
EMPLOYEE
BENEFITS
GUIDEBOOK
Bee Ready to...
Review and Select
Your Benets
2
Superintendent's Message
ALEX® Helps You Pick Your Benefit Plans
MEET ALEX, YOUR PERSONALIZED VIRTUAL BENEFITS
COUNSELOR!
If you want to find that perfect plan, or you have
questions about how your insurance works, you can get
help from your online benefits counselor, ALEX:
Here are three important things to know about the
ALEX tool:
1. It’s personalized, so you can see which plan makes
the most sense for YOU, not your coworkers, or your
boss, or even me, your local benefits genius.
2. It’s fun to use. There’s no boring insurance jargon, or
complicated legal jibber-jabber.
3. It’s confidential, so you can get the guidance you
need without revealing all of your fascinating
secrets.
You can discover your lowest-cost, best-coverage 2024
health plan option - or see if your current plan choice is
still the best one for you - from any computer, tablet, or
smartphone.
Find the plan best for you at: myalex.com/pbcsd/2024
Dear District Employees,
Please review the information included in this benefits
reference guide. We’ve compiled all the information about
benefits available to you as an employee of Palm Beach
County School District into this guide.
MEDICAL
The District provides subsidized medical insurance coverage
to our full-time employees. Premiums start as low as $70 per
month for employee-only coverage. You may also purchase
coverage for your children, spouse, or domestic partner. We
oer options and are confident you will find a plan that meets
your needs and budget.
HEALTH REWARDS PROGRAM
Our award winning Health Rewards Program is one of many
wellness related programs oered to encourage a healthy
lifestyle. The Health Rewards Program encourages you to
be actively engaged in your health and well-being. For your
eorts, you are rewarded with up to $600. Be sure to read
the section titled Health Rewards for more information. What
can you do RIGHT NOW to improve the future you? Join our
culture of health!
TERM LIFE
Basic term life in the amount of $20,000 is provided to you as
a full-time employee.
DENTAL, VISION, LIFE & DISABILITY
Dental, Vision, additional Term Life Insurance, and Disability
are optional benefits you may wish to review and decide if
they are right for you.
SPENDING ACCOUNTS
We oer spending accounts including, Flexible Spending
(Health) Accounts to compliment your enrollment in our
HMO plans. We oer a Health Savings Account (HSA), to
complement your enrollment in the Consumer Driven Health
Plan (CDHP). These tax-free programs allow you to put money
aside from your paycheck and use those funds to oset
eligible health care expenses.
We oer Dependent Care FSA, a pre-tax benefit, to help you
set funds aside for before school, afterschool, daycare, day
camps, or elder day care needs. You save money because
you never have to pay FICA or income tax on these monies.
RETIREMENT PLANS
In addition to the Florida Retirement System (FRS) plans that
you contribute 3 percent of your pay, you are eligible to enroll
in a 403(b) or 457 plan. We oer both tax-deferred and ROTH
accounts. If you start saving now, the funds will grow and you
will be glad you participated at retirement time. Choose from
a preselected list of vendors and enroll today. Plan B allows
you to enroll while you are enrolling for your other benefits,
and get started saving right away.
Sincerely,
Mike Burke, Superintendent
School District of Palm Beach County Non-
Discrimination Statement
The School Board of Palm Beach County, Florida, prohibits
discrimination in admission to or access to, or employment in
its programs and activities, on the basis of race, color, national
origin, sex or sexual orientation, marital status, age, religion,
disability, genetic information, gender identity or expression, or
any other characteristic prohibited by law. The School Board also
provides equal access to the Boy Scouts and other designated
youth groups. The School District of Palm Beach County oers
the following career and technical programs, including career
academies wherein students may earn industry certification,
visit the Programs of Study page for more information as well
as a list of classes. Lack of English language skills will not be a
barrier to admission and participation. The district may assess
each student’s ability to benefit from specific programs through
placement tests and counseling, and, if necessary, will provide
services or referrals to better prepare students for successful
participation.

Connect With Us
Benefits Directory 4
Eligibility Requirements 5
Dependent Verification Guide 7
Domestic Partnership 8
Important Enrollment Information 9
How to Enroll 12
Employee Responsibilities 13
Contribution Overview 14
Changing Your Coverage 15
Leave of Absence Benefits 17
Other Leave Coverage 18
Coverage Termination 20
Retirement or Separation 21
Health Rewards Credit 22
District Onsite Clinic 23
Medical Plan Cost 24
Medical Plans 25
Healthcare Doctors 32
Pharmacy Benefits 34
Dental Benefits 37
Vision Benefits 42
Employee Wellness 47
Wellness Services 48
Flexible Spending Accounts (FSAs) 49
Health Care FSA 51
Dependent Care FSA 52
Accessing FSA Benefits 53
Special Retirement Plan 54
Disability Income Protection 55
Basic Life Insurance 61
Group Term Life Insurance 62
Retirement Investment Plans 66
ID Theft Protection Plan 67
Special Benefits from Trustmark 68
COBRA Notification 70
Beyond Your Benefits 73
Medicare Part D 74
PeopleSoft “My Homepage” 75
Appeals Process 76
Table of Contents
If you (and/or your dependents)
have Medicare or will become eligible
for Medicare in the next 12 months,
a Federal law gives you more choices
about your prescription drug coverage.
Please see page 74 for more details.

4
Benefits Directory
The School District of
Palm Beach County
Risk & Benefits Management
Phone: 561-434-8580
Fax: 561-434-8103
www.hub.palmbeachschools.org/
all_employees/benefits
Medical & Pharmacy
Insurance
UnitedHealthcare® (UHC)
Group #: 704471
www.myuhc.com
Member Services
(888) 380-0389
Dedicated Onsite Service Account
Managers:
A-K: (561) 434-8092
L-Z: (561) 357-7564
Nurse Liaison: Mireille Pierre-Louis, RN,
BSN, CCM. MSN
(561) 434-7417
Telephone-based Coaching Program
(800) 478-1057
Diabetes Health Plan
1 (888) 380-0389
Real Appeal
(844) 344-REAL (7325)
www.member.realappeal.com
Dental Insurance
Humana
Group #: 830206
(800) 233-4013 DHMO & PPO Plans
myhumana.com
Dental Provider Search
- DHMO - http://l.sdpc.net/me0w5
- PPO - http://l.sdpbc.net/rcb7o
Vision Plan
EyeMed Vision Care
Group #: 9705435
Provider Locator
(866) 299-1358
www.eyemed.com
Customer Service
(866) 723-0514
www.eyemed.com
Disability Claims Call Center
Metropolitan Life Insurance Company
(MetLife)
Group #: 106456-1-G
(800) 300-4296
www.MetLife.com/MyBenefits
Life, Statement of Health and
Disability
Metropolitan Life Insurance Company
(MetLife)
Group #: 106456-1-G
(800) 638-6420
www.MetLife.com/MyBenefits
Spending Accounts
Health Savings Account (HSA)
Optum Bank Customer Care
(800) 791-9361
Flexible Spending Accounts
TASC Customer Service
Mon - Fri, 8 a.m. - 5 p.m. ET
(800) 422-4661
TASC Flexible
Spending Account Claims
Mon - Fri, 8 a.m. - 5 p.m. ET
(800) 422-4661
District Onsite Clinic
3300 Forest Hill Blvd
Building E
West Palm Beach, FL 33406
(Rear of Fulton-Holland)
Clinic Hours
Mon, Wed, Fri: 7 am to 6 pm
Tues, Thurs: 7 am to 5 pm
Closed daily from 12 - 1 pm
(561) 899-0758
Register at: https://bit.ly/3DlL6v3
Retirement Savings Plans
401(a) Special Retirement Plan
Administrator
BENCOR Administrative Services
(866) 296-9712
Plan ID#: 100260
www.bencorplans.com
Email: [email protected]
403(b) Plan Administrator TSA
Consulting Group, Inc.
Participant Transactions
28 Ferry Road SE
Fort Walton Beach, FL 32548
Phone: (888) 796-3786
Fax: (866) 741-0645
www.tsacg.com
Employee Assistance Program
Health Advocate Health Care Navigation
& EAP WorkLife Assistance
(855) 424-8400
www.HealthAdvocate.com/
palmbeachschools
Individual Portable Plans
Universal Life Insurance
Accident Insurance
Critical HealthEvents Insurance
Hospital StayPay Insurance
Trustmark Insurance Company
866-636-5525
www.trustmarkvb.com
Email: [email protected]
ID Theft Protection Plan
Ocenture ID Commander
(855) 592-7941 / (561) 434-7442
www.idcommander.com/pbcs
COBRA
Medical, Dental and Vision Benefit
Outsource, Inc. (BOI)
5599 S. University Drive, Suite 201
Davie, FL 33328
(888) 877-2780
Health Care FSA COBRA
TASC COBRA Payments
PO BOX 14015
Madison, WI
53708-0015
On-Site Representatives
FBMC
Fulton-Holland Building, A-103
(561) 434-7442
UHC
Fulton-Holland Building, A-103
(561) 434-8092 / (561) 357-7564

5
Eligibility Requirements
Enrollment Eligibility Requirements
We are excited to provide you with online access to complete your
Benefits Enrollment, which must be completed within 30 calendar
days from your eligibility date. You are provided this time to
review your benefits material. Instructions for accessing the online
enrollment system can be found on page 12.
Carefully review your enrollment materials and make selections
which best meet your insurance needs. Keep in mind that you
will be making choices that will remain in eect until the end of
the plan year. Elections are considered to be irrevocable and are
subject to Internal Revenue Code (IRC) Section 125.
Who Is Eligible?
As an employee of the District you may enroll in the dental and
vision plans as an employee OR as an eligible dependent of
another employee. You may not enroll in any plan as both an
employee and a dependent. If you and another family member
both work for the District, each of you cannot cover the other
family member as a dependent under the medical or life
insurance plans.
401(a) Dollars are contributed to a special retirement plan for any
employee who waives medical coverage. In order to waive the
District’s medical coverage, your medical coverage cannot be a
District-provided plan.
If you and your spouse/domestic partner both work for the District,
only one of you may cover your eligible dependent children.
District employees cannot be covered as a dependent in another
District employee’s medical plan. Each family member is required
to enroll independently for the medical plan.
An eligible regular, full-time employee is defined as an employee
who is in a paid status and works six or more hours per day (7.5
hours per day for those in the CTA bargaining group). Upon certain
qualifying events, a covered employee, spouse and dependents
may be eligible for group health plan continuation coverage under
COBRA law. Refer to the COBRA section beginning on page 70.
An eligible regular, part-time employee is defined as an employee
in a paid status and covered by the CTA bargaining unit working
3.75 hours per day; or, an employee who is in a paid status hired
prior to December 31, 2011, and who remains in an active paid part-
time status working four but less than six hours per day.
Any non-CTA employee is ineligible for benefits if hired or rehired
into a part-time position or transfers from a full-time position into a
part-time position.
If you are a newly-hired or rehired employee, your period of
coverage begins on the first day of the month following 30
calendar days of continuous employment in a benefited position.
For a minimum of 18 months, your medical plan choices include
the Low Option HMO, Consumer Driven Health Plan (CDHP) or
Waive (opting out of coverage). Waiving your medical coverage
requires that you are enrolled in a medical plan oered outside of
the District.

6
Dependent Eligibility
In 2022, the Oce of Inspector General completed a
dependent eligibility audit that revealed the need to perform
a more complete audit of all covered dependents. It was also
recommended that the required documents not only confirm
an eligible relationship exists, but also that the relationship is
current to allow for continued insurance coverage.
Board Policy 3.78 is the approved policy regarding Dependent
Verification requirements.
Dependent Audit Verification
Any dependent being enrolled in medical, dental or vision plans for
the first time or who had a break in coverage, will need to be fully
verified. Refer to page 7 for the complete list of the documents
needed to verify your dependent.
During your enrollment period, you should submit
documents (sucient to verify eligibility) to
dependentverifi[email protected] or fax the
documents to 561.434.8103. Documents must be submitted within
your enrollment period.
Don’t forget to actually enroll your dependent(s).
Enroll Online for Domestic Partner
Benefits
You should enroll in employee-only coverage under medical,
dental and/or vision then scroll down to the domestic partner
medical, dental and/or vision section to enroll your domestic
partner and any children in the after-tax plans. Remember to
provide required documents to Risk & Benefits Management to
finalize your elections.
Dependent Eligibility
Subject to dependent verification documentation, an eligible
dependent includes your legal spouse, domestic partner (subject
to additional eligibility criteria) or a dependent child. The term
“child” is defined as a:
• Biological/Adopted child under age 26.
• Stepchild.
• Child of a covered Domestic Partner.
• Child placed in your home pending adoption.
• Child under legal guardianship.
• Newborn child of a covered family member (birth to 18
months).
NOTE: If a covered family member becomes ineligible for
coverage, his/her child (newborn - 18 months) will also experience
a loss of coverage at the end of the month in which the family
member (child’s parent) is ineligible.
The definition of eligible “child” is subject to the following
conditions and limitations:
• Dependent child under the age of 26.
• Supporting documentation, such as a birth certificate,
will be required for dependent verification.
District employees are not allowed to cover another District
employee as a dependent on medical or life insurance plans.
Over-aged Adult Children
(F.S. 627.6562) Unmarried 26 - 30 years of age
A separate enrollment and contribution are required to enroll an
unmarried, over-aged adult child in the same medical plan you are
enrolled in. The eligibility criteria is that the over-aged adult child is:
• unmarried and has no dependents of his/her own.
• does not otherwise have other major medical health insurance
available (cannot have another option of coverage available).
• lives in Florida or is a student in another state (proof required
of residency or student status).
• has continuously been insured (certificate of creditable
coverage required).
The application for this type of coverage is available at
https://www.palmbeachschools.org/Page/13021
Unmarried Children with Disabilities
Coverage for an unmarried enrolled dependent child who is
incapable of self-sustaining employment because of an intellectual
disability or physical disability will be covered beyond the
specified limiting age, provided that the child was disabled prior to
attainment of the limiting age and the child is primarily dependent
upon you for support and maintenance.
We require that you provide documentation from the Social
Security Administration indicating your child has been deemed
disabled. Proof must be provided 30 calendar days prior to when
your child would no longer meet the eligibility age definition or at
the initial time of enrollment.
Requirements for 2024
Benefit technicians are responsible for verifying documents emailed to dependentverifi[email protected] or faxed to
(561) 434-8103. They are not responsible for adding dependent(s) to any plan. You are responsible for adding your dependent(s)
to each plan and for providing the required documents in a timely manner.

7
Dependent Verification Guide
Submit your documents to Risk & Benefits Management by email:
dependentverifi[email protected] or fax (561) 434-8103.
ELIGIBLE COVERED
DEPENDENT
DOCUMENTS
TO SUBMIT
ADDITIONAL
REQUIREMENTS
Legal Spouse (married less than 1 year)
Government issued marriage certificate None
Legal Spouse (married 1 year or more)
NOTE: A divorce MUST be reported within 30 days
and the ex-spouse removed from all plans.
Government issued marriage certificate
PLUS additional Requirements
(Financial information should be redacted
out for your privacy)
• Current Federal Tax 1040 showing
Married filing status from 2021 or 2022
OR
• Proof of common residence and
• Proof of recent financial
interdependence
(examples: Joint Bank statement, joint
auto insurance, utility bills dated within
the past 60 days )
Domestic Partner (less than 1 year)
Registered Domestic Partnership
Certificate and Receipt and SDPBC
Domestic partner Adavit
None
Domestic Partner (1 year or more)
Registered Domestic Partnership
Certificate and receipt, SDPBC Adavit
PLUS one of the Additional Requirements
• Proof of current common residence
(deed; lease; mortgage; utilities showing
both names/same address)
• Proof of current financial
interdependence (current loan; bank
statement in both Names)
Biological or adopted child up to age 26
Government issued birth certificate or
final adoption decree/certificate
None
Child under legal guardianship up to age 26
Court documents naming you or your
legal spouse as guardian of the child
Periodic updates upon request
Child placed in your home pending adoption up
to age 26
Court document placing child in your
home
Periodic updates upon request
Step-child up to age 26
Government issued birth certificate
Government issued marriage certificate
(Financial information should be redacted
out for your privacy)
If married less than 1 year…None
If married 1 year or more, one of the
following:
• Current Federal Tax Return
• Proof of common residence
• Proof of financial interdependence
Child of covered Domestic Partner up to age 26
Government issued birth certificate
Domestic Partner Proof from above since
Domestic Partner must also be enrolled
Disabled Child (Deemed disabled prior to 26)
(Unable to be self-sustaining and financially
independent)
Government issued birth certificate
Social Security Administration letter
deeming the child disabled
prior to the child turning 26 years of age.
Periodic proof of sustained disabled
and financial dependency
Newborn child of a covered family member
( up to a maximum of 18 months)
Government issued birth certificate if
Newborn’s parent is
enrolled
Your family member (the parent) must
also be insured and eligible under the
plan(s).
Over-aged Adult Child (26 – 30 years) (not
disabled) Adult Child must:
- Be unmarried
- Not have children of their own
- Not have other major medical insurance available
• State ID as proof of FL residence
• Current school registration
• Proof of continuous insurance
• Meet Fla. Statute 627.6562
Over-aged Medical
application
Notes:
• 1. District Employees are not allowed to cover another District employee as a dependent on medical or life insurance
• 2. Disabled Children must have current evidence of medical verification of sustained disabled status
• 3. Blackout any social security and detailed financial information prior to submission to protect your privacy

8
Domestic Partnership
Domestic Partnership Benefits
Guidelines for the domestic partnership benefit can be found on
this page and on the Risk & Benefits Management page at:
https://hub.palmbeachschools.org/all_employees/benefits/
benefit_forms. This is a post-tax benefit.
• Elections may only be made/changed during an Open
Enrollment or New Hire period.
• Residents of Palm Beach, Broward or Miami-Dade County are
required to submit a completed domestic partner adavit
and proof of registration and recording as domestic partners
through the county they reside in.
At the time of publication of this guide, information on how to
register in Palm Beach County could be found at:
www.mypalmbeachclerk.com/records/domestic-partnership
• Non-residents of the tri-county area are required to submit a
completed domestic partner adavit and supporting proof as
outlined in the non-resident section of the adavit.
• All documents must be sent to Risk & Benefits Management.
• Open Enrollment: The domestic partner adavit and any
other required documents must be sent by the close of
enrollment.
• New Hires: The domestic partner adavit and any other
required documents must be sent within 30 calendar days of
your date of hire.
How to Enroll Online for Domestic
Partner Benefits
You should enroll in employee-only coverage under medical,
dental and/or vision, then scroll down to the domestic partner
medical, dental and/or vision section to enroll your domestic
partner and any children in the after-tax plans. You must provide
the following to enroll:
Partnership of Less than 1 Year
• Completed Aadavit
• County Domestic Partner Certificate
• County Paid-Fee Receipt
Partnership of 1 Year or more
• Completed Aadavit
• County Domestic Partner Certificate
• County Paid-Fee Receipt
• Proof of current joint residency
- AND - proof of financial interdependence.
− Proof of Current Joint Residency - a copy of a deed, lease,
mortgage, or utility bill with both names or same address.
− Proof of Financial Interdependence - a copy of a current
joint loan or bank statement with both names or same
address (financial information should be blacked out).
Domestic Partnership Eligibility
All regular employees who are otherwise eligible for medical
benefits are eligible to enroll their domestic partner in the medical,
dental and/or vision plans. You may enroll as a new hire or during
Open Enrollment only.
Employees and their domestic partners must meet the following
requirements in order to enroll in a medical plan:
• Must both be 18 years of age and mentally competent.
• Must not be related by blood in a manner that would bar
marriage under the law of the State of Florida.
• Must be considered each other’s sole domestic partner and
not married to or partnered with any other spouse, spouse
equivalent or domestic partner.
• Must have shared the same regular and permanent residence
in a committed relationship for at least one year and intend to
do so indefinitely.
• Both parties agree to be jointly responsible for each
other’s basic food, shelter and common necessities
of life and welfare.
• Neither partner can have had another domestic partner at any
time during the 12 months preceding this enrollment.
A signed adavit attesting to the above will be required by both
partners as well as proof that both are financially interdependent
and living together. (See page 7 for the required documents.)
Imputed Income
The District subsidizes the actual plan costs, so you only pay
the amounts beginning on page 24. However, due to IRS
regulations, the amount paid by the District will be imputed income
and you will be taxed on that amount.
Remember to provide required documents to Risk
& Benefits Management to finalize your elections.
It is mandatory to provide supporting documentation for enrolled
dependents who are being added to the medical, dental and/or
vision plans.
Failure to provide documentation will result in no coverage for
those dependents.
Enrollment of any children and a domestic partner will be the
equivalent of the family level. The deductions will be reflected as
the employee-only pre-tax rate. The balance of the deduction will
be taken on an after-tax basis.

9
Important Enrollment Information
Existing Employees
Existing employees are able to make changes to their benefits
once per year during the Open Enrollment period. Please make
any required changes during the Open Enrollment period which
will be Nov. 1 - 15, 2023.
Employees Returning from Leave of
Absence
Returning to work can be exciting and stressful. Within 30 calendar
days of your return from a leave of absence, it is critical that you
contact Risk & Benefits Management to make elections. You will
need to complete a paper enrollment form. At this time, elections
due to a return from leave cannot be processed online.
If you fail to complete a benefits change form within 30 calendar
days of your return from leave, you will be enrolled in the default
Low Option HMO medical plan with employee-only coverage.
(For additional information regarding your benefits while on leave,
please refer to the leave information beginning on page 17).
Open Enrollment
During Open Enrollment you may enroll online
independently:
You may enroll in or change any benefit(s) during the Open
Enrollment period. Thereafter, changes during the year are
only allowed if you experience a valid Change in Status event
(see page 15 of this guide for more information on permitted
mid-plan year election changes).
New Hires
As a new employee you are eligible to enroll in many dierent
benefits.
Medical insurance is subsidized by the District, so your premiums
are low!
Full-time employees are also eligible for $20,000 in basic life
coverage at no charge. Higher term life insurance limits as well
as dental, vision, and disability plans are available to you at
negotiated group rates.
You can find information on all the various benefit choices in this
guide. We hope you are pleased with the selection available.
Don’t forget to enroll within 30 days of your start date; otherwise,
you will automatically be enrolled in employee-only Low Option
HMO medical and basic term life. (See page 12 for information
on how to enroll.)
If you are a newly-hired or rehired employee, your period of
coverage begins on the first day of the month following 30
calendar days of continuous employment in a benefited position.
For a minimum of 18 months, your medical plan choices include
the Low Option HMO, Consumer Driven Health Plan (CDHP) or
Waive (opting out of coverage). Waiving your medical coverage
is permitted as long as you are enrolled in a medical plan oered
outside of the District.
Change in Status
Change in Status events will be made eective on a prospective
(future) basis only. This means when you make a timely request,
the eective date will be the first day of the month after we have
received all required documents to approve your eligible status
change. The only exception to the prospective change rule will
be in the event of changes made due to birth or adoption. The
eective date will be the actual date of birth or placement/adoption
as long as all required documents have been submitted within 60
calendar days of the birth or placement/adoption.
To Enroll Online
• Visit www.mysdpbc.org
• Enter your District Username & Password
• Click on the PeopleSoft icon
• Click on “My Benefits/Benefits Enrollment”
or “Open Enrollment”
• Make your selections and submit

10
Important Enrollment Information
Default Plan Enrollment
Newly eligible employees who fail to make enrollment choices will
be automatically processed as being enrolled with employee-only
coverage in the Low Option HMO Medical plan and basic term life
insurance. All other plan options will be waived for that plan year.
Subject to dependent verification, you may enroll eligible
dependents in most plans that you elect to enroll in. However, if
you and your eligible dependent are both employed and eligible
for benefits through the District, keep in mind that you may only
be enrolled in any given product as either an employee or a
dependent; but not both. Domestic partner enrollment is limited to
medical, dental, and vision plans.
Dependent Eligibility
Subject to dependent verification documentation, an eligible
dependent includes your legal spouse, domestic partner
(contingent upon additional eligibility criteria), or a dependent
child. The term “child” is defined as a:
• Child born to or legally adopted by you
• Stepchild
• Child of a covered domestic partner
• Child placed in your home pending adoption
• Child for whom legal guardianship/custody has been awarded
to you or your spouse
• Grandchild added as a newborn up to a maximum of 18
months of age. Coverage continuation beyond 18 months of
age is not available to grandchildren
NOTE: If the grandchild’s parent (your child) becomes ineligible,
coverage for the grandchild and the grandchild’s parent
will terminate at the end of the month in which the eligibility
criteria is not met.
The definition of eligible “child” is subject to the following
conditions and limitations:
• Dependent child under the age of 26.
• Supporting documentation, such as a birth certificate, will be
required for dependent verification.
District employees are not allowed to cover another District
employee as a dependent on medical or life insurance plans.
Dependent Audit Verification
During Open Enrollment you should submit government-certified
documents (to verify your relationship). Send documents to Risk
& Benefits Management by fax or email. Please fax documents to
(561) 434.8103 or email to
dependentverifi[email protected].
Flexible Spending Accounts (FSAs)
• FSAs do not continue from one year to the next. You MUST
make an election each year to have an FSA in the new
plan year. Please consult a tax expert for assistance with
determining household maximums for FSAs.
• The Health Care FSA has an annual minimum of $300 and an
annual maximum of $3,200.
• The Dependent Care FSA has an annual minimum of $300
and an annual maximum of $5,000.
Flexible Spending Account Enrollment
You MUST reenroll in Flexible Spending Accounts (FSAs)
annually. FSA deductions begin the month in which the FSA
becomes eective. If you do not complete the enrollment
process, your FSA benefits will not continue for the new
2024 plan year.
Prior to the last day of the election period be sure to confirm that
your benefit choices are correct and accurate.
If You Already Have Insurance
• Waiving medical coverage is only an option for those who
have medical coverage provided by another employer or an
individual plan.
• Waiving medical coverage requires that an election be made.
Otherwise, default enrollment in the Low Option HMO single
coverage will be processed.

