

Acknowledgements
Written by Dan DeSena, LMSW, DMA
Editors:
Pam Schweitzer, APRN, BC
Laura Lokers, LCSW
Ricks Warren, PhD
Based in part on the knowledge and expertise of:
James Abelson, MD, PhD
Joseph Himle, PhD
Laura Lokers, LCSW
Pam Schweitzer, APRN, BC
Ricks Warren, PhD
i.

Anxiety Program
Depression Program
CBT
Exposure
Group for
Anxiety
CBT
Cognitive
Skills Group
for Anxiety
Mindfulness
for Anxiety
Group
CBT Basic Group for
Anxiety
(2 sections)
CBT
Cognitive
Skills Group
for
Depression
CBT
Behavioral
Activation
Group for
Depression
CBT Basic Group for
Depression
Mindfulness-Based Cognitive Therapy
for depression relapse prevention
ii.

Weekly Group topics:
Anxiety Vulnerability Management (week 1)
Do you ever think you have more anxiety than
other people? Find out why and learn how to use
CBT skills to fight your anxiety over the long term.
Relaxation (week 2)
Just relax! What to do and when to try relaxation
strategies to help make you feel less stress and
tension in your daily life.
Exposure and Desensitization (week 3)
“Avoid avoidance:” how our behaviors can make
anxiety worse, and the surprising way to get it to
leave us alone!
Cognitive Therapy Skills (week 4)
Our thoughts matter! Learn ways our thoughts can
change how we feel and influence what we do.
Turn thoughts into your ally, instead of your enemy.
What is this group all about?
-Our group is an introduction to the basic concepts and
skills of CBT.
-There are four sessions, each with a different topic.
-These are offered weekly, the first four Mondays and
Tuesdays of every month. Each Monday and Tuesday is
the same topic, so you can come to whichever fits your
schedule best.
-You can attend these in any order you like.
-Each session we will cover just some of these CBT
skills. If you have questions during the group, please ask!
It is also possible any confusion you have at the
beginning will clear up as you continue to attend
the sessions.
-This group is not meant to fix your anxiety completely.
We want to give you a chance to try out some of these
techniques and understand your anxiety better. When you
get done with this group you may want to continue with
group or individual CBT treatment here at U of M.
We want to be sure that our treatment is
effective!
Evidence-based means that there is scientific
evidence to show that something works.
CBT is an evidence-based treatment that has been
studied and shown to be effective in hundreds of
scientific experiments.
While there is no 100% guarantee that CBT will
work for you, it is likely that with practice and hard
work you will receive benefit from these
techniques.
What is Cognitive-Behavioral Therapy?
Cognitive-Behavioral Therapy (CBT) is a short-term,
evidence-based treatment for many problems, including
anxiety. It is based on the idea that thoughts (cognitions)
and behaviors affect the way we feel.
Feelings (emotions)
Thoughts (cognitions) Behaviors (actions)
How to use this manual
This manual includes a lot of information on anxiety and CBT– more than we have time to cover in the group sessions, and perhaps more than you
will have time to review on your own! You will get the most out of this group if you take notes during the group and then review the manual
between sessions. Remember that different people get benefit from different CBT skills, so we expect that you will use the skills that work and let
go of the rest. We hope that you will try each skill out to determine if it suits you. Refer to “Appendix IV: This is so much information! Where
do I start?” to make your reading more efficient by starting with the information most pertinent to your particular problem. Finally, be sure to
bring the manual back next week!
iii.

There is a great deal of scientific research on
psychotherapy, and we know a lot about what
can be helpful for people. We continue to
learn more and more about how to use
psychotherapy to help as many people as
possible.
However, because everyone is different, and
our brains and lives are very complex, right
now it is often hard to know exactly what it is
that will help a particular person feel better.
On the next page, follow the
path from the bottom of the
page upward for some tips to
make your “path through
psychotherapy” more helpful
and rewarding.
iv.
See this as just one piece of the puzzle in your process of better understanding
yourself and moving toward what you want in your life. Get all you can out of it
and then make efforts to find out what other types of work could be helpful. For
example, maybe you did a great deal of work on managing your depression with
cognitive and behavioral skills. Now you believe that you want to improve your
relationships to achieve more in that area of your life.
Manage barriers to showing up regularly to treatment and practicing skills: improvement
depends primarily on follow-through and the amount of work you put into your therapy.
Address depression from different angles. There is no one “silver bullet” that will
change depression all by itself. Usually a combination treatment, or mixed
approach is what works best to make depression better. This also means putting in
some effort to understand the different ways to manage your depression.
Practice skills over, and over, and over. It usually takes time for changes in our
behavior and thinking to lead to feeling better. Like learning an instrument, we
are practicing new ways of doing things that will feel “clunky” at first, and
become more comfortable over time.
Take small steps toward change each day. Try not to wait for “light bulb
moments,” “epiphanies,” or for something to take it all away instantly.
Expect ups and downs during the process. Think of it as “2 steps
forward, 1 step back.” Try not to get too discouraged or give up
when things seem to move backward or stagnate.
Make it about you: engage in your treatment because you want to improve your life,
take responsibility for achieving you aims, and feeling better, not because others are
telling you to do so. Remember that even if you are being pushed to engage in therapy
by someone else, that relationship must be important enough for you to consider this
option!
Maintain an open mind about the possibility of change, while being realistic about
how fast this change can happen.
Especially at first, gauge success according to how you change your responses to stress,
uncomfortable emotions, and body sensations, not whether or not these things exist or
continue to occur. Focus on valued action, even more than just “feeling better.”
“Credibility:” Make sure the treatment in which you are engaging makes sense to
you and seems to be addressing your problem. There are different paths to the
same goal. If this type of therapy is not working for you, you are confused about
what you are doing, or you have any other concerns, talk to your clinician right
away. Clinicians are trained to have these discussions with their patients!
Make sure your definition of the “problem” is the same as the clinicians with
whom you are working. Maybe they think it is “depression” and you think it is
something else. Try to clarify this with your clinicians.
v.

Section One: Anxiety 101……………………………………………………………………………………………………………………….…………………………………………………..1.1
Anxiety Is……………………………………………………………………………………………………………………………………………………………………………1.2
Why does my body do this? …………………………………………………………………………………………………………………………………1.3
Anxiety “Triggers” …………………………………………………………………………………………………………………….…………………..……………1.4
Anxiety “Fuel” …………………………………………………………………………………………………………………………….……………………...…………1.6
Anxiety 101 Summary…………………………………………………………………………………………………………………………….…………………1.9
Section Two: Exposure and Desensitization ……………………………………….…………………………………………………………………..………………2.1
What is exposure? …………………………………………………………………………………………………………………………………….…………………2.2
Should I do exposure? ……………………………………………………………………….…………………………………………………………...………2.3
Desensitization……………………………………………………………………………………………..................................................................................................2.4
Exposure: Getting Started……………………………………………………………….........................................................................................................2.6
The Exposure Formula……………………………………………………………………………………………………….………….………….……………2.8
Exposure Tips………………………………………………………………………………………………...………………………………..……………….……………2.9
Exposure: Tracking Your Progress5………………………………………………...………………………………..………………....…………2.10
Exposure examples: “External Cue Exposure” ………………………...……………………………..………………....…………2.11
Exposure Examples: “Internal Cue Exposure” for Panic Disorder……………..……………….…………2.12
Questions about Exposure…………………………………………………………………………………………..……………….…....……….…………2.14
Exposure for Obsessive-Compulsive Disorder…………………………………………..…………..…….…....……….…………2.15
Barriers in Exposure Treatment……………………………………………………………………………..……………….…....….…….…………2.16
The Freedom of Choice: Exposure in Daily Life……………………………………..……………….…....….…….…………..2.17
Exposure and Desensitization Summary………………………………………………………..………..…………….…....….…….……2.18
Fear Hierarchy Homework Form (blank) ………………………………….…………………..………..……………...….…....….……2.19
Exposure Tracking Form (blank) ………………………………………………………………………..……………….…….......……….……….2.20
Exposure Tracking Form for Hourly Exposure (blank) …………………......………………….……...........…….…….2.21
Section Three: Cognitive Therapy Skills……………………………………………………………………..…………………………..…….…….......….…….………3.1
What are Cognitive Therapy Skills? ………………………………………..…………………...……………..…….…….......….…….………3.2
Negative Automatic Thoughts………………………………………..…………………………………………...…..…….…….......….…….………3.4
Identifying Negative Automatic Thoughts………………………………………..…………………………..…….…..….…….………3.6
Thought Cascade Worksheet……………………………………….………………………..…………………………..…….…….......….…….………3.7
Daily Thought Record Worksheet………………………………………..………………………………………..…….…….......….…….………3.8
Cognitive Distortions………………………………………..…………………………..…….…….......….…….………………………………………………..3.9
Examples of Cognitive Distortions………………………………………..……………………………………..…….…….......….…….………3.10
Examining the Evidence………………………………………..…………………………..……………………………………….…….......….…….………3.12
The Gambler: Predicting Ourselves Anxious………………………………………..………...……..…….…….......….…….………3.13
Catastrophizing: “That Would Be Horrible” ……………………………..…………………………..…….…….......….…….………3.14
Examining Thoughts, Written Method………………………………………..……...………………..……..…….…….......….…….………3.16
Examining Thoughts Worksheet…………………………………………………..……..…………………………..…….…….......….…….………3.17
“The Only Thing We Have to Fear is Fear Itself:” How to work on
negative thoughts about anxiety and panic attacks……..…….……..........….…….………3.18
“Don’t worry…”
Cognitive Skills for Daily Worry and Generalized Anxiety.......….……….……3.24
Common Thoughts about Anxiety and its Treatment……………………………..……..….……3.30
Cognitive Therapy Skills Summary…………………………..…………………………………………..……..….….…….......….…….………3.31
Table of Contents, con


This part of the group is meant to explore important information about the anxiety itself. The
first step to managing anxiety is understanding it as well as we can– to “know thine enemy,”
so to speak.
“We experience moments absolutely free from worry. These brief respites are called panic.”
~Cullen Hightower
On the pages entitled “Anxiety is…” and “Why does my body do
this?” we’ll talk about:
-What the anxiety “alarm” really is: the “fight or flight”
response— and what its common symptoms are
-The difference between normal anxiety and “phobic”
anxiety
-What causes anxiety
-Why our bodies do what they do when we are anxious
-Why we can’t just “get rid of” the anxiety
In the section “Anxiety Triggers,” we’ll go over the different
things that can trigger anxiety and how the brain comes to believe
these triggers are dangerous.
In our final section, “Anxiety Fuel,” we learn about common ways
that anxiety can get worse, and how our own thoughts and behaviors
play a role in this process.
1.1

Anxiety Is…
The most pure form of the “fight or flight” response is a panic attack, which involves a rush of anxiety symptoms, many of which are
listed below, usually peaking in about 10 minutes. In these cases, the body is trying to tell us “something dangerous is happening right
now!” Other forms of anxiety that are less acute but often just as debilitating, such as chronic worry, involve symptoms similar to the
“fight or flight” symptoms of panic attacks. However, in these cases, it is as if the body is saying “something dangerous is going to
happen sometime in the future… so watch out!” The differences between the two are the intensity of the response and the context in
which it is triggered. In this manual we will refer to all anxiety symptoms as being related to the “fight or flight” response. The most
common anxiety symptoms are listed below. Try circling the ones that apply to you.
What causes anxiety?
We know from scientific research that anxiety is caused by a combination of factors related to both “nature” (genetics) and
“nurture” (experience). Check out page 82 for a more detailed explanation of the factors that can lead to anxiety.
Why can’t I just get rid
of my anxiety?
Anxiety is as vital to our
survival as hunger and thirst.
Without our “fight or flight”
response we would not be as
aware of possible threats to our
safety. We also might not take
care of ourselves or prepare
adequately for the future. And
we probably wouldn’t enjoy a
scary movie or a roller coaster!
Anxiety is necessary to protect
us and can even be fun at times.
It isn’t in our best interests to
get rid of it completely!
When “fight or flight” goes too far: “Phobic” anxiety
Everyone experiences anxiety from time-to-time. We often get the question: “How do I
know if I have an anxiety disorder?” An anxiety disorder is diagnosed when someone
experiences anxiety symptoms and these symptoms:
-Interfere with a person’s life aims
-Happen too often or with too much intensity, given the actual
danger of a situation
-Are not explained by other factors, such as a medical problem or
substance abuse
Some people experience significant anxiety and choose simply to live with it. It is up to
you to decide if you can handle the anxiety on your own, or if treatment is necessary.
Physical Symptoms
-Rapid heartbeat
-Sweating
-Trouble breathing
-Tightness in the chest, chest pain
-Dizziness
-Feeling: “Things aren’t real”
-Feeling: “I don’t feel like myself.”
-Tingling and numbness in fingers, toes,
and other extremities
-Nausea, vomiting
-Muscle tension
-Low energy, exhaustion
-Changes in body temperature
-Shaking, jitters
-Urgency to urinate or defecate
-Changes in vision and other senses
Take home point:
The symptoms of anxiety are the “fight or flight” response, and are normal, functional, and
necessary for survival. They become a problem when they are too severe or happen too often, given
the real amount of danger present, or if it interferes with the activities of life.
Remember: Anxiety is uncomfortable, not dangerous!
Cognitive (thinking) Symptoms
-Worries
-Negative thoughts about one’s ability to
tolerate emotions or future stress
-Negative predictions about future
events
-Other common thoughts:
“I am going crazy!”
“I am going to have a heart attack!”
“I am going to faint.”
-Trouble concentrating or keeping
attention
-Magical ideas, phrases or images such
as “If I do not wash my hands I will
die or someone will be harmed.”
-Preoccupation with body sensations or
functions
Behavioral Symptoms
-Avoidance of anything that provokes
anxiety, including people, places,
situations, objects, animals,
thoughts, memories, body
feelings, etc.
-Protective, “safety” behaviors
-Aggression, verbal abuse, lashing out
-Alcohol and/or drug use
-Compulsive behaviors, such as
excessive checking or other
unreasonable or harmful rituals or
routines
Anxiety is a part of our bodies’ natural alarm system, the “fight or flight” response, which exists to protect us
from danger. These natural body responses are not harmful— but they are really uncomfortable!
1.2

Anxiety Symptom
1. Rapid heartbeat_______
2. Sweating_______
3. Flushing in face_______
4. Tightness in the chest, chest pain_______
5. Feeling: “Things aren’t real”_______
6. Feeling: “I’m not myself”_______
7. Tingling or numbness in
fingers and toes_______
8. Nausea, vomiting_______
9. Muscle tension, stiffness_______
10. Low energy, exhaustion______
11. Changes in body temperature_______
12. Shaking, jitteriness______
13. Urgency to urinate or defecate_______
14. Hyperventilation or trouble breathing_____
15. Dizziness, lightheadedness_____
16. Worries_______
17. Negative predictions about future events_______
18. Trouble concentrating or keeping attention______
19. Avoiding_______
20. Fight or be aggressive_______
21. Changes in vision, hearing, smell, taste_______
22. Dry mouth______
There is a reason!
We have evolved over millions of years to better protect ourselves. Our brains have learned to automatically signal danger when it is
present or we perceive that we may be harmed in some way. Each symptom of anxiety has a specific evolutionary purpose, to help us
“fight” or “flee.”
Try to figure out how each symptom of anxiety is used by our bodies to protect us when we are in danger, by matching the
evolutionary purpose with the anxiety symptoms. Some in the right-hand column may be used twice, and there may be multiple
answers for some symptoms. Once you are done, you can see if you were right— the answers are at the bottom of the page. Also, a
more detailed diagram of the biology of the “fight or flight” response is in Appendix I, “The Biology of Fight or Flight.”
Purpose
A. Muscles contract and tighten to help us fight or flee
B. Push blood around the body faster to supply cells with
oxygen in case we need to use energy to flee or protect
ourselves
C. Lots of energy is spent for body to protect us
D. Body increases speed and depth of breathing
E. Thoughts tend to be negative and protective; it is dangerous
to have “good” thoughts if we are in danger!
F. Must stay alive, even if it means using force
G. Try to think of ways to protect ourselves in case bad things
happen in future
H. Brain is constantly scanning for danger, from one thing to
next
I. Body stops digestion and attempts to rid itself of excessive
harmful substances
J. If something is dangerous, remember it and get away from it!
K. Cools us off when we are running or fighting and makes it
harder for a predator to grab us
L. Blood is redirected away from head, skin, fingers, and toes; if
we are cut, we will not bleed to death as easily
M. Decrease in salivation
Did you know… when our body’s “fight or flight” alarm is triggered, a domino effect of chemical changes and messages are sent to
various parts of the brain and body, producing these symptoms. This process is programmed to last only about 10 minutes, unless it is
triggered again.
Answers: 1. B 2. K 3. B 4. A,D 5. L 6. L 7. L 8. I 9. A 10. C 11. L 12. A 13. I 14. D 15. L 16. E 17. G 18. H 19. J 20. F 21. L 22. M
1.3

Types of anxiety triggers and the Anxiety Disorder “Diagnosis”
Nearly anything can be trained to trigger the “fight or flight” response. Psychiatrists, psychologists, psychiatric nurses, and clinical
psychiatric social workers have tried to find ways to tell the difference between different types of anxiety triggers. Anxiety disorder
diagnoses come out of this attempt. While a diagnosis is not a perfect way of describing a person’s experiences, it can help us to
know what types of treatments may be effective. Different groups of triggers and the diagnoses most frequently associated with them
are listed below. Some of these categories overlap, and it is possible for one person to have more than one diagnosis.
“One thing leads to another:” how a trigger becomes connected with our “fight or flight” response
When we perceive danger, whatever it is that could be dangerous (in this case, a spider) is remembered by the amygdala. The next
time something reminds us of the spider, or we actually come into contact with one, our anxiety “alarm” goes off.
Our brains are designed to keep us safe. The anxiety
part of the brain, the amygdala, is like a radar that is
trained to spot dangerous objects and situations.
When this “radar” spots something that could be
dangerous, it tells the brain to begin the “fight or
flight” response, producing the uncomfortable
feelings we get when we are anxious.
+ “danger” or something bad happening =
(for example, getting bitten by the spider)
+
!!!
Now and in
future
Diagnosis
Generalized Anxiety Disorder (GAD)
Social Anxiety Disorder (Social Phobia)
Panic Disorder
Agoraphobia
Specific Phobias
Obsessive-Compulsive Disorder (OCD)
Post-Traumatic Stress Disorder (PTSD)
Trigger
Worries, predictions, and negative thoughts about the future
Social situations and people, such as social events and performances, along
with fear of criticism from others
Fear of having a panic attack and fear of body feelings that remind one of
panic attacks
Places a panic attack has happened before or could happen
Places, situations, animals, objects, blood or injury, etc.
Disturbing intrusive thoughts, contamination, doubt and urge to check things,
etc.
Memories and things associated with a traumatic event
1.4
To identify what makes you anxious, ask yourself the following questions:
“When I feel scared or nervous, what is going on around me or what am I thinking about?”
“Am I worried about having more anxiety in the future?”
“Am I afraid of body sensations that remind me of intense anxiety attacks?”
“Do I ever try to do more than I can handle or create unrealistic expectations for myself or others?”
“Am I worried that I will not be able to cope if bad things happen in the future?”
Exercise
My anxiety triggers are:
List here the objects, situations, events, or places that tend to trigger your anxiety. Use
the questions above if you are having trouble figuring out what makes you anxious.
1.
2.
3.
4.
5.
6.
7.
Anxiety “Triggers” take home points:
The brain can learn to be afraid of
almost anything, and some anxiety
“triggers” are more common than
others. These triggers help define
anxiety disorder diagnoses, which we
use to better understand the anxiety
and develop treatments.
Anxiety can be caused by scary events,
and anxiety can also make one more
likely to experience an event as scary.
It is important to understand your
anxiety “triggers.” In most cases it is
possible to figure them out yourself.
Sometimes it is necessary to have the
help of a mental health professional to
do so.
“Which came first, the chicken or the egg?”
Anxiety “Triggers,” continued
Scary event?? Anxiety??
We know from scientific research on anxiety that both are true. Events and stress in our lives can
create more anxiety. For example, a passenger on a flight that barely escapes an serious accident
may feel anxiety the next time they take a flight, especially if this was one of their first flying
experiences. Flying may then become a new anxiety trigger. Conversely, someone that is already
vulnerable to having anxiety (see page 82 for more on this) may experience normal turbulence on a
flight as scary and then feel afraid to fly in the future.
Some people wonder if scary events caused their anxiety, or if their anxiety itself is what causes them to more readily see things as
scary.
What if I don’t know what triggers my anxiety?
For the sake of treatment, it is important to learn to identify what it is that makes you anxious. For some people it is very clear; for
others, anxiety seems to come from “out of nowhere.”
1.5

Each time he avoids the spider, his amygdala gets more feedback that the spider is dangerous. Next time he sees the spider, his
anxiety “alarm” will be louder, or it may go off more quickly than before. The process by which the brain learns that something
is more dangerous over time is called sensitization. It is also called reinforcement of the anxiety because the anxiety response
gets stronger and stronger. Reinforcement can happen both in the short term (when the danger seems to be present) or in the
long term, as we discuss below.
Short-term reinforcement: the anxiety “snowball effect”
Have you ever worried about speaking in front of a group of people? Worries about performing well can lead to jitteriness,
cracking voice, difficulty concentrating, and other “fight or flight” symptoms. Often the physical anxiety symptoms will then
create more worry about the performance; this creates a “snowball effect,” in which anxiety gets worse and worse, even to the
point of panic.
When we feel anxious, we typically want to do something to make ourselves feel better. Most of these
behaviors feel natural because our bodies also want to keep us safe. However, some of these behaviors
can make things worse; we add “fuel” to the anxiety “fire.” We can add fuel gradually over time or
dump lots on all at once. In all cases the anxiety “fire” gets bigger.
What behaviors are in danger of causing the anxiety to get worse? Anything that teaches the amygdala (the anxiety center of
the brain) that something is dangerous. Remember our spider example? Let’s say that every time this man sees a spider he tries
to avoid it by getting away. What does this teach him? That the spider is dangerous, of course!
“Danger!!”
=
Worry about speech
“Fight or flight” symptoms during speech
“People may see that I am nervous!”
(more worry)
1.6
Long-term reinforcement: “Safety Behaviors” and negative thoughts/beliefs
As mentioned earlier, anxiety “fuel” is anything that teaches the anxiety center of the brain, the amygdala, that
something is dangerous. Over the long term, the most common ways to do this involve negative thoughts and beliefs
as well as protective actions called safety behaviors. While these behaviors seem to help the anxiety right now, they
usually make it worse in the long run. Examples are listed below.
Thoughts
Negative thoughts about:
-the future
-yourself
-other people
-the world
Examples:
“I am going to lose my job and end up
homeless.”
“I must have control…”
“That person thinks I am an idiot.”
“If I drive on the highway I will get into an
accident.”
“If I keep having this thought it must be
true.”
Anxiety “Fuel,” continued
Behaviors
Safety behaviors are often justified using “as long as” statements:
Avoidance: “As long as I avoid that, I will be safe.”
Attacking others, acting on anger, etc.: “As long as I use verbal
or physical force to protect myself, I will have control.”
Protective behaviors: “As long as I have my water bottle with
me, I am safe and will not have another panic attack.”
Rituals (usually part of OCD, characterized by excessive,
repetitive checking, washing, counting, asking for reassurance,
etc.): “As long as I knock four times when I have a scary thought,
nothing bad will happen to my daughter.”
Substance use (trying to “numb” the anxiety): “As long as I can
have some alcohol, I will feel better.”
Fearful thoughts
Anxiety symptoms (“fight or flight” response)
Safety behaviors
Whether in the short run or over time, anxiety feelings, fearful thoughts, and protective, “safety” behaviors work
together to keep our anxiety “fire” burning. Each feeds off the others, and any one of these can act as the “match” to
get the fire started. In CBT, our goal is to work on these thoughts and behaviors to help extinguish the fire as
much as possible.
1.7
Exercise
Anxiety “Fuel”
Below, list some of the ways you may accidentally make your anxiety worse, based on the material discussed above.
Anxiety “Fuel” take home points:
Some of our thoughts and behaviors, while they seem to help us, actually make anxiety worse. Safety behaviors, such as
avoidance and protective behaviors, as well as negative thoughts, serve to reinforce anxiety in both the short- and long-term.
It is important to understand what, if any, safety behaviors we are using, so that we can work to reverse this through treatment.
Anxiety “Fuel,” continued
Avoidance
Do I avoid anything because it seems scary
or makes me feel anxious? This may
include avoiding thinking about something
or avoiding certain types of situations or
people.
Things I avoid:
1.
2.
3.
4.
5.
6.
7.
Anger and Irritability
Do I become angry or irritable and
attack others verbally or physically?
Times I become angry:
1.
2.
3.
4.
What I do when I am angry:
1.
2.
3.
4.
Protective “Safety” Behaviors
Do I try to protect myself in certain
situations in order to feel more safe?
How I try to protect myself:
1.
2.
3.
4.
5.
6.
7.
8.
Substance Use
Do I ever use drugs or alcohol in order to “numb” the
anxiety?
Types of drugs or alcohol:
When I tend to drink or use drugs:
Thoughts
Do I have thoughts that come up continually and make me feel
anxious?
Thoughts that make me feel anxious:
1.
2.
3.
4.
5.
6.
1.8

A common question: What if it really is dangerous?
Of course, we are not trying to ignore anxiety or feel calm if something really is dangerous. One of our goals in CBT is to
learn what is dangerous and what is not, what we can control and what we can’t, and how to balance taking risks
with keeping ourselves safe.
If you are here, it is likely that the cost of trying to keep yourself safe is outweighing the advantages. We’ll be exploring
this more in some of our other modules.
Anxiety Is…
We learned that the symptoms of anxiety are the
“fight or flight” response, and are normal,
functional, and necessary for survival. They
become a problem when they are too severe or
happen too much given the real amount of
danger present, or if it interferes with the
activities of life. While having chronic anxiety
over long periods of time puts stress on the
body, it can be helpful to remember that anxiety
itself is not dangerous; but it sure can be
uncomfortable.
Anxiety Triggers
Here we learned that the brain can learn to be afraid
of almost anything, and some anxiety “triggers” are
more common than others. Anxiety disorder
diagnoses are organized based on what triggers the
anxiety.
We know that anxiety can be caused by scary events,
and anxiety can also make one more likely to
experience an event as scary.
It is important to identify your anxiety “triggers.” In
most cases it is possible to figure them out yourself.
Sometimes it is necessary to have the help of a
mental health professional to do this. A few tips are
on page 10.
Why does my body do this?
In this section we covered the ways that each
“fight or flight” symptom functions to protect
us in case we are in real danger.
We also learned that when our body’s “fight or
flight” alarm is triggered, a domino effect of
chemical changes and messages are sent to
various parts of the brain and body, producing
these symptoms. This process is programmed
to last only about 10 minutes, unless it is
triggered again.
Anxiety Fuel
Some of our thoughts and behaviors, while they
seem to help us, actually make anxiety worse.
Safety behaviors, such as avoidance and
protective behaviors, as well as negative
thoughts, serve to reinforce anxiety in both the
short- and long-term.
It is important to understand how we make our
anxiety worse, so that we can work to reverse this
through treatment.
1.9



