1
FRED HUTCHINSON CANCER CENTER
December 20, 2023
LONG-TERM FOLLOW-UP AFTER HEMATOPOIETIC STEM CELL TRANSPLANT
GENERAL GUIDELINES FOR REFERRING PHYSICIANS
These guidelines and the information they contain are copyrighted material of Fred Hutchinson
Cancer Center (“Fred Hutch”), all rights reserved. They are intended solely for the use of
referring physicians who are involved in the care of patients who have had an hematopoietic
stem cell transplant at Fred Hutch. They may not be used for any other purpose, and Fred Hutch
disclaims all liability for the use of these guidelines except as expressly permitted by Fred Hutch.
No portion of these guidelines may be copied, displayed for redistribution to third parties for
commercial purposes or for any non-permitted use without the prior written permission of Fred
Hutch.
These guidelines describe generally accepted practices for medical care after hematopoietic stem
cell transplantation. Care has been taken to assure that the information in these guidelines is
current and accurate based on the available literature and the experience of physicians and
patients at Fred Hutch. Recommendations in these guidelines must be implemented in a
medically reasonable way that accounts for the specific situation of the individual patient.
Recommendations for patients who are enrolled in specific protocols may differ from the
recommendations in these guidelines and will be communicated separately. Questions
concerning the recommendations in these guidelines or their application to particular patients
should be directed to the LTFU office. See Section I of the guidelines for information on how to
contact the LTFU office.
Contributions to these updated guidelines were made by: Paul Carpenter, M.D.; Michael Boeckh,
M.D.; Joachim Deeg, M.D.; Guang-Shing Cheng, MD; Jean Stern, M.S.R.D.; and Leona
Holmberg, M.D., P.H.D.

2
TABLE OF CONTENTS
Page
I. How to Contact the LTFU Office at Fred Hutch 5
II. Frequency of Office Visits 6
III. Laboratory Tests 7-9
A. Complete Blood cell counts
B. Liver function tests
C. Renal function tests
D. Drug levels
E. Fasting Lipids Profile
F. Thyroid Function in Blood
G. Blood cultures
H. CMV monitoring
I. CMV, EBV and Adenovirus monitoring after treatment with ATG (ATGAM or
Thymoglobulin)
J. Disease monitoring of Blood and Bone marrow
IV. Infections Prophylaxis, Pre-emptive Therapy, and Intravenous Immunoglobulin 10-22
A. Pneumocystis carinii
B. Varicella zoster
C. Encapsulated bacteria
D. Cytomegalovirus
E. Fungal organisms
F. Intravenous immunoglobulin (IVIG and CMV IG)
V.Fever of Unknown Etiology 23
VI. Evaluation of Respiratory Problems and Lung Infiltrates 24-26
A. Diagnostic evaluation
B. Bronchoalveolar lavage (Tests recommended for BAL and transbronchial biopsy specimens)
C. Thoracoscopic lung biopsy (Evaluation of pulmonary nodules or persistent infiltrates with negative BAL)
VII. Evaluation of Diarrhea and Other GI Problems 27-29
A. Diagnostic evaluation and initial management
B. Procedures for gastrointestinal endoscopic biopsy
C. Algorithm for Evaluation of Acute Onset Diarrhea in Transplant
VIII. Treatment of Specific Infections 30-31
A. Cytomegalovirus
B. Varicella zoster
C. Pneumocystis carinii
IX. Vaccinations 32-41
3
X.Chronic Graft-Versus-Host Disease (GVHD) 42-52
A. Categories of acute and chronic GVHD (Table 1)
B. Signs and symptoms of chronic GVHD (Table 2)
C. How to diagnosis chronic GVHD
D. How to score each organ/site affected by chronic GVHD (Appendix D)
E. How to assess overall severity of chronic GVHD – Global assessment of
chronic GVHD severity (Table 3)
F. Other Laboratory testing and diagnostic indicators used in chronic GVHD
G. Monitoring and other chronic GVHD information
H. Guidelines for treatment of chronic GVHD
I. Monitoring and Management of Bronchiolitis Obliterans Syndrome after HCT
XI. General Guidelines for Prevention of Osteoporosis and Glucocorticosteroid Induced
Osteoporosis 53-59
A. Patient monitoring
B. Elemental Calcium requirements
C. Vitamin D requirements
D. Magnesium
E. Exercise
F. Gonadal hormone replacement
G. Other treatments
1. Bisphosphonates
2. Rank Land Inhibitors
3. Calcitonin
4. Low Sodium Diet
5. Endocrinology
XII. Hyperlipidemia 60-66
XIII. Hypertension 67-70
XIV. Recurrent Malignancy 71
XV. Secondary Malignancies 72
XVI. Other Complications 73-84
A. Gonadal hormone insufficiency
B. Endocrine abnormalities
C. Ocular complications
D. Oral complications and guidelines for dental care
E. Renal insufficiency
F. Neurological complications
G. Bone complications
H. Chronic Pulmonary complications
I. Hepatobiliary complications
J. Gastrointestinal complications
XVII. Blood Product Transfusion 85
4
XVIII. Viral Hepatitis 86-88
A. Hepatitis B
B. Hepatitis C
XIX. Iron Overload 90-98
A. Evaluation of iron overload after HSC Transplant
B. Phlebotomy after transplant
C. Chelation therapy
XX. Vitamins, Mineral Supplements 99-101
A. Calcium and Vitamin D
B. Magnesium
XXI. Diets and Other Nutritional Guidelines 102-104
A. Diet for immunosuppressive patients
B. Additional dietary recommendations
1. Diet for patients receiving treatment with corticosteroids
2. Diet for patients with GVHD of gastrointestinal tract
XXII. Naturopathic (Herbal and Nutrient supplement preparations) 105
XXIII. Return to Seattle for Long-Term Follow-Up Evaluation 106
XXIV. How to Send Specimens for Testing at Fred Hutch 107
XXV. References 108-112
APPENDICES
A. FAX Consult Request 114
B. LTFU Alert 115
C. Skin Assessment Form 116
D. Chronic GVHD Scoring Form 117-119
E. Skin Thickness Assessment (patients with scleroderma) 120
F. Flexibility 121

5
I. HOW TO CONTACT THE LONG-TERM FOLLOW-UP OFFICE AT THE FRED
HUTCHINSON CANCER CENTER
We offer telephone consultation to all physicians caring for patients who have been
transplanted at the Fred Hutchinson Cancer Center (Fred Hutch). We have developed a
Consultation FAX form (Appendix A) in order to facilitate communication between your
office and the LTFU office. This form can be filed in your medical records and sent to 1-
800-376-8197 (toll-free, USA and Canada) whenever you need assistance. All efforts will be
made to respond within 48 hours on regular workdays. For urgent questions from 8:00 a.m.
to 4:00pm Pacific Time on workdays, you can call (206) 667-4415. For urgent questions after
hours and on weekend and holidays, please call (206) 606-7600 and ask for the transplant
charge nurse. The nurse will triage the call and page the appropriate physician to assist you.
For non-urgent inquiries, you may also contact our LTFU Office at [email protected].
Please include the patient identification and your phone number to contact you back.
Information about LTFU services can be accessed on our website at;
http://www.fhcrc.org/science/clinical/ltfu/contact.html .
You can also find us on Google by typing FHCRC.LTFU, then clicking in the "Information
for Physician" in the left hand navigation column.
We also request that you notify us immediately after certain types of events. We have
developed an LTFU Alert FAX form in order to facilitate the notification from your office to
the LTFU office (Appendix B). This form can be filed in your medical records and sent to
1-800-376-8197 (toll-free, USA and Canada) to report the following events:
1. Death of the patient
2. Diagnosis or change in therapy of chronic GVHD
3. Recurrent malignancy
4. Diagnosis of myelodysplasia or secondary malignancy
5. Surgery or biopsy planned for evaluation of suspected secondary malignancy
6. Change of M.D.
7. Change of M.D. office address
8. Change of patient name or address
9. Requests from patients that we refrain from contacting them
6
II. FREQUENCY OF OFFICE VISITS
After returning home, hematopoietic transplant patients should be followed with weekly office
visits for one month. The interval time between visits can be extended to 2 weeks for 2 months
and then monthly for 6-12 months if the patient's medical condition remains stable. Vital signs
and body weight should be monitored at each clinic visit. Weight and height should be recorded
at monthly intervals for assessment of growth and development in pediatric patients. Patients
who have had an allogeneic hematopoietic stem cell transplant should be monitored for
development of chronic graft-versus-host disease (GVHD). Helpful tips on how to assess and
score chronic GVHD can be found at http://www.fhcrc.org/ltfu by clicking on "Information for
Physicians" in the left hand navigation column. Then click on the right blue “GVHD Tips &
Forms" button. Here you will find the Chronic GVHD Assessment and Scoring form (Appendix
D), Range of Motion Assessment form (Appendix F), Skin Thickness Assessment form/ Rodnan
Score for patients with sclerosis or fasciitis (Appendix E) and other helpful information. More
detailed information about chronic GVHD is outlined in Section X.
If manifestations of chronic GVHD develop or worsen, please contact the LTFU office
(Appendix A).

7
III. LABORATORY TESTS
A. Complete blood cell counts (CBC), differential and platelet counts should be measured at
each office visit. Patients receiving ganciclovir (or ValGANCiclovir), daily
Trimethoprim/Sulfamethoxazole (TMP/SMX), Cellcept (mycophenolate mofetil), and other
myelosuppressive medication should have a CBC at weekly intervals or more often when
counts are low.
B. Liver function tests (LFT's) (alkaline phosphatase, ALT, AST, LDH and total bilirubin)
should be measured at each office visit. Patients receiving immunosuppressive medications
or other hepatotoxic drugs such as itraconazole, voriconazole, INH, should have LFT's
measured at two-week intervals or more often when abnormalities are present. If drug
toxicity suspected, blood levels should be checked if available.
C. Renal function tests (serum creatinine, BUN, and magnesium) should be measured at each
office visit. Patients receiving cyclosporine, tacrolimus (formerly known as FK506),
amphotericin or other nephrotoxic drugs should have renal function monitored at weekly
intervals or more often when abnormalities are present. Dose adjustment may be needed for
medications such as cyclosporine, tacrolimus, ganciclovir, valacyclovir, acyclovir, among
others.
D. Drug levels:
Cyclosporine or tacrolimus (FK506) blood levels should be monitored at least twice monthly
until levels remain stable within the therapeutic range. Sirolimus (rapamycin) should be
monitored weekly until levels remain stable within levels maintained no higher than 10
ng/dL). Sirolimus, cyclosporine or tacrolimus (FK506) levels should be checked more
frequently when toxicity is suspected (i.e., new onset of thrombocytopenia, worsening
anemia, abnormal renal function, abnormal LFT's, development of tremors or other
neurological symptoms), when blood levels are outside the therapeutic range or when
manifestations of GVHD is not under control.
Note: If patients is on immunosuppressive therapy like Cyclosporine, Tacrolimus, or
Sirolimus with Maribavir because of drug-drug interaction, check two times per week
immunosuppressive drug levels for the first two weeks at start of Maribavir and for two weeks
after stopping of Maribavir. Otherwise, monitor immunosuppressive drug levels at least once
a week or as clinically indicated. Adjust immunosuppressive drug dose as needed.
Itraconazole blood levels should be monitored at monthly intervals until levels remain stable
within the therapeutic range. Itraconazole levels should be checked more frequently when
results are outside the therapeutic range and when results of LFT's are abnormal. Voriconazole,
posaconazole and the other azoles should be used with caution during treatment with sirolimus.
If treatment with azoles is warranted please contact the LTFU office to discuss sirolimus dose
adjustment.
E. Fasting lipids profile is recommended periodically due to increased risk of cardiovascular
disease and increased risk of metabolic syndrome in transplant survivors. In patients receiving
sirolimus, tacrolimus or cyclosporine, monthly fasting lipids profile is recommended until
acceptable values are achieved, thereafter, monitoring may be decreased to every 3 to 6
months, or more often if clinically indicated.

8
F. Thyroid function in blood should be monitored yearly due to increased thyroid disease
after transplant. For patients who received radiolabeled iodine antibody therapy, thyroid
function should be checked sooner at 3 and 6 months within the first year after transplant,
and other times as clinically indicated.
G. Blood cultures should be drawn whenever clinically indicated. For high risk patients
(i.e., treatment with prednisone at a dose of more than 1 mg/kg/day), weekly surveillance
blood cultures may be beneficial.
H CMV monitoring in blood should be instituted for all patients who are at risk of CMV
disease after transplant. PCR is the standard assay for CMV surveillance.
Initial CMV Monitoring
CMV seropositive recipients of non-cord blood allogeneic transplants or CD34 selected
autologous transplants should have CMV monitored in blood weekly until day 100 after
transplant. CMV seropositive cord blood recipients should have CMV monitored twice
weekly until day 100 after transplant. CMV seronegative recipients of cord blood should
have CMV monitored weekly until day 100 days after transplant. CMV
seronegative/seronegative non-cord blood allogeneic or seronegative unmodified
autologous transplant recipients should be monitored weekly until day 60 after transplant.
After day 100 to one year post transplant, CMV monitoring
CMV blood testing should be continued, initially weekly, until 1 year after transplant for
allogeneic recipients at risk of late CMV disease which include:
• Patients treated for CMV viremia in the first 100 days after transplantation
• Cord blood transplant recipients who were CMV seropositive
• Patients who received Letermovir prophylaxis beyond day +60 after transplant
• For non-malignant patients except Sickle cell and Thalassemia that received either Anti-
Human Thymocyte Globulin or Campath in transplant conditioning or for GVHD should
have weekly CMV blood testing for at least 6 months after the last serotherapy dose or
until absolute CD4 count is > 200 cells/microliters, whichever is later
• All other patients who received Anti-Human Thymocyte Globulin in conditioning or for
GVHD should have weekly CMV blood testing for at least 6 months after the last dose of
ATG or absolute lymphocyte count >300 cells/microliters, whichever is later (see Section
I)
• Patients treated with > 0.5 mg/kg/day prednisone or prednisone equivalent or other agents (e.g.,
MMF, ibrutinib, etc.) for either late acute or chronic GVHD.
Changes in initial surveillance frequency > 100 days after transplant and before one
year post transplant for NON-CORD BLOOD transplant patients:
The weekly frequency of CMV blood surveillance after day 100 posttransplant may be
changed for non-cord blood transplant ONLY as follows:
• Non-Cord Blood patients can be changed to every other week surveillance if on < 0.5
mg/kg/day prednisone or prednisone equivalent and on stable doses or tapering doses of other
immunosuppressive agents AND have had three consecutive negative surveillance tests (PCR
for CMV DNA)
• Surveillance may be stopped entirely after 2 additional negative tests if tapering of
immunosuppression continues.
• Resume weekly CMV surveillance testing if treatment with immunosuppression is increased or
re-initiated for GVHD.

9
CMV monitoring after one year post transplant
CMV monitoring as clinically indicated based on history of prolonged CMV prophylaxis,
repeated episodes of CMV reactivation, or ongoing active GVHD requiring systemic
immunosuppressive therapy.
I. CMV, EBV and Adenovirus Monitoring After Treatment with Anti-Human Thymocyte
Globulin (ATG) (ATGAM or Thymoglobulin) Unless Specified Differently per Protocol
• For non-malignant patients except sickle cell and Thalassemia that received either Anti-
Human Thymocyte Globulin or Campath in transplant conditioning or for GVHD should
have weekly blood monitoring by PCR for EBV, adenovirus, and CMV for at least 6
months after the last serotherapy dose or until absolute CD4 count is > 200
cells/microliters, whichever is later.
• All other patients who received Anti-Human Thymocyte Globulin in conditioning or for
GVHD should have weekly blood monitoring by PCR for EBV, adenovirus, and CMV
for at least 6 months after last dose of ATG or absolute lymphocyte count > 300 cells/
microliter, whichever is later.
J. Disease Monitoring of Blood and Bone marrow.
Bone Marrow:
Bone marrow should be evaluated at one year after transplant. Testing should include
evaluation of morphology and immunophenotyping, cytogenetics and molecular testing
as applicable. Subsequent bone marrow evaluations should be done as clinically
indicated such as:
• The CBC or platelet count shows any abnormalities
• If the most recent marrow evaluation or other testing showed any evidence of
persistent malignancy
• If the patient has a disease for which maintenance treatment would be indicated if
disease were discovered after a previous evaluation with no evidence of malignant
cells.
Blood:
Patients transplanted for chronic myeloid leukemia (CML) or Philadelphia chromosome-
positive acute lymphocytic leukemia (Ph-positive ALL) should have blood tested for
BCR/abl transcripts at 6 month intervals for the first 2 years after transplant and then at
yearly intervals. When BCR/abl transcripts are detected in the blood, a marrow aspirate
should be evaluated by cytogenetic testing, morphology and molecular testing.
If recurrent malignancy occurs, please contact the LTFU office for consultation for
specific treatment and follow-up recommendations (Appendix A).

10
IV. INFECTIONS PROPHYLAXIS, PREEMPTIVE THERAPY AND INTRAVENOUS
IMMUNOGLOBULIN
All transplant recipients have some degree of immunodeficiency, especially during the first
6-12 months after the transplant. Bacterial, fungal and viral infections occur most frequently
during this time interval. In the absence of GVHD, most patients have adequate immune
reconstitution by one year after the transplant. Patients with chronic GVHD remain
immunodeficient and have a high risk of infections.
A. Pneumocystis jiroveci pneumonia (PCP)
All patients should receive prophylaxis against PCP for at least 6 months after the
transplant or until all immunosuppressive medications have been discontinued, whichever
occur later. The preferred drug is trimethoprim-sulfamethoxazole administered according
to the following regimen:
• Adults: 1 double strength tablet p.o. b.i.d. on 2 consecutive days weekly
• Children > 20 kg: 1 single strength tablet p.o. b.i.d. on 2 consecutive days weekly
• Children < 20 kg: and 5 mg/kg/day of trimethoprim component in two divided doses on
2 consecutive days weekly.
Patients who are allergic to sulfa should be desensitized whenever possible. If
desensitization is not feasible, Dapsone should be administered at a dose of 50 mg p.o.
b.i.d. daily for adults and 1 mg/kg/day in two divided doses (up to 100 mg/day) for
children. Before starting treatment with Dapsone, patients must be tested to rule out G-6-
PD deficiency. For patients who cannot tolerate Bactrim or dapsone, atovaquone or
pentamidine IV may be given.
Atovaquone:
Dosing
Adults and pediatric patients > 50 kg:
1500 mg oral suspension, once daily, to be taken with a meal.
Pediatric patients less than or equal to 50 kg:
30 mg/kg, once daily, to be taken with a meal.
Pentamidine
Dosing
Pediatric:
Children < 24 months:
4 mg/kg/dose (max 300 mg) IV over 90 minutes every two weeks.
Children > 2 years:
4 mg/kg/dose (max 300 mg) IV over 90 minutes every four weeks.
Adult:
300 mg IV over 90 minutes, every four weeks.

11
B. Varicella-zoster virus
All VZV-seropositive patients (via vaccine or via disease) should receive prophylaxis
with acyclovir or valacyclovir throughout the first year after the transplant or until 8
months after systemic immunosuppression ends, whichever is longer.
Acyclovir should be administered according to the following regimen (assuming
adequate renal function):
• Weight > 40 kg, receiving < 0.5 mg/kg/day of corticosteroids: 800 mg P.O. B.I.D.*
• Weight < 40kg, receiving < 0.5 mg/kg/day of corticosteroids: 600 mg/ m
2
P.O. B.I.D.
Alternatively, valacyclovir should be administered according to the following regimen:
• Weight > 40 kg, receiving > 0.5 mg/kg/day of corticosteroids: 500 mg P.O. B.I.D*.
• Weight < 40 kg, receiving > 0.5 mg/kg/day of corticosteroids: 250 mg P.O. B.I.D.
*Note: In VZV seropositive/HSV seronegative, patients > 40 kg, lower doses of prophylaxis
are sufficient, 800 mg/day of acyclovir or 500 mg/day of valacyclovir. For patients < 40 kg,
the dose of acyclovir should be 300 mg/m
2
(maximum 400 mg) P.O. B.I.D.
It is difficult to prevent VZV transmission to susceptible patients because infected
individuals are contagious for 24-48 hours before the rash appears. The incubation period
of VZV is 10-21 days. Individuals with VZV (chickenpox or shingles) remain contagious
until all skin lesions have crusted.
All patients exposed to chickenpox or zoster during the first year after the transplant or
during treatment with immunosuppressive medications should be evaluated. VZV-
seronegative patients and those not receiving prophylactic acyclovir should be treated
with valacyclovir from days 3 to 22 after exposure unless treatment with ganciclovir,
foscarnet or cidofovir is being given for another reason. Valacyclovir should be given at
a dose of 1gm p.o. t.i.d. for patients > 40 kg and at a dose of 500 mg p.o. t.i.d. for patients
< 40 kg. In adults and children without adequate oral intake, acyclovir can be
administered at a dose of 500mg/m
2
IV every 8 hours if renal function is normal. In
seronegative recipients, administration of VZIG within 96 hours of exposure should also
be used, if available, in addition to valcyclovir as outlined above. Patients exposed to
chickenpox or zoster during prophylaxis with acyclovir or valacyclovir must be followed
closely for the development of VZV infection.
Vaccination against VZV should be delayed (See vaccination Section IX for details).
C. Encapsulated bacteria
Patients with chronic GvHD are highly susceptible to recurrent bacterial infections,
especially with encapsulated bacteria such as Streptococcus pneumoniae, Haemophilus
influenzae and Neisseria meningitidis as they are functionally asplenic. Susceptibility to
these organisms may be due to persistent low levels of opsonizing antibodies, low CD4
counts, poor reticuloendothelial function, and long-term use of immunosuppressive
therapy, especially corticosteroids, with their suppressive effects on

12
Encapsulated bacteria (continued)
phagocytosis. Long-term chemoprophylaxis is recommended in this setting due to
unpredictable protection provided by vaccination, which is also recommended after
transplant. Due to the emergence of penicillin resistance (and the concomitant need for
PCP prophylaxis in these patients), trimethoprim-sulfamethoxazole (TMP-SMX) is
recommended as first-line drug for chemoprophylaxis for infections with encapsulated
bacteria. If TMP-SMX is not tolerated, the traditional penicillin-based prophylaxis
should be substituted for encapsulated bacteria and dapsone also should be prescribed to
provide PCP prophylaxis.
Other patient groups who should be considered for encapsulated organism prophylaxis
include those who are:
• Without GVHD but are receiving glucocorticoid or other immunosuppressive
medications.
• With persistent or recurrent manifestations of chronic GVHD without ongoing use of
immunosuppressive medications
• Being treated for relapsed or progressive malignancy after transplant
• Surgically and/or functionally asplenic (see below for more details).
• Patients who are age> 65 years old post-allogeneic stem cell transplantation.
Patients receiving systemic immunosuppressive therapy for chronic GVHD should
receive antibiotic prophylaxis against infection with encapsulated bacteria for at least 6
months after discontinuation of all immunosuppressive medications. Double-strength
(DS) trimethoprim-sulfamethoxazole (800mg sulfamethoxazole) given as a single dose
daily is adequate for prevention of infection with both PCP and encapsulated bacteria in
adults.
In patients with sulfa allergies, Penicillin VK (Pen-Vee-K) should be given for
encapsulated bacteria prophylaxis (see Table below). Children < 30 kg who do not
tolerate daily trimethoprim-sulfamethoxazole (TMP/SMX) should receive Penicillin VK
(See Table below).
Additional medication is required for PCP prophylaxis in patients who receive
penicillin instead of daily trimethoprim-sulfamethoxazole (TMP/SMX). (See Section
IV.A)
Table - Penicillin VK dosing for encapsulated bacterial prophylaxis:
Adults and Children ( > 60 kg)
500 mg PO BID
Adults ( < 60 kg) and
Children (> 3 years and < 60 kg)
250 mg PO BID
Children (< 3 years)
125 mg PO BID

13
For more information, see the Standard Practice Guideline section “Antibiotic
Prophylaxis for Encapsulated Bacteria in Allogeneic Patients with Chronic GVHD
Requiring Immunosuppressive Therapy”
Antimicrobial prophylaxis for asplenic patients
Patient education is paramount to prevent fatal infections in asplenic patients. Studies
have shown that 11% to 50% of postsplenectomy patients remain unaware of their
increased risk for serious infection or the appropriate health precautions that should be
undertaken. Important education points include the following:
• Persons without a functioning spleen are more susceptible to certain infections.
• The risk of infection is life-long, but it is highest in the first year or two after the
surgery.
• If unwell (particularly in case of fever associated with rigors), patients should seek
prompt medical attention. Infections can be rapidly progressive and life-
threatening in a matter of hours. The use of prophylactic or preemptive measures
should never be allowed to engender a false sense of security.
• Travel-related infections (such as babesiosis and malaria) are particularly important;
adherence to antimalarial prophylaxis cannot be overemphasized.
• All physicians caring for the patient should be informed of the condition, no matter
how long after the splenectomy.
Antimicrobial regimens are the same as for prevention of encapsulated bacteria in patients
with chronic GVHD, and include daily Trimethoprim/Sulfamethoxazole (TMP/SMX) or
twice-daily Penicillin VK therapy. Penicillin VK provides no protection against PCP; thus
dapsone or other PCP prophylaxis must be added.
The duration of antibiotic prophylaxis in the asplenic patient after transplant is dependent of
the presence of chronic GVHD (See Table below).
Table - Duration of propylaxis for encapsualted organism in asplenic patients according
to chronic GVHD
HCT recipients with chronic GVHD
Until 6 months after immunosuppression d/c’d
OR until age 6 OR 2 years after splenectomy
(whichever occurs later)
All HCT receipients without chronic
GVHD (allo, auto, syngenic)
1 year after BMT OR until age 6 OR 2 years after
splenectomy (whichever occurs later)
Note:
Sickle Cell: All Sickle cell patients should receive prophylactic penicillin daily for two years
post transplant or until their tenth birthday, whichever is longer. The dose is 125 mg PO
BID for patients < 3 years old and 250 mg PO BID for patients > 3 years.
Antimicrobial prophylaxis should also be considered for patients AT ANY TIME post-
splenectomy during travel to sites where medical care will not be rapidly accessible.

14
Preemptive therapy for the post-splenectomy patient with fever and rigors
Another strategy that has been advocated is the provision of "standby" antipneumococcal
antibiotics; this strategy may be particularly relevant for patients who are not receiving
prophylaxis. Under this strategy, the patient retains a personal supply of antibiotics to be
taken at the first sign of respiratory illness, fever, or rigors, particularly if there is likely
to be a delay in medical evaluation. There is currently no evidence that such early self-
treatment will lower the mortality associated with post splenectomy sepsis (PSS). In fact,
the literature series with the lowest mortality reported to date emphasized patient
education, close follow-up, and prompt physician intervention at the earliest sign of even
minor infection. Thus, even if patients have their own supply of antibiotics, medical help
should be sought immediately, at which time a physician should decide whether to
continue antibiotic therapy.
Recommended antibiotics and doses that may be useful in preemptive approaches include
the following:
• Adults: Amoxicillin 500 mg tablets; take 4 tablets (2 grams) and
report immediately for medical attention
OR
Levofloxacin 750 mg tablets; take 1 tablet and report
immediately for medical attention
• Children 20-40 kg: Amoxicillin 250 mg tablets; take 4 tablets (1 gram) and
report immediately for medical attention
• Children < 20 kg: Amoxicillin 50 mg/kg administered as chewable tablets
and report immediately for medical attention
For penicillin-allergic children, consider Bactrim or other drugs as clinically indicated.
Empiric therapy for post-splenectomy sepsis (PSS) or other serious infections
Early recognition of infection followed by aggressive intervention is the cornerstone of
PSS management. Initial empiric antimicrobial therapy for the splenectomized patient
with unexplained fever, rigors, and other systemic symptoms should always include a
broad-spectrum antibiotic active against S. pneumoniae, H. influenzae, and N.
meningitidis such as ceftriaxone. In areas with high-level penicillin-resistant
pneumococci, vancomycin may be added empirically, particularly in cases with suspected
or proven meningitis
Patients with splenectomy post transplant
Also see Vaccination Section IX

15
D. Cytomegalovirus (CMV)
(See Section III, subsections H. and I for CMV monitoring frequency). `
1. Table 1. Threshold CMV Viral Load for Preemptive Therapy
All transplants that do not
meet above criteria
CMV seropositive CD34-
selected autologous
recipients
a
DAY 0-60
DAY >100
b
≥ 50 IU/ mL
(1.70 log10)
≥ 500 IU/ mL
(2.70 log10)
b
a
If protocol requires testing beyond day 100 > 500 IU/ mL (2.70 log 10)
b
Or rising DNA levels >5x baseline within 1 month
PATIENT
POPULATION
Unmodified autologous,
< 1 mg/kg steroids
≥ 150 IU/ mL
(2.18 log10)
DAY 0-100
b
Post Transplant

16
2. Preemptive Therapy
Table 2. Pre-emptive Induction Treatment Regimen for CMV Reactivation with Adequate
Renal Function After Transplant
Acyclovir/valAcyclovir used for CMV prophylaxis should be discontinued when pre-emptive therapy is
started. Acyclovir/valAcyclovir should be continued, for HSV/VZV prophylaxis, if maribavir is initiated or
restarted when ganciclovir or foscarnet is completed if indicated.
INDUCTION
Preferred
Alternative
ValGANCiclovir*
,
** (ONLY for patients with good
oral intake, no active gut GVHD,
no significant liver
disease and no severe diarrhea):
Adults and Peds > 50 kg:
900 mg PO Q 12 hrs
Peds ≥ 40 to < 50kg:
675 mg PO Q 12 hrs
Peds ≥ 30 to < 40kg:
450 mg PO Q 12 hrs
Peds ≥20 to <30 kg:
450 mg PO Q 12 hrs or
Liquid 14 mg/kg Q 12 hrs
Peds ≥ 15 to <20 kg:
225 mg PO Q12 hrs (= ½ pill) or
Liquid 14 mg/kg Q12 hrs
Peds ≥10 to < 15 kg:
Liquid 14 mg/kg Q12 hrs
OR
Ganciclovir**
5 mg/kg IV Q 12hrs
Foscarnet**
90 mg/kg
IV Q 12hrs
OR
Maribavir*,***, **** 400mg
PO BID
(Age ≥ 12 years and
weight ≥ 35kg )
Duration of Induction:
• For Non-Cord blood transplant, a switch to maintenance dosing may be made if CMV DNA levels are declining (at
least 1-log reduction) after 7 days; if not declining at day 7 of treatment, continue twice daily induction dosing until
CMV DNA levels have decreased over the course of 1 week; at which point transition to maintenance dosing can
occur.
• For Cord blood transplant, CMV DNA levels must be negative at one week in order to transition to maintenance
dosing. Otherwise, continue induction dosing until CMV DNA levels are negative at which point a transition to
maintenance is appropriate.
• All patients failing induction should be considered to switch therapy and do UL97/UL54 resistance testing
* ValGANCiclovir absorption is significantly enhanced when taken with food; thus patients should be
instructed to take ValGANCiclovir with food. Patients with poor oral intake, severe diarrhea/gut GVHD
are NOT good candidates for ValGANCicovir or Maribavir and should receive IV ganciclovir daily.
**Use actual weight unless actual weight is above 150% of ideal weight. For patients who are > 150% ideal body
weight, the weight used should be capped at 150% of ideal body weight.
***Maribavir to be considered in failure/intolerance of “Preferred” agents ; screen for drug-drug interactions.
****Because of drug-drug interaction, Maribavir should not be given simultaneously with CYP3 substrates like
Cytoxan and a 48-hour washout period is recommended.
Table 3: Preemptive Maintenance Treatment Regimen for CMV Reactivation with Adequate
Renal Function After Transplant

17
MAINTENANCE
Preferred
Alternative
ValGANCiclovir*
,
** (ONLY for patients with good oral intake, no
active gut GVHD,
no significant liver disease and no severe diarrhea):
Adults and peds > 50 kg:
900 mg PO Q Day
Peds ≥ 40 to < 50 kg:
675 mg PO Q Day
Peds ≥30 to < 40 kg:
450 mg PO Q Day
Peds ≥20 to <30 kg:
450 mg PO Q Day or
Liquid 14 mg/kg QD
Peds ≥ 15 to <20 kg:
225 mg PO QD (= ½ pill)
or Liquid 14 mg/kg QD
Peds ≥10 to < 15kg:
Liquid 14 mg/kg QD
OR
Ganciclovir**
5 mg/kg IV Q DAY
Foscarnet**
90 mg/kg
IV Q DAY
OR
Maribavir*,***, **** 400mg
PO BID
(Age ≥ 12 years and
weight ≥ 35kg )
Duration of Maintenance therapy:
• Maintenance therapy should be given for at least 2 weeks after induction therapy has been completed.
• Preemptive therapy may be discontinued when the surveillance test is negative after a minimum of 3 weeks
of therapy (at least one week induction). Shorter courses may be appropriate for subsequent episodes of
CMV reactivation. Please consult the LTFU office for questions (206-667-4415)
* ValGANCiclovir absorption is significantly enhanced when taken with food; thus patients should be instructed to
take ValGANCiclovir with food. Patients with poor oral intake, severe diarrhea/gut GVHD are NOT good
candidates for ValGANCiclovir or Maribavir and should receive IV ganciclovir daily.
**Use actual weight unless actual weight is above 150% of ideal weight. For patients who are > 150% ideal body
weight, the weight used should be capped at 150% of ideal body weight.
***Maribavir to be considered in failure/intolerance of “Preferred” agents ; screen for drug-drug interactions.
****Because of drug-drug interaction, Maribavir should not be given simultaneously with CYP3 substrates like
Cytoxan and a 48-hour washout period is recommended.
Note: Any questions on maintenance therapy, including drug resistance, Contact the LTFU office
(Appendix A).

18
Monitoring during treatment:
• CBC and differential must be measured within 24 hours before initiating treatment.
• CBC and differential must be measured 2-3 times weekly during treatment with
ValGANCiclovir or ganciclovir.
• Daily CBC is mandatory if the absolute neutrophil count (ANC) is <1,500/mm
3
.
• If ANC <1,000/mm
3
before ValGANCiclovir or ganciclovir is started, alternative
therapy is foscarnet.
• Renal function tests must be measured at least weekly.
Dose adjustment and other precautions during treatment:
• STOP ValGANCiclovir or ganciclovir if the ANC is below 1,000/mm
3
and consider foscarnet.
• AVOID using ValGANCiclovir, ganciclovir and foscarnet concurrently with acyclovir.
Please contact the LTFU office (Appendix A) for consultation.
• ValGANCiclovir, ganciclovir and foscarnet MUST be adjusted for renal dysfunction.
3. CMV Prophylaxis After Day 100 in Seropositive Cord Blood Transplant Recipients
CMV seropositive cord blood transplant recipients remain at significantly increased risk for CMV
reactivation after day 100 after transplant. Therefore, antiviral prophylaxis and continued close
monitoring after day 100 (see Table 3 below) are recommended for all CMV seropositive cord
blood transplant recipients.
Table 3: CMV Prophylaxis and Monitoring after Day 100 to 1 Year for CMV-seropositive Cord Blood
Recipients with Prior Posttransplant CMV Reactivation
DOSING
PREFERRED
ALTERNATIVE
MONITORING
BLOOD
Able to tolerate PO
Unable to
tolerate PO
Able to tolerate
PO
Adult or Pediatric ≥50 kg
ValGANCiclovir
†
900mg PO QD
Ganciclovir
#
5 mg/kg IV
Q DAY
Valacyclovir*
2 grams PO TID
Weekly:
CMV PCR,
Creatinine,
CBC with
Differential.
Pediatric ≥40 to <50 kg
ValGANCiclovir
†
675 mg PO QD(=1½ pills)
Valacyclovir*
2 grams PO TID
Pediatric ≥30 to <40 kg
ValGANCiclovir
†
450 mg PO QD
Valacyclovir*
1 gram PO TID
Pediatric ≥20 to < 30 kg
ValGANCiclovir
†
450 mg PO QD)
or Liquid 14 mg/kg QD
Valacyclovir*
1 gram PO TID
Pediatric ≥15 to < 20 kg
ValGANCiclovir
†
225 mg PO QD(= ½ pill)
or Liquid 14 mg/kg QD
Acyclovir*
600 mg/m
2
PO
QID
Pediatric ≥10 to < 15 kg
ValGANCiclovir
†
Liquid 14 mg/kg QD
Acyclovir*
600 mg/m
2
PO QID
† Absorption of ValGANCiclovir is significantly enhanced when taken with food; thus patients should be instructed to take ValGANCiclovir
with food. Patients with poor oral intake, severe diarrhea/gut GVHD are NOT good candidates for ValGANCiclovir and should receive IV
ganciclovir daily.
* Valacyclovir tablets should NOT be crushed. Oral acyclovir suspension has poor bioavailability and is not a preferred choice.
#
Use actual weight unless actual weight is above 150% of ideal weight. For patients who are > 150% ideal body
weight, the weight used should be capped at 150% of ideal body weight.

19
Table 4: CMV Prophylaxis and Monitoring after Day 100 for CMV-seropositive Cord Blood
Recipients without Prior Posttransplant CMV Reactivation
DOSING
PREFERRED
ALTERNATIVE
MONITORING
BLOOD
Able to tolerate
PO intake
Unable to
tolerate PO
intake
Adult or Pediatric ≥50 kg
Valacyclovir*
2 grams PO TID
Acyclovir
‡
500 mg/m
2
IV Q 8 hr
Ganciclovir
#
5 mg/kg
IV Q DAY
Weekly:
CMV by PCR
Creatinine and
CBC with
Differential
Pediatric ≥40 to <50 kg
Valacyclovir*
2 grams PO TID
Pediatric ≥30 to <40 kg
Valacyclovir*
1 gram PO TID
Pediatric ≥20 to < 30 kg
Valacyclovir*
1 gram PO TID
Pediatric ≥15 to < 20 kg
Acyclovir
600 mg/m
2
PO QID
Pediatric ≥10 to < 15 kg
Acyclovir
600 mg/m
2
PO QID
* Oral Valacyclovir is the preferred agent and is available in tablets or compounded liquid formulation for
children.
Crushing tablets is NOT recommended.
‡
If patients cannot tolerate oral tablets or liquid formulation, they should receive IV Acyclovir (adjusted to
ideal body weight). Oral acyclovir suspension has poor bioavailability, thus not a preferred choice.
#
Use actual weight unless actual weight is above 150% of ideal weight. For patients who are > 150%
ideal body weight, the weight used should be capped at 150% of ideal body weight.
Dose adjustment and other precautions during treatment:
• STOP ganciclovir or ValGANCiclovir if the ANC is below 1,000/mm
3
and consider
acyclovir, valacyclovir or foscarnet, as clinically indicated.
• AVOID using ganciclovir, ValGANCiclovir, foscarnet and valacyclovir concurrently
with acyclovir. Please contact the LTFU office (Appendix A) for consultation.
• Ganciclovir, foscarnet, ValGANCiclovir, valacyclovir and acyclovir MUST be adjusted
for renal dysfunction.
E. Fungal organisms
The current standard practice for antifungal prophylaxis is to administer fluconazole (400
mg/day) until day 75 after an allogeneic or CD34 selected autologous transplant or until
engraftment and resolution of mucositis after an unselected autologous transplant. This
strategy has been shown to reduce the incidence of candidemia and candidiasis-related
mortality. Fluconazole does not prevent infection with Aspergillus and other mold
species.

20
F. Intravenous immunoglobulin (IVIG) replacement and adjunctive therapy
A) Use of IVIG after hematopoietic cell transplantation (HCT) from day 100
through 1 year.
Reported IVIG studies are listed in the end of the LTFU general guidelines
[1-9]
. For
information regarding IVIG administration before100 days after transplant see
Standard Practice Committee guidelines.
1. Dosing and administration of prophylactic IVIG:
a. For allogeneic patients transplanted for myeloma, low grade lymphoma or CLL,
Administer IVIG 400 mg/kg at monthly intervals to maintain serum IgG levels above
400 mg/dL for 10 months after transplant prior to start of vaccinations.
b. For primary immune deficiency disease (PID):
Pre-infusion IgG serum level
1
(mg/dL)
IVIG dosing regimen
1,2
600 – 1000
Begin at 200 mg/kg/every 2 weeks and
wean to 400 mg/kg/every 4 weeks if
troughs remain satisfactory
< 600
300 mg/kg/every 2weeks up to 500 mg/kg
every week
2
>1000
400 mg/kg/every 4 weeks until B cell
function fully restored
1
When low levels are attributable to increased losses (e.g. chronic diarrhea) both IVIG dose and
frequency should be increased.
2
For pediatric patients the maximum dose of IVIG is 40 grams.
For pediatric patients whose central line is only being used for IVIG
prophylaxis, transition to subcutaneous human immunoglobulin preparation
(Hizentra
) may be considered under the approval and guidance of Pediatric
Immunology Service.
c. Other than above diseases, for allogeneic patients with haploidentical donors
or cord blood transplant, pediatric patients with unrelated donors or for
patients with ongoing infections or chronic GVHD with severe
hypogammaglobulinemia:
Continue to check IVIG levels monthly and administer IVIG 400 mg/kg at monthly
intervals to maintain serum IgG levels above 400 mg/dL. Continue for 10 months
after transplant prior to anticipated start of routine vaccinations.
d. IVIG should be held two months before the annual posttransplant evaluation to assess
immune reconstitution. (e.g. serum immunoglobulins levels and other immunological
panel).
e. Select immunoglobulin product according to precautions to decrease adverse effects
as applicable (see cautionary note below).

