Hospice 101
1

Introduction to
Hospice
Hospice is a health care program designed to meet the needs of
terminally ill individuals when the individual decides that the
physical and emotional toll of curative treatment is no longer in
their best interest.
These individuals choose palliative care, which is not a cure, but
ensures comfort, dignity, and quality of life.
Hospice is intended to address the full range of needs for the
individual with a terminal illness while also considering family needs.
Care must be consistent with the individual’s values regardless of
the location where care is provided.
The primary objective of the Medicaid Hospice Program is to
ensure that essential medical and health services are available to
those who would not otherwise have the financial resources to
purchase them.
Hospice providers must verify eligibility before providing services.
Hospice beneficiaries are identified in CHAMPS 270/271 eligibility
response with the Benefit Plan ID of Hospice.
4

How it Works
Concurrent Hospice and Curative Care of
Children under 21
Medicaid will reimburse for the curative care separately from the
hospice services. Medicaid will not reimburse for these types of
treatments when they are used palliatively.
Palliative care is always a part of hospice and included in the
hospice per diem reimbursement; therefore, cannot be billed
separately or reimbursed by Medicaid.
Palliative care is defined as an active patient and family–centered
approach to pain and symptom management of the terminal illness.
Where as, curative care is defined as medically necessary care that
serves to eliminate the symptoms of a disease with the goal of long-
term disease-free state.
For further instructions on concurrent hospice and curative care
for children under 21 reference the Hospice Chapter, Section 6.8 of
the Michigan Medicaid Provider Manual.
5

How it Works
Medicare Conditions of Participation for Hospice
The duration of hospice coverage is measured in election periods,
also known as benefit periods. A beneficiary may elect to receive
hospice care during one or more of the following election periods:
An initial 90-day period;
A subsequent 90-day period; or
An unlimited number of subsequent 60-day periods
A hospice must obtain written certification of the terminal illness for
each election period before a claim for services is submitted.
If the hospice is unable to obtain a written certification within three
days of initiation of hospice care, a verbal certification must be
obtained, documented, and signed by the person receiving the
certification.
▪ Medicaid follows Medicare’s
hospice guidelines as
outlined in the Medicare
Conditions of Participation
(42 CFR § 418 ).
6
How it Works
Home may include the beneficiary’s private dwelling , apartment,
boarding home, assisted living facility, Adult Foster Care (AFC)
facility, Home For the Aged (HFA), Nursing Facility (NF) or hospice-
owned NF and hospital inpatient care.
Reference Section 6.2 (Other Hospice Covered Services) of the
Michigan Medicaid Provider Manual for other services that may be
necessary and be available but are not considered core services.
▪ The hospice must provide all
or substantially all of the core
services applicable for the
terminal illness in the
beneficiary’s home.
7
Physician care Nursing care
Social work
Counseling:
• Bereavement
• Spiritual
• Dietary
Core Hospice Services
Counseling:
Bereavement
Spiritual
Dietary

How it Works
Transportation Service
Home Setting
Non-emergency and emergency transportation related to the terminal
illness is the responsibility of the hospice provider.
Non-emergency transportation not related to the terminal illness is
available through the local MDHHS office.
Nursing Facility Setting
Non-emergency and emergency transportation related to the terminal
illness is the responsibility of the hospice provider.
Non-emergency transportation not related to the terminal illness must
be provided by the nursing facility as part of their per diem.
8

How it Works
Routine Home
Care
Home care
that is not
continuous.
Continuous
Home Care
In home care
where at
least half of
the hours
are nursing
care
(minimum
of 8 hours).
Inpatient
Respite Care
Short term
care to
relieve the
primary
caregiver.
General
Inpatient Care
Care
provided to
treat
symptoms
that can no
longer be
adequately
treated
under the
routine
hospice care
benefit.
Categories of Care

How it Works
Coordination of Care
Plan of Care (POC):
It is the responsibility of the hospice to develop the POC for hospice services.
If another active program is identified, the hospice provider must contact the
other program(s) and develop a joint POC to coordinate services.
Some examples of places and programs that could potentially be
providing duplicative services are but not limited to:
Adult Foster Care/Home For the Aged
Assisted Living Facility
Nursing Facility
MI Choice Waiver
Private Duty Nursing
10
Provider
Requirements
11