In this part of the group manual we will learn about exposure, one of the most
powerful weapons to battle anxiety and a big part of CBT treatment.
We spoke about sensitization in the section “Anxiety Fuel.” Now we’ll talk about
desensitization, which means we work to make our anxiety alarm less sensitive, so it
doesn’t go off as often or as loudly.
In this section we will learn what exposure is, when and how to use it, and some
important rules to follow to be sure we get the most out of treatment. We’ll also try to
give you lots of examples so it makes sense to you; we want you to know what to do,
but also how and why it works. In other words, we want you to be sold on exposure!
“Do one thing every day that scares you.”
~Eleanor Roosevelt
2.1

Have you ever been afraid of something and found that your fear became less intense over
time, the more you experienced something?
For example, some people can be afraid of flying and find that the more they fly, the easier it
gets.
This is how exposure works. Very simply, the more that we do something we are afraid of
doing, or are exposed to something that we are afraid of, the less afraid we tend to be.
Take home point:
Exposure and desensitization is just one set of skills used in CBT. It works best when we know what triggers our anxiety, and are
aware of avoidance and safety behaviors that we use when anxiety presents itself. The goal of exposure is to gradually expose
ourselves to whatever it is that we are avoiding, which helps us reduce the anxiety and make progress toward our life aims.
Exposure is one set of skills used in CBT. With exposure, we gradually begin doing some of the things we tend to avoid,
especially if these are things we need to do to reach our goals. The good news is that not only are we more likely to reach our goals
if we don’t avoid, but by doing the exposure exercises the anxiety can actually become less, so we feel better. When we feel better,
it is because the anxiety center of the brain, the amygdala, is getting less sensitive to a certain trigger. This is called
desensitization. We’ll talk more about how this works later.
When can I use exposure?
Exposure doesn’t work for all types of anxiety, and there are things we want to know before starting to use it. We hope that by the
end of this part of the group you’ll have an idea of when exposure can be helpful and how to use it.
To get a sense of when exposure may be helpful, ask yourself the following questions:
• Do I know exactly what is triggering my anxiety?
• Is there something important to me that I am avoiding because of the anxiety?
• Are there times when I try to stay safe or protect myself, which may affect my ability to live life the way I want to?
Be sure to review “Anxiety Triggers” if you have trouble determining what your triggers are. Sometimes it is helpful to get the
help of an experienced mental health professional to learn more about your triggers.
In the section of the group entitled “Anxiety Fuel” we learned about the ways that avoidance and safety behaviors can make the
anxiety worse. It may be helpful to review this section before beginning exposure exercises. As a rule of thumb, these behaviors
interfere with the improvement we might experience using exposure techniques. Later in this section we’ll be talking more about
how safety behaviors can get in the way of our progress with exposure.
Here are some examples of situations in which exposure principles can work:
A taxi driver has a fear of traveling over bridges. He avoids bridges at all costs and will even pull over
to the side of the road with a passenger in the car, pretending to have engine trouble. This fear of
bridges severely limits his ability to do his job. With the help of a therapist, he learns gradually to beat
his fear of bridges, starting by going over low bridges with a friend in the passenger seat. Eventually he
works up to driving over larger bridges on his own.
Bill, a college student, has a fear of public speaking. He tries to avoid taking classes that involve oral
presentations and when he does have one of these classes, he tries to avoid giving presentations by missing
class. He often fails to complete his work, and generally performs more poorly in these classes than he does
in classes that do not involve presentations. Bill seeks out treatment to address this and gradually learns to
speak in front of a few people, then small groups, and then ultimately larger audiences. With practice, he
becomes more comfortable speaking in front of others.
2.2

How avoiding public speaking impacts my
life:!
1. I worry about the next speech.!
2. I have to try to take classes that
don’t involve oral presentations.!
3. When I do speak in public, I feel
more anxious.!
4. I sometimes fail classes that involve
public speaking.!
5. I may limit the types of careers that
are possible for me.!
6. I may not be able to move up in my
profession if I avoid public
speaking.!
It is common to question whether or not to do exposure to reduce
anxiety and stop avoiding important things in our lives. Why?
Because facing our fears can be scary and takes hard work.
Before and during exposure we may need to remind ourselves of
why we are seeking treatment in the first place.
It can be helpful to consider how avoiding inconveniences us—
how it may keep us from achieving our goals. For example, Bill,
our friend with public speaking anxiety, could list the ways
avoidance impacts his life.
Writing down the ways avoidance impacts our lives can help us
understand how important it is to stop avoiding. We use
exposure to work on the avoiding itself.
Homework exercise: How can I use exposure?
Go back to the section “Anxiety Triggers” and list the triggers
you wrote under “My anxiety triggers are” here:
1.
2.
3.
4.
5.
6.
7.
Now use the following questions to determine for what triggers
exposure might work:
• Am I avoiding any of these triggers because of
anxiety?
• Are there times when I am exposed to these
triggers and I try to stay safe or protect
myself, which may affect my ability to live my
life the way I want to?
Now list some of the triggers for which the answers to these
questions are “yes:”
1.
2.
3.
4.
5.
6.
Homework exercise: Should I use
exposure?
Use Bill’s example above to write down the ways that
avoidance of some of these triggers either incon-
veniences you or keeps you from achieving your
goals.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
2.3

“This must not be
that dangerous…”
Give it time!
One trick about desensitization is that it usually takes time to retrain the amygdala to think
something is not dangerous, especially if it’s been trained over the years to think it is. As we will
discuss more later, one important thing about desensitization is staying in the anxiety
provoking situation long enough to learn it is not dangerous. Since our amygdala wants to
protect us, it needs a lot of convincing to be willing to turn down that anxiety alarm.
Take home point:
Through experience and over time we can make our brain less sensitive to certain anxiety triggers. This
is called desensitization.
You may remember from the “Anxiety Fuel” section of the manual that we can think and do things that make
the anxiety worse, like thinking over and over what might happen when we have to make that speech, or
avoiding speeches altogether.
Anxiety can also get worse when bad things really happen, or we perceive that some event is dangerous.
As we mentioned earlier, these events, safety behaviors and negative thoughts can make our anxiety alarm
more sensitive to certain triggers. This is called sensitization.
Desensitization is the opposite; our amygdala learns that something is not dangerous, through experience.
Take our spider example: if this guy continues to approach the spider, it teaches the amygdala that the spider is
not as dangerous as he once thought. If he is approaching that spider, it must not be that dangerous…
=
This is also called habituation, which means that we get used to something so that it no longer seems
as scary to us. We will even get bored, if we stay with it long enough. This is OK, because it is better
to be bored, than anxious!
The next time we are around the trigger, we may still feel some anxiety, but it is likely to be less. If we
do this over and over, the alarm gets weaker and weaker. Our anxiety “radar” may detect the trigger,
but our amygdala will not react to it like it did before.
=
less “anxiety alarm”
2.4

Desensitization, continued
Beware of Dog!
Elaine grew up around dogs all her life. Her family had many dogs, so she learned
through experience that dogs tend not to be dangerous. When she’d see something on the
news about a dog attacking a person, she’d think, “Wow, that seems odd,” because in her
experience dogs were not dangerous. This attack seemed like an isolated event and it did
not change her opinion of how dangerous dogs are.
Jessica did not have dogs in her home growing up. When she was six she saw a news clip
in which someone was attacked by a dog. She got the impression that dogs were
dangerous—each time she was around a dog, she remembered that news clip and began
to worry that the dog might attack her. She also felt scared and anxious when she saw a
dog in real life.
Jessica’s friend Rachel got a dog the next year. Jessica gradually learned through
experience that dogs weren’t always dangerous, and she began to feel less afraid.
“Oh, say can you see…”
Imagine that you were asked to sing the Star-Spangled Banner on opening day at
Comerica Park. Would you be nervous?
Now imagine you were asked to do this for every Tigers game– that’s about 80 home
games in a season. Would you be just as nervous after one month? At mid-season? At
the end of the season?
Wait just one second!
You may be thinking “I’ve exposed myself to this trigger over and over for a long time, and it
hasn’t gotten any better; in fact, it is worse! Why would exposure make this any better?”
There are some important rules about doing exposure that are necessary in order for it to work.
We’ll talk about these rules in the section entitled “The Exposure Formula.”
Exercise:
Try to think of some things to which you’ve become desensitized in your life. Examples are driving, scary movies, roller
coasters, air travel, etc. Think of things you’ve gotten good at with practice, and also maybe some fears you’ve overcome by
being exposed to them over and over and over. Then write them down here.
1.
2.
3.
4.
5.
2.5

Now that we know how desensitization works, we can get started. If you are still
questioning whether or not exposure will work for you, review the page “Should I do
exposure?” Remember that if there are currently avoidance or safety behaviors related
to a trigger, it is likely that exposure could be used to help bring the anxiety down.
Exposure exercise (different ways to trigger the anxiety)
-Speaking in front of a large group of professionals who are experts on the
topic on which I am speaking, using a prepared speech!
-Speaking in front of a large group of professionals who are experts on the
topic on which I am speaking, using a more impromptu style and few note cards!
-Speaking about myself in front of a few friends!
-Speaking for a few people who I don’t know and who don’t know my topic well!
-Speaking for about 10 people who are also students and don’t know my topic
well!
-Practicing a planned presentation on my own!
-Performing the speech for my girlfriend!
Anxiety Rating
9!
10!
6!
7!
8!
3!
5!
After listing the different
variations on the left, Bill rates
his anxiety on a scale of 0-10
using the “Subjective Units of
Distress Scale” (SUDS) for
each one. We discuss the SUDS
scale on the next page.
How do I know where to start?
If different anxiety triggers interfere with your life and you are not sure where to start with exposure, ask yourself the
following questions:
1. Which trigger interferes with my life the most?
2. With which one would I predict that my life would improve the most if the anxiety were less?
3. Does one stand out as being more “doable” than others? Would one be easier to start on, so I can start to get my life
back on track?
Based on the questions above, try to pick the most pertinent exposure target. Once you’ve chosen a trigger to start on, list
ways that you might be able to get your anxiety alarm going. For example, Bill might write down different types of situations
that would trigger his public speaking anxiety. We call this a Fear Hierarchy or a Stimuli Map.
When trying to come up with ways to vary the exposure, think about things that can change
how challenging the exposure is. Bill might list:
-Length of speech!
-How well I know the audience!
-How well they know the topic!
-How well practiced I am!
-Speech is more planned out versus more !
impromptu!
It is good to come up with a nice long list at first, so try to think of as many variations as
possible!
2.6

Exposure: Getting Started, continued
Exercise: “My Fear Hierarchy”
Pick a trigger and try designing some exposure exercises by listing possible ways to bring on the anxiety.
Exposure exercise (different ways to trigger the anxiety Anxiety Rating (0-10)
1. ___________________________________________________________________________________________________
2. ___________________________________________________________________________________________________
3. ___________________________________________________________________________________________________
4. ___________________________________________________________________________________________________
5. ___________________________________________________________________________________________________
6. ___________________________________________________________________________________________________
7. ___________________________________________________________________________________________________
8. ___________________________________________________________________________________________________
9. ___________________________________________________________________________________________________
10. __________________________________________________________________________________________________
11. __________________________________________________________________________________________________
12. __________________________________________________________________________________________________
The SUDS Scale
Exposure therapists often use a scale of 0-10 or 0-100 to rate the amount of anxiety someone has during exposure exercises. It
is like a thermometer, measuring how “hot” our anxiety gets.
This is called the Subjective Units of Distress Scale or “SUDS.”
0= no anxiety at all; completely calm
3= some anxiety, but manageable
5= getting tough; wouldn’t want to have it all the time
7-8= severe anxiety that interferes with daily life
10 = worst anxiety you’ve ever felt
Why do I have to rate my anxiety?
There are a few good reasons we ask folks to rate their anxiety before and during exposure treatment:
1. It helps us decide where to start and how to move from one exposure exercise to the next.
2. It keeps track of progress and helps us know if you are improving, staying the same, or getting worse.
3. It helps us start to step back from our anxiety when it happens and see that anxiety is not always the same
severity.
We will be talking about the SUDS scale often in this manual and you will be using it a lot during exposure therapy.
2.7
Take home points:
The first step in exposure practice is setting up a “Fear
Hierarchy” and rating the amount of anxiety you would feel for
each exercise.
Exposure practice requires repetitive, prolonged exposures to the
anxiety itself, with no “safety behaviors.”
There are four main ingredients in the “exposure formula:”
1. It is prolonged
2. It is repetitive
3. We focus on the anxiety
4. We add no safety behaviors
Exposure practice is like a formula; there are certain ingredients that are necessary to get the results we want. We need to
understand these before starting the exposure practice, because if we don’t follow these rules, we aren’t likely to make much
progress. In fact, we could make the anxiety worse! We’ll be talking more about this in the next section.
Ingredient #1: Prolonged
As we discussed earlier, it is important to stay in the anxiety producing situation until the anxiety comes
down. Sometimes people ask if it is possible to do a shorter exposure practice in order to make it easier to
complete. Usually we advise people to adjust the difficulty of the exposure, not the duration, because
staying the situation long enough is necessary for the anxiety to come down. In fact, one important element
of feeling better is staying in the situation long enough and doing it often enough that we eventually get
bored with the trigger. This is important, because being bored it is a surefire way to know that we are not
anxious!
Ingredient #2: Repetitive
Have you ever played a musical instrument or a sport? Your music teacher or coach probably told
you to “practice, practice, practice!” Repetition is important for our brain to learn anything, and
anxiety is no exception. Some people notice that their anxiety goes down quickly after starting
exposure, but most people find that it takes consistent, daily practice to adequately retrain the brain
and feel better.
Ingredient #3: Focus on the anxiety
This is the part that can be difficult; we are going to ask that you try to focus on the feelings (the anxiety “alarm”)
that come up when you are in the anxiety provoking situation. Why? Because we are trying to convince the
amygdala that this trigger is not really dangerous. If we avoid these unpleasant feelings, we send the message that
the trigger is dangerous, and our time spent practicing exposure is wasted.
Ingredient #4: No “Safety Behaviors”
The same could be true if we spend our exposure practice trying to stay safe or protect ourselves from the trigger,
or the anxiety itself. You may remember that safety behaviors are a great way to “fuel” our anxiety and make it
stronger; they also really sabotage our exposure practice! We discussed some examples of safety behaviors in the
section “Anxiety Fuel.” You may want to review this before starting exposure; it is another very important part of
doing exposure correctly.
Important!
The #1 factor in seeing
improvement with exposure
is whether or not you do
the exposure and use all of
the ingredients listed
above.
2.8

Exposure seems simple; just expose yourself to something you are afraid of, and the anxiety comes down
over time. While this is true, going through an exposure program sometimes seems anything but simple.
We should be ready to troubleshoot when things get tough– and sometimes it can be confusing! Below are
some tips to help you through the exposure and improve your results.
Tip #2: Follow the rules of exposure
As we emphasized on the last page, it is very important that all
of the “ingredients” of the exposure formula be included in
order to get good results. It is especially important that the
person doing the exposure stay in anxiety provoking situation
long enough for the anxiety to decrease. Review these
concepts on the previous page.
As we mentioned before, the #1 factor determining whether or
not someone does well with exposure is whether or not they
practiced exposure consistently and followed the rules.
Tip #3: Unify your cognitive and behavioral “forces”
Imagine an army going into battle tentatively, with only half
the number of soldiers, worried that there may be some
casualties. How do you think they would fair against the
enemy? Probably not so well.
Sending the message to the amygdala that the trigger is not
dangerous works best when our thoughts and behaviors
are aligned, a “unified front” against our enemy, the
anxiety.
If we have doubts about whether or not the anxiety
provoking trigger is really dangerous and then try to do
exposure, it’s like going into battle without all of our forces.
The anxiety is likely to win the battle, because our negative
thoughts continue to send the message that the trigger is
dangerous.
For example, when Bill goes to do exposure for his public
speaking anxiety, he reminds himself of the evidence he has
that making a mistake would not be the end of the world. We
discuss the methods to do this in the Cognitive Therapy
Skills module of this group manual.
Tip #1: Choose wisely!
Throughout exposure, try to pick exercises you are
confident you will complete. Often people become
frustrated with exposure because it is “too hard,” and they
may even leave the exposure practice early.
When first starting exposure, it is best to take something
from your Fear Hierarchy in the “5” or “6” range on the
SUDS and then very gradually increase the difficulty of the
exposures. If you are having trouble with an exercise, try
making it a bit easier and commit to becoming comfortable
with that particular trigger.
When designing exposure exercises, it is helpful to try to
make them convenient; in other words, make it hard to
forget to practice, and schedule it into the day so it does not
take a lot of extra work to get going. Give yourself every
chance you can to follow through with the exposure.
Tip #4: Be prepared for some discomfort
and stay aggressive!
Exposure can be difficult at times; after all, if we are going into
battle, we should expect the enemy resist us with everything it
has!
The main defense the anxiety has is discomfort, and we can
expect to feel some during the exposure. Usually the
discomfort is most severe early in the exposure, and some
people even find that the anxiety gets worse before it gets
better. This is our body trying to get us to give in and play
defense; but we know our best bet is to stay aggressive and not
listen to what the anxiety is telling us.
We are going to try to “ride” the anxiety wave, always
remembering that anxiety is uncomfortable, not dangerous!
2.9

Once we begin practicing exposure, it is important and helpful to track our progress. Remember
our Subjective Units of Distress Scale (SUDS)? We’ll use this to rate how much anxiety
comes up when we do an exercise. We rate our anxiety at the beginning, middle, and end of
each exercise. Let’s take our friend Bill’s public speaking exposure as an example.
Exposure task: Performing my presentation for friends !
Length of time SUDS (0-10)
Day/Date Start Stop Beginning Middle End Comments
4/15 10:15 am 11:15 am 2 8 4!
4/16 2:00 pm 3:00 pm 2 8 3!
4/17 5:30 pm 6:30 pm 1 9 4 Lost train of thought!
4/18 5:30 pm 6:30 pm 1 5 2!
4/19 10:00 am 11:00 am 0 4 1!
4/20 6:00 pm 7:00 pm 0 3 1!
4/21 10:15 am 11:15 am 0 2 .5!
This is the type of progress we would expect to see for someone that consistently practices this one exposure
exercise. You may notice that the “middle” levels are often highest, because it takes some time for the anxiety to
come down.
We can also do multiple “mini” exposures to things that are harder to do for a full hour straight. For example, Jane,
who has Obsessive Compulsive Disorder and fear of contamination, is practicing exposing herself to a rag that has
been in contact with a door handle one time every hour, all day long.
Exposure task: Touching rag that had contact with door handle !
SUDS (0-10)
Day/Date: 4/15 4/16 4/17 4/18 4/19 4/20 4/21!
8:00 am 8 8 7 5 3 4 3!
9:00 am 8 6 5 4 2 3 2 !
10:00 am 8 5 4 4 3 3 .5!
11:00 am 7 5 4 4 1 2 0!
12:00 pm 7 5 3 3 . 5 2 0!
1:00 pm 6 4 4 3 1 1 0!
2:00 pm 4 5 3 4 1 1 0!
3:00 pm 4 3 2 2 .5 2 0!
4:00 pm 4 3 1 1 0 .5 0!
5:00 pm 5 4 1 1 0 0 1!
6:00 pm 3 7 1 1 2 0 0!
7:00 pm 3 6 2 .5 0 0 0!
8:00 pm 3 5 1 1 0 0 0!
9:00 pm 4 5 1 1 0 0 0!
10:00 pm 4 5 1 2 1 1 0!
You may notice in both of these examples that there are times when the anxiety will come down, and then go up again.
At other times the anxiety starts high and comes consistently down. When we record our SUDS scores this way, we
can see that over time the numbers tend to come down, with some fluctuations in the middle.
2.10

Step Six: Ending exposure
Bill continues to practice the exposure for about 12
weeks, changing the exposure exercise about each
week as he moves up the hierarchy. After this, he
decides to continue to practice public speaking, but
less formally, to maintain his gains and refine his
skills.
External cue exposure is a fancy way to describe exposure to situations, places, objects, animals, or people
in our environment that make us feel anxious. This is also called in vivo exposure, which means exposure
“in real life.” Let’s take a look at Bill’s in vivo exposure for public speaking anxiety, one step at a time.
Step One: Pick a trigger
Bill has decided he really wants to beat this fear of
public speaking. He decides to focus on this target and
commits to designing an exposure plan to reach his
goal.
Step Four: Starting exposure
Bill picks an item from the list in the “5-6” range on the SUDS. He begins by speaking in front of his friends one hour each day
for one week. He tracks his progress using the SUDS (see Exposure: Tracking Your Progress). He also follows the rules of
exposure outlined in the section “The Exposure Formula.”
Step Three: Rate the hierarchy
Bill rates each item on his list using the SUDS scale (see
“Exposure: Getting Started” for more in-formation on the
SUDS).
Step Two: Create a fear hierarchy
Bill lists ways that he could purposely trigger the anxiety.
He thinks about different ways to make public speaking
situations more or less difficult.
Step Five: Middle sessions of exposure
Once Bill’s anxiety comes down to about a “3” or less
on the SUDS consistently for 3-4 days, he moves on to
the next highest item on his hierarchy. He goes to a
Toastmasters group where he practices in front of
people with whom he feels less comfortable. When he
again habituates to this exercise, he moves on to the
next.
Bill moves through his hierarchy until he feels
comfortable speaking in front of superiors who are
knowledgeable about his topic. Since it was hard to
find superiors to help him practice exposure, he had to
revise his hierarchy to create this fear as realistically
as possible. For instance, he practiced speaking about
current events at Toastmasters, because most people
could be considered “experts” on these topics.
For more information about Toastmasters, visit
www.toastmasters.org.
Exposure exercise (different ways to trigger the anxiety)
-Speaking in front of a large group of professionals who are
experts on the topic on which I am speaking, using a prepared
speech!
-Speaking in front of a large group of professionals who are
experts on the topic on which I am speaking, using a more
impromptu style and few notecards!
-Speaking about myself in front of a few friends!
-Speaking for a few people who I don’t know and who don’t know
my topic well!
-Speaking for about 10 people who are also students and don’t know
my topic well!
-Practicing a planned presentation on my own!
-Performing the speech for my girlfriend!
Exposure exercise
-Speaking in front of a large group of
professionals who are experts on the topic on
which I am speaking, using a prepared speech!
-Speaking in front of a large group of
professionals who are experts on the topic on
which I am speaking, using a more impromptu
style and few notecards!
-Speaking about myself in front of a few friends!
-Speaking for a few people who I don’t know
and who don’t know my topic well!
-Speaking for about 10 people who are also
students and don’t know my topic well!
-Practicing a planned presentation on my own!
-Performing the speech for my girlfriend!
Anxiety Rating
9!
10!
6!
7!
8!
3!
5!
2.11

Internal cue exposure means that the trigger for our anxiety is internal, or inside our bodies. This type of exposure
is used most often for people that struggle with Panic Disorder. Anyone who has had a panic attack knows how
uncomfortable it is; this is the “fight or flight” response at its worst! Often the “trigger” for panic attacks is body
symptoms and feelings. Remember what we discussed in the “Anxiety Fuel” section? Uncomfortable body feelings
can lead to worries about further anxiety symptoms, which then triggers more symptoms, which leads to more
worries, and before we know it we are in the middle of a full-fledged panic attack.
Because the trigger for panic attacks within the context of Panic Disorder is the body, the exposure exercises center
on the anxiety symptoms themselves. If we can become comfortable with the idea of having the anxiety symptoms,
we train the brain that the anxiety is not really dangerous, and the anxiety “alarm” doesn’t need to be sounded as
loudly or as often. These are also called interoceptive exposure exercises, which is a fancy way to say exposure to
feelings of anxiety and panic in the body.
Take a look at these interoceptive exposure exercises that can be used to toughen up against the possibility of having a panic
attack. The person would pick a symptom that they experience when they have panic and practice one exercise daily. Each person
may not respond to each exercise, so it is important try a number of them and find one that will trigger some anxiety.
Symptom: Rapid heartbeat
-Run on the spot or up and down stairs for 1 minute,
then 1 minute break. Do this sequence 8 times.
Symptom: Dizziness or lightheadedness
-Spin slowly in a swivel chair for 1 minute, then 1 minute
break. Do this sequence 8 times.
-Shake head from side-to-side for 30 seconds, then
30 second break. Do this 15 times.
-While sitting, bend over and place head between
legs for 30 seconds, then sit up quickly. Do this 15
times.
-Hyperventilate (shallow breathing at a rate of 100-
120 breaths per minute) for 1 minute, then normal
breathing for 1 minute. Do this 8 times.
Symptom: Breathlessness or smothering feelings
-Hold breath for 30 seconds, then breathe normally
for 30 seconds. Do this 15 times.
-Breathe through a narrow, small straw (plug nose if
necessary) for 2 minutes, then 1 minute breathe
normally. Do this 5 times.
-Sit with head covered by a heavy coat or blanket.
Symptom: Choking feelings, gag reflex
-Place a tongue depressor on the back of the tongue
(a few seconds or until inducing a gag reflex). Do
this repetitively for 15 minutes.
Symptom: Tightness in throat
-Wear a tie, turtleneck shirt, or scarf tightly around
the neck for 5 minutes, then take a one minute
break. Do this three times.
Symptom: Trembling or shaking
-Tense all the muscles in the body or hold a push-up
position for as long as possible for 60 seconds, then
rest 60 seconds. Repeat 8 times.
Symptom: Sweating
-Sit in a hot, stuffy room (or sauna, hot car, small room
with a space heater)
-Drink a hot drink
Symptom: Derealization (feeling that things are not
real)
-Stare at a light on the ceiling for 1 minute, then try
to read for 1 minute. Repeat 8 times.
-Stare at self in a mirror for three minutes, then one
minute break. Repeat three times.
-Stare at a small dot (the size of a dime) posted on
the wall for three minutes.
-Stare at an optical illusion (rotating spiral,
“psychedelic” rotating screen saver, etc.) for two
minutes, then break for one minute. Repeat five
times.
2.12

