
Disease Control Newsletter
Volume 49, Number 1 (pages 1-28) 2023
Annual Summary of Communicable Diseases Reported to the
Minnesota Department of Health, 2021
Introduction
Assessment of the population’s health is a core public health function.
Surveillance for communicable diseases is one type of assessment.
Epidemiologic surveillance is the systematic collection, analysis, and
dissemination of health data for the planning, implementation, and evaluation
of health programs. The Minnesota Department of Health (MDH) collects
information on infectious diseases for the purposes of determining disease
impact, assessing trends in disease occurrence, characterizing affected
populations, prioritizing control efforts, and evaluating prevention strategies.
Prompt reporting allows outbreaks to be recognized in a timely fashion when
control measures are most likely to be effective in preventing additional cases.
In Minnesota, communicable disease reporting is centralized, whereby reporting
sources submit standardized reports to MDH. Cases of disease are reported
pursuant to Minnesota Rules Governing Communicable Diseases (Minnesota
Rules 4605.7000 -4605.7800). The diseases listed in Table 1 must be reported
to MDH. As stated in the rules, physicians, health care facilities, laboratories,
veterinarians, and others are required to report these diseases. Reporting
sources may designate an individual within an institution to perform routine
reporting duties (e.g., an infection preventionist for a hospital).
Since April 1995, MDH has participated as an Emerging Infections Program
(EIP) site funded by the U.S. Centers for Disease Control and Prevention (CDC)
and, through this program, has implemented active hospital- and laboratory-
based surveillance for several conditions, including selected bacterial diseases,
foodborne diseases, tickborne diseases, and hospitalized influenza cases.
Isolates of pathogens from certain diseases are required to be submitted to
MDH (Table 1: Minnesota Rules Governing Communicable Diseases (Minnesota
Rules 4605.7000-4605.7800). The MDH Public Health Laboratory (PHL)
performs microbiologic and molecular evaluation of isolates, such as pulsed-
field gel electrophoresis (PFGE) and whole genome sequencing (WGS), to
determine whether isolates (e.g., enteric pathogens such as Salmonella and
Escherichia coli O157:H7) are related and potentially associated with a common
source. Testing of submitted isolates also allows detection and monitoring of
antimicrobial resistance.
Table 2 summarizes cases of selected communicable diseases reported during
2021 by district of the patient’s residence. Pertinent observations for some
of these diseases are presented below. Incidence rates in this report were
calculated using disease-specific numerator data collected by MDH and a
standardized set of denominator data derived from U.S. Census data. Disease
incidence is categorized as occurring within the seven-county Twin Cities
metropolitan area (metropolitan area) or outside of it in Greater Minnesota
(unless otherwise indicated).
Due to the COVID-19 pandemic, data collection was eliminated or greatly
delayed for some diseases.
Anaplasmosis
Anaplasmosis is a rickettsial disease
caused by the bacteria Anaplasma
phagocytophilum, which is transmitted
by bites from Ixodes scapularis,
the blacklegged tick. Although the
organism that causes anaplasmosis
has been known by other names and
was once thought to be a part of the
genus Ehrlichia, anaplasmosis and
ehrlichiosis are distinct diseases caused
by different rickettsial species. The same
tick vector also transmits the etiologic
agents of Lyme disease, babesiosis,
ehrlichiosis (due to E. muris), and
Powassan virus. In rare circumstances, A.
phagocytophilum may be transmitted by
blood transfusion.
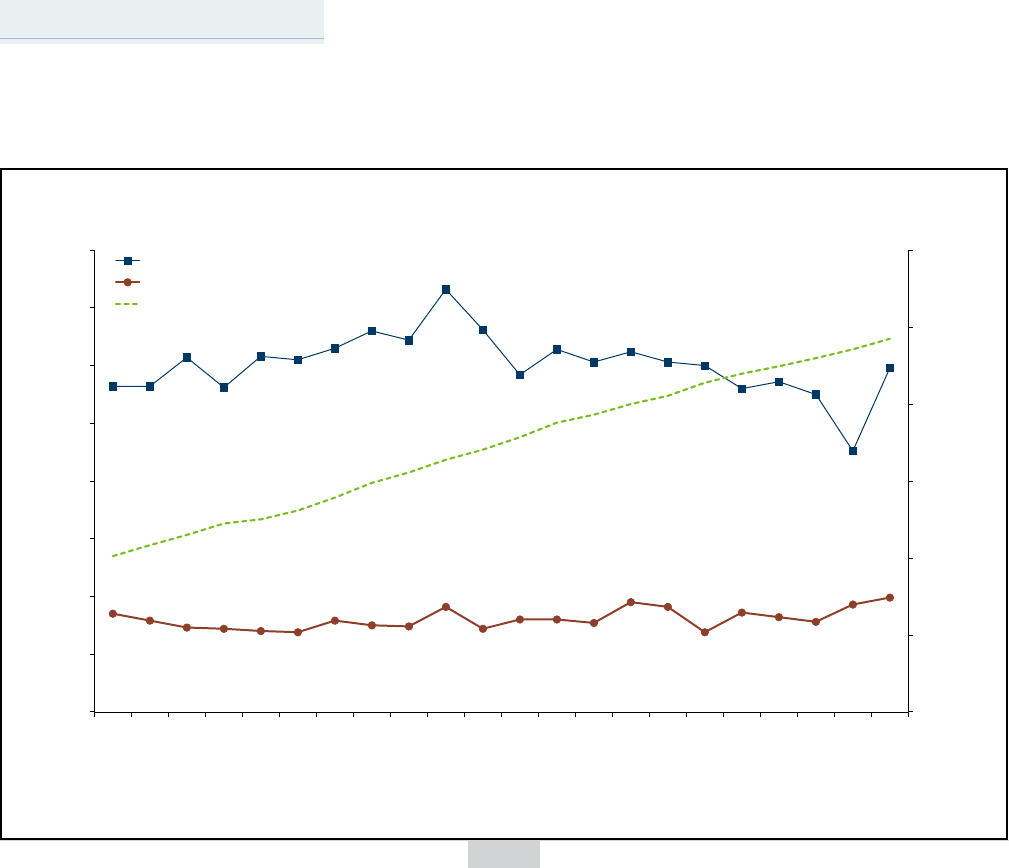
In 2021, 603 confirmed and probable
cases of anaplasmosis (10.5 cases per
100,000) were reported, up from the 407
cases reported in 2019. Although case
numbers were a bit lower the last few
years, the 2021 total is more in keeping
with the trend we saw through the mid-
2010s. A median of 613 cases per year
have reported since 2010 (Figure 1). In
2021, 382 (63%) confirmed and probable
cases reported were male. The median
age for cases was 64 years (range, 1 to
96), 19 years older than the median age
of confirmed Lyme disease cases, but
close to the median age of confirmed or
probable babesiosis cases (69 years). As
is typical, most cases had illness onsets
during the summer months, with 66%
of cases reporting illness onsets in May,
June, or July. This timing is consistent
with exposures occurring during the
typical peak season for blacklegged
tick activity in Minnesota. In 2021, 173
(29%) cases were hospitalized for their
anaplasmosis infection, with a median
duration of 4 days (range, 1 to 44
days). Forty-seven (8%) cases reported
complications (e.g., organ failure) due to
anaplasmosis infection.
continued on page 4

2
DCN 48;1 2022
Note: check website for updates
Table 1. Diseases Reportable to the Minnesota Department of Health

DCN 48;1 2022
3
Table 2. Cases of Selected Communicable Diseases Reported to the Minnesota
Department of Health by District of Residence, 2021
District
(population per U.S. Census 2020 estimates)
Disease
Total
Metropolitan
(3,130,769)
Central
(779.498)
Southwestern
(214,402)
South Central
(292,503)
Southeastern
(512,691)
West Central
(244,473)
Northwestern
(159,468)
Northeastern
(323,538)
Unknown
Residence
Anaplasmosis 603 144 140 1 9 52 45 97 115 0
Babesiosis 63 13 14 0 2 9 5 10 10 0
Blastomycosis 82 25 12 1 3 14 1 8 18 0
Botulism (Infant) 1 1 0 0 0 0 0 0 0 0
Brucellosis 19 18 0 0 0 0 1 0 0 0
Campylobacteriosis 1192 570 182 100 89 161 38 19 33 0
Cryptosporidiosis 373 86 53 33 51 88 40 7 15 0
Cyclosporiasis 66 21 3 15 4 11 4 0 8 0
Escherichia coli O157 infection 69 32 7 1 4 0 7 8 10 0
Hemolytic uremic syndrome 11 3 3 1 0 3 1 0 0 0
Giardiasis
388 184 36 28 28 27 21 9 55 0
Haemophilus influenzae disease 56 21 10 4 6 2 7 3 3 0
Histoplasmosis 190 84 21 14 23 19 21 3 5 0
HIV (non-AIDS) 245 184 25 7 3 10 8 2 6 0
AIDS (diagnosed in 2020) 81 64 6 2 0 7 0 0 2 0
Legionnaires’ disease 130 79 9 6 10 13 1 1 11 0
Listeriosis 12 9 1 0 0 0 1 0 1 0
Lyme disease 1033 458 232 9 14 113 33 44 130 0
Measles (rubeola) 0 0 0 0 0 0 0 0 0 0
Mumps 0 0 0 0 0 0 0 0 0 0
Pertussis 29 20 2 1 0 1 1 0 4 0
Q Fever (acute) 5 1 2 0 0 1 1 0 0 0
Q Fever (chronic)
1 0
0 0 1 0 0 0 0 0
Salmonellosis 853 448 118 63 54 64 41 25 39 1
Sexually transmitted diseases 33709 22910 3196 741 973 1994 1143 681 1579 465
Chlamydia trachomatis - genital infections 22578 14729 2329 585 758 1495 810 455 1075 315
Gonorrhea 9671 7141 749 143 176 453 291 143 425 150
Syphilis, total 1460 1040 118 13 39 46 42 83 79 0
Primary/Secondary 565 419 40 2 12 15 16 22 39 0
Early non-Primary non-Secondary* 415 303 30 1 7 13 10 33 18 0
Unknown Duration or Late** 466 309 48 10 20 18 15 24 22 0
Congenital 14 9 0 0 0 0 1 4 0 0
Other*** n/a n/a n/a n/a n/a n/a n/a n/a n/a n/a
Shigellosis n/a n/a n/a n/a n/a n/a n/a n/a n/a n/a
Streptococcal invasive disease - Group A
214 118 24 2
1 16 15 16 22 0
Streptococcal invasive disease - Group B 584 293 97 16 36 54 29 16 43 0
Streptococcus pneumoniae disease 309 138 58 15 21 22 16 10 29 0
Toxoplasmosis 7 5 0 0 0 2 0 0 0 0
Tuberculosis 134 102 8 9 4 6 2 2 1 0
Tularemia 1 0 0 0 0 0 0 1 0 0
Varicella 169 97 22 5 11 9 14 1 10 0
Viral hepatitis A 12 10 1 1 0 0 0 0 0 0
Viral hepatitis B (acute infections only) 10 6 0 0 1 2 1 0 0 0
Viral hepatitis C (acute infections only) 66 50 3 1 0 1 5 3 3 0
West Nile virus disease 36 28 1 1 2 0 2 2 0 0
* Duration ≤1 year
** Duration >1 year
*** Includes unstaged neurosyphilis, latent syphilis of unknown duration, and latent syphilis with clinical manifestations
County Distribution within Districts
Metropolitan - Anoka, Carver, Dakota, Hennepin, Ramsey, Scott, Washington
Central - Benton, Cass, Chisago, Crow Wing, Isanti, Kanabec, Mille Lacs, Morrison, Pine, Sherburne, Stearns, Todd, Wadena, Wright
Southwestern - Big Stone, Chippewa, Cottonwood, Jackson, Kandiyohi, Lac Qui Parle, Lincoln, Lyon, Murray, Nobles, Pipestone, Redwood, Renville, Rock, Swift, Yellow
Medicine
South Central - Blue Earth, Brown, Faribault, Le Sueur, McLeod, Martin, Meeker, Nicollet, Sibley, Waseca, Watonwan
Southeastern - Dodge, Fillmore, Freeborn, Goodhue, Houston, Mower, Olmsted, Rice, Steele, Wabasha, Winona
West Central - Becker, Clay, Douglas, Grant, Mahnomen, Norman, Otter Tail, Pope, Stevens, Traverse, Wilkin
Northwestern - Beltrami, Clearwater, Hubbard, Kittson, Lake of the Woods, Marshall, Pennington, Polk, Red Lake, Roseau
Northeastern - Aitkin, Carlton, Cook, Itasca, Koochiching, Lake, St. Louis

4
DCN 48;1 2022
0
200
400
600
800
1000
1200
1400
1600
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
Number of Cases
Year of Report
Lyme disease
Anaplasmosis
Babesiosis
Figure 1. Reported I. scapularis-borne Disease Cases in Minnesota by Year of Report
Arboviral Diseases
Endemic Mosquitoborne
Arboviral Diseases
Historically, the primary arboviral
encephalitides found in Minnesota
have been La Crosse encephalitis,
Western equine encephalitis (WEE),
and West Nile virus (WNV) encephalitis,
but in recent years other viruses like
Jamestown Canyon have emerged as
significant causes of disease. While
WNV and WEE are maintained in
mosquito-to-bird transmission cycles
involving several different species of
each, La Crosse and Jamestown Canyon
viruses use mammals instead of birds as
part of their transmission cycles. WNV
is established throughout Minnesota,
and will probably be present in the state
to some extent every year, whereas
human cases of other diseases may
occur more sporadically. Interpreting
the effect of weather on arboviral
transmission is complex, making it
difficult to predict the number of
people who will become infected in any
given year.
In 2021, Minnesota reported 36 WNV
disease cases and 19 asymptomatic
blood donors. Of the reported cases, 27
(75%) had neuroinvasive presentations
including encephalitis or meningitis,
while the remaining nine had West
Nile fever. None of the cases died. Fifty
percent (18) of the cases were male,
and the median age of all cases was
62 years old (range, 10 to 82). Thirty
(83%) cases were hospitalized, with a
median stay of 9 days (range, 2 to 40).
The majority of cases, 92%, reported
symptom onset in August or September.
Although cases are reported from
across Minnesota, risks for human
WNV infection continue to be higher in
central and western Minnesota where
the primary mosquito vector, Culex
tarsalis, is most abundant.
In 2021, there were no reported cases
of La Crosse encephalitis in Minnesota,
which is consistent with the trend
of fewer cases in the last few years.
The disease, which primarily affects
children, is transmitted through the bite
of infected Aedes triseriatus (Eastern
Tree Hole) mosquitoes and is
maintained in a cycle that includes
mosquitoes and small mammals.
Exposure to infected mosquitoes
typically occurs in wooded or shaded
areas inhabited by this species,
especially in areas where water-holding
containers (e.g., waste tires, buckets,
or cans) that provide breeding habitats
are abundant. Since 1985, 145 cases
have been reported from 22 Minnesota
counties, primarily in the southeastern
part of the state. Many people who are
infected have no apparent symptoms,
but severe disease is more common
in children. Most people report an
illness onset during the typical arboviral
season from mid-July through mid-
September.
In 2021, six cases of Jamestown Canyon
virus disease, a California group virus
related to La Crosse, were reported.
The virus is transmitted by Aedes
mosquitoes, and the maintenance cycle
in nature is thought to include deer and
other large mammals. Much remains
unknown about the clinical spectrum
of Jamestown Canyon virus, but the
typical presentation includes fever,
and in more severe cases, meningitis
or encephalitis. The virus is likely
widespread in Minnesota. Cases were
aged 34 to 74 years, with a median of
42 years, and all but one of the cases
were male. Four cases (67%) presented
with neuroinvasive disease, including
meningitis and encephalitis, and three
of the cases were residents of counties
in northeastern Minnesota. Due to
the mosquito vectors involved in the
transmission cycle for this virus, disease
onsets can occur from late spring
through the early part of the fall.
Endemic Tickborne
Arboviral Disease
Powassan virus (POW) is a tickborne
flavivirus that includes a strain (lineage
II or “deer tick virus”) that is transmitted
by Ixodes scapularis. Based on
findings from routine tick surveillance
activities, the virus appears to be
widely distributed in the same wooded
parts of the state that are endemic to
other pathogens transmitted by the
blacklegged tick. The virus can cause
encephalitis or meningitis, and long-
term sequelae occur in approximately
half of those patients. Approximately
10-15% of cases are fatal. Since the first
case in 2008, there have been cases
every year except for 2014 and 2015,
with a peak of 11 cases in 2011 (range, 1
to 11). Five cases of POW were reported
in 2021. All five cases were male in
2021, and ages ranged from 44 to 75
years. All the cases in 2021 had disease
that progressed to severe illness with
meningitis or encephalitis, and two
cases died. Similar to other tickborne
diseases, the majority of patients
report being exposed to ticks in north
central Minnesota. Interestingly, four
of the cases experienced illness onset
in October, with the other patient first
experiencing symptoms in June.

