claim form (used by hospitals and facilities),
Medicaid pays the co-insurance and deductible calculated by Medicare regardless of the revenue code
billed. These Medicare crossover claims may also include specific services such as rehabilitation services,
flu shots, and supplies. After Medicare payment is made, reimburse the Indian Health Services and
Tribal 638 facilities for the full co-insurance and deductible calculated by Medicare regardless of the
service or revenue code used.
For services provided to recipients with primary medical coverage by a third party, such as an insurer or
other third party (excluding Medicare) who may be liable for the medical bill, Medicaid reimbursed the
provider the Medicaid Inpatient or Outpatient OMB rate for that calendar year less the third-party
payment.
Services must be delivered in locations identified in Medicaid policy or locations consistent with
professional standards of practice. Services locations outside the IHS or Tribal 638 facilities may include
locations such as NFs, schools, teen and wellness centers, chapter houses, homes, and non-IHS/Tribal
638 hospitals.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
338 | P a g e
16. Fair Hearings
16.1. Administrative Hearings
Reference: 8.308.15 NMAC Grievances and Appeals
Under managed care rules, the MCO must have a grievance process and an appeal process for members
as described in the above rule. The MCO must be familiar with the provisions of the rule and have
procedures in place that follow the rule.
All rules and requirements related to the appeal and hearing processes must be followed from the initial
adverse determination, which would typically either be the denial or reduction of a requested service or
LOC, or the discontinuation or reduction of an existing service or LOC. However, the right to an appeal
and hearing process is also required when a new decision is made, even if that action is to increase or
extend a benefit and, therefore, may not initially appear to be “adverse.”
The member may still appeal an action that has been taken to increase or extend the same benefit. For
example, if the member receives increased PCS hours, but the hours are less than what the provider
requested or less than what the member feels are needed, the member can still appeal that action; in
the sense that the action is considered an adverse action, if that is how the member perceives it. When
the notice is sent, it should be labeled as the Notice of Action.
Any instance for which an approval, authorization, LOC, frequency, or other amount is not approved to
the extent requested by the provider or member is considered an adverse action and may be referred to
as such.
Time limits requiring advance notice prior to the MCO taking an adverse action against a member’s
existing service or LOC, (including actions by a member’s receiving MCO that did not authorize the
original service) are all important and must be followed. It is from that initial adverse action, and the
adverse action that a receiving MCO may take, that all the remaining provisions of the notification,
rights to continuation of a benefit, MCO appeal, and HSD administrative hearing process may follow.
Therefore, all notices to the member must accurately advise the member of his or her appeal rights, and
all notices must adhere to the time frames specified.
Grievances
The grievance process should not be confused with the appeal and administrative hearing processes.
The appeal process can eventually lead to an HSD administrative hearing before the HSD Fair Hearings
Bureau (FHB). The grievance process is an internal resolution process within the MCO. The MCO must
always make it clear to the member when to file an appeal rather than to file a grievance. A member

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
339 | P a g e
may file an appeal if he or she is unsatisfied with the outcome of the grievance process as long as the
member is still within the time requirement for filing an appeal. However, the appeal is made on the
basis of the Notice of Action and not an appeal on the grievance resolution. Filing a grievance in no way
alters or extends the time that the member has to file an appeal.
Provider Appeal
The provider appeal process is included in the above rule. This process exists only within the member’s
MCO. While HSD does have a provider hearing process for some fee-for-service provider issues, the
MCO provider appeal process does not lead to an HSD administrative hearing before the FHB.
Member Appeal
The member MCO appeal process is included in the above rule. The member MCO appeal process can
eventually lead to an HSD administrative hearing before the FHB.
The MCO must assure that the member is informed of all rights regarding the right to an appeal and the
MCO appeal process, and as applicable, an HSD administrative hearing process. The MCO must follow all
the requirements of the rule related to the MCO appeal process.
In order to consolidate the requirements of state and Federal rules, MAD has developed checklists for
notices and letters contained in the Appendix.
16.2. The Member’s HSD Administrative Hearing
Reference: 8.352.2 NMAC Claimant Hearings
When the member has exhausted his or her MCO appeal process, and if the member acts within the
time frame specified in 8.308.15 NMAC and 8.352.2 NMAC, the member has the right to file a request
for an HSD administrative hearing with the FHB. Within HSD, the terms Administrative Hearing and Fair
Hearing mean the same thing.
Once a member receives an MCO appeal final decision and the member elects to request an HSD
administrative hearing, the member and MCO are governed by the NMAC 8.352.2 rule. The process the
member and MCO are to follow for an HSD administrative hearing is detailed in this rule.
Once a member’s request for an HSD administrative hearing has been received by the FHB, and if the
member was approved for a continuation of his or her benefit during the MCO appeal process, the
member’s continuation of the benefit remains in place until an HSD administrative hearing final decision
is rendered or the member requests the termination of continuation of the benefit.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
340 | P a g e
Once a member notifies the FHB, the FHB acknowledges receipt of the request to the member and
notifies the MAD Administrative Hearing Unit (AHU) and the MCO in writing of the request within
relevant information about the member, including the member’s self-identified issues. MAD AHU
maintains a log of all HSD administrative hearing requests. Once the FHB assigns an administrative law
judge (ALJ), the ALJ will send out a scheduling notice of the HSD administrative hearing date, time, and
call in number to all parties. Parties to the hearing may include legal counsel or other ARs. Unless an
accommodation is requested and approved by the ALJ, all HSD administrative hearings are conducted
telephonically. The assigned ALJ is responsible for the oversight of the HSD administrative hearing
process, including conducting the actual hearing.
The formal rules of evidence and civil procedure do not apply to the HSD administrative hearing
proceedings. Relevant evidence is submitted into the hearing record and testimony is furnished during
the proceedings in an orderly, but less formal, manner. However, the record created for the HSD
administrative hearing is a legal document and is the record which forms the basis for decisions made by
a New Mexico district court, if the member should see redress after his or her HSD administrative
hearing final decision has been rendered. The evidence and testimony entered into the hearing record
forms the official HSD record and only information contained within the hearing record can be admitted
into evidence in a New Mexico district court appeal; HSD, the member or the MCO cannot add to or
delete from this hearing record after the close of the actual HSD administrative hearing. The State
district court is allowed to set aside the HSD administrative final decision only if it finds the decision to
be arbitrary, capricious or an abuse of discretion, not supported by substantial evidence in the hearing
record as a whole, or otherwise not in accordance with the law.
SOE
The MCO must provide MAD with a SOE within 7 calendar days after receipt of a request, but no later
than 15 business days prior to the initial scheduled hearing. The SOE must contain copies of all
documentation used to make the decision, and it must explain the reasons for the benefit determination
and address all of the member’s concerns.
Within the specified time frames, the MCO must submit an electronic copy of the SOE to the MAD AHU
through the DMZ. The SOE must include relevant NMAC rules, demographic information, summary of
issues, clinical and administrative documentation, correspondence, etc. MAD will be responsible for
completing the member demographic section of the summary.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
341 | P a g e
The SOE must refer to all relevant State and Federal statutes, rules, and other criteria used to make the
decision. Upon request and no later than 7 calendar days after receiving the request, the MCO must
provide the member and/or the member’s representative (with written consent of the member) the
member’s case file and provide copies of documents contained therein without charge.
Final Decision
At the conclusion of the HSD administrative hearing, the ALJ prepares a summary of facts and his or her
recommendation and submits this and the entire hearing record to MAD AHU. The record of the HSD
administrative hearing is reviewed by the Director of MAD or his or her designee and the final decision
rests with the Director or his or her designee. Under Federal law, the entire HSD administrative process
must be completed within 90 calendar days of the date the member requested an HSD administrative
hearing. The member and other parties to the hearing are provided with the HSD administrative hearing
final decision.
The member has 30 calendar days to file an appeal of the HSD administrative hearing final decision with
the appropriate New Mexico district court. The filing of a Notice of Appeal shall not stay the
enforcement of the HSD administrative hearing final decision. The member may seek a stay upon a
motion to the court or the member may request the MAD Director or designee to stay the HSD
administrative hearing final decision while the adverse action is on appeal in a New Mexico district
court. If the court orders a stay, the MCO will maintain the benefit at issue in accordance with the State
district court’s order. If the New Mexico district court’s final decision is in favor of HSD and the member
continued utilizing his or her benefit during the district court appeal process, see 8.352.2.19 NMAC for
the repayment process.
Important Aspects of the Process
One of the HSD’s primary goals related to its administrative hearings is to have all MCO’s implement
procedures that are consistent with NMAC and MAD rules and that will be practiced and adhered to by
all parties involved. The following are focus points for process improvement:
• Timeliness in all phases of the process;
• Maintain member confidentiality and protect PHI;
• Emphasize maintenance of complete and organized files;
• Emphasize importance of documentation; and

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
342 | P a g e
• Accountability
The MCOs are key players in this process; therefore, MCO participation to assist with the process is
required. As part of this initiative, and in order to maintain organized and complete files, HSD is
requesting all MCOs use a standardized HSD SOE form. Each SOE shall contain four separate titled
sections. The MCO is to provide the information listed on each titled section of the SOE to MAD AHU in a
timely manner so it may meet HSD administrative hearing and Federal CFR requirements.
Special Situations
There have been questions related to whether both the relinquishing and receiving MCOs are to
respond to their members’ appeals and participate in the HSD administrative hearing when a member is
transitioning from one MCO to another.
Each MCO is responsible for its own process while still following the instructions for continuation of
benefits for the initial 30 calendar days after transfer; the member’s right to request an MCO appeal,
and for a continuation of his or her benefits.
Questions and Answers
• If a member requests an MCO appeal or an HSD administrative hearing for a service that has not
been provided, and it is found they will be transferring to another MCO while the member’s MCO
appeal process or his or her HSD administrative hearing is underway, how should we proceed?
o For a requested benefit that has not been provided:
• The relinquishing MCO must still complete the MCO appeals process even if the appeal
decision or HSD administrative hearing takes place after the member has transferred.
However, if the decision comes after the member has transferred, it may be reasonable for
the MCO’s final appeal decision to be that the member is no longer enrolled in the MCO so
the service cannot be provided through the relinquishing MCO. Even then, the member may
appeal the decision to HSD, but likely the finding would be the same.
• The member needs to file a new request for services with the receiving MCO because that
will be the MCO responsible for providing the service. If the receiving MCO denies the
service, then a new appeal process begins with the receiving MCO.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
343 | P a g e
• If a member is still in the MCO when the decision is made, the MCO decision must be based
on the information provided during the MCO appeal process and not denied on the basis
that the member will be transitioning to a new “receiving” MCO soon.
o For an existing benefit which is being provided subject to a continuation of benefit request:
• The relinquishing MCO must still complete the MCO appeals process even if the appeal
decision or HSD administrative hearing takes place after the member has transferred. This is
essential because a final determination must be made to determine if the member is
responsible for payment for services that were “continued” under the relinquishing MCO for
the time period the member was enrolled with the relinquishing MCO.
• When the relinquishing MCO makes a final decision on the member’s appeal, or when the
HSD administrative hearing final decision is rendered, it is applicable only for the time
period that the member was enrolled in the relinquishing MCO.
• Because a receiving MCO issues its own notice of adverse action concerning the same
benefit, the receiving MCO’s appeal process and possible subsequent HSD administrative
hearing is applicable only for the time period that the member is in the receiving MCO.
Therefore, it is possible that there may be concurrent appeals and administrative hearings
for the same member for the same benefit but for different time periods. The different time
periods correspond to the relevant dates that the member was enrolled in each MCO.
• What happens in the case when the receiving MCO does not agree with the relinquishing MCO’s
decision?
o If the relinquishing MCO makes a decision for a benefit for a time period the member is still
enrolled in the relinquishing MCO, the receiving MCO must accept that as the benefit the
member has in place at the time of the transfer to the receiving MCO. The service must initially
be continued through the receiving MCO under the transition of care provisions. The receiving
MCO can notify the member of its intent to take an adverse action against the member’s benefit
provided it is given 10 calendar days prior to ending the service (Notice of Action). See 8.308.11
NMAC Transition of Care for specific services that may allow for other considerations.
o However, the receiving MCO must initially continue to provide the relinquishing MCO’s
approved benefit. The member and the receiving MCO essentially begin the process of notice
and right to appeal again. The receiving MCO must follow the same process with regard to time
and notice. The receiving MCO would notify the member of its intent to take an adverse action

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
344 | P a g e
concerning the member’s existing benefit, LOC, or service within 10 calendar days prior to the
date of the intended adverse action. The member must file a new appeal request with the
receiving MCO. The member has the right to make a new request for a continuation of the
benefit from the receiving MCO and must do so in order for the benefit to continue during an
appeal process. The member’s request for a continuation of benefits to the relinquishing MCO
does not carry over to the receiving MCO. This process must be made clear to the member.
o HSD want to emphasize the contract provision for the 30 calendar day coverage of the
member’s benefit by the receiving MCO is an HSD contract requirement, but it does not replace
the responsibility of the MCO to follow Federal and State laws, statutes, regulations and rules
for member notification when it intends to take an adverse action against the member, the
member’s right to appeal, and the right for continuation of the member’s benefit.
• How will each MCO’s Medical Director fit into the scenario? Are they going to have to work with the
new MCO to handle a re-review if there is a disagreement?
o See the answer above. Each MCO handles the issue separately.
• Will the member need to know this is going on and who would be responsible to let the member
know this is occurring?
o The member does need to be informed. The member is entitled to a notice of adverse action
from the receiving MCO, as he or she received from the relinquishing MCO. The communication
to the member must be clear about the need to file a new MCO appeal request and make a new
request to his or her receiving MCO for a continuation of his or her benefit during the MCO
appeal process.
• Is the current MCO’s decision binding regardless of the other MCO’s opinion?
o The only sense in which it is “binding” is that if a benefit was provided by the relinquishing MCO,
even if that benefit was provided through an appeal or administrative hearing process, that
member is considered to have that benefit at the time of transfer to the receiving MCO. As for
any benefit which the member is receiving when he or she transfers into a receiving MCO, the
receiving MCO must initially provide the benefit, but it is subject to a new notice of adverse
action or re-authorization.
• Will each receiving and relinquishing MCO need to continue to do this process anytime a member
changes MCO?