Exposure Examples: “Internal Cue Exposure,” continued
Step Six: Ending exposure
Janet continues to practice the exposure for about 10
weeks, changing the exposure exercise about each
week as she moves up the hierarchy. This, with a
combination of external cue exposure and cognitive
skills, improves her panic symptoms and makes her
feel confident that she can manage a panic attack in
the future.
Step One: Pick a trigger
Janet decides to start with the “dizziness” trigger,
because it most often triggers panicky thoughts that
fuel the anxiety and make it worse.
Step Four: Starting exposure
Janet picks an item from the list in the “5-6” range on the
SUDS. She begins by practicing hyperventilating for one
minute, then one minute rest, alternating 8 times, which
takes her about 15 minutes. She tracks her progress using
the SUDS by rating her level of anxiety before, during and
after the exposure. She follows the rules of exposure
outlined in the section “The Exposure Formula,” and
repeats this daily for one week.
Step Three: Rate the hierarchy
Janet rates each potential exercise using the SUDS scale (see
“Exposure, Getting Started,” for more information on the
SUDS).
Step Two: Create a fear hierarchy
Janet lists the different interoceptive exercises she can use
to trigger some anxiety, using a list she got from her
therapist.
Step Five: Middle sessions of exposure
Once Janet feels like her level of anxiety for the
hyperventilation exercise has come down to around a
“3” during the exercise, she moves on to the next
harder exercise on the hierarchy. She continues to
practice these exposure exercises daily.
She continues to move up on the hierarchy until she
becomes more used to the feeling of being lightheaded
and dizzy, as well as more at peace with the possibility
that she will have a panic attack when she feels dizzy.
Since she also becomes worried when she experiences
feelings of tightness in her throat, she decided to do
some of these interoceptive exercises, as well.
Along with her interoceptive exposure exercises, she
added external cue exposure exercises (see previous
page) to places that she avoided because she was
worried about having a panic attack.
Along with her exposure practice, Janet and her
therapist worked on some of the thoughts that tend to
“fuel” the anxiety once it is triggered. We will talk
more about these thoughts in the Cognitive Therapy
Skills module of the manual, in a section entitled “The
Only Thing We Have to Fear Is…”
Exposure exercise (different ways to trigger the anxiety)
-Spin in a swivel chair for 1 minute, then 1 minute !
break. Do this sequence 8 times.!
-Shake head from side to side for 30 seconds, then !
30 second break. Do this 15 times.!
-While sitting, bend over and place head between !
legs for 30 seconds, then sit up quickly. Do this 15 !
times.!
-Hyperventilate (shallow breathing at a rate of 100-!
120 breaths per minute) for 1 minute, then normal !
breathing for 1 minute. Do this 8 times.!
Exposure exercise
-Spin in a swivel chair for 1 minute, !
then 1 minute break. Do this sequence 8 !
times.!
-Shake head from side to side for 30 !
seconds, then 30 second break. Do this !
15 times.!
-While sitting, bend over and place head !
between legs for 30 seconds, then sit !
up quickly. Do this 15 times.!
-Hyperventilate (shallow breathing at a !
rate of 100-120 breaths per minute) for !
1 minute, then normal breathing for 1 !
minute. Do this 8 times.!
Anxiety Rating
7!
9!
7!
5!
Let’s see what a course of interoceptive exposure for panic would look like. Janet is a 24 year-old woman with Panic Disorder. She
has panic attacks that seem to come from “out of nowhere” and she often worries about having another panic attack. Sometimes
she feels a little anxious and she begins to feel dizzy, which then makes her worry the panic will get worse; in fact, it usually does.
2.13

How long do I need to keep doing exposure?
During each practice, do the exposure until the anxiety comes down by about half from where it
started. Remember to use the SUDS scale to help you rate your anxiety.
Stay in the exposure situation for the full amount that you planned. We usually start with one hour
as a rule of thumb. If it is boring, good! Stay with it– it is better to be bored than anxious!
What if it really is dangerous?
If something really is dangerous, we will never ask you to do it. Exposure only works when we are avoiding or protecting ourselves
around something that is not dangerous, or not so dangerous it is worth avoiding.
Sometimes we are not sure if something is really dangerous, and it can be helpful to find out. Social situations are an example. We may
think that trying to talk to people at a party is dangerous, because people may be critical of us. If we like the idea of going to the party
but are afraid, perhaps it is best to get a sense of really how dangerous it is. We can do this using two different techniques:
1. Cognitive skills: looking at evidence to give us a sense of how dangerous it is.
We’ll be talking about this more in the next section of the manual.
2. Behavioral experiments: let’s try it out and get evidence first hand about whether or not it
is dangerous. Ask yourself what the real consequences are of having something bad happen.
How do I know when to move on to the next exercise?
When your anxiety is consistently below about a “3” on the SUDS for a few days, it is a good time to move to the next item on your
hierarchy.
1. If you are still avoiding things related to the trigger in your daily life, it is best to continue to do the exposure.
2. It is best to really dominate the trigger you are working on before deciding to stop exposure. This means that you may even
ramp up the exposure to ridiculous proportions. For example, if you are afraid of dogs, you might spend a weekend dog
sitting for a friend; you could pet, rub, and play with the dog. A social phobic might volunteer to be the MC for a company
event. Once someone becomes comfortable with something that difficult, it is easier to feel OK being exposure to the things
we normally see in our daily lives. Structured, daily exposure practice often takes weeks or months to complete,
depending on the type of problem. It is best to work with a mental health professional or exposure therapy workbook to
determine how long to continue to do exposure therapy.
3. There will always be times when we feel challenged by anxiety and may have the urge to avoid. In this sense, we are never
“done” with exposure; it becomes a way to address anxiety over the long term in our daily lives.
How do I know if I am done with exposure?
Each person must decide when they want to stop doing exposure and move to using exposure principles in the course of daily life (see
“The Freedom of Choice”). However, there are some points that may help you make this decision.
My exposure questions
Write down questions you have about exposure here and be sure to ask the group leader before you finish all the group sessions.
1. ________________________________________________________________________________________________?
2. ________________________________________________________________________________________________?
3. ________________________________________________________________________________________________?
2.14

Obsessive-Compulsive Disorder (OCD) is a chronic and often debilitating condition that affects
thousands of people in the United States each year. OCD is characterized by obsessions (anxiety
provoking, often intrusive thoughts) and compulsions (behaviors that aim to neutralize anxiety).
These compulsions are also called rituals; they are “safety behaviors” that make the person feel less
anxiety in the moment but serve to strengthen the anxiety in the long run.
When most people think about OCD they think about anxiety around contamination that may make
someone want to wash their hands over and over. OCD has many forms, however; unfortunately we
can’t go into them in detail here.
Cognitive-Behavioral Therapy for OCD is called Exposure and Response Prevention (ERP). You now know
all about exposure; the “response prevention” part involves resisting the compulsions— we “prevent” or “block”
our impulse to give in and do the ritual. In this way, we really stand up to the OCD and don’t do what it tells us
to do.
For example, Jeremy tends to check things— irons, locks, stoves, the garage door– because
he feels anxious about the possibility that he has left something unlocked, plugged in,
turned on, etc. He will check locks over and over, and never feels reassured that the locks
are bolted, regardless of how many times he checks. He doubts himself constantly.
ERP for Jeremy involves purposely creating doubt that he locked something (exposure)
and resisting the urge to check (response prevention). He works to see the OCD as
something separate from himself: “It’s not me, it’s the OCD telling me to do that.” He
practices ERP for 60 minutes a day and works to eliminate all OCD rituals in his daily life.
ERP looks a lot like other types of exposure, in that we purposefully expose ourselves to the anxiety-provoking
trigger in order to show the brain that it is not really dangerous. But with OCD it is even more important not to add
any safety behaviors (rituals), because these rituals are ultimately what keep the anxiety fire fueled and burning
over the long run.
OCD is not rational!
Another thing that makes OCD different from other anxiety disorders is that the person that the anxiety producing trigger is not
rational and doesn’t make sense. Jeremy may try to reassure himself that the doors are locked and even see that they are locked, but
his brain continues to signal that anxiety alarm.
For this reason, it does not help to try to rationalize with the OCD. In fact, when we try this the anxiety actually gets worse.
Why? Because we are trying to reassure ourselves to get rid of the anxiety. What does this sound like? Yes, it is a safety behavior–
it tells the brain “In order to be sure that I locked the doors I must continue to reassure myself that it is true.” This is a great way to
“fuel” our anxiety!
I have OCD and want help; what should I do?
If you are planning to do exposure for OCD, it is best to work with
a mental health professional who is trained to administer Exposure
and Response Prevention. Here at the UM Anxiety Disorders Clinic
we have treatment groups and individual therapists that are well-
trained in delivering ERP for OCD. Ask us about how to get
involved in ERP.
There are also some self-help books and internet resources about
OCD that are helpful; these are listed in the section “Appendix II:
Cognitive-Behavioral Therapy Resources for Anxiety.”
Take home point:
Obsessive-Compulsive Disorder is slightly different
than other anxiety disorders. OCD treatment involves
Exposure and Response Prevention (ERP), which is
similar to other types of exposure, with some
modifications. If you have OCD and want to begin
ERP, it is best to receive guidance from a mental
health professional who is trained in ERP.
2.15

Exercise:
Think about and write down possible barriers to completing exposure therapy for one of your
most impairing anxiety triggers, using the information above as a guide.
1._______________________________________________________________________
2._______________________________________________________________________
3._______________________________________________________________________
4._______________________________________________________________________
5._______________________________________________________________________
Some people find exposure treatment to be difficult. There are some barriers along the way that make it
hard to follow through with treatment. It is important to understand these possible barriers and find ways
to work around them. If we do not, exposure therapy is not likely to help. Here are some of the common
problems people have with exposure treatment once they get started.
Take home point:
It is important to
understand possible
barriers to exposure
treatment and find
ways to work around
them.
1. “I don’t have enough time to do this much exposure homework.” It is true that exposure takes a commitment of
time and energy to work well. If we had evidence that exposure would work in less time, we would recommend to
shorten the exposures! But, as we mentioned earlier, repetitive, prolonged exposure practice is essential to success.
One question you may ask yourself is “How much time does the anxiety take from me each day? Each month? Each
year?” It could be that a commitment of time now could save you a lot of time in the future.
2. “These exposure exercises do not fit my lifestyle well.” An important aspects of exposure work is finding ways to
make exposure exercises convenient. Design them in ways that will increase the chances of doing them. This includes
finding ways to remind you to do the homework. Plan times to do the homework when you will not be bothered and
have all of the resources necessary to do it. For example, if someone were doing exposure to driving at night, they
would need to plan to do the exposure at times when they are sure they can get the car.
3. “I feel terrible when I am doing the exposure; I don’t want to experience this.” As we mentioned before, for
exposure to work we actually need to feel the anxiety during the practice session. When the anxiety gets worse it is a
good sign that exposure is working! We just need to stick it out to the end of the exposure. If you are hoping not to feel
any anxiety during the exposure, it may not be the right treatment for you.
4. “Sometimes I do ‘safety behaviors’ and I don’t even know I am doing them.” This is something that comes up
often in exposure treatment. As treatment progresses, our goal is to learn more and more how we may be “fueling” the
anxiety fire with safety behaviors. The more we are aware of them, the sooner we can extinguish these behaviors. A
therapist can be invaluable in identifying potential “covert” safety behaviors and rituals.
5. “I hate having this anxiety and I don’t want to have to keep doing this!” Especially once treatment has gained
some momentum, people often feel discouraged that they will need to continue to fight the anxiety over the long term.
We definitely can resonate with this complaint and would like the anxiety to go away forever! However, we know that
giving in to impulses to protect, avoid, and otherwise stay comfortable can make the anxiety even worse and keep us
from achieving our goals. Accepting that the anxiety exists is necessary before we can do something to manage it.
6. “This exposure isn’t working.” Before making a judgment about whether or not the exposure is working, be sure to
review “The Exposure Formula” to be sure you are following all of the rules. Exposure does not work if we just do it
“halfway.” It is important to follow these guidelines in order to see improvement!
2.16

Exercise
Design your own step-by-step plan to address anxiety in your daily life, using the example above:
Step One: _________________________________________________________
Step Two: _________________________________________________________
Step Three:_________________________________________________________
Take home point:
Either during or after a course of
exposure therapy, it is important to
have ways to handle anxiety triggers in
your daily life and use them over the
long term. We should expect to have
anxiety come up at times and be ready
to use skills when it does.
“Bring it on!
When addressing anxiety in the course of daily life, our attitude is the key. Try some of the following “self-statements” to help keep on track:
“Anxiety is uncomfortable, not dangerous.”
“Bring it on!”
“I won’t let anxiety make decisions for me anymore.”
“I want more anxiety– I hope it gets worse!”
“I can take it!”
“I hope that happens. If it does, it gives me a chance to fight this anxiety and learn to cope with hardships.”
“If bad things happen, I will find a way to cope.”
Remember to stay aggressive; the anxiety is waiting for us to become defensive and when we do this, it tries to take over. Staying aggressive with
anxiety in our daily lives helps to keep the anxiety from coming back in full force.
Have you ever felt like anxiety is making choices for you? In many ways, exposure practice
is about choices; the ability to choose what to do based on our goals and life aims, instead
of what is safest or least anxiety provoking.
In the course of daily life we have many choices, and some of the hardest occur when we
have to decide whether or not to “listen” to the anxiety alarm that tries to keep us safe. We
now know that making choices based on the anxiety can serve to make the anxiety stronger.
It makes sense to have a way to counter this when the anxiety comes up during the day,
using exposure techniques.
Step One: “That’s just my anxiety; I know it is not
dangerous.”
Step Two: “All right, anxiety, go ahead and stay around, I
am going to go about my business.”
Step Three: “Fine, it’s true that this plane is going to crash
(or whatever the fear is). I can’t control that.”
Once we have overcome a fear using exposure, we may
find that we do not experience any anxiety at all around
that certain trigger. This is good!
It is also possible that we may have times in which we
do feel some anxiety around a trigger that we think
we’ve conquered. We use the techniques below to
address anxiety when it seems to come back. When we
experience a trigger, we are going to welcome it with
the anxiety, and commit to fighting the impulse to avoid
or try to protect ourselves.
The first step involves recognizing that the anxiety is
separate from us, the brain trying to convince us to do
something that will hurt us in the long run.
Step two is an attempt to further accept the anxiety at that
moment and resist the urge to avoid or protect ourselves.
In the third step we “ramp up” the approach by doing a
“mini” exposure to the content of the fear.
Why would I start feeling anxiety again?
There are many reasons that someone might begin to feel anxiety
once again after using exposure successfully.
One reason is stress; we can’t predict when stressful things will
happen, and often stress leads to anxiety.
Another reason is that we may not have experienced that trigger for a
while, so our brains become less “bored” with it. Remember that
becoming “bored” with a trigger is important in reducing the anxiety.
2.17
In this part of the group manual we learned that exposure and desensitization is just one set of skills used in
CBT. It works best when we know what triggers our anxiety and we are currently avoiding those triggers or
using safety behaviors when we have to experience the trigger. The goal of exposure is to gradually expose
oneself to whatever it is that is being avoided, which helps one to meet his or her life goals and reduce the
anxiety.
We also learned ways to decide whether or not exposure is right for us by understanding the ways that anxiety
impacts our lives, and we learned about the principle of desensitization: through experience and over time we
can make our brain less sensitive to certain anxiety triggers.
In the “Getting Started” section we learned to begin exposure by creating a fear hierarchy and
using the SUDS scale (anxiety scale of 0-10) to rate the difficulty of each possible exposure
exercise.
In the section “The Exposure Formula” we learned that exposure practice involves repetitive,
prolonged exposures to the anxiety itself, with no “safety behaviors.”
We then offered tips to maximize the effectiveness of the exposure, and ways to “track” the
exposure progress using the Subjective Units of Distress Scale (SUDS) — we rate the anxiety
on a scale of 0-10 or 0-100.
We learned about some common barriers to exposure treatment and discussed why it is
important to understand these possible barriers to find ways to work around them.
In the section “The Freedom of Choice: Exposure in Daily Life” we discussed the importance of
learning to use exposure techniques when anxiety presents itself in the course of daily life.
This helps one manage anxiety over the long term. We learned that we should expect to have
anxiety come up at times and be ready to use skills when it does.
We then learned how a course of exposure looks in the sections titled “Exposure
Examples.” We looked at examples of addressing Panic Disorder using Internal Cue
Exposure and exposure to anxiety triggers in our environment (External Cue
Exposure).
We then discussed ways to use exposure to treat Obsessive-Compulsive Disorder using
a variation of exposure treatment, Exposure and Response Prevention (ERP).
Moving on…
The exposure skills we covered in this section can be used to help us wage our fight against the
“anxiety enemy.” Other skills, including cognitive (thinking) and relaxation skills are often used with
exposure to gain more ground on the anxiety. In the next two sections of this manual we will learn
about these other skills, which can be used either alone, or with the exposure skills.
2.18

List your anxiety trigger below and the list possible exposure exercises that might elicit anxiety. Use the SUDS scale to rate how
difficult it would be to experience the trigger.
Anxiety trigger_____________________________________________________ (for example, “fear of heights”)
Exposure exercise SUDS rating (0-10)
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
________________________________________________________________________________ _________________
Subjective Units of Distress Scale (SUDS)
0= no anxiety at all; completely calm
3= some anxiety, but manageable
5= getting tough; wouldn’t want to have it all the time
7-8= severe anxiety that interferes with daily life
10 = worst anxiety you’ve ever felt
2.19

Exposure Tracking Example
Exposure task: Performing my presentation for friends !
Length of time SUDS (0-100)
Day/Date Start Stop Beginning Middle End Comments
4/15 10:15 am 11:15 am 5 8 4!
4/16 2:00 pm 3:00 pm 3 8 3!
4/17 5:30 pm 6:30 pm 1 9 4 Lost train of thought!
4/18 5:30 pm 6:30 pm 1 5 2!
4/19 10:00 am 11:00 am 0 4 1!
4/20 6:00 pm 7:00 pm 0 3 1!
4/21 10:15 am 11:15 am 0 2 .5!
Subjective Units of Distress Scale (SUDS)
0= no anxiety at all; completely calm
3= some anxiety, but manageable
5= getting tough; wouldn’t want to
have it all the time
7-8= severe anxiety that interferes with
daily life
10 = worst anxiety you’ve ever felt
Length of time * SUDS (0-10)
Day/Date Start Stop Beginning Middle End Comments
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
Exposure task: _____________________________________________________
Amount of time each day and how often:________________________________
Safety behaviors or rituals to eliminate: ________________________________
___________________________________________________________________
Other guidelines:____________________________________________________
2.20

Record one SUDS (0-10) level in each box.
Date:____________________________________________________________________________________
8:00 am___________________________________________________________________________________________________
9:00 am___________________________________________________________________________________________________
10:00 am__________________________________________________________________________________________________
11:00 am__________________________________________________________________________________________________
12:00 pm__________________________________________________________________________________________________
1:00 pm___________________________________________________________________________________________________
2:00 pm___________________________________________________________________________________________________
3:00 pm___________________________________________________________________________________________________
4:00 pm___________________________________________________________________________________________________
5:00 pm___________________________________________________________________________________________________
6:00 pm___________________________________________________________________________________________________
7:00 pm___________________________________________________________________________________________________
8:00 pm___________________________________________________________________________________________________
9:00 pm___________________________________________________________________________________________________
10:00 pm__________________________________________________________________________________________________
Subjective Units of Distress Scale (SUDS)
0= no anxiety at all; completely calm
3= some anxiety, but manageable
5= getting tough; wouldn’t want to
have it all the time
7-8= severe anxiety that interferes with
daily life
10 = worst anxiety you’ve ever felt
Exposure task: _____________________________________________________
Amount of time for each exposure:_____________________________________
Safety behaviors or rituals to eliminate: ________________________________
__________________________________________________________________
Other guidelines:___________________________________________________
Exposure task: Touching rag that had contact with door handle
SUDS (0-10) ____________________
Day/Date 4/15 4/16 4/17 4/18 4/19 4/20 4/21
8:00 am 8 8 7 5 3 4 3
9:00 am 8 6 5 4 2 3 2
10:00 am 8 5 4 4 3 3 .5
11:00 am 7 5 4 4 1 2 0
12:00 pm 7 5 3 3 . 5 2 0
1:00 pm 6 4 4 3 1 1 0
2:00 pm 4 5 3 4 1 1 0
3:00 pm 4 3 2 2 .5 2 0
4:00 pm 4 3 1 1 0 5 0
5:00 pm 5 4 1 1 0 0 1
6:00 pm 3 7 1 1 2 0 0
7:00 pm 3 6 2 .5 0 0 0
8:00 pm 3 5 1 1 0 0 0
Exposure Tracking
Example
2.21



We will help you identify the thoughts that are troubling to you and
understand them as well as possible. We then discuss the basic
techniques that we use to begin to respond to and modify these
thoughts. We respond to thoughts by gathering facts, or “evidence,” to
see a situation as realistically and in as detailed a way as possible.
3.1
“The ancestor of every action is a thought.”
~Ralph Waldo Emerson
In this module, we explore our thoughts and explain how they are closely linked
to our emotions. We discuss how to identify, understand, and respond to our
thoughts as a way to help us feel better.
• “The fear of fear”—fear of the anxiety itself—which is commonly
associated with Panic Disorder. It is also a common part of all
anxiety disorders.
• Worry– often part of “Generalized Anxiety Disorder” but also a
common part of most anxiety problems.
Join us as we learn to change our relationship with our thoughts with Cognitive Therapy Skills!
Later in the module we go into some detail to discuss the thoughts associated with two common
types of anxiety:
You may remember from “Group Guideposts” that thoughts, behaviors, and
emotions influence one another.
Cognitive is a technical word used to describe anything related to thoughts. In
this module, we explore how it is that our thoughts can lead to negative emotions,
and what we can do about it.
Cognitive Therapy Skills involve responding to and modifying our thoughts—
to help us cope better in our daily lives and feel less anxious.
How do Cognitive Therapy Skills Work?
The main goal of cognitive skills is to gather evidence. Like a detective, we look to uncover facts about something that has happened
in the past or is happening right now.
For example, we know that driving on the highway has some risks associated with it.
However, for most of us driving on the highway is a necessary part of everyday life.
We are willing to take this risk because if we didn’t our lives would be limited. A
positive aspect of driving on the highway is that it helps us achieve our goals. A
negative one is that under some circumstances it can be dangerous. When we
examine the evidence, we find it’s true that there are “two sides to every coin.”
Examining the Evidence
Scientists and detectives are good at asking the right questions to better understand a situation. With cognitive skills we learn which
questions to ask to best explain an anxiety-producing situation. For example:
1. What is the likelihood that this anxiety-producing event will happen?
2. If this event were to happen, how bad would it be? Would it be tragic?
3. What would I do if something bad happened? How would I handle it?
4. Is there any other explanation to account for what has happened?
5. Do I know all of the facts about this situation?
Put on your “happy face?”
Cognitive Therapy Skills are not just about “thinking positively.” While being aware of positives is a part of CBT, we want to gather
all evidence, good and bad, to understand best how to cope with a situation.
Practice makes… the brain change?
When we modify thoughts, we actually change the brain! Practicing different types of thought
patterns over and over actually rewires our brain so that new, more realistic and helpful patterns
of thought can become more natural. This does not mean that our brains are permanently changed
by thinking something new just once. It takes consistent practice to keep the brain functioning
well, just like it takes consistent exercise to keep the body healthy. Cognitive skills can
help us keep our brains healthy, if we are willing to stay well-practiced at it.
Thoughts
(cognitions)
Behaviors
(actions)
By examining our thoughts, beliefs, and basic assumptions in detail, we can learn to make informed choices
about issues that impact us. For example, we may find that a thought is not completely true; this helps us
decrease our efforts to protect ourselves and lowers our anxiety. Another option is to take these facts and do
something with them– to problem solve. Finally, these facts may help us understand that nothing can be done
to change a situation; we work to accept this and let go of our efforts to control. In order to choose one of these
options we use cognitive skills to understand thoughts and situations as well as possible.
3.2

“What are Cognitive Therapy Skills,” continued
“Unifying our Cognitive and Behavioral
Forces”… revisited
In the section on Exposure and Desensitization, we
discussed the importance of “unifying our cognitive and
behavioral forces.”
Working with thoughts is just one part of our defense
against anxiety; simply learning to think differently can
be very helpful. However, we can’t underestimate the
importance of behavior in maintaining our anxiety. For
example, if we continue to avoid speaking in public, the
anxiety is very likely to be there when we actually do
go to make a speech, regardless of how we think.
Unifying our forces means learning to use cognitive
skills while practicing confronting our fears with action.
As we will state often in this group, effective anxiety
management means using lots of different “forces”—
CBT skills— to battle anxiety.
When should I use Cognitive Therapy Skills?
Cognitive skills can help us with most types of anxiety problems.
They work best when…
… we can identify negative thoughts that make us
feel worse in certain situations
…anxiety is triggered by worries about the future
and/or negative thoughts about ourselves
Let’s take our example of Bill, our friend from the Exposure and Desensitization module, who has a fear of public speaking. He
has many negative thoughts about speaking in public that come up when he starts to work on his speech. These thoughts cause him
to want to avoid anything connected with the speech: he may procrastinate and not prepare for the speech adequately or try to get
out of the speech completely. Do any of the thoughts below sound familiar to you?
“What if someone notices I am nervous?” “I am going to screw this up.”
“People will laugh at me.” “I am going to fail this class.”
“I may even have to drop out of school.” “I am not a good public speaker.”
Take home points:
Cognitive skills are one set of skills used in CBT. Our goal is to examine the evidence to uncover the facts, both positive and
negative, about a situation. By understanding a situation better, we learn to think realistically about the likelihood of bad things
happening; we also work to find ways to cope in case those things do happen.
In the “Anxiety Fuel” section of the manual we discussed the “snowball effect” that is created when negative
thoughts, avoidant or protective behaviors, and uncomfortable anxiety symptoms get mixed. Thoughts can serve to
make our anxiety worse and even cause more problems for us, especially if they convince us to avoid what makes us
anxious.
Important!
For patients that have Obsessive-Compulsive Disorder (OCD),
some types of cognitive skills may not be helpful. You may
remember from the Exposure and Desensitization module that
OCD is best treated with Exposure and Response Prevention, a
specific style of exposure treatment. If you have OCD it may be
best to work with an individual or group therapist to learn which
skills you can use to treat OCD. That being said, it could still be
useful to practice the skills in this module to learn to handle daily
stress and worry that may exist separate from the OCD.
Most of us can relate to Bill’s dilemma; when he has these thoughts it increases his anxiety and makes him want to avoid the
speech even more.
When we look at our thoughts realistically and in a detailed way, we “throw water on our anxiety fire.” Responding to and
modifying these negative thoughts so they are more realistic can help to keep us from triggering the anxiety over and over again.
Most importantly, they can help to keep us from avoiding things that are important to us. For example, if Bill avoids his class, it
could impact his grade, his program, and ultimately his career.
3.3