DCN 48;1 2022
5
continued...
Average Annual Incidence of
Histoplasmosis, Minnesota, 2017-2021,
(n=872)
Average Annual Incidence of
Blastomycosis, Minnesota, 1999-2021,
(n=915)
Note the difference in geographical distribution of Minnesota’s endemic fungal diseases, blastomycosis and histoplasmosis.
Blastomycosis occurs more frequently in northern and northeastern counties, and histoplasmosis occurs more often in western and
southern counties. While clinicians should test for both diseases when clinical illness is consistent with a fungal infection, these maps
may trigger questions about travel or otherwise help assess risk.
Babesiosis
Babesiosis is a malaria-like illness
caused by a protozoan parasite,
typically Babesia microti, which
infects red blood cells. B. microti is
transmitted to humans by bites
from Ixodes scapularis (the
blacklegged tick), the same vector
that transmits the agents of Lyme
disease, anaplasmosis, one form of
ehrlichiosis, and a strain of Powassan
virus. Babesia parasites can also be
transmitted by blood transfusion.
Although most people infected
with Babesia have asymptomatic
infections, people with weak immune
systems, other co-morbidities, and
the elderly can become seriously ill.
In 2021, there were 63 confirmed and
probable cases reported (1.1 cases
per 100,000), a slight increase from
the 55 cases in 2019. Over the past
decade, slight annual fluctuations in
reported cases have been observed,
however, reported case numbers
continue to trend upward (range, 41
to 72) and are consistently higher
than annual cases reported in the
previous decade, 2000-2010 (range,
1 to 56) (Figure 1). In recent years,
case demographics were similar. In
2021, 37 (59%) of the cases occurred
in males. The median case age was
69 years (range, 2 to 92), up slightly
from 67 in 2019, and older than the
median ages for both anaplasmosis
(64 years) and Lyme disease (45
years). Illness onset dates peaked
in the summer months: 44 (80%)
of the 55 cases with known onset
date reported first experiencing
symptoms in June, July, or August.
Twenty (32%) cases were hospitalized
due to their infection in 2021 with
a median admission duration of 6
days (range, 2 to 18). Seven patients
reported severe complications (e.g.,
organ failure), and one patient with
complications died as a result of their
babesiosis infection.
Blastomycosis
Blastomycosis is an infection caused
by a fungus called Blastomyces. In
2021, 82 blastomycosis cases were
reported. This continues an increase
in cases reported in the past 5 years,
with a median of 79 cases/year from
2017 to 2021 compared to a median
of 33 cases/year for the prior 18
years.
The median age of blastomycosis
cases in 2021 was 56.5 years (range,
8 to 89 years), and 51 (62%) were
male. In 2021, cases were more
likely to be older and female than
in previous years. Of the 77 cases
for whom race and ethnicity was
reported, 63 (82%) cases were white,
6 (8%) were American Indian/Alaska
Native, 5 (7%) were Asian, 1 (1%) was
Black/African American, and 2 were
of another race. One case (1%) was
Hispanic.
Figure 2. Comparison of Average Annual Incidence
of Endemic Fungal Diseases in Minnesota

6
DCN 48;1 2022
When hospitalization status was
known, 54 of 80 (68%) cases
were hospitalized, for a median
of 8 days (range, 1 to 54 days).
Nineteen (23%) cases died, which
is a significantly higher case fatality
rate (CFR) than the 10% mean CFR
during 1999-2020. Blastomycosis
was the listed cause of death for
12 cases, 3 cases had other causes
of death listed, and the cause of
death was unknown for 4 cases.
When it was possible to identify
the body system infected by
Blastomyces, 51 (64%) cases had a
pulmonary-only infection, 22 (27%)
had a disseminated infection, and
7 (9%) had an extra-pulmonary
infection.
There were two blastomycosis
outbreaks identified in 2021.
One case was part of an ongoing
outbreak associated with a family
cabin property in Pine County.
This outbreak began in 2019 and
resulted in 4 cases through 2021.
A second outbreak-related case
was exposed at a dam worksite in
Wisconsin; the other case in that
outbreak was a Wisconsin resident.
From 1999 to 2021, 916 cases
of blastomycosis in Minnesota
residents were reported. Exposure
information is available for 662
cases. The largest number, 138
(21%), were likely exposed in St.
Louis County. Eighty (12%) cases
were likely exposed in Itasca
County, 61 (9%) in Cass County, 24
(4%) in Hennepin County, and 20
(3%) in Beltrami County. Seventy-
six cases (11%) were exposed in
Wisconsin.
In 2021, the statewide incidence
was 1.4 cases/100,000 population,
compared to a 1999-2020
median annual incidence of 0.63
cases/100,000. A map of average
annual incidence of blastomycosis
from 1999 to 2021 clearly shows
the highly endemic regions,
which include the northern
and northeastern counties of
Minnesota (Figure 2). This is in
contrast to the other endemic
fungal disease found in Minnesota,
histoplasmosis, which has higher
incidence levels in southern and
western counties. While clinicians
should test for both diseases when
clinical illness is consistent with
a fungal infection, these maps
may help assess differential risk in
various regions of the state.
Botulism
Botulinum toxin, a neurotoxin, is
produced by the spore-forming
bacteria Clostridium botulinum and
other related Clostridium species.
There are 8 distinct toxin types:
A, B, C, D, E, F, G, and H. Toxin
types A, B, E, F, and H can cause
human intoxication. Botulism is
characterized by a descending,
bilateral paralysis that can be fatal
without treatment. Botulism spores
are ubiquitous in the environment
and cause three main forms of
intoxication: foodborne, wound, and
intestinal toxemia, which includes
infant botulism and intestinal
toxemia. Infant botulism, which is
the most common form in the United
States, results from the ingestion of
C. botulinum spores that germinate
into vegetative bacteria that colonize
the intestinal tract, producing toxin
that is absorbed into the circulation.
In 2021, one infant botulism and
one intestinal toxemia botulism case
were reported. The infant botulism
case occurred in a 21-week-old
male. He received botulism immune
globulin (BabyBIG) and recovered.
The disease was caused by toxin type
B. The intestinal colonization case
occurred in a 10-year-old female
with a medical history including
short bowel syndrome, G-tube
dependence, and D-lactic acidosis.
Despite receiving heptavalent
botulism antitoxin, she succumbed
to the disease. Her illness was
caused by toxin type A.
From 2001 to2021, 16 cases
of infant botulism, 2 cases of
foodborne botulism, 2 cases of
intestinal toxemia botulism, and
1 case of possible iatrogenic
botulism were identified among
Minnesota residents. The median
age of affected infants was 21 weeks
(range, 5 to 41 weeks). Twelve (75%)
infant botulism cases were caused by
botulinum toxin type B and 4 (25%)
by toxin type A. Thirteen infants
were known to be hospitalized, for
a median of 15 days (range, 8 to 30
days); one infant did not require
hospitalization. The 2 foodborne
cases, caused by toxin type A
occurred in 2009 in two men who
consumed home-canned asparagus.
Both cases were hospitalized, for
6 and 16 days. No deaths occurred
among the infant or foodborne
botulism cases.
Brucellosis
Brucellosis is an acute or chronic
illness caused by bacteria of
the Brucella genus. There are 5
important species of Brucella: B.
abortus, B. melitensis, B. suis, B.
canis, and B. ovis, of which cattle,
goats, pigs, dogs, and sheep are
the respective reservoir animals.
Transmission can occur through
ingestion of unpasteurized dairy
products, contact with infected
animal tissue, or inhalation of
aerosolized bacteria in a laboratory
setting. Minnesota’s livestock have
been brucellosis free since 1985.
Most infections are acquired in
Brucella-endemic countries.
In 2021, 19 confirmed cases were
reported. Eleven of these cases were
part of an outbreak of brucellosis
linked to unpasteurized queso
fresco, a homemade soft cheese,
likely made with goat milk, imported
from Mexico by a private seller and
distributed in the Twin Cities. The
eleven cases tested positive for
Brucella melitensis and B. melitensis
was isolated from a sample of the
cheese. The median age of outbreak
cases was 44 years (range, 16-52
years), 7 (64%) were male, and all
were Hispanic. Ten (91%) cases
were hospitalized for a median of 7
days (range, 1-13 days). Some cases
experienced severe complications,
including endocarditis (n=3), sepsis
(n=2), splenomegaly (n=1), and
hepatitis (n=1).
Of the eight sporadic cases, four
were exposed in Somalia, one in
Ethiopia, one in Russia, and one
who ate boar meat from Oklahoma.
One case had an unknown exposure
location. The median age of sporadic
cases was 44 (range, 14-76); 5(63%)
were female. Complications of
brucellosis among sporadic cases
included three (38%) cases who
experienced osteomyelitis and
three (38%) with sepsis. All 2021
brucellosis cases survived their
infection.
From 2007 to 2021, 46 confirmed
cases were reported. Thirty likely
acquired their infection outside
the United States, and 16 were
domestically acquired. The median
number of cases reported annually
was 2 (range, 0 to 19). Thirty-six
were infected with B. melitensis,
seven with B. suis, two with B.

DCN 48;1 2022
7
continued...
0
200
400
600
800
1000
1200
1400
2013 2014 2015 2016 2017 2018 2019 2020 2021
Number of Cases
Year of Report
Campylobacter
Salmonella
Cyclospora
STEC
Shigella
Campylobacter, 1041
Salmonella, 853
STEC, 317
Shigella, 133
Cyclospora, 24
Median
abortus, and one with an unidentified
Brucella species diagnosed by
serology only. The median age of
cases was 47 years (range, 3 to 86).
Twenty of the 42 cases for which race
was known were black, 18 were white
(of which 11 identified as Hispanic),
and four were Asian/Pacific Islander.
Campylobacteriosis
During 2021, 1,562 Campylobacter
cases were reported. Of those,
1,192 were culture-confirmed, and
370 were only tested by a culture-
independent diagnostic test (CIDT)
and not subsequently culture-
confirmed. The rate of culture-
confirmed Campylobacter cases
reported in 2021 was 20.9 per
100,000 population. The 1,192
culture-confirmed Campylobacter
cases represent a 50% increase from
the 793 cases reported in 2020, and a
22% increase from the annual median
of 975 cases reported from 2011 to
2020 (range, 793 to 1,238). In 2021,
48% of cases occurred in people who
resided in the metropolitan area. Of
the 1,104 Campylobacter isolates
confirmed and identified to species
by MDH, 85% were C. jejuni and 9%
were C. coli.
The median age of culture-confirmed
cases was 41 years (range, 2 months
to 99 years). Thirty-eight percent
were between 20 and 49 years of age,
and 11% were ≤5 years of age. Fifty-
four percent were male. Seventeen
percent were hospitalized; the median
length of hospitalization was 3 days.
Two (0.2%) cases died. Forty-nine
percent of infections occurred during
June through September. Of the 982
cases for whom data were available,
62 (6%) reported travel outside the
United States during the week prior to
illness onset. The most common travel
destination was Mexico (n=21).
In 2009, a CIDT became commercially
available for the qualitative detection
of Campylobacter antigens in stool.
In 2021, 40 patients were positive
for Campylobacter by an antigen
detection CIDT conducted in a
clinical laboratory. However, only
19 (48%) of the specimens were
subsequently culture-confirmed.
Beginning In 2015, some clinical
laboratories in Minnesota began
testing stool specimens with PCR-
based gastrointestinal pathogen
panels, another type of CIDT. In
2021, 1,353 patients were positive
for Campylobacter by a PCR
gastrointestinal panel; 1,005 (74%)
of these specimens were culture-
confirmed. The median age of the
CIDT-positive only cases was 49 years
(range, 1 month to 93 years). Sixty-
eight (18%) cases were hospitalized;
the median hospital stay was 3 days
(range, 1 to 123 days). No CIDT-only
cases died.
Four outbreaks of Campylobacter
infections were identified in 2021.
Nineteen cases were associated with
poultry contact at a farm and garden
center, 13 cases were associated
with person-to-person transmission
among men who have sex with men
(MSM) contact, two cases were
associated with chicken liver yakitori
at a restaurant, and two cases were
associated with multiple food items
at a restaurant.
A primary feature of
public health importance
among Campylobacter cases
was the continued presence
of Campylobacter isolates resistant
to fluoroquinolone antibiotics (e.g.,
ciprofloxacin), which are commonly
used to treat campylobacteriosis.
In 2021, the overall proportion
of ciprofloxacin resistance
among Campylobacter isolates tested
was 26%. However, historically, 80-
90% of Campylobacter isolates from
patients with a history of foreign
travel during the week prior to illness
onset, regardless of destination,
were resistant to fluoroquinolones
as compared to approximately 20%
of Campylobacter isolates from
patients who acquired their infection
domestically.
Figure 3. Number of Selected Enteric Pathogen Cases by Year of Report, 2013-2021

8
DCN 48;1 2022
Candidemia
In 2017, surveillance began for
candidemia among residents of the
metropolitan area. Candidemia is a
bloodstream infection caused by the
Candida fungal species and is one of
the most common types of healthcare-
associated bloodstream infections
in the United States. Risk factors
include prolonged hospitalization in
an intensive care unit, having a central
venous catheter, a weakened immune
system, recent surgery (especially
abdominal surgery), recently receipt of
antibiotics, total parenteral nutrition,
kidney failure, hemodialysis, and
diabetes.
In 2021, 160 cases were reported
among residents of the metropolitan
area. The overall incidence rate was 5.2
per 100,000, and the highest county-
level incidence was in Ramsey County
(7.0 per 100,000). The median age
was 59 years (range, newborn to 97
years). Seventy-seven cases (48%) were
male; 108 (69%) were white, 27 (17%)
were black, 11 (7%) were Asian/Pacific
Islander, and race was unknown for 8
cases.
Of the 160 cases, 99% were
hospitalized at time of diagnosis, and
45 (29%) died while hospitalized.
Underlying conditions included
malignancy (29%), chronic lung
condition (28%), diabetes (39%), renal
disease (28%), neurologic condition
(36%), skin condition (16%), and
chronic liver disease (11%). Healthcare
risk factors included receiving systemic
antibiotics in the 14 days prior to
diagnosis (83%); presence of a central
venous catheter in the 2 days prior
to diagnosis (67%); being admitted to
the ICU within 14 days prior to or 14
days after diagnosis (50%); and having
surgery in the 90 days before diagnosis
(23%).
More than 17 different Candida
species are known to be agents of
human infection; however, the two
most common species comprised over
50% of candidemia infections. Of the
160 cases, 38% were C. albicans, 37%
C. glabrata, 10% C. parapsilosis, 3%
C. tropicalis, 3% C. dubliniensis, 1%
C. kefyr, 1% C. krusei, and 3% with
other species including C. nivariensis,
C. guilliermondii, and C. lusitaniae.
Six cases (4%) were co-infected with
multiple species of Candida at the time
of incident specimen collection.
As primarily a healthcare-associated
infection, injection drug use (IDU) has
not been considered a common risk
factor for candidemia. However, with
the increasing opioid epidemic, IDU
has been reported as an increasingly
common condition associated with
candidemia. In 2017, only 2/143 (1.4%)
cases had IDU documented in their
medical chart. However, in 2018, 15
(11%) cases, in 2019, 16 (10%) cases,
in 2020, 13 (7%) cases, and in 2021,
14 (9%) cases had IDU documented
in their medical chart. MDH began
collecting additional information
regarding IDU in 2019 to monitor the
changing trends in IDU and candidemia
epidemiology.
Carbapenem-resistant
Enterobacteriaceae(CRE),
Acinetobacter baumannii
(CRA), and Pseudomonas
aeruginosa(CRPA)
Carbapenem-
resistant Enterobacterales (CRE),
Acinetobacter baumannii (CRAB),
and Pseudomonas aeruginosa
(CRPA) are gram-negative bacilli
that most commonly occur among
patients with significant healthcare
exposures, co-morbid conditions,
invasive devices, and those who
have received extended courses of
antibiotics. Invasive infections caused
by CRE, such as carbapenem-resistant
Klebsiella pneumoniae, are associated
with higher morbidity and mortality
than those caused by carbapenem-
susceptible Enterobacterales. CRAB
is increasingly recognized as one of
the leading causes of healthcare-
associated infections worldwide and
is associated with high mortality rates
and unfavorable clinical outcomes.
Invasive infections caused by CRPA
are associated with higher morbidity
and mortality than those caused
by carbapenem-susceptible P.
aeruginosa.
Carbapenem resistance can
be acquired through a variety
of mechanisms including
transmissible genetic elements.
Some CRE, CRAB, and CRPA carry
resistance genes that produce
enzymes called carbapenemases.
Certain carbapenemases (e.g., K.
pneumoniae carbapenemase
[KPC]) can easily spread between
bacteria of similar species
.
KPC is
the predominant carbapenemase
in the United States while other
carbapenemases (e.g., New Delhi
metallo-β-lactamase [NDM], Verona
integron-encoded metallo-β-
lactamase [VIM], and oxacillinase-48
[OXA-48]) are more frequently
identified in other countries.
Resistance can also be acquired
through the production of a
β-lactamase effective against third
generation cephalosporins (e.g., AmpC
β-lactamases or extended-spectrum
β-lactamases [ESBLs]) when combined
with porin mutations that prevent
carbapenem antibiotics from entering
the cell.
MDH first identified a KPC-
producing CRE in February 2009,
and began voluntary reporting,
including isolate submission,
for all Enterobacterales and A.
baumannii resistant to imipenem,
meropenem, doripenem, or
ertapenem using current Clinical and
Laboratory Standards Institute (CLSI)
breakpoints (ertapenem excluded
for A. baumannii isolates). In 2012,
MDH used standardized CRE and
CRAB definitions developed by the
Emerging Infections Program (EIP)
Multi-site Gram-negative Surveillance
Initiative (MuGSI) and initiated active
laboratory- and population-based
surveillance in Hennepin and Ramsey
Counties. As a subset of statewide
reporting, MuGSI surveillance includes
all isolates from normally sterile
sites or urine of the three most
common types of CRE (Escherichia
coli, Enterobacter spp.,
or Klebsiella spp
.
) and A. baumannii.
A MuGSI incident case is defined as
the first eligible isolate of each species
collected from a Hennepin or Ramsey
County resident in 30 days.
In 2016, MDH initiated statewide CRE
surveillance for E. coli, Enterobacter
spp., Klebsiella spp
.
, and Citrobacter
spp.; MDH also tracks other
Enterobacterales including, but not
limited to, Morganella spp., Proteus
spp., and Providencia spp. The MDH
Public Health Laboratory (PHL) tests
all CRE isolates for carbapenemase
production using a phenotypic assay
(modified carbapenem inactivation
method [mCIM] or CarbaNP) and
conducts PCR on isolates with a
positive phenotypic test for KPC,
NDM, OXA-48-like, VIM, and IMP
genes. All CRAB isolates are tested by
PCR for KPC, NDM, OXA-48, VIM, and
IMP genes, along with Acinetobacter-
specific OXA genes (OXA-23, OXA-24,
and OXA-58).

