Summary Plan
Description
2024
Benefits For
Hilton U.S.
Team Members
(except for Hawaii and
Puerto Rico)
Health Care
Disability Protection
Life and Accident Insurance

This Summary Plan Description (SPD) summarizes the major features of the benefits programs for U.S. full-
time eligible employees and certain eligible leased employees of Hilton Employer Inc. and its affiliates (“Hilton”)
as of January 1, 2024. This SPD does not apply to Team Members in Hawaii or Puerto Rico; benefits for these
Team Members are described in a separate summary plan description. Certain Team Members whose
employment is subject to a collective bargaining agreement are excluded or have modified coverage. You
should also refer to any applicable cover letter accompanying this SPD for changes and additions to the SPD
that apply to employees at:
• Hilton Baltimore
• Hilton McLean
• Hilton Crystal City
• Doubletree – Crystal City
• Embassy Suites – Crystal City
• Hilton – Vancouver
• Doubletree – San Diego Valley
• Embassy Suites – San Diego La Jolla
• Hilton La Jolla Pines
• Hilton San Diego Bay Front
• La Quinta (Palm Springs)
• Hotel Del Coronado
You should not rely on this information other than as a general summary of the features of the Hilton Health
and Welfare Plan (the “Plan”). Any capitalized items not defined in this SPD shall refer to the defined terms in
the Plan.
This SPD should be read in conjunction with the Program Documents. Program Documents are the documents
listed in the Plan Information Section of this SPD. These documents provide further detail on coverage benefits
as well as important exclusions, limitations, and requirements applicable to receive benefits. You may obtain a
copy of the Program Documents online by following the steps below and in the “General Information” section or
by contacting the Plan Administrator.
To access the Program Documents, follow the instructions below:
1. Access YBR via this website: http://digital.alight.com/hilton
2. Click on the drop-down arrow next to the globe symbol within the footer of the logon page, then select
“English” or “Spanish – Español.”
3. Enter your User ID and password on the Logon page.
4. From the YBR Home page, hover over the tab titled “Knowledge Center.”
5. From the Knowledge Center drop-down menu items, click on the Plan Information link.
6. The SPD and available Program Documents will be displayed on the next screen.
This SPD contains only a summary of information about the Plan. Details about the Plan are contained in the
official plan document. If there is a discrepancy between the information in this SPD and the formal plan
document, the formal plan document will govern. If there is a discrepancy between the terms of a fully-insured
benefits option offered under the Plan and the official plan documents, including the SPD, the fully-insured
policy will govern.
Hilton reserves the right to change, suspend or terminate any plan, program, coverage, or contribution at any
time for any reason.
CONTENTS: SUMMARY PLAN DESCRIPTION
INTRODUCTION .............................................................................................. 1
PARTICIPATION .............................................................................................. 3
ADMINISTRATION ......................................................................................... 26
CLAIMS AND APPEALS ................................................................................ 40
MEDICAL COVERAGE .................................................................................. 50
PRESCRIPTION DRUGS .............................................................................. 57
DENTAL COVERAGE .................................................................................... 64
VISION COVERAGE ...................................................................................... 66
FLEXIBLE SPENDING ACCOUNTS ............................................................. 69
EMPLOYEE ASSISTANCE PROGRAM ........................................................ 81
INTERNATIONAL BUSINESS TRAVEL PROGRAM .................................... 83
MEDICAL BENEFITS WHILE ABROAD ........................................................ 86
LEGAL SERVICES......................................................................................... 88
DISABILITY COVERAGE .............................................................................. 90
LIFE AND ACCIDENT PROTECTION ........................................................... 98
GENERAL INFORMATION .......................................................................... 105

1
Introduction
WHAT’S INSIDE
This SPD contains important information on many of the Benefit Programs offered under the Plan. Please
read it carefully.
AN OVERVIEW OF YOUR HEALTH AND WELFARE BENEFITS PROGRAMS
The Plan offers you a variety of benefits and levels of coverage (Benefit Programs) from which you can choose.
(Note: eligibility criteria may vary for each benefit offering):
• Medical Benefits Program with Prescription Drug Program
• Dental Benefits Program
• Vision Benefits Program
• Flexible Spending Accounts (FSAs) currently administered by Alight
• Health Care FSA
• Dependent Care FSA
• Short-term Disability
• Long-Term Disability
• Life Insurance (Basic, Supplemental and Dependent)
• Retiree Life Insurance*
• Accidental Death and Dismemberment (AD&D)
• Employee assistance program (EAP)
• Business Travel Accident Insurance
• Legal Services
• Voluntary Medical Benefits
• International Assignee Healthcare Plan
*This benefit is available only to a closed group of retirees. No new participants are allowed at this time.
THIRD PARTY ADMINISTRATORS
For purposes of administrating the various Benefit Programs under the Plan, the Plan Administrator has
retained the services of certain independent third-party administrators and insurance companies. Generally,
the third-party administrator does not assume liability for benefits payable under this Plan; some third-party
administrators, however, may be designated as a “named fiduciary”, as that term is defined in ERISA, for
purposes of processing claims.

Introduction
2
MORE INFORMATION
We urge you to read this SPD, share it with other family members covered under the Plan, and keep it for
future reference. If you have questions about your benefits, please contact the Hilton Benefits Center. You
may reach the Hilton Benefits Center at 1.877.442.4772 Monday through Friday from 8:00 a.m. to 6:00
p.m. CT.
The role of the Hilton Benefits Center and the service center representatives with the Plan’s insurers and third-
party administrators is to assist you with questions you may have about this Plan. However, statements made
by such representatives do not have a binding effect on the Plan. If you need to bring or appeal a claim under
this Plan, you should follow the formal claims and appeals procedures described in this SPD.

3
PARTICIPATION
ELIGIBILITY ..................................................................................................... 4
Your Eligibility ............................................................................................ 4
Your Eligible Dependents .......................................................................... 6
Proof of Dependent/Disabled Status ......................................................... 8
Qualified Medical Child Support Order (QMCSO) .................................... 8
Dual Coverage........................................................................................... 8
On-Site Medical Clinics ............................................................................. 9
COST OF COVERAGE .................................................................................. 10
Pre-Tax vs. After-Tax .............................................................................. 11
ENROLLMENT ............................................................................................... 12
When to Enroll ......................................................................................... 12
How to Enroll ........................................................................................... 12
Annual Enrollment ................................................................................... 13
Medical Coverage Enrollment – After-Tax Basis .................................... 14
Special Circumstances: Re-employment .............................................. 14
Changing Coverage During the Year ...................................................... 14
WHEN COVERAGE ENDS ............................................................................ 24
PARTICIPATION

4
Participation
ELIGIBILITY
Your Eligibility
Generally, you are eligible for health and welfare benefits if:
• you are a regular U.S. Team Member of Hilton; and
• you are “full-time”, which for purposes of this Plan means you are an hourly or salaried employee and :
o are reasonably expected to work at least 30 hours a week when hired (as determined by Hilton)
(referred to as a Non-Variable Hour Team Member); or
o are not reasonably expected to work at least 30 hours when hired, but who averages 30 or more
hours of service during an applicable measurement period (referred to as a Variable Hour Team
Member).
Note: Team Member does not include individuals employed by a hotel owner or any other non-affiliated entities
(including franchisees). This definition of Team Member shall apply to this SPD and any other communications
sent to participants relating to benefits offered under the Plan.
You are eligible for disability insurance, life and AD&D insurance, business travel accident insurance if you
are a full-time U.S. Team Member of Hilton (and a salaried Corporate Team Member for salary
continuation). Except as provided below for Corporate Team Members, coverage will begin following a
90-day waiting period.
Please note that if you are a Variable Hour Team Member, coverage will begin following completion of your
initial measurement period. See Affordable Care Act Provisions below.
Excluded Individuals
You are not eligible to participate in the Plan if you are:
• are an independent contractor,
• are an individual subject to a consultant or employee leasing agreement,
• are covered by a collective bargaining agreement with Hilton (unless the collective bargaining
agreement requires otherwise),
• are employed by a hotel owner other than Hilton or one of its affiliated entities where Hilton manages
employees at that hotel but does not actually employ them, unless eligibility is approved by the Plan
Administrator, or
• are employed at a franchised property.
Note: If you are otherwise an eligible Employee but work at a property that is managed, but not owned, by Hilton
and the owner sponsors and offers its own health and welfare benefits, you are not eligible to participate in this
Plan.

Participation
5
Note for Corporate Team Members:
If you are a newly hired Corporate Team Member and you are not a Variable Hour Team Member, you
must enroll in the Plan, including the Flexible Spending Accounts or Health Savings Account, within the first
30 days of hire. With the exception of the Flexible Spending Accounts, coverage will be effective as of the
first day of employment, subject to Evidence of Insurability requirements for Life and Accidental Death and
Dismemberment coverage.
Your contributions for medical, dental and vision coverage will be made on an after-tax basis for the first 90
days of your employment. Contributions will be made on a pre-tax basis starting on the 91
st
day of
employment.
Contributions to Health Savings Accounts and Health and Dependent Care Flexible Accounts will begin on
the 91
st
day. During the first 90 days of employment, contributions to Health Savings Accounts and Health
and Dependent Care Flexible Spending Accounts will not be permitted.
If you are a regular U.S. part-time Corporate Team Member hired on or after October 1, 2024, you are
eligible for the Employee Assistance Program (EAP), following a 90-day waiting period. If you are a regular
U.S. part-time Corporate Team Member hired before October 1, 2024, you are eligible for the Employee
Assistance Program effective October 1, 2024.
If you want Life, Accidental Death and Dismemberment, or Disability coverage, the coverage should be
elected during this 30-day period, which, other than Basic Life Insurance, is paid on an after-tax basis. To
the extent required by applicable tax rules, for the first 90 days of coverage, the cost of Basic Life
Insurance coverage, less amounts paid by the Team Member, will be reported to you on your Form W-2 (“C”
in Box 12) and on your paycheck (under “Group Term Life”). See the “Life Insurance” section in this SPD for
information on how Basic Life Insurance will be taxed at the end of the 90-day period.
When Coverage Begins
Corporate Team Members who are hired full-time are generally eligible for all Benefit Programs upon their
date of hire. Hotel Team Members who are hired full-time are generally eligible for all Benefit Programs
following a 90-day waiting period. Once eligibility requirements have been met, Team Members must enroll
in the Plan within 30 days. If you fail to enroll on time, you may not be able to enroll until the next open
enrollment period.
Variable Hour Team Members (who are not expected to work at least 30 hours per week when hired) are
subject to the Affordable Care Act Provisions as set forth below.
Affordable Care Act Provisions
For purposes of medical coverage only, Hilton will determine full-time status and provide coverage to new
Variable Hour Team Members by using an initial measurement period, a stability period, and an
administrative period.
• “Initial measurement period” is the 11-month period beginning on the new Team Member’s date of
hire.
• “Initial administrative period” is the period starting the day after the initial measurement period ends
and ending on the first day of the month following the month in which the anniversary of the new
Team Member’s date of hire occurs.
• “Initial stability period” is the 12-month period beginning on the first day of the month following the

Participation
6
month in which occurs the anniversary of the Team Member’s date of hire.
New Hire Example: A newly hired Variable Hour Team Member is hired on March 15, 2024. The initial
measurement period runs from March 15, 2024 through February 15, 2025. If the Variable Hour Team
Member averages 30 hours of service per week during this initial measurement period, you will be offered
medical coverage for the initial stability period that runs from April 1, 2025 through March 31, 2026.
On-going Variable Hour Team Members will be measured using a standard measurement period, stability
period and an administrative period.
• “Standard measurement period” is the 12-month period beginning on October 3 and ending on
October 2 of the following year.
• “Standard administrative period” is the period starting the day after the standard measurement
period ends and ending on December 31.
• “Stability period” is the calendar year.
An on-going Variable Hour Team Member is an employee who has been employed for at least one
complete standard measurement period.
On-Going Example: For 2025, the standard measurement period begins on October 3, 2023 and ends on
October 2, 2024. If the Variable Hour Team Member averages 30 hours of service per week during this
initial measurement period, you will be offered medical coverage for the 2025 plan year (January 1, 2025 –
December 31, 2025).
Payroll deductions for your share of the coverage costs will begin as soon as administratively feasible based
on your eligibility date and pay cycle. Your contribution for a pay cycle will not be pro-rated by how many
days of coverage are provided during that pay cycle.
For the Employee Assistance Program (EAP), coverage begins on the first day of work.
In some cases, certain coverages may start earlier or be subject to additional requirements. For the following
coverages, you must be actively at work on the date coverage is scheduled to begin:
• Disability;
• Life Insurance;
• Accidental Death and Dismemberment; and
• Business Travel Accident.
See the sections on individual benefit options for other requirements.
Your Eligible Dependents
Subject to certain limitations, your eligible dependents may also participate in the Plan.
Note: You must be enrolled in a coverage option to enroll your eligible dependents. You cannot enroll your
eligible dependents if you are not enrolled.

Participation
7
Your eligible dependents include your:
• Legal Spouse. Unless you are legally separated, “Spouse” means the individual recognized as your
spouse for federal tax purposes. “Spouse” shall not include an individual legally separated from the
Participant under a decree of divorce or separate maintenance nor shall it include, for purposes of the
Dependent Care Account, an individual who, although married to the Participant, files a separate federal
income tax return, maintains a separate residence during the last six months and does not furnish more
than one-half of the cost of maintaining the principal residence of the qualifying individual.
• Domestic Partner. The Plan defines a domestic partnership as a same-sex or opposite-sex relationship
where:
Each partner is age 18 or older;
Each partner is a U.S. citizen or a U.S. resident alien (not applicable for STD, LTD, Life and AD&D
coverage);
The partners are not blood relatives;
Neither partner is currently, nor have been in the past six (6) months, legally married, or legally
separated from each other or someone else, nor does either partner have another domestic partner
(not applicable for STD, LTD, Life and AD&D coverage);
The partners maintain an intimate, committed relationship of mutual caring and support;
The partners have lived together for at least six (6) months, during which time the partners were not
married to, or legally separated from, each other or someone else before enrollment in any of the
coverages;
The partners do and will continue to have the same principal address indefinitely; and
The partners agree to share basic living expenses during their domestic partnership and will permit
anyone who is owed money in connection with these expenses to collect from either partner.
Generally, domestic partners are not eligible for pre-tax coverage, including coverage under the Health Care
FSA, unless he or she is a dependent for federal income tax purposes. Please see “Domestic Partners: Tax
Implications and Other Information” for more details.
Note: For purposes of the Business Travel Accident program, you and your domestic partner must meet the
above requirements for at least 12 months before your domestic partner may be covered under the Business
Travel Accident program. In addition, proof of the domestic partnership relationship may be required for certain
insured benefits. Please contact the Hilton Benefits Center for more information.
• Children to age 26 (unless otherwise set forth in the applicable benefit option documents), which can
include:
Your natural children;
Your stepchildren or except for Life and AD&D coverage, foster children;
Your legally adopted children (including children placed with you for adoption);
Children of your Domestic Partner who you support and who live with you;
Children who live with you and for whom you are the legal guardian;

Participation
8
A child age 26 or older who, because of a mental or physical disability, lives with you and depends on
you for financial support if the child’s disability occurred before the child attained age 26. For
dependent life insurance and/or Accidental Death and Dismemberment coverage, you must have
purchased coverage before his or her 26th birthday for your dependent to be eligible for coverage; and
A child pursuant to the terms of a Qualified Medical Child Support Order (QMCSO) (excluding child life
and AD&D coverage).
Note: Underlying benefit options may have different dependent eligibility criteria (e.g., the Dependent Care
FSA, Dependent Life Insurance, Accidental Death and Dismemberment Insurance, and Business Travel
Accident Insurance). Please see the dependent eligibility criteria for each section of this SPD for more
information).
If you are a new Team Member eligible for health and welfare benefits who has a child that is already age 26
or older with a mental or physical disability, you may enroll your disabled child for health care coverage if the
child was disabled before age 26.
Proof of Dependent/Disabled Status
From time to time, you will be required to provide documentation as proof of your spouse or dependent’s
eligibility status, including such items as a marriage certificate, birth certificate, adoption papers or affidavit of
domestic partnership. Failure to provide adequate documentation, upon request by the deadline provided in
the requesting documents, may result in termination of coverage for the affected individual(s) without any
coverage extension under COBRA. In addition, coverage of ineligible dependents is in violation of company
policy. Team Members identified as covering ineligible dependents may be subject to legal action and
discontinued from Plan coverage.
A disabled child that is continuing coverage beyond any limiting age while he or she is disabled will be required
to provide proof of a mental or physical disability, including the Social Security Administration Disability Award
Notice, to continue coverage. Contact the Hilton Benefits Center for details.
Qualified Medical Child Support Order (QMCSO)
The Plan also provides medical coverage for your child pursuant to the terms of a Qualified Medical Child
Support Order (QMCSO). A QMCSO is either a National Medical Child Support Notice issued by a state child
support agency or an order or a judgment from a state court or administrative body directing Hilton to cover a
child as your dependent under the Plan for medical coverage. Federal law provides that a QMCSO must meet
certain form and content requirements in order to be valid.
If the Plan receives a valid QMCSO and you do not enroll the dependent child, the custodial parent or state
agency may enroll the affected child. If you have any questions or you would like to receive, free of charge, a
copy of the written procedures for determining whether a QMCSO is valid, please contact the Hilton Benefits
Center.
Dual Coverage
If your spouse, domestic partner or eligible dependent child also works for Hilton and is eligible for health care
coverage and the Health Care and Dependent Care FSAs, then he or she can enroll as a Team Member
under his or her own coverage or as a dependent under your coverage, but not both.

Participation
9
If you and your Spouse or Domestic Partner are both employed by Hilton and eligible to participate in the Plan,
only one of you may enroll your eligible dependent children in the health care benefits. Also, only one of you
may cover your eligible children under the dependent life and Accidental Death and Dismemberment insurance
programs.
Dependent life insurance does not cover dependents who are also regular, full-time Team Members of Hilton.
In that situation, each eligible Team Member is covered as a Team Member under the life insurance program.
On-Site Medical Clinics
Hilton offers an on-site medical clinic at its McLean, VA, and Memphis, TN, locations, which provide certain
medical services on location to non-union Hilton Team Members. Please see the on-site clinic documents for
more details regarding eligibility and services.
The on-site clinic documents can be found at
www.hiltonbenefits.com.

Participation
10
COST OF COVERAGE
The chart below highlights who pays for the benefit coverages and on what basis they are paid. Depending on
the benefit chosen, either Hilton or you may pay for all of the coverage, or you may share the cost of the
coverage with Hilton. In addition, it shows you how you pay for each benefit coverage – on a pre-tax or after-
tax basis.
The benefits marked in the “Employer Pays” column require no enrollment; coverage for those benefits
is provided automatically.
Coverage
Employer Pays
You Pay
You and
Employer Pay
You Pay Pre- or
After-Tax
1
Medical
X
Pre-Tax
Dental
X
Pre-Tax
Vision
X
Pre-Tax
Health Care FSA
X
2
Pre-Tax
Dependent Care FSA
X
Pre-Tax
Employee Assistance
Program
X
N/A
Disability
Basic STD
X
X
3
N/A / After-Tax
STD Buy-up Option
X
After-Tax
LTD
X
After-Tax
Life Insurance
4
Basic
X
N/A
Supplemental
X
After-Tax
Dependent
X
After-Tax
Accident Insurance
AD&D
X
After-Tax
Business Travel
5
X
N/A
Group Legal
5
X
After-Tax
1
Even though the above chart indicates payment on a pre-tax basis, you will be required to pay on an after-tax basis for medical
and prescription drug coverage if you failed to enroll within the required period, but actually enrolled within 30 days after the end of
the required enrollment period. Benefits for Domestic Partners may also be on an after-tax basis. In addition, newly-hired Corporate
Team Members must, within the first 30 days of employment, enroll in the Plan. If coverage is elected by such Corporate Team
Members, medical, dental and vision coverage will be effective as of the first day of employment and paid on an after-tax basis
through the 90
th
day of employment and paid on a pre-tax basis starting on the 91
st
day of employment. During the first 90 days of
employment, contributions to Health Savings Accounts and Health and Dependent Care Flexible Spending Accounts will not be
permitted. All company-provided benefits under the Plan and contributions to Health Savings Account and Health and
Dependent Care Accounts, if elected and as applicable, will start following the end of the 90-day waiting period.
2
Certain Team Members may be eligible for a Company-provided contribution to their Health Care FSA if they elect certain medical
coverage. If you are eligible, this benefit will be reflected on your Confirmation of Enrollment.
3
Some states require employees to pay for state short-term disability coverage. Check with your local Human Resources department.
Enrollment is automatic in these states.
4
Payment of retiree life insurance premiums varies between Hilton and the retiree depending on the terms of the policy at the time
of retirement.
5
These benefits are only available to Non-Variable Hour Team Members.

Participation
{- DRAFT 2018 Hilton Welfare Plan SPD - US (1.25.2018 redlined)pdscomments (2.13.2018).doc; 1} 11
LEGAL02/39422011v2
LEGAL02/39965328v1
Pre-Tax vs. After-Tax
As shown in the chart above, you pay for coverage under certain benefits with pre-tax dollars deducted from
your paycheck each pay period. Using pre-tax dollars reduces your taxable income for federal, Social Security
and (in most cases) state income tax purposes, making more of your paycheck available for you and your
family. Using pre-tax dollars to pay for Plan benefits will not, however, reduce your coverage level for any Plan
benefit that is based on your income (e.g., your coverage level of basic life insurance).
You pay for coverage under other benefits on an after-tax basis. This means that you pay for the cost of
coverage with your already-taxed dollars (your take-home pay). Your after-tax contributions are also deducted
from your paycheck each pay period. IRS rules determine how each benefit you receive is taxed.
If Hilton pays for your life insurance benefits, your coverage is tax-free if your coverage does not exceed $50,000. If
Hilton-provided coverage exceeds $50,000, you are taxed on the cost of the coverage over $50,000, which is
added to your Form W-2 for tax purposes.
Please note that coverage under the Plan is subject to payment of any required contribution unless, in the
case of a child who is eligible for coverage pursuant to a QMCSO, payment of the required contribution is
made by a state agency.
Remember that income tax laws change frequently, and these changes affect different individuals in different
ways.
You are encouraged to consult with your tax advisor regarding any tax consequences of participating
in the Hilton Health and Welfare Plan.
Domestic Partners: Tax Implications and Other Information
If you choose to cover your domestic partner as a dependent under your medical, dental and/or vision
coverage, there are important tax implications related to the cost of coverage you should know. While the Plan
permits a domestic partner to be covered as an eligible dependent, many domestic partners do not qualify as
dependents for federal income tax purposes. If your domestic partner does not qualify as your legal dependent,
you must pay for your domestic partner’s medical, dental and/or vision coverage on a post-tax basis. This
means the value of any medical, dental, and vision coverage that you pay for on a pre-tax basis or that Hilton
provides, will be included in your reportable income and subject to taxes.
Generally, to be a dependent for federal income tax purposes, your domestic partner must live in your home
with you for the full tax year, be in a relationship with you that does not violate local law, be a citizen of the U.S.
or a resident of the U.S. and, for your taxable year, be over 50% supported by you.
If you believe that your domestic partner meets the requirements to be a dependent for federal income tax
purposes such that income should not be imputed to you, please submit to the Hilton Benefits Center a
completed Affidavit of “Dependency” for Tax Purposes. Copies of the Affidavit may be obtained from the Hilton
Benefits Center.
Please note that you must make a similar determination with respect to your domestic partner’s children.
You should check with your tax advisor for assistance in determining whether your domestic partner and/or
their children are tax dependents under federal and/or state law.

Participation
12
ENROLLMENT
When to Enroll
The Plan has four types of enrollment opportunities:
• Initial enrollment: You must enroll before your 91st day of eligible full-time employment if you are a Non-
variable Hour Team Member (see definition above) and during the Administrative Period if you are a Variable
Hour Team Member.
• A newly hired Corporate Team Member must enroll in the Plan within the first 30 days of hire. If
coverage is elected, medical, dental and vision coverage will be effective as of the first day of
employment and paid on an after-tax basis through the 90
th
day of employment. Such coverage will
be paid on a pre-tax basis starting on the 91
st
day of employment. Enrollment in Health Savings
Accounts and Health and Dependent Care Flexible Accounts, as applicable, must be
completed during the first 30 days of hire; however, contributions to Health Savings Accounts and
Health and Dependent Care Flexible Accounts would begin on the 91
st
day. During the first 90 days
of employment, contributions to Health Savings Accounts and Health and Dependent Care Flexible
Spending Accounts will not be permitted. Corporate Team Members must elect Life, Accidental
Death and Dismemberment, and Disability coverage during this 30-day period; however, coverage
will not be effective until the 91
st
day of employment. All company-provided benefits under the Plan
will start following the end of the 90-day waiting period.
• Annual Enrollment: During annual enrollment—you must enroll during the enrollment period designated in
the enrollment materials;
• Changes During the Year: Within 31 days after you have a change in status or experience another event that
allows you to make a mid-year election change (60 days may be allowed for very limited types of events
related to state Medicaid assistance); and
• After-Tax “Grace Period” for Medical Coverage Only: You must enroll within 30 days after the expiration of
certain enrollment periods described below.
How to Enroll
Upon becoming initially eligible and before each annual enrollment, you will receive enrollment information
that will let you know how and when to enroll for coverage. To obtain medical coverage, you will be required
to provide a valid Social Security number for yourself and each dependent that you wish to cover, as well as
the date of birth for each covered person. While a Social Security Number is required for all dependents,
newborns should be enrolled within the first 31 days of birth even if a Social Security number has not been
provided for the child. Upon receipt of the Social Security number, you should input the number into the
system on or before the newborn’s first birthday. If you have additional questions about this process, please
contact the Hilton Benefits Center.
The elections you make will stay in effect until you change them upon an event permitting a mid-year change in
elections or during a subsequent annual enrollment period. If you transfer your employment to a new property
(or if you are a Corporate Team Member and your address/zip code changes and the change impacts your
available benefits), your coverage will be changed to the lowest cost plan offered to Team Members at your
new address/zip code. However, you may be able to select other coverage, if you do so within 30 days of
the address/zip code change. See the “Changing Coverage During the Year” section for information on mid-
year enrollment and changes.

Participation
13
Annual Enrollment
Each fall, the Plan has an enrollment period for benefits for the following Plan year (January 1 – December
31). You must review your annual enrollment materials to know whether you need to take action or not. Every
year can be different. Most annual enrollments are “active,” requiring you to take action and make elections
in order to have coverage. Some annual enrollments are “passive,” meaning some or all of your previous
benefit elections will remain in effect and you will not be required to make elections in order to have coverage.
If you elected Supplemental and Dependent Life Insurance or Supplemental Accidental Death & Dismemberment
Insurance for the prior Plan year, no action is required if you want to continue your current elections for the next
Plan year. If you want to make changes to your elections for the following Plan year, you must take action during
Annual Enrollment, or in accordance with the change in status event rules.
Important! This passive enrollment only applies to Supplemental and Dependent Life Insurance and Accidental
Death & Dismemberment Insurance.
You must make an election for all other coverages for each Plan year in which you wish to participate in
these programs.
Failure to elect coverage during Annual Enrollment will result in no coverage for the next Plan year.
IMPORTANT: For the Health Care and Dependent Day Care FSAs and Health Savings Account (HSA), you will
need to make an election for each Plan year in which you wish to participate in these programs. Your elections
for these FSAs and HSA will not automatically continue from Plan year to Plan year, even if the annual
enrollment is “passive” for other benefits.
During annual enrollment, you may elect coverage under any of the applicable Benefit Programs. The elections
you make during annual enrollment generally take effect on the following January 1, the start of the new Plan
year. See the “Coverage During Absences” section for special rules regarding annual enrollment while on an
unpaid leave of absence.
During annual enrollment, you may have the opportunity to:
• Switch from one medical option or dental option to another (if several options are offered in your location),
add or drop dependents, or decline or add medical (including prescription drug), dental or vision coverage
for the next calendar year.
• With respect to the Health Care and Dependent Care FSAs, enroll for coverage and authorize the amount
you want to deduct from your pay on a pre-tax basis, subject to certain maximums and IRS regulations.
• With respect to income protection—disability, life and accident coverage—you may be able to enroll for
coverage (if not automatically provided) or increase or decrease the level of life insurance coverage for you
or your dependents, subject to certain conditions. Certain other restrictions may apply. Please see the
“Disability” and “Life and Accident” sections of this SPD for further details.