21
B) Use of IVIG after hematopoietic cell transplantation (HCT) > 1 year
Dosing and administration of prophylactic IVIG beyond 1 year
For allogeneic patients with Chronic GVHD beyond 1 year with recurrent
sinopulmonary infections and persistent hypogammaglobulinemia
Recommend to check IgG level monthly and administer IVIG 400mg/kg at
monthly intervals to maintain serum IgG levels > 400mg/dl
C) IVIG for treatment of CMV pneumonia:
There is no convincing efficacy data to add standard IVIG to antiviral therapy for
CMV pneumonia after HCT. The overall benefit of CMV IgG combined with
antiviral for treatment of CMV pneumonia has been reported by some but not all
investigators. Due to high mortality associated with CMV pneumonia, some experts
recommends antiviral therapy combine with CMV IgG as follows:
• CMV-IVIG may be administered at 150mg/kg every other day for 2 weeks (7
doses) followed by weekly administration for 4 additional weeks in combination
with anti-CMV medication.
• When high titer CMV-IVIG product (CytoGam) is not available, some experts has
recommended using standard IVIG at 500mg/kg given at the same schedule as
described above for CMV IgG.
D) Premedications before IVIG administration:
Given the high incidence of side effects of IVIG infusion (i.e., fever, chills, nausea,
emesis, headache, myalgias, rash and hypotension without anaphylaxis),
premedication with acetoaminophen and anti-histaminices (i.e., diphenhydramine) is
recommended.
E) Contraindication for IVIG:
1. Antibodies to IgA present
2. Anaphylaxis or severe prior reaction to immunoglobulin or serum therapy.
F) Cautionary note about IVIG:
IgA deficiency: IgA deficiency is considered a contraindication for IVIG use because
patients may develop IgE antibodies to IgA which increases their risk of anaphylaxis
if exposed to a product containing significant quantities of IgA. IVIG formulation
products with the lowest IgA content available should be given to patients known to
be deficient in IgA who require IVIG and who do not have detectable antibodies to
IgA. All patients with absent pre-transplant serum IgA levels should be evaluated for
the presence of anti-IgA antibodies. (see table below)
Renal insufficiency (creatinine clearance less than 60 ml/min):
Sucrose-free containing IVIG products should ONLY be used in the setting of renal
insufficiency. (see table below)

22
Continued F: Cautionary note about IVIG, Renal insufficiency:
IVIG Preparations
Preparation
Sugar Content
IgA Content
CMV IVIG
Cytogam
5% Sucrose
?
IVIG
Carimune
5% Sucrose
720mcg/ml
Panoglobulin
5% Sucrose
720mcg/ml
Gammar
5% Sucrose
?
Sandoglobulin
5% Sucrose
?
Octagam
10% Maltose
<200 mcg/ml
Venoglobulin
5% Sorbitol
15-50mcg/ml
Flebogamma
5% Sorbitol
<50mcg/ml
Gammar
5% Glucose
<25 mcg/ml
Iveegam
5% Glucose
<10mcg/ml
Low IgA containing IVIG
Polygam
2% Glucose
<3.7mcg/ml
Gammagard SD (powder)
2% Glucose
<1 mcg
Sugar Free IVIG
Gamunex
45mcg/ml
Gammagard 10% (liquid)
37 mcg/ml
Privigen
<25mcg/ml
Gammaplex
?
23
V. FEVER OF UNKNOWN ETIOLOGY
Fever should be considered a sign of infection until proven otherwise. The following
evaluation should be instituted promptly in all patients with fever.
1. Complete physical examination including the perineal and rectal area.
2. Blood culture
3. Urine culture
4. Cultures from any site suspicious for infection
5. Chest X-ray. CT of the chest should be obtained if respiratory symptoms are
present even if the chest x-ray is negative.
6. Sinus CT scan should be obtained if respiratory symptoms are present.
Empiric treatment with antibiotics may be indicated after cultures have been obtained.
Sudden, overwhelming sepsis syndrome with Pneumococcus or other encapsulated
organisms can occur, especially in patients who have poor compliance with antibiotic
prophylaxis. Organisms should be tested for antibiotic susceptibility. Please contact the
LTFU office (Appendix A) for consultation or assistance regarding specific treatment and
other evaluation as needed.
24
VI. EVALUATION OF RESPIRATORY PROBLEMS AND LUNG INFILTRATES
If the patient develops respiratory problems that do not resolve after initial diagnostic
evaluation and treatment, we urge you to contact the LTFU office (Appendix A) to discuss
further evaluation and management.
A. Diagnostic Evaluation
1. Chest x-ray PA and lateral
2. Lung CT scan if respiratory symptoms persist
3. Sinus CT scan if symptomatic or suspected sinus infection
4. Blood culture (always)
5. Nasopharynx culture for pertussis if clinically indicated
6. Bronchoalveolar Lavage (BAL) is recommended for patients with pulmonary
symptoms or pulmonary infiltrates to rule out infectious complication.
7. Transbronchial or thoracoscopic biopsy if BAL is negative with persistent pulmonary infiltrates
B. Tests Recommended for BAL and Transbronchial Biopsy Specimens
See algorithm on the end of this section for overview.
1. Bacterial, fungal, mycobacterial, and Legionella cultures
2. Stains specific for viral inclusions and general morphology to rule out malignancy
(Papanicolaou, Wright-Giemsa, Hematoxylin & Eosin)
3. Methenamine silver, Kinyoun AFB, modified Gimenez and Gram stains, KOH
4. for BAL Aspergillus Galactomannan Enzyme Immunoassay (GM EIA) (fluid only) or aspergillus by PCR
5. CMV shell vial test
6. DFA (direct fluorescent antibody) staining for herpes viruses (HSV, VZV),
7. PCR for respiratory viruses (RSV, influenzae A and B, parainfluenzae, adenovirus)
8. DFA (direct fluorescent antibody) for Legionella or PCR for Legionella
9. If clinically indicated, PCR or IHC for EBV.
C. Evaluation of Pulmonary Nodules or Persistent Infiltrates with a Negative BAL
1. Thoracoscopic biopsy or open lung biopsy is recommended for patients with nodular
infiltrates to rule out fungal, malignancy, bronchiolitis obliterans syndrome (BOS),
cryptogenic organizing pneumonia (COP)or other processes. Thoracoscopic lung
biopsy generally causes less morbidity than open lung biopsy. Fresh tissue should be
submitted for microbiologic and pathologic evaluation.
2. Tests recommended for lung tissue
a) Fresh samples should be obtained for DFA and culture or PCR for Legionella.
b) Imprints of the frozen section and permanent section should be made and evaluated
for morphology and assessment of viral inclusions and possible malignancy by
using Papanicolaou, Wright-Giemsa, hematoxylin and eosin stains. Specimens
should be evaluated for Pneumocystis, fungi, mycobacteria, Legionella and other
bacteria by using methenamine silver, Kinyoun AFB, modified Gimenez and
tissue Gram stains. Warthin-Starry stain should be done if needed. When
available, immunohistochemistry staining and in situ hybridization are
recommended for detection of viral infection.
c) Samples should be submitted for microbiologic evaluation to detect fungi,
mycobacteria, and other bacterial organisms.
d) Aspergillus by PCR
e) Samples should be submitted for viral cultures, in addition:
-DFA staining for herpes viruses (HSV, VZV)
25
-PCR for respiratory viruses (RSV, influenzae A and B, parainfluenzae,
adenovirus)
-Shell vial testing for CMV or PCR testing for CMV, VZV, HSV, EBV, HHV-6,
depending on the level of clinical suspicion.
3. If Infections Ruled Out, Then Consider BOS After Allogeneic Transplant
See section X, I for work up and treatment

26
Tests Recommended for Bronchoalveolar Lavage Fluid or
Lung Biopsy Specimens
ALWAYS:
• Bacteria & fungal cultures
• Gram Stains, KOH
• Histology / cytology
(H & E, silver stain)
STRONGLY RECOMMENDED:
• Legionella (culture & DFA or PCR)
• AFB (culture & stain)
• Modified Gimenez stain
• Viral cultures
• Aspergillus by PCR
• Aspergillus Galactomannan Enzyme
Immunoassay (GM EIA) (fluid only)
• Keep material in the refrigerator / freezer until a definitive diagnosis is made.
• If any of the tests above is not available locally, please contact the LTFU office (Appendix A).
During respiratory season:
• RSV and others respiratory virus
(for example influenzae A & B, parainfluenzae,
adenovirus) by PCR
If VZV is suspected (skin lesions, hepatitis):
• DFA or PCR
If HSV is suspected:
• DFA or PCR
If patient or donor are CMV seropositive:
• Shell vial cultures for CMV
If EBV is suspected:
• EBV by PCR or immuno-histo-
chemistry, IHC
SPECIFIC SITUATIONS
27
VII. EVALUATION OF DIARRHEA AND OTHER GI COMPLICATIONS
If the patient develops diarrhea or other gastrointestinal complications that do not resolve
after initial diagnostic evaluation and treatment (see algorithm on the end of this section), we
urge you to contact the LTFU office (Appendix A) to discuss further evaluation and
management.
A. Diagnostic Evaluation and Initial Management
1. Diarrhea caused by oral magnesium supplementation should be ruled out. If
necessary, patients should receive IV replacement of magnesium.
2. The clinical evaluation of diarrhea depends on its duration and volume, the presence of
blood, and the occurrence of fever and other constitutional symptoms. Normal stool
volume is <200 ml/day. Volumes >1000 ml/day indicate a small intestinal source
(GVHD, magnesium effect, enteric virus, giardiasis or cryptosporidiosis). Bloody
diarrhea suggests a bacterial enteric pathogen, GVHD or CMV enteritis. A more
directed approach can be taken if there is a history of foreign travel or history of
exposure to children from day-care setting. An algorithm for evaluation of diarrhea is
summarized on the following page.
3. Patients should remain NPO for 24-48 hours and IV fluids should be given to prevent
volume depletion. Special diets are recommended for patients with diarrhea caused by
GVHD (Section XX).
4. Immunosuppressive medications should be given IV if the volume of diarrhea exceeds
1.5 liter/day in adults of if diarrhea persists for more than 3 days. Contact the LTFU
office (Appendix A) for IV doses of immunosuppressive medications.
5. Monitor creatinine closely, and check the cyclosporine or tacrolimus (FK506) level weekly.
6. Avoid treatment with anti-diarrhea agents containing atropine-like drugs (e.g. Loperimide).
7. If the diarrhea does not resolve with these measures or recurs after the patient resumes oral
medications, a search for enteric pathogens including, for example, norovirus, c. difficile,
adenovirus and for children, rotavirus and endoscopy with biopsies is recommend.
Adequate platelet count and coagulation parameters should exist to do biopsy safely.
B. Procedures for Gastrointestinal Endoscopic Biopsies
1. Maintain platelet counts >50,000 before and for 3 - 4 days after the procedure.
2. Esophagogastroduodenoscopy should be carried out with multiple biopsies. Biopsy
of any erosion or ulcerations is indicated. If there are no macroscopic abnormalities
found, we suggest 6-8 biopsies of the gastric antrum. To minimize the risk of
bleeding, avoid biopsies of the duodenum unless this is the only site of abnormalities.
3. When diarrhea is the major GI symptom in a patient without other manifestations of
GVHD, either upper endoscopy or colonoscopy may be indicated to rule out CMV
infection or occult GVHD. All infections other than CMV can be identified from
stool samples. Biopsies obtained from the gastric antrum are usually sufficient to
diagnose GVHD, even in cases where the major symptom is diarrhea.
4. Biopsies samples (n = 4) should be placed in fresh buffered formalin.
5. Fresh biopsy samples (gastric, rectal or colon) should be placed in viral transport
medium and sent to a virology lab to perform rapid testing (shell vial) for CMV and
Varicella zoster as well as HSV if there are esophageal lesions. The last stomach
sample should be placed in CLO media to test for H. Pylori.
6. Please send slides and biopsy blocks to the address below if you wish our pathologists
to review the specimen. Because GVHD may be found in one but not all sites, it is
important to send as many slides or blocks as possible.
28
7. Please label the material with the patient’s name, the date obtained and sites.
8. Send the material to the following address:
Fred Hutchinson Cancer Center
825 Eastlake Ave. E. / Attn: LTFU G-1500
PO Box 19023
Seattle, WA 98109-1023
9. Please call (206) 667-4415 to notify our office when to expect the arrival of shipments.

29
C. Algorithm for Evaluation of Acute Onset Diarrhea in Transplant Survivors*
*In all patients with diarrhea, oral administration of Mg
++
should be discontinued, and IV
administration should be substituted.
Severity of illness
Asymptomatic or other symptoms limited
to anorexia, nausea or vomiting
Chronic GVHD
in other organs?
Yes
No
Test stool for C.
difficile, giardia
antigen, O&P
Other family
members ill with
similar symptoms?
Pos
Neg
Treat
Consider need to
document intestinal
GVHD and to R/O
CMV by biopsy
No
Yes
Fever, rigors or
bloody diarrhea
Test stool for
• enteric bacterial pathogens:
Salmonella
Shigella
C. fetus jejuni
H7:0157 E. coli
Yersinia
Aeromonas
• C. difficile
• viral culture-including
adenovirus and norovirus
• E. histolytica
• Rotavirus EIA
Neg
Pos
Treat
Endoscopic biopsies
and cultures
CMV
GVHD
Another Dx
Treat
Treat
Treat
Watchful
waiting

30
VIII. TREATMENT OF SPECIFIC INFECTIONS
Please contact the LTFU office (Appendix A) to discuss the most appropriate therapy in
patients developing any of the infections described below.
A. Cytomegalovirus (CMV)
Late onset CMV infections have become an increasingly difficult problem for patients
who have had a hematopoietic stem cell transplant. Reconstitution of the T cells that
respond to CMV is slow and may be delayed by prophylactic use of ganciclovir during
the first 3 months after the transplant. Patients at risk of CMV infection should be
monitored closely and should receive prophylactic antiviral treatment to prevent CMV
disease. Note that some patients present with nausea and vomiting as initial
manifestations of CMV infection, in the absence of CMV viremia. To obtain
recommendations for treatment of patients who develop CMV pneumonia or other
diseases caused by this virus, we urge you to contact the LTFU office (Appendix A).
B. Varicella zoster
Varicella zoster virus (VZV) infection occurs in 40-50% of patients during the first year
after the transplant (peak risk 2-8 months) when prophylactic acyclovir is not given. In
approximately 10% of patients, VZV infection presents with abdominal distension or
pain in the abdomen or back, often accompanied by increased serum ALT, before the
development of any skin lesions. Visceral VZV is frequently fatal if treatment is delayed.
If prodromal zoster or documented VZV infection occurs during the first year after the
transplant or at any time during continued treatment with immunosuppressive
medications, parenteral treatment should be started immediately with high dose acyclovir,
and blood should be sent to confirm the diagnosis by a VZV PCR test.
Patients should be treated according to the following recommendations.
1. Fluids should be administered at twice the daily maintenance level during treatment
with high dose acyclovir.
2. Prophylactic treatment with acyclovir or valacyclovir should be resumed after high–
dose treatment has been completed.
3. Renal function tests must be followed closely during treatment with high dose
acyclovir.
4. Doses of acyclovir must be decreased in patients with renal impairment.
Disseminated zoster:
IV acyclovir 500 mg/m
2
administered as a one hour IV infusion q 8 hr until there is no
evidence of new lesions for 72 hours. Treatment may then be continued with
valacyclovir 1 gm t.i.d. p.o. for patients > 40 kg and 500 mg t.i.d. p.o. for patients < 40
kg to complete the course of treatment (generally 10-14 days).
Localized zoster:
IV acyclovir 500 mg/m
2
administered as a one hour IV infusion q 8 hr for three doses,
then change to oral valacyclovir as outlined above to complete the course of treatment.
Dose adjustment is necessary in patients with impaired renal function.
31
C. Pneumocystis Carinii Pneumonia (PCP)
All patients should receive trimethoprim-sulfamethoxazole prophylaxis (Section IV A).
Patients who do not comply with the recommended prophylactic regimen may develop
PCP and will require appropriate treatment. Trimethoprim-sulfamethoxazole should be
given at a dose of 15-20 mg/kg/day of the trimethoprim component in divided doses every
6-8 hr for 14-21 days for treatment of PCP pneumonia.
32
IX. VACCINATIONS
Antibody titers to vaccine-preventable diseases (e.g. tetanus, polio, measles, mumps,
rubella, and encapsulated organisms) decline between 1 and 4 years after allogeneic or
autologous HCT if the recipient is not revaccinated. The clinical relevance of reduced
antibody titers to these diseases is not readily apparent because only a limited number
of vaccine-preventable diseases have been reported among HCT recipients.
Nonetheless, vaccine-preventable diseases continue to pose risks to the population.
Additionally, there is evidence that infections with encapsulated organisms, measles,
varicella and influenzae can pose risk to HCT recipients. Therefore, HCT recipients
should be routinely vaccinated after HCT so that they can experience immunity to the
same vaccine-preventable diseases as others.
Guidelines for vaccination after HCT have been published by relevant societies
1,2,3,
as
well as the Advisory Committee on Immunization Practices (ACIP) within the Centers
for Disease Control and Prevention (CDC)
4
and provides the foundation for our
vaccination practices explained elsewhere in further detail.
5
Vaccination begins at 3
months for SARS-CoV-2, and 6 months for influenza (or 3-4 months when seasonal
prevalence is high). Other non-live routine childhood vaccinations that must be
repeated after HCT, may begin as early as 6 months in Non-Primary Immune
Deficiency patients but should be considered in conjunction with factors that
significantly delay immune reconstitution. Live vaccines (MMR or MMR-V) are
generally not administered before 2 years after HCT.
See tables for recommendation for vaccinations for adult and pediatric patients:
IX.A1 Adult Vaccination Schema-Non-Live Vaccines: Vaccination before
12 months (if eligible)
IX.A2 Adult Vaccination Schema- Non-Live Vaccines: Standard
vaccination schedule
IX.A3 - Adult Vaccination Schema- For MMR(V) and Zoster Vaccines
IX.P1 Pediatric Vaccination Schema: Vaccination before 12 months (if
eligible)
IX.P2 Pediatric Vaccination Schema: If patient not vaccinated before 12
months
IX.P3: Pediatric Vaccination Schema: For MMR (V) and Zoster Vaccines

33
Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) recommend that vaccine providers should strongly consider observing patients for 15
minutes after they are vaccinated. If syncope develops, patients should be observed until the symptoms resolve.
Table IX.A1: Adult Vaccination Schema for Non-Live Vaccines: starting before 12 months (if eligible)
1,2
Vaccine
>3m
~4m
~5m
>6m
>7m
>8m
>10m
>12m
>13m
>14m
>18m
>24m
Influenzae (IIV4)
(Sept –
March), non-adjuvanted
IIV4 (Flu)
High-
Dose
3
IIV4 (Flu)
High-
Dose
3
Pentacel
®
(DTaP-
IPV/Hib)
4,5
Pentacel
®
Pentacel
®
Pentacel
®
titers
6
titers
6
Meningococcal ACWY
(MenQuadfi, Menveo,
MCV4)
MCV4
MCV4
Meningococcal Group B
(Bexsero
®
)
7
Bexsero
®
Bexsero
®
Pneumococcal-conjugate
(Prevnar 20™)
titers
8
PCV20
9
PCV20
9
PCV20
9
titers
9
Hepatitis A
11
HAV
HAV
Hepatitis B
10,11
HBV
HBV
HBV
HBV
titers
10
HPV (Gardasil), 9 to 45 y
HPV
HPV
HPV
SARS-CoV-2
12
(Moderna or Pfizer)
COVID
COVID
COVID
13
COVID
13
Abbreviations: DTaP, Diphtheria-Tetanus-acellular Pertussis; Hib, H. Influenzae type B; HPV, human papilloma virus; IPV, inactivated polio vaccine; MCV4, meningococcal
conjugate vaccine
Footnotes:
1 For adults transplanted for immunodeficiency disorders, refer to the following section, “Posttransplant Vaccination of Primary Immunodeficiency Disorders.”
2 For non-live vaccine, vaccination may be deferred if receiving ongoing immunoglobulin replacement for delayed immune reconstitution or other factors in Table
IX.1 are present.
3 Ideally start the 2-dose series at 6 months but during high prevalence influenza outbreaks may start as early as 3 months. If non-adjuvanted, high-dose
quadrivalent inactivated influenza vaccine is unavailable, then give standard-dose formulation. The 2-dose series does not apply if no longer on
immunosuppressive therapy and >2y post-HCT.
4 Separate component vaccines (shots) may be used instead for DTaP, IPV, and Hib if Pentacel
®
is unavailable.
5 If not using Pentacel
®
and DTaP is unavailable, then may use Adacel
®
= Tdap (age ≥ 10 y through 64 y) or Boostrix
®
= Tdap (age ≥ 10 y).
6 Check anti-tetanus toxoid and anti-Hib titers if not done at 12 months.
7 Recommended for patients with anatomic or functional asplenia condition (i.e., chronic GVHD) or increased environmental risk. Trumenba® can be substituted for
Bexsero® (3 doses: 0, 2 and 6 months apart).
8 Check baseline titers for S. Pneumonia (IgG, 23 serotypes) before beginning PCV20 vaccination.
9 Check titers for S. Pneumonia (IgG, 23 serotypes) 1-2 months after each PCV20 is given. A positive response to PCV20 is defined: as achieving a seroprotective IgG level
against S. pneumoniae in ≥15 out of 20 PCV20 serotypes at 1-2 months post-vaccination. A positive response requires no further PCV20 vaccination.
10 A complete series of Hepatitis B vaccination is accomplished preferably with a total of 4 x single 0.5 mL doses of Heplisav-B
®
based on data extrapolated from patients with
chronic kidney disease or on hemodialysis for ESRF. Alternatively, a total of 4 x double (2 mL total) doses of Engerix-B
®
may be given. Post-vaccination testing for antibody
to hepatitis B surface antigen is recommended 1-2 months after the 4th dose to ensure protection (Check titers at 24-month visit if not done at 20 months). Patients who do not
respond to the primary vaccine series should receive an additional 1-3 doses of the same vaccine or, alternatively, repeat series with a different vaccine brand (e.g., double
doses of Engerix-B
®
if did not respond to Heplisav-B
®
or single doses of Heplisav-B
®
if did not respond to Engerix-B
®
).
11 If NOT administering hepatitis B series using Heplisav-B
®
, Twinrix
®
can be administered on days when HAV and HBV are given together. (Twinrix
®
approved for age ≥ 18 y)
12 Dose 1 of the SARS-CoV-2 vaccination series should begin at > day +90. For allogeneic transplant patients, the initial dose should be arranged to be given
as part of the day +80 work up. Communications with referring provider should be done to advise when subsequent doses are due.
13 Dose 3 is preferably given 2 months after dose 2 but may be given as early as 1 month after dose 2 to avoid a missed vaccination opportunity; Dose 4 is 2
months after Dose 3.

34
Table IX.A2: Adult Vaccination Schema for Non-Live Vaccines: Standard vaccination schedule
1,2
Abbreviations: DTaP, Diphtheria-Tetanus-acellular Pertussis; Hib, H. Influenzae type B; HPV, human papilloma virus; IPV, inactivated polio vaccine; MCV4, meningococcal conjugate vaccine.
Footnotes:
1 For adults transplanted for immunodeficiency disorders, refer to the following section, “Posttransplant Vaccination of Primary Immunodeficiency
Disorders.”
2 For non-live vaccine, vaccination may be deferred if receiving ongoing immunoglobulin replacement for delayed immune reconstitution or other factors in
Table IX.1 are present.
3 Ideally start the 2-dose series at 6 months but during high prevalence influenza outbreaks may start as early as 3 months. If non-adjuvanted, high-dose
quadrivalent inactivated influenza vaccine is unavailable then give standard-dose formulation. The 2-dose series does not apply if no longer on
immunosuppressive therapy and >2y post-HCT.
4 Separate component vaccines (shots) may be used instead for DTaP, IPV, and Hib if Pentacel
®
is unavailable.
5 If not using Pentacel
®
and DTaP is unavailable, then may use Adacel
®
= Tdap (age ≥ 10 y through 64 y) or Boostrix
®
= Tdap (age ≥ 10 y).
6 Check anti-tetanus toxoid and anti-Hib titers.
7 Recommended for patients with anatomic or functional asplenia condition (i.e., chronic GVHD) or increased environmental risk). Trumenba® can be
substituted for Bexsero® (3 doses: 0, 2 and 6 months apart).
8 Check baseline titers for S. Pneumonia (IgG, 23 serotypes) before beginning PCV20 vaccination.
9 Check titers for S. Pneumonia (IgG, 23 serotypes) 1-2 months after each PCV20. A positive response to PCV20 is defined: as achieving a seroprotective
IgG level against S. pneumoniae in ≥ 15 out of 20 PCV20 serotypes at 1-2 months post-vaccination. A positive response requires no further PCV20
vaccinations.
10 A complete series of Hepatitis B vaccination is accomplished preferably with a total of 4 x single 0.5 mL doses of Heplisav-B
®
based on data
extrapolated from patients with chronic kidney disease or on hemodialysis for ESRF. Alternatively, a total of 4 x double (2 mL total) doses of Engerix-
B
®
may be given. Post-vaccination testing for antibody to hepatitis B surface antigen is recommended 1-2 months after the 4th dose to ensure protection
(Check titers at 24-month visit if not done at 20 months). Patients who do not respond to the primary vaccine series should receive an additional 1-3
doses of the same vaccine or, alternatively, repeat series with a different vaccine brand (e.g., double doses of Engerix-B
®
if did not respond to Heplisav-
B
®
or single doses of Heplisav-B
®
if did not respond to Engerix-B
®
).
11 If NOT administering hepatitis B series using Heplisav-B
®
, Twinrix
®
can be administered on days when HAV and HBV are given together. (Twinrix
®
approved for age ≥ 18 y).
12 Dose 1 of the SARS-CoV-2 vaccination series should begin at > day +90. For allogeneic transplant patients, the initial dose should be arranged to be
given as part of the day +80 work up. Communications with referring provider should be done to advise when subsequent doses are due.
13 Dose 3 is preferably given 2 months after dose 2 but may be given as early as 1 month after dose 2 to avoid a missed vaccination opportunity; Dose 4 is
2 months after Dose 3.
Vaccine
>3m
~4m
>6m
>7m
>8m
>12m
>13m
>14m
>16m
>18m
>24m
Influenzae (IIV4)
(Sept –
March), non-adjuvanted
IIV4 (Flu)
High-Dose
3
IIV4 (Flu)
High-Dose
3
Pentacel
®
(DTaP-
IPV/Hib)
4,5
Pentacel
®
Pentacel
®
Pentacel
®
titers
6
Meningococcal ACWY
(MenQuadfi, Menveo,
MCV4)
MCV4
MCV4
Meningococcal Group B
(Bexsero
®
)
7
Bexsero
®
Bexsero
®
Pneumococcal-conjugate
(Prevnar 20™)
titers
8
PCV20
9
PCV20
9
PCV20
9
titers
9
Hepatitis A
11
HAV
HAV
Hepatitis B
10, 11
HBV
HBV
HBV
HBV
titers
10
HPV (Gardasil), 9 to 45 y
HPV
HPV
HPV
SARS-CoV-2
12
(Moderna or Pfizer)
COVID
COVID
COVID
13
COVID
13
Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) recommend that vaccine providers should strongly consider observing patients for 15 minutes after
they are vaccinated. If syncope develops, patients should be observed until the symptoms resolve.

35
Table IX.A3: Adult Vaccination Schema: For MMR(V)
and Zoster (SHINGRIX)
A) Live MMR or Varicella Vaccines
~24 m
24 m
>25m
~27m
Measles/Mumps/Rubella (MMR)
2-1-8 Rule
a
No Live Vaccines are given
until at least 2 yr post-HCT
and then only when certain
other criteria are met
a
MMR
MMR
Varicella-Zoster (Varivax)
Seronegative ONLY and 2-1-8 Rule
a
First dose may be given with MMR
titers
b
VZV
VZV
titers
c
a. 2-1-8 Rule = Not until 2 years post HCT plus > 1 year off all immunosuppressive therapy (IST) plus >8 months since last dose of IVIG/VZIG or most recent plasma transfusion.
b. Check baseline varicella serology at least 8 months off IVIG/VZIG when ready to vaccinate to determine if necessary.
c. Check at least 1-2 months after Varivax to ensure seroconversion of the VZV seronegative patient.
B) Non-Live Shingles Vaccine
~12 m
>12m
>14m
ALLOGENEIC and AUTOLOGOUS
recipients AGE >18 y ONLY:
VZV Seropositive ONLY
SHINGRIX is not given until at least 1-y post-HCT
and then only when certain other criteria are met
1
titers
2
SHINGRIX
3
SHINGRIX
3
1. Allogeneic recipients must also be age >18 y and >1 y after HCT, >8 m off immunosuppressive therapy without GVHD flare-ups. Autologous recipients must have also completed maintenance
immunotherapy (e.g. PD-1 inhibitors, proteosome inhibitors, daratumumab) which also prolongs duration of acyclovir/valacyclovir.
2. Patients should have VZV serology checked prior to vaccination (at least at least 8 months off IVIG/VZIG) to ensure still VZV-seropositive. If patient is VZV seronegative, do not give SHINGRIX but
follow the table above and offer Varivax while still following the 2-1-8 Rule.
3. Continue acyclovir or valacyclovir until one month after second Shingrix vaccination.
Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) recommend that vaccine providers should strongly consider observing patients for
15 minutes after they are vaccinated. If syncope develops, patients should be observed until the symptoms resolve.

36
Table IX.P1: Pediatric Vaccination Schema: Vaccination before 12 months (if eligible)
1,2
Vaccine
>3m
~4m
~5m
>6m
>7m
>8m
>10m
>12m
>14m
>18m
>24m
IIV4 – Age 6 m to <5 y
(September –March)
IIV4 (Flu)
Std-Dose
3
IIV4 (Flu)
Std-Dose
3
IIV4 – Age ≥5 y
(September –March)
IIV4 (Flu)
High-Dose
3
IIV4 (Flu)
High-Dose
3
Pentacel® (DTaP-IPV/Hib)
4,5
Pentacel
®
Pentacel®
Pentacel®
titers
6
titers
6
Meningococcal ACWY
(MenQuadfi, Menveo, MCV4)
MCV4
MCV4
Meningococcal Group B
(Bexsero®)
7
Bexsero®
Bexsero®
Pneumococcal-conjugate
(Prevnar 20™)
PCV20
PCV20
PCV20
titers
8
PCV20
titers
8
Hepatitis A
HAV
HAV
Hepatitis B
9
HBV
HBV
HBV
titers
10
HPV9 (Gardasil), 9 to 45 years
HPV
HPV
HPV
SARS-CoV-2 – Age ≥6 m
11
Pfizer or Moderna
COVID
COVID
COVID
12
COVID
12
Abbreviations: DTaP, Diphtheria-Tetanus-acellular Pertussis; Hib, H. Influenzae type B; HPV, human papilloma virus; IIV4, inactivated quadrivalent influenza
vaccine; IPV, inactivated polio vaccine; MCV4, meningococcal conjugate vaccine; PCV13, Prevnar 13; PPSV23, Pneumovax.
Footnotes:
1. For patients transplanted for immunodeficiency disorders see following section, “Posttransplant Vaccination of Primary Immunodeficiency Disorders”.
2. For non-live vaccine, vaccination may be deferred if receiving ongoing immunoglobulin replacement for delayed immune reconstitution or other factors in
Table IX.1 are present.
3. Ideally start the 2-dose series at 6 months but during high-prevalence influenza outbreaks may start as early as 3 months. If non-adjuvanted, high-dose
quadrivalent inactivated influenza vaccine is unavailable for children ≥ 5 years then give standard-dose based on Pediatric HCT Flu Study. The 2-dose series
does not apply if no longer on immunosuppressive therapy and >2y post-HCT.
4. Different combination vaccines may be used if Pentacel® is unavailable: Infanrix or Daptacel (= DTaP for age < 7 y), Pediarix = DTaP/HBV/IPV (age < 7 y).
5. If not using Pentacel® and DTaP is unavailable then may use Adacel = Tdap (age ≥ 10 y through 64 y ) or Boostrix = Tdap (age > 10 y).
6. Check Anti-tetanus toxoid and anti-Hib titers.
7. Recommended for anatomic or functional asplenia (i.e. chronic GVHD) or increased environmental risk. If patient is ≥10y, Trumenba® can be substituted for
Bexero® (3 doses: 0, 2, and 6 months apart).
8. Check titers for S. Pneumonia (IgG, 23 serotypes) to determine if an additional dose of PCV20 should be given.
9. If using Hepatitis B vaccine Recombivax HBR, dosing schedule is 0, 1 and 6 months if patient is 0 to 19 years of age.
10. Titer at 24-month visit if not done at 20 months. Post-vaccination testing for antibody to hepatitis B surface antigen is recommended 1-2 months after the 3
rd
dose to ensure protection. Patients who do not respond to the primary vaccine series should receive an additional 1-3 double-doses of the same vaccine (or 4-
single dose series of Heplisav-B if age >18y).
11. Dose 1 of the SARS-CoV-2 vaccination series should begin at > day + 90. For allogeneic transplant patients as part of the day+ 80 work up, the initial dose
should be arranged to be given by the appropriate OPD Team). Communications with referring provider should be done to advise when subsequent doses are
due.
12. Dose 3 is preferably given 2 months after dose 2 but may be given as early as 1 month after dose 2 to avoid a missed vaccination opportunity; Dose 4 is 2
months after Dose 3.
Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) recommend that vaccine providers should strongly consider observing patients for
15 minutes after they are vaccinated. If syncope develops, patients should be observed until the symptoms resolve.

37
Table IX.P2: Pediatric Vaccination Schema: If patient not routinely vaccinated before 12 months
1,2;
Vaccine
>3m
~4m
~5m
>6m
>7m
>8m
>12m
>14m
>16m
>18m
>24m
IIV4 – Age 6 m to <5 y
(September –March)
IIV4 (Flu)
Std-Dose
3
IIV4 (Flu)
Std-Dose
3
IIV4 – Age ≥5 y
(September –March)
IIV4 (Flu)
High-Dose
3
IIV4 (Flu)
High-Dose
3
Pentacel® (DTaP-IPV/Hib)
4.5
Pentacel®
Pentacel®
Pentacel®
titers
6
Meningococcal ACWY
(MenQuadfi, Menveo, MCV4)
MCV4
MCV4
Meningococcal Group B
(Bexsero®)
7
Bexsero®
Bexsero®
Pneumococcal-conjugate
(Prevnar 20™)
PCV20
PCV20
PCV20
titers
8
PCV20
8
Hepatitis A
HAV
HAV
Hepatitis B
9
HBV
HBV
HBV
titers
10
HPV9 (Gardasil), 9 to 45 y
HPV
HPV
HPV
SARS-CoV-2 – Age ≥ 6 m
11
Pfizer or Moderna
COVID
COVID
COVID
12
COVID
12
Abbreviations: DTaP, Diphtheria-Tetanus-acellular Pertussis; Hib, H. Influenzae type B; HPV, human papilloma virus; IIV4, inactivated quadrivalent influenza
vaccine; IPV, inactivated polio vaccine; MCV4, meningococcal conjugate vaccine; PCV13, Prevnar 13; PPSV23, Pneumovax.
Footnotes:
1. For patients transplanted for immunodeficiency disorders see following section, “Posttransplant Vaccination of Primary Immunodeficiency Disorders”.
2. For non-live vaccine, vaccination may be deferred if receiving ongoing immunoglobulin replacement for delayed immune reconstitution or other factors in
Table IX.1 are present.
3. Ideally start the 2-dose series at 6 months but during high-prevalence influenza outbreaks may give as early as 3 months. If non-adjuvanted, high-dose
quadrivalent inactivated influenza vaccine is unavailable for children ≥ 5 years, then give standard-dose based on Pediatric HCT Flu Study. The 2-dose series
does not apply if no longer on immunosuppressive therapy and >2y post-HCT.
4. Different combination vaccines may be used if Pentacel® is unavailable: Infanrix or Daptacel (= DTaP for age < 7 y), Pediarix = DtaP/HBV/IPV (age < 7 y).
5. If not using Pentacel® and DtaP is unavailable, then may use Adacel = Tdap (age ≥ 10 y through 64 y ) or Boostrix = Tdap (age > 10 y).
6. Check Anti-tetanus toxoid and anti-Hib titers.
7. Recommended for anatomic or functional asplenia (i.e. chronic GVHD) or increased environmental risk. If patient is ≤10y, Trumenba® can be substituted for
Bexero® (3 doses: 0, 2 and 6 months apart).
8. Check titers for S. Pneumonia (IgG, 23 serotypes) about 2 months after vaccine to determine if an additional dose of PCV20 should be given.
9. If using Hepatitis B vaccine Recombivax HBR, dosing schedule is 0, 1 and 6 months if patient is 0 to 19 years of age.
10. Titer at 24-month visit if not done at 20 months. Post-vaccination testing for antibody to hepatitis B surface antigen is recommended 1-2 months after the 3rd
dose to ensure protection. Patients who do not respond to the primary vaccine series should receive an additional 1-3 double-doses of the same vaccine (or 4-
single dose series of Heplisav-B if age >18y).
11. Dose 1 of the SARS-CoV-2 vaccination series should begin at > day + 90. For allogeneic transplant patients as part of the day+ 80 work up, the initial dose
should be arranged to be given by the appropriate OPD Team). Communications with referring provider should be done to advise when subsequent doses are
due.
12. Dose 3 is preferably given 2 months after dose 2 but may be given as early as 1 month after dose 2 to avoid a missed vaccination opportunity; Dose 4 is 2
months after Dose 3.
Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) recommend that vaccine providers should strongly consider observing patients for 15
minutes after they are vaccinated. If syncope develops, patients should be observed until the symptoms resolve.

38
Table IX.P3: Pediatric Vaccination Schema: For MMR(V) and Zoster (SHINGRIX)
1
1. 2-1-8 Rule = Not until 2 years post HCT plus > 1 year off all immunosuppressive therapy (IST) plus >8 months since last dose of IVIG/VZIG or most recent plasma transfusion.
2. Check baseline varicella serology at least 8 months off IVIG/VZIG when ready to vaccinate to determine if necessary.
3. Check at least 1-2 months after Varivax to ensure seroconversion of the VZV seronegative patient.
B) Non-Live Shingles Vaccine
<12m
~12 m
>12m
>14m
ALLOGENEIC and AUTOLOGOUS
recipients AGE >18 y ONLY:
VZV Seropositive ONLY
SHINGRIX is not given until at least 1 yr post-
HCT and then only when certain other criteria
are met
a
titers
b
SHINGRIX
c
SHINGRIX
c
a. Allogeneic recipients must also be age >18 y and >1 y after HCT, >8 m off immunosuppressive therapy without GVHD flare-ups. Autologous recipients must have also completed maintenance
immunotherapy (e.g. PD-1 inhibitors, proteasome inhibitors, daratumumab) which also prolongs duration of acyclovir/valacyclovir.
b. Patients should have VZV serology checked prior to vaccination (at least 8 months off IVIG/VZIG) to ensure still VZV-seropositive. If patient is VZV seronegative, do not give SHINGRIX but
follow the table above and offer Varivax while still following the 2-1-8 Rule.
c. Continue acyclovir or valacyclovir until one month after second Shingrix vaccination
.
A) Live MMR or Varicella Vaccines
~24 m
24 m
>25m
~27m
Measles/Mumps/Rubella (MMR)
2-1-8 Rule
1
No Live Vaccines are given until at least 2 yr
post-HCT and then only when certain other
criteria are met
1
MMR
MMR
Varicella-Zoster (Varivax)
Seronegative ONLY and 2-1-8 Rule
1
First dose may be given with MMR
titers
2
VZV
VZV
titers
3
Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) recommend that vaccine providers should strongly consider observing patients for 15 minutes
after they are vaccinated. If syncope develops, patients should be observed until the symptoms resolve.

39
• Please keep records of all vaccinations (dates and types of all vaccines) given to the patient
after the transplant and report any toxicity to the LTFU.
Posttransplant Vaccination of Primary Immunodeficiency Disorders (PID):
❖ From a practical standpoint, patients with primary immunodeficiency disorders (PID) are not
candidates for the Standard Practice early vaccination policy that begins at 6 months after
transplant. Exceptions may be made for epidemics (e.g. seasonal influenza) or novel pandemics
(e.g. COVID-19), per pediatric attending recommendations.
❖ PID patients will first be considered as candidates for vaccination at 1 year after transplant if they
satisfy the following criteria:
A. It is reasonable to attempt a 3-month trial off IgG replacement therapy based on a
negative history of patient infections in the past 6 months and
B. The prevalence of community infections with influenza, RSV, metapneumovirus, or
parainfluenza during the planned trial off IgG therapy is low and
C. All of the following laboratory criteria:
Criteria
Comment
1. Trough IgG > 600 mg/dL
on standard IVIG dosing
Suggests numeric IgG reconstitution
2. Detectable serum IgA (>
6 mg/dL)
A detectable IgA level indicates potential ability to
“class switch”
3. Donor
a
B cell count
> 200 per microliter
Arbitrarily set at 1-log higher than our standard
practice for those transplanted for malignancy
4. Donor
b
CD4 T cell count
> 200 per microliter
Same as our standard practice for those transplanted
for malignancy
a
as determined by donor B cell chimerism divided by 100 x total absolute B cell count
b
as determined by donor CD4 cell chimerism divided by 100 x total absolute CD4 T cell count
Standard Protocol for Re-vaccination with Killed Vaccines after HCT for PID:
1. If patient satisfies criteria A and B above, then obtain results of trough IgG, IgA and IgM
levels, CD19 or CD20 B cell count per microliter and B cell chimerism (% donor), CD4 T cell
donor chimerism and CD4 T cell count per microliter. If patient visit is not timed with the
expected trough following last dose of IVIG, then defer quantitative immunoglobulin testing
until trough levels are expected.
2. If the results of (1) indicate that the patient now satisfies criteria A, B and C then:
o Plan to hold IgG therapy for the next 12 weeks
o Week 0: Give one dose each of: Prevnar, HiB, DTaP (or Tdap) and HBV
(combination vaccines are preferred to limit the number of shots).
o Wks 6-8: Repeat the series given at Week 0
o Week 12: Check antibody response titers including:
Hib, 23-pneumococcal serotypes, tetanus toxoid, and hepatitis B surface antibody
3. Pediatric LTFU Attendings will decide whether patient’s responses to tetanus, HiB and Prevnar
are sufficient for the patient to remain off immunoglobulin therapy and to proceed with
remaining vaccination against pneumococcus, hemophilus influenza Type B, tetanus,
diphtheria, pertussis, and hepatitis B, as well as to begin a standard series of conjugated
meningococcal, hepatitis A and inactivated polio vaccines. Alternatively, if vaccine response is
inadequate then patient will resume IVIG therapy and further vaccination will be deferred.
SARS-CoV-2 and seasonal influenza vaccinations will be given per pediatric LTFU attending
recommendations.

