
November 2015
By Caitlin omas-Henkel, Taylor Hendricks and Kelly Church, Center for Health Care Strategies
Opportunities to Improve Models
of Care for People with Complex
Needs: Literature Review
SUPPORTING A CULTURE OF HEALTH FOR HIGH-NEED, HIGH-COST POPULATIONS:

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
2
TABLE OF CONTENTS
Introduction ................................................. 3
Methods ..................................................... 4
Literature Search ........................................ 4
Limitations ............................................... 4
Summary of Findings ...................................... 6
Care Model Enhancements ............................ 6
Opportunities for Further Exploration .............. 8
Financing and Accountability .......................... 8
Opportunities for Further Exploration .............. 9
Data and Analytics ...................................... 10
Opportunities for Further Exploration .............. 11
Workforce Development ................................ 12
Opportunities for Further Exploration .............. 13
Policy and Advocacy ................................... 13
Opportunities for Further Exploration .............. 14
Conclusion .................................................. 15
Appendices: Index of Literature ......................... 16
Appendix A: Care Model Enhancements ............. 16
Appendix B: Financing and Accountability ........... 22
Appendix C: Data and Analytics ....................... 26
Appendix D: Workforce Development ................. 32
Appendix E: Policy and Advocacy .................... 36
C. Thomas-Henkel, T. Hendricks, and K. Church. Opportunities to Improve Models of Care for People
with Complex Needs: Literature Review. The Robert Wood Johnson Foundation and the Center for
Health Care Strategies, November 2015.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
3
INTRODUCTION
I
ndividuals with high rates of avoidable hospital admissions or emergency department (ED) visits—
sometimes called “high-need, high-cost patients” or “super-utilizers”—tend to have multiple medical,
behavioral health and social needs, resulting in high costs and, typically, poor outcomes. These
individuals often have an array of complex social challenges—potentially including unemployment,
homelessness, substance use disorders, and food insecurity—which must be addressed in order to
sustainably improve health outcomes and reduce their health care utilization.
With support from the Robert Wood Johnson Foundation, and in line with the Foundation’s vision for
building a Culture of Health for all Americans,
1
the Center for Health Care Strategies (CHCS) conducted
a literature review to explore the evidence base regarding effective approaches to care for high-need,
high-cost populations. CHCS organized its analysis of relevant materials around five key domains:
The literature review was designed to identify: (1) effective strategies for improving outcomes and lowering
costs for high-need, high-cost populations; and (2) critical gaps that must be addressed to better integrate
health and social services and produce desired outcomes for this population. This synthesis highlights
key findings and gaps in information gleaned from the literature review. See also a companion report that
synthesizes key findings from a related environmental scan and small group consultation.*
* The companion report, Opportunities to Improve Models of Care for High-Need, High-Cost Populations, includes a
sixth domain, governance and operations, that was identified subsequent to the completion of the literature review.
Care Model
Enhancements
Workforce
Development
Financing &
Accountability
Data &
Analytics
Policy &
Advocacy

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
4
METHODS
LITERATURE SEARCH
T
he review included studies conducted in the United States and published since 2005, as
identified through MEDLINE (using the PubMed interface), Cochrane Library, National Guideline
Clearinghouse, and Google Scholar. We included people with serious mental illness (SMI),
since this population often has a high rate of physical comorbidities, as well as high associated health
care costs.
2
The literature search also used Medical Subject Headings (MeSH) terms by the National
Library of Medicine, whenever a term was available.
3
For example, searches included keywords such
as comorbidity, severe mental illness, delivery of health care, integrated, cost savings, and/or patient
readmission. In addition to the primary search term, the literature review used secondary search terms
to filter findings that corresponded with the five domains and keyword terms such as: integrated +
care + management, financial + alignment + accountability, data + analytics, workforce + strategies,
and policy + advocacy.
Two reviewers scanned the abstracts of articles identified from the database searches to assess relevance
to the search criteria. Discrepancies in inclusion were resolved by discussion and re-review with additional
project team members. The search also included non-peer reviewed studies and relevant tools and
resources. To search for these secondary sources or “gray material” on the key topics, CHCS relied on
the same search terms employed in the peer reviewed material, including the following sources: California
HealthCare Foundation; Center for Health Care Strategies; The Commonwealth Fund; Health Affairs (for
non-peer-reviewed resources in addition to those found through the search described above); Institute for
Healthcare Improvement; National Governor’s Association; Robert Wood Johnson Foundation; and other
reputable health care organizations.
LIMITATIONS
There is an expansive body of literature that arguably could have bearing on efforts to improve care
and outcomes for high-need, high-cost populations. For example, strategies to improve outcomes for
individuals with SMI are generally relevant to “super-utilizer” programs given the prevalence of SMI among
this population. However, a synthesis of the literature around behavioral health treatment modalities for
SMI would be a project unto itself. Thus, CHCS limited its review to studies with greatest direct relevance
to the goals of this analysis—namely, to inform further development and enhancement of complex care

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
5
management programs serving high-need, high-cost populations. In the case of the SMI literature, this
resulted in the exclusion of studies on modalities specific to treating psychiatric illness (such as cognitive
behavioral therapy).
Across a few domains, the literature review was constrained by the relative nascence of this field of
study. For example, many programs for super-utilizers are in the early stages of development and
implementation, and have not yet tackled issues related to financing and accountability. Many programs
lack robust data collection and analysis mechanisms, making evidence on best practices difficult to
discern. Further, few randomized trials on interventions for high-need, high-cost populations exist,
highlighting the need for more robust evaluations of these programs.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
6
SUMMARY OF FINDINGS
CARE MODEL ENHANCEMENTS
B
ecause traditional models of care delivery are typically not effective for individuals with complex
medical, behavioral health, and social needs, enhancements to these models attempt to improve
outcomes and decrease costs by increasing connectivity between providers, tailoring clinical
interventions, coordinating care, integrating disparate systems, and addressing the social determinants
of health.
As reflected in the literature, effective models of care for super-utilizers rely on an intensive care
management approach. For example, a randomized controlled trial of an intensive care management
program that coordinated medical and mental health services for high-risk Medicaid beneficiaries in
Washington State showed increased access to care, lower inpatient medical costs, fewer unplanned
inpatient admissions, lower likelihood of experiencing homelessness, and fewer deaths.
4
A more
recent analysis of a separate Washington State care management program serving high-risk Medicaid
beneficiaries with disabilities revealed significant decreases in inpatient hospital costs for individuals in
the program, as well as non-significant decreases in total medical costs.
5
Reduced ED use and hospital
charges were also observed in various models of intensive care management for frequent ED users.
6–7
Core components of intensive care management programs that demonstrate positive outcomes for
high-need, high-cost patients include: extensive outreach and engagement; initial assessment; goal-
setting and care plan development; health education/coaching; frequent care team contact; follow-up with
patients after discharge; and linkages to housing, substance use disorder services, and other community
resources.
8–11
Several programs incorporate home visiting and round-the clock telephonic access to care
managers.
12–13
Programs that provide face-to-face care management directly with patients have more
evidence of effectiveness than those that employ telephonic care management services.
14–17
Medication
management, pain management, and support for care transitions (e.g., from hospital to community
settings) are also highlighted as integral aspects of achieving positive outcomes in care management
programs for high-need, high-cost patients.
18–21
Another resource defined super-utilizer programs as “data-
driven, high-intensity, community-based, patient-centered models using interdisciplinary teams to deliver
high-quality, comprehensive care, while encouraging self-advocacy and personal accountability.”
22
Effective targeting of services to high-risk patients is critical. For example, the Medicare Chronic Care
Demonstrations revealed a higher likelihood of reducing hospitalizations among beneficiaries at high risk
of hospitalizations than among a general population with chronic conditions.
23

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
7
Care team composition varies among effective programs, but often includes a primary care provider,
nurse, social worker, behavioral health specialist, and community outreach staff (e.g., community health
workers).
24–26
Care managers may be located on site at a provider practice or hospital; at a centrally
located care management agency, providing care management to multiple practices; or at a clinic where
an “intensivist”—a physician specializing in the treatment of patients in intensive care—is assigned a
high-risk patient panel.
27
An abundance of research demonstrates the importance of physical and behavioral health integration in
providing comprehensive health care.
28
Coordination of physical and behavioral health services—through
information exchange, joint care planning, or integration into primary care—is often cited as a key aspect
of complex care management, especially for individuals with serious mental illness.
29–32
Pilot programs in
Pennsylvania that integrated physical and behavioral health services and provided care management
for high-need, high-cost Medicaid beneficiaries resulted in lower mental health-related hospitalizations,
lower all-cause readmission rates, and fewer ED visits.
33
However, not all approaches to integration are
equally effective for high-risk individuals. For example, fully integrated physical and behavioral health
care, coupled with care management for individuals with SMI and substance use disorder, has been
shown to improve physical and mental health symptoms, as well as overall quality of life.
34
However,
simply co-locating primary care providers in substance use disorder treatment facilities without providing
care coordination services does not necessarily improve health outcomes for these individuals.
35
Clinical interventions that incorporate trauma-informed approaches to care for high-need, high-cost
patients may improve patient engagement and enhance quality and cost outcomes for these populations.
36
Qualitative research with complex patients who have high levels of ED and hospital use highlight a
number of psychosocial factors and life experiences that impact their care needs, including: (1) early-life
instability and traumas; (2) a history of difficult interactions with health care providers during adulthood;
and (3) the importance of positive and “caring” relationships with primary health care providers and the
outreach team.
37
Patient activation—or having the knowledge, skills, and confidence to manage one’s health—is recognized
as an important factor in the effectiveness of interventions for individuals with complex needs, and also
as a potential benefit of these interventions. For instance, the use of peer support providers for individuals
with mental illness has shown evidence of increased patient activation.
38–39
Higher patient activation is
linked to better health outcomes in the short- and long-term.
40–41
Acknowledging the critical role of social determinants of health, some intensive care management
programs for high-utilizing populations use nontraditional health care workers (e.g., community health
workers, peers, etc.) to connect individuals to needed social services and supports.
42
As recognition
of the impact of social factors on health outcomes continues to grow, efforts to address housing
instability, in particular, have gained traction as a method for improving outcomes and reducing costs
for high-need individuals.
43–44
Housing First interventions—in which high-utilizing patients are provided
with stable housing without a medical care component
45
—have been linked to reduced ED visits; fewer
hospital admissions; fewer hospital and nursing home days; reduced inpatient costs; and reduced
Medicaid expenditures.
46–49
States and communities across the country are increasingly implementing
housing interventions for high-risk populations, as these programs prove less costly and more effective
than managing homelessness and health problems on the street or in a shelter.
50–53

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
8
Opportunities for Further Exploration
The evidence around effective care models for high-need, high-cost patients is still emerging, with
relatively few high-quality studies revealing significant impacts on costs and utilization. Whereas efforts
over the last decade have clarified some core program elements as described above, key gaps in
understanding remain. For example, given the variation in approach across published studies, there
is limited ability to assess the replicability or generalizability of specific findings. Similarly, the lack of
rigorously tested high-quality models likely creates a significant amount of undocumented variation
in approach across participating providers or care team members even within a given study. Future
studies should seek to standardize models of care—including clearly defined interventions, frequencies
and modes of contact, and follow-up periods—and test their effectiveness across multiple sites.
Outside of a general finding that programs are most effective when targeted to high-risk patients, the
literature is not yet convincing on the most effective way to identify or calculate high risk. For example,
some successful programs rely on predictive modeling, while others specifically target individuals with high
rates of recent ED visits or inpatient admissions.
54–55
This highlights the need for greater understanding
about how to best target care coordination interventions to individuals for maximum impact.
Effective engagement strategies are another opportunity for future exploration, particularly given the
low engagement rates observed across published studies.
56–57
As the transient and vulnerable nature of
this population presents challenges for engagement and follow-up, additional qualitative and quantitative
studies should be designed to understand why some individuals do not engage in care management when
offered as well as strategies for promoting higher engagement rates.
58–59
Finally, further research to distill the discrete impact of housing interventions may be needed. In one
instance, high-utilizing patients were provided with ongoing case management in addition to housing
support, and researchers were unable to distinguish the impact of the housing support from that of the
care management services provided.
60
FINANCING AND ACCOUNTABILITY
Given the evidence indicating that integration of medical and behavioral health care—and more recently,
social services—may improve care and cost outcomes for certain high-need populations, a number
of states and communities are testing financial alignment and accountability models that support this
integration. The literature revealed a number of promising approaches to the alignment of financial
incentives and outcomes that are emerging across the U.S.—particularly in the form of pooled or braided
health and social service funding; global and bundled payments; and shared-risk models like Accountable
Care Organizations (ACOs).
States are increasingly exploring administrative, purchasing, and regulatory strategies to better integrate
physical and behavioral health care for high-need, high-cost Medicaid populations.
61
Some states are:
(1) consolidating the agencies responsible for overseeing physical and mental health and substance use
disorder services; (2) combining responsibility for behavioral health purchasing, contracting, and rate-setting
in the Medicaid agency and maintaining licensing and clinical policy authority in the behavioral health agency;
or (3) establishing informal collaborations to rationalize strategies across agencies.
62
Purchasing strategies
used by states include policies that create linkages across providers and systems (especially in managed
care “carve-out” environments) and implementation of fully integrated managed care approaches (e.g., for
individuals with SMI).
63
State Medicaid contracts with managed care organizations are one mechanism for
aligning incentives across physical and behavioral health systems.
64

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
9
Though models for integrating health and social services are still in the fledgling stages, small-scale
efforts have shown promise in improving care and cost outcomes, and states are exploring financing options
to build on this success.
65–67
Medicaid ACOs across the country are taking preliminary steps to provide
non-clinical supports to high-need, high-cost patients, leveraging financial incentives for providers to use
social services to maximize the impact of care interventions.
68
Programs in Colorado, Minnesota, New York,
Washington, Vermont, and other states are at varying levels of laying the groundwork for social service
integration into their Medicaid ACOs.
69
Community-based ACOs—or “accountable health communities”—
represent another innovative model, serving a coordinating function and taking accountability for providing
and paying for an array of services outside of traditional medical care payments.
70
Shared savings or
capitated payment structures may encourage closer collaboration between the health care and social service
systems. Current state approaches include, at one end of the continuum, grants to support provider capacity
building, and at the other, integrated payment models connecting providers and social services.
71
Future
studies are needed to evaluate whether these financing approaches contribute to the end goals of better
health and lower costs.
Hennepin Health, an ACO in Minnesota, has developed a model that integrates physical, behavioral
health, and social services (e.g., housing) for high-need, high-cost Medicaid beneficiaries using aligned
financial incentives.
72
It operates under a braided financing strategy, receiving a fixed per member per
month (PMPM) payment for the total cost of Medicaid health services (excluding long-term care) and using
grants from the county to cover the cost of some program staff.
73
In the model, social services are paid
for with human service funds from pre-existing state and county sources, supplemented by the health
plan’s PMPM payments.
74
Hennepin Health’s preliminary results have shown a shift in care from the ED
and hospital to outpatient settings, and the percentage of patients receiving optimal diabetes, vascular,
and asthma care has increased. Hennepin Health has also achieved a high patient satisfaction rating, with
87 percent of members reporting that they are satisfied with their care.
75
A number of states including Ohio and Michigan have implemented the Pathways Community HUB
Model, which coordinates clinical and social services at the community level to reduce duplication
of services and create greater efficiency. The model has been shown to reduce costs and improve
outcomes in a high-risk pregnancy population.
76
Opportunities for Further Exploration
While promising approaches to financial alignment and accountability are emerging across the country, there
is a need for increased examination of their effectiveness in supporting programs for high-need, high-cost
populations. As many of these programs are in the early stages of development and implementation, they
do not yet have sustainable financing mechanisms, and so it is difficult to understand what components
of funding and payment structures are most feasible and effective. Additionally, the U.S. has been
cited as lacking in robust population health outcomes, which may be partially attributed to a lack of
comprehensive investment strategies to address non-clinical interventions.
77–78
There are varying levels of capacity among states, communities and providers to align physical,
behavioral health, and social services when dealing with a diverse set of systems and funders that work
primarily in isolation.
79–80
A complicating factor in developing comprehensive payment models is the
limited regulatory authority among state Medicaid agencies to pay for non-clinical services, especially in
fee-for-service (FFS) arrangements.
81
Despite increased flexibilities to reimburse for non-clinical services
under a value-based or PMPM reimbursement system, these services must often meet “medical
necessity” criteria under the state definition. In addition, alignment efforts must often show the capacity

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
10
to yield a return on investment to attract payer interest. This can create challenges as states look to
pursue more integrated care models that align multiple funding sources across payers and finance
alternative “non-clinical” services.
A previously published systematic review of interagency collaboration between local health and local
government agencies failed to produce any evidence that these partnerships, compared to standard care,
led to health improvements.
82
This highlights an opportunity to further explore how models that work
across public systems—such as Hennepin Health—can be most effective in serving high-need,
high-cost populations.
DATA AND ANALYTICS
High-quality data and analytics are highlighted in the literature as a critical component of effective
programs for high-need, high-cost populations.
83–88
Data are used to identify high-need, high-cost patients
for specific interventions and to predict which individuals could be prevented from becoming high-need,
high-cost users.
89–92
The literature also highlighted current efforts to use data to inform clinical and care
management approaches and identify ways to establish data linkages across providers in the health and
social service systems.
A number of articles and resources highlight the value of using predictive modeling and risk stratification
to identify patients at-risk for high ED use and target interventions appropriately.
93–98
One study found
that ‘no-show propensity’ is an independent predictor of poor primary care outcomes, and thus may help
health care systems identify patients at-risk for high utilization.
99
Another found that recent criminal justice
involvement was associated with higher hospital and ED utilization among individuals with substance
use disorder, with psychological disorders, or without insurance.
100
Older patients, Medicaid recipients,
individuals living further away from the point of care, and those with diabetes or depression were more
likely to be high-utilizers, according to a retrospective and longitudinal analysis of medical records from
an urban community health center.
101
In yet another analysis, individuals with substance use disorder who
had high-frequency ED, ambulatory, and inpatient medical care use were more likely to be female, African
American, homeless, or have a history of substance abuse treatment or ambulatory care visits.
102
An
algorithm developed at New York University to classify ED use into various categories—ranging from
non-emergent to unavoidable emergent—was used to analyze ED use in Rhode Island. It revealed that
over 20 percent of ED visits between 2008 and 2012 were non-emergent, and that non-emergent ED users
were more likely to be: between 20-39 years of age, Hispanic, non-Hispanic black, and female.
103–104
In addition to predicting risk, another aspect of patient identification highlighted in the literature
is predicting care sensitivity, or the likelihood that an individual will respond to a particular care
management intervention.
105
This may involve excluding patients whose needs are unlikely to be addressed
by available resources; identifying patients facing certain barriers or care gaps; identifying “windows of
opportunity,” such as care transitions; or identifying patients who have previously experienced difficulty
with care coordination.
106
As an example, care teams may exclude patients undergoing chemotherapy,
dialysis or radiation, because they feel that the care management services may be unlikely to yield positive
outcomes when compared to the specialty-based services already in place.
107
Much of the literature sought to identify characteristics and develop a profile of high-need, high-cost
populations. In 2009, five percent of Medicaid beneficiaries accounted for 54 percent of costs, and those
with disabilities accounted for 30 percent of Medicaid costs.
108
In one analysis, mental health and other
behavioral health conditions were the top diagnoses linked to hospital stays among super-utilizers, followed

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
11
by alcohol-related disorders.
109
Among high-expenditure Medicaid-only enrollees with both substance abuse
and a mental health condition in fiscal year 2011, nearly half had no physical health conditions
110
In another
analysis of inpatient high-utilizers, behavioral health conditions were disproportionate on their billing records
compared to inpatients who were not high utilizers of inpatient services (74.9% v. 32.3%).
111
An additional
study revealed heart failure, septicemia, and mental health disorders as the top three reasons for hospital
admission among super-utilizers.
112
A number of analyses of high-cost Medicaid beneficiaries revealed
patterns of multimorbidity related to higher utilization and expenditures.
113–116
Within the most expensive
one percent of beneficiaries in Medicaid acute care spending, nearly 83 percent had three or more chronic
conditions.
117
Mental illness is nearly universal among Medicaid’s highest-cost, most frequently hospitalized
beneficiaries, and the presence of mental illness or substance use disorder is associated with much higher
per capita costs and hospitalization rates.
118
An analysis of Pennsylvania’s super-utilizers—patients with five or more admissions to a general acute
care hospital in fiscal year 2014—revealed that this population accounted for 10 percent of Medicare
admissions, 18 percent of Medicaid admissions, 20 percent of Medicare-Medicaid admissions, and seven
percent of commercial payer hospital admissions. These statewide results highlight the importance and
collective responsibility for addressing the needs of this population across payers.