Participation
14
If you are on a leave of absence at the time of annual enrollment, your elections may be affected. Please see
the “Paid and Unpaid Absences” section of this SPD for further details.
Special Exception When Adding Dependent(s) Does Not Affect Premium
If you select family medical coverage during annual enrollment but mistakenly fail to include one or more of
your dependents, you may add such dependent(s) to coverage, on a prospective basis only. In order for
this exception to apply, adding such dependent(s) cannot cause an increase in your premium. No other
changes are permitted in this circumstance, unless you experience one of the enumerated change in
status events.
Medical Coverage Enrollment – After-Tax Basis
If you miss the deadline to enroll for medical coverage upon your initial eligibility or due to a mid-year event
that allows you to change or enroll for medical coverage, you may still enroll for medical coverage only during
the 30-day period that begins on the day immediately after your applicable enrollment period expires. Any
enrollment during this additional 30-day period will be on an after-tax basis. You must contact the Hilton
Benefits Center to enroll for coverage during this period. You will not be able to enroll electronically. If you
timely enroll during this “grace period”, coverage will be effective on the day immediately following your
enrollment.
Special Circumstances: Re-employment
If you leave Hilton and subsequently return to Hilton, the following rules will apply:
• You are a Variable Hour Employee: if you are reemployed less than 13 weeks following your employment
termination, you will be treated as if your employment did not terminate and you will be offered the same
coverage upon your return.
• You are a non-Variable Hour Employee: if you are reemployed less than 24 months following your
employment termination, you will be treated as if your employment did not terminate, and you will be
offered the same coverage upon your return.
• If you are rehired within 30 days and within the same year, your prior elections will be reinstated if you are
rehired into a benefits eligible position, but if you are rehired more than 30 days after you terminate, you
will be eligible to make new elections. If you are rehired within 30 days of termination, but a new Plan
year has begun, you will need to make new coverage elections.
If you terminate and are rehired in the same year, special rules will apply to reimbursements from your Health
Care Flexible Spending Account. For more information, see “How Your Flexible Spending Accounts Work” in
the “Flexible Spending Accounts” section of this SPD.
Changing Coverage During the Year
As a general rule, the elections you make when you first enroll in the Plan will remain in place for the
remainder of the Plan year. The elections you make during the regular Annual Enrollment will remain in place

Participation
15
for the next Plan year. If you do not enroll in coverage for the next Plan year, you will default to no
coverage because your elections do not roll over.
Note!
If you complete new hire enrollment or change your current elections in connection with a Change
in Status event…
After the first day of Annual Enrollment, your elections will be carried over to the next Plan Year. You do
not need to enroll again for the next Plan year.
Example: You are hired in September 2023 and enroll in coverage for the 2023 Plan year in
December 2023. Your elections will apply to 2023 and 2024 plan year coverage.
Before the first day of Annual Enrollment, your elections will not carry over to the next Plan year. You
must enroll for coverage during Annual Enrollment if you want coverage for the following Plan year.
Example: You are hired in June 2023 and enroll in coverage for the 2023 Plan year in September
2023. Your elections will only apply to 2023 coverage. If you do not enroll for 2024 coverage during
Annual Enrollment, you will have no coverage in 2024
You will be allowed to change your elections during the Plan year only if you or your dependent experiences a
qualified Change in Status event.
A Qualified “Change in Status” is any event for which Federal law allows you to make a mid-year election
change, unless this SPD specifies that the event does not allow you to change your elections under the Plan.
The following are some common Qualified Change in Status events:
• Your marriage, divorce, or annulment;
• Your declaration of a new, or dissolution of, an existing domestic partnership;
• Birth, adoption, placement for adoption or appointment of legal guardianship of a child.
• Note: New dependent children are not automatically covered even if you are enrolled in You +
Child(ren) or You + Family coverage;
• The death of your covered dependent;
• Your eligible dependent’s loss or gain of employment;
• You or your eligible dependent’s switch from a full-time to a part-time or a part-time to a full-time work
schedule;
• A change in your dependent’s eligibility;
• A change in you or your eligible dependent’s place of residence or work;

Participation
16
• You or your eligible dependent’s eligibility for Medicare or Medicaid;
• The addition or elimination of a Program Benefit coverage option;
• Your requirement to cover your eligible dependent child(ren) according to a judgment, decree or order.
If you experience a Qualified Change in Status and want to change any of your elections, you must notify
the Hilton Benefits Center and make your election changes within 31 days of the event (60 days for a loss of
eligibility for Medicaid or State Child Health Plan or a gain of eligibility for premium assistance under Medicaid or
State Child Health Plan)
The chart on the next page is intended to provide general guidance on when you may make changes to your
Benefits Program elections. This chart does not attempt to address every circumstance under which your
elections may be changed.
The Plan Administrator, in its sole discretion, shall determine whether an event permits an election change and, if
so, whether the election change is consistent with the event, in accordance with rules established by the Internal
Revenue Service or applicable law.
Important! In all circumstances, any changes to your elections must be consistent with the qualified Change in
Status event that you have experienced and must be reported within 31 days from the date of the Change in
Status (60 days in the case of loss of eligibility for Medicaid or CHIP or gain eligibility for premium assistance).
If you do not make your elections within 31 days, you will not be permitted to make any changes until the next
Annual Enrollment period or you experience another qualified Change in Status event.
Note: If you move, your medical or dental coverage options may change as a result of a change in your
address/zip code. In these instances, your coverage will automatically be changed to the most similar medical
or dental coverage option available at your new address/zip code. However, you may be able to select other
coverage, if you do so within 31 days of the address/zip code change. If you have any questions about how
your move may impact your medical and/or dental coverage options, please contact the Hilton Benefits Center
for more information.

Participation
17
Allowable Mid-Year Change Events
The following chart provides general guidance on when you may make changes to your Benefits Program
elections and does not address every circumstance under which your elections may be changed. As noted
above, the Plan Administrator reserves the right to determine whether an election change is permitted and
consider other events recognized by the Internal Revenue Service.
In addition, enrollment or changes in the disability and life coverages may be subject to additional EOI
requirements. Please contact the insurance carrier for more information on permitted changes.
Employment Change Events
Qualified Change
in Status Event
Medical/Dental/Vision
Healthcare FSA
Dependent Care FSA
Termination of
employment,
including failure to
return from a leave
of absence
Coverage ends on the
last day of your
employment. You may
maintain coverage for
yourself and/or your
covered eligible
dependents through
COBRA Continuation
Coverage.
Coverage ends on
the last day of your
employment. You
may continue
contributing to your
flexible spending
account after-tax for
the remainder of the
Plan Year through
Continuation
Coverage.
Coverage ends on the day your
employment ends.
Begin an unpaid
leave of absence
(health, military, etc.)
You may drop coverage
for yourself and/or
eligible dependents
Contributions will be
suspended until you
return to work (if
returning in the
same plan year)
Contributions will be suspended
until you return to work (if
returning in the same plan year)
Return from an
approved unpaid
leave of absence
(health, military etc.)
If you dropped
coverage as a result of
your leave of absence,
you may enroll yourself
and your eligible
dependents in coverage
You may enroll for or
increase
contributions to your
reimbursement
account
You may enroll for or increase
contributions to your
reimbursement account.
You gain eligibility
for another
employer's plan
(e.g., You work two
jobs and becomes
eligible for coverage
through the second
employer)
Drop Coverage
No change allowed
Increase/start spending account
contributions
Decrease/drop spending
account contributions
(permissible if gaining eligibility
results in significant change in
cost/coverage for dependent
care)
You lose eligibility
for coverage under
another employer's
plan (e.g., You work
two jobs and
becomes ineligible
for coverage through
You may enroll yourself
and your eligible
dependents
No change allowed
Increase/start spending account
contributions

Participation
18
the second
employer)
Family Change/Life Events
Qualified Status
Change Event
Medical/Dental/Vision
Healthcare FSA
Dependent Care FSA
Marriage/Gain of
Domestic Partner
(DP)
Enroll
Drop coverage (TM
and eligible
dependents)
Add spouse/DP
Add any eligible
dependent
Change option
Increase/start
spending account
contributions
Decrease/drop
spending account
contributions
Increase/start spending account
contributions
Decrease/drop spending
account contributions
Divorce/Legal
Separation/Dissoluti
on of Domestic
Partnership (DP)
Enroll
You must remove your
former spouse/DP
Add dependent(s) who
lose coverage under
the domestic partner's
plan
You must remove your
former spouse/DP’s
dependent(s)
Change option
Increase/start
spending account
contributions
Decrease/drop
spending account
contributions
Increase/start spending account
contributions
Decrease/drop spending
account contributions
Birth, Adoption, or
placement for
adoption of a child
Enroll
Add any eligible
dependent(s)
Drop coverage
Change option
Increase/start
spending account
contributions
Decrease/drop
spending account
contributions
Increase/start spending account
contributions
Decrease/drop spending
account contributions
Death of dependent
or dependent loss of
eligibility, (e.g. loss
of legal guardianship
or foster child)
You must remove your
deceased or ineligible
dependent
Decrease/drop
spending account
contributions
Decrease/drop spending
account contributions
Death of Spouse or
You must drop your
Increase/start
Increase/start spending account
Participation
19
Qualified Status
Change Event
Medical/Dental/Vision
Healthcare FSA
Dependent Care FSA
Domestic Partner
deceased Spouse/
Domestic Partner
You may enroll yourself
and eligible
dependents
Change option
spending account
contributions
Decrease/drop
spending account
contributions
contributions
Judgment, decree,
or court order (e.g.,
QMCSO) requiring
you to provide
health coverage for
dependent(s)
Enroll
Add newly eligible
dependent only
Increase/start
spending account
contributions
No change allowed
Judgment, decree,
or court order (e.g.,
QMCSO) requiring
spouse to provide
health coverage for
dependents and
coverage is actually
provided
Drop affected
dependent only
Decrease/drop
spending account
contributions
No change allowed
You or your eligible
dependent exhausts
COBRA continuation
coverage under
another plan
Enroll
Add affected
spouse/dependent(s)
Change option
Increase or start
contributions
No change allowed
You or your eligible
dependent
experiences a
significant change in
cost of coverage
You may enroll or
remove yourself and
your impacted eligible
dependents from
coverage impacted by
the cost change.
No change allowed
Increase or add spending
account, Decrease or drop
spending account only if the
cost change is imposed by a
dependent care provider who is
not your relative.
Addition of benefit
option to spouse's or
eligible dependent's
plan
You may drop
coverage for yourself
and your eligible
dependents
No change allowed
No change allowed
Your or your eligible
dependent(s) lose
Enroll yourself and
eligible dependents
No change allowed
No change allowed
Participation
20
Qualified Status
Change Event
Medical/Dental/Vision
Healthcare FSA
Dependent Care FSA
other governmental
or educational
institution coverage
such as tribal
coverage, state
health benefit risk
pool, or foreign
government plan
Change option (e.g.,
PPO to HMO)
Your spouse or
eligible dependent
gains other
coverage (changes
employment status,
returns from an
unpaid leave of
absence, or obtains
a new job)
Drop coverage
Drop affected spouse
Drop affected
dependent(s)
Decrease/drop
spending account
contributions
Increase/start spending account
contributions
Decrease/stop spending
account contributions
If this change involves your
spouse getting a new job
Your spouse or
eligible dependent
loses benefit
coverage in another
plan (changes
employment status,
goes an unpaid
leave of absence,
goes on strike etc.)
You may enroll yourself
and/ or your eligible
dependents
Change option
Increase/start
spending account
contributions
Increase/start spending account
contributions
Decrease/drop spending
account contributions
So long as changes are
consistent with the change in
employment event
Your spouse or
eligible dependent’s
annual enrollment
period differs from
yours and the period
of coverage is not a
calendar year
You may enroll yourself
and/or your eligible
dependents
Drop coverage (if being
added to spouse's
plan)
No change allowed
No change allowed
Your or your spouse
or eligible
dependent gains
entitlement to
Medicare or
Medicaid or financial
assistance under
CHIP
You may drop
coverage for yourself
and affected
spouse/eligible
dependent(s)
Decrease/drop
spending account
contributions
No change allowed

Participation
21
Effective Date of Coverage
If timely made, coverage changes made due to a Change in Status are generally effective on the date of
Change in Status.
Note: If you do not make a timely election, you will not be able to make election changes until annual enrollment
(or a subsequent election change event).
The Plan reserves the right to require, at any time, appropriate documentation of your change in status or
other event.
Important Notes Regarding Mid-Year Election Changes
If you experience a change in status that allows you to decrease your Health Care FSA contributions, you
cannot make an election change that will result in decreasing your annual contribution amount below what
you have already contributed through the date the change will become effective. For example, if you elect
an annual contribution amount of $1,000 and have contributed $600, you cannot elect to decrease your
annual contribution amount to $500.
For changes in status resulting in either you or a dependent becoming ineligible, coverage automatically
ends as of the event resulting in your or your dependent’s ineligibility (except that health coverage extends
through the end of the month for dependents losing eligibility due to reaching age 26). The mid-year election
change will stop the premium deduction that relates to the cost of coverage.
If you become divorced or legally separated or a dependent child is no longer eligible for coverage, your
spouse or child will lose eligibility for medical coverage under the Plan on the day the event occurs (except
that coverage extends through the end of the month for dependents losing eligibility due to reaching age 26).
Please see “Medical Coverage Continuation Rights (COBRA)” later in this section for more information
on COBRA for such individuals.
Even if your spouse or dependent does not have a Social Security number at the time of the mid-year
change, you must contact the Hilton Benefits Center to make your election changes within the required
time frame,. You must provide the Social Security number of your spouse and dependent, as applicable, in
accordance with the instructions provided by the Hilton Benefits Center.

Participation
22
LEGAL02/39965328v1
Paid and Unpaid Absences
As noted above, the beginning of an unpaid absence is a change in status permitting election changes. To assist
you in determining whether your furlough or leave of absence is paid or unpaid, triggering your right to make an
election change, the following chart identifies which leaves of absences or furlough periods (sometimes
referred to as an “LOA” or “Furlough”) will be considered paid and unpaid.
Paid Absence
1
Unpaid Absence
Family and Medical Leave Act (FMLA) plus paid
time off
Sick leave
Bereavement
Jury duty
Leave subject to salary continuation
2
Involuntary military leave with pay differential
3
Furlough
FMLA and no other income source
FMLA and basic STD, buy-up and/or state
mandated disability pay
Non-FMLA medical leave without salary
continuation
STD with basic STD, buy-up and/or state
mandated disability pay
Personal leave of absence and no other income
source
Voluntary military leave
3
Furlough
1
If any of these paid LOAs become unpaid, election changes may be made.
2
The Salary Continuation Program is available to corporate Team Members only.
3
Continuation of elective disability, life insurance and AD&D coverages are subject to the terms of insurance policies and Hilton’s
military leave policy and may not continue during a military leave. Please contact the Hilton Benefits Center for details.
Coverage During Unpaid Leave of Absences and Paid or Unpaid Furloughs
In the event you qualify for an unpaid leave of absence under Hilton’s leave of absence policy (like an FMLA
leave or personal leave) or are on a paid or unpaid furlough, the following describes how your coverages may
be impacted during your LOA or Furlough and what happens when you return from a LOA or Furlough.
Continue to Participate
in All or Some of Your
Coverages For the
Same Plan Year
The coverages in effect when you begin your LOA or Furlough will automatically continue
during your LOA or Furlough, provided any required contributions are timely made.
You
will be directly billed for coverage provided during your LOA or Furlough and will pay for
your coverages with after-tax dollars.
1
As discussed in the Flexible Spending Accounts
section, any Smart Choice Card will be suspended during an unpaid LOA or Furlough. In
addition, for an unpaid LOA or paid or unpaid Furlough you can choose to terminate any
dependent child care election and spend down any remaining contributions for eligible
expenses incurred while on leave.
If you return from a LOA or Furlough and payment for coverage received during your LOA
or Furlough is not received after the 30-day grace period for the second billing period
expires, coverage will terminate retroactively to the beginning of the period for which
payment was not made. If coverage terminates and you incur services during that period,
your services will not be covered.
Terminate All or Some
of Your Coverages
You may choose to terminate your participation in any of your coverages, as long as you
make a timely election within 31 days of the beginning of your approved LOA or Furlough

Participation
23
by notifying the Hilton Benefits Center. You must make election changes via YBR or by
calling the Hilton Benefits Center if you wish to continue some, but not all, of your
coverages during your LOA or Furlough. If you send payment for some, but not all, of
your coverages without first dropping the coverages for which payment is not remitted,
you will lose ALL coverage.
Return From LOA in
Same Plan Year
When you return from a LOA or Furlough in the same Plan Year, you will be enrolled in
the following coverage:
- any coverage in effect at the time of your return will continue upon your return at the
same level unless you choose to drop ALL coverages within 31 days of your date of
return.
2
- If your coverage dropped due to nonpayment during your LOA or Furlough, the
elections in place at the time your LOA or Furlough began (for life and AD&D
coverage, subject to evidence of insurability requirements).
3
When you return from a LOA or Furlough, your payroll withholding will begin for the
coverage in effect after your return. However, you must also make payment on an after-
tax basis for the portion of the month before your return if you continued your coverage
through the end of the preceding month. Failure to remit that amount by the end of the
applicable grace period will result in loss of coverage for the portion of the month before
your return from LOA/FURLOUGH. If you do not pay for the portion of the month before
your return by the end of the applicable grace period, you will have a gap in coverage
and services incurred during that period will not be covered. If you have questions about
the payment due, you should contact the Hilton Benefits Center for details.
If annual enrollment occurs during your LOA or Furlough, your coverage may be affected
as described below.
Exceptions apply for the FSAs—please see the “Flexible Spending Accounts” section for
more information.
Annual Enrollment
During a LOA/Furlough
and Return From a
LOA/Furlough in
Different Plan Year
If the annual enrollment period occurs while you are on a LOA or Furlough, you will be
sent annual enrollment information and may make election decisions for the upcoming
Plan year. It is your responsibility to ensure that Hilton has the most updated information
for you during your LOA or Furlough period. If you fail to provide your contact information,
Hilton will not be responsible for any consequences that may result from your failure to
receive annual enrollment information. Any new elections for disability, life and accident
coverages will be delayed until you return to work as an eligible Team Member or until
you satisfy any required EOI, whichever is later.
The elections you make during annual enrollment may or may not take effect in the
following year as described below:
- Your annual enrollment elections will become effective on the next January 1
st
,
provided:
- you timely pay for your benefits for all months between annual enrollment and
January 1
st
and for the January following annual enrollment,
- your coverage was dropped for nonpayment before annual enrollment but you
timely pay for the benefits elected during annual enrollment in January, or
- you elect or default to no coverage following annual enrollment.
- Your annual enrollment elections will NOT become effective on the next January 1
st
or thereafter, if:
- Your coverage is dropped for nonpayment between annual enrollment and
January 1
st
, or
- Your coverage is dropped for nonpayment of the January contribution amount.
However, you will not be allowed to add or increase the amount of your life, AD&D or
disability coverages while you are on a LOA or Furlough. You must return to active work
before you can elect to increase your coverage amounts.
Participation
24
If you are eligible for annual enrollment but do not make any election changes or if your
annual enrollment elections do not become effective under the rules above, your elections
in effect at the time your LOA or Furlough began will be reinstated upon return from LOA
or Furlough (except for the Health Care and Dependent Day Care FSAs).
Health Care and Dependent Care FSA elections must be made within 31 days of your
return from LOA/Furlough.
Other Mid-Year Events
If you also experience another event permitting a mid-year change in coverage during
your LOA or Furlough period, such as a change in status and/or a HIPAA special
enrollment event (discussed below), you may change your coverages in accordance with
the rules for that event.
Unpaid Military Leave
Keep in mind that, subject to the terms of the underlying insurance policies, coverage
(and your obligation to pay for coverage) will continue unless you drop coverage. If your
coverage is no longer needed you must drop coverage as described above. If you
continue coverage and later experience another event permitting a mid-year change in
coverage during your leave, such as a change in status and/or a HIPAA special
enrollment event (discussed below), you may change your coverages in accordance with
the rules for that event. For more information regarding your rights under USERRA,
please contact the Hilton Benefits Center.
1
You must make election changes via YBR or by calling the Hilton Benefits Center if you wish to continue some, but not all,
of your coverages during your LOA or Furlough period. If you send payment for some, but not all, of your coverages without
first dropping the coverages for which payment is not remitted, you will lose ALL coverage.
2
When you return from a leave of absence, your payroll withholding will begin for the coverage in effect after your return.
However, you must also make payment on an after-tax basis for the portion of the month before your return. Failure to remit
that amount by the end of the applicable grace period will result in loss of coverage for the period before your return from
LOA/FURLOUGH. If you have questions about the payment due, you should contact the Hilton Benefits Center for details.
3
If the coverage you had when you started your LOA or Furlough is no longer offered, you will be enrolled in the coverage
deemed closest to your prior coverage. If you wish to elect different coverage, you must notify the Hilton Benefits Center
within 31 days of your return from your LOA or Furlough to make the change.
WHEN COVERAGE ENDS
Your Coverages
Your coverages end upon the first of the following to occur:
• Your employment with Hilton ends (e.g., you retire, quit or are terminated);
• You are no longer eligible to participate in the Plan (e.g., you do not work, on average, 30 hours per
week);
• You fail to timely pay your required contributions;
• You elect to terminate coverage;
• You go out on strike or are locked out;
• You knowingly make, or cause or permit to be made, false statements in order for you or another person
to obtain Plan services or payment to which you or the other person are not entitled;

Participation
25
• Hilton terminates the Plan or a Benefit Program in whole or in part; or
• Hilton terminates coverages for the eligible class to which you belong.
Termination of your coverages will be effective on the day the triggering event occurs. For example, if your
employment with Hilton ends on May 17, your coverages will end on that same day. As of May 18, you do
not have coverage, subject to your COBRA and life insurance conversion or continuation rights.
Your Dependent’s Coverage
Your dependent’s coverage ends upon the first of the following to occur:
• You fail to submit requested documentation of dependent status in connection with a dependent
coverage verification;
• When your coverage ends; or
• Your dependent no longer meets the eligibility requirements.
Termination of coverage due to attaining age 26 is effective on the last day of the month that includes the
dependent’s 26
th
birthday.
If you intend to leave Hilton, be sure to check with the Hilton Benefits Center about your benefit status as
soon as possible. In addition, you or your dependent may be able to elect COBRA coverage for continued
medical, dental or vision coverage after coverage ends or you may convert certain life insurance coverages to
individual policies if you no longer qualify for group coverage through the Plan.

26
ADMINISTRATION
COORDINATION OF BENEFITS- WHEN YOU HAVE ADDITIONAL
MEDICAL, PRESCRIPTION, OR DENTAL COVERAGE.............................. 27
RECOVERY FOR OVERPAYMENT, SUBROGATION AND
REIMBURSEMENT ........................................................................................ 31
LIFE INSURANCE AFTER YOU LEAVE ....................................................... 35
HEALTH CARE COVERAGE CONTINUATION RIGHTS (COBRA) ............ 35
COBRA .................................................................................................... 35
When to Elect COBRA ............................................................................ 36
Reporting a Qualifying Event .................................................................. 36
Snapshot of COBRA Coverage............................................................... 37
Deciding Whether or Not to Continue Coverage and
Payment of COBRA Premium ................................................................. 38
When Continuation Coverage Ends ........................................................ 38
COBRA Coverage for Disabilities ........................................................... 38
Health Care Flexible Spending Account ................................................. 39
Administration of COBRA ........................................................................ 39
ADMINISTRATION

Administration
27
COORDINATION OF BENEFITS- WHEN YOU HAVE ADDITIONAL MEDICAL,
PRESCRIPTION, OR DENTAL COVERAGE
The following Coordination of Benefits (COB) rules are intended to supplement any COB provisions contained in
the applicable Program Document(s). These rules and the Program Documents should be read together, but in
the event of a conflict the terms of the Program Document(s) will govern.
This COB provision applies when you have health care coverage under more than one plan. Spouses who have
primary insurance with another carrier (other than a government program) are not eligible for medical coverage
under the Plan.
Please note that several terms specific to this provision are listed below. Some of these terms have different
meanings in other parts of the SPD, e.g., Plan. For this provision only, “Plan” will have the meanings as
specified below.
The order of benefit determination rules determine the order in which each Plan will pay a claim for benefits.
The Plan that pays first is called the Primary Plan. The Primary Plan must pay benefits according to its policy
terms regardless of the possibility that another Plan may cover some expenses. The Plan that pays after the
Primary Plan is the Secondary Plan. The Secondary Plan may reduce the benefits it pays so that payments
from all Plans do not exceed 100% of the total Allowable expense.
The Allowable expense under COB is generally the higher of the Primary and Secondary Plans’ allowable
amounts. A Network provider can bill you for any remaining coinsurance and/or deductible under the higher of
the Plans’ allowable amounts. This higher allowable amount may be more than the Plan’s maximum allowable
amount.
COB Definitions
Plan is any of the following that provides benefits or services for medical or dental care or treatment. If separate
contracts are used to provide coordinated coverage for members of a group, the separate contracts are
considered parts of the same Plan and there is no COB among those separate contracts.
1. Plan includes: Group and non group Program Documents; health maintenance organization (HMO)
contracts; uninsured arrangements of group or group-type coverage; coverage under group or non group
closed panel plans; group-type contracts; medical care components of long term care contracts, such as
skilled nursing care; medical benefits under group or individual automobile contracts (whether “fault” or “no
fault”); other governmental benefits, except for Medicare, Medicaid or a government plan that, by law,
provides benefits that are in excess of those of any private insurance plan or other nongovernmental plan.
2. Plan does not include: Accident only coverage; Specified disease or specified accident coverage; limited
health benefit coverage; benefits for non-medical components of long term care policies; hospital indemnity
coverage benefits or other fixed indemnity coverage; school accident-type coverages covering grammar,
high school, and college students for accidents only, including athletic injuries, either on a twenty-four (24)
hour or “to and from school” basis; and Medicare supplement policies.
Each contract for coverage under items 1. or 2. above is a separate Plan. If a Plan has two parts and COB rules
apply only to one of the two, each of the parts is treated as a separate Plan.
This Plan means the part of the contract providing health care benefits that the COB provision applies to and
which may be reduced because of the benefits of other plans. Any other part of the contract providing health
care benefits is separate from This Plan. A contract may apply one COB provision to certain benefits, such as
dental benefits, coordinating only with similar benefits, and may apply another COB provision to coordinate other
benefits.
The order of benefit determination rules determine whether This Plan is a primary plan or secondary plan when
you have health care coverage under more than one Plan.
When This Plan is primary, it determines payment for its benefits first before those of any other Plan without
considering any other Plan’s benefits. When This Plan is secondary, it determines its benefits after those of
another Plan and may reduce the benefits it pays so that all Plan benefits do not exceed 100% of the total

Administration
28
Allowable expense.
Allowable expense is a health care expense, including deductibles and coinsurance, that is covered at least in
part by any Plan covering you. When a Plan provides benefits in the form of services, the reasonable cash
value of each service will be considered an Allowable expense and a benefit paid. An expense that is not
covered by any Plan covering you is not an Allowable expense. In addition, any expense that a provider by law
or in accordance with a contractual agreement is prohibited from charging you is not an Allowable expense;
however, if a provider has a contractual agreement with both the Primary and Secondary Plans, then the higher
of the contracted fees is the Allowable expense, and the provider may charge up to the higher contracted fee.
The following are not Allowable expenses:
1. The difference between the cost of a semi-private Hospital room and a private Hospital room is not an
Allowable expense, unless one of the Plans provides coverage for private Hospital room expenses.
2. If you are covered by 2 or more Plans that calculate their benefit payments on the basis of usual and
customary fees or relative value schedule reimbursement method or other similar reimbursement methods,
any amount in excess of the highest reimbursement amount for a specific benefit is not an Allowable
expense.
3. If you are covered by 2 or more Plans that provide benefits or services on the basis of negotiated fees, an
amount in excess of the highest of the negotiated fees is not an Allowable expense.
4. If you are covered by one Plan that calculates its benefits or services on the basis of usual and customary
fees or relative value schedule reimbursement method or other similar reimbursement method and another
Plan that provides its benefits or services on the basis of negotiated fees, the primary plan’s payment
arrangement will be the Allowable expense for all Plans. However, if the provider has contracted with the
Secondary Plan to provide the benefit or service for a specific negotiated fee or payment amount that is
different than the primary plan’s payment arrangement and if the provider’s contract permits, the negotiated
fee or payment will be the Allowable expense used by the secondary plan to determine its benefits.
5. The amount of any benefit reduction by the primary plan because you have failed to comply with the Plan
provisions is not an Allowable expense. Examples of these types of Plan provisions include second surgical
opinions, precertification of admissions or services, and network provider arrangements.
6. The amount that is subject to the primary high-deductible health plan’s deductible, if the Claims
Administrator has been advised by you that all Plans covering you are high-deductible health plans and you
intend to contribute to a health savings account established in accordance with Section 223 of the Internal
Revenue Code of 1986.
Closed panel plan is a Plan that provides health care benefits primarily in the form of services through a panel
of providers that contract with or are employed by the Plan, and that excludes coverage for services provided by
other providers, except in cases of emergency or referral by a panel member.
Custodial parent is the parent awarded custody by a court decree or, in the absence of a court decree, is the
parent with whom the child resides more than one half of the calendar year excluding any temporary visitation.
Order of Benefit Determination Rules
When you are covered by two or more Plans, the rules for determining the order of benefit payments are:
The primary plan pays or provides its benefits according to its terms of coverage and without regard to the
benefits under any other Plan.
1. Except as provided in Paragraph 2. below, a Plan that does not contain a coordination of benefits provision
that is consistent with this COB provision is always primary unless the provisions of both Plans state that the
complying Plan is primary.
2. Coverage that is obtained by virtue of membership in a group that is designed to supplement a part of a
basic package of benefits and provides that this supplementary coverage will be excess to any other parts
of the Plan provided by the contract holder. Examples of these types of situations are major medical
coverages that are placed over base plan Hospital and surgical benefits, and insurance type coverages that
are written in connection with a closed panel plan to provide out-of-network benefits.

