
The Evidence-Based
Practice Center
Dr. Barbara Mayer, PhD, RN
Executive Director, Professional Practice and
Clinical Improvement
Director, Evidence-Based Practice Center
Clinical Assistant Professor
Improving QI Capability

Evidence-Based Practice
Studies show that when practice is based on empirical
evidence, variations in care that can lead to errors and
missed or inappropriate interventions are reduced,
resulting in:
Improved
patient
outcomes
Reduced
healthcare
costs
Safer, more
efficient care
Optimal use
of resources
Individualized
patient care

Evolution of Evidence-Based Practice
0
100000
200000
300000
400000
500000
600000
700000
800000
1990
1991
1992
1993
1994
1995
1996
1997
1998
1999
2000
2001
2002
2003
2004
2005
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
2019
2020
2021
2022
8,754,036
Guyatt supports
evidence in clinical
decision-making
Cochrane
Collaboration
founded
Sackett defines
EBP
AHRQ EBP Center
Program
established
IOM identifies EBP
as core
competency
1991
1996
1993
1997
2003
2009
IOM goal - 90%
clinical decisions are
evidence-based
EBP Publications
(PubMed)

"Evidence based medicine is the conscientious,
explicit, and judicious use of current best evidence
in making decisions about the care of individual
patients. The practice of evidence-based medicine
means integrating individual clinical expertise with
the best available external clinical evidence from
systematic research."
Sackett, DL, et al. BMJ
1996;312(7023):71-2.
individual clinical expertise
external clinical evidence

Best
Available
Evidence
Clinician
Expertise
Patient
&
Context
Clinically relevant
Sound
methodology
Highest level
available
Education
Experience
Clinical skills
Patient values and
circumstances
Local resources
A way of providing healthcare that is guided by integration of the best
available scientific knowledge, clinical expertise and patient preferences to
correctly identify the clinical problem, apply the most effective
interventions, and re-evaluate outcomes for future improvement. (AHRQ)

Examining our own practice
“Work arounds”
to bypass
barriers.
Our nursing
practice is often
based tradition
rather than
evidence.
We’ve
always done
it this way
I don’t have
time to do
that

Inadequate resources
Lack of dedicated clinician time
Lack of understanding of EBP
Absence of evidence
implementation skills
Not highly prioritized by
organization
Lack of leadership support
Literature Review:
Barriers to
Evidence
Implementation

Literature Review:
Characteristics of
an EBP
Environment
A culture where inquiry is valued
EBP is recognized as a core competency
Leaders who role-model and support EBP
There is a shared model and process for
implementation of EBP
Experiential education programs are offered
EBP implementation projects focus on frontline
clinical practice and align with organizational
priorities
There is coaching and support from a nurse
scientist & clinical nurse specialists
Dissemination is encouraged and opportunities
exist within the organization

Gap Analysis
+/-
+/-
+/-
Executive leader support for EBP
A culture where inquiry is valued
EBP implementation projects focus on frontline clinical
practice and align with organizational priorities
There is coaching and support from a nurse scientist & clinical
nurse specialists
Formal organizational structure to oversee EBP
EBP is recognized as a core competency
There is a shared model and process for implementation of EBP
Dissemination is encouraged and opportunities exist within the
organization
Experiential education programs are offered

ACIS Project
Supporting
Evidence-Based
Practice in
Nursing
Aim
Create a formal structure and defined
processes to facilitate and oversee
adoption of evidence-based practices.

Goals
Ensure excellence in
nursing practice
Create structures and
processes that encourage
critical inquiry
Support staff in evaluating
practice, identifying gaps,
and implementing the
best available evidence
Use an implementation
Science approach

Administrative Structure
The EBP Center is
overseen by a governing
board of clinical experts,
operational leaders, and
bedside staff. The Board
provides direction for the
Center, setting policy and
priorities in alignment
with organizational goals.