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
345 | P a g e
o Yes, when a member is transitioning to another MCO, and the receiving MCO is intending to
take an adverse action effecting a benefit against a member (that is, discontinue or reduce the
existing service). The relinquishing and receiving MCOs each make their decisions separately for
the time period that the member is in their MCO; however, the receiving MCO still has the
responsibility for new notification of its intent to take an adverse action against the member.
• How will each MCO’s Appeal Unite be notified when a member has changed MCO?
o The relinquishing MCO would know when the member leaves. Its appeal unit should review the
enrollment status of the members that have an ongoing appeal on a monthly basis.
o The receiving MCO knows when it receives a transitioning new member. When a provider is
rendering an existing benefit approved by the relinquishing MCO, and that benefit requires
authorization or a LOC, a provider may need to report when requesting an authorization to the
receiving MCO that the member has already been receiving the benefit. The notification that
goes to a member upon denying an existing benefit is significantly different from the notice that
denies a new benefit. The receiving MCO’s member services unit may be the first to learn about
this issue by receiving a call from a member. Several receiving MCO units would likely be aware
of its transitioning member’s rights through the relinquishing MCO to request a continuation of
his or her benefit and of the member’s request for a MCO appeal of the adverse action, as well
as which benefits the relinquishing MCO is covering under a continuation of benefits.
Information to Consider Regarding Member Notices and Letters
All MCOs are required to produce a simple, clear notice or letter that includes the mandated
information detailed in the checklists accompanying this Manual section.
It is the MCO’s choice on how to address this issue. Some MCOs have been handling this requirement by
creating multiple distinct letters and notices that include necessary topics but exclude any irrelevant
information. For example, if the issue is the denial of an authorization for a new service, it is not
necessary to include “Continuation of Benefits” information in the letter or in the accompanying packet.
If the adverse action is a benefit that is not currently being provided, there is no need to include
information about Continuation of Benefits in the letter or packet. If the Standard Appeal was made in
writing, there is no need to include information to the member that if the appeal was made verbally, a
written request must be made within 13 calendar days.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
346 | P a g e
Each checklist allows for some variations in the letters and notices that the MCO must have, but the
MCO is not limited to the variations specified in the checklists. The MCO may have as many letters and
notices as necessary to clearly and effectively communicate to its members.
There must be recognition and use of the standard terms: “Grievance”, “Appeal”, and “HSD
Administrative Hearing”. The MCO may use the term “Formal Complaint” instead of “Grievance”;
however, the letter should clarify that a Formal Complaint is equivalent to the Grievance process, so a
member can relate the terms in the MCO’s notice to the terms used in HSD rules. Notices, letters, forms,
and information on the member’s rights should always be clearly labeled.
A Notice of Action is required when a new decision is made, even if the action is to increase or extend a
benefit. Therefore, MAD uses the term “Notice of Action”, not “Notice of Adverse Action”.
It is important the Notice of Action be clear in distinguishing between what was requested and what was
approved. If everything that was requested is approved, the Notice of Action should state that fact. In
such instances, it would be inappropriate to refer to the action as an adverse benefit determination or
an adverse action.
When the checklist instructs the MCO to provide a “contact” for the member, it does not have to be the
name of a specific individual. The MCO may follow its own process for setting up a contact system.
MCO notices should indicate that a member may request a “quick decision” when the member believes
their health or life is endangered while awaiting a decision. This is an important provision so a member
whose condition has changed or who need immediate attention can be assisted by the MCO.
Additional Aspects of Approvals and Denials Leading to Appeals
It is important the Notice of Action be based on the most complete information available. Therefore,
when considering a LOC or approval of a new item or service, an MCO may ask for additional or
clarifying information from the provider requesting the LOC or service in order to arrive at the most
appropriate decision and avoid an unnecessary appeal.
An MCO is not required to hold any kind of conference or pre-appeal decision discussion with the
requesting provider or the member; however, if the MCO believes this may help resolve the issue, the
MCO may schedule such conferences. Failure on the member’s part to attend such a conference cannot
be used as a reason to dismiss the appeal.
Before an appeal turns into an HSD Administrative Hearing, it is important it be clear what is in dispute
regarding the benefit.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
347 | P a g e
If the Notice of Action is related to a PASRR determination, the member should not be asked to file an
appeal with the MCO. Instead, the member should file for an Administrative Hearing; the proper
agencies will then become involved in the consideration. If the benefit is already being used, the
Continuation of Benefits is automatic and the member never pays for using the continued benefit.
Important Timelines
• Response to Request for Authorized Service or Other Approval
A decision on a standard authorization request must be issued as expeditiously as the member’s
health condition requires, but no later than 14 calendar days following receipt of the request for
new services, and no later than 10 calendar days following receipt of a request to continue ongoing
services.
Note that the checklist contains information about a “quick decision” even though that term is not
found in rules or contracts. It is important that an MCO be able to assist any member who believes
that their health or life is endangered while awaiting a decision; therefore, a member is allowed to
change a request for a Standard authorization request to an Expedited authorization request at any
time during the appeal process. The member is also able to contact the MCO and express the need
for a “quick decision” so that the MCO is informed of any developing medical issues or conditions
and can react, as necessary, to that situation. An extension of up to 14 calendar days is allowed
when following the HSD MCO contract provisions.
• Notice of Action Letter
A Notice of Action of reduction, increase, or termination of any benefit or LOC or budget amount
must be sent to the member at least 10 calendar days prior to the date the intended action will take
effect. The same timeframe and requirement for a Notice of Action is necessary following a review
or re-determination; when a benefit is extended with no change from the current benefit; or, if a
new benefit is approved as requested.
Special provisions apply for members in NFs. Federal regulations in 42 CFR 483.15 require NFs
provide a 30-day notice to the member in many instances related to a transfer or discharge. There
are exceptions provided. The MCO must be certain the NF has followed Federal requirements and
cannot provide a date for the discharge or transfer of a member in an NF that is earlier than the
date the NF states in their notice to the member. The MCO Notice of Action does not replace the

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
348 | P a g e
need for the NF to comply with the Federal requirement. See: Notice Of Action letter to member
regarding VAS.
• Continuation of Benefits may be established using the following process
The member may request a continuation of a current benefit any time prior to the date the adverse
action goes into effect; or within 10 calendar days of the Notice of Action, whichever is later.
• Appeals
The member has 60 calendar days from the date of the Notice of Action to file an appeal. If the
member appeal is a Standard Appeal and the request is made verbally, the member must submit the
appeal in writing within 13 calendar days of the verbal appeal.
If the member appeal is an Expedited Appeal, a verbal request is sufficient; it does not need to be
followed up in writing.
MCO Acknowledgement of Member Appeals
The MCO acknowledges the Standard Appeal within 5 business days of the receipt of the appeal. It is
important that an MCO be able to assist any member who believes that their health or life is
endangered while awaiting a decision: therefore, a member is allowed to change a request for a
Standard Appeal to a request for an Expedited Appeal.
MCO Member Appeal Final Decision Letter
The MCO provides an appeal decision letter within 30 calendar days of the receipt of the appeal for
a Standard Appeal, or within 72 hours for an Expedited Appeal; unless a notice of the need for an
extension is sent within these same time frames.
The MCO must provide notice to the member within 2 calendar days of any decision to extend the
timeframe necessary to provide a decision. See Letter Informing the Member of a Delay for an
Appeal Decision.
• Grievance
A Grievance may be filed at any time. An MCO cannot change a requested Appeal into a Grievance
without written consent from the member.
Acknowledgement of Receipt of a Member-Filed Grievance
An Acknowledgement of a member grievance must be sent within 5 calendar days of receipt by the
MCO.
Member Grievance Final Letter

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
349 | P a g e
A Resolution of Grievance Letter must be provided within 30 calendar days of the date of receipt of
the grievance or as expeditiously as the member’s health require.
Member Grievance Extension Request
The MCO may request an extension from HSD. For any extension not requested by the member, the
member must be provided a written notice within 2 calendar days of the decision to extend the time
frame.
• HSD Administrative Hearing
The member may request an HSD administrative hearing within 90 calendars days of the MCO
appeal final decision letter. For an Expedited Hearing, the request must be within 30 calendar days.
16.3. Appendices
The following pages contain checklists for specific information that must be contained in the Notice of
Action to a member, and the other letters and notices associated with steps relating to grievances,
appeals, and a final decision letter.
The MCOs are to review their notices and letters, revise them as necessary, and submit them to MAD for
final approval.
16.3.1 MCO Checklist – Acknowledgement of Receipt of a Member-filed Grievance
16.3.2 MCO Checklist for Member Grievance Final Letter
16.3.3 MCO Checklist for Notice of Action Letter to Member
16.3.4 MCO Checklist for Notice of Action Letter to Member Regarding Value-Added Services
16.3.5 MCO Checklist for the Acknowledgements of Member Appeals
16.3.6 MCO Checklist for Letter Informing the Member of a Delay for an Appeal Decision
16.3.7 MCO Checklist for the MCO Member Appeal Final Decision Letter

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
350 | P a g e
16.3.1. MCO Checklist – Acknowledgement of Receipt of a Member-Filed Grievance
MCO Checklist - Acknowledgement of Receipt of a Member-filed Grievance
The Acknowledgement must include:
The date that the Grievance was received.
The MCO’s understanding of the issue.
When the member may expect a resolution or other response to the Grievance, not to exceed 30
calendar days from the receipt of the Grievance.
That the member has the right to present evidence and testimony and make legal and factual
arguments on the issue before the MCO determines the resolution of the Grievance. This
presentation may be made by the member, a spokesperson or any designated or authorized
representative. The member or authorized individual must make a request for this presentation and
the MCO must schedule this presentation prior to making a determination on the Grievance. The
MCO must tell the member of the limited time the member has to make this request in order for the
MCO to provide a resolution within the required timeframe.
If the Grievance is related to a response to a Notice of Action for which there could be a member
Appeal, include the following:
Information on the difference between a member Grievance and an Appeal, including if they want
to file an Appeal they must do so within 60 calendar days of the Notice of Action; and that a
Grievance is not considered an Appeal and does not extend the timeframe in which an Appeal must
be filed.
A member may file a Grievance to express dissatisfaction about any matter or aspect of his or her
MCO’s operation. A member files an Appeal to begin a process for reconsidering an adverse action
as described in a Notice of Action.
Instructions on how to file an MCO member Appeal if the issue is better resolved through an MCO
member Appeal instead of an MCO Grievance.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
351 | P a g e
A statement the member cannot request an MCO member Appeal on the issue if he or she does not
agree with the final Grievance decision, unless the timeframe for an Appeal following a Notice of
Action is met and the Appeal is based on the Notice of Action, not on the Grievance decision.
A MCO Grievance contact that includes email and mail addresses, fax and telephone numbers.
Include the hours this contact is available, as well as an emergency number. Inform the member to
use this contact information if he or she has any questions. Inform the member how to access
toll-free numbers with TTY/TTD and interpreter ability.
Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
352 | P a g e
16.3.2. MCO Checklist for Member Grievance Final Letter
MCO Checklist for Member Grievance Final Letter
The letter should include the following:
The date of the letter, which should be the date the letter will be mailed.
A summary of the Grievance.
If an action was taken or is going to be taken, include a description of the action.
OR
An explanation of why no action will be taken to resolve the issue or why no action is necessary. This
explanation must be based on rules and requirements or established MCO policies and procedures.
A statement that the MCO grievance decision letter ends the MCO member Grievance process.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
353 | P a g e
16.3.3. MCO Checklist for Notice of Action Letter to Member
MCO Checklist for Notice of Action Letter to Member
The following sections, at a minimum, should be included in the written Notice of Action Letter. There
may be two versions as necessary:
1. Notice regarding an existing benefit;
2. Notice regarding a newly requested benefit;
➢ Notice of Action letter;
➢ Notice of the Right to file a Grievance;
➢ Notice of the Right to request an Appeal
➢ Notice of the Right to file a Grievance and request an MCO Appeal concurrently; and/or
➢ Notice of the Right to a Continuation of Benefits.
Notice of Action should include:
The date of the Notice, which must be the date the Notice will be mailed. If the Notice is to
terminate an existing benefit, the date must not be less than 10 calendar days prior to the date the
benefit will end.
A description of what action the MCO intends to take or has taken to terminate, suspend, change or
reduce the current benefit, allocation or budget, including a reduction in LOC, or transfer or
discharge of a member residing in a residential facility. If applicable, cite NMAC rules or other
criteria that support the basis of the decision. Include the date the benefit will stop or otherwise
change. A letter is required even if the change is to increase a benefit or if there has been a new
review and the same benefit is extended.
OR
If the action is a denial, in whole or in part, of a new benefit or service for the member, describe
what was requested and what has been denied or otherwise limited. If applicable, cite NMAC rules
or other criteria that support the basis of the decision.
An MCO contact, including email and mail addresses, fax and telephone numbers. Include the hours
this contact is available, as well as an emergency number. Inform the member to use this contact
information if he or she has any questions. Inform the member how to access toll-free numbers with
TTY/TTD and interpreter capability.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
354 | P a g e
Notice of the right to file an Appeal should include:
If the member disagrees with the Action, he or she has the right to appeal the decision to the MCO.
If the member would like to Appeal the decision, the Appeal must be requested within 60 calendar
days of the date of the Notice of Action. Include information that if the member misses the
deadline, they may lose their right to appeal. Offer to assist the member in requesting or filing for an
Appeal and tell them how he or she can obtain that assistance.
Describe the Standard Appeal process, including the request may be made by phone, but a written
request will need to be completed within 13 calendar days of the verbal request.
Describe the Expedited Appeal process, and that such a request may be made by phone.
Describe the criterion that merits an Expedited Appeal.
Inform the member of his or her right to a timely Appeal decision (not longer than 30 calendar days
from the request for a Standard Appeal or 72 hours for an MCO Expedited Appeal) and the
anticipated date of the Final Appeal Decision.
Provide appropriate forms for an Appeal that has the member identify how he or she would like to
be contacted.
Briefly describe the Appeal process:
Tell the member that he or she may file a Grievance even if he or she does not request an Appeal.
Clarify that the Grievance does not act as Appeal of any adverse action. Tell the member how to file
a Grievance.
Tell the member that he or she may file a Grievance and request an Appeal concurrently.
Provide an MCO Appeal contact which includes email and mail addresses, fax and phone numbers.
Include the hours that this contact is available, as well as an emergency number. Inform the
member to use this contact information if he or she has any questions. Inform the member how to
access toll-free numbers with TTY/TTD and interpreter ability.
Tell the member that if he or she requests an Appeal, he or she can obtain assistance from an
authorized representative, authorized provider, designated spokesperson, or legal counsel. Provide
the appropriate form and describe the process to the member.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
355 | P a g e
Tell the member when the he or she requests an Appeal:
He or she the right to designate an authorized representative. The authorized representative can
have access to the case information and may make medical decisions on behalf of the member.
He or she has the right to designate an authorized provider who agrees to assist him or her. The
authorized provider can have access to the case information, but does not have the authority to
make medical decisions on behalf of the member.
He or she has the right to designate a spokesperson. The spokesperson may have access to case
information and may speak for the member, but does not have the authority to make medical
decisions on behalf of the member.
He or she has the right to present evidence and testimony and make legal and factual arguments on
the issue before the MCO makes a final determination on the Appeal. This presentation may be
made by the member, a spokesperson or any designated or authorized representative. The member
or authorized must make a request for this presentation and that the MCO will schedule this
presentation prior to making a final decision on the appeal. The MCO must tell the member of the
limited time the member has to make this request in order that the MCO can provide the decision
within the required time frame; and of the member’s option to extend the time frame for up to an
additional 14 calendar days.
Neither an MCO or HSD can be held responsible for any fees or costs incurred by the member during
the MCO Expedited or Standard Appeal process.
Notice of the Right to Continuation of Benefits when there is an Adverse Action:
If the Action is to terminate, suspend, or reduce the current benefit, allocation or budget, including a
reduction in LOC, or transfer or discharge of a member residing in an NF, the letter must include a notice
of the right to a continuation of benefits:
If the benefit is already being provided, inform the member that he or she can request a
continuation of benefits at any time prior to the date the benefit will be terminated based on
the Notice of Action. (Note that if the Appeal is initiated by the MCO, the continuation of
benefits is automatic and the member never pays for using the continued benefit.)
Inform the member if he or she requests a continuation of benefits, the member will continue
to receive his or her disputed current benefit during the Appeal process, but the member may

