
EVALUATION OF THE INDIANAPOLIS MOBILE CRISIS ASSISTANCE TEAM
Report to the Indianapolis Ofce of Public Health & Safety and the Fairbanks Foundation
MARCH 2018
CENTER FOR CRIMINAL JUSTICE RESEARCH
HORIZONTAL VERSION
CENTER FOR CRIMINAL JUSTICE RESEARCH
VERTICAL VERSION
AUTHORS
Katie Bailey, Program Analyst, IU Public Policy Institute
Brad Ray, Director of the Center for Criminal Justice Research

334 N Senate Avenue, Suite 300
Indianapolis, IN 46204
policyinstitute.iu.edu
CENTER FOR CRIMINAL JUSTICE RESEARCH
HORIZONTAL VERSION
CENTER FOR CRIMINAL JUSTICE RESEARCH
VERTICAL VERSION
CONTRIBUTING AUTHORS
Eric Grommon, Senior Research Associate, IU Public Policy Institute
Evan Lowder, Research Associate, IUPUI School of Public & Environmental Affairs
Staci Rising Paquet, Research Assistant, Center for Criminal Justice Research
RESEARCH SUPPORT
Spencer Lawson, Research Assistant, Center for Criminal Justice Research
Joti K. Martin, Program Analyst, IU Public Policy Institute
Elle Yang, Graduate Research Assistant, IU Public Policy Institute

CONTENTS