Provider
Requirements
Hospice providers are bound to federal and state rules,
regulations, and policies.
The Michigan Medicaid Provider Manual, Hospice Chapter provides
state specific guidance for providers.
Michigan Medicaid requires hospice agencies to be licensed by the
Department of Licensing and Regulatory Affairs (LARA), which
requires certification by Medicare, and enrollment in Medicaid.
Medicaid-enrolled hospice providers must also comply with the
Medicare Conditions of Participation (42 CFR § 418).
12
Beneficiary
Admission and
Discharge:
CHAMPS
Hospice Providers are responsible for admitting and discharging
beneficiaries for hospice services in the Admissions section in
CHAMPS.
Timely completion of the beneficiary’s admission or discharge will
result in real time changes to the beneficiaries Program
Enrollment Type (PET) and Benefit Plan assignment.
The PET and Benefit Plan assignment are required for correct
payment.
14

Beneficiary
Admission
A terminally ill Medicaid beneficiary who lives in a hospice service area
and whose life expectancy is six months or less (if the illness runs its
normal course), as determined by a licensed physician and the Hospice
Medical Director, may receive hospice services.
Medicaid does not cover Hospice services if the following conditions
exist:
The individual is not eligible for the Medicaid benefit.
The beneficiary does not meet the hospice admissions criteria.
Hospice providers are responsible for admitting beneficiaries for
hospice services.
The admission process must be electronically completed in CHAMPS.
For further details reference Modernizing Continuum of Care (MCC)
webpage.
When completing a hospice admission in CHAMPS, hospice providers
must select the beneficiary’s place of service for where the services are
to be provided.
Beneficiary’s Home
Nursing Facility
Hospice Residence
15

Beneficiary
Admission
Duration of Coverage
There is no minimum period of hospice admission.
A change in the beneficiary’s prognosis could eliminate the need for
hospice care.
A beneficiary may cancel their admission in hospice at any time and
without cause.
16

Beneficiary
Discharge
A beneficiary may be discharged from hospice as noted below:
Beneficiary elects voluntary discharge
Beneficiary revokes their election due to hospitalization
Beneficiary no longer meets criteria
Beneficiary becomes ineligible for Medicaid
Beneficiary moves outside the service area
Hospice is revoked due to violation (i.e., fraud, abuse, misconduct)
Death
The provider must complete the Discharge screen in CHAMPS.
Ensure an accurate roster
Ensure beneficiary has the correct PET and Benefit Plan assigned
Ensure correct payment
17

Billing and
Reimbursement:
Claim Completion
Michigan Medicaid Provider Manual
Billing and Reimbursement for Institutional Providers Chapter
Hospice –Section 11
The following contains
information that should
be used in conjunction
with National Uniform
Billing Committee
(NUBC) manual when
preparing Hospice
claims.
19