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
356 | P a g e
choose to end his or her continued disputed benefit at any time during the MCO Appeal process
or HSD Administrative Hearing.
Explain the process to request a continuation of his or her disputed current benefit including
time frames.
Provide a phone number to verbally request a continuation of the disputed current benefit and
a mailing or email address, or fax number to submit a written request for a continuation of the
disputed current benefit.
Provide the MCO member with contact information, the type of disputed current benefit, the
number of times a day, week or month the member receives the disputed current benefit, the
length of time the benefit is delivered, the LOC of the benefit, or the allocation or budget
amount received.
Include information on the recoupment of the cost of the member’s continued disputed current
benefit if the MCO’s final decision upholds, in whole or in part, its adverse action; and state that
if the member later requests an HSD Administrative Hearing in which the final decision upholds
the adverse action, in whole or in part, the member will be financially responsible for paying for
the services they used.
When the MCO is initiating an MCO Expedited Member Appeal on behalf of the member, in addition
to all other requirements, the MCO must:
Inform the member of the process of an MCO-initiated Expedited Member Appeal.
Inform the member that the MCO is continuing the member’s disputed current benefit throughout
the MCO-initiated Expedited Appeal process and that the member is not obligated to repay the
continued disputed current benefit if the MCO Member Appeal Final Decision upholds the action.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
357 | P a g e
16.3.4. MCO Checklist for Notice of Action Letter to Member Regarding VAS
MCO Checklist for Notice of Action Letter to Member Regarding Value-Added Services
Notice of Action should include:
The date of the Notice, which should be consistent with the date the Notice will be mailed. If the
Notice is to terminate an existing benefit, the date must be no less than 10 calendar days prior to the
date the benefit will end.
Describe what action the MCO intends to take or has taken to terminate, suspend, change or reduce
the current value-added benefit. If applicable, cite NMAC rules or other criteria which may support
the basis of the decision. Include the date the benefit will stop or otherwise change. A letter is required
even if the change is to increase a benefit or if there has been a new review and the same benefit is
extended.
OR
If the action is the denial, in whole or in part, of a new benefit or service for the member, describe
what was requested and what has been denied or otherwise limited. If applicable, cite NMAC rules or
other criteria which may support the basis of the decision.
Include a statement that an MCO VAS adverse determination cannot be appealed through the MCO
or reviewed through an HSD Administrative Hearing.
If applicable, describe alternative MAD benefits that the member may utilize to replace the
terminated VAS.
Provide MCO contact, including email and mail addresses, fax and phone numbers. Include the hours
that this contact is available, as well as an emergency number. Inform the member to use this contact
information if he or she has any questions. Inform the member how to access toll-free numbers with
TTY/TTD and interpreter capability.
Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
358 | P a g e
16.3.5. MCO Checklist for the Acknowledgements of Member Appeals
MCO Checklist for the Acknowledgements of Member Appeals
The MCO should have, at a minimum, six separate but similar letters:
• Acknowledgement of a written Standard Appeal;
• Acknowledgement of a verbal Standard Appeal;
• Acknowledgement of a Standard Appeal, but the MCO or member changes it to an Expedited
Appeal;
• Acknowledgement of an Expedited Appeal;
• Acknowledgement of an Expedited Appeal but Denying the Expedited Status; and/or
• Notice of an MCO initiated Expedited Appeal and Continuation of Benefits.
Requirements
An Appeal request must always be followed by an acknowledgement within 5 business days of receipt of
an Appeal. Copies of the acknowledgement and any associated documents must be sent to the member,
any authorized representative, and to the provider who requested the disputed benefit.
If the acknowledgement letter is in response to a verbal request for a Standard Appeal, the
acknowledgement must: contain information about the 13 calendar day requirement to submit a
written Appeal, include the fact that if the member misses that deadline, they may lose their right to
an Appeal, and an offer to assist the member with the written Appeal.
The MCO must provide the Appeal form and offer to assist the member if they need help
completing it. (A request in writing from the member is not required for an Expedited Appeal.)
The Appeal acknowledgement must include the following:
The date of the acknowledgement, which should be consistent with the date the acknowledgement
letter will be mailed.
The date the Expedited or Standard Appeal request was received by the MCO and a brief statement
of the MCO’s understanding of the issue the member is appealing.
The anticipated date of the Appeal decision, which may be in the form of “no later than.”
The date of any scheduled informal conference to help clarify or settle the issue. Inform the member
they must adhere to the date or contact the MCO to change the date, if necessary. The scheduling of
an informal conference is not mandatory, but may be requested by the MCO.
Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
359 | P a g e
A MCO Appeal contact which includes email and mail addresses, fax and phone numbers. Include
the hours that these contacts are available, as well as any other emergency number that may be
available. Inform the member to use this contact information if he or she has any questions. Inform
the member how to access toll-free numbers with TTY/TTD and interpreter capability.
Inform the member of his or her right to have someone with them or to represent them in their
Appeal and that if they would like someone to represent them, they must make a request in writing.
Provide the appropriate form and describe the process to the member.
Inform the member of how to submit additional information regarding the issue, if the member or
provider has more information to provide.
Inform the member of his or her right to a continuation of benefits if the benefit is already being
provided and the member has not already requested a continuation of the disputed current benefit.
(This information should have also been previously provided in the Notice of Action.) Inform the
member that he or she can request a continuation of benefits at any time prior to the date the
benefit will be terminated, based on the Notice of Action, or within 10 calendar days of the date of
the notice, whichever is the longer period of time. (Note that if the Appeal is initiated by the MCO,
the continuation of benefits is automatic and the member never pays for using the continued
benefit.)
Inform the member if he or she requests a continuation of benefits, the member will continue to
receive his or her disputed current benefit during the Appeal process. Include information on the
recoupment of the cost of the member’s continued disputed current benefit if the MCO’s final
decision upholds, in whole or in part, its adverse action; and state that if the member later requests
an HSD Administrative Hearing if the final decision upholds the adverse action, the member will be
financially responsible for paying for the services they used.
Provide the member with contact information for requesting a continuation of benefits.
Inform the member that he or she may choose to end his or her continued disputed benefit at any
time during the MCO Appeal process or HSD Administrative Hearing process.
Include a statement of the member’s rights that includes the following:
The member’s right to a timely decision on the Appeal; a decision must be provided within 30
calendar days from the request for a Standard Appeal or 72 hours from the request for an Expedited
Appeal, unless notice is provided by the member or the MCO that additional time is required.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
360 | P a g e
That either the member or the MCO have the right to extend the time frame up to 14 calendar days
if necessary, but if the MCO extends the time frame, the member has the right to file a Grievance
with the MCO, if he or she disagrees with the extension.
That if the member believes that their health or life is endangered while awaiting a decision, the
member at any time during the appeal process can ask for a “quick” decision by requesting the
Appeal be changed to an Expedited Appeal, in which a decision is usually made within 72 hours; or if
it is an emergency, the decision will be made as soon as possible.
Outline the process that can occur if the Appeal decision is not in the member’s favor:
State that after the MCO Appeals process, if the member would like to continue the Appeal, he or
she may do so by requesting:
An HSD Expedited Administrative Hearing within 30 calendar days of the date of the MCO
Member Appeal Final Decision;
An HSD Standard Administrative Hearing within 90 calendar days of the date of the MCO
Member Appeal Final Decision; and/or
That more information on requesting an HSD Administrative Hearing will be included in the
Appeal Decision Letter if the decision is not in favor of the member.
Inform the member that he or she may also request for an HSD Administrative Hearing, if the
decision on their Appeal is not timely.
Inform the member that he or she may file a request for an HSD Administrative Hearing if the
member requested an Expedited Appeal, but the MCO denies the expedited status. The HSD
Administrative Hearing will be limited to the issue of expediting the MCO Appeal decision.
The acknowledgement must be in clear and simple verbiage. If the MCO has a packet of information
accompanying the letter, some of the detailed information may be in the packet rather than in the
letter, as long as the letter directs the member to look there.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
361 | P a g e
16.3.6. MCO Checklist for Letter Informing the Member of a Delay for an Appeal Decision
MCO Checklist for Letter Informing the Member of a Delay for an Appeal Decision
The Letter should include:
The date of the letter, which should be consistent with the date the letter will be mailed. If the
pending Appeal Decision is regarding termination of an existing benefit, the date must not be less
than 10 calendar days prior to the date the benefit will end. It is also a requirement to make a
reasonable effort to provide the member with information regarding the delay orally, in addition to
the written Acknowledgement.
Describe what action the MCO intends to take or has taken to terminate, suspend, change or reduce
the current benefit, or for a new benefit, intends to deny or limit.
Include the new date the benefit will terminate or otherwise change, if a delay in a decision is going
to delay the date of the benefit change or termination. A letter is required even if the change is to
increase a benefit or if there has been a new review and the same benefit is extended.
State the date a decision was due and the length of time the decision will be delayed. Include the
date a final decision is expected. Include the justification of why the decision is being delayed.
Tell the member that if he or she disagrees with the delay, they have the right to file a Grievance.
Describe the process on how they do so, including any forms that are necessary.
Provide an MCO contact, including email and mail addresses, fax and phone numbers. Include the
hours that this contact is available, as well as an emergency number. Inform the member to use this
contact information if he or she has any questions. Inform the member how to access toll-free
numbers with TTY/TTD and interpreter capability.
Tell the member that if the MCO does not provide a decision within the required 14 calendar day
extended time frame, the member has the right to request an HSD Administrative Hearing which will
result in the Administrative Hearing process making the final decision on the issue being appealed.
Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
362 | P a g e
16.3.7. MCO Checklist for the MCO Member Appeal Final Decision Letter
MCO Checklist for the MCO Member Appeal Final Decision Letter
The MCO should have, at a minimum, three separate but similar letters:
• Reversal of MCO Adverse Action;
• Partial Reversal of MCO Adverse Action; and
• No Reversal of MCO Adverse Action.
1. Letter for Reversal of MCO Action and Approval of the Benefit. Include in the notice of the
reversal of the MCO’s adverse action:
The date of the letter, which should be consistent with the date the letter will be mailed.
The date that the disputed benefit will start if the benefit was not continued or supplied during the
appeal process.
A MCO contact in case the member has any questions. Include email and mail addresses, fax and
phone numbers, the hours that the contact is available, and an emergency number if one is
available. Inform the member to use this contact information if he or she has any questions. Inform
the member how to access toll-free numbers with TTY/TTD and interpreter capability.
2. Letter for partial reversal of MCO Adverse Action.
Approved Benefit:
Inform the member of the date the disputed benefit will start if the benefit was not continued or
supplied during the appeal process.
Provide an MCO contact in case the member has any questions. Include email and mail addresses,
fax and phone numbers, the hours that the contact is available, and an emergency number if one is
available. Inform the member to use this contact information if he or she has any questions. Inform
the member how to access toll-free numbers with TTY/TTD and interpreter capability.
Denied Benefit:
Inform the member what disputed benefit was denied. State the date the denied benefit will be
terminated if it is currently being supplied.
Include a statement describing any rationale for the decision to deny the disputed benefit.
If applicable, cite NMAC rules or other reasoning used to make the final decision.
If the member had a continuation of benefits, inform the member what the recoupment cost is and
how the MCO will start recoupment.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
363 | P a g e
Provide an MCO contact who can explain the recoupment process and who can assist the member
to request an HSD Administrative Hearing if the member chooses to do so. Include email and mail
addresses, fax and phone numbers, the hours that the contact is available, and an emergency
number. Inform the member to use this contact information if he or she has any questions. Inform
the member how to access toll-free numbers with TTY/TTD and interpreter capability.
Include Member Rights and Information to Request an HSD Administrative Hearing: Include the
same information in that letter as described below, under the “Letter Upholding the Action.”
3. Letter Upholding the Action:
Include a statement describing the rationale to deny the disputed benefit.
If applicable; cite NMAC rules or other reasoning used to make the final decision.
Inform the member of the date the denied benefit will be terminated if it has been continued during
the Appeal.
If the member had a continuation of benefits, inform the member what the recoupment cost is and
how the MCO will start recoupment.
Provide an MCO contact who can explain the recoupment process and who can assist the member
to request an HSD Administrative Hearing if the member chooses to do so. The contact information
must include email and mail addresses, fax and phone numbers, the hours that the contact is
available, and an emergency number. Inform the member to use this contact information if he or
she has any questions. Inform the member how to access toll-free numbers with TTY/TTD and
interpreter capability.
Inform the member that he or she may choose to end his or her continued disputed current benefit
at any time prior to and during the HSD Administrative Hearing process.
Inform the member that they may request an HSD Standard Administrative Hearing within
90 calendar days of the date of the MCO Expedited or Standard Member Appeal Final Decision
letter.
Inform the member they may request an HSD Expedited Administrative Hearing within 30 calendar
days of the date of the Appeal Final Decision letter. The request for an HSD Expedited Administrative
Hearing may be made verbally or in writing.
Provide the member with the HSD Fair Hearing Bureau email and mail addresses, fax and phone
numbers, HSD toll-free numbers with TTY/TTD and interpreter capability.