119
Opportunities for Further Exploration
Despite numerous efforts across the country to precisely predict who is likely to become a high-utilizer,
gaps remain in these methods—many of which rely heavily on past claims data to identify high-risk
patients.
120
In fact, many risk prediction models only account for a quarter to a third of the factors that lead
to individuals’ future expenditure, and typically do not perform well for high-need, high-cost patients.
121
Integration of data—particularly across health and social services systems—remains a challenge.
In order to gain an accurate understanding of which patients to target for which interventions, and to
comprehensively address their needs, it is important to see the full picture of health and social service
utilization. Some states and localities have started testing how to achieve cross-system data integration,
but these efforts are rare and in the infancy stages of development.
While the importance of data to identify and target interventions is not disputed, less clear is how data
can be used to measure quality among high-need, high-cost patient populations with multiple medical,
behavioral health, and social challenges.
Further, there is a paucity of rigorous evaluation (e.g., randomized controlled trials, longitudinal analyses)
among programs that target super-utilizers, which makes replication of effective programs problematic
and limits the policy argument for doing so. Several articles emphasized that it takes significant time to
demonstrate the impact of super-utilizer programs, as these individuals are difficult to engage; behaviors
are difficult to change and sustain; and often times, costs for utilization increase in the short term, as
traditionally disconnected individuals are finally linked with needed services.
122
Regression to the mean can
also create difficulties in demonstrating the effectiveness of interventions for high-need, high-cost patients,
due to their often erratic utilization patterns, incurring high costs one year and perhaps far lower costs the
next—even without intervention.
123
Evaluations of these programs should account for regression to the
mean and control for it when possible.
124

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
12
WORKFORCE DEVELOPMENT
The review of literature related to workforce development primarily focused on using non-traditional
health workers—also referred to as lay health workers, community health workers, or peer support
providers—in care delivery for high-need, high-cost populations. Various articles and resources highlighted
programs using these non-traditional health workers, revealing a number of successes and challenges
related to these alternative workforce models. A few resources discussed how workforce training specific
to engaging with complex patients may improve patient/provider experience and patient outcomes, as
described further below.
While their non-traditional role in care delivery is sometimes criticized as ambiguous, the literature
described some common responsibilities for community health workers and peer support providers.
One article highlighted seven core roles for community health workers: providing cultural mediation;
delivering appropriate education; ensuring connections to needed services; offering informal counseling
and social support; advocating; providing direct services; and building capacity.
125
In a model developed
at the University of Pennsylvania, community health workers help patients create individualized action
plans around self-identified goals.
126
In addition, the literature underscored the unique role of community
health workers in addressing persistent health disparities and understanding and responding to the
many challenges faced by patients in navigating the health care system, obtaining necessary supportive
resources, and building self-efficacy and health literacy.
127
The Substance Abuse and Mental Health Services Administration’s (SAMHSA) definition of a ‘peer’ is a
person who has lived experience of recovery from mental illness and/or addiction and who wishes to provide
peer support services to others who are living with these disorders.
128
Some of the literature described the
role of peer support providers on care teams as more ambiguous than that of community health workers.
129
The development of trusting relationships with patients, based on mutual experience, respect, and hope,
is highlighted as a key function of the peer support role.
130
Patient education; social and emotional support;
advocacy; assistance with daily tasks; and connection to medical, behavioral health, legal, and financial
services are also described as responsibilities of peer support providers.
131–133
Numerous studies show promising results based on lay health worker interventions. A randomized
clinical trial of a community health worker model in Philadelphia showed improvements in patient
experience and outcomes, and reductions in hospital readmissions.
134
In another randomized controlled
trial using lay health workers as care guides, patients were 31 percent more likely to meet evidence-
based goals and 21 percent more likely to quit tobacco use.
135
These patients had fewer hospitalizations
and ED visits and reported more positive perceptions of their care, including improved social support,
individualized care, and understanding of how to improve their health.
136
A program for Medicaid super-
utilizers in Oregon, led by a nurse and supported by two community health workers, decreased ED
utilization from 78 percent in 2011 to 59 percent in 2013.
137
Peer support services were broadly recognized in the literature as a promising approach. SAMHSA
suggests that recovery-oriented, peer-provided behavioral health services are supported by a growing
body of evidence showing improved outcomes—sometimes even superior to non-peer provided
services.
138
Similarly, several articles highlighted the potential for peer support services to improve care
and produce substantial cost savings.
139
An analysis of a peer-led program for individuals with serious
mental illness in New York showed promising results: at six-month follow-up, program participants had
a significantly greater improvement in patient activation and higher rates of primary care visits, as well
as improvements in quality of life, physical activity, and medication management.
140
Medically and socially

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
13
vulnerable members of the intervention population showed the greatest improvements in physical health
related quality of life.
141
One assessment of current research related to peer support services for individuals
with serious mental illness, found that when compared to professional staff, peers were better able to
reduce inpatient use and improve a range of recovery outcomes, but that the effectiveness of peers in
existing clinical roles was mixed.
142
The same assessment found a number of other promising outcomes
across several peer provider models, including, improved relationship with providers; better engagement
with care; higher levels of empowerment; and higher levels of hopefulness for recovery.
143
An examination
of peer specialist interventions for veterans with serious mental illness also showed positive outcomes
related to reduced inpatient use and increased patient engagement.
144
The review provided some insight into how workforce training can improve patient experience and
outcomes for complex patient populations. One article highlighted the importance of training providers
to understand and work within the context of complex patients’ lives—starting with conducting a
comprehensive assessment of their array of health and social needs.
145
Another resource, which described
techniques for providers to successfully engage with super-utilizers, centered around creating trusting
relationships. The methods ranged from physical mannerisms and behaviors—such as removing a doctor’s
coat and making eye contact, to engaging with the patient in a sensitive, respectful, and strengths-based
way—for instance, by requesting permission to ask questions or asking what the individual enjoys doing.
146
Opportunities for Further Exploration
The review revealed significant challenges related to workforce development. In addition to role ambiguity,
challenges cited around the use of peer providers included lack of clear expectations, training, and
skills.
147–149
Additionally, supervisors had difficulty providing supervision and evaluating peer provider
performance.
150–152
Low pay and lack of career advancement opportunities were also mentioned as
challenges in the development of a peer support workforce.
153–154
The literature called for more rigorous evaluation of programs that use non-traditional health workers,
in order to establish a more robust evidence base of their efficacy in producing improved care and
cost outcomes.
155–159
SAMHSA cited lack of an accepted typology as a key hindrance to research and
evaluation of peer support programs.
160
Further, programs that are targeted to high-cost or high-utilizing
populations are likely to experience regression to the mean (in which costs/utilization naturally normalize
toward the population average over time), which may call into question any evidence of savings.
161
While
some peer provider and community health worker interventions have shown promising outcomes, these
models are typically developed for specific chronic conditions (e.g., diabetes, serious mental illness),
leaving a gap in knowledge as to whether these programs work for individuals with more complex health
and social needs. And perhaps in part due to these gaps, sustainable funding for non-traditional workforce
models remains a challenge.
POLICY AND ADVOCACY
The literature on policy and advocacy related to high-need, high-cost populations provided a range of
recommendations to support improvements across the above-mentioned domains. Addressing health
system transformation more broadly, one resource suggested that super-utilizer programs—which are
rooted in data, clinical redesign, and stakeholder engagement—can serve as a model in transforming
the overall health care delivery system.
162

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
14
The need for payment reforms that account for the important role of care coordination and multidisciplinary
teams in caring for high-need, high-cost patients was widely cited as a critical policy reform.
163–164
Along
these lines, one article suggested that payment reform should move toward risk-adjusted per patient
payment, and include incentives for quality, services provided by non-clinicians on the care team,
and population-oriented panel management.
165
Other payment mechanisms highlighted include care
management fees, episodic payments, and shared savings contracts.
166
An informational bulletin from the Centers for Medicare & Medicaid Services (CMS) described several
Medicaid policy authorities for supporting super-utilizer programs, including: enhanced federal match
for the design, development, and implementation of Medicaid Management Information Systems;
enhanced federal match for health information exchanges; administrative contracts; Medicaid health
homes; integrated care models; targeted case management services; and Medicare data access
and assistance.
167
Policies that support improved access to high-quality, real-time, all-payer data were underscored
as crucial to the success of programs for high-need, high-cost populations.
168–169
Data can highlight the
discrepancy between health expenditures and outcomes, allowing for more precise resource allocation
and gradual movement toward a high-value health care system.
170
One article referenced the important role that public health strategies can play in mitigating risk factors
associated with chronic diseases, such as those that promote smoking cessation and consumption
of healthy foods.
171
The same article recommended developing policies to support expansion of an
interdisciplinary primary care workforce.
172
Opportunities for Further Exploration
Despite some clear policy opportunities related to financing and data, there remain gaps in understanding
which policies can best support improvements in care for individuals with complex medical, behavioral
health, and social needs. As states continue to test new delivery and payment models for high-need,
high-cost populations through health homes, ACOs, and other innovative approaches, policies that
support these efforts are likely to germinate.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
15
CONCLUSION
T
his review of select literature related to high-need, high-cost populations illuminated key areas
of promise and remaining gaps in knowledge related to care model enhancements; financial
alignment and accountability; data and analytics; workforce development; and policy and
advocacy. Numerous opportunities exist to advance improvements care and cost outcomes by
addressing the gaps remaining in each of these domains.
Notably, there are a number of rigorous evaluations of intensive or complex care management programs
currently underway that promise to add to the collective understanding of what works to improve care
and reduce costs for high-need, high-cost patients. Many of these evaluations are related to programs
receiving funding through the Center for Medicare and Medicaid Innovation’s (CMMI) Health Care
Innovation Awards, with results expected to be published over the next several years. In addition
to site-specific evaluation efforts, a CMMI-funded evaluation further aims to synthesize key findings
across all of the award sites that share a common focus on high-need, high-cost patients.
While these efforts will undoubtedly improve the evidence base, additional multi-site studies—specifically,
ones that test the effectiveness of a clearly defined model of care across multiple study locations—will be
needed to advance the development of a high-fidelity approach that can be replicated broadly throughout
the U.S.
Finally, as the field of “complex care” continues to grow and expand, so will its corresponding evidence
base. Thus, a strategy of continuous quality improvement must be implemented to maintain a cutting-edge
understanding of this emerging field.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
16
APPENDICES
INDEX OF LITERATURE
A
ll of the documents reviewed for this literature review are indexed in the following pages. The following
information is provided for each document analyzed in the literature review: (1) full citation and link as available;
(2) target population; (3) key focus; (4) summary of model/intervention; and (5) a summary of key findings. The
literature is organized under five core domains: (1) Care Model Enhancements; (2) Financing and Accountability; (3) Data
and Analytics; (4) Workforce Development; and (5) Policy and Advocacy.
APPENDIX A: CARE MODEL ENHANCEMENTS
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
Aligning Forces for Quality. “Creating
Regional Partnerships to Improve Care
Transitions.” The Robert Wood Johnson
Foundation. June 2014. Available at:
http://forces4quality.org/node/7600.
Elderly or patients
with serious
or complex
conditions
Care transitions Basics of partnerships include: establishing a
cross-setting oversight team with the common
goal of reducing readmissions and improving
quality of life; providing care transition coaching
services to partner with hospitals with certain
conditions/diagnosis; sharing data and results
to assess progress toward goals; establishing
a subgroup to discuss operational issues,
coordinate scheduling of services, and improve
communication concerns.
Effective care transitions programs call for
building and sustaining strong partnerships
with health care providers in the community so
they can collaborate to achieve shared goals.
Accomplishing this is difficult in single-setting
work and becomes even more challenging and
complex when bringing providers from different
care settings together who do not typically
work with one another and approach their
work differently. Consider partnering with local
hospitals, home health agencies, area agency on
aging, and physicians.
L. Barlow. “Hospitals, Physicians
Embrace Strategies To Reduce Cost of
“Frequent Flyer” ER Visits.” Real World
Health Care. April 2013. Available
at: http://healthwellfoundation.org/
sites/default/files/4.9.13.Hospitals.
Physicians%20Embrace%20
Strategies%20to%20Reduce%20
FF%20Visits%20to%20ER.pdf.
High-frequency
emergency
department (ED)
utilizers
Intensive care
management
Two models in different states (North Carolina
and Washington). In NC, a free clinic integrates
medical checkups and group therapy, with doctors
providing treatment and patients offering each other
tips, ranging from how to obtain legal assistance
to saving money on food and shelter. In WA, a
community program was joined other hospitals and
a regional coalition of providers. It flags patients
with 2+ ED visits in a month or 4+ visits in 6
months for further examination and care planning.
The NC model reduced total ED expenses by
$405,000 over 12 months. Uninsured participants
reduced ED visits from an average of 7 to an
average of 3 per year. In WA, ED visits among
frequent flyers reduced by 50%, with a cost
savings of almost $10,000/patient. The program
saw a reduction of $2.2 million in ED and inpatient
expenses over two years.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
17
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
J. Bell, D. Mancuso, T. Krupski, J.M.
Joesch, D.C. Atkins, B. Court, et al. A
Randomized Controlled Trial of King
County Care Partners’ Rethinking
Care Intervention: Health and Social
Outcomes up to Two Years Post-
Randomization Technical Report.
Center for Health Care Strategies.
November 2012. Available at: http://
www.chcs.org/resource/randomized-
controlled-trial-of-king-county-care-
partners-rethinking-care-intervention-
health-and-social-outcomes-up-to-
two-years-post-randomization/.
Aged, Blind, and
Disabled Medicaid
beneficiaries
with evidence of
mental illness
and/or chemical
dependency,
identified as
being at risk of
having future high
medical expenses
Intensive care
coordination
Washington State’s Rethinking Care intervention
included intensive care management from
a clinical team of RNs and social workers.
Care management included an in-person
comprehensive assessment of medical and
social needs; collaborative setting of health-
related goals; chronic disease self-management
coaching; physician visits of clients accompanied
by their care managers; frequent in-person and
phone monitoring by care managers; connection
to community resources; and coordination of care
across the medical and mental health system.
Participants in the intervention were likelier to
have increased access to care, lower inpatient
medical costs, relatively fewer unplanned inpatient
admissions, and fewer deaths. In particular, those
in the intervention group: (1) had a lower increase
in inpatient medical admissions—8% versus a
20% increase in the comparison group; (2) had a
2% decrease in average PMPM cost for inpatient
medical admissions following an ED visit (e.g.,
unplanned admissions) compared to a 49% cost
increase for the comparison group; (3) had a 5%
increase in outpatient medical costs versus a
12% decrease in the comparison group; and (4)
were less likely to experience homelessness—
there was a 20% decrease in beneficiaries who
experienced at least one month of homelessness
following the intervention compared to an 18%
increase in the comparison group.
T. Bodenheimer and R. Berry-Millett.
“Care Management of Patients With
Complex Health Needs.” Robert Wood
Johnson Foundation. December
2009. Available at: http://www.rwjf.
org/content/dam/farm/reports/issue_
briefs/2009/rwjf49853/subassets/
rwjf49853_1.
Individuals with
complex health
care needs
Complex care
management
Key components to care management: (1)
identify patients most likely to benefit from care
management; (2) assess the risks and needs of
each patient; (3) develop a care plan together
with the patient/family; (4) teach the patient/
family about the diseases and their management,
including medication management; (5) coach the
patient/family on how to respond to worsening
symptoms in order to avoid the need for hospital
admissions; (6) track how the patient is doing over
time; and (7) revise the care plan as needed.
Mixed results as to whether care management
reduces hospital use and health care costs.
Stresses on primary care make it difficult to
implement effective care management. The most
effective programs target complex patients being
discharged from the hospital. Home-based care
management has largely failed to demonstrate
significant cost/quality improvements. More
success is seen if the right patients are picked:
those that are complex, but not those whose
illness is so severe that palliative or hospice care
is more appropriate. Medicare demonstrations of
care management involving patients with complex
health care needs have failed to find consistent
cost reductions (with a few exceptions). Care
management requires personnel with particular
skills not generally taught in traditional health
professional educational institutions. Integrated
delivery systems have the most resources and
capacity to develop care management programs.
T. Bodenheimer. Strategies to Reduce
Costs and Improve Care for High-
Utilizing Medicaid Patients: Reflections
on Pioneering Programs. Center for
Health Care Strategies. October 2013.
Available at: http://www.chcs.org/
resource/strategies-to-reduce-costs-
and-improve-care-for-high-utilizing-
medicaid-patients-reflections-on-
pioneering-programs/.
Super-utilizers Complex care
management
Principal sites for complex care management
models: health plan, primary care, ambulatory
intensive care unit (aICU), hospital discharge,
emergency department-based, home-based,
housing first, and community-based.
High-utilizer programs can make substantial
reductions in hospital admissions, hospital days,
ED visits, and total costs of care. Providing
permanent housing with case management—
with no medical personnel—appears to be the
most powerful way to reduce costly health care
utilization. There is a big difference between the
aICU model and the primary care model. There
is no standard composition of care management
teams. Most programs perform an initial
assessment, develop a care plan, and incorporate
regular follow-up by the care management team.
Programs tend to have a coaching rather than a
rescuing philosophy. Many programs have a home
visit component; some allow patients to access
the care management team 24/7. Coaching
patients to understand their medications and to
become more medication adherent is an essential
feature of all programs. Caseloads vary with team
size, team composition, and patient complexity.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
18
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
R.S. Brown, D. Peikes, G. Peterson, J.
Schore, and C.M. Razafindrakoto. “Six
Features Of Medicare Coordinated
Care Demonstration Programs That
Cut Hospital Admissions Of High-Risk
Patients.” Health Affairs, 31, no. 6
(2012): 1156-66. Care Management
Toolkit.” Available at: http://content.
healthaffairs.org/content/31/6/1156.
abstract.
High-risk
Medicare
beneficiaries
Intensive care
management
The six approaches practiced by care coordinators
in the Medicare Coordinated Care Demonstration
programs that were effective include: (1)
supplementing telephone calls to patients with
frequent in-person meetings; (2) occasionally
meeting in person with providers; (3) acting as a
communications hub for providers; (4) delivering
evidence-based education to patients; (5)
providing strong medication management; and (6)
providing timely and comprehensive transitional
care after hospitalizations.
Four of 11 Medicare Coordinated Care
Demonstration programs reduced hospitalizations
by 8-33 percent among enrollees who had a high
risk of near-term hospitalization. Results suggest
that incorporating these approaches into medical
homes, accountable care organizations, and other
policy initiatives could reduce hospitalizations and
improve patients’ lives. However, the approaches
would save money only if care coordination fees
were modest and organizations found cost-effective
ways to deliver the interventions. None of these
programs generated net savings to Medicare.
California Quality Collaborative
(2012). “Complex Care Management
Toolkit.” Available at: http://www.
calquality.org/storage/documents/
cqc_complexcaremanagement_toolkit_
final.pdf.
Individuals with
multiple chronic
conditions, limited
functional status,
and psychosocial
needs
Complex care
management
Typical complex care management models:
(1) embedded care manager model (care
manager located onsite); (2) centrally located
care management agency provides services to
multiple practice sites; or (3) “brick and mortar”
clinic where an “intensivist” is assigned a high-
risk patient panel. Care teams usually consist
of a nurse care manager, PCP, social worker,
behavioral health specialist, and other care
providers as necessary.
Key considerations for building a care model for
complex patient populations include: developing
levels within your complex care program that vary
based on severity of illness; taking a broad and
interdisciplinary approach to building your complex
care team—build on what you have and align
with the needs of the patients you are managing;
promoting face-to-face interaction between care
managers and patients; emphasizing patient self-
management techniques; making care transitions
support a priority; and using virtual or in-person
multi-disciplinary case conferences.
Corporation for Supportive Housing
(2009). “Summary of Studies:
Medicaid/Health Services Utilization
and Costs.” Available at: http://
pschousing.org/files/SH_cost-
effectiveness_table.pdf.
Criteria varies;
primarily
individuals who
are homeless or
unstably housed
with multiple
chronic conditions
Housing
intervention
Variety of housing programs implementing
“housing first” interventions for complex-needs
individuals. Evaluated for utilization of health and
other services.
Select Key Impacts
San Francisco: During the one year after entering
supportive housing, individuals had fewer ED visits
and fewer inpatient hospital admissions.
Chicago Housing for Health Partnership
Program: Fewer hospitalizations per person per
year; fewer ED visits per person per year (24%
reduction); 45% fewer days nursing home.
Massachusetts Statewide Pilot: Medicaid costs
after housing intervention significantly decreased.
Connecticut Partnership for Strong
Communities (2012). “Connecticut
Integrated Healthcare & Housing
Neighborhoods.” Available at: http://
pschousing.org/files/Connecticut%20
Integrated%20Healthcare%20and%20
Housing%20Neigborhoods%20
Summary%20%28March%20
2012%29.pdf.