Administrative Structure
The EBP Center is
overseen by a governing
board of clinical experts,
operational leaders, and
bedside staff. The Board
provides direction for the
Center, setting policy and
priorities in alignment
with organizational goals.
Professional Practice and Clinical
Improvement
Executive Director
Implementation
Scientist
EBP Center
Coaches

Culture
Shared Governance Councils
EBP language and principles
are embedded in key
organizational documents
Nursing leadership is
committed to providing
resources to support EBP
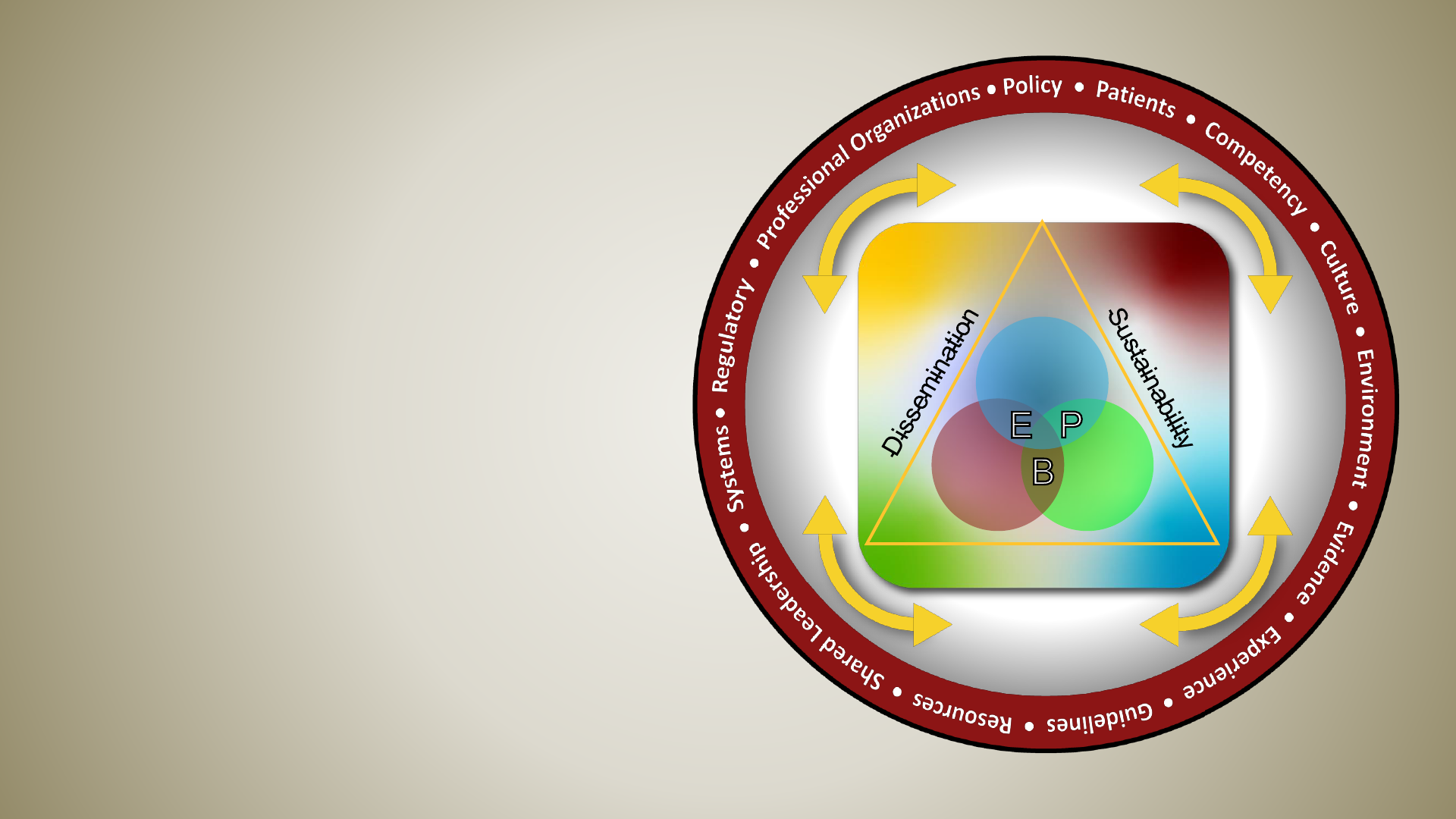
Structure: EBP Model
The EBP Model provides a graphic
representation of the interaction
between the elements of evidence-
based practice; caring science,
ethics, Magnet, and professional
practice; structures within the
organization; and the influence of
implementation science on
sustainable outcomes

