
International Journal of Psychology and Psychological Therapy 2003, Vol. 3, Nº 2, pp. 299-310
Application of the IPT in a Spanish Sample: Evaluation
of the “Social Perception Subprogramme”
Sonia García
*
, Inmaculada Fuentes*
1
, Juan Carlos Ruíz
*
, Elisa Gallach
**
and Volker Roder
***
*Universidad de Valencia, España. **Equipo de Salud Mental de Aldaia, Valencia, España.
***University of Berna, Switzerland.
1
Reprints may be obtained from the first author. Departamento de Personalidad, Evaluación y Tratamiento Psicológicos,
Facultad de Psicología, Avenida de Blasco Ibáñez 21, 46010 Valencia, España. E-mail: fuentesd@uv.es
ABSTRACT
This study analyses the impact of the second IPT subprogramme (Roder, Brenner, Hodel
& Kienzle, 1996) in chronic schizophrenic patients. The programme intends to improve
their ability to perceive and to interpret social situations. The sample was formed by 20
participants, divided into two groups: 11 in the therapy group and 9 in the control group.
Social and clinical measures have been used, as well as an instrument developed for the
assessment of Social Perception, as it is defined in the IPT. This instrument has been
sensitive to changes in the pre-treatment and post-treatment measures, showing that
schizophrenics patients have improved their ability to perceive and to interpret reality in
a more adequate way.
Key Words: Social Perception, Schizophrenia, Assessment, Psychosocial Intervention,
Cognitive Behaviour Therapy.
RESUMEN
Aplicación de la IPT en una muestra española: evaluación del "subprograma de percep-
ción social". Este estudio investiga los efectos del segundo subprograma de la IPT en
pacientes esquizofrénicos crónicos (Roder, Brenner, Hodel y Kienzle, 1996). El programa
pretende mejorar sus habilidades para percibir e interpretar situaciones sociales. La muestra
está formada por 20 participantes, divididos en dos grupos: 11 constituyen el grupo
experimental y 9 el grupo control. Se han utilizado medidas clínicas y sociales, así como
un instrumento desarrollado para la evaluación de la percepción social, tal y como es
trabajada en la IPT. Este instrumento se ha mostrado sensible a los cambios pre y post-
tratamiento, poniendo de manifiesto que los pacientes esquizofrénicos han mejorado sus
habilidades para percibir e interpretar la realidad de un modo más adecuado.
Palabras Clave: Percepción Social, Esquizofrenia, Evaluación, Intervención Psicosocial,
Terapia Cognitivo Conductual.
300
© Intern. Jour. Psych. Psychol. Ther.
S. GARCÍA, I. FUENTES, J. C. RUIZ, E. GALLACH, V. RODER.
People do not react to reality just as it is, but as they build or interpret it (Ibáñez,
1979). Only an adequate interpretation of the environment, physical and social, permits
our adaptation to it. For that reason, reality interpretation and the processes involved
in it should be important aspects to consider in the rehabilitation of mental patients.
Bedell & Lenox (1994) have studied the relation in the way we perceive reality and
how we behave in society. These authors think that the ability to perceive is an important
factor for a good social functioning. They consider that social abilities would include
two groups of skills: cognitive and behavioural. Social perception and information
processing are included in the cognitive skills group. Both of them define, organize and
guide social skills. On the other hand, behavioural skills refer to verbal and nonverbal
behaviour used in applying the action of a decision once cognitive processes have
finished.
In the late eighties, as a result of the investigations that related cognitive deficit
and social skills, it was concluded that schizophrenic patients had a deficit in social
perception. This was particularly true in the recognition of affects, which makes them
answer inadequately to other people (Halford & Hayes, 1991). Other deficit identified
besides facial affect recognition (Morrison, Bellack & Mueser, 1988; Bellack, Blanchard
& Mueser, 1996), and nonverbal perception (Toomey, Wallace, Corrigan, Schulderg &
Green, 1997), has been inapropiate situational stimulus perception (Corrigan & Green,
1993).
In relation with facial affect recognition, Bellack (1992) thinks that schizophrenics
shown a marked deterioration, especially in the ability to identify negative affects
shown by others. Leff & Abberton (1981) related these deficits in schizophrenic patients
with emotional flattening. It is known that different aspects of social perception such
as facial affect recognition, perception of dynamic social stimuli and self-perception are
related to social functioning in schizophrenia (Frith, 1995; Penn, Combs & Mohamed,
2001). Although literature shows the referred results, mediator processes among
neurochemical dysfunction and behavioural symptoms have not been studied in intervention
programmes. Roder, Brenner, Hodel & Kienzle (1996) indicate that among the mediator
processes, attention and perception processes are especially affected, as well as those
of recognition, integration and transformation of internal and external stimuli.