DCN 48;1 2022
9
continued...
In 2017, the Centers for Disease
Control and Prevention (CDC) released
Interim Guidance for a Public Health
Response to Contain Novel or Targeted
Multidrug-resistant Organisms
(MDROs) for state and local public
health departments responding to
cases of novel or targeted MDROs,
including carbapenemase-producing
organisms (CPO). Novel or targeted
MDROs are epidemiologically
important because these organisms
cause severe, difficult-to-treat
infections and have the potential to
spread within healthcare settings.
MDH utilizes the Containment Strategy
in response to all single cases of
carbapenemase-producing CRE, CRAB,
and CRPA in Minnesota. This rapid
and comprehensive action includes
prompt identification of the organism,
notification and investigation with
healthcare facilities, and response or
“containing the spread” to slow the
spread of novel or targeted MDROs in
Minnesota.
In 2021, 479 CRE incident cases
representing 439 patients were
identified from clinical cultures among
Minnesota residents; median age
was 73 years (range, <1 to 99) and
265 (60%) identified as female. The
most common organism for incident
cases was Enterobacter spp. (183)
followed by Klebsiella spp. (98) and
E. coli (94). Other CRE organisms
included Serratia spp. (30), Proteus
spp. (26), Citrobacter spp. (24),
Providencia spp. (16), Morganella
spp. (2), and other Enterobacterales
(6). Among 479 incident cases, there
were 127 CRE MuGSI incident cases
(representing 112 patients) reported
among residents of Hennepin and
Ramsey Counties. Fifty-eight (46%)
isolates were Enterobacter spp., 40
(31%) were E. coli, and 29 (23%)
were Klebsiella spp. with 12 isolates
demonstrating carbapenemase
production (five NDM, five OXA-48-
like, and two KPC). CRE MuGSI incident
cases were most frequently isolated
from urine (117) followed by blood (7)
and other sterile sites (3).
Among 479 CRE incident cases, 43
(9%) were carbapenemase-producing
organisms. Twenty cases (from 18
patients) were KPC positive (E. cloacae
[7], K. pneumoniae [7], K. oxytoca [4],
C. freundii [1], and Hafnia alvei [1]),
nine cases (from 5 patients) were NDM
positive (E. coli [8] and P. mirabilis [1]),
nine cases (from 8 patients) were IMP
positive (P. rettgeri [6], P. mirabilis
[1], M. morganii [1], and E. cloacae
[1]), and five cases (from 4 patients)
were OXA-48 positive (K. pneumoniae
[4] and E. coli [1]). Urine (27) was the
most common isolate source followed
by blood (5), sputum (5), other non-
sterile sites (2), wound (2), bone (1),
and peritoneal fluid (1). We identified
seven additional CRE surveillance cases
(from 7 patients) through colonization
screening harboring NDM (3), KPC (2),
OXA-48 (1), and NDM & OXA-48 dual
mechanism (1). Among surveillance
cases with known organism, there
was one isolate each of E. coli, K.
pneumoniae, and E. cloacae. Among
35 Minnesota residents infected with
carbapenemase-producing CRE, the
median age was 68 years (range, 32 to
89) and 18 (51%) identified as female.
There were cases in 18 counties; 13
(37%) were residents of Hennepin
or Ramsey Counties, six (17%) were
residents of other counties within
the Twin Cities metro area, and the
remaining 16 (46%) were residents
of 12 different counties in greater
Minnesota.
In 2021, 18 CRAB incident cases
representing 14 patients were
identified from clinical cultures among
Minnesota residents. Among these 14
patients, the median age was 53 years
(range, 1 to 85) and 8 (62%) identified
as male. Wound (8) was the most
common isolate source followed by
urine (6), sputum (3), and tissue (1).
Of 18 CRAB incident cases, eight cases
were reported for MuGSI isolated from
wound (4), urine (3), and sputum (1).
Three CRAB incident isolates (from
two patients) possessed genes for
carbapenemase production both of
which were OXA-23.
Active laboratory- and population-
based surveillance for CRPA was
initiated on August 1, 2016 in
Hennepin and Ramsey Counties as
part of MuGSI and ended on July
31, 2018. This surveillance included
all CRPA isolates collected from
normally sterile sites, wounds, urine,
sputum, throat cultures from cystic
fibrosis (CF) patients, or other lower
respiratory sites that are resistant to
imipenem, meropenem, or doripenem
using current CLSI breakpoints. An
incident case was defined as the
first report of CRPA, or a subsequent
report of CRPA ≥ 30 days after the last
incident report. Despite surveillance
discontinuation in 2018, PHL continues
to test any submitted CRPA isolates
for carbapenemase production. In
2021, five CRPA isolates demonstrated
carbapenemase production (4 KPC
and 1 NDM). The CRPA isolates
harboring KPC carbapenemase were
part of an outbreak associated with a
contaminated endoscope.
Clostridioides difficile
Clostridioides difficile is an anaerobic,
spore-forming, Gram-positive bacillus
that produces two pathogenic toxins:
A and B. C. difficile infections (CDI)
range in severity from mild diarrhea
to fulminant colitis and death.
Transmission of C. difficile occurs
primarily in healthcare facilities,
where environmental contamination
by C. difficile spores and exposure to
antimicrobial drugs are common. The
primary risk factor for development
of CDI in healthcare settings is recent
use of antimicrobials, particularly
clindamycin, cephalosporins, and
fluoroquinolones. Other risk factors
for CDI acquisition in these settings
are age >65 years, severe underlying
illness, intensive care unit admission,
nasogastric intubation, and longer
duration of hospital stay.
In the early 2000s, a marked increase
in the number of CDI cases and
mortality due to CDI was noted
across the United States, Canada, and
England. Most notable was a series of
large-scale outbreaks in Quebec first
reported in March 2003. During this
period, Quebec hospitals reported a
5-fold increase in healthcare-acquired
CDI. These and other healthcare
facility (e.g., long-term care facilities)
outbreaks have been associated with
the emergence of a more virulent
strain of C. difficile, designated
North American PFGE type 1 (NAP1),
toxinotype III.
In 2009, in an effort to better
understand the burden of CDI in
Minnesota, the MDH Emerging
Infection Program (EIP) initiated
population-based, sentinel surveillance
for CDI at clinical laboratories serving
Stearns, Benton, Morrison, and Todd
Counties; in 2012 Olmsted County
was added. CDIs that occur outside
the traditional healthcare settings
(i.e., community-associated) have also
been receiving increased attention.
Community-associated (CA) CDI data
from 2009-2011 across 10 EIP sites
showed that 64% of CA CDI patients
received prior antibiotics, and 82% had
some outpatient healthcare exposure.
A CDI case is defined as a positive C.
difficile toxin assay on an incident stool
specimen from a resident (≥ 1 year of
age) of one of the five counties. A CDI

10
DCN 48;1 2022
case is classified as healthcare facility-
onset (HCFO) if the initial specimen
was collected >3 days after admission
to a healthcare facility. Community-
onset (CO) cases who had an overnight
stay at a healthcare facility in the 12
weeks prior to the initial specimen
are classified as CO-HCFA, whereas CO
cases without documented overnight
stay in a healthcare facility in the 12
weeks prior to the initial specimen
result are classified as CA. A more
detailed set of case definitions is
available upon request.
In 2021, 808 incident cases of CDI
were reported in the five sentinel
counties (192 per 100,000 population),
an increase from 180 per 100,000
population in 2020. Sixty-one percent
of these cases were classified as CA,
22% as CO-HCFA, and 16% as HCFO.
The median ages for CA, CO-HCFA, and
HCFO cases were 58 years, 64 years,
and 70 years, respectively. Forty-nine
percent of CA cases were prescribed
antibiotics in the 12 weeks prior to
stool specimen collection compared
to 86% of HCFO cases and 88% of
CO-HCFA cases. Due to the COVID-19
pandemic, interviews were only
conducted on putative CA cases after
July 1, 2021. 227 putative CA cases
prior to that date were not contacted
for interview. Of the remaining 268
putative CA cases eligible for interview,
155 were interviewed and confirmed
as CA cases. Forty-seven percent of CA
cases reported antibiotic use in the 12
weeks prior to illness onset date. Most
common uses of antibiotics included
treatment of ear, sinus, or upper
respiratory infections (28%); urinary
tract infections (24%); and dental
procedures (22%).
Cryptosporidiosis
During 2021, 429 cases of
cryptosporidiosis were reported. Of
those, 56 were positive only on a
rapid antigen screening test and were
considered probable cases.
The 373 confirmed cases of
cryptosporidiosis (6.6 per 100,000
population) in 2021 is similar to the
median number of confirmed cases
reported annually from 2013 to 2020
(median, 353 cases; range, 224 to
439). The median age of confirmed
cases in 2021 was 26 years (range,
9 months to 85 years). Children 10
years of age or younger accounted for
25% of cases. Sixty-one percent were
female. Of the 353 cases for which
race was reported, 305 (86%) were
white, 28 (8%) were Black, 6 (2%) were
Asian American, 1 (<1%) was American
Indian, and 13 (4%) reported being
other or multiple races. Fourteen (4%)
were Hispanic. Sixty percent of cases
occurred from July through October.
The incidence of cryptosporidiosis in
the South Central, Southeastern, West
Central, and Southwestern districts
(17.5, 17.4, 16.5, and 15.2 cases per
100,000, respectively) was significantly
higher than the statewide incidence.
Only 86 (23%) cases occurred among
residents of the metropolitan area (2.7
per 100,000). Fifty-four (15%) cases
required hospitalization, for a median
of 2 days. Two deaths were reported.
Three confirmed outbreaks of
cryptosporidiosis were identified in
Minnesota in 2021, accounting for
17 cases (5 laboratory-confirmed).
All were due to person-to-person
transmission in childcare settings.
Two of these outbreaks occurred in
Hennepin County and one in Dodge
County. In addition, 4 laboratory-
confirmed cases were part of an
outbreak that occurred at a hotel
waterpark in South Dakota.
Cyclosporiasis
There were 66 Cyclospora cases
reported in 2021 (1.17 per 100,000
population). This is markedly higher
than the median number of cases
reported from 2011 to 2020 (median,
4.5; range, 0 to 156 per year). In 2021,
32% of cases occurred in people who
resided in the metropolitan area.
The median age of cases was 52.5
years (range, 6 to 84 years). Fifty-
five percent were female. Of the 63
cases where race was reported, 56
(89%) were white, 2 (3%) were Black,
and 5 (8%) were Other race. Seven
(11%) were Hispanic. Six percent
were hospitalized; the median length
of hospitalization was 4 days (range,
2 to 7 days). Eighty-two percent of
infections occurred from May through
July. Of the 34 non-outbreak cases for
whom data were available, 7 (21%)
reported travel outside the United
States during the 2 weeks prior to
illness onset.
Two foodborne outbreaks of
cyclosporiasis were identified in
Minnesota in 2021. The first was
a multi-state outbreak associated
with pre-packaged romaine lettuce,
accounting for 22 laboratory-confirmed
Minnesota cases. The second was
a multi-state outbreak associated
with butter lettuce, accounting for 2
laboratory-confirmed Minnesota cases.
Escherichia coli O157 Infection,
Other Shiga Toxin-producing
E. coli, and Hemolytic Uremic
Syndrome (HUS)
During 2021, 584 Shiga toxin-
producing Escherichia coli (STEC) cases
were reported. Of those, 69 were
culture-confirmed E. coli O157, 263
were culture-confirmed non-O157
STEC, and 252 were only positive by a
culture-independent test (CIDT) and
not subsequently culture-confirmed.
The 69 culture-confirmed cases
of E. coli O157 infection (1.22 per
100,000 population) reported in 2021
represents a 42% decrease from the
median number of culture-confirmed
cases reported annually from 2011 to
2020 (median, 119 cases; range, 65
to 146). During 2021, 32 (46%) cases
occurred in the metropolitan area.
Fifty-five (80%) cases occurred during
May through October. The median
age of the cases was 17 years (range,
11 months to 79 years). Twenty-nine
percent of the cases were 4 years of
age or younger. Twenty-four (35%)
cases were hospitalized; the median
hospital stay was 3 days (range, 1 to 31
days). No cases died.
The 263 culture-confirmed non-O157
cases (4.65 per 100,000 population)
reported in 2021 represents a 53%
increase from the median number
of culture-confirmed cases reported
annually from 2011 to 2020 (median,
172 cases; range, 105 to 322). E. coli
O103 was the serogroup for 42 (17%)
cases, E. coli O26 for 34 (17%), E. coli
O111 for 33 (13%), E. coli O145 for 19
(4%), E. coli O121 for 15 (5%), and E.
coli O45 for 6 (2%). The median age
of the non-O157 STEC cases was 31
years (range, 4 months to 96 years).
Fifty (19%) cases were hospitalized;
the median hospital stay was 3 days
(range, 1 to 32 days). No cases died.
During 2021, 252 cases were reported
with specimens that were positive by a
CIDT conducted at a clinical laboratory,
but were not subsequently culture-
confirmed. CIDTs have become widely
adopted by clinical laboratories for the
detection of Shiga toxin or Shiga toxin
genes in stool. The median age of the
CIDT-positive only cases was 41 years