Administration
29
A Plan may consider the benefits paid or provided by another Plan in calculating payment of its benefits only
when it is secondary to that other Plan.
Each Plan determines its order of benefits using the first of the following rules that apply:
Rule 1 – Non-Dependent or Dependent. The Plan that covers you as an employee or retiree is the primary plan,
and the Plan that covers you as a dependent is the secondary plan. However, if you are a Medicare beneficiary
and, as a result of federal law, Medicare is secondary to the Plan covering you as a dependent and primary to
the Plan covering you as other than a dependent (e.g., a retired Employee), then the order of benefits between
the two Plans is reversed so that the Plan covering you as an Employee or retiree is the secondary plan and the
other Plan covering you as a dependent is the primary plan.
Rule 2 – Dependent Child Covered Under More Than One Plan. Unless there is a court decree stating
otherwise, when a dependent child is covered by more than one Plan the order of benefits is determined as
follows:
1. For a dependent child whose parents are married or are living together, whether or not they have ever been
married:
• the Plan of the parent whose birthday falls earlier in the calendar year is the primary plan; or
• if both parents have the same birthday, the Plan that has covered the parent the longest is the primary
plan.
2. For a dependent child whose parents are divorced or separated or not living together, whether or not they
have ever been married:
• If a court decree states that one of the parents is responsible for the dependent child’s health care
expenses or health care coverage and the Plan of that parent has actual knowledge of those terms, that
Plan is primary. This rule applies to plan years commencing after the Plan is given notice of the court
decree;
• If a court decree states that both parents are responsible for the dependent child’s health care
expenses or health care coverage, the provisions of 1. above will determine the order of benefits;
• If a court decree states that the parents have joint custody without specifying that one parent has
responsibility for the health care expenses or health care coverage of the dependent child, the
provisions of 1. above will determine the order of benefits; or
• If there is no court decree assigning responsibility for the dependent child’s health care expenses or
health care coverage, the order of benefits for the child are as follows:
- The Plan covering the Custodial parent;
- The Plan covering the spouse of the Custodial parent;
- The Plan covering the non-custodial parent; and then
- The Plan covering the spouse of the non-custodial parent.
3. For a dependent child covered under more than one Plan of individuals who are not the parents of the child,
the provisions of item 1. above will determine the order of benefits as if those individuals were the parents of
the child.
4. For a dependent child covered as a child of an employee and also covered as a spouse under the
dependent’s spouse’s plan, the plan that has covered the dependent for the longest period of time is
Primary.
Rule 3 – Active Employee or Retired or Laid-off Employee. The Plan that covers you as an active employee, that
is, an employee who is neither laid off nor retired, is the primary plan. The Plan also covering you as a retired or
laid-off employee is the secondary plan. The same would hold true if you are a dependent of an active
employee and you are a dependent of a retired or laid-off employee. If the other Plan does not have this rule,
and as a result, the Plans do not agree on the order of benefits, this rule is ignored. This rule does not apply if
“Rule 1 - Non-Dependent or Dependent” can determine the order of benefits.
Rule 4 – COBRA. If you are covered under COBRA or under a right of continuation provided by other federal law
and are covered under another Plan, the Plan covering you as an employee, Member, Subscriber or retiree or
covering you as a dependent of an employee, member, subscriber or retiree is the primary plan and the COBRA
or other federal continuation coverage is the secondary plan. If the other Plan does not have this rule, and as a
result, the Plans do not agree on the order of benefits, this rule is ignored. This rule does not apply if “Rule 1 -
Non-Dependent or Dependent” can determine the order of benefits. This rule does not apply when the person is
Administration
30
covered either: (a) as a non- dependent under both Plans (i.e. the person is covered under a right of
continuation as a qualified beneficiary who, on the day before a qualifying event, was covered under the group
health plan as an employee or as a retired employee and is covered under his or her own Plan as an employee,
member, subscriber or retiree); or (b) as a dependent under both plans (i.e. the person is covered under a right
of continuation as a qualified beneficiary who, on the day before a qualifying event, was covered under the
group health plan as a dependent of an employee, member or subscriber or retired employee and is covered
under the other plan as a dependent of an employee, member, subscriber or retiree). If Medicare coverage is in
effect prior to the COBRA coverage effective date, COBRA coverage can continue for up to 18 months. If
Medicare coverage goes into effect after the COBRA coverage effective date, COBRA coverage will terminate.
Rule 5 – Longer or Shorter Length of Coverage. The Plan that covered you longer is the primary plan and the
Plan that covered you the shorter period of time is the secondary plan.
Rule 6 – If the preceding rules do not determine the order of benefits, the Allowable expenses will be shared
equally between the Plans meeting the definition of Plan. In addition, This Plan will not pay more than it would
have paid had it been the primary plan.
Effect On The Benefits of This Plan
When a member is covered under two or more Plans which together pay more than this Plan’s benefits, the Plan
will pay this Plan’s benefits according to the Order of Benefit Determination Rules. This Plan’s benefit payments
will not be affected when it is primary. However, when this Plan is secondary under the Order of Benefit
Determination Rules, benefits payable by this Plan will be reduced by the combined benefits of all other Plans
covering you or your dependent.
When the benefits of this Plan are reduced, each benefit is reduced in proportion. It is then charged against any
applicable benefit limit of this Plan. If this Plan is secondary, the combined benefits of this Plan and the other
Plan will never exceed what would have been provided by this Plan if primary. No benefits will be provided by
this Plan when the amount paid by the other Plan is equal to or greater than the amount this Plan would have
paid if Primary.
If you are enrolled in two or more closed panel plans and if, for any reason, including the provision of service by
a non-panel provider, benefits are not payable by one closed panel plan, COB will not apply between that Plan
and other closed panel plans.
Right to Receive and Release Needed Information
Certain facts about health care coverage and services are needed to apply these COB rules and to determine
benefits payable under This Plan and other Plans. The Claims Administrator may get the facts it needs from or
give them to other organizations or persons for the purpose of applying these rules and determining benefits
payable under This Plan and other Plans covering the person claiming benefits. The Claims Administrator need
not tell, or get the consent of, any person to do this. Each person claiming benefits under This Plan must give
the Claims Administrator any facts the Claims Administrator need to apply those rules and determine benefits
payable.
Facility of Payment
A payment made under another Plan may include an amount that should have been paid under This Plan. If it
does, This Plan may pay that amount to the organization that made that payment. That amount will then be
treated as though it were a benefit paid under This Plan. This Plan will not have to pay that amount again. The
term “payment made” includes providing benefits in the form of services, in which case “payment made” means
the reasonable cash value of the benefits provided in the form of services.
Right of Recovery
If the amount of the payments made by This Plan is more than should have paid under this COB provision, the
Plan may recover the excess from one or more of the persons:
1. the Plan has paid or for whom the Plan have paid; or
2. any other person or organization that may be responsible for the benefits or services provided for the
member.

Administration
31
The “amount of the payments made” includes the reasonable cash value of any benefits provided in the form of
services.
When a Covered Person Qualifies for Medicare
Determining Which Plan is Primary
This Plan will pay Benefits primary to Medicare for the following Medicare-eligible individuals:
• Subscribers with active current employment status age 65 or older and their spouses age 65 or older; and
• Individuals with end-stage renal disease, for a limited period of time.
The Plan will pay benefits second to Medicare when you become eligible for Medicare, even if you don’t elect it
under all other circumstances.
Determining the Allowable Expense When This Plan is Secondary to Medicare
If this Plan is secondary to Medicare, the Medicare approved amount is the Allowable expense, as long as the
provider accepts Medicare. If the provider does not accept Medicare, the Medicare limiting charge (the most a
provider can charge you if they don’t accept Medicare) will be the Allowable expense. Medicare payments,
combined with Plan Benefits, will not exceed 100% of the total Allowable expense.
If you are eligible for, but not enrolled in, Medicare, and this Plan is secondary to Medicare, benefits payable
under this Plan will be reduced by the amount that would have been paid if you had been enrolled in Medicare.
RECOVERY FOR OVERPAYMENT, SUBROGATION AND REIMBURSEMENT
Recovery for Overpayment
In the event that the Plan mistakenly pays or overpays you, you must return the overpayment or mistaken
payment to the Plan. If you fail to return a mistaken payment or overpayment to the Plan, the Plan may suspend
all further benefit payments on any account to an employee and his or her dependents until the mistaken
payment or overpayment (along with related interest and any expense associated with such recovery) is
returned to the Plan or offset against amounts which would otherwise be paid to you. In addition, to the extent
permitted by law, the Administrator may recover the overpayment from any monies then payable, or which may
become payable including in the form of salary, wages or benefits payable under any Hilton sponsored benefit
program. In addition, to the extent allowed by law, the Administrator may deny eligibility for coverage under the
Hilton Health and Welfare Plan prospectively or retroactively, to the date any incorrect or incomplete information
is submitted. The Administrator also has the right to recover any such overpayment by appropriate legal action.
Payment Condition
The Plan, in its sole discretion, may elect to conditionally advance payment of medical benefits in those
situations where an injury, sickness, disease or disability is caused in whole or in part by, or results from the acts
or omissions of covered persons or their dependents, beneficiaries, estate, heirs, guardian, personal
representative, or assigns (collectively referred to hereinafter in this section as “Plan Beneficiary”) or a third
party, where other insurance is available, including but not limited to no-fault, uninsured motorist, workers’
compensation, underinsured motorist, and medical payment provisions (collectively “Coverage”).
Plan beneficiary, his or her attorney, and/or legal guardian of a minor or incapacitated individual agrees that
acceptance of the Plan’s payment of medical benefits is constructive notice of these provisions in their entirety
and agrees to maintain one hundred percent (100%) of the Plan’s payment of benefits or the full extent of
payment from any one or combination of first and third party sources in trust, without disruption except for
reimbursement to the Plan or the Plan’s assignee. By accepting benefits the Plan Beneficiary agrees the Plan
shall have an equitable lien on any funds received by the Plan Beneficiary and/or their attorney from any source
and said funds shall be held in trust until such time as the obligations under this provision are fully satisfied. The
Plan beneficiary agrees to include the Plan’s name as a co-payee on any and all settlement drafts.

Administration
32
In the event a Plan beneficiary settles, recovers, or is reimbursed by any third party or Coverage, the Plan
Beneficiary agrees to reimburse the Plan for all benefits paid or that will be paid. If the Plan Beneficiary fails to
reimburse the Plan out of any judgment or settlement received, the Plan Beneficiary will be responsible for any
and all expenses (fees and costs) associated with the Plan’s attempt to recover such money.
Subrogation
As a condition to participating in and receiving benefits under this Plan, the Plan beneficiary agrees to subrogate
the Plan to any and all claims, causes of action or rights that may arise against any person, corporation and/or
entity and to any Coverage to which the Plan beneficiary is entitled, regardless of how classified or
characterized.
Except as otherwise prohibited by applicable law, you will be required to reimburse the Plan for any expenses
paid by the Plan from any amounts paid to you or on your behalf from any third party, including any:
• Individual;
• Corporation;
• Entity;
• No fault coverage;
• Uninsured coverage;
• Underinsured coverage; or
• Any other insurance policy or fund.
Any amounts you receive must be applied to fully reimburse the Plan That means you may only use (for
example, to pay your attorney fees) those recovered amounts that remain after the Plan has been fully
reimbursed.
You are required to notify the claims administrator in writing if and when you decide to pursue any action against
any third party. If you decide not to pursue a claim against a third party or fail to notify the claims administrator in
a timely manner, the Plan Administrator will have the authority to pursue, sue, compromise or settle any such
claim in your name and to execute all necessary documents in relation to such pursuit of claim. You are required
to fully cooperate with the Plan Administrator in the prosecution of any claim and to avoid doing anything that
would prejudice or diminish the rights of the Plan.
If a Plan beneficiary receives or becomes entitled to receive benefits, an automatic equitable subrogation lien
attaches in favor of the Plan to any claim, which any Plan beneficiary may have against any party causing the
sickness or injury to the extent of such payment by the Plan plus reasonable costs of collection.
The Plan may in its own name or in the name of the Plan Beneficiary commence a proceeding or pursue a claim
against any third party or Coverage for the recovery of all damages to the full extent of the value of any such
benefits or payments advanced by the Plan.
If the Plan beneficiary fails to file a claim or pursue damages against:
a) the responsible party, its insurer, or any other source on behalf of that party;
b) any first party insurance through medical payment coverage, personal injury protection, no-fault coverage,
uninsured or underinsured motorist coverage;
c) any policy of insurance from any insurance company or guarantor of a third party;
d) worker’s compensation or other liability insurance company; or,

Administration
33
e) any other source, including but not limited to crime victim restitution funds, any medical, disability or other
benefit payments, and school insurance coverages;
then the Plan beneficiary authorizes the Plan to pursue, sue, compromise or settle any such claims in the Plan
Beneficiary’s and/or the Plan’s name and agrees to fully cooperate with the Plan in the prosecution of any such
claims. The Plan Beneficiary assigns all rights to the Plan or its assignee to pursue a claim and the recovery of
all expenses from any sources listed above.
Right of Reimbursement
The Plan shall be entitled to recover 100% of the benefits paid, without deduction for attorneys’ fees and costs
or application of the common fund doctrine, make whole doctrine, or any other similar legal theory, without
regard to whether the Plan Beneficiary is fully compensated by his/her recovery from all sources. The Plan shall
have an equitable lien which supersedes all common law or statutory rules, doctrines, and laws of any state
prohibiting assignment of rights which interferes with or compromises in any way the Plan’s equitable
subrogation lien. The obligation exists regardless of how the judgment or settlement is classified and whether or
not the judgment or settlement specifically designates the recovery or a portion of it as including medical,
disability, or other expenses. If the Plan Beneficiary’s recovery is less than the benefits paid, then the Plan is
entitled to be paid all of the recovery achieved.
No court costs, experts’ fees, attorneys’ fees, filing fees, or other costs or expenses of litigation may be
deducted from the Plan’s recovery without the prior, expressed written consent of the Plan.
The Plan’s right of subrogation and reimbursement will not be reduced or affected as a result of any fault or
claim on the part of the Plan beneficiary, whether under the doctrines of causation, comparative fault or
contributory negligence, or other similar doctrine in law. Accordingly, any lien reduction statutes, which attempt
to apply such laws and reduce a subrogating Plan’s recovery will not be applicable to the Plan and will not
reduce the Plan’s reimbursement rights.
These rights of subrogation and reimbursement shall apply without regard to whether any separate written
acknowledgment of these rights is required by the Plan and signed by the Plan beneficiary.
This provision shall not limit any other remedies of the Plan provided by law. These rights of subrogation and
reimbursement shall apply without regard to the location of the event that led to or caused the applicable
sickness, injury, disease or disability.
Excess Insurance
If at the time of injury, sickness, disease or disability there is available, or potentially available any Coverage
(including but not limited to coverage resulting from a judgment at law or settlements), the benefits under this
Plan shall apply only as an excess over such other sources of Coverage. The Plan’s benefits shall be excess to:
a) the responsible party, its insurer, or any other source on behalf of that party;
b) any first party insurance through medical payment coverage, personal injury protection, no-fault coverage,
uninsured or underinsured motorist coverage;
c) any policy of insurance from any insurance company or guarantor of a third party;
d) worker’s compensation or other liability insurance company; or
e) any other source, including but not limited to crime victim restitution funds, any medical, disability or other
benefit payments, and school insurance coverages.
Wrongful Death Claims

Administration
34
In the event that the Plan beneficiary dies as a result of his or her injuries and a wrongful death or survivor claim
is asserted against a third party or any Coverage, the Plan’s subrogation and reimbursement rights shall still
apply.
Obligations
It is the Plan beneficiary’s obligation to:
a) cooperate with the Plan, or any representatives of the Plan, in protecting its rights, including discovery,
attending depositions, and/or cooperating in trial to preserve the Plan’s rights;
b) provide the Plan with pertinent information regarding the sickness, disease, disability or injury, including
accident reports, settlement information and any other requested additional information;
c) take such action and execute such documents as the Plan may require to facilitate enforcement of its
subrogation and reimbursement rights;
d) do nothing to prejudice the Plan’s rights of subrogation and reimbursement;
e) promptly reimburse the Plan when a recovery through settlement, judgment, award or other payment is
received; and
f) not settle or release, without the prior consent of the Plan, any claim to the extent that the Plan beneficiary
may have against any responsible party or Coverage.
If the Plan beneficiary and/or his or her attorney fails to reimburse the Plan for all benefits paid or to be paid, as
a result of said injury or condition, out of any proceeds, judgment or settlement received, the Plan Beneficiary
will be responsible for any and all expenses (whether fees or costs) associated with the Plan’s attempt to
recover such money from the Plan Beneficiary.
Offset
Failure by the Plan beneficiary and/or his or her attorney to comply with any of these requirements may, at the
Plan’s discretion, result in a forfeiture of payment by the Plan of medical benefits and any funds or payments
due under this Plan may be withheld until the Plan Beneficiary satisfies his or her obligation.
Minor Status
In the event the Plan Beneficiary is a minor as that term is defined by applicable law, the minor’s parents or
court-appointed guardian shall cooperate in any and all actions by the Plan to seek and obtain requisite court
approval to bind the minor and his or her estate insofar as these subrogation and reimbursement provisions are
concerned.
If the minor’s parents or court-appointed guardian fail to take such action, the Plan shall have no obligation to
advance payment of medical benefits on behalf of the minor. Any court costs or legal fees associated with
obtaining such approval shall be paid by the minor’s parents or court-appointed guardian.
Language Interpretation
The Plan Administrator retains sole, full and final discretionary authority to construe and interpret the language
of this provision, to determine all questions of fact and law arising under this provision, and to administer the
Plan’s subrogation and reimbursement rights. The Plan Administrator may amend the Plan at any time without
notice.
Severability

Administration
35
In the event that any section of this provision is considered invalid or illegal for any reason, said invalidity or
illegality shall not affect the remaining sections of this provision and Plan. The section shall be fully severable.
The Plan shall be construed and enforced as if such invalid or illegal sections had never been inserted in the
Plan.
LIFE INSURANCE AFTER YOU LEAVE
This section provides a brief description of the conversion, portability, and continuation rights you may have for
certain insured benefits. For more information about your rights, as well as terms, limitations and restrictions,
please refer to Program Documents for the specific insured benefit.
Conversion Rights
These rights apply to employee basic and supplemental life insurance; and dependent life insurance. You or
your dependent may convert to an individual policy if you cease to be employed by Hilton, you become ineligible
for coverage, or group life insurance (limited rights apply in this circumstance) is terminated under the Plan. To
timely convert to an individual policy, you or your dependent must apply for conversion with the appropriate
insurance company listed in the “General Information” section at the end of this SPD and pay the first premium
within 31 days after your coverage ends.
Portability Rights
These rights apply to employee basic life insurance, supplemental life insurance and dependent life coverage. If
you have basic life insurance coverage or supplemental life insurance coverage (including dependent coverage)
and your coverage ends, you may elect to continue group coverage for yourself and/or your dependent under a
portability plan by paying the premiums due directly to the insurance company instead of converting the
coverage to an individual policy. You must apply within 31 days after your coverage ends. Generally, your
portability rights are in lieu of your conversion rights
HEALTH CARE COVERAGE CONTINUATION RIGHTS (COBRA)
COBRA
A federal law known as COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) allows you and your
covered dependents (including your covered spouse, child, domestic partner or child of your domestic partner)
to continue your medical, dental and vision care, EAP benefits and Health Care FSA coverage (on an after-tax
basis) in certain situations when coverage would otherwise end. Upon a qualifying event (described below), you
and your covered dependents may be able to continue these coverages. If otherwise eligible, you and each of
your covered dependents have an independent right to elect COBRA continuation coverage.
Note about EAP: Although your eligibility may end for the reasons stated in the “Participation” section above, if
you are a full-time Team Member, you and your eligible dependents may continue using EAP benefits if you
elect COBRA continuation coverage for medical coverage. Regular part-time Corporate Team Members can
choose to enroll in COBRA continuation of EAP coverage and pay the full cost of coverage, plus a 2% fee for
administrative costs.
Uniformed Services Reemployment Rights
Your right to continued participation in the Plan during leaves of absence for active military duty is protected by
the Uniformed Services Employment and Reemployment Rights Act (USERRA). If you lose eligibility for

Administration
36
coverage in connection with qualifying military service, you may be eligible for continued coverage for up to 24
months following your loss of eligibility.
USERRA continuation coverage is considered alternative coverage for purposes of COBRA. Therefore, if you
elect USERRA continuation coverage, COBRA coverage will generally not be available.
Contact the Benefits Center for more information.
When to Elect COBRA
If you and/or your dependents choose continuation coverage through COBRA, you and your covered
dependents are offered coverage on the same basis as other participants, except you or your affected
dependents pay the entire cost plus a 2% administrative fee (or a 50% administrative fee in the case of an 11-
month extension due to disability). COBRA coverage is intended to extend the coverage that is in effect for you
and your covered dependents on the day before your qualifying event. COBRA coverage does not create new
classes of covered individuals. To be eligible for continuation of coverage, Hilton provided health care coverage
must be in effect on the date before the qualifying event. For your dependents to be eligible for continuation of
coverage, they must also be enrolled for coverage on the day before the qualifying event.
As noted above, if you elect COBRA coverage, you will receive the same coverage that was in effect on the day
before the qualifying event. However, you may change your coverage choices during the annual enrollment
period that falls during your COBRA continuation coverage period. If your covered dependents elect COBRA,
these same rights apply.
COBRA coverage takes effect on the date coverage is lost on account of the qualifying event if a timely election
is made. While Hilton will notify its COBRA Administrator of your qualifying event in the case of your termination
from employment (or service, as applicable), reduction in hours or death, it is your (or your covered
dependent’s) responsibility to notify the COBRA administrator of any other qualifying event (e.g., divorce,
termination of domestic partnership, child reaching age 26). In addition, you may add a newborn or an adopted
child during the COBRA continuation period in accordance with the HIPAA “special enrollment” rules outlined
earlier. Your newborn or adopted child’s coverage begins immediately.
Reporting a Qualifying Event
You or your affected covered dependent must notify the Hilton Benefits Center either in writing or orally within
60 days after the date on which coverage is lost on account of any of the following qualifying events:
• You divorce or become legally separated, or your domestic partnership ends;
• Your child no longer meets the definition of a dependent (e.g., due to age limit); or
• You (or your covered dependent) are determined to have been disabled under the Social Security Act when
coverage ended or at any time during the first 60 days of receiving COBRA continuation coverage.
When you or your affected covered dependent contact the Hilton Benefits Center, be sure to inform the Hilton
Benefits Center of the specific event, the date of the event and who is affected. Please note that you may be
required to provide documentation concerning the qualifying event.
The COBRA Administrator sends you and/or your affected covered dependent a notice and election form,
including the cost of coverage, within 14 days of receiving this notification.

Administration
37
Hilton informs the COBRA Administrator within 30 days of the loss of your coverage on account of any of the
following qualifying events:
• Reduction in hours that makes you ineligible for coverage;
• You are laid off;
• You do not return from an FMLA leave of absence;
• Your termination of employment (or service, as applicable) for any reason other than gross misconduct;
• You become entitled to Medicare; or
• Your death.
The COBRA Administrator sends you and/or your affected covered dependents a notice and election form,
including the cost of coverage, within 44 days after one of these qualifying events occur.
Snapshot of COBRA Coverage
Here is a snapshot of who is eligible for COBRA continuation coverage, under what circumstances, and how
long COBRA continuation coverage continues for health care coverage. If one of the events listed in the chart
occurs, you and your enrolled dependents may apply for COBRA coverage.
Qualifying Event Who Is Eligible for COBRA
Maximum
COBRA Period*
Termination of your employment
(or service, as applicable) for any
reason except gross misconduct
You and your enrolled dependents
18 months
Reduction in hours of employment
(including a military leave of
absence)**
You and your enrolled dependents
18 months
You become laid off
You and your enrolled dependents
18 months
You do not return from an FMLA
leave of absence
You and your enrolled dependents
18 months
You or your covered dependent
becomes disabled
You and your enrolled dependents
18 months up to 29 months***
Your death
Your enrolled dependents
36 months
Divorce, legal separation or
termination of domestic partnership
(unless a QMCSO provides otherwise)
Your enrolled dependents
36 months
Your child no longer meets the
definition of dependent under the Plan
Your covered dependent
36 months
*The maximum COBRA period is measured from the date you lose coverage on account of the qualifying event. If your qualifying
event is termination of employment or reduction in hours of employment and you became entitled to Medicare less than 18 months
before the date coverage ended, the maximum COBRA period for your enrolled dependents lasts until 36 months after the date you
became entitled to Medicare. If eligible for COBRA under the Health Care FSAs, the maximum COBRA period is through the end of
the calendar year in which the qualifying event occurs. See “Health Care Flexible Spending Account” below for details.
**Note that in the event you become entitled to COBRA coverage due to a loss of coverage triggered by a military leave of
absence covered by the USERRA, you will receive continued coverage at the same cost paid by active Team Members for the first
30 days of your military leave. Also, your continuation coverage period is 24 months, not 18 months.
***See “COBRA Coverage for Disabilities” below for details.
Administration
38
Deciding Whether or Not to Continue Coverage and Payment of COBRA Premium
You have 60 days from the day coverage would otherwise end (or from the day the notice is sent to you, if later)
to choose continuation coverage.
In order to continue your health care coverage, you and/or your covered dependents must pay the full cost of
coverage, plus a 2% fee for administrative costs (or a 50% administrative fee in the case of an 11-month
extension due to disability).
Your first payment (due within 45 days of your election) must include your COBRA contribution for the entire
period from the date coverage ended through the month of the payment. Subsequent contributions are due on
the first of the month, whether or not you receive a bill. If the COBRA Administrator does not receive your
monthly contribution within 30 days of the first of the month, coverage is canceled as of the last day of the month
in which you paid a contribution. If you do not choose to continue coverage, you should make the appropriate
election on the election form and return it to the COBRA Administrator. In that case, your health care coverage
ends on the day on which the qualifying event occurred.
When Continuation Coverage Ends
Continuation coverage ends when any of the following events occur:
• You (or a covered dependent) reach the end of the applicable maximum COBRA period for coverage;
• You (or a covered dependent) do not pay a monthly contribution within 30 days of its due date;
• Upon you or your covered dependent’s written request to cancel coverage;
• You (or a covered dependent) become entitled to Medicare after the COBRA event;
• You (or a covered dependent) subsequently become covered under another group medical or dental plan
that does not contain a preexisting condition rule; or
• Hilton ceases to provide any group health plan coverage.
Please inform the Hilton Benefits Center of any changes in address or in personal circumstances so that you and
your covered dependents can receive the necessary information concerning your rights to continuation of
coverage. However, if you are already receiving COBRA, please contact the COBRA Administrator to update
any changes in address or in personal circumstances.
COBRA Coverage for Disabilities
As shown in the chart above, COBRA coverage can be extended from 18 months up to 29 months if you (or
another qualified beneficiary) are totally disabled when you (or the other qualified beneficiary) become eligible for
COBRA coverage or become disabled during the first 60 days of COBRA coverage. Monthly contributions for
continuation coverage increase to 150% (from 102%) of the monthly amount for each of the 11 additional
months of continuation coverage. (Any covered dependents can also continue their COBRA coverage during this
extension period.)
To be eligible for this extension, the individual must:
• Receive a determination of disability from the Social Security Administration (SSA) that the individual was
disabled on the date coverage ended, or became disabled during the first 60 days of COBRA coverage,
and

Administration
39
• Notify the Hilton Benefits Center prior to expiration of the original 18 month coverage period and within 60
days after the later of:
The date of the SSA’s determination of disability; or
The date of the qualifying event.
If the SSA determines that the individual is no longer totally disabled, continuation of coverage will cease. The
individual must notify the Hilton Benefits Center within 30 days of any such finding. Coverage will terminate on
the earlier of the first day of the month that is at least 30 days after the SSA’s findings or at the end of the 29-
month period.
Health Care Flexible Spending Account
You and your covered dependents may only elect COBRA continuation coverage for the Health Care FSA if
you have contributed more to the account than you have been reimbursed, at the time of the qualifying event
(i.e., you have not “overspent” your Health Care FSA). In this case, you would continue contributions on an
after-tax basis.
For example, if you elected to contribution $2,000 for the plan year, contributed $1,000 prior to your
termination, but were reimbursed for $1,500 in expenses at the time of your termination, you will not be eligible
to elect COBRA continuation coverage for the Health Care FSA.
The maximum period for which you may continue after-tax contributions to your Health Care FSA is the
remainder of the Plan year in which the qualifying event occurs.
Administration of COBRA
If you have any questions about COBRA or if you are required to notify Hilton of any event to trigger Hilton’s
COBRA obligations, please contact the Hilton Benefits Center. Upon any required notification by you, the Hilton
Benefits Center will contact the COBRA Administrator to send you any necessary paperwork. Alight Solutions
has been engaged as the Plan’s COBRA Administrator to assist with the sending and receiving of COBRA
information, including the collection of COBRA premiums if elected by participants.
Other Coverage Options Besides COBRA
Instead of enrolling in COBRA continuation coverage, there may be other coverage options for you and your
family through the Health Insurance Marketplace, Medicaid, or other group health plan coverage options (such as
a spouse’s plan) through what is called a “special enrollment period.” Some of these options may cost less than
COBRA continuation coverage. You can learn more about many of these options at www.healthcare.gov.