Medicaid-
enrolled/ eligible
high-utilizers who
are homeless
or at-risk of
homelessness,
with chronic
conditions
Housing
intervention
Health home outreach model using assertive
outreach and care coordination to link high-cost,
high-need clients with primary care, behavioral
health care, and supportive/affordable housing.
Multidisciplinary health teams established in
multiple regions of the state through partnerships
between Federally Qualified Health Centers, Local
Mental Health Authorities, and supportive housing/
public housing providers, homeless service/
outreach programs, and the state’s Medicaid
Medical Administrative Services Organization
(ASO). High utilizers identified through local
hospitals to ensure effective transitions from care.
In Connecticut, an identified cohort of adult
Medicaid beneficiaries who are homeless,
high-cost utilizers of health services had average
annual Medicaid payments of $67,992 per
person. This is 9 times more expensive than the
average Medicaid beneficiary. In 2011, the state
budget dedicated $100 million to affordable
housing over two years and $30 million in capital
funding to develop 150 new units of additional
supportive housing. In February, Gov. Malloy
announced his housing proposal for the state
budget, which includes $300 million over 10 years
for public housing revitalization, an additional $20
million for affordable housing, and 150 new rental
assistance vouchers for scattered site supportive
housing.
R. Davis and A. Maul. Trauma-Informed
Care: Opportunities for High-Need,
High-Cost Medicaid Populations.
Center for Health Care Strategies.
March 2015. Available at: http://www.
chcs.org/resource/trauma-informed-
care-opportunities-high-need-high-
cost-medicaid-populations/.
High-need, high-
cost Medicaid
beneficiaries
Trauma-informed
care
Individuals who experience trauma, particularly
in childhood, have much higher incidences of
chronic disease and behavioral health issues.
Trauma-informed care seeks to change the
clinical perspective from asking, “What is wrong
with you?” to “What happened to you?”
Using trauma-informed care to better engage
with this difficult-to-reach population can help
providers and case managers build a trusting
relationship with individuals with a history of
trauma, and may help enhance quality and cost
outcomes for the Medicaid program overall.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
19
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
M. Gerrity, E. Zoller, N. Pinson, C.
Pettinari, and V. King. “Integrating
Primary Care into Behavioral Health
Settings: What Works for Individuals
with Serious Mental Illness.” Millbank
Memorial Fund. 2014. Available at:
http://www.milbank.org/uploads/
documents/papers/Integrating-Primary-
Care-Report.pdf.
Individuals with
serious mental
illness and
substance use
disorder
Behavioral health
integration
Behavioral health integration into primary care
for individuals with serious mental illness (SMI).
The continuum of models ranges from separate
systems and practices with little communication
among providers, to enhanced coordination and
collaboration among providers usually involving
care or case managers, to co-located care with
providers sharing the same office or clinic, to
fully integrated care where all providers function
as a team to provide joint treatment planning. In
a fully integrated system, patients and providers
experience the operation as a single system
treating the whole person.
Care management may improve mental health
symptoms and mental health related quality of life
for patients with bipolar disorder and SMI. Fully
integrated care and care management improves
use of preventive and medical services and may
improve physical health symptoms and quality
of life for patients with bipolar disorder and SMI.
Co-locating primary care in chemical dependency
treatment settings without enhanced coordination
and collaboration does not improve mental
or physical health outcomes. All interventions
required additional staff, training, and oversight
except when intervention staff was dually trained
in primary care and substance use treatment.
J. Greene, J.H. Hibbard, R. Sacks, V.
Overton, and C.D. Parrotta. “When
Patient Activation Levels Change,
Health Outcomes And Costs Change,
Too.” Health Affairs, 34, no. 3 (2015):
431-437. Available at: http://content.
healthaffairs.org/content/34/3/431.
abstract.
Adult primary care
patients
Patient activation Patient Activation Measure (PAM) scores collected
during primary care office visits at baseline (in
2010) and two years later (2012) were examined
against health outcomes related to cholesterol,
triglycerides, PHQ-9, smoking, and obesity.
Higher activation in 2010 was associated with
nine out of thirteen better health outcomes—
including better clinical indicators, more healthy
behaviors, and greater use of women’s preventive
screening tests—as well as with lower costs
two years later. More activated patients were
significantly more likely than less activated
patients to have HDL, serum triglycerides, and
PHQ-9 in the normal range; to be nonsmokers;
and not to be obese. Future research is needed
to establish whether or not the association
represents a causal relationship.
D. Hasselman. Super-Utilizer Summit:
Common Themes from Innovative
Complex Care Management Programs.
Center for Health Care Strategies.
October 2013. Available at: http://
www.chcs.org/resource/super-utilizer-
summit-common-themes-from-
innovative-complex-care-management-
programs/.
Super-utilizers Intensive care
management
Care teams typically include nursing, social work,
and community outreach expertise. Interventions
include extensive outreach and engagement;
24-hour on-call system; frequent contacts with
patients (face-to-face is priority); medication
reconciliation/management; patient-caregiver self-
management education; timely outpatient follow-
up post-discharge; linkage to a primary care
provider/medical home; goal setting and care plan
development; health education/coaching; pain
management; management of chronic conditions
(e.g., diabetes, asthma); preparation for provider
visits; and linkages to housing, substance abuse
treatment, and other community resources.
Individuals’ basic needs—housing, jobs, child
care, and food insecurity—must be addressed
before physical health can be impacted. Programs
“frontload social services” and typically use
non-clinicians and non-traditional providers such
as social workers and community health workers
to address gaps in and needs for social services.
Essential to figure out which patients need which
interventions in which setting by which provider—
this complex equation was noted as the “holy
grail.” Medication management is a critical task
that must be done in the patient’s home to be
most effective.
J. Hibbard, J. Greene, and M. Tusler.
“Improving The Outcomes of Disease
Management by Tailoring Care to the
Patient’s Level of Activation.” The
American Journal of Managed Care,
15, no. 6 (2009): 353-360. Available
at: http://www.ncbi.nlm.nih.gov/
pubmed/19514801.
Individuals with
chronic conditions
Patient activation A quasi-experimental pre-post design was
utilized, with an intervention group, using a
tailored approach and a control group was
coached in the usual way. Intervention coaches
used baseline Patient Activation Measure (PAM)
scores to segment patients based on 4 levels of
activation. The coaches were then trained and
given guidelines to customize telephonic coaching
based on the activation level.
Findings suggest that using tailored coaching
models to the patients’ activation level with
alignment of metrics improves outcomes for
disease management.
J. Hibbard, J. Greene, Y. Shi, J. Mittler,
and D. Scanlon. “Taking the Long View:
How Well Do Patient Activation Scores
Predict Outcomes Four Years Later?”
Medical Care Research and Review,
Published online, February 24, 2015:
doi: 10.1177/1077558715573871.
Available at: http://mcr.sagepub.com/
content/early/2015/02/24/10775587
15573871.abstract.
Individuals with
chronic conditions
Patient activation Researchers examined the extent to which
characteristics such as medication adherence,
health behaviors, functional health, and costly
health care utilization were related to PAM scores
at baseline and 4 years later.
The benefits of patient activation are enduring,
and include: better self-management, improved
functioning, and lower use of costly health care
services over time. When activation levels change,
many outcomes change in the same direction.
Health care delivery systems can use this
information to personalize and improve care.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
20
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
J.Y. Kim, T.C. Higgins, D. Esposito,
A.M. Gerolamo, and M. Flick. SMI
Innovations Project in Pennsylvania:
Final Evaluation Report. Mathematica
Policy Research. October 2012.
Available at: http://www.chcs.org/
resource/smi-innovations-project-in-
pennsylvania-final-evaluation-report/.
Adult Medicaid
beneficiaries
with SMI and co-
occurring physical
health conditions
Complex care
management
The programs varied, but were based on five key
principles: (1) information exchange and joint
care planning across physical and behavioral
health; (2) engaging consumers in care; (3)
engaging providers to partner in care and become
designated care homes; (4) providing follow-
up after hospitalizations and ED visits; and (5)
improving medication management. Plans also
had performance bonuses.
Although outcomes varied across the two regions,
the evaluation identified that one or both pilots
were successful at reducing the rate of mental
health hospitalizations, all-cause readmissions,
and emergency department visits. Compared
with projected trends in these outcomes
without the interventions: (1) the rate of mental
health hospitalizations was an estimated 12
percent lower (Southwest); (2) the all-cause
readmission rate was an estimated 10 percent
lower (Southwest); and (3) the rate of emergency
department (ED) use was an estimated 9 percent
lower (Southeast).
K.W. Linkins, JJ. Brya, D.W. Chandler.
“Frequent Users of Health Services
Initiative: Final Evaluation Report.”
California HealthCare Foundation.
August 2008. Available at: http://
www.chcf.org/~/media/MEDIA%20
LIBRARY%20Files/PDF/F/PDF%20
FUHSIEvaluationReport.pdf.
Frequent
emergency
department (ED)
users
Intensive care
management
Six models ranged from various types of
intensive case management to less intensive
peer- and paraprofessional-driven interventions.
All interventions sought to redirect care from
the emergency department to lower-cost
community-based settings by: assisting frequent
users to access and navigate existing resources;
decreasing psychosocial problems such as
homelessness and substance use; and improving
care coordination.
The programs yielded statistically significant
reductions in ED use (30%) and hospital charges
(17%) in the first year of enrollment. ED utilization
and charges decreased by an even greater
magnitude in the second year after enrollment.
Those connected to housing showed significantly
greater reductions in the number of inpatient days
(a 27% decrease for those connected vs. a 26%
increase for those not connected) and inpatient
charges (a 27% decrease for those connected vs.
a 49% increase for those not connected).
D.B. Mautner, H. Pang, J.C. Brenner,
J.A. Shea, K.S. Gross, R. Frasso, et al.
“Generating Hypotheses About Care
Needs of High Utilizers: Lessons from
Patient Interviews.” Population Health
Management, 16, Suppl. (2013): S26-
33. Available at: http://www.ncbi.nlm.
nih.gov/pubmed/24070247.
Complex, high-
utilizing patients
Social
determinants
of health
This qualitative study identifies psychosocial
factors and life experiences described by complex
patients with high levels of emergency and
hospital-based health care utilization that may be
important to their care needs. Semi-structured
interviews were conducted with 19 patients of the
Camden Coalition of Healthcare Providers’ Care
Management Team.
Investigators identified three key themes: (1)
Early-life instability and traumas, including
parental loss, unstable or violent relationships, and
transiency, informed many participants’ health and
health care experiences; (2) many “high utilizers”
described a history of difficult interactions with
health care providers during adulthood; (3) over
half of the participants described the importance
to their well-being of positive and “caring”
relationships with primary health care providers
and the outreach team. Additionally, the transient
and vulnerable nature of this complex population
posed challenges to follow-up, both for research
and care delivery. Investigators should test new
modes of care delivery that attend to patients’
trauma histories.
C. Michalopoulos, M. Manno, S.E. Kim,
and A. Warren. “The Colorado Regional
Integrated Care Collaborative Managing
Health Care for Medicaid Recipients
with Disabilities: Final Report on the
Colorado Access Coordinated Care Pilot
Program.” MDRC, April 2013. Available
at: http://www.mdrc.org/sites/default/
files/Managing_Health_Care_FR.pdf.
Blind or disabled
Medicaid
recipients
(considered
high-risk for
hospitalization)
Intensive care
coordination
Colorado Access provided intensive coordinated
care services, with a focus on social and
nonclinical service delivery. Coordinated care was
provided primarily by telephone, care managers
sometimes met members in person (facilitated by
having care team members in Kaiser Permanente
Colorado’s clinics).
There is little evidence that the Colorado Access
program affected outpatient care. Of the six
outcomes examined, there were significant
estimated impacts only on the probability of
visiting a non-physician. The average number
of admissions per 1,000 client months during
the first year was 24.0 for the program group
compared with 20.0 for the control group.
C.J. Peek, M.A. Baird, and E. Coleman.
“Primary Care for Patient Complexity,
Not Only Disease.” Family, Systems
and Health, 27, no. 4 (2009): 287-302.
Available at: http://www.ncbi.nlm.nih.
gov/pubmed/20047353.
Patients with
multiple chronic
conditions
Assessment Analysis of what is meant by “complexity” in
primary care setting and how to best tailor care
delivery to complex patients.
Patient complexity is defined as “interference with
standard care and decision-making by symptom
severity or impairments, diagnostic uncertainty,
difficulty engaging care, lack of social safety or
participation, disorganization of care, and difficult
patient-clinician relationships. Patient-centered
medical homes must address patient complexity
by promoting the interplay of usual care for
conditions and individualized attention to patient-
specific sources of complexity—across whatever
diseases and conditions the patient may have.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
21
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
B.W. Powers, S.K. Chaguturu, and T.G.
Ferris. “Optimizing High-Risk Care
Management.” Journal of the American
Medical Association, 313, no. 8 (2015):
795-6. Available at: http://jama.
jamanetwork.com.ezproxy.princeton.
edu/article.aspx?articleid=2099528.
Individuals
with complex,
co-occurring
conditions
Complex care
management
Program structure varies, but most involve care
managers who work with panels of high-risk
patients to coordinate care across clinicians;
engage patients in setting and achieving
health-related goals; and monitor and track
health outcomes. Although these programs
have traditionally been managed by payers or
third-party vendors, clinicians and health care
organizations are increasingly adopting programs
of their own.
High-risk care management programs that are
practice-based, payer-catalyzed, and purchaser-
supported have the greatest potential to deliver
better care at lower cost. Achieving the potential of
high-risk care management requires a coordinated
strategy in which purchasers, payers, and health
care organizations leverage their unique capabilities
without redundancy or duplication.
L.S. Sadowski, R.A. Kee, T.J.
VanderWeele, and D. Buchanan. “Effect
of a Housing and Case Management
Program on Emergency Department
Visits and Hospitalizations Among
Chronically Ill Homeless Adults: A
Randomized Trial.” Journal of the
American Medical Association, 301,
no. 17 (2009): 1771-8. Available
at: http://www.ncbi.nlm.nih.gov/
pubmed/19417194.
Social-worker
referred homeless
adults with
chronic medical
illnesses at a
public teaching
hospital and
private nonprofit
hospital
Housing
intervention
Transitional housing offered after hospital
discharge, followed by long-term housing with
case management offered on-site at primary
study sites, transitional housing, and stable
housing sites.
Compared with the usual care group, the
intervention group had a relative reduction of
29% in hospitalizations, 29% in hospital days,
and 24% in emergency department visits. The
researchers did not evaluate the specific types
of case management services provided or their
costs, and were not able to distinguish housing
effects from case management effects.
M. Shumway, A. Boccellari, K. O’Brien,
and R.L. Okin. “Cost-Effectiveness
of Clinical Case Management for
ED Frequent Users: Results of a
Randomized Trial.” American Journal of
Emergency Medicine, 26, no. 2, (2008):
155-64. Available at: http://www.ncbi.
nlm.nih.gov/pubmed/18272094.
Frequent ED users Clinical case
management
A 24- month randomized trial with 252 frequent
ED users were randomized (167 to case
management, 85 to usual care(. The study
included obtaining data on psychosocial problems
through interviews and service usage and cost
data from administrative records.
The participants that received case management
had statistically significant reductions in ED use
and cost. Those individuals that received case
management and usual care patients did not differ
in use or cost of other hospital services.
R. Voss, R. Gardner, R. Baier, K.
Butterfield, S. Lehrman and S.
Gravenstein. “The Care Transitions
Intervention Translating From Efficacy
to Effectiveness.” Archive of Internal
Medicine; 171, no. 14 (2011): 1232-7.
Available at: http://archinte.jama
network.com/article.aspx?articleid=
1105851&resultClick=3.
Medicare patients Care transitions Quasi-experimental prospective cohort study
conducted in Rhode Island with a sample of
fee-for-service Medicare patients, with chronic
health conditions (cardiac or respiratory) eligible to
receive Care Transitions Interventions (CTI) and a
control group that did not receive the intervention.
Participants were not randomized, coaches
used the patient census lists to identify patients
meeting the criteria. CTI is a patient-centered
intervention model that consists of home visits
and one telephone call designed to empower
individuals to manage their health and more
effectively engage with providers.
Among the intervention group that received the
intervention, the odds of hospital readmissions
within 30 days of discharge were lower following
hospitalizations, when compared with those who
were never approached. The intervention group’s
reduced readmission rate (36.0% compared
with the external control group). The study adds
to supporting the use of the CTI upon hospital
discharge for medical patients.
J. Xing, C. Goehring, and D. Mancuso.
“Care Coordination Program For
Washington State Medicaid Enrollees
Reduced Inpatient Hospital Costs.”
Health Affairs, 34, no. 4 (2015):
653-661. Available at: http://content.
healthaffairs.org/content/34/4/653.full.
Medicaid
beneficiaries with
complex health
care needs
Care
coordination
In Washington State, a care coordination
intervention, the Chronic Care Management
program, was implemented for clinically complex
Medicaid beneficiaries who met risk criteria
defined by a predictive modeling algorithm. The
program involved intensive care management,
care coordination, and patient education and
training in self-management skills. We used
propensity score matching to evaluate the
program’s impact on health care spending and
utilization and mortality.
Large and significant reductions in inpatient
hospital costs ($318 per member per month) were
found among patients who used the program.
The estimated reduction in overall medical
costs of $248 per member per month exceeded
the cost of the intervention, but did not reach
statistical significance. These results suggest that
well-designed targeted care coordination services
could reduce health care spending for Medicaid
beneficiaries with complex health care needs.
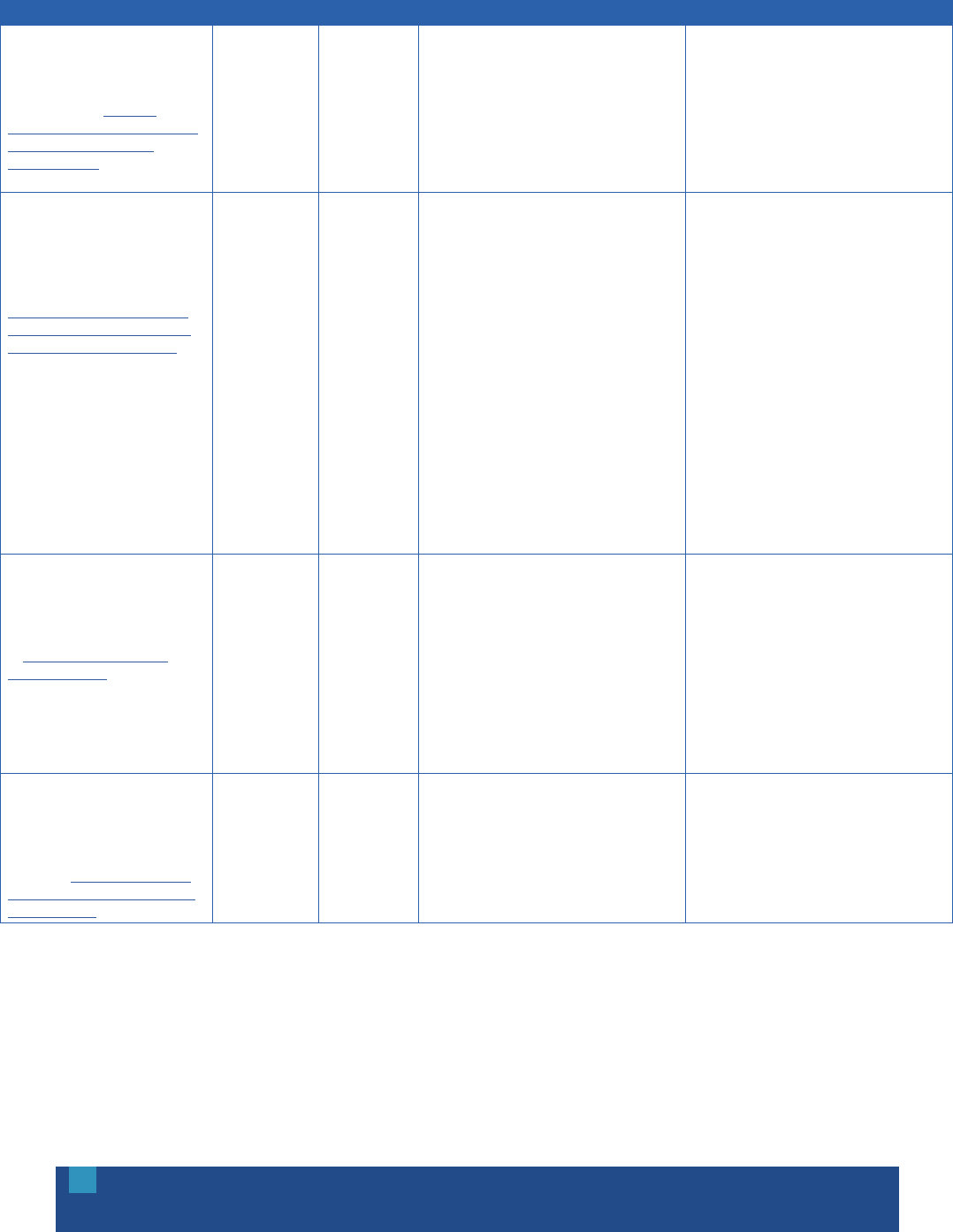
OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
22
APPENDIX B: FINANCING AND ACCOUNTABILITY
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
J. Alper and A. Baciu. “Roundtable
on Population Health Improvement:
Financing Population Health
Improvement.” Institute of Medicine,
2014. Available at: http://iom.
nationalacademies.org/Reports/2014/
Financing-Population-Health-
Improvement.aspx.