11
Important Enrollment Information
Review Your Choices and Current
Information
It is important that you confirm your elections and entries prior
to the end of your enrollment period.
Once Open Enrollment has been closed and
processed, navigate from the Portal page
through PeopleSoft to My Benefits
Enter 01/01/2024 and refresh to view your 2024
Benefit Elections
We will process the choices you have made. Anytime you want
to view your confirmed elections, be sure to enter 01/01/2024 to
view your 2024 benefit elections.
Elections made during the Open Enrollment period are final and
should be reviewed carefully prior to the close of the election
period. This is your one opportunity to make election choices.
Don’t Forget to Double Check!
The cost of medical services can vary greatly based solely on
where you seek services. It pays to be a consumer when it comes
to your health care for non-emergency needs.
While viewing your enrollment choices, please double-check each
plan including the coverage level and payroll deduction.
Plan type: Which medical plan did you choose: Low Option HMO,
High Option HMO or CDHP? Which dental plan did you choose:
DHMO or PPO?
Coverage level: Did you choose coverage for yourself only or did
you include your dependent spouse and/or children?
Dependent section: Did you list all dependents you wish to cover?
Please confirm the date of birth and social security information is
entered correctly.
Flexible Spending Accounts (FSAs): It is Important to review
your FSA election. Transfer of funds between FSA accounts is not
allowed. You are also prohibited to switch from the Health Care
FSA to the Dependent Care FSA.
Health Care FSA: Medical, dental and vision items for you and
your eligible dependents (annual maximum is base upon the IRS
maximum ).
Dependent Care FSA: This covers children daycare and qualified
elderly care expenses. You cannot use the DCFSA for your spouse
or children’s medical expenses.
Payroll deduction: Review your January check(s) to make sure that
the payroll deductions match the plan and coverage level.
Health Savings Account: If you enrolled in the CDHP medical
plan, you may be eligible to enroll and activate an HSA account.
Contributions to the HSA account from (employee and /or District)
can only be made with an active HSA election.
All Spending Accounts: Health Care FSA, Dependent Care FSA
and HSA accounts do not automatically rollover to the new plan
year. Active elections are required!
It is important that you review your enrollment choices during this Open
Enrollment period.

12
How to Enroll
The Enrollment Process
New Hires/Newly Eligible
We are excited to provide our new hires and newly eligible
employees with an online process to complete their benefits
enrollment. Medical plan enrollment for a minimum of 18 months
includes: Low Option HMO, Consumer Driven Health Plan (High
Deductible Plan), or waiving medical benefits (if you are covered
by a medical plan not oered by the District). Enrollment in the
High Option HMO plan will become a choice during the Open
Enrollment period following your completion of a minimum of 18
months of continuous employment in a benefit eligible position.
Benefit Enrollment help is always available!
Visit the HUB to find step-by-step instruction and illustration to
help walk you through using PeopleSoft.
There are also video tools to make it even easier for you to learn
how to use the tools and find the right spot to complete your
enrollment. Short, How- to videos are available on the HUB as
well. We know you have a million responsibilities and that your
time is precious so we have made it a simple as possible. Visit
Benefit Self Service help at:
https://hub.palmbeachschools.org/all_employees/benefits/
benefits_self_service
Online Benefits Enrollment:
Secure, Private, and No
Appointment Necessary!
Online Enrollment
• Go to: www.mysdpbc.org
• Log in to “PeopleSoft/My Benefits/Benefits Enrollment”
• You will need your user ID and password to enroll
− Secure, encrypted information
− Convenient – enroll 24/7
− Allows your spouse to participate with you
− Link to FAQs and providers
− Allows online benefits election verification
How to Obtain your User ID and Password
(NOTE: If you already access PeopleSoft or District email, use
your current user ID and password).
• Go to: www.mysdpbc.org
• Click on the Forgot/Change Password option
• Passwords must be a minimum of eight characters with
uppercase and lowercase letters, contain at least one
numeric character, and a symbol
• Enter your username (generally your Employee ID number)
• If you need help, call 561-242-4100 (option 2)
Log in to PeopleSoft
• Click on “My Benefits”
• Then click on “Benefits Enrollment”

13
Employee Responsibilities
Payroll contributions will start in the eective month of coverage.
Employee Responsibilities during Open Enrollment Responsibilities for Maintaining Employee Benefits
This Benefits Reference Guide provides general information and does not contain all of the applicable terms
and conditions of the various benefit plans referenced. Refer to the specific plan document for detailed plan
benefits, exclusions and limitations. All updates and changes will be made to the online document as deemed
necessary.
Find the most current information by logging in to: https://hub.palmbeachschools.org/all_employees/benefits
and selecting the Benefits Reference Guide link.
• You are responsible for maintaining your personal
information on PeopleSoft.
• Review your personal data such as mailing address and
dates of birth for you and your covered dependents. You can
update your personal information using the PeopleSoft My
Personal Information tool.
• You are responsible for reviewing your paycheck stub
(available online) when your benefits become eective. This
confirms your enrollment and verifies payroll contribution for
benefits you selected.
• You are responsible for notifying Risk & Benefits
Management immediately (within 30 calendar days of the
eective date of your benefits) if payroll deductions are taken
for elections you have not made or if required contributions
are not deducted from your pay.
• You are responsible for notifying Risk & Benefits
Management immediately (no later than within 60 calendar
days) when a covered dependent no longer meets the
eligibility requirements as defined on page 7.
• Benefit elections are irrevocable during the plan year,
unless you experience a valid Change in Status
(see page 15-16) and provide written documentation of
the event. Approved pre-tax deductions will be made on
the first day of the month after the benefits change form
and supporting documentation showing that your request is
consistent with, and on account of, the event.
• Enrollment appeals are granted under very limited
circumstances and generally are not permitted in the case
of accidentally enrolling in a plan or adding/deleting a
dependent in error.
• You are responsible for participating in the Open Enrollment
process.
• You are responsible for participating in and completing the
online web enrollment process. You may do this on your
own. Please carefully review your data to make sure the
information in the system is what you have elected.
• You are responsible for thoroughly reviewing your choices
during the online enrollment and prior to submitting your
elections.
• You are responsible for entering your enrollment data,
including your dependents, your dependents’ dates of birth,
and their Social Security information within the established
enrollment time frames.
• You are responsible for updating required documentation to
satisfy the eligibility criteria for all enrolled dependents.
• Verify that complete and accurate information is properly
reflected for your dependents. Otherwise, dependent
coverage will be canceled.
• You are responsible for providing your tobacco status.
• Review your plan election information, including any
dependents you may have attached to a benefits plan to
ensure accurate enrollment.

14
Contribution Overview
Employee Payroll Contributions
Your portion of the benefits cost will be taken through payroll
deductions over 22 or 24 pay periods, depending on your
paycheck schedule. Changes to your paycheck schedule will
impact your contribution amounts accordingly. Some plan
premiums are based upon your age and/or earnings. Premiums for
these plans are also subject to change.
Enrollment of any child(ren) and a domestic partner will be the
equivalent of the family rate. The deductions will be reflected as
the employee-only pre-tax rate and the balance of the deduction
will be taken on an after-tax basis. Domestic partners must be
covered in order for their children to be covered.
IMPORTANT NOTE: Employees who receive 26 paychecks will
have deductions taken only twice during the months when three
checks are issued. Plan costs displayed in this guide may vary
slightly from your actual payroll deductions due to rounding.
Coverage Levels
You will be able to purchase medical, dental and vision benefits at
the following levels:
1. Employee only
2. Employee + child(ren)
3. Employee + spouse
4. Employee + family
5. Employee + domestic partner
6. Employee + domestic partner + children (partner’s child(ren)
and/or employee’s child(ren)-
This provides you with maximum flexibility to custom-build your
benefits plan. You may select medical, dental and vision coverage
separately. For example, you may need medical coverage for just
you but dental coverage for you and your family.
Over-aged Adult Children
A separate application and contribution are required to enroll
eligible adult children who meet the state’s requirement and are
between the ages of 26 and 30 years of age.
401(a) Dollars
When an eligible employee waives medical coverage,
the District will contribute the dollar amount specified in the table
below into a 401(a) Special Retirement Plan in your name. The
401(a) Special Retirement Plan is administered by Bencor.
You are eligible to receive 401(a) Dollars if you waive medical
coverage as an employee and are not enrolled as a dependent on
a District medical plan.
If you have medical coverage other than a District plan (i.e., under
another employer’s plan), you may waive the School District’s
medical coverage and receive 401(a) Dollars valued at $100 per
month ($50 per month if you are a part-time eligible employee).
However, once you become eligible for medical insurance as an
employee, you are not eligible to be covered as a dependent on
a District medical plan by another District employee or to waive
medical coverage.
PLAN
MONTHLY
401A DOLLARS
FULLTIME PARTTIME
Waive Medical
$100 $50

15
Changing Your Coverage
What Is My Period of Coverage?
Your period of coverage is your eligibility period (e.g. January 1
to December 31), unless you make a permitted mid-plan year
election change.
Am I Permitted to Make Mid-Plan
Year Election Changes?
Yes, under specific circumstances. The District’s plan(s) and the
IRS may permit you to make a mid-plan year election change on
a prospective (future) basis, or vary a salary reduction amount,
depending on the qualifying event and requested change. Making
a change on a prospective basis means that the District will
process all approved mid-year changes on the first day of the
month after you make a Change in Status (CIS) election and submit
all required documentation supporting your request.
How Will Making a Change Aect
My FSA?
For a Health Care FSA, a mid-plan year election change will result
in split periods of coverage, creating more than one period of
coverage within a plan year with expenses reimbursed from the
appropriate period of coverage. Money from a previous period of
coverage can be combined with amounts after a permitted mid-
plan year election change.
However, expenses incurred before the permitted election change
can only be reimbursed from the amount of the balance present in the
Health Care FSA prior to the change. Mid-plan year election changes
are approved only if the extenuating circumstances and supporting
documentation are within the School District of Palm Beach County’s
Health Care FSA plan and the IRS regulations governing the plan.
Split periods of coverage do not apply to the Dependent Care FSA.
How to Make a Change with a
Qualifying Event
Within 60 calendar days of an event that is consistent with one of
the events permitted in the district’s plan design, you must send a
written request to your benefits technician. You must also provide
written documentation supporting your change request. Your
technician will review your request and documentation. If found
to be a valid life event, an event will be created in PeopleSoft My
Benefits to allow you to submit your changes.
Documentation supporting your election change request is
required. Once your request has been reviewed, approved and
processed, your existing elections and contribution amount will
change (as appropriate). Approved changes will become eective
on the first of the month following receipt of the election change
and all required documentation. A full premium payment will be
due for the period including that date. If your FSA election change
request is denied, you will have 30 calendar days from the date
you receive the denial to file a written appeal with FBMC. For more
information, refer to the Appeals Process on page 76.

16
Changing Your Coverage
EVENT PERMITTED CHANGES DOCUMENTS REQUIRED
New marriage
• Add spouse
• Add children of the partner
• Add previously eligible children if spouse/
partner is added
• May waive coverage
• Marriage certificate
• Birth certificate, paperwork from adoption or
legal guardianship
• Social Security Number for all enrolling
• Must provide proof of other group coverage
Legal separation or divorce
• Delete spouse
• Enroll in plans only if you and/or dependents
lost other coverage
• Must delete stepchildren or children of former
partner
• Copy of final judgment or
• Copy of legal separation notice
• Proof of loss of other group coverage
New baby; a child placed for
adoption, new step- children
and/or legal guardianship
• Add newly eligible dependent
• Add previously eligible, but not yet enrolled
dependents
• Birth certificate, paperwork from adoption or
legal guardianship
• Social Security number for all enrolling
NOTE: if the Social Security Number is not available,
enroll the child and provide it later
Loss of a dependent: child
reaches age 26, end of legal
guardianship, stepchild removal
due to divorce, death
• Delete dependent
• Must keep all other currently covered
dependents enrolled
• Court provided proof of the change in the
relationship
Employee and/or dependents
gaining other group coverage
• Delete self and/or spouse & dependents
• Proof of other group coverage for each
individual being deleted
Employee and/or dependents
lose other group coverage
• Add self/spouse/dependent. who lost
coverage
• Add previously eligible dependents
• Proof of loss of group coverage
• Birth certificate, paperwork from adoption or
legal guardianship
• Social Security Numbers for all enrolling
Qualified Medical Support
Order (QMSO)
• Add self if previously waived
• Add dependent(s) per court order
• Plan selection will be determined by court
order; if not ordered, employee may make
a plan selection; if no selection is made the
default plan will be implemented
• Copy of Qualified Medical Support Order
(QMSO)
• Birth certificate, paperwork from adoption or
legal guardianship
• Social Security Number for all enrolling
NOTE: if the employee has waived coverage, the
employee AND the child will be added (even if a birth
certificate, etc. is not provided)
Change in dependent’s
residence to outside of a
service area.
• Delete dependent that moved
• Cannot drop other dependents
• Proof of the move (e.g. utility bill in the
dependent’s name, new drivers’ license, etc.)
Change in dependent’s
residence to inside of a service
area
• Add dependent that moved
• Add all other previously eligible dependent
• Cannot drop other dependents
• Proof of the move (e.g. new drivers’ license,
etc.)
• Birth certificate, paperwork from adoption or
legal guardianship
• Social Security Number for all enrolling
Enrolled in Medicare • Delete self/dependents gaining coverage
• Proof of coverage for individuals to be
deleted
A loss of Medicare
• Add self and/or dependents losing coverage
• Add previously eligible dependents
• Proof of loss of coverage
• Birth certificate, paperwork from adoption or
legal guardianship
• Marriage certificate
• Social Security Numbers for all enrolling
A HIPAA special enrollment
event – gain or loss of either
Medi-Cal or SCHIP
• Add or delete self and dependents (must
have other coverage)
• Add previously eligible, but not yet enrolled
dependent
• Proof of loss of coverage
• Proof of gain of coverage
• Birth certificate, paperwork from adoption or
legal guardianship
*Employees have up to 60 days to
Notify the Benefits Department
for a Life Event Change

17
Leave of Absence Benefits
When Should You Apply for a Leave
of Absence?
To protect your benefits you should apply for a leave of absence
whenever you will be in an unpaid status. If you are out using
sick and/or vacation time for more than 10 consecutive days, you
must apply for a leave of absence. If you miss work as a result of a
work-related injury/illness, you should apply for a leave of absence
even if you receive workers’ compensation. Keep in mind that your
benefits eligibility requires that you work the majority of your duty
days. Therefore, anytime you are in an unpaid status, applying for
a leave preserves your access to benefits. It’s important for you to
notify and keep your supervisor informed of all absences. Failure
to report to work for the majority of your duty days could lead to a
loss of benefits as well as job abandonment processing.
Employees on Leave
Your period of active coverage will end the last day of the month in
which:
A. You are physically at work.
B. You are in a paid status using sick or annual days.
C. Your approved FMLA leave expires.
D. Payments are applied.
However, in most cases, your term life insurance ceases at the
end of the month in which you stop being actively at work. Refer
to your policy for detailed coverage rules, conversion rights and
application deadlines. If you do not pay required contributions
while on leave, your coverage will end and you will be required to
re-satisfy eligibility requirements when you return to active status,
except as otherwise provided by law. If you are on leave for other
than your personal illness or maternity, you may not continue
income protection.
Approved Medical Leave (FMLA)
You may continue your benefits while on approved FMLA
status. The District will make its contribution on your behalf for
District paid benefits. You will be responsible for your regular
contributions. Contact us at (561) 434-7478 or (561) 434-8668 if
you do not receive a monthly billing statement. Coverage will be
terminated for nonpayment if premium payments are not received
within 30 days of the due date.
Non-FMLA Leave
In order for your benefits to continue uninterrupted, you must
physically return to work in a benefited position and have paid all
required contributions prior to the last work day of the month in
which your leave ends.
COBRA continuation would be extended once your FMLA status
has been exhausted or once your benefits have been terminated
due to being in an unpaid status for any reason including unpaid
leave or in an unpaid status for more than 10 working days. You
would be eligible to continue your medical, dental and/or vision
benefits by electing and paying COBRA premiums. You may
continue your Healthcare Flexible Spending Account. Pelase see
Page 18 for more information. Please contact TASC directly for
more information if your FSA is terminated.
Life/Income Protection for Personal Illness
Employees who are enrolled in short-term and/or long-term
disability plans and are on a leave of absence due to their own
personal illness or maternity will be billed for those plans from the
first day of the leave through the date that the disability benefits
are expected to begin. The multiple elimination period for these
plans are outlined in the disability section of this guide. Failure
to pay premiums may result in disability claims being denied.
Employees on leave of absence other than for their own illness or
maternity are not eligible to continue the short-term or long-term
disability plans once they are no longer receiving an income from
the District. Premiums for these plans should not appear on any
billing statements received.
You should contact human resources when you need to take
time sporadically. You may be eligible for an intermittent
FMLA leave.
The reason for your leave also impacts your life insurance
coverage. If you were actively at work immediately before your
leave of absence, your life benefits will continue through the last
day of your approved FMLA leave as long as required premium
payments are made.
If you are totally and permanently disabled, you may continue
paying premiums for a maximum of 12 weeks from the date you
were in a paid status. After 12 weeks, you must either convert
to an individual policy or apply for Continued Protection (waiver
of premium) directly with the life insurance provider. You must
apply for a Continued Protection (waiver of premium) within
nine months of the date of disability. During the waiver premium
process, no premium payments will be due. You will be given the
right to convert your policy if your Continued Protection (waiver of
premium) request is denied. You will have 31 days from the waiver
of premium denial date to convert to an individual policy.
Other Leaves – Ineligible to Continue Life and
Income Protection Plans
Unfortunately, employees on leave for reasons other than personal
illness or maternity are not eligible to continue group life plans
beyond an approved FMLA leave. Coverage for these types of
plans will end the later of the last day of the month you are actively
at work or the last day of the month of an approved FMLA. Charges
for life insurance, short-term and/or long-term disability should not
be paid or appear or your billing statements.
Approved Nonpaid Leave
You can continue to receive coverage for certain benefits
for the duration of your leave if you choose to elect COBRA
continuation. Certain benefits, including short-term and long-
term disability, life products and dependent care FSA cannot be
continued while you are on an unpaid leave of absence. Life and
disability benefits may only continue if the reason for your unpaid
leave is due to your own illness/injury/maternity. You may contact
Risk & Benefits Management representatives regarding premiums
due for these benefits.
Other Benefits Impacted by an Unpaid Leave
We encourage you to contact the insurance providers/
administrators if you are enrolled in any group life plans, MetLife
plans, Trustmark plans, and/or a Health Care FSA. They will be able
to assist you with understanding how your leave of absence will

18
Other Leave Coverage
impact your coverage in these plans. Please contact:
• Trustmark directly at (866) 636-5525 for information
regarding payment of premiums if you had a Trustmark
Universal Life, Accident, Cancer
Protector or Critical Illness policy.
• FBMC’s On-site Representative directly at
(561) 434-7442 for information on continuation
of your Health Care FSA on an after-tax basis.
• MetLife at (800) 638-6420 for information about
Continued Protection (waiver of premium) and/or
(877) ASK-MET7 for discussions with a MetLife agent
about converting your policy.
Flexible Spending Accounts (FSAs)
While on Leave
Reimbursement for FSAs are only considered if expenses are
incurred during the period you have made contributions. No
reimbursement will be made for expenses during an unpaid leave
if you fail to continue to make contributions. You may contact
FBMC’s On-site Representative at 561-434-7442 to arrange
for the continuation of payment for your Health Care FSA. FSA
leave of absence payments must be made directly to FBMC. You
should continue your monthly contribution if you wish to request
reimbursement for the period that you are on leave.
Dependent Care FSA contributions cannot be made while on an
unpaid leave of absence.
To Continue your Health Care FSA while on Leave,
mail your check or money order to:
FBMC Benefits Management
ATTN: Benefits Administration
P. O. Box 1878
Tallahassee, FL 32302-1878
• Make your check payable to “The School District of Palm
Beach County.” (FBMC is unable to accept online payments.)
Write your 16-digit FBMC Member number on your check
or money order. Contact FBMC’s On-site Representative to
obtain your 16-digit FBMC Member number.
• Include a note that indicates you are a School District of Palm
Beach County employee on leave and you wish to continue
contributing to your Health Care FSA.
• If you have any questions about continuing your Health
Care FSA while on leave, please contact FBMC’s On-site
Representative at (561) 434-7442.
District-Paid Benefits While You Are in an
Unpaid Status
You should apply for an approved leave of absence in order to
continue your benefits. Once you are unpaid for the majority of
your duty days in any given month (even if you are not on leave)
you are no longer eligible for benefits. If you do not make sucient
payments to continue benefits, coverage will terminate at the end
of the month in which you were eligible. The length of your leave
of absence may impact your benefit eective date.
Unpaid Status, No Approved Leave
If you are not in a paid status, your benefits will end at the end of
the month in which the unpaid status began. Should you fail to
have payroll deductions taken for any period, coverage would be
retroactively terminated at the end of the month for which premium
payments were last received.
Re-enrollment Upon Return from Leave
Employees on approved leave during our Open Enrollment
period may make changes to their medical, dental or vision plans
and flexible spending accounts when they return to active duty.
Remember, 401(a) Dollars are not available until the first day of the
month after you return to a paid status plus any applicable waiting
periods if you did not continue your benefits while on leave.
Changes to any other benefits or continuation or reinstatement of
any benefits may be made within 30 calendar days of your return
to work. The length of your leave of absence may impact your
benefit eective date.
If you do not contact Risk & Benefits Management to complete
a benefits change form within 30 calendar days of your return to
work, you will be enrolled in the default medical plan and other
voluntary benefits may be dropped. Benefits that were canceled
while on leave (short-term disability, long-term disability) will not
automatically be reinstated. Please complete a benefits change
form within 30 calendar days of your return to reelect these types
of plans.
Contact Risk & Benefits Management at
(561) 434-7478 or (561) 434-8668 within
30 calendar days of your return to work.
Default Plan Enrollment
If you fail to contact Risk & Benefits Management upon your return from leave, you will be automatically enrolled in the Low Option
HMO employee-only medical plan and basic life insurance. No other benefits will be available.
Employee-only medical plan and basic life insurance: Open Enrollment will only be processed for actively working employees. If you
completed enrollment, but are not actively at work on the first working day of 2024, your election will not be processed.

19
Other Leave Coverage
Frequently Asked Questions
Q. Can I continue my Health Care FSA while on leave of absence
(LOA)?
A. You may keep your account active or you may revoke your
election while you are on leave. If you choose to keep your
account active, you may continue to pay into your Health Care
FSA (HCFSA) on a post-tax basis while on LOA. Although you
lose the benefit of tax savings, this approach will keep your
HCFSA period of coverage active and any eligible expenses you
incur while on leave may be submitted and reimbursed while
you are still on leave.
You may also keep your account active by making arrangements
with the School District of Palm Beach County to adjust your
contribution upon your return. Payroll will take the balance of
your FSA pledge for the calendar year and divide it by your
remaining pay dates, spreading the balance over the rest of
your paychecks for the year. Again, any eligible expenses you
incur while on leave will be paid. This approach gives you full
tax advantage, but you must wait until you return from leave,
and the School District of Palm Beach County notifies FBMC/
TASC that you are active again, before you can be reimbursed
for expenses incurred.
Q. What happens to my Health Care FSA while on leave?
A. Your payroll contribution will be discontinued. You may contact
FBMC to continue contributions on a post-tax basis. Otherwise,
you will have a break in coverage. Expenses incurred while on
leave will not be eligible for reimbursement. If you return during
the plan year, your FSA pledge will resume and the outstanding
contribution balance will be deducted from the remaining
paychecks.
Q. How do I continue my Health Care FSA while on LOA?
A. Once you go on leave, make your Health Care FSA contribution
payments payable to “the School District of Palm Beach County”
and mail your check or money order to:
FBMC Benefits Management, Inc.
ATTN: Benefits Administration
P. O. Box 1878
Tallahassee, FL 32302-1878
Phone: 561-434-7442
(Please do not send cash.)
Q. What if I don’t want to continue my Health Care FSA when I
return from LOA?
A. Because your FSA election is for the entire year, the District will
resume taking payroll reductions until the end of the calendar
year, unless you have a valid Change in Status event. However,
you can always opt out of reenrolling in an FSA during the next
Open Enrollment period.
Q. Can I continue my Dependent Care FSA while on LOA?
A. No. The Dependent Care FSA is used to reimburse participants
for work-related child and elder care expenses that enable them
to work, look for work or attend school. While you are on leave
you are considered “not actively at work,” and are thus ineligible
to participate.
Q. When will my Dependent Care FSA terminate if I go
on LOA?
A. It will terminate on the last day of the month in which your leave
begins. Employees may reenroll in the Dependent Care FSA
within 30 days of returning from leave.