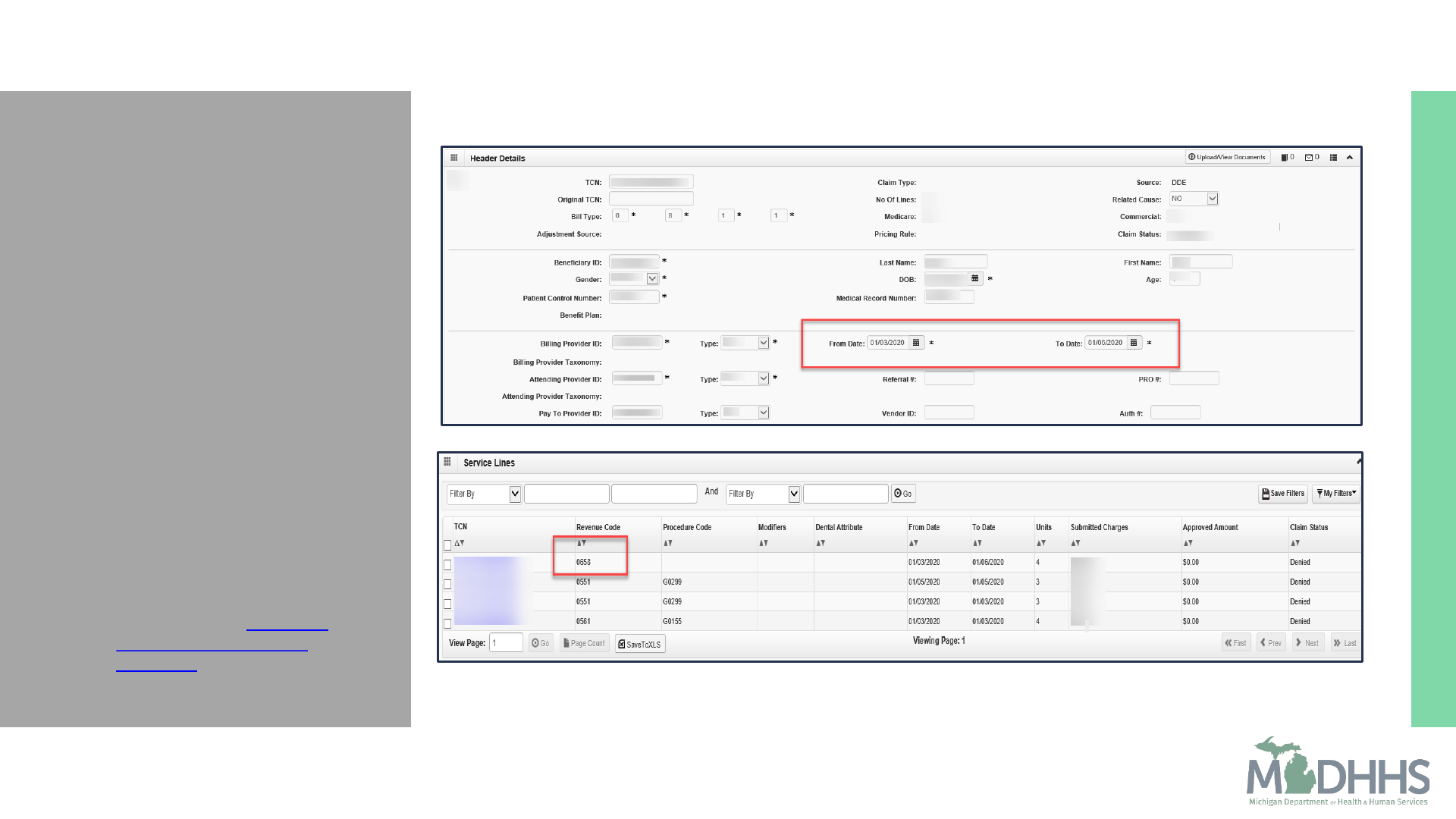
Billing and
Reimbursement:
Claim
Completion
Common billed Revenue codes
0651 – Routine Home Care
0658 – Other Hospice (Room and Board)
0551 – Skilled Nurse Visit
With HCPCS G0299 – Registered Nurse
0561 – Social Worker
With HCPCS G0155 – Social Worker
For a complete list of payable hospice revenue codes reference, Revenue
Code Table.
For more information when completing a claim reference, Billing &
Reimbursement for Institutional Providers Chapter, Section 11.1 – Billing
Instructions for Hospice Claim Completion.
20

Billing and
Reimbursement:
Claim
Completion
Billing for 0651 – Routine Home Care
Reimbursed in two–tier rate:
Higher rate for the first 60 days
Decreased rate for days 61 and beyond
Providers should bill in sequential order to receive correct tier
reimbursement
Hospice day is counted when any level of hospice care is provided. If
a beneficiary is discharged from hospice (not due to death) and
returns to hospice within 60 days, the count will resume from the
point the beneficiary left hospice. If beneficiary is discharged (not
due to death) and returns after more than 60 days have elapsed, the
count will reset to day one . The hospice days do not reset if
beneficiary transfers to a different hospice provider.
21

Billing and
Reimbursement:
Claim
Completion
Billing for 0658 – Other Hospice (Room and Board)
Hospice providers are paid 95% of the Nursing Facility per diem.
Room and board is reimbursable on the day of discharge
If the discharge is due to resident death
If the resident is discharged from hospice but remains in the NF
22