Section 16: Fair Hearings
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
364 | P a g e
Inform the member that if they request an HSD Administrative Hearing, the MCO will not take steps
to recoup the cost of the member’s current disputed benefit until the HSD Administrative Hearing
process is over, unless requested to do so by the member.
Inform the member he or she may choose to end his or her continued disputed current benefit at
any time prior to and during the HSD Administrative Hearing process.
Inform the member of the recoupment of the cost of the member’s continued disputed current
benefit if the HSD Administrative Hearing Final Decision letter upholds the MCO’s Action.
All letters must be in clear and simple verbiage. If the MCO has a packet of information accompanying
the letter, some of the detailed information may be in the packet, as long as the letter directs the
member to look there.

Section 17: Managed Care Reporting
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
365 | P a g e
17. Managed Care Reporting
17.1. General Information
MCOs are required to comply with all reporting requirements established by HSD as specified in the
Agreement, which details requirements for timely submission, formatting, completeness and accuracy
of content. MCOs are provided with State-approved instructions and templates to facilitate timely,
complete, and accurate reporting. A complete list of current reports is incorporated in this Manual as
17.8.1: Centennial Care MCO Reports.
17.2. General Requirements
HSD, at its discretion, may request information and/or data, identified as ad hoc requests. Ad hoc
requests are issued to the MCOs for various reasons and information is generally requested to address a
separate and distinct issue or to provide clarification on issues that fall outside the scope of reporting
(i.e., provider information, claims research, NF census, etc.).
MCOs are required to implement continuous improvement processes to identify instances and patterns
of non-compliance. Identified patterns of non-compliance are addressed internally by MCOs to improve
overall performance and compliance.
At its discretion, HSD may, at any time, revise existing report content, and HSD may seek MCO input on
proposed changes. Once HSD issues finalized Report Instructions and Templates, MCOs will have at least
14 calendar days, and additional time at HSD’s discretion, to implement report content changes
depending on the nature of the changes.
17.3. MCO Reporting and Intake
HSD’s report management process involves the following:
• Downloading MCO report submissions via Xerox secure File Transfer Protocol (FTP) site;
• Processing MCO report submissions, resubmissions and other related documents;
• Acknowledging receipt of reports within 45 calendar days of receipt of the report upload date;
• Performing an initial quality check to ensure the MCO report is timely, accurate, complete,
formatted correctly, submitted on the correct template version and is accompanied by a signed and
dated Attestation;
• Recording all report review information and actions into an MCO Reports Tracking Tool;

Section 17: Managed Care Reporting
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
366 | P a g e
• Assigning MCO reports to Subject Matter Experts (SMEs) who possess the knowledge and
experience to conduct a thorough analysis of MCO reports and verify MCO compliance with HSD
requirements and performance standards;
• Tracking and monitoring the MCO report review and data analysis process;
• Managing HSD Lead Report Reviewer timeframes; and
• Uploading HSD feedback (Acceptance, Rejection, Final Review Tool, etc.) to the FTP site.
17.4. Report Rejection
An MCO Report may be rejected, by HSD, due to the following reason(s):
• Data inaccuracies;
• Signed Attestation not included;
• Incomplete information (e.g., data missing in fields);
• Formatted incorrectly;
• Incorrect template;
• Incorrect naming convention; and/or
• Incorrect reporting period, MCO name and report run date.
The HSD Contract Manager will determine whether a Rejection is warranted, or if a technical assistance
call or other solution is preferred.
17.5. MCO Report Resubmission
HSD has developed and implemented several processes (technical assistance call, self-identified error
resubmission [SIER]) to allow for improvement of the MCOs’ data accuracy and reporting compliance.
Technical Assistance Call Process
HSD Contract Managers and SMEs are available to provide technical assistance to MCOs in the following
areas:
• Review of HSD feedback of reports;
• Discuss extension requests of report submission deadlines; and
• Press to resolve reporting concerns;

Section 17: Managed Care Reporting
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
367 | P a g e
In an effort to maximize and improve MCO reporting and data efficiency levels, HSD may conduct a
technical assistance call to address data-related questions and concerns. This provides an opportunity
for MCOs to gain valuable guidance from HSD Contract Managers and SMEs.
After a technical assistance Call is held, the HSD Contract Manager determines whether the MCO’s
report is Accepted or Rejected.
Self-Identified Error Resubmission
In addition to Section 4.21.1.6 of the Agreement, MCOs must upload a SIER report within the deadline
specified by an HSD Contract Manager.
MCOs are required to accurately label each subsequent report submission with the appropriate version
number (v2, v3, v4).
HSD Contract Managers approve all MCO Report Rejections and SIERs; manage the technical assistance
call process; and direct the overall resubmission of MCO reports.
17.6. Report Revisions
HSD conducts report revisions as necessary through a formal, written process in which MCOs and end
users request needed changes to data reporting metrics. This process is intended to streamline
managed care reporting and reduce administrative burden by limiting data collection, where possible, to
meet Federal and state requirements. Changes to HSD’s managed care data reporting also support the
needs of external agencies and stakeholders.
The report revision process begins with submission of a formal request to HSD. If the request is
approved, the Centennial Care Contracts Bureau will organize a revision workgroup with SMEs and
report reviewers to make required revisions or modifications.
When the workgroup completes this function, a draft reporting package is submitted to MCOs for
comment and testing. Comments may be rejected or accepted, resulting in additional revisions to the
reporting package. HSD then issues the final reporting package to MCOs for implementation.

Section 17: Managed Care Reporting
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
368 | P a g e
17.7. System Availability Reporting
MCOs must notify HSD of MCO’s and its subcontractor’s systems availability and performance. In the
event of scheduled unavailability of critical member and provider Internet and/or telephone-based
functions and information, including but not limited to member eligibility and enrollment systems,
MCOs must notify HSD in advance via email at HSD.MCOSystemsAvail@State.nm.us in order to obtain
approval by HSD. In the event of an unforeseen and unscheduled inaccessibility of any critical systems,
MCOs must notify HSD via email to the above address as soon as possible.
Furthermore, in the event of a problem with system availability that exceeds four hours, MCOs are
directed to notify HSD immediately via email at HSD.MCOSystemsAvail@state.nm.us. MCOs are to
provide HSD within five business days, documentation that includes a CAP describing how MCO will
prevent the problem from occurring again.
In the event of any critical systems unavailability that has been approved by HSD but the amount of
downtime exceeds what was initially approved by HSD, MCOs must notify HSD immediately via email at
HSD.MCOSystemsA[email protected].
During Federal and/or State Holidays and weekends, the same processes included above would apply.
For any critical member or provider system unavailability, MCOs should also immediately contact
John Padilla, MAD, at (505) 827-1340 and email him at JohnH.Padilla@state.nm.us.
For any email notification pertaining to the above direction, MCOs must use the HSD-developed
template included in this Section as 17.8.2: Systems Availability Incident or Event Report.
17.8. Appendices
17.8.1 Centennial Care MCO Reports
17.8.2 Systems Availability Incident or Event Report

Section 17: Managed Care Reporting
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
369 | P a g e
17.8.1. Centennial Care MCO Reports
Report
No.
Report Title
Frequency
Report Objective
Comment
1
Native American Members
Report
Quarterly
To ensure Native American members have access to care and are receiving
needed services.
2
Call Center
Report - Monthly
Monthly
To capture call center statistics and ensure that callers can access a call
center agent in a timely manner.
3
Network Adequacy Report
Quarterly
To monitor the MCO’s compliance in maintaining an adequate and efficient
provider network, tracking new and terminated providers and single-case
agreements.
4
Self-Directed Report
Quarterly
To (i) monitor the amount of the annual SDCB budget used by members, (ii)
identify the services that are highly utilized, (iii) identify members that have
over-utilized or under-utilized their annual CB budget, and (iv) identify
members whose cost of care in the community is greater than 80% of the
cost of care in a private NF.
5
Admissions and
Readmissions Report
Quarterly
To monitor the number of members who are readmitted to a facility such as,
an RTC, TFC, hospital, within 30 calendar days of a previous discharge and to
track follow-up appointments after discharge.
6
Care Coordination Report
Quarterly
The Care Coordination report monitors assessments, ongoing care
coordination activities, and changes of care coordination levels for all levels
of care coordination.
On Hold
8
Level of Care (LOC) Report
Monthly
To capture data regarding the nursing facility (NF) LOC determination
process including timeframes, activities of daily living, and care settings.
9
Agency-Based Community
Benefit (ABCB) Report
Quarterly
To (i) monitor the number of members that changed to ABCB, (ii) identify
the services used by members receiving ABCB, and (iii) identify members
whose cost of care in the community is greater than 80% of the cost of care
in a private NF.

Section 17: Managed Care Reporting
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
370 | P a g e
Report
No.
Report Title
Frequency
Report Objective
Comment
12
Provider Satisfaction
Survey Report
Annually
To review the results from the survey, including information regarding
overall satisfaction (claims, provider relations, network, utilization and
quality management, pharmacy and drug benefits, and continuity of care).
15
Audited HEDIS Results
Annually
To monitor and review audited HEDIS results.
18
UM Program Description,
Associated Work Plan and
Evaluation
Annually
To monitor the MCO's UM Program Evaluation to monitor overall
effectiveness, an overview of UM activities, and an assessment of the impact
of the UM program on management and administrative activities. The
MCO’s review and analysis shall be incorporated in the development of its
following year’s UM Work Plan.
19
UM Program Evaluation
Annually
To evaluate the overall effectiveness of UM including an overview of UM
activities and an assessment of the impact of the UM program on
management and administrative activities.
LOD #29: Combined with 18
20
Disease Management
Description and Evaluation
Annually
To monitor and review the MCO's Disease Management program which
includes a description of MCO activities regarding chronic conditions
identified in the Disease Management program description. Disease
Management is a component of care coordination and must include BH as
part of the program.
21
Disease Management
Annual Evaluation
Annually
To evaluate the MCO's Disease Management program.
LOD #29: – Combined with 20
22
QM/QI Program
Description and
Associated Work Plan
Annually
To monitor and review the MCO's Annual QM/QI Program Description and
Associated Work Plan to include goals, objectives, structure, and policies
and procedures that address continuous QI for PH and BH.
23
QM/QI Program Annual
Evaluation
Annually
To monitor the MCO's QM/QI Program Evaluation for the previous year's
activities.
25
CAHPS Results Report
Annually
To review and evaluate the Consumer Assessment of Healthcare Providers
and Systems (CAHPS) results report.
27
Activities of the Member
Advisory Boards
Semi Annually
To review Member Advisory Board meeting agendas for general MCO
membership, Native American representation, BH, and CB subgroups.
LOD #29: Report 27 Combined
with 27a and 32; now
semi-annually.