20
Coverage Termination
Within 30 Days of Your Termination
of Employment, Contact:
• Risk & Benefits Management if you have not received
information regarding COBRA options or retiree benefits,
or to apply for a conversion policy for optional term life
coverage.
• Trustmark directly toll-free at 866-636-5525 for information
regarding payment of premiums if you had a Trustmark
Universal Life, Cancer Protector or Critical Illness policy.
• Flexible Spending Account (Health) - FBMC Onsite
Representative at (561) 434-7442 to apply for COBRA
continuation on an after-tax basis of your Flexible Spending
Health Care (FSA).Ocenture customer service directly toll-
free at (855) 592-7941 to continue your ID Commander ID
Theft protection plan.
Employee Coverage
During the plan year, except as otherwise provided by law and in
accordance with the School District of Palm Beach County’s plan(s),
terminating employees are covered as follows:
1. Through the last day of the month:
a.
In which employment ends (all interim positions and 12-month
employees are in this category).
b. In which a leave of absence without pay begins.
c. In which suspension without pay begins.
d. In which you cease being in a benefits eligible position.
e. For which required employee contributions are made.
f. In which you do not work the majority of your duty days.
g. In which you are in an unpaid status without an approved leave.
2. Exceptions:
a.
Your position is continued and you qualify for the Family and
Medical Leave Act (FMLA). In that case, coverage will end the
last day of the month in which eligibility for FMLA ends, as long
as required employee contributions are made.
b. You are a regular, but less than a 12-month employee, and you
are in paid status through the last day of your contract period. In
this case, coverage ends the last day of the month for which the
required employee contributions are made. Exception: Term Life
and/or income protection coverage may end as early as June 30
but will not continue beyond the period for which contributions
are made.
Change in Status Termination
Requests
You are permitted to make changes to your pre-tax benefit elections
during the plan year only for legitimate Change in Status (CIS) events.
The request may be granted if the life event is “on account of and
corresponding with a valid CIS that aects eligibility for coverage.”
If you experience a qualifying CIS event, the election changes must
be requested and submitted with proper documentation within
60 calendar days of the qualifying event and the change must be
consistent with the type of event.
Termination Due to Change in Status
Requests to terminate coverage for you and/or a dependent based
upon an approved Change in Status (CIS) event will be eective the
last day of the month after receipt of a completed Change in Status
election and supporting documents.
Retirement
Your benefits as an active employee end on the last day of the month
in which you retire. However, for all employees (with the exception of
12-month employees) who retire at the end of a school year and work
through their contract period, coverage will end on July 31 of that
year. As a retiree of the School District of Palm Beach County, you are
eligible to continue your health, dental and vision coverage if you pay
the monthly premium in full.
PLEASE NOTE: Your retirement date must be in a month in which
you are covered under the District’s benefits plan in order to
continue benefits as a retiree.
If you are eligible for Medicare upon retirement, Medicare will
become the primary payer on the first month following your
retirement date, regardless of your coverage through the District.
In order to be eligible to continue the health insurance benefits
you have to be retired and receiving monthly payments from FRS.
Enrollment in the FRS investment plan may limit your eligibility to
continue health benefits upon retirement. Please refer to School
Board Policy 3.79 for more information.
Termination or Change to Non-Benefited Position
If you terminate employment or have a change in your employment
status that results in you becoming ineligible for benefits, your
coverage will remain in eect until the last day of that month in which
the termination or Change in Status occurred.
Termination followed by rehire within 30 days
If you terminate employment and are rehired within 30 days or less
after termination, we will by default reenroll you into the benefit plans
that were in place prior to the termination (including your Health
Care FSA), unless otherwise provided by law. You will have access to
the Health Care FSA balance up to the full annual limit for expenses
incurred after you return (reduced by prior reimbursement). You may
experience a break in coverage and will be subject to new waiting
periods.
Termination followed by rehire after 30 days
If you terminate employment and are rehired 30 days or more after
termination, you will be permitted to make a new election or enroll into
the benefit plan(s) you had prior to termination. You will experience a
break in coverage and will be subject to new waiting periods and the
plan choices oered during the initial 18 months of employment.
Dependent Coverage
Your dependent’s coverage will terminate on:
• The last day of the month in which they meet the definition of
eligible dependent. Maximum age for dependent coverage is 25
years of age. Coverage terminates on the last day of the calendar
month in which they turn 26 years old.
• The date you, the employee, lose coverage.
• The date they are enrolled in coverage as a District employee.
EXCEPTIONS: If your child is disabled and you have provided
documentation prior to termination of benefits or you have applied
for coverage under the over-age adult child provision, or COBRA
continuation is elected and premium payments are made.
Trustmark voluntary insurance termination provisions may vary by
product. Please consult your policy.

21
Retirement or Separation
In Case of Retirement or Separation
Leaving the District can occur for many reasons such as finding a
new job, relocating to a dierent state, losing a position, reducing
hours or deciding to retire. In any case, you will be oered a way to
continue the District’s benefits.
Keep in mind that you may have to make decisions regarding what
is best for your individual needs as they relate to health insurance.
The cost of continuing coverage will definitely increase and some
choices may be aected by your eligibility and enrollment in other
types of plans, such as Medicare Part B, or your enrollment for
benefits as part of your COBRA rights.
Coordination of Benefits or Separation
Just be aware that once you leave the District, payment of claims
may be aected by coordination rules. We suggest that before you
make decisions on how you will continue to be insured you check
out all of your options.
Being eligible for Medicare may significantly change how claims
are reimbursed by this plan.
In the same manner, claim payments under this plan may be
dierent if you are eligible for Medicare and elect to continue
coverage through COBRA.
We suggest that before you decide to continue the District’s
medical plans, you take the time to read the Medicare information
on “Who Pays First” and the specific coordination of benefits
section of the medical plan document.
For your convenience, you can find out important Medicare
information at www.medicare.gov. Your medical plan documents
can be found on the Risk & Benefits web page under employee
benefits.
If you are eligible for Medicare upon retirement, Medicare will
become the primary payer on the first of the month following your
retirement date, regardless of your coverage through the District
Some plans are portable, which means you can continue the same
plan at the same premium rates. Other plans may be converted to
an individual policy, which may result in plan design changes and
an increase in premium rates. Your benefits as an active employee
end on the last day of the month in which you retire. However, for
all employees (with the exception of 12-month employees) who
retire at the end of a school year and work through their contract
period — coverage will end on July 31 of that year.
As a retiree of the School District of Palm Beach County, you are
eligible to continue your health, dental and vision coverage if you
pay the full monthly cost.
PLEASE NOTE: Your retirement date must be in a month in
which you are covered under the District’s benefits plan in order
to continue benefits as a retiree. For example, for 12-month
employees, benefits are provided for active employees until the
end of the month in which you retire, provided you have actually
worked during that month. For less than 12-month employees, the
same rules apply with the exception that at the end of the school
year, if you complete your contract, most benefits will remain in
place through the end of July.
If you do not physically return to work in August, your benefits
ended in July, so your retirement date must be in July. Continuing
with this example, if you choose an August retirement date, you
will not be eligible to continue benefits as a retiree. For more
information regarding your retiree benefit options visit: https://
www.palmbeachschools.org/careers/benefits/retiree_health_
benefits
The Retiree Benefit Technician is available to answer questions
you may have about Benefits.
When you are within 30 days of your retirement date, schedule
an appointment ith a Retiree Benefit Technician to discuss your
options. Please call (561) 434-8673 for more information.
Ana Swanberg / Email: [email protected]
Please refer to the Coverage Termination section for further
information.
Retiree Q&A
What Should I Do When I Retire?
Health insurance continuation at the time of retirement can take
two dierent paths.
Pre- Medicare (less than 65 years of age) will continue to have
benefits administered by Risk & Benefits Management.
Medicare Eligible (65 or older)
The Florida School Retiree Benefits Consortium (FSRBC) oers
comprehensive and competitive Medicare Medical, Dental and
Vision plans tailored especially for those age 65 or older, who have
retired from the Florida public school system.
FSRBC plan payment options vary depending upon your actual
enrollment choice.
During the 90 days prior to your anticipated retirement date,
contact Risk & Benefits Management, Retiree Technician, at
561-434-8673 at anytime with questions regarding the
continuation of retiree benefits.
Special Consideration for Term Life Insurance
Refer to the Conversion Provision on the Group Term Life pages
as well as your policy certificate for timelines and application
requirements.
When I Retire, to Whom Do I Send Payments?
Retirees who are pre-medicare eligible (pre-65 years of age),
may continue their health, dental, and/or vision plans through
the district group plans. They may elect to pay their full premium
payments through deductions from the Florida Retirement
System or provide authorization for the District to take automatic
deductions (ACH) from your bank account. Until FRS or ACH
deductions begin, payment by personal check or money order is
required.
Medicare Eligible Retirees - (65+ years of age)
Your choice for continuation of health, dental and/or vision service
will be administered by Florida School Retiree Benefits Consortium
(FSRBC). Payment option vary depending upon your plan
enrollment choice. For more information visit www.myfsrbc.com
or call 1-833-686-0983 (TTY 711)

22
Health Rewards Credit
Prepare now and earn a $50 per month
medical premium credit in 2025
Earn a $50 medical premium credit by actively participating in the
Health Rewards program. Complete required activities between
January 1 and August 31, 2024 to earn full credit beginning
January 1, 2025.
Complete the required activities by December 31, 2024 and you
will receive partial credit beginning with the first premium due on or
after June 1, 2025.
Any adult plan participant on a District medical plan is eligible to
participate in the Health Rewards program. Each participant must
earn 100% on their Rally dashboard to complete the requirements.
The premium credit incentive will be reflected in the employee’s
paycheck for anyone covered under that plan that earns the credit.
It is important for each plan participant to take full responsibility for
tracking their progress. For those who use the Provider Screening
form, please be aware that only the first form submitted will apply.
The participant are responsible for faxing that form.
• Complete the confidential Online Health Survey accessible
through www.myuhc.com.
• Complete a Biometric Screening (first submitted screening data
of 2024 will apply).
• Meet three of five Biometric Markers.
• If two or more of your biometric measures do not fall within
the established ranges, you can still earn reward percentages
by participating in one of the alternative programs. These
programs will help you get on the right track by providing
education and coaching on positive health
behaviors.
For more information about the Health Rewards program, visit:
https://hub.palmbeachschools.org/all_employees/employee_
wellness/health_rewards
A $50 per month tobacco surcharge will be added to the medical
premium for employees who use tobacco products.*
Log in to: https://hub.palmbeachschools.org/all_employees/
employee_wellness for available resources to help you be tobacco-
free and save.
*Based upon self-reported information entered in PeopleSoft.
Tobacco surcharge applies to tobacco users or employees who fail
to enter a status on the Wellness and Surcharge page.
Read more at:
https://hub.palmbeachschools.org/all_employees/employee_
wellness
Note: Participant is responsible for tracking progress and
submission of Health Provider Screening form.
100% earned by 8/31/24
Discount awarded 1/1/25
Met 3 of 5 targets
Health Survey
completed
Missed 3 or more targets
Start alternative
program
Health Survey
completed
100% earned by 8/31/24
Discount awarded 1/1/25
100% earned by 12/31/24
Discount awarded 6/1/25
Met 3 of 5 targets
Health Survey
completed
Missed 3 or more targets
Start alternative
program
Health Survey
completed
100% earned by 12/31/24
Discount awarded 6/1/25
For Partial Credit
Biometric Screening
For Full Credit
Biometric Screening
(Onsite Screening/Doctor's Office/Convenience Care Clinic/LabCorp)
(Doctor's Office/Convenience Care Clinic/LabCorp)

23
DOC District Onsite Clinic
Labs
Blood work and lab tests processed at the
center include hemoglobin A1C, lipid panel,
glucose, rapid strep, mono, urinalysis, oxygen
saturation, and pregnancy. Additional lab tests
can be drawn and sent to an outside lab.
• Annual Exams
• Blood pressure
• Body mass index
• Cholesterol
Health Screenings
• Glucose
• School, camp,
and sports
physicals
• Nutrition
• Physical activity
• Quit smoking
• Manage stress
Health Coaching
• Weight loss
• Consultations with
Registered Dietitian
• Arthritis
• Asthma
• COPD
• Depression
• Diabetes
Chronic Condition Management
• Heart health
• Low back pain
• Sleep apnea
• Educational
offerings
• Common Cold
• Constipation
• Cough
• Diarrhea
• Eye infections
• Headache
Acute (Sick) Care
• Joint pain
• Nausea/vomiting
• Nosebleed
• Sinus infections
• Skin infections
• Strep throat
The District Onsite Clinic
3300 Forest Hill Blvd., BuildingE
West PalmBeach, FL33406
561-899-0758
Mon, Wed, Fri: 7 am to 6 pm
Tues, Thurs: 7 am to 5 pm
Medications
Common medications dispensed onsite
including acute medications/antibiotics, allergy
medications and maintenance medications for
chronic conditions.
The District Onsite Clinic
Services Available

24
Medical Plan Cost
2024 Employee Per-Pay-Period Medical Contributions
Due to escalating healthcare costs, an increase for Plan Year ‘24 has been applied to all tiers of coverage to the equivalent of $20 per
month (for both the District and employee rates).
Per pay period
pre-tax deductions
are as follows:
FULLTIME PARTTIME**
24 DEDUCTIONS 22 DEDUCTIONS 24 DEDUCTIONS 22 DEDUCTIONS
EE = EMPLOYEE
District
Contribution
Employee
Deductions
District
Contribution
Employee
Deductions
District
Contribution
Employee
Deductions
District
Contribution
Employee
Deductions
LOW OPTION HMO
EE only
$255.00
$35.00 $278.15 $38.18 $255.00 $35.00 $278.15 $38.18
EE + Child(ren)
$390.00
$78.00 $425.41 $85.08 $375.00 $93.00 $409.05 $101.44
EE + Spouse
$427.50
$99.00 $466.32 $107.99 $412.50 $114.00 $449.96 $124.35
EE + Family
$500.50
$161.00 $545.95 $175.62 $485.50 $176.00 $529.58 $191.98
HIGH OPTION HMO
EE only
$280.00 $55.00 $305.42 $60.00 $230.00 $105.00 $250.88 $114.53
EE + Child(ren)
$415.00 $145.00 $452.68 $158.17 $350.00 $210.00 $381.78 $229.07
EE + Spouse
$450.00 $170.00 $490.86 $185.44 $385.00 $235.00 $419.96 $256.34
EE + Family
$550.00 $240.00 $599.94 $261.79 $485.00 $305.00 $529.04 $332.69
CDHP MEDICAL
EE only
$195.00 $40.00 $212.71 $43.63 $195.00 $40.00 $212.71 $43.63
EE + Child(ren)
$325.00 $88.00 $354.51 $95.99 $310.00 $103.00 $338.15 $112.35
EE + Spouse
$345.00 $109.00 $376.33 $118.90 $330.00 $124.00 $359.96 $135.26
EE + Family
$415.00 $176.00 $452.68 $191.98 $400.00 $191.00 $436.32 $208.34
DISTRICT CONTRIBUTION 401A DOLLARS
Waive Health
$50.00 $54.54 $25.00 $27.27
Amounts reflected on paychecks may vary slightly due to rounding. Rates above do not include Health Rewards discount or tobacco surcharge rates.
**Applies to CTA Bargaining units or those in part-time status as of 12/31/2011.
Enrollment of a Domestic Partner or Domestic partner and child(ren) will be the equivalent of the above rates. The deductions will be
reflected as the employee–only pre-tax rate and the balance of the deduction will be taken on an after-tax basis.
Unless otherwise noted, all benefits listed are valid only for health services received through participating providers or with plan approval.
Notification of services may be required.
This summary information is subject to change. This summary is not to be solely relied upon by members or applicants. If there is a
discrepancy between this summary and the summary plan description (SPD) the information found in the summary plan
description would supersede.

25
Medical Plans
Benefits-at-a-Glance • UnitedHealthcare: Low Option HMO (Choice Network)
This plan gives you the freedom to see any doctor or other healthcare professional from our national network, including specialists,
without a referral. In addition, you do not have to worry about any claim forms or bills.
MEMBER PAYMENTS INNETWORK ONLY
Annual Medical Expense Deductible
$500 for individual / $1,000 family
Annual Out-of-Pocket Maximum
$6,000 individual / $12,000 family
Coinsurance/In-Patient Hospital Coinsurance
20% of eligible expenses after deductible
Primary Care Doctor
Check United's provider directory before making your
decision regarding your health care provider
Choose any doctor from the United Open Access Directory.
You may access any participating specialist without a referral.
Preventive Care
No charge
Oce Visit (Primary Care)
$30 co-pay for UHC Premium Care Physician /
$40 copay non-Premium Care Physician / Deductible does not apply
Specialist Oce Visit
$55 co-pay for UHC Premium Care Physician /
$60 co-pay non-Premium Care Physician / Deductible does not apply.
No referral needed.
Outpatient Hospital and Surgical Services X-ray,
Other diagnostic services (MRI, CT scan, lab test, etc.)
20% of eligible expenses after deductible
Outpatient Rehabilitation Therapy
$35 co-pay per visit
1
Deductible does not apply
Approved Durable Medical Equipment
20% of eligible expenses after deductible
Emergency Ambulance Trip
$150 co-pay per trip
Hospital Pre-Admission Requirement
Your doctor will take care of all prenotification requirements.
Emergency Room Care
$250 co-pay (waived if admitted)
Urgent Care Copay
$75 co-pay - Deductible does not apply
Convenience Care Clinic
- Virtual Oce Visits
$40 co-pay - Deductible does not apply
$25 co-pay - Deductible does not apply
District Onsite Clinic Visit
$10 copay
Outpatient Mental Health & Substance Abuse
Services
- Telemed Services include Mental/Substance Abuse
Counseling
$35 Individual / $25 family
Deductible does not apply
Prescription Drugs
(NOTE: Walgreens is not a participating pharmacy)
• 30-day supply per prescription at participating
pharmacies
• Mail order for a 90-day supply of formulary
maintenance medication per prescription
RETAIL MAILORDER
DED
$100 Individual / $200 Family No Deductible
Tier 1
$10 copay after deductible $25 copay
Tier 2
$30 copay after deductible $75 copay
Tier 3
$60 copay after deductible $150 copay
Tier 4
$100 copay after deductible $250 copay
Network www.myuhc.com. Network name “UnitedHealthcare Choice.” This network is for both the Low/High Option HMO.
1
20 visits of physical, occupational, pulmonary and speech therapy per calendar year, per therapeutic type; 36 visits per year for cardiac therapy.

26
Medical Plans
Benefits-at-a-Glance • UnitedHealthcare: High Option (Choice Network)
This plan gives you the freedom to see any doctor or other healthcare professional from our national network, including specialists,
without a referral. In addition, you do not have to worry about any claim forms or bills. This plan becomes available during Open
Enrollment after you have been benefit eligible for 18 months without a break in service.
MEMBER PAYMENTS INNETWORK ONLY
Annual Medical Expense Deductible
$400 individual/ $800 family
Annual Out-of-Pocket Maximum
$4,000 individual/ $8,000 family
Coinsurance/In-Patient Hospital Coinsurance
10% of eligible expenses after deductible
Emergency Room Coinsurance
15% of eligible expenses after deductible
Primary Care Doctor
Check United's provider directory before making your
decision regarding your health care provider
Choose any doctor from the United Open Access Directory.
You may access any participating specialist without a referral.
Preventive Care
No charge
Oce Visit (Primary Care)
$30 co-pay for UHC Premium Care Physician/ $40 copay
non-Premium Care Physician / Deductible does not apply
Specialist Oce Visit
$40 co-pay for UHC Premium Care Physician/
$50 co-pay for non-Premium Care Physician / Deductible does not apply.
No referral needed.
Outpatient Hospital and Surgical Services, X-ray,
Other diagnostic services (MRI, CT scan, lab test, etc.)
10% of eligible expenses after deductible
Outpatient Rehabilitation Therapy
$20 co-pay per visit
1
Deductible does not apply
Approved Durable Medical Equipment
10% of eligible expenses after deductible
Emergency Ambulance Trip
10% of eligible expenses after deductible
Hospital Pre-Admission Requirement
Your doctor will take care of all prenotification requirements.
Emergency Room Care
15% of eligible expense after deductible
Urgent Care Copay
$50 co-pay
Deductible does not apply
Convenience Care Clinic
- Virtual Oce Visits
$25 co-pay - Deductible does not apply
$25 co-pay - Deductible does not apply
DOC District Onsite Clinic Visit
$10 copay
Outpatient Mental Health & Substance Abuse
Services
- Telemed Services include Mental/Substance Abuse
Counseling
$20 individual/$15 group
Deductible does not apply
Prescription Drugs
(NOTE: Walgreens is not a participating pharmacy)
• 30-day supply per prescription at participating
pharmacies
• Mail order for a 90-day supply of formulary
maintenance medication per prescription
RETAIL MAILORDER
DED
$100 Individual / $200 Family No Deductible
Tier 1
$10 copay after deductible $25 copay
Tier 2
$30 copay after deductible $75 copay
Tier 3
$60 copay after deductible $150 copay
Tier 4
$100 copay after deductible $250 copay
Network www.myuhc.com. Network name “UnitedHealthcare Choice.” This network is for both the Low/High Option HMO.
1
20 visits of physical, occupational, pulmonary and speech therapy per calendar year, per therapeutic type; 36 visits per year for cardiac therapy.

27
Medical Plans
MEMBER PAYMENTS INNETWORK ONLY OUTOFNETWORK ONLY
Annual Medical Expense Deductible
$3,000 individual / $6,000 family $4,500 individual | $9,000 family
Annual Out-of-Pocket Maximum
$6,350 individual / $12,700 family $10,000 individual | $20,000 family
Coinsurance/In-Patient Hospital
Coinsurance
30% of contracted fee after deductible 40% of eligible expenses after deductible
Primary Care Doctor
Choose any doctor from the United network
“UnitedHealthcare Choice Plus.” Access any
participating specialist without a referral.
Choose any licensed doctor
Preventive Care
- Oce visit
- Routine mammogram**
No charge
No charge
40% of eligible expenses after deductible
40% of eligible expenses after deductible
Oce Visit (Primary Care)
30% of contracted fee after deductible 40% of eligible expenses after deductible
Specialist Oce Visit
30% of contracted fee after deductible 40% of eligible expenses after deductible
Outpatient Hospital and Surgical
Services, X-Ray, Other diagnostic
services (MRI, CT scan, lab tests, etc.)
30% of contracted fee after deductible 40% of eligible expenses after deductible
Out-Patient Rehabilitation Therapy
1
30% of contracted fee after deductible 40% of eligible expenses after deductible
Approved Durable Medical
Equipment
30% of contracted fee after deductible 40% of eligible expenses after deductible
Emergency Ambulance Trip
30% of contracted fee after deductible 30% of eligible expenses after deductible
Hospital Pre-Admission Requirement
Your doctor will take care of prenotification
It is your responsibility to see that your
doctor takes care of prenotification
Emergency Room Care
30% of contracted fee after deductible 30% of eligible expenses after deductible
Urgent Care Copay
30% of contracted fee after deductible 40% of eligible expenses after deductible
Convenience Care Clinic
- Virtual Oce Visits
30% of contracted fee after deductible
$50 then 30% of contracted fee after
deductible
40% of eligible expenses after deductible
N/A
DOC District Onsite Clinic Visit
$25 copay
Outpatient Mental Health &
Substance Abuse Services
30% of contracted fee after deductible 40% of eligible expenses after deductible
Network www.myuhc.com. Network name “UnitedHealthcare Choice.” This network is for both the Low/High Option HMO.
1
20 visits of physical, occupational, pulmonary and speech therapy per calendar year, per therapeutic type; 36 visits per year for cardiac therapy.
Prescription Drugs
• 30-day supply per prescription at participating
pharmacies
• Mail order for a 90-day supply of formulary
maintenance medication per prescription
RETAIL MAILORDER
DED
Subject to Deductible Subject to Deductible
Tier 1
$10 copay after deductible $25 copay after deductible
Tier 2
$30 copay after deductible $75 copay after deductible
Tier 3
$60 copay after deductible $150 copay after deductible
Tier 4
$100 copay after deductible $250 copay after deductible
Benefits-at-a-Glance • UnitedHealthcare: CDHP with an HSA* (Choice Plus Network)
The Consumer Driven Health Plan (CDHP) with a Health Savings Account (HSA) puts you in control of your medical spending and gives
you the ability to save money in your HSA for future health care needs. The School District of Palm Beach County will fund monthly the
following amounts into your HSA account: $60 for Employee Only, $90 for Employee + Child(ren), $90 for Employee + Spouse, and
$120 for Employee + Family. This plan gives you the freedom to see any doctor or other health professional from our national network,
including specialists, without a referral. With this plan, you will receive the highest level of benefits when you seek care from a network
doctor, facility or other health care professional. You may also choose to seek care outside the network without a referral. However, you
should know that care received from a non-network doctor, facility, or other health care professional means a higher deductible and
copayment.

28
Medical Plans
Naviguard Member Journey
NVG22-10014-003 03/22 © 2022 United HealthCare Services, Inc. All RIghts Reserved.
*In situations where member is billed above a certain amount.
Administrative services provided by United HealthCare Services, Inc. or their affiliates.
Plan Management
|
Naviguard
®
Out-of-Network Solution
How Naviguard works for members.
We can help resolve unexpected medical bills by negotiating directly with providers.*
Naviguard
®
services are available at no additional cost to members in Naviguard participating
plans through your UnitedHealthcare administered health plan benefits.
1. Call
When a member has an OON service not
covered by the No Surprises Act (NSA), they
receive an EOB and then a balance bill.They
call UHC member services to get started
with Naviguard.
We’ll be with you every step of the way.
2. Connect
Member is connected with a dedicated
Naviguard advisor. The member meets with
their advisor to share their story, upload their
OON bill and sign some forms so we can
begin negotiating on their behalf.
3. Negotiate
Their dedicated Navigaurd advisor begins
negotiations with the OON provider while
keeping the member up to date on progress.
4. Outcome
The member’s Naviguard Advisor sends them
a record of the process and the final outcome
of negotiations. A new EOB may also be sent.
29
Medical Plans
AFTER YOUR CONSULTATION
You’ll receive a written summary of your consultation so you’re
prepared for a conversation with your treating doctor or we can
refer you to another in-network doctor in your area.
WE SPECIALIZE IN
MEDICAL CERTAINTY
Apple, the Apple logo, iPhone, and iPad are trademarks of Apple Inc., registered in
the U.S. and other countries and regions. App Store is a service mark of Apple Inc.
Google Play and the Google Play logo are trademarks of Google LLC.
CALL 911 IMMEDIATELY IF YOU ARE HAVING A MEDICAL EMERGENCY. 2nd.MD
is not an emergency service. 2nd.MD is an independent resource to support you in receiving
information from Expert Medical Specialists. 2nd.MD does not practice medicine or provide
patient care and is independent from the Specialists providing the expert medical consultations.
The information provided through 2nd.MD does not constitute medical advice and does not diagnose,
treat or prescribe treatment of medical conditions. All information provided in connection with
2nd.MD is for informational purposes only, and does not create a physician-patient treatment
relationship. Information provided through 2nd.MD does not substitute medical diagnosis or treatment
from your treating physician, and you should discuss the information provided with your treating
physician before making any decisions. The 2nd.MD service may not be available in all states or for all
group sizes and is subject to change. Coverage exclusions and limitations may apply.
Through your employer, you have an exclusive membership
to 2nd.MD, a virtual expert medical consultation and
navigation service. We connect you with a board-certified,
elite specialist for a virtual expert medical consultation via
phone or video from the comfort of home.
WHO IS ELIGIBLE?
2nd.MD is confidential, fast and no additional cost
to you and covered dependents on the
UnitedHealthcare medical plan.
GET STARTED TODAY
Call at 1.866.269.3534
Visit www.2nd.MD/activate
or download our 2nd.MD app
2nd.MD specializes in medical certainty by providing
access to elite specialists for questions about:
Diseases, cancer, or chronic conditions
• Surgeries or procedures
• Medications and treatment plans
HOW IT WORKS:
3 Simple Steps
1
1
.
.
ACTIVATE YOUR ACCOUNT
AND REQUEST A CONSULT
Visit www.2nd.MD/activate,
download our app or call us at 1.866.269.3534
2
2
.
.
SPEAK WITH A NURSE
Explain your medical issues and an experienced nurse
will handle the rest, including collecting medical
records and connecting you with a leading specialist
who is an expert in your condition.
3
3
.
.
CONSULT WITH A LEADING SPECIALIST
Get information about your diagnosis, treatment plan
and next steps in care from a nationally recognized
specialist. Consult via video or phone at a time that
works best for you, including evenings and weekends!
22-674 © 2022 2nd.MD. All rights reserved.
See how one member avoided an
unnecessary surgery and learned how
to manage her rare condition.