40
CLAIMS AND APPEALS
CLAIMS AND APPEALS ................................................................................ 41
What Is a Claim? ..................................................................................... 41
Timely Filing ............................................................................................ 41
IF A CLAIM IS DENIED .................................................................................. 42
Denial of Insured Benefit Claims ............................................................. 43
Eligibility or Enrollment Claims Process.................................................. 43
Health Benefit Claims and Appeals ........................................................ 44
CLAIMS AND APPEALS

Claims and Appeals
41
CLAIMS AND APPEALS
This section reviews what you need to do to file claims for the different benefit options in the Plan. It also
describes the process for appealing a determination of whether you and/or your dependents are eligible to be
covered under the Plan. If you have any questions about filing claims, please call the appropriate administrator
or carrier as listed in the General Information section of this SPD.
What Is a Claim?
There are two general types of claims: a claim regarding eligibility or enrollment, and a claim for benefits.
Claim Regarding Eligibility or Enrollment.
This is a claim involving eligibility under a benefit program or enrollment in a benefit program. The U.S. Appeals
Committee, to which the Plan Administrator has delegated authority to decide eligibility claims, generally
determines these types of claims. If you are denied disability or life coverage because you did not satisfy an
insurance requirement for coverage (e.g., Evidence of Insurability), any inquiries or claims should be directed to
the Claims Administrator (the insurance company for the coverage).
Claim for Benefits.
A claim for benefits is the more common type of claim and is a request that benefits be paid under the applicable
program or, with respect to the Health or Dependent Care FSAs, a request that expenses be reimbursed.
Do You Need to File a Claim?
You may or may not need to file a claim to receive benefits. Generally, if you use a network provider, you will not
need to file a claim as your provider will submit on your behalf. However, if you receive non-network medical or
dental services you will be responsible for filing your own claims, unless your provider files the claim on your
behalf.
For more information regarding the claims filing process see the Program Documents for your benefit option or
contact the Claims Administrator as listed in the General Information section of this SPD. The following chart
summarizes these requirements for the various benefit options. In the event of a conflict between the claim
procedures below and those shown in the Program Documents the terms of the Program Document will control.
Timely Filing
Important: Be Aware of Timing! In order for your claim or appeal to be considered, you must submit the
claim or appeal within the timeframes identified in this Section or the applicable Program Documents.
If your claim or appeal is late, it will be denied, regardless of whether it is otherwise eligible to be covered
under the Plan.
You should make every reasonable effort to file claims promptly after you incur services. The time period for filing
claims may vary based on the claims administrator. Claims filed or received after the applicable deadline are not
generally eligible for payment. Please check the relevant Program Documents for more information on the
applicable claims and appeals deadlines.

Claims and Appeals
42
If You … Do You Need to File a Claim?
Medical
Receive medical or prescription drug services from a network
provider
No
Receive medical or prescription drug services from a non-
network provider
Yes*
Within 180 days for Cigna
Within 12 months for Anthem
Dental
Receive dental services from a network provider No
Receive dental services from a non-network provider
Yes*
Within 12 months for Delta Dental
Vision
Receive vision services from a Network provider No
Receive vision services from a non-network provider Yes*
Disability
Are an STD participant Yes
Are an LTD participant
Yes, unless you filed an STD claim with
the appropriate Claims Administrator.
See the “Disability” Section of this
chapter for details.
Life and Accident
Are covered under Life & Accident Yes
*Unless your provider submits the claim on your behalf.
IF A CLAIM IS DENIED
If your claim for benefits under the Plan is denied, you may have it reviewed in accordance with the following
claims review procedures. The procedures will vary depending on the type of benefit claim it is.
Insured benefits of the Plan are listed below:
• Short-term disability
• Long-term disability
• Vision
• Life insurance
• Accidental Death & Dismemberment (AD&D)
• EAP
• Business Travel Accident

Claims and Appeals
43
Self-insured benefits of the Plan are listed below:
• Medical with Prescription Drug Coverage (Anthem and Cigna)
• Dental (Delta Dental only)
• Health Care FSA
• Dependent Care FSA
Denial of Fully Insured Benefit Claims
If your claim for an insured benefit is denied under the Plan, you should refer to the applicable Program
Documents provided by the carrier or contact the insurance carrier (see the General information section) for
more information on the applicable claims procedures.
Denial of Self-Insured Benefit Claims
If the benefit is not provided through an insurance contract, you must file an appeal with the appropriate
Claims Administrator (see the General Information section) if you choose to appeal the denial.
If your first level appeal is denied, you may choose to file a second level appeal (if applicable) with the
appropriate Claims Administrator. Contact the Claims Administrator listed in the General Information section
to determine whether a second level appeal is allowed.
With the exception of medical claims for which an external review process may be applicable, the decision of
the Claims Administrator is final.
As a reminder, except as described below regarding eligibility claims and appeals, the Plan Administrator has
delegated responsibility for claims and appeals decisions to the Claims Administrators. If there is an
inconsistency between the “Health Plan Claims and Appeals” provisions in this SPD and the Program
Documents provided by the Claims Administrators, the Program Documents will control.
Eligibility or Enrollment Claims Process
These procedures apply to claims for eligibility or enrollment in a benefit program.
Filing an Eligibility or Enrollment Claim
If you believe that you or your dependent is eligible or entitled to enroll under the Plan or a specific benefit
program, you may file a claim in writing with Claims and Appeal Management within 60 days of the eligibility
determination. Claims and Appeal Management will review initial eligibility claims and first level eligibility
appeals on behalf of the U.S. Appeals Committee.
Initial Eligibility or Enrollment Claim Decision
When an eligibility claim is received, Claims and Appeal Management must notify you of its benefit
determination within 30 days of the receipt of the claim. If Claims and Appeal Management needs more
information or an extension, it will notify you within 30 days of receiving your claim. If the period is extended,
Claims and Appeal Management will have 45 days after receiving the initial claim to notify you of its decision.
Claims and Appeal Management will send you a written notice of an adverse determination. A denial of a
claim will include:
• The reason(s) for the denial;
• References to the specific plan provisions on which the decision was based;
• A description of any additional material or information you should supply in support of your claim and an

Claims and Appeals
44
explanation of why it is necessary, if any;
• A description of the plan’s appeal procedures and the time limits applicable to the appeal process; and
• A statement of your right to bring a civil action under Section 502(a) of ERISA following an adverse
determination on appeal.
Appealing an Eligibility or Enrollment Claim Denial
If you (or your duly authorized representative) believe that a denial is incorrect, you may request a full review
by the U.S. Appeals Committee within 60 days after your receipt of denial of your claim. In connection with
your appeal, you or your representative may submit written comments, documents, records and other
information relating to the claim.
Send your eligibility claim and appeal, as applicable to:
Hilton Claims and Appeals Management
P.O. Box 299107
Lewisville, TX 75029-9107
FAX: 901-374-5073
You also have the right to request copies of all relevant documents (free of charge). The relevant documents
that must be made available to you include documents, records and other information that:
• Were relied on in deciding your claim;
• Were submitted, considered or generated in the course of deciding your claim; or
• Demonstrate that the decision complied with the Plan’s administrative procedures or safeguards.
The U.S. Appeals Committee will furnish you with a written decision providing the final determination of the
claim. The U.S. Appeals Committee’s review will take into account all comments, documents, records and
other information related to the claim, regardless of whether such items were considered in the initial claim
decision. The U.S. Appeals Committee’s decision on appeal usually will be made within 60 days after
receiving your appeal, unless special circumstances require an extension of an additional 60 days. If the
period is extended, the U.S. Appeals Committee will notify you in writing of the extension within 60 days of
receiving your appeal. The U.S. Appeals Committee’s decision on review will be final and binding on you,
your dependents and any other interested party. Your appeal notice will include:
• The specific reason or reasons for the appeal decision;
• Reference to the specific Plan provisions on which the determination is based;
• A statement that you have the right to request access to and copies of all relevant documents free of
charge; and
• A statement that you have the right to bring a civil action under Section 502(a) of ERISA following an
adverse determination on appeal.
Health Benefit Claims and Appeals
These procedures apply to the health care coverage programs (medical, prescription drug, dental, vision and
Health Care FSA), which are all referred to as “medical benefit” claims. Some medical plan options are fully
insured by an insurance carrier, while other options are self-insured by Hilton. The Claims and Appeals
procedures discussed here relate to the self-insured health care coverage programs. With regard to the fully-
insured options, the Program Documents provide more detail with regard to the applicable benefit Claims and
Appeal procedures. The procedures set forth in this SPD will control as to the self-insured programs. The
Program Documents issued by the carrier will control with regard to the applicable benefit Claims and Appeals
for fully-insured programs.

Claims and Appeals
45
Generally, the steps below describe your appeal procedures, regardless of the type of claim. A claim is not
deemed “filed” for purposes of these claims review procedures until it is filed in accordance with the applicable
claims filing procedures established by the applicable Claims Administrator (see General Information section)
and it is received by the Claims Administrator.
The following provides additional detail about how your claims and appeals are processed for all benefits that
are self-insured:
• Each level of appeal will be independent from the previous level (in other words, the same person(s) or
subordinates of the same person(s) involved in a prior level of appeal will not be involved in the appeal)
• On each level of appeal, the claims reviewer will review relevant information that you submit even if it is
new information. In addition, you have a right to request documents or other records relevant (as defined
by ERISA) to your claim.
Step 1: Notice of claim denial is received from Claims Administrator. If your claim is denied in whole or in
part, you will receive written notice from the Claims Administrator that your claim is denied. However, the
Claims Administrator may give you oral notification if your urgent care claim is denied, and the written
notification will follow within three days.
The Claims Administrator may request an extension of time in which to review your claim for reasons beyond
the Claims Administrator’s control, such as needing more information from you. The time periods in which the
Claims Administrator must make a decision are set forth in the Claims and Appeals Procedures Chart below
and will vary based on the type of claim (e.g. pre-service, urgent, post-service).
Once you have received your notice from the Claims Administrator, review it carefully.
The notice will contain:
• The reason(s) for the denial and the Plan provisions on which the denial is based;
• A description of any additional information necessary for you to complete your claim (if you choose to
appeal), why the information is necessary, and your time limit for submitting the information;
• A description of the Plan’s appeal procedures and the time limits applicable to such procedures,
including a statement of your right to bring a civil action once you have exhausted your appeal rights;
• If applicable, a description of the external review process and how to initiate the review process. Note
that external review applies only to medical claims that involve medical judgment or rescissions.
External review does not apply to claims for eligibility and enrollment, dental, vision, or health care
FSA; and
• A statement indicating whether an internal rule, guideline or protocol was relied upon in making the
denial and that a copy of that rule, guideline or protocol will be provided free of charge upon request
(not applicable to claims for eligibility and enrollment);
• If the denial is based on a medical necessity, experimental treatment or a similar Plan exclusion or
limit, either an explanation of the scientific or clinical judgment for the determination, or a statement
that such explanation will be provided free of charge upon request; and
• If the claim was an urgent care claim, a description of the expedited appeal process

Claims and Appeals
46
Step 2: If you disagree with the decision, file a first level appeal with the Claims Administrator.
If you wish to appeal, you must file a written appeal with the Claims Administrator within 180 days of receipt of
the Claims Administrator’s letter referenced in Step 1.
2
You should submit all information referenced in the
notice, and any other information that you believe will support your appeal.
Note: Cigna only offers one level of appeal for medical coverage claims.
Step 3: You receive a notice of the first level appeal from the Claims Administrator. If the appeal denied,
you will be notified by the Claims Administrator within the time period described in the Claims and Appeals
Procedures Table, depending on the type of claim.
You should take the same action you take in Step 1 described above. The notice will contain the same type of
information that is provided in the first notice of denial provided by the Claims Administrator (see Step 1).
Step 4: If you still disagree with the Claims Administrator’s decision, file a second level appeal with the
Claims Administrator, if permitted. If you wish to appeal, you must file a written second (and final) level
appeal to the Claims Administrator within 60 days after receiving the first level appeal denial notice from the
Claims Administrator. You should gather any additional information that is identified in the notice as necessary
to perfect your claim and any other information that you believe will support your claim.
If the Claims Administrator denies your second level appeal, you will receive notice within the time period
described in the Claims and Appeals Procedures Table, depending on the type of claim.
External Review Process for Medical and Prescription Drug Claims
External review is available for claims involving medical judgment or rescissions after you have exhausted
internal review procedures. If you choose to request an external review, you must submit your request within 4
months after you receive a final decision from the Claims Administrator under the mandatory appeal process
described earlier. The Claims Administrator will send your claim to an independent review organization. The
independent review organization will then refer your case for review by a neutral, independent, board-certified
physician with appropriate expertise in the area in question.
The independent review organization will make its determination on your claim within 45 days after your
request and all necessary information have been submitted. Expedited reviews are available if your physician
certifies that a delay in service would jeopardize your health. Expedited reviews will be decided within 72 hours
of your request. Once the review is complete, the independent review organization will send the final
determination letter directly to you. The Claims Administrator will abide by the decision of the external review
organization.
2
If Anthem is your Claims Administrator, you have 180 days from the date of the adverse determination letter to file the appeal.

Claims and Appeals
47
Limitation of Legal Actions for All Self-Insured Benefits and Eligibility Claims
Important!
You cannot bring a legal action against the Plan, the Plan Administrator, Plan fiduciaries, Hilton, or the
Claims Administrators until you have exhausted the Plan’s claim and appeal procedures in their entirety.
If you exhaust the Plan’s claims and appeals procedures, and you wish to bring a legal action, you must
bring this action within one year after the date the Claims Administrator has made a final determination of
the claim or appeal in accordance with the Plan’s internal claims review procedures, or should have been
made in accordance with the Plan’s internal claims review procedures.
With respect to eligibility claims, you must file an action pertaining to a claim within one year after the date
giving rise to the eligibility claim occurred, e.g., termination of active employment with Hilton.

Claims and Appeals
48
Claims and Appeals Procedure Table
Initial Claims
First Level Appeal
Second Level Appeal
Type of Claim
You will be
notified of
determination as
soon as possible
but no later
than…,
Extension period*
allowed for
circumstances
beyond Claims
Administrator’s
If additional
information
is needed,
you must
provide
within...,
You must file
an appeal
within...,
You will be
notified of
determination as
soon as possible
but no later
than…,
You must
file an
appeal
within...,
You will be
notified of
determination
as soon as
possible but
no later than...,
Medical – Urgent Care
Anthem
72 hours (24
hours if
additional
information is
needed from
you before a
determination
can be made)
None
48 hours (Claims
Administrator must
notify you of
determination
within 48 hours of
receipt of your
information)
180 days of
claim denial
72 hours from
receipt of appeal
N/A
N/A
Cigna
72 hours (24
hours if
additional
information is
needed from
you before a
determination
can be made)
None
48 hours (Claims
Administrator must
notify you of
determination
within 48 hours of
receipt of your
information)
180 days of
claim denial
72 hours from
receipt of appeal
N/A
N/A
Medical - Pre-Service (also known as Prior Authorization or Pre-Certification)
Anthem
15 days from
One extension of 15
days
45 days of date of
extension notice
180 days of
claim denial
30 days from
receipt of appeal
60 days of 1st
level appeal
denial*
15 days from
receipt of
appeal*
Cigna
15 days from
One extension of 15
days
45 days of date of
extension notice
180 days of
claim denial
30 days from
receipt of appeal
N/A
N/A
Medical - Concurrent or Expedited: To end or reduce treatment prematurely
Anthem
Notification to
end or reduce
treatment will
allow time to
finalize appeal
before end of
treatment
N/A
N/A
Denial letter will
specify filing limit
180 days of
claim denial
72 hours
Denial letter
will specify
filing limit*
15 days from
receipt of appeal*
Cigna
Extension on course of
treatment already
approved (must
request at least 24
hours prior to
expiration of approved
time period or number
of treatments)
Notification to
end or reduce
treatment will
allow time to
finalize appeal
before end of
treatment
24 hours after
receiving request
N/A
N/A
Denial letter will
specify filing limit
Within 180 days
of claim denial
30 days from receipt
of appeal
N/A
N/A
Medical - Post-Service with 2nd level appeal*
Anthem/
Clinical requests for
CVS
30 days from
receipt of
claim
One extension of 15
days
45 days of date of
extension notice
180 days of
claim denial
Anthem: 60 days
from receipt of
appeal
CVS: 30 days from
receipt of appeal
60 days of 1st
level appeal
denial*
60 days from
receipt of
appeal*
CVS: 30 days
from receipt of
appeal

Claims and Appeals
49
Initial Claims
First Level Appeal
Second Level Appeal
Type of Claim
You will be
notified of
determination as
soon as possible
but no later
than…,
Extension period*
allowed for
circumstances
beyond Claims
Administrator’s
If additional
information
is needed,
you must
provide
within...,
You must file
an appeal
within...,
You will be
notified of
determination as
soon as possible
but no later
than…,
You must
file an
appeal
within...,
You will be
notified of
determination
as soon as
possible but
no later than...,
Cigna/
Non-clinical requests
for CVS
30 days from
receipt of
claim
One extension of 15
days
45 days of date of
extension notice
180 days of
claim denial
Within 30 calendar
days after receiving
an appeal
CVS: 60 days from
receipt of appeal
N/A
N/A
Life Insurance, AD&D, Business Travel Accident, Dependent Care FSA
90 days from
receipt of
claim
One extension of 90
days
45 days of date of
extension notice
60 days of claim
denial
For Dependent
Care FSA, 180
days of claim
denial
60 days from receipt
of appeal (with one
60-day extension
beyond the Plan’s
control).
You must
submit requested
documentation
within 45 days
N/A
N/A
Disability Benefits
45 days from
receipt of
claim for LTD
benefits 10
days for STD
benefits.
Two
extensions of
30 days each
45 days of date of
extension notice
180 days of
claim denial
45 days from receipt
of appeal (with one
45-day extension
beyond the Plan’s
control).
You must
submit requested
documentation
within 45 days
180 days of
claim denial
45 days from
receipt of appeal
(with one 45-day
extension beyond
the Plan’s
control). You
must submit
requested
documentation
Dental Benefits
30 days from
receipt of claim
One extension of 15
days
45 days of date of
extension notice
180 days of
claim denial
30 days from
receipt of appeal
60 days of 1
st
level appeal
denial
30 days from
receipt of appeal
Health Care FSA
Within 180 days
of claim denial
30 days from receipt
of appeal
N/A
N/A
*For fully-insured options, check your Program Documents to determine whether second level appeals are offered.

50
MEDICAL COVERAGE
OVERVIEW OF YOUR MEDICAL COVERAGE............................................ 51
Program Documents and Coverage Details ........................................... 52
Hospital Admissions for Maternity ........................................................... 53
Post-Mastectomy Care ............................................................................ 53
Preventive Care ....................................................................................... 54
Direct Access For Mental Health and Substance Use
Disorder Services .................................................................................... 54
Additional Care Options if you enroll in coverage
through Anthem or Cigna: ....................................................................... 55
MEDICAL COVERAGE

51
Medical Coverage
OVERVIEW OF YOUR MEDICAL COVERAGE
Your medical coverage is a key component of the Plan and offers a variety of medical care options so you can
choose the one that best meets your needs. This coverage pays benefits for the treatment of an illness or injury
and offers many features, such as mental/behavioral health coverage, preventive health care coverage, well-
baby care and prescription drug coverage. Medical coverage includes options administered by Claims
Administrators Cigna and Anthem, as well as fully insured options offered through various carriers. Options
may differ based on where you live.
You may choose medical coverage for yourself and your eligible dependents under the following coverage
levels:
You Only
You + Spouse/Domestic Partner
You + Child(ren)
You + Family
You may choose from one or more of the following medical coverage options, depending on where you reside*:
Broad Network Plans:
• Bronze Plus (High Deductible Health Plan with a Health Savings Account (HSA) PPO)
• Silver (PPO)
• Gold (PPO)
• Platinum (PPO)
High-Performance Network Plans:
• Bronze Plus (High Deductible Health Plan with a Health Savings Account (HSA) PPO or EPO
(depending on your location)
• Silver (PPO or EPO depending on your location)
• Gold (PPO or EPO depending on your location)
• Platinum (PPO or EPO depending on your location)
Regional HMOs*
*Some available insurance carriers in CA, CO, DC, GA, MD, OR, VA and WA, offer an HMO plan option that
covers in-network care only.
The plan options above may be administered by Anthem and/or Cigna. If coverage under a Kaiser or SIMNSA
plan is available to you, it will be an option at enrollment.
As you read about your coverage, keep the following in mind:
The Plan offers medical coverage through Exclusive Provider Organization (EPO), Preferred Provider
Organization (PPO), or Health Maintenance Organization (HMO) options with varying levels of member cost
share. HMO availability varies depending on your location.
Generally, the options differ in the amount you pay for out-of-pocket expenses (deductibles, copayments and
coinsurance) and in the way you may access medical care (through a primary care physician, network
providers or non-network providers).

Medical Coverage
52
If you are eligible and elect medical coverage under an HMO option, care generally must be authorized and
provided by the HMO’s network to be covered. Please refer to the HMO Program Documents for more
information.
If you elect an HMO option, you and your covered dependents must choose a primary care physician.
The Bronze Plus plan is a High Deductible Health Plan (HDHP). An HDHP features a higher deductible than
other traditional medical and pharmacy benefit plans. This means that you will pay out-of-pocket for your
medical and pharmacy expenses until you meet your deductible. After you have met your deductible, the Plan
starts paying benefits. You will pay a percentage of the cost for covered services (coinsurance), until you meet
your out-of-pocket maximum. Once you meet your out-of-pocket maximum, the Plan will pay 100% of covered
services for the remainder of the benefit year. Preventive care medical services performed by an in-network
provider are covered at 100%, which means there is no charge to you. Your monthly premium rates for an
HDHP are generally lower than traditional medical plans. The HDHP can be used with a Health Savings
Account (HSA). Important!
If you elect an HMO or EPO option, only in-network benefits are covered and you will not have out-of-network
benefits.
If you elect a PPO option, both in-network and out-of-network benefits are covered. The Plan pays higher
benefits when you receive care from an in-network provider.
Prescription Drug Coverage.
If you elect one of the self-insured options (administered by Anthem or Cigna), you are automatically enrolled
in prescription drug coverage through Hilton’s prescription drug program, described in the “Prescription
Drugs” section of this SPD.
If you elect coverage with a fully insured option, you will be automatically enrolled in prescription drug coverage
through the carrier.
Program Documents and Coverage Details
Details about covered expenses, plan limitations and exclusions, and other medical coverage information can
be found in the Program Documents made available by the applicable Claims Administrator(s) or carrier(s). The
Program Documents are available online, or hard copy upon request, . See the “General information” section
for how to access the Program Documents.
Below is an overview of the different medical coverage levels. Individual carriers may offer coverage that differs
slightly from the standard coverage reflected here.
BRONZE PLUS
SILVER GOLD PLATINUM
Eligible for HSA? Yes No No No
Payroll Deductions Lowest Lower Higher Highest
Coinsurance – your share of the cost of a covered service
•
In-network
•
Out-of-network (not available with Anthem Blue HPN)
Plan pays 75%
Plan pays 55%
Plan pays 70%
1
Plan pays 50%
Plan pays 75%
1
Plan pays 55%
Plan pays 85%
1
Plan pays 65%
Annual Deductible 2 – how much you pay for covered services before the plan starts to pay benefits
(Individual/Family)
•
In-network
•
Out-of-network (not available with Anthem Blue HPN)
$2,450/$4,900
3
$2,450/$4,900
3
$1,000/$2,000
$2,000/$4,000
$800/$1,600
$1,600/$3,200
$250/$500
$5,000/$10,000

Medical Coverage
53
BRONZE PLUS
SILVER GOLD PLATINUM
Annual Out-of-Pocket Maximum
2
(Individual/Family)
•
In-network
•
Out-of-network (not available with Anthem Blue HPN)
$3,900/$7,800
3
$11,500/$23,000
3
$5,300/$10,600
$10,600/$21,200
$3,600/$7,200
$7,200/$14,400
$2,300/$4,600
$11,500/$23,000
OVERVIEW OF IN-NETWORK BENEFITS
Important! Anthem Blue HPN only covers in-network care; no out-of-network coverage is available except for urgent and
emergency care
Preventive Care
Covered at 100%,
no deductible
Covered at 100%,
no deductible
Covered at
100%, no
deductible
Covered at 100%,
no deductible
Doctor’s Visit
You pay 25% after
deductible
You pay $30 for
primary care; $50
for specialist; $5
for behavioral
health
You pay $25 for
primary care;
$40 for
specialist; $5 for
behavioral health
You pay $25 for
primary care; $40
for specialist; $5
for behavioral
health
Retail Health Clinic
Varies; contact
insurance carrier
directly
Varies; contact
insurance carrier
directly
Varies; contact
insurance carrier
directly
Varies; contact
insurance carrier
directly
Urgent Care Center
You pay 25% after
deductible
You pay 30% after
deductible
You pay 25%
after deductible
You pay 15% after
deductible
Emergency
Room
You pay 25% after
deductible
You pay $150,
then 30% after
deductible
You pay 25%
after deductible
You pay 15% after
deductible
Outpatient Surgery
(Hospital and Surgicenter)
You pay 25% after
deductible
You pay 30% after
deductible
You pay 25%
after deductible
You pay 15% after
deductible
Outpatient Surgery
(Doctor’s Office)
You pay 25% after
deductible
You pay $30 for
primary care;
$50 for specialist
You pay $25 for
primary care;
$40 for
specialist
You pay $25 for
primary care;
$40 for specialist
Inpatient
Services
You pay 25% after
deductible
You pay 30% after
deductible
You pay 25%
after deductible
You
pay 15% after
deductible
1
Copays may apply.
2
There are separate annual deductibles and annual out-of-pocket maximums for in- and out-of-network care. Out-of-network charges do not count toward
your in-network annual deductible or annual out-of-pocket maximum. In-network charges do not count toward the out-of-network annual deductible or
annual out-of-pocket maximum.
3
The entire family deductible must be met before the plan will pay benefits for any covered family member, and the entire family annual out-of-pocket-
maximum must be met before the plan starts to pay for eligible expenses at 100% for the rest of the year. There is no “individual” annual deductible or out-
of-pocket maximum when you have family coverage.
Hospital Admissions for Maternity
The Newborns’ and Mothers’ Health Protection Act requires medical plans to provide a minimum hospital stay
for the mother and newborn child of 48 hours after a normal, vaginal delivery and 96 hours after a cesarean
section unless the attending provider, either a physician or midwife, in consultation with the mother, determines
a shorter hospital length of stay is adequate.
Post-Mastectomy Care
If you or a covered dependent is receiving benefits in connection with a mastectomy and you or your covered
dependent elect breast reconstruction, the medical program options also cover, in a manner determined in
consultation with the attending physician and the patient:
All stages of reconstruction of the breast on which the mastectomy was performed;

Medical Coverage
54
Surgery and reconstruction of the other breast to produce a symmetrical appearance; and
Prostheses and treatment of physical complications of the mastectomy, including lymphedema.
Coverage for prosthetic devices and reconstructive surgery is subject to the same copayments and deductibles
as those established for other benefits under the medical program options.
Preventive Care
Preventive care is generally covered without cost to you and your eligible dependents as defined by
recommendations from the following:
the U.S. Preventive Services Task Force (A and B recommendations);
the Advisory Committee on Immunization Practices (ACIP) for immunizations;
the American Academy of Pediatrics’ Periodicity Schedule of the Bright Futures Recommendations for Pediatric
Preventive Health Care;
the Uniform Panel of the Secretary’s Advisory Committee on Heritable Disorders in Newborns and Children;
and
with respect to women, evidence-informed preventive care and screening guidelines supported by the Health
Resources and Services Administration.
Detailed information is available at www.healthcare.gov. For additional information on immunizations, visit the
immunization schedule section of www.cdc.gov."
For more information about specific preventive care coverage, please see the Program Documents.
Diagnostic Testing for COVID-19:
The Plan covers COVID-19 related vaccines, testing and diagnostic services subject to deductibles, copays and
coinsurance in the same fashion as similar vaccination, testing and diagnostic services covered by the Plan.
If you have any questions about the medical plan coverage available to you, or whether a specific provider or
procedure is covered under a medical plan option, please contact the Hilton Benefits Center or your carrier for
more information. Treatment for a COVID-19 diagnosis is subject to all other plan terms and conditions.
Direct Access For Mental Health and Substance Use Disorder Services
You are allowed direct access to a licensed/certified Participating Provider for covered Mental Health and
Substance Use Disorder Services. There is no requirement to obtain an authorization of care from your Primary
Care Physician for individual or group therapy visits to the Participating Provider of your choice for Mental
Health and Substance Use Disorder.