We all have them. Sometimes they pop into our heads uninvited. Sometimes they
stick in our heads for hours. Negative automatic thoughts are negative thoughts
that come automatically to us when we are feeling anxious, depressed, angry,
frustrated; they can come any time we have a negative emotion.
There are different types of negative automatic thoughts. Worry is related to fear
that something bad might happen in the future. Most troubles with anxiety have
some sort of worry attached. For example, the thought in the upper left corner of
this page is a worry about what might happen if this person loses his or her job.
“If I look nervous
they won’t like me.”
“If that happened I
would not be able to
tolerate it.”
Another type of negative automatic thought is a negative statement about ourselves, other people, or the
world at large. “I am an idiot” is a good example. It is not a worry, but rather a declarative statement; but
it sure can make us feel bad! Often people with depression have these types of thoughts. Cognitive skills
can work on these thoughts, too. In this manual, though, we’ll be focusing primarily on the anxiety-
related thoughts and worries.
“I am an idiot.”
Why do I have all of these negative thoughts?
You may remember from the “Anxiety Is…” section that the “fight or flight” response automatically
causes negative thoughts. You may ask “Why do I think so many negative thoughts when I am anxious?
When I am feeling relaxed I don’t have these thoughts much at all.” As we discussed earlier, there are good
reasons we experience negative thoughts when we are anxious.
When we are anxious, the brain wants us to think about potentially dangerous things in our environment, in
order to keep us safe. We want our anxiety radar to be sensitive if there is actual danger out there.
Imagine what would happen if we did not have negative thoughts when we were in danger… we probably
wouldn’t try to protect ourselves! If we really are in danger, it is helpful to have negative thoughts because
we are more likely to try to stay safe if we think something is dangerous. The trouble is, sometimes we
know that things are not dangerous, yet we have these thoughts anyway. That is why we use cognitive
skills to help our brains get on board with what we know– that right now, we are safe.
“Chicken and Egg” revisited…
On page 10 we discussed the “chicken and the egg” phenomenon—anxiety can make a situation seem
more dangerous, while a dangerous situation can also trigger anxiety. The same thing holds true for
thoughts: negative automatic thoughts certainly can cause anxiety, while when we are anxious we are
more likely to have these negative thoughts.
Anxiety Negative Automatic Thoughts
“I might lose
my job and my
home.”
“One day I am just
going to ‘snap.’”
“If I have a panic
attack it could lead to
a heart attack!”
“If am not anxious I
may be more at risk
for something bad to
happen.”
3.4

Negative Automatic Thoughts, continued
Types of Negative Automatic Thoughts
Anxiety causes people to assume the worst. There are many different types of anxiety producing thoughts, and it is helpful to be
aware of some of the kinds of thoughts that many people with anxiety experience.
1. Overestimating the likelihood of negative events happening: One of the most common tendencies when we are anxious is
to predict that dangerous things will happen in the future. We often imagine that something may happen, even when logically
we know that it is not likely to happen. For example, Bill may predict that “everyone will think I am stupid if I make one
mistake during my presentation.”
2. Catastrophizing: This is a fancy way of saying that we predict things would be “horrible” or “awful” if something bad
actually were to happen. We may predict that we would not be able to cope, and we may try to find ways to prevent it from
happening to avoid catastrophe.
3. Beliefs that anxiety itself is dangerous: We often have negative thoughts about the anxiety itself. We may predict that we
will “go crazy,” “lose control,” not be able to function, have a heart attack, pass out, or suffocate when anxiety symptoms get
more extreme.
4. Belief that one cannot tolerate discomfort, pain, or negative events: We question our ability to cope with future events
because of the anxiety: “If I can’t tolerate this, what will happen if something really bad happens?” We tell ourselves “I cannot
take this” when we experience discomfort and/or pain.
5. Positive beliefs about worry: Anxiety and worry often seem to have a protective function. We may say to ourselves “If I
don’t worry about this it may actually happen.” Sometimes anxiety helps us get things done that we might otherwise avoid; we
rely on it for motivation, even if it is uncomfortable at the same time.
6. Negative thoughts about ourselves, others, the world: We make negative assumptions and blanket statements such as “I
am a loser,” “Nobody will ever like me,” or “The world is a dangerous place.” These types of statements can make us feel more
anxious, and more depressed, as well.
We all have some patterns of negative thinking, depending on our experience; but sometimes these patterns can get out of control.
When these patterns are severe, an anxiety disorder may be at work. Each anxiety disorder has characteristic negative automatic
thoughts associated with it. Here are some examples of negative automatic thoughts related to each disorder:
Diagnosis
Generalized Anxiety Disorder (GAD)
Social Anxiety Disorder
Panic Disorder with Agoraphobia
Specific Phobias
Obsessive-Compulsive Disorder (OCD)
Post-Traumatic Stress Disorder (PTSD)
Thoughts
“I am going to lose my job. I may even end up homeless if that
happens.”
“People don’t like me.”
“People may notice my anxiety and think I am weak.”
“I will have another panic attack.”
“This time I could have a heart attack.”
“The plane could crash… I will worry about this for the whole flight.”
“If I do not count to four each time I feel anxious, something bad could
happen to my husband.”
“The world is a dangerous place; there is nothing I can do to keep
myself safe.”
“A stronger person would have gotten over this by now”
3.5

The first step to begin “restructuring” or responding to negative thoughts is to
identify the thoughts that give us trouble. It’s as if we are putting a magnifying
glass to our minds to learn more about how we think. Use the following tips to
identify the thoughts you’ll start working on using cognitive skills. Once you have
identified a thought, write these thoughts down using the Daily Thought Record
Worksheet.
Exercise:
Use the techniques on this page to begin to identify some of your negative automatic
thoughts. Use the Daily Thought Record and the Thought Cascade Worksheet to
record them for later.
Take home points:
The first step of cognitive “restructuring” is to identify negative automatic thoughts
and record them in the form of the statement. There are many techniques that can be
used to do this, such as writing down thoughts in the course of daily life, visualizing
anxiety-provoking situations, and using the Thought Cascade method.
How to Identify Negative Automatic Thoughts
1. In the course of daily life, write down thoughts that come up when you are
feeling anxious.
2. Sit quietly and try to imagine going into an anxiety producing situation: what
thoughts come up?
3. Recall an event from the past that was anxiety-producing. What thoughts
were going through your mind?
4. Role play an anxiety-producing event with a friend, family member, or
therapist. Write down thoughts that come up during this exercise.
One Thing Leads to Another:
The “Thought Cascade”
When we are feeling anxious, it is
common to have a thought that leads
to a more disturbing thought, which
then leads to an even more disturbing
thought, and so on, like this:
“I am going to lose my job.”
“I won’t be able to pay my bills.”
“I will lose my house and end up
homeless.”
“I will die homeless and penniless”
Believe it or not, this “domino effect”
of negative automatic thoughts is
common. We can use this technique to
uncover some of our most
troublesome worries.
When Identifying Thoughts…
…phrase the thoughts in the form of a statement, and avoid “what if’s” and questions.
For example, if the thought is “What if I lose my job?” it would be better to phrase it “I
will lose my job.”
…be specific about the fear. It is better to break more general thoughts up into more
manageable pieces. If the thought is “I feel like something bad is going to happen,”
make a list of the specific things that you worry might happen. Write down the first
negative automatic thoughts that come into your head. You might use the “Thought
Cascade” approach, to the left, to learn more about what is scary to you.
…notice the thoughts that seem to come up often or are more impairing than others.
You may want to begin with these when you start working on the thoughts.
3.6

Example
“I am going to lose my job.”
“I won’t be able to pay my
bills.”
“I will lose my house and
end up homeless.”
“I will die homeless and
penniless”
When we are feeling anxious, it is common to have a thought that leads to a more disturbing thought, which then leads to an
even more disturbing thought, and so on. Believe it or not, this type of “domino effect” of negative automatic thoughts is
common. We can use this technique to uncover some of our most troublesome worries. Once you find some that are particularly
difficult or relevant for you, you can use the Examining Thoughts Worksheet to begin working on them.
To use this technique, first write down a thought in the form of a statement, as in the example below. Then ask yourself: “What
would be so bad about that?” In other words, what other bad things might happen should the event happen?
Your thoughts
__________________________________
__________________________________
__________________________________
__________________________________
__________________________________
__________________________________
__________________________________
__________________________________
What would be so bad if that
happened?
What other bad things might
happen if this happens?
What would be so bad if that
happened?
Your Thoughts
______________________________
______________________________
______________________________
______________________________
______________________________
______________________________
______________________________
______________________________
Your Thoughts
______________________________
______________________________
______________________________
______________________________
______________________________
______________________________
______________________________
______________________________
Your Thoughts
______________________________
______________________________
______________________________
______________________________
______________________________
______________________________
______________________________
______________________________
3.7

Try using these tricks to identify negative automatic thoughts:
• Sit quietly and try to imagine going into an anxiety producing situation: what types of thoughts might come up?
• Recall an event from the past that was anxiety-producing. What thoughts were going through your mind?
• Role play an anxiety-producing event with a friend, family member, or therapist. Write down thoughts that come up during
this exercise.
• In the course of daily life, write down thoughts that come up when you are feeling anxious.
Date___________Situation___________________________________________Thought____________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
Write down thoughts that you uncover using techniques on the last few pages. Remember to phrase the thoughts as
statements.
3.8

Why is it important to understand
cognitive distortions?
Understanding cognitive distortions is an important part of
understanding our thoughts and preparing to work on them
using cognitive therapy skills. By understanding some
common faulty patterns of thinking, it is easier for us to
notice our own patterns during the course of our daily lives.
The more we notice these patterns, the more likely we are to
be able to modify these thoughts and start feeling better.
What do I do when my negative
automatic thoughts do not seem to be
distorted?
Sometimes anxiety producing thoughts are not completely
distorted. In fact, there is some truth to almost all of our
thoughts. The worry “I am going to lose my job” may have
some truth: it is always possible that one could lose their
job. If one has determined that it is, in fact, likely that they
will lose their job, we would say that this thought is not
distorted. However, at this point we would want to use the
Thought Cascade approach to get to some related
thoughts, such as “If I lose my job I will end up homeless
and destitute.” We would then want to look at possible
distortions in that thought, and so on. As we will discuss
more later, our main goal is to learn how likely it is that
something bad will happen, while also learning how to
cope when bad things do happen to us, so whether or not a
thought is distorted, we still have work to do!
So, for the purpose of these exercises, record the possible
distortion for each thought, even if you are convinced that
the thought is not distorted.
Have you ever seen one of those “fun-house” mirrors? While we know how we really look, what we see
in the mirror looks different than what is real.
When we are anxious, the facts of a situation can become distorted, too. Cognitive distortions are
patterns of thinking that are heavily influenced by our emotions. As you will see when you review the
list of cognitive distortions, these distortions tend to follow certain patterns, and many of them overlap
with others. Here are some “fun facts” about cognitive distortions:
1. Cognitive distortions tend to be extreme: there is often a “black-and-white” or “all-or-
nothing” quality to these thoughts.
2. They tend to emphasize negatives at the expense of positives. As we mentioned earlier, we are
programmed to think of negatives first when we feel anxious, because our bodies are trying
to protect us.
3. They tend to be general instead of specific.
In the Exposure and Desensitization module we used the example of Jessica, our young friend with a
fear of dogs. After she saw a news story about someone being bitten by a dog, she became afraid that
she might get bitten herself. Some of her negative automatic thoughts might have been “All dogs are
dangerous” or “I am going to get bitten by a dog if I get too close to one.” While it is true that dogs can
occasionally be dangerous, there are qualities of these thoughts that are not true. We may call them
“distorted” because of the extreme nature of the thoughts: “all” dogs are not dangerous and most dogs
do not, in fact, bite the people with whom they come into contact.
So here they are! Read through the list of
cognitive distortions on the next page, and
circle the numbers of those that you suspect
may apply to you.
3.9

1. Black-and-White Thinking: We see things, events, and people as perfect or terrible, all
good or all bad. We say “always” or “never” often, not seeing the “grey zone” that is
almost always there.
2. Catastrophizing: We react to a disappointment or failure as though it means the end of
the world.
3. Jumping to Conclusions: We assume the worst without checking the evidence. We
decide that someone dislikes us, but we don't check it out; or we predict that terrible
things will happen even when there is no evidence for this.
4. Ignoring the Positive: We don't pay attention to positive experiences, or we reject
them or say they somehow "don't count.”
5. “My Fault!”: We take blame or responsibility for things outside of our control, or are
not our job.
6. “Shoulds:” We criticize ourselves or other people with ideas about what absolutely
“should” be done without considering where we get this idea. We ignore the reasons
we might have done what we did, or think we could have had knowledge we couldn’t
have actually had. “Shoulds” sometimes leave us feeling inadequate despite our
attempts to be self-motivating.
7. Magnifying and Minimizing: We define ourselves by our shortcomings and minimize
our strengths.
8. Labels: Instead of focusing on peoples’ behaviors, we make blanket statements: “I am
such an idiot” or “He’s such a jerk.”
9. Perfectionism: We believe that all mistakes are bad and to be avoided. Because of this,
we don’t take the necessary risks to be successful. We may also try to control all
circumstances and make them fit what we think is right.
10. Reasoning From Our Emotions: We believe that because we feel a certain way, that
indicates the truth about a situation, and we may even act accordingly even if it hurts
us in the long run.
3.10

Exercise
Write down some of the thoughts you identified earlier. Identify potential distortions related to each thought.
____________________Thought _____________________________________________________Distortion_________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
Take home points:
When we are anxious, it is possible that our thoughts are “distorted” in some way.
Cognitive distortions are thoughts that are heavily influenced by emotions and
may not be consistent with the facts of a situation. An important part of cognitive
skills is identifying ways that thoughts may be distorted and noticing patterns in
our thinking. As we become more aware of these patterns, we are better able to
modify anxiety-producing thoughts.
3.11

Examining the Evidence
“Restructuring” Negative Automatic Thoughts
Imagine you are a scientist studying the causes of pollution in a local river. How would you approach this?
What types of questions would you ask to uncover the truth? You might look at local industry, plant
populations, or invasive species as potential causes. You might look closely at samples of the water to
determine what types of pollutants are in the water. You’d want to get as much information as you could to be
sure you were right about what you find.
Cognitive Restructuring: Basic Questions
When working on our anxiety-related negative automatic thoughts, we look at different lines of evidence for each problem, to get
closer to the truth about that situation. We call the answer to these questions the rational response. We typically start with two basic
lines of evidence when addressing anxiety-producing thoughts:
Scientists know that there are many possible explanations for an event or phenomenon. They spend countless hours trying to prove or
disprove their hypotheses about what is happening and why it happens. To do this, they set up experiments; ultimately the goal is to
find the best possible explanation for something. They might ask questions like: “What are all the possible explanations for this
event? Are there any other possibilities?”
Now imagine this scenario: you are walking down the street or hallway and you see someone you know fairly well. You look at them
to say hello and they look away and say nothing in return. What types of interpretations might you have about this event? Perhaps you
might think “They must not like me-- if they did they would have said hello to me,” or “They must be mad at me.”
What if we replaced these knee-jerk reactions with a more scientific approach? We could look for other explanations, just like the
scientist. What are some other explanations to why this person did not look at you and say hello? List some here:
1._________________________________________________________________________________________________________
2._________________________________________________________________________________________________________
3._________________________________________________________________________________________________________
What you just did is a simple example of examining the evidence, the most important element of cognitive restructuring, a
common cognitive therapy skill. “Restructuring” a thought means gathering evidence to see a situation more completely and
realistically, which can help us feel better.
2. If it did happen, how bad would it be? Would I be able
to cope? What would I do if this happened?
We also know that, when we are anxious, we tend to catastrophize.
This simply means that we tend to blow out of proportion how bad
something would be if it did happen. We often predict that we
would not be able to handle a negative event if it occurred. We also
don’t think much about what we would actually do if this event
happened. For example, most people, if faced with the challenge of
losing their job, would eventually get back out and start looking for
another job. Often we do not think this far ahead; we stop after the
thought about how bad it would be for something to happen and we
focus on preventing that thing from happening.
To look at this question, we might ask ourselves how bad it would
really be if this happened. What would we do if the event
happened? How we might be able to cope with it and move on? If it
did happen, what would be the worst consequence? By looking at
this basic question in a more detailed way, we may find that we
could cope if this unfortunate event actually did happen.
1. How likely is it that this event will happen?
Research has shown that when people are anxious they
typically overestimate the likelihood that something bad
will happen. For example, we may worry about the
possibility of losing our job because the economy
weakens, without knowing the details of how it
specifically impacts our company. We may predict that we
are on the flight that will crash into the ocean. To get some
more details about the likelihood of something bad
happening, we ask questions like:
• What percentage likelihood is it that this event will
happen? Am I 100% sure? 50% sure?
• What evidence do I have that this is likely to
happen in the future?
• Is there any evidence that it is not likely?
• How many times have I predicted this would
happen? How many times has it actually happened?
Our goal here is not to try to prove that this event will not
happen; instead we try to make a realistic assessment of
how likely something is.
3.12

This style of negative thought features predictions. You may remember from the page on Cognitive Distortions that this is also
called “Fortune Telling.” When it comes to anxiety, we will find it is better to get all the information before betting that something
will happen. We look at different lines of evidence to get to the key question:
“How likely is it that this negative event will happen?”
Remember, we are looking at any evidence, not just evidence disputing our fear. Some lines of evidence are:
Are you a gambler? Think of the last time you made a bet with someone. How
much did you bet? How confident did you have to feel in order to make that
bet? 100% sure? 50% sure? You may know that people that bet on horse races
often look at the odds a certain horse has to win before placing their bet. People
like to know how likely it is that they will win, or lose, money before making
their decision.
We don’t often use the same system to gauge the chances of a negative event
happening in our lives. Research has shown that when people are anxious they
typically overestimate the likelihood that something bad will happen. It would
be like betting all our money that the underdog horse is going to win, because
we are feeling lucky that day.
Exercise
Think of a fear you have about the future. Use the techniques on earlier pages to identify a thought that is particularly difficult. For
now, focus on predictions, thoughts like “I will lose my job” or “She will reject me.” Write it on the left. Remember to phrase it in the
form of a statement. On the right, write the answers to the questions listed above.
Thought (prediction) Answers to questions above (rational response)
• What percentage likelihood is it that this event will happen? Am I 100% sure? 50% sure?
• What evidence do I have that this is likely to happen in the future?
• Is there any evidence that it is not likely?
• How much money would I bet that this will happen?
• How many times have I predicted this would happen? How many times has it actually
happened?
When you are finished, you should have a good idea of the likelihood that this event will happen. Sometimes we realize that this event
really is not likely, and we determine that it is not worth the effort trying to protect ourselves or fix the problem. Then we can remind
ourselves of this evidence when we get that thought.
Of course, sometimes bad things actually do happen. If it really is likely that something bad could happen, we go to the next
important question: “If something bad did happen, how bad would it be?” We discuss this on the next page. Remember that the
purpose of the material above is to make a realistic assessment of how likely something is. This is one important part of examining
the evidence.
3.13

Imagine that someone called you on the phone and said “Come home quick-- something horrible has
happened!” What types of events would you think may have happened? List a few possibilities here:
1. ________________________________________________________________________________
2. ________________________________________________________________________________
3. ________________________________________________________________________________
Most people would define “horrible” events as “catastrophic” or “life changing.” Think about some of
the thoughts and worries you identified on earlier pages. How do they compare with the events listed
above?
What if horrible
things really have
happened, or could
happen, to me?
Of course, sometimes horrible
things do happen, and when they do,
it is likely we will experience some
anxiety about these events. In fact,
we all should expect that we will be
confronted with very difficult
circumstances at some point in our
lives; after all, there is no way to
prevent bad things from happening
forever!
When horrible things happen, we
have to find ways to grieve our
losses and learn to cope so that we
can eventually move on with our
lives. An important part of CBT is
learning to cope better when bad
things really do happen.
The “Catastro-meter”
Have you ever had the thought, “I know it is not likely that it will happen, but if it did, it
would be terrible.” It can be helpful to look more closely at a potentially difficult event
to determine how bad the event would be, and how we would cope if that event did
happen.
Let’s use the “catastro-meter” to rate different types of challenging events to measure
how catastrophic these events would be if they happened. Rate each of these events on a
scale of 0-10 in terms of how hard it would be to cope with the event:
0= would have no trouble coping at all
3=would have a few bad days as a result, but recover pretty quickly
5=would take substantial time to recover, but no doubt it would happen
7-8=would be impaired for a while
10=would fall apart, go crazy, never recover
_____Argument with friend or loved one
_____Death of a loved one
_____Get injured in a car accident
_____Loss of job
_____Heard someone said something mean about you
_____Home gets flooded
_____ ________________________________(insert your own here)
_____ ________________________________(insert your own here)
One goal of this exercise is to notice the difference between different types of negative
events. We can learn that not all bad events have the same degree of severity.
We know from research that when people are anxious, they tend to catastrophize: they blow out of proportion how bad something
would be if it happened. Because of this, a big part of cognitive restructuring is getting more evidence to answer the question:
“How bad would it be if this event did happen?”
3.14

Catastrophizing (continued)
Exercise
Think of a prediction about the future that leads to anxiety. Do the exercise on page 48 to determine if it is likely that it will happen. If
you determine that it is likely it will happen, or you worry that it would still be horrible if it did happen, write the thought on the left,
below. Remember to phrase it in the form of a statement. On the right, write the answers to the questions (lines of evidence) listed
here.
• If this happened, would it be horrible?
• What are the likely consequences of this happening?
• If it did happen, would I be able to cope?
• If it did happen, what would I do?
• Would I always be affected by this, or would I eventually get over it?
Thought (prediction) Answers to questions above (rational response)
Another common tendency we have when we are anxious is to underestimate our ability to cope with
difficult events. We may think that we will not be able to handle the emotions associated with a
challenging event. Think back to some difficult events you have had in the past. How did you handle
them? How long did it take to get over them? Pick a few events and do the following exercise to get
some evidence about your ability to cope with tough circumstances.
Past tough event What I did to cope How long it took to overcome this and move on
Were you able to cope? Have you moved on from these events, or are you still mired in their consequences? If you were able to cope,
this may give you some good evidence that you are better at coping than you thought you were. If you feel you were not able to cope,
a part of the work you do in therapy could be to work on developing some coping skills to better handle future negative events. Many
of the techniques we learn in Cognitive-Behavioral Therapy can be helpful to learn to cope with difficult events.
Based on your written examples on the last two pages, do the following exercise, gathering evidence about how bad the predicted
event would be, as well as whether or not you could find a way to cope with it. Remember, we are trying to look at the situations
realistically, so there should be both positive and negative evidence.
3.15

Possible
Distortion Thought Rational Response
She didn’t say much of a
hello. She must hate me.!
I have no friends. No one
likes me.!
I’ll never find a wife. I’ll
always be alone.!
She must think I’m an
idiot.!
If she says no it will be
awful!!!
Jumping to
conclusions!
Black-and-white
thinking!
Jumping to
conclusions!
Labels!
Magnification!
It is possible he was thinking about
other things and does not hate me. In
fact he did ask me to lunch last week…
etc.!
Not true! Jim is my friend. John and Joe
talk to me a lot, they seem to like me. I !
could join the company team and make
more friends,
etc.
!
Wait! I am not alone now; I have some !
friends. I would like more dates; maybe
I could join a dating service,
etc.
!
True, she may say no but she may say
yes. I will miss out for sure if I do not
try,
etc.
!
Sure, it would hurt but probably not
forever. If I practice getting rejected it
may help me worry less about it,
etc.!
Take thoughts identified using
techniques in the “Identifying
Negative Automatic Thoughts”
section and write them here.
Use what you learned from the
section “Cognitive Distortions” to
identify any possible thought
distortions.
Gather evidence for and against your negative
automatic thoughts using multiple lines of
evidence.
Over the last three pages, we discussed the two main questions we ask when trying to learn more about an anxiety provoking
situation. Once we know which questions to ask, we must start to record our evidence to build a strong, realistic argument. When
we are beginning to use cognitive restructuring, it is helpful to write down our thoughts, distortions, and evidence until we get the
hang of it. Here is one method we use to do this is.
You will notice in the example below that this approach uses the skills
of identifying thoughts and thought distortions that we practiced on
previous pages. We add the “rational response” in the third column.
The evidence we gather there is what we will use to remind ourselves
of the truth about the situation when we are feeling anxious.
Get out that pen and paper!
Research shows that people who write things down
as part of CBT practice do better than those that try
to do it all in their heads. While it does involve more
work (and may seem like going back to school), we
hope you will give it a try at first, until the skills
become more natural.
Important: Gather lots of evidence!
You may have noticed the “etc.” after each rational response in the examples above. What
we are trying to communicate is the importance of gathering as much detailed evidence as
possible. For each negative automatic thought, we may have as many as 7 to 10 facts listed.
We use multiple lines of evidence to do this. Each “line of evidence” aims to help us
illuminate a certain aspect of a situation. For example, one common line of evidence is one’s
own personal experience, examined in detail. Another might be the perspective of friends and
family.
On the following pages we look at specific types of anxiety, such as panic, and the lines of
evidence we can use to help us gather evidence about these issues. Use the Examining
Thoughts Worksheet on the next page to record the evidence you gather.
3.16

Possible
Distortion(s) Thought Rational Responses
Take thoughts identified using
techniques in the “Identifying
Negative Automatic Thoughts”
section and write them here.
Use what you learned in the
“Cognitive Distortions” section to
identify any possible thought
patterns.
Gather evidence for and against
your negative automatic thoughts
using multiple “lines of evidence.”
Tips:
-Remember to phrase each thought in the form of a statement.
-You should have between 7 and 10 facts in the “rational response” column for each thought.
-Copy this page to use for other thoughts (some extra pages are included at the end of the manual).
-Carry it with you and bring it out each time you have the thought, to remind yourself of the facts.
Thought
Possible
Distortion(s) Rational Responses
1.
2.
3.
4.
5.
6.
7.
8.
9.
1.
2.
3.
4.
5.
6.
7.
8.
9.
3.17