In fact, it is considered that the interventions focused in the social perception
skills should serve to improve generalization of treatment and its maintenance (Penn et
al., 2001).
Roder et al. (1996) have developed an integrated therapy for schizophrenic patients
(IPT) (Integriertes psychologisches Therapieprogramm fur schizophrene Patienten) with
the purpose of working as much on cognitive functioning as on social functioning in
schizophrenic patients. It is a group intervention programme with five subprogrammes:
Cognitive Differentiation, Social Perception, Verbal Communication, Social Skills Training
and Interpersonal Problem Solving. They are hierarchically ordered so the first interventions
are directed to basic cognitive skills, the next interventions transform the cognitive
skills into social and verbal behaviours, and the last ones train the patients in the
solution of more complex interpersonal problems. Nowadays IPT is considered a good
© Intern. Jour. Psych. Psychol. Ther.
AN APPLICATION OF THE IPT IN A SPANISH SAMPLE 301
procedure, with sufficient empirical support for schizophrenia treatment (Pérez &
Fernández, 2001; Vallina & Lemos, 2001)
In this investigation we have trained social perception skills in a schizophrenic
group of patients through the application of the second IPT programme. Some authors
(Vallina et al., 2001) consider it to be a basic programme because it contains the
essence of all the cognitive interventions which included IPT (reception of information,
its analysis and the emission of responses made after previous information has been
received and analyzed). These three cognitive processes are the basis for the
implementation of techniques and procedures used in the intervention package.
Research in which IPT is evaluated doesn’t specifically assess social perception.
Usually the considered measures in literature are: memory, verbal fluency, executive
functions, synonyms and antonyms, word recognition, concentration and short and long
term memory (Kraemer, 1991; Penadés, 2002; Roder, Studer & Brenner, 1987). Other
assessment instruments used in these studies are: Benton Test (Brenner, Hodel, Kube
& Roder, 1987a), and Frankfurt Test (FCQ) (Brenner, Hodel, Roder & Corrigan, 1992;
Vallina et al., 2001).
Because of this lack of attention to the evaluation of social perception, a Social
Perception Scale (EPS) has been developed considering the three phases of the Social
Perception Programme. This instrument is intended to evaluate changes produced by
the training in social perception, and also to know at which moment the patient is
prepared to go to the next programme. The effectiveness of the programme has also
been studied when applied to patients with more deterioration than those that usually
participate in this type of research. For example, in the study of Brenner et al. (1987a),
the average IQ of the 43 participants was 98, and the duration of the illness was of
nearly 6 years. Although in other studies, the average duration of the illness range
between 7 and 10 years (Brenner, Boker, Muller, Spichtig & Wurgler, 1987b; Hodel &
Brenner, 1994; Vallina et al., 2001).
METHOD
Participants
Patients from this report are users of the Centre of Mental Health of Aldaia
(Valencia), and attend the Association for Support to the Mental Health (AASAM)
association. The following selection criteria were applied: diagnosis of schizophrenia
according to CIE-10, without any organic damage nor abuse of alcohol or drugs, and
to be in an age range between 18 and 50 years. All the patients were receiving
pharmacological treatment either typical (haloperidol, fluphenazine) or atypical
antipsychotics (clozapine, risperidone). A brief interview with the 25 patients with
those requirements was made to evaluate their IQ using two tests: the vocabulary test
of the WAIS-III (verbal), and the Toni-2 test (nonverbal). Criteria for the inclusion in
the program were: a score of 4 in the vocabulary test or an IQ of 65 in the TONI-2 test.
After the application of this criteria the number of participants was reduced to 23. 13
of them were assigned to the therapy group and 10 to the control group. The sample
was matched by demographic and clinical data as shown in Table 1.

302
© Intern. Jour. Psych. Psychol. Ther.
S. GARCÍA, I. FUENTES, J. C. RUIZ, E. GALLACH, V. RODER.
Instruments
Following Wykes (2000) point of view we have considered three levels of analysis:
the neuropsychological, the clinical and the functional. According to this author, the
three levels are necessary to evaluate the effectiveness of any rehabilitation program.
In order to evaluate the changes the following scales were administered at the beginning
of the treatment and three months later, just when the Social Perception Programme
finished.
Social Perception Measures
Social Perception Scale (EPS) (García, 2003). The instrument is structured
according the three phases of the Social Perception Programme of the IPT: First, stimuli
identification; second, interpretation; and third, title assignment.
