
Community Health Needs Assessment
Plano Health Community
2022

•
Baylor Scott & White Medical Center – Plano
•
Baylor Scott & White The Heart Hospital - Plano
Plano health
community hospitals
Approved by: Baylor Scott & White Health - North Texas Operating, Policy and Procedure Board on May 31, 2022
Posted to BSWHealth.com/CommunityNeeds on June 30, 2022

Table of contents
Baylor Scott & White Health mission . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
Community Health Needs Assessment (CHNA) report . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
Demographic and socioeconomic summary .........................................7
Health community data summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
Priority health needs. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
Priority 1: Access to mental healthcare (providers/resources) .......................9
Priority 2: Access to primary healthcare. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
Priority 3: Obesity ......................................................................11
Priority 4: Housing insecurity. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12
Priority 5: Elderly/social isolation .....................................................13
Priority 6: Food insecurity .............................................................14
Priority 7: Transportation. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16
Existing resources to address health needs. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
Next steps .............................................................................19
Appendix A: CHNA requirement details ..................................................20
Appendix B: Key public health indicators .................................................25
Appendix C: Community input participating organizations .............................31
Appendix D: Demographic and socioeconomic summary ..............................32
Appendix E: Proprietary community data. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .39
Appendix F: 2019 Community health needs assessment evaluation . . . . . . . . . . . . . . . . . . . .44

Plano Health Community 4
Baylor Scott & White Health mission
Our commitment to the communities we serve
As the largest not-for-profit healthcare system in Texas and one of the largest in the United States,
Baylor Scott & White Health was born from the 2013 combination of Baylor Health Care System and
Scott & White Healthcare. Today, Baylor Scott & White includes 51 hospitals, 1,100 access points, more
than 7,300 active physicians, and over 49,000 employees and the Baylor Scott & White Health Plan.
Baylor Scott & White Health is a
leading Texas healthcare provider
with a proven commitment to patient
and community health. Baylor Scott
& White Health demonstrates this
commitment through periodic
community health needs assessments,
then addresses those needs with a
wide range of outreach initiatives.
These Community Health Needs
Assessment (CHNA) activities also
satisfy federal and state community
benefit requirements outlined in the
Patient Protection and Affordable
Care Act and the Texas Health and
Safety Code.
Baylor Scott & White Health conducts
a thorough periodic examination
of public health indicators and a
benchmark analysis comparing
communities it serves to an overall state of Texas value. In this way, it can determine where
deficiencies lie and the opportunities for improvement are greatest.
Through interviews, focus groups and surveys, the organization gains a clearer understanding of
community needs from the perspective of the members of each community. This helps it identify
the most pressing needs a community is facing and develop implementation plans to focus on those
prioritized needs.
The process includes input from a wide range of knowledgeable people who represent the myriad
interests of the community in compliance with 501 (r)(3) regulations. The CHNA process overview
can be found in Appendix A.
The CHNAs serve as the foundation for community health improvement planning efforts over the
next three years, while the implementation plans will be evaluated annually.
Health
Experience
Affordability
Alignment
Growth
Founded as a Christian ministry
of healing, Baylor Scott & White Health
promotes the well-being of all
individuals, families and communities.
To be the trusted leader, educator
and innovator in value-based care
delivery, customer experience
and affordability.
We serve
faithfully
We act
honestly
We never
settle
We are in
it together
MISSION
STRATEGIES
AMBITIONVALUES

Plano Health Community 5
Community Health Needs Assessment
(CHNA) report
Baylor Scott & White Health (BSWH) owns and operates numerous individually licensed hospital facilities
serving the residents of North and Central Texas.
The Plano Health Community is home to a number of these hospitals with overlapping communities,
including:
•
Baylor Scott & White Medical Center – Plano
•
Baylor Scott & White The Heart Hospital - Plano
The community served by the hospital facilities listed above is Collin, Dallas, Denton, Grayson and Fannin
Counties and was determined based on the contiguous ZIP codes within the associated counties that
made up nearly 80% of the hospital facilities' inpatient admissions over the 12-month period of FY20.
Those facilities with overlapping counties of patient origin collaborated to provide a joint CHNA report
in accordance with the Internal Revenue Code Section 501 (r) (3) and the US Treasury regulations
thereunder. All of the collaborating hospital facilities included in a joint CHNA report define their
communities to be the same for the purposes of the CHNA report.
Plano Health Community map
10
10
10
10
10
20
20
20
20
27
30
35
35
35
37
40
45
45
45
San Benito
Rio Grande City
Roma
Alice
Portland
Ingleside
Beeville
Port Lavaca
Freeport
Bay City
Uvalde
El Campo
Angleton
Leon Valley
La Marque
Converse
Alvin
Seguin
Richmond
Kerrville
Humble
Groves
Nederland
Brenham
Orange
Vidor
Round Rock
Pflugerville
Taylor
Gatesville
Pecos
Hewitt
Brownwood
Palestine
Corsicana
Stephenville
Big Spring
Athens
Andrews
Ennis
Waxahachie
Sweetwater
Mansfield
Marshall
Snyder
Lamesa
Mount Pleasant
Levelland
Gainesville
Denison
Burkburnett
Vernon
Plainview
Hereford
Canyon
Pampa
Borger
Dumas
Edinburg
Kingsville
Eagle Pass
Lake Jackson
Del Rio
Texas City
Buda
Conroe
Huntsville
Temple
Copperas Cove
Lufkin
Nacogdoches
Socorro
Greenville
McKinney
Sherman
Paris
Harlingen
Victoria
Galveston
Sugar Land
Missouri City
Port Arthur
College Station
San Angelo
Odessa
Midland
Wichita Falls
Corpus Christi
Fort Worth
Arlington
Brownsville
McAllen
Laredo
Pasadena
Beaumont
Waco
Abilene
Irving
Carrollton
Plano
Lubbock
Amarillo
San Antonio
Houston
El Paso
Dallas
Austin

Plano Health Community 6
BSWH engaged with IBM Watson Health, a nationally respected consulting firm, to conduct a
Community Health Needs Assessment (CHNA) in accordance with the federal and state community
benefit requirements for the health communities they serve.
Define the
community
Assess the
community
Identify and prioritize
“significant needs”
The CHNA process included:
•
Gathering and analyzing more than 59 public and 45 proprietary health data indicators to provide
a comprehensive assessment of the health status of the communities. The complete list of health
data indicators is included in Appendix B.
•
Creating a benchmark analysis comparing the community to overall state of Texas and United
States (US) values.
•
Conducting focus groups, key informant interviews and stakeholder surveys, including input from
public health experts, to gain direct input from the community for a qualitative analysis.
°
Gathering input from state, local and/or regional public health department members who have
the pulse of the community’s health.
°
Identifying and considering input from individuals or organizations serving and/or representing
the interests of medically underserved low-income and minority populations in the community to
help prioritize the community’s health needs.
°
The represented organizations that participated are included in Appendix C.
IBM Watson Health provided current and forecasted demographic, socioeconomic and utilization
estimates for the community.
Demographic and socioeconomic summary
The most important demographic and socioeconomic findings for the Plano Health Community
CHNA are:
•
The community is growing at a rate higher than both the state of Texas and the US.
•
The average age of the population is younger than the US and slightly older than Texas overall.
•
The median household income is significantly higher than both the state and the US.
•
The community served has a lower percentage of uninsured and underinsured than Texas.
Further demographic and socioeconomic information for the Plano Health Community is included in
Appendix D.

Plano Health Community 7
Total population
4,868,776
Average income
$79,762
Underserved ZIP codes
35
Insurance coverage
Health community data summary
IBM Watson Health’s utilization estimates and forecasts
indicate the following for the Plano Health Community:
•
Inpatient discharges in the community are expected to
grow by 10.5% by 2030 with the largest growing product
lines to include:
°
Pulmonary medical
°
General medicine
°
Cardiovascular diseases
•
Outpatient procedures are expected to increase by almost
35% by 2030 with the largest areas of growth including:
°
Labs
°
General & internal medicine
°
Physical & occupational therapy
°
Psychiatry
•
Emergency department visits are expected to grow by
almost 15% by 2025.
•
Hypertension represents almost 73% of all heart disease cases.
•
Cancer incidence is expected to increase by over 12% by 2025.
Further health community information for the Plano Health
Community is included in Appendix E.
14.4%
11.2%
9.2%
5.7%
1.3%
55.8%
2.4%
Uninsured
Private - exchange
Private - ESI
Private - direct
Medicare dual eligible
Medicare
Medicaid - pre-reform
Health professional shortage areas (HPSA)
Medically
underserved
area/
population
(MUAP)
County
Dental
health
Mental
health
Primary
care
Grand
total MUAP
Collin 1 1
Dallas 7 14 9 30 10
Denton 1 2 1 4 1
Fannin 1 1 2 1
Grayson 1 1 2 1
The community includes the following health professional
shortage areas and medically underserved areas as designated
by the US Department of Health and Human Services Health
Resources Services Administration. Appendix D includes the
details on each of these designations.
Source: US Department of Health and Human Services, Health Resources and Services Administration, 2021

Plano Health Community 8
Priority health needs
Using the data collection and interpretation methods outlined in this report, BSWH has identified what it
considers to be the community's significant health needs. The resulting prioritized health needs for this
community are:
Priority Need Category of need
1 Access to mental healthcare (providers/services) Access to care/mental health
2 Access to primary healthcare providers Access to care
3 Obesity Conditions/diseases
4 Housing insecurity Environment
5 Elderly/social isolation Environment
6 Food insecurity Environment
7 Transportation Environment

Plano Health Community 9
Priority 1: Access to Mental Healthcare (Providers/Resources)
The following data indicates greater need for access for the population to one mental healthcare provider.
The indicator is defined as the ratio of population to mental health providers and is based on data
from County Health Rankings & Roadmaps; CMS, National Provider Identification Registry (NPPES).
Category Data shows greater need Key informants indicate greater need
Access to
care/mental
health
•
Population to one mental health
provider
•
Limited access to mental
healthcare providers
Counties are listed in alphabetical order within NTX-Plano Health Community.
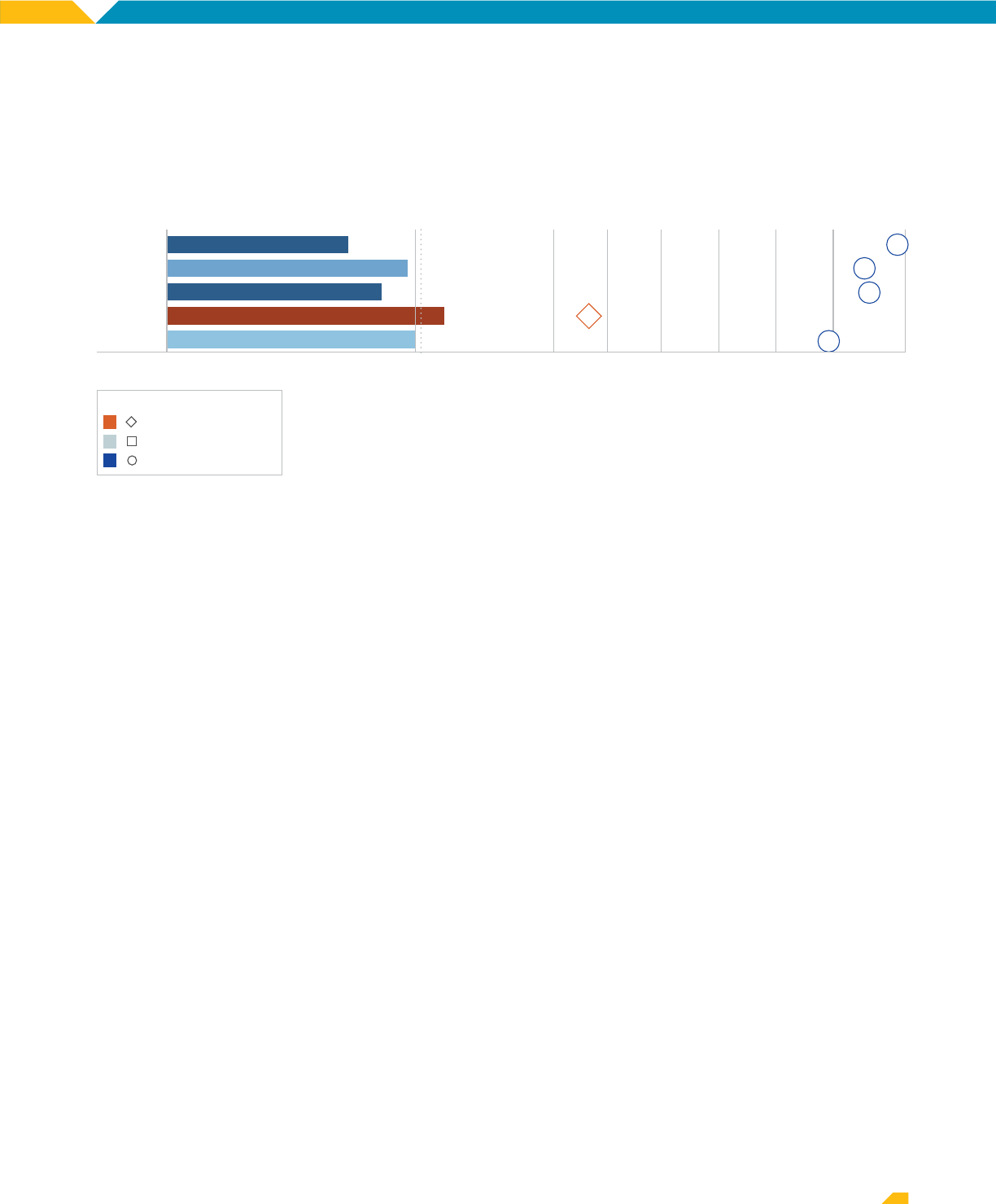
LEFT PANEL: Indicator Values horizontal bar and label shows the county score. Vertical dotted line shows the state
benchmark. Solid line is US score. Orange colors indicate a greater need and potentially larger vulnerable population
in the county relative to the state benchmark. Blue indicates a lesser need and potentially smaller vulnerable population.
Darker intense colors indicate greater differences.
RIGHT PANEL: Rank within county marks show how the indicator ranks compared to other indicators within the county.
Indicators are ranked from 1 to 59, where low numbers show higher need and potentially larger vulnerable population
relative to the state benchmark. Color and shape compare county performance to the state benchmark; orange diamonds
show greater need and blue circles lesser need.
Greater or lesser need than state
greater need
same level of need or NA
lesser need
Collin
Dallas
Denton
Fannin
Grayson
County indicator values 0 10 20 30 40 50 60
45
57
15
14
18
809.00
637.00
843.00
1,015.00
778.00
Access to care: population to one mental health provider (ratio of population to mental health providers
by county)
The focus group participants stated that it is difficult for community residents to access mental/
behavioral health services. They believe that the limited access is due to a combination of an
insufficient number of providers as well as residents’ inability to access care in parts of the
community due to transportation, insurance or funding limitations. Some participants felt that the
area suffered an overwhelming impact of substance abuse and mental health issues and lacks
proactive mental health services, which contribute to the downfall of the physical well-being
of residents. In addition, they acknowledged that there is a stigma present in obtaining mental/
behavioral health services, which also prevents residents from seeking care.
In the prioritization session, the hospital and community leaders were in agreement that the health
community lacks sufficient behavioral health providers. They added that the current providers are
seeing more patients than they have in the past. Many of the patients are presenting with significant
behavioral needs along with complex medical conditions. This is causing difficulty with finding
appropriate care for these individuals. They noted that often mental health facilities will not admit
patients with complex medical needs, thus limiting resources even more in this community.