30
Medical Plans
© 2021 United HealthCare Services, Inc. All Rights Reserved. WF3656609 206015A-102021 OHC
Whether it’s a stiff neck, aching shoulders or more severe back issues, it can
be hard to enjoy life when pain shows up. That’s where Kaia steps in. It’s a
new app here to show how pain relief is possible — at no extra cost as part
of your health plan.
Don’t wish pain away …
do this instead
On-demand pain relief care
in the convenience of an app
Workouts tailored to you with
some as short as 15 minutes
Bite-sized lessons to help
you recognize where pain
is coming from
*Provided at no extra cost as part of your health plan.
1-on-1 health coaching
with certified professionals
No extra cost — this is included
as part of your health plan
Strengthening exercises plus
relaxation techniques for pain
management
Download Kaia today
Kaia tracks your
movements using AI
technology to ensure
you’re doing each exercise
correctly, providing
real-time audio and video
feedback for help along
the way. So you get a
program tailored to your
fitness, pain and mobility
levels to help manage pain.
For real-time
feedback while
you exercise
Download the Kaia app for on-demand, personalized
support to help relieve pain and live healthier
Connecting with Kaia connects you with so much
You’ll get a personalized pain relief program
created on the spot after you sign up. Get started
right away learning helpful exercises just like
in your physical therapist’s office, but with no
scheduling, waiting rooms or travel required.
Visit startkaia.com/uhc

31
Medical Plans
© 2023 United HealthCare Services, Inc. All Rights Reserved.
Through your myUHC.com account on your computer or the UHC App on your
smart phone, you have access to a wide variety of virtual providers. Including
the following areas:
Click on “Find Care & Costs”,
then Virtual Care on
myUHC.com and the UHC App
to get started today!

32
Healthcare Doctors
UnitedHealthcare is pleased that the School District of Palm Beach
County has chosen us as the health plan provider for you and your
family.
Welcome - We’re Glad You’re Here
While no one can predict the future, you can prepare for it. Your
UnitedHealthcare benefits provide you with access to people,
resources and tools to help you when you aren’t feeling your best.
We have also created unique programs to help you improve your
health and wellness. We believe knowledge is the heart of your
healthcare, so we want to give you resources to help you:
• Be active with your healthcare
• Make healthy choices
• Find answers
• Save money
• Take charge of your health
Benefits You’ll Appreciate
Your doctor is likely already in our network. Whether you are at
home, traveling or you have a covered child going to school out-
of-state, a network doctor or hospital is likely close by. In addition,
there are no referrals. You can see the specialist you want.
Emergencies are covered anywhere in the world, and you usually
don’t have to worry about claim paperwork for network care.
Find a Network Doctor or Hospital
Search by facility, location, gender, and languages spoken.
1. www.myuhc.com
2. Click “Find Medical and Mental Health Providers”
3. Choose “Medical Directory” or “Mental Health Directory”
4. Click the “All UnitedHealthcare Plans icon”
5. For the Low or High HMO plan, select the
“Choice” plan
6. For the CDHP plan, select UnitedHealthcare
“Choice Plus”
Your Coverage Plan
Your benefit plan is an important part of your daily life, even if you
don’t need services every day. It protects you and helps you better
manage your health. Right now is the perfect time to find out all
you can about your coverage before you need it, especially how it
works and where to go for care.
Always Carry your ID Card
Your ID card has key information about you and your coverage. Put
your card in your wallet or your pocketbook so you won’t forget
it. When you’re at doctors’ oces, drugstores and hospitals, show
it to make sure you are not billed unnecessarily. You may also be
asked to show a picture ID, such as your driver’s license or another
government ID card with a picture on it, so be sure to bring this
with you, too. You can also access an electronic copy of your ID
card using the UHC App.

33
Healthcare Doctors
Additional Features of Each Plan
When you enroll in a UnitedHealthcare health plan, you’ll not only
have the freedom to use any doctor or hospital in our nationwide
network, including specialists, but you’ll also be able to take
advantage of many valuable programs and services to make your
healthcare experience easier.
Health coaches oer telephonic and online support to help you
lose weight, stop smoking, manage diabetes and more.
Health and wellness programs can help you eat right, stop
smoking and relax. You can participate online, or by phone, in the
comfort of your own home.
Other helpful tools include:
• Healthcare cost estimator
• Physician search
• Hospital comparison
UnitedHealth Premium® Care
Physician - Find Recognized Doctors
and Hospitals in the Network
With the UnitedHealth Premium Tier 1 designation program*, we
help you:
• Find doctors and hospitals in your area that meet quality and
cost-eciency criteria
• Find doctors you can call directly, without prior approval
• Get names quickly online
• Access 27 specialties, including primary care,
cardiology and orthopedics, as well as facilities in specialties,
including:
− congenital heart disease
− cardiac care
− total joint replacement
− spine surgery
Finding a UnitedHealth Premium®
Care Physician
Visit your member website, myuhc.com, to search the directory
and look for this symbol next to your results.
*UnitedHealth Premium Tier 1 is not available in all geographic locations. For a complete description of the UnitedHealth Premium Tier 1 designation program, including details on the
methodology used, geographic availability and program limitation, please visit myuhc.com®.
Criteria for designation come from nationally recognized quality standards and market-based cost eciency standards. For our members with special medical concerns, we also provide
information from the National Committee for Quality Assurance (NCQA) Doctor Recognition Program.
Before your appointment:
1. Make a list of all the questions you have for your doctor,
nurse or pharmacist.
2. Write down medications you are currently taking, including
prescriptions, over-the-counter medicines, and herbal
supplements.
3. Plan to bring a family member or friend to your visit if you
have a hard time remembering what your doctor tells you.
During your appointment:
1. Tell your doctor if a family member has been diagnosed
with a serious disease or condition.
Also mention if you have or will be traveling outside the
country.
2. Ask your doctor at every visit to send any laboratory test to
a network facility.
3. Before you leave, make sure you can read and/or
understand your doctor’s or pharmacist’s instructions. If you
don’t, it’s okay to ask them to explain until you understand.
Tips to Make Your Doctor’s Visit Worthwhile

34
Pharmacy Benefits
A health plan that’s
always with you
Digital tools to keep you connected
Get the most out of your benefits
Register for your personalized website on myuhc.com® and download the
UnitedHealthcare® app. These digital tools are designed to help you understand
your benefits and make informed decisions about your care.
• Find care and compare costs for providers and services in your network
• Check your plan balances, view your claims and access your health plan ID card
• Access wellness programs and view clinical recommendations
• 24/7 Virtual Visits – Connect with providers by phone or video to discuss
common medical conditions and get prescriptions*, * if needed
*
• View your health care financial account(s) such as HSA, FSA or HRA
• Compare prescription costs and order refills
Download the app
Available for iPhone and Android
*Data rates may apply.
** Certain prescriptions may not be available, and other restrictions may apply.
continued
Register today
Scan the QR code or go to
myuhc.com and click Register Now
See next page for registration steps

35
Pharmacy Benefits
Pharmacy
|
Specialty Pharmacy
What is a specialty medication?
An injected, infused, oral or inhaled medication is defined as a specialty medication if it:
• May need ongoing clinical oversight and extra education
• Has unique storage or shipping needs
• May not be available at retail pharmacies
• May need infusion or home nursing
What services does the specialty pharmacy provide?
UnitedHealthcare® offers specialty medication services through Optum® Specialty Pharmacy. Optum
Specialty Pharmacy supports you with a team of pharmacists and nurses who specialize in your
condition — at no extra cost to you. You also have:
• Access to your medications at your plan’s lowest cost
• 24/7 access to pharmacists
• Clinical and adherence programs
• Medication supplies at no extra cost
• Refill reminders
• Timely delivery in confidential packaging
Welcome to the
UnitedHealthcare
specialty pharmacy
program
Specialty medications are important
to maintain or improve your health.
Our specialty pharmacy program has
resources and personalized support to
help you with your condition.
continued

36
Pharmacy Benefits
WF5894210 02/22 © 2022 United HealthCare Services, Inc. All Rights Reserved.
Optum Specialty Pharmacy is affiliated with OptumRx, a pharmacy benefits manager. You may not be required to use Optum Specialty
Pharmacy for your specialty medication. There may other pharmacies available in your network. Call the customer service number on your
member ID card or visit your plan website and use the pharmacy locator to view listings. Your receipt of this communication is acknowledgment
of the information provided. You may contact the customer service number on your member ID card for any questions or concerns.
UnitedHealthcare® and the dimensional U logo are registered trademarks owned by UnitedHealth Group Incorporated. All branded
medications are trademarks or registered trademarks of their respective owners.
Insurance coverage provided by or through UnitedHealthcare Insurance Company or its affiliates. Administrative services provided by
UnitedHealthcare Insurance Company, United HealthCare Services, Inc. or their affiliates. Health Plan coverage provided by or through a
UnitedHealthcare company.
All Optum® trademarks are owned by Optum, Inc. in the U.S. and other jurisdictions. All other brand or product names are trademarks or
registered marks of their respective owners.
Guiding your health journey under the pharmacy benefit
We understand the challenge of living with and managing a complex health condition. Our specialty pharmacy program is here
to assist you every step of the way.
Getting started
Call 1-855-427-4682 to enroll in the specialty
pharmacy program.
Pharmacists and patient care coordinators are
ready 24/7 to take care of everything, including:
• Transferring your prescription
• Helping find affordable ways to get
your medication
• Explaining how to use the specialty pharmacy
Personalized support
Optum Specialty Pharmacy is always available
by phone to answer any questions you may have
about your medication, side effects and more.
The personalized support doesn’t stop there.
Virtual visits let you connect face-to-face with
your care team. Ask for a real-time video chat
with an expert in your condition. Your personal,
confidential appointment gives you as much time
as you need to ask questions from the privacy of
your home. You can even record your session to
review later or to share with your caregivers.
Video series can help you feel more connected
to others with the same condition and give you
a chance to learn more about your treatment.
Hear from other patients with your condition
about their treatment and how they are doing on
it. Video libraries are currently only available for
select conditions.
Working with your pharmacist
or nurse
Tell your pharmacist or nurse about any changes
or complications in your therapy, such as:
• Side effects
• Forgetting to take your medication
If you need help with any other health concerns,
your pharmacist or nurse can help you find
wellness management programs to help you stay
on track.
Staying on track
Quick and easy refills
A few days before your next fill, we’ll send you a
refill reminder by email, phone or text. If you aren’t
already signed up for text messages, you can sign
up by phone.
Fast, safe delivery
With Optum Specialty Pharmacy, shipping your
medication is quick, easy and safe. Refrigerated
medications will be shipped overnight to the
address you choose in a temperature-controlled
package. Others will be shipped within 1–3 days.
Supplies will also be sent at no extra cost.
Save more money
Optum Specialty Pharmacy can only fill your
specialty medications. Use your home delivery
or retail pharmacy for your non-specialty
prescriptions.
If you’re looking to save money on your
medications, finding lower-cost options and filling
your non-specialty prescriptions by mail can help.

37
Dental Benefits
Getting started with Humana dental
We’ve given you a reason to smile with a selection of four flexible
dental plans, paid through a voluntary, pretax benefit.
Register at Humana.com
As a Humana member, you have a secure website on
www.MyHumana.com called MyHumana. With MyHumana, you
have fast, easy access to your personalized benefits information.
Some of what you can do on MyHumana:
• Claims – Check if a claim has been paid along with your
estimated cost, if any
• ID cards – View, print and email up-to-date dental Humana
member ID cards
• Coverage details – Review deductibles, coverage levels and
limits
• Provider search – Use “Find a doctor” to find in-network
dentists near you
• Manage access – Give other adults on your policy permission
to access your health information
• Update your communications preferences – Select which
communications you want to receive from Humana and how
you want to receive them — via paper or email
Registering is easy
• Have your Humana member ID or Social Security number
available
• Go to www.MyHumana.com
• Select “Register” at the top of the page
• Choose “Member all other plan types”
• Fill in some basic information — like your Humana member ID
number or Social Security number, date of birth, ZIP code, and
email and click “next”
• Create a username, password and security prompt and click
“next” to finish
Also, you can download the MyHumana mobile app from the app
store on your smartphone to access plan information.
Access your digital ID Card and
keep it with you
You will have access to view and print your dental ID cards via the
Humana website or the Humana mobile app within 10 working
days of enrollment. Here’s how:
Via the website:
• Go to www.MyHumana.com and sign in/register for
MyHumana (Have your Humana member ID or Social Security
number available)
• Click “Access your ID Card” under “Tools & forms” in the lower
right of your MyHumana home page or in the page’s footer
under “Tools & Resources”
• A new window will appear with links to the ID card or proof of
coverage
• Print if desired.
Via the mobile app:
• Download the MyHumana App for iOS or Android
• Sign in using your MyHumana username and password
• Click “ID Cards” on the dashboard
• Your dental ID card information and an image of the front and
back of the ID card will be visible
Humana Customer Care
For assistance or more information on the Humana Dental benefits
simply call 1-800-233-4013 (TTY: 711), Monday through Friday, 8
a.m. to 6 p.m. Easter Time (TDD: 1-800-325-2025) to speak with a
friendly, knowledgeable Customer Care specialist, or visit
www.MyHumana.com
Humana Info Video - Click Below to View

38
Dental Benefits
The Four Dental Options Oered Are:
Managed Care Plans
Option 1 (DHMO Enhanced) & Option 2 (DHMO Basic) provide a
wide variety of benefits through your participating dentist. At the
time of service, you pay the dentist for any applicable copayments
according to your schedule of benefits.
Both plans feature:
• No primary dentist selection required
• No maximums
• No waiting periods
• No claims to file
• A large panel of providers to choose from
• Same copayment to participating general dentist or specialist
• No referrals required to see a participating specialist
• Pediatric specialist care for age 16 and under
Orthodontics
Both the DHMO Enhanced and DHMO Basic cover orthodontia
services for both adults and children. Copayments under the
DHMO Enhanced are set at $1,600 for children and adolescents;
$1,950 for adults. Copayments under the DHMO Basic are set at
$2,200 for children, $2,250 for adolescents and $2,350 for adults.
PPO Plans
Option 3 (PPO High) allows you and each covered family member
to use the dentist of your choice; however, you’ll receive a higher
level of coverage when you choose a participating dentist. There
is a deductible of $50 per person ($150 per family). There is no
deductible for preventive and diagnostic services. This plan has
an annual maximum benefit of $1,000, plus an extended annual
maximum benefit. This plan covers orthodontia for adults and
children up to the age of 18. The lifetime orthodontic maximum
benefit is $1,000 for adults and $2,000 for children.
Option 4 (PPO Low) allows you and each covered family member
to use the dentist of your choice; however, you’ll receive a higher
level of coverage when you choose a participating dentist. There
is a deductible of $50 per person ($150 per family). There is no
deductible for preventive and diagnostic services. This plan has
an annual maximum benefit of $1,000, plus an extended annual
maximum benefit. This plan does not cover orthodontic services.
Finding an in-network dentist
Go to https://www.humana.com/dental-insurance/find-a-dentist
anytime to find an in-network dentist.
Under the Network drop down box, search for a provider by
selecting one of the following networks:
Palm Beach Schools DHMO
Palm Beach Schools PPO
You can also access the list of in-network providers on your
MyHumana mobile app or by calling the customer care
number on this page.

39
Dental Benefits
*Excludes orthodontia
Preventive Coverage
Early detection is the key to preventing more serious health
conditions including diabetes, heart disease and stroke.
Humana’s enhanced preventive care benefits cover many
services to help you achieve and maintain your best oral health
and save on out-of-pocket expenses.
Our enhanced preventive care benefit covers four periodontal
maintenance cleanings, as well as three routine cleanings every
year, whichever is needed, helping you prevent oral health issues
from becoming chronic conditions. Under enhanced preventive
coverage, periodontal maintenance cleanings are covered under
preventive services.
Additional preventive care through Humana:
• Three routine cleanings per year
• Four periodontal maintenance cleaning procedures per
year—covered as a preventive service
• Oral cancer screenings for members aged 40 plus
DPPO Plan Benefit
Extended Annual Maximum*
As part of Humana’s dental PPO Plans, the Extended Annual
Maximum helps you save money by ensuring you have access
to network discounts and 30% coinsurance, even after you have
reached your annual maximum. You can achieve and maintain
your best health by getting dental care when it’s needed, before
oral health issues may aect your overall health and well-being.
With Humana’s extended annual maximum, you won’t have to put
o important dental care procedures for yourself or your covered
dependents.
Your
Dental Rates
Per pay period pre-tax
deductions are as follows:
HUMANA DHMO PLANS
(FL Only Network)
HUMANA PPO PLANS
(National Networks)
OPTION 1
DHMO ENHANCED
orthodontia
OPTION 2
DHMO BASIC
orthodontia
OPTION 3
PPO DENTAL HIGH
orthodontia
OPTION 4
PPO DENTAL LOW
24 DED 22 DED 24 DED 22 DED 24 DED 22 DED 24 DED 22 DED
Employee only
$7.56 $8.25 $5.75 $6.27 $16.78 $18.30 $13.23 $14.43
Employee + Child(ren)
$16.07 $17.52 $12.29 $13.40 $46.14 $50.33 $36.39 $39.69
Employee + Spouse*
$13.23 $14.43 $9.99 $10.90 $41.12 $44.85 $32.42 $35.36
Employee + Family*
$20.79 $22.68 $15.73 $17.16 $62.09 $67.73 $48.96 $53.40
* NOTE: Domestic partner rates will be the equivalent of the above rates. The deduction will be reflected as the employee-only pre-tax rate and the balance of the deduction will be taken
on an after-tax basis. Amounts reflected on paychecks may vary slightly due to rounding.

40
Dental Benefits
BENEFIT
(Florida Only Networks)
OPTION 1 DHMO ENHANCED OPTION 2 DHMO BASIC
YOU PAY YOU PAY
DEDUCTIBLE
Annual Deductible
None None
Calendar Year Maximum
None None
Claim Forms
None None
Primary Dentist Required
None None
PREVENTIVE & DIAGNOSTIC
Oce visit
No charge No charge
Routine exams (2 per 12 Months)
No charge No charge
Prophylaxis (cleaning) - basic (3 per 12 months)
No charge No charge
Emergency treatment (palliative)
$20 $20
X-ray - complete series including bitewings
(1 per 24 months)
No charge No charge
Fluoride application (1 per 12 months)
$10 $15
BASIC/RESTORATIVE PROCEDURES
Simple extractions
$10 $20
Amalgam fillings - 1 surface permanent
No charge No charge
Anterior Root canals (1 canal)
$100 $110
Endodontic Therapy, Premolar Tooth
$185 $185
Endodontic Therapy, Molar Tooth
$225 $245
Composite resin fillings
No charge No charge
Sealants (up to age 15)
No charge No charge
MAJOR SERVICES
Crowns - porcelain, high noble metal
$495 $500
Dentures - upper/lower
$460 each $525 each
Bridges - porcelain, base metal
$420 $425
PERIODONTICS
Periodontal Maintenance (limit 4 per year)
$0 $0
ORTHODONTICS
Pre-orthodontic treatment visit
$0 $35
Comprehensive treatment of transitional
dentition
$1,600 $2,200
Comprehensive treatment of adolescent
transitional dentition
$1,600 $2,250
Comprehensive treatment of adult dentition
$1,950 $2,350
Network Palm Beach Schools DHMO
Commonly Covered Procedures:
Sample procedure codes, see full schedule for complete listing: www.MyHumana.com

41
Dental Benefits
BENEFIT
OPTION 3 PPO HIGH OPTION 4 PPO LOW
INNETWORK OUTOFNETWORK* INNETWORK OUTOFNETWORK*
DEDUCTIBLE MAXIMUM 3 PER FAMILY CALENDAR YEAR IS JANUARY 1 DECEMBER 31
Class I
None None None None
Class II, III, IV
$50 per year, individual $50 per year, individual
Calendar Year Maximum
$1,000 + Extended Annual Maximum $1,000 + Extended Annual Maximum
Lifetime Orthodontic Maximum
$1,000 Adults / $2,000 Children Not covered Not covered
CLASS I PREVENTIVE & DIAGNOSTIC
Routine Oral Exam
100% 90% 100% 80%
X-rays (diagnostic)
100% 90% 100% 80%
Routine Cleanings
100% 90% 100% 80%
Periodontal cleanings
100% 90% 100% 80%
Fluoride treatment
100% 90% 100% 80%
Sealants
100% 90% 100% 80%
Space maintainers
100% 90% 100% 80%
Oral Cancer Screening (ages 40+)
100% 90% 100% 80%
Panoramic x-rays
100% 90% 100% 80%
CLASS II BASIC SERVICES
Emergency care for pain relief
80% 70% 50% 40%
Amalgam / Composite fillings
80% 70% 50% 40%
Oral Surgery (includes extractions)
80% 70% 50% 40%
Harmful habit appliances
80% 70% 50% 40%
Periodontics
80% 70% 50% 40%
Endodontics
80% 70% 50% 40%
CLASS III MAJOR SERVICES
Inlays/onlays/crowns & bridges
50% 40% 50% 40%
Dentures and other removable
prosthetics
50% 40% 50% 40%
Implants
50% 40% 50% 40%
CLASS IV ORTHODONTIC SERVICES
Orthodontia
50% 50% Not covered Not covered
*Out-of-network percentage is based on allowable charges.
Network Palm Beach Schools PPO
PPO Plans
Sample procedure codes, see full schedule for complete listing: www.MyHumana.com
42
Vision Benefits
Vision Care Premiums
Per pay period pre-tax payroll deductions are as follows:
FULLTIME OR
PARTTIME
EYEMED VISION
Deductions
24 22
Employee
$2.73 $2.97
Employee + Family*
$7.00 $7.64
*Amounts reflected on paychecks may vary slightly due to rounding.
Plan Provider: EyeMed Vision Care
An eye examination means more than getting a prescription; it
evaluates your eye health and is critical in the early detection of
several vision and health-related conditions, including:
• Glaucoma
• Diabetes
• Cataracts
• Hypertension
Since early detection is key for treatment, periodic eye
examinations play a vital role in ensuring the health of your eyes.
This is why EyeMed providers are dedicated to preserving your
vision by making it convenient for you to receive quality eye care.
Eye examinations are also important for the health and safety
of children. The American Optometric Association recommends
that children receive their first eye examination from an eye
care professional as early as six months of age. Afterward, your
provider will advise you when to schedule your child’s next eye
examination.
EyeMed’s thousands of provider locations allow you to begin
receiving substantial savings on your eye care and eyewear needs
at one of many locations nationwide.
Plan Features
You may choose independent ophthalmologists, optometrists,
opticians, or the convenience of a retail facility including
LensCrafters®, most Pearle Vision locations, and Target Optical
locations in your area or throughout the country for:
• Eye examinations
• Contact lenses
• Glasses
• Rx sunglasses
• Lens options and accessories or
• LASIK and PRK laser vision correction discounts.
Claim Forms
Today, with EyeMed, your explanation of benefits (EOB) is provided
online. To access your EOB, visit www.eyemed.com. If you prefer
to continue to receive a paper copy of your EOB, simply log in to
the member website to set up your preferences. You may also
call the customer care center at (866) 723-0514 to update your
preferences.
Lens Options
You can choose from many dierent lenses and lens options for
your frames at participating EyeMed provider locations. Here are
just a few of the lens options you may find at participating provider
locations:
• Ultra Violet (UV) protection – UV rays can be generated from
the sun or other light sources. With enough exposure to these
light rays, there could be an increased risk of cataracts and
macular degeneration. UV protection helps to prevent these
rays from harming the eye.
• Anti-reflective (AR) coating – This coating reduces the
amount of light that reflects o the lenses. These lenses can
be particularly helpful for driving at night, when reflections on
your lenses may be greater than daylight driving conditions.
AR coating also enables people to see your eyes more clearly
as opposed to seeing the reflection o your lenses.
• Scratch-resistant coating – When scratches are present on
your lenses, they may distort or interfere with your vision. This
protective coating is added to the lens surface to protect it
from normal scratches as a result of everyday mishaps. It’s a
great way to extend the life of your eyewear.

43
Vision Benefits
Additional Purchases and Out-of-
Pocket Discount
You will receive a 20% discount on items not covered by the plan
at participating providers, which may not be combined with any
other discounts or promotional oer; additionally, the discount
does not apply to EyeMed’s providers’ professional services or
disposable contact lenses.
Benefits are not provided for services or materials arising from:
orthoptic or vision training; subnormal vision aids and any
associated supplemental testing; aniseikonic lenses; medical and/
or surgical treatment of the eyes; corrective eyewear required by
an employer as a condition of employment, and safety eyewear;
services provided as a result of workers’ compensation law;
plano non-prescription lenses and non-prescription sunglasses
(except for the 20% EyeMed discount); two pairs of glasses in lieu
of bifocals; services or materials provided by any other group
benefit providing for vision care. Benefit allowances provide no
remaining balance for future use within the same benefit period.
Lost or broken lenses, frames, glasses, or contact lenses will not
be replaced except in the next benefit period.
Continued Eyewear Savings - Your EyeMed benefit also provides
for continued savings through our continued eyewear savings
plan. After your initial benefits have been utilized, you may receive
ongoing discounts on additional eyewear purchases at EyeMed
provider locations, which result in discounts up to 40% o the
retail price of complete pair eyeglass purchases, 20% o partial
pair purchases, and 15% o conventional contact lenses. See your
EyeMed provider for details.
To Locate an EyeMed Provider
Near You:
Visit the EyeMed website at www.eyemed.com and choose
“Select” network and enter your ZIP code to find a provider.
Enrollment of any children and a domestic partner will be the
equivalent of the above rates. The deductions will be reflected as
the employee-only pre-tax rate and the balance of the deduction
will be taken on an after-tax basis.
Customer service representatives are available to answer your
questions seven days a week, including evenings. EyeMed
oers easy-to-use benefits, with no claim forms to complete
for in-network services.
Call EyeMed customer call center at 1-866-723-0514 and choose
the “provider locator” automated option or speak to a customer
service representative during normal operating hours:
Monday–Saturday, 7:30 a.m. - 11 p.m. EST
Sunday, 11 a.m. - 8 p.m. EST
How to -
Find a Provider
• Visit the EyeMed website at www.eyemed.com
• Click “Find an Eye Doctor”
• Enter your ZIP code to find a provider
For the most updated listing for members, visit our website at
www.eyemed.com or call 1-866-723-0514.