DCN 48;1 2022
11
continued...
(range, 4 months to 97 years). Seventy
(27%) cases were hospitalized; the
median hospital stay was 3 days
(range, 1 to 56 days). Two cases died.
Two E. coli O157 outbreaks were
identified during 2021. One outbreak
was due to animal contact, and
the other was due to foodborne
transmission. In August, an outbreak
of E. coli O157 infections was likely
associated with indirect contact
with a calf and sheep at a private
home; three cases, all laboratory-
confirmed, were identified. Two
cases developed hemolytic uremic
syndrome (HUS), but none of the
cases died. In November, a national
outbreak of E. coli O157 infections
was associated with spinach. Two
cases were identified in Minnesota,
both laboratory-confirmed. Neither
developed HUS nor died.
Four non-O157 STEC outbreaks
were identified during 2021. One
outbreak was due to person-to-
person transmission in a childcare
setting, one was due to foodborne
transmission, one was due to
animal contact, and one had an
unknown transmission route. In July,
an outbreak of E. coli O103:H11
infections associated with person-
to-person transmission occurred at
a childcare facility in Polk County.
Nineteen cases, one laboratory-
confirmed, were identified. No
cases developed HUS nor died.
In August, an outbreak of E. coli
O145:H28 infections with an unknown
transmission route was identified.
Three cases, all laboratory-confirmed,
were identified. No cases developed
HUS nor died.In October, an outbreak
of E. coli O111:H8 infections was
associated with contact with calves
at an apple orchard. Two cases, both
laboratory-confirmed, were identified.
Neither case developed HUS nor died.
In December, a national outbreak
of E. coli O121:H19 infections was
associated with romaine lettuce. Two
cases were identified in Minnesota.
Neither developed HUS nor died.
Hemolytic Uremic Syndrome
(HUS)
In 2021, 11 HUS cases were reported.
The number of reported cases is
the same as the median number of
cases reported annually from 2011
to 2020 (median, 11 cases; range, 3
to 17). In 2021, the median age of
HUS cases was 2 years (range, 1 to 11
years). All 11 cases were hospitalized,
with a median hospital stay of 13
days (range, 1 to 31 days). No cases
died. From 1997 through 2021, the
overall case fatality rate among HUS
cases was 5.1%. E. coli O157:H7 was
cultured from the stool of 7 (64%)
cases. E. coli O5:H9 was cultured
from the stool of one case and E.
coli O-genotype untypeable:H8 was
cultured from the stool of one case.
Two cases were Shiga toxin positive
by PCR but not culture-confirmed.
In 2021, there were two outbreak-
associated HUS cases.
Giardiasis
During 2021, 388 cases of Giardia
infection (6.9 per 100,000 population)
were reported. This represents a 38%
decrease from the median number
of cases reported annually from 2011
through 2020 (median, 629.5 cases;
range, 416 to 692). Recent immigrants
and refugees accounted for 6% of
cases. An additional 8% of cases
reported international travel in the 3
weeks prior to illness onset. Excluding
recent immigrants and refugees,
the median age of cases was 39
years (range, 5 months to 94 years).
Eighteen percent of cases were less
than 10 years of age, and 38% were
more than 50 years of age. Fifty-six
percent of non-immigrant and refugee
cases were male. Giardia infections
had a summer/fall seasonality; 47%
of non-immigrant and refugee cases
occurred during July through October.
Twenty-eight (7%) cases required
hospitalization, for a median of 4 days
(range, 2 to 17 days). No outbreaks of
giardiasis were identified.
Haemophilus influenzae
Fifty-six Haemophilus
influenzae disease cases (1.0 per
100,000 population) were reported
in 2021. Cases ranged in age from
newborn to 95 years (median 64
years). Allowing for more than one
syndrome per case, 26 (46%) cases
had pneumonia, 5 (9%) bacteremia,
8 (14%) septic shock, 13 (23%)
meningitis, 2 (4%) osteomyelitis, 3
(5%) empyema, and the following
each had 1 (2%): cellulitis, abscess,
septic arthritis, otitis media,
epiglottitis. Eight (14%) cases died.
Of 45 H. influenzae isolates for which
typing was performed, 12 were type
a, 2 type b (Hib), 1 type e, 3 type f,
and 27 were nontypeable. There were
2 Hib disease cases in 2021 compared
to 1 case in 2020, 3 in 2019, 1 in 2018,
2 in 2017, 5 in 2016, and 2 in 2015.
Among the 2021 Hib disease cases,
one was a 2-year old child who had
meningitis and survived; this child had
not received any Hib vaccination. The
second was in a 6-month old who had
meningitis and survived; this child had
documentation of one dose of Hib
vaccine.
The eight deaths occurred in patients
ranging in age from 56 to 92 years.
Three decedents had pneumonia,
two had septic shock, two had
pneumonia and septic shock, and one
had pneumonia, meningitis and septic
shock. Co-morbidities were reported
in seven patients and serotypes
were nontypeable (5) or type f (1);
two isolates were not available for
serotyping.
Histoplasmosis
Histoplasmosis is caused by the
soil-dwelling dimorphic fungus
Histoplasma capsulatum. Infection
typically results from inhalation of
aerosolized spores, and symptomatic
infections usually involve pulmonary
disease, though disseminated or non-
pulmonary infections are possible.
Common activities associated with
exposure include farming, exposure to
soil enriched with bird or bat guano,
remodeling or demolition of old
buildings, and clearing trees or brush
in which birds have roosted.
In 2021, there were 38 confirmed and
152 probable cases of histoplasmosis
reported. These numbers are
consistent with the case counts from
the years prior to the COVID-19
pandemic.
The median age of cases was 48 years
(range, 0 to 88 years), and 112 (59%)
were male. Of the 133 cases for whom
race was reported, 112 (84%) were
white, 11 (8%) were Black, 6 (5%)
were Asian, 2 (1.5%) were American
Indian/Alaska Native, 1 (<1%) was
Native Hawaiian/Pacific Islander and
1 (<1%) was more than one race.
Of the 130 for whom ethnicity was
reported, 4 (3%) were Hispanic.
When hospitalization status was
reported, 38 of 70 (54%) cases were
hospitalized. Median hospitalization
duration was 5 days (range, 1 to 47
days). There were 2 deaths among
the 54 cases for which outcome was
12
DCN 48;1 2022
0
2000
4000
6000
8000
10000
12000
0
50
100
150
200
250
300
350
400
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
Number of People Living with HIV/AIDS
Year
HIV Disease Diagnoses*
All Deaths**
Living with HIV/AIDS
*Includes all new cases of HIV infection (both HIV [non-AIDS] and AIDS at first diagnosis) diagnosed within a given calendar year.
**Deaths in Minnesota among people with HIV/AIDS, regardless of location of diagnosis and cause.
Number of New HIV/AIDS Cases and Deaths
reported, a case fatality rate of 4%.
Histoplasmosis was the primary cause
of death for both of those cases.
From 2017 to 2021, 872 cases of
histoplasmosis were reported. The
annual incidence of histoplasmosis
in Minnesota in 2021 was 3.3 cases
per 100,000 population, similar to
the average annual incidence of 3.0
cases per 100,000 for 2017-2020.
The average annual incidence of
histoplasmosis by county shows
that cases occur more frequently
in southern and western counties
(Figure 2). This is in contrast to the
other endemic fungal disease found in
Minnesota, blastomycosis, for which
the highly endemic region includes the
northern and northeastern counties of
Minnesota. While clinicians should test
for both diseases when clinical illness
is consistent with a fungal infection,
these maps may help assess possible
risks in different parts of the state.
HIV Infection and AIDS
HIV/AIDS incidence in Minnesota
remains moderately low. The most
state-specific recent rate data is from
2020, which shows that state-specific
HIV infection rates ranged from
1.5 per 100,000 population in
Montana to 22.1 per 100,000 in
Georgia. Minnesota had the 14th
lowest rate (4.8 cases per 100,000
population).
As of December 31, 2021, a
cumulative total of 12,643 cases
of HIV infection (2,418 AIDS at
first diagnosis, and 10,225 HIV
[non-AIDS] cases) were reported
among Minnesota residents. By the
end of 2021, an estimated 9,696
persons with HIV/AIDS were living
in Minnesota.
The annual number of AIDS cases
reported in Minnesota increased
steadily from 1982 through the
early 1990s, reaching a peak of 361
cases in 1992. Beginning in 1996,
the annual number of new AIDS
diagnoses and deaths declined
sharply, primarily due to better
antiretroviral therapies. In 2021, 81
new AIDS cases (Figure 4) and 99
deaths among persons living with
HIV infection in Minnesota were
reported.
The number of HIV (non-AIDS)
diagnoses has varied over the past
decade. There was a peak of 278
newly diagnosed HIV (non-AIDS)
cases in 2009, and a low of 183
new HIV (non-AIDS) cases reported
in 2020. Before 2020, the lowest
number of cases reported was 215
new HIV (non-AIDS) cases, reported
in 2017.
In 2021, 74% (222/298) of new HIV
diagnoses (both HIV [non-AIDS] and
AIDS at first diagnosis) occurred in
the metropolitan area. In Greater
Minnesota there were 76 cases in
29 of 80 counties. HIV infection is
most common in areas with higher
population densities and greater
poverty.
The majority of new HIV infections
in Minnesota occur among males.
Trends in the annual number of new
HIV infections diagnosed among
males differ by race/ethnicity. New
infections occurred primarily among
white males in the 1980s and early
1990s. Whites still comprise the
largest number of HIV infections
among males, but the proportion of
cases accounted for by white males
account is decreasing. In 2021,
there were 87 new infections among
white males, which is 37% of new
HIV infections among males. Among
black African American males, there
Figure 4. HIV/AIDS: Number of New Cases, Prevalent Cases, and Deaths by Year

DCN 48;1 2022
13
continued...
were 68 new HIV diagnoses in 2021,
which is about a third of new HIV
infections among males (29%).
Among Hispanic males of any race
and black African-born males, there
were 41 and 21 new HIV infections
in 2021, respectively.
Females account for an increasing
percentage of new HIV infections,
from 11% of new infections in
1990 to 21% in 2021. Trends in
HIV infections diagnosed annually
among females also differ by race/
ethnicity. Early in the epidemic,
whites accounted for the majority
of newly diagnosed infections.
Since 1991, the number of new
infections among women of color
has exceeded that of white women.
In 2021, women of color accounted
for 73% of new HIV infections
among females in Minnesota.
The number of diagnoses among
African-born women has been
increasing over the past decade.
In 2021, the number of new cases
among African-born women was
25, accounting for 39% of all new
diagnoses among women. In
2021, there were 10 cases (16%)
diagnosed among African American
women.
Despite relatively small numbers
of cases, HIV/AIDS affects persons
of color disproportionately in
Minnesota. In 2021, men of color
comprised approximately 17% of
the male population in Minnesota
and 61% of new HIV diagnoses
among men. Similarly, persons of
color comprised approximately
17% of the female population
in Minnesota and 73% of new
HIV infections among women. It
bears noting the use of race can
be a proxy for other risk factors,
including lower socioeconomic
status and education. Race is not
considered a biological cause of
disparities in the occurrence of HIV.
Historically, race/ethnicity data
for HIV/AIDS in Minnesota have
grouped non-African born blacks
and black African-born persons
together as “black.” In 2001, MDH
began analyzing these groups
separately, and a marked trend of
increasing numbers of new HIV
infections among black African-born
persons was observed. In 2021,
there were 46 new HIV infections
reported among black Africans.
While black African-born persons
comprise about 2% of the state’s
population, they accounted for 15%
of all HIV infections diagnosed in
Minnesota in 2021.
In 2021, there were 88 diagnosed
with HIV less than 30 years of age,
accounting for 34% of all cases.
Most of the cases were among
young males, where 87% of cases
were less than 30 years of age.
Since the beginning of the
epidemic, male-to-male sex (men
who have sex with men; MSM)
has been the predominant mode
of exposure to HIV reported
in Minnesota. In 2021, MSM
(including MSM who also inject
drugs) accounted for 53% of new
diagnoses among men. IDU was
the predominant mode of exposure
for women (of those with known
exposure).
In the fall of 2019, an outbreak was
declared among persons who inject
drugs (PWID) diagnosed with HIV
in Minnesota. Statewide there was
a two-fold increase among PWID
with 11 cases in 2018 increasing to
22 cases in 2019. The outbreak area
included residents of Hennepin and
Ramsey counties, where an alert
was indicated among PWID. At the
end of 2020, the outbreak included
101 cases. Persons likely to be at
high risk for HIV infection include
sex partners or syringe-sharing
partners of people known to be
living with HIV, PWID and their
sex partners and needle sharing
partners, persons who exchange
sex for income or other items they
need, and persons who experienced
or are currently experiencing
homelessness.
In the fall of 2020, an alert for the
Duluth area was indicated among
newly diagnosed HIV infections,
after which an outbreak was
declared in March 2021. There
were 23 cases associated with
the outbreak between September
2019 and the beginning of 2021.
Typically, there are from one to
five cases of HIV per year in St.
Louis County. The health alert also
indicated a rise in the number
of syphilis cases in the Duluth
area. Both declared outbreaks are
currently on-going.
HIV perinatal transmission in the
United States decreased 90%
since the early 1990s. The trend
in Minnesota has been similar.
While the number of births to HIV-
infected women increased nearly
7-fold between 1990 and 2019,
with 60 births to pregnant persons
in 2021, the rate of perinatal
transmission decreased, from 15%
in 1994-1996 to 0% over the last 4
years (2018-2021), with the last HIV-
positive Minnesota birth in 2017.
Influenza
Several influenza surveillance
methods are employed. Data are
summarized by influenza season
(generally October-April) rather than
calendar year.
Hospitalized Cases
Surveillance for pediatric (<18
years of age) laboratory-confirmed
hospitalized cases of influenza
in the metropolitan area was
established during the 2003-2004
influenza season and expanded to
include adults for the 2005-2006
influenza season. For the 2008-
2009 season surveillance was
expanded statewide. Since the
2013-2014 season, clinicians have
been encouraged to collect a throat
or nasopharyngeal swab, or other
specimen from all patients admitted
to a hospital with suspect influenza
and submit the specimen to the
Public Health Lab (PHL) for influenza
testing. For the 2014-2015 season,
influenza B subtyping was added.
During the 2020-2021 influenza
season (October 1, 2020 – April 30,
2021), there were 35 laboratory-
confirmed hospitalized cases
reported. This represents a rate of
0.62 cases per 100,000 persons,
compared to 71.3 cases per 100,000
in 2019-2020 and 44.6 cases per
100,000 in 2018-2019. Cases
included 11 influenza A (all unknown
A type) and 24 influenza B (all
unknown lineage). Among the cases,
9% were 0-18, 17% were 19-49, 14%
were 50-64, and 60% were 65 years
of age and older. Median age was 69
years. Residents of the metropolitan
area made up 57% of cases.
Case report forms have been
completed on 100% of the 20
metropolitan area cases that were
selected for review. Of these, 28%
were diagnosed with pneumonia,
17% required admission into an
intensive care unit, and 11% were
placed on mechanical ventilation. An
invasive bacterial co-infection was
present in 22% of hospitalized cases.

14
DCN 48;1 2022
Antiviral treatment was prescribed for
67% of cases. Overall, 82% of adult
and 0% of pediatric cases had at least
one chronic medical condition that
would have put them at increased risk
for influenza disease.
Pediatric Deaths
There were 0 pediatric influenza-
associated deaths during this season.
Laboratory Data
The Minnesota Laboratory System
(MLS) Laboratory Influenza Surveillance
Program is made up of more than 110
clinic- and hospital-based laboratories
which voluntarily submit testing data
on a weekly basis. These laboratories
perform rapid testing for influenza and
respiratory syncytial virus. Significantly
fewer laboratories perform viral culture
testing. Some laboratories perform
PCR testing for influenza, and others
also perform PCR testing for other
respiratory viruses. The PHL provides
further characterization of submitted
influenza isolates to determine the
hemagglutinin serotype. Tracking
laboratory results assists healthcare
providers with patient diagnosis of
influenza-like illness (ILI) and provides
an indicator of the progression of the
influenza season, as well as prevalence
of disease in the community. Between
October 4, 2020–May 22, 2021,
laboratories reported data on 54,981
influenza molecular tests, 24 (<1%) of
which were positive for influenza. Of
these, 0 were positive for influenza A
(H3), 0 were positive for influenza A
(H1N1)pdm09, 10 (42%) were positive
for influenza A-not subtyped, and 14
(58%) were positive for influenza B.
Sentinel Surveillance
We conduct sentinel surveillance for
ILI (fever >100° F, and cough, and/or
sore throat in the absence of known
cause other than influenza) through
outpatient medical providers, including
those in private practice, public health
clinics, urgent care centers, emergency
rooms, and university student health
centers. There were 85 sites in 39
counties. Participating providers report
the total number of patient visits each
week and number of patient visits
for ILI by age group (0-4 years, 5-24
years, 25-64 years, ≥65 years). The
percentage of ILI peaked during the
week October 4-10, 2020, at 0.9%.
Influenza Incidence Surveillance
MDH continued to participate in
Optional Influenza Surveillance
Enhancements during the 2020-2021
influenza season. Each week, nine
clinic sites reported the number of ILI
patients divided by the total patients
seen by the following age groups: 0-4
years, 5-24 years, 25-49 years, 50-64
years, and ≥65 years. Clinical specimens
were collected on the first 10 patients
with acute respiratory illness for PCR
testing performed by the PHL for
influenza, SARS-CoV-2, and 13 other
respiratory pathogens.
Minimal demographic information
and clinical data were provided with
each specimen. From October 4,
2020–May 22, 2021, these clinics saw
1,777 ILI patients. They submitted 984
specimens for influenza testing; none
were positive for influenza.
ILI Outbreaks in Schools and Long-
term Care Facilities
Since 2009, schools report outbreaks
when the number of students absent
with ILI reaches 5% of total enrollment,
or when three or more students with ILI
were absent from the same elementary
classroom. Six schools in 3 counties
reported ILI outbreaks during the
2020-2021 school year. The number of
schools reporting ILI outbreaks since
the 2009-2010 school year ranged from
a low of 6 in 2020-2021 to a high of
1,302 in 2009-2010.
An influenza outbreak is suspected in a
long-term care facility (LTCF) when two
or more residents in a facility develop
symptoms consistent with influenza
during a 48- to 72-hour period. An
influenza outbreak is confirmed when
at least one resident has a positive
culture, PCR, or rapid antigen test for
influenza and there are other cases
of respiratory illness in the same unit.
Six facilities in 5 counties reported
confirmed outbreaks during the 2020-
2021 influenza season. The number of
LTCFs reporting outbreaks ranged from
a low of three in 2008- 2009 to a high
of 212 in 2017-2018.
Legionnaires' Disease
In 2021, 130 confirmed cases of
Legionnaires’ disease (2.3 per 100,000
population) were reported. This is
a 38% increase from the 94 cases
reported in 2020 and a 13% increase
from the median number of cases
reported annually from 2016 to 2020
(median, 115; range, 94 to 152).
Of the 130 confirmed cases, 123 (95%)
were hospitalized, with a median
duration of hospitalization of 5
days (range, 1 to 43 days). Of those
hospitalized, 36 (29%) were admitted
to an intensive care unit, and 23 (19%)
required mechanical ventilation. Nine
(7%) cases died. Seventy-five (58%)
cases were male. Older adults were
more often affected, with 105 (81%)
cases occurring among individuals ≥50
years (overall median age, 64 years;
range, 29 to 90 years). Of the 129 cases
for which race and ethnicity were
reported, 114 (88%) were white (of
which 2 were Hispanic), 11 (9%) were
Black, two (2%) were Asian American,
one (<1%) was American Indian, and
one (<1%) was other race. Sixty-six
(51%) cases were diagnosed during
June through September. Seventy-nine
(61%) were residents of the Twin Cities
metropolitan area and 51 (39%) were
residents of Greater Minnesota. Three
(2%) confirmed cases were part of an
outbreak associated with a hotel spa
pool (the outbreak had 2 additional
confirmed cases who were non-
Minnesota residents).
Although most cases are diagnosed by
Legionella urinary antigen test, culture
is useful for public health purposes
because clinical and environmental
isolates can be compared by molecular
typing in outbreak investigations. MDH
requests that clinical laboratories
submit Legionella isolates, as well
as available lower respiratory tract
(sputum, BAL) specimens from
confirmed and suspect cases for
culture and molecular typing.
Listeriosis
Twelve culture-confirmed listeriosis
cases were reported in 2021.
All were hospitalized, and three
died. The median age of cases
was 68 years (range, 44 to 93
years). Ten (83%) cases had Listeria
monocytogenes isolated from blood
and two from cerebrospinal fluid
(CSF). There were no pregnancy-
associated cases among culture-
confirmed cases in 2021. Nine cases
were white, two were Asian, and
three were Black; none were of
Hispanic ethnicity. The 12 cases are
slightly greater than the median
number of cases reported from 1996
through 2020 (median, 8 cases;
range, 3 to 19). Three cases were
part of outbreaks in 2021; two cases
were part of a multi-state outbreak
associated with an unknown
commercially distributed vehicle, and
one 2021 case was part of a multi-