40
Standard Protocol for Re-vaccination with Live Vaccines after HCT for PID:
1. If patient has responded adequately to killed vaccines the patient may be considered for the live
attenuated measles, mumps and rubella vaccine, and the varicella-zoster vaccine (in VZV
seronegative patients only) assuming the following additional criteria are met:
a. At least 2 years posttransplant
b. At least 1 year off all systemic immunosuppressive therapy
c. At least 8 months after last dose of IVIG therapy
Posttransplant Vaccination of All Other Patients (NON-PID)
Clinically relevant, 2-4-fold rises in specific antibody levels, or a rise from undetectable to a
level considered protective, require at least partial reconstitution of adaptive (T and B cell)
immunity. Therefore, factors that might influence a decision to delay a series of vaccinations
include:
Table IX.1
Delay of T cell recovery
Delay of B cell recovery
• CD4 T cells < 200/microliters
• CD19 or CD20 B cells < 20/microliters
• Active GVHD
• Anti-CD20 antibody ≤ 6 months
• IVIG therapy ≤ 2 months ago
• Moderate to severe GVHD
• Receiving chemotherapy or
biological therapeutic agents
*
• Receiving chemotherapy or biological
therapeutic agents
*
*Note Lenalidomide alone maintenance therapy should not affect lymphocyte counts and patients can receive
vaccination per standard schedule.
General Recommendations:
• The “Pink Book” recommends time intervals for pediatric vaccines.
10
• All patients should receive seasonal flu
11
and SARS-COV-2 vaccinations per Tables
IX.A1-A2 and Tables IX.P1-P2.
• If patient is on disease-associated maintenance therapy that can affect T or B cell
numbers, then before beginning other vaccinations (Follow Table IX.1 above):
✓ Check CD 19 or CD 20 B cells to determine > 20/microliters and
✓ Check CD4 T cells to determine > 200/microliters.
• Vaccination for S. pneumoniae and H. influenzae is recommended for all transplant
recipients but does not supplant chemoprophylaxis due to variable serologic responses.
• Inactivated vaccine injections should be used for family members who need vaccinations
against polio. Isolation is necessary if live (oral) polio vaccine is administered to family
members or other persons in close contact with the patient during the first year after the
transplant or at any time during treatment with immunosuppressive medications. The
virus can be shed for 8 to 12 weeks after vaccination.
• Influenzae vaccination: Live attenuated influenzae vaccine is not recommended.
• Hepatitis B Vaccination Formulas: In patients > 18 years old who did not respond to
the initial Hepatitis B vaccination series, there is a new Hepatitis B vaccine formulation
with (Toll-like receptor 9) adjuvant ((Heplisav)). However, its safety especially in
allogeneic HCT patients and its impact on GVHD has not been studied. Our Hepatitis B
vaccination policy parallels what is done for patients with chronic kidney disease or on
hemodialysis who are considered immunocompromised.
6-8

41
•
Smallpox vaccine is comprised of live vaccinia virus. Smallpox vaccination is
contraindicated in HCT recipients because it may result in development of generalized
vaccinia or inadvertent inoculation at other sites such as the face, eyelid, nose, mouth,
genitalia, and rectum. Smallpox vaccine should not be administered to any family
members or other persons who share living space with the patient during the first year after
transplant and beyond one year if the patient continues treatment with immunosuppressive
medications. If smallpox vaccination is administered to these close contacts, then these
individuals should be prevented from having close contact with the immunocompromised
HSCT recipient. See the CDC website for further detailed information
http://www.bt.cdc.gov.
•
Other live vaccines (i.e., BCG, oral polio, yellow fever, typhoid) should not be
administered in patients with active manifestation of GVHD or receiving
immunosuppressive therapy.
•
MMR or Varivax should not be given within 8 months of IVIG and VZIG.
9
•
Anthrax vaccine is an inactivated, cell-free filtrate vaccine (e.g., no dead or live bacteria in
the preparation). Currently, anthrax vaccination is not routinely recommended for anyone
except certain high-risk groups such as persons working directly with the organism in the
laboratory or certain military personnel. Recommendations for HSCT recipients would be
the same as for other at-risk individuals. Detailed information is available at the CDC
website http://www.bt.cdc.gov
Patients with splenectomy post transplant:
Vaccination recommendations for the post-SCT, post-splenectomy patient are the same as for
the HCT recipient who has an intact spleen (SEE LONG-TERM FOLLOW-UP AFTER
HEMATOPOIETIC STEM CELL TRANSPLANT, GENERAL GUIDELINES FOR
REFERRING PHYSICIANS, SECTION IX VACCINATIONS). Thus, a full series of
vaccination against pneumococcus with PCV20 (Prevnar20®), and against H. influenzae with
3 doses is particularly important. Antibody titers should be checked at least 8 weeks later to
ensure immunization responses.
Vaccination against Neisseria meningidtidis groups A, C, W, Y with two doses of MCV4
Menactra® or Menveo®, (if under 2 years old, discuss with ID) and against serogroup B if ≥ 10y
with two doses of Bexsero® is recommended. If Bexsero is unavailable, vaccination against
serogroup B with the Trumenba vaccine series could be considered, and requires 3
immunizations on a 0, 2, 6 month schedule. Patients should receive a complete series with a
single vaccine type (no mixing between Bexsero® and Trumenba®)
3
.
Re- Booster immunizations with MCV4 (Menactra® or Menveo®) and Bexsero® are
recommended every 5 years
2
and strep pneumonia as clinically indicated.
Note: For non-elective splenectomy, vaccination should begin at or after post-operative
Day 14. Post-transplant with PCV20, H. influenzae B and Neisseria meningidtidis groups
A, C, W, Y, MCV4, and also group B

42
IX. CHRONIC GRAFT-VERSUS-HOST DISEASE (GVHD)
Chronic GVHD is a major complication of allogeneic hematopoietic cell transplantation. The
incidence of chronic GVHD varies between 20 to 85% and depends on many factors such as the
transplant source (blood stem cell vs. marrow vs. umbilical cord), donor type and other
characteristics (previous pregnant female versus male donor), age (older vs. younger) and others
factors. Chronic GVHD syndrome has features resembling autoimmune and other immunologic
disorders such as scleroderma, Sjogren’s syndrome, primary biliary cirrhosis, wasting syndrome,
bronchiolitis obliterans, immune cytopenias, and chronic immunodeficiency. Symptoms usually
present within three years after allogeneic HCT and are often preceded by a history of acute
GVHD. Approximately 50% of patients who develop chronic GVHD are diagnosed by 6 months
after transplant.
Features of chronic GVHD can begin before day 100 after the transplant and manifestations that
are typical or “classical” of acute GVHD can develop or persist long after day 100. Moreover,
chronic and acute GVHD features may present simultaneously
[1,2]
. For this reason, the differential
diagnosis between acute and chronic GVHD cannot be made solely according to the time interval
from transplant
[3,4]
. Criteria to categorize acute and chronic GVHD by the chronic GVHD NIH
consensus working group is outlined in Table 1
[4]
. Helpful tips on how to assess and score chronic
GVHD can be found at http://www.fhcrc.org/ltfu by clicking on "Information for Physicians" in
the left hand navigation column. Then click on the right blue “GVHD Tips & Forms" button. Here
you will find the Chronic GVHD Assessment and Scoring form (Appendix D), Range of Motion
Assessment form (Appendix F), Skin Thickness Assessment form/ Rodnan Score for patients with
sclerosis or fasciitis (Appendix E) and other helpful information.
A. Table 1. Categories of acute and chronic GVHD
[4]
Category
Time of
symptoms
after HCT
or DLI
†
Presence
of Acute
GVHD
Features
Presence of
Chronic
GVHD
Features*
Acute GVHD
Classic acute GVHD
100 days
Yes
No
Persistent, recurrent or late onset
acute GVHD
> 100 days
Yes
No
Chronic GVHD
Classic chronic GVHD
No time limit
No
Yes
Overlap syndrome
No time limit
Yes
Yes
†
DLI (donor lymphocyte infusion)
* See Table 2 below

43
B. Table 2. Signs and Symptoms of chronic GVHD
[4]
ORGAN
OR SITE
DIAGNOSTIC
(Sufficient to establish
the diagnosis of chronic
GVHD)
DISTINCTIVE
(Seen in chronic GVHD, but
insufficient alone to establish a
diagnosis of chronic GVHD)
OTHER
FEATURES*
COMMON
(Seen with both
acute and
chronic GVHD)
Skin
● Poikiloderma
● Lichen planus-like
features
● Sclerotic features
● Morphea-like
features
● Lichen sclerosus-
like features
● Depigmentation
● Sweat impairment
● Ichthyosis
● Keratosis pilaris
● Hypopigmentation
● Hyperpigmentation
● Erythema
● Maculopapular
rash
● Pruritus
Nails
● Dystrophy
● Longitudinal ridging,
splitting or brittle features
● Onycholysis
● Pterygium unguis
● Nail loss** (usually
symmetric, affects most nails)
Scalp and
Body
Hair
● New onset of scarring or non-
scarring scalp alopecia, (after
recovery from
chemoradiotherapy)
● Scaling, papulosquamous
lesions
● Thinning scalp
hair, typically
patchy, coarse or
dull (not explained
by endocrine or
other causes),
● Premature gray hair
Mouth
● Lichen-type features
● Hyperkeratotic
plaques
● Restriction of mouth
opening from
sclerosis
● Xerostomia
● Mucocele
● Mucosal Atrophy
● Pseudomembranes**
● Ulcers**
● Gingivitis
● Mucositis
● Erythema
● Pain
Eyes
‡
● New onset dry, gritty, or
painful eyes
†
● Cicatricial conjunctivitis
● Keratoconjunctivitis sicca
†
• Confluent areas of punctate
keratopathy
● Photophobia
● Periorbital
hyperpigmentation
● Blepharitis
(erythema of the
eye lids with
edema)
Genitalia
● Lichen planus-like
features
● Vaginal scarring or
stenosis
• Erosions**
• Fissures**
• Ulcers**
GI Tract
• Esophageal web
• Strictures or stenosis in
the upper to mid third of
the esophagus**
• Exocrine
pancreatic
insufficiency
• Anorexia
• Nausea
• Vomiting
• Diarrhea
• Weight loss
• Failure to
thrive (infants
and children

44
ORGAN
OR SITE
DIAGNOSTIC
(Sufficient to establish
the diagnosis of chronic
GVHD)
DISTINCTIVE
(Seen in chronic GVHD, but
insufficient alone to establish a
diagnosis of chronic GVHD)
OTHER
FEATURES*
COMMON
(Seen with both
acute and
chronic GVHD)
Liver
• Total bilirubin,
alkaline
phosphatase >
2 x upper limit
of normal
†
● ALT or AST >
2x upper limit
of normal
†
Lung
● Bronchiolitis
obliterans diagnosed
with lung biopsy
• Bronchiolitis obliterans
diagnosed with PFTs and
radiology
†
• BOOP
Muscles,
Fascia,
Joints
• Fasciitis
• Joint stiffness or
contractures
secondary to sclerosis
• Myositis or
polymyositis
†
• Edema
• Muscle cramps
• Arthralgia or
arthritis
Hematopoietic
and Immune
• Thrombocytopenia
• Eosinophilia
• Lymphopenia
• Hypo- or hyper-
gammaglobulinemia
• Autoantibodies
(AIHA, ITP)
Other
• Pericardial or pleural
effusions
• Ascites
• Peripheral neuropathy
• Nephrotic syndrome
• Myasthenia gravis
• Cardiac conduction
abnormality or
cardiomyopathy
* Can be acknowledged as part of the chronic GVHD symptomatology if diagnosis is confirmed
** In all cases, infection, drug effect, malignancy or other causes must be excluded.
†
Diagnosis of chronic GVHD requires biopsy or radiology confirmation (or Ophthalmology exam for eyes).
‡
Schirmer’s test with a mean value < 5 mm (average of both eyes) at 5 minutes, or values of 6-10 mm in
patients who have sicca symptoms, or keratitis detected by slit lamp examination are used for the diagnosis of
chronic GVHD or the eyes (again other causes of dry eyes need to be ruled out (e.g., drug effect).
Abbreviations: GVHD (graft versus host disease); ALT (alanine aminotransferase); AST (aspartate
aminotransferase); BOOP (bronchiolitis obliterans organizing pneumonia); PFTs (pulmonary function tests);
AIHA (autoimmune hemolytic anemia); ITP (idiopathic thrombocytopenic purpura).
(continued) Table 2 - Signs and Symptoms of chronic GVHD
[4]
Table 2 - Signs and Symptoms of Chronic GVHD

45
C. How to diagnosis chronic GVHD
Signs and symptoms of chronic GVHD have been reviewed and reported by the NIH consensus
Working Group to standardize criteria for diagnosis and classification of chronic GVHD for the
purpose of clinical trials (Table 2)
[4]
. The diagnosis of chronic GVHD has no time limit and
requires the presence of at least one diagnostic clinical sign of chronic GVHD (e.g. poikiloderma
or esophageal web) or the presence of at least one distinctive manifestation (e.g.
keratoconjunctivitis sicca) confirmed by pertinent biopsy or other relevant tests in the same or
another organ (Table 2)
The criteria for the diagnosis of chronic GVHD include:
i. Distinction from acute GVHD (Table 1)
ii. Presence of at least one diagnostic clinical manifestation OR at least one distinct
manifestation confirmed by pertinent biopsy or other relevant tests (Table 2)
iii. Exclusion of other possible diagnosis for the clinical manifestation (e.g., infection, drug effect,
others)
D. How to score each organ/site severity with chronic GVHD (Appendix D)
The new scoring system (0-3) has been developed to describe the severity of chronic GVHD for
each organ or site taking functional impact into account
[4]
. Appendix D is a modified chronic
GVHD Scoring and Assessment form to help physicians to evaluate their patients with chronic
GVHD. Appendix E is another tool developed to help physicians to assess skin thickness in
patients with sclerotic features or fasciitis related to chronic GVHD.
E. How to assess overall severity of chronic GVHD - Global Assessment
Manifestations of chronic GVHD may be restricted to a single organ or tissue or may be
widespread. Historically, chronic GVHD was classified as “limited” or “extensive” based on a
small cohort patients reported more than two decades ago
[5]
. Because of inadequacies of the
original classification (e.g., difficulty to apply the historical criteria in patients transplanted with
newer HCT approaches and progress in our understanding of chronic GVHD), overtime, this
widely adopted chronic GVHD classification has proved to have limitation
[3,4]
. The new global
assessment of chronic GVHD severity (mild, moderate or severe) is based on numbers of
organs/sites involved and the degree of involvement in affected organs/sites (Table 3)
[4]
. This new
global assessment of chronic GVHD severity has been developed to replace the historical
“extensive/limited” classification.
Table 3. Global assessment of chronic GVHD severity
Global severity
No. organs/sites affected
Maximum score in all affected organ/site*
Mild
One or two (except lungs
‡
)
1
‡
Moderate
Three or more
or
1
‡
One or more
2
‡‡
Severe
Any
3
* See Appendix D.
‡
A lung score of 1 is considered moderate.
‡‡
A lung score of 2 or greater is considered severe.

46
F. Other laboratory testing and diagnostic indicators used in chronic GVHD
Biopsy (Skin, lip and other tissues). Histological confirmation is necessary in the
absence of diagnostic clinical features or distinctive features confirmed by other
pertinent test (Table 2). Nonetheless, diagnostic histological features of chronic
GVHD are uncommon.
Lung New obstructive lung defect may represent GVHD lung involvement if:
infectious process, asthma or recurrent aspiration from the sinuses or from
gastroesophageal reflux have been ruled out (Table 2 and Appendix D). In the
absence of prior history of chronic GVHD or concomitant GVHD in any other
organ, the diagnosis of bronchiolitis obliterans (BO) requires specific
spirometric criteria with negative workup for infection and evidence of signs of
bronchiolitis by high resolution end-expiratory and end-inspiratory CT scan of
the lungs, or confirmation by lung biopsy.
For information on monitoring of lung function post transplant and treatment of
bronchiolitis obliterans syndrome (BOS), see section I.
Esophagus Esophageal web formation, stricture or dysmotility demonstrated by barium
swallow, endoscopy or manometry.
Muscle Elevated CPK or aldolase, EMG findings consistent with myositis
with biopsy revealing no other etiological process.
Blood Thrombocytopenia (usually 20,000-100,000/microliter), eosinophilia
(> 500/microliter), hypogammaglobulinemia. Hypergammaglobulinemia and
autoantibodies occur in some cases.
G. Monitoring and other chronic GVHD information
Karnofsky or Lansky Clinical Performance scores <60%, >15% weight loss, and recurrent
infections are usually signs of poorly controlled chronic GVHD. Chronic GVHD can lead to
debilitating consequences, e.g., joint contractures, loss of sight, end-stage lung disease, or
mortality resulting from profound chronic immune suppression leading to recurrent or life-
threatening infections. Close monitoring is recommended after allogeneic HCT or donor
lymphocyte infusion so that appropriate treatment and supportive care can be instituted promptly
to prevent serious outcome.

47
H. Guidelines for treatment of chronic GVHD
We strongly recommend that you consult the LTFU office (Appendix A) before beginning treatment and
before making changes in immunosuppressive treatment for patients with chronic GVHD. Clinical trials
should always be considered because current standard therapies are associated with high morbidity and
decreased survival for patients with high risk chronic GVHD (Section X.A. 2).
Appendix D is a modified chronic GVHD Scoring and Assessment form to help physicians to evaluate
patients for chronic GVHD. Appendix E is another tool developed to help physicians to assess skin
thickness in patients with sclerotic features or fasciitis related to chronic GVHD. Appendix C provides a
cartoon with body area surface to help calculating the percentage of skin involved by GVHD.
Table 4 outlines the criteria currently used for indication of systemic therapy in patients diagnosed
with chronic GVHD according to global severity (Table 3) and risk factors.
Table 4. Indication for systemic treatment for chronic GVHD
Global severity
‡
High risk*
Prolonged systemic therapy
Mild
No
No
Mild
Yes
Yes
‡‡
Moderate
Yes or No
Yes
‡‡
Severe
Yes or No
Yes
‡
See Table 3
* Patients with either thrombocytopenia (<100,000/microliter) or receiving glucocorticoids at time of
diagnosis of chronic GVHD.
‡‡
The benefits of graft-versus-tumor effect and the risk of chronic GVHD require careful consideration
especially in patients transplanted for malignancy with high risk of relapse.
Standard treatment of chronic GVHD usually begins with administration of glucocorticoids
(1mg/kg/day) followed by taper to eventually reach an alternate-day regimen, with or
without daily cyclosporine or tacrolimus (FK506). For information on other medications
used for glucocorticoid-resistant or dependent chronic GVHD or in combination, telephone
consultation with the LTFU medical team is available to you, seven days a week, to discuss
appropriate treatment and provide other follow up recommendations (Appendix A).
The duration of systemic immunosuppressive treatment of chronic GVHD varies but requires at
least one year of therapy. Approximately 80% of patients require systemic immunosuppressive for
2 years and 40% of them requires therapy for at least 4 years.

48
I. Monitoring and Management of Bronchiolitis Obliterans Syndrome after HCT
Introduction
• Bronchiolitis obliterans syndrome (BOS) is a late non-infectious pulmonary complication that
affects 5.5% of allogeneic HCT recipients and 14% of those with chronic GVHD (7).
• BOS is the clinical correlate of obliterative bronchiolitis which is considered a pulmonary
manifestation of chronic GVHD.
• Lung function impairment is generally irreversible but may stabilize with treatment (8).
• The median time to BOS diagnosis is 1.5 years after HCT (8, 9) and 6 months after diagnosis of
chronic GHVD (10).
Definition of BOS after allogeneic HCT
A. Definition of BOS by NIH Consensus Guidelines (adapted from Reference 11)
1. Significant new obstructive change on spirometry:
a. Decrease of the absolute FEV
1
(mL) by 10% in comparison in prior 2 years or
pre-transplant baseline
b. FEV
1
is <75% predicted
c. FEV
1
/VC
1
ratio < 0.7 or FEV
1
/FVC <LLN
d. Meet criteria for obstruction (a-c) after bronchodilator challenge even if there is a
bronchodilator response
2. BOS according to severity is clarified as:
Mild or Asymptomatic = with mild FEV
1
decline (FEV
1
>70% predicted)
Moderate/severe or symptomatic = FEV
1
decline (FEV
1
<70% predicted)
3. Absence of other conditions that cause airflow obstruction including infection, asthma,
chronic obstructive pulmonary disease (COPD)
4. A history of chronic GHVD, or active chronic GVHD affecting other organs or presence
of a distinctive manifestation of chronic GVHD by 2015 NIH consensus criteria is highly
supportive of BOS if above criteria are met.
5. Other supportive findings:
a. Significant air-trapping: residual volume (RV) > 120%, or RV/TLC > 20% of
predicted value
b. Air-trapping or other features of bronchiolitis including centrilobular nodules,
airway thickening, or bronchiectasis noted on high resolution computed
tomography (HRCT).
B. Lung biopsy showing obliterative bronchiolitis may be required to make the diagnosis of lung
GVHD in patients with no prior history of chronic GVHD or other organ manifestations of
chronic GVHD for the purposes of enrollment into a clinical trial.
C. Diagnostic considerations for BOS:
1. Alternative spirometric phenotype (12)
a. Reduced FVC and FEV
1
b. Normal FEV
1
/FVC ratio
c. Normal TLC
2. Patients with baseline pretransplant supranormal FEV
1
:
a. FEV
1
decline >10 % (meets criteria 1a)
b. FEV
1
/VC <0.7 (meets criteria 1c)
c. FEV
1
>75% predicted (does not meet criteria 1b)
Monitoring of lung function after day +100 after allogeneic transplant
1
Slow VC, which is always greater than or equal to FVC, should be used for this calculation if available as per
ATS/ERS guidelines (13). Otherwise FVC is used.
49
A. Pulmonary function test (PFT) monitoring including spirometry, lung volumes, and DLCO.
1. PFTs for asymptomatic allo-HCT recipients:
a. At 6 months
b. At 1 year
c. Yearly thereafter until 5 years as clinically indicated
d. At diagnosis of chronic GVHD (14)
i. Full PFT testing including: spirometry, lung volumes, and DLCO
ii. Q3 months after diagnosis of chronic GVHD for at least one year.
(spirometry alone may be adequate)
iii. Thereafter, at Q6 months for 1 year (spirometry alone may be adequate)
iv. With at least yearly full PFT testing including: spirometry, lung volumes,
and DLCO until year 5 post HCT
Evaluation and monitoring of new airflow decline detected by PFTs
A. Pulmonary consult should be initiated.
B. New lung function decline:
Airflow obstruction is defined as decline in absolute FEV
1
>/=10%, with FEV
1
/VC <0.7. Lung
function decline may be due to obstructive, restrictive, or mixed processes.
a. Evaluate for upper respiratory infection or other etiologies of airflow decline
i. Nasal swab for respiratory virus PCR if indicated by symptoms
ii. Perform high resolution chest CT (HRCT)
o If there are infiltrates, consider bronchoscopy to evaluate for
infection
b. If diagnostic criteria for BOS are met → Start treatment promptly
c. If alternative diagnosis is made, repeat spirometry monthly for at least 3 months
i. If % FEV
1
stabilizes at 3 months, monitor PFTs every 3 months for one year
ii. If stable at 1 year, q6 month intervals for one year
iii. Thereafter, if stable, yearly.
C. High Resolution CT (HRCT):
1. Indication: Unexplained lung function changes and/or suspicion for BOS
2. Order with inspiratory and expiratory phases
3. Radiographic findings consistent with BOS (15, 16):
a. Mosaic attenuation (indicative of air-trapping)
b. Peripheral ground glass opacities or centrilobular ground glass opacities/nodules
c. Airway thickening or bronchiectasis (usually a late finding)
4. Patient may still have diagnosis of BOS with normal chest CT
D. Bronchoscopy is indicated when there are signs and symptoms of potential infection.
1. Clinical symptoms
Productive cough, fever, runny nose, sore throat
2. Imaging findings
Pulmonary infiltrate including ground glass opacities and/or new pulmonary nodules
Treatment of suspected or confirmed BOS (Figure 1)
A. Prior to specific BOS treatment, all confounding etiologies of airflow obstruction should be
investigated and treated. However, treatment for BOS should not be delayed if suspicion is
strong.
1. Infection: Diagnostic evaluation as directed by clinical symptoms include the following:
a. Sinus CT, nasal washes for respiratory virus PCR panel, sinus aspiration, CXR,
CT chest, sputum culture, bronchoalveolar lavage, and/or surgical lung biopsy.
2. Gastroesophageal reflux
a. Consider treating with proton pump inhibitor if not already on one
b. Lifestyle modifications including elevation of the head of bed

50
3. Post-nasal drip/sinus symptoms
a. Evaluate for URI
b. Evaluate for environmental allergies/triggers
c. Nasal saline, antihistamine, or steroid as needed
d. Consider ENT evaluation if chronic sinusitis is suspected
B. Initial Treatment
2
1. Initiate Fluticasone, azithromycin and montelukast (Singulair) (FAM) + Long-Acting
Beta-Agonist (LABA) (9,17,18)
a. FAM = Fluticasone (Flovent) 440 mcg BID + azithromycin 250mg po MWF +
montelukast (Singulair) 10mg po QD
b. LABA = long-acting beta2-agonist (such as salmeterol)
c. For FAM + LABA, inhaled corticosteroid (ICS)/LABA combination may be
prescribed in lieu of separate inhaled medications.
d. Inhaled corticosteroid combinations:
i. First choice: Symbicort HFA 160/4.5 mcg 2 inh BID
ii. Alternatives:
o Advair HFA 230/21mcg 2 inh BID
o Advair Diskus 500/50 mcg 1 inh BID
o Dulera 200/5 mcg 2 inh BID
o Breo Ellipta 200/25 mcg 1 inh QD
e. Treatment should continue without exacerbation after resolution of active chronic
GVHD, which is at least 6 months after discontinuation of all systemic
immunosuppressive treatments for other organ manifestations of chronic GVHD.
2. Prednisone
a. Asymptomatic with mild FEV
1
decline (FEV
1
>70% predicted): no new or
increase in prednisone
b. Symptomatic, or with moderate to severe FEV
1
decline (FEV
1
<70% predicted):
Start or increase prednisone to 1mg/kg/day x 2 weeks then taper (see below)
c. Other immunosuppressive treatments as indicated to control GVHD in other
organs.
d. After 2 weeks of therapy, begin taper over next 3 weeks to get down to a total
dose of 0.25mg/kg/day or to pre BOS therapy dose by week 5, as tolerated by
stability of FEV
1
and/or other organ manifestations of chronic GVHD.
e. If prednisone is not required, taper prednisone off within 6-8 weeks as tolerated
(including adrenal insufficiency issues).
C. PFT Monitoring during treatment of BOS
1. After initial diagnosis: Q4-6 weeks x 6 months (Qmonthly) while on prednisone taper.
2. If % FEV
1
stabilizes after 3 months, space out to q2-3 months for at least a year or longer
per pulmonary recommendations.
3. If % FEV
1
continues to decrease, see D below.
4. If % FEV
1
normalizes, see E below
D. Persistent FEV
1
decline despite initiation of above treatment (FEV
1
decline of >/= 10%):
1. Rule out infection or other confounding etiologies
2. Consider enrollment in a clinical trial
3. Consider extracorporeal photopheresis (ECP) or other immunosuppression therapies with
LTFU attending
4. If FEV
1
has stabilized, taper prednisone to 1mg/kg/day x 2 weeks and follow taper
schedule in section B.#2.
2
Dosages provided are for adult patients. For pediatric patients, please consult pharmacist for dosing.

51
E. After minimum 6 months of FAM and LABA therapy, a taper of BOS-specific medications can be
considered if all the following conditions are met:
a. Full PFTs with Lung volumes and DLCO remain stable or improved compared with BOS diagnosis
b. There are no new extrapulmonary manifestations of cGVHD requiring an addition or increase in
systemic immunosuppression
c. Patient is on a stable prednisone taper of <10mg/day equivalent
F. Taper Schedule
1. Full PFTs with Lung Volume and DLCO before starting taper.
2.
a. Step 1: D/C Azithromycin first. Ensure that Spirometry without lung volumens are stable over 3
months.
b. Step 2: D/C montelukast. Ensure that Spirometry without lung volumes is stable over 3 months.
c. Step 3: D/C LABA. If Spirometry without lung volumes is stable after stopping azithromycin and
montelukast, drop LABA component of ICS+LABA. This step may be skipped if the patient
prefers to remains on a combination inhaler (such as Symbicort).
d. Steps 4-6: If symptomatically stable after 1 month with stable Spirometry without lung volumes,
drop ICS dose by 50%. If Spirometry without lung volumes is stable after 1 month, continue
tapering ICS to off over 1-2 months.
e. Step 7:Full PFTs with lung volumes and DLCO 1 month after completion of FAM and LABA
therapy.
i. Follow FEV
1
closely with each step
ii. If FEV
1
is stable, then next step of taper can proceed.
iii. After FAM+LABA are off, check Spirometry without lung volumes at 1 month 3 months
and 6 months (assuming FEV1 is stable)
iv. Full PFTs with lung volumes and DLCO is recommended at least once a year.
3.
If FEV
1
decline of >10% occurs during taper:
a. Evaluate for respiratory infection, other exacerbating factors (GERD, post-nasal drip, new cGVHD
manifestations, restrictive lung disease)
b. If a reversible etiology is not identified, stop the taper and resume all components.
G. Supportive treatment
1. Vaccinations
2. Prophylactic antibiotics
3. Treat infections
4. Pulmonary rehabilitation
5. Supplemental oxygen if resting or ambulatory O2 sat </=88%
H. End-stage lung disease from BOS
1. Consider lung transplantation (19)
2. Discuss with UWMC Lung Transplantation service.
3. Basic criteria for referral for lung transplant includes
3
:
a. >2 years after HCT without evidence of malignancy
b. Life expectancy <2 years from respiratory failure
c. No other end-organ damage
d. No significant requirement for immunosuppression (prednisone < 20mg/qd
e. BMI >/= 18
f. Appropriate social support and compliance
For details on References, see Section XXV, References, Chronic GVHD
3
There is no specific FEV
1
criteria for lung transplant eligibility.

52
Figure 1. Schema for Treatment of Bronchiolitis Obliterans Syndrome (BOS) according to severity
A.
A. Suspected or
confirmed BOS
Mild or asymptomatic
1
Moderate/severe or
symptomatic
2
Start FAM
+LABA
No Prednisone
Start FAM
+LABA
+Prednisone
1mg/kg/d
Stable
Progression
Stable
Progression
Go to B
Continue
FAM + LABA
Continue
FAM + LABA
Taper prednisone
Go to B
1
Mild or Asymptomatic = with mild FEV
1
decline (FEV
1
>70% predicted)
2
Moderate/severe or symptomatic = FEV
1
decline (FEV
1
<70% predicted)
B.
B. Progression of BOS
on treatment
+Infection
No Infection
Treat Infection
Consider other
chronic GVHD
treatments
Inprovement
No Improvement
< 2 years from HCT
Prednisone > 20 mg/qd
> 2 years from HCT
Prednisone < 20 mg/qd
Continue
FAM + LABA
Taper prednisone
Supportive Care
Refer for Lung
Transplantation
Evaluate for
infection
Consider Clinical
Trial
Taper
prednisone
Progression to chronic
respiratory failure
Taper Prednisone

53
X. GENERAL GUIDELINES FOR PREVENTION OF OSTEOPOROSIS AND
GLUCOCORTICOSTEROID INDUCED OSTEOPOROSIS AFTER HCT
Treatment with glucocorticoids has been recognized as the primary risk factor for
development of osteoporosis after hematopoietic cell transplantation (HCT). Areas of loss
include the femoral neck, vertebrae, ribs. Glucocorticoid myopathy and muscle weakness
may contribute to osteoporosis by removing the normal forces on bone that are produced by
muscle contraction. In HCT recipients, other factors that may contribute to osteoporosis
include electrolyte imbalances, inactivity, significant weight loss, and endocrine deficiencies
(1).
Bone loss can be measured semi-quantitatively using a dual energy x-ray absorptiometry
(DEXA) scan which can compare bone mineral density (BMD) of an individual to an
appropriate normative population using a standard deviation score. BMD-standard deviation
scores have been determined for healthy 30 year old male and female Caucasians (T-scores)
or have been age adjusted (Z-score).
Osteopenia is defined as a bone mineral density T-score of –1 to –2.5 (standard deviations
below the peak mean density of young healthy controls). Osteoporosis is defined by a T-
score of <-2.5. It is also important to evaluate the individuals’ change in BMD over time
when determining appropriate interventions to optimize BMD.
T-scores are used to report bone mineral density for post-menopausal women (regardless of
age) and men >50 years. Z-scores are used to report bone marrow density in all children, pre-
menopausal women, and adult males < 50 years.
T-scores are less appropriate for the interpretation of pediatric DEXA scans, especially in the
very young children where BMD is confounded by normal growth and development.
Therefore, Z-scores are used with children since they are too young to have achieved peak
BMD. Z-scores obtained from the Hologic DEXA scanner (UWMC) for the spine are
available for ages >4 years. Z-scores for the femoral neck are limited to age >12 years. Z-
scores obtained from the General Electric Lunar DEXA scanner for the spine and total body
are available for ages 5 through 19 years. Z-scores
Management of osteopenia and osteoporosis at a minimum includes: (a) minimizing daily
and total cumulative glucocorticoid exposure, (b) optimizing calcium and vitamin D intake,
and (c) participating in weight-bearing exercise. Bone strengthening drugs including
bisphosphonate (5) may also be appropriate for some patients (2,3)
A. Patient Monitoring
Women: Annual measurement of FSH and estradiol for ages > 10 and < 61 years
Men: Annual measurement of:
LH, FSH, and free testosterone for ages ≥ 10 years and < 60 years,
Free testosterone for ages ≥ 60 years
Baseline and followup prostate exam, measurements of PSA and lipid profile in men who are
being treated with testosterone

54
All patients:
• Height: twice yearly
• Weight: with each clinic visit.
• DEXA SCANS:
a) 1-year after autologous HCT for lymphoma and myeloma in adults.
b) 1-year after allogeneic HCT in adults.
c) 1 year after allogeneic, or autologous-HCT in children
d) Continue annually after allogeneic HCT as clinically indicated for any patient on
steroid therapy >1 year posttransplant after completing initial DEXA scan at 1 year
• Vitamin D (25 Hydroxy) blood level
a) Should be checked at 1-year post transplant for all patients.
b) Are generally rechecked 2-3 months after beginning therapy and target to be within
normal range
• Patients treated with bisphosphonate or rank ligand inhibitors: Recommend liver
function tests, calcium, magnesium, creatinine and electrolytes be measured at baseline
and as clinically indicated.
B. Calcium Requirements
i. FOR PATIENTS ON STEROID THERAPY:
Calcium intake above these levels is not recommended, as it may interfere with the absorption of
other nutrients.
ii. FOR PATIENTS NOT ON STEROIDS
Age
Daily Minimum Requirement
after Transplant (milligrams)
Children 7-12 months
260
Children 1-3 years
700
Children 4-8 years
1000
Children 9-18 years
1300
Adult Males
1000-1200
Adult Females;
On hormone therapy
No hormone therapy
1000-1200
1500
Calcium intake above these levels is not recommended, as it may interfere with the absorption of
other nutrients.
Age
Daily Minimum Requirement
after Transplant (milligrams)
7-12 months:
600
1-3 years:
1000
4-8 years:
1200
> 9 years:
1500

55
C. Vitamin D Requirement
Table 3: Vitamin D3 (or D2) Supplementation
*,****
Adults (>18 yrs)
Children (<18 yrs)
Treatment of Insufficiency [Vitamin D (25 Hydroxy) levels 20-30 ng/mL] ***
▪ Routine
▪ 25 mcg/day
▪ Age < 1 yr:
─ 10 mcg daily
(20 mcg in dark skinned)
▪ Age 1-8 yr:
─ 15 mcg daily
▪ Age 9-18 yr:
─ 20 mcg daily
▪ Malabsorption syndromes**
▪ 1,250 mcg per week
▪ Age < 1 yr:
─ Consult Endocrinology
▪ Age 1-18 yr:
─ 1,250 mcg per week or
125 mcg daily
▪ Chronic Renal Disease
▪ Consult Nephrology
▪ Consult Nephrology
Treatment of Deficiency [Vitamin D (25 Hydroxy) level <20 ng/mL]***
▪ Uncomplicated
▪ 1,250 mcg per wk x 8 (Repeat
if Vitamin D (25 Hydroxy) level
< 30 ng/mL otherwise treat as
for insufficiency above)
▪ Age 1-12 months:
─ 25-50 mcg daily x 8 wks
▪ Age 1-18 yr:
─ 25-125 mcg daily x 8 wks
or
1,250 mcg weekly x 8
(Repeat if Vitamin D (25
Hydroxy) level < 30 ng/mL
otherwise treat as for
insufficiency above)
▪ Malabsorption syndromes**
▪ 250-1,250 mcg daily or every
other day
▪ UVB irradiation in patients
also with skin GVHD
▪ Age < 1 yr:
─ Consult Endocrinology
▪ Age 1-18 yr:
─ 1,250 mcg per week
▪ Chronic Renal Disease
▪ Consult Nephrology
▪ Consult Nephrology
*
Currently there does not seem to be substantive benefit by choosing Vitamin D2 or vitamin D3 over the other
with regard to correcting Vitamin D (25 Hydroxy) levels. The more important decision is prescribing enough.
Dose frequency appears to be less important than cumulative amount so that 50 mcg daily for 50 days is
approximately equivalent to giving 1,250 mcg monthly for 2 months.
**
Patients who remain deficient or insufficient after adequate therapy are generally treated with hydroxylated
vitamin D metabolites which are more readily absorbed or, if feasible, with sun or sunlamp exposure. While 25-
OH vitamin D (calcidiol) is the most logical choice of activated vitamin D for patients with liver disease,
calcidiol is not readily available in the U.S. The 1,25-OH activated formulation of vitamin D (Calcitriol) is used
most commonly in chronic renal disease when there is secondary hyperparathyroidism. Calcitriol can also be
used in patients with liver disease or severe malabsorption when there is a lack of the 25-OH vitamin D
substrate to be converted to 1,25-OH vitamin D by the kidney.
***
Vitamin D (25 Hydroxy) levels are generally rechecked 2-3 months after beginning therapy and the target level
should be within normal range.
****1000 IU = 25mcg and 50,000 IU = 1,250 mcg
56
D. Magnesium
Magnesium depletion results in cessation of bone growth, decreased osteoblast and
osteoclast activity. Hypomagnesemia may result in hypocalcemia, peripheral vitamin D
resistance and resistance to parathyroid hormone. Normal serum magnesium levels are
necessary to prevent osteopenia and bone fragility. Patients taking cyclosporine or
tacrolimus should receive adequate magnesium supplementation to maintain normal
concentrations of serum magnesium (see Section XX)
E. Exercise
An exercise program that combines weight bearing (in which bones and muscles work
against gravity as the feet and legs bear the body's weight) and muscle strengthening
exercise is recommended. It is advised that daily duration of these activities be increased
gradually. Thirty to 60 minutes daily has been recommended by the American Heart
Association. Specific time guidelines have not been established for maintenance of bone
density. However, exercise has been shown to minimize bone loss, strengthen skeletal
muscle and prevent falls by improving balance.
Recommended forms of exercise include low-impact walking, low-impact aerobics, stair
climbing, biking (on a stationary bike if the patient has poor balance), Nordic tracking, low
impact dancing or rowing. Weight-lifting can help to improve muscle mass and bone
strength. Speed and duration should be gradually increased. Although high impact exercise
improves bone density more quickly (running, jumping, etc.), it should be avoided during
steroid treatment due to potential harm caused by increased joint stress.
F. Lifestyle
Avoidance of smoking and excessive consumption of alcohol, caffeine, sucrose and animal
protein is recommended as these activities increase urinary calcium excretion and risk of
bone loss.
G. Gonadal hormone replacement
Females: FSH and estradiol levels should be tested annually for ages >10 and <61 years.
(see section XVI about gonadal hormone insufficiency recommendations)
Males: Free testosterone, FSH and LH serum levels should be evaluated as follows:
Male patients 10 and < 60 years: LH, FSH, and free testosterone levels
Male patients 60 years: Free testosterone levels
(see section XVI about gonadal hormone insufficiency recommendations)
Females:
• The use of hormonal therapy is not recommended as the first line of treatment or for
prevention of osteoporosis/osteopenia in women except for children or young adults.
• If estrogen replacement therapy (ERT) is started in an individual, the duration of
therapy should be individualized based on the clinical setting. A consultation is
recommended with the gynecologist.
• Systemic estrogen alone or combined with progesterone should not be prescribed for
patients with a history of thromboembolic diseases (i.e., venous thrombosis,
pulmonary embolism, strokes, etc.), hypercoagulation disorders, breast cancer,
coronary artery disease or active liver disease.

57
• Transdermal ERT if given is preferred owing to lower risks of thromboembolism
and stroke but like other forms of ERT, should not be used in patients with
unprovoked DVT.
• When ERT is prescribed for women with an intact uterus, low-dose progesterone is
added to prevent endometrial hyperplasia, despite the only slightly increased risk of
breast cancer.
Males:
• Male HCT survivors are at risk for developing hypogonadism which increases the
risk for reduced BMD and fractures.
• If the free serum testosterone level is low, symptoms of hypogonadism are present,
and there are no contraindications, including history or risk of prostate cancer,
testosterone replacement can be considered.
Children:
Gonadal hormone replacement in children needs to be coordinated with age-appropriate
linear growth and pubertal development. Pediatric Endocrinology consultation is advised
for additional work-up as indicated including assessment of gonadal and growth
hormones (See also Section G below).
H. Other treatments
An endocrinology consult may be appropriate for patients at high risk of osteoporosis and
those for whom pharmaceutical therapy is being considered. Therapies to reduce
osteoporosis may include:
Note: For bisphosphonate and rank ligand inhibitor therapy, we recommend adequate
calcium and Vitamin D supplementation.
1. Bisphosphonates are effective for prevention and treatment of post-menopausal and
glucocorticoid-induced osteoporosis (4, 5). Because the risks and benefits of
bisphosphonates during the early posttransplant period are unclear, consideration of
bisphosphonate therapy for osteoporosis is not recommended until at approximately 3
months posttransplant.
Adults with hip or vertebral fractures, or documented osteoporosis (DEXA T score < -
2.5) may receive either oral or intravenous bisphosphonate therapy. Therapy is also
advised for posttransplant patients with osteopenia (T-score -1.0 to -2.5) who are not
receiving hormone replacement therapy and who are to receive prolonged glucocorticoid
therapy. For postmenopausal women, and men age 50 and over, the widely used FRAX®
WHO Fracture Risk Assessment Tool (http://www.shef.ac.uk/FRAX/) can be used to
help guide which patients with osteopenia might benefit from bisphosphonate therapy
based on their estimated 10-year hip fracture probability being ≥ 3% or their 10-year
major osteoporosis related fracture probability being ≥ 20%.
Therapy is usually continued until glucocorticoid therapy has been discontinued and the T-
score enters the normal range (-1.0 to +1.0) or the risk for fractures based on the FRAX®
tool is no longer increased.

58
In patients taking alendronate for 5 years or more, post-marketing reports have recently
highlighted the occurrence of atypical hip fractures (6). Secondary analyses of the results
from 3 large randomized bisphosphonate trials showed that rates of subtrochanteric or
diaphyseal femoral fractures were very low (1 to 6 cases per 10,000 patient years). While
these analyses did not demonstrate an increase in risk associated with bisphosphonate
use, the study was underpowered for definitive conclusions (7). One approach to consider
for patients at mild risk for fracture is to stop bisphosphonate therapy after 3 to 5 years
and remain off as long as bone mineral density is stable and no fractures occur. Higher
risk patients may be treated longer than 3 to 5 years as clinically indicated and consider
referral to endocrinology for alternative therapy (6).
Children with low bone mineral density (BMD) should be considered for referral to pediatric
endocrinology if they:
a) develop a fracture in the setting of low bone mineral density,
b) have ongoing risk factors for low BMD and/or avascular necrosis (AVN) like steroid
therapy or chronic GVHD , hypogonadism or growth hormone deficiency.
The Pediatric Oncologist and Pediatric Endocrinologist will jointly determine the need for
bisphosphonate therapy. Pediatric Endocrinology will initiate additional work-up as
indicated including assessment of gonadal and growth hormones. In children, initiation of
hormonal therapy may precede bisphosphonate therapy in the appropriate clinical setting.
Children should have an EKG and formal dental evaluation prior to initiation of
bisphosphonate therapy.
For All Patients
• Intravenous bisphosphonates are not recommended for patients with creatinine
clearance <35 ml/minute.
• Oral bisphosphonate therapy can cause esophageal ulceration (pill esophagitis) and
should be discontinued if patients develop esophageal symptoms.
• Due to increased risk of AFF (Atypical Femoral Fractures) and MRO (Osteonecrosis of
the jaw) with prolonged bisphosphonate therapy, after 3 to 5 years of treatment
reassess the risks and benefits of continuing therapy, pursuing a drug holiday or
referring to Endocrinology for consideration of alternative treatment.
Commonly used bisphosphates include:
For Adults
i. Alendronate (Fosamax
)
Osteoporosis treatment: Administer alendronate as a single dose of 70 mg
weekly (or 35 mg twice weekly).
ii. Risedronate (Actonel
)
Osteoporosis treatment: Administer risedronate as a single dose of 35 mg
weekly (or 150 mg monthly).
iii. Pamidronate (Aredia
)
59
Pamidronate has been used primarily in patients who cannot receive oral
bisphosphonates. In adults a regimen of 60 mg IV for the first dose followed
by 30 mg every 3 months has been used successfully in the nontransplant
setting.
iv. Zoledronate (Reclast®)
Zoledronate may be given as a single 5 mg intravenous dose once a year.
For Children
Drug selection and dosing of bisphosphonate therapy will be determined by
Pediatric Endocrinologist
2. Rank Ligand Inhibitor
Rank Ligand Inhibitors: Denosumab (Prolia®) 60 mg SQ every 6 months for adult
osteoporosis. Denosumab has not been studied to treat osteoporosis in children.
Strongly recommend an endocrinology consult prior to starting rank ligand
inhibitors. Severe hypocalcemia can be seen in patients with renal dysfunction.
Monitor for infection at injection site in patients on immunosuppressive therapy.
Because there is an increased risk for vertebral fracture with discontinuation or
missed doses of denosumab (8, 9), if you are considering discontinuing the drug, we
highly recommend getting an endocrinology consult first.
3. Calcitonin
Calcitonin is secondary therapy for osteoporosis Calcitonin (100-200 International
Units nasal spray daily) may be given if bisphosphonates are inadequate or
contraindicated. There are no data to support the use of calcitonin (salmon) nasal
spray in children. Calcitonin may be given if bisphosphonate of Rank Ligand
Inhibitors are inadequate or contraindicated. Recommend getting an endocrinology
consult prior to starting Calcitonin therapy.
4. Low Sodium Diet
Sodium increases urinary calcium loss. A reduced sodium diet (<4 grams daily) is
encouraged during steroid therapy.
5. Endocrinology
Refer for endocrinology consult if clinically indicated.
60
XII. HYPERLIPIDEMIA
The syndrome of abdominal obesity, dyslipidemia, hypertension, insulin resistance and
prothrombotic or inflammatory states (metabolic syndrome) is a risk factor for premature
cardiovascular disease. By itself, chronically elevated serum low-density lipoprotein cholesterol
(LDL-C) is also strongly associated with premature cardiovascular disease (< age 55 years) in
the general population. Hyperlipidemia is also associated with reduced survival in the recipients
of solid organ transplants. Chronic immunosuppressive therapy (IST) in hematopoietic cell
transplantation (HCT) or organ transplant recipients may aggravate pre- existing risk factors for
premature cardiovascular disease, or promote development of new risk factors, notably
hyperlipidemia and hypertension. Even after discontinuation of IST, the long-term survivors of
allogeneic HCT appear to be at increased risk relative to their siblings for developing diabetes
and hypertension. Adjustment was made in the analysis for age and gender, and the observation
is independent of obesity.
1
Based on a retrospective analysis at the Fred Hutch more than half of 349 HCT recipients had
serum cholesterol >200 mg/dL at 75-100 days after HCT. Median cholesterol and triglyceride
levels increased relative to before transplant by 34% and 65% respectively in adults, and 45%
and 125% in children. Marked elevations of serum triglycerides (>750 mg/dL) were observed in
4.8% of adults and 8.1% of children. The prevalence of premature cardiovascular disease after
HCT has not been determined but recent case reports have described premature and fatal
coronary artery disease (CAD) in HCT recipients.
6-10
At least 30 patients who received HCT at
the median age of 35 years (range 4-52 years) at Fred Hutch (08/73-05/98) died at a median of
7.5 years after the transplant due to CAD or heart failure of unspecified etiology. Hyperlipidemia
was present in the majority of patients who had serum lipids levels documented beyond Day 90.
Looking to the future, because the earliest successful HCT were performed in younger patients
just over 40 years ago, it is possible that the prevalence of premature CAD might increase as
earlier transplant survivors mature.
HMG-CoA reductase inhibitors (statins) effectively reduce serum total cholesterol, protect
against premature cardiovascular disease, and improve survival in adults with a wide range of
cholesterol levels whether or not they have a history of coronary artery disease.
2-5
Statin therapy
has been safely administered to solid organ transplant recipients, it has been effective at lowering
serum lipid levels, and appears to protect against premature cardiovascular disease and improve
survival.
11-19
Similar benefits could be expected in HCT recipients with hyperlipidemia.
Pleiotropic effects of statins suggest potential additional roles in mediating improved renal
function, control of hypertension, osteopenia, avascular necrosis, and even control of GVHD.
20-28
The following general guidelines begin with therapeutic lifestyle changes before drug
therapies, in accordance with Adult Treatment Panel III/National Cholesterol Education
Program (ATPIII/NCEP) guidelines for the management of hyperlipidemia in the general
population.
30-31
The risk benefit ratio of drug therapy always needs to be considered and should be
individualized.
A. Working Definitions of Fasting Hyperlipidemia

61
1. Fasting serum LDL-C > 130 mg/dL or
2. Fasting total cholesterol minus fasting HDL-C >160 and fasting serum triglycerides >
200 mg/dL or
3. Fasting serum triglycerides > 500 mg/dL if >18 years old and > 400mg/dL if ≤18 years
old
35
or
4. High-risk or very high-risk category patients with fasting serum LDL-C > 100 mg/dL
Table 1: ATP III Risk Categories and Definitions**
29
**Electronic 10-year risk calculators are available at https://www.nhlbi.nih.gov/files/docs/guidelines/atglance.pdf
Risk category
Definitions
Very High Risk
1. Established cardiovascular disease and > 2 major risk factors
2. Severe and poorly controlled risk factors,
3. Multiple risk factors of the metabolic syndrome
4. An acute coronary syndrome
High-Risk
(10 yr risk >20%)
CHD or CHD risk equivalents
Moderately High Risk
(10 yr risk 10-20%)
2+ risk factors
Moderate Risk (10 yr
risk < 10%)
2+ risk factors
Low-Risk**
0-1 risk factors
CHD
History of myocardial infarction, stable angina, coronary artery
procedures (angioplasty or bypass surgery) or evidence of clinically
significant myocardial ischemia.
CHD Risk Equivalents
Clinical manifestations of non-coronary forms of atherosclerotic
disease (peripheral arterial disease, abdominal aortic aneurysm and
carotid artery disease), diabetes, and 2+ risk factors.
Metabolic Syndrome
1. Abdominal obesity
2. Elevated triglycerides, small LDL particles and low HDL
3. Hypertension
4. Insulin resistance
5. Prothrombotic and proinflammatory states
Risk Factors
1. Cigarette smoking
2. Hypertension (BP >140/90 mmHg) or on antihypertensive
medication
3. Low HDL cholesterol <40 ml/dL
4. Family History of premature CHD in male first-degree
relative < 55 years of age
5. CHD in female first-degree relative < 65 years of age
6. Age (men > 45 years; women > 55 years)
62
B. General Guidelines for Management of Hyperlipidemia in HCT Patients
1. Diet: If clinically appropriate, reduce daily fat: saturated fat <7% calories, cholesterol <
200 mg/day [NCEP] or <300 mg /day (American Heart Association).
2. Omega-3-fatty acid supplements may improve triglyceride and LDL-C levels but most
are not regulated and are of variable content. Therefore, consuming a diet rich in these
fatty acids is currently the preferable method of supplementation (major sources include
flaxseed oil, canola oil, walnut oil, wheat germ, soybeans, mackerel, herring, salmon,
sardines in oil, and swordfish).
3. Weight management
4. Regular exercise regimen.
5. Exclude untreated hypothyroidism.
6. Exclude nephrotic syndrome.
7. Exclude obstructive liver disease..
If patient has high CHD risk treat dyslipidemia also with appropriate drugs. If a patient has low to
moderate CHD risk, consider drug therapy based on severity of dyslipidemia, estimated prognosis after
transplant and risk of lipid lowering drug therapy. In patients with low CHD risk that develop secondary
dyslipidemia this must likely can be managed conservatively if immunosuppressive therapy can be
tapered off. Patients with low and moderate risk though with serum triglycerides >500 mg/dL should be
treated to prevent pancreatitis.
C. Important Prescribing Precautions for Hyperlipidemia
Statins are the most widely used class of drugs, but proper selection of statin preparation and
dose are important, as a number of drugs used specifically in the HCT setting can interact with
them. Cyclosporine’s metabolism is by the cytochrome CYP3A4 a key factor in drug-drug
interactions, as it raises levels of statins (for example lovastatin, simvastatin and atorvastatin)
also metabolized by this pathway and thus increases the risk for myopathy
32
. Tacrolimus and
sirolimus also appear to be metabolized by his pathway
33
. Cyclosporine can also increase statin
drug levels through inhibition of the member transport OATP1B1. Consequently, cyclosporine
potentially increases the risk for toxicity of any statin
34
. Other inhibitors of CYP3A4 including
azole antifungals, non-dihydropyridine calcium channel blockers and macrolide antibiotics also
can interact with statins. For other drugs like Ruxolitinib that can impact CYP3A4 metabolism,
contact pharmacy. Since pravastatin, rosuvastatin and fluvastatin are metabolized by
alternative pathways, these statins may be better choices for patients requiring
coadministration of CYP3A4 inhibitory agents.
NOTE: Toxicity may be increased in patients treated with calcineurin inhibitors,
Ruxolitinib, sirolimus, antifungal azoles, or macrolide antibiotics. Patients on these
medications should be started on the lowest dose of statin or fibrate therapy to limit
toxicity. Patients coming to transplant on hyperlipidemia treatment should have their doses
of statin or fibrate therapy reduced prior to start of calcineurin inhibitors, Ruxolitinib,
sirolimus or antifungal azole therapy.