United States
population
Population health A fundamental but often overlooked driver of the
imbalance between spending and outcomes in the
U.S. is the nation’s inadequate investment in non-
clinical strategies that promote health and prevent
disease and injury population-wide, strategies that
fall under the rubric of “population health.”
Given that it is unlikely that government funding
for governmental public health agencies, whether
at the local, state, or federal levels, will see
significant and sustained increases, there is
interest in finding creative sources of funding
for initiatives to improve population health, both
through the work of public health agencies
and through the contributions of other sectors,
including non-health entities.
D. Bachrach, S. Anthony, and A. Detty.
“State Strategies for Integrating
Physical and Behavioral Health
Services in a Changing Medicaid
Environment.” The Commonwealth
Fund. August 2014. Available at:
http://www.commonwealthfund.org/
publications/fund-reports/2014/aug/
state-strategies-behavioral-health.
Medicaid
beneficiaries with
comorbid physical
and behavioral
health conditions
Physical/
behavioral health
Integration
States are deploying various administrative,
purchasing, and regulatory strategies to address
or eliminate system-level barriers to integrated
care for this medically complex and high-cost
Medicaid population.
Administrative strategies include: consolidating
the agencies responsible for physical/mental
health and substance use disorder services;
consolidating behavioral health purchasing,
contracting, and rate-setting in their Medicaid
agency and retaining licensing and clinical policy
in the behavioral health agencies; or informal
collaborations to rationalize strategies across
agencies. Purchasing strategies include: policies
to create linkages across providers and systems,
especially in states with carve-out models; and
implementation of fully integrated managed
care approaches, in some cases targeted to
individuals with serious mental illness. Regulatory
strategies include: streamlining licensing rules and
creating credentialing programs for nontraditional
providers; revising Medicaid same-day visit
policies; establishing billing codes for emerging
treatments; and supporting policies allowing for
greater information exchange.
E.H. Bradley, B.R. Elkins, J. Herrin, and
B. Elbel. “Health and Social Services
Expenditures: Associations with Health
Outcomes.” BMJ Quality and Safety,
20, no. 10 (2011): 826-31. Available
at: http://www.ncbi.nlm.nih.gov/
pubmed/21447501.
Various Health care
spending
Examined variations in health service expenditures
and social services expenditures across
Organisation for Economic Co-operation and
Development (OECD) countries and assess their
association with five population-level health
outcomes: life expectancy at birth, infant mortality,
low birth weight, maternal mortality, and potential
years of life lost.
Health services expenditures adjusted for
gross domestic product (GDP) per capita were
significantly associated with better health
outcomes in only two of five health indicators;
social services expenditures adjusted for GDP
were significantly associated with better health
outcomes in three of five indicators. The ratio of
social expenditures to health expenditures was
significantly associated with better outcomes in
infant mortality, life expectancy and increased
potential life years lost, after adjusting for the level
of health expenditures and GDP.
J. Corrigan and E. Fisher. “Accountable
Health Communities: Insights from
State Health Reform Initiatives.” The
Dartmouth Institute for Health Policy
& Clinical Practice, November 2014.
Available at: http://tdi.dartmouth.edu/
images/uploads/AccountHealthComm-
WhPaperFinal.pdf.
Geographically
defined
populations
Accountable
health
communities
Three states—Colorado, Minnesota, and
Oregon—have health reform plans that envision
evolving roles at the community level in health
system oversight and financing.
Breadth of vision, local leadership, delivery system
integration, payment reform, accountability, and
investment strategy for addressing non-health
determinants are all important factors in designing
these programs. While substantial uncertainty
remains, this approach suggests that community-
level engagement in health reform—“accountable
health communities”—is promising.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
23
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
M. Crawford and R. Houston. State
Payment and Financing Models to
Promote Health and Social Service
Integration. Center for Health Care
Strategies. February 2015. Available at:
http://www.chcs.org/resource/state-
payment-financing-models-promote-
health-social-service-integration/.
High-cost, high-
need Medicaid
beneficiaries
Financial
alignment
While models for integrating health and social
services have not yet been fully tested, states
are eager to develop new programs and
expand existing small-scale efforts to reap the
potential health and cost benefits of integration
and build a more effective and sustainable
health care system. Many states will pursue
a gradual transformation toward financing
integration, characterized by three phases: (1)
pilot or demonstration; (2) intermediate ramp-up/
expansion; and (3) advanced, fully operational.
Pilots/demonstrations are typically financed using
federal grants, philanthropic funds, or social
impact investments. Financing for expansion
of integration programs is typically via state
trust funds/pools or Medicaid waivers. And fully
operational integration programs can be financed
using braided/blended funding from Medicaid,
federal funds, block grants, state/local budgets.
Payment mechanisms that incentivize providers to
encourage or facilitate connections include shared
savings arrangements, bundled payments, direct
payment to social service entities, and a global
community health budget, etc.
M. Crawford, T. McGinnis, J. Auerbach,
and K. Golden. “Population Health in
Medicaid Delivery System Reforms.”
Milbank Memorial Fund. March 2015.
Available at: http://www.milbank.org/
uploads/documents/papers/CHCS_
PopulationHealth_IssueBrief.pdf.
Medicaid
beneficiaries
Population health Many see policies focused on the health of
a population as a vehicle for bringing health
care delivery systems, public health agencies,
behavioral health, social services, and other
entities together to improve health outcomes in
their communities.
New opportunities provided by the Affordable
Care Act enable states and regional jurisdictions
to test innovative payment and delivery system
reform initiatives, often through accountable care
collaboratives, including Medicaid ACOs and
regional care organizations.
M. Evans. “Residential Therapy:
Hospitals Take on Finding Housing for
Homeless Patients, Hoping to Reduce
Readmissions, Lower Cost.” Modern
Healthcare, September 2012. Available
at: http://www.modernhealthcare.
com/article/20120922/
MAGAZINE/309229988.
Chronically ill/
costly patients;
homeless patients
Housing first Pilots programs underway across the country
(e.g., Hennepin County, MN, San Francisco,
New York City) that provide costly and complex
Medicaid patients with housing in an effort to
reduce hospital readmissions.
In preliminary results for homeless patients in
New York City’s pilot, monthly Medicaid spending
dropped by one-fifth, or $855, to $3,426 a
person. Overall, hospitalizations dropped by 47%
and emergency room visits fell by more than
half. Spending for hospital care fell by 27% and
emergency room spending by 30%. Early results
in Hennepin County are promising. Key takeaway:
Under pressure to cut costs? Find housing for the
most expensive patients who need a place to live.
A. Hamblin, J. Verdier, and M. Au. State
Options for Integrating Physical and
Behavioral Health Care. Center for
Health Care Strategies. October 2011.
Available at: http://www.chcs.org/
resource/state-options-for-integrating-
physical-and-behavioral-health-care/.
High-need, high-
cost Medicaid
beneficiaries
Physical/
behavioral health
Integration
Four integration models with various lead
organizations serving as the core integrated care
entity, including: (1) managed care organizations
(MCOs); (2) primary care case management
programs (PCCMs); (3) behavioral health
organizations (BHOs); and (4) MCO/PCCM and BHO
partnerships as facilitated by financial alignment.
Key elements to each model, which can be
enforced by state purchasing contracts, include
the following: (1) Aligned financial incentives
across physical and behavioral health systems; (2)
Real-time information sharing across systems to
ensure that relevant information is available to all
members of a care team; (3) Multidisciplinary care
teams that are accountable for coordinating the
full range of medical, behavioral, and long-term
supports and services, as needed; (4) Competent
provider networks; and (5) Mechanisms for
assessing and rewarding high-quality care.
S.L. Hayes, M.K. Mann, F.M. Morgan,
M.J. Kelly, and A.L. Weightman.
“Collaboration Between Local Health
and Local Government Agencies
for Health Improvement.” Cochrane
Database of Systematic Reviews,
October 2012. Available at: http://www.
ncbi.nlm.nih.gov/pubmed/23076937.
All population
types and all
age groups
were included
Interagency
collaboration
Evaluated the effects of interagency collaboration
between local health and local government
agencies on health outcomes, by conducting a
literature review of studies that reported individual
health outcomes arising from interagency
collaboration between health and local
government agencies compared to standard care.
Collaboration between local health and local
government is commonly considered best
practice. However, the review did not identify any
reliable evidence that interagency collaboration,
compared to standard services, necessarily leads
to health improvement. Collaborative community
partnerships can be established to deliver
interventions, but it is important to agree on goals,
methods of working, monitoring and evaluation
before implementation to protect program fidelity
and increase the potential for effectiveness.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
24
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
R. Mahadevan and R. Houston.
Supporting Social Service Delivery
through Medicaid Accountable Care
Organizations: Early State Efforts.
Center for Health Care Strategies.
February 2015. Available at: http://
www.chcs.org/resource/supporting-
social-services-medicaid-accountable-
care-organizations-early-efforts/.
Medicaid
beneficiaries
Accountable
care
Medicaid accountable care organizations
across the country that are taking initial steps
to provide essential non-medical supports to
high-need, high-cost beneficiaries. Financial
incentives offer a powerful vehicle for fostering
social service coordination.
By instituting a shared savings or capitated
payment for ACO programs, states can motivate
closer collaboration between the health care
delivery system and non-medical agencies and
providers. State approaches range from integrated
payment models connecting social services and
providers, to one-time grants supporting provider
capacity-building.
Massachusetts Housing and Shelter
Alliance. “Home and Healthy for
Good—Permanent Supportive Housing:
A Solution-Driven Model.” Progress
Report, January 2014. Available at:
https://givingcommon.guidestar.org/
ViewEdoc.aspx?eDocId=2698132&
approved=True.
Chronically
homeless adults
Housing first Housing first model in Massachusetts called Home
and Healthy for Good (HHG). The state allocated
$600,000 to the Massachusetts Housing and
Shelter Alliance (MHSA) through the Department
of Transitional Assistance to operate the Home
& Healthy for Good (HHG) program. The state
allocation for HHG is flexible, allowing the resource
to be used for supportive services, housing or
both. Seventeen homeless service providers
now participate in the program as agencies
subcontracted by MHSA.
Providing housing and supportive services to
chronically homeless individuals through a
Housing First model is less costly and more
effective than managing their homelessness
and health problems on the street or in shelter.
Results show a trend toward tremendous savings
in health care costs, especially hospitalizations,
when chronically homeless individuals are placed
into housing with services. Improvements in
quality of life and overall health outcomes indicate
that Housing First is an effective intervention for
chronically homeless individuals.
S.F. Sandberg, C. Erikson, R. Owen,
K.D. Vickery, S.T. Shimotsu, M. Linzer,
et al. “Hennepin Health: A Safety-Net
Accountable Care Organization For
The Expanded Medicaid Population.”
Health Affairs, 33, no. 11 (2014):
1975-84. Available at: http://content.
healthaffairs.org/content/33/11/1975.
abstract.
Medicaid Accountable
care
Hennepin Health assumes full risk for Medicaid
expansion patients enrolled in the plan, and
receives a per member per month capitation
payment from the state to cover the cost of all
Medicaid services for the enrolled population.
Social services are paid for with human service
funds from preexisting state and county sources,
supplemented by the health plan’s per member
per month payments. Monthly social service
expenses are tracked to analyze whether savings
in medical care are offset by an increase in
costs for social services. Hennepin Health has
strategically used reinvestment funds from
previous years to provide additional training; hire
additional team members; and further the overall
strategy of coordinating medical, behavioral, and
social services.
Hennepin Health has had an impact on shifting
care from the ED and the hospital to outpatient
settings. Decrease in ED visits of 9.1% per
1,000 member months, with a corresponding
increase in outpatient visits of 3.3% during the
same time period. The percentage of patients
receiving optimal diabetes care increased from
8.6% in the second half of 2012 to 10% in the
second half of 2013. The percentage of patients
receiving optimal vascular care increased from 25
to 36.1%. The percentage of patients receiving
optimal asthma care increased from 10.6% in
the last five months of 2012 to 13.8% in the last
five months of 2013. Hennepin Health has also
achieved a high patient satisfaction rating: 87%
of members report that they are satisfied with
their care.
L.C. Weinstein, M.D. LaNoue, J.D.
Plumb, H. King, B. Stein and S.
Tsemberis. “A Primary Care-Public
Health Partnership Addressing
Homelessness, Serious Mental Illness,
and Health Disparities.” Journal of the
American Board of Family Medicine,
26, no. 3 (2013): 279-87. Available
at: http://www.ncbi.nlm.nih.gov/
pubmed/23657696.
Individuals with
SMI who are
homeless
Housing first Jefferson Department of Family and Community
Medicine and Pathways to Housing-PA (PTH-PA)
formed a formal partnership, and a primary
care physician was embedded into the PTH-PA
Assertive Community Treatment team to provide
on-site primary care and population-based
health monitoring and services. The partnership
draws from general departmental resources, the
St. Elizabeth’s community satellite clinic, and
the main family medicine practice, Jefferson
Family Medicine Associates. Additional clinical,
evaluation, and educational partnerships have
been formed with the Jefferson’s Center for Urban
Health, Department of Emergency Medicine,
School of Nursing, and School of Public Health.
The intersection of primary care with public
health efforts, including the potential overlap of
outcomes, is relatively new. Preliminary program
evaluation results suggest that this partnership is
evolving to function as an integrated person-
centered health home and an effective local public
health monitoring system. Multiple measures
provide preliminary evidence that this model
is feasible and can address the challenges of
integrated community health services.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
25
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
B.P. Zeigler, S.A. Redding, B.A. Leath,
and E.L. Carter. “Pathways Community
HUB: A Model for Coordination of
Community Health Care.” Population
Health Management, 17, no. 4 (2014):
199-201. Available at: http://online.
liebertpub.com/doi/abs/10.1089/
pop.2014.0041.
Individuals with
care needs
spanning multiple
systems
Integration The Pathways Community HUB Model is a delivery
system for care coordination services provided
in a community setting. The Pathways model
provides a unique strategy to effectively supplement
clinical services with the social services needed
to overcome social barriers to health for those
most at risk. The HUB coordinates agencies and
service providers in the community to eliminate the
inefficiencies and duplication that exists among
them. At the foundation of the model are these
primary features: 1) Core Pathways, 2) the HUB
itself, and 3) payments linked to outcomes.
The HUB model requires extensive change on
many levels—contracting, payment methodology,
and collaboration. The Pathways Community HUB
model not only requires that all care coordination
activities in a region be transmitted through a
central organization (i.e., the HUB), but also that
payments are directly aligned with the production
of positive outcomes through the Pathways.
Payers save money because of efficiencies
afforded by dealing with only one HUB rather than
a multitude of individual agencies. Savings also
accrue because of the reduction/elimination of
redundant services.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
26
APPENDIX C: DATA AND ANALYTICS
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
D.W. Bates, S. Saria, L. Ohno-Machado,
A. Shah, and G. Escobar. “Big Data
In Health Care: Using Analytics To
Identify And Manage High-Risk And
High-Cost Patients.” Health Affairs,
33, no. 7 (2014): 1123-31. Available
at: http://content.healthaffairs.org/
content/33/7/1123.abstract.
High-risk, high-
cost patients
Identification/
Stratification
Examines six use cases for high-risk patients
where some of the clearest opportunities exist to
reduce costs through the use of big data.
Big data can be particularly effective at reducing
costs when focused on: high-cost patients,
readmissions, triage, decompensation (when a
patient’s condition worsens), adverse events,
and treatment optimization for diseases affecting
multiple organ systems.
J. Billings and M.C. Raven. “Dispelling
An Urban Legend: Frequent Emergency
Department Users Have Substantial
Burden Of Disease.” Health Affairs, 32,
no. 12 (2013): 2099-2108. Available
at: http://content.healthaffairs.org/
content/32/12/2099.abstract.
Frequent ED
utilizers
Identification/
Stratification
Study of Medicaid ED users in New York City,
looking retrospectively at Medicaid fee-for-service
claims and managed care records for Medicaid
patients (ages 18-62). Examined eligibility, use,
spending, and diagnostic history to determine
whether it is possible to predict who will become a
frequent ED user with predictive modeling.
Extremely frequent ED users (those with 10+
visits) represented only 1.7 percent of all ED
users; 29 percent of all ED users made 3+ visits.
The percentage of ED users who were disabled
increased progressively with ED utilization rates.
The percentage of patients enrolled in managed
care was relatively stable, except that it began to
decline with patients who had seven or more ED
visits. Levels of chronic illness were relatively high
among ED users (50.4 percent overall), with rates
increasing from 45.5 percent for patients with
a single visit to 84.5 percent for the ultra-high
users. The overall burden of disease or condition
acuity increased with ED use. Principal diagnoses
of substance use and mental illness accounted
for a relatively small share of ED visits. Findings
suggest that predictive modeling can identify
patients who will become frequent users in the
coming year at the time of their initial ED visit.
C. Boyd, C. Weiss, B. Leff, J. Wolff, A.
Hamblin, L. Martin. Faces of Medicaid:
Clarifying Multimorbidity Patterns
to Improve Targeting and Delivery
of Clinical Services for Medicaid
Populations. Center for Health
Care Strategies. December 2010.
Available at: http://www.chcs.org/
resource/faces-of-medicaid-clarifying-
multimorbidity-patterns-to-improve-
targeting-and-delivery-of-clinical-
services-for-medicaid-populations/.
Medicaid
beneficiaries with
disabilities
Identification/
Stratification
Examination of multimorbidity patterns and the
implications of specific patterns on hospitalization
and cost.
A number of specific conditions and combinations
of conditions are frequently associated with high
per capita costs and hospitalization rates. Mental
illness is nearly universal among the highest-
cost, most frequently hospitalized beneficiaries.
The presence of mental illness and/or drug and
alcohol disorders is associated with substantially
higher per capita costs and hospitalization rates.
S. Chakravarty, J. C. Cantor, J.
T. Walkup, and J. Tong. “Role of
Behavioral Health Conditions in
Avoidable Hospital Use and Cost.”
Rutgers Center for Health Policy,
e-pub, November 2014. Available
at: http://www.cshp.rutgers.edu/
Downloads/10530.pdf.
Super-utilizers Identification/
behavioral health
Using New Jersey uniform billing (UB) data, from
Camden, Trenton and Newark and 10 other low
income communities, from the Department of
Health (DOH), Rutgers Center for Health Policy
examined the role of behavioral health conditions
in potentially avoidable hospital use and costs
for “super utilizers.” This research with data
from 2008-2011, focuses on reducing avoidable
hospitalizations and costs, and the role of BH
conditions in preventable hospital utilization
patterns and associated costs.
Patients that are high users of hospital care and
those with avoidable inpatient hospital use are
more disproportionally affected by behavioral
health (BH) conditions. BH conditions were
disproportionate on billing records of inpatient
high users compared to inpatients who were not
high users (74.9% v. 32.3%). Among Medicaid
beneficiaries the difference was higher (80.8%
v. 25.1%). Total inpatient costs associated with
BH was $880.1 million, with ED costs at $73.1
million. Conclude that improved behavioral health
integration with medical services for complex
patients can result in lowed preventable hospital
use and cost savings.