DCN 48;1 2022
15
continued...
state outbreak associated with leafy
greens that occurred from 2014 to
2022.
In 2019, national case definitions
were modified to include “probable”
and “suspected” cases of listeriosis.
In 2021, three probable or suspected
cases were identified. Two probable
cases were a maternal-neonate pair;
the neonate had a CSF specimen test
positive by a culture-independent
diagnostic test that was not
subsequently culture-confirmed at
the MDH PHL, and the mother was
not tested. One suspected case was
identified in an individual with L.
monocytogenes isolated from an
ankle swab at a clinical laboratory.
Lyme Disease
Lyme disease is caused by Borrelia
burgdorferi, a spirochete transmitted
to humans by bites from Ixodes
scapularis, the blacklegged tick.
Recently, a new species, B. mayonii,
has also been identified as a cause
of human disease, and 11 cases have
been reported in Minnesota residents
since 2013, 1 in 2021. Data for these
cases is included in the summary data
below. In Minnesota, the same tick
vector also transmits the agents of
babesiosis, anaplasmosis, one form of
ehrlichiosis, and a strain of Powassan
virus.
In 2021, 1,033 confirmed Lyme
disease cases (18 cases per 100,000
population) were reported. In
addition, 869 probable cases
(physician-diagnosed cases that did
not meet clinical evidence criteria
for a confirmed case but that had
laboratory evidence of infection)
were reported. Overall, the number
of reported cases of Lyme disease
has been increasing for many years,
despite yearly fluctuations. The
median number of cases from 2010
through 2019 (median, 1,190; range,
896 to 1,431) was higher compared
to the median from 2000 to 2009
(median, 915; range, 463 to 1,239)
(Figure 1). Data for 2020 are not
available due to surveillance changes
made during the COVID-19 pandemic.
Of the confirmed Lyme disease cases
reported, 642 (62%) cases were male,
and the median case age was 45 years
(range, 2 to 94). Physician-diagnosed
erythema migrans (EM) was present
in 697 (67%) cases. Three hundred
seventy-one (36%) cases had one or
more late manifestations of Lyme
(5), and Togo (5), as well as several
other countries in sub-Saharan Africa.
The case reporting Asian travel had
visited Thailand.
Meningococcal Disease
No meningococcal cases were reported
in 2021.
Mumps
No mumps cases were reported in
2021.
Neonatal Sepsis
Statewide surveillance for neonatal
sepsis includes reporting of any
bacteria (other than coagulase-
negative Staphylococcus) isolated
from a sterile site in an infant <7 days
of age, and mandatory submission of
isolates. In 2021, 43 cases (0.68 cases
per 1,000 live births) were reported
compared to 45 cases in 2020. There
were 5 deaths. All were identified
via blood. Most cases (81%) were
culture-positive within the first 2
days of life. Group B Streptococcus
was most common (13) followed by,
Escherichia coli (12), Streptococcus
viridans (6), Enterococcus spp.
(4), Haemophilus influenzae (2), and 1
each of Actinomyces, Brevivacterium
spp., Gordonia spp., Streptococcus
pneumoniae, and Staphylococcus
aureus.
Pertussis
In 2021, 29 pertussis cases (1 per
100,000 population) were reported.
Laboratory confirmation was available
for 26 (90%) cases, none (0%) of
which were confirmed by culture and
8 (28%) of which were confirmed by
PCR. In addition, 7 (24%) cases met
the clinical case definition and were
epidemiologically linked to laboratory
confirmed cases, and 3 (10%) met the
clinical case definition only. Twenty
(69%) cases occurred in residents of
the metropolitan area.
Paroxysmal coughing was the
most common reported symptom,
which 24 (83%) cases experienced.
Approximately 36% (10) reported
disease, including 241 with a history
of objective joint swelling, 108 with
cranial neuritis including Bell’s Palsy,
6 with lymphocytic meningitis, 16
with acute onset of 2nd or 3rd degree
atrioventricular conduction defects,
and 1 with radiculoneuropathy, and
confirmation by Western immunoblot
(positive IgM ≤30 days post-onset
or positive IgG). Of the 934 cases
with known onset dates, onset
of symptoms peaked from June
through August, with 68% of EM
cases experiencing symptom onset in
June or July. This timing corresponds
with peak activity of nymphal I.
scapularis ticks in mid-May through
mid-July. Most cases either resided
in or traveled to endemic counties
in north-central, east-central, or
southeast Minnesota, or Wisconsin.
Malaria
Malaria is a febrile illness caused
by several protozoan species in the
genus Plasmodium. The parasite is
transmitted to humans by bites from
infected Anopheles genus mosquitoes.
The risk of malaria is highest in the
tropical and sub-tropical regions of
the world. Although local transmission
of malaria frequently occurred in
Minnesota over 100 years ago, all
cases reported in Minnesota residents
in recent years have been imported
infections acquired abroad.
In 2021, 64 cases (1.1 per 100,000
population) were reported. Fifty-
six (88%) cases were identified
with P. falciparum, 2 (3%) with P.
vivax, 2 (3%) with P. ovale, 1 (2%)
with P. malariae and 1 (2%) with
mixed Plasmodium species infection.
In 2 cases (3%), the testing performed
was unable to identify a species. The
median age of cases was 40 years
(range, 3 to 81). Of the 53 cases with
known race, 48 (91%) were Black, 3
(5%) were white, 1 (2%) was Asian, and
1 (2%) identified as other race. Sixty-
three cases were Minnesota residents
at the time of their illness, 48 (75%)
of whom resided in the seven-county
metropolitan area. Of the 36 cases with
known country of birth, 4 (6%) were
born in the United States. Exposure
and travel information was not
available for 3 cases, while 60 (94%)
cases likely acquired malaria in Africa,
and 1 patient reported travel to Asia.
Sixteen countries were considered
possible exposure locations in Africa
for malaria infections, including Liberia
(17), Nigeria (8), Cameroon (6), Kenya

16
DCN 48;1 2022
whooping. Although commonly
referred to as “whooping cough,”
very young children, older individuals,
and persons previously immunized
may not have the typical “whoop”.
Post-tussive vomiting was reported
in 14 (49%) cases. Infants and young
children are at the highest risk for
severe disease and complications. In
2021, no cases were diagnosed with
Pneumonia, none were hospitalized,
and no deaths occurred.
Pertussis is increasingly recognized
in older children and adults. During
2021, cases ranged in age from 9
months to 74 years. No cases were
diagnosed in children <6 months of
age, 5 (19%) in children 6 months
through 4 years, none in children
5-12 years, two (8%) cases occurred
in adolescents 13-17 years, and
19 (73%) in adults ≥18 years. The
median age of cases was 38 years.
Infection in older children and
adults may result in exposure of
unprotected infants. During 2021,
one case was in an infant <1 year
of age. A likely source of exposure
wasn’t identified for that case. ACIP
recommends vaccination of women
at ≥20 weeks gestation during each
pregnancy to protect young infants.
Ensuring up-to-date vaccination of
children, adolescents, and adults,
especially those in contact with
young children, is also important.
Children aged 7 and under receive
the DTaP vaccine, while older
children and adults receive the Tdap
vaccine. Vaccinating adolescents
and adults with Tdap will decrease
the incidence of pertussis in the
community and thereby minimize
infant exposures.
Although unvaccinated children
are at highest risk for pertussis,
fully immunized children may also
develop disease, particularly as the
number of years since vaccination
increases. Disease in those
previously immunized is usually
mild. Efficacy for currently licensed
DTaP vaccines is estimated to be
71-84% in preventing typical disease
within the first 3 years of completing
the series. Waning immunity
sharply increases at 7 years of age,
and most are susceptible by 11-12
years of age when the Tdap booster
is recommended. Recent studies
suggest that immunity wanes
sharply 2 years from receipt of Tdap.
Of the 8 (28%) cases who were 7
months to 6 years of age, 5 (63%)
were known to have received at
least a primary series of 3 doses of
DTP/ DTaP vaccine prior to onset
of illness; 3 (38%) received fewer
than 3 doses and were considered
preventable cases.
Reporting rules require clinical
isolates of Bordetella pertussis
be submitted to the PHL to track
changes in circulating strains.
Isolates were not subtyped using
pulsed-field gel electrophoresis
(PFGE). Nationally, isolates have
had low minimum inhibitory
concentrations (falling within the
reference range for susceptibility)
to erythromycin and azithromycin.
Only 11 erythromycin-resistant B.
pertussis cases have been identified
in the United States.
Laboratory tests should be
performed on all suspected cases.
B. pertussis is rarely identified
late in the illness, therefore, a
negative culture does not rule out
disease. A positive PCR result is
considered confirmatory in patients
with a 2-week history of cough
illness. PCR can detect non-viable
organisms. Consequently, a positive
PCR result does not necessarily
indicate current infectiousness.
Patients with a 3-week or longer
history of cough illness, regardless
of PCR result, may not benefit
from antibiotic therapy. Whenever
possible, culture should be done
in conjunction with PCR testing.
Serological tests may be useful for
those with coughs >2 weeks.
Pertussis remains endemic despite
an effective vaccine and high
coverage rates with the primary
series. Reported incidence of
pertussis has consistently increased
over the past 10 years, particularly
in middle school-aged children,
adolescents, and adults.
Q Fever
Q fever is an acute to chronic illness
caused by Coxiella burnetii. Cattle,
sheep, and goats are the primary
sources of infection. Transmission
can occur through contact with
infected animals or animal tissue,
inhalation of aerosolized bacteria,
ingestion of unpasteurized dairy
products, and tick bites.
In 2021, six confirmed cases of Q
fever were reported, including one
chronic case and five acute cases.
The confirmed chronic case was
a 71-year-old male whose illness
included splenomegaly, vasculitis, and
endocarditis. He was likely exposed
through drinking raw milk in the past.
The median age of the acute cases
was 36 years (range, 9 to 67 years); all
were male. Four (80%) identified as
white, one (20%) identified as Black,
and all identified as non-Hispanic.
All were likely exposed through
contact with animals, including goats,
camels, and sheep. One (20%) case
was likely acquired internationally.
Three (60%) cases were hospitalized
for a median of 3 days (range, 3 to
17 days). Three (60%) acute cases
developed hepatitis as a result of
their infection, one (20%) developed
hepatosplenomegaly, and one (20%)
developed myocarditis.
From 1997 to 2021, 32 confirmed
acute cases and 11 chronic cases of
Q fever were reported. The median
age of acute cases was 60 years
(range, 11 to 77 years); the median
age of chronic cases was also 60
years (range, 5 to 78 years). Twenty-
four (86%) of the 28 cases for which
both race and ethnicity were known
identified as White, non-Hispanic;
3 (11%) identified as Black, non-
Hispanic; and 1 (4%) identified as
mixed race, non-Hispanic. During
this time, 26 (79%) of the 33 cases
for whom exposure information
was available were likely exposed
through direct or indirect contact with
animals; 4 (12%) were likely exposed
through ingestion of unpasteurized
dairy products; and, 3 (9%) were
likely exposed through a tick bite. Ten
(36%) of the 28 cases with known
occupations were employed in an
agriculture-related occupation at the
time of their exposure.
Rabies
In Minnesota, the animal reservoirs
for rabies are skunks, which carry the
North-central U.S. skunk rabies virus
variant and multiple bat species, each
with their own host-adapted rabies
virus variant. Dogs, cats, and livestock
are generally exposed to rabies
through encounters with skunks.
Vaccinating these domestic animals
for rabies provides a buffer between
wildlife and people.
In 2021, 42 (2.2%) of 1,932 animals
tested were positive for rabies. This
is similar to those identified in 2020
(40, [1.9%] of 2,114 animals tested)
and similar to the number of positives
identified annually in the previous

DCN 48;1 2022
17
continued...
Murray
Pine
Aitkin
Cass
Hubbard
Wilkin
Itasca
St. Louis
Cook
Wash-
ing-
ton
Lake
Le
Sueur
Rice
Goodhue
NoblesRock Jackson Martin Faribault Freeborn Mower Fillmore Houston
Winona
Olmsted
DodgeSteeleWasecaBlue EarthWatonwanCottonwood
Pipestone
Nicollet
Wabasha
Dakota
Scott
Isanti
Brown
Sibley
Carver
WrightMeeker
Kandiyohi
Renville
Redwood
Sherburne
LyonLincoln
Yellow Medicine
Lac Qui Parle
Swift
Big Stone
PopeStevens
Traverse
Chippewa
Stearns
Benton
Carlton
Kanabec
Mille
Lacs
Crow Wing
Morrison
Wadena
Todd
DouglasGrant
Otter Tail
Becker
Clay
Clear
Water
Mahnomen
Norman
Red Lake
Pennington
Polk
Beltrami
Marshall
Koochiching
Lake
of the
Woods
RoseauKittson
McLeod
Ramsey
Anoka
Hennepin
Chisago
* Placement of symbol in county does not represent exact geographical location of the case.
Species No.
Skunk 3
Cat
1
Bat
38
decade. In 2021, 90% (38/42) of rabid
animals were bats followed by skunks
(3/42 [7%]). There was one rabid
domestic animal, a cat (Figure 5).
Cases of human rabies in the
United States are rare, with 1 to 6
cases reported annually. In 2021,
Minnesota reported its first human
rabies case since 2007. This case
was bitten by a rabid bat, received
timely and appropriate rabies post-
exposure prophylaxis (PEP), yet
developed rabies 6 months after the
bite. This was the first documented
failure of rabies PEP in the western
hemisphere and the first to involve
bat variant rabies virus. An extensive
investigation was conducted and
determined that this case had a
previously unrecognized, impaired
immune system, which likely
prevented an appropriate immune
Figure 5. Rabid Animals by County, 2021*
response against the rabies virus.
Ensuring adequate immune response
to rabies vaccines is increasingly
important given the rising prevalence
of immunocompromised adults in the
United States. This investigation does
not challenge the high efficacy or
safety profile of rabies PEP biologics.
From 2003 to 2021, 983 (2.3%) of
43,621 animals tested in Minnesota
were positive for rabies. The median
number of rabies-positive animals
identified annually was 48 (range 28
to 94). From 2003 to 2021, 337/761
(44.3%) skunks, 57/966 (5.9%) cattle,
490/12,978 (3.8%) bats, 9/375
(2.4%) horses, 49/12,729 (0.4%) cats,
29/12,419 (0.2%) dogs, 1/1,323 (0.1%)
raccoons, and 12/2,137 (0.6%) other
animals (fox [6], goat [3], woodchuck,
bison, deer) tested were positive
for rabies. In contrast to the eastern
United States, where raccoons carry
a raccoon host-adapted variant of
the virus and are the most common
source of terrestrial rabies, rabies in
raccoons is rare in Minnesota.
Respiratory Syncytial Virus
(RSV)
Laboratory-confirmed respiratory
syncytial virus disease (RSV) became
reportable for all hospitalized residents
of the metropolitan area in September
2016. Any death occurring statewide
within 60 days of a positive RSV test
is also reportable. Typically, RSV
circulates during the colder months of
the year (October-April), however RSV
activity has differed in recent years
from the usual seasonality.
From October 1, 2021 – April 30, 2022,
623 cases were reported. From May
1, 2022 – September 30, 2022, 365
cases were reported. Combined, from
October 1, 2021 – September 30, 2022,
there were 988 cases reported (32
cases per 100,000 persons), compared
to 670 cases were reported (22 cases
per 100,000 persons) from October
2020 – September 2021. The overall
median age was 11 months (range: 0
days – 98 years). Sixty-eight percent
(674) were <2 years of age: 35% (347)
were <6 months, 17% (163) were 6
months – 11 months, and 17% (164)
were 1 year – <2 years. Fourteen
percent (137) were 2-4 years, 4% (36)
were 5 – 17 years, 3% (30) were 18 –
49 years, 3% (27) were 50 – 64 years,
and 9% (84) were >65 years of age.
Overall, 51% of RSV cases were male
and 50% were white.
Thirty-nine percent (393) of cases
had a co-morbid condition at the
time of their illness and presence
of a co-morbid condition increased
significantly as age increased. The most
common co-morbid conditions for
cases <2 years of age were prematurity
(58%), chronic lung disease (19%)
and cardiovascular disease (15%). For
cases 2 – 17 years of age, the most
common co-morbid conditions were
chronic lung disease (55%), neurologic
conditions (42%), cardiovascular
disease (24%), and feeding tube
dependent (18%). The most common
underlying conditions for adults
18-64 years of age and older adults
(≥65 years) were chronic metabolic
disease (38% and 52% respectively),
cardiovascular disease (48% and
66% respectively), chronic lung
disease (56% and 49% respectively),

