
New Jersey
Hepatitis C Epidemiologic Profile
Issued July 2023
New Jersey Department of Health
COMMUNICABLE DISEASE SERVICE | INFECTIOUS AND ZOONOTIC DISEASE PROGRAM
Page | 1
CONTRIBUTORS
Author
Bernice Carr, MPH, MS
Epidemiologist, Communicable Disease Service,
Infectious and Zoonotic Disease Program,
Epidemiology, Environmental and Occupational
Health, New Jersey Department of Health
Fellow, Leading Epidemiologists Advancing
Data, Council of State and Territorial
Epidemiologists
Mentor
Daniel Church, MPH
Epidemiologist, Viral Hepatitis Coordinator, Division
of Epidemiology, Bureau of Infectious Disease and
Laboratory Sciences, Massachusetts Department of
Public Health
Contributors
Maryellen Wiggins MSN, RN, ACRN
Public Health Consultant, Hepatitis C Nurse
Stella Tsai, PhD, CIH
Research Scientist, Data Analyst Coordinator
Vibha Gujar, PhD, MS
Health Data Specialist
Mojisola Ojo, MPH
Epidemiologist
Communicable Disease Service, Infectious and
Zoonotic Disease Program, Epidemiology,
Environmental and Occupational Health, New Jersey
Department of Health
Editors
Edward Lifshitz, MD, FACP
Medical Director
Kim Cervantes, MA, MPH, CIC
Program Manager
Laura Taylor, PhD, MCHES
Viral Hepatitis Coordinator
Keerti Kalluru, BSPH
Public Health Associate
Callie Shane
Management Assistant
Communicable Disease Service, Infectious and Zoonotic
Disease Program, Epidemiology, Environmental and
Occupational Health, New Jersey Department of Health
Acknowledgments
Council of State and Territorial Epidemiologists, Leading Epidemiologists Advancing Data Program
New Jersey Viral Hepatitis Elimination Advisor Group
Page | 2
CONTENTS
CONTRIBUTORS ............................................................................................................................................................ 1
EXECUTIVE SUMMARY .................................................................................................................................................. 3
ABBREVIATIONS ............................................................................................................................................................ 4
BACKGROUND ............................................................................................................................................................... 5
New Jersey Geographical Distribution and Population Overview ............................................................................ 5
Social Characteristics/Social Determinants of Health............................................................................................... 6
VIRAL HEPATITIS SURVEILLANCE AND EPIDEMIOLOGY IN NEW JERSEY ....................................................................... 10
Testing for HCV Infection ........................................................................................................................................ 10
Scope of Hepatitis C Disease in New Jersey ............................................................................................................ 10
Acute Hepatitis C in New Jersey ............................................................................................................................. 10
Chronic Hepatitis C in New Jersey ............................................................................................................................ 15
Perinatal Hepatitis C ............................................................................................................................................... 15
Morbidity and Mortality ......................................................................................................................................... 17
VIRAL HEPATITIS IN SPECIAL POPULATIONS IN NEW JERSEY ....................................................................................... 21
HIV Co-infections .................................................................................................................................................... 21
Persons Who Use or Inject Drugs ........................................................................................................................... 21
Incarcerated individuals.......................................................................................................................................... 22
ADDRESSING VIRAL HEPATITIS IN NEW JERSEY ........................................................................................................... 24
Prevention and Education ...................................................................................................................................... 24
Hepatitis C Testing .................................................................................................................................................. 24
Hepatitis C Treatment ............................................................................................................................................ 25
Laboratory Based HCV Clearance Cascade ............................................................................................................. 26
SUMMARY .................................................................................................................................................................. 27
REFERENCES ............................................................................................................................................................... 28
APPENDIX .................................................................................................................................................................... 31
Page | 3
EXECUTIVE SUMMARY
Hepatitis C virus (HCV) is one of the most common types of viral hepatitis in the United States.
An estimated 2.4 million people in the United States were living with hepatitis C during 2013–
2016 (1). Hepatitis means inflammation of the liver. HCV does not only impact the liver but can
affect an individual’s overall health. HCV is transmitted by infected blood and blood products.
HCV may present as either an acute or chronic illness. The most common method of
transmission is intravenous drug use and the sharing of injecting equipment. People at greatest
risk for HCV include people who use or used injection drugs, who have HIV infection or other
comorbidities, certain occupations, and children born to mothers who have HCV.
HCV is one of the most frequently reported infectious diseases in the state of New Jersey. The
yearly overview of HCV in New Jersey includes:
• About 100 to 145 acute HCV infections reported
• An average of 6820 new chronic cases reported
• Based on reported cases, about 470 babies who were exposed to HCV
This HCV epidemiologic profile describes the burden of HCV on the population of New Jersey
over a five-year period, from 2016 through 2020. More specifically, the epidemiologic profile’s
three main purposes are to:
• Provide a description of HCV among the state’s population/subpopulations in terms
of sociodemographic, geographic, behavioral, and clinical characteristics.
• Describe the status of persons with HCV infection and provide some understanding
of future HCV distribution.
• Identify characteristics of populations who are living with, or who are at high risk
for, HCV in defined geographic areas and who need prevention or care services.
This epidemiologic profile can serve as a valuable tool at the state and local levels to assist in
making hepatitis C related decisions around resource allocations for prevention and care
resources, planning and evaluation programs, and policymaking. Moreover, this profile can be
used to streamline the work of the New Jersey Department of Health (NJDOH) and its partners
who are involved in viral hepatitis elimination planning.
Page | 4
ABBREVIATIONS
AASLD: American Association for the Study of Liver Diseases
ACA: Affordable Care Act
ACS: American Community Survey
AIDS: Acquired Immunodeficiency Syndrome
CDC: Centers for Disease Control and Prevention
CDS: Communicable Disease Service within the NJDOH
CDRSS: Communicable Disease and Surveillance System
DAA: Direct Acting Antiviral
DMHAS: Division of Mental Health and Addiction Services
within the NJ Department of Human Services
EBC: Electronic Birth Registration
ELR: Electronic Laboratory Reporting
HCV: Hepatitis C Virus
HIV: Human Immunodeficiency Virus
ICD: International Classification of Diseases
IDSA: Infectious Diseases Society of America
IDU: Injection Drug Use
IZDP: Infectious and Zoonotic Disease Program
within the NJDOH
MMC: Medicaid Managed Care
MSM: Men Who Have Sex with Men
NCI: National Cancer Institute
NCHS: National Center for Health Statistics
NHANES: National Health and Nutrition Examination Survey
NJAC: New Jersey Administrative Code
NJDOH: New Jersey Department of Health
NNDSS: National Notifiable Disease Surveillance System
PWID: People Who Inject Drugs
PWUD: People Who Use Drugs
RNA: Ribonucleic Acid
STD: Sexually Transmitted Diseases
US: United States