Four photographs and register sheets were used to assess patients in the three
aspects in which the programme focuses. Photographs were taken from the 40 slides
that integrate the program (numbers: 02, 05, 06 and 07). Two of them were chosen
because they had a high cognitive complexity, and the other two because they had a
high emotional content. After giving a photograph to the subject and inviting him to
observe it, the following questions were asked: What details/stimuli can you see in the
photograph? (First part); What is happening in the photograph? (Second part); What
title can summarise the more relevant aspects in the photograph? (Third part). Answers
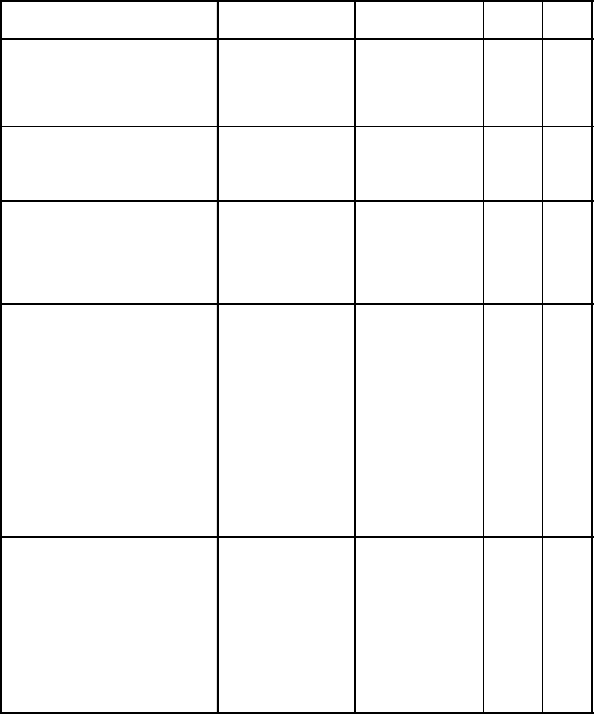
Table 1. Demographic and social characteristics of subjects
Characteristics Treatment group Control group
Number of subjects 11 9
Age (mean/sd) 40.45 (7.10) 36.88 (8.10)
IQ (mean/sd) 75.90 (14.07) 73.55 (10.63)
Sex: Male
Female
9
2
5
4
Education: Illiteracy
Primary school not completed
Primary school
Secondary school
1
4
4
2
0
5
2
2
Occupational situation: Pensioner 11 9
Housing situation: Alone
Sheltered home
With parents
With brothers/sisters
1
2
6
2
0
1
7
1
Ma rital status: Single
Divorced
11
0
8
1
Diagnostics: Hebefrenic
Undifferentiated
Paranoid
Residual
3
1
5
2
1
1
6
1
Duration illness (mean years) 21 14.77
© Intern. Jour. Psych. Psychol. Ther.
AN APPLICATION OF THE IPT IN A SPANISH SAMPLE 303
corresponding to each part were noted on to the register sheet. In the first part of the
register sheet there is a list containing the stimuli present in the image with which to
score patients later. In this part the patient has one and a half minutes to say which
stimuli were in the photographs. With answers of the patient in this first part three
scores were obtained: proportion of identified stimuli, number of errors, and number of
interpretations made. In the second part, subject answers were valued using a Likert
scale: 0 (no answer), 1 (no appropriate interpretation), 2 (partially appropriate
interpretation) and 3 (appropriate interpretation). In the third part patient answers were
again valued using a Likert scale: 0 (no answer), 1 (no appropriate title), 2 (partially
appropriate title) and 3 (appropriate title). These two scores were then transformed into
proportions, taking into account the maximum score in each part was 12.
In the assessment of the second and third part, it was relevant that the answers
of the subjects made reference to the situational context, actor/s, and the action or
interaction among them. So when answers didn’t allude to any of these aspects or only
to one of them, but add imagined aspects, the score of the answer was 1. If it made
reference to two of the indicated aspects, the score was 2. And finally, if it made
reference to three, the score was 3.
Attention
Test of Sustained and Selective Attention (TASS) (Batle and Tomás, 1999). It has
different geometric figures, and the task consists of ticking some of them with a cross.
Specifically the patient has to mark "the yellow circles and all the squares of any
colour". The time for the task, in the form that we have used (A) is 8 minutes. This test
evaluates sustained and selective attention.
Psychopathology
Brief Psychiatric Rating Scale (BPRS) (Lukoff, Nuechterlein and Ventura, 1986).
The scale contains 24 items. Each one scores according to a Likert type scale (1 is
equivalent to no symptoms and 7 to extreme gravity). It also gives scores in 5 subscales
and a global score (see table 2). This instrument, as well as the next two, were not
administered by the investigators, but by an expert of the mental health personnel of
Aldaia.
Frankfurt Complaint Inventory (FBF-3) (Süllwold and Huber, 1986). We have
used the version of this self-report made by Jimeno, Jimeno & Vargas (1996), which
contains 98 items distributed in 10 scales (see table 2).
Social Functioning
Disability Assessment Schedule (DAS II) (WHO, 1985). The adaptation made by
Montero, Bonet, Puche & Gomez Beneyto (1988) was used. This test is conducted
through an interview between the expert and the patient or someone known the patient.