Plano Health Community 10
Priority 2: Access to Primary Healthcare
The following data indicates greater need for access for the population to one primary care provider
and access for the population to one non-physician primary care provider.
Category Data shows greater need Key informants indicate greater need
Access to
care
•
Population to one primary care physician
•
Population to one non-physician
primary care provider
•
Limited access to primary care providers
•
Limited access to social workers and
care navigators
The population to one primary care physician indicator is defined as the number of individuals served by
one physician in a county if the population was equally distributed across physicians and is based on data
from County Health Rankings & Roadmaps and Area Health Resource File/American Medical Association.
Collin
Dallas
Denton
Fannin
Grayson
County indicator values 0 10 20 30 40 50 60
51
52
3
1
11
986.00
1,438.00
1,851.00
5,881.00
2,161.00
Access to care: population to one primary care physician (number of individuals served by one physician
by county)
The population to one non-physician primary care provider indicator is defined as the ratio of
population to primary care providers other than physicians and is based on data from County Health
Rankings & Roadmaps; CMS, National Provider Identification Registry (NPPES).
Counties are listed in alphabetical order within NTX-Plano Health Community. LEFT PANEL: Indicator Values horizontal bar and label
shows the county score. Vertical dotted line shows the state benchmark. Solid line is US score. Orange colors indicate a greater
need and potentially larger vulnerable population in the county relative to the state benchmark. Blue indicates a lesser need and
potentially smaller vulnerable population. Darker intense colors indicate greater differences. RIGHT PANEL: Rank within county
marks show how the indicator ranks compared to other indicators within the county. Indicators are ranked from 1 to 59, where
low numbers show higher need and potentially larger vulnerable population relative to the state benchmark. Color and shape
compare county performance to the state benchmark; orange diamonds show greater need and blue circles lesser need.
Greater or lesser need than state
greater need
same level of need or NA
lesser need
Collin
Dallas
Denton
Fannin
Grayson
County indicator values 0 10 20 30 40 50 60
56
2
3
2
26
1,313.00
879.00
1,474.00
2,368.00
1,238.00
Access to care: population to one non-physician primary care provider (ratio of population to primary
care providers other than physicians by county)
The focus group participants felt that the overall community area has limited access to primary care
and a shortage of those providers. Participants cited that limited access to providers is a problem
regardless of insurance coverage. Language and cultural barriers also prevent access to medical care.
In the prioritization session, the hospital leadership noted that primary care provider access will
always be a need as the population continues to grow and age in Plano.

Plano Health Community 11
Priority 3: Obesity
The following data indicates greater need in the area of adult obesity although it was not discussed
by the key informants specifically.
Category Data shows greater need
Key informants indicate less need
or not mentioned
Conditions/
diseases
•
Adult obesity
•
Not specifically mentioned
The adult obesity indicator is defined as the percentage of the adult population (age 20 and older)
that reports a body mass index (BMI) greater than or equal to 30 kg/m2 and is based on data from
County Health Rankings & Roadmaps, CDC Diabetes Interactive Atlas and The National Diabetes
Surveillance System.
Counties are listed in alphabetical order within NTX-Plano Health Community.
LEFT PANEL: Indicator Values horizontal bar and label shows the county score. Vertical dotted line shows the state
benchmark. Solid line is US score. Orange colors indicate a greater need and potentially larger vulnerable population
in the county relative to the state benchmark. Blue indicates a lesser need and potentially smaller vulnerable population.
Darker intense colors indicate greater differences.
RIGHT PANEL: Rank within county marks show how the indicator ranks compared to other indicators within the county.
Indicators are ranked from 1 to 59, where low numbers show higher need and potentially larger vulnerable population
relative to the state benchmark. Color and shape compare county performance to the state benchmark; orange diamonds
show greater need and blue circles lesser need.
Greater or lesser need than state
greater need
same level of need or NA
lesser need
Collin
Dallas
Denton
Fannin
Grayson
County indicator values 0 10 20 30 40 50 60
42
33
15
34
17
25.40
30.60
32.00
32.10
38.10
Conditions/diseases: adult obesity (% of adults with BMI =>30 by county)
In the prioritization session, hospital leadership discussed obesity as a need that should be elevated to
a significant need. They noted that obesity is a risk factor for many other chronic conditions.

Plano Health Community 12
Priority 4: Housing Insecurity
Although the data did not indicate greater need in the case of housing, specifically in the measures of
renter-occupied housing and severe housing problems, the key informants felt the lack of affordable
housing was a greater need in the community.
Category Data shows less need or no data Key informants indicate greater need
Housing/
environment
•
Renter-occupied housing
•
Severe housing problems
•
Lack of affordable housing
The renter-occupied housing indicator is defined as the percentage of households that utilize renter-occupied
housing and is based on data from US Census Bureau, American Community Survey One-Year Estimates.
Collin
Dallas
Denton
Fannin
Grayson
County indicator values 0 10 20 30 40 50 60
14
31
56
3
37.40
50.10
33.90
30.80
Housing: renter-occupied housing (% of households that are renter-occupied by county)
The severe housing problems indicator is defined as the percentage of households with at least one
of four housing problems: overcrowding, high housing costs, or lack of kitchen or plumbing facilities.
The indicator is based on data from County Health Rankings & Roadmaps; National Center for HIV/AIDS,
Viral Hepatitis, STD, and TB Prevention (NCHHSTP).
Counties are listed in alphabetical order within NTX-Plano Health Community. LEFT PANEL: Indicator Values horizontal bar and label
shows the county score. Vertical dotted line shows the state benchmark. Solid line is US score. Orange colors indicate a greater
need and potentially larger vulnerable population in the county relative to the state benchmark. Blue indicates a lesser need and
potentially smaller vulnerable population. Darker intense colors indicate greater differences. RIGHT PANEL: Rank within county
marks show how the indicator ranks compared to other indicators within the county. Indicators are ranked from 1 to 59, where
low numbers show higher need and potentially larger vulnerable population relative to the state benchmark. Color and shape
compare county performance to the state benchmark; orange diamonds show greater need and blue circles lesser need.
Greater or lesser need than state
greater need
same level of need or NA
lesser need
Collin
Dallas
Denton
Fannin
Grayson
County indicator values 0 10 20 30 40 50 60
44
38
50
53
7
12.89
21.28
13.69
12.72
14.46
Housing: severe housing problems (% of households with one of four housing problems by county)
The focus group participants stated that housing is unaffordable in the community. Significant
gentrification has occurred, and the resulting impact is residents are being priced out of neighborhoods.
While housing assistance is available, there are too many requirements to apply and qualify. In addition,
there is a lack of safe housing, resulting in hospitalized patients being discharged to unsafe environments.
In the prioritization session, hospital leadership felt strongly that housing is central to accessing care.
Stable housing helps patients manage chronic diseases better and reduces their utilization of the
emergency department. They note that there is a lack of resources for homeless individuals in parts of
the community, which increases the utilization of resources in other parts.

Plano Health Community 13
Priority 5: Elderly/Social Isolation
Although the data did not indicate greater need to address elderly isolation, the key informants felt it
was a greater need in the community.
Category Data shows less need or no data Key informants indicate greater need
Environment
•
Elderly isolation
•
Social isolation and loneliness in
community caused by COVID
The elderly isolation measure is defined as the percent of non-family households (householder living
alone) age 65 years and over. The indicator is based on data from American Community Survey
Five-Year Estimates, US Census Bureau - American FactFinder.
Counties are listed in alphabetical order within NTX-Plano Health Community.
LEFT PANEL: Indicator Values horizontal bar and label shows the county score. Vertical dotted line shows the state
benchmark. Solid line is US score. Orange colors indicate a greater need and potentially larger vulnerable population
in the county relative to the state benchmark. Blue indicates a lesser need and potentially smaller vulnerable population.
Darker intense colors indicate greater differences.
RIGHT PANEL: Rank within county marks show how the indicator ranks compared to other indicators within the county.
Indicators are ranked from 1 to 59, where low numbers show higher need and potentially larger vulnerable population
relative to the state benchmark. Color and shape compare county performance to the state benchmark; orange diamonds
show greater need and blue circles lesser need.
Greater or lesser need than state
greater need
same level of need or NA
lesser need
Collin
Dallas
Denton
Fannin
Grayson
County indicator values 0 10 20 30 40 50 60
48
50
41
4
7
6.10
7.60
5.60
14.50
11.50
Environment: elderly isolation (% householder age 65+ living alone by county)
The key informants described elderly isolation, especially due to COVID, as a social challenge for the
community. As a result of the isolation, the elder community has increased mental health needs and
limited access to resources with no one to provide transportation.
In the prioritization session, hospital leadership discussed the significant uptick in patients presenting
with altered mental/dementia status to the hospitals. They attribute this to older adults living alone
in their homes past the time their capabilities allow them to do so safely. They noted that this can
increase emergency visits for patients with mental health and other medical needs.