Page | 5
BACKGROUND
New Jersey Geographical Distribution and Population Overview
New Jersey is in the Mid-Atlantic region of the United States. It is about 150 miles long and 70
miles wide, comprising 8,722 square miles and includes urban, suburban, and rural areas. New
Jersey has a population of approximately nine million residents and borders two large
metropolitan areas, New York City and Philadelphia (Figure 1). It is the most densely populated
state in the United States and is composed of 21 counties and 564 municipalities. Hudson County
is the smallest county (46.19 square miles), and Burlington County is the largest (798.58 square
miles). The capital of New Jersey is the City of Trenton, located in Mercer County, which is also
the approximate geographic center of the state (2).
Figure 1: State of New Jersey counties and
transportation network
Source: State of New Jersey Profile
(mit2019_section4_State_Profile.pdf (nj.gov))
In 2018, the estimated population of New
Jersey was 8,908,520 with 51% female and 49%
male (3). The three most populous counties
were Bergen, Middlesex, and Essex, whereas
the three least populated counties were Salem,
Cape May, and Warren (Figure 2). The largest
population by age group was between 25 and
54 years of age (Figure 3). When categorized by
race alone or in combination, with one or more
other races, the largest population was White
69.1%, followed by Black/African American
15%, then Asian 10.7% (Figure 4). In terms of
Hispanic or Latino race, 79.40% of the
population was non-Hispanic and 20.60%
Hispanic. The proportion of foreign-born
persons in 2018 was 22.8%, second highest in
the nation after California (26.9%), and higher
than the United States average of 13.7% (4),
with most residing in northern counties:
Hudson, Bergen, Passaic, Union, and Essex.
For public health planning and assessment purposes regarding HCV, NJDOH groups
New Jersey counties into the following six public health regions:
Northwest:
Morris, Passaic, Sussex, Warren
Northeast
Bergen, Essex, Hudson
Central West:
Hunterdon, Mercer, Somerset
Central East:
Middlesex, Monmouth, Ocean, Union
Southwest:
Burlington, Camden, Gloucester, Salem
Southeast:
Atlantic, Cape May, Cumberland

Page | 6
Figure 2: New Jersey population by
county, population estimate, 2018
Figure 3: New Jersey population by age group, 2018
Source: American Community Survey (ACS)
Figure 4: New Jersey population by race, 2018
80%
70%
60%
50%
40%
30%
20%
10%
0%
White Black/African
American
Source: American Community Survey
Asian Other Amer Indian/
Alaska Native
Race
Social Characteristics/Social Determinants of Health
Social determinants indicators (i.e., social, behavioral, and environmental factors), such as
education level and income, contribute substantially to an individual’s health outcome. People
with lower socioeconomic status are more likely to have unhealthy lifestyle behaviors and lack
access to health care and information on preventive measures for communicable diseases.
69.1%
New Jersey
United States
15.0%
10.7%
7.5%
0.6%
Percent
of population

Page | 7
Education Attainment
People who do not graduate from high school or attend college are less likely to be employed in
safe, high-paying jobs and more likely to have health problems (5). In 2018, for the population
aged 25 years and older in New Jersey, 9.8% did not graduate high school and fewer than 50%
received a bachelor’s degree or higher Figure 5 (6).
Figure 5: Education attainment for the population 25 years and over, 2018
Source: American Community Survey
Median Household Income and Poverty Rate
Socioeconomic factors, such as poverty and living conditions, play a significant role in shaping
infection risk and disease outcomes. Often, people in poverty live in crowded conditions, must
continue to work when they are sick, encounter more stress, and are more likely than others to
use drugs and alcohol (7). Based on the American Community Survey, the estimated median
household income by New Jersey County for 2018 ranged from $55,709 to $117,858 (Figure 6)
(6).
4.7%
26.3%
16.4%
6.6%
24.8%
16.0%
5.1%
0.0%
5.0%
10.0%
15.0%
20.0%
25.0%
30.0%
Proportion of Population
Education Attainment Level
Less than 9th grade
High school graduate
Some college, no degree
Associate's degree
Bachelor's degree
Graduate degree
12th grade, no diploma

Page | 8
Figure 6: New Jersey median household income for the population 25 years and over, 2018 by county
Source: American Community Survey
Civilian Non-institutionalized Population Who Are Uninsured
A lack of health insurance is associated with decreased care seeking and uptake of HCV
treatment, with cost being a driving factor. Having insurance coverage is associated with
increased linkage to care, faster approval times for treatment, and subsequent retention in care
(8). Since the Affordable Care Act (ACA) was enacted in March 2010, the number of uninsured
persons in New Jersey decreased by 40% from 2010 to 2019 (9). In 2018, the overall proportion
of uninsured, non-institutionalized residents under 65 years of age in New Jersey was 8.7%, with
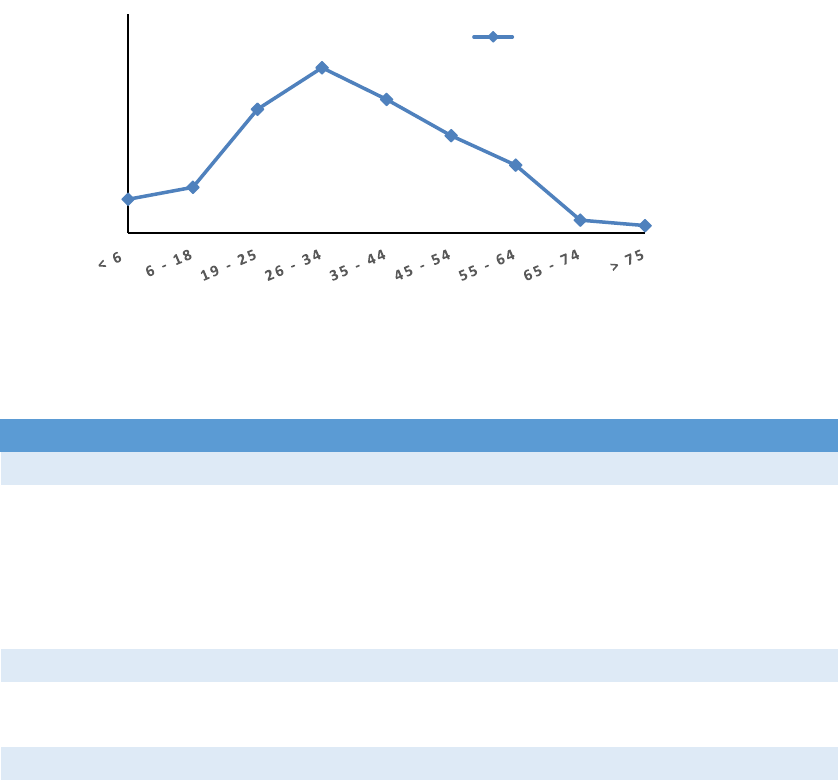
the highest proportion among the 26-34 age group, 15.1% (Figure 7). Of the non- institutionalized
residents between 19 through 64 years old, 9.5% of those employed, and 22.8% of those not
employed were uninsured (Table 1).
Page | 9
Figure 7: Percent of individuals uninsured by age group
Table 1: Number of residents uninsured based on employment status, nativity, and race/ethnicity, 2018.
Categories
Total
Uninsured
Uninsured %
Employment Status
Noninstitutionalized 19 to 64 years old
5,344,092
561,302
10.5%
In labor force
4,315,480
438,499
10.2%
Employed
4,112,267
392,099
9.5%
Unemployed
203,213
46,400
22.8%
Not in labor force
1,028,612
122,803
11.9%
Nativity
Native born
6,784,192
297,209
4.4%
Foreign born
2,019,796
357,791
17.7%
Race and Hispanic Origin
White
5,894,799
350,689
5.9%
Black
1,174,370
102,553
8.7%
American Indian/Alaska Native
20,790
3,732
18.0%
Asian
866,383
45,750
5.3%
Some other race
599,238
135,390
22.6%
Hispanic or Latino
1,822,422
315,286
17.3%
Source: American Community Survey
3.1%
4.2%
11.3%
15.1%
12.2%
8.9%
6.2%
1.2%
0.7%
0.0%
5.0%
10.0%
15.0%
20.0%
Proportion Uninsured
Age Group
Uninsured by Age
Page | 10
VIRAL HEPATITIS SURVEILLANCE AND EPIDEMIOLOGY IN NEW JERSEY
Testing for HCV Infection
Testing for HCV infection begins with either a rapid or laboratory-conducted assay for hepatitis C
virus (HCV) antibody in blood. A nonreactive HCV antibody result indicates no HCV antibody
detected. A reactive result indicates one of the following: 1) current HCV infection, 2) past HCV
infection that has resolved, or 3) false positivity. A reactive result should be followed by nucleic
acid testing (NAT) for HCV ribonucleic acid (RNA). If HCV RNA is detected, that indicates current
HCV infection. If HCV RNA is not detected, that indicates either past, resolved HCV infection, or
false HCV antibody positivity (10). Per N.J.A.C. 8:57, laboratories and health care providers must
report all suspected cases of newly diagnosed acute and chronic cases of HCV within 24 hours of
diagnosis to NJDOH (11).
Scope of Hepatitis C Disease in New Jersey
HCV represents one of the most common communicable diseases in New Jersey. On average,
NJDOH receives more than 10,000 reports of hepatitis C annually. After data cleaning,
deduplication, and case classification, the number of reports that meet the public health
surveillance case definition for acute and chronic HCV and that were reported to the Centers for
Disease Control and Prevention (CDC) during the 2016-2020 period ranged between 5,517
to 8,125 annually. Regarding overall prevalence of HCV in New Jersey, an analysis of serum
specimens taken from participants in the National Health and Nutrition Examination Survey
(NHANES) between 2013-2016 revealed a prevalence of 680 persons/100,000 population (12).
Acute Hepatitis C in New Jersey
Estimated Incidence of Hepatitis C in New Jersey
Despite being a reportable disease, many cases of diagnosed acute hepatitis C are not reported to
NJDOH. Most individuals with acute HCV infection do not have a clinically evident illness and, as
a result, do not seek medical care. Thus, determining the true incidence of new HCV infections
per year based on the number of reported cases requires complex epidemiological modeling
techniques. For each new acute HCV case that is reported in the United States, the CDC estimates
there are approximately 13.9 actual cases of new acute HCV (13). Using these estimates, in New
Jersey the estimated number of new cases per year can be as high as 2,000 (Figure 8). In 2018,
the actual number of acute cases reported was 112 compared to the estimated expected number
of 1,557.
Page | 11
Figure 8: Estimated incidence of acute hepatitis C in New Jersey versus reported cases, 2016-2020
2500
2000
1500
1000
500
0
2016 2017 2018 2019 2020
Year
New Jersey’s rate of acute cases ranked midway among states with reported acute hepatitis C
data in 2018 (13) and that are similar in geographic location and/or population density (14)
(Figure 9).
Figure 9: Rate per 100,000 population of reported cases of acute hepatitis C by selected states, 2018
2
1.8
1.6
1.4
1.2
1
0.8
0.6
0.4
0.2
0
CA CT MD VT IL NJ NY MA ME NH PA
Source: Centers for Disease Control and Prevention, and United States Census Bureau
Surveillance of Acute Hepatitis C in New Jersey
Between 2016 through 2020, 605 acute hepatitis C cases were reported to NJDOH (Figure 10).
The increase in reported cases from 2016 to 2017 could be related to a change in the public health
surveillance case definition applied in 2017
1
. More than 50% of reported acute HCV cases were
between 25 and 50 years of age, with case rates were highest in Cumberland, Burlington, and
Salem counties (Figure 11). The majority by gender at birth were male, 67.4%. In 2018, the rate
of confirmed acute HCV
cases
in
New
Jersey
was
1.1 per 100,000,
compared
to
1.2 per
100,000 population nationally. For each year over this five-year period, the most reported race
for acute HCV cases was White, followed by Black/African American (cumulative data with
numbers less than 5 were excluded) (Figure 12).
1
Hepatitis C, Acute 2016 Case Definition; https://ndc.services.cdc.gov/case-definitions/hepatitis-c-acute-2016/
Reported
Estimated
1556.8
112
Number
of Cases
1.8
1.9
1.6
1.7
1.1
1.2
0.6
0.6
0.7
0.3 0.3
Rate per 100,000
population