Section 17: Managed Care Reporting
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
371 | P a g e
Report
No.
Report Title
Frequency
Report Objective
Comment
27a
Subgroup of the Member
Advisory Board (BH,
Self-Directed, etc.)
10 business
days following
each meeting
To Monitor the activities of subgroups of the Member Advisory Board.
LOD #29: Combined with 27 and
32.
31
Health Education
Evaluation Report
Annually
To evaluate the MCO's Health Education Plan, relating to initiatives in the
plan and present findings, lessons learned and performance improvement
initiatives as a result of the findings.
LOD #29: Combined with 30.
32
Activities of the Native
American Advisory Board
Report
10 business
days following
each meeting
To monitor the activities of the Native American Advisory Board, including a
summary of the MCO's approach to inviting Native American advisory
members, the meeting agenda, minutes, attendees and scheduling of the
next meeting.
LOD #29: Combined with 27 and
27a.
35
Electronic Visit Verification
(EVV)
Quarterly
To review and evaluate the use of EVV systems of the MCOs.
36
Critical Incidents
Report - Quarterly
Quarterly
To monitor key metrics regarding critical incident reporting for specific
subpopulations and the MCO’s actions in response to critical incidents.
LOD #29: Report Number changed
from 36B to 36.
37
Grievances and Appeals
Report
Monthly
To monitor member and provider grievances, appeals and fair hearings and
to track MCO adherence to contractual timeframes.
38
Provider Training and
Outreach Plan and
Evaluation Report
Annually
To monitor and review the MCO's plans for provider training and outreach.
39
Provider Training and
Outreach Plan Evaluation
Report
Annually
To evaluate specific training topics such as (i) prior authorization process, (ii)
claims/encounter data submission(iii) how to access ancillary providers; (iv)
members rights and responsibilities; (v) quality improvement (QI)
program/QI initiatives; (vi) provider and Member Appeals and Grievances;
(vii) recoupment of funds processes and procedures; (viii) Critical Incident
management; and (ix) EPSDT benefit requirements, including preventative
healthcare guidelines.
LOD #29B:
Combined with #38
42
Prior Authorization Report
Quarterly
To capture information on services requiring prior authorization and
examine changes and trends in authorizations and denials of services over
time.

Section 17: Managed Care Reporting
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
372 | P a g e
Report
No.
Report Title
Frequency
Report Objective
Comment
44
Pharmacy Report
Monthly
To monitor pharmacy utilization and cost, including dispensing fees,
over- and under-utilization of drugs including controlled substances,
utilization of formulary drugs, non-formulary drugs, over the counter,
generic, and brand drugs.
45
BH Members Services/CSA
Report
Quarterly
To monitor the number and types of members served through CSAs and the
types of services provided to such members.
On Hold
Pending Revision
47
Claims Activity Report
Quarterly
Claims Activity Section – To capture data related to the disposition of claims,
timeliness of claims adjudication, payments on clean claims to providers,
interest paid, and claim aging. This section of the report captures claims
data separately for PH providers, BH providers, I/T/Us (Indian Health Service,
Tribal health providers, and Urban Indian providers), and specialty-pay
providers (day activity providers, assisted living providers, nursing facilities,
home care agencies, and CB providers).
Claims Payment Accuracy Section – To report the findings of the MCO’s
internal audit of quarterly claim payments and to monitor the accuracy of
those claims paid.
LOD #29 C: Frequency of
submission changed from
Monthly to Quarterly
48
Patient Centered Medical
Homes (PCMH) Report
Quarterly
To track (i) the number of PCMHs established, (ii) the number of members
that were referred to and joined a PCMH, (iii) outcomes, including
emergency room utilization and hospital admission and readmission, and (iv)
PCMH NCQA recognition and other accreditation.
LOD #29: Frequency of
submission changed from
Semi-Annually to Quarterly
49
Provider Network
Development,
Management Plan and
Evaluation
Annually
To monitor and review the MCO's plans for developing and managing its
provider network to ensure all medically necessary services are accessible
and available.
50
Provider Network
Development and
Management Evaluation
Report
Annually
To evaluate the Provider Network Development and Management Plan that
provides information on a summary of providers, monitoring activities,
contract provider issues, network deficiencies and on-going activities for
provider development and expansion.
LOD #29: Combined with 49
51
Provider Suspensions and
Terminations Report
Semi Annually
To monitor the suspensions and terminations of providers and the number
of members impacted.
LOD #29: Frequency of report
submission changed from
Quarterly to Semi-Annually

Section 17: Managed Care Reporting
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
373 | P a g e
Report
No.
Report Title
Frequency
Report Objective
Comment
53
PCP Report
Quarterly
To capture information regarding PCP member ratios, open panels and
assignment/change activity for non-dual members.
LOD #29: Frequency of
submission changed from
Monthly to Quarterly
55
Geo/Access Report
Quarterly
To monitor access to services by county and across urban, rural, and frontier
counties.
56
Program Integrity Report
Quarterly
To monitor fraud, waste, and abuse cases, preliminary investigations,
suspicious activities, adverse actions, and financial program integrity
activities of the managed care organization.
61
Medicaid School-Based
Health Centers (SBHC)
Quarterly
To track the quantity and types of services billed by school-based health
centers.
On Hold – LOD #29 (pending
revision)
63
Developmental Disabilities
(DDs) Specialty Dental
Report
Quarterly
To monitor dental visits for members with DDs.
64
Jackson Class Members
Report
Quarterly
To monitor MCO performance in processing requests for and delivering new
adaptive equipment and modifications or repairs to adaptive equipment.
66
Health Homes (HHs)
Report
Quarterly
To track (i) the number of HHs established; (ii) the number of members
referred to and joined a HH (iii) outcomes, including emergency room
utilization and hospital admissions and readmissions.
On Hold – LOD #29
This report is in development

Section 17: Managed Care Reporting
Revision dates: August 15, 2014; March 3, 2015;
January 1, 2019
Effective dates: January 1, 2014
374 | P a g e
17.8.2. Systems Availability Incident or Event Report

Section 18: Quality
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
375 | P a g e
18. Quality
18.1. Performance Improvement Projects (PIPs)
In addition, to the three PIPs outlined in the Agreement (one related to long-term services, one related
to prenatal and postpartum, and one related to adult obesity), the MCO shall be required to do the
following two PIPs based on the most current CMS Adult Core Set.
• Diabetes prevention and enhanced disease management:
o PQI01-AD: Diabetes, Short-Term Complications Admission Rate (NQF #0272); and
o HA1C-AD: Comprehensive Diabetes Care: Hemoglobin A1c Testing (NQF #0057)
• Screening and management for clinical depression
o AMM-AD: Antidepressant Medication Management (NQF #0105); and
o CDF-AD: Screening for Clinical Depression and Follow-Up Plan (NQF #0418)
These PIPs shall follow all CMS EQR protocols and will be reviewed annually by the EQRO based on the
most current EQR protocols.
18.2. Provider Satisfaction Survey
The Provider Satisfaction Survey is an annual report that provides the MCO with an assessment of its
activities, policies and procedures related to identifying healthcare performance, improvements and
internal systems based upon satisfaction of its contracted providers. HSD has outlined specific
requirements to be included in the provider satisfaction survey. Those requirements are incorporated
into the Provider Satisfaction Survey reporting instructions. The survey requirements list the detailed
description of:
• Three populations to target;
• Rating system to follow;
• Topics to address; and
• Template of the required questions, which are attached in 18.4.1.

Section 18: Quality
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
376 | P a g e
18.3. Critical Incident Reporting
All agencies in New Mexico providing HCBS and BH services are required to report Critical Incidents
within 24 hours of knowledge of the occurrence. The critical incident(s) should be reported to the
member’s MCO and/or Adult Protective Services (APS) or Child Protective Services (CPS) as necessary.
Critical incident reporting responsibilities and reporting requirements include:
• HCBS critical incidents involving members with a qualifying COE must be reported on the HSD
Critical Incident Reporting System for the following reportable incidents: abuse; neglect;
exploitation; deaths; environmental hazards; missing/elopement; law enforcement; and emergency
services.
o Qualifying COEs include: 001; 003; 004; 081; 083; 084; 090; 091; 092; 093; 094; 100; and 200
with a NF LOC.
• Critical Incident Reports filed as the result of a member's death and accepted for investigation by
the Office of the Medical Investigator (OMI) shall remain in a pending state within the HSD Critical
Incident Reporting Portal until the OMI has issued its findings. The MCO is responsible to update
the HSD Critical Incident Reporting Portal with the results from the OMI.
• The MCO shall require all staff and Contracted Providers to document updates regarding initiated
action(s) taken for the member and all follow-up activities related to the intervention(s)
implemented as a result of the incident. The information should be entered into the HSD Critical
Incident Reporting Portal until the established intervention(s) demonstrate the member's health,
safety and welfare are no longer issues of concern.
o The follow-up action(s) include but are not limited to:
• Requiring an investigation or intervention for issues of health and safety;
• Information related to the member’s health, safety and welfare;
• Communication with internal or external agencies; and
• Any changes in the member's health status, including but not limited to; care
coordination visits or care coordination investigations or interventions, and/or
reassessment or change in the member’s comprehensive care plan.
• BH critical incidents and all Sentinel Events are defined by the BH Critical Incident Protocol.
o Critical incidents involving BH services for members with a non-qualifying COE must be
reported on the Centennial Care Behavioral Health Critical Incident form for any known, alleged

Section 18: Quality
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
377 | P a g e
or suspected events of abuse, neglect, exploitation, injuries of unknown origin or other
reportable incidents.
o The MCO shall have a process and designate one fax line to receive critical incident reports
from BH providers for Medicaid recipients. The MCO shall provide this fax number to HSD and
the MCO contracted BH provider network.
o The MCO is responsible for reviewing and ensuring complete follow up has occurred regarding
all submitted BH critical incidents reported by or on behalf of their members, including APS and
CPS.
o The MCO will notify BHSD of all Sentinel Events in accordance with the BH Critical Incident
Protocol.
• Critical Incident Reporting Upon Termination of MCO Contract
o The MCO shall submit a report to HSD containing identified Critical Incident Reports
(CIRs) and any pending death investigations associated with its members thirty (30)
Calendar Days prior to the termination of the MCO contract, using a template provided
by HSD. The MCO shall submit weekly updates regarding these outstanding CIRs until all
reports are resolved and closed.
o The MCO shall be responsible for completing all follow-up activities, such as
investigations and final reporting of unresolved critical incidents for members who were
part of the MCO's membership at the time the incident was filed.
o Sixty (60) Calendar Days after the resolution of all outstanding Critical Incident Reports
and death investigations, the MCO's access to the HSD Critical Incident Reporting Portal
will be terminated.
18.4. Appendix
18.4.1 Centennial Care Reporting Survey Template

Section 18: Quality
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
378 | P a g e
18.4.1. Centennial Care Reporting Survey Template
Centennial Care Reporting Survey Template
MCO survey results shall utilize the following rating system:
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
The survey shall include the following required questions:
Care Coordination/Continuity of Care
Effectiveness of MCOs care coordination/care management programs for members.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Assistance provided by care coordination/care management staff.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
MCO provides information needed to care for its members.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Overall Satisfaction
Likelihood you would recommend the MCO to other members?
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Likelihood you would recommend the MCO to other physicians?
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Overall satisfaction with MCO.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Claims
MCOs accuracy of claims processing.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1

Section 18: Quality
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
379 | P a g e
MCOs timeliness of claims processing.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
MCOs timeliness of adjustment/appeal claims processing.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Ease of resolving claims issues without making multiple inquiries.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Provider Relations
MCOs process of obtaining member information (eligibility, benefit coverage, co-pay amounts).
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Satisfaction with MCOs customer service in answering questions and/or resolving problems when calling the
MCO.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
MCOs frequency and effectiveness of provider representative visits to the provider’s office.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Usefulness of MCOs written communications, policy bulletins, and manuals.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Quality of provider orientation and education processes.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Ease of completing MCO credentialing and re-credentialing.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
MCOs attentiveness to the provider’s overall needs.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1

Section 18: Quality
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
380 | P a g e
Provider Network
Quality of the MCO’s primary care practitioners.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Quality of the MCO’s specialists.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
The number of quality specialists to whom the provider can refer patients.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
The number of specialists in the MCO’s provider network.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Utilization/Quality Management
Ease of the prior authorization process.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Timeliness of obtaining outpatient authorization of services.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Timeliness of obtaining inpatient authorization of services.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Satisfaction with coordination of home health and DME services.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Procedures for obtaining pre-certification/referral/authorization information.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Degree to which the plan covers and encourages preventive care and wellness.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1

Section 18: Quality
Revision dates: August 15, 2014; March 3, 2015,
January 1, 2019; October 1, 2020
Effective dates: January 1, 2014
381 | P a g e
Clinical appropriateness of UM decision.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Pharmacy/Drug Benefits
Ease of using formulary.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Ease of the pharmacy prior authorization process.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
MCOs variety of drugs available in formulary.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Timeliness of response to pharmacy prior authorization requests.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Extent to which formulary reflects current standards of care.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Ease of prescribing preferred medications within formulary guidelines.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1
Availability of comparable drugs to substitute those not included in the formulary.
Excellent – 6 Very Good – 5 Good – 4 Fair – 3 Poor – 2 Don’t know – 1

Section 19: Program Integrity
Revision dates:
Effective date: January 1, 2019
382 | P a g e
19. Program Integrity
19.1. General Information
The Centennial Care MCOs shall comply with all Program Integrity provisions of the Patient Protection
and Affordable Care Act (P.L. 111-148), as amended by the Health Care and Education Reconciliation Act
of 2010 (P.L. 111-152) (collectively "PPACA "), and its regulations.
19.2. Fraud, Waste and Abuse Requirements
This section provides further guidance to the Agreement and clarifies the requirements set forth in the
following sections of the Agreement: 4.17.1 (Program Integrity - General); 4.17.2 (Program
Integrity - Reporting and Investigating Suspected Fraud and Abuse); and 7.27 (Cooperation Regarding
Fraud).
Provider profiling, auditing and data mining must occur on a regular basis to assist in the identification
of potential fraud, waste and abuse. This includes, but is not limited to, an automated review of claims
or a clinical audit. Information may also be used from external sources. When an MCO identifies
potential fraud, or becomes aware of an allegation of potential fraud or suspicious activity, it must
comply with the following:
Initial Report
• For PH or LTC services, make an initial report within five business days from the time the MCO
identifies potential fraud, or becomes aware of an allegation of potential fraud or suspicious activity
to the New Mexico HSD, OIG’s Program Integrity Unit (PIU). The MCO must identify whether it is an
initial report.
• For BH services provided to Medicaid recipients, make an initial report within five business days
from the time the MCO identifies potential fraud, or becomes aware of an allegation of potential
fraud or suspicious activity to PIU and the New Mexico Behavioral Health Collaborative (the
"Collaborative"). The MCO must identify whether it is an initial report.
• The MCO must document the identification of potential fraud, or allegation of potential fraud or
suspicious activity on the HSD Program Integrity Report ("Report 56") pursuant to the "Centennial
Care Reporting Instructions Program Integrity- Report #56".