Plano Health Community 14
Priority 6: Food Insecurity
While the data did not indicate a need, the key informants cited a greater need in response to the
food environment index, food insecurity and limited access to healthy foods.
Category Data shows less need or no data Key informants indicate greater need
Environment
•
Food environment index
•
Food insecure
•
Limited access to healthy
foods
•
Food deserts exist
•
Lack of supply of food in some areas
•
Healthy choices not affordable and not
accessible everywhere
The food environment index measure is defined as index of factors that contribute to a healthy food
environment. A value of zero “0” is worst and a value of ten “10” is best in the county. The indicator is
based on data from County Health Rankings & Roadmaps, USDA Food Environment Atlas, Map the
Meal Gap from Feeding America, United States Department of Agriculture (USDA).
Collin
Dallas
Denton
Fannin
Grayson
County indicator values 0 10 20 30 40 50 60
51
44
55
55
54
8.40
7.20
8.20
6.70
7.00
Environment: elderly isolation (% householder age 65+ living alone by county)
The food insecure measure is defined as the percentage of population who lack adequate access to
food during the past year. The indicator is based on data from County Health Rankings & Roadmaps,
Map the Meal Gap, Feeding America.
Counties are listed in alphabetical order within NTX-Plano Health Community.
LEFT PANEL: Indicator Values horizontal bar and label shows the county score. Vertical dotted line shows the state
benchmark. Solid line is US score. Orange colors indicate a greater need and potentially larger vulnerable population
in the county relative to the state benchmark. Blue indicates a lesser need and potentially smaller vulnerable population.
Darker intense colors indicate greater differences.
RIGHT PANEL: Rank within county marks show how the indicator ranks compared to other indicators within the county.
Indicators are ranked from 1 to 59, where low numbers show higher need and potentially larger vulnerable population
relative to the state benchmark. Color and shape compare county performance to the state benchmark; orange diamonds
show greater need and blue circles lesser need.
Greater or lesser need than state
greater need
same level of need or NA
lesser need
Collin
Dallas
Denton
Fannin
Grayson
County indicator values 0 10 20 30 40 50 60
40
37
43
34
31
0.11
0.15
0.12
0.15
0.16
Environment: food insecure (% who lack adequate access to food by county)
Plano Health Community 15
The indicator limited access to healthy foods is defined as the percentage of population who are low-
income and do not live close to a grocery store. The indicator is based on data from County Health
Rankings & Roadmaps; USDA Food Environment Atlas, United States Department of Agriculture (USDA).
Counties are listed in alphabetical order within NTX-Plano Health Community.
LEFT PANEL: Indicator Values horizontal bar and label shows the county score. Vertical dotted line shows the state
benchmark. Solid line is US score. Orange colors indicate a greater need and potentially larger vulnerable population
in the county relative to the state benchmark. Blue indicates a lesser need and potentially smaller vulnerable population.
Darker intense colors indicate greater differences.
RIGHT PANEL: Rank within county marks show how the indicator ranks compared to other indicators within the county.
Indicators are ranked from 1 to 59, where low numbers show higher need and potentially larger vulnerable population
relative to the state benchmark. Color and shape compare county performance to the state benchmark; orange diamonds
show greater need and blue circles lesser need.
Greater or lesser need than state
greater need
same level of need or NA
lesser need
Collin
Dallas
Denton
Fannin
Grayson
County indicator values 0 10 20 30 40 50 60
55
54
49
59
7
2.25
6.97
4.35
13.47
7.89
Environment: limited access to healthy foods (% population low income and do not live close to a
grocery store by county)
While the key informants acknowledged that COVID helped with food access in North Texas as
more resources were made available, they noted that food distributions are slowing down and that
there are typically issues in the community around fresh and healthy food options. They added that
chronically ill residents are not helped by food banks or Meals on Wheels because those food sources
often lack dietary-restricted options such as low sodium. Even when healthy food choices are
available, they are not affordable for most residents.
In the prioritization session, the hospital and community leaders agreed that food is a critical
foundation for all needs, including good health. They also agreed that the issue is not the availability
of food but access to food, which is linked to transportation issues. They cited that there is a huge
amount of food wasted at the community’s medical centers, which could be utilized. Despite
stringent state and federal government guidelines for food disposal, the group felt there might be
opportunities to reuse the excess food.

Plano Health Community 16
Priority 7: Transportation
Although the data did not illustrate a need, the focus group participants indicated greater need to
address transportation needs.
Category Data shows less need or no data
Key informants indicate less need or
not mentioned
Environment
•
No vehicle available
•
Transportation is a challenge,
especially in rural areas
The no vehicle available measure is defined as the percent of households with no vehicle available
(percent of households). The indicator is based on data from US Census Bureau, American Community
Survey One-Year Estimates.
Counties are listed in alphabetical order within NTX-Plano Health Community. LEFT PANEL: Indicator Values horizontal bar and label
shows the county score. Vertical dotted line shows the state benchmark. Solid line is US score. Orange colors indicate a greater
need and potentially larger vulnerable population in the county relative to the state benchmark. Blue indicates a lesser need and
potentially smaller vulnerable population. Darker intense colors indicate greater differences. RIGHT PANEL: Rank within county
marks show how the indicator ranks compared to other indicators within the county. Indicators are ranked from 1 to 59, where
low numbers show higher need and potentially larger vulnerable population relative to the state benchmark. Color and shape
compare county performance to the state benchmark; orange diamonds show greater need and blue circles lesser need.
Greater or lesser need than state
greater need
same level of need or NA
lesser need
Collin
Dallas
Denton
Fannin
Grayson
County indicator values 0 10 20 30 40 50 60
56
57
50
2
3.30
7.20
2.70
4.20
Environment: no vehicle available (% of households with no vehicle available by county)
According to key informants, there is limited public transportation across the community. Even with the
existing programs in place to assist in transporting the population, public transportation is not convenient
and can be cost-prohibitive. In addition, current voucher programs are still inefficient at getting residents
to their healthcare appointments. The group felt that more could be done to address this need.
Removing some of the transportation barriers by improving public transportation accessibility and
providing more ride-share or voucher arrangements was a highly rated opportunity as well as expanding
telehealth to accommodate those without easy transportation options to get to healthcare visits.
In the prioritization session, the hospital and community leaders noted that there are very few options
for public transportation in the Plano Health Community. This is more pronounced in rural areas and low
socioeconomic households that cannot afford ride-sharing services such as Lyft and Uber. Transportation
is critical for getting to appointments, obtaining medications and buying groceries and is a significant
need for these reasons.
The Community Health Dashboards data referenced above can be found at BSWHealth.com/About/
Community-Involvement/Community-Health-Needs-Assessments.
The prioritized list of significant health needs approved by the hospitals’ governing body and the full
assessment are available to the public at no cost. To download a copy, visit BSWHealth.com/CommunityNeeds.

Plano Health Community 17
Plano community resources
Need Organization Address Phone
Access
to mental
healthcare
providers/
resources
First Step Counseling Center 900 E. Park Boulevard
Plano, TX 75074
214.942.8808
Child & Family Guidance Center (CFGC) 4031 W. Plano Parkway
Plano, TX 75093
866.695.3794
A Children At Heart Ministries, Inc. - STARRY Counseling 4501 Medical Center Drive
McKinney, TX 75069
469.617.7476
LifePath System (behavioral health services) 7308 Alma Drive
Plano, TX 75025
877.422.5939
CK Family Services (CK) (reduced cost) 710 E. Park Boulevard
Plano, TX 75074
817.516.9100
Access to
primary
healthcare
providers
Carevide 111 N. Johnson Street
Farmersville, TX 75442
903.455.5958
Community Healthcare Center 1620 W. Virginia Street
McKinney, TX 75069
940.766.6306
Community Health Clinic 120 Central Expressway
McKinney, TX 75070
972.547.0606
Hope Clinic 103 E. Lamar Street
McKinney, TX 75069
469.712.4246
Collin County Primary Care Services (PrimaCare
Program)
1920 Eldorado Parkway
McKinney, TX 75069
469.952.3737
Obesity
YMCA of Metropolitan Dallas - Plano Location 3300 McDermott Road
Plano, TX 75025
214.705.9459
Carevide (disease management/preventive medicine) 111 N. Johnson Street
Farmersville, TX 75442
903.455.5958
YMCA of Metropolitan Dallas (recreational center,
nutrition education)
300 Ridge Road
McKinney, TX 75072
972.529.2559
Collin County Health Care Services
(WIC, nutrition education)
825 N. McDonald Street
McKinney, TX 75069
972.548.5543
Brighter Bites - Dallas 2800 18th Street
Plano, TX 75074
469.752.2400
Existing resources to address health needs
One part of the assessment process includes gathering input on potentially available community
resources. The community is served by several large healthcare systems and multiple community-
based health clinics. Below is a list of some of the community resources available to address
identified needs in the community.

Plano Health Community 18
Need Organization Address Phone
Housing
insecurity
Hope's Door New Beginning Center (emergency
shelter)
860 F Avenue
Plano, TX 75074
972.276.0057
Samaritan Inn 1514 N. McDonald Street
McKinney, TX 75071
972.542.5302
City House (transitional living program for youth) 830 Central Parkway East
Plano, TX 75074
972.424.4626
Plano Community Homes (senior housing reduced
cost)
3905 American Drive
Plano, TX 75075
972.867.1905
Family Promise of Collin County (rotational shelter) 325 W. Lucas Road
Allen, TX 75002
972.442.6966
Elderly isolation
HMG Healthcare LLC - Long-Term Care Program 1801 Pearson Avenue
McKinney, TX 75069
972.473.3456
Custer Road United Methodist Church (pastoral care/
spiritual support)
6601 Custer Road
Plano, TX 75023
972.618.3450
ext. 227
The Center for Integrative Counseling and Psychology
(counseling for seniors)
3901 N. Star Road
Richardson, TX 75082
214.526.4525
Widowed Persons Support Group 9027 Midway Road
Dallas, TX 75209
214.358.4155
SMU Counseling Services by Graduate Students
(all ages, grief/loss, depression)
5228 Tennyson Parkway
Plano, TX 75024
972.473.3456
Food insecurity
Meals on Wheels Collin County 600 N. Tennessee Street
McKinney, TX 75069
972.562.6996
Texas Health and Human Services Commission (HHSC)
- SNAP
901 N. McDonald Street
McKinney, TX 75069
877.541.7905
The Salvation Army of North Texas - Food Pantry 3528 14th Steet
Plano, TX 75074
214.637.8100
Brighter Bites - Dallas 2800 18th Street
Plano, TX 75074
469.752.2400
Seven Loaves Food Pantry 1401 Mira Vista Boulevard
Plano, TX 75093
469.385.1813

Plano Health Community 19
Need Organization Address Phone
Transportation
Family Promise of Collin County - Vehicle Program 325 W. Lucas Road
Allen, TX 75002
972.442.6966
Code Pink Productions Inc. 9652 Nathan Way
Plano, TX 75025
972.767.7797
DART 1401 Pacific Avenue
Dallas, TX 75202
214.979.1111
White Rock Center of Hope - East Dallas Plano Health
Community
10021-A Garland Road
Dallas, TX 75218
214.324.8996
Parkland Senior Outreach Services - Southeast Dallas
Plano Health Community
2231 Butler Street
Dallas, TX 75235
214.590.0646
There are many other community resources and facilities serving the Plano Health Community
area that are available to address identified needs and can be accessed through a comprehensive
online resource catalog called Find Help (formerly known as Aunt Bertha). It can be accessed 24/7
at BSWHealth.FindHelp.com.
Next steps
BSWH started the Community Health Needs Assessment process in April 2021. Using both qualitative
community feedback as well as publicly available and proprietary health indicators, BSWH was
able to identify and prioritize community health needs for their healthcare system. With the goal of
improving the health of the community, implementation plans with specific tactics and time frames
will be developed for the health needs BSWH chooses to address for the community served.

Plano Health Community 20
Appendix A: CHNA requirement details
The Patient Protection and Affordable Care Act
(PPACA) requires all tax-exempt organizations
operating hospital facilities to assess the health
needs of their community every three (3) years.
The resulting Community Health Needs
Assessment (CHNA) report must include
descriptions of the following:
•
The community served and how the
community was determined;
•
The process and methods used to conduct
the assessment, including sources and dates
of the data and other information as well as
the analytical methods applied to identify
significant community health needs;
•
How the organization used input from
persons representing the broad interests
of the community served by the hospital,
including a description of when and how the
hospital consulted with these persons or the
organizations they represent;
•
The prioritized significant health needs
identified through the CHNA as well as a
description of the process and criteria used in
prioritizing the identified significant needs;
•
The existing healthcare facilities,
organizations and other resources within the
community available to meet the significant
community health needs; and
•
An evaluation of the impact of any actions
that were taken since the hospitals' most
recent CHNA to address the significant
health needs identified in that report.
°
Hospitals also must adopt an
implementation strategy to address
prioritized community health needs
identified through the assessment.
CHNA process
BSWH began the 2022 CHNA process in April
of 2021. The following is an overview of the
timeline and major milestones:
Define the community
▼
Assess the community
▼
Identify “significant needs” and “prioritize”
▼
Document in written report
▼
CHNA board approvals
▼
Make CHNA widely available on website
▼
Written implementation strategy
▼
Implementation strategy board approval
▼
Make implementation strategy widely
available on website
▼
Act on strategy, measure and report

Plano Health Community 21
Consultant qualifications
IBM Watson Health delivers analytic tools, benchmarks and strategic consulting services to the
healthcare industry, combining rich data analytics in demographics, including the Community Needs
Index, planning and disease prevalence estimates, with experienced strategic consultants to deliver
comprehensive and actionable Community Health Needs Assessments.
Health needs assessment
process overview
To identify the health needs of the community, the hospitals established a comprehensive method
using all available relevant data including community input. They used the qualitative and quantitative
data obtained when assessing the community to identify its community health needs. Surveyors
conducted interviews and focus groups with individuals representing public health, community
leaders/groups, public organizations and other providers. In addition, data collected from public
sources compared to the state benchmark indicated the level of severity. The outcomes of the
quantitative data analysis were compared to the qualitative data findings.
These data are available to the community via an interactive dashboard at BSWHealth.com/
CommunityNeeds.
Data gathering: quantitative assessment of health needs – methodology and data
sources
The IBM team used quantitative data collection and analysis garnered from public health indicators
to assess community health needs. This included over 100 data elements grouped into over 11
categories evaluated for the counties where data was available. Recently, indicators expanded to
include new categories addressing mental health, healthcare costs, opioids and social determinants
of health. A table depicting the categories and indicators and a list of sources are in Appendix B.
A benchmark analysis of each indicator determined which public health indicators demonstrated a
community health need. Benchmark health indicators included overall US values, state of Texas values
and other goal-setting benchmarks, such as Healthy People 2020.
According to America’s Health Rankings 2021 Annual Report, Texas ranks 22nd out of the 50 states in
the area of Health Outcomes (which includes behavioral health, mortality and physical health) and
50th in the area of Clinical Care (which includes avoiding care due to cost, providers per 100,000
population and preventive services). When the health status of Texas was compared to other states,
the team identified many opportunities to impact community health.