Page | 12
Figure 10: Total reported acute cases in New Jersey, 2016-2020
Figure 11: Characteristics of reported hepatitis C acute cases in New Jersey, 2016-2020
122
147
112
103
121
0
20
40
60
80
100
120
140
160
2016 2017 2018 2019 2020
Number of Cases
Year

Page | 13
Figure 12: Reported acute hepatitis C cases by race in New Jersey, 2016-202
Source: New Jersey Department of Health, Communicable Disease Service
Risk Factor Characteristics of Acute Hepatitis C Viral Infections
HCV was historically a concern among the “baby boomer” population, those born between 1946-
1964. However, in recent years, most new infections of HCV nationally and in New Jersey have
been among people who share needles, syringes, or other equipment used to prepare and inject
drugs (15). 2018 surveillance data for acute hepatitis C showed that 41 out of the 112 reported
cases or 36.7% were people who use drugs/people who inject drugs (PWUD/PWID), and most
were between the ages of 25-44 years. Other risk factors included unprotected sex (10.87%) and
close contact with a person with confirmed hepatitis infection (7.25%). Approximately 20% to
30% of persons who inject drugs become infected with HCV within the first two years of starting
injection drug use, and 50% become infected within five years of starting injection drug use (12).
Chronic Hepatitis C in New Jersey
Chronic Hepatitis C Surveillance in New Jersey
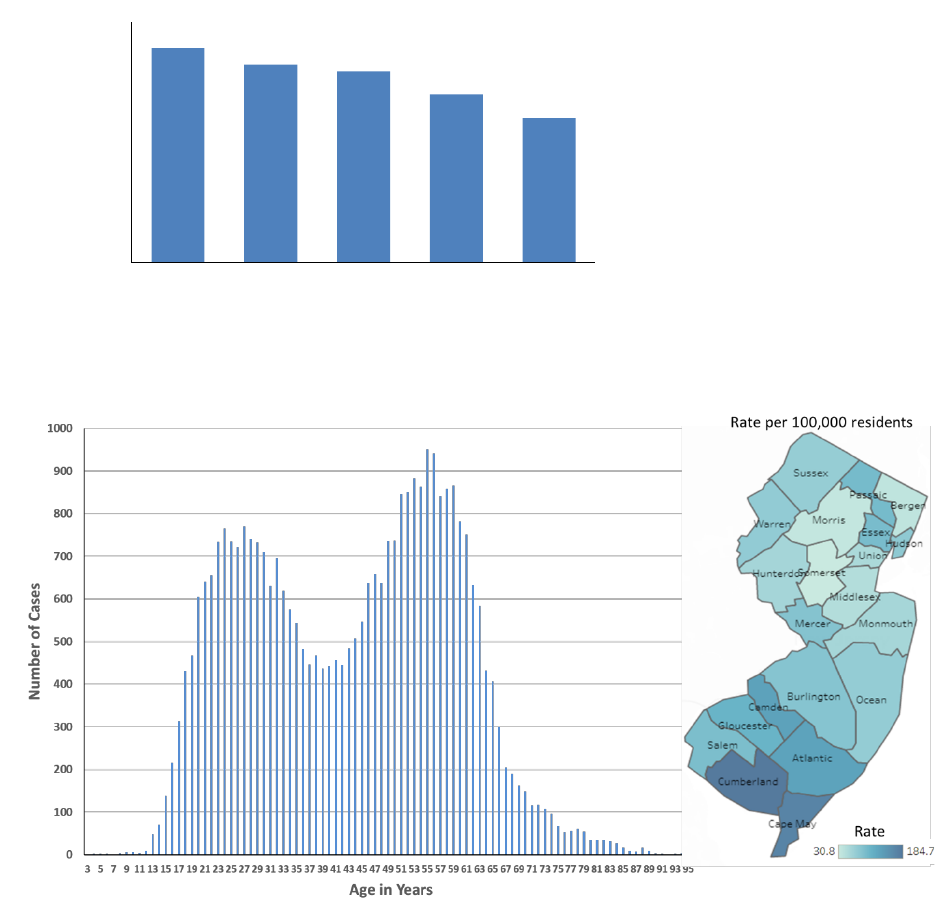
Between 2016 and 2020, there were a total of 34,098 reported chronic hepatitis C cases in New
Jersey (Figure 13). Over the five-year period, the number of reported cases steadily declined, with
a relatively larger decrease in 2020 (Figure 13) that may be due to COVID-19 and associated
reductions in care seeking and testing. The distribution of reported chronic HCV cases by age, and
gender is illustrated below. A bimodal age distribution with peaks occurring at age 30 years and
60 years is observed (Figure 14). This pattern is consistent with national trends (16). The highest
case rates over the five-year period were in Cumberland, Cape May, and Camden counties (Figure
14). Most chronic HCV cases by gender at birth were male, 61.6%.
0
20
40
60
80
100
120
140
160
2016 2017 2018 2019 2020
Number of Cases
Asian Black/African American Unknown White
Page | 14
Figure 13: Total reported chronic cases in New Jersey, 2016-2020
Figure 14: Characteristics of reported chronic hepatitis C cases in New Jersey, 2016-2020
Between 2016 and 2020, only 43% of reported chronic hepatitis C cases included information on
race. Obtaining race information for reported chronic HCV cases has been a challenge due to the
large number of cases and limited number of public health investigators at the local level focused
on chronic hepatitis C. Like acute HCV cases for each year, the most frequently reported race for
chronic HCV cases was White, followed by Black/African American (Figure 15). Unlike acute cases,
the proportion of cases with ethnicity information is low for chronic cases.
8006
7402
7148
6289
5396
0
1000
2000
3000
4000
5000
6000
7000
8000
9000
2016 2017 2018 2019 2020
Number of Cases
Year