Section 19: Program Integrity
Revision dates:
Effective date: January 1, 2019
383 | P a g e
MCO Investigation
• Once initially reported, the MCO must begin the investigation promptly in order to ensure that is
completed within 12 months, including all reports as required by the Agreement or set forth herein
(see, information below), from when the MCO identified potential fraud, or became aware of an
allegation of potential fraud or suspicious activity, from when it was initially reported to the PIU. The
MCO must use the PIU supplied Special Investigative Unit (SIU) Case Summary form when reporting
Fraud, Waste and Abuse to the PIU. The SIU Case Summary form may include, but is not limited to,
the following information:
o Date of the initial report to PIU;
o With each update to PIU, identify the report as an update and the date of the update;
o Provider(s), member(s), and/or caregiver(s) full name, and any other known names used, that
are the subject(s) of the referral;
o Any known relationships between provider(s), member(s), and/or caregiver(s) (i.e., business,
personal, etc.);
o If a provider, whether they are a billing or rendering provider, and the name(s), address,
telephone number of the reciprocal billing or rendering provider;
o If known, NPI, TIN, SSN, DOB, Medicaid/Medicare Provider Number, Medicare Number,
Medicaid Number, address, phone number, and/or product line for the subject(s) of the referral.
If not known, identify as "Unk";
o If known, the complainant's contact information to include, name, physical address, email
address and phone number. If not known, identify as "Unk";
o MCO's case file number, date the MCO opened the case, allegation description and code
number, and source of the complaint, i.e. hotline, letter, email, etc.;
o Verify whether the member, caregiver, or provider has been previously investigated during the
previous five years and summarize what was found previously;
o Identify and review claim(s), billing(s), and payment history, and summarize what was found;
o Identify and review internal policies and procedures, and summarize what was found;
o Identify and review provider's credentials and member's eligibility status, and summarize what
was found;
o Identify and review state rules, service definitions, and manuals, and summarize what was
found;

Section 19: Program Integrity
Revision dates:
Effective date: January 1, 2019
384 | P a g e
o Determine if the MCO previously provided education to the provider or member as it relates to
the suspicious activities, and summarize what was found;
o Document all investigative findings in the SIU Case Summary form;
o Identify the total potential overpayment resulting from fraud and the time period for the claims
reviewed; and
o Identify whether the potential overpayment was recovered in whole or in part, and if in part,
the amount recovered and the remaining balance.
The information identified above is fundamental for the PIU to determine a credible allegation of fraud
and if the MCO has this information, it should be included in the MCO's SIU Case Summary form to the
PIU. The MCO should also identify and summarize those investigative steps taken that have no results
and include them in the MCO's SIU Case Summary form to the PIU.
• In conducting their investigation, the MCO should keep in mind the definition of a credible
allegation of fraud, 42 CFR 455.2, and the obligations for an investigation set forth in 42 CFR 455.14.
• During the time that the MCO is conducting its investigation, it shall provide the PIU, and when
appropriate the Collaborative, with updates as requested.
• Within the 12-month period and within 10 business days of completing their investigation, the MCO
shall report the results to the PIU, and when appropriate the Collaborative, using the SIU Case
Summary form and state whether the MCO determined:
o The allegations are unsubstantiated and no further action is recommended;
o The allegations resulted in a potential overpayment; or
o The allegations resulted in a referral to the PIU with a recommendation that a credible
allegation of fraud may have been identified.
The MCO will use their last significant investigative action resulting in information that is significant and
relevant to the investigation as the date their investigation was completed. This may include, but is not
limited to, interview, document analysis, document receipt, etc.
• Upon completion of their investigation, the MCO shall update Report 56 pursuant to the "Centennial
Care Reporting Instructions Program Integrity-Report #56".
Overpayments
• If, as a result of their investigation, the MCO determines that an overpayment exists, the MCO shall
report to the PIU, and when appropriate to the Collaborative, using the SIU Case Summary form:
o The overpayment amount;

Section 19: Program Integrity
Revision dates:
Effective date: January 1, 2019
385 | P a g e
o The claims identified for overpayment recoupment such claims being reflected on the MCO's
encounter data;
o If the overpayment amount is extrapolated, the methodology used for the extrapolation;
o The date the provider was notified of the overpayment;
o The terms of any repayment; and
o Whether the overpayment was recovered in whole or in part, and if in part, the amount
recovered and the remaining balance.
• Providers may also self-disclose overpayments to the MCO as indicated in Section 4.17.4 (Recoveries
of Overpayments and/or Fraud) of the Agreement and 42 U.S.C. § 1320a-7k(d)(l), codifying Section
6402(a) of PPACA.
• All overpayments resulting from situations other than fraud, including self-reported overpayments
to the MCO, shall be considered the MCO's property unless:
o The HSD, OIG, CMS or its contractors, HSD's Recovery Audit Contractor, or the New Mexico
Attorney General's Office, Medicaid Fraud and Elder Abuse Division (MFEAD, also commonly
referred to as the Medicaid Fraud Control Unit) notified the provider that an overpayment
existed;
o The MCO fails to initiate recovery within 12 months from the date the MCO first paid the claim;
or
o The MCO fails to complete the recovery within 15 months from the date the MCO first paid the
claim.
Credible Allegations of Fraud
• If, as a result of their investigation, the MCO determines the allegations appear credible, a SIU Case
Summary form and all supporting documentation must be submitted to the PIU within 12 months
from when the MCO identifies potential fraud, or becomes aware of an allegation of potential fraud
or suspicious activity, and 10 business days from completion of the MCO's investigation. The MCO
shall also document the referral on Report 56 pursuant to the "Centennial Care Reporting
Instructions Program Integrity Report #56".
• If the PIU does not refer the matter to MFEAD or other law enforcement agency, the MCO may take
whatever action it deems appropriate, including but not limited to, seeking overpayment from the
provider and/or conducting educational training with the provider.

Section 19: Program Integrity
Revision dates:
Effective date: January 1, 2019
386 | P a g e
• If the PIU refers the matter to MFEAD, the PIU shall, within 10 business days, notify the MCO of such
referral. Thereafter, the PIU shall attempt provide the MCO with quarterly updates based on the
State Fiscal Year cycle. This is in addition to any other requirements, including payment suspension,
as outlined in the Agreement, specifically 7.27.1.1. (Referrals for Credible Allegations of Fraud) of
the Agreement.
• If the PIU refers the matter to MFEAD and it is not accepted or it is later returned by MFEAD, the PIU
shall, within 30 calendar days notify the MCO. In such a situation, HSD, at its sole discretion and
related to administrative and civil remedy available to HSD, may seek recovery against the provider
for any overpayments and any refund shall be HSD's property. This is in addition to any other
requirements set forth in 7.27.1 1 (Referrals for Credible Allegations of Fraud) of the Agreement.
• If MFEAD accepts the matter and brings a civil or criminal charge against the provider which results
in a recovery, 7.27.12 of the Agreement shall apply.
19.3. Suspension of Medicaid Payments for Credible Allegations of Fraud
All providers are required to comply with PPACA's program integrity requirements and its corresponding
Federal regulations. This includes 42 CFR 455.23 which requires payment suspension of pending
investigations when the OIG has verified, on a case-by-case basis, that there is a credible allegation of
fraud. In addition to the requirements set forth in 7.27.11 (Referrals for Credible Allegations of Fraud) of
the Agreement:
• The OIG will provide written notice of provider payment suspension, in whole or in part, as follows:
o Notice to MFEAD;
o Notice to the MCO to impose suspension of payments to the provider; and
o Notice to the provider within five calendar days, or 30 calendar days if requested by law
enforcement, in writing requesting a delay in sending the notice.
▪ Law enforcement’s request to delay sending notice may be renewed in writing up to twice
and in no event may exceed 90 days.
▪ In such instances, the PIU will notify the MCOs in writing that an initial delay has been
requested and when 20 calendar days after law enforcement's request has been rescinded
or the 90 days has passed, advise the MCOs whether payment suspension should be
imposed in whole or in part.

Section 19: Program Integrity
Revision dates:
Effective date: January 1, 2019
387 | P a g e
• The MCO shall adjudicate the provider's suspended claims as part of their regular course of business
and track the total amount(s) suspended. These amounts shall be reported to the PIU quarterly and
updated through ad hoc reporting, as requested.
• The MCO shall continue the suspension of payments, in whole or in part, until further notified in
writing by the PIU to release suspended funds. Release of funds will be authorized when law
enforcement agencies, such as MFEAD, determine that there is insufficient evidence of fraud by the
provider; or legal proceedings, to include any type of administrative or civil action, either by MFEAD
or HSD, related to the provider's alleged fraud are completed. The MCO shall release funds as
directed within 10 business days of the date of release authorization.
19.4. Adverse Action Reporting
Federal regulations, specifically 42 CFR 1002.3(b)(3) requires a state to report all adverse actions taken
on provider applications in the Medicaid program directly to the Federal Department of Health and
Human Services, Office of Inspector General (DHHS/OIG). Adverse actions that must be reported include
a denial of credentialing or enrollment of a provider when the denial is due to concerns other than
fraud, such as integrity or quality, or termination. For entities that are not natural persons, the
information required includes those individuals that have control of, ownership interest in, or managing
employees of the business entity. Examples of conduct that would constitute reporting to HSD (the PIU
and the MAD) include providers that are denied enrollment or termination:
• As a result of adverse licensure actions, e.g., providers who are reported to the Medicare Exclusion
Database, DHHS/OIG/General List of Excluded Individual Entities;
• Due to the engagement of fraudulent conduct;
• Due to abuse of billing privileges (e.g., billing for services not rendered or unnecessary Medical
services);
• Due to misuse of their Medicaid provider billing number;
• Due to falsification of information on enrollment application or information submitted to maintain
enrollment;
• Due to continued billing after suspension or revocation of the provider's professional licensure or
certification;
• Based on a State and/or Federal exclusion; or

Section 19: Program Integrity
Revision dates:
Effective date: January 1, 2019
388 | P a g e
• Due to falsification of medical records which support services billed to Medicaid.
The MCO is directed to notify the PIU Manager and the MAD Provider Enrollment unit in writing of
identified provider adverse actions within five business days from the date the adverse action was
taken. An email is acceptable.
The MCO is required to develop policies and procedures for reporting all adverse actions taken on
provider applications in accordance with this provision and in accordance with HSD's requirements set
forth in 42 CFR 1002.3(b)(3).
The MCO is required to document and report all adverse actions taken on providers on Report 56
pursuant to the "Centennial Care Reporting Instructions Program Integrity-Report #56".
19.5. Recipient Explanation of Medical Benefits
The MCO is required to develop and implement policies and procedures for verifying with managed care
beneficiaries whether billed services were received through Recipient Explanation of Medical Benefits’
correspondence verification process and procedures as set forth in 42 CFR 455.20.
19.6. Fraud, Waste and Abuse Compliance Plan
The MCO is required to have a written Fraud, Waste and Abuse Compliance Plan ("Compliance Plan")
per 4.17.3 of the Agreement. The Compliance Plan must contain procedures designed to detect and
prevent fraud, waste and abuse in the administration and delivery of services under the Agreement. The
Compliance Plan is due to the PIU on July 1 of every State fiscal year. In addition to what is stated in the
Agreement, the Compliance Plan must also contain:
• Written policies and procedures that supports the execution of the Compliance Plan to prevent and
detect fraud, waste and abuse in the administration and delivery of services under the Centennial
Care Program;
• Designate a Compliance Officer and Compliance Committee;
• Training and Education of the MCO's employees, contractors, and providers;
• Auditing and Monitoring;
• Responding to identified or alleged potential fraud and suspicious activities; and
• Whistleblower protection and non-retaliation policy.