63
Toxicity related to statins should be discussed before starting therapy:
1. Liver enzyme abnormalities.
2. Rhabdomyolysis with associated renal failure
3. Onset of toxicity may occur weeks to months after initiation of treatment
4. Combination fibrate-statin therapy can be medically appropriate but may increase the
incidence of myopathy.
5. Patients should be advised to report immediately unexplained muscle pain, tenderness,
or weakness, especially when accompanied by fever or malaise.
D. Intervention for Elevated LDL-C with Minimal Elevation of Triglycerides
Any patient who has lifestyle-related risk factors (e.g., obesity, physical inactivity, elevated
triglyceride, low HDL-C, or metabolic syndrome) is a candidate for therapeutic lifestyle changes
to modify these risk factors regardless of LDL-C level.
TABLE 2. ATP III LDL-C Goals and Cut points for TLC and Drug Therapy in
Different Risk Categories and Proposed Modifications (adapted from reference 29) and
Based on Recent Clinical Trial Evidence
Risk Category
LDL-C Goal
Recommendations for Drug
Therapy**
Very high risk
< 70 mg/dL
> 100 mg/dL††
High risk
< 100 mg/dL
> 100 mg/dL††
Moderately high risk
< 130 mg/dL
> 130 mg/dL
Moderate risk
< 130 mg/dL
> 130 mg/dL
Low risk
< 160 mg/dL
> 160 mg/dL
**When LDL-lowering drug therapy is employed, it is advised that intensity of therapy be sufficient to achieve at least a 30% to 40% reduction in
LDL-C levels.
††If a high-risk person has high triglycerides or low HDL-C, combining a fibrate or nicotinic acid with an LDL-lowering drug can be considered.
For persistent and clinically significant elevations of fasting serum LDL-C who have not
responded sufficiently to therapeutic lifestyle changes, treatment with any of the following
statins in Table 3 may be considered.

64
Table 3. Suggested Medication Options for High LDL-C in Adults* after BMT
Drug
Daily Dose
mg
Class Effects
Precautions
Statins (HMG-CoA
reductase inhibitors)
Start at lowest
doses and rarely
exceed middle of
the dose range
when taking
concomitantly
calcineurin
inhibitors.
LDL 18-55%
HDL 5-15%
TG 7-30%
• Contraindicated in liver disease
• Counsel patient to report muscle pain,
weakness, dark or cola-colored urine,
especially when accompanied by fever
and malaise.
• If myopathy or rhabdomyolysis is
suspected, or if AST/ALT are
significantly elevated stop therapy and
check CK and creatinine.
• Toxicities may occur weeks to many
months after starting therapy.
• Toxicity may be increased in
patients treated with calcineurin
inhibitors, Ruxolitinib,
sirolimus, antifungal azoles, or
macrolide antibiotics. Patients
on these medications should be
started on the lowest dose of
statin therapy to limit toxicity
• Atorvastatin
(Lipitor)
10-80
• Pravastatin
(Pravachol)
10-40
• Simvastatin (Zocor)
5-40
• Rosuvastatin
(Crestor)
5-40
NOTE: Pediatric patients refer to hyperlipidemia specialty clinic.
E. Medical Intervention for Mixed Hyperlipidemia
1. For persistent and clinically significant elevations of fasting serum LDL-C and
triglycerides who have not responded sufficiently to therapeutic lifestyle changes, it is
reasonable to consider initial treatment with a statin.
2. If statin therapy alone does not result in a satisfactory lowering of both LDL-C and
triglycerides then consideration of combination therapy with either a fibrate or ezetimibe
is recommended through consultation with a subspecialty hyperlipidemia clinic,
particularly for children.
F. Medical Intervention for Isolated Hypertriglyceridemia
Fasting serum triglycerides > 800 mg/dL may increase the risk for acute pancreatitis.
Treatment with either of the following fibrates, omega-3-fatty acids, or icosapent ethyl
may be considered at > 500 mg/dL of fasting serum triglycerides.
Fibrates reduce triglycerides by 20-50%. Potential side effects of fibrates include
cholelithiasis, GI upset and myopathy. Risk for myopathy increases when fibrates are
65
Table 4: Triglycerides Lowering Agent for Adult Patients**
Drug
Daily Dose
mg
Class
Effects
Precautions and Monitoring
Omega-3-Acid
Ethyl Esters
a
• Lovaza
4000 Daily
OR
2000 BID
LDL may
HDL 9%
TG 45%
VLDL40%
• Generally minimal side effects, eructation,
dyspepsia
• May potentiate INR if on warfarin
• Avoid if fish/shellfish allergic
• Monitor AST/ALT periodically
• Has been combined with simvastatin for mixed
hyperlipidemia
Fibric Acids
• Fenofibrate
(Tricor)
• Gemfibrozil
(Lopid)
Start at lowest
doses and
rarely exceed
middle of the
dose range
when taking
concomitantly
calcineurin
inhibitors.
48-145
600-1200
LDL 5-20%
HDL 10-20%
TG 20-50%
• Contraindicated in severe liver or renal disease
• May cause myopathy especially when combined
with statins, and in setting of impaired renal
function in patients receiving cyclosporine or
other drugs that interact with statins
• May cause cholelithiasis and GI symptoms
• May cause reversible increase in serum creatinine
• Fenofibrate-statin combination may be better that
gemofribrozil-statin therapy because gemfibrozil
can increase statin levels by 2-6 fold
• Counsel patient to report muscle pain, weakness,
dark or cola-colored urine, especially when
accompanied by fever and malaise.
• If myopathy or rhabdomyolysis is suspected, or if
AST/ALT are significantly elevated stop therapy
and check CK and creatinine.
• Toxicities may occur weeks to many months after
starting therapy.
a
Note over the counter omega-3-acid ethyl esters are generally insufficient to significantly lower
triglycerides and VLDLs. Only Lovaza® has been approved for this indication.
**In patients with severe thrombocytopenia, recommend give lower doses.
NOTE: Pediatric patients refer to hyperlipidemia specialty clinic.

66
Table 5: Summary for Recommendations for Managing Hyperlipidemia
1.
Exclude untreated hypothyroidism, nephrotic syndrome or obstructive liver disease
2.
Adjust Diet to be high in fiber, (fruits, vegetables, whole grains), high in polyunsaturated and
monounsaturated fats and low in saturated fat and devoid of trans fat
Consider referral to dietitian
Add omega 3 fatty acid supplements
3.
Determine Risk of CHD (see Table 1)
a)
If high or very high CHD risk, consider drug therapy
b)
If low to moderate CHD risk, consider drug therapy based on dyslipidemia, estimated
prognosis of treatment, and risk of statins.
c)
If low risk CHD and immunosuppressive therapy can be tapered off, manage conservatively
4.
Assess LDL-C and TG levels to help determine drug therapy.
a)
If elevated LDL-C with minimal elevated TG, statin therapy (Pravastatin, rosuvastatin,
and fluvastatin) preferred because of drug-drug interactions with statins with
calcineurin inhibitors, Ruxolitinib, sirolimus, or antifungal azole therapy. If starting
drug, begin dosing at lowest dose and monitor carefully. If already on drug, consider dose
reducing statins.
b)
If mixed hyperlipidemia and on statin that fails to lower both LDC-C and TG
Add fibrate or ezetimibe
Consider Hyperlipidemia consult
c)
If isolated hypertriglyceridemia (>500 mg/dL), fibrate therapy for adults. For children, refer
to hyperlipidemia specialty clinic.
5.
Begin long term plan for:
Weight management
Regular exercise program
G. Monitoring during treatment with statins or fibrates:
Table 6: Monitoring
CK measure if clinically indicated (i.e. symptoms of myalgia, muscle weakness, etc, develop).
LFT’s at baseline, 2 and 4 weeks after start therapy and monthly while on therapy.
Stop therapy for significantly elevated serum transaminase or if symptoms of myositis or
rhabdomyolysis occur.
1. Serum creatine kinase (CK) should be checked when clinically indicated (i.e. when symptoms
such as myalgia, muscle weakness, etc. develop).
2. Doses of statins or fibrates may be adjusted at four-week intervals as needed.
3. Consultation with a subspecialty hyperlipidemia clinic is generally recommended in patients
taking concomitant immunosuppressive therapy who do not respond adequately to the above
measures.
4. Patients should be advised to report immediately any unexplained muscle pain, tenderness, or
weakness, especially if accompanied by malaise or fever.
5. Statin or fibrate therapy should be withdrawn if serum transaminase concentrations are
significantly elevated or if symptoms of myositis or rhabdomyolysis occur.
6. Liver function tests (LFT) levels should be checked at baseline and at 2 and 4 weeks after
starting statin or fibrate therapy and at least monthly while on immunosuppressive therapy.

67
XIII. HYPERTENSION
New onset or aggravation of hypertension occurs frequently after hematopoietic cell
transplantation (HCT) with the most common cause of hypertension after allogeneic HCT being
due to treatment with glucorticoids and tacrolimus or cyclosporine. It is important to recognize
also that HCT survivors have a high prevalence metabolic syndrome which represents a cluster
of risk conditions associated with premature coronary heart disease (CHD).
1
Components of the
metabolic syndrome including hypertension, dyslipidemia, and diabetes occurred with higher
cumulative incidence among HCT survivors compared to a randomly selected matched control.
2
Thus, adequate control of hypertension is strongly recommended in HCT recipients to minimize
target organ damage and most importantly in the brain, heart and kidneys.
A. Key Points about Hypertension and its treatment
• In uncomplicated hypertension, without diabetes mellitus, renal dysfunction or
cardiac dysfunction the blood pressure (BP) goals are indicated in the table
below
Age (y)
Male
Female
≥18
140/90
140/90
17
132/82
125/80
16
130/80
124/80
15
127/79
123/79
14
125/78
122/78
13
122/77
121/77
12
120/76
119/76
11
117/76
117/75
10
115/75
115/74
9
114/75
113/73
8
112/73
111/72
7
111/72
109/71
6
110/70
108/70
5
108/68
106/68
4
107/65
104/66
3
105/61
103/63
2
102/57
101/59
1
99/52
100/54
Pediatric data based on 90
th
percentile limits for blood pressure at
The 50
th
percentile for height (1999-2000 NHANES)
• If an adult patient has a diagnosis of diabetes and/or renal dysfunction, the BP goal is
< 130/80 mm HG. If an adult patient has more than 1 gm of proteinuria, the BP goal is
< 125/75 mm HG.
B. Other key points about control of hypertension and treatment:
• Reductions in myocardial infarctions, stroke incidence and heart failure with BP
lowering below 140/90 mm HG are approximately 25%, 35%, and 50%, respectively.
• Patients with SBP > 160 mm HG and/or DBP > 100 mm HG tend to need two
different agents and it is recommended that two agents are begun at the same time.

68
• Caffeine intake and nicotine use an hour before blood pressure monitoring may give
falsely elevated readings.
• Referral to a hypertension specialist is advised for patients with poorly controlled
blood pressure.
• In the general population, thiazide diuretics should be used in drug treatment for most
patients with uncomplicated hypertension, alone or combined with drugs from other
classes but the potential of thiazides to aggravate pre-renal azotemia and other
electrolyte abnormalities often limit their use in HCT.
• No single class of drugs has emerged as the standard of care for management of
hypertension in patients receiving calcineurin inhibitors (CNI). Other agents may be
indicated for patients with other co-morbidities (see Table 1).
Table 1 - Antihypertensive Medications According to Clinical Setting
Clinical Setting
Anti-Hypertensive Therapy
Monitoring
Uncomplicated
Hypertension
Options include CCB, beta-
blockers, thiazide diuretics,
ACE-I** or ARBs
• If not on a CNI or at risk for volume depletion,
thiazide diuretics are the treatment of choice. If used
with CNI, limit dose to 12.5-25 mg per day to limit most
metabolic side effects.
• Calcium Channel Blockers (CCB) can affect CNI levels
(cyclosporine and tacrolimus). Check CNI levels with
K and Cr 7-10 days after starting CCB.
• Non-dihydropyridine CCBs (e.g. verapamil, diltiazem)
may potentiate the toxicity of CNI, statins and fibrates
• CCB may worsen proteinuria
• Beta-blockers may diminish sympathetic activity
including CNI induced headaches/migraines and
tachyarrhythmias.
Chronic kidney
disease*, history of
AKI, presence of
proteinuria or
microalbuminuria
(see Table 2)
• ACE-I**/ARB,
• Possibly in combination with CCB if still on CNI.
• Avoid CCB alone due to further increase in proteinuria
• Consider holding during persistent diarrhea, vomiting
or poor fluid intake
• Check serum K and Cr 7-10 days after adding
Diabetes
With or without
proteinuria
Angiotensin converting
enzyme inhibitors (ACE-I**)
or angiotensin II receptor
blockers (ARBs)
• No known interactions with CNI.
• May aggravate hyperkalemia and prerenal azotemia;
avoid in patients with or at risk for volume depletion.
Consider holding during persistent diarrhea, vomiting
or poor fluid intake
• Check serum K and Cr 7-10 days after adding
Heart Failure
• Diuretics
• ACE-I** or ARBs
• Beta-blockers
• Careful to avoid pre-renal azotemia with potent loop
diuretics.
• Consider adding spironolactone or eplerenone if no
hyperkalemia but monitor for subsequent hyperkalemia.
• Carvedilol and metoprolol are beta-blockers of choice
• For those unable to tolerate ACE-I and ARB’s, therapy
with hydralazine plus isosorbide may be beneficial,
particularly in African Americans

69
Table 1 - Antihypertensive Medications According to Clinical Setting (continued)
Clinical Setting
Anti-Hypertensive Therapy
Monitoring
High-risk for
Coronary Artery
Disease
• ACE-I**, ARBs,
calcium channel blockers
and beta-blockers.
• Diuretic may also be indicated based on risk/benefits
profile
• Calcium Channel Blockers (CCB) can affect CNI levels
(cyclosporine and tacrolimus). Check CNI levels with
K and Cr 7-10 days after starting CCB.
Ischemic Heart
Disease
• Beta blockers
• Carvedilol and metoprolol are the beta-blockers of
choice
History of
Myocardial
Infarction
• ACE-I**, aldosterone
antagonists and the beta-
blockers carvedilol or
metoprolol are indicated.
• Consider adding spironolactone or eplerenone if
hyperkalemia is not present
History of Strokes
• Calcium channel
blockers, thiazides or
ARB.
• Calcium Channel Blockers (CCB) can affect CNI levels
(cyclosporine and tacrolimus). Check CNI levels with
K and Cr 7-10 days after starting CCB.
Hypertensive
Urgency not
requiring
hospitalization
• Clonidine
• Labetatlol
• Hydralazine
• Preferred option is to
consult a hypertension
expert
• Clonidine has rapid onset of action, can cause dry mouth
and somnolence; avoid for general use
• Hydralazine can cause edema and tachycardia
• Evaluate patient every 1-3 days to assess response to
therapy
CCB; calcium channel blockers,
* Definition of chronic kidney disease (CKD) criteria
1. Kidney damage for > 3 months, as defined by structural or functional abnormalities of the kidney, with or
without decreased GFR, manifest by either:
• Pathological abnormalities; or
• Markers of kidney damage, including abnormalities in the composition of the blood or urine, or
abnormalities in imaging tests
2. GFR < 60 mL/min/1.73 m
2
for > 3 months, with or without kidney damage
**Due to rare, potential complication of angioedema, caution should be exercised with use of
ACE-1 inhibitors in combination with sirolimus. Use of ARB is acceptable.
C. Evaluation for microalbuminuria and additional recommendations
Screening for microalbuminuria before and after transplant is helpful for early diagnosis of
proteinuria and to guide treatment. Microalbuminuria is determined by measuring the
albumin and creatinine ratio in an urine sample.

70
Table 2. Recommendations based on albumin/creatinine ratio and hypertension
Spot Urine
Albumin/creatinine ratio
(U
ACR
)
Interpretation
Recommendations
Less 30 mg/g
Normal
– Repeat U
ACR
in 1 year
30-300 mg/g
without hypertension and
not on hypertensive
medications
Abnormal
– Repeat U
ACR
in 3-6 months
30-300 mg/g
with hypertension and on
hypertensive medications
Abnormal
– If not already on, consider change to
ACE-I**or ARB therapy
– Repeat U
ACR
in 3-6 months
Greater than 300 mg/g
on hypertensive
medications
Abnormal
– If not already on, consider treating
with ACE-I**or ARB therapy
– Quantify 24-hr total urine protein
– If proteinuria (>1 gram) confirmed,
refer to nephrologist
– Monitor spot U
ACR
in 3 months
**Due to rare, potential complication of angioedema, caution should be exercised with use of
ACE-1 inhibitors in combination with sirolimus. Use of ARB is acceptable.
71
XIV. RECURRENT MALIGNANCY
In most cases recurrent malignancy occurs within the first 2 years after the transplant, with
few occurring more than 5 years after the transplant.
For patients who had leukemia or other hematological malignancies, peripheral blood counts
should be monitored at least monthly for the first year. Monitoring for minimal residual
disease and recurrent malignancy will vary according to the specific disease and enrollment
in specific protocols. Chimerism testing in blood or bone marrow may be needed to help
establish the diagnosis of recurrent malignancy and to assess options for treatment (adoptive
immunotherapy, biologic response modifiers, gene therapy among others).
If recurrent malignancy is suspected or confirmed, please contact the LTFU office (Appendix
A) promptly to discuss additional diagnostic tests and treatment options.

72
XV. SECONDARY MALIGNANCIES
Recipients of hematopoietic stem cell transplant have an increased risk of developing
secondary malignancies, including skin cancers, solid tumors, myelodysplastic syndromes,
leukemias and post-transplant lymphoproliferative disorder (PTLD). Solid tumors that occur
at increased frequency include skin cancers (squamous cell, basal cell, malignant melanoma)
and cancers of the buccal cavity, followed by liver, central nervous system, thyroid, bone,
and connective tissue. PTLD generally occurs within the first year after the transplant,
predominantly in patients who received T cell-depleted grafts and in patients treated with
intensive immunosuppressive regimens to control GVHD.
All transplant recipients should have oncologic screening evaluations at annual intervals
throughout life. We recommend the following general guidelines for oncologic screening.
1. Skin exam with the complete physical and history
2. Pap smears & mammogram (women > 35 years) & education to reinforce self breast
exams
3. Prostate exam and PSA (men > 45 years)
4. Occult blood in stool (> 40 years)
5. Colonoscopy (baseline at age 50 years and as clinically indicated thereafter)
6. Oral exam by the dentist at 6 month intervals
7. Complete blood counts, thyroid function, and other tests as applicable
All patients should use sunblocking creams (> 30 SPF – sun protection factor) when outdoors
to prevent skin cancers and to prevent activation of chronic GVHD.
Please contact the LTFU office (Appendix A) if you are planning surgery or a biopsy for
evaluation of suspected secondary malignancy or if secondary malignancy has been
diagnosed.
73
XVI. OTHER COMPLICATIONS
A. GONADAL HORMONE INSUFFICIENCY
Gonadal hormone insufficiency is related to the age of the patient and the intensity of the
transplant preparative regimen.
MALES:
Post puberty: Men who were past puberty at the time of transplant may develop primary
gonadal failure. Testosterone replacement should also be considered in men who are
receiving corticosteroids for long-term treatment of chronic GVHD (see Section XI). Men
who receive testosterone replacement therapy should have a baseline prostate exam and
measurement of prostate specific antigen (PSA), liver enzymes and serum lipids. Follow-up
monitoring of these parameters may be appropriate.
Prepubertal: For boys without signs of puberty at age 14 years or failure of pubertal
progression or abnormal growth velocity with hypergonadotropic hypogonadism (high FSH
and LH and low free testosterone) should be considered for androgen or gonadotropic
therapy. Initially a lower dose should be considered to accelerate growth velocity without
advancing bone age. Subsequently, the dose can be increased closer to end of growth spurt
when fusion of growth plates is then acceptable. Hormonal replacement in prepubertal boys
should be done in collaboration with a pediatric endocrinologist.
FEMALES: Women often develop primary ovarian failure and have symptoms of premature
menopause. They are also at risk for development of osteoporosis. Permanent ovarian
failure invariably occurs in all female patients who receive busulfan and cyclophosphamide
(BU/CY). Recovery of ovarian function has been observed after transplant in 54% of
younger patients (less than 26 years) conditioned with cyclophosphamide alone. The
probability of ovarian function recovery after fractionated TBI is at least 10% by 6 years
after transplant.
Premature (<40 years) or early (40 – 50 years) onset of menopausal symptoms and
osteoporosis can significantly affect the quality of life of women after a hematopoietic cell
transplant (HCT). During the past 30 years, replacement therapy with estrogen alone (for
patients without a uterus) or combined with progestin (for patients with a uterus) has been
used to prevent or treat menopausal symptoms and to prevent bone loss. In children,
hormonal replacement therapy (HRT) is needed after transplant to promote the development
of secondary sexual characteristics.
Estrogen can treat hot flashes, vaginal and vulvar symptoms, prevent bone loss and improve
the quality of life for HCT recipients who are postmenopausal or who have premature
ovarian failure. The positive effect on cognitive function claimed by many women taking
estrogen remains to be confirmed. In young girls, estrogen replacement therapy is often
critical for the development of secondary sexual characteristics and for the attainment of
peak bone mass in early adulthood.
74
a) Special Considerations:
It is unclear if estrogen alone or combined with progesterone replacement will add to the
already increased risk of secondary breast cancer in posttransplant women (Friedman et
al.Blood;2008;111:939-944). Among patients who survived for more than 10 years
posttransplant the observed/expected risk ratio is 3.2 for breast cancer (Rizzo et al, Blood
2009; 113: 1175-1193). Radiation has been identified as the primary risk factor associated
generally with the development of solid tumors after a stem cell transplant.
b) Hormonal Replacement Guidelines for Girls:
In young girls, estrogen replacement therapy is often critical for the development of
secondary sexual characteristics during the transitional from adolescence to adulthood and
for the attainment of peak bone mass in early adulthood. Survivors with
hypergonadotrophic (high FSH, low estradiol ) and hypogonadotropic (low FSH, low
estradiol) should be considered for hormone replacement therapy. Initially low dose
hormone therapy should be used . Cyclic dosing should be used at later stages to induce
regular menstrual cycles. It is recommended to hold hormone replacement therapy for 2
months at regular intervals to check for resolution of gonadal insufficiency . Hormonal
replacement in prepubertal girls should be done in collaboration with a pediatric
endocrinologist.
c) Hormonal Replacement Guidelines for Women:
Temporary relief of menopausal symptoms:
Unless medically contraindicated, a finite course of estrogen alone (women without
uterus) or combined with progesterone (women with uterus) may be prescribed for the
temporary relief of menopausal symptoms, provided that patients are frequently
reassessed by their physician to determine the appropriate duration of therapy.
General considerations for posttransplant Gonadal Hormonal Therapy (HRT) include:
• Management of ovarian failure should be tailored according to a patient’s particular
clinical manifestations and individual risks for side effects of HRT such as:
a) history (or family history) of breast cancer
b) history of deep venous thrombosis, stroke or hypercoaguable state
c) history (or family history) of colorectal cancer
d) severe osteoporosis with vertebral crush fractures
e) presence of absence of a uterus
• Overall benefits and risks of long-term HRT should be discussed with each patient.
• Information about non-hormonal alternatives for management of ovarian failure
manifestations should be discussed with all patients.
• A patient and her physician should be able to clearly state the indication (s) for which the
patient is to start (or continue) posttransplant HRT.
• HRT should be prescribed at the lowest effective dose.
• Annual gynecological follow-up evaluation is recommended for all women.
• Monthly self-breast examination is recommended for all women.
• Baseline mammography is recommended for all women from 35-40 years of age. Annual
follow-up is also recommended.

75
• Yearly re-evaluation of a patient’s ovarian failure management plan is recommended to
determine if it remains the most appropriate plan for that patient.
Specific Contraindications to HRT:
• Systemic estrogen alone or combined with progesterone should not be prescribed for patients
with a history of thromboembolic diseases (i.e., venous thrombosis, pulmonary embolism,
strokes, etc.), hypercoagulation disorders, breast cancer, coronary artery disease, or active
liver disease.
Alternatives to HRT:
• Diet, exercise and other non-hormonal strategies are available for management of hot flashes,
insomnia and mood disturbances.
• Topical estrogen alone may relieve local vaginal/vulva symptoms caused by gonadal
insufficiency.
Use of hormone of supplementation as first line of treatment is not recommended for
osteoporosis/osteopenia except for children or young adults. Please see LTFU Section XI:
General Guidelines For Prevention of Osteoporosis and Glucocorticosteroid Induced
Osteoporosis After HCT
• Difficulties such as decreased libido and/or dyspareunia may be multifactorial in etiology and
may often be managed without the use of systemic conjugated equine estrogen and
medroxyprogesterone.
B. Endocrine Abnormalities
Compensated or overt hypothyroidism, thyroiditis and thyroid neoplasms may develop in
patients who received radiation. The incidence of compensated hypothyroidism after
fractionated total body irradiation (TBI) before transplant ranges between 15-25%.
Patients should be evaluated yearly with physical examination and thyroid function tests.
Growth hormone (GH) deficiency and growth failure (decreased growth rate/year) occurs
in 70-80% of children who received total body irradiation or 1800 cGy cranial
irradiation. The onset of GH deficiency and growth failure varies with the age of the
child at the time of irradiation. The onset of these problems appears to occur later in
younger children than in peri-pubertal children. All children should have height
monitored at least annually, and those <14 years of age should have annual GH testing
until they either develop GH deficiency or are >14 years of age, whichever occurs first.
Among pre-pubertal children, treatment with total body irradiation, busulfan or >2400
cGy testicular irradiation may delay subsequent pubertal development. Children who
received busulfan appear to have the highest risk of delayed or absent pubertal
development. Approximately half of the very young children treated with total body
irradiation progress through pubertal development at an appropriate age, while older
children treated with total body irradiation have a higher risk of delayed pubertal
development. Treatment with cyclophosphamide alone does not delay pubertal
development.

76
Beginning at age 10, all children should have Tanner development scores determined as
part of an annual physical examination. Children who are Tanner Stage I or II by age 12
years should be referred to a pediatric endocrinologist to evaluate the need for hormonal
supplementation.
C. Ocular complications
An annual eye exam with slit lamp examination is recommended for all patients who
have had an allogeneic transplant and for those who are at risk of cataracts. The risk of
cataracts after transplant is high for patients who received fractionated TBI (30 – 50%)
and for patients treated with corticosteroids after the transplant (45%). In patients who
received neither TBI or prior cranial irradiation, the incidence for cataract is
approximately 15% and, is primarily due to corticosteroids. The median time to develop
cataracts after transplant ranges from 2 to 5 years. Cataract extraction can be performed
safely even when ocular sicca is present. Unanticipated complications after placement of
an intraocular lens have not been reported. Other late complications involving the eyes
are related to chronic GVHD as described in Section X A and B.
D. Oral complications and guidelines for dental care
New oral pain or dryness beyond day + 100 after allogeneic transplant suggests
development of chronic GVHD involving the salivary glands or mucosal surface.
Cultures for candida and DFA or rapid cultures for herpes simplex virus should be
obtained to rule out concomitant infections if clinically indicated. A dental/oral medicine
consultation should be strongly considered in all patients with oral complications. If you
have questions about dental care during treatment for GVHD that are unanswered below,
please call the LTFU office who will provide instructions on how to take oral cavity
photos that you can send to [email protected] with your clinical impression and
question. Our LTFU/Oral Medicine can then review these and provide further advice.
General guidelines for dental care for autologous and allogeneic transplant recipients are
provided in the Table below.
General guidelines for dental care in hematopoietic transplant recipients include (see Table 1):
• Routine dental health examinations (with radiographs as needed) are recommended to
monitor for tooth decay and oral hygiene effectiveness, gingivitis and/or periodontitis.
Dental exams can take place any time after transplant and should be done every 6-12
months for routine oral health assessment, to evaluate/treat chronic GVHD (allogeneic
patients) and to screen for oral cancers. (see Table 1)
• Routine dental exam/cleanings should be delayed for first 6 months after transplant due
to increased risk of bacteremia and pneumonia while patients are still
immunocompromised. After the first 6 months, routine (not deep) cleaning either by
ultrasonic or manual dental scaling are reasonable provided certain other criteria are met
(see Table 1).
• Periodontal therapy (Deep cleaning) can be done after the first 6 months if the additional
criteria over and above those set for routine cleaning are met (see Table 1).
77
• Elective (non-urgent/non-emergency) restorative dental treatment like fillings and
crowns, or elective surgical procedures like dental extraction of non-infected teeth,
implants and gum graft surgery should be delayed until immunity is recovered and
patient has discontinued systemic immunosuppressive treatments. (see Table 1)
• “Cosmetic” dental care like dentures are considered safe so long as no extractions or
surgeries are needed. Veneers and other elective restorative procedures should be delayed.
Teeth whitening is reasonable beyond 6 months posttransplant. Invisalign therapy is not
recommended within the first 6 months. Traditional orthodontia is deferred until patient has
no active GVHD and is off all systemic immunosuppression. (see Table 1)
• Emergency or Urgent Care should be carefully coordinated between managing
dentist/oral surgeon and medical team so that appropriate supportive and medical care
can be discussed. Important considerations include:
1. Prophylactic and/or therapeutic antibiotics to minimize risk of bacteremia
complications:
a. For patients with an indwelling central venous catheters, follow American Heart
Association (AHA) recommendations for low-moderate endocarditis risk.
b. For short non-surgical/non-invasive surgical procedures, also follow AHA
prophylactic antibiotic recommendations, and extend treatment if there is
significant local dental infection and risk of subsequent spread of infection
(local or disseminated).
2. Other strategies to reduce spread of infection:
a. Chlorhexidine oral rinse for 3 minutes immediately prior to treatment.
b. Minimize aspiration of aerosolized bacteria by using a rubber dam, high
volume suction, minimal air-water sprays during procedures.
3. Platelet support depending on invasiveness of treatment and risk of bleeding.
Other medical support (e.g. stress dose steroids, adjustments to anticoagulation therapy).
Other key points / recommendations:
• More frequent cleanings may be required based on oral health conditions. Ultrasonic
cleaning carries slightly more risk of aspiration than manual scaling but is generally
acceptable.
• Patients should carry out focused and effective oral hygiene (brushing, flossing, etc.) as
good oral hygiene can be protective in preventing oral GVHD flares.
• Patients with dry mouth should be placed on dental decay prevention regimen that
minimally includes daily brush-on prescription-strength fluoride gel or toothpaste or
rinses to reduce the risk of dental decay. Other measures to promote salivation should be
encouraged (oral moisturizing agents, sugar-free gums or candy, and prescription drugs
to stimulate saliva flow).
• Patients who have received bisphosphonate therapy or on or just completed
denosumab therapy are at a risk for osteonecrosis of the jaw (ONJ). Risk depends on
the type of bisphosphonate, dose, frequency, and total duration of treatment. Reclast
(zoledronic acid) is considered to be at very low risk for ONJ. Zometa (another brand of
zoledronic acid) and pamidronate (Aredia) are considered to be at highest risk for

78
development of ONJ. The risk for MRONJ in patients treated with oral bisphosphonates
increases steadily over time and is of higher concern in those with greater than 3 years of
use. Bisphosphonates will persist in bone for as long as 10-15 years after discontinuation.
Denosumab (Xgeva) has also been associated with ONJ but the risk for ONJ with
denosumab will decrease over 6-7 months after discontinuation. Patients who previously
received bisphosphonates and switched to denosumab may be at an even higher risk for
ONJ compared to either agent used alone.
Recommendations for patients who have received bisphosphonate therapy or on or just
completed denosumab therapy are at a risk for osteonecrosis of the jaw (ONJ:
a. Prevent trauma and irritation from dentures
b. Support excellent dental and periodontal health in order to avoid advancing dental
infections or problems that would ultimately need dental surgery to manage.
c. When patients at risk for ONJ need dental procedures, the least invasive but
effective procedure to solve the problem should be chosen.
Stabilization/restoration of a tooth with a root canal or crown is preferable to
extracting the tooth.
d. Any dental surgery – extractions, implants, periodontal, or endodontic, is
considered high risk for development of ONJ if there has been prior or
ongoing therapy with bisphosphonates or denosumab therapy.
e. If the risk/benefit ratio has been explored and a tooth must be removed, the
procedure should be done by a skilled Oral Surgeon who will use extreme
caution to avoid any excessive trauma to the bone and achieve primary closure
of the site.
• Special attention should be paid to potential head and neck cancers in transplant
survivors – especially lip and oral cavity cancer. Risk is related to cumulative total body
or local irradiation exposure and chronic GVHD.
General guidelines include:
a. Patient counseling to avoid additional risks, specifically, to follow protection
against sun exposure to lips, avoid tobacco products and avoid excess alcohol
beverage intake.
b. Adjunctive examination techniques such as increased uptake of applied toluidine
blue vital dye within dysplastic or neoplastic oral mucosal lesions may be
diagnostically helpful for screening.
c. Serial lesion photographs can be an important component of patient management.
d. Suspicious lesions should be managed comprehensively and followed closely
until resolved or definitive diagnosis is made.

79
Table 1: Dental Care Guidelines for Autologous and Allogeneic Transplant Recipients
Dental Procedure
Time after Transplant
Until 6 months
After 6 months ****
LOW-RISK HIGH-RISK
Not receiving IST for active GVHD* or
getting maintenance with anti-CD20
therapy or other cytotoxic therapy AND
with ANC >1000, Plts >30K
Receiving IST or
maintenance with anti-CD20
therapy or other cytotoxic
therapy, CD34 selected
transplant or ANC <1000,
Plts <30K
Routine Dental Care
Exam every 6-12 months
YES
YES
YES
Routine Dental Cleanings
NO
YES, with antibiotics if central line still in
place
YES, with antibiotics and/or
IVIG** as clinically
indicated
Periodontal Therapy
Scaling/root planning +/-
curettage (dental deep
cleaning)
NO
YES, for autologous (no contraindications)
YES, for allogeneic with considerations for
additional medical support
NO
Restorative Dental Care***
Crowns
Emergent ONLY
with antibiotics
Emergent ONLY with antibiotics
Emergent ONLY with
antibiotics and/or IVIG
Fillings
Emergent ONLY
with antibiotics
Emergent ONLY with antibiotics
Emergent ONLY with
antibiotics and/or IVIG
Surgical Treatments
Dental extractions
Emergent ONLY
with antibiotics
Emergent ONLY with antibiotics
Emergent ONLY with
antibiotics and/or IVIG
Implants
NO
Autologous – NO
Allogeneic – NO
NO
Gingival grafts
NO
YES, for autologous (no contraindications)
YES, for allogeneic with considerations for
additional medical support
NO
Cosmetic Dental Care
Teeth whitening
NO
YES
YES
Orthodontia
NO
NO
NO
Dentures
YES, if no
surgery needed
YES, if no surgery needed
YES, if no extractions are
needed
Abbreviation: IST = immunosuppression; ANC = absolute neutrophils count, Plts = platelets.
* Prophylactic IST or prednisone dose < 0.5mg/kg/day is OK if GVHD considered inactive
** IVIG should be considered if serum IgG level is below 400 mg/dL
***
If treatment is urgent/or emergency due to overall immune/GVHD status – that is, dental disease is at risk for
seriously compromising patient status, planning should consider strategies to reduce local and systemic infection spread
and bleeding.
****Beyond 1 year posttransplant, all dental procedures without additional precaution are OK, if all conditions
below are met:
– No indwelling central venous catheter
– At least 3 months recovery from the last Rituxan
– No active GVHD defined by discontinuation of all IST at least for 8 months
– IgG level > 400 mg/dL
– ANC >1000 cells/ul
– Platelet count > 30K/ul
– Not receiving cytotoxic therapy as maintenance treatment
80
E. Renal insufficiency
Nephrotoxic drugs are the most common cause of impaired renal function after a stem
cell transplant. Monitoring renal function and drug levels is recommended for all patients
who are at risk of renal insufficiency (Section III C & D).
F. Neurological Complications
Peripheral neuropathy and central nervous system complications may develop after
transplantation. Neurological complications may be caused by drugs used to control
GVHD (cyclosporine, tacrolimus) (Section X), electrolyte abnormalities, infection
(HHV-6, HSV, VZV, fungal organisms, toxoplasma, among others), prior cranial
irradiation, intrathecal chemotherapy, GVHD and malignancy. The following evaluation
is recommended:
1) Perform neurological examination including mini-mental state exam.
2) Consider
- Medications (CSA, FK506, opiods, benzodiazepines, high-dose steroids, voriconazole, etc) and check
CSA/FK506 levels
- Metabolic abnormalities (hypo/hypernatremia, hypercalcemia, hypercapnia, hyperosmolarity, renal or
hepatic failure, hypothyroidism, adrenal insufficiency, hypoglycemia, etc.)
- Non-CNS infection such as UTI, pneumonia, etc.
- Unremitting pain or insomnia
- Intracranial hemorrhage
- Hypovolemia – due to bleeding or other cause
- Head trauma
- CNS malignancy
- CNS infection
When available, refer to institutional policies on the management of patients with delirium.
If medication/metabolic/endocrine/pain effect/sleep deprivation are felt to be unlikely etiologies OR if symptoms
persist for >24-48 hours despite efforts to correct what’s felt to be underlying cause:
1) Brain Imaging (MRI preferred)
2) Lumbar puncture
Standard: cell count, protein, glucose, cytology, gram stain, bacterial/fungal cultures, HHV-6 PCR (viremia
should not be assumed to be a marker for HHV-6 detection in the CSF), additional CSF saved for future
studies
Additional testing for malignancy of infection (see table below) may be considered as clinically indicated:
3) Consider ID consult for evaluation of infectious etiologies of delirium
4) Consider Neurology consult for evaluation of neurological etiologies of delirium
5) Consider psychiatry consult for evaluation and treatment of delirium
Depending on the clinical scenario, the following additional tests for infectious etiologies
may be considered:

81
Pathogen
Relative
Frequency
Clinical Setting
Recommended Initial Evaluation
Viruses
HHV-6
Frequent
• Early after transplant
• Temporal lobe contrast-enhancing lesions
• Memory loss characterizing delirium
CSF: HHV-6 PCR
HSV
Occasional
• Temporal lobe contrast-enhancing lesions
• Seropositive and not on ACV/GCV
CSF: HSV PCR
VZV
Occasional
• Seropositive or following significant
exposure and not on ACV/GCV
CSF: VZV PCR
CMV
Rare
• Donor or recipient seropositive and late
after transplant
CSF: CMV PCR
EBV
Occasional
• T-cell depleted, including CD 34+
selected
• Receipt of anti-T cell antibodies
CSF: EBV PCR
Enterovirus
Occasional
• Child
• Summer/fall
CSF: Enterovirus PCR
West Nile Virus*
Occasional
• Donor is from endemic state
• Significant mosquito exposure
• Neuromuscular weakness as component
of meningoencephalitis
CSF: WNV PCR (low sensitivity),
IgM (MAC-ELISA)
Serum: IgM (MAC-ELISA)
Contact Public Health
JC virus
Rare
• Brain imaging: non-enhancing white
matter lesions
• other work-up negative
CSF: JCV PCR
Brain biopsy
Zika virus
Very Rare
• Donor or Recipient from endemic area
ID Consult
Parasites
Toxoplasma
Occasional
• Ring-enhancing lesions
• Seropositive pretransplant and not on
prophylaxis – TMP/SMX, dapsone, etc.
CSF: PCR (low sensitivity)
Plasma: PCR
Fungi
Aspergillus and other
molds
Frequent
• Enhancing brain lesion (s) consistent with
abscess
• Concurrent pulmonary lesions (nodules)
• High degree of immunosuppression, or
neutropenia
CSF: PCR and galactomannan
(unknown sensitivity/specificity),
fungal culture
Plasma: galactomannan
Cryptococcus
Rare
• High degree of immunosuppression, or
neutropenia
• +/- enhancing meningitis or nodule or
hydrocephalus
CSF: cryptococcal antigen, fungal
culture
Serum: cryptococcal antigen
Bacteria
Usual bacterial
pathogens: S.
pneumoniae,
Listeria, GNR,
Nocardia, etc.
Frequent
• Meningitis
• Enhancing brain lesion (s) consistent with
abscess
No additional testing
recommended as these pathogens
should be identified by standard
bacterial culture.
Syphilis
Rare
• Positive pre-transplant serology
• Significant exposure
CSF: VDRL, FTA, or TPPA; IgM
immunoblotting: intrathecal T.
pallium antibody (ITPA) index,
PCR,
Tuberculosis**
Rare
• Meningitis (basilar or diffuse) or ring-
enhancing lesion(s)
• Recipient from endemic area
• Positive PPD pretransplant
• Significant exposure
CSF: AFB stain and culture, PCR
(both, low sensitivity)
* If concerned about other arboviruses, please discuss with Infectious Diseases.
** If concerned about non-tuberculous mycobacteria, please discuss with Infectious Diseases.

