Client Initial
Date
DEPARTMENT OF HEALTH SERVICES
Division of Care and Treatment Services
F-24277 (05/2024)
STATE OF WISCONSIN
42 CFR483.420(a)(2)
DHS 134.31(3)(o)
DHS 94.03 & 94.09
§§ 51.61(1)(g) & (h)
INFORMED CONSENT FOR MEDICATION
Dosage and / or Side Effect information last revised on 11/13/2017
Completion of this form is voluntary. If informed consent is not given, the medication cannot be administered without a court order unless in
an emergency.
This consent is maintained in the client’s record and is accessible to authorized users.
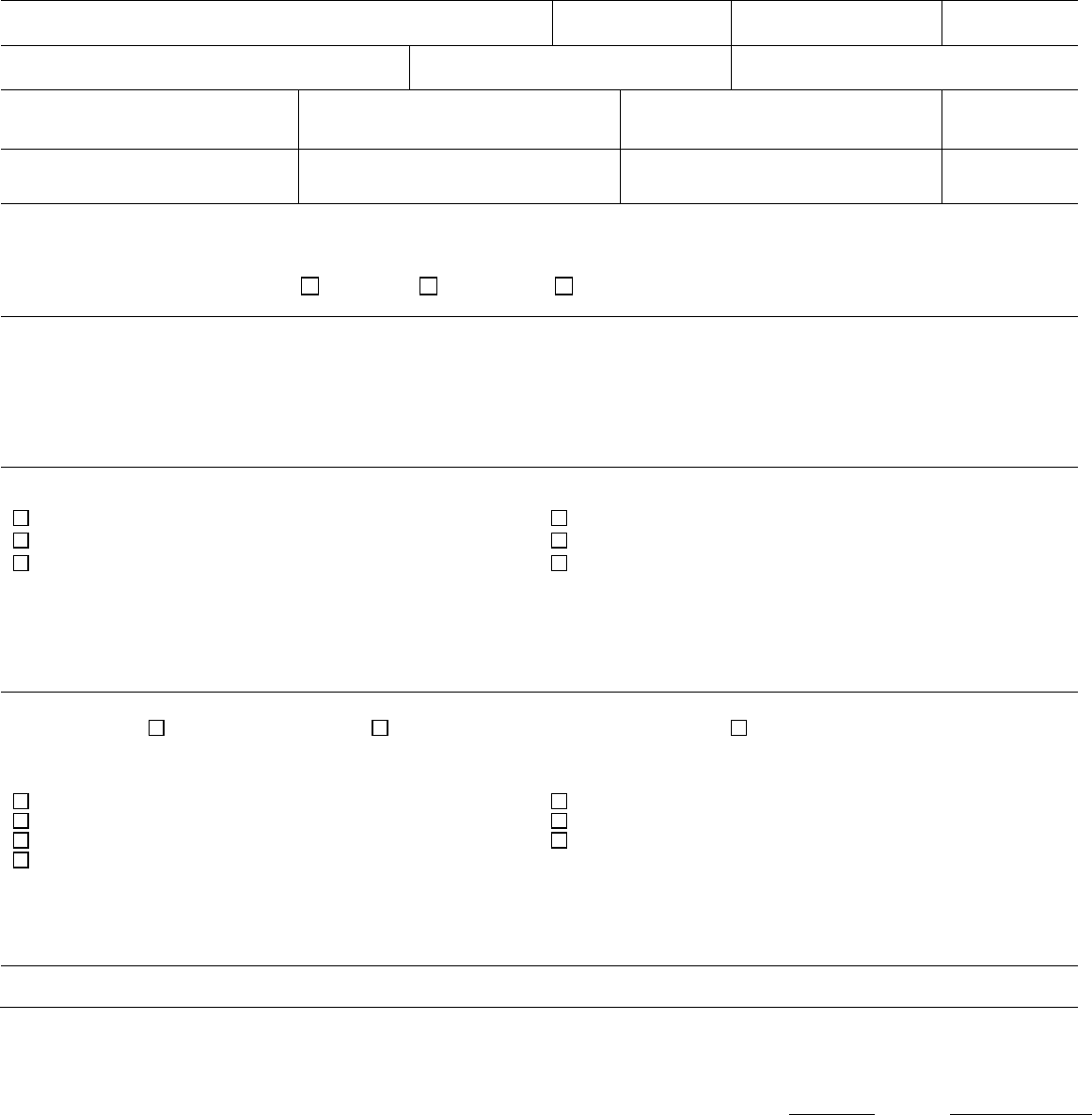
Name – Patient / Client (Last, First MI)
,
ID Number
Living Unit
Date of Birth
Name – Individual Preparing This Form
Name – Staff Contact
Name / Telephone Number – Institution
MEDICATION CATEGORY MEDICATION
RECOMMENDED
DAILY TOTAL DOSAGE RANGE
ANTICIPATED
DOSAGE
RANGE
Antianxiety Agent
(benzodiazepine)
Xanax
(alprazolam)
0.25 - 4mg
The anticipated dosage range is to be individualized, may be above or below the recommended range but no medication will be administered
without your informed and written consent.