Plano Health Community 22
The quantitative analysis of the health community used the following methodology:
•
The team set benchmarks for each health community using state value for comparison.
•
They identified community indicators not meeting state benchmarks.
•
From this, they determined a need differential analysis of the indicators, which helped them
understand the community’s relative severity of need.
•
Using the need differentials, they established a standardized way to evaluate the degree that
each indicator differed from its benchmark.
•
This quantitative analysis showed which health community indicators were above the 25th
percentile in order of severity—and which health indicators needed their focus.
The outcomes of the quantitative data analysis were compared to the qualitative data findings.
Information gaps
In some areas of Texas, the small population size has an impact on reporting and statistical
significance. The team has attempted to understand the most significant health needs of the entire
community. It is understood that there is variation of need within the community, and BSWH may not
be able to impact all of the population who truly need the service.
Community input: qualitative health needs assessment - approach
To obtain a qualitative assessment of the health community, the team:
•
Assembled a focus group representing the broad interests of the community served;
•
Conducted interviews and surveys with key informants—leaders and representatives who serve
the community and have insight into its needs; and
•
Held prioritization sessions with hospital clinical leadership and community leaders to review
collection results and identify the most significant healthcare needs based on information gleaned
from the focus groups and key informants.
Focus groups helped identify barriers and social factors influencing the community’s health needs.
Key informant interviews gave the team even more understanding and insight about the general
health status of the community and the various drivers that contributed to health issues.
Multiple governmental public health department individuals were asked to contribute their
knowledge, information and expertise relevant to the health needs of the community. Individuals or
organizations who served and/or represented the interests of medically underserved, low-income
and minority populations in the community also took part in the process. NOTE: In some cases, public
health officials were unavailable due to obligations concerning the COVID-19 pandemic.
The hospitals also considered written input received on their most recently conducted CHNA and
subsequent implementation strategies if provided. The assessment is available for public comment or
feedback on the report findings by going to the BSWH website (BSWHealth.com/CommunityNeeds)
or by emailing CommunityHealth@BSWHealth.org.

Plano Health Community 23
Approach to prioritizing significant
health needs
On January 31, 2022, a session was conducted
with key leadership members from Baylor
Scott & White along with community leaders
to review the qualitative and quantitative data
findings of the CHNA to date, discuss at length
the significant needs identified, and complete
prioritization exercises to rank the community
needs. Prioritizing health needs was a two-
step process. The two-step process allowed
participants to consider the quantitative
needs and qualitative needs as defined by the
indicator dataset and focus group/interview/survey participant input.
In the first step, participants reviewed the top health needs for their community using associated
data-driven criteria. The criteria included health indicator value(s) for the community and how the
indicator compared to the state benchmark.
High data/
Low qualitative
High data/
High qualitative
Low data/
Low qualitative
Low/no data/
High qualitative
QUALITATIVE QUALITATIVE
DATA
High data and high qualitative: The community indicators that showed
a greater need in the health community overall when compared to
the state of Texas comparative benchmark and were identified as a
greater need by the key informants.
High data/
Low qualitative
High data/
High qualitative
Low data/
Low qualitative
Low/no data/
High qualitative
QUALITATIVE QUALITATIVE
DATA
High data and low qualitative: The community indicators showed a
greater need in the health community overall when compared to the
state of Texas comparative benchmark but were not identified as a
greater need or not specifically identified by the key informants.
High data/
Low qualitative
High data/
High qualitative
Low data/
Low qualitative
Low/no data/
High qualitative
QUALITATIVE QUALITATIVE
DATA
Low/no data and high qualitative:
The community indicators showed less need or had no data available
in the health community overall when compared to the state of Texas
comparative benchmark but were identified as a greater need by the
key informants.
Participants held a group discussion about which needs were most significant, using the professional
experience and community knowledge of the group. A virtual voting method was invoked for
individuals to provide independent opinions.
This process helped the group define and identify the community’s significant health needs. Participants
voted individually for the needs they considered the most significant for this community. When the
votes were tallied, the top identified needs emerged and were ranked based on the number of votes.
High data/Low qualitative High data/High qualitative
Data compared to state
benchmark indicates need by
a greater magnitude
BUT
Topic was not raised in
interviews and focus groups
Data compared to state
benchmark indicates need by
a greater magnitude
AND
Topic was a frequent theme in
interviews and focus groups
Data compared to state
benchmark indicates need by
a lesser magnitude
AND
Topic was not raised in
interviews and focus groups
Data compared to state
benchmark indicates need by
a lesser magnitude
BUT
Topic was a frequent theme in
interviews and focus groups
Low data/Low qualitative Low/no data/High qualitative
High data = Indicators worse than state benchmark by greater magnitude
High qualitative = Frequency of topic in interviews and focus groups
Qualitative Qualitative
Data Data

Plano Health Community 24
Prioritization of significant needs
In the second step, participants ranked the significant health needs based on prioritization criteria
recommended by the focus group conducted for this community.
•
Severity (outcome if ignored): The problem results in disability or premature death or creates
burdens on the community, economically or socially.
•
Root cause: The need is a root cause of other problems. If addressed, it could possibly impact
multiple issues.
•
Feasibility/cost: Is the problem amenable to interventions? What technology, knowledge or
resources are necessary to effect a change? Is the problem preventable? Is it too expensive for the
community to tackle?
The group rated each of the seven significant health needs on each of the three identified criteria,
using a scale of 1 (low) to 10 (high). The criteria score sums for each need created an overall score.
They prioritized the list of significant health needs based on the overall scores. The outcome of this
process was the list of prioritized health needs for this community.
Priority Need Category of need
1 Access to mental healthcare (providers/services) Access to care/mental health
2 Access to primary healthcare providers Access to care
3 Obesity Conditions/diseases
4 Housing insecurity Environment
5 Elderly/social isolation Environment
6 Food insecurity Environment
7 Transportation Environment

Plano Health Community 25
Appendix B: key public health indicators
IBM Watson Health collected and analyzed fifty-nine (59) public health indicators to assess and
evaluate community health needs. For each health indicator, a comparison between the most
recently available community data and benchmarks for the same/similar indicator was made. The
basis of benchmarks was available data for the US and the state of Texas.
The indicators used and the sources are listed below:
Indicator name Indicator source Indicator definition
Adult obesity 2021 County Health Rankings & Roadmaps;
CDC Diabetes Interactive Atlas, The National
Diabetes Surveillance System
2017 Percentage of the adult population
(age 20 and older) that reports a body mass
index (BMI) greater than or equal to 30 kg/m2
Adults reporting fair
or poor health
2021 County Health Rankings & Roadmaps;
The Behavioral Risk Factor Surveillance
System (BRFSS)
2018 Percentage of adults reporting fair or poor
health (age-adjusted)
Binge drinking 2021 County Health Rankings & Roadmaps;
The Behavioral Risk Factor Surveillance
System (BRFSS)
2018 Percentage of a county’s adult population
that reports binge or heavy drinking in the past
30 days
Cancer incidence:
all causes
State Cancer Profiles
National Cancer Institute (CDC)
2013 - 2017 Age-adjusted cancer (all) incidence
rate cases per 100,000 (all races, includes
Hispanic; both sexes; all ages. Age-adjusted to
the 2000 US standard population)
Cancer incidence:
colon
State Cancer Profiles
National Cancer Institute (CDC)
2013 - 2017 Age-adjusted colon and rectum
cancer incidence rate cases per 100,000
(all races, includes Hispanic; both sexes; all
ages. Age-adjusted to the 2000 US standard
population). Data has been suppressed to
ensure confidentiality and stability of rate
estimates. Counts are suppressed if fewer than
16 records were reported in a specific area-sex-
race category. If an average count of three is
shown, the total number of cases for the time
period is 16 or more, which exceeds suppression
threshold (but is rounded to three).
Cancer incidence:
female breast
State Cancer Profiles
National Cancer Institute (CDC)
2013 - 2017 Age-adjusted female breast cancer
incidence rate cases per 100,000 (all races,
includes Hispanic; female; all ages. Age-adjusted
to the 2000 US standard population). Data has
been suppressed to ensure confidentiality
and stability of rate estimates. Counts are
suppressed if fewer than 16 records were
reported in a specific area-sex-race category.
If an average count of three is shown, the total
number of cases for the time period is 16 or
more, which exceeds suppression threshold
(but is rounded to three).

Plano Health Community 26
Indicator name Indicator source Indicator definition
Cancer incidence:
lung
State Cancer Profiles, National Cancer
Institute (CDC)
2013 - 2017 Age-adjusted lung and bronchus
cancer incidence rate cases per 100,000
(all races, includes Hispanic; both sexes;
all ages. Age-adjusted to the 2000 US
standard population)
Cancer incidence:
prostate
State Cancer Profiles, National Cancer
Institute (CDC)
2013 - 2017 Age-adjusted prostate cancer
incidence rate cases per 100,000 (all races,
includes Hispanic; males; all ages. Age-adjusted
to the 2000 US standard population)
Children in poverty 2021 County Health Rankings & Roadmaps;
Small Area Health Insurance Estimates
(SAHIE), United States Census Bureau
2019 Percentage of children under age 18 in
poverty.
Children in single-
parent households
2021 County Health Rankings & Roadmaps;
American Community Survey (ACS), Five-
Year Estimates (United States Census Bureau)
2015 - 2019 Percentage of children that live in a
household headed by single parent
Children uninsured 2021 County Health Rankings & Roadmaps;
Small Area Health Insurance Estimates
(SAHIE), United States Census Bureau
2018 Percentage of children under age 19
without health insurance
Diabetes admission 2018 Texas Health and Human Services
Center for Health Statistics Preventable
Hospitalizations
Number observed/adult population age 18 and
older. Risk-adjusted rates not calculated
for counties with fewer than five admissions.
Diabetes diagnoses
in adults
CMS.gov Chronic Conditions 2007 - 2018 Prevalence of chronic condition across all
Medicare beneficiaries
Diabetes prevalence County Health Rankings (CDC Diabetes
Interactive Atlas)
2017 Prevalence of diagnosed diabetes in a
given county. Respondents were considered to
have diagnosed diabetes if they responded "yes"
to the question, "Has a doctor ever told you that
you have diabetes?" Women who indicated that
they only had diabetes during pregnancy were
not considered to have diabetes.
Drug poisoning
deaths
2021 County Health Rankings & Roadmaps,
CDC WONDER Mortality Data
2017 - 2019 Number of drug poisoning
deaths (drug overdose deaths) per 100,000
population. Death rates are null when the rate is
calculated with a numerator of 20 or less.
Elderly isolation 2018 American Community Survey Five-Year
Estimates, US Census Bureau - American
FactFinder
Percent of non-family households -
householder living alone - 65 years and over
English spoken "less
than very well" in
household
2015 - 2019 American Community Survey
Five-Year Estimates, US Census Bureau -
American FactFinder
2019 Percentage of households that 'speak
English less than "very well"' within all
households that 'speak a language other than
English'
Food environment
index
2021 County Health Rankings & Roadmaps;
USDA Food Environment Atlas, Map the Meal
Gap from Feeding America, United States
Department of Agriculture (USDA)
2015 and 2018 Index of factors that contribute
to a healthy food environment, 0 (worst)
to 10 (best)
Food insecure 2021 County Health Rankings & Roadmaps;
Map the Meal Gap, Feeding America
2018 Percentage of population who lack
adequate access to food during the past year