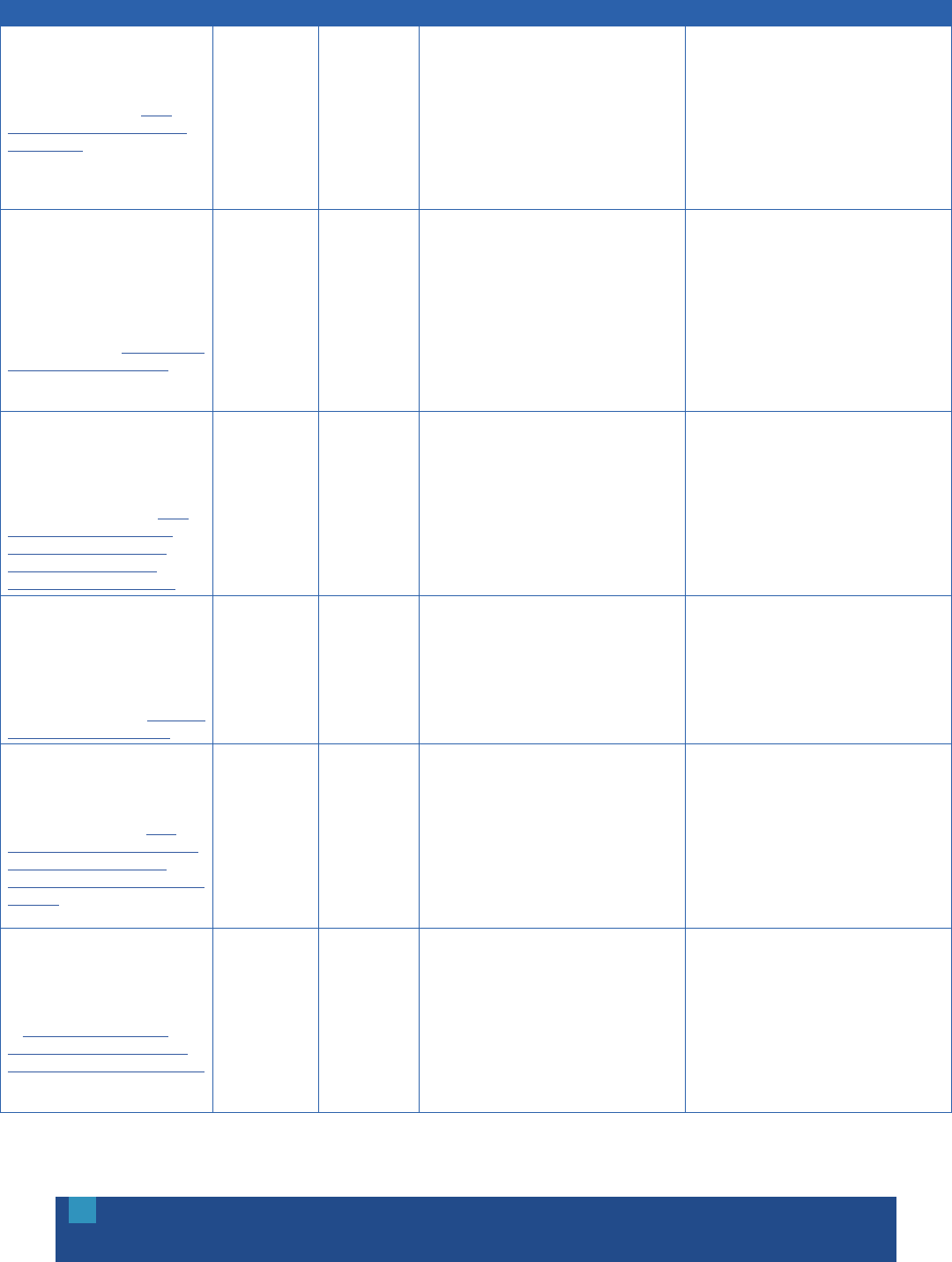
OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
27
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
J.A. Fleishman and J. Cohen “Using
Information on Clinical Conditions to
Predict High-Cost Patients” Health
Services Research. (2010) Apr; 45
(2): 532-552. Available at: http://
www.ncbi.nlm.nih.gov/pmc/articles/
PMC2838159/
High cost patients Predicting future
high users
The study used the Medical Expenditure Panel
Survey (MEPS) using cohorts initiated between
1996-1999 and validated between 2000-2003.
The MEPD interview collects socioeconomic
information and medical conditions on interview
participants. The study estimated regression model
from year 1 and compared the risk summary based
on the diagnostic cost group (DCG) to count chronic
conditions and indicators for the top 10 specific
highest chronic conditions.
The medical condition information greatly
improved prediction of high expenditures beyond
using gender, age, with the combination of
the DCG risk score in providing the greatest
improvements in prediction.
J.W. Frank, J.A. Linder, W.C. Becker,
D. Fiellin, and E. Wang. “Increased
Hospital and Emergency Department
Utilization by Individuals with Recent
Criminal Justice Involvement: Results of
a National Survey.” Journal of General
Internal Medicine, 29, no. 9 (2014):
1226-33. Available at: http://www.ncbi.
nlm.nih.gov/pubmed/24817280.
Adult participants
in the National
Survey on Drug
Use and Health,
with recent
criminal justice
involvement
Identification/
Stratification
Cross-sectional survey to examine hospital and
ED utilization and related costs by individuals with
recent criminal justice involvement.
Recent criminal justice involvement was associated
with both hospital and ED utilization among
vulnerable subgroups: uninsured, those with a
substance use disorder, and those reporting serious
psychological disorders. The findings of the potential
independent effect of criminal justice involvement on
hospital and ED utilization which may be explained
by disruptions in insurance coverage, access to
outpatient care and prescription medications, and
use of acute care services (EDs) for non-urgent or
preventable conditions.
T. Gilmer and A. Hamblin. Hospital
Readmissions among Medicaid
Beneficiaries with Disabilities:
Identifying Targets of Opportunity.
Center for Health Care Strategies.
December 2010. Available at: http://
www.chcs.org/resource/hospital-
readmissions-among-medicaid-
beneficiaries-with-disabilities-
identifying-targets-of-opportunity/.
Medicaid
beneficiaries with
disabilities
Identification/
Stratification
Analysis of Medicaid beneficiaries with disabilities
through a variety of lenses: by number and type
of chronic conditions; by state; and by whether
or not beneficiaries had a physician visit between
discharge and readmission.
The 30-day readmission rate for Medicaid
beneficiaries with disabilities was 16 percent,
rising to 53 percent within one year. Fifty percent
of those readmitted within 30 days did not visit
a physician between discharge and readmission.
The likelihood of readmission increased with the
number of chronic conditions.
Government Accountability Office.
(2014). “A Small Share of Enrollees
Consistently Accounted for a Large
Share of Expenditures.” (GAO
Publication No. GAO-15-460)
Washington, DC: US Government
Printing Office. Available at: http://www.
gao.gov/assets/680/670112.pdf.
Medicaid
beneficiaries
Identification/
stratification
Analysis of the characteristics among high-
expenditure beneficiaries for preventable/
avoidable ED use.
From 2009 through 2011, the most expensive
5 percent of Medicaid-only enrollees accounted
for almost half of the expenditures. The least
expensive 50 percent of Medicaid-only enrollees
accounted for less than 8 percent of the
expenditures for these enrollees. There was wide
variation on the distribution of Medicaid-only
enrollees’ expenditures (from 0 to 75 percent).
D. Hasselman. Super-Utilizer Summit:
Common Themes from Innovative
Complex Care Management Programs.
Center for Health Care Strategies.
October 2013. Available at: http://
www.chcs.org/resource/super-utilizer-
summit-common-themes-from-
innovative-complex-care-management-
programs/.
Super-utilizers Program
evaluation
Super-utilizer programs need ongoing support
from funders to evaluate and demonstrate the
impact of complex care management and to
build the evidence base of what works, for whom,
when, etc.
Demonstrating the impact of super-utilizer
programs takes significant time. It takes a
long time enroll a sufficient number of patients
into super-utilizer programs. Patients are not
only difficult to engage, but to keep engaged.
Changes to behavior and utilization do not happen
overnight. Utilization and costs often increase in
the beginning of the care management program
because the patient engages with the system and
finally gets the treatment he/she needs.
C.S. Hong, A.S. Hwang, and T.G. Ferris.
“Finding a Match: How Successful
Complex Care Programs Identify
Patients.” California HealthCare
Foundation. March 2015. Available
at: http://www.chcf.org/~/media/
MEDIA%20LIBRARY%20Files/PDF/F/
PDF%20FindingMatchComplexCare.pdf.
High-need, high-
cost patients
Identification/
Stratification
The two key aspects to patient identification are
(1) Predicting risk in specific patients along the
outcomes of interest, and (2) predicting care
sensitivity—the likelihood that a particular high-
risk patient will respond to the care management
intervention.
Successful complex care management programs
align the selected population, the planned
interventions, and the outcomes of interest by
performing the following three tasks: (1) Specify,
prioritize, and agree on the outcomes of interest
and the time frame for achieving them; (2)
Identify a sufficiently high-risk and care-sensitive
target population; and (3) Match the planned
staffing/resources and interventions to the target
population, building on existing services.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
28
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
A.S. Hwang, S.J. Atlas, P. Cronin,
J.M. Ashburner, S.J. Shah, W. He, et
al. “Appointment “No-Shows” Are an
Independent Predictor of Subsequent
Quality of Care and Resource Utilization
Outcomes.” Journal of General Internal
Medicine, e-pub, March 17, 2015.
Available at: http://www.ncbi.nlm.nih.
gov/pubmed/25776581.
Patients with a
high propensity
for appointment
“no-show”
Identification /
Stratification
No-show propensity factor (NSPF) was calculated
for patients using 5 years of outpatient
appointment data. Patients were then divided
into three NSPF risk groups and the association
between NSPF and clinical and acute care
utilization outcomes was evaluated.
NSPF appears to be an independent predictor
of suboptimal primary care outcomes and acute
care utilization. NSPF may play an important role
in helping health care systems identify high-risk
patients. Compared to patients in the low NSPF
group, patients in the high NSPF group were
significantly more likely to have incomplete
preventive cancer screening for colorectal,
cervical, or breast cancer; above-goal chronic
disease control measures for HbA1c and LDL;
and increased rates of acute care utilization for
hospitalization and emergency department visits.
Y. Jiang, A.P. Novais, S. Viner-Brown,
and M. Fine. “Non-emergent Hospital
Emergency Department Use and
Neighborhood Poverty in Rhode Island.”
Rhode Island Medical Journal, 97, no. 7
(2014): 47-51. Available at: http://www.
ncbi.nlm.nih.gov/pubmed/24983023.
Patients who
use ED for non-
emergent visits
Identification/
Stratification
Uses New York University ED classification
algorithm, Rhode Island ED database, and
American Community Survey (ACS) data, to
describe characteristics of patients in Rhode
Island who use ED for non-emergent visits
and examine whether ED non-emergent use is
associated with neighborhood poverty, how those
patients are distributed geographically, and how
the distribution is correlated with neighborhood
poverty status.
Data reveal that 1 of every 5 ED visits (20.3%)
in 2008-2012 was non-emergent. ED use for
non-emergent conditions was higher for patients’
ages 20-39 years of age, Hispanics, and non-
Hispanic blacks and females. Non-emergent
ED users were especially common among
self-pay patients or Medicaid beneficiaries.
Non-emergent ED visit percentages were
moderately correlated with neighborhood poverty
level. The highest percentages of ED visits for
non-emergent conditions were in four core-city
census tract codes. Profiling algorithm can identify
characteristics of non-emergent ED use. The
NYU algorithm provided an opportunity to study
the quality of ED care to improve health care
efficiency.
H.J. Jiang, M.L. Barrett, and M. Sheng.
“Characteristics of Hospital Stays for
Nonelderly Medicaid Super-Utilizers,
2012.” Healthcare Cost and Utilization
Project. November 2012. Available at:
http://www.hcup-us.ahrq.gov/reports/
statbriefs/sb184-Hospital-Stays-
Medicaid-Super-Utilizers-2012.jsp.
Medicaid super-
utilizers
Identification/
Stratification
Analysis of data from the Healthcare Cost
and Utilization Project 2012 State Inpatient
Databases (SID) shows patient demographics
and characteristics of hospital stays for Medicaid
super-utilizers. Patients were tracked across
hospital stays.
Medicaid super-utilizers had more hospital stay
(5.9 to 1.3) longer length stays were 6.1 to 4.5
higher hospital cost per stay 11,766 to 9,032.
Mental and behavioral health conditions were
the top diagnosis linked to hospital stays among
super-utilizers. Alcohol-related disorders followed.
Kaiser Family Foundation (2013).
“Medicaid: A Primer—Key Information
on the Nation’s Health Coverage
Program for Low-Income People.”
Available at: http://kff.org/medicaid/
issue-brief/medicaid-a-primer/.
Medicaid
beneficiaries
Identification/
Stratification
Analysis of Medicaid spending based on data from
the Medicaid Statistical Information System.
In FY 2011, Medicaid spending excluding
administration totaled about $414 billion. Roughly
two-thirds of Medicaid spending is attributable
to seniors and people with disabilities, and a
relatively small share of Medicaid beneficiaries
with very high costs account for more than half of
total spending. Dual eligible beneficiaries account
for nearly 40% of all Medicaid spending. In FY
2009, the 5% of beneficiaries with the highest
health and long-term care costs accounted for
54% of all Medicaid spending. The disabled
individuals among these high-cost beneficiaries
alone accounted for 30% of total Medicaid
expenditures.
R.G. Kronick, M. Bella, T.P. Gilmer. The
Faces of Medicaid III: Refining the
Portrait of People with Multiple Chronic
Conditions. Center for Health Care
Strategies. October 2009. Available
at: http://www.chcs.org/resource/
the-faces-of-medicaid-iii-refining-
the-portrait-of-people-with-multiple-
chronic-conditions/.
Medicaid
beneficiaries with
multiple chronic
conditions
Identification/
Stratification
Analysis of two Medicaid data sets—pharmacy
claims and five years of diagnostic data—to refine
what is known about Medicaid beneficiaries with
multiple chronic conditions.
The proportion of Medicaid beneficiaries with
disabilities diagnosed with three or more chronic
conditions increased from 35% to 45%. The
frequency of psychiatric illness among Medicaid
beneficiaries with disabilities increased from
29% to 49% versus solely looking at diagnostic
data. Costs for Medicaid-only beneficiaries with
three or more chronic conditions increased from
66% to 75% of total spending for beneficiaries
with disabilities.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
29
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
R.G. Kronick, M. Bella, T.P. Gilmer, and
S.A. Somers. The Faces of Medicaid II:
Recognizing the Care Needs of People
with Multiple Chronic Conditions.
Center for Health Care Strategies.
October 2007. Available at: http://
www.chcs.org/resource/the-faces-
of-medicaid-ii-recognizing-the-care-
needs-of-people-with-multiple-chronic-
conditions/.
Medicaid
beneficiaries with
multiple chronic
conditions
Identification/
Stratification
Analysis of patterns of multiple chronic conditions
among Medicaid beneficiaries.
Within the most expensive 1% of beneficiaries in
acute care spending, almost 83% had three or
more chronic conditions, and over 60% had five or
more chronic conditions. For Medicaid-only persons
with disability, each additional chronic condition is
associated, on average, with an increase in costs
of approximately $700/month, or approximately
$8,400 per year. The top most prevalent diagnostic
pairs of diseases among the highest cost 5%
of patients are: cardiovascular-pulmonary;
cardiovascular-gastrointestinal; cardiovascular-
central nervous system; central nervous system-
pulmonary, and pulmonary-gastrointestinal.
A. Lind. Measuring Quality for Complex
Medicaid Beneficiaries in New York.
Medicaid Institute, United Hospital
Fund. December 2011. Available at:
http://www.uhfnyc.org/publications/
880803?tr=y&auid=9958859.
Individuals with
multiple chronic
conditions,
behavioral health
conditions,
and long-term
care needs
Quality
Measurement
Most states and health care organizations leverage
existing measurement systems—whether HEDIS
or similar ones—to collect data on the care and
outcomes of individuals with complex conditions.
Disease-specific measurement (e.g., diabetes,
asthma) works for relatively healthy individuals
and those with a single chronic disease,
but it is inadequate for assessing care for
high-need, high-cost Medicaid beneficiaries.
Quality measures for high-risk populations
should be closely aligned with requirements
for care management organizations. Sharing
data at the provider level has multiple positive
effects—providers use information to improve
care for individual beneficiaries, and data-
sharing improved the overall collection of quality
measurement information. Underdeveloped sets of
measures for Medicaid beneficiaries with multiple
chronic conditions, behavioral health conditions,
and long-term care needs are moving forward at
a rapid pace.
A. Linden. “Assessing Regression to the
Mean Effects in Health Care Initiatives.”
BMC Medical Research Methodology,
13, no. 119 (2013). Available at:
http://www.biomedcentral.com/1471-
2288/13/119#refs.
High-need, high-
cost populations
Program
evaluation
Individuals at risk for high utilization in health care
may represent outlier values on utilization, cost,
or clinical measures. Typically, such individuals
participate in an intervention intended to reduce
their level of risk, and after a period of time,
a follow-up measurement is taken. However,
individuals initially identified by their outlier values
will likely have lower values on re-measurement
in the absence of an intervention. This statistical
phenomenon is known as “regression to the
mean” (RTM) and often leads to an inaccurate
conclusion that the intervention caused the effect.
Concerns about RTM are rarely raised in
connection with most health care interventions,
and it is uncommon to find evaluators who
estimate its effect. This may be due to lack of
awareness, cognitive biases that may cause
people to systematically misinterpret RTM effects
by creating (erroneous) explanations to account
for it, or by design.
A. Miller, M. Cunningham, and N. Ali.
“Bending the Cost Curve and Improving
Quality of Care in American’s Poorest
City.” Population Health Management,
16, Suppl. 1 (2013): S17-19. Available
at: http://online.liebertpub.com.ezproxy.
princeton.edu/doi/pdf/10.1089/
pop.2013.0038.
Super-utilizers Predictive
modeling
Camden Coalition’s data initiative is supported
primarily by a health information exchange, which
offers Camden city and regional health care
providers real-time access to patients’ important
medical information. This resource makes it
possible to perform accurate predictive analyses,
enabling better, more cost-effective care, reducing
unnecessary duplication and inefficiencies,
and fostering improved treatment coordination.
Innovative use of this data drives the patient
engagement cycle. An individual may graduate from
the Coalition’s intervention program in 30 to 90
days, but his or her progress is monitored for up to
1 year to confirm sustained improvement.
Used correctly, data can uncover system
deficiencies and inform disease-specific metrics
to identify high-utilizing patients. Once the patient
intervention is completed, data are an effective
means to continually monitor progress. Although
qualitative feedback from patients is valuable, the
numbers are critical to assess the population’s
health and identify gaps in the care delivery
system. In the long term, data make it possible to
track patient utilization and gauge improvement.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
30
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
NYU Center for Health and Public
Service Research. ED Utilization
Algorithm. NYU Wagner. Available at:
http://wagner.nyu.edu/faculty/billings/
nyued-background.
ED utilizers Identification/
Stratification
An algorithm developed to classify ED utilization,
based on an examination of a sample of almost
6,000 full ED records. Data abstracted from these
records included the initial complaint, presenting
symptoms, vital signs, medical history, age, gender,
diagnoses, procedures performed, and resources
used in the ED. Based on this information, each
case was classified into one of the following
categories: non-emergent; emergent/primary
care treatable; emergent—ED care needed—
preventable/avoidable; and emergent—ED care
needed—not preventable/avoidable.
Non-emergent—The patient’s initial complaint,
presenting symptoms, vital signs, medical history,
and age indicated that immediate medical care
was not required within 12 hours. Emergent/
Primary Care Treatable—Based on information
in the record, treatment was required within
12 hours, but care could have been provided
effectively and safely in a primary care setting.
Emergent—ED Care Needed—Preventable/
Avoidable—ED care was required based on the
complaint or procedures performed/resources
used, but the emergent nature of the condition
was potentially preventable/avoidable if timely
and effective ambulatory care had been received
during the episode of illness. Emergent—ED Care
Needed—Not Preventable/Avoidable—ED care
was required and ambulatory care treatment could
not have prevented the condition.
Partnership to Fight Chronic Disease
(2012). “Understanding and Addressing
“Hot Spots” Critical to Bending the
Medicaid Cost Curve.” Available at:
http://www.scribd.com/doc/95465593/
Understanding-and-Addressing-
Hot-Spots-Critical-to-Bending-the-
Medicaid-Cost-Curve.
Super-utilizers Identification/
Stratification
A small portion of Medicaid enrollees account
for a large share of spending. This concentration
presents opportunities for targeted, well-designed
interventions particularly when these high costs
persist over time with the same individuals.
Analyzing claims data for extreme uncoordinated
care provides a clear view of where there are ripe
opportunities for care coordination and targeted
care management services to bring down costs
and improve outcomes.
States need the technology that enables data
mining to identify and understand driving forces
behind the “hot spots” in their Medicaid programs,
to match effective interventions with the people
most likely to benefit based on predictive
modeling and to measure and track changes.
Risk stratification and predictive modeling target
interventions to identify the patients for whom
an intervention holds the greatest promise.
Supportive public policies enable states to deploy
health information technology, analytics predictive
modeling, and delivery system reforms that
both improve health for individuals affected and
manage costs for the system.
Pennsylvania Health Care Cost
Containment Council (2014).
“Pennsylvania’s “Super-Utilizers” of
Inpatient Hospital Care.” Available
at: http://www.phc4.org/reports/
researchbriefs/super-utilizers/2014/
docs/researchbrief_super-
utilizers_2014.pdf.