44
Vision Benefits
EYEMED PLAN SERVICES
INNETWORK
Member Cost
OUTOFNETWORK
Maximum Reimbursement
Exam
$10 Co-Pay ($0 for Plus-Provider) $35
Retinal Imaging
Up to $39 N/A
EXAM OPTIONS
Standard contact lens fit and follow-up*
Premium contact lens fit and follow-up**
Up to $40
10% o retail price
N/A
N/A
FRAMES
$0 copay; $130 allowance;
($180 for Plus-Provider)
$65
STANDARD PLASTIC LENSES
Single vision
$15 co-pay $25
Bifocal
$15 co-pay $40
Trifocal
$15 co-pay $55
Standard progressive
$60 co-pay $55
Premium progressive
$60, 80% of charge
less $130 allowance
$55
LENS OPTIONS PAID BY THE MEMBER AND ADDED TO THE BASE PRICE OF THE LENS
Anti-reflective - Standard
$45 N/A
Photochromic - Non-Glass
20% o retail price Not Covered
Polycarbonate - Standard
$35 $3
Scratch-coating - Standard
$15 N/A
Tint (solid and gradient)
$12 $2
UV Coating
$12 $2
All other lense options
20% o retail price N/A
CONTACT LENSES INCLUDES MATERIALS ONLY; IN LIEU OF LENSES
Conventional
$0 co-pay; $125 allowance
+ 15% o balance over $125
$100
Disposables
$0 co-pay; $125 allowance
+ 100% of balance over $125
$100
Medically necessary
$0 co-pay, paid in full $200
Contact Booster
$0 co-pay; $145 allowance when lens
are purchased through contactsdirect.
com
N/A
HEARING CARE FROM AMPLIFON NETWORK
†
Up to 64% o hearing aids N/A
LASIK AND PRK VISION CORRECTION PROCEDURES
††
15% o retail price
OR 5% o promotional pricing
N/A
FREQUENCY
Exams
Once every calendar year
Frames
Once every other calendar year
Standard plastic or contact lenses
Once every calendar year
* Standard contact lens fitting - spherical clear contact lenses in conventional wear and planned replacement (Examples include but not limited to
disposable, frequent replacement, etc.)
** Premium contact lens fitting - all lens designs, materials and specialty fittings other than standard contact lenses (examples include toric, multifocal, etc.)
† Call 1 (877) 203-0675 for details & authorization.
†† LASIK and PRK correction procedures are provided by the U.S. laser network, owned by LCA-Vision. You must first call 1 (800) 988-4221 for the nearest
facility and to receive authorization for the discount.

45
Vision Benefits
EyeMed Vision Care has many
unique online capabilities,
including following:
• Locate the provider nearest you by going to
www.eyemed.com and click on “Select” network.
• View your benefits, including service eligibility and the next
date of service.
• Printable replacement ID cards.
• Online claims status.
• Ability to “go paperless” and receive explanation of benefits
electronically.
• Learn more about the importance of vision care through Vision
Wellness content.
• Access the mobile website to locate a provider, view ID cards,
benefits and contact EyeMed.
• EyeMed mobile app available for iPhone, iPad and most
Android touch users.
• Know-Before-You-Go- The newest feature that educates
employees on the cost of their purchases with their benefits
before visiting their provider!
Contactsdirect.com is an online
in-network benefit
How Does the Program Work? Three easy steps:
Use your contact lens allowance online by using your in-network
benefits. Simply go to www.contactsdirect.com. Select your lenses
from a wide selection of top selling brands. In-network benefits
instantly apply to your purchase, and contact lenses will ship as
soon as the prescription* is verified-most ship the same day.
1. Click on register in the top navigation
2. Fill out the registration form
3. Check the box to apply your vision insurance
4. www.contactsdirect.com will find your plan and apply your
vision insurance online, right in the cart. EyeMed Vision Care
oers replacement contact lenses by mail. This service option
is available to all EyeMed Vision Care members!
*Some states do not require the provider to release the prescription.
Additional services with your EyeMed Vision Plan Enrollment:
The following additional service are included with your vision plan at no added cost to you.
• ContactLens Booster
− Contactsdirect.com on-line solutions
• International Travel Solutions
− Temporary emergency glasses within 24 hours**
− 24/7 support with translation services in 160 languages
− Online directory of trusted providers in 20 countries
• Additional Saving and Resources
− Mobile App Option
− 40% additional pair discount
− Emergency Solutions for international travel
− 20% o non-prescription sunglasses
− 20% o any remaining frame balance/non covered item
− Eyesiteonwellness.com (Vision Wellness Resources)
** Available in most cases. Check your plan benefits to be sure.

46
Vision Benefits
PDF-2105-M-370
INNOVATIVE ANSWERS FOR TOTAL HEALTH & WELLNESS
Hear all the sweet
sounds of life
Hearing loss is more common than you might think. It affects 1 in 9
Americans
1
and can come on so gradually you may not even notice it.
But the good news is 95% of hearing loss can be easily treated with
hearing aids.
1
That’s why we give you access to affordable hearing care discounts
through Amplifon, the nation’s largest independent hearing discount
network — so you can enjoy all of life’s sights and sounds.
YOUR HEARING DISCOUNT THROUGH AMPLIFON INCLUDES:
64% off hearing aids at
thousands of convenient
locations nationwide
2
Discounted, set pricing on
thousands of hearing aids
60-day hearing aid
trial period with no
restocking fees
Free batteries for 2 years
with initial purchase
3-year warranty and loss
and damage coverage
Call 877.203.0675 to find a hearing care
provider near you and schedule a hearing
exam today.
SEE THE GOOD STUFF
Register on eyemed.com or grab the EyeMed app
(App Store or Google Play)
1
https://www.amplifonusa.com/hearing-loss
2
Savings based on Amplifon Hearing Health Care
average member savings data for 2020
PDF-2105-M-370
INNOVATIVE ANSWERS FOR TOTAL HEALTH & WELLNESS
Hear all the sweet
sounds of life
Hearing loss is more common than you might think. It affects 1 in 9
Americans
1
and can come on so gradually you may not even notice it.
But the good news is 95% of hearing loss can be easily treated with
hearing aids.
1
That’s why we give you access to affordable hearing care discounts
through Amplifon, the nation’s largest independent hearing discount
network — so you can enjoy all of life’s sights and sounds.
YOUR HEARING DISCOUNT THROUGH AMPLIFON INCLUDES:
64% off hearing aids at
thousands of convenient
locations nationwide
2
Discounted, set pricing on
thousands of hearing aids
60-day hearing aid
trial period with no
restocking fees
Free batteries for 2 years
with initial purchase
3-year warranty and loss
and damage coverage
Call 877.203.0675 to find a hearing care
provider near you and schedule a hearing
exam today.
SEE THE GOOD STUFF
Register on eyemed.com or grab the EyeMed app
(App Store or Google Play)
1
https://www.amplifonusa.com/hearing-loss
2
Savings based on Amplifon Hearing Health Care
average member savings data for 2020

47
Employee Wellness
Employee Wellness
The School District of Palm Beach County is committed to
helping employees adopt a healthy lifestyle and improve their
quality of life.
It has been proven that people who are healthy are more
productive, more motivated, and more satisfied at home and at
work. While our focus is to promote the health and well-being of
School District sta through education, behavior modification,
guidance, and support, Employee Wellness also produces
good role models for students while supporting high student
achievement.
Your Employee Wellness program oers many opportunities
to improve your health, including onsite screenings, health
challenges and programs, health education and benefit education,
and support.
Our goal is to keep people healthy, reduce the risk factors among
at-risk members and improve the health of those who already have
chronic conditions by encouraging them to make lifestyle changes.
To do this we give employees easy access to the resources
needed to make well-informed decisions about their health and
health care.
Key Components of Employee
Wellness
Our health promotion eorts are comprised of awareness,
educational activities, behavior or lifestyle change programs, and
the creation of supportive environments. The following highlights
some of our numerous eorts to give employees the opportunities
and information they need to be proactive and address their health
& wellness:
• Accessible physical activity & healthy eating options
• Advocacy health care help
• Apps - MyUHC, HealthAdvocate, MyHumana, EyeMed,
Headspace, AbleTo, Talkspace, and more.
• Clinical program engagement
• Community fitness events
• Diabetes prevention programs
• Disease & care management
• Employee Assistance Program
• Health & wellness seminars
• Health Rewards
• HealthyLiving-Lessons for Life Nurseline
• Healthy Pregnancy Program
• On-site health screenings & mammography, dermatology
screenings and more
• Online & telephonic health coaching
• Online health information & resources
• Preventive care campaigns
• Real Appeal weight loss program
• Sta sports program
• Stress management strategies
• Substance Use Quit Kits
• Virtual visits
• Wellness Champion Program
• Wellness newsletter
• OnePass gym membership discounts
• Onsite activities
Visit us on the HUB for more information
about our program oerings, including:
• Health Rewards
• Upcoming Wellness Events
• Monthly Health Tips
https://hub.palmbeachschools.org/all_employees/
employee_wellness

48
Wellness Services
Wellness Services to Help you Meet
your Personal Health Goals
Current members: You can access our wellness services today.
Just log in to myuhc.com® and click on “Health & Wellness,” or call
the Customer Care number on the back of your health plan ID card.
Find Support by Working with a Personal
Health Coach
If you have health risks, our health coaches may call you to oer
their support. They can set up a personal plan to help provide
health tips and coaching support, or you can call them for help in
finding ways to improve your health.
Get Help to Stop Smoking or Quit Using
Tobacco
We know it’s not easy to quit, but we’ll give you the support you
need. You’ll receive tips on how to quit, set a “quit date” and begin
a step-by-step program with access to online tools that can help
you stay on track by:
• Identifying common obstacles to quitting
• Understanding nicotine replacement therapy options
• Dealing with temptations and preventing relapse.
Learn How We Can Help You Lose Weight
There are real advantages to losing weight. Being overweight
can lead to diseases, such as heart disease, diabetes, high blood
pressure and high cholesterol. Our online health coaches will
guide you through a staged approach to learning about proper
nutrition and how to plan healthy meals.
• Learn dierent ways to lose weight.
• Plan more nutritional meals.
• Manage your exercise and track your progress.
• Avoid temptations.
Tobacco Use Comes with a Surcharge -
Quit to Save Your Health, and Save Dollars
in the Future
Avoid premium surcharges!
You know that tobacco is bad for you. So, why not quit? It’s hurting
your health, draining your wallet and leaving you behind in a world
that’s becoming tobacco-free. We encourage you to take steps to
quit and save on premium dollars in the future. Also, think of the
added saving you will have when you no longer spend money to
buy tobacco products. The potential savings are waiting for you.
How Does it Work?
The School District of Palm Beach County asked that each
employee log in to PeopleSoft and click on the My Benefits tile.
Click the Wellness Rewards and Surcharge option to review
or update your tobacco status. You only need to provide this
information once, unless you have a change in your tobacco status
while at the District.
Tobacco users (or those who fail to indicate their tobacco status)
will have a $50 per month surcharge added to their medical
premium. We encourage you to take steps to quit and save in the
future. If you are not a tobacco user, you will not have monthly
tobacco charges added to your insurance premium payroll
deduction. If you start using tobacco products, you must notify Risk
& Benefits Management for a classification change.

49
Flexible Spending Accounts (FSAs)
What is a Flexible Spending Account
(FSA)?
FSAs are tax-advantage account that let you use pre-tax
dollars to pay for eligible medical expenses.
FSAs Feature:
• IRS approved reimbursement of eligible expenses
tax-free
• Per-pay-period deposits from your pre-tax salary
• Savings on income and Social Security taxes
• Security of paying anticipated expenses with your FSA
Is an FSA Right for Me?
If you spend any money on recurring eligible expenses
during your plan year, you may save money by paying for
them with an FSA. A portion of your salary is deposited into
your FSA each pay period.
• Decide the amount you want deposited.
• You are reimbursed for eligible expenses before income
and Social Security taxes are deducted.
• Save income and Social Security taxes each time you
receive wages.
• To estimate potential savings based on your income and
expenses, use the Tax Savings Calculator at
www.tasconline.com/tasc-calculators/tasc-flexsystem-
calculator/
What Types of FSAs Are Available?
The School District of Palm Beach County oers you a
Health Care FSA as well as a Dependent Care FSA. If you
incur both types of expenses during a plan year, you can
establish both types of FSAs.
Health Care FSA
A health FSA is a tax-favored account that pays for or
reimburses the qualified medical expenses of an employee
and his or her dependents, including:
• Prescription drugs
• Eyeglasses
• Orthodontia
Dependent Care FSA (day care/elder care)
Dependent Care FSAs are tax-advantaged accounts that let
you use pre-tax dollars to pay for eligible dependent care
expenses. A qualifying ‘dependent’ may be a child under
age 13, a disabled spouse, or an older parent in eldercare.
Eligible expenses include:
• Daycare
• Nursery School Preschool
• Summer Day Camp
• Before or After School Programs
• Elder Day Care.
Receiving Reimbursement
Complete and properly submitted claim forms are generally
process for reimbursement within five business days.
To avoid delays, follow the instructions for FSA claims
submissions.
Direct Deposit
Enroll in direct deposit to expedite the time of your
reimbursement.
• Enroll in Direct Deposit by accessing your participant
portal at http://www.tasconline.com or by contacting
TASC Customer Care at 1-800-422-4661.
• FSA reimbursement funds are automatically deposited
into your checking or savings account within 48 hours of
your claim approval.
• There is no fee for this service.
NOTE: Processing your FSA direct deposit enrollment may
take between four and six weeks.
FSA Grace Period
An IRS Revenue Notice permits a “grace period” of two
months and 15 days following the end of your 2024 plan
year (December 31, 2024) for an FSA. This grace period
ends on March 15
th
, 2025. During the grace period, you
may incur expenses and submit claims for these expenses.
Your TASC card cannot be used for transactions during the
grace period. Funds will be automatically deducted from
any remaining dollars in your 2024 Health Care FSA or
Dependent Care FSA.
You should not confuse the grace period with the plan’s
“run-out period”. The run-out period extends until March
31
st
, 2025. This is a period for filing claims incurred anytime
during the 2024 plan year, as well as claims incurred during
the grace period mentioned above.
Claims will be processed in the order in which they are
received, and your accounts will be debited accordingly.
This is true for both paper claims and TASC Card
transactions. If you have funds remaining in an account
for the prior plan year, these funds will be used first until
exhausted. Then subsequent claims will be debited from
your new plan year account balance.
Will Contributions Aect My Income Taxes?
Salary reductions made under a cafeteria plan, including
contributions to one or both FSAs, will lower your taxable
income and taxes. These reductions are one of the money-
saving aspects of starting an FSA. Depending on the state,
additional state income tax savings or credits may also be
available. Your salary reductions will reduce earned income
for purposes of the federal Earned Income Tax Credit (EITC).

50
Flexible Spending Accounts (FSAs)
To help you choose between the available taxable and
tax-free benefits, or a combination of both, consult your tax
adviser and/or the IRS for additional information.
Where Can I Get Information About FSAs?
If you have specific questions about FSAs, contact the
Customer Service department. Visit www.tasconline.com
or call TASC Customer Service at 1-800-422-4661.
NOTE: your account information will not be discussed with
others without your verbal or written authorization.
How Do I Get the Forms I Need?
Log in to www.tasconline.com to obtain:
• Claim forms
• A letter of medical need
• Direct deposit form
For more information call TASC Customer Service at
1-800-422-4661 for further assistance.
FSA Guidelines:
1. The IRS does not allow you to pay your medical or other
insurance premiums through either type of FSA.
2. You cannot transfer money between FSAs or pay a
dependent care expense from your Health Care FSA or
vice versa.
3. You have a 90-day run-out period (until March 31, 2024)
at the end of the plan year for reimbursement of eligible
FSA expenses incurred during your period of coverage
and any applicable grace period within the 2023 plan
year.
4. You may not receive insurance benefits or any other
compensation for expenses that are reimbursed through
your FSAs.
5. You cannot deduct reimbursed expenses for income
tax purposes.
6. You may not be reimbursed for a service that you have
not yet received.
7. You may only be reimbursed for expenses incurred
while you are actively enrolled and making
contributions.
8. Be conservative when estimating your medical and/or
dependent care expenses for the 2024 plan year. IRS
regulation states that, any unused funds remaining in
your FSA account after plan year and any applicable
grace periods ends, and all reimbursable requests have
been submitted and processed, cannot be returned to
you or carried forward to the upcoming plan year.
9. When enrolling in either or both FSAs, written notice of
agreement with the following will be required:
• I will only use my FSA to pay for IRS-qualified expenses
eligible under my employer’s plan, and only for my IRS-
eligible dependents and myself.
• I will exhaust all other sources of reimbursement,
including those provided under my employer’s plan(s),
before seeking reimbursement from my FSA.
• I will not seek reimbursement through any additional
source.
• I will collect and maintain sucient documentation to
validate the foregoing.
PRETAX BENEFITS SAVINGS EXAMPLE
(With
FSA)
(Without
FSA)
$30,000 Annual Gross Income $30,000
- $2,700 FSA Contributions - $0
$27,300 Taxable Gross Income $30,000
- $3,689 Est. Federal & Social Security Taxes* - $4,845
$23,611 Annual Net Income $25,155
- $300
Eligible out-of pocket medical and
dependent care expenses
- $3,000
$23,311 Spendable Income $22,155
By using an FSA to pay for anticipated recurring expenses, you
convert the money you save in taxes to additional spendable
income. That’s a potential annual savings of:
+ $1,156!
*Assumes standard deductions and four exemptions

51
Health Care FSA
What is a Health Care FSA?
A Health Care FSA is an IRS tax-favored account you can use
to pay for your eligible medical expenses not covered by your
insurance or any other plan. These funds are set aside from your
salary before taxes are deducted, allowing you to pay your eligible
expenses tax-free.
Whose expenses are eligible?
Your Health Care FSA may be used to reimburse eligible
expenses incurred by:
• Yourself • Your spouse
• Your qualifying children • Your qualifying relative
When Are My Funds Available?
Once you sign up for a Health Care FSA and decide how much
to contribute, the maximum annual amount of reimbursement for
eligible health care expenses will be available throughout your
period of coverage.
Since you don’t have to wait for the cash to accumulate in your
account, you can use it to pay for your eligible health care
expenses at the start of your deductions.
How Do I Request Reimbursement?
• Simply log in to your TASC account and click the request a
reimbursement button and follow the steps for the fastest
possible claims reimbursement. Alternatively TASC also has
manual claim forms available by contacting Customer Care at
1-800-422-4661.
PLEASE NOTE that canceled checks or credit card receipts
(or copies) listing the cost of eligible expenses are not valid
documentation for Health Care FSA reimbursement.
Fax TOLL-FREE to: 608-661-9601
Mail to TASC:
TASC
PO Box 7308
Madison, WI 53707-7308
*EOBs are not required if your coverage is through an HMO.
Card
Experience
The hassles of carrying
multiple cards and trying
to remember which card
pays for what are a thing
of the past with the
TASC Card. Just swipe
this stacked card at the
point of purchase and eligible expenses are paid automatically with
smart technology to know which account to draw funds from. Every
participating employee receives a TASC Card and has access to
several value-added card features:
TASC Card Decline Protection
As a bonus, each TASC Card comes with card decline protection
which means participants never have to deal with the hassle
or embarrassment of having a card declined due to insucient
funds in a benefit or MyCash account. And if a participant doesn’t
have enough funds to cover a purchase, TASC will approve the
transaction and pay the dierence, then be reimbursed from the
participant’s bank account (up to a pre-authorized amount) linked
to their TASC Card.
My Cash
When it’s necessary to pay out-of-pocket and request a
reimbursement, we make sure participants get their money
back fast with MyCash. TASC deposits reimbursement payments
directly into the linked MyCash account within 12 hours—faster
than the speed of bank direct deposit. Participants can then
use MyCash funds to cover non-benefit expenses everywhere
Mastercard® is accepted or withdraw as cash from an ATM.
TASC Card Lock
If a TASC Card is lost or stolen, the participant can quickly disable
it with TASC Card Lock online or via the TASC mobile app. If found,
simply unlock the card to use it again.
TASC Wallet
This convenient organizer oers mobile and web access to the
TASC Card with features like:
Card Management. Stores image of TASC Card; lets participants
lock a card, report lost/stolen cards, or request more cards.
Card Holder. Stores digital images of other important cards
(insurance cards, rewards cards – even a gym membership card).
The TASC Card is backed with seamless cross-channel customer
care. Participants can get the help they need to manage their
benefits and TASC Card through our website, mobile app, or call
center.
Minimum Annual Deposit: $300
Maximum Annual Deposit: Up to IRS
Published Maximum

52
Dependent Care FSA
What Is a Dependent Care FSA?
A Dependent Care FSA is an IRS tax-favored account you can use
to pay for your eligible dependent day care expenses to ensure
your dependents (child or elder) are taken care of while you and
your spouse (if married) are working. These funds are set aside
from your salary before taxes are deducted, allowing you to pay
your eligible expenses tax-free.
Whose Expenses Are Eligible?
You may use your Dependent Care FSA to receive reimbursement
for eligible dependent day care expenses for qualifying individuals.
A qualifying individual includes a qualifying child,
if he or she:
• Is a U.S. citizen, national or a resident of the U.S., Mexico
or Canada
• Has a specified family-type relationship to you
• Lives in your household for more than half of the taxable year
is 12 years old or younger and
• Has not provided more than one-half of his or her own support
during the taxable year
A qualifying individual includes your spouse,
if he or she:
• Is physically and/or mentally incapable of self-care
• Lives in your household for more than half of the taxable year
• Spends at least eight hours per day in your home
A qualifying individual includes your qualifying
relative, if he or she:
• Is a U.S. citizen, national or a resident of the U.S., Mexico
or Canada
• Is physically and/or mentally incapable of self-care
• Is not someone else’s qualifying child
• Lives in your household for more than half of the taxable year
• Spends at least eight hours per day in your home and
• Receives more than one-half of his or her support from you
during the taxable year
NOTE: Only the custodial parent of divorced or legally-separated
parents can be reimbursed using the Dependent Care FSA.
What Is My Maximum
Annual Deposit?
• If you are married and filing separately, your maximum annual
deposit is $2,500.
• If you are single and head of household, your maximum
annual deposit is $5,000.
• If you are married and filing jointly, your maximum annual
deposit is $5,000.
• If either you or your spouse earn less than $5,000 a year,
your maximum annual deposit is equal to the lower of the two
incomes.
• If your spouse is a full-time student or incapable of self-care,
your maximum annual deposit is $3,000 a year for one
dependent and $5,000 a year for two or more dependents.
When Are My Funds Available?
Once you sign up for a Dependent Care FSA and decide how
much to contribute, unlike a Health Care FSA, your maximum
contribution amount will not be available during the plan year, but
rather after your payroll deductions are received.
How Do I Request Reimbursement?
Simply log in to your TASC account and click the request a
reimbursement button and follow the steps for the fastest possible
claims reimbursement. Alternatively TASC also has manual claim
forms available by contacting Customer Care at 1-800-422-4661.
Fax TOLL-FREE to: 608-661-9601
Mail to TASC:
TASC
PO Box 7308
Madison, WI 53707-7308
To help you choose between the available taxable and
tax-free benefits, or a combination of both, consult your tax
adviser and/or the IRS for additional information.
You may also visit irs.govand www.tasconline.com to
complete a tax savings analysis.

53
Accessing FSA Benefits
Customer Care oers you a variety of resources to make inquiries
on your benefits and Flexible Spending Accounts (FSAs), including
information from the WageWorks website and Customer Care.
On the Web and Mobile App
TASC’s web and mobile tools ensure easy access, account
management, and benefit fund security for our customers.
TASC Card Lock. All participants receive a TASC Card to access
their benefit funds. If a card is lost or stolen, TASC Card Lock lets
them disable a card in seconds from the TASC website or mobile
app—and unlock it once it’s found.
Fingerprint (Touch ID) and Facial Recognition. These capabilities
protect participant account information without the hassle of
remembering another password.
Picture to Pay. Take a picture of an eligible benefit expense then
submit it via the TASC mobile app. There are no forms to fill out
and no need to sign in to a website. Just click and submit and we’ll
take care of the rest.
Expense Eligibility Check. Not sure an item is eligible for
reimbursement? Find out in seconds on the app. It’s the quickest
way to make sure benefits are being spent correctly.
Mobile Alerts
1
. Participants are notified when we’ve received a
request and when it’s been paid, making it easy to stay on top of
account activity and available funds.
1
Standard message and data rates may apply.
Pay the Provider. Instead of paying out of pocket and waiting to be
reimbursed, participants can use their TASC Card to pay for eligible
expenses, or they can use our convenient web payment feature.
Simply scan or take a picture of the provider bill and upload it.
TASC will then pay the bill directly from the appropriate benefit
account.
Email Alerts. Participants are notified when requests are received
and paid, making it easy to stay on top of account activity and
available funds.
Seamless Account Management. Our website, mobile app,
and customer care call center make it easy for participants to
manage their account and get the support they need, anytime
and anywhere! Plus, account information is connected across all
platforms, which means participants don’t have to re-enter data or
restart a process between devices.
Access to Individual Giving Accounts. TASC believes in giving
back to the community and that’s why every participant receives
a complimentary giving account. They can designate a regular
payroll deduction or do one-time transfers from their bank or
MyCash account and select favorite charities to allocate donations
to – all via the TASC website or mobile app. And with no fees
to use the giving account, 100% of donations go to designated
causes.
TASC Wallet. These user-friendly features make benefits
management simple and fast:
• ATM Locator. Finds the nearest ATM to withdraw cash from
MyCash account via TASC Card.
• Card Management. Stores image of TASC Card; lets participants
lock a card, report lost/stolen cards, or request more cards.
• Card Holder. Stores digital images of other important cards
(insurance cards, rewards cards – even a gym membership card).
• Receipt Repository. Keeps benefits-related receipts in one
convenient place.