Page | 15
Figure 15: Reported chronic hepatitis C cases by race a) and ethnicity b) in New Jersey, 2016-2020
Source: New Jersey Department of Health, Communicable Disease Service
Perinatal Hepatitis C
The increase in HCV infection related to injection drug use in young adults has resulted in a
corresponding increase among women of childbearing age, age 15 to 44, and women diagnosed
during pregnancy (17). A doubling of HCV diagnoses among women of childbearing age was
observed between 2006 and 2014, surpassing the number among women in older age cohorts
(17). Vertical transmission of HCV occurs in approximately 5.8% of infants born to women who
are infected with HCV and in up to twice as many infants born to women who have high HCV viral
loads (18). In 2018, universal hepatitis C screening during pregnancy was recommended by the
American Association for the Study of Liver Diseases (AASLD) and the Infectious Diseases Society
of America (IDSA) (19). Hepatitis C screening is recommended for all pregnant women during
each pregnancy.
NJDOH began monitoring babies born to pregnant people with known HCV infection in 2018. New
Jersey recommends that babies are monitored until they reach 36 months of age to capture HCV
laboratory test results. Additionally, NJDOH works with birthing facilities in New Jersey to ensure
the birthing parent’s HCV status is included on the electronic birth certificate. This process aims
to better capture the HCV burden among this population and to identify babies born to HCV
positive parents to ascertain perinatal HCV transmission.
0
2000
4000
6000
8000
10000
2016 2017 2018 2019 2020
Number of Cases
ASIAN BLACK/AFRICAN AMERICAN
UNKNOWN WHITE
AMERICAN INDIAN/ALASKAN NATIVE NATIVE HAWAIIAN/PACIFIC ISLANDER

Page | 16
Between 2017 and 2020, the number of women of childbearing age infected with HCV was
highest among those 25-34 years of age (Figure 16). The southern regions of the state had the
highest rates of HCV-infected women of childbearing age per 10,000 population (Figure 17) and,
similarly, had the highest rates of babies exposed to women infected with HCV (data was
retrospectively collected for the year 2017) (Figure 18). Electronic birth certificate reporting
varies widely by birthing hospital, which may impact regional estimates from 2018 to 2019. At
least one birthing hospital in each region did not report any births associated with hepatitis C. In
2019, in the northeast region there were five hospitals who reported no births associated with
hepatitis C. Ultimately, the number of babies in New Jersey who tested positive for HCV and met
the perinatal HCV case definition in 2017, 2018, 2019, and 2020 was 6, 10, 11, and 8, respectively.
Figure 16: Number of reported women of childbearing age infected with HCV by age group, 2017-2020
800
600
400
200
0
2017 2018 2019 2020
Years
Source: New Jersey Department of Health, Communicable Disease Service
Figure 17: Rate of HCV-infected women of childbearing age per 10,000 population by region, 2017-2020
20.0
15.0
10.0
5.0
0.0
Northwest Northeast
Central West Central East
Southwest Southeast
Regions
Source: New Jersey Department of Health, Communicable Disease Service
15-24 25-34 35-44
2017 2018 2019 2020
Rate per 10,000
Population
Number of
women
infected

Page | 17
Figure 18: Rate of reported perinatal HCV exposure per 10,000 female population of childbearing age, by
public health regions, 2017-2020
10.0
8.0
6.0
4.0
2.0
0.0
Northwest Northeast
Central West Central East South West Southeast
Regions
Source: New Jersey Department of Health, Communicable Disease Service
Morbidity and Mortality
Hepatocellular Cancer
Each year in the United States, around 31,000 people are diagnosed with liver cancer. Among
people with certain liver cancers in the United States, more than 50% have HCV at the time of
cancer diagnosis. Early detection and treatment of viral hepatitis could prevent 90,000 liver
cancer deaths by 2030, starting with 2015 as the baseline year (20). In New Jersey, the observed
incidence rates of liver and intrahepatic bile duct cancer steadily increased from 2009 through
2018 for all ages (Figure 19) (21). During 2018, 561 male and 211 female New Jersey residents
were diagnosed with liver cancer (22).
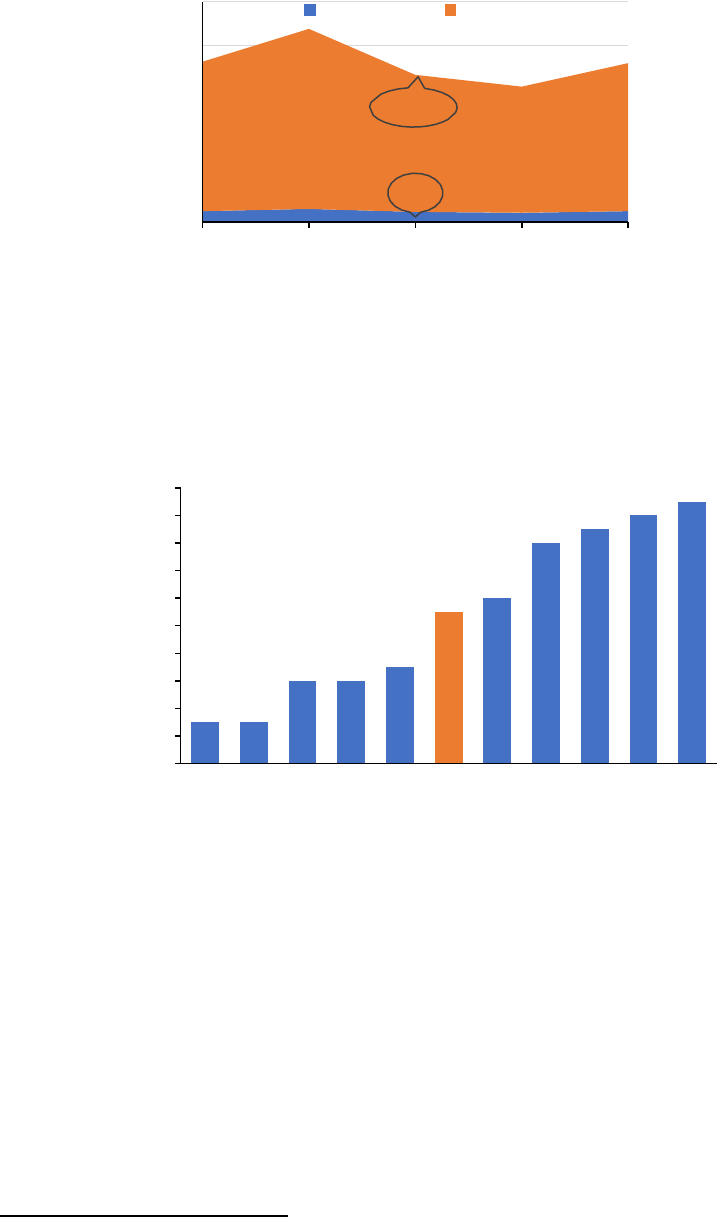
Figure 19: Observed liver and intrahepatic bile duct cancer incidence rates in New Jersey, 2009-2018
Source: National Cancer Institute
6
6.5
7
7.5
8
8.5
2009 2010 2011 2012 2013 2014 2015 2016 2017 2018
Incidence rate per 100,000 population
Years
2017 2018 2019 2020
Exposure
per 10,000
Population