It is evaluated in a 9 points scale of gravity, that range from "non-dysfunctial" (0) to
304
© Intern. Jour. Psych. Psychol. Ther.
S. GARCÍA, I. FUENTES, J. C. RUIZ, E. GALLACH, V. RODER.
"completely dysfunctional most of the time" (8). The first part of the interview (General
Behaviour), the second part (Social Roll Execution) and the fifth part (Global Assessment)
were used. Four items of the second part were excluded, due to the characteristics of
the sample, as they were impossible to evaluate (see table 2).
Procedure
Two groups, one of control and one experimental, were used in a completely
randomized design. Both groups were evaluated in the different dependent variables
before and after the application of the treatment. The therapy group was divided into
two groups for the psychological intervention programme, so the number of participants
in each group was, at the beginning, 7 and 6 but, due to the absence of two of the
subjects, the final groups were formed by 6 and 5 respectively. The clinical intervention
in the therapy group was based on the application of the Social Perception Programme.
The duration of the treatment was 3 months. The frequency of the sessions was twice
a week for each therapy group, with a duration of 30 minutes in the first five sessions
(because only one slide was used) and 60 minutes for the rest (working with two slides
per session). The total number of sessions was 21.
In the first sessions, slides with low cognitive complexity and low emotional
content were used. Later on, slides with more cognitive complexity were added, and
from time to time, slides with more emotional content were included. The total number
of slides used was 36 (because 4 were employed in the EPS). Positioning of the chairs
in a semicircle was habitual in the application of the programme, with a big table in
the centre to write the titles. The distribution of the seats guaranteed the visual contact
between the participants themselves and with the therapists. Two professionals applied
the programme, a therapist and a Co-therapist, both of them assuming the recommended
functions of the IPT authors (Roder et al., 1996).
The application of the Social Perception Programme intends to improve the
perception and interpretation of social situations. This programme has three phases:
first, the participants must say all possible details presented in the image. This phase
is essential for the rest of the programme because the collected information will be used
by the participants to explain and justify their own interpretations; second, participants
give their opinion about the content of the image, and it must be justified with the
visual information gathered before. Later on, a debate begins looking for the most
appropriate interpretation of the social situation that appears in the slide. Finally, in the
third phase, each patient gives a title to the image making reference to the more
relevant aspects of it.
RESULTS
Non-parametrical statistical procedures were used throughout the analyses. Group
differences before and after the treatment between the experimental and control groups
were calculated using the Mann-Whitney U-test. Pre-test/post-test intervention differences
in both groups were analyzed using the Wilcoxon test. Effect sizes were also calculated

© Intern. Jour. Psych. Psychol. Ther.
AN APPLICATION OF THE IPT IN A SPANISH SAMPLE 305
in order to describe the relevance of changes after the treatment in the therapy group.
Group differences before treatment: Baseline differences between groups were
examined by the Mann-Whitney U-test. This analysis showed significant differences in
just three measures: EPS (quality of the title, z= 2.41, p= 0.016); Frankfurt (lost of
control, z= 2.00, p= 0.045); and DAS II (social contacts, z= 2.01, p= 0.044), indicating
that the two groups, were to a great extent, homogeneous before the intervention.
Group differences after treatment: Due to the absence of some data, the statistical
analysis of the FBF scores were calculated with 7 subjects corresponding to the control
group and 5 to the the experimental group. The analysis revealed that although there
were no clinical differences between the two groups, they differ in four of the five
scores of the social perception scale: proportion of identified stimuli (z= 2.43, p=
0.015); number of interpretations (z= 2.81, p= 0.005); proportion of adequate interpretations
(z= 2.02, p= 0.043); and quality of the title (z= 2.97, p= 0.003). There were no differences
Table 2. Pre-test/post-test treatment measures for the control group and
Wicolxon “z” values (NS= not significant).
VARIABLES PRE-TEST
MEAN (SD)
POST-TEST
MEAN (SD)
Z P
EPS
Proportion of identified stimuli
Number of interpretations
Number of errors
Proportion of adequate interpretations
Proportion of quality title
35.32 (10.50)
5.22 (2.11)
2.44 (1.42)
63.89 (12.50)
55.56 (10.21)
36.65 (9.96)
5.33 (1.66)
2.11 (1.45)
61.11 (8.33)
49.07 (15.28)
-0.42
-0.28
-0.72
-0.68
-1.15
NS
NS
NS
NS
NS
TASS
Direct Score
Hits
Omission
Errors
10 2.22 (45.45)
10 9.78 (31.79)
13.89 (14.40)
1.67 (3.91)
107.09 (36.25)
114.78 (33.33)
10.00 (12.94)
.67 (1.12)
-1.01
-1.76
-2.20
-0.14
NS
NS
.028
NS
BPRS
Anxiety / Depression
Thought disorders
Anergia
Activation
Hostility
Total Score
7.44 (3.40)
12.33 (7.38)
8.89 (4.51)
7.00 (5.63)
8.56 (6.21)
44.22 (21.92)
8.33 (3.54)
8.78 (4.60)
5.00 (1.00)
4.11 (2.62)
5.00 (3.04)
31.22 (7.22)
-0.86
-1.52
-2.20
-1.78
-1.61
-2.10
NS
NS
.028
NS
NS
.035
FBF-3
Loss of control
Simple perception
Complex perception
Speech
Cognition and Thought
Memory
Motor behavior
Loss of automatic behavior
Depression
Stimuli overload
Factor 1. Cognition Disorder.