54
Special Retirement Plan
What Is the Special Retirement
Plan?
This Special Retirement Plan is for those employees who are
eligible for medical insurance through the District, but because
they have other medical insurance, waive their medical coverage.
Instead these employees receive 401(a) dollars which are
deposited into the BENCOR special retirement plan. This plan is a
tax-deferred retirement plan, in which you may direct where funds
are deposited by choosing from investment options.
The BENCOR 401(a) Special Retirement Plan is tax qualified under
Internal Revenue Code Section 401(a). BENCOR Administrative
Services provides a full range of administrative services to the
BENCOR 401(a) Special Retirement Plan and its participants.
Plan Provider: BENCOR
A 401(a) Special Retirement Plan is a benefit option you have as
you create your benefits package. Only 401(a) Dollars can be
deposited into this account.
How Much Money Can I Contribute?
The District will contribute 100 percent of the value of your 401(a)
Dollars into this plan. Unfortunately, no other dollars can be used
to fund this 401(a) Special Retirement Plan.
Am I Eligible for 401(a) Dollars and
Medical Coverage as a Dependent?
If you have medical coverage other than a District plan (i.e., under
another employer’s plan or a retirement plan), you may waive the
school District’s coverage and receive $100 401(a) Dollars per
month ($50 per month if you are a part-time eligible employee).
However, you are not eligible for the 401(a) Dollars if you are
covered as a dependent by another District employee.
How Does It Work?
If you elected to participate in this tax-advantaged plan, the District
will make monthly contributions on your behalf. All contributions to
the BENCOR Plan are made on a pre-tax basis. You will never pay
Social Security or Medicare taxes on plan contributions. Income
taxes are deferred until withdrawals are made.
Contributions are allocated to an individual account in your name
and initially deposited in a guaranteed or fixed account. You will
be able to direct how the money is invested from a menu of 17
dierent funds with a wide range of investment objectives. You
also have the ability to change the investment choices. You may
change your investment options online at: www.bencorplans.com
When you retire or otherwise terminate employment with the
District, your accumulated account balance may remain in the plan
or be distributed to you in a lump sum cash payment or transferred
to an IRA or another retirement plan. You pay income taxes only
when you receive a cash distribution. No taxes are imposed when
the contributions are made or until earnings are actually paid to
you. Thus, the BENCOR Special Retirement Plan oers you an
excellent tax deferral opportunity.
When Do I Receive Statements?
Statements are sent semi-annually. You may enroll in
e-statements online to save time, paper and ink.
How Do I Access My Account?
Go to www.bencorplans.com, click on “Participant Log On,” then
select the “Get Started box and follow the prompts to create your
personalized user ID and password.
Be sure to designate your beneficiary and select your investment
options online at: www.bencorplans.com
Features of the Participant Website
• Unit Values
• Account Balance
• Account Balance by Fund
• Fund Transfers
• Online Beneficiary Designation
• Download Forms
• Investment Fund Objectives
• Fund Performance
• Address Changes
• Investment Allocation Changes
• Transaction History
• Plan Overview
How Can I Get More Information?
Contact Bencor Administrative Services at 1-866-296-9712, or
email: [email protected]

55
Disability Income Protection
Plan Provider: Metropolitan Life
Insurance Company (MetLife)
Your greatest asset is your ability to earn a living. What if you lost
your ability to work? You may be eligible to replace a portion of
your income if you become disabled due to a covered accident or
illness.
You may select the Short-Term Disability Plan (STD) or Long-Term
Disability Plan (LTD), or both. These benefits work in conjunction
with, and not in addition to, sick leave. Premiums are based on
your age and salary and will be updated as these may change.
About the Plan Provider
MetLife underwrites the Short-Term and Long-Term Disability Plans.
If you have any questions regarding these plans or need to file a
claim, then please call MetLife at 1-800-300-4296 between 8 a.m.
and 11 p.m. ET, Monday through Friday.
The Disability Certificate issued by MetLife is available at:
https://hub.palmbeachschools.org/all_employees/benefits/disability
Eligibility
This program is available to employees who:
• Are actively at work
• Work full time or at least 40 hours per week for all
regular employees or 18.75 hours per week for
those in the CTA bargaining group
• Meet the eligibility requirements of the school
District.
You may elect this coverage during the Open Enrollment period or
within the first 30 days of your employment date.
Earning/Salary Definition
For the purpose of disability premiums and benefit determinations,
earnings or salary includes most year-round supplements
limited to:
• Degree supplements
• Complexity level supplements
• Retention supplement (subject to renewal of tax referendum)
• Shift dierentials
• Supervisory supplements and certifications
• Other salary included in the District’s multiple components
of pay
Please refer to the certificate issued by MetLife for further information.
Provisions Aecting the STD
and LTD Plans
Elimination Period – The time between the start of the disability
and the date the benefit payments begin. This will vary for each
person in the STD Plan based on the plan that you choose.
Maternity Benefits – Disability caused by pregnancy is
covered the same as sickness, and as with other sicknesses,
is subject to both the pre-existing exclusion clause as well as
the 7-day, 14-day, or 60-day elimination period during which no
benefits are payable (Short-Term Disability only).
Integration – The benefits will be reduced by other
sources of income the employee receives. Examples of other
sources of income include: retirement benefits, Social Security and
workers’ compensation. A more detailed explanation is available in
the certificate issued to all participants.
Waiver of Premium – This provision applies to LTD disability
coverage only, and the premium that is waived is Life Insurance
Coverage. You do not pay premiums while disability benefits are
payable. Premiums are waived beginning with the next premium
due date following the completion of the elimination period, which
is usually six months (or when you are notified by MetLife’s Claims
Department).

56
Disability Income Protection
Benefits for Mental Illness,
Alcoholism, or Drug Abuse
Benefits are payable for a limited period.
Please refer to the disability certificate issued by MetLife for
further information.
Short-Term Disability Plan
The Short-Term Disability (STD) Plan is designed to oer temporary
income protection. You have three options from which to
choose. Each plan provides coverage for up to 26 weeks (unless
otherwise stated in the disability certificate issued by MetLife).
Commencement of benefit and benefit amount depends on which
option you choose. Refer to the chart in this section to determine
which option best fits your needs. The maximum benefit under this
plan is $2,500 per week. An employee cannot collect sick pay and
STD benefits at the same time.
Definition of Disability
Disabled or disability means that, due to sickness or as a direct
result of accidental injury:
• You are receiving appropriate care and treatment and
complying with the requirements of such treatment; and
• You are unable to earn more than 80% of your pre disability
earnings at your own occupation for any employer; and unable
to perform each of the material duties of your own occupation.
If your occupation requires a license, the fact that you lose your
license for any reason will not, in itself, constitute disability.
What’s Not Covered
A benefit will not be paid for any disability caused or
contributed to by:
• War, whether declared or undeclared, or act of war,
insurrection, rebellion, or terrorist act;
• Active participation in a riot;
• Intentionally self-inflicted injury;
• Attempted suicide;
• Commission of or attempt to commit a felony;
• Any injury or illness for which the employee is eligible to
receive benefits under workers’ compensation or a similar law.
A benefit will not be paid for any disability caused or contributed to
by elective treatment or procedures such as:
• Cosmetic surgery or treatment primarily to change
appearance;
• Sex-change surgery;
• Reversal of sterilization;
• Liposuction;
• Visual correction surgery;
• In vitro fertilization, embryo transfer procedure, or
artificial insemination.
NOTE: Pregnancies and complications from any of these
procedures will be treated as a sickness.
When Coverage Ends
Coverage ends on the earliest:
• Date group policy ends;
• Date insurance ends for employee’s class;
• End of period for which premium has been paid;
• Date employee ceases to be eligible;
• Date employment ends;
• Date employee retires.
Preexisting Condition
The STD Plan contains a preexisting condition limitation which will
not pay benefits for any disability that results from, or is caused or
contributed to by, a preexisting condition, unless at the time
you became disabled:
• You have not received medical care for the condition for six
months while insured under the plan; or,
• You have been continuously insured under the plan for 12
months.
Preexisting Condition Means a
Sickness or Accidental Injury for
which you
• Received medical treatment, consultation, care, or services;
• Took prescription medication or had medications prescribed; or
• Had symptoms or conditions that would cause a reasonably
prudent person to seek diagnosis, care or treatment; in the
six months before your insurance under this certificate
takes eect.
DISABILITY
OPTION
% OF WEEKLY
INCOME
ACCIDENT SICKNESS
A
66
2
/3 % 1st day* 8th day*
B
60% 15th day* 15th day*
C
60% 61st day* 61st day*
* Except as otherwise stated in the disability certificate issued by MetLife.
Important:
Your premium and any benefit will be based on your salary,
which includes:
(1) Degree supplements;
(2) Other eligible supplements;
(3) Complexity level supplements, etc.
Your salary is annualized then divided by 52 to determine
your weekly salary.

57
Disability Income Protection
What is the Definition of Disability?
Disabled or disability means that, due to sickness or as a direct
result accidental injury:
• You are receiving appropriate care and treatment and
complying with the requirements of such treatment; and
• You are, during the elimination period and the next 60 months
of sickness or accidental Injury:
• Unable to earn more than 80% of your predisability earnings at
your own occupation for any employer in your local economy;
and,
• Unable to perform each of the material duties of your own
occupation; and
You are, after such period:
• Unable to earn more than 60% of your predisability earnings at
any gainful occupation for any employer in your local economy;
and,
• Unable to perform the duties of any gainful occupation for
which you are reasonably qualified taking into account your
training, education and experience.
If your occupation requires a license, the fact that you lose your
license for any reason will not, in itself, constitute disability.
When to Submit a Short-Term
Disability Claim
You should file your claim with MetLife if you anticipate being
disabled or are disabled and will be unable to work for a period
of time that exceeds the elimination period you selected during
enrollment.
How to Submit a Short-Term
Disability Claim
You may initiate your claim by calling MetLife’s toll-free telephonic
claim intake number at 1-800-300-4296 and report your claim. You
will not need to submit a paper claim form as MetLife’s clinical intake
specialist will take your information by phone. However, it will be
your responsibility to provide an authorization form to your doctor to
be signed/dated and faxed or mailed to MetLife. This allows MetLife
to access your medical information in order to process your claim.
Recurrent Disability
A recurrent disability is a disability that is related to, or due to,
the same cause or causes of a prior disability for which a monthly
benefit was paid. A recurrent disability will be treated as part of
the prior disability and you will not have to complete another
elimination period if, after receiving disability benefits under the
plan, an employee returns to work on a full-time basis for less than
six months and performs all of the duties of the employee’s own
occupation. If You return to Active Work for a period of 90 days or
less, and then become Disabled again due to the same or related
Sickness or accidental injury, We will not require You to complete
a new Elimination Period. Benefit payments will be subject to the
terms of the plan for the prior disability.
When to Submit a Long-Term
Disability Claim
If you are enrolled for STD, the transition process to LTD is
automated – you do not need to file a separate claim form.
If you are not enrolled in the STD Plan and have enrolled in the LTD
Plan only, you should file your claim with MetLife halfway through
your LTD elimination period (on or around the 90th day).

58
Disability Income Protection
Long-Term Disability Plan
The Long-Term Disability (LTD) Plan is designed to oer financial
protection for you and your family. Features include:
• a benefit amount of up to 60% of your predisability
monthly Salary;
• the greater of the Short Term Disability Maximum Benefit
Period or 180 Days
• a minimum monthly benefit of the greater of $100 or 10%
of the benefit based on monthly income loss before the
deduction of other income benefits; and,
• a maximum monthly benefit amount of $12,500.
How to Submit a Long-Term
Disability Claim
If you are enrolled in STD and switch to LTD, the transition process
for a claim is automated by MetLife’s claim system. A separate LTD
claim form is not needed if you have already filed a claim under
the STD plan during the transition. However, you must complete
a claimant questionnaire. It is required and requests information
about other income/oset information, past work experience/
education and medical providers. MetLife may also obtain
additional information from the School District of Palm Beach
County.
If you did not enroll in the Short-Term Disability plan and have
enrolled in the Long-Term Disability plan only, you may file a claim
telephonically by calling MetLife at 800-300-4296.
What Benefits are Included in Long-
Term Disability?
AGE ON DATE OF
YOUR DISABILITY
BENEFIT PERIOD
Less than 63
The Later of your Normal
Retirement Age or 42 months
63
The Later of your Normal
Retirement Age or 36 months
64
30 months
65
24 months
66
21 months
67
18 months
68
15 months
69 and over
12 months
If you become disabled, the following benefits can help until you
get back to full-time work.
Work Incentive Benefit – When a medical provider states
specific medical restrictions, MetLife’s Rehabilitation team will work
with employees who cannot do their own job, assisting them to
be employable. During this time, if approved, a portion of benefits
may be payable.
Rehabilitation and Return to Work Assistance – MetLife
vocational rehabilitation experts provide qualified employees with
formalized assessment and planning as well as financial support
to help you return to productive, independent lifestyles. Monthly
benefit is increased by 10 percent while participating in a MetLife
approved rehabilitation program.
Moving Expense Incentive – Reimburses claimants for expenses
associated with moving to a new residence if recommended as
part of an approved MetLife rehabilitation — no dollar maximum or
minimum distance requirement.
Worksite Modification Benefit – Assists the School District
of Palm Beach County with the cost of making job modifications/
accommodations and supports compliance with the American with
Disabilities Act (ADA). The job modifications/accommodations have
no stated dollar maximum or number of occurrences limit.
Worksite Modification Benefit and Survivor Benefit – Up to $400
per month per eligible family member for 24 months (no aggregate
dollar or family number maximums) while employee is participating
in approved MetLife Rehabilitation Program. Cannot be paid after
the maximum benefit period ends.
Survivor Benefit – If you were receiving a monthly disability
benefit at the time of your death, we will pay a survivor income
benefit, when we receive proof satisfactory to us:
1. Of your death; and
2. That the person claiming the benefit is entitled to it.
Designated Beneficiary – We must receive the satisfactory
proof for survivor income benefits within one year of the date of
your death.
Upon Your death, We will pay any amount that is or becomes
due to Your designated Beneficiary. If there is no Beneficiary
designated or no surviving designated Beneficiary at Your death,
we may determine the Beneficiary for any amount that is or
becomes due, according to the following order:
1. Your Spouse, if alive;
2. Your child(ren), if there is no surviving Spouse;
3. Your estate, if there is no such surviving child.
However, we will first apply the survivor income benefit to any
overpayment which may exist on your claim.
NOTE: These product descriptions do not constitute an insurance
certificate or policy. The information provided is intended only to
assist in the selection of benefits. Final determination of benefits,
exact terms and exclusion of coverage for each benefit plan are
contained in certificates of insurance issued by the participating
insurance companies.
Certificate(s) of coverage for your insurance benefits are available
to you online throughout the year. A hard copy of these certificates
will not be mailed to you automatically. Your Certificate(s) of
coverage are document(s) issued by the insurance company for
benefits registered with the state of Florida. These documents are
available for the benefits you selected during Open Enrollment or
as a new employee.
To view or print a copy of a certificate of coverage, visit:
https://hub.palmbeachschools.org/all_employees/benefits/disability

59
Disability Income Protection
DISABILITY INCOME PROTECTION PROGRAM RATES:
24 Payroll Deductions Per Year For Employees
How to Estimate Payroll Deduction Based on
24 Payroll Deductions Per Year (for Employees
Receiving 26 Payroll Checks Per Year)
SHORTTERM LONGTERM
1. Enter Annual Salary
$ $
2. Divide by 100
$ $
3. Multiply by your appropriate rate below
$ $
4. Divide by number of payroll deductions/year
$ $
Example:
SHORTTERM LONGTERM
A. Enter Annual Salary
$20,000.00 $20,000.00
B. Divide by 100
$200.00 $200.00
C. Multiply by your appropriate rate below
($0.611 for STD / $0.317 for LTD)
$122.20 $63.40
D. Divide by 24 (number of payroll deductions/yr)
$5.09 $2.64
SHORTTERM DISABILITY MONTHLY RATES
Rates per $100 of Covered Payroll
EMPLOYEE’S
AGE
OPTION A OPTION B OPTION C
54 & Under
$0.611 $0.423 $0.334
55 - 59
$0.804 $0.548 $0.438
60 - 64
$0.923 $0.628 $0.503
65 & Over
$1.122 $0.771 $0.611
LONGTERM DISABILITY MONTHLY RATES
EMPLOYEE’S
AGE
RATES PER $100 OF
COVERED PAYROLL
24 & Under
$0.037
25 - 29
$0.048
30 - 34
$0.074
35 - 39
$0.121
40 - 44
$0.169
45 - 49
$0.227
50 - 54
$0.317
55 - 59
$0.369
60 & Over
$0.385
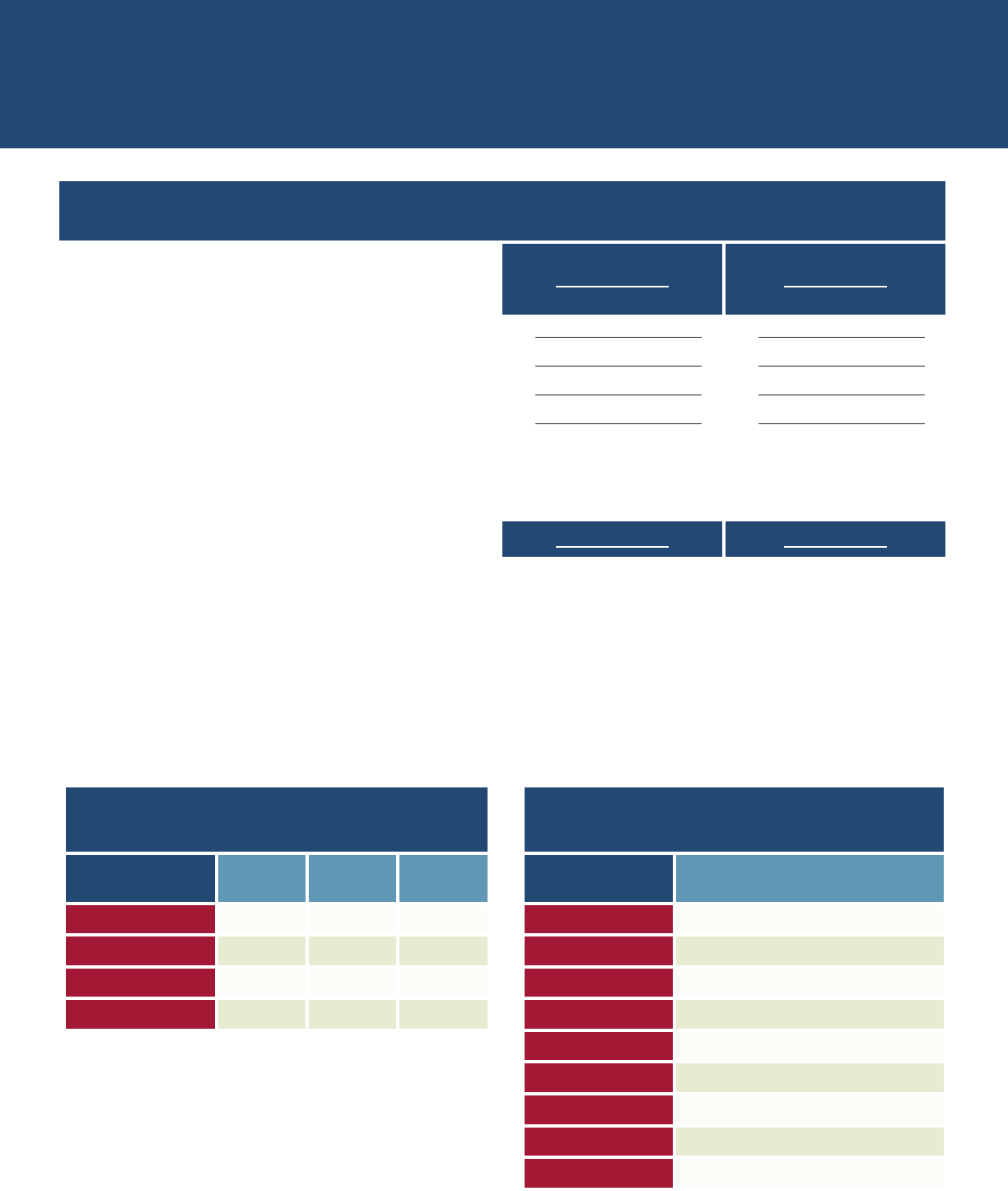
60
Disability Income Protection
DISABILITY INCOME PROTECTION PROGRAM RATES:
22 Payroll Deductions Per Year For Employees
How to Estimate Payroll Deduction Based on
22 Payroll Deductions Per Year
SHORTTERM LONGTERM
1. Enter Annual Salary
$ $
2. Divide by 100
$ $
3. Multiply by your appropriate rate below
$ $
4. Divide by number of payroll deductions/year
$ $
Example:
SHORTTERM LONGTERM
A. Enter Annual Salary
$20,000.00 $20,000.00
B. Divide by 100
$200.00 $200.00
C. Multiply by your appropriate rate below
($0.722 for STD/ $0.3746 for LTD)
$144.40 $72.92
D. Divide by 22 (number of payroll deductions/yr)
$6.56 $3.31
SHORTTERM DISABILITY MONTHLY RATES
Rates per $100 of Covered Payroll
EMPLOYEE’S
AGE
OPTION A OPTION B OPTION C
54 & Under
$0.722 $0.500 $0.395
55 - 59
$0.950 $0.648 $0.518
60 - 64
$1.091 $0.742 $0.594
65 & Over
$1.326 $0.911 $0.722
LONGTERM DISABILITY MONTHLY RATES
EMPLOYEE’S
AGE
RATES PER $100 OF
COVERED PAYROLL
24 & Under
$0.0437
25 - 29
$0.0567
30 - 34
$0.0875
35 - 39
$0.1430
40 - 44
$0.1997
45 - 49
$0.2683
50 - 54
$0.3746
55 - 59
$0.4361
60 & Over
$0.4550

61
Basic Life Insurance
Post-tax Benefits
Plan Provider: Underwritten by Metropolitan Life Insurance
Company (MetLife).
The School District of Palm Beach County is always looking for
ways to improve your benefits plan and wants you to have the
opportunity to apply for the life insurance you need at a price you
can aord. Getting the income protection needed to guard against
life’s uncertainties should not be dicult or expensive. That’s
why the School District of Palm Beach County is oering you a
life benefits plan from MetLife. This coverage is designed to help
provide your family with a financial foundation that you can build
upon. You have the opportunity to benefit from all that MetLife
oers, including:
• Basic Life Insurance and Personal Accident Insurance
(employer paid);
• Optional Life Insurance and Optional Accident Insurance
(employee paid);
• Spouse Life Insurance and Optional (Spouse) Accident
Insurance (employee paid);
• Child Life Insurance (employee paid).
Basic Life Insurance
Protecting your family’s future is no doubt one of your highest
priorities. One way to help achieve this goal is through life
insurance. The School District of Palm Beach County provides you
with a valuable basic life insurance plan at no cost to you.
What Are My Basic Life Insurance
Benefits?
The School District of Palm Beach County provides you with basic
life insurance in the amount of $20,000 for full-time employees
and $10,000 for part-time employees.
What Are the Basic Life Insurance
Features?
• Accelerated Benefits Option
• Conversion
• Continued Protection (waiver of premium)
• Extended Death Benefit
For more information regarding these features, please refer to the
product features section on page 64.
Exclusion - This plan will not pay benefits if loss of life is the result
of suicide that occurs within the first two years of coverage.
Dependent Children
Coverage available: Life Insurance only
Only valid for: Dependent children from age 6 months up to 26
years of age.
Personal Accident Insurance
MetLife insurance products are designed to provide full-time
protection against accidental death or injuries – 24 hours a day,
365 days a year.

62
Group Term Life Insurance
What benefits are available?
When enrolled in Basic Life Insurance you automatically receive
Personal Accident Insurance in an amount equal to your Basic
Life Insurance. Provided alongside your Basic Life Insurance, this
coverage is designed to help safeguard you and your family from a
financial loss due to an unexpected accidental death or injury.
MetLife and the School District of Palm Beach County know that
you are the best judge of your life insurance needs.
Optional Life Insurance
What benefits are available?
In addition to your Basic Life Insurance, the School District of Palm
Beach County is oering the opportunity to purchase additional
life insurance protection through MetLife’s Optional Life Insurance
program. This benefit is designed to help provide financial security
for you and your family. Since this coverage is an employee-
paid benefit, premiums will be conveniently deducted from your
paycheck post-tax.
Life Insurance Reduction
At age 70, your Supplemental Life Insurance and Supplemental
Accidental Death and Dismemberment Insurance will be
determined by applying the appropriate percentage from the
following table.
EMPLOYEE’S AGE
REDUCTION
70 - 74
65%
75 - 79
45%
+80
30%
During Open Enrollment, you must submit a
completed Statement of Health form directly to
MetLife by mail or fax no later than December
17, 2023. Submission of an incomplete
application will not extend the deadline.
To download the Statement of Health form go to:
https://hub.palmbeachschools.org/all_employees/benefits
Metropolitan Life Insurance Company
Statement of Health Unit
P.O. Box 14069
Lexington, KY 40512-4069
Phone: (800) 638-6420, Option 1
FAX: 1 (859) 225-7909
Rates (Monthly)
Optional Life Insurance & Optional Accident Insurance
Employee only: $0.15 per $1,000 of
coverage per month
Dependent Optl: $0.87 per $1,000 of
coverage per month
NOTE: If you are covered as an employee, you cannot also
be covered as a spouse or dependent child. No person
may be eligible for insurance under this policy as both an
employee and a spouse at the same time.
Your dependent child(ren) may be enrolled for Optional
Child Life Insurance under one insured employee’s plan
of benefits. You may either be enrolled as an employee
or a dependent but not covered and enrolled under both
classifications.