Page | 18
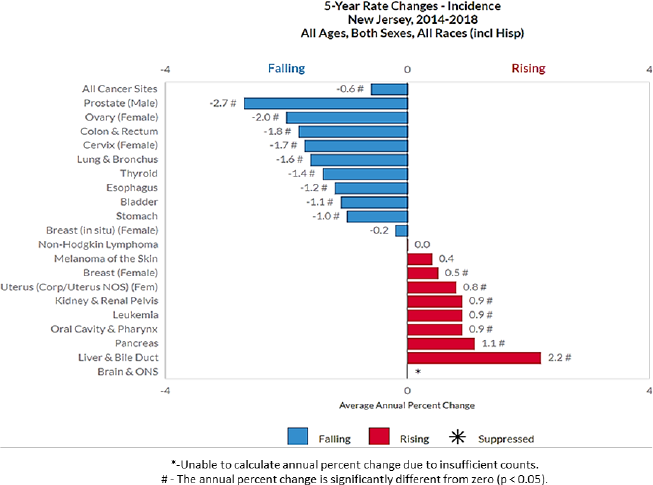
In New Jersey, the average incidence rates of liver and bile duct cancer vary by county and sex
(Figure 20). Camden, Cape May, Cumberland, Hudson, and Ocean counties have the highest
incidence rate for females whereas Atlantic, Camden, Cape May, and Cumberland counties have
the highest incidence rate for males. Cancer of the liver is more common in older people and is
more common in men than in women. In New Jersey, after brain and other nervous system
cancers, liver and bile duct cancer had the greatest increase in incidence rates between 2014 and
2018 (23) (Figure 21).
Figure 20: Average Incidence rates of liver and bile duct cancer in females and males by county, 2014-2018
Source: National Cancer Institute
*Data has been suppressed to ensure confidentiality and stability of rate estimates. Data is currently being
suppressed if there are less than 16 counts in a period.
Page | 19
Figure 21: Average annual percent change of different types of cancer, 2014-2018
Source: National Cancer Institute
Hepatitis C as Cause of Death
Death certificate data is used to characterize deaths in the United States associated with hepatitis
C (23). An overall decline in death rates associated with HCV is noted from 2016 through 2020
(Figure 22). This decline is consistent with the decrease in reported chronic HCV cases and could
be related to people with chronic hepatitis C receiving treatment. The slight increase in 2020
could be due to fewer people receiving treatment and/or people with hepatitis C dying from
causes related to COVID-19. Counties with the highest death rates of hepatitis C as the underlying
cause of death from 2016 to 2020 were Essex, Hudson, Camden, Mercer, and Passaic, with crude
rates of 1.5 to 1.1 per county population (24).