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
389 | P a g e
20. Pharmacy
20.1. General Information
Pharmacy Benefits: Centennial Care Programs
Prescription drugs are a benefit under the Centennial Care program to be covered by the MCOs. MCOs
shall support HSD in promptly responding to public and legislative inquiries involving the design and
management of the MCO’s pharmacy benefit.
Preferred Drug List (PDL) and Formulary Requirements
MCOs shall comply with the NMAC 8.308.9.14 Pharmacy Services and the Pharmacy Services section of
the Agreement.
Treatment Guidance for Chronic HCV Infection
MCOs shall establish a system to cover treatment of members over the age of 17 years old with active
Hepatitis C infection for the appropriate amount of time that the therapy requires for the member’s
diagnosis. The system will consist of:
• The approval process of properly requested treatments for members with chronic HCV infection
using the Uniform New Mexico HCV Checklist for Centennial Care (See MAD 634 Attached);
• The development of a provider incentive plan to expand the number of practitioners treating HCV in
New Mexico, including:
o Incentive(s) to receive training in the treatment of chronic HCV infection;
o Incentive(s) to begin treating such patients; and
o Incentives for treatment of each patient;
• Not using active alcohol or drug use as screening criteria for the treatment, approval or denial
process;
• Not using the specialty of the requesting provider as screening criteria for treatment, approval or
denial;
• Referral of all members to a community health worker, Care Coordinator, or MCO specialty
pharmacist at the time of a drug treatment request for guidance and treatment compliance;
• Quarterly data submission concerning number of requests, approvals, and denials by fibrosis stage
(or equivalent) and genotype for all treatment requests;
• A comprehensive plan of outreach to the MCOs’ referring providers requesting oral drug treatment
for chronic HCV-infected patients;

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
390 | P a g e
• A comprehensive plan to expand HCV case finding efforts and screening efforts; and
• A comprehensive plan to expand HCV screening efforts to conform to USPSTF/CDC/ American
Association for the Study of Liver Diseases (AASLD)/ Infectious Diseases Society of America (IDSA)
guidelines.
MCOs are to approve properly requested treatments for the following Centennial Care members with
chronic HCV infection:
• All members over age 17, all HCV genotypes, with a positive Hepatitis C RNA level;
• In all cases, the MCOs shall ensure (using the AASLD/IDSA guidelines) that each treatment request is
appropriate with respect to:
o HCV genotype and viral load;
o Drug dose(s) and duration(s). The MCO’s preferred formulary agent may be given preference if
the level of evidence and effectiveness (as measured by Systemic Vascular Resistance) is equal
or greater, and no drug interactions are of concern;
o The presence or absence of advanced fibrosis or cirrhosis. For the purpose of making treatment
decisions using the AASLD/IDSA guidance, "cirrhosis" can be considered to be present if any of
the following are present:
▪ APRI >= 1.0;
▪ Fib-4 >= 3.25;
▪ Transient Elastography Score>= 12.5 kP (F4 equivalent);
▪ Fibrotest > = 0.73 (F4 equivalent) OR Fibrometer with F4 predominance;
▪ Radiographic imaging or physical exam findings consistent with cirrhosis; and
▪ Liver biopsy confirming a METAVIR Score of F4.
o Prior HCV treatment experience:
▪ Plans may require resistance-associated substitutions testing, based on AASLD guidance.
• Guidance regarding lost or stolen medications:
o MCOs shall use the same criteria currently used for refills of other lost or stolen medications;
and
o MCOs shall use Care Coordination and other functions to minimize this occurrence.
• Guidance regarding requests for off-label, experimental, and other forms of treatment that are not
specified in the guidelines:

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
391 | P a g e
o MCOs shall initiate a peer to peer consultation with the requesting physician to further
understand the request and its rationale; and
o MCOs shall present the case to Project ECHO before issuing a denial.
• Note that a "properly requested treatment" as defined above means that:
o The Uniform Checklist form is completed fully as directed and submitted;
o Necessary lab data and copies of medical records are attached; and
o The requested drug(s), dose(s), and length of treatment are consistent with AASLD/IDSA
guidance as written (the level of evidence in the guidance should not be considered relevant to
length of treatment decisions). If not consistent, MCOs shall provide an appropriate alternative.
• MCOs are granted the option to expand their treatment criteria beyond these guidelines (e.g., to
those 17 years of age and under), with advance notice to and approval by MAD.
Community Pharmacy Reimbursement
• MCOs shall ensure that reimbursement to community-based pharmacies realistically reflect buying
power, buying volume, and price negotiating potential. MCOs must ensure that the Maximum
Allowed Cost (MAC) for ingredient cost generic drugs for community-based pharmacies is no lower
than the current National Average Drug Acquisition Cost (NADAC) listed for the NDC for the drug
item. The dispensing fees will be paid in accordance with the terms of the applicable pharmacies'
contracts.
Where there is no NADAC price available, such as for certain OTC drug items, certain generic drugs
that have few manufacturers, and some repackage products, the MAC must be no lower than the
published Wholesaler’s Average Cost (WAC) listed for the NDC plus 6%. The WAC must come from a
published national pharmacy pricing source such as Medispan or First Data Bank that is not
associated with the MCO or PBM. This pricing methodology for certain OTC drug items aligns with
the State's reimbursement structure under Medicaid FFS. Such pricing is in effect only for drug items
that do not have a NADAC price available.
If the pharmacy submits an ingredient cost less than NADAC (or the WAC plus 6% when applicable),
then the MCO's PBM may use that lower submitted amount as the ingredient cost.
o A community-based pharmacy is a pharmacy that has the following characteristics:

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
392 | P a g e
▪ Is open to the public for prescriptions to be filled, regardless of the facility or practice where
the prescription was written. This includes multi-site pharmacy operations and franchises
whose locations are in New Mexico;
▪ Is located in New Mexico or near the state border, if the border town is a primary source of
prescription drugs for Centennial Care members residing in the border area;
▪ Is not government-owned, not hospital-owned or hospital-based, not an extension of a
hospital, not owned by a corporation owning hospitals, and not an extension of a medical
practice or specialty facility;
▪ Is not owned by a corporate chain with stores outside of New Mexico;
▪ Is not a mail order pharmacy; and
▪ Is not part of a national network of pharmacies or specialty pharmacies, including those
primarily used for supplying IV admixtures.
o A list of pharmacies to which this section of this policy applies is included at the end of this
policy. HSD develops and maintains the criteria for inclusion on the list and applies only to
community-based pharmacies that participate in the MCOs’ Centennial Care network. Inclusion
of a pharmacy on the list does not mandate inclusion of the pharmacy in the MCOs’ Centennial
Care network. This does not supersede any credentialing requirements established by the MCO
or its PBM. Pharmacies on the list that are not contracted for participation in the MCOs’
Centennial Care network will be subject to the MCOs’ out-of-network payment rules.
o The MCO is not obligated to adjust claims retroactively based on changes made by HSD/MAD to
the list.
• Calculation of Payment:
o A pharmacy cannot be required to submit a dispensing fee on the claim, nor shall the payer use
a submitted dispensing fee to limit payment. MCOs must ensure that the contracted dispensing
fee is used in the payment calculations including any applicable professional dispensing fees for
Community Based Pharmacies, as directed by HSD; and
o MCOs must pay for compounding fees when a pharmacist must prepare a compound
medication for a covered FDA approved drug/ingredient, for a dosage form or strength not
already commercially available, as written in a clinician’s prescription. Neither compounding
fees nor reimbursement will apply to a compound that includes non-covered pharmacy products
as defined by MAD regulations. MCOs must also pay HSD-required administration and incentive

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
393 | P a g e
fees for pharmacist’s prescribing/consultation services, when the pharmacist is enrolled with
HSD, permitted by license, and credentialed by the MCO, such as may be done for vaccines,
smoking cessation products, combined hormonal and injectable contraceptives, and Naloxone.
When specifically established by MAD, MCOs will reimburse for administration fees for
injections, including but not limited to injectable vaccines and injectable contraceptives; and
MCOs will reimburse for the counseling fee for Naloxone, in all formulations/delivery methods.
Other counseling for FDA approved drugs, and products, as required by OBRA 90, is a
pharmacist’s dispensing responsibility.
• Updating Prices:
o NADAC prices (or WAC prices plus 6% for OTC drug items) must be implemented within seven
calendar days of NADAC price changes. If a price increase is not made within seven calendar
days, MCOs must ensure that pharmacy claims are adjusted to reflect the price increase for
claims that were not paid at the increased price. A price decrease cannot be implemented
retroactively.
o For MAC prices determined by an MCO (other than NADAC and WAC plus 6%), the MCO must
ensure all MAC payment levels are reviewed, at a minimum, once per week. If there is a price
increase that took place during the week that resets the MAC price, an increase must be
implemented within seven calendar days. If a price increase is not made within seven calendar
days, the MCO must ensure that paid pharmacy claims are adjusted to reflect the price increase,
if they were not paid at the increased price. A price decrease cannot be implemented
retroactively.
o MAC prices must be established by evaluation a range of prices from sources with prices
available in New Mexico. Documentation must be retained on how the price was selected and
how it was determined that the price was available in New Mexico. If an MCO selects the lowest
price available, documentation must be maintained showing that the source of the MAC price is
available from wholesalers in New Mexico. Short-term, special deal prices cannot be used to set
a MAC price at the lowest available price.
MCOs must cover flu shots, including the booster-enhanced flu shots for members when prescribed for
recipients 65 and older and for other conditions per CDC seasonal recommendations.
o MCOs must follow MAD direction regarding the minimum amount of information that must be
reported back to the pharmacy on a price challenge. When a MAC price challenge is made on

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
394 | P a g e
the basis of failing to update a price within the applicable timeframes, and a pharmacy "wins"
the challenge, MCOs must ensure that all pharmacy claims that were underpaid, due to the lack
of a timely update, are adjusted.
o MCOs must require that if the pharmacy does not "win" the challenge, the response to the
pharmacy shall state: the drug price that is in effect on the date of service; the date that the
price was established as the MAC price; if the MAC price has subsequently changed since the
date of the prescription and the current MAC price; the basis of that price (i.e., how the price
was established); the NDC if the price is based on specific NDC; and how they concluded the
price was available in New Mexico.
o MCOs must accept the price challenges directly from the pharmacy if the MCO’s PBM is setting
the price unless the pharmacy contract with the Pharmacy Services Administration Organization
(PSAO) requires challenges to go through the PSAO, in which case the MCO must require the
PSAO to forward challenges to the MCO within three business days of receipt from the
pharmacy, and require the PSAO to forward any response to the pharmacy within three
business days of receipt from the MCO.
o For a claim recoupment or payment reduction made more than seven calendar days after initial
payment, a provider must be notified about the reason for the recoupment or reduction, the
amount of the recoupment or reduction, and given an opportunity to appeal or file a grievance.
There is no fair hearing right. This requirement does not apply if the pharmacy is reversing or
rebilling the claim that results in a recoupment or payment reduction.
o If the pharmacy contract with the PSAO requires that notice of payment recoupment or
reduction go through the PSAO, the MCO must require the PSAO to forward such notices
including language regarding the opportunity to appeal the pharmacy within three business days
of receipt from the MCO and the PSAO to forward any response to the MCO within three
business days of receipt from the pharmacy.
MCO Participation in the DUR Board and Submission of a DUR Annual Report
MCOs shall take part in a DUR program that complies with the requirements set forth in 42 C.F.R. §
438.3(s) and 42 CFR Part 456 Subpart K, and Section 1927(g) of the Social Security Act, to ensure
prescriptions are appropriate, medically necessary, and minimize the potential for adverse medical

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
395 | P a g e
results. MCO representation on the DUR Board shall consist of one physician and one or two
pharmacists.
DUR Reporting Requirements:
MCOs are contractually responsible for providing outpatient drug benefits and for conducting utilization
review activities to promote the delivery of quality medically necessary care in a cost effective and
programmatically responsible manner. To ensure all areas of section 1927(g) of the Act are met, MCOs
must provide a detailed description of their DUR program activities to the State on an annual basis.
MCOs are required to take part in a DUR program and as part of this program, per CMS requirements,
each MCO will be required to submit a DUR report to HSD that will be submitted to CMS. The report
template is provided by CMS and at minimum shall contain the following:
• A description of the nature and scope of the prospective and retrospective drug review program;
• Detailed information on the specific criteria and standards in use;
• A summary of the educational interventions used and an assessment of the effect of these
• interventions on the quality of care; and
• An estimate of the cost savings generated as the result of the program.
For your reference, the following are links to the CMS website for previous DUR reports:
All States:
https://www.medicaid.gov/medicaid/prescription-drugs/drug-utilization-review/annual-reports/index.h
tml
New Mexico:
https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Prescription-Drugs/Downloa
ds/2016_New Mexico_DUR.pdf
MCO requirements regarding the Drug Rebate Analysis and Management System (DRAMS) and drug
rebate dispute resolution
HSD’s PBM will continue to send drug rebate invoices to manufacturers based on the encounter data for
pharmacy and medical claims submitted by the MCOs. HSD’s PBM will receive copies of the
manufacturers' checks. If the manufacturer does not pay the invoice in full because the manufacturer
disputes some of the data on the invoice, HSD’s PBM will refer the manufacturer dispute to the
appropriate MCO staff.