Factor 2. Perception-Motor skills
Factor 3. Depression
Factor 4. Stimuli Overload.
Total Score
4.14 (1.77)
2.00 (2.00)
3.57 (3.21)
5.71 (2.14)
4.57 (3.21)
5.00 (3.27)
2.86 ( .69)
5.00 (2.24)
3.29 (2.50)
4.14 (1.57)
9.14 (4.63)
7.57 (4.58)
13.57 (6.21)
9.00 (4.08)
40.00 (17.33)
4.00 (2.00)
3.29 (2.69)
4.29 (2.50)
6.71 (2.69)
5.00 (3.16)
5.43 (2.51)
4.43 (2.07)
5.86 (1.86)
4.43 (2.23)
4.43 (1.81)
11.00 (3.91)
10.71 (5.35)
15.57 (5.74)
9.00 (4.08)
48.29 (18.13)
-0.37
-0.77
-0.81
-0.86
-0.43
-0.54
-1.63
-0.85
-0.85
-0.70
-1.02
-1.27
-1.02
-0.35
-0.95
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
DAS II
Self -Care
Leisure time
Slowness
Communication
Participation in household
Social Contacts
Performance at work
Interest in getting a job
General Interest
Emergency or crisis behavior
Social Adjustment Total Score
2.22 (3.03)
4.56 (3.13)
2.56 (2.55)
3.56 (2.92)
3.22 (3.15)
2.44 (2.46)
3.63 (2.13)
4.11 (2.33)
4.44 (3.54)
4.11 (3.02)
3.11 (1.05)
2.56 (2.74)
2.33 (1.66)
1.56 (1.42)
3.56 (3.05)
1.67 (1.41)
2.11 (2.71)
3.89 (2.80)
4.89 (2.52)
4.78 (2.91)
4.22 (3.11)
3.00 ( .87)
-0.55
-1.87
-1.06
-0.09
-1.36
-0.53
-0.68
-0.17
-0.34
-0.07
-0.38
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
306
© Intern. Jour. Psych. Psychol. Ther.
S. GARCÍA, I. FUENTES, J. C. RUIZ, E. GALLACH, V. RODER.
in the EPS score ‘number of errors’ probably due to a floor effect. These results point
out an improvement in the perception and interpretation of social situations in the
therapy group.
Pre-test/post-test intervention changes: Pre-tests/post-test changes were analyzed
in both groups in every measure. As shown in Tables 2 and 3 there were no significant
differences in most of the cognitive, social functioning and psychopathology measures
in both groups. However some specific changes were observed. In the control group
there were significant changes in one TASS score (omissions) and in two BPRS scores
(anergia and total score). In the therapy group there were significant changes in one
Table 3. Pre-test/post-test treatment measures for the therapy group and
Wilcoxon´s “z” values (NS= not significant).
VARIABLES PRE-TEST
MEAN (SD)
POST-TEST
MEAN (SD)
Z P
EPS
Proportion of identified stimuli
Number of interpretations
Number of errors
Proportion adequate interpretations
Proportion quality title
34.87 (10.43)
6.00 (2.57)
1.82 (1.25)
56.82 (9.73)
43.18 (11.07)
48.98 (9.90)
2.45 (1.97)
1.36 ( .81)
78.79 (18.40)
80.30 (19.82)
-2.86
-2.50
-0.97
-2.81
-2.81
.004
.012
NS
.005
.005
TASS
Direct Score
Hits
Omission
Errors
104.37 (50.90)
115.36 (51.50)
5.45 (6.58)
3.60 (9.93)
106.16 (40.00)
110.73 (33.66)
7.09 (10.63)
.45 (1.21)
-0.62
-0.66
-0.46
-1.07
NS
NS
NS
NS
BPRS
Anxiety / Depression
Thought disorders
Anergia
Activation
Hostility
Total Score
7.27 (3.64)
9.82 (5.36)
7.45 (2.62)
5.09 (2.66)
4.64 (2.50)
34.36 (13.06)
7.18 (2.75)
6.73 (3.13)
5.00 (2.41)
4.36 (2.01)
4.18 (2.99)
27.36 (8.29)
-0.18
-1.47
-1.84
-0.85
-0.53
-1.56
NS
NS
NS
NS
NS
NS
FBF-3
Loss of control
Simple perception
Complex perception
Speech
Cognition and Thought
Memory
Motor behavior
Loss of automatic behavior
Depression
Stimuli overload
Factor 1. Cognition Disorder.