Process: Implementation Framework
Find & appraise the
evidence
Assess practice gaps
Develop
Implementation Plan
Apply the Evidence Evaluate the results
Sustain and
Disseminate
Implementation Framework
Ask the question
6/21/23(rev)
TOOLS
• Poster templates
TOOLS
• Run charts
• Control charts
• Pareto charts
TOOLS
• SMART Goal worksheet
• Ishikawa diagram
• Whysworksheet
• I/O Grid
• Driver Diagram
TOOLS
• PICO worksheet
• IRB decision tool
• A3
Identify the practice issue or
problem
A3
Problem & background
statements
A3
PICO question
Is this research
or QI?
A3
Process map current state
Identify search terms
Perform search
Select articles for review
Critically appraise articles
Create evidence table
Describe future state
A3
Process map future state
Perform Gap Analysis
Compare current state &
future state process maps
A3
SMART Goal
A3
Action plan
Are there potential barrier?
What prep will staff require?
What resources are required?
Baseline data?
Identify process, outcome, and
implementation science
measure(s)
Manage the process, adhere to
plan
Ensure data is collected as
planned
Communicate progress to key
stakeholders and end users
Analyze the data
A3
Data/Results
Discuss data analysis with key
stakeholders
Proposed action?
Adopt and spread
the change
Adapt and
re-test
Abandon and try
new action
Determine sustainability plan
How will you disseminate
results
What will you measure to
ensure adoption of
intervention?
TOOLS
• REDcap
• Change process
TOOLS
• Librarian
• Critical appraisal tool
• Evidence table template
• Reference management software
A3
Sustainability plan
QI?
Continue to next
step
Research?
STOP!
Contact ORPCS
TOOLS
• SBAR template
Identify Key Drivers
Develop data collection tool(s)
PLAN
ACTDO
STUDY
EBP PROCESS
Synthesize the evidence
A3
Key Drivers
Considerations?
Get leadership and staff buy-in
Identify actions to address key
drivers
Create timeline
Formulate recommendation
The
Implementation
Framework
incorporates the
PDSA cycle and
change process to
provide clinicians
with a step-by-step
guide.

Clinical Nurse
UNDERSTAND the EBP model and concepts of
evidence-based practice
EBP Fellows
SUPPORT EBP through evidence implementation
EBP Coaches
FACILITATE EBP through the synthesis of
evidence
Leadership Team
PROMOTE EBP by ensuring availability of
tools and resources
Behaviors
Practice evidence-based nursing
Question practice; ask why
Identify improvement opportunities
Behaviors
Promote concepts of EBP throughout SHC
Encourage a culture of inquiry
Be aware of emerging practice changes
Evaluate current practice and identify
opportunities for improvement
Mentor clinical staff in EBP
Serve as EBP project leader
Behaviors
Mentor others
Serve as faculty
Contribute to development of strategic &
operating plans
Behaviors
Ensure availability of resources
Engage SHC leadership
Develop Center strategic plan
Represent Center internally and
externally
Roles and Responsibilities

Resources
QI/EBP Toolkit
Tools & templates designed to
guide project leader through the
implementation process
Coaching &
Consultation
Clinical Nurse Specialists
Nursing Quality Coordinators
Assistance with:
Developing PICO
question
Literature searches
Implementation
planning and execution
Website

OVID Synthesis

FACT SHEET
Nurse Residency Program
Nurse Residents are provided 20 hours of didactic content
and practical application. Residents are assigned to a
group and provided an EBP Coach to guide them through
completion of a literature review based on a PICO
question developed by the group.
Content is based on the Stanford EBP Model and
Implementation Framework and focuses on the EBP
process. Resulting literature reviews are available in OVID
Synthesis Clinical Evidence Manager for later
implementation.
The Nurse Residency program is a 12-month program aimed at
preparing newly graduated registered nurses for independent
practice art Stanford.
Incorporated into the program, Residents learn the principles
of evidence-based practice and quality improvement processes
and complete a literature review on topics curated by the
Professional Practice and Clinical Improvement department.
Completed projects are presented during Nursing Grand
Rounds and other relevant venues and are posted on the EBP
Center website.
These EBP literature reviews serve as one pipeline into the
mission of the EBP Center to ensure all nursing practice is
based on the best available evidence.
EBP@stanfordhealthcare.org