Recommended daily total dosage range of manufacturer, as stated in Physician’s Desk Reference (PDR) or another standard reference.
This medication will be administered Orally Injection Other – Specify:
1. Reason for Use of Psychotropic Medication and Benefits Expected (note if this is ‘Off-Label’ Use)
Include DSM-5 diagnosis or the diagnostic impression (“working hypothesis.”)
2. Alternative mode(s) of treatment other than OR in addition to medications include
Note: Some of these would be applicable only in an inpatient environment.
Environment and/or staff changes
Rehabilitation treatments/therapy (OT, PT, AT)
Positive redirection and staff interaction
Treatment programs and approaches (habilitation)
Individual and/or group therapy
Use of behavior intervention techniques
Other Alternatives:
3. Probable consequences of NOT receiving the proposed medication are
Impairment of Work Activities Family Relationships Social Functioning
Possible increase in symptoms leading to potential
Use of seclusion or restraint
Limits on recreation and leisure activities
Limits on access to possessions
Intervention of law enforcement authorities
Limits on personal freedoms
Risk of harm to self or others
Limit participation in treatment and activities
Other Consequences:
Note: These consequences may vary depending upon whether or not the individual is in an inpatient setting. It is also possible that in
unusual situations, little or no adverse consequences may occur if the medications are not administered.
See Page 2

Client Initial
Date
2
F-24277
Medication: Xanax – (alprazolam)
4. Possible side effects, warnings, and cautions associated with this medication are listed below. This is not an all-inclusive list but is
representative of items of potential clinical significance to you. For more information on this medication, you may consult further with your
physician or refer to a standard text, such as the PDR. As part of monitoring some of these potential side effects, your physician may
order laboratory or other tests. The treatment team will closely monitor individuals who are unable to readily communicate side effects in
order to enhance care and treatment.
Continued – Possible side effects, warnings, and cautions associated with this medication.
Less Common Side Effects
Other Less common side effects include: Accidental injury; bladder pain; bloody or cloudy urine; blurred vision; changes in sexual desire or
decreased sexual ability; constipation; cramps; diarrhea; difficult, burning, or painful urination; difficulty in speaking; dizziness or
lightheadedness; dryness of mouth or unpleasant taste; fast or pounding heartbeat; frequent urge to urinate; headache; heavy bleeding with
menstrual period; inability to have or keep an erection; increased sensitivity of skin to sunlight; increased sweating; itching, redness or other
discoloration of skin; loss of appetite; lower back or side pain; nausea or vomiting; pain; severe sunburn; sleepiness or unusual drowsiness;
tooth disorder; twitching; weight loss; memory impairment; insomnia.
Rare Side Effects
Rare side effects include: Abnormal thinking, including disorientation, delusions (holding false beliefs that cannot be changed by facts), or
loss of sense of reality; agitation; behavior changes, including aggressive behavior, bizarre behavior, decreased inhibition, or outbursts of
anger; convulsions (seizures); hallucinations (seeing, hearing, or feeling things that are not there); hypotension (low blood pressure); muscle
weakness; skin rash or itching; sore throat, fever, and chills; trouble in sleeping; ulcers or sores in mouth or throat (continuing); uncontrolled
movements of body, including the eyes; double vision; unusual bleeding or bruising; unusual excitement, nervousness, or irritability; unusual
tiredness or weakness (severe); yellow eyes or skin.
BLACK BOX WARNING
Risks from concomitant use with opioids:
Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve
concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and
durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation.