82
If the appropriate test is not locally available, arrangements should be made to send the
specimen to another laboratory. Please contact the LTFU office (see Appendix A)
Some children, especially those given cranial irradiation before the transplant, may have
learning disabilities (particularly in mathematics and abstract thinking). These
abnormalities typically begin to appear 24-42 months after the transplant. When
recognized as a problem, refer for psychological testing. Special educational instruction
should be considered for these children. Short-term memory deficit can occur in adults,
and psychometric testing should be performed as clinically indicated.
Total body irradiation can delay the onset of developmental landmarks in very young
children. These effects are most severe throughout the first year after transplant, and
affected children benefit from occupational therapy to assist their normal development.
After they have achieved appropriate developmental landmarks, further development
appears to proceed normally. IQ and ability to succeed in school do not appear to be
affected by total body irradiation.
G. Bone Complications (see Section XI)
Osteoporosis, fractures and avascular necrosis (AVN) are common complications after
transplantation. Long-term treatment with corticosteroids is the primary risk factor for
these complications, while gonadal failure, electrolyte imbalances, physical inactivity and
treatment with cyclosporine play an additional contributory role. Approximately 50% of
patients receiving long-term corticosteroid therapy will eventually develop bone
fractures. Increased osteoclast-mediated bone resorption and decreased osteoblast-
mediated bone formation cause trabecular bone loss. In HCT recipients, evaluation for
bone loss and osteoporosis includes a careful assessment of risk factors
(www.shef.ac.uk/FRAX/) and exposures in addition to BMD measurement. Bone loss
can be minimized by decreasing glucocorticoid dose, optimizing calcium and vitamin D
intake, participating in weight-bearing exercise, using bone strengthening drugs, and if
clinically indicated by hormonal replacement therapy. Section XI provides detailed
guidelines for preventing and monitoring osteoporosis in patients. Section XX describes
vitamins and other minerals requirements. Section XXI outlines diet for patients treated
with corticosteroids. Section XI outlines hormone replacement therapy.
H. Chronic Pulmonary Complications
Some reports have shown that the FEV
1
/FVC is less than 70% in 15% of patients by one
year after the transplant and in 30% of patients by three years after an allogeneic
transplant. Among patients with chronic GVHD, 5-10% will develop severe obstructive
airway disease that resembles obliterative bronchiolitis.
Monitoring of lung function after day +100 after allogeneic transplant.
Pulmonary function test (PFT) monitoring including: spirometry, lung volumes, and DLCO.
PFTs for asymptomatic allo-HCT recipients:
a. At 6 months
b. At 1 year
c. Yearly thereafter until 5 years as clinically indicated
d. At diagnosis of chronic GVHD
83
i. Full PFT testing including: spirometry, lung volumes, and DLCO
ii. Q3 months after diagnosis of chronic GVHD for at least one year.
(spirometry alone may be adequate)
iii. Thereafter, at Q6 months for 1 year (spirometry alone may be
adequate)
iv. With at least yearly full PFT testing including: spirometry, lung
volumes, and DLCO until year 5 post HCT.
(Section X B). If new abnormalities are noted in PFTs please contact the LTFU office to
discuss further recommendations (Appendix A).
Children who received total body irradiation are at risk of delayed onset pulmonary
restrictive disease 5-20 years after the transplant. All patients who were in the pediatric
age group at the time of transplant should have annual pulmonary function tests.
I. Hepatobiliary Complications
(see References, section XXV, Liver)
Elevations of serum ALT, alkaline phosphatase or bilirubin may occur after day 100, even
in patients who had no indication of liver problems earlier. The presentations fall into
four clinical categories.
• Acute hepatitis. Elevations of serum ALT after day 100 are most commonly
caused by drug-induced liver injury (an azole antifungal or trimethoprim-
sulfamethoxazole are the most common causes of Drug Induced Liver Injury (DILI)
in this setting), chronic GVHD, an exacerbation of hepatitis B or C, or a herpesvirus
hepatitis (VZV, HSV).
Four clinical situations demand immediate diagnosis and treatment.
1) Rapidly rising ALT accompanied by anorexia, abdominal distension or pain in
the abdomen or back can be signs of visceral VZV infection (Section VIII B).
2) Patients who have indications of hepatitis B before transplant (HBsAg-positive
or anti-HBc-positive) or who had a donor who was infected with hepatitis B are
at risk of fulminant hepatitis B after the transplant if they did not receive
antiviral prophylaxis.
3) Chronic GHVD can present as an acute hepatitis, usually after tapering or
discontinuation of immunosuppressive medications, particularly cyclosporine or
tacrolimus, or after DLI.
4) In Hepatitis C infected patients, a diagnosis of fulminant immune-rebound
hepatitis should be considered, especially if patient is tapering
immunosuppression, and, if clinically indicated, treatment with Direct Acting
Antiviral (DAA) drugs.
Patients with a rapidly rising ALT and those with ALT values >500 u/L should be
given IV acyclovir until VZV hepatitis is ruled out. An urgent PCR for VZV DNA
84
in serum is needed to establish the diagnosis. Contact the LTFU office (Appendix
A) for guidance in difficult cases.
• Chronic hepatitis. Chronic fluctuations in serum ALT levels without a discrete
episode of acute hepatitis may represent DILI, hepatitis B or C virus infection
(Section XVII), iron overload (Section XVIII) or cGVHD (Section X).
• Jaundice or signs of cholestasis. Elevated serum bilirubin and elevated alkaline
phosphatase can be caused by chronic GVHD (Section X), drug-induced
cholestasis, acute hepatitis (see above), or biliary obstruction. An ultrasound should
be obtained to evaluate whether the common bile duct is dilated. Liver biopsy
might not be needed in patients who have cholestasis with biopsy-documented
chronic GVHD in other organs. Some patients have liver involvement as the
dominant manifestation of chronic GVHD, and liver biopsy might be needed in
order to establish the diagnosis when other manifestations of chronic GVHD are
absent.
• Hepatomegaly or right upper quadrant pain. The sudden onset of
hepatomegaly suggests acute hepatitis, Epstein-Barr virus-induced
lymphoproliferative disorder involving the liver, or rarely, Budd-Chiari syndrome.
More indolent hepatomegaly can occur with metastatic tumor, leukemia infiltration
or rarely, constrictive pericarditis or mycobacterial infection. Right upper quadrant
pain can be caused by acute cholecystitis, biliary obstruction with cholangitis,
biliary sludge syndrome, or rarely, fungal liver abscess. Liver imaging with helical
CT X-ray or ultrasound is needed to resolve the diagnosis.
Suggestions for liver biopsy and handling of liver tissue. The technique of liver
biopsy depends on the clinical situation (diffuse process vs. focal lesion) and the platelet
count. A percutaneous biopsy is preferred if platelet counts are >100,000/mm
3
and the
risk of bleeding is small (including normal PT/PTT) but transvenous biopsy through
either the femoral or jugular route is satisfactory for diagnosis of any diffuse hepatitis or
GVHD. Tissue should be cultured for viruses and fungi and should be fixed in freshly-
prepared neutral buffered formalin.
J. Gastrointestinal Complications:
(see References, section XXV, Liver)
GVHD is the most common cause of anorexia, nausea, vomiting and diarrhea after an
allogeneic transplant. However, each of these symptoms has a narrow differential
diagnosis that requires careful evaluation before concluding that GVHD is the sole cause.
Anorexia, nausea and vomiting can be caused by HSV, VZV, and CMV infections and by
certain medications such as trimethoprim-sulfamethoxazole, voriconazole, itraconazole,
mycophenolate mofetil, cyclosporine or tacrolimus. Abdominal pain can be caused by
visceral VZV infection, biliary sludge syndrome, acute cholecystitis, or rarely, Epstein-
Barr virus-induced lymphoproliferative disease. Diarrhea occurring more than 3 months
after transplant is commonly caused by magnesium – containing medications, unresolved
GVHD, or less commonly by an infection (giardiasis, cryptosporidiosis, C. difficile, or
CMV). Section VII provides guidelines for evaluation of diarrhea and endoscopy.
85
XVII. BLOOD PRODUCT TRANSFUSIONS
All blood products should be irradiated to prevent transfusion related Graft Versus Host Disease
(GVHD), with the exception of pathogen reduced blood products that do not need to be
irradiated. Red blood cells and platelets should also be leukocyte reduced to prevent HLA
alloimmunization and reduce the risk of CMV transmission. Leukocyte reduced blood
components are accepted as “CMV safe” for CMV seronegative patients. Granulocytes are
never leukoreduced.
If the donor and recipient had ABO blood group incompatibility, low-grade hemolysis can
delay erythroid recovery for many months after the transplant. Hemagglutinin titers and
reticulocyte counts should be followed to monitor the change from recipient to donor ABO
type. Type O red cells should be used for patients who have isoagglutinins against donor red
blood cell antigens until the donor blood group type is fully established in the recipient.
Treatment with erythropoietin can be beneficial in some patients. Donor-type platelets
should be used for transfusions.
86
XVIII. VIRAL HEPATITIS in long term transplant survivors
(see References, section XXV, Liver)
Compared to hepatitis C, hepatitis B is more likely to result in severe clinical hepatitis and
death from post-transplant liver disease, although these outcomes occur only in the minority
of HBV-infected patients. One exception: patients infected by HCV who are receiving
MMF for GVHD prophylaxis may develop a more severe, potentially fatal form of liver
disease called fibrosing cholestatic hepatitis C. In this setting, it should be assessed whether
MMF may be discontinued. Antiviral treatment should be considered for HBV-and HCV-
infected transplant recipients unless contraindications are present. Liver test abnormalities
post-transplant may be caused by hepatic GVHD, HBV, HCV, a herpes virus infection
(VZV, CMV, HSV), adenovirus, or drug-induced injury (Sections I, X and XV). In this
situation, liver biopsy should be performed to determine the dominant pathologic process.
A. Hepatitis B
Even in patients with very low levels of viral replication before transplantation and relatively
normal liver function and histology, impaired cellular immunity can permit reactivation of
HBV. Serological patterns of HBV infection may be atypical in transplant survivors, likely
as a consequence of immunosuppression. Patients with HBV requiring systemic
immunosuppressive medications for control of chronic GVHD remain at risk for acute
exacerbation of hepatitis whenever immunosuppression is tapered or ceased. Such flares
may result in hepatic failure and death. Cirrhosis due to chronic HBV has not emerged as a
major problem after transplantation.
The risk of fatal HBV liver disease among patients who are persistently HBsAg-positive
after transplant and who are not receiving entecavir is approximately 12%. In hematopoietic
cell transplant recipients who are anti-HBc and anti-HBs-positive, but HBsAg-negative,
reactivation of latent infection can occur and may lead to fulminant hepatic failure,
particularly if nucleotide substitutions in the precore region of the genome interfere with
production of HBcAg. Because these patients remain HBcAg-negative despite high levels of
viral replication, monitoring of HBV DNA levels is necessary in these HBsAg-positive
patients.
Posttransplant HBV infection may result from
Active HBV infection before transplant
Reactivation of latent HBV infection
New infection during the transplantation process
o Infected hematopoietic cell product from an infected donor
o Infected blood products (risk estimated in U.S. to be 1 in 500, 000 units).
1) Monitoring of Patients at Risk for HBV Infection
For allogeneic transplant patients who had a donor who was either HBsAg or
antiHepB core positive:
Serum ALT and HBV DNA monthly to six months post transplant or 6 months
after stopping entecavir (whichever is longer).
87
For allogeneic transplant patients where patient is HBsAg positive and on entecavir:
Monitor HBV DNA and serum ALT monthly until 6 months after stopping
entecavir. If increased Serum ALT consider testing for viral resistance and
switching to TAF if checked HBV DNA increased >1.0 log above nadir.
For allogeneic transplant patients where patient is antiHepB core positive:
Serum ALT and HBV DNA monthly until 6 months after stopping entecavir.
For autologous transplant patients who is either HBsAg or antiHepB core positive:
o Monitor HBV DNA and Serum ALT monthly until 6 months after stopping
entecavir. If HBV DNA increases > 1.0 log above nadir. Consider testing for
viral resistance and switching if medically indicated to TAF.
2) Treatment
For patients at risk for HBV infection after transplant who are NOT receiving antiviral
prophylaxis, we recommend initiation of antiviral treatment with entecavir when HBV
DNA is first detected after transplant. For patients already on entecavir and not
appropriately responding, consider alternative antiviral therapy. The aim of antiviral
treatment is to suppress viral replication completely, thereby minimizing the risk of viral
mutation. Patients should be treated for 12 months or 6 months after discontinuation of
systemic immunosuppressive treatment, whichever is longer.
3) Other considerations
-Clearance of antigenemia is commonly observed and is particularly likely if the
hematopoietic cell donor was anti-HBs-positive.
- Based on CDC guidelines, vaccination with HAV is considered particularly important
and is strongly recommended for any patient with evidence of infection with HBV to
prevent the development of fulminant liver failure secondary to hepatitis A infection.
(See section IX Vaccinations)
B. Hepatitis C
Infection with HCV virus is more frequent in patients who received blood product transfusions
before 1991 when HCV testing was unavailable than with transfusions given after 1991. The
prevalence of chronic hepatitis C in long-term HCT survivors ranges from 5% to 70%,
depending on the endemic prevalence. Long-term survivors with HCV infection commonly
have fluctuating levels of AST and ALT. During the first 10 years after infection, hepatitis C
has little impact in morbidity or mortality—with the exception possibly of HCV-infected
patients who are receiving MMF. The frequency of cirrhosis and end-stage liver disease caused
by Hepatitis C in 40-year survivors of hematopoietic cell transplant is about 33%.
Regardless of whether HCV infection occurred before or after the transplant, clinical or
biochemical evidence of hepatitis usually coincides with the return of cellular immunity and
the tapering of immunosuppressive drugs used for GVHD prophylaxis. During this time, it

88
is difficult to differentiate the hepatitic variant of GVHD of the liver from an exacerbation
of HCV. The presence of hepatitis C viremia, even in high titer, is insufficient to make the
distinction between these two disorders. The absence of hepatitis C viremia, however,
means that HCV is not a cause of ALT elevations. Unless there is evidence of active GVHD
in other organs, a liver biopsy may be required before a therapeutic decision is made.
Pathologic distinction between hepatitis C and GVHD may be difficult, since both processes
may be associated with portal lymphoid infiltration and bile duct injury. Marked bile duct
injury with epithelial cell dropout and loss of interlobular bile ducts is more typical of
GVHD. A flare of hepatitis C and hepatic GVHD may occur simultaneously. If the liver
biopsy suggests both processes, immunosuppressive therapy should be administered, since
ongoing lymphocytic attack leading to loss of interlobular bile ducts may result in severe
and progressive cholestasis.
Fulminant immune-rebound hepatitis C has been reported only rarely after withdrawal of
immunosuppression. Patients infected by HCV who are receiving MMF may be at risk to
develop fatal fibrosing cholestatic hepatitis C. After the initial flare of hepatitis during
immune reconstitution, the serum ALT levels may again return to normal, but laboratory
abnormalities often settle into the pattern of chronic hepatitis seen in other patients with
HCV infection.
Monitoring:
Liver function tests at least weekly to day 100, then bimonthly until 1 year
HCV RNA should be checked around day 50 post transplant in those rare patients who
were HCV antibody positive but HCV RNA negative pretransplant or whose donor was
HCV RNA positive.
Patients known to have HCV should be referred to a hepatologist to assess three major
issues: 1) Has the virus infection caused any damage to the liver yet? 2) Are there other
causes of liver damage (i.e., alcohol, medications, chronic GVHD, hemosiderosis or the
hepatitis B virus? 3) Should medications for HCV be instituted?
All HCV-infected long-term HCT survivors should be evaluated for progression of liver
disease every 6 to 12 months with a hepatic function panel, complete blood count, and
evaluation of prothrombin time/international normalized ratio. If fibrosis is suspected in
long-term HCT survivors, noninvasive tests such as serologic panels and transient
elastography can be used to evaluate for the presence of advanced fibrosis (Scoring System
for Histological Stage Metavir score > F3) and cirrhosis (Metavir score F4).
For HCV-infected HCT long-term survivors with advanced fibrosis (Metavir score > F3),
surveillance for hepatocellular carcinoma with ultrasonography every 6 months is
recommended. For patients with cirrhosis, endoscopic surveillance for esophageal varices is
recommended.
89
Therapy
Direct-acting anti-viral therapy for chronic HCV infection should be considered after the
patient has discontinued all immunosuppressive drugs, and has no evidence of active
GVHD. Be aware of possible drug-drug interactions (see References, section XXV,
Liver).`
In patients with concomitant iron overload, phlebotomy or chelation therapy may be
indicated to reduce hepatic iron stores (Section XVIII) before Direct Acting Antiviral
(DAA) therapies. The mobilization of iron after transplant largely depends on the iron
burden, especially cardiac iron. A review of this topic has been published. (see
References, section XXV, Liver)
In all HCT survivors with active HCV infection, cofactors that can lead to fibrosis should be
addressed. Patients should be counseled to avoid excessive weight gain, ethanol and
medications or herbal supplements that are hepatotoxic, as well as on treatment of other
causes of liver disease (nonalcoholic fatty liver disease, hepatitis B virus, HIV, and
extrahepatic obstruction), and mobilization of excess iron.
HCT recipients who develop end-stage liver disease can be considered for liver transplant;
in rare cases, a living donor liver transplant from the original hematopoietic cell donor may
be feasible.
Other Considerations:
- Based on CDC guidelines, vaccination against HAV and HBV are considered
particularly important and are strongly recommended for any patient with evidence of
infection with HCV to prevent the development of fulminant liver failure secondary to
infection with other hepatitis viruses.
(See section IX Vaccinations)

90
XIX IRON OVERLOAD
A. Summary of evidence
1. Epidemiology
Iron overload occurs frequently in hematopoietic cell transplantation (HCT) patients, often
caused by red cell transfusions prior and during HCT, in addition to ineffective
erythropoiesis with associated intestinal hyperabsorption, and, in some patients, underlying
genetic hemochromatosis. Elevated ferritin estimates 32-58% of HCT survivors may be
overloaded with iron [1, 2, 3]. One autopsy study found 40% of patients with significantly
high liver iron content (LIC) above 5.6mg/g [4]. A cross-sectional study showed 31/56 HCT
recipients had elevated ferritin, and 50% of those with high ferritin had significant liver
siderosis with LIC>6.5mg/g [1].
2. Natural history of iron overload in HCT and its consequences
Once transplant has restored normal hematopoiesis and red cell transfusions are no longer
required, body iron stores decline over several years [5]. Elevated liver iron content (LIC)
defined as >1.8mg/g by T2- magnetic resonance imaging (MRI) was not associated with
survival or complications in adult patients at 1 year post-HCT [6]. High LIC (above 7mg/g)
as determined by magnetic resonance in patients post HCT for myelodysplastic syndromes
or acute myeloid leukemia was a significant risk factor for non-relapse mortality
(particularly in older patients undergoing reduced intensity conditioning), and ferritin above
1,000ng/mL has been associated with decreased survival. [7;8, 9]. Extreme tissue iron
overload (> 15 mg/g dry weight) has been associated with extensive organ toxicity in the
post-transplant survivors of thalassemia, in whom organs at risk include the heart, liver,
pancreas and pituitary gland, resulting in dysrhythmias and cardiac failure, portal fibrosis
and cirrhosis, insulin-dependent diabetes mellitus and other endocrine insufficiencies. Iron
overload increases the susceptibility to mucormycosis, aspergillosis, and infections caused
by Listeria monocytogenes, non-cholera Vibrio species, Yersinia enterocolitica and Yersinia
pseudotubera, among others [2, 4]. In patients with chronic hepatitis C, iron overload may
accelerate the development of cirrhosis.
3. Assessment of iron overload post-HCT
Although ferritin measurement is recommended as part of long-term follow-up post-HCT, it
also changes with inflammation and cell injury. Assessment of body iron by MRI is non-
invasive and has been calibrated with liver biopsies and ex vivo heart tissue iron
measurements, allowing accurate and more frequent assessment of iron overload than liver
biopsy [10]. Liver or marrow iron content correlates poorly with number of transfused red
blood cell units. Marrow and liver iron contents have been determined by spectrophotometry
among 10 consecutive autopsied patients who were transplanted for hematological
malignancy. The median liver iron content (LIC) at 50 to 100 days post-transplant was 4.307
mg/g dry weight (range 1.832-13.120; normal 0.530-0.900) and the median marrow iron
content was 1.999 mg/g dry weight (range 0.932-3.942). Marrow iron content can also be
measured by morphometry based on digital photomicrographs of a Prussian blue-stained
marrow biopsy. Because of correlation between morphometric and spectrophotometric
analyses of marrow iron content (r = 0.8, P= 0.006) and hepatic iron index (r = 0.82, P =

91
0.004) morphometric analysis of marrow iron content is an acceptable alternative for
quantifying tissue iron stores [11]. Earlier work also demonstrated a close relationship
between biochemical concentration and histologic grading of marrow iron [12] although
histological grading is subject to variation between and within observers [13]. Because the
carrier frequency for homozygous High Fe (HFE) gene mutations is relatively high (0.3 to
0.5%) among individuals of Northern and Western European ancestry, the possibility of
hereditary hemochromatosis (HH) contributing to post-transplant iron overload needs to be
considered in relevant individuals. Two point mutations, C282Y (Cys282Tyr) and H63D
(His63Asp), are the most frequently found within the HFE gene. Homozygosity for C282Y
is associated with hemochromatosis with variable penetrance; the effect of compound
heterozygosity (C282Y/H63D) on iron status in HCT recipients is variable.
4. Management of iron overload post-HCT
Mobilization of iron in heavily overloaded patients improves cardiac function, normalizes
serum alanine aminotransferase (ALT) levels, and results in improved liver histology
[14;15]. Phlebotomies were well-tolerated by 14/16 patients, and they reached the target
ferritin below 500ng/mL after a median of 16.5 phlebotomies in a median of 287 days [3].
Ferritin levels decreased significantly in 49/55 (80%) of patients after a median of 9
phlebotomies in another study [16]. One study showed that recipients of marrows from
donors with mutated HFE had lower reduction in ferritin levels per phlebotomy than those
who received marrow from wild-type donors [16]. A retrospective study found that
deferoxamine use post-HCT in 37 patients was associated with lower ferritin and lower
relapse incidence [17]. Oral chelation with 20-30mg/kg/day of deferasirox has been
evaluated retrospectively and showed a possible association with longer survival after HCT
[18], and a prospective, phase IV, open-label trial showed 10mg/kg/day of deferasirox
provided a significant reduction in serum ferritin and liver iron concentration over one year
of treatment with mild to moderate adverse events [19].
B. Evaluation of Iron Overload after HCT for autologous and allogeneic patients
1. Timepoints of evaluation:
a. at 80-100 days post HCT;
b. 1 year post HCT;
c. at least yearly if still receiving red blood cell transfusions.
2. Laboratory testing:
a. Iron studies (ferritin, iron, total iron-binding capacity [TIBC], and
transferrin saturation [TS])
Biochemical lab tests are non-specific and can be significantly affected by inflammation,
infection (which falsely elevate ferritin and decrease iron, TIBC and TS) and graft versus
host disease (GVHD) (which increases iron absorption), so biochemical tests should NOT
be used as sole criteria to consider the presence of iron overload and should be confirmed
by MRI-T2*.

92
b. HFE genotype
Consider for patients with:
i. family member with diagnosed hereditary hemochromatosis (HH)
ii. TS > 45% AND Northern or Western European ethnicity.
Genetic analysis for other rare mutations described in association with hemochromatotic
phenotypes such as in HAMP (hepcidin), SLC40A1 (ferroportin), HJV (hemojuvelin),
TFR2 (transferrin receptor 2) genes is recommended on a case-by-case basis.
3. Assessment of Tissue Iron
a. Magnetic resonance - MRI-T2*
All patients should undergo T2*-weighted magnetic resonance imaging test (MRI-T2*) if
there are concerns about iron overload. MRI-T2* is highly accurate in measuring tissue
iron in heart, liver, spleen, and pancreas. Recommend first getting MRI of abdomen for
assessing liver, spleen, and pancreas. If abnormal uptake in pancreas or other high-risk
factors see below, get cardiac MRI.
Cardiac MRI are indicated for patients with the following high-risk factors:
1.Lifetime history of receiving 75 RBC units or more;
2.Thalassemia;
3.Sickle cell disease ;
4.Other congenital anemias (Diamond-Blackfan; hereditary sideroblastic);
5.Associated hereditary hemochromatosis (HH)
b. Endocrine screen: Patients that fulfill criteria for iron overload (LIC>2mg/g),
particularly those with detectable cardiac iron (T2*<20ms) in adult patients, or
below 1 standard deviation or age based references in pediatric patients, may
benefit from earlier screening for endocrine gland abnormalities secondary to iron
overload with fasting glucose, thyroid stimulating hormone (TSH), free thyroxine
(T4), parathyroid hormone (PTH), follicle stimulating hormone (FSH), and
luteinizing hormone (LH).
c. Transient elastography: This is the preferred method if assessment of liver
fibrosis and cirrhosis is a concern, particularly in thrombocytopenic patients for
whom a liver biopsy poses significant risk of bleeding.
d. Liver biopsy: Given the risks of the procedure, risk of sampling variability, and
indolent course of hepatic siderosis, measurement of hepatic iron by
spectrophotometry of liver biopsy should be an exception to be discussed case-by-
case, e.g. in patients with absolute contraindications to MRI.
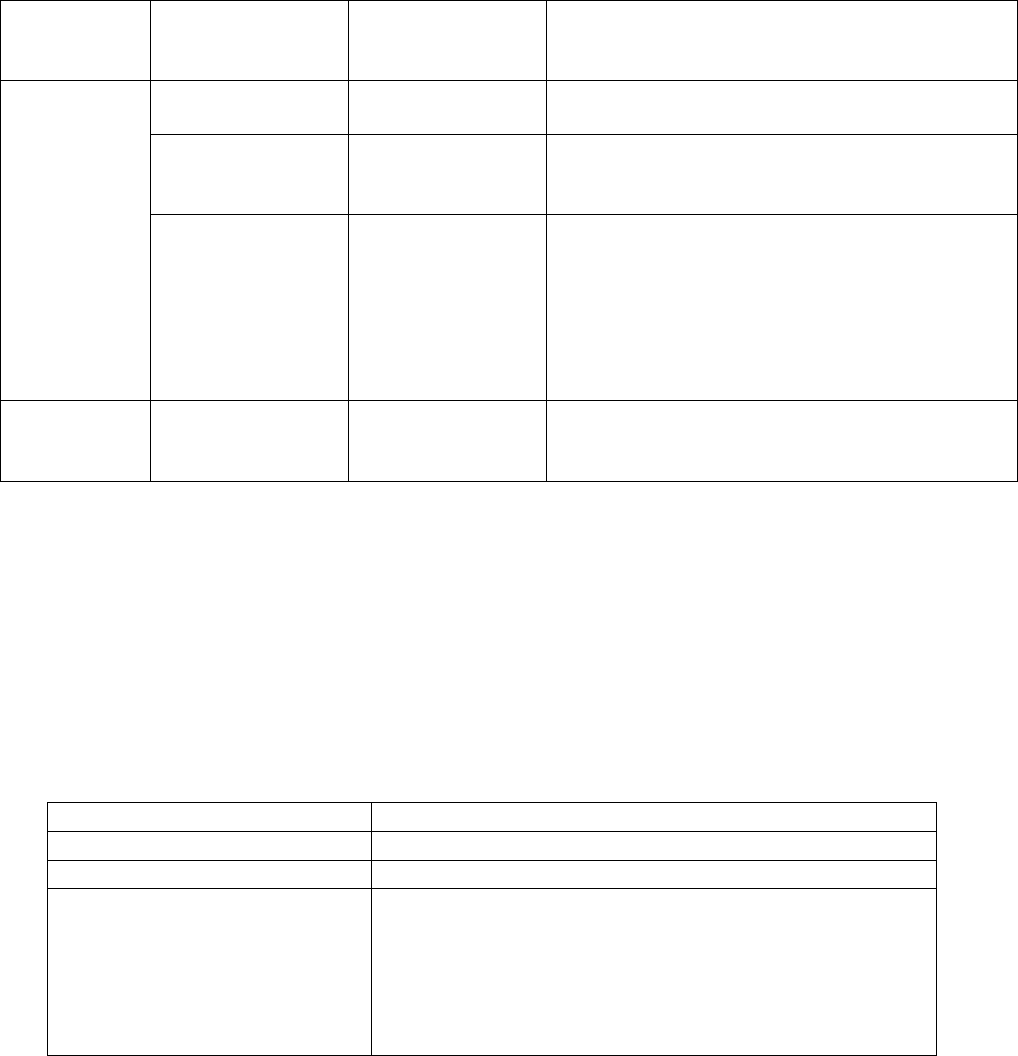
93
4. Indication for Iron Mobilization Therapy According to Tissue Iron Content
Cardiac T2*
(ms)
LIC
(mg/g dry weight)
Marrow Iron
Content
Mobilization of Iron
>20ms*
(normal)
>15
Very high
++++
Phlebotomy ± single iron chelator
7 – 15
Moderately high
++ to +++
1
st
choice: Phlebotomy
2
nd
choice: Single iron chelator (especially if
HCV-positive)
2-7
Mildly increased
+
1) HFE
wildtype
:
observe
2) HFE
C282Y/C282Y or C282Y/H63D
:
Phlebotomy aiming at ferritin level <100
3) Hemoglobinopathies and other congenital
anemia disorders
Phlebotomy aiming at ferritin level <500
<20ms*
Any
Any
Phlebotomy + combination iron chelation;
consider admission if symptomatic or T2*<8ms;
consider erythrocytapheresis for faster removal
*For pediatric patients: Use age-based reference ranges for cardiac T2* values. Abnormal
cardiac iron content is defined as below 1 standard deviation for age-based reference
values
C. Phlebotomy for iron overload after HCT
• If indicated, phlebotomy is likely to be the safest and most cost-effective approach for the
mobilization of tissue iron.
• Regular phlebotomy requires adequate venous access, normal hematopoiesis or
hematopoiesis that can respond satisfactorily to weekly or every-other-week
erythropoietic stimulating agents (ESAs).
• Phlebotomy Regimen:
Phlebotomy volume
5 mL/kg as tolerated
Frequency
every 3-4 weeks as tolerated
Monitoring monthly
CBC, ferritin, iron, TIBC, and TS
Discontinue Phlebotomy
Symptomatic anemia with hematocrit below 35%, or
MRI-T2* LIC below 7mg/g (non-HH patients), or
ferritin below 500ng/mL (non-HH patients and patients
with hemoglobinopathies/other congenital anemias), or
ferritin below 100ng/mL (hereditary hemochromatosis
(HH) patients)

94
• Erythropoietic Stimulating Agents (ESAs) may be administered subcutaneously to
facilitate regular phlebotomy. The smallest number of whole vials should be prescribed
per dose:
Body Weight
(kg)
Erythropoietin
1
(Units weekly)
Darbepoetin
2
(micrograms every-other-week)
10-14
6,000 to 8,000
25 to 60
15-20
10,000
60
21-24
10,000 to 14,000
60 to 100
25-29
14,000
100
30-39
20,000
100
40-60
40,000
200
>60
Use darbepoetin
200
1
Erythropoetin (Epogen) vial sizes (2,000; 4,000; 10,000; 20,000; 40,000 units)
2
Darbepoetin (Aranesp) vial sizes (25; 60; 100; 150; 200; 300 micrograms)
• Erythrocytapheresis is a grade 1B recommendation for iron overload in hereditary
hemochromatosis (HH). It has been compared with phlebotomies in two randomized
studies with hereditary hemochromatosis (HH) patients, with faster removal of iron, no
differences in adverse events, and controversial differences in cost [20,21].
Note: Though patients with GVHD continue to hyperabsorb iron from dietary sources and
may be an exception to the normal situation when patients mobilize their excessive iron
stores when effective erythropoiesis returns after HCT.
D. Chelation therapy for iron overload after HCT
If phlebotomy or erythrocytapheresis cannot be performed despite the use of ESAs within
3 - 6 months after transplantation, and if treatment to mobilize iron stores is indicated
(see item 4 above), iron chelation therapy with single agents desferoxamine (DFO) -
Desferal or deferasirox (DFX) - Exjade or Jadenu - should be initiated. Patients with
evidence of cardiac iron overload should undergo combination therapy (DFO and
deferiprone – DFP, Ferriprox).
1. Deferoxamine (DFO) - Desferal
1.1. Administration:
DFO can be administered by continuous subcutaneous or intravenous infusion with less
toxicity if administered subcutaneously.
1.2. Toxicity:
Ocular and auditory abnormalities, sensorimotor neurotoxicity, renal insufficiency,
pulmonary toxicity, and failure of linear growth. In rare cases, treatment with DFO has
enhanced susceptibility to certain microorganisms, such as Vibrio vulnificus, Yersinia
enterocolitica and Yersinia pseudotubera, among others, resulting in generalized
infections by providing these agents with a siderophore otherwise missing.
1.2.1. AVOID ascorbic acid (vitamin C) (>200mg/day) in patients receiving DFO due to
possible impact on left ventricular function. DO NOT administer ascorbic acid with
DFO in patients with heart failure.

95
1.2.2. Toxicity can be avoided by regular assessment of the body iron stores with annual
MRI-T2*. In general, assessment of body iron stores should also follow when
deferoxamine toxicity occurs.
1.3. Dosing:
20 to 40 mg/kg/day, administered 5-7 days per week by continuous overnight infusion,
typically for 8-12 hours.
Dose should not exceed 50 mg/kg/day
Infusion rate should not exceed 15 mg/kg/hour to avoid hypotension.
1.4. Monitoring:
1.4.1. Prior to starting treatment: obtain baseline CBC, creatinine, ferritin, liver function
tests, audiogram, and eye examinations.
1.4.2. Monthly complete blood count (CBC), ferritin, creatinine, and liver function tests.
1.4.3. Therapeutic index: Most of the toxicity caused by deferoxamine occurs when the
dose exceeds 50 mg/kg/day or when the iron burden is not high. Dose reductions
can be done by aiming at a therapeutic index below 0.025. Therapeutic index is
calculated by: (number of days per week X daily dose in mg/kg) / (7 X serum
ferritin in ng/mL) [22].
1.4.4. Discontinue for six months if LIC <3 mg/g dry weight, or marrow iron content is
not increased or only mildly increased. Thereafter, the dose of DFO should be
adjusted to maintain liver iron content between 3 and 7 mg/g dry weight and
therapeutic index below 0.025.
Suggested monitoring of DFO-related toxicity is shown below.
Toxicity
Tests
Frequency
Alteration In Rx
High frequency
sensorineural hearing
loss
Audiogram
Annually; if
symptomatic, check
immediately
Stop DFO;
repeat audiogram at 3
month intervals until
normal or stable
Retinopathy (pigmentary
degeneration); cataracts;
corneal opacities; visual
impairment
Eye exam
including visual
acuity, slit-lamp
and fundoscopy
Annually; if
symptomatic, check
immediately
Stop desferoxamine if
retinopathy or hearing
impairment
Metaphyseal/Spinal
Plain x-ray of
wrists, knees,
spine; bone age in
children
Annually
Reduce deferoxamine to
20-25 mg/kg/day
Growth retardation
Sitting and
standing height
Every 6 months
Reduce deferoxamine
to 20-25 mg/kg/day;
reassess every 6 months
2. Deferasirox (DFX) - Exjade, Jadenu, or Jadenu Sprinkles
2.1. Contraindications:
a) Serum creatinine greater than two times the age-appropriate upper limit of normal or
creatinine clearance less than 40 mL/min;
b) Poor performance status;

96
c) High-risk myelodysplastic syndromes;
d) Advanced malignancies;
e) Platelet counts less than 50,000;
f) Known hypersensitivity to DFX or any component of the medication.
2.2. Toxicity:
Gastrointestinal (GI) symptoms (diarrhea, vomiting, nausea, abdominal pain),
headaches, pyrexia, skin rash, increases in serum creatinine, intermittent proteinuria,
cytopenias (including agranulocytosis, neutropenia, and thrombocytopenia), hepatic
dysfunction, auditory disturbances, and ophthalmic disturbances. Post marketing
surveillance has shown cases of acute renal failure or cytopenias with fatal outcomes in
patients taking DFX. The relation to DFX in these cases is uncertain.
2.3. Dosing: see below, items 2.6 and 2.7.
2.4. Monitoring:
2.4.1. Prior to starting treatment: obtain baseline CBC, creatinine with clearance
estimation in duplicate, ferritin, liver function tests, audiogram, and eye
examinations.
2.4.2. Monthly CBC, ferritin, creatinine, urine protein levels, and liver function tests.
2.4.3. Discontinue temporarily if ferritin level falls below 500ng/mL.
Suggested monitoring of DFX-related toxicity is shown below.
Toxicity
Tests
Frequency
Alteration In Rx
High frequency
sensorineural hearing
loss
Audiogram
Annually; if
symptomatic, check
immediately
Stop DFX;
repeat audiogram at 3
month intervals until
normal or stable
Retinopathy (pigmentary
degeneration); cataracts;
corneal opacities; visual
impairment
Eye exam
including visual
acuity, slit-lamp
and fundoscopy
Annually; if
symptomatic, check
immediately
Stop DFX if retinopathy
or hearing impairment
Renal impairment
Creatinine and
protein/creatinine
ratio
Creatinine weekly
for the first month,
then monthly;
Protein/creatinine
ratio every 3 months
See dose modification
below (items 2.5.4 and
2.6.4)
2.5. Specific information about Exjade
2.5.1. Exjade is available in 125mg, 250mg, and 500mg tablets;
2.5.2. Starting dose: 20mg/kg/day.
2.5.3. Dose modification: 5-10mg/kg/day increments every 3-6 months if necessary
depending on serum ferritin trends. Doses should not exceed 40mg/kg/day.
2.5.4. Dose reduction: 50% for starting dose if creatinine clearance 40-60mL/min or
moderate (Child-Pugh B) hepatic impairment. If the serum creatinine level increases
more than 33% over the course of two consecutive visits, the dose should be
reduced by 10mg/kg. For pediatric patients, the dose should be reduced by 10mg/kg
if the serum creatinine is greater than the upper limit of normal on 2 consecutive
visits.

97
2.5.5. Administration: Exjade should be taken once daily on an empty stomach (at least
30 min prior to eating). Tablets should be completely dispersed by stirring in water,
orange juice, or apple juice until there is a fine suspension. Doses <1 gram should
be dispersed in 3.5 ounces of liquid, and doses 1 gram should be dispersed in 7
ounces of liquid. After swallowing, any residue should be resuspended in a small
volume of liquid and swallowed. Doses should be separated by 2 hours from
aluminum containing antacids.
2.6.Specific information about Jadenu and Jadenu Sprinkles
2.6.1. Jadenu is available in 90mg, 180mg, and 360mg tablets or granules (Jadenu
Sprinkles).
2.6.2. Starting dose: 14mg/kg/day.
2.6.3. Dose modification: 3.5-7mg/kg/day increments every 3-6 months if necessary
depending on serum ferritin trends. Doses should not exceed 28mg/kg/day.
2.6.4. Dose reduction: 50% for starting dose if creatinine clearance 40-
60mL/min/1.73m
2
or moderate (Child-Pugh B) hepatic impairment. If the serum
creatinine level increases more than 33% over the course of two consecutive visits,
the dose should be reduced by 7mg/kg. For pediatric patients, the dose should be
reduced by 7mg/kg if the serum creatinine is greater than the upper limit of normal
on 2 consecutive visits.
2.6.5. Administration: Jadenu should be taken once daily preferably at the same time of
the day, on an empty stomach or with a light meal (contains less than 7% fat content
and approximately 250 calories). Examples of light meals include 1 whole wheat
English muffin, 1 packet jelly (0.5 ounces), and skim milk (8 fluid ounces) or a
turkey sandwich (2 oz. turkey on whole wheat bread w/ lettuce, tomato, and 1
packet mustard). Jadenu tablets may be crushed and mixed with soft foods (e.g.,
yogurt or apple sauce) immediately prior to use and administered orally.
Commercial crushers with serrated surfaces should be avoided for crushing a single
90 mg tablet. The dose should be immediately and completely consumed and not
stored for future use. Take Jadenu Sprinkles by sprinkling the full dose on soft food
(e.g. yogurt or apple sauce) immediately prior to use and administered orally. Doses
should be separated by 2 hours from aluminum containing antacids.
3. Combination therapy: deferoxamine – Desferal, and deferiprone (DFP) - Ferriprox
3.1. In combination therapy, deferoxamine should be prescribed as above, preferably 7
days a week; if patient is admitted, it may be placed as a 24-hour infusion.
3.2. Deferiprone is an oral medication for iron chelation, available in 500mg tablets and
100mg/mL oral solution.
3.3. Contraindications: severe hepatic impairment, creatinine clearance below
15ml/min/1.73m
2
, known hypersensitivity to deferiprone or any component of the
medication.
3.4. Toxicity: neutropenia (6.2%), agranulocytosis (1.7%), zinc deficiency, chromaturia
(reddish brown discoloration of the urine), GI symptoms (nausea, vomiting,
abdominal pain or discomfort), joint pain, headache.
3.4.1 Avoid concomitant use of drugs known to be associated with neutropenia
or agranulocytosis if possible.