FACT SHEET
The S.C.I.E.N.C.E. Fellowship provides support for
direct care nurses wanting to implement solutions to
pressing clinical practice issues. The program
combines didactic learning with practice application of
EBP principles and QI processes. Fellows are expected
to disseminate project results by:
EBP Fellowship Program
The 8-month Fellowship provides 12 hours of paid time per month which includes
48 hours of didactic content. Each candidate is assigned a coach for the duration of
their project, along with a laptop computer and access to the OVID Synthesis
Clinical Evidence Manager.
Using the Stanford EBP Model and Implementation Framework, Fellows learn how
to perform a literature review and analysis, implement an evidence-based practice,
present their findings, and sustain change.
Presenting during Nurse Week and/or other
internal venues
Writing a project summary to be included in
the Looking Forward Newsletter and posting
on the Center website
Submitting an abstract to a regional or
national meeting and presenting if accepted
EBP@stanfordhealthcare.org
Eligible Candidates will:
Be a Clinical Nurse, Nurse Coordinator or similar role, at Stanford Health Care for
at least 1 year, and in good standing.
Attend all to scheduled classes, EBP meetings and coaching sessions
Have a feasible EBP project idea that can be completed within the program
duration
Comply with program requirements for project dissemination
Application Process
Obtain a letter from your Manager to support full participation and the ability to
schedule 4 hours per week for the EBP project
Complete and submit an online application by Monday, August 14, 2023 using
the link or QR code.
https://app.smartsheet.com/b/form/a292b138d18f4ecca7784e6c59892432
Program Participation
EBP Fellowship NRP
# Cohorts* 2 3
# Participants 5 246
# projects 5 40
Number participants in training programs and number
projects produced (EBP = evidence
-based practice; NRP =
nurse residency program)
*New cohorts for both the Fellowship and NRP programs
will begin this Fall.

Examples of Project Topics
✓ Using pictograms to improve patient recall of discharge medication
administration times.
✓ Improving timely image upload in Hepatic Cancer Clinic patients prior to first
clinic visit.
✓ Reduce the number of unnecessary peripheral IV insertions using a standard
algorithm.
✓ Probiotics for Prevention of Constipation in Oncology Patients Receiving
Chemotherapy
✓ Weight Based Fluid Status Evaluation Versus I&O on ICU Patients
✓ Comparison on the Postoperative Effects of Incentive Spirometry and Deep
Breathing
✓ Outcomes of Proactive Toileting on Fall Prevention

Formalize process for practice evaluation
Continue to refine our EP Model
Expand EBP Center to our sister hospital and
outpatient clinics
Increase frequency of educational offerings
Expand eligibility for Fellowship program to other
disciplines
Seek philanthropic funding/endowment to ensure
sustainability of Center and programs
Build a more robust website
Summary
Future of the EBP Center
Select References
1. Bissett, K., et al.. (2016). Improving Competence and Confidence With Evidence-Based Practice Among Nurses. Journal for Nurses
in Professional Development;32(5):248-255.
2. Breckenridge-Sproat ST, Throop MD, Raju D, Murphy DA, Loan LA, Patrician PA. (2015). Building a Unit-Level Mentored Program to
Sustain a Culture of Inquiry for Evidence-Based Practice. Clin Nurse Spec; Nov-Dec;29(6):329-37.
3. Gallagher-Ford, L., et al. (2020). The effects of an intensive evidence-based practice educational and skills building program on EBP
competency and attributes. Worldviews Evid Based Nur's;17(1):71-81.
4. Nelson-Brantley, H. & Chipps, E. (2021). Implementation Science and Nursing Leadership: Improving the Adoption and
Sustainability of Evidence-Based Practice. JONA: The Journal of Nursing Administration,;51(5):237-239.
5. Nelson-Brantley, H. & Chipps, E. (2023). Implementation Science for the Practice-Oriented Nurse Leader. Nursing Administration
Quarterly, 47 (2), 107-117.
6. Newhouse RP. (2007)Creating infrastructure supportive of evidence-based nursing practice: leadership strategies. Worldviews Evid
Based Nurs:4(1):21-9.
7. Reynolds, S. & Granger, B. (2023). Implementation Science Toolkit for Clinicians. Dimensions of Critical Care Nursing; 42(1): 33-41.
8. Selig PM, Lewanowicz W. (2008). Translation to practice: developing an evidence-based practice nurse internship program. AACN
Adv Crit Care. Jul-Sep;19(3):325-32.
9. Stanley T, Sitterding M, Broome ME, McCaskey M. (2011). Engaging and developing research leaders in practice: creating a
foundation for a culture of clinical inquiry. J Pediatr Nurs. Oct;26(5):480-8.
10. Tucker, S, et al. (2021) Implementation Science: Application of evidence-based practice models to improve healthcare quality.
Worldviews Evid Based Nur’s;18(2):76-84.