EXECUTIVE SUMMARY
KEY FINDINGS
BACKGROUND
LITERATURE REVIEW
INDIANAPOLIS MOBILE CRISIS ASSISTANCE TEAM
STUDY DESIGN
Focus Groups
Interviews with Stakeholders
Field Observations
OfcerSurvey
MCAT Response Data
BARRIERS AND FACILITATORS TO MCAT IMPLEMENTATION
Barriers to Program Implementation
Policies and Procedures
External Coordination
Outpatient Resources
RoleConictandStigma
Facilitators to Program Implementation
Initial Citywide Collaboration and Buy-In
Information Sharing
Team Building
IMPD EAST DISTRICT OFFICER SURVEY
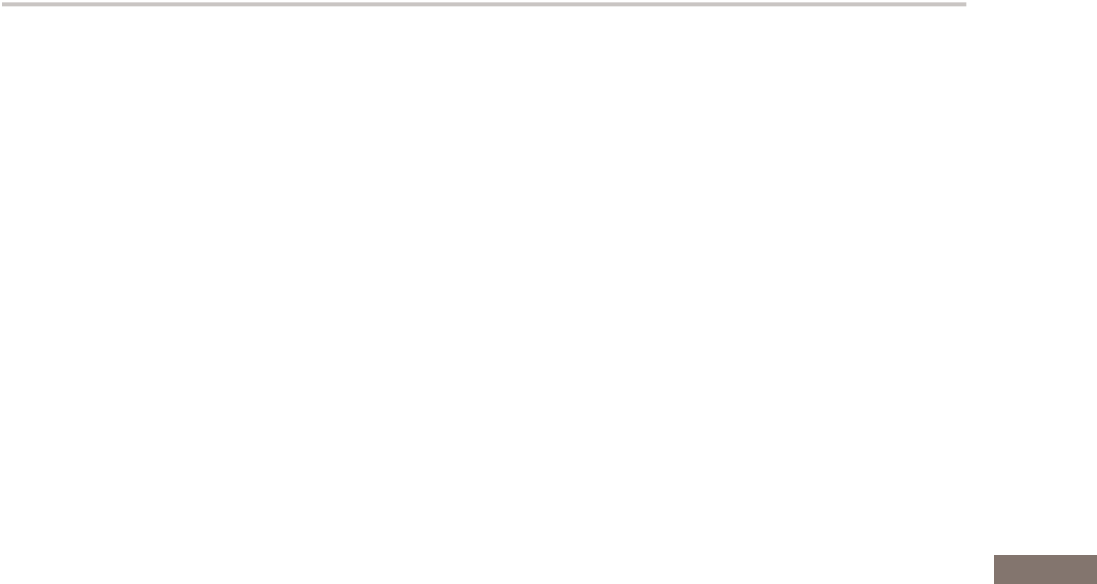
Exhibit 1: Clarity of Roles and Expectations of the MCAT Unit
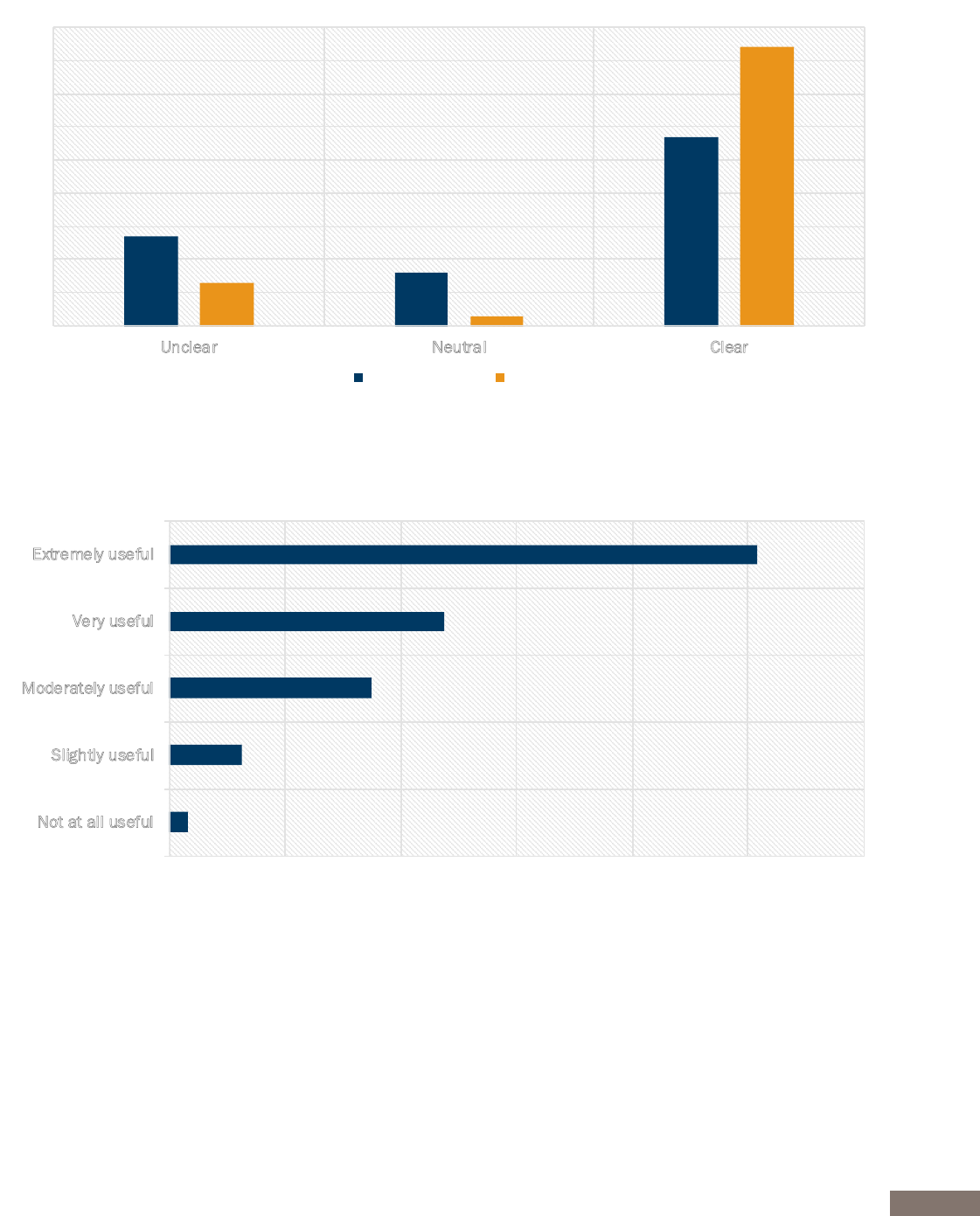
Exhibit 2: Perceptions of MCAT Usefulness
QUANTITATIVE DATA ON MCAT RESPONSES
Client Demographics
Exhibit 3: Demographic Characteristics of MCAT Response Cases
Reason for Response
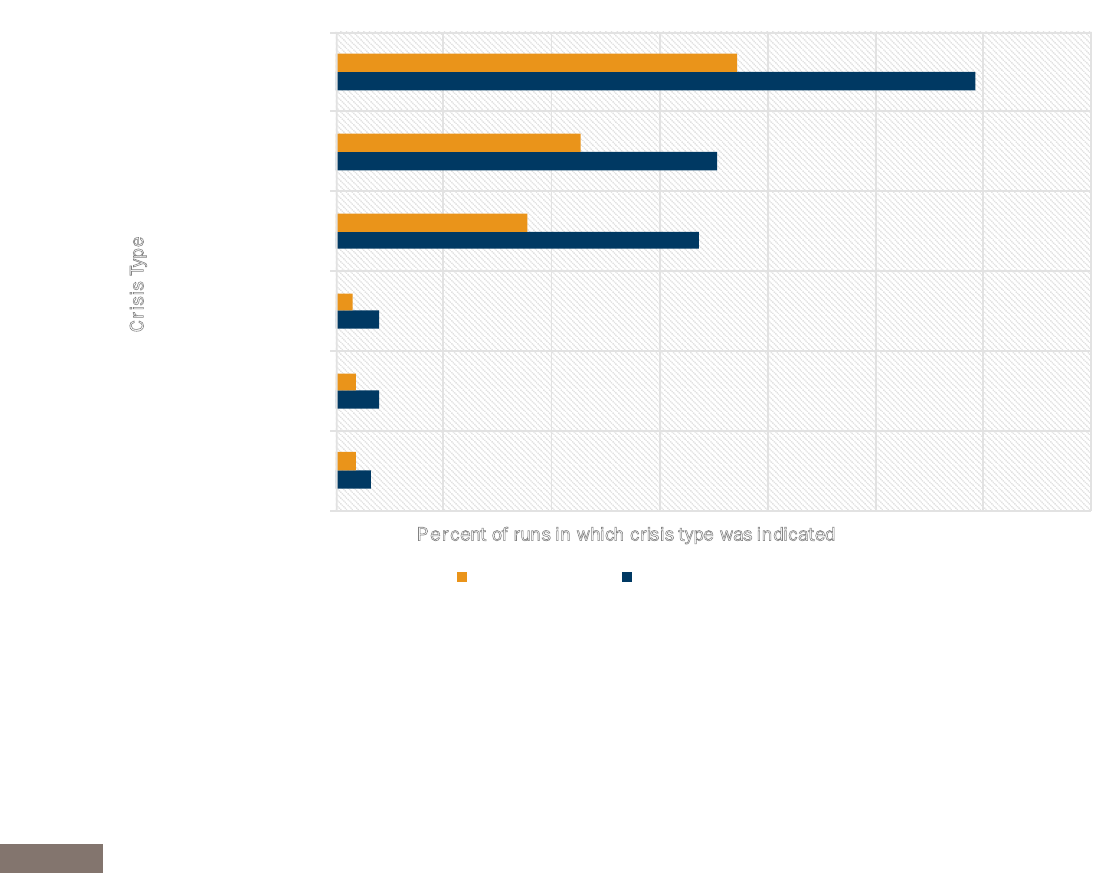
Exhibit 4: Reasons for MCAT Response
Exhibit 5: MCAT Response Types over Time
Scene of an MCAT Response
MCAT Response Outcomes
Exhibit 6: MCAT Response Outcomes
Repeat Encounters
Exhibit 7: MCAT Repeat Encounters
Differences by MCAT Units
Exhibit 8: Variation by MCAT Units
CONCLUSIONS AND FUTURE RESEARCH
REFERENCES
1
1
2
3
5
6
6
7
7
7
7
8
8
8
8
9
10
11
11
12
13
13
14
14
16
16
16
17
17
18
18
19
19
19
20
20
21
22
24

1
In May 2016, Indianapolis Mayor Joe Hogsett formed the Criminal Justice Reform Task Force to address,
amongotherissues,thesignicantnumberofindividualsenteringthecriminaljusticesystemwithmentalhealth
or substance abuse issues. This resulted in the establishment of a Mobile Crisis Assistance Team (MCAT) pilot
program that integrated police, paramedics and mental health professionals into teams to respond to emergency
calls involving people with behavioral health and/or substance use issues. The pilot program aimed to divert
thosepeopletomentalhealthandsocialservicesinsteadofthecriminaljusticesystem,andtorelieveother
rst-respondersfromthesceneofthesetime-consumingandcomplicatedemergencysituations.TheMCATpilot
began in the Indianapolis Metropolitan Police Department (IMPD) East District.