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
396 | P a g e
Typically, when the manufacturer disputes the invoice based on incorrect data on the claims, the
manufacturer will request claim level detail (CLD). HSD’s PBM will send the CLD to the manufacturer.
After the manufacturer reviews the CLD, the manufacturer may issue a dispute in the form of an email
or letter, and request that the payer review the claims.
When a dispute is reported to the MCO, the MCO is responsible for reviewing their pharmacy claims
data to determine if the data needs to be corrected or if the data is correct. This entails reviewing claims
and possibly contacting pharmacy and medical providers to obtain information to resolve the dispute.
The MCO must report the resolution of the dispute to HSD’s PBM within 30 calendar days from the date
of receiving the notice of the dispute.
A smaller number of disputes are initiated after the manufacturer has already paid the invoice. These
disputes will be handled in the same manner as other disputes.
HSD’s PBM will review the MCO pharmacy and medical drug claims data prior to printing invoices in an
attempt to minimize disputes. Often, for specific drug items, reporting the correct number of units is a
common problem and the correction may be obvious to HSD’s PBM. In such cases it will make the
change prior to printing invoices. Usually, the problem occurs when the standard billing units differ from
the units that CMS expects to be used on the rebate invoices. A problem also may occur when an MCO
allows a provider to bill incorrect units. HSD’s PBM will notify an MCO of any situation where the MCO
continues to make the same error in data and the MCO will be required to implement corrections in
their processing of claims.
Common Dispute Reasons
Disputes frequently result from recurring circumstances and often for the same drug items each quarter.
When the error that will likely lead to a dispute originates with the provider and the MCO does not
detect the error when processing the claim, the MCO will be asked to correct their claims processing
editing to avoid continual disputes.
The following sections identify the most common reasons for disputes.
Unit Type Discrepancy
A provider bills a claim utilizing a unit type that differs from the unit type that was utilized in
calculating the rebate. Most claims processing systems allow providers to utilize only three unit types
when billing claims. Common claim processing system unit types:

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
397 | P a g e
• Each (caps, tabs, kits, and vials)
• Milliliters (liquids)
• Grams (solids)
CMS has eight unit types for claims:
• AHF (refers only to injectable Anti-Hemophilic Factor units)
• CAP (capsule)
• SUP (suppository)
• GM (grams)
• ML (milliliter)
• TAB (tablet)
• TDP (transdermal patch)
• EA (each, refer to drugs not identifiable by any other unit type as given in program instructions)
Staff of HSD’s PBM will convert the common claims processing unit types before preparing manufacturer
invoices. If a dispute occurs based on unit conversion or for units that were not converted, HSD’s PBM
will make the correction in order to resolve the dispute.
If the unit type appears to be incorrect on the original encounter claim, the dispute will be sent to the
MCO DRAMS contact for resolution.
Data Entry Errors Regarding the Quantity
Incorrect quantities are sometimes entered on the claims by the provider. If the MCO does not detect
the incorrect quantities, this can cause discrepancies
with the number of units shown as dispensed on
the claim.
In resolving this type of dispute, the MCO DRAMS contact should review the claims data and determine
if the provider billed incorrectly. This will entail looking at the claim; contacting the provider and
requesting what the units represent (ML, GRAMS, and EACH). If it is an “each”, determine what the
“each” represents (CAP, TAB, kits or vials). If the claim was billed incorrectly, the provider must adjust
the claim with the correct units.

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
398 | P a g e
Decimals
When the drug strength does not equal a whole number, or the units of measure or package size has a
decimal in the units, a decimal point in the units could mean a provider error.
If the MCO does not detect the incorrect quantities, this can cause discrepancies because use of a
decimal point may be illogical for many unit types for drug items.
In resolving this type of dispute, the MCO DRAMS contact should review the claims data in question and
determine if the provider likely billed incorrectly. It may be necessary to contact the provider if the units
are unusual and the MCO DRAMS contact cannot tell whether the provider's units are correct or
incorrect.
Units or Quantities Appear Inconsistent
If the units billed for a particular NDC are inconsistent with the number of prescriptions, the pharmacy
reimbursement or lowest dispensable package size, the drug manufacturers will question the amount
dispensed, if it appears to be an unexpected amount.
In resolving this type of dispute, the MCO DRAMS contact should review the claims data in question and
determine if the provider likely billed incorrectly. It may be necessary to contact the provider if the units
are unusual and the MCO DRAMS designate cannot tell whether the provider's units are correct or
incorrect.
Terminated/Invalid NDCs
Terminated NDCs (dispute code N) are those products where the shelf life for the last lot produced has
expired. Per CMS guidelines, the affected manufacturer or labeler is required to submit pricing data and
pay rebates for four quarters past the termination date, but only for claims with a date of service prior
to the termination date.
HSD’s PBM will contact the manufacturer to obtain the termination date and determine whether the
date has been provided to CMS. If advised that a termination date has been sent to CMS and a sufficient
amount of time has elapsed since that submission (two quarters), HSD’s PBM will provide the MCO
DRAMS contact staff with a list of the providers involved (i.e., those with the most claims for the drug
and quarter in question). The MCO DRAMS contact must notify the providers. If the provider has the
product on the shelf, they will need to provide the lot number and expiration date and provide the
information to staff of HSD’s PBM.

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
399 | P a g e
Affected claims must be checked to identify all DOS that fall after the termination date. For those claims,
an adjustment must be made. The provider must adjust the claim if the incorrect NDC code was used.
State Units Exceed Expected Sales/No Record of Sales in the State
Manufacturers have a threshold on their NDC numbers and if they hit that threshold they will dispute
claims based on units exceed expected sales. They also will dispute if they show no record of sales of
their product within the state.
In resolving this type of dispute, the MCO DRAMS contact should determine if the provider used the
NDC code. Sometimes the provider can show they did order an item from out of state or have other
documentation that their billing was correct. The MCO must obtain documentation from the provider of
purchase, such as an invoice from their wholesaler with the NDC in question and the amount purchased.
This must be forwarded to HSD’s PBM so that it may provide the information to the drug manufacturer
when requested. The provider must adjust the claim, if the incorrect NDC code was used originally.
Inaccurate NDC
A pharmacy or medical provider may submit a claim in which the NDC billed is not the NDC dispensed. In
resolving this type of dispute, the MCO should contact the provider and determine if they really used
the NDC code reported.
The provider must adjust the claim if the incorrect NDC code was used.
Communicating with HSD’s PBM on Disputes and Correcting Errors
The MCO is to notify HSD’s PBM of claims on which the units were incorrect. HSD’s PBM will enter a
comment into DRAMS that the units were incorrect and that the MCO is working on adjustments. HSD’s
PBM will notify the manufacture regarding the status of the dispute.
HSD’s PBM cannot change the units on a claim, therefore, it is necessary for the MCO to have the
provider adjust the claim. When the encounter data is adjusted, the DRAMS system will back out the
incorrect quantity and issue new invoices with the new quantity as a prior quarter adjustment.
If the MCO verifies that some of the disputed quantities are correct, the MCO must notify HSD’s PBM.
HSD’s PBM will enter a comment into DRAMS that the units were correct and state how the quantity
was verified such as, a call to the provider. HSD’s PBM will notify the manufacturer. The manufacturer

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
400 | P a g e
may request further documentation such as an invoice from the provider. When further documentation
is requested, HSD’s PBM will notify the MCO who will be responsible for obtaining the documentation.
MCO Compliance with the PBM Regulation Act
The MCO will ensure the PBMs are in compliance with the requirements outlined in the Pharmacy
Benefits Manager Regulation Act, NMSA 1978 § 59A-61. The MCOs shall ensure they are monitoring the
PBMs’ performance on an ongoing basis and the applicable requirements outlined in the Agreement
7.14: Major Subcontractors and Subcontractors are followed.

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
401 | P a g e

Section 20: Pharmacy
Revision dates: October 1, 2020
Effective dates: January 1, 2019
402 | P a g e

Section 21: Manual Acronyms
Revision dates:
Effective dates: January 1, 2019
403 | P a g e
21. Manual Acronyms
The following is a list of acronyms used throughout the document.
AAAHC Accreditation Association for Ambulatory Health Care
AASLD American Association for the Study of Liver Diseases
ABCB Agency Based Community Benefit
ABP Alternative Benefit Plan
ADHD Attention Deficit/Hyperactivity Disorder
ADL Activities of Daily Living
AHU Administrative Hearing Unit
ALJ Administrative Law Judge
ALTSD/ADRC Aging and Long-Term Services Department, Aging and Disability
Resource Center
APS Adult Protective Services
ARTC Accredited Residential Treatment Center
BH Behavioral Health
BHSD Behavioral Health Services Division
BISF Brain Injury Services Fund
BLN Business Leadership Network
BRCA Breast Cancer Susceptibility Gene
BSC Behavior Support Consultant
CAHPS Consumer Assessment of Healthcare Providers and Systems
CAP Corrective Action Plan
CB Community Benefit
CBC Criminal Background Check
CBMA Community Benefit Member Agreement
CBSQ Community Benefit Service Questionnaire
CCL Care Coordination Level
CCP Comprehensive Care Plan
CCU Care Coordination Unit
CDC U.S. Centers for Disease Control and Prevention

Section 21: Manual Acronyms
Revision dates:
Effective dates: January 1, 2019
404 | P a g e
CFR Code of Federal Regulations
CHR Community Health Representative
CHW Community Health Worker
CIA Client Individual Assessment
CIU Client Information Update
CLD Claim Level Detail
CNA Comprehensive Needs Assessment
COE Category of Eligibility
COR Consolidated Online Registry
COTA Certified Occupational Therapy Assistants
CPR Cardiopulmonary Resuscitation
CPS Child Protective Services
CRI Community Reintegration
CSA Core Service Agencies
CTA Community Transition Agency
CYFD New Mexico Children, Youth and Families Department
DD Developmentally Disabled
DDW Developmental Disabilities Waiver
DHHS/OIG U.S. Department of Health and Human Services, Office of
Inspector General
DHI Department of Health Improvement
DME Durable Medical Equipment
DMZ DMZ is short for DeMilitarized Zone and is software/web page
for the transmission and storage of data.
DOH/OSAH Department of Health’s, Office of School and Adolescent Health
DOS Dates of Service
DRAMS Drug Rebate Analysis and Management System
DSP Direct Support Professionals
DTE Difficult to Engage
DVR Division of Vocational Rehabilitation
DWS Department of Workforce Solutions

Section 21: Manual Acronyms
Revision dates:
Effective dates: January 1, 2019
405 | P a g e
EOB Explanation of Benefits
EOR Employer of Record
EPSDT Early Periodic Screening, Diagnostic, and Treatment
EQRO External Quality Review Organization
EVV Electronic Visit Verification
FFS Fee for Service
FHB Fair Hearings Bureau
FMA Financial Management Agency
FQHC Federally Qualified Health Center
FTP File Transfer Protocol
Geo/Access Geographical Access
HCBS Home and Community Based Services
HCV Hepatitis C Virus
HHA Home Health Agency
HHR/HRU High Health Risk/High Resource Utilization
HNF High Nursing Facility
HRA Health Risk Assessment
HSD New Mexico Human Services Department
I/T/U Indian Health Services, Tribal Health Providers, and Urban
Indian Providers
IADL Instrumental Activities of Daily Living
ICF IID Intermediate Care Facilities for Individuals with Intellectual
Disabilities
ID/RC Intellectual Disability/Related Condition
IDEA Individuals with Disabilities Education Act
IDSA Infectious Diseases Society of America
IDT Interdisciplinary Team
IHS Indian Health Service
IPoC Individual Plan of Care
ISD Income Support Division
ISP Individual Service Plan

Section 21: Manual Acronyms
Revision dates:
Effective dates: January 1, 2019
406 | P a g e
JAN Job Accommodation Network
JCAHO Joint Commission on Accreditation of Healthcare Organizations
LISW Licensed Independent Social Worker
LMFT Licensed Marriage and Family Therapist
LMSW Licensed Master Social Worker
LNF Low Nursing Facility
LOC Level of Care
LOD Letter of Direction
LOI Letter of Interest
LPAT Licensed Practicing Art Therapist
LPC Licensed Professional Counselor
LPCC Licensed Professional Clinical Counselor
LPN Licensed Practical Nurse
LRI Legally Responsible Individual
LTC Long Term Care
LTSS Long Term Services and Supports
LTSSB Long Term Services and Supports Bureau
MAC Maximum Allowed Cost
MAD Medical Assistance Division
MCO Managed Care Organization
MCO/UR Managed Care Organization/Utilization Review
MDS Minimum Data Set
MF Medically Fragile
MFCMP Medically Fragile Case Management Program
MFEAD New Mexico Medicaid Fraud and Elder Abuse Division
MFW Medically Fragile Waiver
MH Mental Health
MMIS Medicaid Management Information System
MSDS Material Safety Data Sheets
NADAC National Average Drug Acquisition Cost
NCQA National Committee for Quality Assurance

Section 21: Manual Acronyms
Revision dates:
Effective dates: January 1, 2019
407 | P a g e
NF Nursing Facility
NMAC New Mexico Administrative Code
NMSA New Mexico Statute Annotated
NOA Notice of Allocation
NOME Not Otherwise Medicaid Eligible
NPI National Provider Identifier
OT Occupational Therapy
OTC Over the Counter
PASRR Preadmission Screening and Resident Review
PCMH Patient Centered Medical Home
PCO Planning Center Online
PCP Primary Care Physician/ Primary Care Provider
PCS Personal Care Services
PDL Preferred Drug List
PFOC Primary Freedom of Choice
PH Physical Health
PHI Protected Health Information
PIPs Performance Improvement Projects
PIU Program Integrity Unit
POC Plan of Care
PPA Provider Participation Agreement
PPACA Patient Protection and Affordable Care Act
PRF Payment Request Form
PSA Prostate-Specific Antigen
PSAO Pharmacy Services Administration Organization
PT Physical Therapy
PTA Physical Therapy Assistants
QA Quality Assurance
QI Quality Improvement
RFA Request for Administrative Action
RFI Request for Information

Section 21: Manual Acronyms
Revision dates:
Effective dates: January 1, 2019
408 | P a g e
RHC Rural Health Clinic
RN Registered Nurse
RTM Return to Member
SB Support Broker
SDCB Self-Directed Community Benefit
SIER Self-Identified Error Resubmission
SIU Special Investigative Unit
SLP Speech Language Pathologist
SLT Speech and Language Therapy
SMEs Subject Matter Experts
SMI Serious Mental Illness
SNF Skilled Nursing Facility
SOC Setting of Care
SOE Summary of Evidence
SSI Supplemental Security Income
SSN Social Security Number
SSP Service and Support Plan
STI Sexually Transmitted Infection
SUD Substance Use Disorder
TB Tuberculosis
TBI Traumatic Brain Injury
TFC Therapeutic Foster Care
TPA Third Party Assessor
UB Universal Billing
UM Utilization Management
USPSTF United States Preventive Services Task Force
VAS Value Added Services
VBP Value Based Purchasing
WAC Wholesaler’s Average Cost