Have you ever heard of the speech President Franklin Roosevelt made in 1933 about the economy? In
the midst of one of the most difficult periods in the nation’s history, he said: “The only thing we have
to fear is fear itself.” Sometimes our reaction to negative events is fearful, which ends up causing more
problems. For example, when the stock market crashes as it did in 1929 and 2008, people become
afraid they will lose more and pull their money out of the stock market and banks. This, in turn, causes
even more trouble for the economy.
Similarly, our own fearful reactions to our body’s “fight or flight” response, its attempt to try
to keep us safe, can make our anxiety much worse. In this case, the “fear of fear” is really the
“fear of anxiety.” This means that we:
• Are afraid of having anxiety symptoms
• Believe the anxiety symptoms will be intolerable and/or last forever
• Worry that others will notice our anxiety symptoms
• Try to get rid of, push away, or distract from the anxiety
Earlier we discussed how anxiety can be triggered by something in the world or in our minds.
Once the anxiety related to a trigger becomes severe, we begin to fear the anxiety symptoms
themselves. We may try to avoid anything that makes us feel anxious, or try to protect
ourselves against the anxiety.
“I hate this anxiety!”
Have you ever tried to stop
feeling anxious? How does it
work? We may think that
getting angry and frustrated
about the anxiety may somehow
get it to go away. But what is
your experience? Does it go
away?
Typically when we try to push
anxiety away, it comes back
even stronger, just like
scratching an itch repetitively
leads to the itch getting redder,
itchier, and more swollen.
Perhaps we could take a
different approach: instead of
pushing thoughts away, we
learn to restructure them when
they come up to make them less
scary. This way, we don’t have
to spend so much energy
pushing the thoughts away, and
we can feel better in case they
do come. Learning not to
avoid unpleasant thoughts is
an important part of CBT.
We also have negative thoughts about the anxiety itself. In the section entitled “Anxiety
Fuel” we learned that our thoughts can make anxiety worse. These thoughts often sound like
this:
• “If that happens I will have anxiety; I won’t be able to tolerate that.”
• “This anxiety will never end.”
• “If I have anxiety or a panic attack, I could have a heart attack, faint,
suffocate, go crazy, or even die.”
As we discussed before, these thoughts can create a “snowball effect” of thoughts and anxiety
symptoms acting on one another, so our brain really thinks we are in danger! In CBT, we learn
to step in and restructure these thoughts so they cannot continue to make our anxiety worse.
On the next page we learn ways to fight the “fear of fear” by learning to talk back to each of these anxiety fueling thoughts. On the
following pages we outline some effective lines of evidence to use when battling these troubling thoughts.
3.18

The only thing we have to fear is… (con.)
Just count to ten!
Has anyone ever told you to “count to ten” when you have a strong emotion, to let yourself calm down a bit? Have you ever tried it?
For some of us, it seems hard to believe that just giving yourself the count of ten could help us feel better. After all, sometimes it
really feels like the anxiety will never end!
The truth is, our bodies are not programmed to allow anxiety to last forever. In fact, once the anxiety response is triggered, it is
programmed to last only around 10 minutes. That’s right! So why does it seem to go on and on?
As we discussed in the “Anxiety Fuel” section, the main reason this anxiety stays around is that the “fight or flight” response
continues to get triggered again and again. Repetitive negative thoughts are one way this “snowball effect” happens. However, if we
do not retrigger the anxiety by thinking about it over and over or trying hard to protect ourselves, the anxiety response is programmed
to turn off. So the truth is, anxiety will not last forever, if we give it a chance to shut down. This is why even just “counting to ten”
can be helpful. We can practice this technique of “emotion regulation” by reminding ourselves to “ride out” the anxiety without
acting on it or trying to fix it, to give it a chance to come down on its own.
As important as this is, it does not mean our only job is to learn to “ride out” panic and anxiety. Over the long run we can work to
reprogram our thoughts using cognitive therapy skills so the anxiety gets triggered—and retriggered—much less.
“If that happens I will have anxiety; I won’t be able to
tolerate that feeling.”
Line of evidence #1: Past experience
• How many days have I experienced anxiety in your
life?
• Of those days, how many times did I think “I can’t
tolerate this?”
• How did it work out? Did I get through it?
• How many times did I not get through it? What did
I do?
• What is more important, how I feel, or how I respond to
adversity?
• Was it intolerable, or was it really uncomfortable? Is
there a difference?
Line of evidence #2: The future with or without anxiety
• What would it be like not to have this anxiety?
• Do I think it is worth it to work on minimizing the
anxiety, using whatever methods necessary?
• Am I willing to do this for the future, even if it means
feeling some discomfort now?
• Is it really best to be completely anxiety free? Is this
realistic?
Line of evidence #3: Likelihood of experiencing some pain in the future
• Is it likely that I will experience some pain in the
future? Is it possible to prevent pain completely?
• Is it best to try to avoid pain and discomfort completely,
or to learn to cope with pain and discomfort in order to
make it less unbearable?
Of course, anxiety is uncomfortable, and we don’t want you to have to experience it. Sometimes, however, negative thoughts about
the anxiety and the avoidance that comes with them can serve to make our anxiety much worse. Let’s look at a few common thoughts
that often fuel this “fear of fear.” Here we clearly define the thought that gives us trouble and look at different “lines of evidence” we
might use to better understand the anxiety.
“This anxiety will never end.”
Line of evidence #1: Personal experience
• I can think back to an event in
which I felt anxious. How long did
it last?
• Did the severity of the feelings
change during the episode at all?
• If and when the event ended, how
did I feel?
Line of evidence #2: Our body is programmed to
“turn off” the “fight or flight” response after
about 10 minutes
• Review the evidence from the “Just
count to ten” section, below.
3.19

The only thing we have to fear is… (con.)
“What about this panic?!”
Sometimes our “fear of fear” can reach panic proportions; our heart races, we get dizzy and lightheaded, there is pressure in the
chest and the feeling of choking, racing thoughts, and a sense of dread and doom. Because these symptoms are so intense, it is
understandable that one might worry that they could get worse. There are typically four “catastrophic” predictions that we make
when feeling panic. Let’s look at them more closely, one at a time.
Could I have a heart attack during
a panic attack?
This is one of the most common thoughts
people have during panic attacks; it is a
thought that could land you in an emergency
room, only to be told “you are fine” when the
medical tests come back. While many predict
that they may have a heart attack during a
panic attack, we have no evidence that there
is any connection between panic attacks and
heart attacks. Senior clinicians in our clinic
and others like it around the country nearly
always report that they have never seen a
heart attack that was caused by panic. This
means that in thousands of patients, with
possibly millions of panic attacks, there are
few to no reports of panic attacks leading to
heart attacks. This means the chance of a
heart attack occurring during your next panic
attack is very, very small. Do you think it
might be helpful to remind yourself of this
the next time you feel some panic?
“Is this a heart attack, or panic?”
Symptoms of a heart attack and panic are very similar. Common symptoms of a heart attack are uncomfortable pressure, fullness,
squeezing or pain in the center of the chest lasting more than a few minutes, and mild to intense pain spreading to the shoulders,
neck or arms. It may feel like pressure, tightness, burning, or heavy weight. It may be located in the chest, upper abdomen, neck,
jaw, or inside the arms or shoulders. Chest discomfort with lightheadedness, fainting, sweating, nausea or shortness of breath is
also common, along with anxiety, nervousness and/or cold, sweaty skin, increased or irregular heart rate and a feeling of
impending doom. Sound familiar? Many of these symptoms are the same as those listed in the “Anxiety Is…” section on page 7.
One thing that separates panic from heart attacks is that panic attacks tend to improve with movement and exercise, while heart
attack symptoms get worse under those conditions. Also, panic tends to reach its peak within 10 minutes and then predictably
decline gradually over time. A heart attack will not get better over time. Of course it is important to be aware of potential physical
problems, especially if there is a history of heart disease. But given the fact that the symptoms are so similar, we must go with our
best bet, given our family history of heart disease, age, and knowledge about our heart health. The best way to solve this dilemma
is to get treatment for panic; if panic is not a problem, we’ll have a better idea of whether or not we are in danger of having a heart
attack.
Common panic thought #1: “I will have a heart attack.”
Line of evidence #1: Personal history
It is easy to understand why it feels like we are having a heart attack during a
panic attack, especially because the heart beats strong and hard, there is often
tightness in the chest, as well as feelings of dread and doom. Let’s look at this
prediction in more detail, in order to at least get a sense of the likelihood of
having a heart attack when we feel panicky.
• How many panic attacks have I had in the past?
• How many of these panic attacks were accompanied by
predictions that I could have a heart attack?
• How many heart attacks connected with panic attacks have I
had?
• Have I been a good predictor of heart attacks in the past?
• Have I gotten any medical tests to assess my current risk of
having a heart attack? What have the doctors told me?
• Given my history with panic attacks versus my history with
heart trouble, is it more likely this is a panic attack, or a heart
attack?
Line of evidence #2: Clinic history/research
• See “Can I have a heart attack during a panic attack?” to the
right.
Line of evidence #3: Difference between heart attacks and panic attacks
• Are there any differences between heart attacks and panic
attacks and how they feel? (See “Is it a heart attack, or panic,”
below)
3.20

The only thing we have to fear is… (con.)
“I can’t get enough air!”
During a panic attack, the feeling of smothering and tightness in the chest often leads to the worry that one will not
get enough oxygen and suffocate. What we find, however, is that when one is panicking, they are actually getting too
much oxygen by breathing very quickly. This “over-oxygenation” is hyperventilation, which makes one feel dizzy
and lightheaded. Suffocation occurs when the body does not get enough oxygen. It is highly unlikely that panic will
lead to suffocation.
Common panic thought #2: “I will suffocate.”
Line of evidence #1: Personal history
• How many panic attacks have I had in the past?
• How many of these panic attacks were accompanied by predictions
that I would suffocate?
• Have I ever suffocated due to a panic attack?
• Have I been a good predictor of suffocation in the past?
Line of evidence #2: Possibility of suffocating when having panic
• See “I can’t get enough air!” below.
Common panic thought #3: “I will faint.”
Line of evidence #1: Personal history
• How many times have I fainted in the past? Have I been
evaluated to determine if I have a medical problem that
might lead to fainting?
• How many panic attacks have I had that were associated
with fainting spells in which I actually passed out and lost
consciousness?
• If I did pass out, how bad would it be? Would I be able to
cope in the unlikely event that I did pass out? Would it be
a catastrophe?
Line of evidence #2: Compatibility between panic attacks and fainting
• See “Fainting, panic, and blood pressure” to the right.
Fainting, panic, and blood pressure
The idea that we might faint during a panic
attack is common, because anxiety causes
dizziness, lightheadedness, tunnel vision, and
other strange sensations that make us feel like
we are going to faint. That being said, it is
very rare for a person to pass out during an
anxiety attack. This is because during panic
attacks and periods of high anxiety blood
pressure is elevated; when we pass out, it is
due to a drop in blood pressure.
Some people have a type of anxiety called
blood/injury/illness phobia, in which
passing out is common. If you think you
might have this condition, or if you have
passed out multiple times in the past, discuss
this with your doctor or therapist; there are
ways to deal with this tricky combination of
anxiety and fainting.
If you do not have a predisposition to
fainting, it is highly unlikely that you will
pass out during a panic attack. During a
panic attack you might remind yourself that it
will feel like you will pass out, but it is most
likely that you will simply continue to feel
dizzy and lightheaded until the panic
subsides.
3.21

The only thing we have to fear is… (con.)
Common panic thought #5: “This panic will hurt me in the long run.”
Line of evidence #1: Pros and cons: aggressive treatment versus avoiding panic
• What will happen if I continue to avoid the sensations of panic? Will the panic get better?
• If the panic does not get better by avoiding, is it possible that continuing to take this approach could hurt
me even more in the long run?
• Is it better to avoid in order to feel safe now, or to accept that it will be uncomfortable now so I can feel
better in the long run?
• See “long term effects of anxiety,” below.
Common panic thought #4: “I could go crazy!”
Line of evidence #1: Personal history
• How many panic attacks have I had in the past?
• How many of these panic attacks were accompanied by predictions that I would “go crazy” or “lose it?”
• Have I ever “gone crazy” or “lost it” due to a panic attack?
• Have I been a good predictor of “going crazy” in the past?
Line of evidence #2: Define “going crazy” and “losing it.”
• What does this mean? Am I worried about having “crazy” thoughts or feelings? Am I worried about doing
something “crazy?”
• Is there something specific I am worried I might do (e.g. hurt myself or someone else, make a scene, etc.)? If
so, what are the chances I would actually do this?
• What can I do when I am feeling panicky to prevent any erratic and/or harmful behaviors?
Line of evidence #3: Clinic history
• What is my clinician’s experience with this? How many of this clinician’s patients have “gone crazy” or
“lost it” as a result of panic attacks?
Line of evidence #4: Relationship between panic and psychosis or schizophrenia
• See “Could I ‘lose it?’” below.
Could I “lose it?”
Often folks with extreme anxiety and panic worry that eventually they will “lose it,” and lose touch with reality or do something
extreme. “Losing it” is often equated with “going crazy” or becoming psychotic, which means that a person loses touch with
reality. So is it possible? Based on current research, there is no evidence that anxiety and panic are directly causative of disorders
that include psychosis, such as schizophrenia and bipolar disorder. If you do not have a history of one of these illnesses, panic is
not likely to lead you there. We can remind ourselves, “This feels very uncomfortable, but I am not going crazy; this is my body’s
attempt to protect me.”
If you are worried about doing something harmful or have a history of erratic behavior during panic attacks, it may be helpful to
talk to a therapist about ways to cope with these difficult feelings so we can keep ourselves and others safe.
Long term effects of anxiety
It is true that chronic, uncontrolled anxiety causes stress on our bodies, which can make us more susceptible to illness and
chronic health conditions.
One way to view this dilemma is to assess how well our methods of treating the anxiety have worked; if they have not worked, is
it likely that they will work in the future? If not, we could be increasing the lifespan of the anxiety, which could cause even more
stress in the long run. Addressing the anxiety through treatment, while it may cause some stress in the short term, may reduce
stress in the long term. It is common to find that “short term pain” can offer us “long term gain.”
3.22

• A common type of anxiety has to do with “fear of fear,” which is fear of the
anxiety symptoms themselves.
• While this type of anxiety is a defining feature of Panic Disorder, it is also
common in other types of anxiety.
Exercise*
1. If you have not done so already, use the techniques in the “Identifying Negative Automatic Thoughts” section to identify
thoughts about the anxiety itself that may fuel your anxiety.
2. Use the “lines of evidence” to examine the evidence about your anxiety.
3. Use the “Examining Thoughts Worksheet” to write down the thoughts, possible cognitive distortions, and evidence you find.
4. Remind yourself of this evidence in the morning before you start your day. When you experience anxiety during the course of
the day, remember to “ride out” the anxiety without reacting to it; use the “Examining Thoughts Worksheet” to remind yourself of
the evidence. Remember, it takes repetition to retrain the brain!
• It is common to feel frustrated when we feel anxious. Our attempts to rid ourselves of the anxiety may not
work, which causes more anxiety and frustration.
• Often our thoughts about anxiety are negative and make the problem worse. Common thoughts related to
anxiety include worries that panic will cause a heart attack, suffocation, fainting, going crazy, or long-
term harm to the body.
• In the short term, it is helpful to learn to “ride out” episodes of anxiety so that we do not “fuel” the anxiety.
We remind ourselves that anxiety is “uncomfortable, but not dangerous,” and that episodes of anxiety are
meant to last only about 10 minutes, if we do not trigger it again.
• In the longer term, we use cognitive skills to address these thoughts, using lines of evidence such as
personal history and pros and cons to treat these thoughts when they come up in the course of daily life.
Important!
Restructuring thoughts related to our “fear of fear” is just one part of our overall treatment. It may also be helpful to
use these skills to address other types of thoughts, such as everyday worries and/or negative thoughts about social
situations. We may also need to use behavioral skills such as exposure or relaxation skills. Most people find that a
combination of methods and skills works best in managing anxiety over the long term.
*If you suffer from Panic Disorder, talk to your treatment group leader or individual therapist about starting a
structured CBT treatment. This treatment will combine these cognitive skills with exposure skills, among other things.
Experimenting with these skills now may have some benefit, but a structured treatment is typically necessary to treat a
full-blown case of Panic Disorder successfully.
3.23

When we are worried, people want to reassure us— “Don’t worry…” they say. Of course, just “not
worrying” is much more easily said than done! Trying to control worry can be challenging and frustrating.
Generalized Anxiety Disorder (GAD) is the technical term for the condition in which we experience
uncontrollable worry. One fearful thought is replaced by another. After awhile, it may seem that we worry
about just about everything.
These two types of worry, uncomfortable feelings, and our
responses to the worry create a “snowball effect” of anxiety
that makes us feel worse and worse over time:
Type II Worry
(Worry about the worry and anxiety itself)
Examples:
• “I will never stop worrying.”
• “I can’t tolerate this anxiety.”
• “I must find a way to stop worrying.”
• “If I keep worrying like this I will eventually go crazy.”
• “Maybe this worry will overcome me and I’ll be trapped
inside of it forever.”
• “I am causing harm to my mind and body by
worrying all the time.”
• “I hate the way this anxiety feels.”
Type I Worry
(Worry about bad things happening to us or people we care
about)
Examples:
• “I am going to lose my job.”
• “My children will get sick or be hurt.”
• “I am not going to pass this test.”
• “Our country could be attacked by a terrorist.”
• “I am going to end up homeless on the street.”
Repetitive, automatic negative thoughts (worry) about the future is the hallmark characteristic of Generalized Anxiety Disorder. The
“triggers” of anxiety are the thoughts themselves. Because thoughts are such a big part of GAD, cognitive skills are a primary
component of treatment for this problem.
There are two basic types of worries common in GAD. One type is worry about bad things happening to us or the people close to us.
According to anxiety researchers, this is called “Type I” worry. “Type II” worry is worry about the worrying itself, which is almost
always a part of GAD, and resembles the “fear of the fear” we discussed earlier. In order to treat GAD effectively, it is best to
address both types of worries. Observe the examples below to clarify these important aspects of GAD.
Type I Worry:
“I will lose my job.”
Type II Worry:
“I hate this worrying.”
Physical anxiety symptoms:
Muscle tension, irritability,
feeling “on edge,” trouble with
sleep, low energy, etc.
Sensitizing Behaviors:
Protective efforts to avoid
worrying or “fix” the worry
(anxiety “fuel”)
Related Type I Worry:
“I will lose my house and
my wife will leave me.”
3.24

Cognitive Skills for Daily Worry and Generalized Anxiety (con.)
Generalized Anxiety Disorder Example #1:
“I am going to lose my job.”
Step #1: Identify the potential cognitive distortions: Examples may be: “Magnification” or
“Jumping to Conclusions”
Step #2: Examine the evidence:
Line of evidence #1 (likelihood): Right now, are there reasons to believe that I will lose my job?
• Firstly, what has happened to make me believe I may lose my job? Have there been rumors going around?
Have I heard anything about my job being in jeopardy?
• Have I gotten any feedback from supervisors about my performance? Positive? Negative? Have there been
performance evaluations? How did I do?
• How likely is it that I will lose my job? 100% likely? 50% likely? (assign a percentage to your chances)
Line of evidence #2 (likelihood): My past job performance
• Have I ever gotten fired from a job before?
If so, is there any direct evidence that I got fired because of my job performance? Are there any
other factors that may have contributed to this? What were the circumstances at the time? Do they at
all differ from the circumstances now?
If not, how does this fit with the idea that I am likely to get fired now? Are the circumstances now
the same or different?
• Have I ever worried about getting fired because of my job performance before? What has happened? Have
I been a good predictor of getting fired in the past?
• Have I gotten feedback from supervisors in the past assessing my job performance? What were the results?
Line of evidence #3: If it is likely that I will lose my job, how bad would that be?
• If this happened, what would I do? Would I give up? Would I continue to look for jobs?
• Are there other possibilities?
• Is it likely that the people closest to me would be frustrated with me and disrespect me, or are they likely to be
supportive?
• When other people lose their job, what do you think of them? Do you tend to feel critical of them, or
do you chalk this up to misfortune or some other factor?
• If there are things I could improve in order to reduce the likelihood of losing a job in the future, what
would they be?
• What have I done in the past when I was faced with adversity? Did I find a way to cope? How did things
turn out?
Step #3: Write down the evidence gathered on a copy of the Examining Thoughts Worksheet, or list the evidence on a note
card. Carry this with you and take it out when this thought occurs in your daily life. Remind yourself of the facts of the situation
and then continue with your day.
Step #4: Use the “Thought Cascade” approach to uncover other thoughts related to this thought, especially if you determine
that it is likely that you will lose your job. Ask “If I did lose my job, what would be bad about that? What would be the
consequence?” Use the same techniques to examine the evidence around the other thoughts.
Step #5: Use problem solving techniques to determine if the situation can be improved.
Step #6: Use acceptance skills to let go of effort to fix things you cannot change.
Below we give some examples of negative automatic thoughts common with Generalized Anxiety Disorder and outline ways to
begin to restructure these thoughts, using some of the techniques we learned earlier in this module, such as “defining terms,” using
the Thought Cascade approach, and examining the evidence. Use the Examining Thoughts worksheet to record some of the facts
you gather from the “lines of evidence” below.
3.25

Cognitive Skills for Daily Worry and Generalized Anxiety (con.)
Generalized Anxiety Disorder Example #2:
“What if something bad happens to one of my children?”
Step #1: Phrase the thought in the form of a statement and define “something
bad happens.”
• Specify: “My child will get hurt” or “He will be made fun of at school,” etc.
Step #2: Identify the potential cognitive distortions:
• Examples may be: fortune telling, magnification.
Step #3: Examine the evidence:
Line of evidence #1 (likelihood): How likely is it that this will happen to my child?
• Has something like this happened to my child in the past?
• Have I heard of this happening to children in the past? How common is this? Are there statistics available
on how likely this is?
• Have I predicted that this would happen before? What did I think about my prediction later? Did it seem
just as urgent? How good a predictor am I of this happening?
Line of evidence #2: If this did happen, how might we cope with it?
• If this happened, what would I do?
• Have we dealt with difficult circumstances in the past? How did I cope then? If something really bad
happened, did we eventually recover, at least partially, and continue to live our lives? What could we do to cope?
• Are others resilient enough to cope with a difficult event like this and continue to live their lives?
Line of evidence #3: Pros and cons: Protection versus allowing children to live life fully
• Look at the pros and cons of keeping a child protected from all danger. List these on a piece of paper.
• Look at the pros and cons of allowing a child to live a life without so much protection. List these.
• Consider the following questions:
1. Is it possible that trying to protect against all danger could leave a child less able to cope with the
normal risks we all have to accept in our daily lives?
2. Could allowing children to live with some risk make them stronger and more able to flourish?
3. Is here any way to protect against all possible dangers?
4. Does this worry help me protect against these things?
5. How does my worry affect my children? Does it help them to feel safe and secure?
6. Are there things I can do to keep my child adequately protected while also helping them feel confident,
competent, and able to cope with adversity?
Step #4: Write down the evidence gathered on a copy of the Examining Thoughts Worksheet, or list the evidence on a note
card. Carry this with you and take it out when this thought occurs in your daily life. Remind yourself of the facts of the situation
and then continue with your day.
Step #5: Use problem solving techniques to determine if things can be done to improve safety. Be aware of efforts to
overprotect in ways that way interfere with your child’s life.
• Try to find a balance of “protection” with “living life” that works for you. Determine which precautions
make sense and which achieve little in the way of protection, and instead interfere with your child’s ability
to develop and flourish.
Step #6: Write down results of this examination on a note card and carry it with you. When you feel worried or the
need to try to take some precaution, review what makes the most sense for the long-term benefit of your
child.
Step #7: Use acceptance skills to let go of effort to fix things you cannot change.
3.26
Cognitive Skills for Daily Worry and Generalized Anxiety (con.)
Generalized Anxiety Disorder Example #3:
“I am going to get a bad grade on this test.”
Step #1: Define terms
• Ask yourself: “What is a ‘bad’ grade? Is it failing? Is it a “C?” Is it a “B?”
Step #2: Identify potential cognitive distortions
• Examples may be: fortune telling and all-or-nothing thinking.
Step #3: Examine the evidence:
Line of evidence #1: (likelihood) How likely is it that I will get a bad grade on this test?
• How have I performed on tests in the past?
• Have I ever predicted I would perform poorly on a test before? How did the test turn out? Write down
the results of the last 5 tests you can remember. Did these tests come with predictions of getting a bad
grade? How did they turn out?
• Is this class any different than other classes?
Line of evidence #2: If I did get a bad grade on this test, what would be the consequences?
• If this happened, what would I do? Would I give up, or keep trying?
• Have I ever done poorly on a test in the past? What were the consequences of this? How did this test
score affect my overall grade?
• Is it likely that getting a bad grade on this test will significantly impact my ability to achieve my long
term academic goals?
Line of evidence #3: Preparedness
• Have I prepared for this test?
• How does my performance on tests in the past align with my preparedness? Was I ever unprepared for a
test on which I performed poorly? How have I performed when I prepare adequately?
• Does anxiety ever interfere with my ability to remember facts? Do I have trouble concentrating?
Step 4: Address “worry about anxiety” (type II worry)
• Often when we worry about tests or other performance situations, there is a concern that the
anxiety will make us perform poorly or people will notice it. We do not have time to address this in this
manual; however, this is an important issue to address with your group leader or individual therapist.
Step #5: Use the “Thought Cascade” approach to uncover other thoughts related to this thought. Ask “If I did get a bad grade,
what would be so bad about that? What would be the consequence?” Use the same cognitive techniques to examine the evidence
around the other thoughts.
Step #6: Uncover core beliefs
• Ask: “Is it possible that my concern about getting a bad grade is related to having unrealistic expectations for myself? Do
I ever think that I must be perfect or get an ‘A’ on every test?”
Step #7: Behavioral techniques
• Use problem solving techniques to determine if the situation can be improved. Is there anything I can do to
improve my study habits? Could I practice taking tests to become more comfortable with the anxiety? Do I have good
test taking skills?
• Are there any “safety behaviors” or protective behaviors I am using that may actually be making we perform more
poorly on tests? For example, do I ever second guess myself repetitively about answers and change them? Do I take
more time than necessary deciding on answers?
• Along with cognitive techniques, use exposure skills to get practice taking tests and address avoidance or
protective behaviors that may be making the anxiety worse over time.
Step #8: Use acceptance skills to let go of effort to fix things you cannot change. For example, we do not know exactly what
questions will be on every test, and it may be healthiest to accept that we may get some questions wrong.
3.27