63
Group Term Life Insurance
Post-tax Benefits Guaranteed
Issue: New Hires
At the time of hire and during the benefit selection process, a
new hire employee may select up to five (5) times their basic
annual salary in $20,000 increments, not to exceed $500,000,
with a minimum selection amount of $20,000. A Statement of
Health (SOH) form is required for coverage exceeding $100,000.
To download the Statement of Health form go to: https://hub.
palmbeachschools.org/all_employees/benefits/benefit_forms
For Optional Spouse Life Insurance, an employee may
select coverage in $10,000 increments, not to exceed 50%
of the employee’s Optional Life Insurance coverage with
a minimum amount of $10,000 and a maximum amount of
$250,000. A Statement of Health (SOH) form for the spouse is
required for coverage exceeding $50,000. Go to https://hub.
palmbeachschools.org/all_employees/benefits/benefit_forms to
download the Statement of Health form.
For Optional Child Life Insurance, an employee may select
coverage of $5,000 or $10,000. A Statement of Health form is
NOT required for either election as both are guaranteed issue. The
following age limit payout and eligibility applies:
• Live birth to six months: $1,500; and
• Six months to 26 years: $5,000 or $10,000
During Open Enrollment
Statement of Health Forms are available to download from the
PeopleSoft system. Simply, download the application, fill in all
required fields and mail, fax, or email the form directly to MetLife.
MetLife will notify you of any additional steps and ultimately the
final determination of your request.
You may also apply for additional coverage for yourself, your
spouse or dependent child(ren) at Open Enrollment. A MetLife
Statement of Health form may be required. Coverage maybe
subject to Underwriting Approval.
What are the Optional Life Insurance features?
• Accelerated Benefits Option
• Will Preparation Services
• Conversion
• Continued Protection (waiver of premium)
For more information regarding these features, please refer to the
product features section that starts on page 64.
Imputed Income
Imputed Income will apply for selected amounts over $50,000 for
employees over the age of 50: Because our group rate is the same
for all employees, the IRS requires employers to report taxable
imputed income for each employee whose charged premium is
lower than it’s published Rate Table. Visit the HUB’s Benefits Page
for more information on Imputed Income for Life Insurance.
Optional Life coverage is provided under a group insurance policy,
issued in Florida to the School District of Palm Beach County by
MetLife. Optional Life Insurance under the School District of Palm
Beach County’s plan ends the earliest of:
• Date insurance ends for employees’ class;
• End of the period for which the last premium has been paid
for employee;
• Date employee ceases to be in eligible class;
• End of the month in which employment ends; or
• End of the month the employee retires in accordance with the
policyholder’s retirement plan.
Benefits end on the last day of the month following the event.
Post-tax Benefits
Optional Accident Insurance
Provided alongside your Optional Life Insurance, Optional
Accident Insurance oers a matching amount of Optional Accident
Insurance benefits in addition to the Personal Accident Insurance
that the School District of Palm Beach County has made available
to you.
What Benefits are available?
When you enroll in Optional Life Insurance, you are automatically
enrolled in Optional Accident Insurance. The benefit amount for
Optional Accident Insurance is equal to the benefit amount for
Optional Life Insurance. Since this coverage is an employee-paid
coverage, post-tax premiums will be conveniently deducted from
your paycheck.
What are the Optional Accident
Insurance features?
For Wearing a Seat Belt and Protection by an Airbag-
Death benefits will be increased by 10%, but not more than
$25,000, if the insured person dies as a direct result of injuries in
a covered automobile accident while wearing a properly fastened
seat belt. We will increase the death benefit by an additional 5%,
but not more than $10,000, if the insured was in a seat protected
by a properly functioning and deployed airbag.
For Child Care Expense - MetLife will pay a benefit for a
surviving child under 13 who is enrolled in a licensed child care
center at the time of the accident or within 90 days afterward. This
benefit is three percent of the benefit amount, to a maximum of
$3,000 a year for four continuous years or until the child turns 13,
whichever occurs first.
For Home Alteration and Vehicle Modification - If
you or your insured spouse requires home alteration or vehicle
modification within one year of a covered accident, we will pay 10%
of your benefit amount, to a maximum of $25,000, for alterations
or modifications that are doctor-certified as necessary for an
independent lifestyle.
For Rehabilitation - If you or your insured spouse incurs
rehabilitative expenses within two years of a covered loss, we will
pay an additional 5% of the benefit amount, up to $10,000, for each
covered accident.

64
Group Term Life Insurance
For Furthering Child Education - If you die in a covered
accident, for each child who qualifies for this benefit, we will pay an
amount equal to the tuition charges incurred for a period of up to
four consecutive academic years, not to exceed:
• An academic year maximum of $10,000; and
• An overall maximum of 20% of the full amount
of the benefit.
We may require proof of the child’s continued enrollment as a full-
time student during the period for which a benefit is claimed.
For Training for Your Spouse - If you die in a covered
accident and your insured spouse is enrolled in an accredited
school or enrolls within one year of your death:
• $5,000 per year for one year
• Maximum: 5% of Full Amount
For Hospital Confinement - If confinement occurs within
12 months of an accidental injury:
• 1% of full amount up to $2,500 max per month
• Beginning on the fifth day of confinement
• Maximum: 12 months
How much coverage can I buy?
You – You will automatically receive an amount equal to your
Optional Life Insurance.
Your spouse – The spouse is allowed to receive half of your
Optional Spouse Life Insurance.
Dependents
You may need to request changes to your existing coverage if,
in the future, you no longer have dependents who qualify for
coverage. We will refund premium if you do not notify us of this
and it is determined at the time of a claim that premium has been
overpaid.
If a divorce occurs, at time of claim, premium will be returned. If a
dependent is over age 26, premium would be refunded at time
of claim.
Post-tax Benefits
What is not covered?
• Sickness, disease, physical or mental or surgical treatment
thereof, or bacterial or viral infection, regardless of how
contracted. (This does not include bacterial infection that is
the natural and foreseeable result of an accidental external cut
or wound, or accidental food poisoning.);
• Suicide or attempted suicide;
• Intentionally self-inflicted injury;
• Infection, other than infection occurring in an external
accidental wound, not including accidental food poisoning;
• Service in the armed forces of any country or international
authority. However, service in reserve forces does not
constitute service in the armed forces, unless in connection
with such reserve service an individual is on active military
duty as determined by the applicable military authority other
than weekend or summer training.
Reserve forces are defined as reserve forces of any branch of the
military of the United States or of any other country or international
authority, including but not limited to the National Guard of the
United States or the National Guard of any other country.
Any incident related to travel in an aircraft or device:
• As a pilot, crew member, flight student or while acting in
any capacity other than as a passenger;
• For parachuting or otherwise exiting from the aircraft while the
aircraft is in flight except for the purpose of self-preservation;
• For testing or experimental purposes;
• By or for any military authority;
• For travel or designed for travel beyond the earth’s atmosphere;
• War, whether declared or undeclared; or act of war,
insurrection, rebellion or active participation in a riot;
• If the injured party is intoxicated at the time of the incident
and is the operator of a vehicle or other device involved in the
incident. Intoxicated means that the injured person’s blood
alcohol level met or exceeded the level that creates a legal
presumption of intoxication under the laws of the jurisdiction
in which the incident occurred;
• If the injured party is committing or attempting to commit
a felony;
• Voluntary intake or use by any means of any drug, medication
or sedative, unless it is:
a. Taken or used as prescribed by a doctor, or;
b. An “over the counter” drug, medication or sedative taken as
directed;
• Alcohol in combination with any drug, medication, or sedative;
• Or Poison, gas, or fumes.
Product Features
Accelerated Benefit Option: Terminal Illness Benefit
MetLife will pay a Terminal Illness Benefit if we determine you
or your spouse are terminally ill. The amount of this benefit is
80 percent of the life insurance benefit in eect for you or your
spouse on the date we determine you are terminally ill up to the
max. Benefit amount is shown in your Schedule of Benefits for this
option. The Terminal Illness Benefit is payable only once in an
insured’s lifetime.
Will Preparation and Estate Resolution Services –
Will preparation is oered by Hyatt Legal Plans, a MetLife company,
and provides eligible employees and their spouses with face-to-
face access to attorneys participating in Hyatt Legal Plan’s network
for preparing or updating a will, living will and power of attorney.
When you choose a participating Hyatt Legal Plan’s attorney, the
attorney’s fees are fully covered and there are no claim forms to
file. You also have the flexibility of using a non-network attorney
and being reimbursed for covered services according to a set fee
schedule. www.WillsCenter.com is also available and provides
online interactive tools to assist with the creation of a will and other
legal documents on your own, at your own pace, 24 hours a day,
7 days a week. The site also provides access to other valuable
financial educational materials. Face-to-Face Estate Resolution
Services provides beneficiaries and executors/administrators
access to face-to-face legal representation for probating your and
your spouse’s estates.

65
Group Term Life Insurance
Conversion
If your coverage is reduced or ends due to age, disability or
termination of employment, you can obtain an individual life
insurance policy without proof of good health. To convert
coverage, you must apply for the individual policy and pay the
first premium payment within 31 days after your group coverage
ends. Eligible insured dependents may convert their coverage as
well. Converted policies are subject to additional restrictions if you
convert because of termination or amendment of the group policy.
Continued Protection (waiver of premium) and
Extended Death Benefit
To make sure you can keep the life insurance protection you
need during a dicult period of your life, the life insurance plan
provides continued protection (waiver of premium). If you are
totally disabled prior to age 60 and satisfy a nine-month waiting
period, your life insurance will continue and you won’t need to
pay premiums while you are disabled. Once approved, continued
protection (waiver of premium) can remain in force until age 65.
How It Works
If you are totally and permanently disabled prior to age 60, you
may continue paying premiums for a maximum of 12 weeks from
the date you were in a paid status. After 12 weeks, you will be
given both the option to convert to an individual policy and an
option to apply for a continued protection (waiver of premium)
directly with the life insurance provider. You must apply for a
continued protection (waiver of premium) within 9 months of the
date of disability.
During the wait period for continued protection (waiver of
premium), a loss would be covered under the plan’s extended
death benefit if you were totally and permanently disabled at the
time of loss. Any conversion policy in place would be surrendered
at this time and premiums paid for the conversion policy would
be refunded.
A loss during the continued protection (waiver of premium) wait
period where you are not deemed to have been disabled at time of
loss would require a conversion policy to be in place for a claim to
be payable.
Online Plan Description
You will be able to review any of the Life and Accident Insurance
provisions in more detail through the School District of Palm
Beach County’s website at: https://hub.palmbeachschools.org/
all_employees/benefits
Travel Assistance with Identity
Theft Solutions
To complement your MetLife Insurance coverage, you have access
to Travel Assistance, a special travel service administered by AXA
Assistance USA, Inc. (AXA) through a marketing arrangement
with MetLife. Travel Assistance oers you and your dependents
worldwide medical, travel, concierge and legal and financial
assistance services, 24 hours a day, 365 days a year.
Travel Assistance Coverage
While traveling internationally or domestically, two participants
have access to medical assistance if faced with an emergency.
With one simple phone call, you and your dependents will have
access to:
− Over 600,000 prequalified providers worldwide;
− Air and ground ambulance service;
− Trained multilingual personnel who can advise and assist you
quickly and professionally in a travel emergency.
General Travel Information
Before you travel, you can visit the AXA Assistance website
to obtain information about your visa, passport, inoculation
requirements and local customs as well as 24-hour predeparture
information on weather, currency and much more.
Identity Theft Solutions
You and your dependents also have access to Identity Theft
Solutions, a benefit accessible while you are home or traveling.
This service provides:
• Education & Protection: An identity theft risk and prevention
toolkit and resolution guide;
• Personal Guidance: Assistance with filing and obtaining police
and credit reports, contacting creditor fraud departments,
taking inventory of lost or stolen items and more.
• Concierge Services: Also included are concierge services
designed to fulfill various travel and entertainment requests
as well as arrangements for business-related services such as
flight, hotel and dining reservations, general destination and
transportation information, city guides and much more.
This summary provides an overview of your plan’s benefits.
These benefits are subject to the terms and conditions of the
contract between Metropolitan Life Insurance Company and the
School District of Palm Beach County. Specific details regarding
these provisions can be found in the life and accident insurance
certificate issued by MetLife. If you have additional questions
regarding your life or accident insurance, please contact your
benefits administrator.
Coverage is underwritten by: Metropolitan Life Insurance
Company, 200 Park Avenue, New York, NY 10166.
A certificate of coverage for your Group Life Insurance Plan
is available online at https://hub.palmbeachschools.org/
all_employees/benefits or can be accessed by contacting Risk &
Benefits Management.

66
Retirement Investment Plans
Retirement Investment Plans
Employees can enroll in Voluntary Retirement Investment plans
at any time of the year. Employees can also increase, decrease or
suspend deductions at any time by using PeopleSoft.
403(b) Traditional, Roth & 457(b)
Deferred Plans
Want to start saving, but not sure where to invest?
Get started with Plan B, a quick enrollment plan that allows you to
start saving and makes it easy for you to switch to an approved
investment plan later.
Call 1-866-752-6286 for more information.
Quick Enroll Plan B
Quick Enroll Plan B is a simplified voluntary retirement savings
plan. You do not have to make an investment decision immediately
and your contribution for this plan is deposited into a Guaranteed
Income Fund (GIF) which has a guarantee of principle and interest
crediting. The earlier you start saving for your retirement the better!
Traditional Pretax
The School District of Palm Beach County provides the opportunity
for eligible employees to make tax-sheltered investments through
payroll deductions in accordance with Internal Revenue Code
403(b) & 403(b)(7). You will not have to pay federal income tax on
the money you invest until the money is withdrawn. This is a smart
way to save money for retirement.
Roth Post-Tax
Roth plans allow you to invest funds from your salary on a post-tax
basis. Your investments will grow tax-free and you will not have to
pay any income tax on the investments or profits when the funds
are withdrawn after you retire or otherwise qualify. Most of the
vendors on this page also administer the Roth plans.
Please visit: www.tsacg.com/individual/plan-sponsor/florida/
school-district-of-palm-beach-county for a complete listing of
what program each vendor oers.
Employees are able to use the “My Benefits” section of PeopleSoft
to enroll in these benefits. An account must first be established
with a participating vendor before payroll deductions can begin.
“My Benefits” can also be used to increase or decrease your
existing contributions by simply logging in to “My Benefits/
Retirement Savings Plan” and then clicking on the “EDIT” button of
your existing savings plan.
All employees receiving a W-2 each year are
eligible to participate in any of the voluntary
retirement plans.
Visit our website for important information:
https://hub.palmbeachschools.org/all_employees/
benefits/retirement
Contact the Agent/Broker of Record for the company of your choice listed below for investment
options and to schedule an appointment with a company representative:
Corebridge
Elaine Roberts - (561) 684-3775 /
(954) 946-1765 / (800) 448-2542
Buttelman & Associates Financial
Services (GWN)
Michael Buttelman -
(561) 965-1000, ext. 1237
Equitable
Michael Goldberg - (954) 298-9977
Fidelity Retirement Services
(No Agent of Record) - (800) 343-0860
Group Code for 403(b): 88020 ; 457 86608
Horace Mann
Brooks Hannula - (561) 894-7933
Lincoln Investment
Mike Mracna - (561) 649-9200
MetLife
Kristina Bergman - (561) 207-2311
National Life Group a.k.a LSW
Joshua Bogaards - (800) 579-2878 ext.
9294
PFS Investments (Primerica)
R. Ken Sloan - (561) 635-0947
Quick Enroll Plan B - 1 (866) 752-6286
Voya Financial
Keista Ransom - (877) 882-5050
Voya Reliastar
Keista Ransom - (877) 882-5050

67
ID Theft Protection Plan
67
ID Theft Protection Plan
School District of Palm Beach County
• Full-service identity restoration
• 24/7 lost wallet assistance
• $1 million insurance policy
• Identity safety resource center
Detection:
• Internet surveillance monitoring and alerts
• Social Security monitoring and alerts
1
• Change of address monitoring and alerts
• Court/criminal monitoring and alerts
• Sex oender monitoring and alerts
• Payday loan monitoring and alerts
• Anti-virus/anti-spyware software
• Anti-phishing, Anti-spam software
• Software firewall
• Digital vault
• Digital file shredder
NEW! ID THEFT PROTECTION PLAN
Identity theft is the fastest growing crime in
America, with an identity stolen once every
four seconds.
ID Commander, a leader in proactive
identity theft protection, uses a variety of
industry-leading tools to help protect you
from the growing crime of identity theft:
• Advanced Identity Monitoring
and Alerts
• $1 Million Identity Theft Insurance
Policy, with $0 deductible
• Full-service Identity Restoration
• 24/7 Lost Wallet Assistance
• Award-winning Computer Protection
Software
ID Commander’s comprehensive identity
theft protection plans are available
to both individuals and families with complete
access to benefits the moment membership
begins. The ID Commander Family Protection
Plan provides a managed household program
and empowers individual family members
with the tools and data needed to proactively
manage the health of their identities.
If the worst happens, and you become the
victim of identity theft while covered by ID
Commander, we will restore your identity and
any related credit accounts to pre-theft
status. No limits, no fine print, no “service
guarantee.” In addition, if you suer any
covered out-of-pocket expenses as a result
of a breach, you’re covered by a real
insurance policy that will put money in your
hands for qualified losses.
1
Member must provide a Social Security number in order for the
SSN Trace functionality to monitor SSN activity.
Note: Email address is required to receive
notifications.
Take command of your future with ID Commander.
Visit IDCommander.com/pbcs to enroll for
the ID Commander ID Theft plan today!
The ID Commander plan oers the convenience of
payroll deduction. (See the chart above.)
Ultimate Protection Plan
Includes the following valuable benefits:
Restoration:
Per Pay Period Payroll Deduction
Deductions 22 24
Individual $ 5.73 $ 5.25
Family $12.28 $ 11.25
Online Enrollment Is Simple:

68
Special Benefits from Trustmark
68
Special Benefits from Trustmark®
Voluntary insurance can pay cash benefits to you or your
beneficiaries when that money is needed most. Protect your family,
finances and future with these valuable benefits from Trustmark:
Trustmark Universal LifeEvents®
Insurance with Accelerated Death
Benefit for Long-Term Care Services
Trustmark Universal Life and Universal LifeEvents are permanent
life insurance with an accelerated death benefit that can provide
protection against the high costs of long-term care services. It
features rates that won’t increase due to age, and it builds cash
value over time.
The Universal LifeEvents® option provides a higher death benefit
– for the same rate – during your working years, when your need
for protection is greatest. After age 70, the death benefit reduces
to one-third, but the accelerated death benefit for long-term care
services never reduces.
Trustmark Critical HealthEvents®
Insurance
A major illness can come with hidden costs, even if you have
health insurance. Trustmark Critical HealthEvents is critical illness
insurance that pays you directly (independent of your health
insurance) if you are diagnosed with cancer, heart attack or stroke,
or a related covered condition.
Trustmark Critical HealthEvents provides a lifetime of benefits with
a max benefit that refreshes every year. It pays not just for the most
serious illnesses, but also for earlier stages and early identification
of critical illnesses.
Increases are also available for policyholders with Trustmark’s
traditional Critical Illness plan.
Trustmark Accident Insurance
Accident insurance from Trustmark pays benefits directly to you
for a covered accident and the services to help treat them — for
instance, deductibles, co-payments, transportation and lodging
costs, and everyday bills.
It pays benefits for a variety of covered o-the-job unexpected
accidents, such as fractures, dislocations, burns, and concussions,
and for covered services like ambulance transport, hospital
admissions, physical therapy and more.
Trustmark Hospital StayPay®
Hospital stays can be really expensive, and health insurance might
not cover everything. Trustmark Hospital StayPay helps you keep a
hospital trip aordable. It’s designed to pair with your medical plan
so you can be more confident in your protection.
Hospital StayPay pays you a cash benefit when you’re admitted
to the hospital, and another for each day you spend there. With
Hospital StayPay, you can worry less about your bills, and focus on
recovering.
With All Trustmark Benefits:
• Take your policy with you if you change jobs or retire.
• Pay through convenient payroll deduction.
• Apply for family members as well as for yourself.
Enrollment
The voluntary benefits period is an opportunity to learn about
and to enroll in these Trustmark products. Information on how to
schedule an appointment to meet with an FBMC Representative
virtually will be sent to you electronically later in the year.
Enrollment in Trustmark products is only available through your
FBMC Representative.
Register for your Trustmark portal
today.
Please see the next page for more information - OR - view the
“how to register” video on the District’s website.
Underwritten by Trustmark Insurance Company, Lake Forest, Illinois. Underwriting conditions may vary, and determine eligibility for the oer of insurance. Universal LifeEvents death benefit
reduces to one-third at the latter of age 70 or the 15th policy anniversary; issue age is 18-64. Preexisting condition limitations may apply. Benefits, availability, exclusions and limitations may
vary by state and may be named dierently. Your policy will contain complete information. Trustmark®, LifeEvents®, Trustmark Critical HealthEvents® and Trustmark Hospital StayPay® are
registered trademarks of Trustmark Insurance Company. This is a supplement to health insurance. It is not a substitute for medical or hospital expense insurance, a health maintenance
organization (HMO) contract or major medical expense insurance. Products underwritten by Trustmark Insurance Company.

69
Special Benefits from Trustmark
©2021 Trustmark Insurance Company A112-2717 (3-21)_portal
Underwritten by Trustmark Insurance Company and Trustmark Life
Insurance Company of New York . Rated A- (EXCELLENT) A.M. Best
400 Field Drive • Lake Forest, IL 60045
TrustmarkVB.com
Trustmark Voluntary Benefits’ portals for policy owners
meet customers where they are 24/7, making interacting with us online
at TrustmarkVB.com or by phone easy.
Policy owners can log in on laptops, mobile devices
or tablets to view their personal policies and benefit
details; update personal and contact information;
quickly file claims online and enable text updates
on claim status; and switch to direct bills or make
payments online.

70
COBRA Notification
Important Continuation
Coverage Information
What Is Continuation Coverage?
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives
workers and their families who lose their health benefits the right to
choose to continue group health benefits provided by their group health
plan for limited periods of time under certain circumstances such as
voluntary or involuntary job loss, reduction in the hours worked, transition
between jobs, death, divorce, and other life events. This right extends to
your plan’s Health Care FSA.
Each qualified beneficiary who elects continuation coverage will have the
same rights under the plan as other participants or beneficiaries covered
under the plan, including special enrollment rights. Specific information
describing continuation coverage can be found in the summary plan
description (SPD), which can be downloaded from:
https://hub.palmbeachschools.org/all_employees/benefits
How Long Will Continuation Coverage Last?
COBRA beneficiaries generally are eligible for group coverage during
a maximum of 18 months for qualifying events due to employment
termination or reduction of hours of work. Certain qualifying events, or a
second qualifying event during the initial period of coverage, may permit a
beneficiary to receive a maximum of 36 months of coverage.
For Health Care FSAs, continuation coverage is generally limited to the
remainder of the plan year in which your qualifying event occurs, if you
have not already received, as reimbursement, the maximum benefit
available under the account for the year. For example, if you elected a
Health Care FSA benefit of $1,000 for the plan year and have received
only $200 in reimbursement, you may continue your Health Care FSA
for the remainder of the plan year or until such time that you receive the
maximum Health Care FSA benefit of $1,000.
If your employer funds all or any portion of your Health Care FSA, you
may be eligible to continue your Health Care FSA beyond the plan year
in which your qualifying event occurs and you may have open enrollment
rights at the next open enrollment period. There are special continuation
rules for employer-funded Health Care FSAs.
If you have questions about your Health Care FSA, call:
TASC Customer Care:
1-800-422-4661
www.tasconline.com
A notice form is provided for your use and can be found on the District’s
website at: https://hub.palmbeachschools.org/all_employees/benefits.
You may also obtain the notice form by writing to Benefit Outsource,
Inc. (BOI), 5599 S. University Drive, Suite 201, Davie, FL 33328 or calling
1-888-877-2780.
Continuation coverage will be terminated before the end of the maximum
period if:
A. any required premium is not paid on time, or
B. a qualified beneficiary becomes covered under another group
health plan that does not impose any pre-existing condition
exclusion for a pre-existing condition of the qualified beneficiary, or
C. if a covered employee enrolls in Medicare, or
D. if the employer ceases to provide any group health plan for its
employees.
How Can You Extend the Length of Continuation
Coverage?
For Group Health Plans (Except Health Care FSAs): If you elect
continuation coverage, an extension of the maximum period of 18 months
of coverage may be available if a qualified beneficiary is disabled or a
second qualifying event occurs. You must notify BOI of a disability or a
second qualifying event in order to extend the period of continuation
coverage. Failure to provide notice of a disability or second qualifying
event may aect the right to extend the period of continuation coverage.
Disability: An 11-month extension of coverage may be available if any of
the qualified beneficiaries are disabled. The Social Security Administration
(SSA) must determine that the qualified beneficiary was disabled at some
time during the first 60 days of continuation coverage, and you must notify
BOI of that fact within 60 days of the SSA’s determination and before
the end of the first 18 months of continuation coverage. All qualified
beneficiaries who have elected continuation coverage and qualify will be
entitled to the 11-month disability extension. If the qualified beneficiary is
determined by SSA to no longer be disabled, you must notify BOI of that
fact within 30 days of SSA’s determination.
Second Qualifying Event
An 18-month extension of coverage will be available to spouses and
dependent children who elect continuation coverage if a second qualifying
event occurs during the first 18 months of continuation coverage, resulting
in a maximum amount of continuation coverage of 36 months. Such
second qualifying events include the death of a covered employee,
divorce or separation from the covered employee or a dependent child’s
ceasing to be eligible for coverage as a dependent under the plan. You
must notify BOI within 60 days after a second qualifying event occurs.
How Can You Elect Continuation Coverage?
Each qualified beneficiary has an independent right to elect continuation
coverage. For example, both the employee and the employee’s spouse,
or only one of them, may elect continuation coverage. Parents may
elect to continue coverage on behalf of their dependent children only.
A qualified beneficiary must elect coverage by the date specified on the
COBRA election form. Failure to do so will result in loss of the right to elect
continuation coverage under the plan. A qualified beneficiary may change
a prior rejection of continuation coverage any time until that date.
You should take into account that a failure to continue your group health
coverage will aect your future rights under federal law. First, you can
lose the right to avoid having pre-existing condition exclusions applied
to you by other group health plans if you have more than a 63-day gap
in health coverage, and election of continuation coverage may help
you not have such a gap. Second, you will lose the guaranteed right to
purchase individual health insurance policies that do not impose such
pre-existing condition exclusions if you do not get continuation coverage
for the maximum time available to you. Finally, you should take into
account that you have special enrollment rights under federal law. You
have the right to request special enrollment in another group health plan
for which you are otherwise eligible (such as a plan sponsored by your
spouse’s employer) within 30 days after your group health coverage ends
because of the qualifying event listed above. You will also have the same
special enrollment right at the end of continuation coverage if you get
continuation coverage for the maximum time available to you.