98
3.5. Starting dose: 25mg/kg tid (75mg/kg/day daily). Maximum dose is 33mg/kg tid
(daily total 99mg/kg/day).
3.6. Dose reduction: not recommended for mild or moderate liver impairment, or
creatinine clearance above 15ml/min/1.73m
2
.
3.7. Administration: take first dose in the morning, second dose at midday, third dose in
the evening, with meal. Allow at least 4-hour intervals between deferiprone and
medications or supplements containing polyvalent cations, e.g. aluminum or zinc.
3.8. Monitoring:
3.8.1. Prior to starting treatment: obtain complete blood count with neutrophil
count, serum transaminases, and zinc levels.
3.8.2. Weekly neutrophil counts
3.8.3. Monthly ferritin, transaminases, and zinc.
3.8.4. Discontinue if ferritin level falls below 500ng/mL.
3.8.5. Management of neutropenia: discontinue DFP and all medications that can
cause neutropenia and follow blood counts daily until recovery. DO NOT
resume DFP in patients who develop agranulocytosis, DO NOT
rechallenge patients with neutropenia above 500 unless benefit outweighs
the risks.
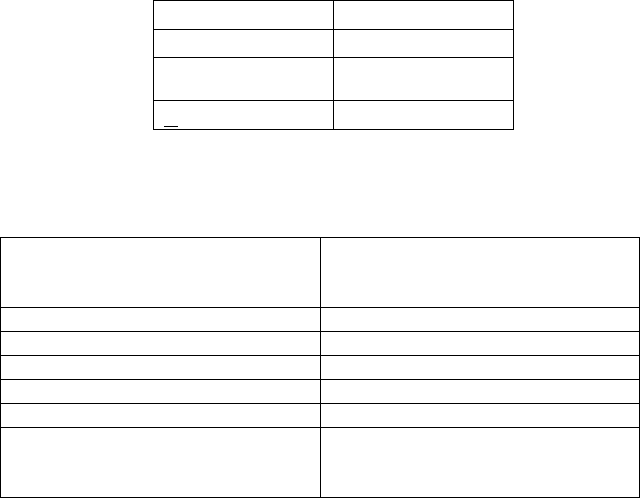
99
XX. VITAMINS AND OTHER MINERAL SUPPLEMENTS
It is recommended that all allogeneic patients have iron-free multiple vitamin/mineral
supplementation for one year or until all immunosuppressive therapy is discontinued after the
transplant. Autologous patients should continue supplementation for one year if dietary
intake does not meet daily requirements. Iron supplementation should not be used routinely
in any patient unless iron deficiency is clearly documented. Most patients have iron-overload
because of red cell transfusions and increased absorption of iron in the GI tract (see Section
XIX).
A. Calcium and Vitamin D daily intake requirements
Adequate calcium and vitamin D intake are necessary in order to decrease the risk of
bone complications after transplant. Women with ovarian failure and patients who
require long-term treatment with corticosteroids have a high risk of osteoporosis, and
pediatric patients can have poor bone development after chemotherapy and radiation.
Avoidance of sunlight and the use of sunscreen to block UV radiation can contribute to
vitamin D deficiency.
Patients who cannot consume adequate calcium or vitamin D from foods should receive
supplements to meet their daily requirements. Supplemental calcium should be given in
divided doses, preferably as calcium citrate. Some "natural" calcium supplements do not
contain enough bioavailable calcium to prevent osteopenia. The maximum amount that
can be absorbed with each dose is 500 mg. See Section XI for prevention of
osteoporosis.
i. CALCIUM REQUIREMENTS FOR PATIENTS DURING STEROID
THERAPY:
Calcium intake above these levels is not recommended, as it may interfere with the
absorption of other nutrients.
ii. CALCIUM REQUIREMENTS FOR PATIENTS NOT ON STEROIDS
Age
Daily Minimum
Requirement after
Transplant (milligrams)
Children 7-12 months
260
Children 1-3 years
700
Children 4-8 years
1000
Children 9-18 years
1300
Adult Males
1000-1200
Adult Females;
On hormone therapy
No hormone therapy
1000-1200
1500
7-12 months:
600 mg/day
1-3 years:
1000 mg/day
4-8 years:
1200 mg/day
> 9 years:
1500 mg/day

100
iii. Vitamin D requirement
Table 1: Vitamin D3 (or D2) Supplementation
*, ****
Adults (>18 yrs)
Children (<18 yrs)
Treatment of Insufficiency [Vitamin D (25 Hydroxy) levels 20-30 ng/mL]***
▪ Routine
▪ 25 mcg/day
▪ Age < 1 yr:
─ 10 mcg daily
(20 mcg in dark skinned)
▪ Age 1-8 yr:
─ 15 mcg daily
▪ Age 9-18 yr:
─ 20 mcg daily
▪ Malabsorption syndromes**
▪ 1,250 mcg per week
▪ Age < 1 yr:
─ Consult Endocrinology
▪ Age 1-18 yr:
─ 1,250 mcg per week or
─ 125 mcg daily
▪ Chronic Renal Disease
▪ Consult Nephrology
▪ Consult Nephrology
Treatment of Deficiency [Vitamin D (25 Hydroxy) level <20 ng/mL]***
▪ Uncomplicated
▪ 1,250 mcg per wk x 8 (Repeat
if Vitamin D (25 Hydroxy) level
< 30 ng/mL otherwise treat as
for insufficiency above)
▪ Age 1-12 months:
─ 25-50 mcg daily x 8 wks
▪ Age 1-18 yr:
─ 25-125 mcg daily x 8 wks
or
─ 1,250 mcg weekly x 8
(Repeat if Vitamin D (25
Hydroxy) level < 30 ng/mL
otherwise treat as for
insufficiency above)
▪ Malabsorption syndromes**
▪ 250-1,250 mcg daily or every
other day
▪ UVB irradiation in patients
also with skin GVHD
▪ Age < 1 yr:
─ Consult Endocrinology
▪ Age 1-18 yr:
─ 1,250 mcg per week
▪ Chronic Renal Disease
▪ Consult Nephrology
▪ Consult Nephrology
*
Currently there does not seem to be substantive benefit by choosing Vitamin D2 or vitamin D3 over the other
with regard to correcting Vitamin D (25 Hydroxy) levels. The more important decision is prescribing enough.
Dose frequency appears to be less important than cumulative amount so that 50 mcg daily for 50 days is
approximately equivalent to giving 1,250 mcg monthly for 2 months.
**
Patients who remain deficient or insufficient after adequate therapy are generally treated with hydroxylated
vitamin D metabolites which are more readily absorbed or, if feasible, with sun or sunlamp exposure. While 25-
OH vitamin D (calcidiol) is the most logical choice of activated vitamin D for patients with liver disease,
calcidiol is not readily available in the U.S. The 1,25-OH activated formulation of vitamin D (Calcitriol) is used
most commonly in chronic renal disease when there is secondary hyperparathyroidism. Calcitriol can also be
used in patients with liver disease or severe malabsorption when there is a lack of the 25-OH vitamin D
substrate to be converted to 1,25-OH vitamin D by the kidney.
***
Vitamin D (25 Hydroxy) levels are generally rechecked 2-3 months after beginning therapy and the target level
is within normal range.
****1000 IU = 25mcg
50,000 IU = 1,250 mcg
101
B. Magnesium supplementation
Cyclosporine and tacrolimus (FK-506) increase urinary excretion of magnesium, resulting in low
serum magnesium levels. Hypomagnesemia has been associated with seizures in patients treated
with cyclosporine or tacrolimus (FK506). All patients receiving these immunosuppressive drugs
require magnesium supplementation and monitoring serum magnesium levels monthly, or more
often as indicated. Oral magnesium with protein (133 mg/tablet) is better tolerated than
magnesium oxide. The magnesium requirements range from 6 to 20 or more tablets daily for
adults and 1 to 9 or more tablets daily for children. Some patients may require intravenous
supplementation (magnesium sulfate) if oral administration causes diarrhea.

102
XXI. DIETS AND OTHER NUTRITIONAL GUIDELINES
A. Diet for immunosuppressed patients after transplant
Patients after hematopoietic transplant or after high dose chemotherapy are at increased
risk of developing food-related infections. It is recommended that all transplant
recipients follow the nutrition guidelines for discharge home, including the Diet for
Immunosuppressed Patients. These guidelines can be found at www.seattlecca.org
under patientsandfamilies/nutrition/nutritionDietsguidelines/
osteoporosisNutritionguidelines. The duration of immunosuppressed patient diet
depends on the immunocompromised status of the patient and the type of transplant, as
described below:
Allogeneic transplant recipients should follow the immunosuppressed patient diet
guidelines until all immunosuppressive treatments are discontinued.
Autologous transplant recipients should follow the immunosuppressed patient diet
guidelines until one month after discontinuation of corticosteroids or three months
after chemotherapy or transplant (whichever occurs later) and as long as there are
no GI symptoms.
B. Additional dietary recommendations:
1. Diet for patients receiving treatment with corticosteroids:
In addition to the Diet for Immunosuppressed Patients, nutritional recommendations
to minimize the risk of osteoporosis are needed (see Section XI). These nutritional
guidelines can also be found at www.seattlecca.org/ patientsandfamilies/nutrition/
nutritionDietsguidelines/osteoporosisNutritionguidelines.
2. Diet for patients with graft-versus-host disease of gastrointestinal tract:
In addition to the Immunosuppressed Patient Diet, specific diets are recommended
for patients with GVHD of the GI tract to help alleviate the gastrointestinal
symptoms. Two different gastrointestinal diets (GI1 and GI2) have been developed
by the dietitians at the Fred Hutch. These GI1 and GI2 diets have limited amounts of
fats, fiber, lactose, acidic items and GI irritants. The diets can be found at
www.seattlecca.org under patientsandfamilies/nutrition/nutritionDietsguidelines/.
For patients with severe diarrhea (exceeds 8-10 ml/kg/day) or significant crampy
abdominal pain, bowel rest (NPO) is recommended. TPN at 1.5 x basal energy needs
or higher, 1.5-2.0 g protein/kg with supplemental zinc is also usually needed.
Replacement of stool losses on a mL/mL basis with half-normal saline hydration is
recommended. As diarrhea subsides, the response to oral feeding is highly variable.
103
When oral intake is appropriate, we recommend beginning with isotonic beverage in
small amounts and gradually progressing to the GI1 diet and subsequently to the GI2
diet as tolerated (see Table next page).
GVHD of the upper intestine or stomach may present only as anorexia, nausea, and
early satiety. High-fat foods are generally poorly tolerated. Empiric lactose
restriction should be considered. Patients may find it easier to meet energy and
protein needs with nutritional supplements sipped continuously throughout the day.

104
Gastrointestinal GVHD Diet Progression*
Phase
Symptoms
Diet Diet Intolerance
1. Bowel rest
GI cramping
Large volume watery diarrhea
Depressed serum albumin
Severely reduced transit time
Small bowel obstruction or diminished
bowel sounds
Nausea and vomiting
Oral: NPO
IV: stress energy and protein
Requirements
2. Introduction of
oral feeding
Minimal GI cramping
Diarrhea less than 500 ml/day
Guaiac-negative stools
Improved transit time (minimum 1.5
hours)
Infrequent nausea and vomiting
Oral: isosmotic, low-residue,
low-lactose beverages,
initially 60 ml every 2-3
hours, for
several days
IV: as for Phase 1
Increased stool volume
or
diarrhea
Increased emesis
Increased abdominal
Cramping
3. Introduction of
solids
Minimal or no GI cramping
Formed stool
Oral: allow introduction of
solid food, once every 3-4
hours: minimal lactose
a
,
low fiber, low fat (20-40
gm/day)
b
, low total
acidity, no gastric irritants
IV: as for Phase 1
As in Phase 2
4. Expansion of
diet
Minimal or no GI cramping
Formed stool
Oral: minimal lactose
a
, low
fiber, low total acidity, no
gastric irritants; if stools
indicate fat
malabsorption: low fat
b
IV: as needed to meet
nutritional requirements
As in Phase 2
5. Resumption of
regular diet
No GI cramping
Normal stool
Normal transit time
Normal albumin
Oral: progress to regular
diet by introducing one
restricted food per day:
acid foods with meals,
fiber-containing foods,
lactose-containing foods.
Order of addition will
vary, depending on
individual tolerances and
preferences.
Patients no longer
exhibiting steatorrhea
should have the fat
restriction liberalized
slowly
IV: discontinue when oral
nutritional intake meets
estimated needs
As in Phase 2
a
Lactose is one of the last disaccharidases to return following villous atrophy. A commercially-prepared lactose solution (Lactaid
R
) is used
to reduce the lactose content of milk by >90%. Lactaid
R
milk (100% lactose-free) is also commercially available.
b
Additional calories may be provided by commercially available medium chain triglycerides which do not exacerbate symptoms.
*Adapted from Darbinian J, Schubert MM. Special management problems. In: Lenssen P, Aker SN, eds. Nutritional Assessment
and Management During Marrow Transplantation. A Resource Manual. Seattle, WA: Fred Hutchinson Cancer Research Center;
1985;63-80.

105
XXII. NATUROPATHIC REMEDIES: HERBAL AND NUTRIENT SUPPLEMENT
PREPARATIONS
Allogeneic transplant patients:
Herbal/botanical preparations should not be given during immunosuppressive
therapy or in patients with chronic GVHD. One month after discontinuation of all
systemic immunosuppressive treatment and resolution of manifestations of chronic
GVHD, herbal/botanical preparation may be given at the discretion of the primary
physician.
Autologous transplant patients:
Herbal/botanical preparations should not be given until complete recovery of any
gastrointestinal toxicity and until prednisone therapy has been discontinued for one
month.
Further information regarding guidelines for the use of herbal and nutrient supplement
preparations can be found at www.seattlecca.org under
patientsandfamilies/nuritionDietsguidelines, Guidelines for herbal & nutrient supplements during
hematopoietic stem cell transplantation and high-dose chemotherapy.
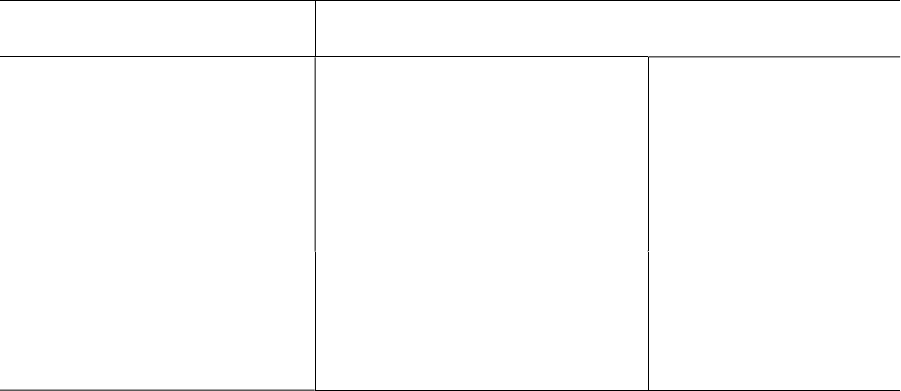
106
XXIII. RETURN TO SEATTLE FOR LONG-TERM FOLLOW-UP EVALUATION
All adults who have had an allogeneic transplant and all children who have had either an
allogeneic or autologous transplant should return to the Fred Hutch for a comprehensive
evaluation at one year after the transplant. Depending on clinical indications, follow-up
evaluations at subsequent intervals may be arranged. Children should return for subsequent
evaluations at 2, 3, 5, 10, 15, and 20 years after the transplant. These evaluations focus on
hematologic and immunologic function, assessment of the original disease, and thorough
screening for any late transplant complications. The LTFU evaluation requires four to five
working days to complete. A detailed summary of findings and recommendations will be
forwarded to the referring physician. Appointments must be scheduled at least 4 months in
advance by calling the LTFU office assistant at (206) 667-4415 or by sending a FAX to
1-800-376-8197 (toll-free, USA and Canada).
TYPE OF TRANSPLANT
TIME TO RETURN FOR
COMPREHENSIVE EVALUATION
Allogeneic (ADULT)
Autologous (ADULT)
One year after the transplant
One year after the transplant
based on protocol, patient or
physician request
Follow-up evaluations
at other times per
protocol or as clinically
indicated
Allogeneic & Autologous
(PEDIATRIC)
One year, 2, 3, 5, 10, 15, and 20
years after the transplant

107
XXIV. HOW TO SEND SPECIMENS FOR TESTING AT FRED HUTCH
Clinical laboratory testing for patients who received treatment at Fred Hutchinson Cancer
Center (Fred Hutch) is available at the Fred Hutch. The tests most often performed in our
laboratories at the request of referring physicians include BCR/abl transcripts by polymerase
chain reaction (PCR), CMV PCR and chimerism studies by assessment of variable number
tandem repeat polymorphisms.
We ask that you notify the LTFU office by telephone at (206) 667-4415 or by FAX
(Appendix A) to indicate the expected date and time of arrival for specimens that are sent for
testing at the Fred Hutch. The LTFU office will provide detailed instructions regarding
sample collection and shipment information for the specific test(s) requested.
If surgery or biopsy is planned for evaluation of suspected secondary malignancy or
recurrence of disease, please contact our LTFU office before the procedure, whenever
possible.
Guidelines for Sending Clinical Specimens
1. Call the LTFU office at (206) 667-4415 before sending the specimen (Appendix A).
2. Do not send fresh / frozen samples to arrive on Fridays, weekends or governmentholidays.
3. Ship the specimen via an overnight courier service on the day the samples were obtained.
4. Label each tube with
Patient's name
Patient's social security number (if not available, date of birth)
Date that the sample was obtained
Type of specimen (i.e., peripheral blood, bone marrow, serum, left breast mass, etc.)
5. Please complete Test Request Forms that will be faxed to you by our office
6. SAMPLE(S) MUST BE ACCOMPANIED BY THE FRED HUTCH TEST REQUEST
FORMS
7. Shipment charges are the responsibility of the patient or the facility sending the sample.
A study coordinator will forward shipment instructions to patients who are enrolled in
specific protocols that require samples to be sent to the Fred Hutch for research studies.

108
XXV. REFERENCES
Chronic GVHD
1. Sullivan KM. Graft vs. Host Disease. In: Blume KG, Forman SJ, Appelbaum FR eds. Thomas’ Hematopoietic
Cell Transplantation, 3
rd
Edition. Blackwell Publishing; 2004; 635-664.
2. Lee SJ, Vogelsang G, Flowers MED. Chronic graft-versus-host disease. Biol Blood Marrow Transplant 2003;
9: 215-233.
3. Flowers MED, Parker PM, Johnston LJ, et al. Comparison of chronic graft-versus-host disease after
transplantation of peripheral blood stem cells versus bone marrow in allogeneic recipients: long-term follow-
up of a randomized trial. Blood 2002; 100:415-419.
4. Filipovich AH, Weisdorf D,
Pavletic S, et al: NIH Consensus Development Project on Criteria for Clinical
Trials in Chronic GraftVersus-Host Disease: I. Diagnosis and Staging Working Group Report: Biol Blood
Marrow Transplant 2005; 11: 945-955.
5. Shulman HM, Sullivan KM, Weiden PL, et al. Chronic Graft vs. Host syndrome in man. A long-term
clinicopathologic study of 20 Seattle patients. Am. J. Med. 1980; 69:204-217.
6. Stewart BL, Storer B, Storek J, et al. Duration of immunosuppressive treatment for chronic graft-versus-host disease.
Blood 2004; 104:3501-3506.
7. Au BK, Au MA, Chien JW. Bronchiolitis obliterans syndrome epidemiology after allogeneic hematopoietic
cell transplantation. Biol Blood Marrow Transplant 2011;17:1072-8. doi:10.1016/j.bbmt.2010.11.018
8. Cheng GS, Storer B, Chien JW, et al. Lung Function Trajectory in Bronchiolitis Obliterns Syndrome after
Allogeneic Hematopoietic Cell Transplant. Ann Am Thorac Soc. 2016 Nov;13(11);1932-1939.
9. Williams KM, Cheng GS, Pusic I, Jagasia M, Burns L, Ho VT, Pidala J, Palmer J, Johnston L, Mayer S, Chien
JW, Jacobsohn DA, Pavletic SZ, Martin PJ, Storer BE, Inamoto Y, Chai X, Flowers ME, Lee SJ. Fluticasone,
azithromycin, and montelukast treatment for new-onset bronchiolitis obliterans syndrome after hematopoietic
cell transplantation. Biol Blood Marrow Transplant 2016;22:710-6. doi:10.1016/j.bbmt.2015.10.009
10. Flowers ME and Martin PJ. How we treat chronic graft-versus-host disease. Blood 2015;125:606-615.
doi:10.1182/blood-2014-08-551994
11. Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, Palmer J, Weisdorf D, Treister NS,
Cheng GS, Kerr H, Stratton P, Duarte RF, McDonald GB, Inamoto Y, Vigorito A, Arai S, Datiles MB,
Jacobsohn D, Heller T, Kitko CL, Mitchell SA, Martin PJ, Shulman H, Wu RS, Cutler CS, Vogelsang GB, Lee
SJ, Pavletic SZ, Flowers ME. National institutes of health consensus development project on criteria for
clinical trials in chronic graft-versus-host disease: I. The 2014 diagnosis and staging working group report.
Biol Blood Marrow Transplant 2014;doi:10.1016/j.bbmt.2014.12.001
12. Bergeron A, Godet C, Chevret S, Lorillon G, Peffault de Latour R, de Revel T, Robin M, Ribaud P, Socie G,
Tazi A. Bronchiolitis obliterans syndrome after allogeneic hematopoietic sct: Phenotypes and prognosis. Bone
Marrow Transplant 2013;48:819-24. doi:10.1038/bmt.2012.241
13. Pelligrini R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CPM,
Gustafasson P, Hankinson J, Jensen, R, Johnson DC, MacIntyre N, McKay R Miller MR, Navajas D, Pedersen
OF, Wanger J. Interpretative strategies for lung function tests. Eur Respir J 2005;26:948-968. Williams KM,
Chien JW, Gladwin MT, Pavletic SZ. Bronchiolitis obliterans after allogeneic hematopoietic stem cell
transplantation. JAMA 2009;302:306-14. doi:10.1001/jama.2009.1018
14. Carpenter PA, Kitko CL, Elad S, Flowers ME, Gea-Banacloche JC, Halter JP, Hoodin F, Johnston L,
Lawitschka A, McDonald GB, Opipari AW, Savani BN, Schultz KR, Smith SR, Syrjala KL, Treister N,
Vogelsang GB, Williams KM, Pavletic SZ, Martin PJ, Lee SJ, Couriel DR. National institutes of health
consensus development project on criteria for clinical trials in chronic graft-versus-host disease: V. The 2014
ancillary therapy and supportive care working group report. Biol Blood Marrow Transplant 2015;21:1167-87.
doi:10.1016/j.bbmt.2015.03.024
15. Gunn ML, Godwin, JD, Kanne JP, Flowers ME, Chien JW. High-resolution CT findings of bronchiolitis
obliterans syndrome after hematopoietic stem cell transplantation. J Thorac Imaging 2008 Nov;23(4):244-450.
doi:10.1097/RTI.0b013e3181809df0
16. Williams KM, Chien JW, Gladwin MT, Pavletic SZ. Bronchiolitis obliterans after allogeneic hematopoietic
stem cell transplantation. JAMA 2009;302:306-14. doi: 10.1001/jama.2009.1018.
108
XVI. OTHER COMPLICATIONS
A. GONADAL HORMONE INSUFFICIENCY
Gonadal hormone insufficiency is related to the age of the patient and the intensity of the
transplant preparative regimen.
MALES:
Post puberty: Men who were past puberty at the time of transplant may develop primary
gonadal failure. Testosterone replacement should also be considered in men who are
receiving corticosteroids for long-term treatment of chronic GVHD (see Section XI). Men
who receive testosterone replacement therapy should have a baseline prostate exam and
measurement of prostate specific antigen (PSA), liver enzymes and serum lipids. Follow-
up monitoring of these parameters may be appropriate.
Prepubertal: For boys without signs of puberty at age 14 years or failure of pubertal
progression or abnormal growth velocity with hypergonadotropic hypogonadism (high
FSH and LH and low free testosterone) should be considered for androgen or
gonadotropic therapy. Initially a lower dose should be considered to accelerate growth
velocity without advancing bone age. Subsequently, the dose can be increased closer to
end of growth spurt when fusion of growth plates is then acceptable. Hormonal
replacement in prepubertal boys should be done in collaboration with a pediatric
endocrinologist.
FEMALES: Women often develop primary ovarian failure and have symptoms of premature
menopause. They are also at risk for development of osteoporosis. Permanent ovarian
failure invariably occurs in all female patients who receive busulfan and cyclophosphamide
(BU/CY). Recovery of ovarian function has been observed after transplant in 54% of
younger patients (less than 26 years) conditioned with cyclophosphamide alone. The
probability of ovarian function recovery after fractionated TBI is at least 10% by 6 years
after transplant.
Premature (<40 years) or early (40 – 50 years) onset of menopausal symptoms and
osteoporosis can significantly affect the quality of life of women after a hematopoietic cell
transplant (HCT). During the past 30 years, replacement therapy with estrogen alone (for
patients without a uterus) or combined with progestin (for patients with a uterus) has been
used to prevent or treat menopausal symptoms and to prevent bone loss. In children,
hormonal replacement therapy (HRT) is needed after transplant to promote the development
of secondary sexual characteristics.
Estrogen can treat hot flashes, vaginal and vulvar symptoms, prevent bone loss and improve
the quality of life for HCT recipients who are postmenopausal or who have premature
ovarian failure. The positive effect on cognitive function claimed by many women taking
estrogen remains to be confirmed. In young girls, estrogen replacement therapy is often
critical for the development of secondary sexual characteristics and for the attainment of
peak bone mass in early adulthood.
108
XVI. OTHER COMPLICATIONS
A. GONADAL HORMONE INSUFFICIENCY
Gonadal hormone insufficiency is related to the age of the patient and the intensity of the
transplant preparative regimen.
MALES:
Post puberty: Men who were past puberty at the time of transplant may develop primary
gonadal failure. Testosterone replacement should also be considered in men who are
receiving corticosteroids for long-term treatment of chronic GVHD (see Section XI). Men
who receive testosterone replacement therapy should have a baseline prostate exam and
measurement of prostate specific antigen (PSA), liver enzymes and serum lipids. Follow-
up monitoring of these parameters may be appropriate.
Prepubertal: For boys without signs of puberty at age 14 years or failure of pubertal
progression or abnormal growth velocity with hypergonadotropic hypogonadism (high
FSH and LH and low free testosterone) should be considered for androgen or
gonadotropic therapy. Initially a lower dose should be considered to accelerate growth
velocity without advancing bone age. Subsequently, the dose can be increased closer to
end of growth spurt when fusion of growth plates is then acceptable. Hormonal
replacement in prepubertal boys should be done in collaboration with a pediatric
endocrinologist.
FEMALES: Women often develop primary ovarian failure and have symptoms of premature
menopause. They are also at risk for development of osteoporosis. Permanent ovarian
failure invariably occurs in all female patients who receive busulfan and cyclophosphamide
(BU/CY). Recovery of ovarian function has been observed after transplant in 54% of
younger patients (less than 26 years) conditioned with cyclophosphamide alone. The
probability of ovarian function recovery after fractionated TBI is at least 10% by 6 years
after transplant.
Premature (<40 years) or early (40 – 50 years) onset of menopausal symptoms and
osteoporosis can significantly affect the quality of life of women after a hematopoietic cell
transplant (HCT). During the past 30 years, replacement therapy with estrogen alone (for
patients without a uterus) or combined with progestin (for patients with a uterus) has been
used to prevent or treat menopausal symptoms and to prevent bone loss. In children,
hormonal replacement therapy (HRT) is needed after transplant to promote the development
of secondary sexual characteristics.
Estrogen can treat hot flashes, vaginal and vulvar symptoms, prevent bone loss and improve
the quality of life for HCT recipients who are postmenopausal or who have premature
ovarian failure. The positive effect on cognitive function claimed by many women taking
estrogen remains to be confirmed. In young girls, estrogen replacement therapy is often
critical for the development of secondary sexual characteristics and for the attainment of
peak bone mass in early adulthood.
109
a) Special Considerations:
It is unclear if estrogen alone or combined with progesterone replacement will add to the
already increased risk of secondary breast cancer in posttransplant women (Friedman et
al.Blood;2008;111:939-944). Among patients who survived for more than 10 years
posttransplant the observed/expected risk ratio is 3.2 for breast cancer (Rizzo et al, Blood
2009; 113: 1175-1193). Radiation has been identified as the primary risk factor associated
generally with the development of solid tumors after a stem cell transplant.
b) Hormonal Replacement Guidelines for Girls:
In young girls, estrogen replacement therapy is often critical for the development of
secondary sexual characteristics during the transitional from adolescence to adulthood and
for the attainment of peak bone mass in early adulthood. Survivors with
hypergonadotrophic (high FSH, low estradiol ) and hypogonadotropic (low FSH, low
estradiol) should be considered for hormone replacement therapy. Initially low dose
hormone therapy should be used . Cyclic dosing should be used at later stages to induce
regular menstrual cycles. It is recommended to hold hormone replacement therapy for 2
months at regular intervals to check for resolution of gonadal insufficiency . Hormonal
replacement in prepubertal girls should be done in collaboration with a pediatric
endocrinologist.
c) Hormonal Replacement Guidelines for Women:
Temporary relief of menopausal symptoms:
Unless medically contraindicated, a finite course of estrogen alone (women without
uterus) or combined with progesterone (women with uterus) may be prescribed for the
temporary relief of menopausal symptoms, provided that patients are frequently
reassessed by their physician to determine the appropriate duration of therapy.
General considerations for posttransplant Gonadal Hormonal Therapy (HRT) include:
• Management of ovarian failure should be tailored according to a patient’s particular
clinical manifestations and individual risks for side effects of HRT such as:
a) history (or family history) of breast cancer
b) history of deep venous thrombosis, stroke or hypercoaguable state
c) history (or family history) of colorectal cancer
d) severe osteoporosis with vertebral crush fractures
e) presence of absence of a uterus
• Overall benefits and risks of long-term HRT should be discussed with each patient.
• Information about non-hormonal alternatives for management of ovarian failure
manifestations should be discussed with all patients.
• A patient and her physician should be able to clearly state the indication (s) for which the
patient is to start (or continue) posttransplant HRT.
• HRT should be prescribed at the lowest effective dose.
• Annual gynecological follow-up evaluation is recommended for all women.
• Monthly self-breast examination is recommended for all women.
• Baseline mammography is recommended for all women from 35-40 years of age. Annual
follow-up is also recommended.
• Yearly re-evaluation of a patient’s ovarian failure management plan is recommended to
determine if it remains the most appropriate plan for that patient.

110
Specific Contraindications to HRT:
• Systemic estrogen alone or combined with progesterone should not be prescribed for patients
with a history of thromboembolic diseases (i.e., venous thrombosis, pulmonary embolism,
strokes, etc.), hypercoagulation disorders, breast cancer, coronary artery disease, or active
liver disease.
Alternatives to HRT:
• Diet, exercise and other non-hormonal strategies are available for management of hot flashes,
insomnia and mood disturbances.
• Topical estrogen alone may relieve local vaginal/vulva symptoms caused by gonadal
insufficiency.
Use of hormone of supplementation as first line of treatment is not recommended for
osteoporosis/osteopenia except for children or young adults. Please see LTFU Section XI:
General Guidelines For Prevention of Osteoporosis and Glucocorticosteroid Induced
Osteoporosis After HCT
• Difficulties such as decreased libido and/or dyspareunia may be multifactorial in etiology and
may often be managed without the use of systemic conjugated equine estrogen and
medroxyprogesterone.
B. Endocrine Abnormalities
Compensated or overt hypothyroidism, thyroiditis and thyroid neoplasms may develop in
patients who received radiation. The incidence of compensated hypothyroidism after
fractionated total body irradiation (TBI) before transplant ranges between 15-25%.
Patients should be evaluated yearly with physical examination and thyroid function tests.
Growth hormone (GH) deficiency and growth failure (decreased growth rate/year) occurs
in 70-80% of children who received total body irradiation or 1800 cGy cranial
irradiation. The onset of GH deficiency and growth failure varies with the age of the
child at the time of irradiation. The onset of these problems appears to occur later in
younger children than in peri-pubertal children. All children should have height
monitored at least annually, and those <14 years of age should have annual GH testing
until they either develop GH deficiency or are >14 years of age, whichever occurs first.
Among pre-pubertal children, treatment with total body irradiation, busulfan or >2400
cGy testicular irradiation may delay subsequent pubertal development. Children who
received busulfan appear to have the highest risk of delayed or absent pubertal
development. Approximately half of the very young children treated with total body
irradiation progress through pubertal development at an appropriate age, while older
children treated with total body irradiation have a higher risk of delayed pubertal
development. Treatment with cyclophosphamide alone does not delay pubertal
development.
Beginning at age 10, all children should have Tanner development scores determined as
part of an annual physical examination. Children who are Tanner Stage I or II by age 12
years should be referred to a pediatric endocrinologist to evaluate the need for hormonal
supplementation.

111
C. Ocular complications
An annual eye exam with slit lamp examination is recommended for all patients who
have had an allogeneic transplant and for those who are at risk of cataracts. The risk of
cataracts after transplant is high for patients who received fractionated TBI (30 – 50%)
and for patients treated with corticosteroids after the transplant (45%). In patients who
received neither TBI or prior cranial irradiation, the incidence for cataract is
approximately 15% and, is primarily due to corticosteroids. The median time to develop
cataracts after transplant ranges from 2 to 5 years. Cataract extraction can be performed
safely even when ocular sicca is present. Unanticipated complications after placement of
an intraocular lens have not been reported. Other late complications involving the eyes
are related to chronic GVHD as described in Section X A and B.
D. Oral complications and guidelines for dental care
New oral pain or dryness beyond day + 100 after allogeneic transplant suggests
development of chronic GVHD involving the salivary glands or mucosal surface.
Cultures for candida and DFA or rapid cultures for herpes simplex virus should be
obtained to rule out concomitant infections if clinically indicated. A dental/oral medicine
consultation should be strongly considered in all patients with oral complications. If you
have questions about dental care during treatment for GVHD that are unanswered below,
please call the LTFU office who will provide instructions on how to take oral cavity
photos that you can send to [email protected] with your clinical impression and
question. Our LTFU/Oral Medicine can then review these and provide further advice.
General guidelines for dental care for autologous and allogeneic transplant recipients are
provided in the Table below.
General guidelines for dental care in hematopoietic transplant recipients include (see Table 1):
• Routine dental health examinations (with radiographs as needed) are recommended to
monitor for tooth decay and oral hygiene effectiveness, gingivitis and/or periodontitis.
Dental exams can take place any time after transplant and should be done every 6-12
months for routine oral health assessment, to evaluate/treat chronic GVHD (allogeneic
patients) and to screen for oral cancers. (see Table 1)
• Routine dental exam/cleanings should be delayed for first 6 months after transplant due
to increased risk of bacteremia and pneumonia while patients are still
immunocompromised. After the first 6 months, routine (not deep) cleaning either by
ultrasonic or manual dental scaling are reasonable provided certain other criteria are met
(see Table 1).
• Periodontal therapy (Deep cleaning) can be done after the first 6 months if the additional
criteria over and above those set for routine cleaning are met (see Table 1).
• Elective (non-urgent/non-emergency) restorative dental treatment like fillings and
crowns, or elective surgical procedures like dental extraction of non-infected teeth,
implants and gum graft surgery should be delayed until immunity is recovered and
patient has discontinued systemic immunosuppressive treatments. (see Table 1)

112
• “Cosmetic” dental care like dentures are considered safe so long as no extractions or
surgeries are needed. Veneers and other elective restorative procedures should be delayed.
Teeth whitening is reasonable beyond 6 months posttransplant. Invisalign therapy is not
recommended within the first 6 months. Traditional orthodontia is deferred until patient has
no active GVHD and is off all systemic immunosuppression. (see Table 1)
• Emergency or Urgent Care should be carefully coordinated between managing
dentist/oral surgeon and medical team so that appropriate supportive and medical care
can be discussed. Important considerations include:
1. Prophylactic and/or therapeutic antibiotics to minimize risk of bacteremia
complications:
a. For patients with an indwelling central venous catheters, follow American Heart
Association (AHA) recommendations for low-moderate endocarditis risk.
b. For short non-surgical/non-invasive surgical procedures, also follow AHA
prophylactic antibiotic recommendations, and extend treatment if there is
significant local dental infection and risk of subsequent spread of infection
(local or disseminated).
2. Other strategies to reduce spread of infection:
a. Chlorhexidine oral rinse for 3 minutes immediately prior to treatment.
b. Minimize aspiration of aerosolized bacteria by using a rubber dam, high
volume suction, minimal air-water sprays during procedures.
3. Platelet support depending on invasiveness of treatment and risk of bleeding.
Other medical support (e.g. stress dose steroids, adjustments to anticoagulation therapy).
Other key points / recommendations:
• More frequent cleanings may be required based on oral health conditions. Ultrasonic
cleaning carries slightly more risk of aspiration than manual scaling but is generally
acceptable.
• Patients should carry out focused and effective oral hygiene (brushing, flossing, etc.) as
good oral hygiene can be protective in preventing oral GVHD flares.
• Patients with dry mouth should be placed on dental decay prevention regimen that
minimally includes daily brush-on prescription-strength fluoride gel or toothpaste or
rinses to reduce the risk of dental decay. Other measures to promote salivation should be
encouraged (oral moisturizing agents, sugar-free gums or candy, and prescription drugs
to stimulate saliva flow).
• Patients who have received bisphosphonate therapy or on or just completed
denosumab therapy are at a risk for osteonecrosis of the jaw (ONJ). Risk depends on
the type of bisphosphonate, dose, frequency, and total duration of treatment. Reclast
(zoledronic acid) is considered to be at very low risk for ONJ. Zometa (another brand of
zoledronic acid) and pamidronate (Aredia) are considered to be at highest risk for
development of ONJ. The risk for MRONJ in patients treated with oral bisphosphonates
increases steadily over time and is of higher concern in those with greater than 3 years of
use. Bisphosphonates will persist in bone for as long as 10-15 years after discontinuation.
Denosumab (Xgeva) has also been associated with ONJ but the risk for ONJ with

113
denosumab will decrease over 6-7 months after discontinuation. Patients who previously
received bisphosphonates and switched to denosumab may be at an even higher risk for
ONJ compared to either agent used alone.
Recommendations for patients who have received bisphosphonate therapy or on or just
completed denosumab therapy are at a risk for osteonecrosis of the jaw (ONJ:
a. Prevent trauma and irritation from dentures
b. Support excellent dental and periodontal health in order to avoid advancing dental
infections or problems that would ultimately need dental surgery to manage.
c. When patients at risk for ONJ need dental procedures, the least invasive but
effective procedure to solve the problem should be chosen.
Stabilization/restoration of a tooth with a root canal or crown is preferable to
extracting the tooth.
d. Any dental surgery – extractions, implants, periodontal, or endodontic, is
considered high risk for development of ONJ if there has been prior or
ongoing therapy with bisphosphonates or denosumab therapy.
e. If the risk/benefit ratio has been explored and a tooth must be removed, the
procedure should be done by a skilled Oral Surgeon who will use extreme
caution to avoid any excessive trauma to the bone and achieve primary closure
of the site.
• Special attention should be paid to potential head and neck cancers in transplant
survivors – especially lip and oral cavity cancer. Risk is related to cumulative total body
or local irradiation exposure and chronic GVHD.
General guidelines include:
a. Patient counseling to avoid additional risks, specifically, to follow protection
against sun exposure to lips, avoid tobacco products and avoid excess alcohol
beverage intake.
b. Adjunctive examination techniques such as increased uptake of applied toluidine
blue vital dye within dysplastic or neoplastic oral mucosal lesions may be
diagnostically helpful for screening.
c. Serial lesion photographs can be an important component of patient management.
d. Suspicious lesions should be managed comprehensively and followed closely until
resolved or definitive diagnosis is made.

114
Table 1: Dental Care Guidelines for Autologous and Allogeneic Transplant Recipients
Dental Procedure
Time after Transplant
Until 6 months
After 6 months ****
LOW-RISK HIGH-RISK
Not receiving IST for active GVHD* or
getting maintenance with anti-CD20
therapy or other cytotoxic therapy AND
with ANC >1000, Plts >30K
Receiving IST or
maintenance with anti-CD20
therapy or other cytotoxic
therapy, CD34 selected
transplant or ANC <1000,
Plts <30K
Routine Dental Care
Exam every 6-12 months
YES
YES
YES
Routine Dental Cleanings
NO
YES, with antibiotics if central line still in
place
YES, with antibiotics and/or
IVIG** as clinically
indicated
Periodontal Therapy
Scaling/root planning +/-
curettage (dental deep
cleaning)
NO
YES, for autologous (no contraindications)
YES, for allogeneic with considerations for
additional medical support
NO
Restorative Dental Care***
Crowns
Emergent ONLY
with antibiotics
Emergent ONLY with antibiotics
Emergent ONLY with
antibiotics and/or IVIG
Fillings
Emergent ONLY
with antibiotics
Emergent ONLY with antibiotics
Emergent ONLY with
antibiotics and/or IVIG
Surgical Treatments
Dental extractions
Emergent ONLY
with antibiotics
Emergent ONLY with antibiotics
Emergent ONLY with
antibiotics and/or IVIG
Implants
NO
Autologous – NO
Allogeneic – NO
NO
Gingival grafts
NO
YES, for autologous (no contraindications)
YES, for allogeneic with considerations for
additional medical support
NO
Cosmetic Dental Care
Teeth whitening
NO
YES
YES
Orthodontia
NO
NO
NO
Dentures
YES, if no
surgery needed
YES, if no surgery needed
YES, if no extractions are
needed
Abbreviation: IST = immunosuppression; ANC = absolute neutrophils count, Plts = platelets.
* Prophylactic IST or prednisone dose < 0.5mg/kg/day is OK if GVHD considered inactive
** IVIG should be considered if serum IgG level is below 400 mg/dL
***
If treatment is urgent/or emergency due to overall immune/GVHD status – that is, dental disease is at risk for
seriously compromising patient status, planning should consider strategies to reduce local and systemic infection spread
and bleeding.
****Beyond 1 year posttransplant, all dental procedures without additional precaution are OK, if all conditions
below are met:
– No indwelling central venous catheter
– At least 3 months recovery from the last Rituxan
– No active GVHD defined by discontinuation of all IST at least for 8 months
– IgG level > 400 mg/dL
– ANC >1000 cells/ul
– Platelet count > 30K/ul
– Not receiving cytotoxic therapy as maintenance treatment

115
E. Renal insufficiency
Nephrotoxic drugs are the most common cause of impaired renal function after a stem
cell transplant. Monitoring renal function and drug levels is recommended for all patients
who are at risk of renal insufficiency (Section III C & D).
F. Neurological Complications
Peripheral neuropathy and central nervous system complications may develop after
transplantation. Neurological complications may be caused by drugs used to control
GVHD (cyclosporine, tacrolimus) (Section X), electrolyte abnormalities, infection
(HHV-6, HSV, VZV, fungal organisms, toxoplasma, among others), prior cranial
irradiation, intrathecal chemotherapy, GVHD and malignancy. The following evaluation
is recommended:
1) Perform neurological examination including mini-mental state exam.
2) Consider
- Medications (CSA, FK506, opiods, benzodiazepines, high-dose steroids, voriconazole, etc) and check
CSA/FK506 levels
- Metabolic abnormalities (hypo/hypernatremia, hypercalcemia, hypercapnia, hyperosmolarity, renal or
hepatic failure, hypothyroidism, adrenal insufficiency, hypoglycemia, etc.)
- Non-CNS infection such as UTI, pneumonia, etc.
- Unremitting pain or insomnia
- Intracranial hemorrhage
- Hypovolemia – due to bleeding or other cause
- Head trauma
- CNS malignancy
- CNS infection
When available, refer to institutional policies on the management of patients with delirium.
If medication/metabolic/endocrine/pain effect/sleep deprivation are felt to be unlikely etiologies OR if symptoms
persist for >24-48 hours despite efforts to correct what’s felt to be underlying cause:
1) Brain Imaging (MRI preferred)
2) Lumbar puncture
Standard: cell count, protein, glucose, cytology, gram stain, bacterial/fungal cultures, HHV-6 PCR (viremia
should not be assumed to be a marker for HHV-6 detection in the CSF), additional CSF saved for future
studies
Additional testing for malignancy of infection (see table below) may be considered as clinically indicated:
3) Consider ID consult for evaluation of infectious etiologies of delirium
4) Consider Neurology consult for evaluation of neurological etiologies of delirium
5) Consider psychiatry consult for evaluation and treatment of delirium
Depending on the clinical scenario, the following additional tests for infectious etiologies
may be considered:

116
Pathogen
Relative
Frequency
Clinical Setting
Recommended Initial Evaluation
Viruses
HHV-6
Frequent
• Early after transplant
• Temporal lobe contrast-enhancing lesions
• Memory loss characterizing delirium
CSF: HHV-6 PCR
HSV
Occasional
• Temporal lobe contrast-enhancing lesions
• Seropositive and not on ACV/GCV
CSF: HSV PCR
VZV
Occasional
• Seropositive or following significant
exposure and not on ACV/GCV
CSF: VZV PCR
CMV
Rare
• Donor or recipient seropositive and late
after transplant
CSF: CMV PCR
EBV
Occasional
• T-cell depleted, including CD 34+
selected
• Receipt of anti-T cell antibodies
CSF: EBV PCR
Enterovirus
Occasional
• Child
• Summer/fall
CSF: Enterovirus PCR
West Nile Virus*
Occasional
• Donor is from endemic state
• Significant mosquito exposure
• Neuromuscular weakness as component
of meningoencephalitis
CSF: WNV PCR (low sensitivity),
IgM (MAC-ELISA)
Serum: IgM (MAC-ELISA)
Contact Public Health
JC virus
Rare
• Brain imaging: non-enhancing white
matter lesions
• other work-up negative
CSF: JCV PCR
Brain biopsy
Zika virus
Very Rare
• Donor or Recipient from endemic area
ID Consult
Parasites
Toxoplasma
Occasional
• Ring-enhancing lesions
• Seropositive pretransplant and not on
prophylaxis – TMP/SMX, dapsone, etc.
CSF: PCR (low sensitivity)
Plasma: PCR
Fungi
Aspergillus and other
molds
Frequent
• Enhancing brain lesion (s) consistent with
abscess
• Concurrent pulmonary lesions (nodules)
• High degree of immunosuppression, or
neutropenia
CSF: PCR and galactomannan
(unknown sensitivity/specificity),
fungal culture
Plasma: galactomannan
Cryptococcus
Rare
• High degree of immunosuppression, or
neutropenia
• +/- enhancing meningitis or nodule or
hydrocephalus
CSF: cryptococcal antigen, fungal
culture
Serum: cryptococcal antigen
Bacteria
Usual bacterial
pathogens: S.
pneumoniae,
Listeria, GNR,
Nocardia, etc.
Frequent
• Meningitis
• Enhancing brain lesion (s) consistent with
abscess
No additional testing
recommended as these pathogens
should be identified by standard
bacterial culture.
Syphilis
Rare
• Positive pre-transplant serology
• Significant exposure
CSF: VDRL, FTA, or TPPA; IgM
immunoblotting: intrathecal T.
pallium antibody (ITPA) index,
PCR,
Tuberculosis**
Rare
• Meningitis (basilar or diffuse) or ring-
enhancing lesion(s)
• Recipient from endemic area
• Positive PPD pretransplant
• Significant exposure
CSF: AFB stain and culture, PCR
(both, low sensitivity)
* If concerned about other arboviruses, please discuss with Infectious Diseases.
** If concerned about non-tuberculous mycobacteria, please discuss with Infectious Diseases.