Billing and
Reimbursement:
Claim
Completion
Billing for 0551 – Skilled Nurse Visit or 0561 – Social Worker
In order to be considered for the Service Intensity Add-On (SIA) rate
the following billing requirements must be met:
Minimum of 15 minutes but not more than four hours daily during the
last 7 days of beneficiary’s life when the beneficiary is receiving routine
home care.
Occurrence Code 55 with the date of death
Discharge status of 20 death
Allowable codes:
Registered Nurse 0551 / G0299
Social Worker 0561 / G0155
23

Top Claim
Denials
• CARC – 16 / RARC -N322
• Hospice certification date
missing
• CARC - B9
• Certification date not in
sequential order
• CARC – 16 / RARC - N65
• Unable to determine rate
when billing 0651
• CARC – 16 / RARC - N65
• Unable to determine rate
when billing 0658
• CARC – 16 / RARC - N330
• Service intensity missing or
incomplete
24
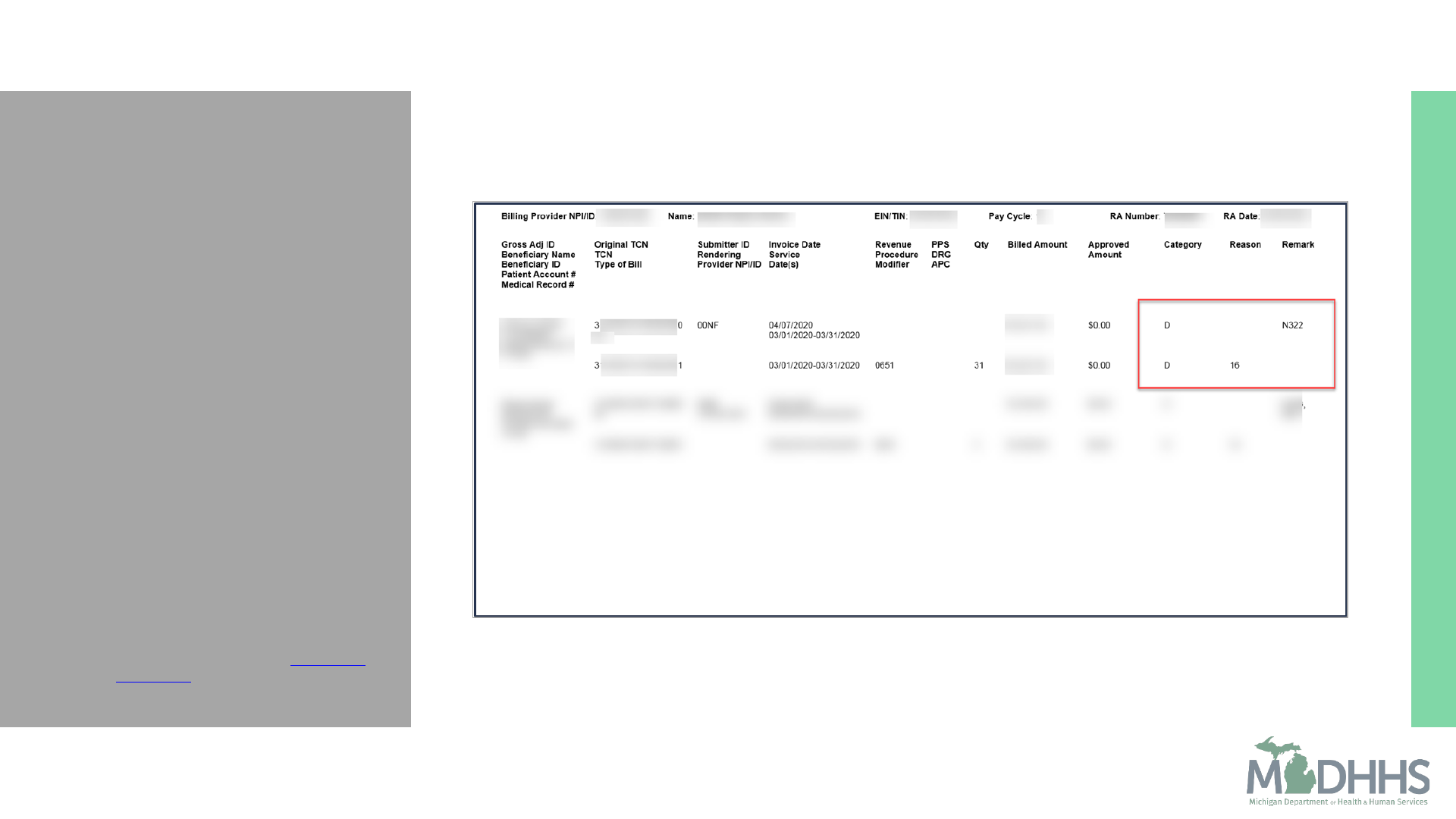
Top Claim Denials:
16/N322
▪ Claim Service lacks
information/Missing
Incomplete Invalid Last
certification date
▪ Hospice Certification date
missing or invalid
▪ Admission Date: The
Certification (start) date must
be reported on every hospice
claim with Occurrence Code 27
and the applicable date.
▪ Additional Resources:
• Retrieving Medicaid Paper RA
and RA Explanation - My Inbox
webpage
25