Medical Coverage
55
Additional Care Options if you enroll in coverage through Anthem or Cigna:
• Accordant Care: If you are managing certain rare or complex health conditions you can generally
access Accordant Care, a program which provides a support team (e.g., nurse, care coordinator,
doctor) who will assist in developing an individualized action plan and periodically check in with the
Team Member. CVS Caremark will directly contact those Team Members who qualify for this program.
• SurgeryPlus: Program participants have access to a nationwide network of surgery providers at
various surgical centers of excellence (COE) for certain elective surgeries. Team Members who use an
in-network qualified surgeon may have their copay, coinsurance, and/or deductible waived for their
surgical procedure (depending on their elected medical plan option). Please note that, as is standard
for high deductible health plans per IRS guidelines, procedure costs for Team Members who are
enrolled in a Bronze Plus plan will be covered only after their applicable plan deductible is satisfied –
SurgeryPlus will collect any remaining deductible at the time of the procedure. Effective January 1,
2024, bariatric surgery for members enrolled in Anthem or Cigna will only be covered if you go to a
surgeon in the SurgeryPlus network.
• Progyny: Effective January 1, 2023, in order for Anthem and Cigna medical plan participants’ fertility
treatments to be covered by your applicable medical coverage option, Team Members will need to
access the fertility management services offered through Progyny, Hilton’s third-party family planning
benefit vendor, which is integrated with the Plan’s Anthem and Cigna medical coverage options.
Progyny covers a lifetime maximum of two Smart Cycles per eligible participant, including pre-tax
coverage of a frozen donor tissue purchase and a live donor cycle, and provides for a lifetime
pharmacy maximum of $10,000. Services and supplies furnished by out-of-network providers or not
listed as covered in the Progyny member guide are excluded from coverage. The Progyny benefit does
not cover elective egg freezing, unless determined to be medically necessary. Additionally, if there is a
need for tissue storage, the Progyny benefit will cover one year of storage (with the eligible participant
covering the coinsurance and deductible amounts, as for other services); beyond that, storage will no
longer be covered by Progyny, and the participant will need to pay the storage fees out of pocket. If
you have any questions about the Progyny benefit, or the covered services available to you, please
contact the Hilton Benefits Center for more information, or Progyny at 1.855.614.2056.
• Sword: Sword provides virtual physical therapy, designed to offer the benefits of physical therapy
from the convenience of home. Sword is available at no cost to Team Members, spouses/domestic
partners and their dependents age 13 and older enrolled in the Anthem or Cigna Silver, Gold or
Platinum Plan. Participants in the Anthem or Cigna Bronze Plus Plan are eligible for services at a cost
of $29/month. Find out how to get started with Sword at https://join.swordhealth.com/hilton
.
• Bloom: Bloom provides virtual, clinical-grade pelvic health care from the convenience and privacy of
home. The program addresses pelvic health disorders such as urinary leaking, bowel issues and
chronic pelvic pain, across all life stages including pregnancy, postpartum and menopause. Bloom is
available at no cost to Team Members, spouses/domestic partners and dependents age 18+ who are
enrolled in an Anthem or Cigna Silver, Gold or Platinum medical plan. At this time, Bloom is not
available to those who are enrolled in an Anthem or Cigna Bronze Plus Plan. Find out how to get
started with Bloom at https://join.hibloom.com/hilton
.
• Vida: Vida Health offers free coaching for diabetes and cardiovascular conditions. Vida Health
provides access to a dedicated health coach who can help you reach your goals – including improving
blood sugar/blood pressure/cholesterol, nutrition, weight loss, overall wellbeing and more – to address
diabetes, prediabetes, hypertension, obesity. Your coach will provide a personalized plan and support
you throughout your journey, all at no cost to you. Effective January 1, 2025, prescriptions for anti-
obesity medications taken for weight loss must be obtained through a Vida Health medical provider in
order to be covered under the Plan. Access to Vida Health is free as part of your Hilton benefits. For
more information, visit Vida.com/Hilton. Find out how to get started with Vida at https://vida.com/hilton
.

Medical Coverage
56
• Parsley Health: Parsley Health is a virtual women’s+ health medical service. Parsley’s personalized
programs address risk factors and health conditions including infertility, menopause, autoimmune
issues, digestive issues, heart issues, hormonal issues, and more. Parsley is available to members
enrolled in an Anthem or Cigna plan. Find out how to get started at
https://www.parsleyhealth.com/hilton.

57
PRESCRIPTION DRUGS
THE PRESCRIPTION DRUG BENEFIT PROGRAM ..................................... 58
How Much to Pay — Your Deductible and Co-payment ......................... 58
Member initiates enrollment: .................................................................... 61
Physician initiates enrollment: ................................................................. 62
What’s Included and What’s Not Included .............................................. 62
Quantity Limits ......................................................................................... 62
The Prescription Drug Authorization Process ......................................... 62
When You Have Questions ..................................................................... 63
PRESCRIPTION DRUGS
58
THE PRESCRIPTION DRUG BENEFIT PROGRAM
Your prescription drug coverage is a key component of the Plan. Prescription drug coverage is included when
you enroll in medical coverage under the Plan.
All prescription drugs must be medically necessary and used in an appropriate manner in order to be
covered under the Plan.
If you choose a medical coverage option administered by Anthem or Cigna, CVS Caremark will administer your
pharmacy benefits. Anthem and Cigna participants will receive a separate ID card for pharmacy coverage.
CVS/Caremark will provide an initial benefit card upon enrollment in the plan. Present your ID card when filling
a prescription at a Network Pharmacy. Should you need additional or replacement ID cards, please contact
Customer Care at 1-855-311-3158 or visit www.caremark.com
to either request a new card or print a temporary
card.
If you enroll in coverage under Kaiser or another fully insured option, the insurance carrier will manage your
pharmacy benefits. Use your insurance ID card for prescriptions.
Note: Prescription drug coverage provided through a fully insured option is not described in this SPD. Please
refer to the applicable Program Documents provided by the carrier for coverage details.
If your medical coverage is administered by Anthem or Cigna, you may obtain your prescription medications
through either:
• Retail pharmacies
• Mail order
How Much to Pay — Your Deductible and Co-payment
The table below provides an overview of the Plan’s prescription drug coverage.
The prescription drug coverage is not subject to a deductible, unless you are enrolled under the Bronze High
Deductible Health Plan (HDHP).
However, you are responsible for paying the
amounts below until you reach the out-of-pocket maximum
(OOP). The applicable out of pocket costs
vary
depending on which medical plan you enrolled in.
Your prescription costs will contribute towards the out-of-pocket (OOP) maximum in combination with your
costs under the medical plan. The Plan pays 100% for eligible prescriptions once you have met the OOP
maximum.
Your choice will affect the amount you pay for your prescription:

59
Prescription Drug (Retail) for Anthem and Cigna Participants – 30 day
supply
3
Note: For 2024, the deductible under the Bronze Plus HDHP is $2,450 for an individual and $4,900 for a
family.
Bronze Plus
Plan (HDHP)
Silver Plan
Gold Plan
Platinum
Plan
Generic
25% co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $3,900
individual/$7,800
family is met.
(Deductible and OOP
Max are combined
with medical)
$12 co-pay per fill.
Plan pays 100% for
eligible
prescriptions once
the out of pocket
maximum of $5,300
individual/$10,600
family is met.
$10 co-pay per fill.
Plan pays 100% for
eligible
prescriptions once
the out of pocket
maximum of $3,600
individual/$7,200
family is met.
$8 co-pay per fill.
Plan pays 100%
for eligible
prescriptions once
the out of pocket
maximum of
$2,300
individual/$4,600
family is met.
Brand/Formulary
*If a generic version of
your prescription is
available, your
prescriber will need to
confirm medical
necessity for your
brand-name drug to be
covered.
25% co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $3,900
individual/$7,800
family is met.
(Deductible and OOP
Max are combined
with medical)
$50 co-pay per fill.
Plan pays 100% for
eligible
prescriptions once
the out of pocket
maximum of $5,300
individual/$10,600
family is met.
$40 co-pay per fill.
Plan pays 100% for
eligible
prescriptions once
the out of pocket
maximum of $3,600
individual/$7,200
family is met.
$30 co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $2,300
individual/$4,600 family
is met.
Brand/Non-
Formulary
*If a generic
version of
your
prescription
is available,
your
prescriber
will need to
confirm
medical
necessity to
have your
brand-name
drug
covered.
25% co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $3,900
individual/$7,800
family is met.
(Deductible and OOP
Max are combined
with medical)
$70 co-pay per fill.
Plan pays 100%
for eligible
prescriptions once
the out of pocket
maximum of
$5,300
individual/$10,600
family is met.
$60 co-pay per fill.
Plan pays 100% for
eligible
prescriptions once
the out of pocket
maximum of $3,600
individual/$7,200
family is met.
$50 co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $2,300
individual/$4,600 family
is met.
Specialty
Medicines
25% co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $3,900
individual/$7,800
family is met per 30-
day supply of
specialty medications
through CVS
Specialty. Visit
CVSSpecialty.com to
get started.
$12 for generic/ $50
for preferred brand/
$70 for non-preferred
brand for a 30-day
supply of specialty
medicines. Visit
CVSSpecialty.com to
get started.
$10 for generic/ $40
for preferred brand/
$60 for non-preferred
brand for a 30-day
supply of specialty
medicines. Visit
CVSSpecialty.com to
get started.
$8 for generic/ $30 for
preferred brand/ $50
for non-preferred
brand for a 30-day
supply of specialty
medicines. Visit
CVSSpecialty.com to
get started.
3
If you are enrolled in medical coverage through Kaiser or another fully insured plan, your pharmacy benefits may differ from
those shown here. Contact your insurance carrier for more information.

60
Prescription Drug (Mail Order or Retail-90) for Anthem and Cigna Participants – 90 day
supply
4
Bronze Plus
Plan
Silver Plan
Gold Plan
Platinum
Plan
Generic
25% co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $3,900
individual/$7,800
family is met.
(Deductible and OOP
Max are combined
with medical)
$30 co-pay per fill.
Plan pays 100%
for eligible
prescriptions once
the out of pocket
maximum of
$5,300
individual/$10,600
family is met.
$25 co-pay per fill.
Plan pays 100% for
eligible
prescriptions once
the out of pocket
maximum of $3,600
individual/$7,200
family is met.
$20 co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $2,300
individual/$4,600 family
is met.
Brand/Formulary
*If a generic version of
your prescription is
available, your
prescriber will need to
confirm medical
necessity to have your
brand-name drug
covered.
25% co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $3,900
individual/$7,800
family is met.
(Deductible and OOP
Max are combined
with medical)
$125 co-pay per fill.
Plan pays 100%
for eligible
prescriptions once
the out of pocket
maximum of
$5,300
individual/$10,600
family is met.
$100 co-pay per fill.
Plan pays 100% for
eligible
prescriptions once
the out of pocket
maximum of $3,600
individual/$7,200
family is met.
$75 co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $2,300
individual/$4,600 family
is met.
Brand/Non-
Formulary
*If a generic
version of
your
prescription
is available,
your
prescriber
will need to
confirm
medical
necessity to
have your
brand-name
drug
covered.
(Deductible and OOP
25% co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $3,900
individual/$7,800
family is met. Max are
combined with
medical)
$175 co-pay per fill.
Plan pays 100%
for eligible
prescriptions once
the out of pocket
maximum of
$5,300
individual/$10,600
family is met.
$150 co-pay per fill.
Plan pays 100% for
eligible
prescriptions once
the out of pocket
maximum of $3,600
individual/$7,200
family is met.
$125 co-pay per fill.
Plan pays 100% for
eligible prescriptions
once the out of pocket
maximum of $2,300
individual/$4,600 family
is met.
4
If you are enrolled in medical coverage through Kaiser, your pharmacy benefits may differ from those shown here. Contact
Kaiser for more information.
If the cost of your prescription is less than the co-pay, you will only pay the cost of the
prescription.
NOTE: It is your responsibility to discuss the availability of a generic drug before the doctor writes you a
prescription.
CVS Customer Care
Visit CVS/Caremark website, www.caremark.com, to view your prescription drug benefits and co-payment information,
search for details on your prescription medications, locate a participating pharmacy near you, and manage your home

61
delivery prescriptions or to obtain a list of preferred and non-preferred medications. For additional inquiries, you may
call CVS Customer Care directly at 1-855-311-3158.
Your Local CVS/Caremark Pharmacy
When you use a CVS/Caremark-affiliated pharmacy, you pay your co-payment when the prescription is filled, and
there is no need to submit a written claim form. You must
obtain prescriptions at a CVS/Caremark pharmacy, a
pharmacy participating in the CVS/Caremark
Network, or through CVS Specialty Pharmacy in order to receive
prescription benefits through the
Plan. Log into your www.caremark.com member portal to find an in-network
pharmacy near you by going to the “Plans & Benefits” menu and choosing the “Pharmacy Locator” option.
Note: If you obtain a prescription through a pharmacy that is not affiliated with CVS/Caremark, you will be
required
to pay the full cost of the prescription to the pharmacy.
Choosing a Generic or Brand-Name Drug
CVS/Caremark’s generic drug incentive program only addresses United States FDA rated class “A”
generic drugs,
which are widely accepted as bioequivalent to their brand-name counterparts by the
medical and pharmacy
communities. Using a generic drug may cost you less money. Talk to your doctor about appropriate
options for you .
CVS Specialty Pharmacy
All specialty
prescriptions must be filled through CVS Specialty Pharmacy. Infused drugs cannot be purchased at a
pharmacy. If a particular infused
drug is available through CVS Specialty Pharmacy that drug must be purchased
through the CVS
Specialty Pharmacy program. If a particular infused drug is not available through CVS Specialty
Pharmacy and you purchase it from another source, the Plan will only cover the
costs that the Plan would have
paid had the drug been purchased through the CVS Specialty
Pharmacy program and only if approved in
advance by CVS.
Participation in the Specialty Pharmacy Program can be initiated by a phone call from the member or
the physician.
There are no mailers necessary for the CVS Specialty Pharmacy program. This means that there are no
required forms needed for participation in the Specialty Pharmacy Program and this can be initiated by a
phone call to CVS from the member or the physician. Most
orders through CVS Specialty Pharmacy can be
processed and shipped by overnight delivery within
two days of receipt of the prescription from the physician. Orders
require a signature for delivery and
can be shipped to your home. Alternatively, you are able to request to have
specialty prescriptions
delivered to any CVS Pharmacy retail location, as this may be a more convenient option. All
orders
receive necessary supplies to administer the drug at no cost.
Note: If you are enrolled in a plan with Cigna, certain specialty medications are covered through Pathwell Specialty.
Effective January 1, 2025, medications administered at an in-network provider’s office and covered through Pathwell
Specialty are subject to deductible and coinsurance. For more information, please contact Cigna or refer to the
applicable Program Documents.
Member initiates enrollment:
1.
You call CVS Specialty Pharmacy customer service line (1-800-237-2767) and request
specialty medication
through the program.
2.
Customer Service Associate will ask you for your ID number, address, day-time phone number,
specialty drug,
date of next fill, and physician name and phone number.
3.
The CVS Specialty Pharmacy team will contact physician for prescription and initiate order
processing.
4.
If prior authorization is required, the Pharmacy team will follow predetermined Prior Authorization
process for
client to obtain the Prior Authorization.
5.
After claim is processed, CVS Specialty Pharmacy will contact you to confirm copayments
and arrange delivery
(within two days of receiving prescription). If a copayment exists, payment
will be required prior to shipping.

62
Physician initiates enrollment:
1.
Physician calls CVS Specialty Pharmacy physician line (1-866-814-5506) for direct access to a
pharmacist; or
physician faxes prescription directly to the CVS Specialty Pharmacy at 1-800-323-
2445.
2.
CVS Specialty Pharmacy team initiates order processing
3.
Prior authorization is obtained if required.
4.
You are contacted to confirm copayments and arrange delivery (within two days of physician’s
initial call).
CVS Specialty Pharmacy Refill Process:
1.
CVS Specialty Pharmacy team calls you 5-7 days prior to their next order.
2.
If you are continuing on drug therapy, delivery of next order is arranged.
What’s Included and What’s Not Included
For an all-inclusive list of covered or excluded prescription drug benefits, please visit www.caremark.com or contact
CVS/Caremark Customer Care to verify specific coverage. PrudentRx Copay Savings Program (PrudentRx)
As part of your Hilton CVS prescription plan, you may be eligible for the PrudentRx Copay Program. This program can
reduce your out-of-pocket cost for certain specialty drugs on the PrudentRx Specialty Drug List. It allows you to get
select specialty medications at no cost to you. That means $0 out-of-pocket for any medications on your plan’s
exclusive Specialty Drug List when you fill by CVS Specialty®.
PrudentRx will work with manufacturers to get copay card assistance, and will manage enrollment and renewals on
your behalf. Even if there is no copay card program for your medication, your cost will be $0 for as long as you are
enrolled in the Prudent Rx Copay Program.
If you qualify for the program, you will receive a welcome letter and a phone call directly from PrudentRx that provides
information about the program as it pertains to your medication. The PrudentRx Copay Program is available to
participants enrolled in the Anthem or Cigna Platinum, Gold and Silver plans.
Quantity Limits
The Plan may have certain coverage limits. For example, a medication might be limited to a certain amount (such as
the number of pills or total dosage) within a specific time period. For more information, please visit www.caremark.com
or contact Customer Care at 1-855-311-3158.
The Prescription Drug Authorization Process
The Prescription Drug Authorization Process applies:
•
If you have been required in the past to receive Prior Authorization to obtain a prescription,
injectable or
infused drug;
•
For any prescription that your pharmacist or CVS/Caremark indicates a requirement for Prior
Authorization.
These are generally not routine prescriptions. You may talk with your pharmacist, physician, or call
CVS/Caremark
for information only. Clinical information for Prior Authorization review is accepted
only from physicians or
pharmacists, not from you.
Also note: Any Prior Authorizations currently in place will remain in effect until that prescription’s Prior
Authorization
has expired. Physicians and pharmacists are advised how long the Prior Authorization
is valid when the Prior

63
Authorization is issued. If continued authorization is required after the
expiration date, the physician or
pharmacy must contact CVS/Caremark to request a new Prior
Authorization.
Here’s how the process will work:
•
Your doctor must call CVS/Caremark toll-free at 1-800-294-5979 to request prior
authorization. Early
notification will avoid delays.
•
Once CVS/Caremark receives the prior authorization request, the turnaround time for review
is two business
days or sooner.
•
If the drug in question will be covered, CVS/Caremark will set up the Prior Authorization and
the physician or
pharmacist will be notified by return fax. If the drug is not covered,
CVS/Caremark will notify the requesting
physician or pharmacist by return fax indicating why
the drug is being denied. You will be mailed a notice
of denial that will also
explain how you can appeal this decision.
When You Have Questions
For any assistance or information about specific features of this prescription drug program benefit, please
contact:
Customer Care Support: 855-311-3158
Web Support: www.caremark.com

64
DENTAL COVERAGE
OVERVIEW OF YOUR DENTAL COVERAGE BENEFIT
PROGRAM ..................................................................................................... 65
DENTAL COVERAGE

Dental Coverage
65
OVERVIEW OF YOUR DENTAL COVERAGE
The Dental Benefit Program covers preventive dental care and corrective services. Except in certain select
markets where SIMNSA and Aetna Dental coverage options remain available, Delta Dental and Cigna are the
only dental coverage carriers under the Plan. You may choose from one of more of the following dental options,
available in your area:
As of January 1, 2023, the Plan’s dental coverage funding under the Delta Dental options is moving to a self-
insured model, with the following options:
• Bronze tier Delta Dental PPO, covering both in- and out-of-network care;
• Silver tier Delta Dental PPO, covering both in- and out-of-network care;
• Gold tier Delta Dental PPO, covering both in- and out-of-network care.
Please see the applicable Delta Dental Member Program Documents for more information on your specific
benefit coverage.
You may also have the option to enroll in coverage under the Cigna Platinum tier DHMO option, which covers
in-network care only. This option is only available in select markets, and coverage is not provided under this
option if you seek care outside of the network or do not get a proper referral. Eligible participants who choose
this option must also select an in-network primary care dentist upon enrollment and must receive a referral from
the primary care dentist to have any in-network dental specialist care covered.
• Platinum tier Cigna DHMO, covering in-network care only
You may choose dental coverage for yourself and your eligible dependents under the following coverage
levels:
You Only
You + Spouse/Domestic Partner
You + Child(ren)
You + Family
Your dental plan options that are not offered through Delta Dental are fully insured by an insurance carrier. The
separate Program Documents provided by the insurance carrier will govern the terms of the insured dental plan
options.
If you have any questions about the dental plan coverage available to you, or whether a specific provider or
procedure is covered under a dental plan option, please contact the Hilton Benefits Center or your carrier for
more information.
Delta Dental can be reached at 1.866.437.9880 and Cigna can be reached at 1.800.244.6224.

66
VISION COVERAGE
OVERVIEW OF YOUR VISION COVERAGE ............................................... 67
VISION COVERAGE

67
Vision Coverage
OVERVIEW OF YOUR VISION COVERAGE
Under the Plan, you can elect vision coverage as part of your overall health and wellness program for you and
your eligible dependents. Effective January 1, 2023, except in certain markets where VSP coverage options
remain available, EyeMed is the only accepted vision coverage carrier under the Plan.
You may choose from one of more of the following vision options, available in your area:
• Bronze
• Silver
• Gold
You may choose vision coverage for yourself and your eligible dependents under the following coverage levels:
You Only
You + Spouse/Domestic Partner
You + Child(ren)
You + Family
Your vision plan options are fully insured by an insurance carrier. The separate Program Documents provided
by the insurance carrier will govern the terms of the insured vision plans.
Here is a brief overview of your vision coverage levels. Individual carriers may offer coverage that differs
slightly from the standard coverage reflected here.
Bronze
Silver
Gold
Type of Plan
Exam-only
option that
provides certain
discounts
PPO that covers both in- and out-
of-network care
PPO that covers both in- and out-
of-network care
Payroll
Deductions
Lowest
Lower
Higher
In-network
In-network
Out-of-network
In-network
Out-of-network
Routine Vision
Exam (one per
plan year)
Covered at
100%
1
You pay $20
Up to $40
reimbursement
You pay $10
Up to $40
reimbursement
Frames (one
per plan year)
2
Discounts may
apply
$130 allowance
Up to $91
reimbursement
$200 allowance
Up to $140
reimbursement
Lenses (one
per plan year)
2
Discounts may
apply
You pay $20
3
Reimbursement
amount varies
by lens
You pay $10
3
Reimbursement
amount varies by
lens

Vision Coverage
68
Medically
Necessary
Contact
Lenses
Discounts may
apply
Covered in full
Up to $300
reimbursement
Covered in full
Up to $300
reimbursement
Elective
Contact
Lenses
2
Discounts may
apply
$130 allowance
Up to $91
reimbursement
$200 allowance
Up to $140
reimbursement
Contact
Lenses Fit and
Evaluation
Discounts may
apply
You pay $20
Up to $40
reimbursement
You pay $10
Up to $40
reimbursement
1
$40 reimbursement for exams received out-of-network.
2
Reimbursements can be used for lenses or elective contact lenses, but not both.
3
This applies to single vision, bifocal, trifocal, lenticular and standard progressive lenses. For additional lens options, you pay a
copay of $15 or more, depending on the option you choose.
If you have any questions about the vision plan coverage available to you, or whether a specific provider is
covered under the EyeMed coverage network, please contact the Hilton Benefits Center or EyeMed at
1.844.409.3401.

69
FLEXIBLE SPENDING ACCOUNTS
OVERVIEW OF YOUR FLEXIBLE SPENDING ACCOUNTS ....................... 70
A SNAPSHOT OF YOUR FLEXIBLE SPENDING ACCOUNTS ................... 70
HOW YOUR FLEXIBLE SPENDING ACCOUNTS WORK ........................... 71
What You Need to Do ............................................................................. 71
If You Terminate Employment ................................................................. 71
While You are on a Leave of Absence or Furlough ................................ 72
“Use-It-or-Lose-It” Rules.......................................................................... 73
When are Your FSA Funds Available? ................................................... 73
A Word About Taxes ............................................................................... 73
THE HEALTH CARE FSA .............................................................................. 74
Reimbursable and Non-Reimbursable Expenses ................................... 74
THE LIMITED USE HEALTH CARE FSA ...................................................... 75
THE DEPENDENT CARE FSA ...................................................................... 75
If You Are Married ................................................................................... 76
Eligible Dependents ................................................................................ 76
Reimbursable and Non-Reimbursable Expenses ................................... 76
APPLYING FOR REIMBURSEMENT ............................................................ 77
Health Care FSA Reimbursements ......................................................... 77
Dependent Care Reimbursements ......................................................... 78
Using Your Smart Choice Card ............................................................... 78
FLEXIBLE SPENDING
ACCOUNTS

70
Flexible Spending Accounts
OVERVIEW OF YOUR FLEXIBLE SPENDING ACCOUNTS
Hilton offers eligible Team Members a way to pay certain health care and dependent day care expenses with
pre-tax dollars through two types of Flexible Spending Accounts (the “FSAs”) — a Health Care FSA and a
Dependent Care FSA. As you read about the FSAs, keep the following in mind:
Each year at annual enrollment, you decide whether or not to use one or both of the FSAs and how much
to contribute during the upcoming year. Because your contributions are not considered taxable, you may
want to consider whether an FSA can reduce the amount you pay in taxes in an upcoming year.
You make contributions to your FSAs through authorized pre-tax salary deductions. These contributions
remain in your FSAs until you file an appropriate claim form for reimbursement or pay for health care
expenses using the Smart Choice Card (or until they are forfeited after the end of the year). After filing a
claim form, you are reimbursed for eligible expenses with tax-free dollars from the appropriate FSA.
If you have any money left in either FSA at the end of the year, you can submit claims incurred through
March 15 of the following year (the “grace period”) by April 30
th
to be reimbursed from the prior year’s
balance.
If, at the end of the year and its grace period, there are funds remaining in either FSA for which you do not
submit a timely claim form, you forfeit those amounts as required by Internal Revenue Service (IRS)
regulations.
A SNAPSHOT OF YOUR FLEXIBLE SPENDING ACCOUNTS
By using pre-tax dollars to pay certain eligible health care and dependent day care expenses, you may save
some taxes each year. Here is a snapshot of the Health Care and Dependent Care FSAs.
Health Care FSA Dependent Care FSA
Eligible Expenses Generally, medical, prescription
drug, dental, vision and hearing
expenses not eligible for
reimbursement from any other
source, but are otherwise tax
deductible
1
Eligible dependent day care
expenses you incur while you and
your spouse, if any, are at work
Qualified Dependents Your eligible dependents under the
Plan, whether or not they are
covered under the other health care
programs (excludes domestic
partners) of Hilton
A child under age 13
Any dependent that is incapable of
self-care that resides with you and
whom you claim as a dependent on
your tax return
1
If you elect a Limited Purpose FSA, only dental and vision expenses will be Eligible Expenses.

Flexible Spending Accounts
71
HOW YOUR FLEXIBLE SPENDING ACCOUNTS WORK
FSAs are reimbursement arrangements that allow you to pay for eligible expenses with amounts you contribute
to the accounts. Your contributions are deducted from your wages before Federal taxes are applied to your
wages. You can decide how much to contribute each year into the Health Care FSA or Dependent Care FSA.
The FSAs are administered by Alight.
• Note: amounts credited to your Health Care FSA may not be used to reimburse you for your
dependent care expenses, and amounts credited to your Dependent Care FSA may not be used
to reimburse you for your health care expenses. The Health Care FSA is for reimbursement of
eligible health care expenses for you and your eligible dependents, even if they are not covered
under the Plan; and
• The Dependent Care FSA is for reimbursement of eligible dependent care expenses for your
dependent children under age 13 to make it possible for you or your spouse to work. Under certain
circumstances, it may also be used to help pay for care of elderly parents, a disabled spouse or
dependent (dependents older than 13 must be incapacitated or in a day care facility).
What You Need to Do
To make the FSAs work for you, follow these steps:
Estimate your expenses
Consider your estimate carefully because you forfeit any unused amounts left in your FSAs under the IRS’s
“use-it-or-lose-it” rule.
Determine how much to contribute
After you decide on the annual dollar amount (subject to each FSA’s maximum) for your estimated
expenses, you will make a separate election for each FSA.
Incur expenses
The FSAs reimburse enrolled participants for eligible expenses they or their dependents incur during the
Plan year (January 1 through December 31) and until the following March 15 (the “grace period”).
Receive reimbursement
You can use your Health Care FSA to pay for eligible health care expenses by using your Smart Choice
Card or by seeking reimbursement for expenses you paid directly. For eligible dependent day care
expenses, you must pay the service provider and then seek reimbursement from your Dependent Care
FSA. See “Using Your Smart Choice Card” at the end of this FSA Section for more information about the
Smart Choice Card.
If You Terminate Employment
For the Health Care FSA, only the expenses incurred while you are an active Employee and contributing to the
FSA are eligible for reimbursement, unless, with respect to the Health Care FSA only, you continue your
participation through COBRA. (See “Medical Coverage Continuation Rights” in the “Participation” section of
this SPD for more details.)
If you terminate employment and are rehired within the same year, special rules apply to your new Health Care
FSA contributions. If when you terminated you had received reimbursements totaling more than you
contributed for the year, any new contributions made when you are rehired will first be used to reimburse the
Plan for the excess payments made to you earlier in the year.