Cognitive Skills for Daily Worry and Generalized Anxiety (con.)
Generalized Anxiety Disorder Example #5:
“If I worry, it will help me be safe.” “If I don’t worry, it is more likely something bad will happen.”
“Worrying helps me accomplish things and solve problems.”
Step #1: Examine the evidence:
Line of evidence #1: Past experience
• Has worrying helped me prevent catastrophe in the past? Does it protect me?
• Is it necessary for me to worry to be safe, or could I stay safe even without this anxiety?
• Have I ever accomplished a lot without worry?
Line of evidence #2: Pros and cons of worrying to stay safe versus living with some risk
• What are the good things about worrying to stay safe? What are the problems that this worrying creates in my life?
• What are the good things about letting go of the worry? Are there any potential downfalls to this?
• Do I like this worry? Do I want to continue to live with it? Would life be better without it, even if I had to accept some
risks?
Generalized Anxiety Disorder Example #4:
“This worry will never end” or “This worry will make me go crazy” (Type II worry)
Step #1: Identify potential cognitive distortions
• Examples may be fortune telling and magnification.
Step #2: Examine the evidence:
Line of evidence #1: (likelihood) Past experience
• How has my anxiety and worry fluctuated over the years? Have I ever had times in which I felt better? Was
it true that the anxiety lasted forever?
• Have I ever gone “crazy” as a result of worry?
Line of evidence #2: Ability to function with anxiety
• Have I been able to function at times, at least well enough to accomplish some of my goals, even with the
anxiety and worry?
• Does the anxiety make me avoid things? (If so, this could contribute to the idea that you “can’t function.” Consider
exposure skills to practice functioning better with anxiety to manage it and still achieve some
of your life aims)
Line of evidence #3: Anxiety is uncomfortable, not dangerous
• See “Anxiety is…” & “Could I lose it” (in the previous section on panic disorder) to remind yourself about the danger of
anxiety. Although anxiety is uncomfortable and does put stress on the body, remind yourself that it is not dangerous,
and does not lead to “going crazy” or becoming psychotic.
Step #3: Emotion regulation and “acceptance of emotion” skills
• Remember that trying to “fix” or avoid anxiety reinforces the anxiety.
• Remind yourself: “Trying to get rid of this anxiety or avoid it will just make it worse. I can accept and
tolerate this anxiety feeling and allow it to happen. I can then try to learn the facts about this situation. I can
do things that will help me reach my goals, instead of spending time trying so hard to get rid of this anxiety.”
Step #4: Work on other “Type I” worries (everyday worries about bad things happening) that may contribute to this worry, as in
examples 1-3 on the previous three pages.
Note: see “The only thing we have to fear is fear itself” for more help with “worry about worry,”
especially if worry has led to panic attacks.
Step #2: Identify negative automatic thoughts and examine the evidence around the specific problems happening
at this time.
Step #3: Use problem solving skills to best find a solution to a problem. If there is no feasible solution, use
acceptance skills to let go of attempts to control what cannot change.
3.28

“Unifying Your Forces:” other CBT skills for Generalized Anxiety
On the previous four pages there are examples of specific thoughts that occur when people worry. While thoughts are an important
part of generalized anxiety, there are other factors that influence how anxious we are on a daily basis. One factor is our core beliefs
and ideas about the world, called “core schemas.” Thoughts such as “I must always give 110% to everything in my life” and
“People that make less than $100,000 a year are failures” are examples of core schemas that may be helpful to modify.
Modification of core schemas are a part of CBT that could be helpful for you.
There are also factors, other than the way we think, that can contribute to generalized anxiety. Examples are the goals we set (and
whether or not we are reaching them) and how busy we are. Setting reasonable, achievable goals and managing our time
effectively are often addressed in a course of CBT.
• Generalized Anxiety Disorder (GAD) is characterized by uncontrollable worry
about multiple areas of one’s life.
• The two types of worry are worry about bad things happening to ourselves and
people close to us (type I worry) and worry about the worry itself (type II worry),
both of which contribute to chronic anxiety symptoms.
• Worries, related worries, frustration and worry about the anxiety, attempts to fix or avoid the anxiety, and
physical anxiety symptoms create the “snowball effect” that makes the anxiety worse, both in the moment and
in the long run.
• Since thoughts are the primary “triggers” of anxiety in GAD, cognitive therapy skills are an important part
of treatment for this concern. We use “lines of evidence” to gather facts about the situation; we look at the
likelihood of bad things happening as well as ways to cope with the consequences of them happening.
• Problem solving and acceptance skills are also used to address GAD’s negative automatic thoughts.
Exercise
1. If you have not done so already, use the techniques in the section on “Identifying Negative Automatic
Thoughts” about the future (type I worry), or thoughts about the worry itself (type II worry).
2. Use the examples on previous pages as a guide to ask questions about these thoughts and examine the
evidence.
3. Use the “Examining Thoughts” worksheet to write down the thoughts, possible cognitive distortions, and
evidence you find. You can also write down the evidence on a note card and carry it with you.
4. Remind yourself of this evidence in the morning before you start your day. When these thoughts pop up
during the course of the day, take out the “Examining Thoughts” worksheet or the note card to remind
yourself of the evidence. Remember, it takes repetition to retrain the brain!
3.29

The following are common thoughts that many people have about their own anxiety. Some of these thoughts make it hard to
move forward to address the anxiety problem assertively. Check any of the thoughts below that you may have from time-to-
time. If there are others you experience that are not listed below, write them in the provided box below. Part of CBT is looking
at these thoughts, so be sure to bring them up to your therapist or group leader when you start the active phase of treatment
following the group.
Thoughts about anxiety being outside of one’s control
____“My anxiety just happens, and I have no control over it.”
____“I am completely frozen by my anxiety and can’t do anything about it.”
____“My anxiety is different than everyone else’s.”
____“I can’t control my anxiety.”
Pessimistic predictions about treatment
____“This anxiety will never go away.”
____“I haven’t gotten better yet, so it won’t happen.”
Unrealistic expectations about the speed of improvement
____“I want the anxiety to go away right now. I want a cure.”
____“I want this to happen right now.”
____“I don’t have time to spend on this.”
Deficiencies in knowledge
____“I don’t understand.”
____“I don’t even know why it happens.”
____“I don’t understand how this could be helpful for me.”
Worry/anxiety/panic is harmful
____“Treating anxiety by having to think about it will cause harm to me.”
____“Worry is harming me.”
____“If I have anxiety during treatment I won’t be able to handle it.”
____“If I open this can of worms, it will never close.”
____“It will just be too overwhelming.”
____“Anxiety will never end if I let it happen.”
____“If I don’t control my thoughts and emotions they will take over and never end.”
____“If I allow myself to worry it will get out of control.”
____“If I treat my panic by challenging the anxiety, I will have a heart attack, suffocate, go crazy, or faint.”
Positive beliefs about anxiety/worry
____“Anxiety helps me: if I get rid of it, I will not perform as well, or fail.”
____“Worries help me solve problems.”
____“Anxiety and worry makes me perform better.”
Other thoughts about anxiety or treatment I have, not listed above:
“___________________________________________________________________________________________”
“___________________________________________________________________________________________”
“___________________________________________________________________________________________”
“___________________________________________________________________________________________”
“___________________________________________________________________________________________”
3.30

Cognitive Therapy Skills are one set of skills used in CBT. They are
based on the idea that our thoughts can affect how we feel.
We learned what cognitive therapy skills are and how they work: we
gather evidence to understand a situation as realistically and in as detailed
a way as possible.
Cognitive Therapy Skills are not just “thinking positive.” In fact, some situations are really bad. Our goal is to
Examine the Evidence and practice reminding ourselves of this evidence when we are in a challenging situation, in
order to cope better with that situation.
Cognitive skills are best used in combination with behavioral skills such as exposure. If we can understand how
dangerous a situation is, we can make good decisions about whether or not it would improve our lives if we were to
stop avoiding a situation or over-protecting ourselves, which can be limiting.
We learned how to identify Negative Automatic Thoughts and the “worst-case scenario” thoughts that are often
connected with them. Identifying Negative Automatic Thoughts is the first important step in using Cognitive Therapy
Skills.
We learned about Cognitive Distortions, such as “All-or-Nothing Thinking,” which are unhelpful patterns of
negative thinking. Sometimes it can be helpful to understand whether or not we have some of these patterns in order
to more effectively battle our Negative Automatic Thoughts.
We Examine the Evidence, using techniques to understand two important questions:
1. How likely is it that something bad will happen?
2. If it did happen, how bad would it be? What would I do if it happened? How might I cope?
The Examining Thoughts Worksheet is one tool that can help us organize the evidence we gather when we are first
learning cognitive skills. Writing down evidence about a thought helps us see things more objectively and remind
ourselves of information that is hard to remember when we are feeling anxious. Eventually, we hope to be able to
remind ourselves of the evidence quickly in the course of daily life, without needing these types of aids.
One important part of an anxiety problem is fear of the anxiety itself; because anxiety feels so bad and makes it hard
to accomplish our aims, we worry about having it. We also may start wondering if the anxiety could harm us in some
way; these thoughts about the anxiety can make the anxiety even worse. We dispute some of these thoughts to battle
the “fear of fear.”
Worries are a common part of anxiety, and we give examples of how to battle these worries using cognitive skills.
“I’m going to lose my job” and “What if something happens to one of my children?” are examples.
Problem solving, acceptance skills, setting achievable goals, and managing time effectively are other important
factors that can reduce anxiety. We combine cognitive therapy skills, relaxation skills, and exposure skills with these
other skills to manage GAD and chronic worry.
3.31



Have you ever been told to “just relax?” Of course feeling relaxed would be ideal– this is
why we come to get help in the first place! But anyone who has felt panic or extreme
anxiety knows “just” relaxing is much easier said than done.
One set of skills used to supplement other CBT skills (such as exposure and cognitive
skills) are relaxation skills. Relaxation skills address anxiety from the standpoint of the
body by reducing muscle tension, slowing down breathing, and calming the mind.
Relaxation skills can be structured; examples are slow diaphragmatic breathing,
meditation, and yoga. Other factors, such as self-care and enjoying pleasurable activities,
are also helpful to make us feel more relaxed. In this module we’ll explore some of these
strategies, explaining how they are used and why they work.
As we will emphasize in this section, relaxation skills are best used in conjunction with
other CBT skills and are most effective when practiced consistently. Different skills work
for different people, so the first step is to try to find the relaxation strategies that appeal
to you and try them out. Enjoy!
4.1
“The time to relax is when you don't have time for it.”
~Attributed to both Jim Goodwin and Sydney J. Harris

What are relaxation exercises?
The Problem: “Somatic” Anxiety Symptoms
Most people that experience anxiety also experience unpleasant physical sensations regularly. In
medical lingo, the fancy term for “physical” is somatic. We all know some of the most common
somatic symptoms of anxiety: muscle tension, headaches, backaches, a clenched jaw, feeling keyed
up, restless, and “on edge,” as well as difficulty concentrating. You may remember that these
symptoms are a side effect of our body’s attempts to protect us; blood moves around our body and
brain, into our large muscles, like our arms, legs, back, and neck, to get us ready to ”fight” or to
“flee.” This changes the feelings in our bodies. In short the body is working hard to protect us, and
these feelings are uncomfortable! Relaxation happens when the body stops trying to protect us,
which helps us feel more calm and at ease.
When we experience mild to moderate levels of anxiety on a daily basis for long periods of time, we
get used to this tense, jittery state, until it is hard to even know what it is like to be relaxed! In this
case, we would say a person’s anxiety and tension is resting, or “baseline,” at a high level. The goal
of these types of relaxation exercises is to change this baseline to a lower level.
Very relaxed
Very tense
With stress and worry,
levels of anxiety and
tension become higher
over time.
1. Find a relaxation exercise that you can practice daily or
multiple times per week. Examples are progressive muscle
relaxation, yoga, mindfulness, and deep breathing.
2. Adjust your lifestyle to make it less busy, hectic, and rushed.
3. Take part in activities that give you pleasure, make you feel
competent, or give you a chance to take a break from other,
more stressful activities.
Relaxation skills are like exercise!
Imagine a friend of yours telling you that she is planning to train for a
10K race. Despite the fact that she has never run a race before and does
not jog regularly, she tells you her training will consist singularly of
practicing running the full 10 kilometers on the day before the race. What
would you think about this?
We know that the body needs time to learn how to run for long distances
and build strength. She would need to practice at least a few times per
week for a number of weeks to be ready.
Relaxation skills are developed just like exercise: in order to see
significant results, we must use them regularly over long periods of time.
This is not a one shot deal!
Goals of relaxation skills
1. Learn when and how to use these skills.
2. Learn to breathe in ways that will promote
calm and relaxation.
3. Slow down activity in the mind to avoid or
learn to better tolerate “racing thoughts.”
4. Increase awareness of tension in the body and
improve awareness of the difference between
tension and relaxation.
5. Lower general levels of tension and
restlessness in the body.
6. Learn to incorporate activities into our lives
that are fun and/or make us feel competent.
7. Be calmer in our daily lives by learning to
“slow down” and set realistic goals for our
time.
The goal of relaxation
strategies is to lower
general levels of anxiety
and tension in the body
over time.
Each person is different-- we all relax in different ways. In this
module we’ll discuss a number of different methods to try:
4.2

1. _________________________________________
2. _________________________________________
3. _________________________________________
4. _________________________________________
5. _________________________________________
6. _________________________________________
7. _________________________________________
8. _________________________________________
9. _________________________________________
10. _________________________________________
Take home points:
Relaxation strategies can be useful in reducing general
levels of anxiety and tension over time. They are not
typically a “cure” for anxiety; they are best used together
with other CBT skills such as cognitive restructuring and
exposure and practiced regularly, like exercise. They also
should not be used to prevent or get rid of panic or severe
anxiety symptoms. For each person there is a different set of
activities and skills that help them relax. Our best strategy is
to find the ones that work for us and practice them.
Relaxation strategies are just one set of skills used in CBT. We all would like to spend more time feeling relaxed, but
relaxation skills are not always the right skills to improve our anxiety in the long run. One important CBT skill is
knowing when to use certain techniques, so we want to know when relaxation strategies are or are not helpful for us.
Relaxation strategies are best used as a companion to exposure and cognitive skills, but not as a replacement to
them. Sometimes relaxation strategies can actually make anxiety worse in the long run. Why? Because sometimes
relaxation strategies are used as a way to get rid of anxiety when we are in distress; trying to get rid of something trains
our brains to see it as “bad.” So we teach the brain to set off the anxiety “alarm” even louder when the anxiety presents
itself. In the long run, this makes the anxiety worse. In short, there are times and places for relaxation skills!
When to use relaxation strategies
-As a daily practice, like exercise, to lower tension and feel
calmer in our bodies over time
-During times of distress in order to prevent avoidance of
something that is integral to our life aims
Why? It is more assertive: “Doing this exercise will
not cure my anxiety, but it will keep me from
avoiding the situation.”
(When we face the anxiety, the brain learns that
it is not so dangerous, which, in turn, lowers the
anxiety in the long run)
“How should I relax?
What will work for me?”
Everyone is different— some relaxation skills work well for
some people, and others for other people. It is likely that there
are some methods that you already use to relax. Think about
exercises, practices, or activities you use regularly in order to
relax and list them below. If you are having a hard time
coming up with something, see page 74, “Finding Relaxation
Strategies That Work for You” and review the list of some
common methods of relaxation.
When not to use relaxation strategies
-In times of panic or severe distress as a way to get rid of the
anxiety
-As a replacement for other types of CBT skills such as
cognitive restructuring and exposure
Why? It is overprotective: “This anxiety is unbearable!
I must do something to make it feel better!”
(This trains in the idea that anxiety is dangerous,
which causes more anxiety over time)
4.3

1. The speed of the breath is more
important than the depth of the
breath. Avoid trying to “catch” your
breath by taking really deep
breaths.
2. Don’t use breathing exercises to
“get rid of” the anxiety; use the
breath to help get you through a
tough situation, or practice it daily
to “train in” a slower, calmer
breathing style over time.
3. Practice! It takes time to learn how
to calm the body using the breath.
Take home points:
Slow diaphragmatic breathing is one
relaxation skill used in CBT. It is best
used as a daily practice, like exercise, or
as a way to get through a tough situation
without leaving or making things worse.
For best results, practice slow breathing
twice a day for around 10 minutes each
time.
You may have been told in the past to “take a few deep breaths” when you were
feeling worried or upset about something. On one hand this is helpful to just slow
down and cool off. However, altering the speed of our breath actually can slightly
change our body’s anxiety response. Slow diaphragmatic breathing is a developed
technique that involves slowing down the breath to communicate “safety” to the
brain.
“Slow Diaphragmatic Breathing”
1. Sit comfortably in a chair with your feet on the floor. You can lie
down if you wish.
2. Fold your hands on your belly.
3. Breathe in slowly and calmly. Fill up the belly with a normal breath.
Try not to breathe in too heavily. The hands should move up when
you breathe in, as if you are filling up a balloon. Avoid lifting the
shoulders as you inhale; rather, breathe into the stomach.
4. Breathe out slowly to the count of “5.” Try to slow down the rate of
the exhale. After the exhale, hold for 2-3 seconds before inhaling
again.
5. Work to continue to slow down the pace of the breath.
6. Practice this for about 10 minutes.
7. This works best if you practice this two times each day for 10 minutes
each time. Try to find a regular time to practice this each day.
While we do not recommend that you use breathing techniques to try to eliminate
anxiety when you are feeling anxious, it can be a way to get through a tough
situation and calm the body some so that we can make a good decision about what to
do next. Try the following exercise:
Slow Diaphragmatic Breathing Tips:
4.4
The techniques you were just using are called mindfulness skills. These
are techniques that originate in Buddhist meditation practices, but they
have been studied and used more and more by psychologists and
physicians in the last 20 years or so to help people regulate their
emotions and calm their minds. So how do they work?
It is not fully understood why mindfulness is so helpful, but we have
some ideas. The goal of mindfulness is to describe all kinds of
experiences objectively and non-judgmentally, focusing on the facts
about the present moment. Sound familiar? It may remind you of
cognitive skills, which are an attempt to gather evidence around a
thought that triggers our anxiety, which lessens the power of that
thought. Another way to lessen the power of the thought is to see it for
what it is: just a thought. And one thing we know about thoughts is that
they change. It is difficult to adequately capture the gist of mindfulness
by trying to explain it, so try the exercise to the right.
1. Sit quietly with your feet on the floor, or lie
down, and relax your body. Begin with some
slow, diaphragmatic breathing. Focus your
mind on your breath as it flows in and out of
your nostrils. Continue to follow your breath
to whatever extent you can.
2. As you breathe, notice the tendency of the
mind to wander. Instead of trying to focus just
on the breath, just notice what the mind does.
It may wander to a worry, or a memory, or to
what you plan to do later today. You may
notice sensations in your body, such as a pain
or itch. You may hear or smell things. Just
notice whatever happens and then gently bring
yourself back to your breath. You can remind
yourself that you will tend to these other
things later, and for now you will just spend
time paying attention to your breath and to
your mind.
3. Allow the mind to wander as it will, time after
time. Avoid the tendency to try hard to focus
on something. Simply allow your mind to
wander and then bring yourself back to your
breath. Notice the tendency of your experience
to change. Imagine that each thought,
sensation, emotion—anything— is like a cloud
floating through the sky, soon to be replaced
by another one.
4. Continue to practice this for about 10 minutes.
Depending on your schedule you can add time
to your practice if you want. Practice once or
twice a day.
5. Remember that there is no “right” way to do
this, other than to just notice whatever comes
into your consciousness. It is impossible to
“fail” at mindfulness—just let your mind
wander!
Mindfulness Exercise
Take a moment to observe the photo to the right and then try this
exercise:
Just describe what you see in completely objective terms. Just notice
colors, shapes, shades, etc. Write what you see here:
_________________________________________________________
_________________________________________________________
_________________________________________________________
Now notice the memories and thoughts that come up when you look at
this picture. Allow your mind to wander as it will, and write down what
“pops” into your mind as it comes up. Take 1-2 minutes to do this.
_________________________________________________________
_________________________________________________________
_________________________________________________________
4.5

Slow down the mind, con
“I can’t control my mind!”
On the last page we suggested that you “let your mind wander.” This may seem to be
the opposite of what you have been told to do while trying to meditate or complete a
task. We go into something expecting to have “control” of our minds.
We know from research that we cannot completely “control” our minds, no matter how
hard we try, especially when we are feeling anxious. Why do you think this is true?
Think back to the “Anxiety 101” section of this manual where we described the
function of anxiety to help protect us. When we are anxious, the amygdala, our anxiety
center of the brain is trying to send off its “anxiety alarm.” One way it does this is by
trying to alert us to the possibility that something is dangerous, either “out there” in the
environment or inside our bodies. After all, if we are too focused on one thing, we
could be hurt by something else! So the mind tries to distract us, making it very
difficult to “control” the mind. In fact, you may find that the more you try to control it,
the more the mind tries to distract you!
“Why should I practice mindfulness?”
Mindfulness techniques are an important part of CBT for the
following reasons:
-Trying to “control” the mind is a futile endeavor. In fact,
trying to control the mind often makes us feel worse,
because we keep failing at it! The first step to any CBT
intervention is to stop trying to control the mind through
force; only after we do this are we prepared to influence the
anxiety using CBT skills.
-Mindfulness helps us practice observing but not reacting to
anxiety and other emotions. We learn to accept or tolerate
these emotions, rather than trying to eradicate them.
-Mindfulness helps to retrain the brain; by not reacting to the
anxiety and not trying to fix it, we communicate to the
amygdala that it is not dangerous. This is one way to work
on addressing the “fear of fear.”
-When we stop and pay attention to the present moment, we
listen to our anxiety “alarm.” If we give it time and keep
from “fueling” the anxiety, the body can eventually learn
that it does not need this alarm any longer, so it can turn it
off.
Mindfulness: Take Home Points
Mindfulness is a relaxation strategy that can be helpful in calming the mind by reducing our tendency to try to control it, which
often makes the anxiety worse. Mindfulness techniques focus on facts and objective information about current experiences,
including emotions, thoughts, memories, and sensations. Our aim is to notice these experiences without judgment or any attempt
to change them; we simply observe them, like clouds in the sky or the images on a movie screen. Mindfulness techniques are not
likely to cure anxiety all by themselves, but they can be helpful if used with other CBT skills, and can provide a foundation upon
which to develop these skills.
Having trouble getting “mindful?”
Try this: pretend your mind is like a movie screen. You are
sitting in the movie theater, observing what is projected on the
screen, but you are not in control; you just watch and follow
what you see.
Try closing your eyes and just notice what images, thoughts, or
memories get projected on that screen. They may be related or
not—whatever gets projected is fair game! If you start feeling
attached to the content of the “movie,” just notice that
attachment and then let the movie continue to something else.
4.6

One way to think about relaxation is that it is the absence of tension in the body’s muscles. Imagine
being able to simply release your body’s tension instantly without taking medication or having a drink!
In the 1920’s Edmund Jacobson, a Chicago physician, created a set of exercises aimed to do just that—
he published his intervention in a book entitled Progressive Relaxation. What Jacobson knew to be true
is that deep muscle relaxation is incompatible with our body’s anxiety response. He worked with the
knowledge that by consciously working to reduce muscle tension, we can actually influence how
anxious we feel.
The aim of what we now call Progressive Muscle Relaxation (PMR) is to gradually learn to release
tension in the muscles through daily exercises. This communicates calm and safety to our body,
reducing the body’s need to activate the “fight or flight” response.
Exercise
Progressive Muscle Relaxation: Take Home Points
Progressive Muscle Relaxation (PMR) is a set of exercises aimed at helping
us reduce anxiety and tension in the body. Through the practice of tensing
and relaxing groups of muscles, we learn to feel the difference between
tension and relaxation and release muscle tension when we feel it. It works
best if practiced regularly. As with any skill, relaxation takes time and
practice to master.
Applied Relaxation (see the next page) builds on the skills learned in PMR
to more quickly reach a relaxed state, even under stressful circumstances.
For more information about Progressive Muscle Relaxation and Applied
Relaxation, refer to Davis, Robbins, and McKay’s Relaxation and Stress
Reduction Workbook, which has written scripts for these techniques.
To get a full “dose” of Progressive Muscle Relaxation, try the track “Progressive Muscular Relaxation” on the Anxiety
Disorders Program Website. This will take you about 16 minutes. This track will help you relax the body, one muscle group at a
time. It is best to try to practice this for two weeks, once or twice a day. Some people find that it is helpful to do it in the morning
when they wake up, or at night before going to bed.
After you try this, you can decide if you want to continue with Applied Relaxation, which is the program
described on the next page. This program builds on what we have learned from Progressive Muscle Relaxation
by helping us to learn to relax more and more quickly.
To get a taste of this, try tensing the muscles of the arms by “flexing” your biceps, as in the picture to the
right. Tense your biceps hard enough to feel significant tension for between 5 and 7 seconds.
Now let go, dropping your arm to your side. Feel the difference between the tension you just felt and the
relaxation that is coming over your arm now. You may notice the feeling of blood flowing to the arm, and
a feeling of warmth. PMR involves doing this with each group of muscles in the body, as a regularly
practiced exercise that takes effect over a period of time.
4.7