Super-utilizers Identification/
Stratification
Analysis of utilization and costs among super-
utilizers admitted to a Pennsylvania hospital five or
more times during FY 2014. Medicare payments
analyzed include fee-for-service patients only;
Medicaid payments include managed care and
fee-for-service patients (2012 data). The figures
represent general acute care discharges for adult
PA residents only, and do not include maternity
care, rehabilitation, or ED visits.
Super-utilizers represent 3% of hospitalized
patients; 11% of hospital admissions; and 14%
of hospital days. The average length of stay was
5.9 days for patients admitted five or more times,
compared to 4.4 days for patients admitted 1-2
times. Ten percent of Medicare admissions and
18% of Medicaid admissions were for super-
utilizers. $545 million (14%) of Medicare payments
for inpatient stays were for super-utilizers. $216
million (17%) of Medicaid payments for inpatient
stays were for super-utilizers.
J.A. Savageau, M. McLoughlin, A.
Ursan, Y. Bai, M. Collins, and S.B.
Cashman. “Characteristics of Frequent
Attenders At a Community Health
Center.” Journal of the American Board
of Family Medicine, 19, no. 3 (2006):
265-75. Available at: http://www.ncbi.
nlm.nih.gov/pubmed/16672680.
Frequent
attenders/
High-utilizers
Identification/
Stratification
Through medical record abstraction, retrospective
and longitudinal patient data were obtained for
a 30-month time period for 382 established
patients. Profile and comparison of frequent
attenders/high-utilizers of an urban community
health center in MA vs. non-high utilizers.
Older patients 45 to 64 years and Medicaid
recipients were more likely to be frequent
attenders. Patients residing furthest away from
the community health center were also the
most frequent of attenders as were those with
a diagnosis of diabetes or depression. Patients
who used the ED more had the highest number
of visits, although those patients who missed
more appointments as a proportion of the
number of scheduled appointments were less
likely to be frequent attenders.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
31
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
T.P. O’Toole, R. Pollini, P. Gray, T.
Jones, G. Bigelow, and D.E. Ford.
“Factors Identifying High-Frequency
and Low-Frequency Health Service
Utilization Among Substance-Using
Adults.” Journal of Substance Abuse
Treatment, 33, no. 1 (2007): 51-9.
Available at: http://www.ncbi.nlm.nih.
gov/pubmed/17588489.
Medically ill
substance-using
adults
Identification/
Stratification
A retrospective/prospective cohort study of 326
medically ill substance-using adults to identify
factors associated with 12-month high-frequency
utilization of ambulatory care, ED, and inpatient
medical care.
High-frequency ED use was independently
associated with being female, being African
American, being homeless, having a history of
substance abuse treatment, and a history of
ambulatory care visits. The combination of having
certain chronic conditions (seizure disorder,
hepatitis B, and hepatitis C) and accessing
ambulatory care was protective against high-
frequency use of ED. In contrast, high frequency
ambulatory care use was independently associated
with having insurance (Medicare/ Medicaid), having
HIV/AIDS, and receiving substance abuse treatment
during the study period.
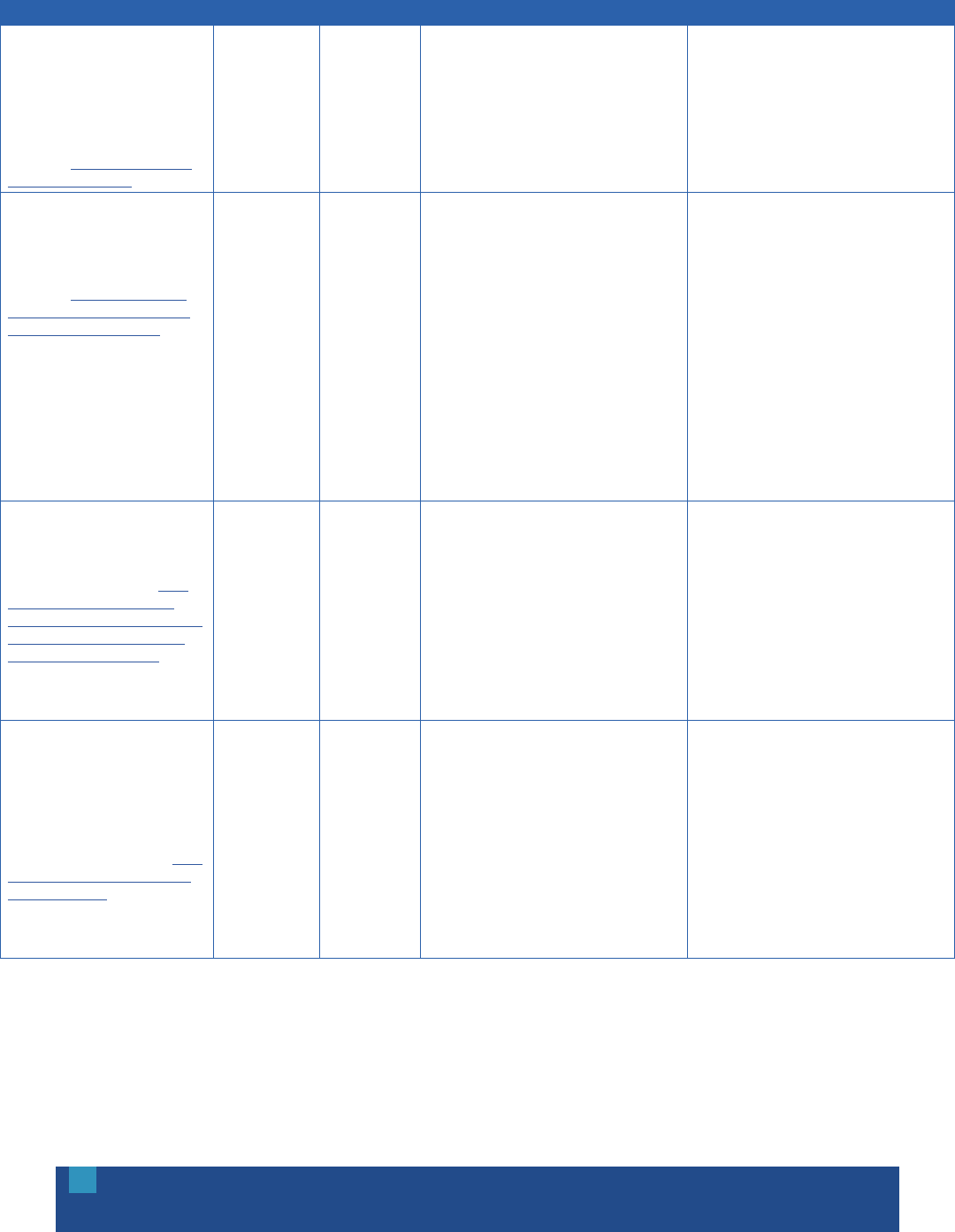
OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
32
APPENDIX D: WORKFORCE DEVELOPMENT
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
R. Adair, D.R. Wholey, J. Christianson,
K.M. White, H. Britt, and S. Lee.
“Improving Chronic Disease Care by
Adding Laypersons to the Primary
Care Team: A Parallel Randomized
Trial.” Annals of Internal Medicine,
159, no. 3 (2013): 176-84.
Available at: http://annals.org/article.
aspx?articleid=1722498.
Adults with
hypertension,
diabetes, or
heart failure
Lay health
workers
Randomized controlled trial to determine whether
patients with chronic disease working with lay
“care guides” would achieve more evidence-based
goals than those receiving usual care. Care guides
were 12 laypersons who received brief training
about these diseases and behavior change.
Patients with care guides achieved more goals
than usual care patients; reduced unmet goals
by 30.1% compared with 12.6% for usual care
patients; and improved more than usual care
patients in meeting several individual goals,
including not using tobacco. Estimated cost
was $286 per patient per year.
Association of American Medical
Colleges (2014). “Tips and Sample
Questions for Interviewing Patients Who
Have Been Hospitalized Three or More
Times in the Last Six to Nine Months.”
Available at: https://www.aamc.org/
initiatives/hotspotter/toolkit/356828/
patientinterviewquestions.html.
Super-utilizers Patient
engagement
Providers can behave in a manner and ask certain
questions to elicit a more positive, trusting, and
engaged response from patients at high risk for
hospital and ED use.
Sitting next to the patient at the bedside, making
eye contact, removing the white coat, introducing
oneself, and asking the patient if he or she would
mind if you ask a few questions to get to know
him or her better are good preliminary strategies.
If the patient does not want to talk to you, respect
his or her decision. Ask if the patient would like
you to come back if he or she is admitted to the
hospital again. If the patient is willing to talk, some
sample questions include: What are some of the
things you enjoy doing? Can you tell me about
some of your good and bad experiences with the
health care system? Do you have any problems
getting the care you need? It may take time to
draw out the patient. Work more on forming a
connection with the patient and getting to know
him or her, rather than following a rigid script.
L. Blash, S. Chapman, C. Dower. “The
Special Care Center—A Joint Venture
to Address Chronic Disease.” Center
for the Health Professions at UCSF.
November 2011. Available at: http://
www.iorahealth.com/wp-content/
uploads/2014/07/UCSF_The_Special_
Care_Center_A_Joint_Venture_to_
Address_Chronic_Disease.pdf.
Patients with
multiple chronic
illnesses
Complex care
management
The Atlantic City HEREIU Local 54 Health and
Welfare Fund and AtlantiCare Regional Medical
Center partnered to develop the “Special
Care Center” (SCC), a new clinic that provides
coordinated care management to patients with
multiple chronic illnesses. The center recruited
and trained a group of frontline health workers to
serve the functions of both health coaches and
medical assistants. The SCC developed a new job
category and wage scale within the AtlantiCare
system to recognize the challenging and vital work
of this group of Patient Care Assistants.
Costs escalated in the first 12-18 months, likely
due to an increase in care, but now numbers
for emergency visits and non-planned hospital
stays leveling off. Initial analysis suggested that
the model had the potential to produce first year
savings of up to 38% of net total spending for the
care of the highest-risk quintile of patients.
L.M. Cabral, H. Strother, K. Muhr, L.A.
Sefton, J.A. Savageau. “Clarifying
the Role of the Mental Health Peer
Specialist in Massachusetts, USA:
Insights from Peer Specialists,
Supervisors and Clients.” Health and
Social Care in the Community, 22, no.
1 (2013): 104-112. Available at: http://
onlinelibrary.wiley.com/doi/10.1111/
hsc.12072/abstract.
Individuals with
mental illness
Peer specialists Although the number of peer specialists in use
has been increasing, their role in care teams is
less defined than that of the community health
worker. Mental health peer specialists develop
peer-to-peer relationships of trust with clients to
improve their health and well-being, functioning in
ways similar to community health workers. Peer
specialists reported that the most important role
they play is to develop a relationship with another
peer based on mutuality, respect and hope. They
also educate others about recovery.
People receiving services overall had positive
experiences. Challenges included: lack of
expectations and role ambiguity. Supervisors had
difficulty providing supervision and evaluating
performance. More guidance from the state
mental health authority, as the entity that funds
the peer specialist training, may make for a
smoother implementation. The integration of
peer specialists into health teams could foster
collaboration. However, this would need to be
done in an environment where team members’
roles are clear and training on care team
participation has been provided.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
33
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
M. Chinman, P. George, R.H. Dougherty,
A.S. Daniels, S.S. Ghose, A. Swift, et al.
“Peer Support Services for Individuals
With Serious Mental Illnesses:
Assessing the Evidence.” Psychiatric
Services, 65, no. 4 (2014): 429-41.
Available at: http://ps.psychiatryonline.
org/doi/abs/10.1176/appi.
ps.201300244
People with a
serious mental
illness or co-
occurring mental
and substance
use disorders
Peer services Three service types for individuals with serious
mental illnesses or co-occurring mental and
substance use disorders: peers added to traditional
services, peers in existing clinical roles, and peers
delivering structured curricula.
Results were mixed. The effectiveness varied by
service area/ type. A majority of studies of two
service type peers added and peers delivering
curricula/education, showed some improvement
favoring peers. When compared with professional
staff, peers were better able to reduce inpatient
use and improve a range of recovery outcomes.
One study found a negative impact. The
effectiveness of peers in existing clinical roles
was mixed. Across the service types, the following
outcomes were observed: reduced inpatient
service use; improved relationship with providers;
better engagement with care; higher levels of
empowerment; higher levels of patient activation;
and higher levels of hopefulness for recovery.
M. Chinman, K. Henze, and P. Sweeney.
“Peer Specialist Toolkit: Implementing
Peer Support Services in VHA.”
VISN 1 New England MIRECC Peer
Education Center and VISN 4 MIRECC
Peer Resource Center. March 2013.
Available at: http://www.mirecc.va.gov/
visn4/peer_specialist_toolkit.asp.
Veterans
diagnosed with
serious mental
illness
Peer specialists Peer specialists are required in Veterans Health
Administration transformation. Peer Specialists
promote recovery by sharing their own recovery
stories, providing encouragement, instilling a
sense of hope, and teaching skills to Veterans.
Eight of 14 studies in non-VA clinical settings
showed some positive benefits of peer support,
such as less inpatient use and better treatment
engagement. Challenges related to peer support
include: role confusion, staff resistance, and
unequal treatment
B.G. Druss, L. Zhao, S.A. von Esenwein,
J.R. Bona, L. Fricks S. Jenkins-Tucker,
et al. “The Health and Recovery
Peer (HARP) Program: A Peer-Led
Intervention to Improve Medical
Self-Management for Persons with
Serious Mental Illness.” Schizophrenia
Research, 118 (2010): 264–270.
Available at: http://www.integration.
samhsa.gov/workforce/Druss_
HARP_2010.pdf.
People with SMI
and chronic
medical illness
Peer services New York’s Health and Recovery Program (HARP),
employs a manualized, six-session intervention,
delivered by mental health peer leaders, to help
participants become more effective managers of
their chronic illnesses.
This peer-led, medical self-management program
was feasible and showed promise for improving
a range of health outcomes among mental health
consumers with chronic medical comorbidities. The
HARP intervention may provide a vehicle for the
mental health peer workforce to actively engage
in efforts to reduce morbidity and mortality among
mental health consumers. At six month follow-up,
participants in the HARP program had a significantly
greater improvement in patient activation than
those in usual care, and in rates of having one or
more primary care visit. Intervention advantages
were observed for physical health related quality
of life, physical activity, and medication adherence.
Improvements in physical health related quality
of life were largest among medically and socially
vulnerable subpopulations.
E.B. Fisher, M.M. Coufal, H. Parada,
J.B. Robinette, P.Y. Tang, D.M. Urlaub,
et al. “Peer Support in Health Care and
Prevention: Cultural, Organizational,
and Dissemination Issues.” Annual
Review of Public Health, 35 (2014):
363-83. Available at: http://www.ncbi.
nlm.nih.gov/pubmed/24387085.
Many populations Peer support
services
Four key peer support functions include:
assistance in daily management, social and
emotional support, linkage to clinical care and
resources, and continual support.
Appreciable evidence is emerging for the
cost-effectiveness of peer support services
interventions in a variety of settings and types of
application. Peer support services that addresses
adherence, provide emotional support and
encouragement, and encourage appropriate
contact with providers has potential to produce
substantial cost savings. Peer support needs
to reflect its contexts—intended audience,
health problems, organizational and cultural
settings. Dissemination policies that lead to
flexible response to contexts, rather than overly
prescriptive guidelines, are critical.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
34
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
M. Hutchison and A. Hunt. Why Lay
Healthcare Workers in Care Delivery?
Care Copilot Institute. October
2014. Available at: http://www.
healthcarecopilot.com/wp-content/
uploads/2014/08/Article_Why-
Lay-Healthcare-Workers_white-
border_0100114.pdf.
Individuals living
with chronic
illness in its later
stages (LifeCourse
Project)
Lay health
workers
LHWs perform various functions for patients and
families while supporting traditional healthcare
roles and enhancing care. In one lay health worker
model, the LifeCourse Project, a care guide
works with the patient and their care providers
to strive toward a unified approach in gathering
information and discussing options for medical
and non-medical care.
Patients working with care guides in the
LifeCourse Project were 31% more likely to meet
evidence-based goals and 21% more likely to
quit tobacco use than usual care patients. Care
guide patients had fewer hospitalizations and
ED visits and reported significantly more positive
perceptions of their care. Recent research and
evaluation supports the value lay healthcare
workers provide in the way of quality outcomes
and patient engagement. However, these studies
are limited in number, scope, and quality, therefore
identifying a need for further research and
evaluation of lay healthcare worker programs and
models in order to clearly examine their full impact
on patient experience, outcomes, and cost of care.
G.S. Moran, Z. Russinova, V. Gidugu,
and C. Gagne. “Challenges Experienced
by Paid Peer Providers in Mental
Health Recovery: A Qualitative Study.”
Community Mental Health Journal,
49, no. 3 (2012): 281-91. Available
at: http://www.ncbi.nlm.nih.gov/
pubmed/23117937.
Individuals with
psychiatric
conditions
Peer providers Research in the last two decades has
demonstrated that peer providers have beneficial
impact on recipients of their services; less is
known about the challenges and outcomes of
those employed in peer roles, who have lived
experience of mental illnesses.
Themes related to the challenges faced by
mental health peer support providers include:
work environment, occupational path, and peer
providers’ mental health status. Challenges
in the work environment differed between
conventional mental health settings and
consumer-run agencies. Occupational domain
challenges included lack of clear job descriptions,
lack of skills for using one’s life story and lived
experience, lack of helping skills, and negative
aspects of carrying a peer provider label. Personal
mental health challenges included overwork
and symptom recurrence. Further investigation
into challenges related to work environment
are suggested, especially examining sources of
resilience in successful peer-run organizations.
National Center for Chronic Disease
Prevention and Health Promotion
Division for Heart Disease and Stroke
Prevention. Addressing Chronic Disease
Through Community Health Workers:
A Policy and Systems-Level Approach.
Centers for Disease Control and
Prevention. 2011. Available at: http://
stacks.cdc.gov/view/cdc/12052.
Individuals
with or at risk
of developing
chronic disease
Community
health workers
Seven core community health worker roles
include: cultural mediation; appropriate education;
ensuring connections to needed services; informal
counseling and social support; advocating;
providing direct services; and building capacity.
A variety of studies support community health
worker involvement with patients who have
hypertension and diabetes. Community health
workers can play an important role in facilitating
the prevention and control of chronic diseases
among a variety of populations, especially those
that have disparities in health.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
35
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
Substance Abuse and Mental Health
Services Administration (SAMHSA).
“Equipping Behavioral Health
Systems and Authorities to Promote
Peer Specialists/Peer Recovery
Coaching Services.” Expert Panel
Meeting Report, 3/21-22, 2012.
Available at: http://www.naadac.org/
assets/1959/samsha_2012_expert_
panel_meeting_report_-_equipping_
behavioral_health.pdf.
Individuals with
mental illnesses
and/or addictions
Peer support
providers
A peer is a person who has lived experience of
recovery from mental illness and/or addiction and
who wishes to provide peer support services to
others who are living with these disorders. Peers
motivate through hope and inspiration and support
many pathways to recovery. Peers function as an
advocate for the person in recovery, teaches the
person how to accomplish daily tasks, teaches
how to acquire needed resources, including
money; help the person find basic necessities;
use language based on common experiences; and
help the person find professional services from
lawyers, doctors, psychologists, financial advisers.
A growing body of evidence suggests that peer-
provided, recovery-oriented behavioral health
services produce outcomes as good as—and in
some cases superior to—services from non-peer
professionals. Programs likely to be successful
in implementing peer support/recovery coaching
have strong recovery values and principles that
guide their service delivery. Lack of an accepted
typology hinders research and evaluation of peer
services. The literature that does exist tends to be
descriptive and lacks experimental rigor. Lack of
training and lack of peer-focused supervision and
support can create confusion in the workplace
because the staff is unclear about the peer’s role
in the workplace. Among the major concerns for
peers are low—or no—pay and a lack of career
advancement opportunities. Misunderstanding and
discrimination continue to be key challenges to
integrating peers into the workforce. Suggestions
for the future: develop “how-to” manuals for
behavioral health programs to implement peer
support, and for States to develop, fund, and
monitor such programs.
M. Takach and R. Yalowich, National
Academy for State Health Policy.
Transforming the Workforce to Provide
Better Chronic Care: The Role of a
Community Health Nurse in a High-
Utilizer Program in Oregon. AARP
Public Policy Institute. January
2015. Available at: http://www.
nashp.org/sites/default/files/
NursingCareinOregon_Spotlight.pdf.
Medicaid super-
utilizers
Community
health nurses/
workers
Yamhill Community Care Organization’s (YCCO)
Community HUB program provides care to
individuals with chronic conditions with the goals
of reducing inappropriate emergency department
use and improving connections to primary care.