Page | 20
Figure 22: Deaths per 100,000 population where underlying cause of death was hepatitis C in New Jersey
and the United States, 2016-2020
4.5
4
3.5
3
2.5
2
1.5
2016 2017 2018 2019 2020
Year
Source: Centers for Disease Control and Prevention
Liver Cancer as Cause of Death
Liver and intrahepatic bile duct cancer is the sixth leading cause of cancer death in the United
States. The death rate was 6.6 per 100,000 population per year based on 2016-2020 age- adjusted
deaths (21). In 2019, for every 100,000 people, there were eight new liver and intrahepatic bile
duct cancer cases, and seven deaths. In New Jersey, between 2018 and 2020, there were 2048
liver cancer-related deaths reported, with a crude rate of 7.7 per 100,000 population (25). The
number of liver cancer related deaths was largest among people aged 65-74 years (Figure 23).
Figure 23: Number of liver-related cancer deaths for New Jersey residents by age group, 2018-2020
400
350
300
250
200
150
100
50
0
35-39 40-44 45-49 50-54 55-59 60-64 65-69 70-74 75-79 80-84 85-89 90-94 95-99
Age Group
Source: Centers for Disease Control and Prevention
New Jersey
United States
Death per 100,000
Number
of deaths
Page | 21
VIRAL HEPATITIS IN SPECIAL POPULATIONS IN NEW JERSEY
HIV Co-infections
HCV and human immunodeficiency virus (HIV) are bloodborne viruses transmitted through direct
contact with the blood of an infected person, and, as a result, co-infection with HIV and HCV is
common. Among injection-drug users who have HIV, 62-80% are co-infected with HCV (26).
Although transmission via injection-drug use remains the most common mode of HCV acquisition
in the United States, sexual transmission is an important mode of acquisition among Men Who
Have Sex with Men (MSM) with HIV who also have risk factors, including those who use non-
injection drugs. HCV infection may also affect the management of HIV infection (26).
Of the 7,258 HCV cases reported to NJDOH in 2018, 258 (3.6%) were co-infected with HIV/AIDS.
Over 60% of those infected with HCV or HIV/AIDS, resided in Essex, Hudson, Union, Passaic, and
Middlesex counties. Fifty-two percent of the co-infected individuals were exposed to HIV/AIDS
through injection drug use (IDU) or MSM/IDU, 2.8 times the proportion among the HIV/AIDS
group that is not co-infected with HCV. Mortality was higher among HCV cases co-infected with
HIV, 6.4% died between the beginning of 2018 through August 2019, compared to 2% for HCV
cases not co-infected. The risk of mortality among HCV cases co-infected with HIV is greater than
3 times that of the HCV non co-infection group.
Persons Who Use or Inject Drugs
A deadly consequence of the opioid crisis is an increase in blood-borne infections, including viral
hepatitis (27). PWUD or PWID are at risk for HCV infection through the sharing of needles and
equipment used to prepare and inject drugs. In recent years, an emerging HCV epidemic has been
occurring among young PWID, particularly in rural and suburban settings (28). Between 2016 and
2019, the highest rate of drug-related hospital visits were among persons 25-34 years of age,
followed by persons 15-24 and 35-44 years of age (Figure 24) (29).
Page | 22
Figure 24: Rate of drug-related hospital visits per 100,000 population by age group in New Jersey, 2016-
2019
600
500
400
300
200
100
0
<15 15-24 25-34 35-44 45-54 55-64 65-74 75-84 85+
Age Group
Source: New Jersey Department of Health, Population Health
PWID/PWUD was the most frequently reported risk factor for reported acute hepatitis C cases in
2018, 2019, and 2020 at 36.6%, 46.6% and 33%, respectively. Acute HCV cases between 25
through 34 years of age had the highest proportion of PWID/PWUD (Figure 25).
Figure 25: Proportion of reported acute HCV cases with identified PWID/PWUD by age group, New
Jersey, 2018-2020
60
50
40
30
20
10
0
15-24 25-34 35-44 45-54 55-64
Age Group
Source: Source: New Jersey Department of Health, Communicable Disease Service
Incarcerated individuals
Hepatitis C prevalence in U.S. correctional settings is disproportionately high because of
disproportionately high incarceration rates among persons who use drugs (30). Compared
with the general population, the prevalence of viral hepatitis and other bloodborne related
diseases such as HIV is higher among people who are incarcerated, with hepatitis C rates 10 times
higher in jails and prisons (31). The correctional institutions and jails in New Jersey that house
2019
2018
2017
2016
2018 2019 2020
Proportion
of Cases
Visits
per 100,000
Page | 23
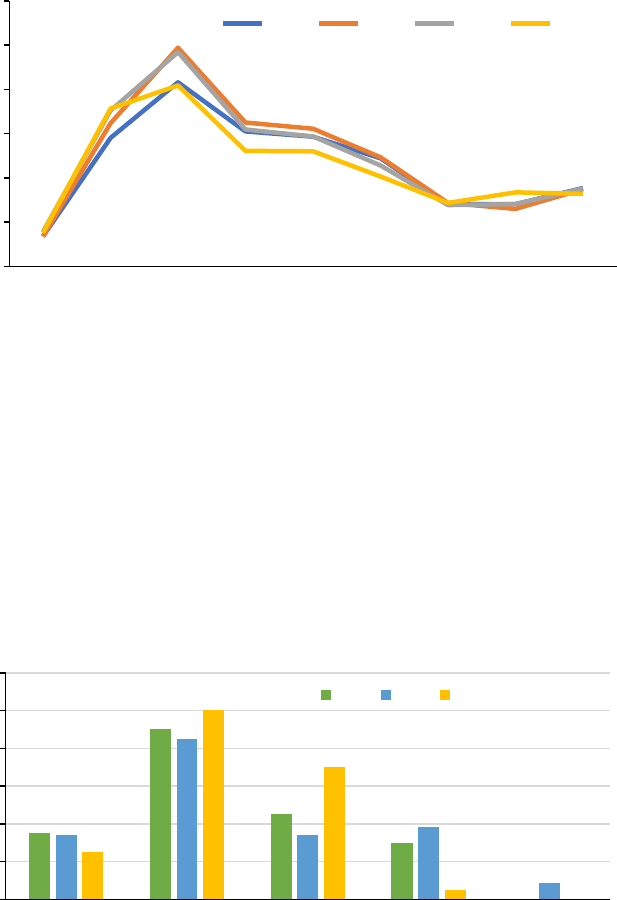
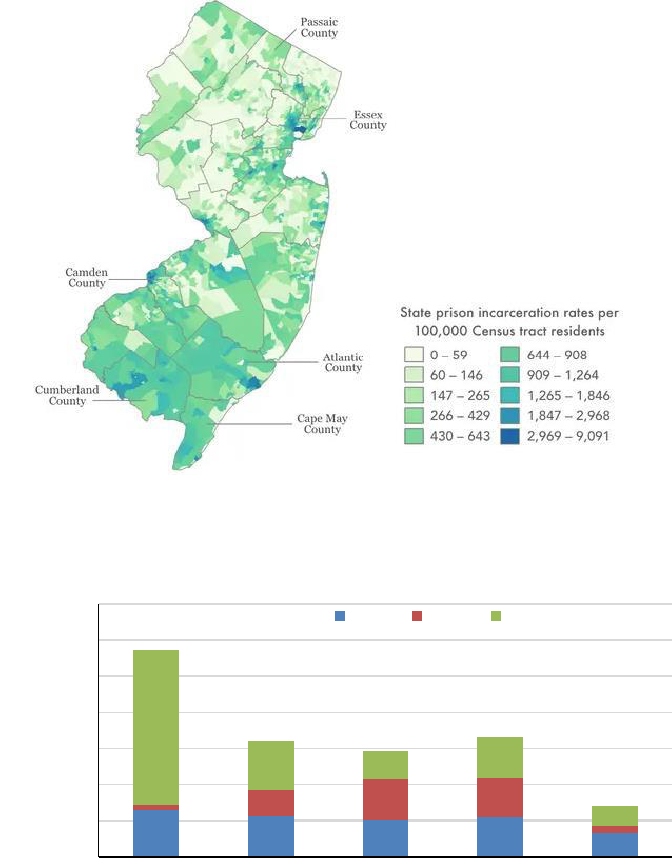
confined inmates are mainly federal, state, and county facilities. Six counties in New Jersey account
for roughly a quarter of the state’s population, however, more than half of the state’s imprisoned
population come from those counties (Figure 26) (32). Between 2016 and 2020, there has been an
increased number of HCV reports from federal facilities and a decreased number from state
facilities (Figure 27) (8).
Figure 26. State prison incarceration rates per 100,000 population (2020)
Source: Prison Policy Initiative
Figure 27: Number of cases reported with hepatitis C by correctional facility, 2016-2020
700
600
500
400
300
200
100
0
2016 2017 2018 2019 2020
Year
Source: New Jersey Department of Health, Population Health
County Federal State
Number
of cases
Page | 24
ADDRESSING VIRAL HEPATITIS IN NEW JERSEY
Prevention and Education
Successful hepatitis C surveillance and prevention plans require strong collaboration. The goal of
this collaboration is to use surveillance data to accurately identify high-impact settings and
populations, linking those in need to services, and prevention of new infections. The NJDOH
Communicable Disease Service (CDS) is continually working collaboratively with partners at the
federal, state, and local levels to accomplish such goals.
In October 2019, NJDOH participated in a statewide Viral Hepatitis Summit. This event drew 200
stakeholders and partners from across the state and served as the kickoff to the ongoing viral
hepatitis elimination planning in the state. Elimination planning is an integrative and
collaborative approach, with several focus areas, including HCV testing, data sharing, educational
outreach, linkage to care, harm reduction and technical support.
Hepatitis C Testing
CDC’s 2020 updated testing recommendations for HCV infection call for universal screening: a
one‑time hepatitis C testing regardless of age or setting prevalence among people with
recognized conditions or exposures, routine periodic testing for people with ongoing risk factors,
and ad hoc testing of any person who requests hepatitis C testing (33). One of the main goals of
the CDS HCV program is to promote HCV testing with a focus on the populations most at-risk. CDS
encourages health care providers, through education and outreach, to incorporate universal HCV
testing using recommended diagnostic tests (Appendix Figure 30). Currently, New Jersey only
requires positive HCV test results to be reported to the state. This makes it difficult to calculate
the total number of individuals tested for HCV, as well as those who may develop an acute
infection. Revised regulations targeted for 2024 are expected to include a requirement for the
reporting of negative hepatitis C results. This should facilitate better understanding of the
hepatitis C burden in New Jersey.
In New Jersey, 12 commercial labs conduct hepatitis C testing and report results via electronic
laboratory reporting (ELR) to NJDOH, as do all 71 acute care hospitals and three public health
laboratories (New Jersey, New York, and Florida). NJDOH has a viral hepatitis service locator
interactive dashboard available to the public 24/7 (34). This dashboard includes an HCV testing
facility locator as illustrated below (Figure 28).