Factor 2. Perception-Motor skills
Factor 3. Depression
Factor 4. Stimuli Overload.
Total Score
1.80 (1.30)
4.00 (3.08)
3.40 (2.07)
5.60 (2.88)
4.60 (2.70)
5.00 (2.92)
4.60 (2.70)
4.00 (2.74)
4.00 (2.12)
3.80 (1.79)
8.80 (3.27)
11.00 (7.48)
11.00 (5.05)
8.80 (3.42)
40.80 (17.04)
4.40 (2.30)
4.00 (2.74)
5.40 (2.41)
6.60 (2.30)
6.80 (1.30)
5.60 (2.19)
5.20 (3.70)
6.20 (3.03)
5.00 (1.41)
6.00 (1.41)
13.60 (4.39)
15.00 (8.15)
16.00 (2.65)
11.40 (2.88)
56.00 (15.65)
-1.46
-0.00
-0.81
-0.68
-1.84
-0.54
-0.37
-0.41
-0.96
-1.51
-1.49
-0.73
-1.22
-0.96
-0.94
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
DAS II
Self -Care
Leisure time
Slowness
Communication
Partic ipation in household
Social Contacts
Performance at work
Interest in getting a job
General Interest
Emergency or crisis behavior
Social Adjustment Total Score
1.82 (2.79)
4.18 (2.60)
2.27 (2.53)
4.27 (3.00)
2.50 (2.88)
0.60 (1.35)
2.20 (2.30)
3.78 (2.59)
4.73 (2.90)
5.27 (3.10)
3.00 ( .89)
1.64 (1.57)
1.91 (1.22)
1.64 (2.06)
2.09 (2.74)
2.09 (1.92)
.64 (1.21)
2.27 (2.28)
3.36 (3.11)
4.64 (2.87)
4.45 (2.46)
2.64 (1.12)
-0.21
-2.30
-0.67
-1.69
-0.85
-0.00
-0.26
-0.17
-0.12
-1.18
-1.27
NS
.021
NS
NS
NS
NS
NS
NS
NS
NS
NS

© Intern. Jour. Psych. Psychol. Ther.
AN APPLICATION OF THE IPT IN A SPANISH SAMPLE 307
DAS II score (leisure time). But the results were quite different in social perception
measures. There wasn’t any pre-test/post-test change in the control group, but there
were significant and positive differences in four EPS scores (proportion of identified
stimuli; number of interpretations; proportion of adequate interpretations; and quality
of the title). Comparing the changes which occurred in the group it can be observed that
experimental patients: increase the proportion of identified stimuli, decrease the number
of interpretations, increase the proportion of adequate interpretations, and also increase
the quality of the title. There were probably no differences in the number of errors due
to a floor effect. Taken together, the obtained results reveal that the IPT program was
effective in producing a significant positive effect on the perception and correct
interpretation of social situations in these patients, measured through the EPS.
Effect sizes defined by the difference of the baseline with the measurement point
after treatment divided by the standard deviation of the whole sample at baseline (Roder
et al., 2002) were also calculated for all measurements in the therapy group (see Table
4). The overall strongest effects were obtained on EPS measurements, all the effects
indicated improvement and, except in the ‘number of errors’, they reached the level of
large effect size. In the rest of the measurements the group has also shown some
important improvements as in: BPRS scores (anergia and total score) and DAS II scores
(free time and communication).
Additionally, the correlation (Pearson coefficient) between the scores of the two
Table 4. Effect size measurements for the therapy group
EPS
ES
Proportion of identified stimuli 1.39
Number of interpretations -1. 51
Number of errors -0. 34
Proportion of adequate interpretations 1.94
Proportion of quality title 3.05
TASS
Direct Score 0.04
Hits -0. 11
Omission 0.14
Errors -0. 46
BPRS
Anxiety / Depression
-0. 03
Though t disorders
-0. 49
Anergia
-0. 69
Activation
-0. 17
Hostility
-0. 09
Total Score
-0. 39
DAS II
Self-Care
-0. 06
Leisure time
-0. 82
Slowness
-0. 26
Communication
-0. 75
Participation in household
-0. 14
Social Contacts 0.02
Performance at work
0.03
Interest in getting a job
-0. 17
General Interest -0. 03
Emergency or crisis behavior
-0. 27
Social Adjustment Total Score
-0. 38
308
© Intern. Jour. Psych. Psychol. Ther.
S. GARCÍA, I. FUENTES, J. C. RUIZ, E. GALLACH, V. RODER.
therapists who marked the EPS was calculated to evaluate the fiability of the scores.