A community health nurse leads the program
and works with two community health workers to
achieve these aims. The nurse educates providers
and hospitals about the program, manages the
program, and identifies potential high-utilizer
patients through claims and referrals.
YCCO decreased emergency department
utilization from 77.7 percent in 2011 to 58.9
percent in 2013. Key recommendations based
on the program include: invest time in patient
engagement; keep the program flexible; regularly
engage outside input; use a combination of
data and referrals to identify patients; improve
opportunities for more immediate communication
with providers; and develop more resources for
patients with chronic pain.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
36
APPENDIX E: POLICY AND ADVOCACY
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
T. Bodenheimer, E. Chen, and H.D.
Bennett. “Confronting The Growing
Burden Of Chronic Disease: Can The
U.S. Health Care Workforce Do The
Job?” Health Affairs, 28, no. 1 (2009):
64-74. Available at: http://content.
healthaffairs.org/content/28/1/64.long.
Individuals with
chronic conditions
Delivery system
and payment
reform
The paper addresses four specific policy questions:
(1) Can dramatic public health prevention slow
down the rate of increase of chronic disease
prevalence? (2) Should chronic care be delivered
chiefly by specialist physicians, generalist
physicians, or multidisciplinary teams of health
personnel? (3) Is the future health care workforce
optimally positioned to provide the best care for
patients with chronic diseases? (4) Is fee-for-service
payment the best way to reimburse personnel who
care for patients with chronic conditions?
A larger interdisciplinary primary care workforce
is needed, and payment for primary care should
reward practices that incorporate multidisciplinary
teams. Multidisciplinary teams in primary care
can improve care, and at times lower costs,
for patients with chronic diseases. Many highly
prevalent chronic illnesses have risk factors
that can be mitigated by effective public health
measures, such as policies that reduce tobacco
use; cut consumption of unhealthy foods; and
increase physical activity. Payment reform should
move toward risk-adjusted per patient payment
with incentives for quality, services provided by
non-clinician team members, and population-
oriented panel management.
CMCS Informational Bulletin. “Targeting
Medicaid Super-Utilizers to Decrease
Costs and Improve Quality.” Center
for Medicaid and CHIP Services. July
24, 2013. Available at: http://www.
medicaid.gov/federal-policy-guidance/
downloads/CIB-07-24-2013.pdf.
Medicaid super-
utilizers
Medicaid policy Key policy questions for states related to super-
utilizer programs include: (1) whether to pursue
a super-utilizer program; (2) which payers are
involved; (3) who will provide the services and
the relationship to primary care; (4) what is the
targeting strategy; (5) what services are provided;
and (6) what is the funding strategy.
Medicaid can support states in building super-
utilizer programs in a number of ways, including:
enhanced federal match for design, development,
and implementation of MMIS; enhanced federal
match for health information exchanges;
administrative contracts; Medicaid health
homes; integrated care models; Targeted Case
Management services; and Medicare data access
and assistance.
D. Hasselman. Super-Utilizer Summit:
Common Themes from Innovative
Complex Care Management Programs.
Center for Health Care Strategies.
October 2013. Available at: http://
www.chcs.org/resource/super-utilizer-
summit-common-themes-from-
innovative-complex-care-management-
programs/.
Super-utilizers Policy and
advocacy
Targeting complex care management services
and supports to high-cost, complex patients is
an increasingly well-recognized best practice in
health care; however, this approach is still no
“slam dunk.”
Overcoming society’s cognitive bias that more
medical care, more expensive medical care, and
more high-tech medical care is better remains
challenging. The current U.S. health care system
is not designed to flexibly and creatively address
the complexity and uniqueness of each super-
utilizer, so taking super-utilizer programs to scale
within our health care system is also an unsolved
challenge. There is a need to shift the role of
hospitals from treating people who are sick to
keeping more people healthy. If the concept of
health expands from delivering medical care to
creating healthy populations and communities,
the concept of the health care team must also
expand. A linkage between traditional medicine
and population health must be forged.
E. Rich, D. Lipson, J. Libersky, and
M. Parchman. “Coordinating Care for
Adults With Complex Care Needs in
the Patient-Centered Medical Home:
Challenges and Solutions.” Agency
for Healthcare Research and Quality.
January 2012. Available at: http://
pcmh.ahrq.gov/page/coordinating-
care-adults-complex-care-needs-
patient-centered-medical-home-
challenges-and.
Individuals with
complex health
and social needs
Care
coordination
Essential elements of care coordination for
complex populations: conducting and regularly
updating a comprehensive needs assessment;
developing and updating an individualized care
plan; facilitating access to medical care and
home- and community-based services; and
regularly monitoring a patient’s health status,
needs and services, and communicating among
all service providers.
Policies and strategies that can support care
coordination for complex patients include: primary
care provider payment reforms that take into
account care coordination services; expansion of
organization’s clinical competence, through expert
consultation or hired staff with specific clinical
expertise; systematic quality improvement; and
extra resources to manage urgent concerns.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
37
Citation Target Population Key Focus Summary of Model/Intervention Key Findings/Outcomes
W. Warning, J. Wood, A. Letcher,
N. Srouji, C. Echterling, and C.
Carpenter. “Working with the Super
Utilizer Population: The Experience
and Recommendations of Five
Pennsylvania Programs.” Aligning
Forces for Quality, The Highmark
Foundation. 2014. Available at: http://
www.aligning4healthpa.org/pdf/
High_Utilizer_report.pdf.
Super-utilizers Policy Super-utilizer (SU) programs are data-driven, high-
intensity, community-based, patient-centered,
inter-disciplinary team that engages patients
to deliver high-quality, comprehensive care,
while encouraging self-advocacy and personal
accountability. The five programs in the South
Central Pennsylvania Super-Utilizer Collaborative
vary in terms of structures and processes, but
share the common goal of working with SU
patients to improve quality of care and quality of
life, and to reduce preventable utilization. Four of
the programs are based in health systems; one is
based in a neighborhood health center. Patients
may be engaged during a hospital admission, in
the ED, or in a primary care practice.
Policy recommendations related to supporting
SU programs include: Provide state support for
the development of health information exchanges
that deliver real-time, all-payer data to programs
on a daily basis, including utilization data from
all hospitals. (A crucial step would be to facilitate
access for super-utilizer programs to Medicaid
data including medical, behavioral and substance
abuse data from all sources.) Use alternative
payment mechanisms such as case management
fees, for SU programs. Provide access to: 1) real-
time utilization data for super-utilizer patients, and
2) current and historical charge, payment and cost
data for super-utilizer patients.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
38
ENDNOTES
1 For more information, visit: http://www.rwjf.org/en/about-rwjf/annual-reports/presidents-message-2014.html.
2 People with serious mental illness (SMI) have a high rate of physical comorbidities, as well as high associated
health care costs. M. De Hert, C.U. Correll, J. Bobes, M. Cetkovich-Bakmas, D. Cohen, I. Asai, et al. “Physical
Illness in Patients with Severe Mental Disorders: Prevalence, Impact of Medications and Disparities in Health
Care.” World Psychiatry, 10 (2011): 52-77.
3 U.S. National Library of Medicine. Medical Subject Heading (MeSH) Database. Available at: http://www.ncbi.nlm.
nih.gov/mesh.
4 J. Bell, D. Mancuso, T. Krupski, J.M. Joesch, D.C. Atkins, B. Court, et al. A Randomized Controlled Trial of
King County Care Partners’ Rethinking Care Intervention: Health and Social Outcomes up to Two Years Post-
Randomization Technical Report. Center for Health Care Strategies. November 2012. Available at: http://www.
chcs.org/resource/randomized-controlled-trial-of-king-county-care-partners-rethinking-care-intervention-health-
and-social-outcomes-up-to-two-years-post-randomization/.
5 J. Xing, C. Goehring, and D. Mancuso. “Care Coordination Program For Washington State Medicaid Enrollees
Reduced Inpatient Hospital Costs.” Health Affairs, 34, no. 4 (2015): 653-661. Available at: http://content.
healthaffairs.org/content/34/4/653.full.
6 K.W. Linkins, JJ. Brya, and D.W. Chandler. “Frequent Users of Health Services Initiative: Final Evaluation
Report.” California HealthCare Foundation. August 2008. Available at: http://www.chcf.org/~/media/MEDIA%20
LIBRARY%20Files/PDF/F/PDF%20FUHSIEvaluationReport.pdf.
7 L. Barlow. “Hospitals, Physicians Embrace Strategies To Reduce Cost of “Frequent Flyer” ER Visits” Real
World Health Care. April 2013. Available at: http://healthwellfoundation.org/sites/default/files/4.9.13.Hospitals.
Physicians%20Embrace%20Strategies%20to%20Reduce%20FF%20Visits%20to%20ER.pdf.
8 T. Bodenheimer. Strategies to Reduce Costs and Improve Care for High-Utilizing Medicaid Patients: Reflections
on Pioneering Programs. Center for Health Care Strategies. October 2013. Available at: http://www.chcs.org/
resource/strategies-to-reduce-costs-and-improve-care-for-high-utilizing-medicaid-patients-reflections-on-
pioneering-programs/.
9 T. Bodenheimer and R. Berry-Millett. “Care Management of Patients With Complex Health Needs.” Robert
Wood Johnson Foundation. December 2009. Available at: http://www.rwjf.org/content/dam/farm/reports/issue_
briefs/2009/rwjf49853/subassets/rwjf49853_1.
10 D. Hasselman. Super-Utilizer Summit: Common Themes from Innovative Complex Care Management Programs.
Center for Health Care Strategies. October 2013. Available at: http://www.chcs.org/resource/super-utilizer-
summit-common-themes-from-innovative-complex-care-management-programs/.
11 Xing, et al., op cit.
12 Ibid.
13 Bodenheimer (2013), op cit.
14 R.S. Brown, D. Peikes, G. Peterson, J. Schore, and C.M. Razafindrakoto. “Six Features Of Medicare Coordinated
Care Demonstration Programs That Cut Hospital Admissions Of High-Risk Patients.” Health Affairs, 31, no. 6
(2012): 1156-66. Available at: http://content.healthaffairs.org/content/31/6/1156.abstract.
15 California Quality Collaborative (2012). “Complex Care Management Toolkit.” Available at: http://www.calquality.
org/storage/documents/cqc_complexcaremanagement_toolkit_final.pdf.
16 C. Michalopoulos, M. Manno, S.E. Kim, and A. Warren. “The Colorado Regional Integrated Care Collaborative
Managing Health Care for Medicaid Recipients with Disabilities: Final Report on the Colorado Access Coordinated
Care Pilot Program.” MDRC, April 2013. Available at: http://www.mdrc.org/sites/default/files/Managing_Health_
Care_FR.pdf.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
39
17 P.Y. Takahashi, J.L. Pecina, B. Upatising, R. Chaudhry, N.D. Shah, H. Van Houten, et al. “A Randomized Controlled
Trial of Telemonitoring in Older Adults with Multiple Health Issues to Prevent Hospitalizations and Emergency
Department Visits.” Archive of Internal Medicine, 172, no. 10 (2012): 773-9. Available at: http://www.ncbi.nlm.nih.
gov/pubmed/22507696.
18 Ibid.
19 California Quality Collaborative, op cit.
20 Aligning Forces for Quality. “Creating Regional Partnerships to Improve Care Transitions.” The Robert Wood
Johnson Foundation. June 2014. Available at: http://forces4quality.org/node/7600.
21 Kim, et al., op cit.
22 Warning, et al., op cit.
23 Brown, et al., op cit.
24 Hasselman, op cit.
25 Bell, et al., op cit.
26 California Quality Collaborative, op cit.
27 Ibid.
28 A.S. Daniels, N. Adams, C. Carroll, and R. Beinecke. “A Conceptual Model for Behavioral Health and Primary Care
Integration: Emerging Challenges and Strategies for Improving International Mental Health Services.” International
Journal of Mental Health, 38, no. 1 (2009): 100–112. Available at: http://www.tandfonline.com/doi/abs/10.2753/
IMH0020-7411380109#.VR7NcvnF9Ac.
29 J.Y. Kim, T.C. Higgins, D. Esposito, A.M. Gerolamo, and M. Flick. “SMI Innovations Project in Pennsylvania:
Final Evaluation Report.” Mathematica Policy Research. October 2012. Available at: http://www.chcs.org/
resource/smi-innovations-project-in-pennsylvania-final-evaluation-report/.
30 Bell, et al., op cit.
31 C.S. Hong, A.L. Siegel, and T.G. Ferris. “Caring for High-Need, High-Cost Patients: What Makes for
a Successful Care Management Program?” The Commonwealth Fund. August 2014. Available at:
http://www.commonwealthfund.org/publications/issue-briefs/2014/aug/high-need-high-cost-patients.
32 M. Gerrity, E. Zoller, N. Pinson, C. Pettinari, and V. King. “Integrating Primary Care into Behavioral Health
Settings: What Works for Individuals with Serious Mental Illness.” Milbank Memorial Fund. 2014. Available at:
http://www.milbank.org/uploads/documents/papers/Integrating-Primary-Care-Report.pdf.
33 J.Y. Kim, T.C. Higgins, D. Esposito, A.M. Gerolamo, and M. Flick. “SMI Innovations Project in Pennsylvania: Final
Evaluation Report.” Mathematica Policy Research. October 2012. Available at: http://www.chcs.org/resource/smi-
innovations-project-in-pennsylvania-final-evaluation-report/.
34 Gerrity, et al., op cit.
35 Ibid.
36 R. Davis and A. Maul. Trauma-Informed Care: Opportunities for High-Need, High-Cost Medicaid Populations.
Center for Health Care Strategies. March 2015. Available at: http://www.chcs.org/resource/trauma-informed-care-
opportunities-high-need-high-cost-medicaid-populations/.
37 D.B. Mautner, H. Pang, J.C. Brenner, J.A. Shea, K.S. Gross, R. Frasso, et al. “Generating Hypotheses About Care
Needs of High Utilizers: Lessons from Patient Interviews.” Population Health Management, 16, Suppl. (2013):
S26-33. Available at: http://www.ncbi.nlm.nih.gov/pubmed/24070247.
38 B.G. Druss, L. Zhao, S.A. von Esenwein, J.R. Bona, L. Fricks, S. Jenkins-Tucker, et al. “The Health and Recovery
Peer (HARP) Program: A Peer-Led Intervention to Improve Medical Self-Management for Persons with Serious
Mental Illness.” Schizophrenia Research, 118 (2010): 264–270. Available at: http://www.integration.samhsa.gov/
workforce/Druss_HARP_2010.pdf.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
40
39 M. Chinman, P. George, R.H. Dougherty, A.S. Daniels, S.S. Ghose, A. Swift, et al. “Peer Support Services for
Individuals With Serious Mental Illnesses: Assessing the Evidence.” Psychiatric Services, 65, no. 4 (2014): 429-41.
40 J. Greene, J.H. Hibbard, R. Sacks, V. Overton, and C.D. Parrotta. “When Patient Activation Levels
Change, Health Outcomes And Costs Change, Too.” Health Affairs, 34, no. 3 (2015): 431-437.
Available at: http://content.healthaffairs.org/content/34/3/431.abstract.
41 J. Hibbard, J. Greene, Y. Shi, J. Mittler, and D. Scanlon. “Taking the Long View: How Well Do Patient
Activation Scores Predict Outcomes Four Years Later?” Medical Care Research and Review, Published
online, February 24, 2015: doi:10.1177/1077558715573871. Available at: http://mcr.sagepub.com/content/
early/2015/02/24/1077558715573871.abstract.
42 Hasselman, op cit.
43 Ibid.
44 Bodenheimer (2013), op cit.
45 Ibid.
46 Corporation for Supportive Housing. “Summary of Studies: Medicaid/Health Services Utilization and Costs.”
September 2009. Available at: http://pschousing.org/files/SH_cost-effectiveness_table.pdf.
47 L.S. Sadowski, R.A. Kee, T.J. VanderWeele, and D. Buchanan. “Effect of a Housing and Case Management
Program on Emergency Department Visits and Hospitalizations Among Chronically Ill Homeless Adults: A
Randomized Trial.” Journal of the American Medical Association, 301, no. 17 (2009): 1771-8. Available at: http://
www.ncbi.nlm.nih.gov/pubmed/19417194.
48 M. Evans. “Residential Therapy: Hospitals Take on Finding Housing for Homeless Patients, Hoping to Reduce
Readmissions, Lower Cost.” Modern Healthcare, September 2012. Available at: http://www.modernhealthcare.
com/article/20120922/MAGAZINE/309229988.
49 K.W. Linkins, JJ. Brya, D.W. Chandler. “Frequent Users of Health Services Initiative: Final Evaluation Report.”
California Healthcare Foundation. August 2008. Available at: http://www.chcf.org/~/media/MEDIA%20
LIBRARY%20Files/PDF/F/PDF%20FUHSIEvaluationReport.pdf.
50 Massachusetts Housing and Shelter Alliance (MHSA). “Home and Healthy for Good—Permanent Supportive
Housing: A Solution-Driven Model.” Progress Report, January 2014. Available at: https://givingcommon.guidestar.
org/ViewEdoc.aspx?eDocId=2698132&approved=True.
51 M. Evans, op cit.
52 L.C. Weinstein, M.D. LaNoue, J.D. Plumb, H. King, B. Stein and S. Tsemberis. “A Primary Care-Public Health
Partnership Addressing Homelessness, Serious Mental Illness, and Health Disparities.” Journal of the American
Board of Family Medicine, 26, no. 3 (2013): 279-87. Available at: http://www.ncbi.nlm.nih.gov/pubmed/23657696.
53 Connecticut Partnership for Strong Communities (2012). “Connecticut Integrated Healthcare & Housing
Neighborhoods.” Available at: http://pschousing.org/files/Connecticut%20Integrated%20Healthcare%20and%20
Housing%20Neigborhoods%20Summary%20%28March%202012%29.pdf.
54 Bodenheimer and Berry, op cit.
55 Xing, et al., op cit.
56 Bell, et al., op cit.
57 Kim, et al., op cit.
58 Mautner, et al., op cit.
59 Bell, et al., op cit.
60 Sadowski, et al., op cit.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
41
61 D. Bachrach, S. Anthony, and A. Detty. “State Strategies for Integrating Physical and Behavioral Health
Services in a Changing Medicaid Environment.” The Commonwealth Fund. August 2014. Available at:
http://www.commonwealthfund.org/publications/fund-reports/2014/aug/state-strategies-behavioral-health.
62 Ibid.
63 Ibid.
64 A. Hamblin, J. Verdier, and M. Au. State Options for Integrating Physical and Behavioral Health Care. Center for
Health Care Strategies. October 2011. Available at: http://www.chcs.org/resource/state-options-for-integrating-
physical-and-behavioral-health-care/.
65 Evans, op cit.
66 S.F. Sandberg, C. Erikson, R. Owen, K.D. Vickery, S.T. Shimotsu, M. Linzer, et al. “Hennepin Health: A Safety-Net
Accountable Care Organization For The Expanded Medicaid Population.” Health Affairs, 33, no. 11 (2014):
1975-84. Available at: http://content.healthaffairs.org/content/33/11/1975.abstract.
67 M. Crawford and R. Houston. State Payment and Financing Models to Promote Health and Social Service
Integration. Center for Health Care Strategies. February 2015. Available at: http://www.chcs.org/resource/
state-payment-financing-models-promote-health-social-service-integration/.
68 R. Mahadevan and R. Houston. Supporting Social Service Delivery through Medicaid Accountable Care
Organizations: Early State Efforts. Center for Health Care Strategies. February 2015. Available at:
http://www.chcs.org/resource/supporting-social-services-medicaid-accountable-care-organizations-early-efforts/.
69 Ibid.
70 J. Corrigan and E. Fisher. “Accountable Health Communities: Insights from State Health Reform Initiatives.”
The Dartmouth Institute for Health Policy & Clinical Practice, November 2014. Available at:
http://tdi.dartmouth.edu/images/uploads/AccountHealthComm-WhPaperFinal.pdf.
71 Ibid.
72 Sandberg, op cit.
73 Crawford and Houston, op cit.
74 Ibid.
75 Sandberg, et al., op cit.
76 B.P. Zeigler, S.A. Redding, B.A. Leath, and E.L. Carter. “Pathways Community HUB: A Model for Coordination
of Community Health Care.” Population Health Management, 17, no. 4 (2014): 199-201. Available at: http://online.
liebertpub.com/doi/abs/10.1089/pop.2014.0041.
77 J. Alper and A. Baciu. “Roundtable on Population Health Improvement: Financing Population Health
Improvement.” Institute of Medicine, 2014. Available at: http://iom.nationalacademies.org/Reports/2014/
Financing-Population-Health-Improvement.aspx.