Page | 25
Figure 28: HCV testing facilities in New Jersey.
Source: New Jersey Department of Health
Hepatitis C Treatment
While there are many challenges regarding HCV treatment, both personal and systematic, NJDOH
and other partners aim to address some of these barriers through elimination initiatives.
Systematically, there have been some improvements. As of 2018, fibrosis restrictions for access
to HCV treatment for Medicaid Managed Care (MMC) clients were lifted in New Jersey. There are
also no restrictions on the time abstained from drug or alcohol use, prescriber, or retreatment
restrictions. However, prior authorization requirements currently remain in place for HCV
treatment from MMC plans. There are several free or low-cost providers in the state who provide
HCV treatment, (34) (Figure 29), and HCV treatment is also provided in state correctional settings.
Figure 29: HCV treatment facilitates in New Jersey.
Source: New Jersey Department of Health

Page | 26
Laboratory Based HCV Clearance Cascade
Construction of an HCV testing cascade that quantifies screening and confirmatory testing can
help public health agencies ensure equity in diagnosis and linkage to HCV care at the population
level (35). Using CDC’s guidance, a laboratory-based care cascade model was developed from
HCV antibody and HCV RNA test results reported to the Communicable Disease Reporting and
Surveillance System (CDRSS) for the first time for a resident between 2018 and 2020. Cases were
evaluated for subsequent testing up to September 2022.
The HCV cure rate in New Jersey is low. The model shows that of the 18,787 persons who had a
positive anti-HCV test during the evaluation period (ever infected), 52.9% had an initial positive
HCV RNA reported (initial infection), with a subsequent positive HCV RNA 49.3% (not cured) and
6.6% had a subsequent negative HCV RNA (cured) reported (Figure 30). This cascade also suggests
that infection status is unknown for nearly half of individuals who were ever infected.
Figure 30: Laboratory-based HCV clearance cascade for New Jersey, 2018–2020
18787
Ever Infected Initial Infection Not Cured Cured/Cleared
In terms of specific populations, the HCV care cascade analysis highlights some disparities, (Table
2). Males are more likely to be infected with HCV, but less likely to receive confirmatory testing
and to achieve cure compared to females. The cascade analysis also shows that the 15-34-years
and 55-64 years age groups were most likely to not achieve cure despite receiving confirmatory
test results.
Because only positive HCV laboratory results are required to be reported to NJDOH, determining
the number of HCV infected persons who receive treatment is a challenge. A subset of
laboratories and hospitals do provide negative laboratory HCV results to NJDOH. However,
mandatory reporting of negative HCV results will better inform the progress of and gaps in HCV
treatment in the state.
9929, 52.9%
9269, 49.3%
660, 6.6%