WARNING
Dependence and Withdrawal Reactions, Including Seizures.
Certain adverse clinical events, some life threatening, are a direct consequence of physical dependence to alprazolam. These include a
spectrum of withdrawal symptoms; the most important is seizure. Even after relatively short-term use at the doses recommended for the
treatment of transient anxiety and anxiety disorder (i.e., 0.75 to 4.0 mg per day), there is some risk of dependence. Spontaneous reporting
system data suggest that the risk of dependence and its severity appear to be greater in patients treated with doses greater than 4 mg/day
and for long periods (more than 12 weeks). However, in a controlled postmarketing discontinuation study of panic disorder patients, the
duration of treatment (3 months compared to 6 months) had no effect on the ability of patients to taper to zero dose. In contrast, patients
treated with doses of alprazolam greater than 4 mg/day had more difficulty tapering to zero dose than those treated with less than 4 mg/day.
The importance of dose and the risks of Alprazolam as a treatment for panic disorder.
Because the management of panic disorder often requires the use of average daily doses of alprazolam above 4 mg, the risk of dependence
among panic disorder patients may be higher than that among those treated for less severe anxiety. Experience in randomized placebo-
controlled discontinuation studies of patients with panic disorder showed a high rate of rebound and withdrawal symptoms in patients treated
with alprazolam compared to placebo-treated patients.
Relapse or return of illness was defined as a return of symptoms characteristic of panic disorder (primarily panic attacks) to levels
approximately equal to those seen at baseline before active treatment was initiated. Rebound refers to a return of symptoms of panic
disorder to a level substantially greater in frequency, or more severe in intensity than seen at baseline. Withdrawal symptoms were identified
as those which were generally not characteristic of panic disorder and which occurred for the first time more frequently during discontinuation
than at baseline.
In a controlled clinical trial in which 63 patients were randomized to alprazolam and where withdrawal symptoms were specifically sought, the
following were identified as symptoms of withdrawal: heightened sensory perception, impaired concentration, dysosmia, clouded sensorium,
paresthesias, muscle cramps, muscle twitch, diarrhea, blurred vision, appetite decrease, and weight loss. Other symptoms, such as anxiety
and insomnia, were frequently seen during discontinuation, but it could not be determined if they were due to return of illness, rebound, or
withdrawal.
In two controlled trials of 6 to 8 weeks duration where the ability of patients to discontinue medication was measured, 71%–93% of patients
treated with alprazolam tapered completely off therapy compared to 89%–96% of placebo-treated patients. In a controlled postmarketing
discontinuation study of panic disorder patients, the duration of treatment (3 months compared to 6 months) had no effect on the ability of
patients to taper to zero dose.
Seizures attributable to alprazolam were seen after drug discontinuance or dose reduction in 8 of 1980 patients with panic disorder or in
patients participating in clinical trials where doses of alprazolam greater than 4 mg/day for over 3 months were permitted. Five of these cases
clearly occurred during abrupt dose reduction or discontinuation from daily doses of 2 to 10 mg. Three cases occurred in situations where
there was not a clear relationship to abrupt dose reduction or discontinuation. In one instance, seizure occurred after discontinuation from a
single dose of 1 mg after tapering at a rate of 1 mg every 3 days from 6 mg daily. In two other instances, the relationship to taper is

Client Initial
Date
3
F-24277
Medication: Xanax – (alprazolam)
indeterminate; in both of these cases the patients had been receiving doses of 3 mg daily prior to seizure. The duration of use in the above 8
cases ranged from 4 to 22 weeks. There have been occasional voluntary reports of patients developing seizures while apparently tapering
gradually from alprazolam. The risk of seizure seems to be greatest 24–72 hours after discontinuation.
Status Epilepticus and its Treatment
The medical event voluntary reporting system shows that withdrawal seizures have been reported in association with the discontinuation of
Alprazolam. In most cases, only a single seizure was reported; however, multiple seizures and status epilepticus were reported as well.
Interdose Symptoms
Early morning anxiety and emergence of anxiety symptoms between doses of Alprazolam have been reported in patients with panic disorder
taking prescribed maintenance doses of alprazolam. These symptoms may reflect the development of tolerance or a time interval between
doses which is longer than the duration of clinical action of the administered dose. In either case, it is presumed that the prescribed dose is
not sufficient to maintain plasma levels above those needed to prevent relapse, rebound or withdrawal symptoms over the entire course of
the interdosing interval. In these situations, it is recommended that the same total daily dose be given divided as more frequent
administrations.