78 E.H. Bradley, B.R. Elkins, J. Herrin, and B. Elbel. “Health and Social Services Expenditures: Associations with
Health Outcomes.” BMJ Quality and Safety, 20, no. 10 (2011): 826-31.
79 M. Crawford, T. McGinnis, J. Auerbach, and K. Golden. “Population Health in Medicaid Delivery System Reforms.”
Milbank Memorial Fund. March 2015. Available at: http://www.milbank.org/uploads/documents/papers/CHCS_
PopulationHealth_IssueBrief.pdf.
80 Bachrach, et al., op cit.
81 Ibid.
82 S.L. Hayes, M.K. Mann, F.M. Morgan, M.J. Kelly, and A.L. Weightman. “Collaboration Between Local Health and
Local Government Agencies for Health Improvement.” Cochrane Database of Systematic Reviews, October 2012.
Available at: http://www.ncbi.nlm.nih.gov/pubmed/23076937.
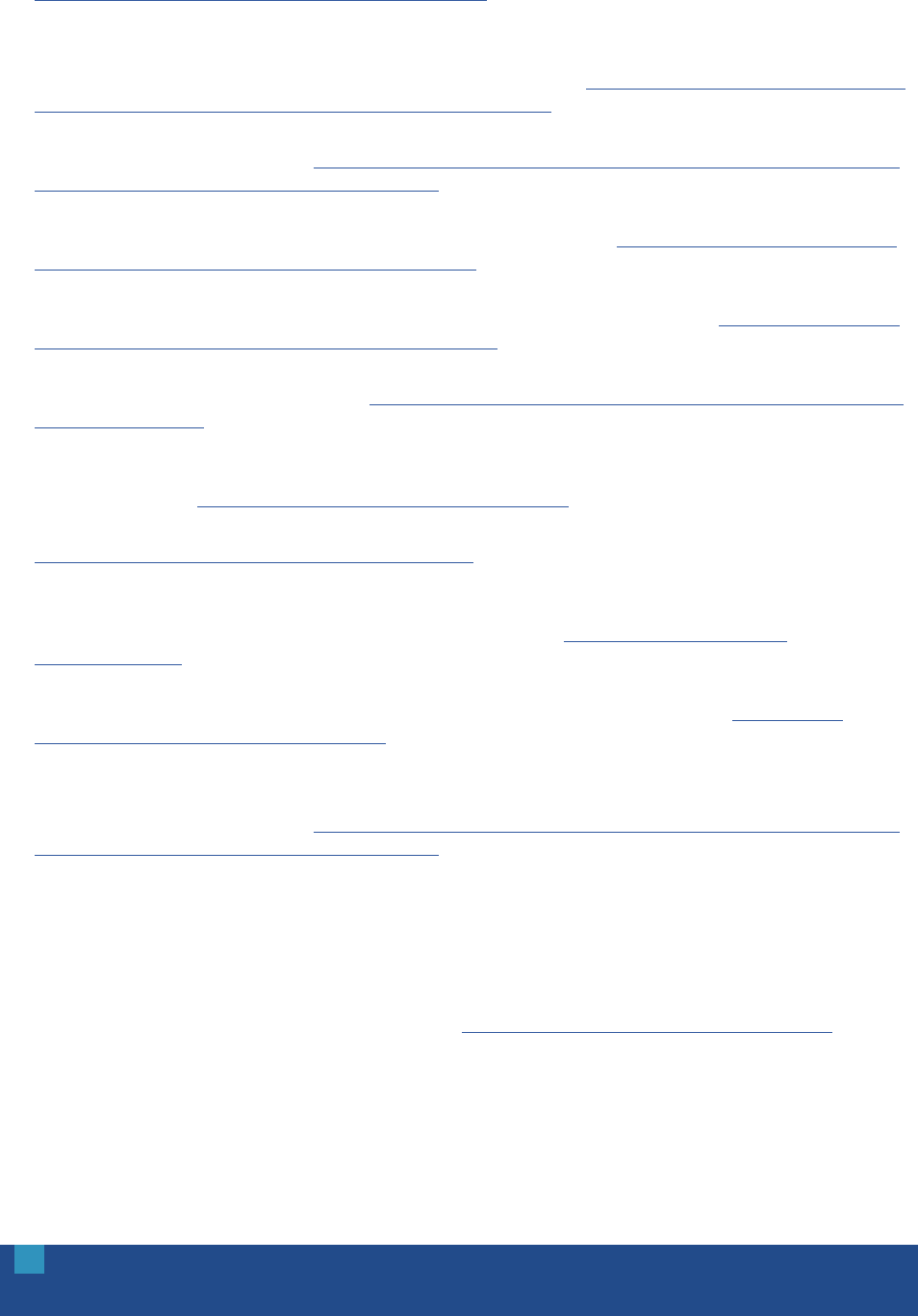
OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
42
83 D.W. Bates, S. Saria, L. Ohno-Machado, A. Shah, and G. Escobar. “Big Data in Health Care: Using Analytics to
Identify and Manage High-Risk and High-Cost Patients.” Health Affairs, 33, no. 7 (2014): 1123-31. Available at:
http://content.healthaffairs.org/content/33/7/1123.abstract.
84 Hong, et al. (2014), op cit.
85 C.S. Hong, A.S. Hwang, and T.G. Ferris. “Finding a Match: How Successful Complex Care Programs Identify
Patients.” California Health Care Foundation. March 2015. Available at: http://www.chcf.org/~/media/MEDIA%20
LIBRARY%20Files/PDF/F/PDF%20FindingMatchComplexCare.pdf.
86 Partnership to Fight Chronic Disease (2012). “Understanding and Addressing “Hot Spots” Critical to Bending the
Medicaid Cost Curve.” Available at: http://www.scribd.com/doc/95465593/Understanding-and-Addressing-Hot-
Spots-Critical-to-Bending-the-Medicaid-Cost-Curve.
87 S.R. Green, V. Singh, and W. O’Byrne. “Hope for New Jersey’s City Hospitals: The Camden Initiative.”
Perspectives in Health Information Management, Spring 2010. Available at: http://search.proquest.com.ezproxy.
princeton.edu/docview/213202979?pq-origsite=summon.
88 A. Miller, M. Cunningham, and N. Ali. “Bending the Cost Curve and Improving Quality of Care in American’s
Poorest City.” Population Health Management, 16, Suppl. 1 (2013): S17-19. Available at: http://online.liebertpub.
com.ezproxy.princeton.edu/doi/pdf/10.1089/pop.2013.0038.
89 D. Knutson, M. Bella, K. Llanos. Predictive Modeling: A Guide for State Medicaid Purchasers. Center for Health
Care Strategies. August 2009. Available at: http://www.chcs.org/resource/predictive-modeling-a-guide-for-state-
medicaid-purchasers/.
90 J.A. Savageau, M. McLoughlin, A. Ursan, Y. Bai, M. Collins, and S.B. Cashman. “Characteristics of Frequent
Attenders at a Community Health Center.” Journal of the American Board of Family Medicine, 19, no. 3 (2006):
265-75. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16672680.
91 NYU Center for Health and Public Service Research. ED Utilization Algorithm. NYU Wagner. Available at:
http://wagner.nyu.edu/faculty/billings/nyued-background.
92 J.W. Frank, J.A. Linder, W.C. Becker, D. Fiellin, and E. Wang. “Increased Hospital and Emergency Department
Utilization by Individuals with Recent Criminal Justice Involvement: Results of a National Survey.” Journal
of General Internal Medicine, 29, no. 9 (2014): 1226-33. Available at: http://www.ncbi.nlm.nih.gov/
pubmed/24817280.
93 J. Billings and M.C. Raven. “Dispelling An Urban Legend: Frequent Emergency Department Users Have
Substantial Burden Of Disease.” Health Affairs, 32, no. 12 (2013): 2099-2108. Available at: http://content.
healthaffairs.org/content/32/12/2099.abstract.
94 Knutson, et al., op cit.
95 Partnership to Fight Chronic Disease (2012). “Understanding and Addressing “Hot Spots” Critical to Bending the
Medicaid Cost Curve.” Available at: http://www.scribd.com/doc/95465593/Understanding-and-Addressing-Hot-
Spots-Critical-to-Bending-the-Medicaid-Cost-Curve.
96 Hong, et al. (2015), op cit.
97 Xing, et al., op cit.
98 Miller, et al., op cit.
99 A.S. Hwang, S.J. Atlas, P. Cronin, J.M. Ashburner, S.J. Shah, W. He, et al. “Appointment “No-Shows” Are an
Independent Predictor of Subsequent Quality of Care and Resource Utilization Outcomes.” Journal of General
Internal Medicine, e-pub, March 17, 2015. Available at: http://www.ncbi.nlm.nih.gov/pubmed/25776581.
100 Frank, et al., op cit.
101 Savageau, et al., op cit.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
43
102 T.P. O’Toole, R. Pollini, P. Gray, T. Jones, G. Bigelow, and D.E. Ford. “Factors Identifying High-Frequency and
Low-Frequency Health Service Utilization Among Substance-Using Adults.” Journal of Substance Abuse
Treatment, 33, no. 1 (2007): 51-9. Available at: http://www.ncbi.nlm.nih.gov/pubmed/17588489.
103 NYU Center for Health and Public Service Research, ED Utilization Algorithm, op cit.
104 Y. Jiang, A.P. Novais, S. Viner-Brown, and M. Fine. “Non-emergent Hospital Emergency Department Use and
Neighborhood Poverty in Rhode Island.” Rhode Island Medical Journal, 97, no. 7 (2014): 47-51. Available at:
http://www.ncbi.nlm.nih.gov/pubmed/24983023.
105 Hong, et al. (2015), op cit.
106 Ibid.
107 Ibid.
108 Kaiser Family Foundation, op cit.
109 H.J. Jiang, M.L. Barrett, and M. Sheng. “Characteristics of Hospital Stays for Nonelderly Medicaid Super-Utilizers,
2012.” Healthcare Cost and Utilization Project. November 2012. Available at: http://www.hcup-us.ahrq.gov/
reports/statbriefs/sb184-Hospital-Stays-Medicaid-Super-Utilizers-2012.jsp.
110 Government Accountability Office. (2014). “A Small Share of Enrollees Consistently Accounted for a Large Share
of Expenditures.” (GAO Publication No. GAO-15-460) Washington, DC: US Government Printing Office. Available
at: http://www.gao.gov/assets/680/670112.pdf.
111 S. Chakravarty, J. C. Cantor, J. T. Walkup, and J. Tong. “Role of Behavioral Health Conditions in Avoidable
Hospital Use and Cost.” Rutgers Center for Health Policy, e-pub, November 2014. Available at: http://www.cshp.
rutgers.edu/Downloads/10530.pdf.
112 Pennsylvania Health Care Cost Containment Council (2014). “Pennsylvania’s “Super-Utilizers” of Inpatient
Hospital Care.” Available at: http://www.phc4.org/reports/researchbriefs/super-utilizers/2014/docs/researchbrief_
super-utilizers_2014.pdf.
113 R.G. Kronick, M. Bella, and T.P. Gilmer. The Faces of Medicaid III: Refining the Portrait of People with Multiple
Chronic Conditions. Center for Health Care Strategies. October 2009. Available at: http://www.chcs.org/resource/
the-faces-of-medicaid-iii-refining-the-portrait-of-people-with-multiple-chronic-conditions/.
114 R.G. Kronick, M. Bella, T.P. Gilmer, and S.A. Somers. The Faces of Medicaid II: Recognizing the Care Needs
of People with Multiple Chronic Conditions. Center for Health Care Strategies. October 2007. Available at:
http://www.chcs.org/resource/the-faces-of-medicaid-ii-recognizing-the-care-needs-of-people-with-multiple-
chronic-conditions/.
115 C. Boyd, C. Weiss, B. Leff, J. Wolff, A. Hamblin, and L. Martin. Faces of Medicaid: Clarifying Multimorbidity
Patterns to Improve Targeting and Delivery of Clinical Services for Medicaid Populations. Center for Health
Care Strategies. December 2010. Available at: http://www.chcs.org/resource/faces-of-medicaid-clarifying-
multimorbidity-patterns-to-improve-targeting-and-delivery-of-clinical-services-for-medicaid-populations/.
116 T. Gilmer and A. Hamblin. Hospital Readmissions among Medicaid Beneficiaries with Disabilities: Identifying
Targets of Opportunity. Center for Health Care Strategies. December 2010. Available at: http://www.chcs.
org/resource/hospital-readmissions-among-medicaid-beneficiaries-with-disabilities-identifying-targets-of-
opportunity/.
117 R.G. Kronick, et al. (2007), op cit.
118 C. Boyd, et al., op cit.
119 Pennsylvania Health Care Cost Containment Council, op cit.
120 Hong, et al. (2015), op cit.
121 Ibid.
122 Hasselman, op cit.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
44
123 A. Linden. “Assessing Regression to the Mean Effects in Health Care Initiatives.” BMC Medical Research
Methodology, 13, no. 119 (2013). Available at: http://www.biomedcentral.com/1471-2288/13/119#refs.
124 Ibid.
125 National Center for Chronic Disease Prevention and Health Promotion Division for Heart Disease and Stroke
Prevention. Addressing Chronic Disease Through Community Health Workers: A Policy and Systems-Level
Approach. Centers for Disease Control and Prevention. 2011. Available at: http://stacks.cdc.gov/view/cdc/12052.
126 S. Kangovi, N. Mitra, D. Grande, M. White, S. McCollum, J. Sellman, R. Shannon, and J.A. Long. “Patient
Centered Community Health Worker Intervention to Improve Post-Hospital Outcomes: A Randomized
Clinical Trial.” JAMA Internal Medicine, 174, no. 4 (2014): 535-43. Available at: http://www.ncbi.nlm.nih.gov/
pubmed/24515422.
127 A.C. Davis. “Leveraging Community Health Workers within California’s State Innovation Model: Background,
Options and Considerations.” California Health and Human Services Agency. July 2013. Available at: http://www.
chhs.ca.gov/Documents/Issue%20Brief%20on%20Leveraging%20Community%20Health%20Workers%20
Under%20California%27s%20State%20Innovation%20Model%20%28SIM%29%20Initiative.pdf.
128 Substance Abuse and Mental Health Services Administration (SAMHSA). “Equipping Behavioral Health Systems
and Authorities to Promote Peer Specialists/Peer Recovery Coaching Services.” Expert Panel Meeting Report,
3/21-22, 2012. Available at: http://www.naadac.org/assets/1959/samsha_2012_expert_panel_meeting_report_-_
equipping_behavioral_health.pdf.
129 L.M. Cabral, H. Strother, K. Muhr, L.A. Sefton, J.A. Savageau. “Clarifying the Role of the Mental Health Peer
Specialist in Massachusetts, USA: Insights from Peer Specialists, Supervisors and Clients.” Health and Social
Care in the Community, 22, no. 1 (2013): 104-112. Available at: http://onlinelibrary.wiley.com/doi/10.1111/
hsc.12072/abstract.
130 Ibid.
131 Ibid.
132 SAMHSA, op cit.
133 E.B. Fisher, M.M. Coufal, H. Parada, J.B. Robinette, P.Y. Tang, D.M. Urlaub, et al. “Peer Support in Health Care
and Prevention: Cultural, Organizational, and Dissemination Issues.” Annual Review of Public Health, 35 (2014):
363-83. Available at: http://www.ncbi.nlm.nih.gov/pubmed/24387085.
134 Kangovi, et al. op cit.
135 R. Adair, D.R. Wholey, J. Christianson, K.M. White, H. Britt, and S. Lee. “Improving Chronic Disease Care by
Adding Laypersons to the Primary Care Team: A Parallel Randomized Trial.” Annals of Internal Medicine, 159,
no. 3 (2013): 176-84. Available at: http://annals.org/article.aspx?articleid=1722498.
136 Ibid.
137 M. Takach and R. Yalowich, National Academy for State Health Policy. “Transforming the Workforce to Provide
Better Chronic Care: The Role of a Community Health Nurse in a High-Utilizer Program in Oregon.” AARP Public
Policy Institute. January 2015. Available at: http://www.nashp.org/sites/default/files/NursingCareinOregon_
Spotlight.pdf.
138 SAMHSA, op cit.
139 Fisher, et al., op cit.
140 B.G. Druss, L. Zhao, S.A. von Esenwein, J.R. Bona, L. Fricks S. Jenkins-Tucker, et al. “The Health and Recovery
Peer (HARP) Program: A Peer-Led Intervention to Improve Medical Self-Management for Persons with Serious
Mental Illness.” Schizophrenia Research, 118 (2010): 264–270. Available at: http://www.integration.samhsa.gov/
workforce/Druss_HARP_2010.pdf.
141 Ibid.
OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
45
142 M. Chinman, P. George, R.H. Dougherty, A.S. Daniels, S.S. Ghose, A. Swift, and M.E. Delphin-Rittmon. “Peer
Support Services for Individuals with Serious Mental Illnesses: Assessing the Evidence.” Psychiatric Services, 65,
no. 4 (2014): 429-41.
143 Ibid.
144 M. Chinman, K. Henze, and P. Sweeney. “Peer Specialist Toolkit: Implementing Peer Support Services in VHA.”
VISN 1 New England MIRECC Peer Education Center and VISN 4 MIRECC Peer Resource Center. March 2013.
Available at: http://www.mirecc.va.gov/visn4/peer_specialist_toolkit.asp.
145 C.J. Peek, M.A. Baird, and E. Coleman. “Primary Care for Patient Complexity, Not Only Disease.” Family, Systems
and Health, 27, no. 4 (2009): 287-302. Available at: http://www.ncbi.nlm.nih.gov/pubmed/20047353.
146 Association of American Medical Colleges (2014). “Tips and Sample Questions for Interviewing Patients Who
Have Been Hospitalized Three or More Times in the Last Six to Nine Months.” Available at: https://www.aamc.org/
initiatives/hotspotter/toolkit/356828/patientinterviewquestions.html.
147 Cabral, et al., op cit.
148 SAMHSA, op cit.
149 G.S. Moran, Z. Russinova, V. Gidugu, and C. Gagne. “Challenges Experienced by Paid Peer Providers in Mental
Health Recovery: A Qualitative Study.” Community Mental Health Journal, 49, no. 3 (2012): 281-91. Available at:
http://www.ncbi.nlm.nih.gov/pubmed/23117937.
150 Cabral, et al., op cit.
151 SAMHSA, op cit.
152 Moran, et al., op cit.
153 Ibid.
154 SAMHSA, op cit.
155 Davis, op cit.
156 M. Hutchison and A. Hunt. “Why Lay Healthcare Workers in Care Delivery?” Care Copilot Institute. October
2014. Available at: http://www.healthcarecopilot.com/wp-content/uploads/2014/08/Article_Why-Lay-Healthcare-
Workers_white-border_0100114.pdf.
157 SAMHSA, op cit.
158 Chinman, et al. (2014), op cit.
159 Moran, et al., op cit.
160 SAMHSA, op cit.
161 Davis, op cit.
162 U. Emeche. “Is a Strategy Focused on Super-Utilizers Equal to the Task of Health Care System Transformation?
Yes.” Annals of Family Medicine, 13, no.1 (2015): 6-7. Available at: http://annfammed.org/content/13/1/6.full.
163 E. Rich, D. Lipson, J. Libersky, and M. Parchman. “Coordinating Care for Adults With Complex Care Needs in
the Patient-Centered Medical Home: Challenges and Solutions.” Agency for Healthcare Research and Quality.
January 2012. Available at: http://pcmh.ahrq.gov/page/coordinating-care-adults-complex-care-needs-patient-
centered-medical-home-challenges-and.
164 T. Bodenheimer, E. Chen, and H.D. Bennett. “Confronting The Growing Burden Of Chronic Disease: Can The
U.S. Health Care Workforce Do The Job?” Health Affairs, 28, no. 1 (2009): 64-74. Available at: http://content.
healthaffairs.org/content/28/1/64.long.
165 Ibid.

OPPORTUNITIES TO IMPROVE MODELS OF CARE FOR PEOPLE WITH COMPLEX NEEDS: LITERATURE REVIEW
46
166 W. Warning, J. Wood, A. Letcher, N. Srouji, C. Echterling, and C. Carpenter. “Working with the Super Utilizer
Population: The Experience and Recommendations of Five Pennsylvania Programs.” Aligning Forces for Quality,
The Highmark Foundation. 2014. Available at: http://www.aligning4healthpa.org/pdf/High_Utilizer_report.pdf.
167 CMCS Informational Bulletin. “Targeting Medicaid Super-Utilizers to Decrease Costs and Improve Quality.” Center
for Medicaid and CHIP Services. July 24, 2013. Available at: http://www.medicaid.gov/federal-policy-guidance/
downloads/CIB-07-24-2013.pdf.
168 Warning, et al., op cit.
169 CMCS, op cit.
170 Emeche, op cit.
171 Bodenheimer, et al. (2009), op cit.
172 Ibid.