Flexible Spending Accounts
72
If you terminate employment with Hilton and are immediately hired by either of the other employers
participating in this Plan, you will not be treated as having terminated employment for purposes of the Plan.
While You are on a Leave of Absence or Furlough
If you go on a paid leave of absence, you continue participating in the FSAs, as described in the
following chart.
If you take a paid leave
of absence…
During the leave…
Health Care FSA
Contributions- will continue
Claims- will continue to be reimbursed
Dependent Care FSA
Contributions: will continue
Claims- can continue to be reimbursed for services incurred up to your last day
worked in the Play Year (immediately prior to your unpaid leave) and up to the
contribution amount already in the DC FSA. Claims incurred while on leave will not
be reimbursed.
When you return to
work
When you return to work within the same Plan Year, your contributions will
continue.
If you go on an unpaid leave of absence, the FSAs are handled differently for the two accounts, as
described in the chart below.
If you take an unpaid
leave of absence…
During the leave…
Health Care FSA
Contributions- will be suspended. You may have the opportunity to elect COBRA
continuation coverage and make after-tax payments.
Claims- will continue to be reimbursed
Dependent Care FSA
Contributions: will be suspended.
Claims- can continue to be reimbursed for services incurred up to your last day
worked in the Play Year (immediately prior to your unpaid leave) and up to the
contribution amount already in the Dependent Care FSA.
Claims incurred while on leave will not be reimbursed.
When you return to
work
When you return to work within the same Plan Year, your participation and/or
required contributions will resume, except as described below. You can choose to:
• Reinstate your per pay period deduction amount (which may result in a
lower total contribution amount for the Plan Year), or
• Adjust your per-pay-period deduction to meet your elected annual
contribution (which may result in a higher contribution amount deducted
per pay period)
Note: Any Smart Choice Card will be deactivated during an unpaid leave.
If you begin your leave of absence in one plan year and return in a later plan year, you must make new FSA
elections within 31 days of your return to work.

Flexible Spending Accounts
73
“Use-It-or-Lose-It” Rules
Tax laws require that all amounts that you contribute to your FSA during the year be used to reimburse eligible
expenses that you incur during the same year. If you overestimate your expenses, the tax laws require that
any unused pre-tax contributions be forfeited.
As an exception to this requirement, the FSAs offer a grace period that automatically extends the coverage
period of all participants who are covered on the last day of the Plan year (December 31). You have until
March 15 of the new year to incur claims for reimbursement from your prior year’s FSA. Any claims or provider
payments that cover expenses incurred during the grace period will be automatically paid out of the prior Plan
year’s account first and then, when that account balance is exhausted, the new Plan year account.
You have until April 30 of the next year to submit claims for reimbursement from your FSAs for eligible
expenses incurred between the previous January 1 and December 31 and during the grace period. Once this
deadline passes, you will forfeit any balance remaining in your FSA after all proper claims have been submitted
and paid.
When are Your FSA Funds Available?
For the Health Care FSA, you are entitled to reimbursement for eligible expenses for the full amount of your
annual election as of your first day of coverage. You will continue to be reimbursed for eligible expenses until
your total reimbursements equal the annual amount you elected to contribute to your Health Care FSA.
The uniform coverage rule does not apply to your Dependent Care FSA. As you submit claims for eligible
expenses, you will be reimbursed for all proper claims up to the actual amount that is credited to your
Dependent Care FSA when the claim is received. If the balance in your Dependent Care FSA is less than the
amount of a claim, the claim will be held and reimbursed after additional contributions sufficient to cover the
claim have been credited to your Dependent Care FSA.
A Word About Taxes
FSA contributions reduce your taxable income – meaning you pay less in taxes. Your FSA contributions, as
well as the money reimbursed to you, are not subject to:
Federal income taxes
Social Security (FICA) taxes
In most cases, state and local income taxes
1
Note: Rules vary, and state and local tax laws are subject to frequent change. You may wish to consult with
your own tax advisor regarding the tax aspects of the FSAs.
Note: If you receive back-up care subsidies in a calendar year by using the Back-Up Care Advantage Program
(when combined with your annual Dependent Care FSA election) over the annual $5,000 tax free limit allowed
by the Internal revenue Service, you will have imputed income reflected in a later paycheck after the back-up
care has been provided. The amount of imputed income will be the amount in excess of the $5,000 limit.
1
Not applicable to employees in New Jersey.

Flexible Spending Accounts
74
THE HEALTH CARE FSA
Reimbursable and Non-Reimbursable Expenses
Generally, the Health Care FSA reimburses you for many, but not all, health care expenses that are tax
deductible. However, you cannot be reimbursed from the Health Care FSA for expenses you claim as a
deduction on your tax return, nor can you be reimbursed for the portion of the expenses that are paid by any
health plan that covers you or your family. Not all expenses that are considered tax deductible are eligible for
reimbursement under the Health Care FSA. In general, you can receive reimbursement for expenses incurred
for medical care, which includes amounts paid for the diagnosis, cure, mitigation, treatment or prevention of
disease.
However, note that you may only submit expenses for your domestic partner if your domestic partner qualifies
as your dependent and satisfies the requirements of a Qualifying Relative. See “Domestic Partners: Tax
Implications and Other Information” in the “Participation” section of this SPD for more information.
Remember that, except in the event you elect to continue your participation in the Health Care FSA through
COBRA upon a qualified event, you must be contributing to your Health Care FSA in order to be eligible to be
reimbursed for covered expenses. For example, if you stop contributing to your Health Care FSA due to a
change in status event but are still covered as a Team Member under other benefits offered under the Plan,
you will not be eligible to receive reimbursements from your Health Care FSA for expenses incurred after the
date you stop contributing to the Health Care FSA. To learn more, contact Smart Choice at the number set
forth in the General Information section.
The following chart identifies just some examples of eligible and ineligible expenses. Other expenses not listed
below may or may not be eligible for reimbursement. For those participating in the general purpose Health
Care FSA, expenses incurred on or after January 1, 2020 for over-the-counter drugs or medicines will no
longer need a prescription to be reimbursed from your Health Care FSA. Also, menstrual products (i.e.,
tampons, liners, and similar products) will be considered a medical care expense eligible for reimbursement
from your Health Care FSA (subject to all other requirements, such as substantiation).

Flexible Spending Accounts
75
Health Care FSA Reimbursable Expenses Health Care FSA Non-Reimbursable Expenses
Insurance deductibles and copay for office visits and
prescriptions
Charges that exceed reasonable and customary
limits
Acupuncture if treating a medical condition
All out-of-pocket non-cosmetic dental expenses not
covered by a benefit plan
Hearing care expenses, including those for
examinations and hearing aids, if not covered under
the medical program or other source
Vision care expenses such as examinations,
treatments, eyeglasses and contact lens expenses
and laser eye surgery not covered by a benefit plan
Weight loss treatment (with the exception of food
costs) associated with a diagnosed disease or
ailment such as obesity or hypertension, prescribed
by your doctor
Expenses for medical treatments and procedures that
are not covered by insurance
Drugs available through prescription only and not
covered by the medical program and not used for
cosmetic purpose
Over-the-counter medicines and drugs purchased to
alleviate or treat physical injury or illness (such as
antacid medicine, allergy medicine, pain reliever and
cold medicines, and menstrual products), but not
medicines merely beneficial for general health
Insulin purchased without a prescription
Cosmetic treatment or drugs (unless prescribed to treat
a congenital defect or accident reconstruction),
including:
Hair loss treatments or transplants
Face lifts
Piercings
Teeth whitening
Health club memberships or exercise classes to
promote general health
Household help (even if recommended by your
doctor because you are unable to do housework)
Individual or group health or dental insurance
premiums
Nutritional supplements, vitamins, herbal
supplements or “natural medicines,” which are
merely beneficial to general health
Weight loss programs or medications to promote
general health
THE LIMITED USE HEALTH CARE FSA
The Limited Use Health Care FSA is designed for you if you participate in a high deductible health plan and
want to contribute to a health savings account (HSA). The Limited Use Health Care FSA is subject to the same
contribution and eligibility requirements that apply to the Health Care FSA. However, the Limited Use Health
Care FSA will only reimburse you for dental and vision care expenses not covered by the Plan.
THE DEPENDENT CARE FSA
You can use the Dependent Care FSA to pay for some or all of the expenses you incur for the care of a child or
adult dependent who resides with you and is incapable of self-care while you work. However, to qualify as an
eligible expense, all of the following must be true:
Care for your dependent(s) must be necessary for you and your spouse, if any, to work, look for work, go
to school full-time, or if your spouse, who lives with you, is incapable of self-care as defined by the IRS. In
other words, expenses are not eligible if they are for services provided while you are out for the evening
socially or on vacation.

Flexible Spending Accounts
76
If the care is provided by a day care facility that cares for six or more individuals at the same time, the
facility must be licensed and comply with all federal, state and local regulations governing day care
centers.
Your care provider is anyone other than the child’s parent or a person whom you claim as a dependent on
your federal income tax return (a relative who provides care must be at least age 19). In addition, you
must provide your caregiver’s name, address and Social Security number or taxpayer identification number
when you file for reimbursement. You also must provide this information on your federal income tax return,
unless your caregiver is a church or other religious organization.
If You Are Married
Under federal law, if you participate in the Dependent Care FSA and your spouse participates in a similar
account through his or her own employer, your combined contributions to both accounts in a calendar
year may not exceed $5,000 (a lesser limit may apply to highly compensated employees). This limit applies
regardless of the number of dependents receiving care. If you and your spouse file separate income tax
returns, the most each of you may contribute is $2,500. In addition, your Dependent Care FSA contributions
may not exceed the annual income of the lower-paid spouse, if that amount is smaller than the benefit limits
indicated above.
In general, you may not participate in the Dependent Care FSA if your spouse does not work outside the home.
There are two exceptions: if your spouse does not work outside the home and is physically or mentally unable
to care for himself or herself, or if he or she is a full-time student. In either of these cases, for purposes of
calculating the contribution limit, the IRS considers your spouse’s earned income to be:
$250 a month ($3,000 a year) if you have one dependent
$500 a month ($6,000 a year) if you have two or more dependents
If you participate, it is your responsibility to comply with the federal limits.
Eligible Dependents
An eligible dependent is a child younger than age 13 whom you claim as a dependent on your income tax
return. An eligible dependent can also be an older dependent who:
Depends on you for at least half of his or her support;
Has the same principal residence as you for more than one-half of the taxable year; and
Is physically or mentally unable to care for himself or herself.
Your dependent may be a spouse, an elderly parent, or any other relative or dependent, as long as he or she is
incapable of self-care and meets all of the above requirements.
Reimbursable and Non-Reimbursable Expenses
Similar to the Health Care FSA, the Dependent Care FSA reimburses you for dependent day care expenses so
that you and your spouse, if any, may work or attend school full time.
The following chart identifies just some examples of eligible and ineligible expenses. Other expenses not listed
below may or may not be eligible for reimbursement. To learn more, contact Smart Choice at the number set
forth in the General Information section.
Flexible Spending Accounts
77
Dependent Care FSA Reimbursable Expenses Dependent Care FSA Non-Reimbursable Expenses
Dependent care provided in your home, including
care provided by a babysitter or housekeeper. The
provider may be a relative (provided he or she is
not the child’s parent or your child under age 19,
your spouse or any other person whom you claim
as a dependent on your federal tax return)
Care provided in a neighbor’s home or in a
licensed day care center, provided your dependent
regularly spends at least eight hours a day in your
home
Before- and after-school programs for children
under age 13
Day camp services for children under age 13, but
not overnight camp
Preschool expenses for pre-kindergarten and
below
Transportation provided by the day care provider
Care provided in 24-hour nursing care facilities
Expenses you claim as an after-tax dependent day
care tax credit on your federal income tax return, or
expenses paid by any similar reimbursement plan
Expenses to attend kindergarten or beyond
Services provided by a child’s parent, your spouse,
your child under age 19, or someone you or your
spouse claim as a dependent on your tax return
Payments to a housekeeper while you are home
from work because of illness
Child or dependent day care provided while:
You are on a leave of absence from work
You are at work and your spouse is doing
volunteer work (or vice versa), even if a nominal
fee is paid
You and your spouse are doing volunteer work
(even if a nominal fee is paid)
You or your spouse is not working (such as
weekend or evening babysitting fees)
Transportation expenses to and from the care site
(unless the transportation is furnished by the
provider)
Expenses for overnight camp
Expenses for food, clothing and entertainment of a
qualified dependent, unless charges are incidental
and cannot be separated easily from the overall
dependent day care cost
APPLYING FOR REIMBURSEMENT
Reimbursement from either FSA is available only after the service for which you are seeking reimbursement is
performed and you receive reimbursement from all other sources. As described above, you can pay for eligible
health care expenses by using your Smart Choice Card or by seeking reimbursement for expenses you paid
directly. For eligible dependent day care expenses, you must pay the service provider and then seek
reimbursement from your Dependent Care FSA.
Health Care FSA Reimbursements
You may use your prepaid Smart Choice card (Smart Choice Card) to pay for eligible health care expenses,
which means you do not have to submit a claim for reimbursement for certain approved merchants (see the
section below titled “Automatic Validation with Approved Merchants” for more details). If you participate in the
Limited Use Health Care FSA, this will be the same Smart Choice card used to pay eligible expenses from the
HSA.
Supporting Documentation
Along with the claim form, submit the appropriate supporting documentation, such as:

Flexible Spending Accounts
78
• The explanation of benefits (EOB) from the insurance company
• An itemized bill for services not covered by insurance, including the name of the service provider, cost of
the service, patient name, description of the services rendered and date of service
• Receipts for any medications and copays
• Copies of any prescriptions if the receipt for the medication does not include an Rx number. This applies to
over-the-counter drugs and medicine as well. No reimbursement will be provided for an over-the-counter
drug without a prescription or Rx number.
Dependent Care Reimbursements
For Dependent Care FSA claims, only your current account balance is available to reimburse claims. If the
dependent day care services exceed your account balance, you receive a partial reimbursement. You receive
the unreimbursed portion of the claim as you make additional contributions to your Dependent Care FSA.
Supporting Documentation
When you seek reimbursement, please submit:
Your provider’s bill or itemized receipt; and
Your dependent day care provider’s name, address, and Social Security or federal tax identification
number
Signed provider certification on the Smart Choice claim form along with dependent day care provider’s
name, address, and Social Security or federal tax identification number.
Using Your Smart Choice Card
You may use your prepaid Smart Choice card (Smart Choice Card) to pay for eligible health care expenses if
you’ve chosen to contribute to your Health Care FSA.
Dependent care expenses aren’t eligible for reimbursement through the Smart Choice Card program.
If you elect to contribute to a Health Care FSA, you will receive a package containing one Smart Choice Card
issued in your name, activation instructions, a cardholder agreement, additional disclosures, and information
explaining approved use of the card.
The Smart Choice Card remains active for up to three years as long as your Health Care FSA is in good status,
you consecutively re-enroll in the Health Care FSA, and you remain actively employed. Your card will be
cancelled upon termination of employment—inactive participants may not use the Smart Choice Card. By
signing and using the card, you certify that:
You will only use the card for your own eligible health care expenses and those of your eligible dependents
under the Health Care FSA.
Incurred expenses were for health care services or supplies purchased on or after the date your Health
Care FSA took effect.
Your expenses don’t include any amounts that are otherwise payable by plans for which you or your
dependents are eligible.

Flexible Spending Accounts
79
Any expense paid with the card has not been, or will not be, reimbursed by another source.
You can present your Smart Choice Card for eligible health care expenses anywhere Debit VISA cards are
accepted.
Important: Save your itemized receipts
Because all Smart Choice Card transactions must be verified as eligible health care expenses, you may be
required to provide the Plan with supporting documentation to validate your expenses. Make sure that you save
all of your itemized receipts (indicating the date of service, the name of the service provider, the name of the
person receiving service, the name of the product or service, and any amount paid by other coverage).
After the end of any given year, expenses incurred in the prior Plan year (plus the grace period) can be
submitted via the manual claim process through April 30. If you re-enrolled, your balance on the Smart Choice
Card will be updated to your new election amount on January 1. Smart Choice Card transactions that are not
automatically validated will apply toward the new Plan year balance until additional documentation is provided
and the claim is approved.
Automatic Validation with Approved Merchants
When you purchase eligible health care items by using your Smart Choice Card with approved merchants, your
transaction may be validated automatically without having to provide an itemized receipt or supporting
documentation. For a complete listing of eligible expenses and approved merchants, visit the Smart Choice
Web site. Please note that the listing is subject to change at any time.
Automatic Validation for Other Medical Providers
Your Smart Choice Card can also be used for other types of health care transactions without the need for
submission of itemized receipts or further review. These transactions include recurring expenses, copayments
and specific merchant category code. Below is a brief explanation of each type of transaction.
Recurring Transactions
If you purchase an eligible health care item or service using your Smart Choice Card, that same item or service
will be validated automatically the next time you purchase it with your Smart Choice Card (at the same provider
and for the same dollar amount). Your Smart Choice Card will be programmed to recognize your plan’s
copayment amounts without any additional validation being required (for example, a $25 copayment at a
physician’s office).
Supporting Documentation
Manual claim submission and supporting documentation are required for the purchase of any prescription drug
or health care service or item that isn’t validated automatically. These types of purchases are conditionally
reimbursed, pending validation of the expenses. You will be sent a letter or email informing you that itemized
receipts or other documentation are required to validate the Smart Choice Card transaction. Expenses for
which you don’t provide adequate documentation are considered ineligible and treated as overpayments. See
the Overpayment Process section for more information. You are responsible for retaining receipts or
documentation to support reimbursement.
Limited Use Health Care FSA Expenses
When you use your Smart Choice card to pay for eligible expenses, your Limited Use Health Care FSA account
will reimburse you first, if the expense is for dental or vision care. If the eligible expense is for medical care, the
reimbursement will come from your HSA. This will happen automatically.

Flexible Spending Accounts
80
Overpayment Process
If you purchase products or services with your Smart Choice Card that are ineligible for reimbursement through
your Health Care FSA, you will receive notification from Smart Choice that your transaction has been deemed
an overpayment. This notification will be sent by email, so be sure that the Hilton Benefits Center has your valid
email address.
Once an overpayment has been identified, the following actions will be taken immediately:
Your Smart Choice Card will be suspended and will remain suspended when your overpayment exceeds
$100.
If you provide the required validation documentation, the overpayment(s) will be cancelled and any claim(s)
applied to offset the overpayment will be applied to the appropriate Plan year.
Future paper claims will be processed, and eligible amounts will be applied to the outstanding
overpayment. Payment will not be made on any paper claim until the overpayment has been fully repaid.
You will be notified that you must refund the overpayment by mailing a check to Smart Choice.
Smart Choice will allow you to resolve an overpayment on your account in one of the following ways. You
will be given the option to:
Resubmit your claim with additional information;
Submit a new claim; or
Repay your overpayment by repaying online, the Reimbursement mobile application, or mailing a
check to Smart Choice.
The overpayment will remain active on the account until all amounts are recovered. If the overpayment amount
isn’t recovered through the options above, Hilton will determine whether further action should be taken.
When Not to Use Your Smart Choice Card —Coinsurance
If you enrolled in a plan that has coinsurance and you visit your doctor, wait until after your doctor submits a
claim to your health plan to pay for any coinsurance using your Smart Choice Card. Doctors often have
negotiated reduced rates, so using your Smart Choice Card at the time of service may result in an
overpayment. Once your health plan pays its portion of the claim, your doctor will bill you for your portion. At
that time, you may use your Smart Choice Card to pay your portion of the bill. Remember to save your receipt
in case it is requested.
Prior year balances are available on your Smart Choice card until the grace period. Card transactions during
the plan year run-out automatically applies to the prior year balance first.

81
EMPLOYEE ASSISTANCE PROGRAM
OVERVIEW OF THE EMPLOYEE ASSISTANCE PROGRAM ..................... 82
ACCESSING SERVICES ............................................................................... 82
AVAILABLE SERVICES ................................................................................. 82
EMPLOYEE ASSISTANCE
PROGRAM

82
Employee Assistance Program
OVERVIEW OF THE EMPLOYEE ASSISTANCE PROGRAM
The Employee Assistance Program (EAP)offered through Lyra Health, is available at no cost to you. Lyra
provides a network of therapists and coaches with expertise in a variety of specialties, such as
child/adolescent care and substance use disorder. Online scheduling is available to help you get you
connected to care quickly.
ACCESSING SERVICES
If you are a full-time regular U.S. Team Member, you and your eligible dependents (spouse/domestic partners
and dependents up to age 26) may utilize the EAP services immediately upon employment . If you are a
regular U.S. part-time Corporate Team Member hired on or after October 1, 2024, you are eligible for the
Employee Assistance Program, following a 90-day waiting period. If you are a U.S. part-time Corporate Team
hired before October 1, 2024, you are eligible for the Employee Assistance Program effective October 1,
2024.You and your eligible dependents can access Lyra by phone or the Internet 24 hours a day, 7 days a
week. Call 877-848-7910 or visit lyrahealth.com/Hilton.
AVAILABLE SERVICES
You and your family members are each eligible for up to eight (8) free face-to-face or virtual sessions per Plan
year with experienced therapists or coaches. Participants in a Hilton medical plan through Anthem or Cigna
have the option to continue care with their Lyra provider beyond eight visits through their medical plan
coverage and applicable cost share.
The eight face-to-face or virtual counseling or coaching sessions offered through the EAP are available
separately and apart from any mental health or other related benefits that may be available under the Plan.
Self-help tools are available to support your ongoing mental wellbeing. You can access an extensive digital
library of self-guided skill-building resources on topics such as stress, sleep, relationships, and parenting. You
also can create a guided self-care plan, with self-paced activities and feedback from a coach.

83
International Business Travel Program
OVERVIEW OF THE INTERNATIONAL BUSINESS TRAVEL
PROGRAM ..................................................................................................... 84
ACCESSING SERVICES ............................................................................... 84
MEDICAL SERVICES .................................................................................... 84
SAFETY AND SECURITY ADVICE ............................................................... 85
INTERNATIONAL BUSINESS
TRAVEL PROGRAM

84
International Business Travel Program
OVERVIEW OF THE INTERNATIONAL BUSINESS TRAVEL PROGRAM
The International Business Travel Program provides assistance to you when you are traveling outside your
home country if you have a medical question or concern, medical emergency, safety concern, security
emergency, or if you require travel assistance. The International Business Travel Program provides services 24
hours a day, 365 days a year, worldwide. The International Business Travel Program offers services at no cost
to you.
ACCESSING SERVICES
You may utilize the International Business Travel Program services immediately upon employment if you are
an eligible Team Member of Hilton. Expats and employees traveling with their immediate family (spouse and
dependents) on company paid and approved travel may access services for their immediate family members.
Before you travel, you can access real-time information by following these steps:
• Download the Global Guardian App onto your mobile phone
• Call an alarm center for pre-travel information.
While you are out of the country, if you need medical or security advice or assistance, you may access services
24 hours a day, 7 days a week, by any of the following methods:
• Use the Global Guardian app
• Call the Operations Center closest to you:
United States: (703) 485-2999
United Kingdom +44 (20) 3827-7779•
Singapore +65 6971-6262
MEDICAL SERVICES
Global Guardian offers a wide range of medical services and provides support in many languages. Contact
Global Guardian while you are traveling for any of the following services:
• If you need health or safety advice at any time;
• If you are ill or injured and need advice on whether you should visit a doctor;
• If you need a referral or help with doctor or hospital appointments;
• If you require supplies of medication or equipment;
• If you need to arrange an ambulance;
• To pay medical fees when approved;
• To monitor your condition and advise on your condition;
• To evacuate you to a center of medical excellence;

85
• To evacuate you to a safe area;
• To help with your family; or
• To deal with a fatality.
SAFETY AND SECURITY ADVICE
Global Guardian also offers safety and security advice. Global Guardian will answer questions regarding safety
in particular regions (for example, “Is it safe to leave my hotel for a coffee?”). Global Guardian will provide
services in a security emergency (for example, “There are rioters outside my hotel!”). Global Guardian will also
provide travel assistance (for example, “I’ve been pick-pocketed”).

86
Medical Benefits While Abroad
OVERVIEW OF THE INTERNATIONAL ASSIGNEE PLAN ......................... 87
OVERVIEW OF THE MEDICAL BENEFITS ABROAD PROGRAM ............. 87
ACCESSING SERVICES ............................................................................... 87
MEDICAL SERVICES .................................................................................... 87
MEDICAL BENEFITS
WHILE ABROAD

87
Medical Benefits While Abroad
OVERVIEW OF THE INTERNATIONAL ASSIGNEE PLAN
International Assignee Plan is comprehensive health coverage, including medical, prescription drug, vision and
dental. It also includes International Employee Assistance Program, telehealth and evacuation and assistance
services. Please see program documentation for more information.
OVERVIEW OF THE MEDICAL BENEFITS ABROAD PROGRAM
The Medical Benefits Abroad Program provides emergency medical benefits to you and your Eligible
Dependents when you are traveling outside your country of residence on business if you have a medical
emergency. The Medical Benefits Abroad Program offers these emergency care services at no cost to you.
ACCESSING SERVICES
You may utilize the Medical Benefits Abroad Program emergency services in accordance with the timing listed
in the “Participation” section if you are:
• an eligible Team Member of Hilton who is classified by Hilton as full-time;
• you normally work thirty (30) or more hours per week and are actively at work; and
• you are traveling outside the country of your residence or permanent assignment for no more than 180
consecutive days per trip on business of or at the expense of Hilton.
While you are out of the country, if you need emergency medical services or security advice or assistance, you
may access services 24 hours a day, 7 days a week, by contacting the number on your benefits identification
card.
MEDICAL SERVICES
Medical Benefits Aboard offers emergency medical services such as hospitalization, physician services,
outpatient facilities, etc. as set forth in the Program Documents. The Medical Benefits Abroad Program benefits
are fully insured by an insurance carrier. The separate Program Documents provided by the insurance carrier
will govern the terms of the insured Medical Benefits Abroad Program.

89
Legal Services
OVERVIEW OF THE LEGAL SERVICES BENEFIT PROGRAM
The ARAG Legal Plan provides voluntary legal services for you, your spouse or domestic partner and your
dependents. You pay 100% of the cost of services.
For more information about the services provided by ARAG, and to access relevant Program Documents, go to
ARAGLegal.com/Hiltoninfo (click on “Member Login” and “Create Account”). You can also call the customer
service center at 1-800-247-4184.
The Legal Services Benefits Program is not sponsored or endorsed by Hilton and is not subject to ERISA.