Plano Health Community 27
Indicator name Indicator source Indicator definition
Food: limited access
to healthy foods
2021 County Health Rankings & Roadmaps;
USDA Food Environment Atlas, United States
Department of Agriculture (USDA)
2015 Percentage of population who are low-
income and do not live close to a grocery store
High school
graduation
Texas Education Agency 2019 A four-year longitudinal graduation rate
is the percentage of students from a class of
beginning ninth graders who graduate by their
anticipated graduation date or within four years
of beginning ninth grade.
Household income 2021 County Health Rankings (Small Area
Income and Poverty Estimates)
2019 Median household income is the income
where half of households in a county earn more
and half of households earn less.
Income inequality 2021 County Health Rankings & Roadmaps;
American Community Survey (ACS),
Five-Year Estimates (United States Census
Bureau)
2015 - 2019 Ratio of household income at
the 80th percentile to income at the 20th
percentile. Absolute equality = 1.0. Higher ratio is
greater inequality.
Individuals below
poverty level
2018 American Community Survey Five-Year
Estimates, US Census Bureau - American
FactFinder
Individuals below poverty level
Low birth weight rate 2019 Texas Certificate of Live Birth Number low birth weight newborns /number of
newborns. Newborn’s birth weight – low or very
low birth weight includes birth weights under
2,500 grams. Blanks indicate low counts or
unknown values. A null value indicates unknown
or low counts. The location variables (region,
county, ZIP) refer to the mother’s residence.
Medicare population:
Alzheimer's disease/
dementia
CMS.gov Chronic Conditions 2007 - 2018 Prevalence of chronic condition across all
Medicare beneficiaries. A null value indicates
that the data have been suppressed because
there are fewer than 11 Medicare beneficiaries
in the cell or for necessary complementary cell
suppression.
Medicare population:
atrial fibrillation
CMS.gov Chronic Conditions 2007 - 2018 Prevalence of chronic condition across all
Medicare beneficiaries. A null value indicates
that the data have been suppressed because
there are fewer than 11 Medicare beneficiaries
in the cell or for necessary complementary
cell suppression.
Medicare population:
COPD
CMS.gov Chronic Conditions 2007 - 2018 Prevalence of chronic condition across all
Medicare beneficiaries. A null value indicates
that the data have been suppressed because
there are fewer than 11 Medicare beneficiaries
in the cell or for necessary complementary cell
suppression.
Medicare population:
depression
CMS.gov Chronic Conditions 2007 - 2018 Prevalence of chronic condition across all
Medicare beneficiaries
Medicare population:
emergency
department use rate
CMS 2019 Outpatient 100% Standard
Analytical File (SAF) and 2019 Standard
Analytical Files (SAF) Denominator File
Unique patients having an emergency
department visit/total beneficiaries, CY 2019

Plano Health Community 28
Indicator name Indicator source Indicator definition
Medicare population:
heart failure
CMS.gov Chronic Conditions 2007 - 2018 Prevalence of chronic condition across all
Medicare beneficiaries. A null value indicates
that the data have been suppressed because
there are fewer than 11 Medicare beneficiaries
in the cell or for necessary complementary cell
suppression.
Medicare population:
hyperlipidemia
CMS.gov Chronic Conditions 2007 - 2018 Prevalence of chronic condition across all
Medicare beneficiaries
Medicare population:
hypertension
CMS.gov Chronic Conditions 2007 - 2018 Prevalence of chronic condition across all
Medicare beneficiaries
Medicare population:
inpatient use rate
CMS 2019 Inpatient 100% Standard Analytical
File (SAF) and 2019 Standard Analytical Files
(SAF) Denominator File
Unique patients being hospitalized/total
beneficiaries, CY 2019
Medicare population:
stroke
CMS.gov Chronic Conditions 2007 - 2018 Prevalence of chronic condition across all
Medicare beneficiaries. A null value indicates
that the data have been suppressed because
there are fewer than 11 Medicare beneficiaries
in the cell or for necessary complementary cell
suppression.
Medicare spending
per beneficiary
(MSPB) index
CMS 2019 Medicare Spending Per Beneficiary
(MSPB), Hospital Value-Based Purchasing
(VBP) Program
Medicare spending per beneficiary (MSPB):
for each hospital, CMS calculates the ratio of
the average standardized episode spending
over the average expected episode spending.
This ratio is multiplied by the average episode
spending level across all hospitals. Blank values
indicate missing hospitals or missing score.
Associated to the hospitals
Mentally unhealthy
days
2021 County Health Rankings & Roadmaps;
The Behavioral Risk Factor Surveillance
System (BRFSS)
2018 Average number of mentally unhealthy
days reported in past 30 days (age-adjusted)
Mortality rate:
cancer
Texas Health Data, Center for Health
Statistics, Texas Department of State
Health Services
2017 Cancer (all) age-adjusted death rate
(per 100,000 - all ages. Age-adjusted using
the 2000 US Standard population). Death rates
are null when the rate is calculated with
a numerator of 20 or less.
Mortality rate:
heart disease
Texas Health Data, Center for Health
Statistics, Texas Department of State
Health Services
2017 Heart disease age-adjusted death rate
(per 100,000 - all ages. Age-adjusted using
the 2000 US Standard population). Death rates
are null when the rate is calculated with a
numerator of 20 or less.
Mortality rate:
infant
2021 County Health Rankings & Roadmaps,
CDC WONDER Mortality Data
2013 - 2019 Number of all infant deaths (within
one year), per 1,000 live births. Blank values
reflect unreliable or missing data.
Mortality rate:
stroke
Texas Health Data, Center for Health
Statistics, Texas Department of State Health
Services
2017 Cerebrovascular disease (stroke) age-
adjusted death rate (per 100,000 - all ages.
Age-adjusted using the 2000 US Standard
population). Death rates are null when the rate
is calculated with a numerator of 20 or less.

Plano Health Community 29
Indicator name Indicator source Indicator definition
No vehicle available US Census Bureau, 2019 American
Community Survey One-Year Estimates
2019 Households with no vehicle available
(percent of households). A null value entry
indicates that either no sample observations
or too few sample observations were available
to compute an estimate, or a ratio of medians
cannot be calculated because one or both of
the median estimates fall in the lowest interval
or upper interval of an open-ended distribution,
or the margin of error associated with a median
was larger than the median itself.
Opioid involved
accidental poisoning
death
US Census Bureau, Population Division and
2019 Texas Health and Human Services
Center for Health Statistics Opioid related
deaths in Texas
Annual estimates of the resident population:
April 1, 2010, to July 1, 2017. 2019 Accidental
poisoning deaths where opioids were involved
are those deaths that include at least one of the
following ICD-10 codes among the underlying
causes of death: X40 - X44, and at least one of
the following ICD-10 codes identifying opioids:
T40.0, T40.1, T40.2, T40.3, T40.4, T40.6. Blank
values reflect unreliable or missing data.
Physical inactivity 2021 County Health Rankings & Roadmaps;
CDC Diabetes Interactive Atlas, The National
Diabetes Surveillance System
2017 Percentage of adults ages 20 and over
reporting no leisure-time physical activity in the
past month
Physically unhealthy
days
2021 County Health Rankings & Roadmaps;
The Behavioral Risk Factor Surveillance
System (BRFSS)
2018 Average number of physically unhealthy
days reported in past 30 days (age-adjusted)
Population to one
dentist
2021 County Health Rankings & Roadmaps;
Area Health Resource File/National Provider
Identification file (CMS)
2019 Ratio of population to dentists
Population to one
mental health
provider
2021 County Health Rankings & Roadmaps;
CMS, National Provider Identification Registry
(NPPES)
2020 Ratio of population to mental health
providers
Population to one
non-physician
primary care provider
2020 County Health Rankings & Roadmaps;
CMS, National Provider Identification Registry
(NPPES)
2020 Ratio of population to primary care
providers other than physicians
Population to
one primary care
physician
2021 County Health Rankings & Roadmaps;
Area Health Resource File/American Medical
Association
2018 Number of individuals served by one
physician in a county, if the population was
equally distributed across physicians
Population under age
65 without health
insurance
2021 County Health Rankings & Roadmaps;
Small Area Health Insurance Estimates
(SAHIE), United States Census Bureau
2018 Percentage of population under age 65
without health insurance
Prenatal care:
first trimester entry
into prenatal care
2020 Texas Health and Human Services -
Vital statistics annual report
2016 Percent of births with prenatal care onset
in first trimester

Plano Health Community 30
Indicator name Indicator source Indicator definition
Renter-occupied
housing
US Census Bureau, 2019 American
Community Survey One-Year Estimates
2019 Renter-occupied housing (percent
of households). A null value entry indicates
that either no sample observations or too
few sample observations were available to
compute an estimate, or a ratio of medians
cannot be calculated because one or both of
the median estimates fall in the lowest interval
or upper interval of an open-ended distribution,
or the margin of error associated with a median
was larger than the median itself.
Severe housing
problems
2021 County Health Rankings & Roadmaps;
Comprehensive Housing Affordability
Strategy (CHAS) data, US Department of
Housing and Urban Development (HUD)
2013 - 2017 Percentage of households
with at least one of four housing problems:
overcrowding, high housing costs, or lack of
kitchen or plumbing facilities
Sexually transmitted
infection incidence
2021 County Health Rankings & Roadmaps;
National Center for HIV/AIDS, Viral Hepatitis,
STD, and TB Prevention (NCHHSTP)
2018 Number of newly diagnosed chlamydia
cases per 100,000 population
Smoking 2021 County Health Rankings & Roadmaps;
The Behavioral Risk Factor Surveillance
System (BRFSS)
2018 Percentage of the adult population in a
county who both report that they currently
smoke every day or most days and have
smoked at least 100 cigarettes in their lifetime
Suicide: intentional
self-harm
Texas Health Data Center for Health Statistics 2019 Intentional self-harm (suicide) (X60 - X84,
Y87.0). Death rates are null when the rate is
calculated with a numerator of 20 or less.
Teen birth rate 2021 County Health Rankings & Roadmaps;
National Center for Health Statistics - Natality
files, National Vital Statistics System (NVSS)
2013 - 2019 Number of births to females ages
15 - 19 per 1,000 females in a county
(The numerator is the number of births to
mothers ages 15 - 19 in a seven-year time
frame, and the denominator is the sum of the
annual female populations, ages 15 - 19.)
Teens (16 - 19) not
in school or work -
disconnected youth
2021 County Health Rankings (Measure of
America)
2015 - 2019 Disconnected youth are teenagers
and young adults between the ages of 16 and
19 who are neither working nor in school. Blank
values reflect unreliable or missing data.
Unemployment 2021 County Health Rankings & Roadmaps;
Local Area Unemployment Statistics (LAUS),
Bureau of Labor Statistics
2019 Percentage of population ages 16 and
older unemployed but seeking work

Plano Health Community 31
Appendix C: community input
participating organizations
Representatives from the following organizations participated in the focus group and a number of
key informant interviews/surveys:
•
Baylor Scott & White Health
•
Baylor Scott & White Health -
McKinney
•
Baylor Scott & White Health -
Plano
•
Baylor Scott & White Health –
Sherman
•
Baylor Scott & White Heart &
Vascular Hospital
•
Baylor Scott & White The Heart
Hospital – Denton
•
Baylor University Medical Center
•
Bridge Breast Network
•
Brighter Tomorrows
•
Callier Center for
Communication Disorders
•
Collin County RHP 18
•
Church of Jesus Christ of LDS
•
City of Denton
•
Collin College Homeless Coalition
•
Collin County Coalition Charitable
Clinics
•
Collin County Health Care Services
•
Collin County Health Department
•
Collin County Public Health
•
Community Lifeline Center
•
Community Services, Inc.
•
Crossroads
•
Dallas Area Interfaith
•
Dallas Area Rape Crisis Center
(DARCC)
•
Dallas Area Rapid Transit (DART)
•
Denton County MHMR Center
•
Department of State Health
Services, Public Health Region 2
and 3
•
Eligibility Consultants Inc.
•
Empowering the Masses
•
Family Promise of Living
•
First Refuge Ministries
•
First United Methodist
•
First United Methodist,
Richardson
•
For Oak Cliff
•
Frazier Revitalization
•
Golden SEEDS
•
Goodwill Dallas
•
Grayson County Health Clinic
•
Health Services of North Texas
•
Julia's Center
•
Methodist Dallas Medical Center
•
Methodist Health System
•
Methodist Health System Golden
Cross Academic Clinic
•
Metrocare Services
•
Metroport Meals on Wheels
•
My Possibilities
•
North Central Texas Health Care
Center Comm.
•
North Texas Food Bank
•
Plano Fire-Rescue
•
Sharing Life
•
Sherman Chamber of
Commerce
•
Sherman High School
•
Sherman Independent School
District
•
South Dallas Fair Park Faith
Coalition
•
Southern Methodist University
•
State Fair of Texas
•
Texas Health Resources
•
Texoma Community Center
•
Texoma Health Foundation
•
The Bridge Homeless Recovery
Center
•
The Concilio
•
The Stewpot
•
United Way
•
United Way of Grayson County
•
United Way of Metropolitan Dallas
(UWMD)
•
Visiting Nurse Association (VNA)
•
Visiting Nurse Association of
Texas – Dallas/Fort Worth
•
Wellness Center for Older Adults
•
Wells Fargo Advisors
•
YMCA Dallas

Plano Health Community 32
Appendix D: demographic and
socioeconomic summary
According to population statistics, the community served is similar to Texas in terms of projected
population growth; both outpace the country. The median age is slightly older than Texas but younger
than the United States. Median income is significantly higher than both the state and the country.
The community served has a lower percentage of Medicaid beneficiaries and a lower percentage of
uninsured individuals than the state of Texas.
Demographic and socioeconomic comparison: community served and state/US benchmarks
Geography
Benchmarks Community served
United States Texas
Plano Metropolitan
health community
Total current population 330,342,293 29,321,501 4,868,776
Five-year projected population change 3.3% 6.6% 7.4%
Median age 38.6 35.2 35.9
Population 0 - 17 22.4% 25.7% 25.5%
Population 65+ 16.6% 13.2% 11.6%
Women age 15 - 44 19.5% 20.5% 21.2%
Hispanic population 19.0% 40.7% 30.9%
Insurance
coverage
Uninsured 9.9% 18.8% 14.4%
Medicaid 20.9% 13.0% 11.2%
Private market 8.3% 8.4% 8.1%
Medicare 13.8% 12.7% 10.5%
Employer 47.2% 47.1% 55.8%
Median HH income $65,618 $63,313 $79,762
No high school diploma 12.2% 16.7% 14.9%
Source: IBM Watson Health Demographics, Claritas, 2020, Insurance Coverage Estimates, 2020.