117
If the appropriate test is not locally available, arrangements should be made to send the
specimen to another laboratory. Please contact the LTFU office (see Appendix A)
Some children, especially those given cranial irradiation before the transplant, may have
learning disabilities (particularly in mathematics and abstract thinking). These
abnormalities typically begin to appear 24-42 months after the transplant. When
recognized as a problem, refer for psychological testing. Special educational instruction
should be considered for these children. Short-term memory deficit can occur in adults,
and psychometric testing should be performed as clinically indicated.
Total body irradiation can delay the onset of developmental landmarks in very young
children. These effects are most severe throughout the first year after transplant, and
affected children benefit from occupational therapy to assist their normal development.
After they have achieved appropriate developmental landmarks, further development
appears to proceed normally. IQ and ability to succeed in school do not appear to be
affected by total body irradiation.
G. Bone Complications (see Section XI)
Osteoporosis, fractures and avascular necrosis (AVN) are common complications after
transplantation. Long-term treatment with corticosteroids is the primary risk factor for
these complications, while gonadal failure, electrolyte imbalances, physical inactivity and
treatment with cyclosporine play an additional contributory role. Approximately 50% of
patients receiving long-term corticosteroid therapy will eventually develop bone
fractures. Increased osteoclast-mediated bone resorption and decreased osteoblast-
mediated bone formation cause trabecular bone loss. In HCT recipients, evaluation for
bone loss and osteoporosis includes a careful assessment of risk factors
(www.shef.ac.uk/FRAX/) and exposures in addition to BMD measurement. Bone loss
can be minimized by decreasing glucocorticoid dose, optimizing calcium and vitamin D
intake, participating in weight-bearing exercise, using bone strengthening drugs, and if
clinically indicated by hormonal replacement therapy. Section XI provides detailed
guidelines for preventing and monitoring osteoporosis in patients. Section XX describes
vitamins and other minerals requirements. Section XXI outlines diet for patients treated
with corticosteroids. Section XI outlines hormone replacement therapy.
H. Chronic Pulmonary Complications
Some reports have shown that the FEV
1
/FVC is less than 70% in 15% of patients by one
year after the transplant and in 30% of patients by three years after an allogeneic
transplant. Among patients with chronic GVHD, 5-10% will develop severe obstructive
airway disease that resembles obliterative bronchiolitis.
Monitoring of lung function after day +100 after allogeneic transplant.
Pulmonary function test (PFT) monitoring including: spirometry, lung volumes, and DLCO.
PFTs for asymptomatic allo-HCT recipients:
a. At 6 months
b. At 1 year
c. Yearly thereafter until 5 years as clinically indicated
d. At diagnosis of chronic GVHD
118
i. Full PFT testing including: spirometry, lung volumes, and DLCO
ii. Q3 months after diagnosis of chronic GVHD for at least one year.
(spirometry alone may be adequate)
iii. Thereafter, at Q6 months for 1 year (spirometry alone may be
adequate)
iv. With at least yearly full PFT testing including: spirometry, lung
volumes, and DLCO until year 5 post HCT.
(Section X B). If new abnormalities are noted in PFTs please contact the LTFU office to
discuss further recommendations (Appendix A).
Children who received total body irradiation are at risk of delayed onset pulmonary
restrictive disease 5-20 years after the transplant. All patients who were in the pediatric
age group at the time of transplant should have annual pulmonary function tests.
I. Hepatobiliary Complications
(see References, section XXV, Liver)
Elevations of serum ALT, alkaline phosphatase or bilirubin may occur after day 100, even
in patients who had no indication of liver problems earlier. The presentations fall into
four clinical categories.
• Acute hepatitis. Elevations of serum ALT after day 100 are most commonly
caused by drug-induced liver injury (an azole antifungal or trimethoprim-
sulfamethoxazole are the most common causes of Drug Induced Liver Injury (DILI)
in this setting), chronic GVHD, an exacerbation of hepatitis B or C, or a herpesvirus
hepatitis (VZV, HSV).
Four clinical situations demand immediate diagnosis and treatment.
1) Rapidly rising ALT accompanied by anorexia, abdominal distension or pain in
the abdomen or back can be signs of visceral VZV infection (Section VIII B).
2) Patients who have indications of hepatitis B before transplant (HBsAg-positive
or anti-HBc-positive) or who had a donor who was infected with hepatitis B are
at risk of fulminant hepatitis B after the transplant if they did not receive
antiviral prophylaxis.
3) Chronic GHVD can present as an acute hepatitis, usually after tapering or
discontinuation of immunosuppressive medications, particularly cyclosporine or
tacrolimus, or after DLI.
4) In Hepatitis C infected patients, a diagnosis of fulminant immune-rebound
hepatitis should be considered, especially if patient is tapering
immunosuppression, and, if clinically indicated, treatment with Direct Acting
Antiviral (DAA) drugs.
Patients with a rapidly rising ALT and those with ALT values >500 u/L should be
given IV acyclovir until VZV hepatitis is ruled out. An urgent PCR for VZV DNA
in serum is needed to establish the diagnosis. Contact the LTFU office (Appendix
A) for guidance in difficult cases.
119
• Chronic hepatitis. Chronic fluctuations in serum ALT levels without a discrete
episode of acute hepatitis may represent DILI, hepatitis B or C virus infection
(Section XVII), iron overload (Section XVIII) or cGVHD (Section X).
• Jaundice or signs of cholestasis. Elevated serum bilirubin and elevated alkaline
phosphatase can be caused by chronic GVHD (Section X), drug-induced
cholestasis, acute hepatitis (see above), or biliary obstruction. An ultrasound should
be obtained to evaluate whether the common bile duct is dilated. Liver biopsy
might not be needed in patients who have cholestasis with biopsy-documented
chronic GVHD in other organs. Some patients have liver involvement as the
dominant manifestation of chronic GVHD, and liver biopsy might be needed in
order to establish the diagnosis when other manifestations of chronic GVHD are
absent.
• Hepatomegaly or right upper quadrant pain. The sudden onset of
hepatomegaly suggests acute hepatitis, Epstein-Barr virus-induced
lymphoproliferative disorder involving the liver, or rarely, Budd-Chiari syndrome.
More indolent hepatomegaly can occur with metastatic tumor, leukemia infiltration
or rarely, constrictive pericarditis or mycobacterial infection. Right upper quadrant
pain can be caused by acute cholecystitis, biliary obstruction with cholangitis,
biliary sludge syndrome, or rarely, fungal liver abscess. Liver imaging with helical
CT X-ray or ultrasound is needed to resolve the diagnosis.
Suggestions for liver biopsy and handling of liver tissue. The technique of liver
biopsy depends on the clinical situation (diffuse process vs. focal lesion) and the platelet
count. A percutaneous biopsy is preferred if platelet counts are >100,000/mm
3
and the
risk of bleeding is small (including normal PT/PTT) but transvenous biopsy through
either the femoral or jugular route is satisfactory for diagnosis of any diffuse hepatitis or
GVHD. Tissue should be cultured for viruses and fungi and should be fixed in freshly-
prepared neutral buffered formalin.
J. Gastrointestinal Complications:
GVHD is the most common cause of anorexia, nausea, vomiting and diarrhea after an
allogeneic transplant. However, each of these symptoms has a narrow differential
diagnosis that requires careful evaluation before concluding that GVHD is the sole cause.
Anorexia, nausea and vomiting can be caused by HSV, VZV, and CMV infections and by
certain medications such as trimethoprim-sulfamethoxazole, voriconazole, itraconazole,
mycophenolate mofetil, cyclosporine or tacrolimus. Abdominal pain can be caused by
visceral VZV infection, biliary sludge syndrome, acute cholecystitis, or rarely, Epstein-
Barr virus-induced lymphoproliferative disease. Diarrhea occurring more than 3 months
after transplant is commonly caused by magnesium – containing medications, unresolved
GVHD, or less commonly by an infection (giardiasis, cryptosporidiosis, C. difficile, or
CMV). Section VII provides guidelines for evaluation of diarrhea and endoscopy.
120
XVII. BLOOD PRODUCT TRANSFUSIONS
All blood products should be irradiated to prevent transfusion related Graft Versus Host Disease
(GVHD), with the exception of pathogen reduced blood products that do not need to be
irradiated. Red blood cells and platelets should also be leukocyte reduced to prevent HLA
alloimmunization and reduce the risk of CMV transmission. Leukocyte reduced blood
components are accepted as “CMV safe” for CMV seronegative patients. Granulocytes are
never leukoreduced.
If the donor and recipient had ABO blood group incompatibility, low-grade hemolysis can
delay erythroid recovery for many months after the transplant. Hemagglutinin titers and
reticulocyte counts should be followed to monitor the change from recipient to donor ABO
type. Type O red cells should be used for patients who have isoagglutinins against donor red
blood cell antigens until the donor blood group type is fully established in the recipient.
Treatment with erythropoietin can be beneficial in some patients. Donor-type platelets
should be used for transfusions.
121
XVIII. VIRAL HEPATITIS in long term transplant survivors
(see References, section XXV, Liver)
Compared to hepatitis C, hepatitis B is more likely to result in severe clinical hepatitis and
death from post-transplant liver disease, although these outcomes occur only in the minority
of HBV-infected patients. One exception: patients infected by HCV who are receiving
MMF for GVHD prophylaxis may develop a more severe, potentially fatal form of liver
disease called fibrosing cholestatic hepatitis C. In this setting, it should be assessed whether
MMF may be discontinued. Antiviral treatment should be considered for HBV-and HCV-
infected transplant recipients unless contraindications are present. Liver test abnormalities
post-transplant may be caused by hepatic GVHD, HBV, HCV, a herpes virus infection
(VZV, CMV, HSV), adenovirus, or drug-induced injury (Sections I, X and XV). In this
situation, liver biopsy should be performed to determine the dominant pathologic process.
A. Hepatitis B
Even in patients with very low levels of viral replication before transplantation and relatively
normal liver function and histology, impaired cellular immunity can permit reactivation of
HBV. Serological patterns of HBV infection may be atypical in transplant survivors, likely
as a consequence of immunosuppression. Patients with HBV requiring systemic
immunosuppressive medications for control of chronic GVHD remain at risk for acute
exacerbation of hepatitis whenever immunosuppression is tapered or ceased. Such flares
may result in hepatic failure and death. Cirrhosis due to chronic HBV has not emerged as a
major problem after transplantation.
The risk of fatal HBV liver disease among patients who are persistently HBsAg-positive
after transplant and who are not receiving entecavir is approximately 12%. In hematopoietic
cell transplant recipients who are anti-HBc and anti-HBs-positive, but HBsAg-negative,
reactivation of latent infection can occur and may lead to fulminant hepatic failure,
particularly if nucleotide substitutions in the precore region of the genome interfere with
production of HBcAg. Because these patients remain HBcAg-negative despite high levels of
viral replication, monitoring of HBV DNA levels is necessary in these HBsAg-positive
patients.
Posttransplant HBV infection may result from
• Active HBV infection before transplant
• Reactivation of latent HBV infection
• New infection during the transplantation process
o Infected hematopoietic cell product from an infected donor
o Infected blood products (risk estimated in U.S. to be 1 in 500, 000 units).
1) Monitoring of Patients at Risk for HBV Infection
• For allogeneic transplant patients who had a donor who was either HBsAg or
antiHepB core positive:
Serum ALT and HBV DNA monthly to six months post transplant or 6 months
after stopping entecavir (whichever is longer).
122
• For allogeneic transplant patients where patient is HBsAg positive and on entecavir:
Monitor HBV DNA and serum ALT monthly until 6 months after stopping
entecavir. If increased Serum ALT consider testing for viral resistance and
switching to TAF if checked HBV DNA increased >1.0 log above nadir.
• For allogeneic transplant patients where patient is antiHepB core positive:
Serum ALT and HBV DNA monthly until 6 months after stopping entecavir.
• For autologous transplant patients who is either HBsAg or antiHepB core positive:
o Monitor HBV DNA and Serum ALT monthly until 6 months after stopping
entecavir. If HBV DNA increases > 1.0 log above nadir. Consider testing for
viral resistance and switching if medically indicated to TAF.
2) Treatment
For patients at risk for HBV infection after transplant who are NOT receiving antiviral
prophylaxis, we recommend initiation of antiviral treatment with entecavir when HBV
DNA is first detected after transplant. For patients already on entecavir and not
appropriately responding, consider alternative antiviral therapy. The aim of antiviral
treatment is to suppress viral replication completely, thereby minimizing the risk of viral
mutation. Patients should be treated for 12 months or 6 months after discontinuation of
systemic immunosuppressive treatment, whichever is longer.
3) Other considerations
-Clearance of antigenemia is commonly observed and is particularly likely if the
hematopoietic cell donor was anti-HBs-positive.
- Based on CDC guidelines, vaccination with HAV is considered particularly important
and is strongly recommended for any patient with evidence of infection with HBV to
prevent the development of fulminant liver failure secondary to hepatitis A infection.
(See section IX Vaccinations)
B. Hepatitis C
Infection with HCV virus is more frequent in patients who received blood product transfusions
before 1991 when HCV testing was unavailable than with transfusions given after 1991. The
prevalence of chronic hepatitis C in long-term HCT survivors ranges from 5% to 70%,
depending on the endemic prevalence. Long-term survivors with HCV infection commonly
have fluctuating levels of AST and ALT. During the first 10 years after infection, hepatitis C
has little impact in morbidity or mortality—with the exception possibly of HCV-infected
patients who are receiving MMF. The frequency of cirrhosis and end-stage liver disease caused
by Hepatitis C in 40-year survivors of hematopoietic cell transplant is about 33%.
Regardless of whether HCV infection occurred before or after the transplant, clinical or
biochemical evidence of hepatitis usually coincides with the return of cellular immunity and
the tapering of immunosuppressive drugs used for GVHD prophylaxis. During this time, it

123
is difficult to differentiate the hepatitic variant of GVHD of the liver from an exacerbation
of HCV. The presence of hepatitis C viremia, even in high titer, is insufficient to make the
distinction between these two disorders. The absence of hepatitis C viremia, however,
means that HCV is not a cause of ALT elevations. Unless there is evidence of active GVHD
in other organs, a liver biopsy may be required before a therapeutic decision is made.
Pathologic distinction between hepatitis C and GVHD may be difficult, since both processes
may be associated with portal lymphoid infiltration and bile duct injury. Marked bile duct
injury with epithelial cell dropout and loss of interlobular bile ducts is more typical of
GVHD. A flare of hepatitis C and hepatic GVHD may occur simultaneously. If the liver
biopsy suggests both processes, immunosuppressive therapy should be administered, since
ongoing lymphocytic attack leading to loss of interlobular bile ducts may result in severe
and progressive cholestasis.
Fulminant immune-rebound hepatitis C has been reported only rarely after withdrawal of
immunosuppression. Patients infected by HCV who are receiving MMF may be at risk to
develop fatal fibrosing cholestatic hepatitis C. After the initial flare of hepatitis during
immune reconstitution, the serum ALT levels may again return to normal, but laboratory
abnormalities often settle into the pattern of chronic hepatitis seen in other patients with
HCV infection.
Monitoring:
• Liver function tests at least weekly to day 100, then bimonthly until 1 year
• HCV RNA should be checked around day 50 post transplant in those rare patients who
were HCV antibody positive but HCV RNA negative pretransplant or whose donor was
HCV RNA positive.
• Patients known to have HCV should be referred to a hepatologist to assess three major
issues: 1) Has the virus infection caused any damage to the liver yet? 2) Are there other
causes of liver damage (i.e., alcohol, medications, chronic GVHD, hemosiderosis or the
hepatitis B virus? 3) Should medications for HCV be instituted?
• All HCV-infected long-term HCT survivors should be evaluated for progression of liver
disease every 6 to 12 months with a hepatic function panel, complete blood count, and
evaluation of prothrombin time/international normalized ratio. If fibrosis is suspected in
long-term HCT survivors, noninvasive tests such as serologic panels and transient
elastography can be used to evaluate for the presence of advanced fibrosis (Scoring System
for Histological Stage Metavir score > F3) and cirrhosis (Metavir score F4).
• For HCV-infected HCT long-term survivors with advanced fibrosis (Metavir score > F3),
surveillance for hepatocellular carcinoma with ultrasonography every 6 months is
recommended. For patients with cirrhosis, endoscopic surveillance for esophageal varices is
recommended.
124
Therapy
Direct-acting anti-viral therapy for chronic HCV infection should be considered after the
patient has discontinued all immunosuppressive drugs, and has no evidence of active
GVHD. Be aware of possible drug-drug interactions (see References, section XXV,
Liver).`
In patients with concomitant iron overload, phlebotomy or chelation therapy may be
indicated to reduce hepatic iron stores (Section XVIII) before Direct Acting Antiviral
(DAA) therapies. The mobilization of iron after transplant largely depends on the iron
burden, especially cardiac iron. A review of this topic has been published. (see
References, section XXV, Liver)
In all HCT survivors with active HCV infection, cofactors that can lead to fibrosis should be
addressed. Patients should be counseled to avoid excessive weight gain, ethanol and
medications or herbal supplements that are hepatotoxic, as well as on treatment of other
causes of liver disease (nonalcoholic fatty liver disease, hepatitis B virus, HIV, and
extrahepatic obstruction), and mobilization of excess iron.
HCT recipients who develop end-stage liver disease can be considered for liver transplant;
in rare cases, a living donor liver transplant from the original hematopoietic cell donor may
be feasible.
Other Considerations:
- Based on CDC guidelines, vaccination against HAV and HBV are considered
particularly important and are strongly recommended for any patient with evidence of
infection with HCV to prevent the development of fulminant liver failure secondary to
infection with other hepatitis viruses.
(See section IX Vaccinations)

125
XIX IRON OVERLOAD
A. Summary of evidence
1. Epidemiology
Iron overload occurs frequently in hematopoietic cell transplantation (HCT) patients, often
caused by red cell transfusions prior and during HCT, in addition to ineffective
erythropoiesis with associated intestinal hyperabsorption, and, in some patients, underlying
genetic hemochromatosis. Elevated ferritin estimates 32-58% of HCT survivors may be
overloaded with iron [1, 2, 3]. One autopsy study found 40% of patients with significantly
high liver iron content (LIC) above 5.6mg/g [4]. A cross-sectional study showed 31/56 HCT
recipients had elevated ferritin, and 50% of those with high ferritin had significant liver
siderosis with LIC>6.5mg/g [1].
2. Natural history of iron overload in HCT and its consequences
Once transplant has restored normal hematopoiesis and red cell transfusions are no longer
required, body iron stores decline over several years [5]. Elevated liver iron content (LIC)
defined as >1.8mg/g by T2- magnetic resonance imaging (MRI) was not associated with
survival or complications in adult patients at 1 year post-HCT [6]. High LIC (above 7mg/g)
as determined by magnetic resonance in patients post HCT for myelodysplastic syndromes
or acute myeloid leukemia was a significant risk factor for non-relapse mortality
(particularly in older patients undergoing reduced intensity conditioning), and ferritin above
1,000ng/mL has been associated with decreased survival. [7;8, 9]. Extreme tissue iron
overload (> 15 mg/g dry weight) has been associated with extensive organ toxicity in the
post-transplant survivors of thalassemia, in whom organs at risk include the heart, liver,
pancreas and pituitary gland, resulting in dysrhythmias and cardiac failure, portal fibrosis
and cirrhosis, insulin-dependent diabetes mellitus and other endocrine insufficiencies. Iron
overload increases the susceptibility to mucormycosis, aspergillosis, and infections caused
by Listeria monocytogenes, non-cholera Vibrio species, Yersinia enterocolitica and Yersinia
pseudotubera, among others [2, 4]. In patients with chronic hepatitis C, iron overload may
accelerate the development of cirrhosis.
3. Assessment of iron overload post-HCT
Although ferritin measurement is recommended as part of long-term follow-up post-HCT, it
also changes with inflammation and cell injury. Assessment of body iron by MRI is non-
invasive and has been calibrated with liver biopsies and ex vivo heart tissue iron
measurements, allowing accurate and more frequent assessment of iron overload than liver
biopsy [10]. Liver or marrow iron content correlates poorly with number of transfused red
blood cell units. Marrow and liver iron contents have been determined by spectrophotometry
among 10 consecutive autopsied patients who were transplanted for hematological
malignancy. The median liver iron content (LIC) at 50 to 100 days post-transplant was 4.307
mg/g dry weight (range 1.832-13.120; normal 0.530-0.900) and the median marrow iron
content was 1.999 mg/g dry weight (range 0.932-3.942). Marrow iron content can also be
measured by morphometry based on digital photomicrographs of a Prussian blue-stained
marrow biopsy. Because of correlation between morphometric and spectrophotometric
analyses of marrow iron content (r = 0.8, P= 0.006) and hepatic iron index (r = 0.82, P =

126
0.004) morphometric analysis of marrow iron content is an acceptable alternative for
quantifying tissue iron stores [11]. Earlier work also demonstrated a close relationship
between biochemical concentration and histologic grading of marrow iron [12] although
histological grading is subject to variation between and within observers [13]. Because the
carrier frequency for homozygous High Fe (HFE) gene mutations is relatively high (0.3 to
0.5%) among individuals of Northern and Western European ancestry, the possibility of
hereditary hemochromatosis (HH) contributing to post-transplant iron overload needs to be
considered in relevant individuals. Two point mutations, C282Y (Cys282Tyr) and H63D
(His63Asp), are the most frequently found within the HFE gene. Homozygosity for C282Y
is associated with hemochromatosis with variable penetrance; the effect of compound
heterozygosity (C282Y/H63D) on iron status in HCT recipients is variable.
4. Management of iron overload post-HCT
Mobilization of iron in heavily overloaded patients improves cardiac function, normalizes
serum alanine aminotransferase (ALT) levels, and results in improved liver histology
[14;15]. Phlebotomies were well-tolerated by 14/16 patients, and they reached the target
ferritin below 500ng/mL after a median of 16.5 phlebotomies in a median of 287 days [3].
Ferritin levels decreased significantly in 49/55 (80%) of patients after a median of 9
phlebotomies in another study [16]. One study showed that recipients of marrows from
donors with mutated HFE had lower reduction in ferritin levels per phlebotomy than those
who received marrow from wild-type donors [16]. A retrospective study found that
deferoxamine use post-HCT in 37 patients was associated with lower ferritin and lower
relapse incidence [17]. Oral chelation with 20-30mg/kg/day of deferasirox has been
evaluated retrospectively and showed a possible association with longer survival after HCT
[18], and a prospective, phase IV, open-label trial showed 10mg/kg/day of deferasirox
provided a significant reduction in serum ferritin and liver iron concentration over one year
of treatment with mild to moderate adverse events [19].
B. Evaluation of Iron Overload after HCT for autologous and allogeneic patients
1. Timepoints of evaluation:
a. at 80-100 days post HCT;
b. 1 year post HCT;
c. at least yearly if still receiving red blood cell transfusions.
2. Laboratory testing:
a. Iron studies (ferritin, iron, total iron-binding capacity [TIBC], and transferrin
saturation [TS])
Biochemical lab tests are non-specific and can be significantly affected by inflammation,
infection (which falsely elevate ferritin and decrease iron, TIBC and TS) and graft versus
host disease (GVHD) (which increases iron absorption), so biochemical tests should NOT
be used as sole criteria to consider the presence of iron overload and should be confirmed
by MRI-T2*.

127
b. HFE genotype
Consider for patients with:
i. family member with diagnosed hereditary hemochromatosis (HH)
ii. TS > 45% AND Northern or Western European ethnicity.
Genetic analysis for other rare mutations described in association with hemochromatotic
phenotypes such as in HAMP (hepcidin), SLC40A1 (ferroportin), HJV (hemojuvelin),
TFR2 (transferrin receptor 2) genes is recommended on a case-by-case basis.
3. Assessment of Tissue Iron
a. Magnetic resonance - MRI-T2*
All patients should undergo T2*-weighted magnetic resonance imaging test (MRI-T2*) if
there are concerns about iron overload. MRI-T2* is highly accurate in measuring tissue
iron in heart, liver, spleen, and pancreas. Recommend first getting MRI of abdomen for
assessing liver, spleen, and pancreas. If abnormal uptake in pancreas or other high-risk
factors see below, get cardiac MRI.
Cardiac MRI are indicated for patients with the following high-risk factors:
1.Lifetime history of receiving 75 RBC units or more;
2.Thalassemia;
3.Sickle cell disease ;
4.Other congenital anemias (Diamond-Blackfan; hereditary sideroblastic);
5.Associated hereditary hemochromatosis (HH)
b. Endocrine screen: Patients that fulfill criteria for iron overload (LIC>2mg/g),
particularly those with detectable cardiac iron (T2*<20ms) in adult patients, or
below 1 standard deviation or age based references in pediatric patients, may
benefit from earlier screening for endocrine gland abnormalities secondary to iron
overload with fasting glucose, thyroid stimulating hormone (TSH), free thyroxine
(T4), parathyroid hormone (PTH), follicle stimulating hormone (FSH), and
luteinizing hormone (LH).
c. Transient elastography: This is the preferred method if assessment of liver
fibrosis and cirrhosis is a concern, particularly in thrombocytopenic patients for
whom a liver biopsy poses significant risk of bleeding.
d. Liver biopsy: Given the risks of the procedure, risk of sampling variability, and
indolent course of hepatic siderosis, measurement of hepatic iron by
spectrophotometry of liver biopsy should be an exception to be discussed case-by-
case, e.g. in patients with absolute contraindications to MRI.
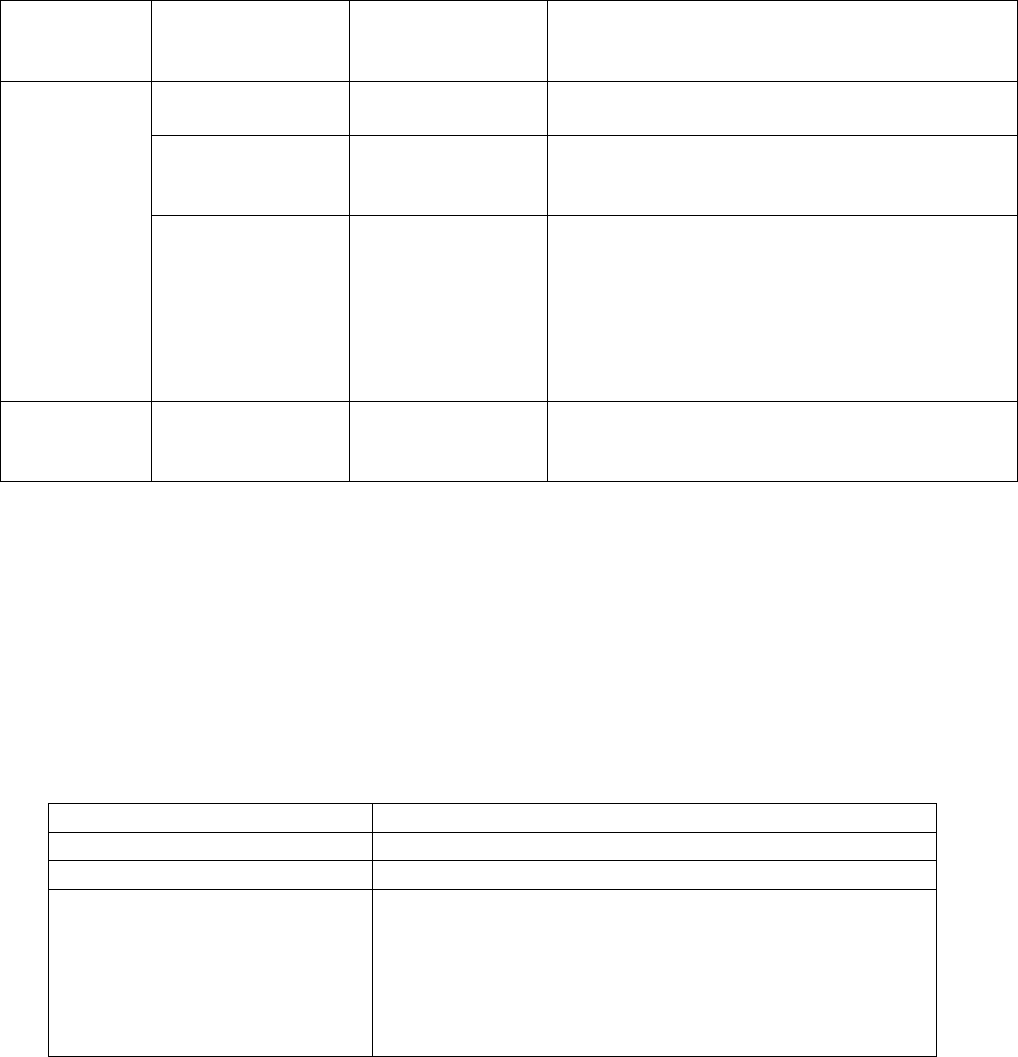
128
4. Indication for Iron Mobilization Therapy According to Tissue Iron Content
Cardiac T2*
(ms)
LIC
(mg/g dry weight)
Marrow Iron
Content
Mobilization of Iron
>20ms*
(normal)
>15
Very high
++++
Phlebotomy ± single iron chelator
7 – 15
Moderately high
++ to +++
1
st
choice: Phlebotomy
2
nd
choice: Single iron chelator (especially if
HCV-positive)
2-7
Mildly increased
+
1) HFE
wildtype
:
observe
2) HFE
C282Y/C282Y or C282Y/H63D
:
Phlebotomy aiming at ferritin level <100
3) Hemoglobinopathies and other congenital
anemia disorders
Phlebotomy aiming at ferritin level <500
<20ms*
Any
Any
Phlebotomy + combination iron chelation;
consider admission if symptomatic or T2*<8ms;
consider erythrocytapheresis for faster removal
*For pediatric patients: Use age-based reference ranges for cardiac T2* values. Abnormal
cardiac iron content is defined as below 1 standard deviation for age-based reference
values
C. Phlebotomy for iron overload after HCT
• If indicated, phlebotomy is likely to be the safest and most cost-effective approach for the
mobilization of tissue iron.
• Regular phlebotomy requires adequate venous access, normal hematopoiesis or
hematopoiesis that can respond satisfactorily to weekly or every-other-week
erythropoietic stimulating agents (ESAs).
• Phlebotomy Regimen:
Phlebotomy volume
5 mL/kg as tolerated
Frequency
every 3-4 weeks as tolerated
Monitoring monthly
CBC, ferritin, iron, TIBC, and TS
Discontinue Phlebotomy
Symptomatic anemia with hematocrit below 35%, or
MRI-T2* LIC below 7mg/g (non-HH patients), or
ferritin below 500ng/mL (non-HH patients and patients
with hemoglobinopathies/other congenital anemias), or
ferritin below 100ng/mL (hereditary hemochromatosis
(HH) patients)

129
• Erythropoietic Stimulating Agents (ESAs) may be administered subcutaneously to
facilitate regular phlebotomy. The smallest number of whole vials should be prescribed
per dose:
Body Weight
(kg)
Erythropoietin
1
(Units weekly)
Darbepoetin
2
(micrograms every-other-week)
10-14
6,000 to 8,000
25 to 60
15-20
10,000
60
21-24
10,000 to 14,000
60 to 100
25-29
14,000
100
30-39
20,000
100
40-60
40,000
200
>60
Use darbepoetin
200
1
Erythropoetin (Epogen) vial sizes (2,000; 4,000; 10,000; 20,000; 40,000 units)
2
Darbepoetin (Aranesp) vial sizes (25; 60; 100; 150; 200; 300 micrograms)
• Erythrocytapheresis is a grade 1B recommendation for iron overload in hereditary
hemochromatosis (HH). It has been compared with phlebotomies in two randomized
studies with hereditary hemochromatosis (HH) patients, with faster removal of iron, no
differences in adverse events, and controversial differences in cost [20,21].
Note: Though patients with GVHD continue to hyperabsorb iron from dietary sources and
may be an exception to the normal situation when patients mobilize their excessive iron
stores when effective erythropoiesis returns after HCT.
D. Chelation therapy for iron overload after HCT
If phlebotomy or erythrocytapheresis cannot be performed despite the use of ESAs within
3 - 6 months after transplantation, and if treatment to mobilize iron stores is indicated
(see item 4 above), iron chelation therapy with single agents desferoxamine (DFO) -
Desferal or deferasirox (DFX) - Exjade or Jadenu - should be initiated. Patients with
evidence of cardiac iron overload should undergo combination therapy (DFO and
deferiprone – DFP, Ferriprox).
1. Deferoxamine (DFO) - Desferal
1.1. Administration:
DFO can be administered by continuous subcutaneous or intravenous infusion with less
toxicity if administered subcutaneously.
1.2. Toxicity:
Ocular and auditory abnormalities, sensorimotor neurotoxicity, renal insufficiency,
pulmonary toxicity, and failure of linear growth. In rare cases, treatment with DFO has
enhanced susceptibility to certain microorganisms, such as Vibrio vulnificus, Yersinia
enterocolitica and Yersinia pseudotubera, among others, resulting in generalized
infections by providing these agents with a siderophore otherwise missing.
1.2.1. AVOID ascorbic acid (vitamin C) (>200mg/day) in patients receiving DFO due to
possible impact on left ventricular function. DO NOT administer ascorbic acid with
DFO in patients with heart failure.

130
1.2.2. Toxicity can be avoided by regular assessment of the body iron stores with annual
MRI-T2*. In general, assessment of body iron stores should also follow when
deferoxamine toxicity occurs.
1.3. Dosing:
20 to 40 mg/kg/day, administered 5-7 days per week by continuous overnight infusion,
typically for 8-12 hours.
Dose should not exceed 50 mg/kg/day
Infusion rate should not exceed 15 mg/kg/hour to avoid hypotension.
1.4. Monitoring:
1.4.1. Prior to starting treatment: obtain baseline CBC, creatinine, ferritin, liver function
tests, audiogram, and eye examinations.
1.4.2. Monthly complete blood count (CBC), ferritin, creatinine, and liver function tests.
1.4.3. Therapeutic index: Most of the toxicity caused by deferoxamine occurs when the
dose exceeds 50 mg/kg/day or when the iron burden is not high. Dose reductions
can be done by aiming at a therapeutic index below 0.025. Therapeutic index is
calculated by: (number of days per week X daily dose in mg/kg) / (7 X serum
ferritin in ng/mL) [22].
1.4.4. Discontinue for six months if LIC <3 mg/g dry weight, or marrow iron content is
not increased or only mildly increased. Thereafter, the dose of DFO should be
adjusted to maintain liver iron content between 3 and 7 mg/g dry weight and
therapeutic index below 0.025.
Suggested monitoring of DFO-related toxicity is shown below.
Toxicity
Tests
Frequency
Alteration In Rx
High frequency
sensorineural hearing
loss
Audiogram
Annually; if
symptomatic, check
immediately
Stop DFO;
repeat audiogram at 3
month intervals until
normal or stable
Retinopathy (pigmentary
degeneration); cataracts;
corneal opacities; visual
impairment
Eye exam
including visual
acuity, slit-lamp
and fundoscopy
Annually; if
symptomatic, check
immediately
Stop desferoxamine if
retinopathy or hearing
impairment
Metaphyseal/Spinal
Plain x-ray of
wrists, knees,
spine; bone age in
children
Annually
Reduce deferoxamine to
20-25 mg/kg/day
Growth retardation
Sitting and
standing height
Every 6 months
Reduce deferoxamine
to 20-25 mg/kg/day;
reassess every 6 months
2. Deferasirox (DFX) - Exjade, Jadenu, or Jadenu Sprinkles
2.1. Contraindications:
a) Serum creatinine greater than two times the age-appropriate upper limit of normal or
creatinine clearance less than 40 mL/min;
b) Poor performance status;

131
c) High-risk myelodysplastic syndromes;
d) Advanced malignancies;
e) Platelet counts less than 50,000;
f) Known hypersensitivity to DFX or any component of the medication.
2.2. Toxicity:
Gastrointestinal (GI) symptoms (diarrhea, vomiting, nausea, abdominal pain),
headaches, pyrexia, skin rash, increases in serum creatinine, intermittent proteinuria,
cytopenias (including agranulocytosis, neutropenia, and thrombocytopenia), hepatic
dysfunction, auditory disturbances, and ophthalmic disturbances. Post marketing
surveillance has shown cases of acute renal failure or cytopenias with fatal outcomes in
patients taking DFX. The relation to DFX in these cases is uncertain.
2.3. Dosing: see below, items 2.6 and 2.7.
2.4. Monitoring:
2.4.1. Prior to starting treatment: obtain baseline CBC, creatinine with clearance
estimation in duplicate, ferritin, liver function tests, audiogram, and eye
examinations.
2.4.2. Monthly CBC, ferritin, creatinine, urine protein levels, and liver function tests.
2.4.3. Discontinue temporarily if ferritin level falls below 500ng/mL.
Suggested monitoring of DFX-related toxicity is shown below.
Toxicity
Tests
Frequency
Alteration In Rx
High frequency
sensorineural hearing
loss
Audiogram
Annually; if
symptomatic, check
immediately
Stop DFX;
repeat audiogram at 3
month intervals until
normal or stable
Retinopathy (pigmentary
degeneration); cataracts;
corneal opacities; visual
impairment
Eye exam
including visual
acuity, slit-lamp
and fundoscopy
Annually; if
symptomatic, check
immediately
Stop DFX if retinopathy
or hearing impairment
Renal impairment
Creatinine and
protein/creatinine
ratio
Creatinine weekly
for the first month,
then monthly;
Protein/creatinine
ratio every 3 months
See dose modification
below (items 2.5.4 and
2.6.4)
2.5. Specific information about Exjade
2.5.1. Exjade is available in 125mg, 250mg, and 500mg tablets;
2.5.2. Starting dose: 20mg/kg/day.
2.5.3. Dose modification: 5-10mg/kg/day increments every 3-6 months if necessary
depending on serum ferritin trends. Doses should not exceed 40mg/kg/day.
2.5.4. Dose reduction: 50% for starting dose if creatinine clearance 40-60mL/min or
moderate (Child-Pugh B) hepatic impairment. If the serum creatinine level increases
more than 33% over the course of two consecutive visits, the dose should be
reduced by 10mg/kg. For pediatric patients, the dose should be reduced by 10mg/kg
if the serum creatinine is greater than the upper limit of normal on 2 consecutive
visits.

132
2.5.5. Administration: Exjade should be taken once daily on an empty stomach (at least
30 min prior to eating). Tablets should be completely dispersed by stirring in water,
orange juice, or apple juice until there is a fine suspension. Doses <1 gram should
be dispersed in 3.5 ounces of liquid, and doses 1 gram should be dispersed in 7
ounces of liquid. After swallowing, any residue should be resuspended in a small
volume of liquid and swallowed. Doses should be separated by 2 hours from
aluminum containing antacids.
2.6. Specific information about Jadenu and Jadenu Sprinkles
2.6.1. Jadenu is available in 90mg, 180mg, and 360mg tablets or granules (Jadenu
Sprinkles).
2.6.2. Starting dose: 14mg/kg/day.
2.6.3. Dose modification: 3.5-7mg/kg/day increments every 3-6 months if necessary
depending on serum ferritin trends. Doses should not exceed 28mg/kg/day.
2.6.4. Dose reduction: 50% for starting dose if creatinine clearance 40-60mL/min/1.73m
2
or moderate (Child-Pugh B) hepatic impairment. If the serum creatinine level
increases more than 33% over the course of two consecutive visits, the dose should
be reduced by 7mg/kg. For pediatric patients, the dose should be reduced by
7mg/kg if the serum creatinine is greater than the upper limit of normal on 2
consecutive visits.
2.6.5. Administration: Jadenu should be taken once daily preferably at the same time of
the day, on an empty stomach or with a light meal (contains less than 7% fat content
and approximately 250 calories). Examples of light meals include 1 whole wheat
English muffin, 1 packet jelly (0.5 ounces), and skim milk (8 fluid ounces) or a
turkey sandwich (2 oz. turkey on whole wheat bread w/ lettuce, tomato, and 1
packet mustard). Jadenu tablets may be crushed and mixed with soft foods (e.g.,
yogurt or apple sauce) immediately prior to use and administered orally.
Commercial crushers with serrated surfaces should be avoided for crushing a single
90 mg tablet. The dose should be immediately and completely consumed and not
stored for future use. Take Jadenu Sprinkles by sprinkling the full dose on soft food
(e.g. yogurt or apple sauce) immediately prior to use and administered orally. Doses
should be separated by 2 hours from aluminum containing antacids.
3. Combination therapy: deferoxamine – Desferal, and deferiprone (DFP) - Ferriprox
3.1. In combination therapy, deferoxamine should be prescribed as above, preferably 7
days a week; if patient is admitted, it may be placed as a 24-hour infusion.
3.2. Deferiprone is an oral medication for iron chelation, available in 500mg tablets and
100mg/mL oral solution.
3.3. Contraindications: severe hepatic impairment, creatinine clearance below
15ml/min/1.73m
2
, known hypersensitivity to deferiprone or any component of the
medication.
3.4. Toxicity: neutropenia (6.2%), agranulocytosis (1.7%), zinc deficiency, chromaturia
(reddish brown discoloration of the urine), GI symptoms (nausea, vomiting,
abdominal pain or discomfort), joint pain, headache.
3.4.1 Avoid concomitant use of drugs known to be associated with neutropenia
or agranulocytosis if possible.

133
3.5. Starting dose: 25mg/kg tid (75mg/kg/day daily). Maximum dose is 33mg/kg tid
(daily total 99mg/kg/day).
3.6. Dose reduction: not recommended for mild or moderate liver impairment, or
creatinine clearance above 15ml/min/1.73m
2
.
3.7. Administration: take first dose in the morning, second dose at midday, third dose in
the evening, with meal. Allow at least 4-hour intervals between deferiprone and
medications or supplements containing polyvalent cations, e.g. aluminum or zinc.
3.8. Monitoring:
3.8.1. Prior to starting treatment: obtain complete blood count with neutrophil count,
serum transaminases, and zinc levels.
3.8.2. Weekly neutrophil counts
3.8.3. Monthly ferritin, transaminases, and zinc.
3.8.4. Discontinue if ferritin level falls below 500ng/mL.
3.8.5. Management of neutropenia: discontinue DFP and all medications that can
cause neutropenia and follow blood counts daily until recovery. DO NOT
resume DFP in patients who develop agranulocytosis, DO NOT
rechallenge patients with neutropenia above 500 unless benefit outweighs
the risks.

134
XX. VITAMINS AND OTHER MINERAL SUPPLEMENTS
It is recommended that all allogeneic patients have iron-free multiple vitamin/mineral
supplementation for one year or until all immunosuppressive therapy is discontinued after the
transplant. Autologous patients should continue supplementation for one year if dietary
intake does not meet daily requirements. Iron supplementation should not be used routinely
in any patient unless iron deficiency is clearly documented. Most patients have iron-overload
because of red cell transfusions and increased absorption of iron in the GI tract (see Section
XIX).
A. Calcium and Vitamin D daily intake requirements
Adequate calcium and vitamin D intake are necessary in order to decrease the risk of
bone complications after transplant. Women with ovarian failure and patients who
require long-term treatment with corticosteroids have a high risk of osteoporosis, and
pediatric patients can have poor bone development after chemotherapy and radiation.
Avoidance of sunlight and the use of sunscreen to block UV radiation can contribute to
vitamin D deficiency.
Patients who cannot consume adequate calcium or vitamin D from foods should receive
supplements to meet their daily requirements. Supplemental calcium should be given in
divided doses, preferably as calcium citrate. Some "natural" calcium supplements do not
contain enough bioavailable calcium to prevent osteopenia. The maximum amount that
can be absorbed with each dose is 500 mg. See Section XI for prevention of
osteoporosis.
i. CALCIUM REQUIREMENTS FOR PATIENTS DURING STEROID THERAPY:
Calcium intake above these levels is not recommended, as it may interfere with the
absorption of other nutrients.
ii. CALCIUM REQUIREMENTS FOR PATIENTS NOT ON STEROIDS
Age
Daily Minimum
Requirement after
Transplant (milligrams)
Children 7-12 months
260
Children 1-3 years
700
Children 4-8 years
1000
Children 9-18 years
1300
Adult Males
1000-1200
Adult Females;
On hormone therapy
No hormone therapy
1000-1200
1500
7-12 months:
600 mg/day
1-3 years:
1000 mg/day
4-8 years:
1200 mg/day
> 9 years:
1500 mg/day

135
iii. Vitamin D requirement
Table 1: Vitamin D3 (or D2) Supplementation
*, ****
Adults (>18 yrs)
Children (<18 yrs)
Treatment of Insufficiency [Vitamin D (25 Hydroxy) levels 20-30 ng/mL]***
▪ Routine
▪ 25 mcg/day
▪ Age < 1 yr:
─ 10 mcg daily
(20 mcg in dark skinned)
▪ Age 1-8 yr:
─ 15 mcg daily
▪ Age 9-18 yr:
─ 20 mcg daily
▪ Malabsorption syndromes**
▪ 1,250 mcg per week
▪ Age < 1 yr:
─ Consult Endocrinology
▪ Age 1-18 yr:
─ 1,250 mcg per week or
─ 125 mcg daily
▪ Chronic Renal Disease
▪ Consult Nephrology
▪ Consult Nephrology
Treatment of Deficiency [Vitamin D (25 Hydroxy) level <20 ng/mL]***
▪ Uncomplicated
▪ 1,250 mcg per wk x 8 (Repeat
if Vitamin D (25 Hydroxy) level
< 30 ng/mL otherwise treat as
for insufficiency above)
▪ Age 1-12 months:
─ 25-50 mcg daily x 8 wks
▪ Age 1-18 yr:
─ 25-125 mcg daily x 8 wks
or
─ 1,250 mcg weekly x 8
(Repeat if Vitamin D (25
Hydroxy) level < 30 ng/mL
otherwise treat as for
insufficiency above)
▪ Malabsorption syndromes**
▪ 250-1,250 mcg daily or every
other day
▪ UVB irradiation in patients
also with skin GVHD
▪ Age < 1 yr:
─ Consult Endocrinology
▪ Age 1-18 yr:
─ 1,250 mcg per week
▪ Chronic Renal Disease
▪ Consult Nephrology
▪ Consult Nephrology
*
Currently there does not seem to be substantive benefit by choosing Vitamin D2 or vitamin D3 over the other
with regard to correcting Vitamin D (25 Hydroxy) levels. The more important decision is prescribing enough.
Dose frequency appears to be less important than cumulative amount so that 50 mcg daily for 50 days is
approximately equivalent to giving 1,250 mcg monthly for 2 months.
**
Patients who remain deficient or insufficient after adequate therapy are generally treated with hydroxylated
vitamin D metabolites which are more readily absorbed or, if feasible, with sun or sunlamp exposure. While 25-
OH vitamin D (calcidiol) is the most logical choice of activated vitamin D for patients with liver disease,
calcidiol is not readily available in the U.S. The 1,25-OH activated formulation of vitamin D (Calcitriol) is used
most commonly in chronic renal disease when there is secondary hyperparathyroidism. Calcitriol can also be
used in patients with liver disease or severe malabsorption when there is a lack of the 25-OH vitamin D
substrate to be converted to 1,25-OH vitamin D by the kidney.
***
Vitamin D (25 Hydroxy) levels are generally rechecked 2-3 months after beginning therapy and the target level
is within normal range.
****1000 IU = 25mcg
50,000 IU = 1,250 mcg
136
B. Magnesium supplementation
Cyclosporine and tacrolimus (FK-506) increase urinary excretion of magnesium, resulting in low
serum magnesium levels. Hypomagnesemia has been associated with seizures in patients treated
with cyclosporine or tacrolimus (FK506). All patients receiving these immunosuppressive drugs
require magnesium supplementation and monitoring serum magnesium levels monthly, or more
often as indicated. Oral magnesium with protein (133 mg/tablet) is better tolerated than
magnesium oxide. The magnesium requirements range from 6 to 20 or more tablets daily for
adults and 1 to 9 or more tablets daily for children. Some patients may require intravenous
supplementation (magnesium sulfate) if oral administration causes diarrhea.