The Center for Criminal Justice Research at the Indiana University Public Policy Institute evaluated the pilot
program using data from MCAT run reports between August 1 and December 9, 2017. Additionally, East District
IMPDofcersweresurveyed,keystakeholdersandprogramdesignerswereinterviewed,focusgroupswere
heldwiththeMCATteammembers,andeldobservationswerecompleted.
EXECUTIVE SUMMARY
• MCATtransportedapersontojailinlessthan2%ofallresponsesduringthepilot
• MCATunitswereabletorelieveoneormoreotherrstresponseunitsfromthesceneofan
emergency in two-thirds of all runs during the study period
• ThemajorityofMCATencounterswerecompletedinunder90minutes-Inencountersthat
tooklongerthan90minutes,MCAThadrelievedotherrstresponseunits80%ofthetime
• MCATunitsencounteredasmallsubsetof“frequentyers”—individualsreceivingmultiple
MCATresponsesduringthestudyperiod—whoweremorelikelytobegravelydisabledand/
or have mental health issues than those who had only received one MCAT response
• Eighty-vepercentofIMPDEastDistrictpoliceofcerssurveyedindicatedtheMCATunitwas
very useful or extremely useful to them as an additional resource in responding to emergencies
• One-thirdofIMPDEastDistrictpoliceofcerssurveyedindicatedbeinginterestedinserving
asanMCATofcerinthefuture
• A lack of outpatient treatment options and clear policies and procedures appeared as the
most salient barriers to implementation of the MCAT pilot program
• Access to and triangulation of collaborating agency information on persons experiencing
emergencies;supportfromcityofcials;andteambuildingexercisesduringMCATtraining
emerged as the most salient facilitators to implementation of the MCAT pilot program.
KEY FINDINGS

2
AccordingtotheMarionCountySheriff’sOfce,approximately40%ofdetaineesinMarionCounty’sjailsat
any one time suffer from mental illness, resulting in $8 million of medical care and services annually (McQuaid,
2015). In addition, roughly 85% of detainees with a mental illness are also diagnosed as suffering from
substanceabuseissues(McQuaid,2017).Thepastveyearshaveshownanalarmingincreaseinpoliceand
emergency medical service runs involving individuals suffering from mental illness and drug addiction. Although
lawenforcementexpertsestimatethatasmanyas 7%to10%ofpatrolofcerencountersinvolvepersons
withmentalillness,historicallypoliceofcersreportfeelingillequippedtorespond(Deane,Steadman,Borum,
Veysey, & Morrissey, 1999).
In May 2016, Indianapolis Mayor Joe Hogsett formed the Criminal Justice Reform Task Force. In December of
thatyear,theTaskForceissuedacomprehensiveplanforcriminaljusticereformthatincluded,amongother
initiatives,divertingpersonssufferingfrommentalillnessandaddictionawayfromthecriminaljusticesystem
and into evidence-based treatment and services, when appropriate.