Risk of Dose Reduction
Withdrawal reactions may occur when dosage reduction occurs for any reason. This includes purposeful tapering, but also inadvertent
reduction of dose (eg, the patient forgets, the patient is admitted to a hospital). Therefore, the dosage of alprazolam should be reduced or
discontinued gradually.
CNS Depression and Impaired Performance
Because of its CNS depressant effects, patients receiving alprazolam should be cautioned against engaging in hazardous occupations or
activities requiring complete mental alertness such as operating machinery or driving a motor vehicle. For the same reason, patients should
be cautioned about the simultaneous ingestion of alcohol and other CNS depressant drugs during treatment with alprazolam.
Risk of Fetal Harm
Benzodiazepines can potentially cause fetal harm when administered to pregnant women. If alprazolam is used during pregnancy, or if the
patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Because of experience
with other members of the benzodiazepine class, alprazolam is assumed to be capable of causing an increased risk of congenital
abnormalities when administered to a pregnant woman during the first trimester. Because use of these drugs is rarely a matter of urgency,
their use during the first trimester should almost always be avoided. The possibility that a woman of childbearing potential may be pregnant
at the time of institution of therapy should be considered. Patients should be advised that if they become pregnant during therapy or intend to
become pregnant they should communicate with their physicians about the desirability of discontinuing the drug.
Suicide
As with other psychotropic medications, the usual precautions with respect to administration of the drug and size of the prescription are
indicated for severely depressed patients or those in whom there is reason to expect concealed suicidal ideation or plans. Panic disorder has
been associated with primary and secondary major depressive disorders and increased reports of suicide among untreated patients.
Mania
Episodes of hypomania and mania have been reported in association with the use of alprazolam in patients with depression.
See standard reference text for an all-inclusive list of side effects.

Client Initial
Date
4
F-24277
Medication: Xanax – (alprazolam)
By my signature below, I GIVE consent for the named medication on Page 1 and anticipated dosage range. My signature also
indicates that I understand the following:
1. I can refuse to give consent or can withdraw my consent at any time with written notification to the institution director or designee. This
will not affect my right to change my decision at a later date. If I withdraw consent after a medication is started, I realize that the
medication may not be discontinued immediately. Rather, it will be tapered as rapidly as medically safe and then discontinued so as to
prevent an adverse medical consequence, such as seizures, due to rapid medication withdrawal.
2. Questions regarding this medication can be discussed with the Interdisciplinary Team, including the physician. The staff contact person
can assist in making any necessary arrangements.
3. Questions regarding any behavior support plan or behavior intervention plan, which correspond with the use of the medication, can be
directed to the client’s social worker, case manager, or psychologist.
4. I have the right to request a review at any time of my record, pursuant to § 51.30(4)(d) or § 51.30(5)(b).
5. I have a legal right to file a complaint if I feel that client rights have been inappropriately restricted. The client’s social worker, case
manager, or agency/facility client rights specialist may be contacted for assistance.
6. My consent permits the dose to be changed within the anticipated dosage range without signing another consent.
7. I understand the reasons for the use of the medication, its potential risks and benefits, other alternative treatment(s), and the probable
consequences that may occur if the proposed medication is not given. I have been given adequate time to study the information and find
the information to be specific, accurate, and complete.
8. This medication consent is for a period effective immediately and not to exceed fifteen (15) months from the date of my signature. The
need for and continued use of this medication will be reviewed at least quarterly by the Interdisciplinary Team. The goal, on behalf of the
client, will be to arrive at and maintain the client at the minimum effective dose.
SIGNATURES
DATE SIGNED
Client – If Presumed Competent to Consent/Parent of Minor/Guardian (POA-HC)
Relationship to Client Self
Parent Guardian (POA-HC)
Staff Present at Oral Discussion
Title
Client / Parent of Minor / Guardian (POA-HC) Comments
As parent/guardian (POA-HC) was not available for signature, he/she was verbally informed of the information in this consent.
Verbal Consent
Obtained by – PRINT – Staff Name
Date Obtained
Written Consent Received
Yes No
Obtained from – PRINT – Parent / Guardian (POA-HC) Name
Date Expires
Date Received