Top Claim Denials:
B9
▪ Patient is Enrolled in a Hospice
▪ Hospice Cert date prior to
initial cert date
▪ Admission Date: The
Certification (start) date must
be reported on every hospice
claim with Occurrence Code 27
and the applicable date.
▪ Additional Resources:
• Retrieving Medicaid Paper RA
and RA Explanation - My Inbox
webpage
27
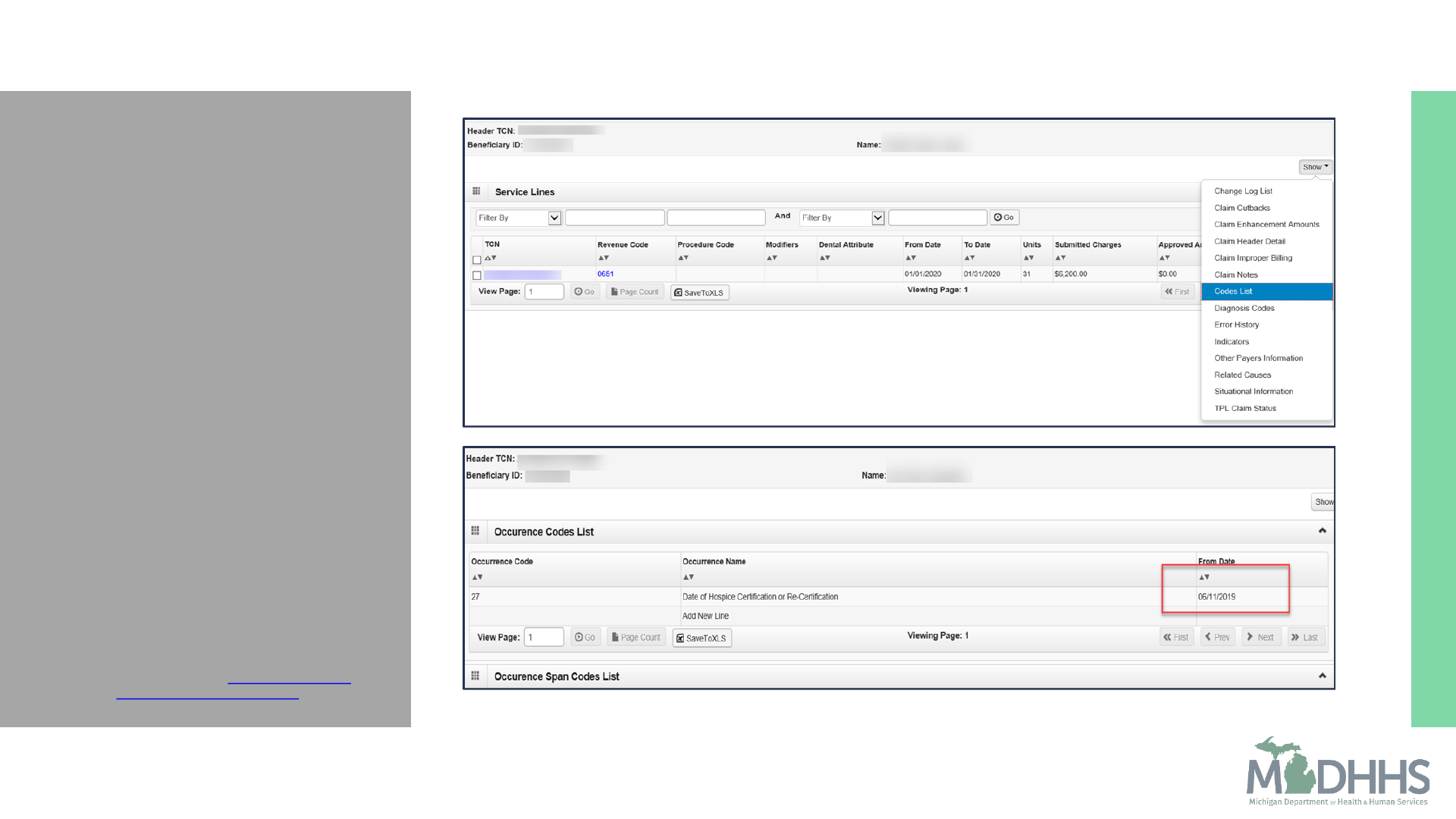
Top Claim Denials
▪ Pull up the TCN in CHAMPS
under Claim Inquiry
▪ Go into the claim service line
▪ Click the show drop-down
▪ Select Codes List
▪ This is where the certification
date is reported.
▪ Its important to make sure the
hospice claims are billed in
sequential order to avoid this
denial.
▪ Additional Resources
• Claim Inquiry - CHAMPS Claims
and Encounter webpage
28