18
DCN 48;1 2022
multi-state outbreak associated with
a specific producer of raw, frozen,
breaded, stuffed chicken products that
included 36 cases in 11 states. This
was the 10th outbreak associated with
this type of product in Minnesota, and
the 5th with products from the same
producer since 1998.
Three culture-confirmed cases of S.
Javiana infection were part of a multi-
state outbreak of 4 cases from 2 states
associated with pre-packaged Napa
salad. The Napa cabbage component
was the most plausible contaminated
ingredient. However, the source or
mechanism of contamination could
not be determined.
Two culture-confirmed cases of S.
Muenster infection were part of a
multi-state outbreak associated with
contact with bearded dragons. The
genetic relatedness of isolates from
this outbreak to S. Muenster isolates
from a previous 2020 outbreak
associated with bearded dragons
indicates a continuing source of
contamination in the pet bearded
dragon industry.
One culture-confirmed case of S.
Vitkin infection was part of a multi-
state outbreak of 12 cases from 10
states associated with contact with
bearded dragons.
Two culture-confirmed cases of S.
Uganda infection were part of a multi-
state outbreak of 56 cases from 26
states associated with contact with
bearded dragons.
Seven culture-confirmed cases and
one probable case of S. Enteritidis
infection were linked to a Mexican-
style restaurant where the potential
vehicle was chicken or guacamole
salad. Improper cold holding and lack
of adequate cleaning/sanitization may
have contributed to the outbreak.
One culture-confirmed case of S.
Typhimurium infection and one
culture-confirmed case of S. Infantis
infection were part of a multi-state
outbreak that included 40 cases (26
S. Typhimurium and 14 S. Infantis)
from 17 states. The outbreak vehicle
was antipasto trays containing various
Italian-style meats.
Twenty-four laboratory-confirmed (22
culture-confirmed and 2 CIDT-positive
only) cases and four probable cases of
S. Enteritidis infection were associated
with watermelon consumption at an
Asian-style buffet restaurant. The
and hypertension (46% and 81%
respectively).
Thirteen RSV-associated deaths were
reported during the regular the 2021-
2022 respiratory season. Eleven deaths
occurred during hospitalization and 3
within 60 days of hospital discharge.
From May 1, 2021 – September 30,
2021, 3 deaths were reported: 2 during
hospitalization and 1 within 60 days of
hospital discharge. The median age of
all deaths was 78 years (range 69 years
to 96 years), and all 17 deaths had
co-morbid conditions. Identification
of additional RSV-associated deaths is
ongoing.
Salmonellosis
During 2021, 1,024 Salmonella
cases were reported. Of those, 853
were culture-confirmed Salmonella
and 171 only tested positive by a
culture-independent diagnostic test
(CIDT) and not subsequently culture-
confirmed.The 853 culture-confirmed
cases of Salmonella infection (15.1
per 100,000 population) reported
in 2021 represents a 6% increase
from the median number of culture-
confirmed cases reported annually
from 2011 to 2020 (median, 808
cases; range, 660 to 1,009) (Figure 2).
Of the 91 serotypes identified
among culture-confirmed cases
in 2021, 6 serotypes, S. Enteritidis
(191), S. Typhimurium (108), S. I
4,[5],12:i:- (90), S. Infantis (63), S.
Newport (51), and S. Oranienburg
(40) accounted for 64% of cases.
Salmonella was isolated from stool
in 741 (87%), urine in 58 (7%),
and blood in 48 (6%) cases. Other
specimen sources included body fluid,
groin, left knee, perineal swab, skin/
subcutaneous tissue, and vaginal
swab.
The incidence of Salmonella infections
was 16.2 per 100,000 population
among cases who reported Black
race, 14.3 among cases who reported
Asian race, 12.5 among cases who
reported white race, and 11.2 among
cases who reported American Indian/
Alaska Native race. The incidence of
Salmonella infections was 20.8 per
100,000 population for cases who
reported Hispanic ethnicity.
One hundred eighty-four (22%)
culture-confirmed cases were
hospitalized; the median length of
hospital stay was 4 days (range, 1 to
70 days). Two culture-confirmed
cases died. An 80 year-old died of
bacteremia, Salmonella infection,
and respiratory distress 7 days after
S. Newport was isolated from blood.
A 76 year-old died of respiratory
failure, air embolism, septic
shock, and Salmonella infection
9 days after S. Paratyphi B var.
L(+) tartrate+ (formerly Java) was
isolated from stool.
Of the 730 culture-confirmed cases
with known travel history, 94 (13%)
had traveled internationally during
the week prior to their illness onset.
There were three S. Typhi cases;
one travelled to Sierra Leone, one
traveled to Mexico, and one had no
known international travel. There
was one S. Paratyphi A case with no
known international travel.
During 2021, 171 cases with
specimens that were positive
by a CIDT conducted at a
clinical laboratory, but were not
subsequently culture-confirmed,
were reported. CIDTs have
become widely adopted by clinical
laboratories for the detection of
Salmonella in stool. The median
age of the CIDT-positive only cases
was 52 years (range, 0 to 92 years).
Fifty (29%) cases were hospitalized;
the median hospital stay was 6 days
(range, 2 to 66 days). Two cases
died.
One hundred sixty-eight laboratory-
confirmed (166 culture-confirmed
and 2 CIDT-positive only) cases were
part of 20 Salmonella outbreaks in
2021. Sixteen of the 20 outbreaks
involved foodborne transmission,
and 4 were due to animal contact.
Twelve of the outbreaks involved
cases with exposure in multiple
states. The 20 outbreaks resulted
in a median of 3 culture-confirmed
cases per outbreak (range, 1 to 56).
In addition, there was one multi-
state investigation that included
two Minnesota cases, which CDC
classified as an outbreak with an
unknown source.
Five culture-confirmed cases and
two probable (clinically defined
illness) cases of S. I 4,5,12:i:-
infection were associated with
a funeral event that served food
prepared in private homes. The
source of contamination and vehicle
of transmission were not identified.
Four culture-confirmed cases of S.
Enteritidis infection were part of a

DCN 48;1 2022
19
continued...
Disease
2017 2018 2019 2020 2021
No. Rate No. Rate No. Rate No. Rate No. Rate
Chlamydia
23,528 444 23,564 444 24,535 463 21,942 413.7 22,578 425.7
Gonorrhea
6,519 123 7,542 142 8,063 152 10,217 192.6 9,671 182.3
Syphilis, Total
934 17.6 918 17.3 1127 21.2 1093 20.6 1457 27.5
Primary/
Secondary
292 5.5 292 5.5 385 7.3 461 7.8 564 10.6
Early NP/NS*
313 5.9 286 5.4 367 6.9 365 6.9 415 7.8
Unknown/Late
327 6.2 330 6.2 354 6.7 303 5.7 463 8.7
Congenital**
2 3 10 15.1 21 32.3 7 11.2 15 23.6
*NP=Non-primary; NS=Non-secondary
**Congenital syphilis rate per 100,000 live births.
Note: Data exclude cases diagnosed in federal or private correctional facilities.
most likely cause of the outbreak was
cross contamination from raw meat to
watermelon, partially due to the use
of a spray hose. This was the third S.
Enteritidis outbreak associated with
this restaurant since 2018.
Eight culture-confirmed cases and
nine probable cases of S. Typhimurium
infection were associated with a
graduation party. The vehicle of
transmission was not identified.
Two culture-confirmed cases of S.
Enteritidis infection were part of a
multi-state outbreak for which the
suspected vehicle was chicken. There
were 50 cases from 20 states.
Twenty-eight culture-confirmed
cases and 10 probable cases of S.
Oranienburg infection were part of a
multi-state outbreak associated with
whole, fresh onions imported from
Mexico that included 1,040 cases in
39 states. Following a 2020 multi-
state S. Newport outbreak, this was
the second consecutive year in which
there was a multi-state outbreak
of over 1,000 Salmonella infections
associated with onions.
Two culture-confirmed cases of S.
Thompson infection were part of a
multi-state outbreak associated with
seafood primarily from a distributor in
Colorado. There were 115 cases from
15 states, and one of the Minnesota
cases was part of a subcluster in
Colorado.
Table 3. Number of Cases and Incidence Rates (per 100,000 Persons)
of Chlamydia, Gonorrhea, and Syphilis
Three culture-confirmed cases of S.
I 4,5,12:i:- infection were part of a
multi-state outbreak associated with
Italian-style meat sticks that included
36 cases from 11 states. Timely and
detailed reinterviewing of cases
allowed MDH staff to rapidly identify
the outbreak vehicle with only three
cases.
Three culture-confirmed cases of S.
Typhimurium infection were linked
to a Minnesota restaurant where
the vehicle of transmission was not
identified. Poor hand-washing and
bare-hand contact practices at the
restaurant might have contributed to
the outbreak.
Ten culture-confirmed cases and one
probable case of S. Typhimurium
infection were linked to a Minnesota
Mexican-style restaurant. Lettuce was
a possible vehicle of transmission. An
infected food worker was the most
plausible source of contamination,
and therefore any ready-to-eat food
item could have been a vehicle of
transmission.
One culture-confirmed case and
four probable cases of S. Enteritidis
infection, plus a culture-confirmed
case in an out-of-state resident, were
linked to the same Asian-style buffet
restaurant that was the source of
another S. Enteritidis outbreak that
occurred earlier in 2021 (reported
above). No specific food vehicle was
identified, but extensive issues in
the restaurant created a high risk for
contamination of equipment, food
preparation surfaces, and ready-to-eat
food items.
Two culture-confirmed cases of
S. Newport infection were likely
associated with a college cafeteria;
however, a vehicle was not identified.
One culture-confirmed case of S.
Saintpaul infection was part of a
multi-state outbreak of 60 cases from
14 states that was likely associated
with tomatoes. One specific grower
in Florida was identified as a
common source of tomatoes for
three subcluster establishments by
traceback.
Fifty-six culture-confirmed cases
of Salmonella infection with
various serotypes (S. Infantis [37],
S. Enteritidis [9], S. Hadar [8], S.
Mbandaka [1], and S. Muenchen
[1]) were associated with a multi-
state outbreak linked to live poultry
contact. Nationally, there were 1,135
people infected with the outbreak
strains across 48 states, with illness
onset dates ranging from December
15, 2020 to October 10, 2021.
Sexually Transmitted Diseases
Gonorrhea and chlamydia are
monitored through a mostly passive
surveillance system involving review of
submitted case reports and laboratory
reports. Syphilis is monitored

20
DCN 48;1 2022
*Residence information missing for 247 cases of chlamydia and 75 cases of gonorrhea.
**Suburban is defined as the metropolitan area (Anoka, Carver, Dakota, Hennepin, Ramsey, Scott, and
Washington Counties), excluding the cities of Minneapolis and St. Paul.
^Case counts include persons by race alone. Population counts used to calculate results include race alone or in
combination.
^^No comparable population data available to calculate rates.
^^^Persons of Hispanic ethnicity may be of any race.
Note: Data exclude cases diagnosed in federal or private correctional facilities.
through active surveillance, which
involves immediate follow-up
with the clinician upon receipt
of a positive laboratory report.
Although overall incidence rates
for sexually transmitted diseases
(STDs) in Minnesota are lower than
those in many other areas of the
United States, certain population
subgroups have very high STD rates.
Specifically, STDs disproportionately
affect adolescents, young adults, and
persons of color.
Chlamydia
Chlamydia trachomatis infection
is the most commonly reported
infectious disease in Minnesota.
In 2021, 22,578 chlamydia cases
(425 per 100,000 population) were
reported. This is a 3% increase
compared to 2020 (Table 3).
Adolescents and young adults are at
highest risk for acquiring a chlamydia
infection (Table 4). The chlamydia
rate is highest among 20 to 24-year-
olds (2,249 per 100,000), followed
by the 15 to 19-year-old age group
(1,494 per 100,000). The incidence
of chlamydia among adults 25 to 29
years of age (1,041 per 100,000) is
considerably lower but has increased
in recent years. The chlamydia rate
among females (541 per 100,000) is
nearly twice the rate among males
(308 per 100,000), most likely due
to more frequent screening among
females.
Chlamydia infection incidence is
highest in communities of color
(Table 4). The rate among black
non-Hispanics (2,024 per 100,000)
is 10.3 times higher than the rate
among white non-Hispanics (196
per 100,000). Although black,
non-Hispanic persons comprise
approximately 5% of Minnesota’s
population, they account for 25%
of reported chlamydia cases. Rates
among Asian/Pacific Islanders (382
per 100,000), Hispanic, any race (900
per 100,000), and American Indian/
Alaska Natives (970 per 100,000) are
4.6 to 4.9 times higher than the rate
among white, non-Hispanic persons.
Chlamydia infections occur
throughout the state, with the
highest reported rates in Minneapolis
(1,206 per 100,000) and St. Paul (894
per 100,000). All geographical areas
around our state saw an increase in
the rate of chlamydia between 2020
and 2021. Every county in Minnesota
had at least 2 cases in 2021.
Table 4. Number of Cases and Incidence Rates (per
100,000 Persons) of Chlamydia, Gonorrhea, and
Primary/Secondary Syphilis by Residence, Age,
Race/Ethnicity, and Gender, 2021
Disease
Chlamydia Gonorrhea
Primary/
Secondary
Syphilis
No. Rate No. Rate No. Rate
Total
22,578 426 9,606 181 564 10.6
Residence
Minneapolis
4,613 1206 2,923 764 190 49.7
St. Paul
2,548 894 1,466 514 81 28.4
Suburban**
7,585 348 2,755 126 147 6.7
Greater Minnesota
7,519 306 2,377 97 146 5.9
Age
<15 years
166 16 64 6 1 0.1
15-19 years
5,494 1494 1,328 361 18 4.9
20-24 years
7,997 2249 2,282 642 61 17.2
25-29 years
3,880 1041 1,982 532 105 28.2
30-34 years
2,293 669 1,595 465 113 33.0
35-39 years
1,267 386 1067 325 78 23.8
40-44 years
649 184 594 168 60 17.0
45-49 years
361 89 319 79 30 7.4
50-54 years
222 55 188 47 41 10.2
55+ years
249 19 252 19 57 4.3
Gender
Male
8109 308 5,306 202 420 16
Female
14452 541 4,351 163 143 5.4
Transgender/
unknown^^
17 14 1
Race^/Ethnicity
White, non-Hispanic
9,066 196 3,075 67 239 5.2
Black, non-Hispanic
5,687 2024 3,849 1370 144 51.3
American Indian/
Alaska Native
653 970 410 609 58 86.1
Asian/PI
844 382 216 98 15 6.8
Other^^
625 169 53
Unknown^^
3,450 1,328 15
Hispanic^^^
2,253 900 559 223 40 16.0

DCN 48;1 2022
21
continued...
Gonorrhea
Gonorrhea is the second most
commonly reported STD in
Minnesota. In 2021, 9,671 cases
(182 per 100,000 population) were
reported. This is a 5% decrease
compared to 2020 (Table 4).
Adolescents and young adults are
at greatest risk for gonorrhea (Table
4), with rates of 361 per 100,000
among 15 to 19- year-olds, 642
per 100,000 among 20 to 24-year
old, and 532 per 100,000 among
25 to 29-year-olds. Gonorrhea
rates for males (202 per 100,000)
were higher than females (163 per
100,000).
Communities of color are
disproportionately affected by
gonorrhea. The incidence of
gonorrhea among black, non-
Hispanics (1370 per 100,000) is
20.6 times higher than the rate
among white, non-Hispanics (67 per
100,000). Rates among Asian/Pacific
Islanders (98 per 100,000), Hispanic,
any race (249 per 100,000), and
American Indian/Alaska Natives
(609 per 100,000) are up to 9 times
higher than among white, non-
Hispanic persons.
Gonorrhea rates are highest in
the cities of Minneapolis and St.
Paul (Table 4). The incidence in
Minneapolis (764 per 100,000) is
over 1.5 times higher than the rate
in St. Paul (514 per 100,000), almost
6 times higher than the rate in the
suburban metropolitan area (126
per 100,000), and almost 8 times
higher than the rate in Greater
Minnesota (97 per 100,000).
Syphilis
Surveillance data for primary
and secondary syphilis are used
to monitor morbidity trends
because these represent recently
acquired infections. Data for early
syphilis (which includes primary,
secondary, and early non-primary/
non-secondary stages of disease)
are used in outbreak investigations
because these represent infections
acquired within the past 12 months
and signify opportunities for disease
prevention.
The incidence of primary/secondary
syphilis in Minnesota is lower than
that of chlamydia or gonorrhea
(Table 3), but has remained elevated
since an outbreak began in 2002
among men who have sex with men
(MSM). In 2021, there were 564
cases of primary/secondary syphilis
in Minnesota (10.6 cases per 100,000
persons), which is a 35% increase
compared to 2020.
In 2021, the number of early syphilis
cases increased by 25%, with 979
cases, compared to 783 cases in
2020. The incidence remains highly
concentrated among MSM. Of the
early syphilis cases in 2021, 723 (73%)
occurred among men; 444 (61%) of
these were MSM. Thirty-one percent of
the MSM diagnosed with early syphilis
were co-infected with HIV. The number
of women reported has continued to
increase over the past 10 years from 13
early syphilis cases in 2011 to the near
historic high of 253 cases reported in
2021.
14 congenital syphilis cases were
reported in 2021. Syphilis may be
passed from a pregnant person to the
unborn baby through the placenta. The
infection can cause miscarriages and
stillbirths. Infants born with congenital
syphilis can suffer a variety of serious
health problems, including deformities,
seizures, anemia, and jaundice. The
CDC reported this fall that the number
of infants born with syphilis has
increased more than 200% in the past
four years and last year reached a 20-
year high. In Minnesota, the number
and rate of congenital syphilis cases
among infants has increased from 2.9
in 2015 to 23.6 per 100,000 live births
in 2021.
Shigellosis
In 2021, 220 Shigella cases were
reported. Of those, 109 were
culture-confirmed (1.9 per 100,000
population). The remaining 111 were
only tested by a culture-independent
diagnostic test (CIDT) and not
subsequently confirmed. The 220
culture-confirmed Shigella cases
represents a 38% increase from the
79 cases reported in 2020, and is 22%
less than the median annual number
of cases reported from 2011 to 2020
(median, 140 per year; range, 79 to
556). S. flexneri accounted for 76
(70%) cases, S. sonnei for 28 (26%)
cases, S. boydii for 2 (2%) cases, and
S. dysenteriae for 1 (1%) case. The
species was not identified for 2 (2%)
cases. Culture-confirmed cases ranged
in age from 1 to 89 years (median, 32
years). Nine percent of cases were
≤5 years of age; 85% of cases were
18 years of age or older. Seventy-five
percent of cases were male. Twenty-
three (21%) cases were hospitalized.
No cases died.
In 2021, of the 220 reported cases, 217
patients were positive for Shigella by a
CIDT conducted in a clinical laboratory.
Of the 208 corresponding specimens
that were received at MDH, 104
(50%) were subsequently culture-
confirmed. The remaining 111 cases
only had specimens that were positive
by a CIDT conducted at a clinical
laboratory and were not subsequently
culture-confirmed. The median age
of the CIDT-positive only cases was 32
years (range, 1 to 89 years). Thirteen
(12%) CIDT-positive only cases were
hospitalized; the median hospital stay
was 2 days (range, 1 to 7 days). One
CIDT-positive only case died.
Thirty-eight percent of cases reported
either non-white race (30 of 100
cases) or Hispanic ethnicity (16 of
100 cases). Of the 93 cases for which
travel information was available, 21
(23%) travelled internationally (8 of 25
[32%] S. sonnei and 12 of 65 [18%] S.
flexneri). Eighty-four percent of cases
resided in the Twin Cities metropolitan
area, including 61% in Hennepin
County and 17% in Ramsey County.
There was one outbreak of shigellosis
associated with a restaurant.
In 2021, 35 of the 103 Shigella isolates
received at MDH were tested
for antimicrobial resistance. Of
the 35 isolates, 74% (26 isolates)
were resistant to ampicillin, 74%
(26 isolates) were resistant to
trimethoprim-sulfamethoxazole,
and 46% (16 isolates) had decreased
susceptibility to azithromycin (DSA). All
but one of the 16 of the DSA isolates
were collected from adult males; the
remaining isolate was collected from
an adult female with no history of
international travel. Among the 10
adult male cases with DSA infection
and available information, 7 (70%)
reported sexual contact with a male
during the week before illness onset.
Staphylococcus aureus
Invasive Staphylococcus aureus (SA)
infections are classified into one of
three categories: hospital-onset (HO-
SA); healthcare-associated, community-
onset (HACO-SA); and community-
associated (CA-SA). SA must be
isolated from a normally sterile body
site greater than three days after the
date of initial hospital admission for a