Plano Health Community 33
The community served expects to grow 7.5% by 2025, an increase of over 362,000 people.
The projected population growth is higher than the state’s five-year projected growth rate (6.6%) and
higher than the national projected growth rate (3.3%). The ZIP codes expected to experience
the most growth in five years are:
•
75052 Grand Prairie – 8,690 people
•
75002 Allen – 7,402 people
•
75035 Frisco – 7,244 people
•
75098 Wylie – 7,020 people
The community’s population is younger with 51.6% of the population ages 18 - 54 and 25.4% under
age 18. The age 65-plus cohort is expected to experience the fastest growth (27%) over the next five
years. Growth in the senior population will likely contribute to increased utilization of services as the
population continues to age.
Population statistics are analyzed by race and by Hispanic ethnicity. The community was primarily white
non-Hispanic, but diversity in the community will increase due to the projected growth of minority
populations over the next five years. The expected growth rate of the Hispanic population (all races) is
over 175,000 people (11.6%) by 2025. The non-Hispanic white population is expected to decline by -1.1%.
Population distribution Household Income distribution
Age
group
Age distribution
2020 Household
income
Income distribution
2020
% of
total 2025
% of
total
USA
2020 %
of total
HH
count
% of
total
USA
% of total
0 - 14 1,025,532 21.1% 1,048,474 20.0% 18.5% <$15K 132,132 7.5% 10.0%
15 - 17 212,504 4.4% 228,764 4.4% 3.9% $15 - 25K 118,719 6.8% 8.6%
18 - 24 457,791 9.4% 505,771 9.7% 9.5% $25 - 50K 343,594 19.6% 20.7%
25 - 34 696,904 14.3% 682,028 13.0% 13.5% $50 - 75K 294,730 16.8% 16.7%
35 - 54 1,355,443 27.8% 1,427,733 27.3% 25.2% $75 - 100K 224,360 12.8% 12.4%
55 - 64 554,607 11.4% 621,592 11.9% 12.9% Over $100K 639,027 36.5% 31.5%
65+ 565,995 11.6% 716,461 13.7% 16.6%
Tot a l 4,868,776 100.0% 5,230,823 100.0% 100.0% Tot a l 1,752,562 100.0% 100.0%
Education level Race/ethnicity
2020 Adult education level
Education level distribution
Race/ethnicity
Race/ethnicity distribution
Pop age
25+ % of total
USA
% of total
2020 pop % of total
USA
% of total
Less than high school 244,467 7.7% 5.2% White non-Hispanic 1,974,024 40.5% 59.3%
Some high school 227,868 7.2% 7.0% Black non-Hispanic 824,682 16.9% 12.4%
High school degree 652,117 20.6% 27.2% Hispanic 1,506,166 30.9% 19.0%
Some college/assoc. degree 862,339 27.2% 28.9% Asian & Pacific is.
non-Hispanic
442,733 9.1% 6.0%
Bachelor's degree or greater 1,186,158 37.4% 31.6% All others 121,171 2.5% 3.3%
Tot a l 3,172,949 100.0% 100.0% Total 4,868,776 100.0% 100.0%

Plano Health Community 34
Population estimates
Population National Selected area
2010 total 308,745,538 4,021,625
2020 total 330,342,293 4,868,776
2025 total 341,132,738 5,230,823
2030 total 353,513,931 5,659,291
% change 2020 - 2025 3.27% 7.44%
% change 2020 - 2035 7.01% 16.24%
Population
Males
all ages
Females
all ages
Females
childbearing
2010 total 1,984,763 2,036,862 896,917
2020 total 2,399,194 2,469,582 1,033,272
2025 total 2,577,167 2,653,656 1,069,134
2030 total 2,786,354 2,872,937 1,130,632
10Y % 16.14% 16.33% 9.42%
National 7.02% 7.01% 4.01%
2020 race and ethnicity with total population
White
non-Hispanic
Black
non-Hispanic
Hispanic Asian and
Pacific Is.
non-Hispanic
All
others
2,500,000
2,000,000
1,500,000
1,000,000
500,000
0
70%
60%
50%
40%
30%
20%
10%
0%
■ 2020 population ▲ 2020 % of total US % of total
Population by sex 2010 - 2030
Males all ages Females all ages Females childbearing
3,500,000
3,000,000
2,500,000
2,000,000
1,500,000
1,000,000
500,000
0
■ 2010 population ■ 2020 population ■ 2025 population ■ 2030 population
Population by age group 2010 - 2030
0 - 14 15 - 17 18 - 24 25 - 34 35 - 44 45 - 54 55 - 64 65+
120,000
100,000
80,000
60,000
40,000
20,000
0
■ 2010 population ■ 2020 population ■ 2025 population ■ 2030 population

Plano Health Community 35
The 2020 median household income for the United States was $65,618 and $63,313 for the state of
Texas. The median household income for the ZIP codes within this community ranged from $173,555
for 75022 Flower Mound to $28,568 for 75210 Dallas. There were thirty-five (35) ZIP codes with median
household incomes less than $52,400—twice the 2020 federal poverty limit for a family of four.
A majority of the population (55.8%) is insured through employer sponsored health coverage.
The remainder of the population was fairly equally divided between Medicaid, Medicare and private
market (the purchasers of coverage directly or through the health insurance marketplace).
The median household income ZIP code map below illustrates ZIP codes that are lower or higher
than twice the federal poverty level for a family of four in 2020.
© 2022 Mapbox © OpenStreetMap
(a) NTX-Plano Health Community Median Household Income
ZIP code map color shows 2020 Median Household Income. ZIP codes are colored on a scale from orange to blue. Orange color indicates median
income less than twice the federal poverty level for a family of 4, which is $52,400, blue color indicates median is greater, and gray colors are similar
to this benchmark.
$26,200 $104,800
Median Household Income is Lower or Higher than $52,400
Twice the Federal Poverty Limit for a Family of 4
(b) Median Household
Income
$65,620
projected increase 9.4%
$72,400 by 2025
$63,310
projected increase 6.5%
$67,740 by 2025
Select Health Community
NTX-Plano Health Community
(1) Which areas have the highest and lowest estimated median
household income?
2020 values are statistical estimates not actual census values.
County City ZIP
0K 10K 20K 30K 40K
Households
0K 1K 2K 3K
Projected # Change in HH
0% 5% 10%
Projected % Change in HH
Collin
Allen
75002
75013
Anna 75409
Blue Ridge 75424
Celina 75009
Dallas 75252
Farmersville 75442
Frisco
75034
75035
Lavon 75166
McKinney
75069
75070
75071
25,295
15,383
6,114
1,465
4,837
14,119
3,941
16,949
23,319
1,559
14,531
20,229
2,198
1,318
623
154
506
1,069
378
1,671
2,104
173
1,227
2,034
9%
9%
10%
11%
10%
8%
10%
10%
9%
11%
10%
8%
NTX-Plano Health Community Estimated Households
Hover on the column headers to expand [+] or collapse [-] geography
The bar chart reports 3 panes of data. The left pane shows 2020 Households, the center pane shows projected change (new households) by 2025 and the right pane shows projected
percentage change in households by 2025. Values are shown at the County, City and ZIP levels.
Access To Care Children Uninsured
Collin
Dallas
Denton
Fannin
Grayson
Population under Age 65 without Health Insurance
Collin
Dallas
Denton
Fannin
Grayson
Environment Elderly Isolation
Collin
Dallas
Denton
Fannin
Grayson
Food Insecure
Collin
Dallas
Denton
Fannin
Grayson
Food: Limited Access to Healthy Foods
Collin
Dallas
Denton
Fannin
Grayson
No Vehicle Available Collin
5
7
4
7
2
Principal County Public Indicators NTX-Plano Health Community
Numbers are actual values from publicly available sources not estimates or projections.
Bar chart of a subset of the Counties by Public Indicator dashboard relevant to the Median Household Income and Insurance Coverage Estimates metrics. Bar chart is organized by indicator
category within the county selected from the map above. Horiz
ontal bar shows the county score. Vertical dotted line shows the state benchmark. Orange colored bars indicate the county
score is greater need relative to the state. Blue colored bars indicate the county score is lesser need relative to the state. Gray colored bars indicate the county score is similar to the state.
Darker colors indicate greater differences between county and state scores. Light c
olors have smaller differences. Indicators that rank in the top 10 highest needs within the county are shown
with rank number in the lollipop bar end.
(3) Which areas have the largest number of households and how is it projected to change in
the next 5 years?
2020 values are statistical estimates and not actual census values. 2025 values are statistical projections of the 2020 estimates.
(5) Which county-level public indicators are related to these estimates?
County City ZIP
Median HH Income
(weighted)
Difference from Twice
Federal Poverty Level for a
Family of 4
Projected $ Change Median
HH Income
Projected % Change Median
HH Income
Collin Allen
75002
75013
Anna 75409
Blue Ridge 75424
Celina 75009
Dallas 75252
Farmersville 75442
Frisco
75034
75035
Lavon 75166
McKinney
75069
75070
$111,810
$136,440
$91,500
$72,290
$120,750
$69,820
$78,560
$108,570
$138,480
$95,380
$63,820
$98,590
70,750
95,160
48,880
29,500
82,240
24,350
35,600
101,070
67,380
52,730
18,890
54,460
$11,340
$11,120
$9,780
$9,610
$13,890
$6,930
$9,440
$11,210
$14,990
$9,750
$7,470
$8,270
10%
8%
11%
13%
12%
10%
12%
10%
11%
10%
12%
8%
NTX-Plano Health Community 2020 Median Household Income, Dollar and Percent Growth by 2025
Hover on the column headers to expand [+] or collapse [-] geography
The bar chart reports 4 panes of data at the ZIP level. The left pane shows current estimated Median Household Income for each ZIP broken down by County, City and Community. A vertical
dotted line references $52,400 which is twice the federal
poverty level for a family of 4 (2xFPL-4). The second pane shows the difference between median income and the 2xFPL-4
benchmark. Orange color indicates values less than 2xFPL-4; blue colors are greater; grey colors are about the same. The third pane shows the projected dollar increase or decrease in
median household income in 5 years. The fourth pane shows the projected percentage increase p or d
ecrease q in median household income in 5 years.
(2) What is the median household income estimate; how does it compare to twice the federal
poverty level for a family of four; and how is it projected to change in the next 5 years?
2020 values are statistical estimates and not actual census values. 2025 values are statistical projections of the 2020 estimates.
(4) How do people use insurance to cover health care costs
and how is it projected to change in the next 5 years?
2020 values are statistical estimates and not actual census values. 2025 values are statistical projections of the 2020 estimates.
-50.0% 50.0%
County Values and Need Rank
higher need - - - - - - - - - - - - - - - state benchmark - - - - - - - - - - - - - - - lower need
Design by [email protected] Watson Health © IBM Corporation 2021
Hover for
Information
The state and U.S. values are the 2020
estimate from IBM proprietary statistical
models.
County
0K 200K 400K 600K 800K 1000K
Lives
0K 10K 20K 30K 40K 50K 60K
Projected # Change (5 yrs)
0.0% 2.0% 4.0% 6.0% 8.0%
Projected % Change in 5 years
Collin
Dallas
Denton
Fannin
Grayson
7.8%
5.0%
6.9%
3.0%
4.2%
226,341
17,556
1,118,421
56,395
232,144
15,997
12,668
383
52,958
2,225
(c) NTX-Plano Health Community - Insurance Coverage Estimates - Vulnerable Populations
Populations vulnerable to losing access to health care include the exchange or direct Private Market, Medicaid, and Uninsured
Hover on the column headers to expand [+] and drill down or collapse [-] and roll up
County to ZIP-level bar chart with 3 panes showing statistics for Unisured, Medicaid and Private Market populations. Left pane shows total number of covered lives. Center pane shows the
projected change in the next 5 years. Right pane shows the projected percentage change in the next 5 years. ZIP level results can roll-up to City and County level by selecting the collapse [-]
button above the column headings. Drill down from County to ZIP by selecting the expand [+] buttons.
© Mapbox © OSM
(b) Uninsured ZIP map
NTX-Plano Health Community
ZIP Level Map showing the estimated number of
Uninsured. Darker colors indicate greater numbers. ZIP
codes with total population greater than 25% college
students are noted in the pop-up.
0 20,000
5,000 10,000 15,000
47%47%
16%13%
8%8%
15%13%
14%19%
Percentage of Total 2020 Population
broken down by Insurance Group.
0M 1M 2M 3M
Lives
0K 100K 200K
Projected # Change (5
yrs)
0.0% 20.0%
Projected % Change in 5
years
Uninsured
Medicaid
Private
Market
Medicare
Employer
14%
11%
10%
56%
8%
127,658
141,834
58,833
28,847
4,875
25.0%
8.4%
5.3%
1.2%
5.2%
(a) NTX-Plano Health Community
Bar chart has 3 panes. The left pane shows the estimated number and percentage of 2020
covered lives with insurance type: Uninsured, Medicaid, Private Market, Medicare, or
Employer. The center pane shows the projected change in 5 years and the right pane shows
the projected percentage change in the 5 years. Color indicates population vulnerable to
losing access to healt
h care services. Orange colors have greater vulnerability than blue.
Insurance Coverage
Benchmarks
increase
$52,400