90
DISABILITY COVERAGE
OVERVIEW OF YOUR DISABILITY COVERAGE ........................................ 91
Evidence of Insurability (EOI) .................................................................. 91
Basic Weekly and Monthly Earnings ....................................................... 91
A SNAPSHOT OF YOUR DISABILITY COVERAGE .................................... 92
SHORT-TERM DISABILITY ........................................................................... 93
Eligibility for STD Coverage .................................................................... 93
Eligibility for STD Benefits ....................................................................... 93
Amount of STD Benefits .......................................................................... 94
Duration of STD Benefits......................................................................... 94
LONG-TERM DISABILITY ............................................................................. 95
Eligibility for LTD Benefits ....................................................................... 95
Covered Disabilities and Elimination Period ........................................... 95
Amount of LTD Benefits .......................................................................... 96
Duration of LTD Benefits ......................................................................... 96
Recurring Disabilities ............................................................................... 97
Survivor’s Benefit .................................................................................... 97
Recovery of Overpayments ..................................................................... 97
DISABILITY COVERAGE

91
Disability Coverage
OVERVIEW OF YOUR DISABILITY COVERAGE
Corporate Team Members receive short-term disability benefits through their Employer’s salary continuation program
and may have other options in lieu of the Optional STD Buy-Up. If you have a question as to whether you are a
corporate or non-corporate Team Member, please check with your HR team. If you are a Corporate Team Member,
contact the HRX Team to request a copy of the salary continuation Program Document for more details.
Note: The salary continuation program is not subject to ERISA.
If you become disabled from a non-work-related injury or illness and can’t work, the Plan helps you meet the
challenge by offering two disability coverages: short-term disability (STD) (salary continuation for Corporate
Team Members) and long-term disability (LTD). As you read about these coverages, keep the following in
mind:
After you have satisfied the eligibility waiting period, you must be capable of active work on the first
day that disability coverage would become effective. If you are not capable of active work on the day
that coverage would otherwise become effective, then the coverage will not start until you are capable
of active work.
If you are on a leave of absence and elect to increase the amount of your disability coverage, the new
coverage amount will not take effect until you are actively at work. See the “Coverage During Unpaid
Absences” section in the Participation chapter for more details on when election changes take effect.
Evidence of Insurability (EOI)
If you elect coverage under the optional STD Buy-Up or optional LTD when you are first eligible, you will not
have to satisfy any EOI requirements. However, if you elect optional coverage at any later date, you will have
to satisfy the insurance company’s EOI requirements. EOI requires you to provide a statement of your medical
history that the insurance company will use to determine if you are approved for coverage.
Consult your Program Documents for the EOI rules that apply to the coverages you’ve chosen.
Basic Weekly and Monthly Earnings
Although the STD benefit is based on “basic weekly earnings” and the LTD benefit is based on “basic monthly
earnings”, both benefits actually base these calculations on the same annual earnings figure.
Your annual earnings figure will be updated once annually and communicated to you at annual enrollment.
The amount will be effective for benefits purposes starting the next January 1
st
. This figure will remain constant
throughout the year even if your earnings change during the year. For example, if your annual enrollment
materials indicate that your annual earnings are $26,000 per year (which would be $500 per week or $2,000
per month) in 2023, your disability benefits for 2024 will be based on annual earnings of $26,000, even if your
actual annual earnings at the time of your disability in 2024 are higher or lower than $26,000.

Disability Coverage
92
A SNAPSHOT OF YOUR DISABILITY COVERAGE
Here’s a snapshot of your disability benefits.*
Feature Duration Amount of Benefit
Basic STD***
Provides a portion of your
income if you become
temporarily disabled due
to a non-work related
illness or injury
Length of disability up to
26 weeks
60% of basic weekly
earnings, less any
deductible sources of
income up to $250 per
week**
Optional STD Buy-Up Provides a higher portion
of your income during the
STD period. Note: In some
cases where state
mandated temporary
disability benefits are
higher, there may be
little/no additional
coverage available from
the STD Buy-Up.
Length of disability up to
26 weeks
60% of basic weekly
earnings, less any
deductible sources of
income up to $2,308 per
week (Basic and Buy-Up
combined)***
LTD
Provides a portion of your
income if your disabling
illness or injury lasts
longer than the STD
period
Begins after 180 days and
continues for length of
disability up to age 65 or
the Social Security
retirement age generally
Option 1 – 50% of basic
monthly earnings, less any
deductible sources of
income, up to $3000 per
month
Option 2 - 60% of basic
monthly earnings, less any
deductible sources of
income, up to $20,000 per
month
*Additionally, you may be eligible for Social Security benefits for your disability. Contact your local Social Security
office for more detailed information. Also, if you are disabled under the LTD program, the Claims Administrator can
offer assistance with your application for Social Security disability benefits or appeal. Please contact the Claims
Administrator (at the address and phone number in the General Information section) for more information if you would
like this assistance.
**The amount of the STD benefit for Corporate Team Members and Team Members in certain states with statutory
short-term disability benefits may vary. For information on the amount of your STD coverage, see the Corporate
Team Members’ Handbook.
***Corporate Team Members receive short-term disability benefits through their Employer’s salary continuation
program and may have other options in lieu of the Optional STD Buy-Up. If you have a question as to whether you
are a corporate or non-corporate Team Member, please check with your HR team. If you are a Corporate Team
Member, contact the HRX Team to request a copy of the salary continuation Program Document for more details.

Disability Coverage
93
SHORT-TERM DISABILITY
Under the STD program, a disability is considered short-term if it lasts for 26 weeks or less. If it lasts for more
than 26 weeks and you purchased LTD coverage, you may become eligible to receive long-term disability
benefits, which are described later in this section.
Eligibility for STD Coverage
Depending on where you work, you may be eligible to participate in either the Basic STD or a state mandated
short-term disability program. Regardless of which program covers you, coverage is provided automatically. In
some states a mandatory employee contribution is required for state mandated STD coverage. In addition, you
may be eligible to increase your STD coverage level by participating in the STD Buy-Up program.
Basic STD
You are eligible to participate in the Basic STD program if you meet the eligibility requirements described in the
“Participation” section of this SPD and do not work in one of the following states: California, New Jersey, New
York or Rhode Island. This section describes the benefits under the Basic STD program. If you are a
Corporate Team Member, your STD benefits may vary.
If you have a question as to whether you are a corporate
or non-corporate Team Member, please check with your HR team.
State Mandated Benefits
Some states have state mandated short term disability programs. If you work in these states, please contact
your HR representative for more information on how to obtain short-term disability benefits under your state’s
program.
STD Buy-Up
You may purchase additional STD coverage under the optional STD Buy-Up program if:
You participate in:
The Basic STD program; or
A state-mandated short-term disability insurance program and are otherwise an eligible Employee (see
“Eligibility” in the “Participation” section of this SPD for more details); and
Your annual earnings are at least $10,833. Note that some state mandated coverages may have different
base salary limits that may impact whether or not you can elect STD Buy-Up and/or the value of such
additional coverage. Please contact the appropriate state agency for more information.
Corporate Team Members are eligible to participate in the Salary Continuation Plan, rather than STD Buy-
Up. You should review Hilton’s Salary Continuation Plan document if this benefit applies to you.
Eligibility for STD Benefits
Covered Disabilities and Elimination Period
Before you can qualify for Basic STD and STD Buy-Up benefits, you must be “disabled” (defined below) for
seven consecutive days because of a non-work related covered injury or sickness. This seven-day period is
referred to as the “elimination period” and begins on the day you become disabled. Please refer to the Program
Documents provided by the insurance carrier for more information on the insurance carrier’s requirements for
determining whether a covered person is “disabled”, as well as for a list of excluded disabilities. If you work in

Disability Coverage
94
California, New Jersey, New York or Rhode Island, you will be considered “disabled” in accordance with your
state’s disability benefit program.
Physical Examination
The Claims Administrator, at its expense, may require you to undergo a physical examination if you submit a
claim for STD benefits or while you are receiving STD benefits. If you refuse to be examined, the Claims
Administrator may deny your claim or terminate your benefits.
Amount of STD Benefits
If you are eligible for STD benefits, the STD program pays the following:
Basic STD Coverage. You receive 60% of your basic weekly earnings minus amounts from other
deductible sources of income. The maximum benefit is $250 per week for up to 26 weeks. If you work in
California, New Jersey, New York or Rhode Island, your STD benefits are paid at the level provided under
the state-mandated short-term disability insurance plan that covers you. Corporate Team Members’
disability benefits may vary. See the Corporate Team Member handbook for more information.
STD Buy-Up Coverage. You receive 60% of your basic weekly earnings minus amounts from other
deductible sources of income. The maximum benefit is $2,308 per week for up to 26 weeks (Basic and
Buy-Up combined; or, if applicable, state-mandated benefits and Buy-Up combined). Corporate Team
Member may have other options in lieu of the STD Buy-Up coverage.
If you are covered under the state-mandated benefits provided in New York, California, New Jersey or Rhode
Island, it is your responsibility to file with the state for any state-mandated benefits due to you. If you do not file
for such state-mandated benefits and you receive benefits under STD Buy-Up, your STD Buy-Up coverage
benefits will be reduced by the amount you would have received under the state-mandated disability program.
Your STD benefit amount will be reduced by any disability income benefits you may receive under any state
compulsory benefit act or law. This minimum benefit may be applied to any overpayment that results, for
example, from an error in processing your benefit amount. Your STD benefit amount will not be reduced by
income from profit sharing, thrift, 401(k), Keogh, employee stock option, and tax-sheltered annuity plans.
Working While Disabled
If you are eligible to receive STD benefits, but return to work after satisfying the elimination period, you may still
receive some benefits. See the Program Documents issued by the insurance carrier for more details.
If you have any questions regarding the amount of your STD benefits, please contact:
If you work in California, New Jersey or Rhode Island, the appropriate state agency.
If you work anywhere else, Claims Administrator
Duration of STD Benefits
STD benefits will begin when the Claims Administrator approves your claim, generally the eighth day you are
disabled. As noted above, before your claim can be approved, you must be disabled for the elimination period.
Until STD benefits begin, you may use your Paid Time Off (if available).
You will need to file a claim for benefits to be paid, and you may be required to submit proof of your continued
disability during your STD period. See “Applying for Benefits” at the end of this section for details. If your claim
is approved, you generally receive your STD benefit check from the insurance company. The amount you

Disability Coverage
95
receive may be subject to income tax withholding. See the Program Documents issued by the insurance
carrier for details such as payment frequency and when benefits end.
If You Return to Work
If you return to work full-time, and, again become disabled from the same or a related cause, your second
disability may be treated as part of your prior claim. See the Program Documents issued by the insurance
carrier for more details.
Concurrent Disability
If a new, non-work related disability occurs while you are receiving benefits for another covered disability, your
benefits will continue while you remain disabled. These benefits will be subject to the maximum length of
benefits described above and any limitations and exclusions applied to the initial cause of disability.
LONG-TERM DISABILITY
If you are receiving STD benefits and your disabling illness or injury lasts longer than 26 weeks, and you
purchased LTD insurance, you may be eligible for LTD benefits, which helps provide continued income
replacement.
Eligibility for LTD Benefits
If you purchased LTD coverage and are determined to be disabled under the LTD program, you will be eligible
for LTD benefits in accordance with the terms of the LTD program. The LTD program administrator is
responsible for making claim determinations.
Covered Disabilities and Elimination Period
Similar to the eligibility requirements for STD benefits, you must be continuously disabled for an elimination
period. For LTD, the elimination period is 180 consecutive days, and must be satisfied before you are eligible
to receive benefits.
You will be eligible for LTD benefits if, after you satisfy the elimination period and for the first 24 months for
which LTD benefits are payable, the Claims Administrator determines that you are disabled.
Please refer to the Program Documents provided by the insurance carrier for more information on the
insurance carrier’s requirements for determining whether a covered person is “disabled”, as well as for a list of
excluded disabilities.
Physical Examination
The Claims Administrator, at its expense, may require you to undergo a physical examination if you submit a
claim for LTD benefits or while you are receiving LTD benefits. If you refuse to be examined, the Claims
Administrator may deny your claim or terminate your benefits.
Disabilities Excluded From Coverage
You will not be eligible for LTD benefits if you incur a disability that is caused by, contributed to by, or results
from:
An intentionally self-inflicted injury (sane or insane);
Your committing, or attempt to commit, an assault, battery or felony;
War or any act of war (declared or not declared);
Insurrection, rebellion, or taking part in a riot or civil commotion; or
A disability that starts during the first 12 months of your current LTD coverage, if it is caused or contributed
to by a “preexisting condition.” This means a condition for which, during the last 3 months before you last

Disability Coverage
96
became covered, you: Were diagnosed; Received treatment or services; or Took drugs or medicines
prescribed or recommended by a physician.
Amount of LTD Benefits
Determining the Benefit Amount
The LTD program provides you with a monthly benefit based on a percentage of your basic monthly earnings.
If you qualify for LTD benefits, you will receive a benefit equal to the following amounts, depending on which
option you elected:
Option 1 - 50% of your basic monthly earnings minus amounts from other deductible sources of income.
The maximum benefit is $3,000 per month
Option 2 - 60% of your basic monthly earnings minus amounts from other deductible sources of income.
The maximum benefit is $20,000 per month
The minimum benefit under either option is $100 per month.
Please refer to the Program Documents provided by the insurance carrier for more information on how your
LTD benefit amount will be reduced by other benefits.
Working While Disabled
Even if you are disabled, you may feel well enough to return to work. Depending on how much you earn while
working (your “disability earnings”), your LTD benefit amount may remain unchanged, may be adjusted or may
terminate. If you are working while disabled, the Claims Administrator may require you to send proof of your
disability earnings on a monthly basis.
Please contact the Claims Administrator or refer to the Program Documents provided by the insurance carrier
for more information on working while disabled.
Rehabilitation Services
The LTD program offers you services to help you get back to work. Please refer to the Program Documents
provided by the insurance carrier for more information on the criteria for this program.
Duration of LTD Benefits
Benefits will begin after the Claims Administrator approves your claim, provided you have satisfied the
elimination period. Please refer to the Program Documents provided by the insurance carrier for more
information on the frequency of payment and when benefits end.
Maximum Period for Payment
Subject to the limited pay period described in the Program Documents provided by the insurance carrier, the
maximum period is the longest period for which you can receive LTD benefits. This period will depend on your
age when your disability begins. Please see the Program Documents provided by the insurance carrier for
more information.
Limited Pay Period
A period of disability may be limited if it is determined that the disability is primarily caused by a Mental Health
or Psychiatric condition, including physical manifestations of these conditions, but excluding those conditions
with demonstrable, structural brain damage. Please refer to the Program Documents provided by the
insurance carrier for more information on limitations and exclusions applicable in this situation.

Disability Coverage
97
Recurring Disabilities
If you return to work full-time after receiving LTD benefits and you have a recurrent disability, your recurrent
disability may be treated as part of your prior claim and you will not have to complete another elimination period
under certain circumstances. Please refer to the Program Documents provided by the insurance carrier for
more information on the timing rules and other requirements applicable to recurring disabilities.
Survivor’s Benefit
Your survivor will be entitled to receive a survivor benefit if he or she meets the insurance carrier’s
requirements. Please refer to the Program Documents provided by the carrier.
Recovery of Overpayments
Please note that you will be required to return to the insurance company any overpayment of STD or LTD
benefits paid to you as a result of:
Fraud;
Any error the Claims Administrator may make in processing your claim; or
Your receipt of any deductible sources of income.
If your survivors become entitled to the survivor benefit, the insurance company may first apply the survivor
benefit to any overpayment that may exist on your claim.

98
LIFE AND ACCIDENT PROTECTION
OVERVIEW OF YOUR LIFE AND ACCIDENT PROTECTION .................... 99
WHEN YOU ENROLL .................................................................................. 100
Naming a Beneficiary ............................................................................ 100
Regular Annual Earnings ...................................................................... 101
LIFE INSURANCE ........................................................................................ 101
Basic and Supplemental Life Insurance................................................ 101
Tax Alert ................................................................................................ 102
Dependent Life Insurance ..................................................................... 102
Conversion and Portability Rights ......................................................... 102
Accelerated Life Insurance Benefit ....................................................... 102
ACCIDENT INSURANCE ............................................................................. 102
Accidental Death and Dismemberment Insurance ............................... 102
Business Travel Accident Insurance ..................................................... 103
Maximum Benefit Amount ..................................................................... 103
When Benefits Are Not Paid ................................................................. 104
LIFE AND ACCIDENT
PROTECTION

99
Life and Accident Protection
OVERVIEW OF YOUR LIFE AND ACCIDENT PROTECTION
The life and accident insurance program provides financial protection for you and your family in the event of a
death or accidental loss. Basic Life Insurance is paid for by your Employer. You can purchase optional
Supplemental Life Insurance and Dependent Life Insurance, and optional Accidental Death and
Dismemberment (AD&D) Insurance and Business Travel Accident Insurance.
Effective January 1, 2023, your life and accident coverage options are fully insured by MetLife.
Note: This information is designed to explain, in simple language, important features of the life and accident
insurance programs. Every effort has been made to provide clear ,and understandable information. However,
the separate Program Documents provided by the insurance carrier will govern the terms of the Life and AD&D
options available to you, and where applicable, the rights of a participant and his or her representative,
beneficiary or estate.
If you have any questions about the life and AD&D coverage options available to you, please contact the Hilton
Benefits Center for more information, or MetLife at 1.877.208.2363.
A SNAPSHOT OF THE LIFE AND ACCIDENT INSURANCE COVERAGE
Here’s a snapshot of your life and accident benefits.
Type of Insurance Coverage Amount
Basic Life Insurance
Provides a benefit to your survivors in the event
of your death
1 times regular annual earnings rounded to the
next higher $1,000 up to $2,500,000
Optional Supplemental Life Insurance
Life Insurance available in addition to Basic Life
Insurance. Can be purchased through Metropolitan
Life Insurance Company.
Up to 8 times regularly annual earnings*
Maximum benefit: $2,500,000 (in addition to basic
life insurance)
Optional Dependent Life Insurance
Life insurance for your dependents. Can be
purchased through Metropolitan Life Insurance
Company.
Spouse/Domestic Partner: $5,000,
$10,000, $25,000, $50,000 or $100,000**
Each covered dependent child from live
birth to age 26: $5,000 or $10,000

Life And Accident Protection
100
Optional AD&D Insurance
Protection for you and your dependents if you or a
covered dependent should die or become
dismembered as a result of a covered accident. Can
be purchased through Metropolitan Life Insurance
Company.
You:
Up to
8 times regular annual earnings
Maximum benefit: $2,500,000
Spouse/Domestic Partner: 40% (50% if you do
not have eligible dependent children at the time of
the accident) of your coverage amount.
Spouse/Domestic Partner coverage cannot
exceed $500,000.
Each covered dependent child up to age 26: 10%
(15% if you do not have an eligible
spouse/domestic partner at the time of the
accident) of your coverage amount. The
coverage for a covered dependent child cannot
exceed $50,000
Business Travel Accident Insurance
Protection in the event of a covered accident while you are
traveling on Hilton business
For eligible dependents, insurance protection in the event
of a covered accident while traveling with a Team Member
on Hilton business
You: Either $100,000, $500,000 or $1,500,000
***
Spouse/Domestic Partner: Either $50,000 or
$100,000***
Each covered dependent child to age 19, or age
25 if a full-time student: $50,000
*Evidence of Insurability required if coverage exceeds 3 times annual earnings or, if lower, $1,000,000, or for certain
enrollments made after your initial eligibility period. This requirement does not apply to AD&D coverage.
**Your spouse’s or domestic partner’s coverage cannot exceed 100% of your combined Basic Life and Supplemental
Life Insurance. EOI is required for spouse life coverage of $25,000 or more or for certain enrollments made after
initial eligibility. This requirement does not apply to AD&D coverage.
***Refer to the Program Documents to determine which amount is applicable to you.
WHEN YOU ENROLL
Naming a Beneficiary
When you first enroll for coverage, you must designate one or more beneficiaries to receive the proceeds of
your Basic Life and Business Travel Accident insurances by providing your beneficiary information online using
the Your Benefits Resource website at http://digital.alight.com/hilton. You may also change your designation at
any time by using this same website. Your beneficiary designation is effective on the date you complete the
online designation, but will apply to any insurance amounts paid after the insurance company receives your
change. If you elect to purchase Supplemental Life and/or Accidental Death and Dismemberment (AD&D),
please refer to the Program Documents. Please contact the Hilton Benefits Center with any questions.

Life and Accident Protection
101
If you elect the optional Dependent Life Insurance coverage, or AD&D Insurance coverage for your
dependents, you are the named beneficiary. You are the beneficiary for your eligible dependents under
Business Travel Accident Insurance. If a benefit becomes payable after your death (for example, your
dependent dies during the 31-day conversion period for dependent life insurance following termination of
coverage after your death), the benefit will be paid to your estate.
No Beneficiary Designation
If you do not designate a beneficiary to receive any of your life, and AD&D death benefits, your beneficiary or
beneficiaries for any applicable life and accident insurance coverages is the first surviving person(s) listed
below:
1. Your lawful spouse (or domestic partner
2. Your natural or legally adopted children (benefit divided equally)
3. Your parents (benefit divided equally)
4. Your natural or legally adopted brothers and sisters (benefit divided equally)
5. Your estate, payable to your executor or administrator
Regular Annual Earnings
Basic Life, Supplemental Life, and AD&D benefits are based on your regular annual earnings. Your regular
annual earnings for purposes of these benefits are based on your current year’s pay, plus:
a) overtime, bonus and tips received July 1 through December 31 of the calendar year immediately preceding
the prior calendar year; and
b) overtime, bonus and tips received January 1 through June 30 of the prior calendar year.
Earnings does not include the amount of any pre-tax contributions the Team Member makes to the Hilton
401(k) savings plan or the cost of health care coverage the Team Member pays on a pre-tax basis.
Please refer to the Program Documents for more information.
LIFE INSURANCE
Basic and Supplemental Life Insurance
As noted in the “Snapshot” chart, Basic Life Insurance coverage is equal to one times your regular annual
earnings, rounded up to the next higher $1,000, up to a maximum benefit of $2,500,000 as of the date of
enrollment. Your Basic Life Insurance coverage amount (as well as any Supplemental Life Insurance coverage
you have elected for yourself) changes annually at annual enrollment, effective for the following plan year. Any
mid-year adjustment will not be made effective until January 1 of the following plan year, provided you are still
enrolled in the benefit at that time.
Supplemental Life Insurance coverage pays benefits in addition to your Basic Life Insurance coverage and is
subject to a maximum benefit of $2,500,000. The cost of coverage for Supplemental Life Insurance is based
on your age and tobacco use.
Your Basic and Supplemental Life Insurance coverage may be reduced beginning the year you reach age 65.
Please refer to the Program Documents provided by the insurance carrier for details.
Life and Accident Protection
102
Tax Alert
Your Basic Life Insurance coverage may be automatically provided to you at Hilton’s cost. If Hilton-provided
Basic Life Insurance coverage does not exceed $50,000, the coverage is tax free to you. However, if Hilton-
provided Basic Life Insurance coverage exceeds $50,000, you must include in your gross income the cost of
the excess coverage that is paid by Hilton. For this purpose, the cost is computed using a uniform premium
table published by the Internal Revenue Service and is reported to you on your Form W-2 (“C” in Box 12) and
on your paycheck (under “Group Term Life”).
Dependent Life Insurance
You may elect to purchase Dependent Life Insurance for your eligible spouse or domestic partner as well as
any dependent children. If you elect dependent life insurance for any dependent who is confined for medical
care or treatment at home or elsewhere, coverage for your dependent begins when the dependent is medically
released from confinement.
Conversion and Portability Rights
If your Basic Life, Supplemental Life and Dependent Life Insurance end or are reduced for certain reasons, you
have certain rights to continue the lost coverages at your expense. Please refer to the insurance carrier’s
documents for details.
Accelerated Life Insurance Benefit
An accelerated benefit feature is part of your Basic Life, Dependent Life and Supplemental Life Insurance
coverage.
ACCIDENT INSURANCE
Hilton offers two types of accident protection: Accidental Death and Dismemberment (AD&D) and Business
Travel. If your loss happens to be payable under both types of protection, then benefits will be paid from both
the AD&D and Business Travel Accident programs. Benefits will not be offset in this instance. (See the
Program Documents for information about exclusions from accident coverage.)
Accidental Death and Dismemberment Insurance
AD&D Insurance is available for purchase and pays benefits for a death or dismemberment occurring within
365 days of, and resulting from, a covered accident while your coverage is in effect. You must elect AD&D
coverage. For AD&D Insurance, two coverage levels are available:
You Only
You + Family
For you, AD&D Insurance coverage is in salary increments of 1 – 8 x your annual earnings, rounded up to the
nearest $1,000. The maximum coverage is the amount set forth in the Program Documents provided by the
insurance carrier.
If you elect Accidental Death and Dismemberment coverage for a dependent who is confined to a health care
facility or disabled due to sickness or injury, coverage for your dependent begins when the confinement ends or
your dependent is no longer disabled.
Your AD&D Insurance coverage may be reduced beginning the year you reach age 65.

Life and Accident Protection
103
Please refer to the Program Documents for details.
Business Travel Accident Insurance
Business Travel Accident Insurance (BTAI) is provided by Hilton at no cost to you. BTAI is insured by Chubb
and pays benefits in the event of accidental dismemberment or death while traveling on Hilton business if the
loss occurs within 365 days of the accident. Generally, non-union Team Members working at least 30 hours per
week are eligible for coverage under Business Travel Accident Insurance
Business Travel Accident Insurance provides you with accident coverage while you are traveling on Hilton
business away from your regular place of employment at Hilton’s authorization, direction and expense and for
periods of 365 days or less. Business travel includes travel or activities that are unrelated to business and
which take place away from your residence or regular place of employment. Such travel or activities must
coincide with your business travel and is limited to any consecutive seven-day period immediately prior to,
during or immediately following your business travel.
Your spouse or domestic partner and covered dependent children are covered if they accompany you while
you are traveling on Hilton business, at Hilton’s authorization, direction and expense, for periods of 365 days or
less. Coverage is also provided while your dependents are traveling with you on relocation travel that is more
than 50 miles from your current work location. To qualify as a “covered dependent child” for purposes of
Business Travel Accident Insurance, your dependent child must be:
• Unmarried
•
Your natural child, grandchild, stepchild, or adopted child
•
Primarily dependent upon you for maintenance and support
•
Under age 19, or under age 25 if enrolled as a full-time student at an institution of higher learning, or
classified as an incapacitated dependent child.
Business Travel Accident benefits are paid in addition to those under your AD&D Insurance in the event the
loss is covered by both types of insurance.
Additional benefits may be available. Please review the Program Documents for details.
Maximum Benefit Amount
Under AD&D Insurance, the total payment for all losses due to any one accident will not be more than 100% of
the applicable coverage amount, up to a maximum amount, as set forth in the Program Documents provided by
the insurance carrier.
If your loss due to an accident occurs while you are traveling on Hilton business, your Business Travel Accident
Insurance benefit amount will be paid as well. The benefit amounts for you, your spouse or domestic partner
and/or your dependent children) may vary. See the Program Documents provided by the insurance carrier for
more details. The total payment for all losses due to any one aircraft accident will not be more than $25 million
for all covered persons with claims resulting from the accident.

Life and Accident Protection
104
When Benefits Are Not Paid
Both the AD&D Insurance coverage and Business Travel Accident Insurance coverage have a number of
exclusions or circumstances under which benefits will not be paid. Please review the applicable Program
Documents carefully to make sure you understand when benefits are not payable.
Retiree Life Insurance
You are eligible for retiree life insurance benefits if:
You are an Employee who retired from Hilton Worldwide, Inc. (or Hilton Hotels
Corporation) prior to September 1, 2000:
o With 10 years of service (if you were age 65 or older at retirement), or
o With 20 years of service (if you were older than age 55 at retirement); and
o your name is on a list of eligible individuals maintained by the Plan Administrator; OR
You were an Executive Officer of Hilton Worldwide, Inc. when you retired and your name
is on a list of eligible individuals maintained by the Plan Administrator.
The retiree life insurance benefits provided under the Plan are governed by the Program Documents provided to
you by the applicable insurance carrier. Please see the Program Documents for terms of coverage, including
any exclusions or limitations that may apply. Contact the Plan Administrator for more information about eligibility
for these benefits.