22
DCN 48;1 2022
case to be considered HO-SA. HACO-
SA cases have at least one healthcare-
associated (HA) risk factor identified
in the year prior to infection. Examples
of HA risk factors include residence
in a long-term care facility, recent
hospitalization(s), dialysis, presence of
an indwelling central venous catheter,
and surgery. CA-SA cases do not have
any identifiable HA risk factors present in
the year prior to infection.
In 2005, as part of the Emerging
Infections Program (EIP) Active Bacterial
Core surveillance (ABCs) population-
based surveillance of invasive methicillin-
resistant S. aureus (MRSA) was initiated
in Ramsey County. Surveillance was
expanded to include Hennepin County
in 2008. The incidence rate was 15.8
per 100,000 in 2021 compared to 14.8
per 100,000 population in 2020. In 2021,
MRSA was most frequently isolated from
blood (88%, 250/286), and 15% (43/286)
of the cases died in the hospital. HACO-
MRSA cases comprised the majority
(61%, 175/286) of invasive MRSA
infections in 2021, CA-MRSA cases
accounted for 27% (76/286) and 12%
(35/286) cases were HO-MRSA. The
median age for all cases was 50 years
(range, 3 to 98); the median age was 53
(range, 3 to 98), 52 (range, 9 to 89), and
43 (range, 3 to 93) for HO-, HACO-, and
CA-MRSA cases, respectively.
In August 2014, as part of the EIP Active
Bacterial Core surveillance (ABCs)
population-based surveillance of invasive
methicillin-sensitive S. aureus (MSSA)
was initiated in Hennepin and Ramsey
Counties. The incidence rate was 29.5
per 100,000 in 2021 compared to 30.6
per 100,000 population in 2020. In 2021,
MSSA was most frequently isolated from
blood (80%, 425/533), and 11% (60/533)
of the cases died in the hospital. HACO-
MSSA cases comprised the majority
(54%, 291/533) of invasive MSSA
infections in 2021, CA-MSSA cases
accounted for 35% (189/533) and 10%
(53/533) cases were HO-MSSA. The
median age for all cases was 58 years
(range, <1 to 97); the median age was 61
(range, 4 to 97), 54 (range, <1 to 78), and
53 (range, 2 to 97) for HO-, HACO-, and
CA- MSSA cases, respectively.
Vancomycin-intermediate S. aureus
(VISA) and vancomycin-resistant
S. aureus (VRSA) are reportable in
Minnesota, as detected and defined
according to Clinical and Laboratory
Standards Institute approved standards
and recommendations. These
recommendations stipulate a minimum
inhibitory concentration (MIC)=4-8 μg/
ml for VISA and MIC≥16 μg/ml for
VRSA. Patients at risk for VISA and
VRSA generally have underlying health
conditions, such as diabetes and end
stage renal disease requiring dialysis,
previous MRSA infections, recent
hospitalizations, and recent exposure
to vancomycin. There have been no
VRSA cases in Minnesota (MN). There
were no VISA cases reported in 2021.
Between 2008 and 2021, we had 19
VISA confirmed cases: 2008 (3), 2009
(3), 2010 (2), 2011 (5), 2013 (3), 2016
(2) and 2019 (1). Among all cases of
VISA in MN, 11 (58%) were male and the
median age was 64 years (range, 27 to
86). Of those cases with known history
(18), 89% reported recent exposure to
vancomycin.
Streptococcal Invasive Disease
– Group A
Invasive Group A Streptococcus disease
(GAS) is defined as GAS isolated from
a usually sterile site such as blood,
cerebrospinal fluid, or a wound
when accompanied with necrotizing
fasciitis or streptococcal toxic shock
syndrome (STSS). Two-hundred and
fourteen cases (3.8 cases per 100,000
population), including 19 deaths,
were reported in 2021, compared to
271 cases and 20 deaths in 2020. The
median age of cases was 55 years
(range, 6 months to 93 years). Fifty-
five percent of cases were residents
of the metropolitan area. Allowing for
multiple presentations per patient,
105 (49%) had cellulitis, 42 (20%)
bacteremia without another focus
of infection, 30 (14%) septic shock,
29 (13.5%) had septic arthritis and/
or osteomyelitis, 16 (7.5%) abscess
(not skin), 16 (7.5%) pneumonia, and
11 (5%) necrotizing fasciitis. Forty-
three (20%) cases were injection drug
users in 2021, including one death,
compared to 48 cases (18%) and 0
deaths in 2020. Twelve (5.6%) cases
were residents of long-term care
facilities. Ten facilities had a single
case, one facility had 2 cases.
Allowing for multiple infection types
per patient, the 19 deaths included 11
that were diagnosed with septic shock,
11 cellulitis, 2 bacteremia without
another focus of infection, 1 abscess
(not skin), 1 necrotizing fasciitis, 1
pneumonia, and 1 with STSS. Of the 19
deaths, the most frequently reported
underlying conditions were diabetes
(11), chronic kidney disease (7),
atherosclerotic cardiovascular disease
(6), current tobacco smoker (6),
heart failure (5), chronic obstructive
pulmonary disease (4), solid organ
malignancy (3), and obesity (3). Sixteen
fatal cases had two or more underlying
conditions, and 1 had none reported.
Streptococcal Invasive Disease
– Group B
Five-hundred-eighty-four cases of
invasive group B Streptococcus (GBS)
disease (10.3 per 100,000 population),
including 41 deaths, were reported in
2021. By age group, annual incidence
was highest among infants <1 year
of age (49.7 per 100,000 population)
and cases aged ≥70 years (30.1 per
100,000). Nineteen (46%) of the 41
deaths were among cases ≥65 years.
Fifty percent of cases were residents
of the metropolitan area. Bacteremia
without a focus of infection occurred
most frequently (27%), followed by
cellulitis (20%), septic arthritis (10%),
osteomyelitis (9%), septic shock
(9%), pneumonia (6%), abscess (5%),
and meningitis (1%). The majority
(85%) of cases had GBS isolated from
blood; other isolate sites included
joint fluid (9%), peritoneal fluid (3%),
cerebrospinal fluid (<1%), and bone
(<1%).
Thirty-four cases were infants and 4
were maternal cases, compared to
33 cases in 2020. Thirteen infants
developed early-onset disease
(occurred within 6 days of birth [0.2
cases per 1,000 live births]), and 17
infants developed late-onset disease
(occurred at 7 to 89 days [0.3 cases
per 1,000 live births]). One stillbirth/
spontaneous abortion was associated
with the 4 maternal GBS infections.
Since 2002, there has been a
recommendation for universal
prenatal screening of all pregnant
women at 35 to 37 weeks gestation.
In light of this, we reviewed the
maternal charts for all early-onset
cases reported in 2021. Overall, 7
of 13 women who delivered GBS-
positive infants underwent prenatal
screening for GBS. Of these, 2 were
positive and 5 were negative. One
of the 6 women who did not receive
prenatal screening was screened
upon admission to the hospital
prior to delivery and was positive.
Among the 13 women who delivered
GBS-positive infants, 7 received
intrapartum antimicrobial prophylaxis.
An update of GBS perinatal prevention
guidance was published by the
American College of Obstetricians and

DCN 48;1 2022
23
0
20
40
60
80
100
120
1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
Cases per 100,000 Population
Year of Diagnosis
Unknown Serotype
Other Serotypes
Additional Serotypes in PCV-13
Serotypes in PCV-7
PCV-13 contains the 7 serotypes in PCV-7 (4,6B,9V,14,18C,19F, and 23F) plus 6 additional serotypes (1,3,5,6A,7F, and 19A).
Gynecologists, and by the American
Academy of Pediatrics in July 2019.
Streptococcus pneumoniae
Invasive Disease
In 2021, 309 (5.5 per 100,000) cases of
invasive pneumococcal disease (IPD)
were reported. By age group, annual
incidence rates per 100,000 were 7.2
cases among children aged ≤5 years,
1.3 cases among children and adults
aged 5-39 years, 7.9 cases among
adults 40-64 years, and 13.1 cases
among adults aged ≥65 years.
Pneumonia occurred most frequently
(48% of infections), followed by
bacteremia without another focus of
infection (16%), septic shock (11%),
and meningitis (6%). Forty-six (15%)
cases died. Health histories were
available for 45 deaths, of which 40
had an underlying health condition.
The conditions most frequently
reported were current tobacco
smoker (16), diabetes (14), solid organ
Figure 6. Invasive Pneumococcal Disease Incidence Among Children <5 Years of Age,
by Year and Serotype Group, Metropolitan Area
malignancy (10), emphysema/chronic
obstructive pulmonary disease (10),
current alcohol abuse (9), obesity
(9), atherosclerotic cardiovascular
disease/ coronary artery disease (7),
chronic kidney disease (6), and heart
failure (6).
In 1999, the year before the pediatric
pneumococcal conjugate vaccine
(Prevnar [PCV-7]) was licensed, the
rate of IPD among children <5 years
of age in the metropolitan area
was 111.7 cases/100,000. Over the
years 2000-2002 there was a major
downward trend in incidence in this
age group (Figure 6). Rates in each
of the subsequent 8 years were level
or somewhat higher. Based on the
distribution of serotypes among
isolates from these cases, this increase
was limited to disease caused by
non-vaccine serotypes (i.e., serotypes
other than the 7 included in PCV-7)
(Figure 6).
In March 2010, the U.S. Food and Drug
Administration approved a 13-valent
pediatric pneumococcal conjugate
vaccine (PCV-13 [Prevnar 13]) which
replaced PCV-7. This vaccine provides
protection against the same serotypes
in PCV-7, plus 6 additional serotypes
(serotypes 1, 3, 5, 6A, 7F, and 19A).
From 2007 to 2010, the majority of
IPD cases among children <5 years
of age was caused by the 6 new
serotypes included in PCV-13 (Figure
6). Since 2011, the majority of IPD
cases among children <5 years of age
has been caused by serotypes not
included in PCV-13. In 2021, 13% of
cases with isolates available for testing
were caused by 7 of the PCV-13-
included serotypes: 3 (13%), 19F (5%),
19A (2%), 4 (1%), 18C (<1%), and 6B
(<1%).
In August 2014, the Advisory
Committee on Immunization Practices
(ACIP) recommended that all adults
≥65 years receive 1 dose of PCV-
13 followed by 1 dose of 23-valent
pneumococcal polysaccharide vaccine
6 to 12 months later. Among adults
≥65 years, 11% of cases in 2021 had
PCV-13 serotypes.

24
DCN 48;1 2022
0
10
20
30
40
50
60
70
80
90
100
2017 2018 2019 2020 2021
Number of Cases
Sub- Saharan Africa
South/ Southeast Asia
East Asia/ Pacific
Latin America/ Caribbean
Other*
* “Other” includes: Eastern Europe, North Africa/Middle East, and Western Europe
Year of Diagnosis
Figure 7. Non U.S.-Born Tuberculosis Cases by Region of Birth and Year of Report
Toxoplasmosis
Toxoplasmosis is an illness caused by
the coccidian protozoan Toxoplasma
gondii. Cats are the primary reservoir
and definitive host for T. gondii. T.
gondii transmission in the United
States is primarily foodborne,
through handling or consumption
of undercooked pork, lamb, or
venison containing bradyzoites, the
microscopic tissue cyst form of the
parasite. People also can be infected
through direct contact with cat feces
or soil that contains Toxoplasma
oocysts, or though consumption
of food or water that has been
contaminated with oocysts.
In 2021, 7 cases were reported (6
confirmed and 1 probable). This was
similar to the annual median of 9
cases reported from 2013 to 2020
(range, 2 to 14 cases). Fourteen
confirmed cases were identified in
2019 but only 2 confirmed cases
were identified in 2020, likely
reflecting challenges in toxoplasmosis
surveillance resulting from the
COVID-19 response.
In 2021, two cases were diagnosed
with ocular toxoplasmosis, 3 cases
with generalized toxoplasmosis,
and 2 with cerebral toxoplasmosis.
All 7 cases were acquired; no
cases were congenital. There
were no pregnancies reported
among cases. Three cases had
immunocompromising conditions.
The median age of cases was 43
years (range, 36 to 62 years). Five
cases (71%) were male. Two cases
were Asian/Pacific Islander, 1 case
was Black/African American, 1 case
was white, and 3 were of unknown
race; four cases were non-Hispanic, 2
were Hispanic, and 1 was of unknown
ethnicity.
Tuberculosis
In 2021, 134 tuberculosis (TB) cases
(2.4 per 100,000 population) were
reported. This represents a 15%
increase in the number of cases
compared to 2020, when there were
117 newly reported cases. Despite
this rebound in the number of new
cases in 2021, it was still 9% below
the case count in 2019. This followed
a similar trend seen at the national
level, most likely reflecting
lingering effects of the COVID-19
pandemic. This could be due to a
combination of factors, including
delayed diagnosis or misdiagnosis
of TB from shifting resources in
public health and underutilization
of healthcare services, together
with a true decrease in TB
incidence from COVID-19
mitigation strategies during the
pandemic. The TB incidence rate
in Minnesota was the same as the
overall rate in the United States.
Fourteen cases (10%) from 2021
have died as of March 2023, 11
(8%) due to TB disease.
Twenty-six counties (30%)
reported at least one case in 2021.
The majority of TB cases (76%)
occurred in the metropolitan area,
primarily in Hennepin (24%) and
Ramsey Counties (30%). Thirty
cases (22%) were from the other
five metropolitan counties, and
the remaining 24% of cases were
reported from greater Minnesota.
Among metropolitan area counties,
the highest TB incidence rate in
2021 was reported in Ramsey
County (7.3 per 100,000), followed