Progressive Muscle Relaxation, con.
Applied Relaxation
Stage 1A: Progressive Muscle
Relaxation (PMR) (Track One): 2x
per day in 18 minute increments for
2 weeks.
Stage 1A: PMR Shorthand
Procedure (Track Two): 2x per day
in 7-8 minute increments for 2
weeks.
Stage 2: Release-Only Relaxation
(Track Three): 2x per day in 5-7
minute increments for 1-2 weeks.
Stage 3: Cue-Controlled
Relaxation (Track Four): 2x per
day in 2-3 minute increments for
1-2 weeks.
Stage 4: Differential Relaxation
(Tracks Five and Six): 2x per day in
10 minute increments
Stage 5: Rapid Relaxation (Track
Seven): Practiced multiple times a
day in the flow of daily life.
Stage 6: Applied Relaxation
(Track 8): Here the goal is to learn
to relax quickly under actual
stressful circumstances.
1A: Progressive Muscle Relaxation
Progressive Muscle Relaxation (PMR) is the basic skill (this is discussed further on the previous page). While guided by a therapist
(or recording), a person practices tensing and then relaxing individual muscle groups, which releases tension and makes one more
aware of the difference between tension and relaxation. It is good to practice in the morning or at night before going to bed. Try
practicing it one or two times per day for two weeks before expecting to see results.
1B: Progressive Muscle Relaxation:
“Shorthand Procedure”
Once a person has mastered the basics of
Progressive Muscle Relaxation, we can
begin to learn to reach this relaxed state
more quickly, by tensing and relaxing
larger groups of muscles at one time. This
shortens the time to do the exercises to 8
to 9 minutes.
2: Release-Only Relaxation
In this phase of Applied Relaxation
treatment, we take out the “tensing” step,
to learn to release muscles and feel
relaxed even more quickly-- in around
5-7 minutes.
Applied Relaxation
The Swedish physician L.G. Öst took the principles of Progressive Muscle Relaxation and developed Applied Relaxation, a program
that aims to increase our ability to relax quickly, even in stressful circumstances. This is a set of skills that takes time to develop—as you
can see from the outline of the stages below, each of the stages of treatment involves one to two weeks of practice. Full scripts of this
program are available in Davis, Robbins, and McKay’s Relaxation and Stress Reduction Workbook.
3: Cue-Controlled Relaxation
Cue-Controlled Relaxation reduces the
amount of time to deep relaxation. We
learn to be able to relax whenever we
choose, for example, when we say the
word “relax.” It is possible to reduce the
time to relaxation to around 2-3 minutes in
most cases.
4. Differential Relaxation
The goal of Differential Relaxation is to help one learn to relax in the midst of daily activities. Most daily activities involve
use of some muscles but not others. In this step we learn to isolate the muscles we need for a specific task and relax the rest of
our body. In this way we can learn to incorporate relaxation into the flow of daily life.
5. Rapid Relaxation
Rapid Relaxation allows us to
bring the time to relaxation down
to 20-30 seconds. We learn to pick
something in our daily life with
which we have contact regularly,
such as a clock or watch, and
associate this cue to the relaxation
we have learned in the previous
stages. Some people find it helpful
to put a piece of colored tape on
whatever cue they pick. It works
best if we can practice this 15-20
times a day in normal, non-
stressful situations.
You will know when you are ready
to move on to the next step when
you can bring a sense of relaxation
to the body within 20-30 seconds.
6. Applied Relaxation
This final stage uses the same
techniques used in Stage 5, now
applied to more stressful situations,
including those that involve some
degree of anxiety.
4.8
Did you know?
Yoga is a well-established, historic discipline that incorporates a powerful combination of mental and physical elements: breathing,
stretching, meditation, and strengthening exercises, aimed at improving physical and mental well-being. It involves a series of
challenging body positions that stretch and strengthen muscles. It is best learned by taking a class with a certified yoga instructor,
and has many benefits, both physical and mental.
When it comes to relaxation strategies, there are many options. We have
to find the ones that work for us. So far we’ve introduced three available
“brands” of relaxation: breathing, mindfulness, and Progressive
Muscle Relaxation.
You may have listed some relaxation strategies that work for you in the
section: “Relaxation Strategies: When? How? Why?” Below we list a
number of other popular, formal relaxation strategies that have been used
successfully by others. You might try some and add them to your list!
“Soothing” Activities
• Sounds: music you enjoy; ambient music;
“new age,” repetitive music; sounds of nature,
such as babbling brooks or ocean waves
• Smells (Aromatherapy): incense, candles, etc.
• Sights: Visualization: beaches, falling leaves,
etc.
• Nature: hiking, swimming, parks, etc.
“Body-based” Relaxation Strategies
• Slow-paced diaphragmatic breathing
• Yoga
• Progressive Muscle Relaxation and Applied
Relaxation
• Massage
• Hot tubs, hot baths, or sauna
“Mind-based” Relaxation Strategies
• Meditation (Mindfulness meditation,”
Transcendental Meditation, etc.)
• “Body Scan”/body awareness exercises
• Prayer
• Autogenics
Imagine that you are at a supermarket shopping for breakfast cereal. So
many choices! Some people like a simple granola, others enjoy their
cereal sweet, and others like something with fruit in it. You might choose
something you’ve enjoyed before, or you might try something new
because it looks like it would be tasty or nutritious.
On this page we introduced some of the structured approaches to relaxation that have been used successfully by others over the
years. However, some of the most relaxing activities are those that we enjoy, or make us feel good because we are good at them
and can be creative or skillful. On the next page we discuss mastery and pleasure, two important elements of living a relaxing and
enjoyable life.
4.9

A Life Worth Living: Pleasure and Mastery
“Pleasure” “Mastery”
Hobbies and other “play”
• Reading
• TV, movies, plays
• Dancing
• Playing or listening to
music
• Board games or cards
• Arts and crafts, sewing, painting
• Cooking
• Walking, hiking, enjoying nature,
fishing
• Sports (basketball, softball,
swimming, etc.) or going as a
spectator
• Martial arts (karate, etc.)
• Museums/zoos
• Video games
• Traveling, sightseeing, going
to the beach, sunbathing
• Shopping
• Gardening/decorating
• Photography
• Comedy: TV, recordings, live
• Religion or spirituality
Social activities
• Spending time
with family
• Enjoying own
children and/or
young relatives
• Enjoying close
friends
• Hanging out
with large
groups of
friends/acquain-
tances
• Parties, meeting
new people
• Romance
• Pets
• Clubs: meeting
people with
similar interests
• Enjoying food
and drink with
others
If someone were to ask you “What do you do to relax?” it is likely that you would say something like “I like to hang out with
friends,” “I watch TV,” or “I play golf.” While these are not formal relaxation strategies, they bring us pleasure and/or make us feel
good about ourselves; we certainly feel more relaxed when that is the case. These are the things that the anxiety tries to take away
from us, which is even more of a reason to spend time doing them!
For the purpose of exploration here, we outline two important generators of good feelings: pleasure and mastery. Pleasure involves
activities, or “play” that we enjoy for the sake of the activity itself. Mastery involves activities, such as work or sports, that involve
the development of skills; we are able to accomplish things and feel a sense of mastery over our environment. When enjoyed in
moderation and diversified well with other activities, they can increase positive emotions and improve how we feel about ourselves.
List enjoyable activities in which you take part now or have
enjoyed in the past. Add others from the list above that appeal
to you or others that you think you might enjoy:
1. _________________________________________________
2. _________________________________________________
3. _________________________________________________
4. _________________________________________________
5. _________________________________________________
List skill-based activities, such as work or sports, that are a
part of your daily routine and lead to positive feelings and
a sense of self-worth. Choose others from the list above or
fantasize about possible activities that seem rewarding.
Write them here.
1. _______________________________________________
2. _______________________________________________
3. _______________________________________________
4. _______________________________________________
5. _______________________________________________
Job or Meaningful Daytime Activity
Look for or attempt to develop some of
these qualities in your occupation
volunteer work, or other meaningful
daytime activity:
• Enjoyment
• Creativity
• Feelings of competence (able to
accomplish tasks satisfactorily)
Other skill-based activities
• Sports
• Music practice and performance
• Home improvement/building
• Woodworking
• Visual art (painting, drawing,
pottery, sewing, knitting
• Learning about interests
(history, politics, food,
language, culture, etc.)
• Potential for development of skills
• Ability to “move up” in the organization or take
on more responsibility, if this is desired
• Social contact with coworkers, colleagues, others
in the field
4.10

Confront Conflict
Do not allow interpersonal
conflicts to fester; learn assertive-
ness and other communication
skills and address conflict
proactively and
diplomatically.
Treat Physical Illness
Scientific research shows a connection
between physical health, mood, and anxiety.
Learn about your family medical history,
go to the doctor as needed, and take
prescribed medications.
Sleep
Research has shown that most
people need an average of about 7 hours
of sleep per night. Sleeping well is an
important aspect of managing anxiety. Talk to
your doctor or therapist about a referral
for a consultation with a sleep expert if
you suffer from insomnia or
sleep apnea.
Diet
Eating a balanced diet
helps us maintain health,
improves energy, and contributes
to good mood. Be aware of the
quality of your food, as well as how
much you eat; eating either too
much or too little can affect
how you feel on a
daily basis.
Avoid or limit
use of “mind altering
drugs”
Be aware that all drugs that alter state of
mind such as alcohol, caffeine, nicotine, mari-
juana, other illicit drugs, can exacerbate an-
xiety in both the short and long term. Discuss
your use of these substances openly with a
prescribing clinician to understand
better your own risk factors.
Social Support
When we feel supported
by others, we feel more safe,
secure, and happy. One important
approach to treating anxiety is to
reduce symptoms; another way is
to increase positive experiences,
especially with people that help
us feel good about
ourselves.
Exercise
Regular exercise has been
shown to be as good as
antidepressant medication for treating
depression and increases our resistance to
debilitating anxiety. Try to get a minimum
of 20 minutes of vigorous cardiovascular
exercise at least three times a week. Of
course, be sure to ask your doctor
if you are healthy enough for
more intensive exercise.
“Slow down”
Ask yourself: “Has
there been a day this week
in which I did not “rush” at
all? Keeping a constant fast
pace in activity, whether walking,
working, or even planning leisure
activities, communicates a sense of
urgency to the brain, raising blood
pressure and tension in the body.
This has an impact on our anxiety
from day-to-day. Practice
“slowing down” your pace of
life consciously to reduce
this sense of
urgency.
Goal Setting
Set realistic goals in line with your
life aims. Strive for balance of
meaningful work, interpersonal (family
and friends), and enjoyment-oriented
goals. Remember to take one small
step at a time to reach larger
goals.
Treat Mental Illness
Learn to manage anxiety using
CBT skills. Treat other forms of
mental illness if they interfere with your
life. If the therapy you try does not seem
to be working, try another therapy style
or therapist. Consider a “combination
therapy,” which combines a assort-
ment of therapy skills, medi-
cation, and self-care.
Time Management
Set realistic goals about what can be
accomplished in a certain amount of time.
Avoid multi-tasking excessively. Plan your day
with enough time left over to sleep enough,
exercise, and enjoy a leisure activity. If you feel
that you have trouble managing your
time, discuss it with a therapist
or life coach.
As we have discussed throughout this manual, battling anxiety requires a multifaceted strategy; we have to “unite our forces” to keep
anxiety from interfering with our life aims. CBT supplies us with some of the ammunition to wage this battle, but other lifestyle factors are
important. as well. Below we discuss some of these factors; consider them when assessing your challenges with anxiety and consider trying
out some changes to see if they help.
Moderate and Balance Coping Skills
Address anxiety from a variety of different angles by confronting fear, problem solving,
accepting that which cannot be controlled, and modifying thinking when necessary. Take care of the body and
mind, addressing the important elements of self-care listed below. Remember that “diversity” is the cardinal
rule when it comes to coping with challenges; the more skills and coping methods we have,
the more flexible we can be when challenges arise.
4.11

My Relaxation Plan
(how I plan to incorporate relaxation into my daily life)
Formal relaxation exercises (Progressive Muscle Relaxation, Mindfulness, Slow Diaphragmatic Breathing, Yoga):
____________________________________________________________________________________________
How often (days per week, time of day, etc.):___________________________________________________
Pleasure and Mastery (activities I enjoy, socializing, things I am good at): _______________________________
____________________________________________________________________________________________
Self-care (see the section on “Self-care” and write down examples that would improve your life): _____________
____________________________________________________________________________________________
Other soothing activities: ______________________________________________________________________
____________________________________________________________________________________________
Are there any aspects of my lifestyle (time management, too many projects, etc.) that increase my level of
tension and anxiety on a daily basis?
_____________________________________________________________________________________________
What could be modified? _______________________________________________________________________
How would my life improve if I incorporated some of the elements above into my daily life?
_____________________________________________________________________________________________
What is one thing I can do today or tomorrow to make a small step toward more relaxation in my daily life?
_____________________________________________________________________________________________
Use the following worksheet and design your own relaxation plan to begin incorporating relaxation skills into your
daily life. Be specific and come up with as many choices as you can imagine— remember that not all strategies will
“stick,” but in time you can find the ones that feel best to you. The only thing left to do is give them a try!
4.12

Relaxation strategies battle anxiety from the standpoint of the body. They are just one set
of exercises used in CBT.
We discussed what relaxation strategies are and how we can use them to help us battle
anxiety symptoms. We learned that relaxation strategies work best if they are practiced
over the long term, like exercise, to reduce muscle tension, slow down the pace of
breathing, and “slow down the mind.”
Relaxation strategies are not ultimately helpful as a way to reduce severe anxiety symptoms, such as panic, when these
symptoms arise. Relaxation skills are used in combination with the cognitive and behavioral skills discussed
throughout this manual. Cognitive therapy and exposure skills work to retrain the brain to have fewer anxiety triggers.
Relaxation exercises are not very effective at “retraining” these triggers, which is why they are not typically enough on
their own to teach the brain that it can let the “guard” down.
We discuss breathing skills. The most important element of breathing is slowing down the pace of the breath, which
takes practice, especially if anxiety is in the picture.
We introduced mindfulness skills, which are techniques that aim to “slow down the mind.” We
learn to see thoughts and feelings for what they are— thoughts and feelings—that come in and
out of our awareness. By allowing them to come and go without trying to “fix” them, we
communicate less urgency and more “calm” to the body.
There are many formal relaxation strategies, and each person may find something different that
works for them. The important thing is to find the strategies that work for you and practice them
consistently over time.
Some of the most relaxing activities are those that involve things we enjoy or are good at.
“Pleasure” and “mastery” feel good, so doing more of these things can only help! The anxiety
often gets in the way of some of these things, but avoiding pleasurable activities is likely to make
things worse. It is important to incorporate some of these activities into our daily lives on a regular
basis.
Finally, we review important elements of self-care, such as exercise, diet, and time management. It is
difficult, for example, to feel relaxed when we do not get enough sleep or are too busy. Slowing
down the pace of life and taking care of our bodies can help us feel more relaxed from day-to-day.
So now what?
So far we have discussed many of the skills used in CBT. Our final step is to learn how to put them all together and
manage anxiety over the long term. That’s what the next section, “Anxiety Management,” is all about. We’ll also learn
about the CBT treatment options that we offer here at U of M. It’s time to take your life back from anxiety by formally
starting your CBT treatment!
Progressive Muscle Relaxation (PMR) involves tensing and relaxing groups of muscles to learn to better understand
the difference between tension and relaxation. Through a program called Applied Relaxation, we can learn to do this
more and more quickly with practice.
4.13



Now that we’ve learned about many of the skills you’ll see in CBT, let’s talk about
how to put them all together. This section uses the analogy of a “tug of war” to
describe our battle with anxiety and stress over time. The information in this
section helps us approach treatment of anxiety in a realistic, effective way. This
especially applies to treatment of anxiety over long periods of time—periods in which
it is inevitable that we will experience stress of some sort or another.
We talk about the balance between risk and protection
that underlies each decision we make, and how these
decisions make us more or less vulnerable to anxiety. We
also spend time in this section discussing what “causes”
anxiety, the risk factors that make us more vulnerable to
it, including genetics and stress.
We briefly discuss some “other” CBT skills for anxiety,
problem solving and acceptance skills.
At the end of this section we also describe the CBT
treatment options available to you at the University of
Michigan Anxiety Disorders Clinic to help you with the
next steps in your journey to free yourself from anxiety.
5.1
“Courage is resistance to fear, mastery of fear—not absence of fear.”
~Mark Twain
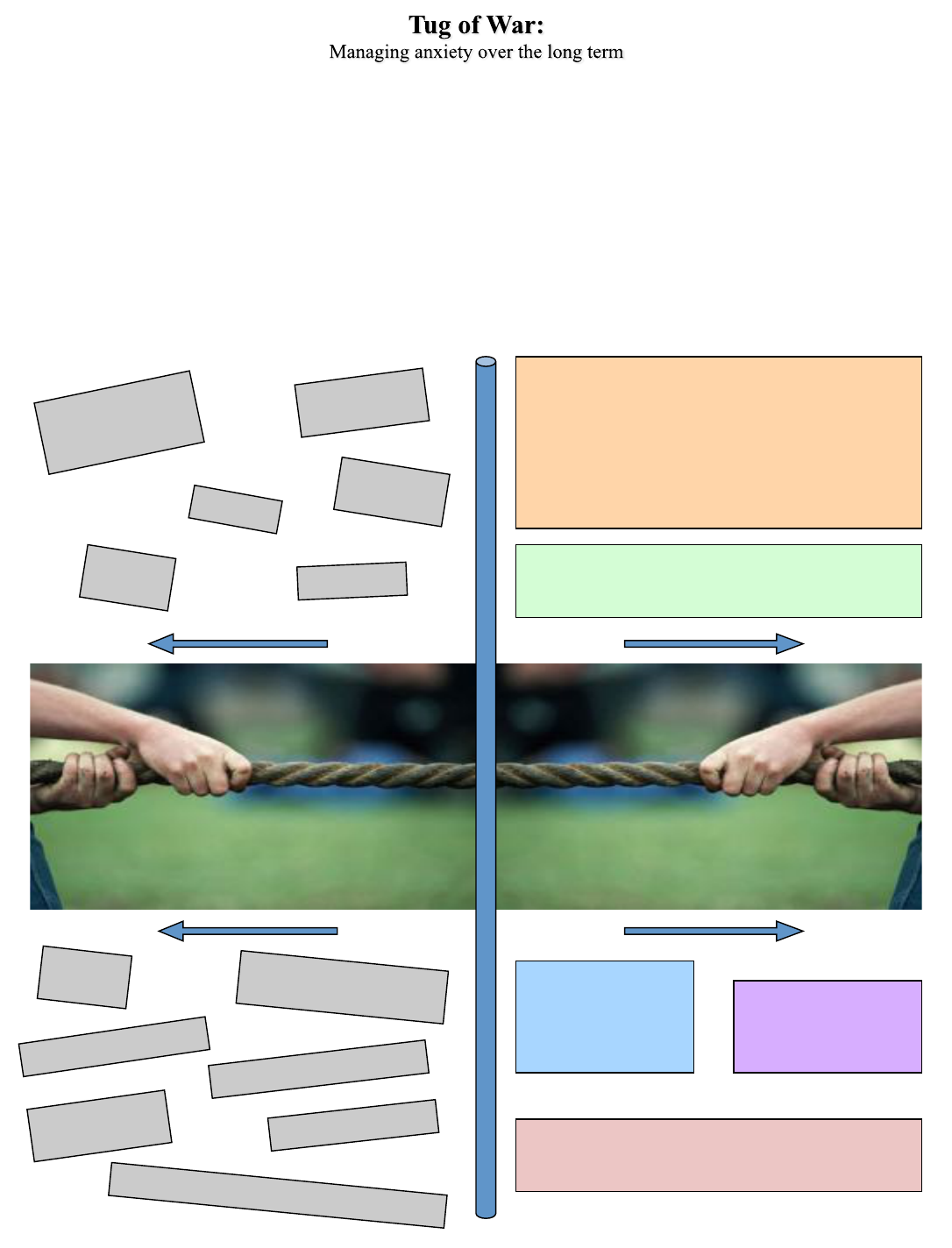
Use exposure skills to confront anxiety provoking
situations actively. Use Cognitive Therapy Skills to
understand a situation as realistically and in as detailed a
way as possible to determine how likely and how
dangerous a situation could be. These skills work to
“reprogram” the anxiety response and are the most
powerful CBT skills to change anxiety feelings in the
long run.
Think back to the last time you had a “tug of war” at a fair or on the beach. Your team has some influence on the outcome; but the
other team may (or may not…) make things hard for you to achieve your aim.
Managing anxiety over the long term can sometimes feel like a “tug of war.” Despite our attempts at creating a happy, comfortable
life, there is always the possibility that some “external stressor,” like an accident, job loss, or interpersonal conflict, could arise. One
important goal of CBT skills is to give us confidence that we can cope with these unexpected stressors when they happen.
The opponent in a game of “tug of war” is as integral to the game as stress is to our lives. And just as it is in the game, we can only
win if we participate. Participation in the game of life means accepting stress and finding ways to manage it to achieve our life aims.
The diagram below may help you to understand how to use CBT skills to assist you in your “tug of war” with stress.
To the left are stressors that are often outside of our control; on the right are the coping skills we need to keep the anxiety from
interfering with our life aims.
Practice relaxation skills regularly to address anxiety by
slowing down breathing, reducing muscle tension, and
quieting the mind.
Find ways to add
“pleasure” and
“mastery” to your
daily life. These are the
things we live for!
Take care of yourself!
Consider issues of self-
care to give the anxiety
less of an edge.
Accidents
Interpersonal
conflicts
Job loss
Genetics: Parents or
grandparents with
anxiety
Physical
Illness
Breakup of a relationship
Depressive episodes
“Positive” stressors such as
marriage, children
Big life
changes
Death of
loved ones
Financial stressors
Moving to a new
home
Post-partum anxiety or depression
Use problem solving skills to proactively address
problems you can control, and acceptance skills to let go
of things you can’t control.
5.2

“Tug of War,” continued
Another way to look at our battle with stress and anxiety is to try to balance a normal desire for protection with a hope of achieving
certain life aims. This may seem like an abstract concept, so let’s look at some specific examples of balancing risk with life aims.
Should I take the chance? Or…
How often do you drive or ride as a passenger in a car? Probably every day! Automobiles have
changed how we live our lives; they are convenient and help us achieve our life aims quickly and
efficiently. It is hard to imagine living without them.
Of course, driving or riding in a car involves some risk. According to the United States
Department of Transportation, there is a 1 in 84 chance of being killed in an automobile accident
at some point in our lives. So why do we take this risk?
It must be worth it to take this chance. We take the small risk of getting into an accident in order
to take advantage of the benefits automobile travel can afford us. Of course, the fact that it is
relatively unlikely certainly helps!
Every day we take risks to reach our life aims. While we probably aren’t noticing this process, we
have “pros and cons” playing in our head about most decisions we make. Check out the example
below:
Pros and Cons: Driving or riding in a car!
“Pros”
1. Get to destination faster!
2. Accomplish more of my goals each day: work, !
daily chores, fun and hobbies, etc.!
3. Increase number of activities that are available to !
me!
“Cons”
1. Small chance of getting hurt or killed in an !
accident!
1. Costs associated with driving (gas, repairs, !
etc.)!
Greater risks, fewer precautions, more freedom, better quality of life
Fewer risks, more precautions, less freedom
As the above example illustrates, our lives are filled with decisions about when to take risks and when to protect ourselves. Usually
we are trying to find a balance between protection and risk. We try to have as much as we can without increasing the chance of harm
too much. There are many options. Below, we illustrate this continuum and decisions we make that move us more toward risk (and
more freedom) or protection (and less freedom). It is our choice to decide how much risk to take most people try to find a reasonable
balance between risk and protection.
Drive with “reasonable safety
behaviors” in place (balance between
risk and protection:
- Drive safely: moderate speeds,
drive with the flow of traffic, etc.
-No multitasking while driving
-Keep car in good repair
-Take defensive driving classes
-Be careful when there is bad
weather
“These are the things I enjoy and I
won’t let anxiety take them from me.
It is worth taking that small chance
to have some of the things I want.”!
Drive with no concern for safety at all
(too much risk):
“There is no risk here; nothing bad
could happen to me. I don’t need
to be careful.”!
No driving at all (complete protection):
“It is best to be safe and prevent bad
things from happening at all costs.”!
“I would rather not do that if it is
going to make me feel anxious.” !
“I want to take all precautions to be
sure that everything will be OK.”!
5.3

“Tug of War,” continued
“I Want Control!”
Most of us work hard to maintain some control over our
lives: we plan, protect, and organize our lives so they are
more predictable and feel safer.
Nature or nurture? Revisited…
In the “Anxiety 101” section of this manual we briefly discussed the causes of anxiety. While there are many factors that lead to an
anxiety problem, we know that our vulnerability to anxiety is related to both “nature” and “nurture.” Nature is what we inherit from
our parents: our genetics. Nurture is life experiences. Risk factors (genetics or experiences that make one more “at risk” for
developing anxiety) are a mixture of these two basic elements. Below we list some of the most common risk factors for anxiety.
“Nurture” “Nature”
Learned patterns of cognitive inflexibility (rigid
thinking), such as extreme criticality or perfectionism
Early life experience:
Patterns of attachment with parents,
early life stress, traumatic experiences
early in life, etc.
Patterns of uncertainty in treatment by others:
Abuse or neglect during upbringing, moving frequently from area to area,
unpredictable parenting
Modeling from important elders/
authority figures:
learned protective behaviors, ideas about
what is/is not dangerous, etc.
Traumatic experiences: accidents, assault,
deaths of loved ones, near death experiences,
being attacked by an animal, etc.
Genetics: inherited
vulnerability to
physical and/or
mental illness
and
While there are some things in our lives that we can successfully control, there are other things that we cannot. In fact, we may find
that the more we try to control some things, the more this control eludes us.
One thing that is very hard to control completely is our body; sometimes it seems as if we experience a constant influx of pain,
anxiety, emotion, and thought. The truth about these automatic impulses is that we cannot completely control them, no matter how
hard we try. Once a thought comes into our head, it is there; once an emotion happens, it happens. As we have learned at times earlier
in this manual, trying to get rid of thoughts and feelings often makes them last longer or grow in intensity. However, our responses to
these impulses can influence how we experience the anxiety in the future. We use skills learned in CBT to influence the anxiety in this
way.
It is for this reason that in CBT we frame anxiety management as an effort to influence the anxiety, through skills and adaptive
responses to it, rather than to “control” it. Complete control is impossible, but at the least we can manage the symptoms of anxiety,
which are likely to come up from time to time. Look at the quotations below to further understand this difference.
Influence
“While my decisions have a part to play in how things
turn out, there are some things out of my control.”!
“I can’t prevent thoughts and feelings from happening,
but my responses to these impulses can influence how
I experience the anxiety in the future.”!
“Learning to cope with hardships is a part of life. I
can respond well to make it the ‘best case scenario’,
whatever happens.”
Control
“If I work hard enough, I can make things just right.”!
“I need to be sure everything will be safe at all costs.”!
“If there is even the slightest chance something bad could
happen I do not want to do it.”!
“I hope nothing bad happens today.”!
5.4

“Tug of War,” continued
Exercise #2: See the connection between stressful life events and anxiety/depression
Think about times in which you were particularly anxious or depressed an write them on the left. What external stressors were
going on at the time? Write those on the right. While our own anxiety sensitivity is one factor in developing an anxiety problem,
stress usually plays a role!
Time of life (e.g. “When I was 16”) External stressors (e.g. grandfather passed away)
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
“Tug of War” Take Home Points:
Managing anxiety over the long term can feel like a “tug of war;” as we have experienced stress in the past,
it is also likely to come up in the future. One important goal of CBT is to understand our vulnerability to
anxiety and use coping skills to offset this vulnerability.
We all have to find our own balance of “risk” versus “protection” to achieve our life aims. While we all
would like to be completely safe, there is always some risk in each decision we make. With CBT we learn
what risks are worth taking to reach our aims.
Exercise #1: “How I can balance my anxiety vulnerability with coping skills”
Vulnerability factors
(Check the ones that apply to you)
Genetics (family member with anxiety or depression)
Traumatic experiences (especially in early life)
Modeling of important elders/authority figures (how
we learn what is/is not dangerous)
Learned patterns of cognitive inflexibility (rigid
thinking such as extreme perfectionism)
Patterns of uncertainty in treatment by others (parents,
elders, etc.)
Skills I can use to manage anxiety and balance my
vulnerability
Exposure skills (confront anxiety to desensitize
triggers and achieve aims)
Cognitive skills (challenging negative automatic
thoughts)
Relaxation strategies (slow diaphragmatic breathing,
mindfulness meditation, Progressive Muscle Relaxation, etc.)
Self-care (exercise, diet, sleep, manage illnesses, limit
use of substances, etc.)
Mastery and Pleasure (time to enjoy activities, achieve
life aims)
Problem solving and acceptance skills (adaptively address
problems and accept things we cannot control
5.5