Plano Health Community 36
Federally designated health professional shortage areas and medically underserved
areas and populations
Health professional shortage areas (HPSA)
County HPSA ID HPSA name HPSA discipline class Designation type
Collin 7485109304 LI - MHCA - Collin County Mental health Low-income population HPSA
Dallas 1487790622 OFAC - Parkland Center for
Internal Medicine (PCIM)
Primary care Other Facility
Dallas 7486259744 LI - Irving Mental health Low-income population HPSA
Dallas 7482835384 LI - South Central Dallas Mental health Low-income population HPSA
Dallas 7482563929 LI - Southeast Dallas Mental health Low-income population HPSA
Dallas 7486982533 LI - Grand Prairie-West Dallas Mental health Low-income population HPSA
Dallas 7483797081 LI - Central Dallas County Mental health Low-income population HPSA
Dallas 7484799626 LI - North Dallas County Mental health Low-income population HPSA
Dallas 7482166324 LI - Northeast Dallas County Mental health Low-income population HPSA
Dallas 14899948OZ Mission East Dallas and Metroplex
Project
Primary care Federally qualified health center
Dallas 74899948MN Mission East Dallas and Metroplex
Project
Mental health Federally qualified health center
Dallas 64899948MO Mission East Dallas and Metroplex
Project
Dental health Federally qualified health center
Dallas 14899948Q0 Healing Hands Ministries, Inc. Primary care Federally qualified health center
Dallas 74899948O2 Healing Hands Ministries, Inc. Mental health Federally qualified health center
Dallas 64899948NX Healing Hands Ministries, Inc. Dental health Federally qualified health center
Dallas 148999485F Martin Luther King Jr. Family Clinic
Inc.
Primary care Federally qualified health center
Dallas 748999481V Martin Luther King Jr. Family Clinic
Inc.
Mental health Federally qualified health center
Dallas 6489994897 Martin Luther King Jr. Family Clinic
Inc.
Dental health Federally qualified health center
Dallas 14899948P6 Dallas County Hospital District Primary care Federally qualified health center
Dallas 748999482V Dallas County Hospital District Mental health Federally qualified health center
Dallas 64899948C2 Dallas County Hospital District Dental health Federally qualified health center
Dallas 1488622370 Urban Inter-Tribal Center of Texas Primary care Indian health service,
tribal health and urban Indian
health organizations
Dallas 7485754448 Urban Inter-Tribal Center of Texas Mental health Indian health service,
tribal health and urban Indian
health organizations
Dallas 6485188079 Urban Inter-Tribal Center of Texas Dental health Indian health service,
tribal health and urban Indian
health organizations
Dallas 14899948D3 Los Barrios Unidos Community
Clinic, Inc.
Primary care Federally qualified health center
Dallas 748999481L Los Barrios Unidos Community
Clinic, Inc.
Mental health Federally qualified health center
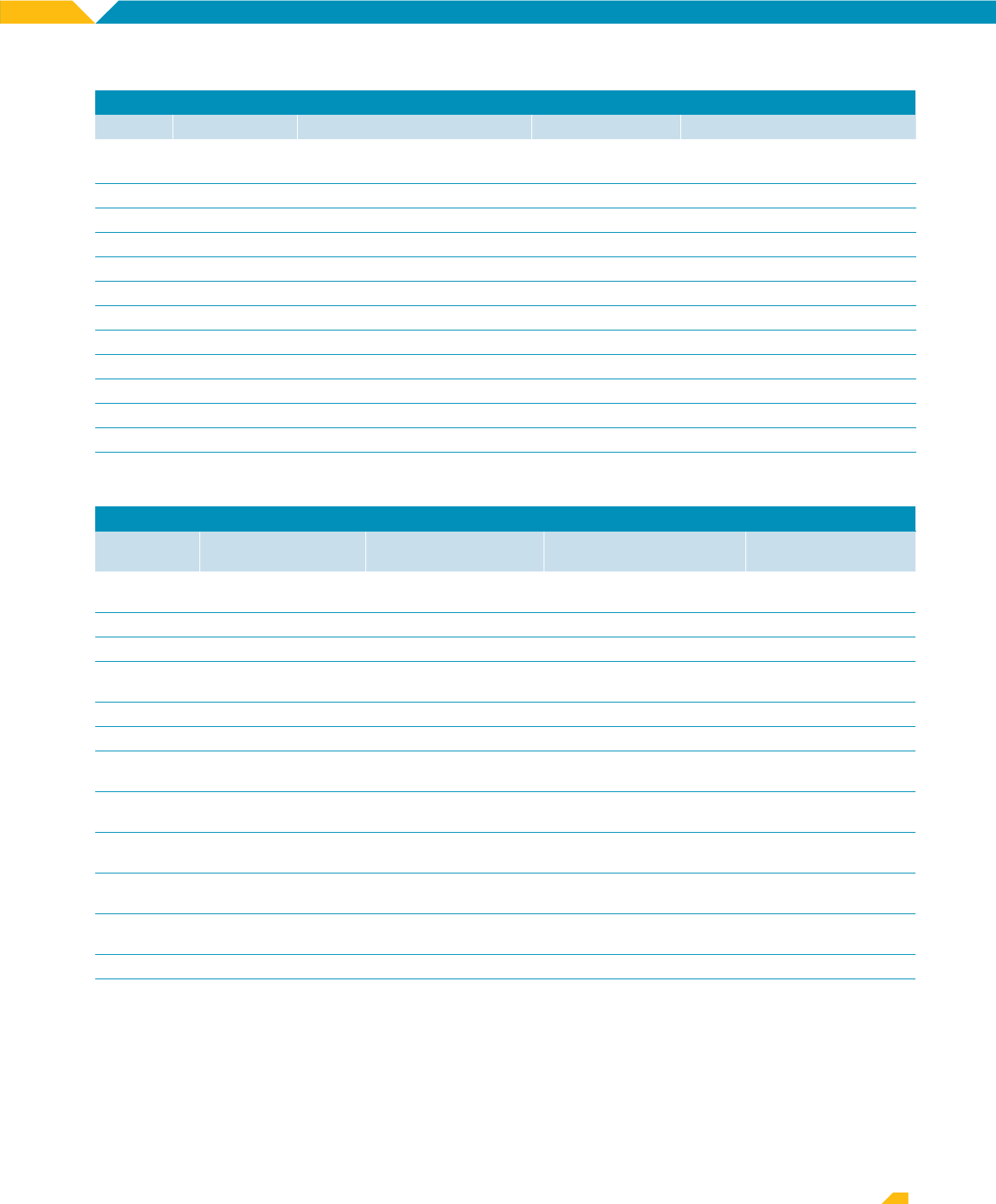
Plano Health Community 37
Health professional shortage areas (HPSA), continued
County HPSA ID HPSA name HPSA discipline class Designation type
Dallas 6489994889 Los Barrios Unidos Community
Clinic, Inc.
Dental health Federally qualified health center
Dallas 1489814978 FCI - Seagoville Primary care Correctional facility
Dallas 6481843658 FCI - Seagoville Dental health Correctional facility
Dallas 7483425946 FCI - Seagoville Mental health Correctional facility
Dallas 1487991263 LI - Central Dallas County Primary care Low-income population HPSA
Denton 7487902282 LI - MHCA - Denton County Mental health Low-income population HPSA
Denton 14899948PA Health Services of North Texas, Inc. Primary care Federally qualified health center
Denton 74899948MQ Health Services of North Texas, Inc. Mental health Federally qualified health center
Denton 64899948MR Health Services of North Texas, Inc. Dental health Federally qualified health center
Fannin 7485674459 Fannin County Mental health Geographic HPSA
Fannin 1489550240 LI - Fannin County Primary care Low-income population HPSA
Grayson 7487593472 LI - Grayson County Mental health Low-income population HPSA
Grayson 1485849525 LI - Grayson County Primary care Low-income population HPSA
Medically underserved areas and populations (MUA/P)
County
MUA/P source
identification number Service area name Designation type Rural status
Dallas 1485024236 Dallas County - Dallas
South
Medically underserved area Non-rural
Dallas 03469 Dallas service area Medically underserved area Non-rural
Dallas 1487043129 East Dallas County Medically underserved area Non-rural
Dallas 05213 Forest Glenn service
area
Medically underserved area Non-rural
Dallas 07959 Lillycare Dallas Medically underserved area Non-rural
Dallas 1484709099 Southeast Dallas County Medically underserved area Non-rural
Dallas 1486572106 Dallas County - Dallas
Southwest
Medically underserved
population
Non-rural
Dallas 1489157042 LI - Grand Prairie Medically underserved
population
Non-rural
Dallas 1483247641 LI - Irving Medically underserved
population
Non-rural
Dallas 07753 Mission East Dallas area Medically underserved
population
Non-rural
Denton 03463 Poverty population Medically underserved area –
Governor’s exception
Non-rural
Fannin 1489926052 Fannin County Medically underserved area Rural
Grayson 1481877977 LI - Grayson County Medically underserved
population
Partially rural

Plano Health Community 38
Community Needs Index
The IBM Watson Health Community Need Index (CNI) is a statistical approach that identifies areas
within a community where there are likely gaps in healthcare. The CNI takes into account vital socio-
economic factors, including income, culture, education, insurance and housing, about a community
to generate a CNI score for every population ZIP code in the US.
The CNI is strongly linked to variations in community healthcare needs and is a good indicator of
a community’s demand for a range of healthcare services. Not-for-profit and community-based
hospitals, for whom community need is central to the mission of service, are often challenged to
prioritize and effectively distribute hospital resources. The CNI can be used to help them identify
specific initiatives best designed to address the health disparities of a given community.
The CNI score by ZIP code shows specific areas within a community where healthcare needs may
be greater.
Plano Health Community
The overall CNI score for the Plano Health Community was 3.61. The difference in the numbers
indicates both a strong link to community healthcare needs and a community’s demand for various
healthcare services. In portions of the community, the CNI score was greater than 4.5, indicating
more significant health needs among the population.
Composite CNI score
3.61
Texas CNI score
3.85
US composite CNI score
3.00
Barrier State US
Income 3.0 3.0
Culture 4.7 3.0
Education 3.5 3.0
Insurance 4.3 3.0
Housing 3.9 3.0
Composite CNI: high scores indicate high need.
ZIP map where color shows the 2020 Community Need Index on a scale of 1 to 5. Orange color indicates high need
areas (CNI = 4 or 5); blue color indicates low need (CNI = 1 or 2). Gray colors have needs at the national average (CNI = 3).
©2022 Mapbox ©OpenStreetMap
1.000 5.000

Plano Health Community 39
Appendix E: proprietary
community data
IBM Watson Health supplemented the publicly available data with estimates of localized inpatient
demand discharges, outpatient procedures, emergency department visits, heart disease, as well as
cancer incidence estimates.
Social determinants of health are the structural determinants and conditions in which people are
born, grow, live, work and age. All of which can greatly impact healthcare utilization and play a major
role in the shifting healthcare landscape. Social determinants, such as education, income and race,
are factored into Inpatient Demand Estimates and Outpatient Procedure Estimates utilization rate
creation methodologies.
Inpatient demand estimates
Inpatient demand estimates provide the total volume of annual acute care admissions by ZIP code
and DRG Product Line for every market in the United States. IBM uses all-payor state discharge data
for publicly available states and Medicare (MEDPAR) data for the entire US. These rates are applied to
demographic projections by ZIP code to estimate inpatient utilization for 2020 through 2030.
The following summary is reflective of the inpatient utilization trends for Plano Health Community.
Total discharges in the community are expected to grow by 10.5% by 2030, with pulmonary medical,
general medicine and cardiovascular diseases projecting the largest growth.
Source: IBM Watson Health Inpatient Demand Estimates, 2020.
Product line
2020
discharges
2025
discharges
2030
discharges
2020 - 2025
discharges
change
2020 - 2025
discharges
% change
2020 - 2030
discharges
change
2020 - 2030
discharges
% change
Alcohol and Drug Abuse 5,084 5,184 5,714 99 1.9% 629 12.4%
Cardio-Vasc-Thor Surgery 13,470 14,351 15,122 880 6.5% 1,651 12.3%
Cardiovascular Diseases 27,668 30,201 34,631 2,533 9.2% 6,963 25.2%
ENT 2,284 2,107 2,019 (177) -7.8% (264) -11.6%
General Medicine 68,556 72,053 77,774 3,496 5.1% 9,217 13.4%
General Surgery 30,214 30,540 32,160 326 1.1% 1,946 6.4%
Gynecology 2,556 1,262 742 (1,294) -50.6% (1,813) -71.0%
Nephrology/Urology 17,322 18,549 20,382 1,228 7.1% 3,060 17.7%
Neuro Sciences 20,237 21,233 23,566 996 4.9% 3,329 16.4%
Obstetrics Del 53,471 49,064 48,875 (4,407) -8.2% (4,596) -8.6%
Obstetrics ND 4,104 3,537 3,364 (566) -13.8% (740) -18.0%
Oncology 8,005 8,245 8,737 239 3.0% 731 9.1%
Ophthalmology 461 437 422 (24) -5.3% (39) -8.5%
Orthopedics 31,748 32,313 34,465 565 1.8% 2,717 8.6%
Psychiatry 4,888 5,137 5,435 249 5.1% 547 11.2%
Pulmonary Medical 28,291 33,226 38,457 4,935 17.4% 10,166 35.9%
Rehabilitation 349 396 464 47 13.4% 114 32.7%
TOTAL 318,709 327,833 352,328 9,124 2.9% 33,618 10.5%