137
XXI. DIETS AND OTHER NUTRITIONAL GUIDELINES
A. Diet for immunosuppressed patients after transplant
Patients after hematopoietic transplant or after high dose chemotherapy are at increased
risk of developing food-related infections. It is recommended that all transplant
recipients follow the nutrition guidelines for discharge home, including the Diet for
Immunosuppressed Patients. These guidelines can be found at www.seattlecca.org
under patientsandfamilies/nutrition/nutritionDietsguidelines/
osteoporosisNutritionguidelines. The duration of immunosuppressed patient diet
depends on the immunocompromised status of the patient and the type of transplant, as
described below:
• Allogeneic transplant recipients should follow the immunosuppressed patient diet
guidelines until all immunosuppressive treatments are discontinued.
• Autologous transplant recipients should follow the immunosuppressed patient diet
guidelines until one month after discontinuation of corticosteroids or three months
after chemotherapy or transplant (whichever occurs later) and as long as there are
no GI symptoms.
B. Additional dietary recommendations:
1. Diet for patients receiving treatment with corticosteroids:
In addition to the Diet for Immunosuppressed Patients, nutritional recommendations
to minimize the risk of osteoporosis are needed (see Section XI). These nutritional
guidelines can also be found at www.seattlecca.org/ patientsandfamilies/nutrition/
nutritionDietsguidelines/osteoporosisNutritionguidelines.
2. Diet for patients with graft-versus-host disease of gastrointestinal tract:
In addition to the Immunosuppressed Patient Diet, specific diets are recommended
for patients with GVHD of the GI tract to help alleviate the gastrointestinal
symptoms. Two different gastrointestinal diets (GI1 and GI2) have been developed
by the dietitians at the Fred Hutch. These GI1 and GI2 diets have limited amounts of
fats, fiber, lactose, acidic items and GI irritants. The diets can be found at
www.seattlecca.org under patientsandfamilies/nutrition/nutritionDietsguidelines/.
For patients with severe diarrhea (exceeds 8-10 ml/kg/day) or significant crampy
abdominal pain, bowel rest (NPO) is recommended. TPN at 1.5 x basal energy needs
or higher, 1.5-2.0 g protein/kg with supplemental zinc is also usually needed.
Replacement of stool losses on a mL/mL basis with half-normal saline hydration is
recommended. As diarrhea subsides, the response to oral feeding is highly variable.
138
When oral intake is appropriate, we recommend beginning with isotonic beverage in
small amounts and gradually progressing to the GI1 diet and subsequently to the GI2
diet as tolerated (see Table next page).
GVHD of the upper intestine or stomach may present only as anorexia, nausea, and
early satiety. High-fat foods are generally poorly tolerated. Empiric lactose
restriction should be considered. Patients may find it easier to meet energy and
protein needs with nutritional supplements sipped continuously throughout the day.

139
Gastrointestinal GVHD Diet Progression*
Phase
Symptoms
Diet
Diet Intolerance
1. Bowel rest
GI cramping
Large volume watery diarrhea
Depressed serum albumin
Severely reduced transit time
Small bowel obstruction or diminished
bowel sounds
Nausea and vomiting
Oral: NPO
IV: stress energy and protein
Requirements
2. Introduction of
oral feeding
Minimal GI cramping
Diarrhea less than 500 ml/day
Guaiac-negative stools
Improved transit time (minimum 1.5
hours)
Infrequent nausea and vomiting
Oral: isosmotic, low-residue,
low-lactose beverages,
initially 60 ml every 2-3
hours, for
several days
IV: as for Phase 1
Increased stool volume
or
diarrhea
Increased emesis
Increased abdominal
Cramping
3. Introduction of
solids
Minimal or no GI cramping
Formed stool
Oral: allow introduction of
solid food, once every 3-4
hours: minimal lactose
a
,
low fiber, low fat (20-40
gm/day)
b
, low total
acidity, no gastric irritants
IV: as for Phase 1
As in Phase 2
4. Expansion of
diet
Minimal or no GI cramping
Formed stool
Oral: minimal lactose
a
, low
fiber, low total acidity, no
gastric irritants; if stools
indicate fat
malabsorption: low fat
b
IV: as needed to meet
nutritional requirements
As in Phase 2
5. Resumption of
regular diet
No GI cramping
Normal stool
Normal transit time
Normal albumin
Oral: progress to regular
diet by introducing one
restricted food per day:
acid foods with meals,
fiber-containing foods,
lactose-containing foods.
Order of addition will
vary, depending on
individual tolerances and
preferences.
Patients no longer
exhibiting steatorrhea
should have the fat
restriction liberalized
slowly
IV: discontinue when oral
nutritional intake meets
estimated needs
As in Phase 2
a
Lactose is one of the last disaccharidases to return following villous atrophy. A commercially-prepared lactose solution (Lactaid
R
) is used
to reduce the lactose content of milk by >90%. Lactaid
R
milk (100% lactose-free) is also commercially available.
b
Additional calories may be provided by commercially available medium chain triglycerides which do not exacerbate symptoms.
*Adapted from Darbinian J, Schubert MM. Special management problems. In: Lenssen P, Aker SN, eds. Nutritional Assessment
and Management During Marrow Transplantation. A Resource Manual. Seattle, WA: Fred Hutchinson Cancer Research Center;
1985;63-80.

140
XXII. NATUROPATHIC REMEDIES: HERBAL AND NUTRIENT SUPPLEMENT
PREPARATIONS
• Allogeneic transplant patients:
Herbal/botanical preparations should not be given during immunosuppressive
therapy or in patients with chronic GVHD. One month after discontinuation of all
systemic immunosuppressive treatment and resolution of manifestations of chronic
GVHD, herbal/botanical preparation may be given at the discretion of the primary
physician.
• Autologous transplant patients:
Herbal/botanical preparations should not be given until complete recovery of any
gastrointestinal toxicity and until prednisone therapy has been discontinued for one
month.
Further information regarding guidelines for the use of herbal and nutrient supplement
preparations can be found at www.seattlecca.org under
patientsandfamilies/nuritionDietsguidelines, Guidelines for herbal & nutrient supplements during
hematopoietic stem cell transplantation and high-dose chemotherapy.

141
XXIII. RETURN TO SEATTLE FOR LONG-TERM FOLLOW-UP EVALUATION
All adults who have had an allogeneic transplant and all children who have had either an
allogeneic or autologous transplant should return to the Fred Hutch for a comprehensive
evaluation at one year after the transplant. Depending on clinical indications, follow-up
evaluations at subsequent intervals may be arranged. Children should return for subsequent
evaluations at 2, 3, 5, 10, 15, and 20 years after the transplant. These evaluations focus on
hematologic and immunologic function, assessment of the original disease, and thorough
screening for any late transplant complications. The LTFU evaluation requires four to five
working days to complete. A detailed summary of findings and recommendations will be
forwarded to the referring physician. Appointments must be scheduled at least 4 months in
advance by calling the LTFU office assistant at (206) 667-4415 or by sending a FAX to
1-800-376-8197 (toll-free, USA and Canada).
TYPE OF TRANSPLANT
TIME TO RETURN FOR
COMPREHENSIVE EVALUATION
Allogeneic (ADULT)
Autologous (ADULT)
One year after the transplant
One year after the transplant
based on protocol, patient or
physician request
Follow-up evaluations
at other times per
protocol or as clinically
indicated
Allogeneic & Autologous
(PEDIATRIC)
One year, 2, 3, 5, 10, 15, and 20
years after the transplant

142
XXIV. HOW TO SEND SPECIMENS FOR TESTING AT FRED HUTCH
Clinical laboratory testing for patients who received treatment at Fred Hutchinson Cancer
Center (Fred Hutch) is available at the Fred Hutch. The tests most often performed in our
laboratories at the request of referring physicians include BCR/abl transcripts by polymerase
chain reaction (PCR), CMV PCR and chimerism studies by assessment of variable number
tandem repeat polymorphisms.
We ask that you notify the LTFU office by telephone at (206) 667-4415 or by FAX
(Appendix A) to indicate the expected date and time of arrival for specimens that are sent for
testing at the Fred Hutch. The LTFU office will provide detailed instructions regarding
sample collection and shipment information for the specific test(s) requested.
If surgery or biopsy is planned for evaluation of suspected secondary malignancy or
recurrence of disease, please contact our LTFU office before the procedure, whenever
possible.
Guidelines for Sending Clinical Specimens
1. Call the LTFU office at (206) 667-4415 before sending the specimen (Appendix A).
2. Do not send fresh / frozen samples to arrive on Fridays, weekends or government
holidays.
3. Ship the specimen via an overnight courier service on the day the samples were obtained.
4. Label each tube with
• Patient's name
• Patient's social security number (if not available, date of birth)
• Date that the sample was obtained
• Type of specimen (i.e., peripheral blood, bone marrow, serum, left breast mass, etc.)
5. Please complete Test Request Forms that will be faxed to you by our office
6. SAMPLE(S) MUST BE ACCOMPANIED BY THE FRED HUTCH TEST REQUEST
FORMS
7. Shipment charges are the responsibility of the patient or the facility sending the sample.
A study coordinator will forward shipment instructions to patients who are enrolled in
specific protocols that require samples to be sent to the Fred Hutch for research studies.

143
XXV. REFERENCES
Chronic GVHD
1. Sullivan KM. Graft vs. Host Disease. In: Blume KG, Forman SJ, Appelbaum FR eds. Thomas’ Hematopoietic
Cell Transplantation, 3
rd
Edition. Blackwell Publishing; 2004; 635-664.
2. Lee SJ, Vogelsang G, Flowers MED. Chronic graft-versus-host disease. Biol Blood Marrow Transplant 2003;
9: 215-233.
3. Flowers MED, Parker PM, Johnston LJ, et al. Comparison of chronic graft-versus-host disease after
transplantation of peripheral blood stem cells versus bone marrow in allogeneic recipients: long-term follow-
up of a randomized trial. Blood 2002; 100:415-419.
4. Filipovich AH, Weisdorf D,
Pavletic S, et al: NIH Consensus Development Project on Criteria for Clinical
Trials in Chronic GraftVersus-Host Disease: I. Diagnosis and Staging Working Group Report: Biol Blood
Marrow Transplant 2005; 11: 945-955.
5. Shulman HM, Sullivan KM, Weiden PL, et al. Chronic Graft vs. Host syndrome in man. A long-term
clinicopathologic study of 20 Seattle patients. Am. J. Med. 1980; 69:204-217.
6. Stewart BL, Storer B, Storek J, et al. Duration of immunosuppressive treatment for chronic graft-versus-host disease.
Blood 2004; 104:3501-3506.
7. Au BK, Au MA, Chien JW. Bronchiolitis obliterans syndrome epidemiology after allogeneic hematopoietic
cell transplantation. Biol Blood Marrow Transplant 2011;17:1072-8. doi:10.1016/j.bbmt.2010.11.018
8. Cheng GS, Storer B, Chien JW, et al. Lung Function Trajectory in Bronchiolitis Obliterns Syndrome after
Allogeneic Hematopoietic Cell Transplant. Ann Am Thorac Soc. 2016 Nov;13(11);1932-1939.
9. Williams KM, Cheng GS, Pusic I, Jagasia M, Burns L, Ho VT, Pidala J, Palmer J, Johnston L, Mayer S, Chien
JW, Jacobsohn DA, Pavletic SZ, Martin PJ, Storer BE, Inamoto Y, Chai X, Flowers ME, Lee SJ. Fluticasone,
azithromycin, and montelukast treatment for new-onset bronchiolitis obliterans syndrome after hematopoietic
cell transplantation. Biol Blood Marrow Transplant 2016;22:710-6. doi:10.1016/j.bbmt.2015.10.009
10. Flowers ME and Martin PJ. How we treat chronic graft-versus-host disease. Blood 2015;125:606-615.
doi:10.1182/blood-2014-08-551994
11. Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, Palmer J, Weisdorf D, Treister NS,
Cheng GS, Kerr H, Stratton P, Duarte RF, McDonald GB, Inamoto Y, Vigorito A, Arai S, Datiles MB,
Jacobsohn D, Heller T, Kitko CL, Mitchell SA, Martin PJ, Shulman H, Wu RS, Cutler CS, Vogelsang GB, Lee
SJ, Pavletic SZ, Flowers ME. National institutes of health consensus development project on criteria for
clinical trials in chronic graft-versus-host disease: I. The 2014 diagnosis and staging working group report.
Biol Blood Marrow Transplant 2014;doi:10.1016/j.bbmt.2014.12.001
12. Bergeron A, Godet C, Chevret S, Lorillon G, Peffault de Latour R, de Revel T, Robin M, Ribaud P, Socie G,
Tazi A. Bronchiolitis obliterans syndrome after allogeneic hematopoietic sct: Phenotypes and prognosis. Bone
Marrow Transplant 2013;48:819-24. doi:10.1038/bmt.2012.241
13. Pelligrini R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CPM,
Gustafasson P, Hankinson J, Jensen, R, Johnson DC, MacIntyre N, McKay R Miller MR, Navajas D, Pedersen
OF, Wanger J. Interpretative strategies for lung function tests. Eur Respir J 2005;26:948-968. Williams KM,
Chien JW, Gladwin MT, Pavletic SZ. Bronchiolitis obliterans after allogeneic hematopoietic stem cell
transplantation. JAMA 2009;302:306-14. doi:10.1001/jama.2009.1018
14. Carpenter PA, Kitko CL, Elad S, Flowers ME, Gea-Banacloche JC, Halter JP, Hoodin F, Johnston L,
Lawitschka A, McDonald GB, Opipari AW, Savani BN, Schultz KR, Smith SR, Syrjala KL, Treister N,
Vogelsang GB, Williams KM, Pavletic SZ, Martin PJ, Lee SJ, Couriel DR. National institutes of health
consensus development project on criteria for clinical trials in chronic graft-versus-host disease: V. The 2014
ancillary therapy and supportive care working group report. Biol Blood Marrow Transplant 2015;21:1167-87.
doi:10.1016/j.bbmt.2015.03.024
15. Gunn ML, Godwin, JD, Kanne JP, Flowers ME, Chien JW. High-resolution CT findings of bronchiolitis
obliterans syndrome after hematopoietic stem cell transplantation. J Thorac Imaging 2008 Nov;23(4):244-450.
doi:10.1097/RTI.0b013e3181809df0
16. Williams KM, Chien JW, Gladwin MT, Pavletic SZ. Bronchiolitis obliterans after allogeneic hematopoietic
stem cell transplantation. JAMA 2009;302:306-14. doi: 10.1001/jama.2009.1018.

144
17. Bergeron A, Chevret S, Chagnon K, Godet C, Bergot E, Peffault de Latour R, Dominique S, de Revel T, Juvin
K, Maillard N, Reman O, Contentin N, Robin M, Buzyn A, Socie G, Tazi A. Budesonide/formoterol for
bronchiolitis obliterans after hematopoietic stem cell transplantation. Am J Respir Crit Care Med
2015;191:1242-9. doi:10.1164/rccm.201410-1818OC
18. Norman BC, Jacobsohn DA, Williams KM, Au BK, Au MA, Lee SJ, Moravec CK, Chien JW. Fluticasone,
azithromycin and montelukast therapy in reducing corticosteroid exposure in bronchiolitis obliterans syndrome
after allogeneic hematopoietic sct: A case series of eight patients. Bone Marrow Transplant 2011;46:1369-73.
doi:10.1038/bmt.2010.311
19. Cheng GS, Edelman JD, Madtes DK, Martin PJ, Flowers ME Outcomes of lung
transplantation after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2014
Aug;20(8):1169-75. doi: 10.1016/j.bbmt.2014.04.008. Epub 2014 Apr 13
Hyperlipidemia:
References:
1. Baker KS, Ness K, Steinberger J, et al. Diabetes, hypertension and cardiovascular events in survivors of hematopoietic cell transplantation
(HCT): a report from the bone marrow transplant survivor study. Blood 2006; 109:1765-1772.
2. Seipelt IM, Crawford SE, Rodgers S, et al. Hypercholesterolemia is common after pediatric heart transplantation: initial experience with
pravastatin. J Heart Lung Transplant. 2004; 23: 317-322.
3. Stranberg TE, Pyorala K, Cook TJ, et al. Mortality and incidence of cancer during 10-year follow-up of the Scandinavian Simvastatin Survival
Study (4S). Lancet. 2004; 364: 771-777.
4. LIPID study group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of
initial cholesterol levels. N Engl J Med. 1998; 339: 1349-1357.
5. Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary artery disease with pravastatin in men with hypercholesterolemia. N Engl J Med.
1995; 333: 1301-1307.
6. Ghobrial IM, Bunch TJ, Caplice NM, et al. Fatal coronary artery disease after unrelated donor marrow transplantation. Mayo Clin Proc. 2004;
79: 403-406.
7. Gatt ME, Liebster D, Leibowitz D, Matzner Y. Acute myocardial infarction after bone marrow transplantation: an unsuspected late complication.
Ann Hematol. 2003; 82: 136-138.
8. Kupari M, Volin L, Suokas A, et al. Cardiac involvement in bone marrow transplantation: electrocardiographic changes, arrhythmias, heart
failure and autopsy findings. Bone Marrow Transplant. 1990; 5: 91-98.
9. Chan KW, Taylor GP, Shepherd JD, et al. coronary artery disease following bone marrow transplantation. Bone Marrow Transplant. 1989; 4:
327-330.
10. Wang B, Cao LX, Liu HL, et al. Myocardial infarction following allogeneic bone marrow transplantation. Bone Marrow Transplant. 1996; 18:
479-480.
11. O’Rourke B, Barbir M, Mitchell AG. Efficacy and safety of fluvastatin therapy for hypercholesterolemia after heart transplantation. Results of a
randomized double-blind placebo controlled study. Int. J. Cardiology. 2004; 94: 235-240.
12. Kobashigawa JA, Katznelson S, Laks H, et al. Effect of pravastatin on outcomes after cardiac transplantation. N Engl J Med. 1995; 333: 621-627.
13. Wenke K, Meiser B, Thiery J, et al. Simvastatin initiated early after heart transplantation: 8-year prospective experience. Cirulation. 2003; 107:
93-97.
14. Holdaas H, Fellstrom B, Jardine AG, et al. Effect of fluvastatin on cardiac outcomes in renal transplant recipients: a multicenter, randomized,
placebo-controlled trial. Lancet. 2003; 361: 2024-2031.
15. Cosio F, Pesavento TE, Pelletier RP, et al. Patient survival after renal transplantation III: the effects of statins. AM J Kidney Dis. 2002; 40: 638-
643.
16. Del Castillo D, Cruzado JM, Diaz MJ, et al. The effects of hyperlipidemia on graft and patient outcome in renal transplantation. Nephrol Dial
Transplant. 2004; 19; Suppl 3: 67-71.
17. Chin C, Gamberg P, Miller J, et al. Efficacy and safety of atrovastatin after pediatric heart transplantation. J Heart Transplant. 2002; 21: 1213-
1217.
18. Mahle WT, Vinvent N, Berg AM. Pravastatin therapy is associated with reduction in coronary allograft vasculopathy in pediatric heart
transplantation. J. Heart Lung Transplant. 2005; 24: 63-66.
19. Argent E, Kainer G, Aitken M, et al. Atorvastatin treatment for hyperlipidemia in pediatric renal transplant recipients. Pediatr Transplantation.
2003; 7: 38-42.
20. Prasad GV, Ahmed A, Nash MM. Blood pressure reduction with HMG-CoA reductase inhibitors in renal transplant recipients. Kidney Int. 2003;
63: 360-364.
21. Borghi C, Dormi A, Veronesi M, et al. Association between different lipid-lowering treatment strategies and blood pressure control in the
Brisighella Heart Study. Am Heart J. 2004; 148: 285-292.
22. Tsira S, Elisaf M, Mikhailidis DP. Early vascular benefits of statin therapy. Curr Med Res Opin. 2003; 19: 540-556.
23. Mach F. Statins as immunomodulatory agents. Circulation. 2004; 109 (21 Suppl 1): II, 15-17.
24. Fehr T, Kahlert C, Fierz W, et al. Statin-induced immunomodulatory effects on human T cells in vivo. Atherosclerosis. 2004; 175: 83-90.
25. Koc S, Leisenring W, Flowers ME, et al. Therapy for chronic graft-versus-host disease: a randomized trial comparing cyclosporine plus
prednisone versus prednisone alone. Blood. 2002; 100: 48-51.
26. Prasad GV, Chiu R, Nash MM, et al. Statin use and bone mineral density in renal transplant recipients. Am J Transplant. 2003; 3: 1320-1321.
27. Pritchett JW. Statin use decreases the risk of osteonecrosis in patients receiving steroids. Clin Orthop. 2001; 386: 173-178.
28. Wang GJ, Cui Q, Balian G. The pathogenesis and prevention of steroid-induced osteonecrosis. Clin Orthop. 2000; 370: 295-310.
29. Adapted from Circulation 2004;110:227-239.

145
30. Fletcher B, Berra K, Ades P, Braun LT, et al. Managing abnormal lipids, a collaborative approach. Circulation. 2005; 112:3184-3209.
31. Lichtenstein Ah, Appel Lj, Brands Mm, Carnethon M, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the
American Heart Association Nutrition Committee. Circulation. 2006; 114:82-96.
32. Tong J et al. Rhabdomyolysis after concomitant use of cyclosporine and simvastatin in a patient transplanted for multiple myeloma, BMT 2005;
36, 739-740.
33. Miller Lw Cardiovascular toxicities of immunosuppressive agents Am J Transpl 2002; 2 (9): 807-818.
34. Kasiske B et al. Clinical practice guidelines for managing dyslipidemia in kidney transplant patients: a report from the Managing dyslipidemia in
chronic kidney disease work group of the national kidney foundation kidney disease outcomes quality imitative Am J Transpl 2004, 4: 13-53.
35. de Ferranti SD, Steinberger J, Ameduri R, et al. Cardiovascular Risk Reduction in High-Risk Pediatric Patients: A Scientific Statement From the
American Heart Association. Circulation 2019, 139: e603–e634.
Hypertension
1. Chow et al, Ann Intern Med, 2011 in press
2. Majhail NS et al, High prevalence of metabolic syndrome after allogeneic hematopoietic cell
transplantation. Bone Marrow Transplant 2009;43:49-54.
3. http://www.nhlbi.nih.gov/guidelines/hypertension/express.pdf
Iron Overload:
1. Christian Rose, Olivier Ernst, Bernard Hecquet, Patrice Maboudou, Pascale Renom, Marie Pierre Noel, Ibrahim
Yakoub-Agha, Francis Bauters, Jean Pierre Jouet. Quantification by magnetic resonance imaging and liver
consequences of post-transfusional iron overload alone in long-term survivors after allogeneic hematopoietic
stem cell transplantation. Haematologica June 2007 92: 850-853; doi:10.3324/haematol.11063
2. T.E. DeFor, B. Kang, C. Paley, H. Lazarus, L.J. Burns. High Prevalence of Iron Overload in Adult Allogeneic
Hematopoietic Cell Transplant suvivors. Biol Blood Marrow Transplant 2008; July , Volume 14 (7):790-4
3. Alessandro Busca, Michele Falda, Paola Manzini, Sergio D'Antico, Adriano Valfrè, Franco Locatelli, Roberto
Calabrese, Annalisa Chiappella, and others. Iron Overload in Patients Receiving Allogeneic Hematopoietic
Stem Cell Transplantation: Quantification of Iron Burden by a Superconducting Quantum Interference Device
(SQUID) and Therapeutic Effectiveness of Phlebotomy. Biology of Blood and Marrow Transplantation, 2009
Vol. 16, Issue 1, p115–122
4. Altes A, Remacha AF, Sarda P, Sancho FJ, Sureda A, Martino R et al. Frequent severe liver iron overload after
stem cell transplantation and its possible association with invasive aspergillosis. Bone Marrow Transplant 2004;
34: 505–509.
5. Lucarelli G, Angelucci E, Giardini C, Baronciani D, Galimberti M, Polchi P, Bartolucci M, Muretto P, Albertini
F. Fate of iron stores in thalassaemia after bone-marrow transplantation. Lancet. 1993 Dec 4;342(8884):1388-91.
6. Trottier BJ, Burns LJ, DeFor TE, Cooley S, Majhail NS. Association of iron overload with allogeneic
hematopoietic cell transplantation outcomes: a prospective cohort study using R2-MRI-measureed liver content.
Blood. 2013:122(9): 1678-1684Wermke, Clin Cancer Res, 2012
7. Martin Wermke, Anne Schmidt, Jan Moritz Middeke, Katja Sockel, Malte von Bonin, Claudia Schönefeldt, Sabine
Mair, Verena Plodeck, Michael Laniado, Günter Weiss, Johannes Schetelig, Gerhard Ehninger, Igor Theurl, Martin
Bornhäuser and Uwe Platzbecker. MRI-Based Liver Iron Content Predicts for Nonrelapse Mortality in MDS and
AML Patients Undergoing Allogeneic Stem Cell Transplantation. Clin Cancer Res 2012;Sept18:6460-6468
8. Armand, Philippe et al. Iron Overload in Allogeneic Hematopoietic Cell Transplantation Outcome: A Meta-
Analysis. Biology of Blood and Marrow Transplantation , Volume 20 , Issue 8 , 1248 - 1251
9. Wermke M, Eckoldt J, Götze KS, Klein SA, Bug G, de Wreede LC, Kramer M, Stölzel F, von Bonin M,
Schetelig J, Laniado M, Plodeck V, Hofmann WK, Ehninger G, Bornhäuser M, Wolf D, Theurl I, Platzbecker
U. Enhanced labile plasma iron and outcome in acute myeloid leukaemia and myelodysplastic syndrome after
allogeneic haemopoietic cell transplantation (ALLIVE): a prospective, multicentre, observational trial. Lancet
Haematol. 2018 May;5(5):e201-e210
10. Charles T. Quinn, MD, MS
and Tim G. St Pierre, PhD.
.
MRI Measurements of Iron Load in
Transfusion‐Dependent Patients: Implementation, Challenges, and Pitfalls. Pediatr Blood Cancer. 2016 May;
63(5): 773–780.
11. Strasser S I, Kowdley K V, Sale G E and McDonald G B. Iron overload in bone marrow transplant recipients.
BMT 1998;22:2:167-173
12. Gale, E, Torrance, J, Bothwell, T. The Quantitative Estimation of Total Iron Stores in Human Bone Marrow.
JCI. 1963; Jul; 42(7): 1076–1082. doi: 10.1172/JCI104793
13. Cavill I, Ricketts C (1978) Erythropoiesis and iron kinetics. Br J Haematol 38:433–437

146
14. Emanuele Angelucci, Pietro Muretto, Guido Lucarelli, Marta Ripalti, Donatella Baronciani, Buket Erer, Maria
Galimberti, Claudio Giardini, Djavid Gaziev, Paola Polchi and the Italian Cooperative Group for Phlebotomy
Treatment of Transplanted Thalassemia Patients. Phlebotomy to Reduce Iron Overload in Patients Cured of
Thalassemia by Bone Marrow Transplantation. Blood 1997 90:994-998;
15. Mariotti, E. Angeluuci, E, Agostini, A. et al. Evaluation of cardiac status in iron loaded thalassemia patients
following bonew marrow transplantation: improvement in cardiac function during reduction in body iron
burden. Br J Haematol 1998: 103: 916-921
16. Eisfeld AK, Krahl R, Jaekel N, Niederwieser D, Al-Ali HK. Kinetics of iron removal by phlebotomy in patients
with iron overload after allogeneic hematopoietic cell transplantation. Am J Blood Res.2012;2(4):243-253
17. Kaloyannidis P, Yannaki E, Sakellari I, et al. The impact of desferrioxamine postallogeneic hematopoietic cell
transplantation in relapse incidence and disease-free survival: a retrospective analysis. Transplantation.
2010/2/27;89(4):472-479.
18. Sivgin S, Baldane S, Akyol G, et al. . The oral iron chelator deferasirox might improve survival in allogeneic
hematopoietic cell transplant (alloHSCT) recipients with transfusional iron overload. Transfus Apheresis Sci.
2013;49(2):295-301.
19. Carlos Vallejo, Montserrat Batlle, Lourdes Vázquez, Carlos Solano, Antonia Sampol, Rafael Duarte, Dolores
Hernández, Javier López, Montserrat Rovira, Santiago Jiménez, David Valcárcel, Vicente Belloch, Mónica
Jiménez, Isidro Jarque. Phase IV open-label study of the efficacy and safety of deferasirox after allogeneic stem
cell transplantation. Haematologica October 2014 99: 1632-1637; doi:10.3324/haematol.2014.105908
20. Eva Rombout‐Sestrienkova. Erythrocytapheresis versus phlebotomy in the maintenance treatment of HFE
hemochromatosis patients: results from a randomized crossover trial. Transfusion 2016. Vol 56, Issue 1,
January 2016, pages 261-270
21. Sundic T, Hervig T, Hannisdal S, et al. Erythrocytapheresis compared with whole blood phlebotomy for the
treatment of hereditary haemochromatosis. Blood Transfus. 2014;12 Suppl 1(Suppl 1):s84–s89.
doi:10.2450/2013.0128-13
22. J.B.PorterE.R.Huehns. The toxic effects of desferrioxamine. Baillière's Clinical Haematology. Volume 2, Issue
2, April 1989, Pages 459-474
IV Immunoglobulin:
1. Cooperative Group for the Study of Immunoglobulin in Chronic Lymphocytic Leukemia. Intravenous
immunoglobulin for the prevention of infection in chronic lymphocytic leukemia. A randomized, controlled
clinical trial. N Engl J Med. 1988;319(14):902-7.
2. The National Institute of Child Health and Human Developments Intravenous Immunoglobulin Study Group.
Intravenous immune globulin for the prevention of bacterial infections in children with symptomatic human
immunodeficiency virus infection. N Engl J Med. 1991;325(2):73-80.
3. Magny JF, Bremard-Oury C, Brault D, et al. Intravenous immunoglobulin therapy for prevention of infection in
high-risk premature infants: report of a multicenter, double-blind study. Pediatrics. 1991;88(3):437-43.
4. Winston DJ, Antin JH, Wolff SN, et al. A multicenter, randomized, double-blind comparison of different doses
of intravenous immunoglobulin for prevention of graft-versus-host disease and infection after allogeneic bone
marrow transplantation. Bone Marrow Transplant. 2001;28(2):187-96.
5. Cordonnier C, Chevret S, Legrand M, et al. Should immunoglobulin therapy be used in allogeneic stem-cell
transplantation? A randomized, double-blind, dose effect, placebo-controlled, multicenter trial. Ann Intern Med.
2003;139(1):8-18.
6. Sokos DR, Berger M.and Lazarus HM. Intravenous immunoglobulin: appropriate indications and uses in
hematopoietic stem cell transplantation [Review]. Biol. Blood and Marrow Transplantation. 2002.8(3):117-30.
7 Sullivan, KM, Kopecky, KJ, Jocom, J, et al. Immunomodulatory and antimicrobial efficacy of intravenous
immunoglobulin in bone marrow transplantation. N.Engl.J.Med. 323:705-712, 1990.
8. Sullivan, KM, Storek, J, Kopecky, KJ, et al. A controlled trial of long-term administration of intravenous
immunoglobulin to prevent late infection and chronic graft-vs.-host disease after marrow transplantation:
clinical outcome and effect on subsequent immune recovery. Biol. Blood and Marrow Transplantation 2: 44-53,
1996.
9. Bhella, Sita et al. Choosing Wisely BMT: American Society for Blood and Marrow Transplantation and
Canadian Blood and Marrow Transplant Group's List of 5 Tests and Treatments to Question in Blood and
Marrow Transplantation. Biology of Blood and Marrow Transplantation , Volume 24 , Issue 5 , 909 - 913

147
Liver:
1. Strasser SI, McDonald GB. Hepatitis Viruses and Hematopoietic Cell Transplantation: A Guide to Patient and
Donor Management. Blood 93: 1127-1136, 1999.
2. Murakami CS, Louie W, Chan GS, et al. Biliary obstruction in hematopoietic cell transplant recipients: An
uncommon diagnosis with specific causes. Bone Marrow Transplantation 23: 921-927, 1999.
3. Strasser SI, Sullivan KM, Myerson D, et al. Cirrhosis of the liver in long-term marrow transplant survivors.
Blood 93: 3259 – 3266, 1999.
4. Strasser SI, Myerson D, Spurgeon CL, et al. Hepatitis C virus infection after bone marrow transplantation: A
cohort study with 10 year follow-up. Hepatology 29: 1893 – 1899, 1999.
5. Strasser SI, Shulman HM, McDonald GB. Cholestasis after hematopoietic cell transplantation. Clinics in Liver
Disease 3: 651 – 668, 1999.
6. Strasser SI, Shulman HM, Flowers MED, et al. Chronic graft-vs-host disease of the liver: Presentation as an
acute hepatitis. Hepatology 32: 1265 – 1271, 2000.
7. Strasser SI, McDonald GB. Chapter 56, Gastrointestinal and hepatic complications, in Hematopoietic Cell
Transplantation, Second Edition, edited by Thomas ED, Blume KG, Forman SJ. Cambridge, MA., Blackwell
Scientific Publications, 1999, pp.627 – 658.
8. Strasser SI, McDonald GB. Chapter 67, Hepatobiliary complications of hematopoietic cell transplantation, in
Schiff’s Diseases of the Liver, Ninth Edition, edited by Schiff ER, Sorrell MF, Maddrey WC. Philadelphia, PA.,
J.B. Lippincott Company, 2002.
9. McDonald GB. Hepatobiliary complications of hematopoietic cell transplantation, 40 years on. Hepatology 51:
1450 – 1460, 2010.
10. Hockenbery DM, Strasser SI, McDonald GB. Chapter 96, Gastrointestinal and hepatic complications, in
Thomas’ Hematopoietic Cell Transplantation, Fifth Edition, edited by Appelbaum FR, Forman SJ, Negrin RS,
Antin JH. Oxford, UK, Wiley-Blackwell Publishing, in press.
11. Kida A, McDonald GB. Gastrointestinal, hepatobiliary, pancreatic, and iron-related diseases in long term
survivors of allogeneic hematopoietic cell transplantation. Seminars in Hematology 49:43-58, 2012).
12. AMERICAN ASSOCIATION FOR THE STUDY OF LIVER DISEASES (AASLD) AND Infectious
Diseases Society of America (IDSA) Recommendations for Testing, Managing, and Treating Hepatitis C.
http://hcvguidelines.org Accessed on February 20, 2014.
Prevention of Osteoporosis and Glucocorticosteroid Induced Osteoporosis:
1. Kovvuru K, Kanduri SR, Vaitla P, et al. Risk factors and management of osteoporosis post-transplant.
Medicinia. 56: 302, 2020.
2. Kendler DL, Body JJ, Brandi ML, et al. Bone management in hematologic stem cell transplant recipients.
Osteoporosis International. 29:2598-2610, 2018.
3. NOF’s clinician’s guide to prevention and treatment of osteoporosis. Washington, D.C.: National Osteoporosis
Foundation, 2009.
4. Tu KN, Lie JD, Wan CKW, et al. Osteoporosis: A review of treatment options. P&T. 43:2, 92-104, 2018.
5. Miller PD. Management of severe osteoporosis. Exp Opin Pharm. 17:4, 473-488, 2016.
6. Watts NB and Diab DL. Long-term use of bisphosphonates in osteoporosis. J Clin Endocrinol Metab. 95: 1555-
1565, 2010.
7. Black DM et al. Bisphosphonates and fractures of the subtronchanteric or diaphyseal femur. N Engl J Med. 362:
1761-1771, 2010.
8. Tsourdi E, Langdahl B, Cohen-Solal M, et al. Discontinuation of Denosumab therapy for osteoporosis: A
systematic review and position statement by ECTS. Bone. 105:11-17, 2017.
9. Gonzalez-Rodriguez E, Aubry-Rozier B, Stoll D, Zaman K, Lamy O. Increased Risk of Multiple Spontaneous
Vertebral Fractures at Denosumab Discontinuation Must Be Taken Into Account. J Clin Oncol. 38(14):1641-
1642, 2020.

148
Vaccinations
1. Rubin LG, Levin MJ, Ljungman P, et al. Infectious Diseases Society of America. 2013 IDSA clinical practice
guideline for vaccination of the immunocompromised host. Clin Infect Dis. 2014; 58(3):309-318.
2. Tomblyn M, Chiller T, Einsele H, et al. Center for International Blood and Marrow Research; National Marrow
Donor program; European Blood and MarrowTransplant Group; American Society of Blood and Marrow
Transplantation; Canadian Blood and Marrow Transplant Group; Infectious Diseases Society of America;
Society for Healthcare Epidemiology of America; Association of Medical Microbiology and Infectious Disease
Canada; Centers for Disease Control and Prevention. Guidelines for preventing infectious complications among
hematopoietic cell transplantation recipients: a global perspective [published correction appears in Biol Blood
Marrow Transplant. 2010;16(2):294]. Biol Blood Marrow Transplant. 2009;15(10):1143-1238.
3. Cordonnier C, Einarsdottir S, Cesaro S, et al. Vaccination of haemopoietic stem cell transplant recipients:
guidelines of the 2017 European Conference on Infections in Leukaemia (ECIL 7). Lancet Infect Dis.
2019;19:e200-e212
4. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/immunocompetence.html
5. Carpenter PA, Englund JE. How I vaccinate blood and marrow transplant recipients. Blood 2016;127(23):2824-
2832.
6. Janssen RS, Mangoo-Karim R, Pergola PE, et al. Immunogenicity and safety of an investigational hepatitis B
vaccine with a toll-like receptor 9 agonist adjuvant (HBsAg-1018) compared with a licensed hepatitis B vaccine
in patients with chronic kidney disease. Vaccine 2013;31(46):5306-5313.
7. Awad AM, Ntoso A, Connaire JJ, et al. An open-label study evaluating the immunogenicity and safety of the
hepatitis B vaccine HepB-CpG (HEPLISAV-B
®
) in adults receiving hemodialysis. Vaccine 2021;39(25)3346-
3352.
8. Manley HJ, Aweh G, Frament J, et al. A real-world comparison of Hep B (Engerix-B
®
) and HepB-CpG
(Heplisav-B
®
) vaccine seroprotection in patients receiving maintenance dialysis. Nephrol Dial Transplant. 2022
Feb12:gfac039.
9. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/timing.html
10. https://www.cdc.gov/vaccines/pubs/pinkbook/downloads/appendices/a/age-interval-table.pdf
11. Schuster JE, Hamdan L, Dulek DE, et al. Influenza Vaccine in Pediatric Recipients of Hematopoietic-Cell
Transplants. N Engl J Med. 2023;388(4):374-376.

149
APPENDIX A
FAX LTFU CONSULT
Date: __________
To: FRED HUTCHINSON CANCER CENTER From: ______________________________
Long Term Follow Up
Fax: 1-800-376-8197 (toll-free, USA & Canada) Fax: ________________________________
Phone: (206) 667-4415 Phone: ______________________________
Patient name: _______________________________ Date of birth: ______________________
Current GVHD Treatments (check all the apply):
Corticosteroids: daily alternate day (dose: _________) Trimethoprim-sulfamethoxazole
Cyclosporine (Neoral, Sandimmune) (or equivalents) Penicillin
Tacrolimus (FK506) Dapsone
Mycophenolate Mofetil (MMF) (Cellcept) Acyclovir or valacyclovir
Thalidomide (Thalomid) Ganciclovir, ValGANCiclovir
Rapamycin (Sirolimus) Fluconazole or itraconazole
Rituximab
Extracorporeal photopheresis (ECP)
Other:
No immunosuppressive medications
Current problems(s):
What questions would you like the consultant to address?
Laboratory and other reports are being sent with this FAX: YES NO
Reply to (if other than sender listed above): ______________________________________________
Fax (____ ) ___________________ Phone (_____) ___________________
150
APPENDIX B
FAX LTFU ALERT
Date: ____________
To: FRED HUTCHINSON CANCER CENTER From: ____________________________
Long Term Follow Up
Fax: 1-800-376-8197 (toll-free, USA & Canada) Fax: ______________________________
Phone: (206) 667-4415 Phone: ___________________________
Patient name: ______________________________ Date of birth: _________________
❑This patient expired on _____/_____/_____ due to ___________________________________.
❑This patient was newly diagnosed with clinical extensive chronic GVHD.
(Please send copies of any records regarding this diagnosis.)
❑Check here if you would like a consultation regarding the management of GVHD in this case.
❑This patient has now started immunosuppressive therapy.
❑This patient has now stopped all immunosuppressive therapy.
❑The immunosuppressive therapy for this patient has been changed.
❑The original disease (see above) has recurred.
❑This patient was diagnosed with a secondary malignancy of (primary site)_________________.
❑Surgery or biopsy has been planned for evaluation of suspected secondary malignancy.
(We are interested in obtaining fresh tissue specimens.)
❑This patient has been diagnosed with myelodysplasia.
❑This patient’s name and/or address has changed to:
❑This patient is now being seen by (practitioner, address, phone number):
❑This office has moved/ changed it’s phone number to:
❑This patient requests discontinuation of further contact from the Fred Hutch due to
(reason, if stated):
Reply to (if other than sender listed above): ____________________________________
Fax (_______) ___________________ Phone (________) _________________

151
APPENDIX C
FORM FOR DESCRIPTION OF SKIN INVOLVEMENT
NAME:
Date of Birth:
DATE OF ASSESSMENT:___________________
Region
% Area
Involved
Region
% Area
Involved
Head (9%)
Right leg (8%)
Neck (1%)
Right foot (1%)
Chest (9%)
Left arm (4%)
Abdomen (9%)
Left forearm (4%)
Back (18%)
Left hand (1%)
Right arm (4%)
Left thigh (8%)
Right forearm (4%)
Left leg (8%)
Right hand (1%)
Left foot (1%)
Right thigh (8%)

APPENDIX –D (Pages 1-3 of the CHRONIC GVHD ASSESSMENT AND SCORING FORM)
152

APPENDIX –D (Pages 1-3 of the CHRONIC GVHD ASSESSMENT AND SCORING FORM)
153

APPENDIX –D (Pages 1-3 of the CHRONIC GVHD ASSESSMENT AND SCORING FORM)
154

155
APPENDIX E
ASSESSMENT OF SKIN THICKNESS
Modified Rodnan Score*
Patient Name: ___________________________________Date of Birth: ____________
Calculate skin score by summing the scores from all evaluated anatomic areas.
A. Evaluate skin thickness by clinical palpation:
0 = normal skin thickness
1 = mildly increased skin thickness
2 = moderately increased skin thickness
3 = severely increased skin thickness (inability to pinch skin into a fold)
B. Surface of anatomic areas evaluated (N = 17)
Area of Body
Dates:
Range
Score
Score
Score
Score
Score
Face
0-3
Anterior chest
0-3
Abdomen
0-3
Fingers
R
0-3
L
0-3
Dorsum of hands
R
0-3
L
0-3
Forearms
R
0-3
L
0-3
Upper arms
R
0-3
L
0-3
Thighs
R
0-3
L
0-3
Lower legs
R
0-3
L
0-3
Dorsum of feet
R
0-3
L
0-3
TOTAL
0-51
“Skin Thickness Score in Systemic Sclerosis: An Assessment of Inter-observer Variability in 3 Independent Studies,” Clements et al,
The Journal of Rheumatology 1993, 20:11, 1892-1896
C-GVHDassessment&scoringform.medf.2.28.2006

APPENDIX F
156