105
GENERAL INFORMATION
PLAN ADMINISTRATION ............................................................................ 106
Amendment and Termination ................................................................ 106
Representations Contrary to the Plan ................................................... 106
No Assignment ...................................................................................... 106
Recovery of Payments Made by Mistake and Failure to
Cash Benefit Checks ............................................................................. 107
Responsibility for Tax Implication of Benefits ....................................... 107
No Contract of Employment or Service ................................................. 107
Severability ............................................................................................ 107
Plan Funding ......................................................................................... 107
Applicable Law ...................................................................................... 108
Governmental Benefits Exclusion ......................................................... 108
Interpretive Authority ............................................................................. 109
Statement of ERISA Rights ................................................................... 109
Assistance With Your Questions ........................................................... 110
GENERAL INFORMATION .......................................................................... 111
PLAN INFORMATION .................................................................................. 112
GENERAL INFORMATION

General Information
106
PLAN ADMINISTRATION
The Plan Administrator has the sole and complete discretionary authority to determine eligibility for Plan
benefits and to construe the terms of the Plan, including the making of factual determinations. The Plan
Administrator shall have the discretionary authority to grant or deny benefits under the Plan. Benefits under the
Plan will be paid only if the Plan Administrator decides in its discretion that the applicant is entitled to them.
The decisions of the Plan Administrator shall be final and conclusive with respect to all questions relating to the
Plan. If a Claims Administrator has the only review authority, the Claims Administrator’s decision will be final
and conclusive with respect to all questions.
The Plan Administrator may delegate certain of its Plan duties to other persons and may seek such expert
advice as the Plan Administrator deems reasonably necessary with respect to the Plan. The Plan
Administrator shall be entitled to rely on the information and advice furnished by such delegates and experts,
unless actually knowing such information and advice to be inaccurate or unlawful.
The Plan Administrator may adopt uniform rules for the administration of the Plan from time to time, as it deems
necessary or appropriate.
Amendment and Termination
Hilton intends to offer the Plan indefinitely, but reserves the sole discretionary right to modify, amend or
terminate the Plan, in any respect, at any time and from time to time, retroactively or otherwise, by a written
instrument adopted by the Plan Administrator or its designee. Hilton’s decision to change or terminate the Plan
could result from:
Changes in federal or state laws governing employee benefits;
Changes in an insurance contract or policy involving an insurance company;
Changes in a collective bargaining agreement; or
Any other reason.
If the Plan is modified, amended or terminated, you will be notified of the effect of such change to your Plan
benefits or coverage. However, the modification, amendment or termination may be effective before you are
notified, to the extent permitted by law. Subject to the terms of any collective bargaining agreement, no
consent of any employee or any other person will be necessary for Hilton to modify, amend or terminate the
Plan described in this SPD.
Representations Contrary to the Plan
No employee, director or officer of Hilton has the authority to alter, vary or modify the terms of the Plan except
by means of a duly authorized written amendment to the Plan. No verbal or written representations contrary to
the terms of the Plan are binding upon the Plan, the Plan Administrator or Hilton.
No Assignment
You may not alienate, sell, transfer, assign, , or encumber benefits for which you may become eligible under
the Plan, unless otherwise required by applicable law or expressly permitted by the Plan Administrator, at its
discretion.
Any attempt to do so will be null and void. In other words, you cannot assign your rights to receive health
benefits to a health care provider or any other person. However, the claims administrator may choose to make
payments directly to:
• Any provider of health care services or supplies;

General Information
107
• Any institution or facility where you are now or have in the past been hospitalized or received
treatment.
Only eligible participants have benefit rights under the Plan. However, benefits under the Plan may be subject
to a Qualified Medical Child Support Order (QMCSO).
You may assign your benefits under the Plan with the Plan’s consent. When you assign your benefits under the
Plan with the Plan’s consent, and a provider submits a claim for payment, you and the provider represent and
warrant that the covered health services were actually provided and were medically appropriate. When the
Plan has not consented to an assignment, the Plan will send the reimbursement directly to you (the participant)
for you to reimburse the provider upon receipt of their bill. However, the Plan reserves the right, in its discretion,
to pay a provider directly for services rendered to you. When exercising its discretion with respect to payment,
the Plan may consider whether you have requested that payment of your benefits be made directly to the
provider. Under no circumstances will the Plan pay benefits to anyone other than you or, in its discretion, your
provider. Direct payment to a provider shall not be deemed to constitute consent by the Plan to an assignment
or to waive the consent requirement. When the Plan in its discretion directs payment to a provider, you remain
the sole beneficiary of the payment, and the provider does not thereby become a beneficiary. Accordingly,
legally required notices concerning your benefits will be directed to you, although the Plan or its Claim
Administrator may in its discretion send information concerning the benefits to the provider as well. If payment
to a provider is made, the Plan reserves the right to offset benefits to be paid to the provider by any amounts
that the provider owes the Plan (including amounts owed as a result of the assignment of other plans'
overpayment recovery rights to the Plan).
Recovery of Payments Made by Mistake and Failure to Cash Benefit Checks
You will be required to return to Hilton any benefits, or portion thereof, paid under the Plan by a mistake of fact
or law. If you do not return benefits paid under the Plan by a mistake of fact or law, the Plan may offset your
future benefits up to the amount you owe the Plan.
With respect to any self-funded benefits provided under this Plan, the payee’s failure to cash a benefit check
(whether due to an inability to locate the whereabouts of such person after reasonable efforts have been made
or for other reasons) shall result in a forfeiture of such payment to the Plan upon the later of (i) the stale date
indicated on the benefit check or (ii) one year anniversary of issuance of such payment.
Responsibility for Tax Implication of Benefits
You will be responsible for the tax implications of and determination of imputed income with respect to any
benefits you elect for eligible dependents who are not entitled to tax-free benefits under current federal law.
No Contract of Employment or Service
Your participation in the Plan does not assure you of continued employment with Hilton or rights to benefits
except as specified under the terms of the Plan. Nothing in the Plan or in this SPD confers any right of
continued employment (or service, as applicable) to any employee or leased employee, as applicable.
Severability
If a court of competent jurisdiction finds, holds or deems any provision of the Plan described in this book to be
void, unlawful or unenforceable under any applicable statute or other controlling law, the remainder of the Plan
shall continue in full force and effect.
Plan Funding
Benefits offered under the Plan are provided on either a self-insured basis by Hilton or are fully insured, as
shown in the following chart.

General Information
108
Self-Insured Fully Insured
Benefits
Medical Coverage with Prescription Drug
Coverage
Flexible Spending Accounts
ental Coverage
(only Delta Dental)
6
Medical Coverage with Prescription Drug
Coverage
Dental Coverage
Vision Coverage
Life Insurance (Basic, Supplemental and
Dependent)
Accident Insurance (AD&D and Business
Travel)
STD (Basic and Buy-Up)
Disability Benefits Law Plan (New York
STD plan)
LTD
Employee Assistance Program
Retiree Life
Voluntary Medical Benefits**
Legal Services **
Definition As claims are made, covered benefits are paid
from Hilton’s general assets. However, Hilton
has administrative services contracts with third-
party administrators to decide on and process
claims.
An insurance carrier insures the benefits and
pays the covered benefits. Hilton pays premiums
to the insurance carrier for benefit coverages
from its own funds as well as employee payroll
deductions. In addition, an insurance carrier
provides administrative services and makes
decisions regarding benefits.
6
Dental coverage options through Delta Dental are self-insured. Dental coverage options through Cigna or Aetna are fully-insured.
** Voluntary Medical Benefits and legal services are not covered by ERISA.
Please see the “Plan Information” chart at the end of this section for more details on which third-party
administrators and insurance companies Hilton has contracted with to provide services and benefits.
Applicable Law
The Plan described in this SPD shall be governed and construed in accordance with the laws of the
Commonwealth of Virginia to the extent not preempted by the laws of the United States.
Governmental Benefits Exclusion
If services or benefits are reasonably available under any plan or program established by any government or
under any plan or program in which any government participates (other than as an employer), benefits under
the Plan are not payable for such services or benefits unless payment is legally required. In the case of any
person who is not enrolled for all coverage for which he or she has become eligible under any such plan or
program, services and benefits available shall nevertheless include all benefits to which he or she would be
entitled if he or she were enrolled for such coverage. The term “any government” includes the federal, state,
provincial or local government or any political subdivision thereof of the United States or any country. This
provision is subject to any provision or regulation of such plan or program that requires that benefits be utilized
before benefits are available thereunder.

General Information
109
Interpretive Authority
If the Plan document does not clearly dictate whether an expense is eligible under the Plan and/or what
percentage of the eligible charge is covered, the Claims Administrator or insurer will make a determination and
pay benefits accordingly. Except as provided above, if a question arises as to the interpretation of the terms of
the Plan document, the Plan Administrator has discretionary authority to interpret, construe and apply the terms
of the Plan document and to decide any such question, including but not limited to a question as to a Team
Member’s eligibility to participate in the Plan.
Statement of ERISA Rights
As a Plan participant, you are entitled to certain rights and protections under the Employee Retirement Income
Security Act of 1974 (ERISA). ERISA provides that you are entitled to:
Receive Information About Your Plan and Benefits
Examine without charge at 7930 Jones Branch Drive, McLean, VA 22102, and major Human Resources
offices of Hilton, all Plan documents, including Program Documents, and copies of all documents filed by
the Plan with the U.S. Department of Labor and available at the Public Disclosure Room of the Employee
Benefits Security Administration, such as annual financial reports (Form 5500 Series).
Obtain copies of documents governing the operation of the Plan, including Program Documents, and
copies of the latest annual report (Form 5500 Series) and updated summary plan description upon written
request to the Plan Administrator (at the address above). The Plan Administrator may make a reasonable
charge for the copies.
Receive summaries of the Plan’s annual financial reports. These summaries are prepared and distributed
to Plan participants each year. The Plan Administrator is required by law to furnish each participant a copy
of the summary annual report.
Continue Group Health Plan Coverage
Continue health care coverage for yourself, spouse or dependents if there is a loss of coverage under the Plan
as a result of a qualifying event. You or your dependents may have to pay for such coverage. Review this
summary plan description and the documents governing the plan on the rules governing your COBRA
continuation coverage rights.
Prudent Actions by Plan Fiduciaries
In addition to creating rights for Plan participants, ERISA imposes duties upon the people who are responsible
for the operation of the Plan. The people who operate the Plan, called “fiduciaries,” have a duty to do so
prudently and in the interest of you and other Plan participants and beneficiaries.
No one, including Hilton or any other person, may discharge you or otherwise discriminate against you in any
way to prevent you from obtaining a welfare benefit or exercising your rights under ERISA.
Enforce Your Rights
If your claim for a welfare benefit is denied in whole or in part, you must receive a written explanation of the
reasons for the denial. You have the right to know why this was done, to obtain copies of documents relating to
the decision without charge, and to appeal any denial, all within certain time schedules.
Under ERISA there are steps you can take to enforce the above rights. For instance, if you request a copy of
Plan documents or the latest annual report from the Plan and do not receive them within 30 days, you may file
suit in a federal court. In such a case, the court may require the Plan Administrator to provide the materials
and pay you up to $110 a day until you receive the materials, unless the materials were not sent because of
reasons beyond the control of the Plan Administrator.

General Information
110
If you have a claim for benefits that is denied or ignored, in whole or in part, you may file suit in a state or federal
court. In addition, if you disagree with the Plan’s decision or lack thereof concerning the qualified status of a
medical child support order, you may file suit in federal court. If it should happen that Plan fiduciaries misuse the
Plan’s money, or if you are discriminated against for asserting your rights, you may seek assistance from the U.S.
Department of Labor, or you may file suit in a federal court. The court will decide who should pay court costs and
legal fees. If you are successful, the court may order the Plan Administrator to pay these costs and fees. If you
lose, the court may order you to pay these costs and fees if, for example, it finds your claim is frivolous. However,
no legal action may be commenced or maintained against the Plan until you exhaust the Plan’s claims
procedures, which are described in this SPD.
Assistance With Your Questions
If you have any questions about the Plan, you should contact the Plan Administrator (at the address below). If
you have any questions about this statement or about your rights under ERISA, or if you need assistance
obtaining documents from the Plan Administrator, you should contact the nearest office of the Employee Benefits
Security Administration, U.S. Department of Labor, listed in your telephone directory, or the Division of Technical
Assistance and Inquires, Employee Benefits Security Administration, U.S. Department of Labor, 200 Constitution
Avenue, N.W., Washington, DC 20210. You may also obtain certain publications about your rights and
responsibilities under ERISA by calling the publications hotline of the Employee Benefits Security Administration.

111
GENERAL INFORMATION
Plan Sponsor
Hilton Employer Inc.
7930 Jones Branch Drive
McLean, VA 22102
1.703.883.1000
Employer Identification Number: 84-2071583
Participating Employers
Contact the Plan Administrator for a complete list of participating employers.
Plan Administrator
Global Benefits Administrative Committee
7930 Jones Branch Drive
McLean, VA 22102
1.703.883.1000
You may obtain a copy of any of the Plan and Program Documents from the Plan
Administrator at the above address.
Appeals Committee
(Eligibility Claims)
Hilton Employer Inc.
U.S. Appeals Committee
7930 Jones Branch Drive
McLean, VA 22102
1.703.883.1000
Agent for Legal Service
Hilton Employer Inc.
General Counsel
7930 Jones Branch Drive
McLean, VA 22102
1.703.883.1000
Service of legal process may also be made on the Plan Administrator.
Plan Name
Plan Number
Plan Year
Hilton Health and Welfare Plan
502
January 1 – December 31
Plan Type
The Plan is an employee welfare benefit plan offering group health plan, disability,
life and accident coverage.
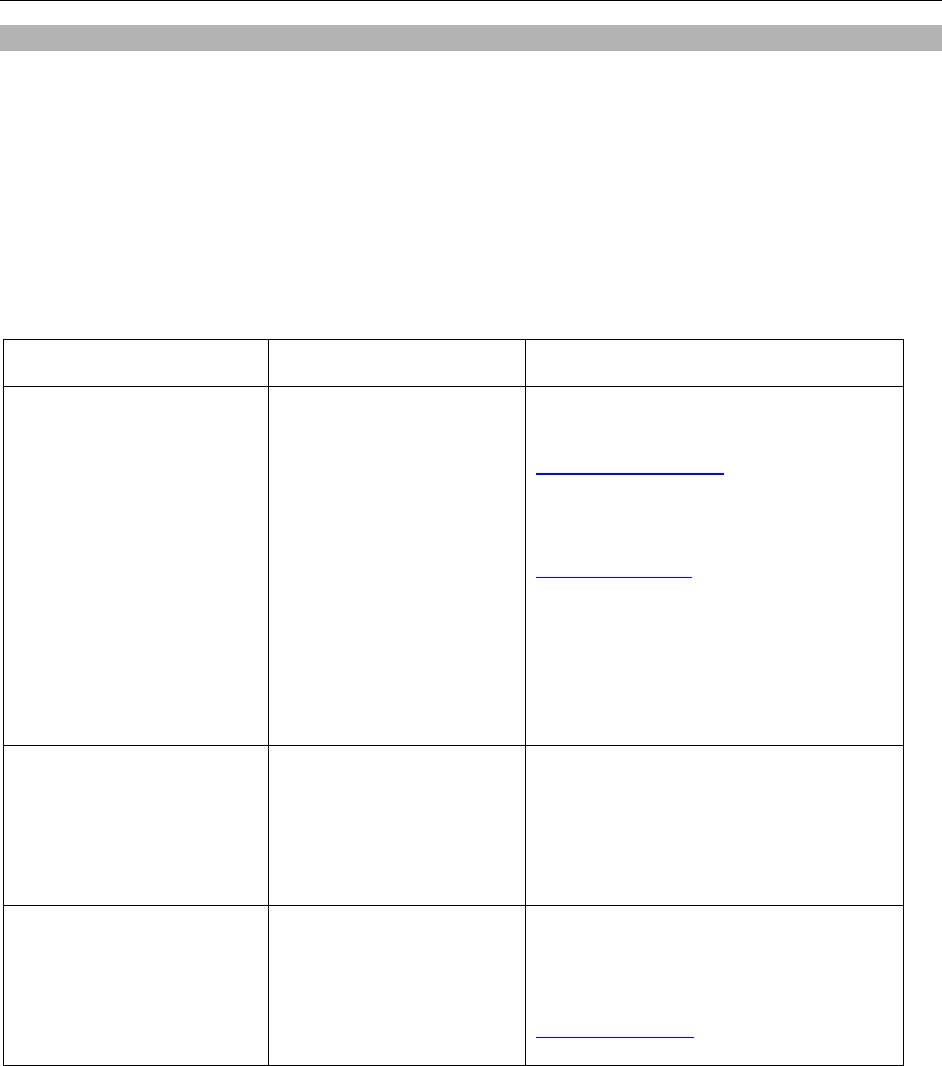
Plan Information
112
PLAN INFORMATION
To access any available insurance certificates:
1. Access YBR via this website: http://digital.alight.com/hilton
2. Click on the drop-down arrow next to the globe symbol within the footer of the logon page, then select
“English” or “Spanish – Espanol.”
3. Enter your User ID and password on the Logon page.
4. From the YBR Home page, hover over the tab titled “Knowledge Center.”
5. From the Knowledge Center drop-down menu items, click on the Plan Information link.
6. The SPD and available Program Documents will be displayed on the next screen.
***Not covered by ERISA
Benefit Program Funding Claims Administration
Medical with Prescription
Drug
Self-insured
Fully-insured
Anthem
1.844.451.2060
http://www.anthem.com
Cigna
1.800.244.6224
http://my.cigna.com
Various
Contact the Hilton Benefits Center at
1.877.442.4772 or the applicable carrier for
details.
Voluntary Medical***
• Hospital Insurance
• Accidental Death &
Dismemberment
• Critical Illness
Fully-insured
Cigna
1.800.351.9214
Contact the Hilton Benefits Center at
1.877.442.4772 for details.
Prescription Drug Self-insured
CVS Caremark
1.855.311.3158
www.caremark.com

Plan Information
113
Benefit Program Funding Claims Administration
Dental Self-insured
Fully-insured
Delta Dental
1.866.437.9880
Cigna
1.800.244.6224
Aetna
1.877.384.8899
Vision Fully-insured
EyeMed
1.844.409.3401
VSP
1.800.877.7195
Contact the Hilton Benefits Center at
1.877.442.4772 for details.
Health Savings Account*** For inquiries regarding
individual HSA Accounts
(Note: Although available
with HDHP coverage, the
HSA is an individual account
arrangement with UMB
Bank, and is not a benefit
plan sponsored by Hilton).
UMB Bank
1010 Grand Boulevard
Kansas City, MO 64106
https://hsa.umb.com
Flexible Spending
Accounts
Full purpose Healthcare
FSA
Limited purpose Healthcare
FSA
Dependent Care FSA***
Funded by employee
contributions
Smart Choice
P.O. Box 64009
The Woodlands, TX 77387-4009
1.800.964.6307
http://digital.alight.com/hilton
Claim fax number:
1.855.673.6719

Plan Information
114
Benefit Program Funding Claims Administration
COBRA Not applicable
Alight Solutions
http://digital.alight.com/hilton
Phone: 1.877.442.4772
Fax: 901.374.5073
Hilton Benefits Center
DEPT 01250
PO Box 64116
The Woodlands, TX 77387-4116
Employee Assistance
Program
Fully-insured insurance
contract with:
Lyra
Lyra
1.877.848.7910
lyrahealth.com/Hilton
Short-Term Disability
Long-Term Disability
Fully-insured insurance
contract with:
MetLife
MetLife
1.877.208.2363
Basic Life Insurance
Supplemental Life
Insurance
Dependent Life Insurance
AD&D Insurance
Retiree Life Insurance***
Fully-insured insurance
contract with:
Metropolitan Life Insurance
Company
Metropolitan Life Insurance Company
P.O. Box 6100
Scranton, PA 18505
Phone: 877-208-2363
Fax: 1-570-558-8645
Lifeclaimsubmit@metlife.com
Customer # 116341
To file a claim for life benefits, call the Hilton
Benefits Center at 1.877.442.4772 Monday
through Friday from 8:00 a.m. to 6:00 p.m.
CT.
Group Life Insurance
Conversion***
Metropolitan Life Insurance
Company
Metropolitan Life Insurance Company
P.O. Box 14401
Lexington, KY 40512
Phone: 1-877-275-6387
Fax: 1-866-545-7517

Plan Information
115
Benefit Program Funding Claims Administration
Business Travel
Accident Insurance
Group Policy # N16743872
Medical Abroad Benefits
Fully-insured insurance
contract with:
Chubb
Chubb Group of Insurance Companies
Claims Service Center
600 Independence Parkway
P.O. Box 4700
Chesapeake, VA 23327-4700
1.800.252.4670
International Assignee Plan United HealthCare
United HealthCare
Global Customer Support
1.877.844.0280
Legal Services*** Fully-insured insurance
contract with:
ARAG Insurance Company
ARAG Insurance Company
1.800.247.4184
***Not covered by ERISA

Plan Information
116
HIPAA Notice of Privacy Practices for the Hilton Health and Welfare Plan
This Notice applies only to the self-insured health benefits of the Hilton Health and Welfare Plan, which are identified
in the Plan Information section chart above.
THIS NOTICE DESCRIBES HOW MEDICAL INFORMATION ABOUT YOU MAY BE USED AND DISCLOSED AND
HOW YOU CAN GET ACCESS TO THIS INFORMATION. PLEASE REVIEW IT CAREFULLY.
The effective date of this Notice of Privacy Practices is January 1, 2023.
USES AND DISCLOSURES. How do we typically use or share your health information?
A claims administrator, administrator, insurance carrier or pharmacy benefit manager uses health information about
you for treatment, to obtain payment for treatment, and for administrative purposes. Below are some examples of the
uses/disclosures for each of these purposes.
• Help manage the health care treatment you receive. A claims administrator, administrator, insurance
carrier or pharmacy benefit manager may disclose information to a doctor, dentist, pharmacy, hospital or
other health care provider that provides you with treatment or services.
o For example, a doctor may request medical information from a claims administrator to supplement
his or her own records or to assist in your treatment. Also, the pharmacy benefit manager may
disclose to a network pharmacy the drugs you currently take to avoid unintended adverse drug
interaction.
• Payment. A claims administrator, administrator, insurance carrier or pharmacy benefit manager may use
and disclose your health information to others for purposes of determining the amount of payment and to
whom payment should be made for treatment or services you receive.
o Example: We share information about you with your dental plan to coordinate payment for your
dental work.
• Health Care Administration of the Plan. A claims administrator, administrator, insurance carrier or
pharmacy benefit manager may use and disclose your personal information during operational activities
such as quality assessment and improvement, performance measurement and outcomes assessment,
health services research, licensing, accreditation by independent organizations, and preventive health,
disease management, case management and care coordination. We may disclose your health information to
your health plan sponsor for plan administration.
o Example: A claims administrator may use the information to provide a disease management
program for members with certain conditions such as diabetes, asthma or heart failure Other
operational activities requiring use and disclosure include administration of reinsurance and stop
loss, underwriting and rating, detection and investigation of fraud, administration of programs and
payments and other general administrative activities, including data and information systems
management and customer service.
How else can we use or share your health information without your permission? We are allowed or required to
share your information in other ways – usually in ways that contribute to the public good, such as public health and
research. We have to meet many conditions in the law before we can share your information for these purposes. For
more information, see www.hhs.gov/ocr/privacy/hipaa/understanding/consumers/index.html.
• Help with public health and safety issues. We can share health information about you for certain
situations such as:
o Preventing disease

Plan Information
117
o Helping with product recalls
o Reporting adverse reactions to medications
o Reporting suspected abuse, neglect, or domestic violence
o Preventing or reducing a serious threat to anyone’s health or safety
• Do research. We can use or share your information for health research.
• Comply with the law. We will share information about you if state or federal laws require it, including the
Department of Health and Human Services if it wants to see that we’re complying with federal privacy law.
• Respond to organ and tissue donation requests. We can share health information about you with organ
procurement organizations.
• Work with a medical examiner or funeral director. We can share health information with a coroner,
medical examiner, or funeral director when an individual dies.
• Address workers’ compensation, law enforcement, and other government requests. We can use or share
health information about you:
o For workers’ compensation claims
o For law enforcement purposes or with a law enforcement official
o With health oversight agencies for activities authorized by law
o For special government functions, such as military, national security, and presidential protective
services
• Respond to lawsuits and legal actions. We can share health information about you in response to a court
or administrative order, or in response to a subpoena.
Your Rights. This section explains your rights and some of our responsibilities to help you. You have the right to:
• Ask us not to use or share certain health information for treatment, payment, or Plan operations. Such
requests will be considered but may not be granted.
• Inspect and obtain a copy of your health record as provided by federal regulation. A request must be in
writing and you may be charged a reasonable fee for producing and mailing the copies.
• Request to amend your health or claims record if you think they are incorrect or incomplete. A request must
be in writing and include the reason for the request. If your request is denied, you’ll receive a written denial
within 60 days.
• Request confidential communications or ask us to contact you in a specific way or at a different address. We
will consider all reasonable requests and must agree if you tell us you would be in danger if we do not.
• Request a list (accounting) of the times we’ve shared your health information for six years prior to the date
you ask, who we shared it with, and why. We will include all the disclosures except for those about
treatment, payment, and health care operations, and certain other disclosures (such as any you asked us to
make). We’ll provide one accounting a year for free but will charge a reasonable, cost-based fee if you ask
for another one within 12 months.

Plan Information
118
Get a copy of this privacy notice
• You can ask the Privacy Officer identified below for a paper copy of this notice at any time, even if you have
agreed to receive the notice electronically. We will provide you with a paper copy promptly.
Choose someone to act for you
• If you have given someone medical power of attorney or if someone is your legal guardian, that person can
exercise your rights and make choices about your health information.
• We will make sure the person has this authority and can act for you before we take any action.
File a complaint if you feel your rights are violated
• You can complain if you feel we have violated your rights by contacting us using the information on page 1.
• You can file a complaint with the U.S. Department of Health and Human Services Office for Civil Rights by
sending a letter to 200 Independence Avenue, S.W., Washington, D.C. 20201, calling 1-877-696-6775, or
visiting www.hhs.gov/ocr/privacy/hipaa/complaints/.
• We will not retaliate against you for filing a complaint.
YOUR CHOICES
For certain health information, you can tell us your choices about what we share. If you have a clear
preference for how we share your information in the situations described below, talk to us. Tell us what you want us
to do, and we will follow your instructions.
In these cases, you have both the right and choice to tell us to:
• Share information with your family, close friends, or others involved in payment for your care
• Share information in a disaster relief situation
If you are not able to tell us your preference, for example if you are unconscious, we may go ahead and share
your information if we believe it is in your best interest. We may also share your information when needed to
lessen a serious and imminent threat to health or safety.
In these cases, we never share your information unless you give us written permission:
• Marketing purposes
• Sale of your information
If you give such permission, you may later revoke it by sending written notice of revocation to the Privacy Officer.
OUR RESPONSIBILITIES
Our responsibilities include:
• We are required by law to maintain the privacy and security of your protected health information.
• We will let you know promptly if a breach occurs that may have compromised the privacy or security of
your information.

Plan Information
119
• We must follow the duties and privacy practices described in this notice and give you a copy of it.
• We will not use or share your information other than as described here unless you tell us we can in
writing. If you tell us we can, you may change your mind at any time. Let us know in writing if you
change your mind.
CONTACT INFORMATION. If you have any questions or complaints, please contact:
HIPAA Privacy Officer
Hilton Employer Inc.
7930 Jones Branch Drive
McLean, VA 22102
1-703-883-1000
CHANGES TO THE TERMS OF THIS NOTICE We can change the terms of this notice, and the changes will apply to
all information we have about you. The new notice will be available upon request, and a copy will be provided to you.
FOR MORE INFORMATION For more information, contact the Privacy Officer or visit
www.hhs.gov/ocr/privacy/hipaa/understanding/consumers/noticepp.html
.

Plan Information
120
Your Rights and Protections Against Surprise Medical Bills
When you get emergency care or get treated by an out-of-network provider at an in-network hospital or ambulatory
surgical center, you are protected from surprise billing or balance billing.
What is “balance billing” (sometimes called “surprise billing”)?
When you see a doctor or other health care provider, you may owe certain out-of-pocket costs, such as a copayment,
coinsurance, and/or a deductible. You may have other costs or have to pay the entire bill if you see a provider or visit
a health care facility that isn’t in your health plan’s network.
“Out-of-network” describes providers and facilities that haven’t signed a contract with your health plan. Out-of-network
providers may be permitted to bill you for the difference between what your plan agreed to pay and the full amount
charged for a service. This is called “balance billing.” This amount is likely more than in-network costs for the same
service and might not count toward your annual out-of-pocket limit.
“Surprise billing” is an unexpected balance bill. This can happen when you can’t control who is involved in your
care—like when you have an emergency or when you schedule a visit at an in-network facility but are unexpectedly
treated by an out-of-network provider.
You are protected from balance billing for:
Emergency services
If you have an emergency medical condition and get emergency services from an out-of-network provider or facility,
the most the provider or facility may bill you is your plan’s in-network cost-sharing amount (such as copayments and
coinsurance). You can’t be balance billed for these emergency services. This includes services you may get after
you’re in stable condition, unless you give written consent and give up your protections not to be balanced billed for
these post-stabilization services.
Certain services at an in-network hospital or ambulatory surgical center
When you get services from an in-network hospital or ambulatory surgical center, certain providers there may be out-
of-network. In these cases, the most those providers may bill you is your plan’s in-network cost-sharing amount. This
applies to emergency medicine, anesthesia, pathology, radiology, laboratory, neonatology, assistant surgeon,
hospitalist, or intensivist services. These providers can’t balance bill you and may not ask you to give up your
protections not to be balance billed.
If you get other services at these in-network facilities, out-of-network providers can’t balance bill you, unless you give
written consent and give up your protections.
You’re never required to give up your protections from balance billing. You also aren’t required to get care
out-of-network. You can choose a provider or facility in your plan’s network.
When balance billing isn’t allowed, you also have the following protections:
• You are only responsible for paying your share of the cost (like the copayments, coinsurance, and
deductibles that you would pay if the provider or facility was in-network). Your health plan will pay out-of-
network providers and facilities directly.
• Your health plan generally must:
o Cover emergency services without requiring you to get approval for services in advance (prior authorization).
o Cover emergency services by out-of-network providers.

Plan Information
121
o Base what you owe the provider or facility (cost-sharing) on what it would pay an in-network provider or facility
and show that amount in your explanation of benefits.
o Count any amount you pay for emergency services or out-of-network services toward your deductible and out-of-
pocket limit.
If you believe you’ve been wrongly billed, you may contact the Employee Benefits Security Administration
(EBSA), the No Surprise Help Desk (NSHD) at 1-800-985-3059 or cms.gov/nosurprises. If the plan benefit option in
which you are enrolled is fully insured, reach out to your state regulator to ask whether charges are allowed by law.