When a problem arises, there many possible responses. As we have discussed throughout this manual, some
responses to anxiety and problems can help to solve these problems; others can serve to make things worse.
Below we describe three ways of addressing a problem. One approach may work best, or all three may apply.
The “take home point” here is that all situations are different, and require different types of approaches to help
you meet your life aims.
Adaptive Response #1: Problem solving (actions/behaviors)
Sometimes the best answer to a problem is working to “solve” the problem somehow
—it is not a problem with our thinking or behavior, it is a problem with the external
circumstances. For example, if someone is consistently aggressive or abusive of us,
we may want to find a way to set firm limits with that person or leave the relationship
altogether. There are many problem solving skills, some of which are outlined below:
-Exposure skills to address avoidance
-Assertively address interpersonal conflicts
-Take small steps to make progress on long-term projects
-Plan for the future
-Manage your time effectively
-many others…
Talk to your therapist or group leader about other behavioral skills to directly address
problems that arise.
Adaptive Response #2: Get the facts (thinking)
Use cognitive skills to better understand the “facts” of a situation. Perhaps there is a
problem, and perhaps there is not. Sometimes the first step is to understand the facts
of a situation, and then decide whether or not to use problem solving skills (above) or
accept things that are outside of our control (below). See the section on “Cognitive
Therapy Skills.”
Adaptive Response #3: Accept what cannot be controlled (letting go)
There are times that we believe we should be able to control something, yet our
consistent attempts to do so are met with failure. This “beating a dead horse”
makes us more and more frustrated, angry, anxious, and depressed. Sometimes
letting go of things we cannot control is necessary to prevent problems from
getting even worse; we also lift some of the burden of failing over and over.
How to take
action to solve a
problem
1. Write down clearly what
the problem is.
2. Brainstorm about ways
to solve the problem, even
“ridiculous” ways, writing
down all possibilities.
3. Rank the possible
solutions in order, from
best to worst. Think “how
likely is it for this approach
to work?”
4. Decide on a plan of
action for each reasonable
solution. Rate how
probable it would be each
each plan to work.
5. Pick the most reasonable
plan and put the plan into
action. If it doesn’t work,
go to the next best solution
and try that one. Continue
to try until you solve the
problem.
How do I know what to do to make it better?
Sometimes it is difficult to know which approach to take to make a situation better. While it is ultimately an
individual decision, one that may take trial and error, therapy is a place to work out some of these difficult
choices. The various skills in CBT are meant to help us get some clarity around some of these decisions.
While we don’t have room in this manual to discuss in detail how to make these decisions, this is something
to discuss with your group or individual therapist as you move through treatment.
5.6

Cognitive-Behavioral Therapy is an effective, evidence-based treatment that has been proven to have an impact on
anxiety in both the short and long term. Our clinic specializes in delivery of this intervention to people like you, who
want anxiety to stop interfering with their lives. Below we explain some of what to expect from CBT treatment.
Cognitive Behavioral Therapy…
…is regular. It works best when you come to treatment once per week for most of the treatment course. It is
common to go to once every other week or once a month once the symptoms have been reduced and you have
entered the “maintenance” period of treatment.
…typically lasts for between 12 and 16 sessions. Depending on the problem, it may take more or less. This is
not a treatment that is meant to last for significant amounts of time.
…is structured. This is not the style of therapy in which one comes into the session only to “vent” or have
someone with whom to talk. The treatment is focused specifically on treatment aims, which usually include
reducing the impact of anxiety on our lives and feeling better, by learning skills and techniques to respond to
anxiety when it arises.
…has a variety of skills. As you may have noticed from this manual, there are different ways to manage an
anxiety problem. Most people find it helpful to use a variety of skills, instead of searching for just one “silver
bullet.” There is most likely not just one answer to your anxiety problem. However, the anxiety symptoms can
usually be managed well if one practices multiple skills repetitively over time and incorporates them into the
flow of daily life.
…requires practice. Call it homework, daily practice, or whatever you choose. Regardless, it takes daily
repetition to learn skills and retrain one’s anxiety response. A rule of thumb is to expect to spend about one hour
a day practicing CBT in between sessions. We want you to feel better outside of sessions and after you finish
treatment, not just while you are at our clinic.
…depends on follow-through. The most important factor in whether or not treatment works is the amount of
work you put into it. Consider it an investment in a future with more freedom and flexibility.
…is collaborative. Individual and group CBT are structured, but are also centered around your life aims. The
patient and therapist work together to define treatment targets, adapt skills to the patient’s unique circumstances,
and troubleshoot as barriers arise. If certain skills do not work, it is common to try others. If something does not
seem to be working, one can discuss this with the therapist or group leader. Communication is an important part
of CBT.
On the next page we discuss the different treatment options at this
clinic to continue with CBT once you finish the basic group.
…is evidence-based. This means that the concepts and skills are based on scientifically-validated concepts, and
the interventions have been tested to be sure they are helpful.
5.7

CBT Treatment in the University of Michigan Anxiety Disorders Clinic, con.
Option 1: Cognitive-Behavioral Therapy Treatment Groups
A popular option for the next step in treatment is our CBT Treatment Groups, which takes the skills we discussed in the Basic Group one
step further. These groups focus on the two main skill sets of CBT, Exposure and Desensitization and Cognitive Therapy Skills. Individuals
that take part in these groups are asked to share with the group their treatment targets and anxiety triggers, while designing cognitive and
behavioral interventions to address specific problems. Patients are expected to practice skills in between sessions.
Each group meets for one month of weekly sessions at a time, and the two groups alternate months. For example, the Exposure group may
meet in January for four sessions, and the Cognitive Therapy Skills group meets in February for the same amount. This pattern repeats. If a
patient wishes to take part in both groups they may, and they are encouraged to repeat groups to get more experience and practice with CBT
skills.
The Exposure and Desensitization groups are ideal for patients with panic disorder, agoraphobia, social anxiety, obsessive-compulsive
disorder, and specific phobias. Patients with generalized anxiety disorder are encouraged to attend this group, but may find the most benefit
from the Cognitive Therapy Skills group.
The Cognitive Therapy Skills group is ideal for chronic worry, generalized anxiety disorder, social anxiety, panic disorder, and specific
phobias. Patients with Obsessive-Compulsive Disorder (OCD) may find this group helpful, but the primary mode of treatment for OCD is
exposure.
Patients with a primary diagnosis of Post-Traumatic Stress Disorder (PTSD) are encouraged to pursue individual therapy, which typically
involves an exposure-based mode of treatment called Prolonged Exposure for PTSD. Talk to your referring clinician or group leader about
this option if you are interested.
Option 2: Individual Cognitive Behavioral Therapy
If treatment groups are not the best option for you, another option is individual therapy. Individual CBT therapy is recommended if you
cannot attend the CBT Treatment Groups due to a schedule conflict. Also, some anxiety problems are best treated in individual therapy. If
you have a question about whether to attend groups or individual therapy, talk to your CBT Basic Group leader or the clinician that referred
you to the group. If it is determined that individual therapy would be most helpful for you, we will discuss your case in the Anxiety Team
Meeting on the following Monday and get back to you with our recommendations and referral options.
Option 3: Some other form of psychotherapy
CBT is not for everyone. If after you complete this group you realize that you are not interested in group or individual CBT, talk to your
referring clinician about other therapy options. Some of these options include group and individual therapy aimed at addressing such
problems as relationship issues, depression, and Bipolar Disorder. Whatever your problem, the best option is to discuss what you are
looking for with the clinician that worked with you at your initial evaluation. You can also ask your Basic Group Leader for advice about
this. For some, we recommend a one-session “therapy evaluation” with an experienced clinician to help make decisions about the next steps
in treatment with us.
What about medication?
Research suggests that the most effective treatments for anxiety often involve a combination of therapy with some sort of psychotropic
medication, usually an antidepressant. Sometimes a medication can be helpful in reducing some of the most painful anxiety symptoms in
order for a patient to better take advantage of therapy. That being said, medication is not typically a “cure” by itself, but can be used in
combination with other forms of treatment to manage anxiety. Your psychiatrist or nurse practitioner is the expert on this subject. If you
have not had a medication evaluation, you can tell the person who referred you to this group or your group leader that you are interested in
exploring this option. Just let us know!
What do I do after the CBT Basic Group for Anxiety?
Option 4: Individual therapy evaluation
For some, especially anyone that is confused about which direction to go with their treatment, we recommend a one-session “therapy
evaluation” with an experienced clinician to help make decisions about the next steps in treatment with us. Let us know if you are interested
in this option.
5.8

Congratulations on finishing the CBT Basic Group for Anxiety! We hope the group was
helpful in explaining the basics of CBT and preparing you for the next steps in your
treatment. Please let us know if there is anything we can do to help you with these next
steps in treatment.
Your understanding of the material in this manual before the next steps of treatment will
enhance your response to CBT treatment. If you haven’t already, try some of the
exercises in the manual to further clarify you treatment aims and start seeing how these
skills may be helpful for you.
Also, see the “Resources” section for further reading and other media on anxiety and
CBT.
Good luck with your treatment!
5.9



Appendix I!
The Biology of “Fight or Flight”
6.1

Comprehensive Self-help Workbooks for All Anxiety Disorders:
Bourne, Edmund: The Anxiety & Phobia Workbook (Fourth Edition)
Bourne, Edmund: Coping with Anxiety: 10 Simple Ways to Relieve Anxiety, Fear & Worry
Burns, David: When Panic Attacks: The New Drug-Free Anxiety Therapy That Can Change Your
Life
Davis, McKay, Eshelman: The Relaxation and Stress Reduction Workbook
Farchione, Fairholme, Ellard, Barlow, Boisseau, Allen, May: Unified Protocol for Transdiagnostic
Treatment of Emotional Disorders (workbook) from the “Treatments That
Work” series
Ramirez-Basco, Monica: Never Good Enough: How to Use Perfectionism to Your Advantage
Without Letting it Ruin Your Life
Smits, Jasper and Otto, Michael: Exercise for Mood and Anxiety Disorders
Otto, Pollack, Barlow: Stopping Anxiety Medication: Panic Control Therapy for Benzodiazepine
Discontinuation
Generalized Anxiety Disorder
Craske, Michelle and Barlow, David: Mastery of Your Anxiety and Worry (workbook) from the
“Treatments That Work” series
Brantley, Jeffrey: Calming Your Anxious Mind: How Mindfulness and Compassion Can Free You
from Anxiety, Fear, and Panic
Davis, McKay, Eshelman: The Relaxation and Stress Reduction Workbook
Ramirez-Basco, Monica: Never Good Enough: How to Use Perfectionism to Your Advantage
Without Letting it Ruin Your Life
Benson, Herbert and Proctor, William: Relaxation Revolution: Enhancing Your Personal Health
Through the Science & Genetics of Mind Body Healing
Lackner, Jeffrey: Controlling IBS the Drug-free Way: A 10-step Plan for Symptom Relief
Social Anxiety Disorder
Hope, Heimberg, Turk: Managing Social
Anxiety (workbook) from the “Treatments
That Work” series
Rapee, Ronald: Overcoming Shyness and Social
Phobia: A Step-by-Step Guide
Markway, Carmin, Pollard, & Flynn: Dying of
Embarrassment
Antony, Martin and Swinson, Richard: The
Shyness and Social Anxiety Workbook:
Proven, Step-by-Step Techniques for
Overcoming Your Fear
Erika Hilliard: Living Fully With Shyness and
Social Anxiety: A Comprehensive Guide to
Gaining Social Confidence
Soifer, Zqourides, Himle, Pickering: Shy
Bladder Syndrome: Your Step-by-Step Guide
to Overcoming Paruresis
Fine, Debra: The Fine Art of Small Talk
Obsessive-Compulsive
Disorder
Hyman, Bruce and Pedrick, Cherry: The
OCD Workbook: Your Guide to Breaking Free
from Obsessive-Compulsive Disorder
Foa, Edna and Kozak, Michael: Mastery of
Obsessive-Compulsive Disorder: A Cognitive-
Behavioral Approach (workbook) from the
“Treatments That Work” series
Panic Disorder and
Agoraphobia
Barlow, David and Craske, Michelle: Mastery
of Your Anxiety and Panic (workbook)
from the “Treatments That Work” series
Carbonell, David: Panic Attacks Workbook: A
Guided Program for Beating the Panic Trick
Wilson, Reid: Don’t Panic: Taking Control of
Anxiety Attacks (3
rd
Edition)
Post-Traumatic Stress Disorder
Foa, Edna: Reclaiming Your Life From a Traumatic Experience (workbook) from the “Treatments
That Work” series
Hickling, Edward, and Blanchard, Edward: Overcoming the Trauma of Your Motor Vehicle
Accident (workbook) from the “Treatments That Work” series
Olasov, Barbara and Foa, Edna: Reclaiming Your Life After Rape: Cognitive-Behavioral Therapy
for Posttraumatic Stress Disorder (workbook) from the “Treatments That Work” series
Williams, Mary Beth and Poijula, Soili: The PTSD Workbook: Simple, Effective Techniques for
Overcoming Traumatic Stress Symptoms
Follette, Victoria and Pistorello, Jacqueline: Finding Life Beyond Trauma: Using Acceptance and
Commitment Therapy to Heal from Post-Traumatic Stress and Trauma-Related Problems
U.S Department of Health and Human Services: Directory of Services and Resources for
Survivors of Torture
Specific Phobias
Antony, Craske, and Barlow: Mastering Your
Fears and Phobias (workbook) from the
“Treatments That Work” series
Ridley, Layne: White Knuckles: Overcoming
the Fear of Flying
Brown, Duane: Flying Without Fear: Effective
Strategies to Get Your Where You Need to
Go
6.2

Body Dysmorphic Disorder
Claiborn, James and Pedrick, Cherry: The BDD Workbook
Impulse Control Disorders:
(Trichotillomania (compulsive hair pulling), skin picking, pathological gambling, compulsive stealing, pyromania/fire setting,
compulsive buying)
Penzel, Fred: The Hair-Pulling Problem: A Complete Guide to Trichotillomania
Grant, Donahue, Odlaug: Overcoming Impulse Control Problems (workbook) from the “Treatments That Work” series
Ladouceur, Robert, and Lachance, Stella: Overcoming Your Pathological Gambling (workbook) from the “Treatments That Work” series
Woods, Douglas, and Twohig, Michael: Trichotillomania: An ACT-enhanced Behavior Therapy Approach (workbook) from the
“Treatments That Work” series
Shulman, Terrence: Something for Nothing: Shoplifting Addiction and Recovery
Attention Deficit/Hyperactivity Disorder (ADHD) in Adults
Sprich, Safren, Perlman, Otto: Mastering Your Adult ADHD (workbook) from the “Treatments That Work” series
Depression and Bipolar Disorder
Burns, David: Feeling Good: The New Mood Therapy
Burns, David: The Feeling Good Handbook
Gilson, Freeman, Yates, Freeman: Overcoming Depression (workbook) from the “Treatments That Work” series
Otto, Reilly-Harrington, Knauz, Henin, Kogan, Sachs: Managing Bipolar Disorder (workbook) from the “Treatments That Work”
series
Rohan, Kelly: Coping with the Seasons: A Cognitive-Behavioral Approach to Seasonal Affective Disorder (workbook) from the “Treatments
That Work” series
Williams, Teasdale, Segal, and Kabat-Zinn: The Mindful Way Through Depression: Freeing Yourself From Chronic Unhappiness
Hoarding
Neziroglu, Bubrick, & Yaryura-Tobias: Overcoming Compulsive Hoarding: Why You Save & How You Can Stop
Steketee, Gail, and Frost, Randy: Compulsive Hoarding and Acquiring (workbook) from the “Treatments That Work” series
Tolin, Frost, Steketee: Buried in Treasures: Help for Compulsive Acquiring, Saving, and Hoarding
Frost, Randy and Steketee, Gail: Stuff
Health Worries/Hypochondriasis
Asmundson, Gordon J.G. and Taylor, Steven:
It’s Not All in Your Head: How Worrying
About Your Health Could Be Making You
Sick– and What You Can Do About It
6.3

Anxiety Disorder Foundations and Associations
Anxiety Disorders Association of America: www.adaa.org
Obsessive-Compulsive Foundation: www.ocfoundation.org
Agoraphobics in Motion: www.aim-hq.org
Social Phobia/Social Anxiety Association: http://www.socialphobia.org/
Social Anxiety Institute: http://www.socialanxietyinstitute.org
Posttraumatic Stress Disorder Association: http://www.ptsdassociation.com
African American Post Traumatic Stress Disorder Association: http://www.aaptsdassn.org
Heal My PTSD, LLC: http://healmyptsd.com
Support Groups in Michigan
Obsessive-Compulsive Disorder
Ann Arbor OCD Support Group
1st Thursday of each month 1:00-2:30
Community Support & Treatment Services
(CSTS)
2140 E. Ellsworth Rd., Ann Arbor, MI
Contact Jim: 734-477-0326, [email protected]
OR
Jeannie at 734-761-4629,
Depression and bipolar
Support Groups for patients and families of persons
with depression or bipolar disorder
UM Depression Center, Rachel Upjohn Building,
4250 Plymouth Rd., Ann Arbor
2
nd
and 4
th
Wednesdays of each month,
7:00pm-8:15pm
Listing of other Michigan Support Groups:
http://www.anxietypanic.com/michigan.htm
Books on Anxiety Disorders (informational)
Anxiety Disorders and Mental Health (general)
Ross, Jeriyln and Carter, Rosalynn: Triumph Over Fear: A Book of Help and Hope for People with
Anxiety, Panic Attacks, and Phobias
Schwartz, Jeffrey and Begley, Sharon: The Mind and the Brain: Neuroplasticity and the Power of
Mental Force
Obsessive Compulsive Disorder
Osborn, Ian: Tormenting Thoughts and Secret Rituals
Baer, Lee: The Imp of the Mind: The Silent Epidemic of Obsessive Bad Thoughts
Posttraumatic Stress Disorder
Phillips, Suzanne and Kane, Dianne: Healing Together: A Couple’s Guide to Coping with Trauma
and Post-traumatic Stress
Orange, Cynthia: Shock Waves: A Practical Guide to Living with a Loved One’s PTSD
Paulson, Daryl and Krippner, Stanley: Haunted by Combat: Understanding PTSD in War
Veterans Including Women, Reservists, and Those Coming Back from Iraq
Judith Herman: Trauma and Recovery
Body Dysmorphic Disorder
Phillips, Katharine: The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder
Social Phobia
Swiggett, Chelsea Rae: My True Story of Fear, Anxiety and Social Phobia (Louder Than Words)
Cunningham, Terry: The Hell of Social Phobia: One Man’s 40 Year Struggle
Panic Disorder
Berman, Carol: 100 Questions and Answers about Panic Disorder (2
nd
Edition)
Books on Mindfulness
Kabat-Zinn, Jon: Full Catastrophe Living:
Using the Wisdom of Your Body and Mind
to Face Stress, Pain and Illness.
Williams, Teasdale, Segal, and Kabat-
Zinn: The Mindful Way Through
Depression: Freeing Yourself From Chronic
Unhappiness
Other Mental Health Resources
General
National Alliance on Mental Illness (NAMI): http://www.nami.org/
Treatments That Work: http://www.oup.com/us/companion.websites/umbrella/treatments/?view=usa
Michigan Mental Health Networker: http://www.mhweb.org/
Hoarding
Children of Hoarders: http://childrenofhoarders.com/wordpress/
Washtenaw County Hoarding Task Force
Info: http://www.hoardingtaskforce.org/taskforces/the-hoarding-task-force-of-washtenaw-county
Contact: Harriet Balakar at 734-998-9355
Social Anxiety Disorder
Toastmasters: http://www.toastmasters.org/
University of Michigan Anxiety
Disorders Clinic, Department of
Psychiatry, Rachel Upjohn Building
4250 Plymouth Road, Ann Arbor, MI
48109; Phone: 734-764-0231; http://
www.psych.med.umich.edu/anxiety/
clinic.asp
6.4

Generalized Anxiety Disorder
Sections to review, in order of importance:
1. Anxiety 101
2. Cognitive Therapy Skills
3. Relaxation
4. Anxiety Management
5. Exposure
Panic Disorder with Agoraphobia
Sections to review, in order of importance:
1. Anxiety 101
2. Cognitive Therapy Skills
3. Exposure
4. Anxiety Management
5. Relaxation
Social Anxiety Disorder
Sections to review, in order of importance:
1. Anxiety 101
2. Cognitive Therapy Skills
3. Exposure
4. Relaxation
5. Anxiety Management
Posttraumatic Stress Disorder
Sections to review, in order of importance:
1. Anxiety 101
2. Exposure
3. Cognitive Therapy Skills
4. Relaxation
5. Anxiety Management
Obsessive-Compulsive Disorder
Sections to review, in order of importance:
1. Anxiety 101
2. Exposure
3. Cognitive Therapy Skills
4. Anxiety Management
5. Relaxation
Wondering where to start? We know this is a lot of information to consume at once, so refer to the information
below to focus your reading on the specific problems with which you are dealing.
Specific Phobias
Sections to review, in order of importance:
1. Anxiety 101
2. Cognitive Therapy Skills
3. Exposure
4. Relaxation
5. Anxiety Management
6.5

Some people ask themselves “is it worth it to put in some hard work to get my anxiety under control?” This is a personal
choice, and everyone has different reasons for working on their anxiety. One way to help answer this question is to examine
different parts of your life and how the anxiety impacts them.
6.6
First, let’s make a list of the different parts of your life that are important to you. Some examples are below.
Areas of my life that are important to me are: How important (0-10)
1. ___________________________________ _________
2. ___________________________________ _________
3. ___________________________________ _________
4. __________________________________ _________
5. __________________________________ _________
6. __________________________________ _________
7. __________________________________ _________
8. __________________________________ _________
9. __________________________________ _________
Sample important life areas:
Family
Friends
Social life
Work/career
School
Leisure
Hobbies
Spirituality/religion
Volunteering/giving back
Physical health
Mental health
Free time
Others…
Life area: How anxiety interferes with my goals in this area:
_________________ ___________________________________________________________________________
_________________ ___________________________________________________________________________
_________________ ___________________________________________________________________________
_________________ ___________________________________________________________________________
_________________ ___________________________________________________________________________
_________________ ___________________________________________________________________________
_________________ ___________________________________________________________________________
_________________ ___________________________________________________________________________
_________________ ___________________________________________________________________________
_________________ ___________________________________________________________________________
_________________ ___________________________________________________________________________

Blank page!
Remember to tear out this page after you have filled out the “Anxiety Inconvenience Review Form” and
put it somewhere you can see it easily as you go through your day.


Exposure Tracking Example
Exposure task: Performing my presentation for friends !
Length of time SUDS (0-100)
Day/Date Start Stop Beginning Middle End Comments
4/15 10:15 am 11:15 am 5 8 4!
4/16 2:00 pm 3:00 pm 3 8 3!
4/17 5:30 pm 6:30 pm 1 9 4 Lost train of thought!
4/18 5:30 pm 6:30 pm 1 5 2!
4/19 10:00 am 11:00 am 0 4 1!
4/20 6:00 pm 7:00 pm 0 3 1!
4/21 10:15 am 11:15 am 0 2 .5!
Subjective Units of Distress Scale (SUDS)
0= no anxiety at all; completely calm
3= some anxiety, but manageable
5= getting tough; wouldn’t want to
have it all the time
7-8= severe anxiety that interferes with
daily life
10 = worst anxiety you’ve ever felt
Length of time * SUDS (0-10)
Day/Date Start Stop Beginning Middle End Comments
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
Exposure task: _____________________________________________________
Amount of time each day and how often:________________________________
Safety behaviors or rituals to eliminate: ________________________________
___________________________________________________________________
Other guidelines:____________________________________________________

Exposure Tracking Example
Exposure task: Performing my presentation for friends !
Length of time SUDS (0-100)
Day/Date Start Stop Beginning Middle End Comments
4/15 10:15 am 11:15 am 5 8 4!
4/16 2:00 pm 3:00 pm 3 8 3!
4/17 5:30 pm 6:30 pm 1 9 4 Lost train of thought!
4/18 5:30 pm 6:30 pm 1 5 2!
4/19 10:00 am 11:00 am 0 4 1!
4/20 6:00 pm 7:00 pm 0 3 1!
4/21 10:15 am 11:15 am 0 2 .5!
Subjective Units of Distress Scale (SUDS)
0= no anxiety at all; completely calm
3= some anxiety, but manageable
5= getting tough; wouldn’t want to
have it all the time
7-8= severe anxiety that interferes with
daily life
10 = worst anxiety you’ve ever felt
Length of time * SUDS (0-10)
Day/Date Start Stop Beginning Middle End Comments
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
Exposure task: _____________________________________________________
Amount of time each day and how often:________________________________
Safety behaviors or rituals to eliminate: ________________________________
___________________________________________________________________
Other guidelines:____________________________________________________

Possible
Distortion(s) Thought Rational Responses
Take thoughts identified using
techniques in the “Identifying
Negative Automatic Thoughts”
section and write them here.
Use what you learned in the
“Cognitive Distortions” section to
identify any possible thought
patterns.
Gather evidence for and against
your negative automatic thoughts
using multiple “lines of evidence.”
Tips:
-Remember to phrase each thought in the form of a statement.
-You should have between 7 and 10 facts in the “rational response” column for each thought.
-Copy this page to use for other thoughts (some extra pages are included at the end of the manual).
-Carry it with you and bring it out each time you have the thought, to remind yourself of the facts.
Thought
Possible
Distortion(s) Rational Responses
1.
2.
3.
4.
5.
6.
7.
8.
9.
1.
2.
3.
4.
5.
6.
7.
8.
9.
52

Possible
Distortion(s) Thought Rational Responses
Take thoughts identified using
techniques in the “Identifying
Negative Automatic Thoughts”
section and write them here.
Use what you learned in the
“Cognitive Distortions” section to
identify any possible thought
patterns.
Gather evidence for and against
your negative automatic thoughts
using multiple “lines of evidence.”
Tips:
-Remember to phrase each thought in the form of a statement.
-You should have between 7 and 10 facts in the “rational response” column for each thought.
-Copy this page to use for other thoughts (some extra pages are included at the end of the manual).
-Carry it with you and bring it out each time you have the thought, to remind yourself of the facts.
Thought
Possible
Distortion(s) Rational Responses
1.
2.
3.
4.
5.
6.
7.
8.
9.
1.
2.
3.
4.
5.
6.
7.
8.
9.
52

Possible
Distortion(s) Thought Rational Responses
Take thoughts identified using
techniques in the “Identifying
Negative Automatic Thoughts”
section and write them here.
Use what you learned in the
“Cognitive Distortions” section to
identify any possible thought
patterns.
Gather evidence for and against
your negative automatic thoughts
using multiple “lines of evidence.”
Tips:
-Remember to phrase each thought in the form of a statement.
-You should have between 7 and 10 facts in the “rational response” column for each thought.
-Copy this page to use for other thoughts (some extra pages are included at the end of the manual).
-Carry it with you and bring it out each time you have the thought, to remind yourself of the facts.
Thought
Possible
Distortion(s) Rational Responses
1.
2.
3.
4.
5.
6.
7.
8.
9.
1.
2.
3.
4.
5.
6.
7.
8.
9.
52