71
COBRA Notification
The Health Insurance Marketplace is an available
alternative Health Care coverage option for you and
your dependent(s).
Beginning with open enrollment in 2023, for an eective date of
January 1, 2024, you will be able to buy coverage through the Health
Insurance Marketplace. In the Marketplace, you could be eligible for a
new kind of tax credit that right away lowers your monthly premiums. You
can see what the premium, deductibles and out-of-pocket costs will be
before you make a decision to enroll. Being eligible for COBRA does not
limit your eligibility for coverage for a tax credit through the Marketplace.
Additionally, if you request enrollment within 30 days, you may qualify for
a special enrollment opportunity for another group health plan for which
you are eligible (such as a spouses’ plan), even if the plan generally does
not accept late enrollees.
How Much Does Continuation Coverage Cost?
Generally, each qualified beneficiary may be required to pay the entire
cost of continuation coverage. This amount may not exceed 102 percent of
the cost to the group health plan (including both employer and employee
contributions) for coverage of a similarly situated plan participant or
beneficiary who is not receiving continuation coverage (or, in the case of
an extension of continuation coverage due to a disability, 150 percent).
For Health Care FSAs, the cost for continuation of coverage is a monthly
amount calculated and based on the amount you were paying via pre-tax
salary reductions before the qualifying event.
When and How Must Payments for Continuation
Coverage Be Made?
First Payment for Continuation Coverage: If you elect continuation
coverage, you do not have to send any payment for continuation coverage
with the COBRA election form. However, you must make your first
payment for continuation coverage within 45 days after the date of your
election. (This is the date the election notice is postmarked, if mailed). If
you do not make your first payment for continuation coverage within that
45 days, you will lose all continuation coverage rights under the plan.
Your first payment must cover the cost of continuation coverage from the
time your coverage under the plan would have otherwise terminated up to
the time you make the first payment. You are responsible for making sure
that the amount of your first payment is enough to cover this entire period.
You may contact BOI to confirm the correct amount of your first payment.
Your first payment for continuation coverage should be sent to:
Benefit Outsource, Inc. (BOI)
5599 S. University Drive, Suite 201
Davie, FL 33328
Periodic Payments for Continuation Coverage
After you make your first payment for continuation coverage, you will be
required to pay for continuation coverage for each subsequent month
of coverage. Under the plan, these periodic payments for continuation
coverage are due on the first day of each month. Instructions for sending
your periodic payments for continuation coverage will be shown on your
COBRA election notice form. BOI will send coupons for use in making
periodic payments.
Periodic payments for continuation coverage should be sent to:
Benefit Outsource, Inc. (BOI)
5599 S. University Drive, Suite 201
Davie, FL 33328
Grace Periods for Periodic Payments
Although periodic payments are due on the first day of the month, you
will be given a grace period of 30 days to make each periodic payment.
Your continuation coverage will be provided for each coverage period as
long as payment for that coverage period is made before the end of the
grace period for that payment. If you pay a periodic payment later than its
due date but during its grace period, your coverage under the plan will
be suspended as of the due date and then retroactively reinstated (going
back to the due date) when the periodic payment is made. This means
that any claim you submit for benefits while your coverage is suspended
may be denied and may have to be resubmitted once your coverage is
reinstated. If you fail to make a periodic payment before the end of the
grace period for that payment, you will lose all rights to continuation
coverage under the plan.
General Notice of COBRA Continuation Coverage
Rights Introduction
You are receiving this notice because you have recently become covered
under a group health plan sponsored by the School District of Palm
Beach County (the plan). This notice contains important information
about your right to COBRA continuation coverage, which is a temporary
extension of coverage under the plan. The right to COBRA continuation
coverage was created by a federal law, the Consolidated Omnibus Budget
Reconciliation Act of 1985 (COBRA). COBRA continuation coverage can
become available to you and to other members of your family who are
covered under the plan when you would otherwise lose your group health
coverage.
This notice generally explains COBRA continuation coverage, when it
may become available to you and your family, and what you need to do
to protect the right to receive it. This notice gives only a summary of your
COBRA continuation coverage rights. For more information about your
rights and obligations under the plan and under federal law, you should
either review the plan’s summary plan description or get a copy of the plan
document from the School District of Palm Beach County (Risk & Benefits
Management).
COBRA Continuation Coverage
COBRA continuation coverage is a continuation of plan coverage when
coverage would otherwise end because of a life event known as a
“qualifying event.” Specific qualifying events are listed later in this notice.
COBRA continuation coverage must be oered to each person who is a
“qualified beneficiary.” A qualified beneficiary is someone who will lose
coverage under the plan because of a qualifying event. Depending on
the type of qualifying event, employees, spouses of employees, and
dependent children of employees may be qualified beneficiaries. Under
the plan, qualified beneficiaries who elect COBRA continuation coverage
must pay for COBRA continuation coverage.
Keep Your Plan Informed of
Address Changes
In order to protect your family’s rights, you should keep your
employer and Wageworks/FBMC informed of any changes
in the addresses of family members. You should also keep
a copy, for your records, of any notices you send to your
employer and Wageworks/FBMC.
Further information on FMLA is available from the nearest
oce of the Wage and Hour Division, listed in most telephone
directories under U.S. Government, U.S. Department of Labor.

72
COBRA Notification
If you are an employee, you will become a qualified beneficiary if you will
lose your coverage under the plan because either one of the following
qualifying events happens:
1. Your hours of employment are reduced, or
2. Your employment ends for any reason other than your gross misconduct.
If you are the spouse of an employee, you will become a qualified
beneficiary if you will lose your coverage under the plan because any of the
following qualifying events happens:
1. Your spouse dies;
2. Your spouse’s hours of employment are reduced;
3. Your spouse’s employment ends for any reason other than his or her
gross misconduct;
4. Your spouse becomes enrolled in Medicare (Part A, Part B, or both); or
5. You become divorced or legally separated from your spouse. Your
dependent children will become qualified beneficiaries if they will lose
coverage under the plan because any of the following qualifying events
happens:
A. The parent-employee dies;
B. The parent-employee’s hours of employment are reduced;
C. The parent-employee’s employment ends for any reason other than
his or her gross misconduct;
D. The parent-employee becomes enrolled in Medicare (Part A, Part B,
or both);
E. The parents become divorced or legally separated; or
F. The child stops being eligible for coverage under the plan
as a “dependent child.”
Sometimes filing a proceeding in bankruptcy under Title 11 of the United
States Code can be a qualifying event. If a proceeding in bankruptcy is
filed with respect to the School District of Palm Beach County, and that
bankruptcy results in the loss of coverage of any retired employee covered
under the plan, the retired employee is a qualified beneficiary with respect
to the bankruptcy. The retired employee’s spouse, surviving spouse, and
dependent children will also be qualified beneficiaries if bankruptcy results
in the loss of their coverage under the plan.
The plan will oer COBRA continuation coverage to qualified beneficiaries
only after BOI has been notified that a qualifying event has occurred. When
the qualifying event is the end of employment or reduction of hours of
employment, death of the employee, commencement of a proceeding in
bankruptcy with respect to the employer or enrollment of the employee
in Medicare (Part A, Part B or both), BOI will oer COBRA continuation
coverage to each qualified beneficiary.
For the other qualifying events (divorce or legal separation of the employee
and spouse or a dependent child’s losing eligibility for coverage as a
dependent child), you must notify BOI. The plan requires you to notify BOI
within 60 days after the qualifying event occurs. Benefit Outsource, Inc.
(BOI), 5599 S. University Drive, Suite 201, Davie, FL 33328.
Once BOI receives notice that a qualifying event has occurred, COBRA
continuation coverage will be oered to each of the qualified beneficiaries.
For each qualified beneficiary who elects COBRA continuation coverage,
COBRA continuation coverage will begin on the date that plan coverage
would otherwise have been lost.
COBRA continuation coverage is a temporary continuation of coverage.
When the qualifying event is the death of the employee, enrollment of
the employee in Medicare (Part A, Part B or both), your divorce or legal
separation, or a dependent child losing eligibility as a dependent child,
COBRA continuation coverage lasts for up to 36 months.
When the qualifying event is the end of employment or reduction of the
employee’s hours of employment, COBRA continuation coverage lasts
for up to 18 months. There are two ways in which this 18-month period of
COBRA continuation coverage can be extended.
Disability Extension of 18-Month Period of
Continuation Coverage
If you or anyone in your family covered under the plan is determined
by the Social Security Administration (SSA) to be disabled at any time
during the first 60 days of COBRA continuation coverage and you notify
BOI in a timely fashion, you and your entire family can receive up to
an additional 11 months of COBRA continuation coverage, for a total
maximum of 29 months. You must make sure that BOI is notified of the
Social Security Administration’s determination within 60 days of the date
of the determination and before the end of the 18-month period of COBRA
continuation coverage.
This notice should be sent to:
Benefit Outsource, Inc. (BOI)
5599 S. University Drive, Suite 201
Davie, FL 33328
You must attach a copy of the SSA Determination Letter to the notice.
Second Qualifying Event Extension of 18-Month
Period of Continuation Coverage
If your family experiences another qualifying event while receiving COBRA
continuation coverage, the spouse and dependent children in your family
can get additional months of COBRA continuation coverage, up to a
maximum of 36 months. This extension is available to the spouse and
dependent children if the former employee dies, enrolls in Medicare (Part A,
Part B, or both), or gets divorced or legally separated. The extension is also
available to a dependent child when that child stops being eligible under
the plan as a dependent child. In all of these cases, you must make sure
that BOI is notified of the second qualifying event within 60 days of the
second qualifying event.
This notice must be sent to:
Benefit Outsource, Inc. (BOI)
5599 S. University Drive, Suite 201
Davie, FL 33328
You must attach a copy of the applicable supporting documentation to the
notice (i.e., the divorce decree, death certificate).
For more Information
This COBRA Q&A section does not fully describe continuation coverage or
other rights under the plan. More information about continuation coverage
and your rights under the plan is available from your employer.

73
Beyond Your Benefits
Social Security
Social Security consists of two tax components: the FICA or OASDI
component (the tax for old-age, survivors’ and disability insurance) and
the Medicare component. A separate maximum wage to which the tax is
assessed applies to both tax components. There is no maximum taxable
annual wage for Medicare. The maximum taxable annual wage for FICA
is subject to federal regulatory change. If your annual salary after salary
reduction is below the maximum wage cap for FICA, you are reducing
the amount of taxes you pay and your Social Security benefits may be
reduced at retirement time.
However, the tax savings realized through the Flexible Benefits Plan
generally outweighs the Social Security reduction. Call FBMC Customer
Care at 1-855-5MYFBMC (1-855-569-3262) for an approximation.
Itemized Deductions
The portion of your salary set aside for before-tax benefit premiums and
flexible spending accounts through the School District of Palm Beach
County’s plans will not be included in the taxable salary or reported to
the IRS on your W-2 form. However, your annualized Dependent Care
FSA contributions will appear on your W-2 form as a non-taxable item.
You will not have to claim these payments as deductions at the end
of the calendar year. Your before-tax deductions cannot be used as
itemized deductions for income tax purposes at the end of the calendar
year.
Special Enrollment Rights Pertaining to Medical
Benefits
If you are declining enrollment for yourself or your dependent (including
your spouse) because of other health plan insurance coverage, you
may in the future be able to enroll yourself or your dependent in the
School District of Palm Beach County’s plan provided that you request
enrollment within 60 days after the other coverage ends.
Disclaimer - Health Insurance Benefits Provided
Under Health Insurance Plan(s)
Health Insurance benefits will be provided, not by the School District of
Palm Beach County’s Flexible Benefits Plan, but by the Health Insurance
Plan(s) Certificates of Coverage. The types and amounts of health
insurance benefits available under the Health Insurance Plan(s), and
the other terms and conditions of coverage and benefits of the Health
Insurance Plan(s) are set forth from time to time in the Health Insurance
Plan(s) Certificates of Coverage. All claims to receive benefits under the
Health Insurance Plan(s) shall be subject to and governed by the terms
and conditions of the Health Insurance Plan(s) Certificates of Coverage.
Notice of Administrator’s Capacity
This notice advises insured persons of the identity and relationship
among the contract administrator, the policyholder and the insurer:
1. Contract Administrator – FBMC Benefits Management (FBMC)
has been authorized by your employer to provide administrative
services for your employer’s insurance plans oered within your
benefit program. In some instances, FBMC may also be authorized
by one or more of the insurance companies underwriting the
benefits to provide certain services, including, but not limited to:
marketing; billing and collection of premiums; and processing
insurance claims payments. FBMC is not the policyholder or the
insurer.
2. Policyholder – This is the entity to whom the insurance policy has
been issued; the employer is the policy holder for group insurance
products and the employee is the policyholder for individual
products. The policyholder is identified on either the face page or
schedule page of the policy or certificate.
3. Insurer – The insurance companies noted herein have been
selected by your employer, and are liable for the funds to pay your
insurance claims.
If FBMC is authorized to process claims for the insurance company, we
will do so promptly.
In the event there are delays in claims processing, you will have
no greater rights to interest or other remedies against FBMC than
would otherwise be aorded to you by law. FBMC is not an insurance
company.
FBMC Privacy Statement
This statement applies to products administered by FBMC Benefits
Management, Inc. and its wholly-owned subsidiaries, including VISTA
Management Company (collectively “FBMC”). FBMC takes your privacy
very seriously. As a provider of products and services that involve
compiling personal-and sometimes, sensitive-information, protecting
the confidentiality of that information has been, and will continue to
be, a top priority of FBMC. This Privacy Statement explains how FBMC
handles and protects the personal information we collect. Please note
that the information we collect and the extent to which we use it will vary
depending on the product or service involved. In many cases, we may
not collect all of the types of information noted below. Note this Privacy
Statement is not meant to be a Privacy Notice as defined by the Health
Insurance Portability and Accountability Act (HIPAA), as amended.
FBMC’s privacy statement is as follows:
1. We collect only the customer information necessary to
consistently deliver responsive services. FBMC collects
information that helps serve your needs, provide high standards
of customer service, and fulfill legal and regulatory requirements.
The sources and types of information collected generally vary
depending on the products or services you request and may
include:
• Information provided on enrollment and related forms - for example,
name, age, address, Social Security number, e-mail address, annual
income, health history, marital status, and spousal and beneficiary
information.
• Responses from you and others such as information relating to your
employment and insurance coverage.
• Information about your relationships with us, such as products
and services purchased, transaction history, claims history, and
premiums.
• Information from hospitals, doctors, laboratories and other
companies about your health condition, used to process claims and
prevent fraud.
2. Under Federal Law you have certain rights with respect to your
protected health information. You have rights to see and copy
the information, receive an accounting of certain disclosures of
the information and, under certain circumstances, amend the
information. You also have the right to file a complaint with your
Employer or with the Secretary of the U.S. Department of Health
and Human Services if you believe your privacy rights have
been violated.
3. We maintain safeguards to ensure information security. We
are committed to preventing unauthorized access to personal
information. We maintain physical, electronic, and procedural
safeguards for protecting personal information. We restrict access
to personal information to those employees, insurance companies,
and service providers who need to know that information to
provide products or services to you.
4. We limit how, and with whom, we share customer information.
We do not sell lists of our customers, and under no circumstances
do we share personal health information for marketing purposes.
With the following exceptions, we will not disclose your personal
information without your written authorization. We may share your
personal information with insurance companies with whom you are
applying for coverage, or to whom you are submitting a claim. We
will share personal information of participants with the plan’s record
keeper. We also may disclose personal information as permitted
or required by law or regulation. For example, we may disclose
information to comply with an inquiry by a government agency or
regulator, in response to a subpoena, or to prevent fraud. If you
no longer have a customer relationship with us, we will still treat
your information under our Privacy Policy, the words “you” and
“customer” are used to mean any individual who obtains or has
obtained an insurance, financial product or service from FBMC that
is to be used primarily for personal or family purposes.

74
Medicare Part D
Medicare Part D Certificate of
Creditable Coverage
It also explains the options you have under Medicare prescription
drug coverage and can help you decide whether or not you want
to enroll. At the end of this notice is information about where
you can get help to make decisions about your prescription drug
coverage.
There are two important things you need to know about your
current coverage and Medicare’s prescription drug coverage:
1. Medicare prescription drug coverage became available
in 2006 to everyone with Medicare through Medicare
prescription drug plans and Medicare Advantage Plans that
oer prescription drug coverage.
All Medicare prescription drug plans provide at least a
standard level of coverage set by Medicare. Some plans may
also oer more coverage for a higher monthly premium.
2. The School District of Palm Beach County has determined that
the prescription drug coverage oered by UnitedHealthcare
is, on average for all plan participants, expected to pay out as
much as the standard Medicare prescription drug coverage
will pay and is considered creditable coverage.
Because your existing coverage is on average at least as good as
standard Medicare prescription drug coverage, you can keep this
coverage and not pay extra if you later decide to enroll in Medicare
prescription drug coverage.
Individuals can enroll in a Medicare prescription drug plan each
year from October 15 through December 7 and when they first
become eligible for Medicare. However, if you lose your current
creditable prescription drug coverage through no fault of your own,
you will also be eligible for a two month special enrollment period
(SEP) to join a Medicare drug plan.
If you do decide to enroll in a Medicare prescription drug plan and
drop your UnitedHealthcare prescription drug coverage, be aware
that you will not be able to get this coverage back. Prescription
drug coverage is a part of the total health insurance plan oered
by UnitedHealthcare and cannot be purchased separately.
Please contact us for more information about what happens to
your coverage if you enroll in a Medicare prescription drug plan.
If you drop your coverage with the School District of Palm Beach
County and enroll in a Medicare prescription drug plan, you will
not be able to get this coverage back later. You should compare
your current coverage, including which drugs are covered, with the
coverage and cost of the plans oering Medicare prescription drug
coverage in your area.
Your current coverage pays for other health expenses, in addition
to prescription drugs, and you will still be eligible to receive all of
your current health and prescription drug benefits if you choose to
enroll in a Medicare prescription drug plan.
You should also know that if you drop or lose your coverage
with the School District of Palm Beach County and don’t enroll
in Medicare prescription drug coverage after your current
coverage ends, you may pay more (a penalty) to enroll in Medicare
prescription drug coverage later.
If you go 63 days or longer without prescription drug coverage
that’s at least as good as Medicare’s prescription drug coverage,
your monthly premium will go up at least 1 percent per month for
every month that you did not have that coverage. For example, if
you go 19 months without coverage, your premium will always be
at least 19 percent higher than what many other people pay. You’ll
have to pay this higher premium as long as you have Medicare
prescription drug coverage. In addition, you may have to wait until
the following October to enroll.
For more information about this notice or your current prescription
drug coverage: contact our oce at 1-561-434-8580.
NOTE: You will receive this notice at other times in the future, such
as before the next period you can enroll in Medicare prescription
drug coverage, or if this coverage changes. You also may request a
copy of this notice at any time.
For more information about your options under Medicare
prescription drug coverage:
More detailed information about Medicare plans that oer
prescription drug coverage is in the “Medicare & You” handbook.
You’ll get a copy of the handbook in the mail every year from
Medicare. You may also be contacted directly by Medicare
prescription drug plans. For more information about Medicare
prescription drug plans:
• Visit: www.medicare.gov
• Call your state health insurance assistance program for
personalized help (see your copy of the “Medicare & You”
handbook for their telephone number).
• Call 1 (800) MEDICARE (1-800-633-4227). TTY users should
call 1 (877) 486-2048.
For people with limited income and resources, extra help paying
for Medicare prescription drug coverage is available. Information
about this extra help is available from the Social Security
Administration (SSA) online at www.ssa.gov or by phone at
1 (800) 772-1213 (TTY 1 (800) 325-0778).
Remember: Keep this notice. If you enroll in one of the new plans
approved by Medicare that oer prescription drug coverage, you
may be required to provide a copy of this notice when you join to
show that you are not required to pay a higher premium amount.
Date: October 1, 2023
Name of Entity: School District of Palm Beach County
Contact: Benefits Technician
Address: 3370 Forest Hill Boulevard, Suite A-103
West Palm Beach, FL 33406-5870
Phone: (561) 434-8580
Please read this notice carefully and keep it where you
can find it. This notice has information about your current
prescription drug coverage with the school District of Palm
Beach County and prescription drug coverage available for
people with Medicare.

75
PeopleSoft “My Homepage”
My Homepage Tiles
Keeping your data updated and close at hand just got a lot easier.
The PeopleSoft Tiles provide you with 24/7 access to your
personal data. By taking advantage of the “My Homepage” feature
of PeopleSoft, you can:
• view your personal data and benefit information including
enrollment and dependent information
• and modify beneficiary information at your convenience.
Q: What am I able to view or change using PeopleSoft?
A: You can:
• Manage payroll data
− View/print paychecks or W2 information
− Verify payroll deductions
− Manage direct deposit
− View payable time
− Review/manage emergency and personal contact
information
• Manage benefits actions
− Review/change life insurance beneficiary information
− View health plan coverage
− Enroll/change 403(b)
− Verify/update tobacco status
− View/manage 1095-C information
• Manage eLearning courses
• And much more
Q: I cannot seem to log in to PeopleSoft to complete my
benefits enrollment; who should I contact?
A: Make sure you have reviewed the instructions on
how to obtain or reset your password. If you still need
help, contact the IT Help Desk at 561-242-4100 for further
assistance. Remember your enrollment is time sensitive, so
do not delay completing your enrollment by the enrollment
deadline.
Q: How much time do I have to complete my online enrollment?
A: You have up to 30 calendar days from your employment start
date (or transfer to a benefited position) to complete your
online benefits enrollment and tobacco adavit. During
Open Enrollment time, you have until the close of the Open
Enrollment period.
Q: Will more time be granted to me if there is a holiday, system
outage or if I have problems with my password?
A: In most cases, no additional time will be granted. Since you
have 30 days to complete your enrollment, it is expected that
you will act promptly and resolve any unexpected issues well
before the final date to enroll.
Q: When should I be able to access the online enrollment system?
A: Within 48 to 72 hours of your start date, you should be able to
access the system and complete your enrollment.
Q: How do I get my User Name and Password?
A: District User ID and Password is assigned to you as a new
employee. Do not share your password with anyone, including
anyone presenting themselves as a member of the IT
Department. All activities performed while using your District
computer account will be attributed to you. Once you receive
your initial password, and you have District Portal access,
you will need to change your password. Please contact the IT
Service Desk for assistance.

76
Appeals Process
Enrollment appeals are granted under very narrow circumstances
as provided by IRS guidance and consistent with District and
insurer practices. It is important to note that failure to provide
dependent verification information during enrollment, or
accidentally electing or dropping a plan, adding or deleting a
dependent in error are not errors that will be considered as an
appeal and if submitted will be returned to you unprocessed.
If you experience one of the
following types of enrollment errors
FBMC will review and consider your
request:
• Enrolling in a Dependent Care Flexible Spending Account
and you do not have dependents who attend day care/elder
care.
• Electing dependent coverage but you do not have eligible
dependents (i.e. electing employee and spouse coverage,
but you are not legally married).
• Other extenuating circumstances related to the enrollment
process that would otherwise be deemed outside of your
control by the plan or the IRS.
To ensure your appeal is handled promptly and with due
consideration:
• Include the School District of Palm Beach County as your
employer. Include your District Employee ID and your
email address.
• Provide a detailed reason for the appeal.
• Include any additional supporting documents, information or
comments you think may have a bearing on your appeal.
FBMC reviews and makes the final determination for all
enrollment appeals based upon established guidelines. All appeal
determinations made by FBMC are final.
You are provided an enrollment period to make your elections
and during that same period you are expected to confirm that
your elections are correct. You have until the last day of your
election period to make any updates or corrections to your
coverage, including adding or dropping dependents. After the
last day of your election period, the coverage you have elected
will remain in place throughout the plan year unless you have a
valid Change in Status.
Appeals are granted under very narrow circumstances and
generally are not permitted due to accidentally selecting a plan or
adding or deleting a dependent.
With that understanding, you may submit written enrollment
appeals within 30 days of your enrollment period close date to:
ENROLLMENT APPEALS:
FBMC Benefits Management
ATTN: Compliance & Risk Management
P.O. Box 1878
Tallahassee, FL 32302-1878
All enrollment appeals decisions are final.
FSA Claim Appeals
TASC, the FSA claims administrator, reviews and makes the final
determination for a denied Health Care FSA or Dependent Care
FSA claim. You will need to provide a written letter that explains
why you believe the claim should be approved. Employees must
submit their appeal for a denied FSA claim within 30 calendar
days of notification.
FSA Appeals
TASC Appeals
PO Box 7091
Madison, WI 53707-0791
or Fax to: (608) 663-2759

©FBMC FBMC/050PB/ACTIVE 2022/081120
This guide does not contain a complete listing of all terms, conditions, or exclusions of the benefits listed herein. Please refer to the policy
and/or certificate of coverage for more information.
Information contained herein does not constitute an insurance certificate or policy.
Certificates will be provided to participants following the start of the plan year, if applicable.
C A
FBMC Benefits Management, Inc.
PO Box 1878 • Tallahassee, FL 32302-1878
FBMC.com