DCN 48;1 2022
25
by Anoka County (3.6 per 100,000).
The combined TB incidence rate
for the 7-county metropolitan area
was 3.3 per 100,000, compared
to 1.3 per 100,000 for all greater
Minnesota counties.
The largest groups of new TB cases
were those 25-44 and 45-64 years
of age at time of diagnosis (28%
each), followed by cases 65 years of
age and older (20%). Eight patients
(6%) were <5 years of age when
they were diagnosed.
Most TB cases (79%) were
identified only after seeking
medical care for symptoms of
disease. Targeted public health
interventions identified a portion
of the remaining 21% of cases,
including contact investigations
surrounding potentially infectious
patients (9%) and screening of new
refugee arrivals (2%). An additional
6% were identified through
other targeted testing for TB,
including employment screening
and other medical examinations
for immigration purposes. The
remaining five cases (4%) were
diagnosed with active TB disease
incidentally while being evaluated
for another medical condition.
TB incidence is disproportionately
high among racial and ethnic
minorities in Minnesota, as well
as nationally. In 2021, 11 cases
occurred among non-Hispanic
whites, a case rate of 0.2 per
100,000. In comparison, among
non-Hispanic persons of other
races, 56 cases occurred among
blacks/African-born persons (12.8
cases per 100,000), 52 among
Asians or Pacific Islanders (16.5
cases per 100,000), and one case
among American Indian or Alaska
Native persons (1.5 cases per
100,000). Fourteen cases were
Hispanic/Latino persons of any
race (4.4 cases per 100,000). The
majority of Hispanic/Latino (79%),
Asian/Pacific Islander (79%), and
black/African-born cases (96%)
were non-U.S. born.
In 2021, the percentage of TB
cases in Minnesota occurring in
persons born outside the United
States was 81%, compared to 71%
of TB cases reported nationally.
The 108 non-U.S.–born TB cases
represented 33 different countries
of birth; the most common region
of birth among these cases was
Sub-Saharan Africa (50% of non-
U.S. born cases), followed by South/
Southeast Asia (31%), Latin America
(including the Caribbean) (10%),
East Asia/Pacific (8%), and Eastern
Europe (<1%). (Figure 7).
Compared to the percentage of
cases who have lived in areas of the
world where TB is more common,
individuals in other high-risk groups
comprised smaller proportions
of the cases. Note that patients
may fall under more than one risk
category. Fifty percent occurred
in persons with certain medical
conditions (not including HIV/
AIDS), which increase the risk for
progression from latent TB infection
to active TB disease (e.g., diabetes,
COVID-19 infection, active smoking,
prolonged corticosteroid or other
immunosuppressive therapy, end
stage renal disease). One percent
of cases were co-infected with HIV.
Substance use (including excess
alcohol use and/or injection and
non-injection drug use) during
the 12 months prior to their TB
diagnosis was reported by 3% of
cases, and one percent reported
experiencing homelessness during
the 12 months prior to diagnosis.
By site of disease, 65% of cases
had pulmonary disease exclusively.
Another 9% had both pulmonary
and extrapulmonary sites of disease,
and 26% had extrapulmonary
disease exclusively. Among the 47
patients with an extrapulmonary
site of disease, the most common
sites were lymphatic (45%),
followed by peritoneal (19%)
and musculoskeletal (19%).
Extrapulmonary disease is generally
more common among persons
born outside the United States, as
seen in cases reported nationally
as well as in Minnesota. Thirty-
eight percent of non-U.S.–born
cases in Minnesota had at least one
extrapulmonary site of disease,
compared to only 23% of U.S.-born
cases.
Of 94 culture-confirmed TB cases
with drug susceptibility results
available, 10 (11%) were resistant
to at least one first-line anti-TB
drug (i.e., isoniazid [INH], rifampin,
pyrazinamide, or ethambutol),
including 9 cases (10%) resistant
to at least INH. There were 4 new
cases of multidrug-resistant TB
(MDR-TB, or resistance to at least
INH and rifampin) reported in 2021,
making up 4% of culture-confirmed
cases.
Tularemia
Tularemia is an acute illness
caused by Francisella
tularensis subspecies tularensis (type
A) or holarctica (type B). Routes of
transmission include arthropod bites
(particularly ticks and deer flies),
contact with infected animals, and
exposure to contaminated water
or soil. There are six main clinical
forms of disease and all include
fever: ulceroglandular, glandular,
pneumonic, oropharyngeal,
oculoglandular, and typhoidal.
In 2021, one probable glandular
tularemia case was reported. The case
was a 13-year-old female who was
likely exposed through a tick bite.
From 2007 to 2021, 24 tularemia
cases were reported in Minnesota,
with a range of 0 to 6 cases annually.
Twelve cases had ulceroglandular,
7 had glandular, 2 had pneumonic,
and 3 had typhoidal tularemia. Ten
of 15 cases with a known tularemia
subtype had type B, and 5 had type
A. The median age of cases was 40
years (range, 2 to 87 years). Thirteen
cases were likely exposed through a
tick or biting fly bite, 2 through water
exposure, 3 through a cat scratch or
bite, and 2 by inhaling the bacteria;
likely exposures for 3 cases could not
be determined. Sixteen of 20 cases for
whom race was known were White,
1 was Black, 2 were American Indian/
Alaska Native, and 1 was Asian/Pacific
Islander.
Unexplained Critical Illnesses
and Deaths of Possible
Infectious Etiology and Medical
Examiner Deaths Surveillance
MDH conducts surveillance for
unexplained deaths and critical
illnesses in an effort to identify those
that may have an infectious etiology.
This surveillance is performed through
two complementary surveillance
systems, Unexplained Critical Illnesses
and Deaths of Possible Infectious
Etiology (known as UNEX), and Medical
Examiner (ME) Infectious Deaths
Surveillance (known as MED-X), which
is not limited to deaths with infectious
hallmarks. Focus is given to cases
<50 years of age with no significant
underlying conditions; however, any
case should be reported regardless of
the patient’s age or underlying medical

26
DCN 48;1 2022
conditions to determine if further
testing conducted or facilitated
by MDH may be indicated. Testing
of pre-mortem and post-mortem
specimens is conducted by the MDH
Public Health Lab (PHL) and the
CDC Infectious Diseases Pathology
Branch (IDPB).
In 2021, 206 cases met UNEX criteria
(191 deaths,15 critical illnesses),
compared to 131 cases in 2020. Of
the 206, 193 (94%) were reported
by providers and 13 deaths were
found by death certificate review.
One hundred twenty-five (60.5%)
cases presented with respiratory
symptoms; 55 (27%) with sudden
unexpected death; 14 (7%) with
neurologic symptoms; 4 (2%)
with shock/sepsis; 5 (2%) with
gastrointestinal symptoms; 2 (1%)
with cardiac symptoms; 1 (0.5%)
with multiple symptoms. The age
of cases ranged from 8 days to 89
years, with a median age of 47
years. Fifty-one percent resided in
the 7-county metropolitan area,
64% were male, and 16% were
non-MN residents who were either
hospitalized in MN or investigated
by a MN medical examiner.
There were 554 MED-X cases in
2021; 191 of these also met UNEX
criteria. The median age of the
cases was 48.5 years, and 62% were
male. There were 262 (47%) cases
found through death certificate
review and MEs reported 292 (53%)
cases. The most common syndrome
was pneumonia/upper respiratory
infection (n=319 [58%]).
There were 582 potential UNEX or
MED-X cases that had specimens
tested at the PHL and/or the IDPB.
Two hundred and sixty-one cases
were determined to be non-
infectious. One hundred forty-five
cases had pathogens identified as
confirmed, probable, or possible
cause of illness, including 139
UNEX deaths (Table 5). Among 49
unexplained deaths occurring in
those <50 years of age without any
immunocompromising conditions,
UNEX helped to identify the
pathogen(s) involved in 28 (57%)
cases. MED-X surveillance detected
an additional 129 cases with
pathogens identified by MEs as
the cause of death (Table 5). Cases
with pathogens of public health
importance detected included an
84-year-old male who developed
neurologic symptoms 5 months
after being bitten by a rabid bat
Table 5. UNEX/MED-X Pathogens Identified as
Confirmed, Probable, or Possible Cause of Illness, 2021*
Pathogen Identified
UNEX
(n=145)
MED-X
(n=129)**
Aspergillus spp.
0 1
Blastomyces dermatitidis
1 0
Candida albicans
0 1
Clostridioides difficile
0 1
Enterococcus spp.
0 1
Enterococcus faecalis
0 3
Escherichia coli
2 6
Fusobacterium spp.
1 1
Group A Streptococcus/Streptococcus pyogenes
2 2
Group B Streptococcus
1 3
Haemophilus spp.
1 0
Haemophilus haemolyticus
1 0
Haemophilus influenzae
2 1
Histoplasma capsulatum
0 1
Influenza A virus (no hemagglutinin typing information available)
1 1
Influenza A – H3
2 0
Klebsiella oxytoca
0 1
Klebsiella pneumoniae
2 0
Legionella pneumophila
4 0
Metapneumovirus
1 0
Mycobacterium spp.
0 1
Pneumocystis jirovecii
0 1
Powassan virus
1 0
Pseudomonas aeruginosa
0 1
Rabies virus
1 0
Respiratory Syncytial virus
0 2
Rhinovirus
1 0
Rhinovirus/Enterovirus
1 0
SARS-CoV-2 virus
105 86
Staphylococcus spp.
2 0
Staphylococcus aureus
2 6
Staphylococcus aureus - MRSA
4 4
Staphylococcus epidermiditis
0 1
Streptococcus spp.
7 0
Streptococcus anginosus
1 0
Streptococcus pneumoniae
10 8
Ureaplasma spp.
1 0
* Some cases had multiple pathogens identified as possible coinfections contributing to illness/death.
** MED-X includes pathogens identified by the Medical Examiner. If the cause was found through testing at
MDH/CDC it is included in the UNEX column.

DCN 48;1 2022
27
and received appropriate rabies
post exposure prophylaxis (PEP). An
autopsy revealed meningoencephalitis
consistent with rabies virus and
postmortem samples submitted to IDPB
and the CDC Rabies Branch confirmed
the presence of rabies virus. This case
represented the first documented
rabies PEP failure since the introduction
of modern cell-culture vaccines and
was contributed to the patient having
previously unrecognized impaired
immunocompromising condition.
The UNEX program also identified102
deaths due to SARS-CoV-2 virus
that occurred outside of traditional
healthcare facilities such as hospitals or
congregate care settings.
Due to the COVID-19 pandemic,
the UNEX/MED-X team expanded
surveillance testing to include swab
autopsies that were performed on
suspect infectious deaths that did not
have an autopsy performed. Nasal
pharyngeal swabs were collected
from decedents at funeral homes,
decedents’ homes and at long-term
care facilities. A total of 52 specimens
were submitted to MDH. 43 decedents
had known symptoms prior to death.
Of those, 25 (58%) had potential
pathogens detected, including SARS-
CoV-2 (n=24) and influenza A (n=1).
Varicella and Zoster
In 2021, 169 varicella cases were
reported (3.0 per 100,000 population).
Ninety-seven cases (57%) were from
the metropolitan area. Case ages
ranged from 95 days to 69 years.
Thirty-two cases (19%) were < 1 year,
73 (43%) were 1-6 years, 36 (21%) were
7-12 years, 10 (6%) were 13-17 years,
and 18 (11%) were ≥ 18 years of age.
Four cases were hospitalized; 1 was <
1 year, one was 1-6 years, and 2 were
>18 years. Two of the hospitalized
cases had not been vaccinated; one
had medical contraindications and
one was underage for vaccination. The
vaccination status of the other two
hospitalized cases was not available.
Varicella cases are often identified by
parents/guardians reporting to schools
and childcare facilities, rather than
directly reported by a clinician. In 2021,
108 cases (64%) had visited a health
care provider, 21 (12%) had consulted
a provider or clinic by telephone, 16
(10%) had been identified by a school
health professional, and 24 (14%) had
not consulted a health care provider.
Of the 168 cases for which information
regarding laboratory testing was
available, 64 (38%) had appropriate
testing performed.
One outbreak, defined as ≥5 cases
in the same setting, was reported in
2021. This occurred in an infant room
at a daycare center and included 5
cases, 4 of which were unvaccinated
due to being underage (first dose
recommended at age 12-15 months).
Zoster cases in children <18 years of
age are reportable in Minnesota; 34
cases were reported in 2021. Cases
may be reported by school health
personnel, childcare staff, or healthcare
providers. Ages ranged from 10 months
to 16 years (median 11 years). Varicella
vaccine became a requirement for
entry into kindergarten and 7th grade
in 2004, and the incidence of zoster
in children has declined from 15.7 per
100,000 population in 2006 to 2.6 per
100,000 population in 2021.
Zoster with dissemination or
complications (other than post-
herpetic neuralgia) in persons of
any age is also reportable; 56 such
cases were reported, and 44 (79%)
were hospitalized. Cases ranged
from 2 to 94 years of age, with a
median age of 60. Thirty-seven (66%)
had co-morbidities or were being
treated with immunosuppressive
drugs. Fourteen had disseminated
rash or disease, 17 had meningitis,
11 had cellulitis or other bacterial
superinfection, 8 had encephalitis, 3
had meningoencephalitis and 7 had
Ramsay-Hunt Syndrome. Cases with
disseminated rash or disease tended
to be older than cases with meningitis
without dissemination (median age of
63 vs. 43 years) and were more likely to
have immunocompromising conditions
or immunosuppressive drug treatment
(64% vs. 27%). Five deaths occurred;
two had encephalitis, two had
meningoenchephalitis, and one had
meningitis and Ramsay Hunt Syndrome.
All deaths were in cases > 65 years.
Only 19% of cases ≥50 years of age had
a record of receiving zoster vaccine.
Vibriosis
There were 91 Vibrio spp. (several
species) cases reported in 2021. Of
those, 24 were culture-confirmed and
67 were positive by culture-independent
diagnostic tests (CIDT) and not
subsequently culture-confirmed.
The 24 culture-confirmed cases of
Vibrio spp. infection reported in 2021
represent a 71% increase from the
14 cases reported in 2020, and a 20%
increase from the median annual
number of cases reported from 2010 to
2020 (median, 20 cases; range, 9 to 40).
V. parahaemolyticus accounted for 12
(50%) cases, V. alginolyticus, V. cholerae,
and V. fluvialis for 3 (13%) each, and V.
vulnificus for 1 (4%). Two isolates were
not received by the MDH Public Health
Laboratory for confirmation and species
identification. Serotyping was performed
on all three V. cholerae specimens, and
all were non-O1/non-O139.
Vibrio was isolated from stool in 16
(67%) cases, wounds in 3 (13%) cases,
blood in 2 (8%) cases, ear effusion in
2 (8%) cases, and urine in 1 (4%) case.
Three (13%) cases were hospitalized
for a median of 3 days (range, 1 to 4
days), and one case died.Travel history
was available for 21 cases. Fourteen
(67%) cases traveled out of Minnesota
in the week before their symptom
onset, including five (24%) who traveled
internationally. Two cases traveled
to Mexico, and one case each to the
Bahamas, Egypt, and Somalia. Of the
16 cases with Vibrio isolated from
stool who were able to be interviewed
about exposure to seafood in the week
before illness onset, 10 (63%) reported
consuming oysters. Of the remaining
six cases, three had other raw or
undercooked seafood.
In 2021, 74 patients were positive by
CIDTs conducted at a clinical laboratory.
Of these 67 (91%) were not culture-
confirmed and thus were classified as
probable cases. Eight (12%) specimens
were not received by the public health
laboratory for culture confirmation.
Fifty-nine (79%) were received at MDH
and tested negative by culture. Fifteen
(22%) probable cases were hospitalized
and two (3%) died.
Ten (19%) of the 53 probable cases
who were interviewed traveled
outside Minnesota, and five (9%)
traveled internationally (one each
to Cameroon, France, Mexico, New
Zealand, and Somalia). Among the 43
probable cases interviewed about food
exposures, three (7%) reported eating
raw oysters, and three (7%) reported
eating another type of raw seafood in
the week prior to illness onset. Thus,
probable cases differed markedly from
culture-confirmed cases regarding
exposures, suggesting a high proportion
of CIDT-positive tests represented false
positives.
There were no outbreaks of Vibrio spp.
infections identified in 2021.

Brooke Cunningham, Commissioner of Health
Division of Infectious Disease Epidemiology, Prevention and Control (IDEPC)
Beth Gyllstrom, PhD, MPH ............................................................................................................ Editor
Ruth Lyneld, M.D. ................................................................................................ State Epidemiologist
Elly Pretzel ........................................................................................................................... Producon
The Disease Control Newsletter is available on the MDH IDCN web site:
(http://www.health.state.mn.us/divs/idepc/newsletters/dcn/index.html)
Viral Hepatitis A
In 2021, 12 cases of hepatitis A
(0.2 per 100,000 population) were
reported. Ten cases were residents of
the metropolitan area. Six cases were
male. The median age was 33.5 years
(range 3 to 85). Race was known for all
cases; 9 (75%) were white, one (8.3%)
was Asian, and two (16.7%) were
reported as other race. Three (25%)
cases were known to be of Hispanic
ethnicity.
Ongoing outbreaks of hepatitis A
have been occurring in states across
the country since 2016, with at least
37 states reporting outbreaks. An
outbreak was declared in Minnesota in
August 2019 and 1 case was identified
as a part of the outbreak in 2021.
This case did not report risk factors,
but traveled to states with ongoing
outbreaks. The end of the Minnesota
outbreak was declared in September
2021. There were a total of 128 cases
identified over the course of the
outbreak. Of these cases, 89 (70%)
were hospitalized and there was one
death.
Of the 11 cases not associated with the
outbreak, 6 cases were associated with
international travel and two cases are
presumed to be a result of foodborne
exposure. No risk factor was identified
for the three remaining cases.
Viral Hepatitis B
In 2021, 10 cases of acute hepatitis
B virus (HBV) infection (0.2 per
100,000 population) were reported.
In 2012, the case definition for acute
hepatitis B was revised to include
laboratory confirmed asymptomatic
acute cases. Five of the 10 cases were
asymptomatic, laboratory-confirmed
infections.
The median age was 43 years (range
21 to 72). Six cases were residents of
the metropolitan area. Six cases were
male. Race was known for 9 cases:
four (44%) were White, one (11%)
was Asian, two (22%) were Black, one
(11%) was reported as multi-racial, and
one (11%) was reported as other race.
One (10%) case was known to be of
Hispanic ethnicity.
MDH received 190 reports of newly
identified chronic hepatitis B infections
in 2021. A total of 27,464 persons
are estimated to be alive and living in
Minnesota with chronic HBV infection.
The median age of chronic HBV cases
in Minnesota is 48 years.
In 2021, no perinatal hepatitis B
infections were identified in infants
born to hepatitis B-positive mothers.
Three hundred and six infants born
to hepatitis B-positive women during
2020 had post-serologic testing
demonstrating no infection.
Viral Hepatitis C
In 2021, 66 cases of acute hepatitis C
virus (HCV) infection (1.2 per 100,000)
were reported. In 2012, the case
definition for acute hepatitis C changed
to include documented asymptomatic
seroconversion. Of the 66 cases, 25
(38%) were asymptomatic, laboratory-
confirmed acute infection.
Fifty (76%) were residents of the
metropolitan area. The median age was
32 years (range, 18 to 66). Thirty-nine
(59%) cases were male. Race was known
for 61 cases: 29 (48%) were White, 18
(30%) were American Indian/Alaskan
Native, 7 (11%) were Black, one (2%)
was Asian, three (5%) were reported
as multi-racial, and three (5%) were
reported as other race. Six (10%) cases
were known to be of Hispanic ethnicity.
MDH received 1,049 reports of newly
identified chronic hepatitis C infections
in 2021. In 2016, the case definition for
chronic hepatitis C changed to exclude
those reported as having resolved their
infection. A total of 32,810 persons
are estimated to be alive and living in
Minnesota with chronic HCV infection.
The median age of these cases is 60
years.
In 2018, perinatal hepatitis C was added
as a nationally notifiable condition. In
2021, one case of perinatal hepatitis C
was reported. This case was known to
be White, non-Hispanic.