Top Claim Denials:
16/N65
▪ Claim/service lacks
information/Procedure rate
count cannot be determined
▪ Unable to determine rate
when billing 0651
▪ Value code 61 with
applicable CBSA code is
required on every hospice
claim
▪ Additional Resources:
• Retrieving Medicaid Paper
RA and RA Explanation - My
Inbox webpage
29

Top Claim Denials:
16/N65
▪ Claim/service lacks
information/Procedure rate
count cannot be determined
▪ Unable to determine rate
when billing 0658
▪ Room and Board (0658):
Hospice services are payable
for room and board in a
Nursing Facility.
▪ Additional Resources:
• Retrieving Medicaid Paper
RA and RA Explanation - My
Inbox webpage
31

Top Claim Denials
▪ Take the Bene ID and verify
their admission/enrollment
under the member tab. To do
this:
• Exit out of claim
• Select Member Tab to look
up Admission Record by
selecting Program
Enrollment/Admission
• The Member
Enrollment/Admission List
will display
• Select Member ID
• Enter beneficiary ID number
• Find the applicable
Admission record
33

Top Claim Denials
▪ Once the Admission record is
located, select the View
Details from the Action drop-
down.
34

Top Claim Denials
▪ The Admission/Enrollment
Information page will display
with the nursing facility NPI
reported
▪ Validate the nursing facility
NPI
35

Top Claim Denials
▪ 16/N330 Claim lacks
information /Missing
incomplete/invalid patient
death date
▪ Hospice Add on Payment
Denied for missing/mismatch
information
▪ Service Intensity Add On:
Payable during the
beneficiary’s last seven days of
life.
▪ Additional Resources:
• Retrieving Medicaid Paper RA
and RA Explanation - My Inbox
webpage
36

Summary
General Overview
Hospice is a health care program designed to meet the needs of terminally ill
individuals. Michigan’s Medicaid Program goal is to ensure these essential
medical and health services are available to individuals who would not
otherwise have the financial resources to receive them.
State and Federal Regulations
Hospice providers must follow regulatory guidelines and policies as set forth
by Medicare, Medicaid, and LARA.
Beneficiary Admissions and Discharges
Admissions and Discharges must be completed in a timely manor to allow
for real time PET and Benefit Plan assignment to support claim payment.
38
Summary
Billing and Reimbursement
Revenue codes are required for claim submission.
For a complete list of revenue codes visit Revenue Code Table.
Top Claim Denials
16/N322 Hospice certification date missing or invalid
B9 Certification date prior to initial certification date
16/N65 Unable to determine rate
16/N330 Hospice Add on payment denied for missing information
39

Provider
Resources
MDHHS website:
www.michigan.gov/medicaidproviders
We continue to update our
Provider Resources:
CHAMPS Resources
Listserv Instructions
Medicaid Provider Training Sessions
Provider Alerts
Provider Enrollment Website
Provider Support:
1-800-292-2550
Thank you for participating in the Michigan Medicaid
Program
40