Correlation was high in every EPS score with ranges between 0.96 and 1.00 in both,
pre-test and post-test measurements.
DISCUSSION
Results show that the Social Perception of the patients who participated in the
programme has improved, and this fact reveals that this programme contributes to the
acquisition of social perception cognitive skills. Subjects that have received training in
Social Perception learn to collect more information (identifying more stimuli) of an
image, to make better interpretations of it and to summarise, with a title, the most
important information of it. In addition, we found that the EPS is very sensitive to the
produced changes, and that inter-observer agreement is very high. Therefore, we have
developed an instrument which can help the therapist to decide when a patient is
prepared for the next IPT programme.
Results have not shown significant differences in attention between the therapy
and control group. So, it can be assumed that the Social Perception Programme does
not improve attention capacities as we have evaluated them. In fact, another IPT
programme, the Cognitive Differentiation one, is the one orientated to improve attentional
processes, especially selective, focused and sustained attention. The intervention has
not reduced the symptoms in the schizophrenic patients. Although significant improvements
in psychopathological parameters and social role-functioning were not expected because
it was a short intervention and patients were of long illness duration, analysis of effect
sizes have shown positive changes in some scores: anergia, thought disorders, and total
score (BPRS); leisure time and communication (DAS-II).
These results are in line with the Capability of Penetration Model (Brenner,
1989). This model is based on three assumptions: (1) schizophrenics show deficits in
different functional levels of behaviour organization, (2) deficits in one level can affect
functions in other levels, and (3) different levels follow a hierarchic relation among
them. The model also affirms that an improvement in cognitive functioning has a deep
effect on all behaviour organization levels.
Our results are similar to the ones obtained by Kraemer et al. (1991) who, after
applying the Cognitive Differentiation, Social Perception and Interpersonal Problem
Solving programs, found differences in cognitive functioning but non-significant
improvements in psychopathology. So it can be confirmed that those investigations that
find differences in psychopathology and social functioning are those that use the com-
plete IPT like Brenner’s et al. (1987a), or at least four of its five programs like Vallina´s
et al. (2001).
Finally, emphasis must be made that, although IPT authors recommend to work
with patients with a minimum IQ of 85, in our investigation patients with less IQ also
benefited from the intervention. In summary, it can be stated that if only the Social
Perception Programme of the IPT is applied, chronic schizophrenics improve their
capacity to perceive and to interpret social reality.
© Intern. Jour. Psych. Psychol. Ther.
AN APPLICATION OF THE IPT IN A SPANISH SAMPLE 309
Acknowledgements
The authors would like to thank María Huertas, the AASAM and Amparo Bonora for their
help.
REFERENCES
Batlle, S. & Tomás, J. (1999). Evaluación de la Atención en la Infancia y la Adolescencia: Diseño de
un Test de Atención Selectiva y Sostenida. Estudio piloto. Revista Española de Psiquiatría
Infanto-Juvenil, 3, 142-148.
Bedell, J.R. & Lennox, S.S. (1994). The standardised assessment of cognitive and behavioral components
of social skills. In J.R. Bedell (ed.). Psychological assessment and treatment of persons with
severe mental disorders. London: Taylor & Francis.
Bellack, A.S. (1992). Cognitive rehabilitation for schizophrenia: Is it possible? Is it necessary?.
Schizophrenia Bulletin, 18, 43-50.
Bellack, A.S., Blanchard, J.J. & Mueser, K. (1996). Cue availability and affect perception in
schizophrenia. Schizophrenia Bulletin, 22, 535-544.
Brenner, H.D., Hodel, B., Kube, G. & Roder, V. (1987a). Kognitive Therapie bei Schizophrenen:
Problemanalyse und empirische Ergebnisse. Nervenarzt, 58, 72-83.
Brenner, H.D., Boker, W., Muller, J., Spichtig, L. & Wurgler, S. (1987b). On autoprotective efforts of
schizophrenics, neurotics and controls. Acta Psychiatrica Scandinavica, 75, 405-414.
Brenner, H.D. (1989). The treatment of basic psychological dysfunctions from a systemic point of
view. British Journal of Psychiatry, 155, 74-83.
Brenner, H.D., Hodel, B., Roder, V. & Corrigan, P.W. (1992). Treatment of cognitive Dysfunctions
and Behavioral Deficits in schizophrenia. Schizophrenia Bulletin, 18, 21-26.
Corrigan, P.W. & Green, M.F. (1993). Schizophrenics Patients Sensitivity to Social Cues: The Role of
Abstraction. American Journal of Psychiatry, 150, 589-594.
Frith, C.D. (1995). La esquizofrenia. Un enfoque neuropsicológico cognitivo. Barcelona: Ariel.