Plano Health Community 40
Outpatient procedures estimates
Outpatient procedure estimates predict the total annual volume of procedures performed by ZIP
code for every market in the United States using proprietary and public health claims, as well as
federal surveys. Procedures are defined and reported by procedure codes and are further grouped
into clinical service lines. The Plano Health Community outpatient procedures are expected to
increase by almost 35% by 2030 with the largest growth in the categories of labs, general & internal
medicine, physical & occupational therapy and psychiatry.
Source: IBM Watson Health Outpatient Procedure Estimates, 2020.
Source: IBM Watson Health Inpatient Demand Estimates, 2020.
Clinical service category
2020
procedures
2025
procedures
2020-2025
procedures
% change
2030
procedures
2020 - 2030
procedures
% change
Allergy & Immunology 1,227,607 1,356,284 10.5% 1,505,743 22.7%
Anesthesia 327,624 395,367 20.7% 461,933 41.0%
Cardiology 2,640,485 3,445,074 30.5% 4,523,428 71.3%
Cardiothoracic 2,784 3,283 17.9% 3,820 37.2%
Chiropractic 2,000,664 2,048,770 2.4% 2,067,047 3.3%
Colorectal Surgery 33,332 36,339 9.0% 39,696 19.1%
CT Scan 820,169 1,144,324 39.5% 1,576,710 92.2%
Dermatology 826,158 981,531 18.8% 1,158,090 40.2%
Diagnostic Radiology 4,758,881 5,328,190 12.0% 5,950,854 25.0%
Emergency Medicine 2,317,865 2,605,519 12.4% 2,940,128 26.8%
Gastroenterology 320,772 376,386 17.3% 436,965 36.2%
General & Internal Medicine 38,763,171 45,245,471 16.7% 51,737,126 33.5%
General Surgery 265,215 305,262 15.1% 351,658 32.6%
Hematology & Oncology 7,149,409 8,704,331 21.7% 10,219,570 42.9%
Labs 47,565,513 54,048,309 13.6% 61,488,029 29.3%
Miscellaneous 2,029,924 2,317,920 14.2% 2,626,818 29.4%
MRI 408,467 468,784 14.8% 537,061 31.5%
Nephrology 1,013,716 1,222,540 20.6% 1,449,449 43.0%
Neurology 662,097 727,682 9.9% 801,218 21.0%
Neurosurgery 19,972 29,399 47.2% 35,308 76.8%
Obstetrics/Gynecology 842,045 886,676 5.3% 962,896 14.4%
Ophthalmology 2,179,306 2,673,448 22.7% 3,206,134 47.1%
Oral Surgery 26,091 29,078 11.4% 32,788 25.7%
Orthopedics 649,724 743,555 14.4% 844,350 30.0%
Otolaryngology 1,622,641 1,799,942 10.9% 1,993,362 22.8%
Pain Management 365,027 417,030 14.2% 467,770 28.1%
Pathology 815 962 18.1% 1,132 38.8%
PET Scan 23,667 28,298 19.6% 33,228 40.4%
Physical & Occupational Therapy 13,486,888 16,218,756 20.3% 19,377,663 43.7%
Plastic Surgery 40,029 47,250 18.0% 55,694 39.1%
Podiatry 176,596 194,788 10.3% 211,787 19.9%
Psychiatry 6,019,862 7,768,719 29.1% 9,779,380 62.5%
Pulmonary 843,032 964,317 14.4% 1,108,047 31.4%
Radiation Therapy 377,016 435,627 15.5% 497,838 32.0%
Single Photon Emission CT Scan (SPECT) 54,136 62,598 15.6% 73,115 35.1%
Urology 258,226 309,743 20.0% 367,735 42.4%
Vascular Surgery 113,426 132,611 16.9% 153,080 35.0%
TOTAL 140,232,354 163,504,164 16.6% 189,076,651 34.8%

Plano Health Community 41
Emergency department visits
Emergency department estimates predict the total annual volume of emergency department (ED)
visits by ZIP code and level of acuity for every market in the United States. IBM uses an extensive
supply of proprietary claims, public claims and federal surveys to construct population-based use
rates for all payors by age and sex. These use rates are then applied to demographic and insurance
coverage projections by ZIP code to estimate ED utilization for 2020 through 2030.
Visits are broken out into emergent and non-emergent ambulatory visits to identify the volume of
visits that could be seen in a less-acute setting, for example, a fast-track ED or an urgent care facility.
In addition, visits that result in an inpatient admission are broken out into a third, separate category.
In the Plano Health Community, ED visits are expected to grow by almost 15% by 2025.
Source: IBM Watson Health Emergency Department Visits, 2020.
Emergent status 2020 visits 2025 visits
2020 - 2025
visits change
2020 - 2025
visits % change
Emergent 1,012,251 1,224,998 212,747 21.0%
Inpatient Admission 292,564 365,479 72,916 24.9%
Non-Emergent 888,255 927,020 38,765 4.4%
TOTAL 2,193,070 2,517,497 324,427 14.8%
Inpatient admission
Emergent
Non-emergent
37%
49%
14%
Emergency department visit estimates 2025

Plano Health Community 42
Heart disease estimates
The heart disease estimates dataset predicts the number of cases by heart disease type and
ZIP code for every market in the United States. IBM uses public and private claims data as well as
epidemiological data from the National Health and Nutritional Examination Survey (NHANES) to build
local estimates of heart disease prevalence for the current population. County-level models by age
and sex are applied to the underlying demographics of specific geographies to estimate the number
of patients with specific types of heart disease.
In Plano Health Community, the most common heart disease is hypertension at 73.1% of all heart
disease cases.
Disease type 2020 prevalence 2020 % prevalence
Arrhythmia 210,814 12.3%
Heart Failure 92,253 5.4%
Hypertension 1,255,053 73.1%
Ischemic Heart Disease 157,689 9.2%
TOTAL 1,715,808 100.0%
Source: IBM Watson Heart Disease Estimates, 2020.

Plano Health Community 43
Cancer estimates
IBM Watson Health builds county-level cancer incidence models that are applied to the underlying
demographics of specific geographies to estimate incidence (i.e., the number of new cancer cases
annually) of all cancer patients. Cancer incidence is expected to increase by 12.4% in the Plano Health
Community by 2025.
Cancer type
2020
incidence
2025
incidence
2020 - 2025
change
2020 - 2025
% change
Bladder 943 1,126 184 19.5%
Brain 431 480 49 11.3%
Breast 4,929 5,695 766 15.5%
Colorectal 2,771 2,702 -69 -2.5%
Kidney 1,019 1,220 202 19.8%
Leukemia 761 888 127 16.7%
Lung 2,540 2,892 351 13.8%
Melanoma 1,088 1,286 197 18.1%
Non-Hodgkin’s Lymphoma 1,192 1,395 203 17.1%
Oral Cavity 741 869 128 17.3%
Other 3,047 3,593 546 17.9%
Ovarian 399 443 44 11.1%
Pancreatic 649 793 144 22.2%
Prostate 3,084 3,101 17 0.5%
Stomach 427 483 55 13.0%
Thyroid 717 829 112 15.6%
Uterine Cervical 181 185 4 2.4%
Uterine Corpus 636 751 115 18.1%
TOTAL 25,554 28,729 3,175 12.4%
Source: IBM Watson Health Cancer Estimates, 2020.

Plano Health Community 44
Appendix F: 2019 community health
needs assessment evaluation
It is Baylor Scott & White Health's privilege to serve faithfully in promoting the well-being of all individuals,
families and communities. Our 2019 Implementation Strategy described the various resources and
initiatives we planned to direct toward addressing the adopted health needs of the 2019 CHNA.
The following is a snapshot of the impact of actions taken by Baylor Scott & White to address the below
priority health issues.
Dates: Fiscal Years 2020 - March 2022
Facilities: Baylor Scott & White Medical Center – Plano, Baylor Scott & White The Heart Hospital - Plano
Community served: Collin, Dallas, Denton, Hunt, Kaufman, Rockwall and Tarrant Counties
Food insecurity and children eligible for free lunch
Baylor Scott & White Medical Center – Plano
Baylor Scott & White The Heart Hospital - Plano
Action/tactics Anticipated outcome Evaluation of impact
Enrollment services
The hospital provides staff to help
enroll patients in public programs,
such as CHIP and Medicaid,
to increase access and quality of
care, especially for persons living in
poverty and vulnerable situations.
Overcome access issues and reduce
hospital expenses.
BSWMC – Plano
•
Persons served: 238
•
$46,893 community benefit
BSWTHH – Plano
•
Persons served: 57
•
$39,468 community benefit
Charity care
Provide free/discounted care to
financially or medically indigent
patients as outlined in the financial
assistance policy. Healthcare
infrastructure/supplies/staff.
Increased access to primary care and/
or specialty care for indigent persons
regardless of their ability to pay.
BSWMC – Plano
•
$12,433,477 community benefit
BSWTHH – Plano
•
$23,368,866 community benefit

Plano Health Community 45
Drug poisoning death rate and accidental poisoning deaths where opioids were involved
Baylor Scott & White Medical Center – Plano
Baylor Scott & White The Heart Hospital - Plano
Baylor Scott & White The Heart Hospital - Plano
Action/tactics Anticipated outcome Evaluation of impact
Medical education
The hospital is committed to the
education of future nurses at entry
and advanced levels to establish
a workforce of qualified nurses,
including knowledge about proper
use of opioids and signs of abuse.
Increased quality and size of the
nursing workforce.
BSWMC – Plano
•
Persons served: 180
•
$469,849 community benefit
BSWTHH – Plano
•
Persons served: 1,316
•
$160,555 community benefit
Action/tactics Anticipated outcome Evaluation of impact
Pharmaceutical support
Pharmaceutical support through
the provision of free/discounted
medications for patients who are
unfunded and have no other means
to acquire them.
Improved health outcomes with proper
medication that follows designated safety
protocol.
•
$36,456 community benefit

Plano Health Community 46
Addressing all needs
Baylor Scott & White Medical Center – Plano
Baylor Scott & White The Heart Hospital - Plano
Action/tactics Anticipated outcome Evaluation of impact
Financial and in-kind donations
Financial and in-kind donations to
community organizations aimed
at improving community health
and addressing identified needs.
Hospitals donate retired medical
supplies and equipment to the office
of Faith in Action Initiatives Second
Life program for the purpose of
providing for the healthcare needs
of populations in the community and
nation whose needs cannot be met
through their own organization.
Improved access to community resources.
Better network of safety net support
services.
Patients can get assistance with SDOH as
well as improved access to health services.
Lacking consistent access to food is
associated with negative health outcomes,
such as weight gain, increased risk of heart
disease, diabetes, and other comorbidities
and premature mortality.
BSWMC – Plano
•
Persons served: 45,033
•
$233,955 community benefit
BSWTHH – Plano
•
Persons served: 22,696
•
$412,885 community benefit
Community education/outreach
Events and activities provided by
BSWH in the community or on-site to
provide education and information
on wellness and health improvement
often done in collaboration with
community partners. Includes health
screenings and heart health series.
To encourage lifelong healthy eating and
physical activity habits. To build nutrition
knowledge and skills to positively influence
states of wellness, recovery from illness,
disease prevention and chronic disease
management.
BSWMC – Plano
•
Persons served: 4,422
•
$23,013 community benefit
BSWTHH – Plano
•
Persons served: 511
•
$16,376 community benefit
Total investment in adopted community needs since 2019 CHNA
BSWMC – Plano
$13.2 million
BSW The Heart Hospital – Plano
$24 million

Physicians provide clinical services as members of the medical staff at one of Baylor Scott & White Health’s subsidiary, community or affiliated medical centers and do not provide clinical
services as employees or agents of those medical centers or Baylor Scott & White Health. ©2022 Baylor Scott & White Health. 99-ALL-540615 BID