Page | 27
Table 2: Conditional proportions for the laboratory-based HCV clearance cascade by subpopulation
Characteristics
Ever
Infected
No Viral
Tests
No Viral
Tests
Proportion
(%)
Initial
Infection
Not
Cured or
Cleared
Not Cured or Cleared
Proportion (%)
Age Group
<15
106
55
0.3
40
39
0.4
15-34
4862
1709
9.1
2945
2754
27.7
35-44
3215
1269
6.8
1823
1716
17.3
45-54
2921
1325
7.1
1482
1382
13.9
55-64
4500
2186
11.6
2177
2008
20.2
65-74
2516
1218
6.5
1180
1099
11.1
75+
667
349
1.9
282
271
2.7
Sex at birth
Female
7348
3393
18.1
3602
3355
33.8
Male
11415
4703
25
6318
5905
59.5
Unknown
24
15
0.1
9
9
0.1
Race/Ethnicity
White, NH
7924
2932
15.6
4660
4303
43.3
Black, NH
2608
1114
5.9
1406
1322
13.3
Hispanic
1978
829
4.4
1075
1004
10.1
Asian, NH
27
14
0.1
12
12
0.1
Asian
382
172
0.9
185
177
1.8
Other/Unknown
5868
3050
16.2
2591
2451
24.7
Total
18787
8111
43.2
9929
9269
93.4
SUMMARY
In observing data over the period 2018 through 2020, the New Jersey Hepatitis C Epidemiologic
Profile provides background information related to HCV disease burden and the overall landscape
of HCV in the state. HCV is one of the most common communicable diseases in the state of New
Jersey. From 2016 through 2020, there were 605 newly acquired, 34,098 chronic, and 35 perinatal
cases reported to NJDOH. Not all individuals are aware of their hepatitis status, and there is
significant underreporting of cases. Many individuals face various social constraints that impact
infection risk, access to health care, and information on preventative measures for this
communicable disease. Currently, the primary risk factor for HCV infection is injection drug use.
This profile points to the importance of appropriate testing, improved surveillance, aggressive
prevention and education activities, and collaboration with various partners to keep New Jersey
on track for HCV elimination. Furthermore, this document can be used as a resource for
researchers, providers, policymakers, and all residents of New Jersey who are dedicated to the
elimination of hepatitis C.
Page | 28
REFERENCES
1. Estimating prevalence of hepatitis C virus infection in the United. Hofmeister, Megan G. 3, Atlanta:
Hepatology, 2019, Vol. 69.
2. State of New Jersey. 2019 New Jersey State Hazard Mitigation Plan. Office of Emergency
Management. [Online] January 25, 2019. [Cited: March 7, 2022.]
https://www.state.nj.us/njoem/mitigation/2019-mitigation-plan.shtml.
3. United States Census Bureau. Demographics and Housing Estimates, 2018: ACS 1-Year Estimates
Subject Tables. American Community Survey. [Online] 2018. [Cited: May 20, 2022.]
https://data.census.gov/table?q=DP05&g=0400000US34,34$0500000&y=2018.
4. Selected Social Characteristics in the United States, 2018: ACS 1-Year Estimates Subject Tables.
American Community Survey. [Online] 2018. [Cited: May 27, 2022.]
https://data.census.gov/table?q=Native+and+Foreign+Born&g=0100000US_0400000US06,34,36&tid=A
CSDP1Y2018.DP02.
5. U.S. Department of Health and Human Services. Education Access and Quality. Healthy People 2020.
[Online] [Cited: April 17, 2023.] https://health.gov/healthypeople/objectives-and-data/browse-
objectives/education-access-and-quality.
6. United States Census Bureau. Selected Economic Characteristics. American Community Survey.
[Online] 2018. [Cited: May 20, 2022.]
https://data.census.gov/table?g=040XX00US34_050XX00US34001&tid=ACSDP1Y2018.DP03.
7. Vaida, Bara. Covering Health. Association of Health Care Journalists. [Online] September 27, 2018.
[Cited: April 17, 2023.] https://healthjournalism.org/blog/2018/09/connecting-the-dots-between-social-
determinants-and-infectious-diseases/.
8. Alexandra DeBose-Scarlett, Raymond Balise, Deukwoo Kwon, Susan Vadaparampil, Steven Xi Chen,
Eugene R. Schiff, Gladys Patricia Ayala, and Emmanuel Thomas. Obstacles to Successful Treatment of
Hepatitis C in Uninsured Patients from a Minority Population. Journal of Translational Medicine. 16,
2018, Vol. 178.
9. Healthinsurance.org. New Jersey and the ACA's Medicaid Expansion. A Trusted Independent Health
Insurance Guide Since 1994. [Online] Healthinsurance.org, 1994-2023. [Cited: February 28, 2023.]
https://www.healthinsurance.org/medicaid/new-jersey/.
10. Centers for Disease Control and Prevention. Laboratory Testing. Viral Hepatitis. [Online] March 28,
2019. [Cited: October 10, 2022.] https://www.cdc.gov/hepatitis/hcv/labtesting.htm.
11. State of New Jersey Department of Health. NJ Administrative Code. Communicable Disease Service.
[Online] April 5, 2017. [Cited: May 20, 2022.]
https://www.nj.gov/health/cd/imm_requirements/acode/index.shtml.
Page | 29
12. University of Washington. HCV Epidemiology in the United States. Hepatitis C Online. [Online] May
26, 2021. [Cited: July 25, 2022.] https://www.hepatitisc.uw.edu/go/screening-diagnosis/epidemiology-
us/core-concept/all.
13. Hepatitis, Division of Viral. 2018 Surveillance Report. Viral Hepatitis. [Online] August 7, 2020.
[Cited: July 22, 2022.]
https://www.cdc.gov/hepatitis/statistics/2018surveillance/pdfs/2018HepSurveillanceRpt.pdf.
14. United States Census Bureau. Historical Population Density Data (1910-2020). Census.gov. [Online]
April 26, 2021. [Cited: July 20, 2022.] https://www.census.gov/data/tables/time-series/dec/density-
data-text.html.
15. Centers for Disease Control and Prevention. Hepatitis C Questions and Answers for Health
Professionals. Viral Hepatitis. [Online] Division of Viral Hepatitis, National Center for HIV, Viral Hepatitis,
STD, and TB Prevention, August 7, 2020. [Cited: July 22, 2022.]
https://www.cdc.gov/hepatitis/hcv/hcvfaq.htm#b1.
16. Hepatitis C now heavily impacting multiple generations. NCHHSTP Newsroom. [Online] April 9,
2020. [Cited: June 21, 2021.] https://www.cdc.gov/nchhstp/newsroom/2020/hepatitis-c-impacting-
multiple-generations.html.
17. Changing epidemiology, implications, and recommendations for hepatitis C in women of childbearing
age and during pregnancy. Tatyana Kushner, Nancy Reau. New York: Journal of Hepatology, 2021, Vol. 74.
18. Alaya Koneru, et al. Increased Hepatitis C Virus (HCV) Detection in Women of Childbearing Age and
Potential Risk for Vertical Transmission — United States and Kentucky, 2011–2014. Morbidity and
Mortality Weekly Report (MMWR). 2016, Vol. 65, 28.
19. Sarah Schille et al. CDC Recommendations for Hepatitis C Screening Among Adults — United States,
2020. Morbidity and Mortality Weekly Report (MMWR). 2020, Vol. 69, 2.
20. Centers for Disease Control and Prevention. Viral Hepatitis & Liver Cancer Prevention Profile. CDC
Stacks. [Online] March 23, 2018. [Cited: August 16, 2022.] https://stacks.cdc.gov/view/cdc/109302.
21. National Institute of Health. Cancer Stat Facts: Liver and Intrahepatic Bile Duct Cancer. National
Cancer Institute, Surveillance Epidemiology and End Results Program. [Online] Surveillance Epidemiology
and End Results Program, 2022. [Cited: September 14, 2022.]
https://seer.cancer.gov/statfacts/html/livibd.html.
22. New Jersey Department of Health. Health Indicator Report of Incidence of Liver Cancer. New Jersey
State Health Assessment Data. [Online] December 03, 2021. [Cited: July 25, 2022.] https://www-
doh.state.nj.us/doh-shad/indicator/view/LiverCa.YearSex.html.
23. National Cancer Institute. Interactive Maps. State Cancer Profiles. [Online] September 14, 2022.
[Cited: September 14, 2022.]
https://statecancerprofiles.cancer.gov/map/map.withimage.php?34&county&001&035&00&1&01&0&
1&5&0#results.
24. Centers for Disease Control and Prevention. Viral Hepatitis. [Online] Numbers and rates* of deaths
with hepatitis C listed as a cause of death† among residents, by state or jurisdiction — United States,
Page | 30
2016-2020, August 17, 2022. [Cited: September 09, 2022.]
https://www.cdc.gov/hepatitis/statistics/2020surveillance/hepatitis-c/table-3.7.htm.
25. About Underlying Cause of Death, 1999-2020. CDC Wonder. [Online] National Center for Health
Statistics. National Vital Statistics, September 14, 2022. [Cited: September 14, 2022.]
https://wonder.cdc.gov/ucd-icd10.html.
26. Prevention, Centers for Disease Control and People Coinfected with HIV and Viral Hepatitis. Viral
Hepatitis. [Online] September 21, 2020. [Cited: September 19, 2022.]
https://www.cdc.gov/hepatitis/populations/hiv.htm.
27. Persons Who Inject Drugs (PWID). National Center for HIV, Viral Hepatitis, STD, and TB
Prevention. [Online] July 2018, 2018. [Cited: September 21, 2022.] https://www.cdc.gov/pwid/.
28. People Who Use or Inject Drugs and Viral Hepatitis. Viral Hepatitis. [Online] August 24, 2020.
[Cited: September 21, 2022.] https://www.cdc.gov/hepatitis/populations/idu.htm.
29. New Jersey Department of Health. Drug Related Hospital Visits. Population Health. [Online]
2022. [Cited: September 16, 2022.]
https://www.state.nj.us/health/populationhealth/opioid/opioid_hospital.shtml.
30. Center for Disease Control and Prevention. CDC Recommendations for Hepatitis C Screening Among
Adults — United States, 2020. Morbidity and Mortality Weekly Report (MMWR). [Online] April 10, 2020.
[Cited: September 21, 2022.] https://www.cdc.gov/mmwr/volumes/69/rr/rr6902a1.htm.
31. Centers for Disease Control and Prevention. CDC Recommendations for Correctional and Detention
Settings. National Center for HIV, Viral Hepatitis, STD, and TB Prevention. [Online] April 18, 2022. [Cited:
September 21, 2022.] https://www.cdc.gov/nchhstp/dear_colleague/2022/dcl-041822-correctional-
health.html.
32. Emily Widra, Henal Patel, and Ronald Pierce. Where people in prison come from: The geography of
mass incarceration in New Jersey. Where people in prison come from. [Online] June 2022. [Cited: April
17, 2023.] https://www.prisonpolicy.org/origin/nj/2020/report.html.
33. Centers for Disease Control and Prevention. Testing Recommendations for Hepatitis C Virus
Infection. Viral Hepatitis. [Online] July 29, 2020. [Cited: February 14, 2023.]
https://www.cdc.gov/hepatitis/hcv/guidelinesc.htm.
34. New Jersey Department of Health. New Jersey Department of Health Hepatitis Services Locator.
[Online] March 2022. [Cited: February 14, 2023.]
https://dashboards.doh.nj.gov/views/HepatitsServicesDashboard/Introduction?%3Aorigin=viz_share_lin
k&%3Aembed=y&%3AisGuestRedirectFromVizportal=y&_gl=1*vahojy*_ga*MTEzNDM5OTUwLjE2NDg1
NTg0NTU. *_ga_5PWJJG6642*MTY2OTA2Mjc0MS40MS4xLjE2NjkwNjI3NjQuM.
35. Quynh T Vo, Shauna Onofrey, Daniel Church, Kevin Cranston, Alfred DeMaria, R Monina Klevens.
The Massachusetts Hepatitis C Testing Cascade 2014-2016. Microbiology Insights. 2019, Vol. 12.

Page | 31
APPENDIX
Figure 31. CDC recommended HCV testing sequence

Page | 32
Figure 32. New Jersey median age by county, population estimate 2018
Table 3. Median household income and poverty rate for population 25 years and over based on
education level
Population > 25 years/
Earnings and Poverty Rate
Earnings,
all
Poverty %
all
Earnings
Male
Poverty %
Male
Earnings
Female
Poverty
%
Female
Population > 25 years
50,913
(X)
60,183
(X)
41,869
(X)
Less than high school graduate
24,963
22.4
30,484
19.1
18,126
25.5
High school graduate
34,431
10.1
41,717
7.7
27,460
12.3
Some college/Associate degree
42,079
7.5
51,474
5.7
35,177
9.1
Bachelor’s degree
65,658
3.4
79,360
2.9
55,702
3.7
Graduate or professional degree
89,332
(X)
109,510
(X)
73,106
(X)
Source: American Community Survey (ACS)

Page | 33
Table 4. Percent of individuals uninsured by year for residents under the age 65 years
16.0%
14.0%
12.0%
10.0%
8.0%
6.0%
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020
% Uninsured by Year
Source: New Jersey State Health Assessment Data
Figure 33. Age adjusted death rate, 2018-2020
45 - 49 50 - 54 55 - 59 60 - 64 65 - 69 70 - 74 75 - 79 80 - 84
Age Group
*Age groups without population data were excluded
Source: Centers for Disease Control and Prevention
Age Adjusted
Crude
Death
Rate
1.7
4
8.2
16.8
24.9
29
37.5
40.1