García, S. (2003). Rehabilitación de enfermos mentales crónicos: Entrenamiento en Percepción So-
cial. Trabajo de Investigación. Departamento de Personalidad, Evaluación y Tratamientos Psi-
cológicos. Universidad de Valencia.
Halford, W.K. & Hayes, R. (1991). Psychological rehabilitation of chronic schizophrenic patients:
recent finding on social skills training and family psychoeducation. Clinical Psychology Review,
11, 23-44.
Hodel, B. & Brenner, H.D. (1994). Cognitive therapy with schizophrenic patients: conceptual basis,
present state, future directions. Acta Psychiatrica Scandinavica, 90, suppl 384, 108-115.
Ibáñez, T. (1979). Factores sociales de la percepción. Hacia una psicosociología del significado. Cua-
dernos de Psicología, 1, 71-81.
Jimeno, N., Jimeno, A. & Vargas, M.L. (1996). El Síndrome psicótico y el Inventario de Frankfurt.
Conceptos y resultados. Barcelona: Springer.
Kraemer, S. (1991). Cognitive training and social skills training in relation to basic disturbances in
chronic schizophrenic patients. In C.N. Stefanis (ed.). Proceedings of the World Congress of
310
© Intern. Jour. Psych. Psychol. Ther.
S. GARCÍA, I. FUENTES, J. C. RUIZ, E. GALLACH, V. RODER.
Psychiatry. Amsterdam: Elsevier.
Leff, J. & Abberton, B. (1981). Voice pitch measurements in schizophrenia and depression. Psychological
Medicine, 11, 849-852.
Lukoff, D., Nuechterlein, K.H. & Ventura, J. (1986). Manual for Expanded Brief Psychiatric Rating
Scale (BPRS). Schizophrenia Bulletin, 12, 594-602.
Montero, I., Bonet, A., Puche, E. & Gómez Beneyto, M. (1988). Adaptación española del DAS-II
(Disability Assesment Shedule). Psiquis, 175, 17-22.
Morrison, R.L., Bellack, A.S. & Mueser, K.T. (1988). Deficits in facial-affect recognition and
schizophrenia. Schizophrenia Bulletin, 14, 67-83.
Organización Mundial de la Salud (1992). CIE-10. Trastornos Mentales del Comportamiento. Ma-
drid: Meditor.
Penadés, R. (2002). La Rehabilitación neuropsicológica del paciente esquizofrénico. Tesis Doctoral.
Departamento de Psiquiatría y Psicobiología Clínica. Universidad de Barcelona.
Penn, D.L., Comb D. & Mohamed, S. (2001). Social Perception in Schizophrenia. In P.W. Corrigan &
D.L. Penn (Eds.), Social Cognition and Schizophrenia. Washington: American Psychological
Association.
Pérez, M. & Fernández, J.R. (2001). El grano y la criba de los tratamientos psicológicos. Psicothema,
13, 523-529.
Roder, V., Studer, K. & Brenner, H.D. (1987). Erfahrunger mit einem intergrierten psychologischen
therapieprogramm zum training kommunikativer und kognitiver fahigkeiten in der rehabilitation
schwer chronisch schizophrener patienten. Schweizer Archiv Fur Neurologie und Psychiatrie,
138, 31-44.
Roder, V., Brenner, H.D, Muller, D, Lachler, M., Muller, R. & Zorn, P. (2002). Social skills training for
schizophrenia: Research update and empirical results. In H. Kashima., I.R.H. Falloon., M.
Mizuno, & M. Asai (Eds.), Comprehensive Treatment of Schizophrenia. Tokyo: Springer.
Roder, V., Brenner, H.D., Hodel, B. & Kienzle, N. (1996). Terapia Integrada de la Esquizofrenia.
Barcelona: Ariel.
Süllwold, L. & Huber, G. (1986). Schizophrene basisstörungen. Berlin: Springer.
Toomey, R., Wallace, C.J., Corrigan, P.W., Schulderg, D. & Green, M.F. (1997). Social processing
correlates of nonverbal perception in schizophrenia. Psychiatry, 60, 292-300.
Vallina, O., Lemos, S., Roder, V., García, A., Otero, A., Alonso, M. & Gutiérrez, A.M. (2001). Controlled
study of an integrated psychological intervention in schizophrenia. The European Journal of
Psychiatry, 15, 167-179.
Vallina, O. & Lemos, S (2001). Tratamientos psicológicos eficaces para la esquizofrenia. Psicothema,
13, 345-364.
World Health Organization (1985). A procedure and schedule for assessment of disability in patients
with severe psychiatric disorders. Disability Assessment Schedule-DAS-II. Geneva: WHO.
Wykes, T. (2000). Cognitive rehabilitation and remediation in schizophrenia. In T. Sharma & P. Arvey
(eds). Cognition in Schizophrenia. New York: Oxford University Press.
Received September 10, 2003
Final acceptance November 13, 2003