This resulted in the establishment of a Mobile Crisis Assistance Team (MCAT) pilot program, an integrated
co-responding police-mental health team model with the addition of a medical professional. The MCAT pilot
began August 1, 2017 with four teams operating within the boundaries of the Indianapolis Metropolitan Police
Department(IMPD)EastDistrict.TheMCATteamsconsistofspecially-trainedpoliceofcers(IMPD),paramedics
from Indianapolis Emergency Medical Services (IEMS), and crisis specialists from Eskenazi Health Midtown
Community Mental Health (Midtown). The pilot program aimed to divert time-consuming, challenging, and
complicated pre-arrest situations to a dedicated, specially-trained team that could better assess and engage
individuals,routingthemtomentalhealthandsocialservicesinsteadofthecriminaljusticesystem.
TheIndianapolisOfceofPublicHealthandSafetypartneredwiththeIndianaUniversityCenterforCriminal
Justice Research (CCJR) of the Indiana University Public Policy Institute (PPI), to provide an evaluation of the
MCAT pilot program. This evaluation was based on an expansion design where evaluators used a mixed-methods
approach to extend the scope, breadth, and range of inquiry (Greene, Caracelli, & Graham, 1989). In this
approach, qualitative methods are generally used to assess program implementation and quantitative methods
to assess program outcomes. For the MCAT evaluation, qualitative data collection included: focus groups with
MCATunits,interviewswithkeyprogramdevelopersandcommunitystakeholders,eldobservationswithan
MCATunit,andasurveyofEastDistrictpoliceofcers.QuantitativeanalysisexaminedMCATresponsedata
provided by MCAT units. The primary purpose of qualitative data collection was to better understand barriers
and facilitators to program implementation, while quantitative data points from MCAT runs were developed
using a program-theory approach whereby the measures captured are based on stakeholder beliefs regarding
the important outcomes of the pilot program.
This report begins by providing an overview of the academic literature on the challenges presented by persons
withamentalillnessandco-occurringsubstanceusetopoliceofcersandthecriminaljusticesystemasawhole,
along with efforts to mitigate these challenges. Next, this report describes the MCAT pilot program in greater
detail before presenting the study design and results. Implications for research and future pilot programs are
discussed.
BACKGROUND

3
Sincethe1970s,personswithmentalillness(hereafter,“PMI”)havebeenhandledincreasinglybythecriminal
justicesystem,aprocessreferredtoasthe“criminalizationofmentally-disorderedbehavior.”Manysuspect
that deinstitutionalization contributed to increases in the incarceration of PMI (Lamb & Grant, 1982; Stelovich,
1979; Swank & Winer, 1976; Whitmer, 1980), as these individuals were no longer in hospitals, but out in the
communityandatriskofarrest(Whitmer,1980).Today,PMIarethreetimesmorelikelytobeinjailorprison
thaninahospitalreceivingappropriatetreatment(Taheri,2016).Thisislargelybecausethecriminaljustice
system is the only social institution that cannot turn away these cases. Private centers can refuse to treat patients
theydeemtoberiskyordisruptive;communitymentalhealthproviderscanrejectthosewhohaveacriminal
history; and hospitals can turn away those who appear threatening or intoxicated.
Criminal justice systems across the country have responded by developing programs aimed at reducing
incarceratedPMIbydivertingthemawayfromthecriminaljusticesystemandintocommunity-basedtreatments
andservices.Servicesprovidedbymanyoftheseprogramsoccur“post-booking”(e.g.,mentalhealthcourts)
and can only be accessed once an individual has been arrested or charged with a crime. Many studies suggest,
however,thatthemosteffectivewayofdivertingPMIfromthecriminaljusticesystemisbyintervening“pre-
booking”aspoliceofcersrespondto911emergencycalls(Muntez&Grifn,2006).
Approximately 10% of law enforcement encounters involve PMI, about three quarters of whom have co-
occurringsubstanceusedisorders(Steadman,2005;Skubbyetal.,2013).Often,policeofcersdon’thave
the resources or training to handle mental health crises effectively, or the people who experience them. During
these encounters, PMI in crisis can exhibit strange or hostile behavior, creating a situational ambiguity that can
compromisethesafetyofofcers(Taheri,2016).Oneofthemostpopularresponsestothisissuehasbeenthe
implementationofCrisisInterventionTraining(CIT),wherepoliceofcersaretrainedaboutmentalillnessand
how to respectfully and safely interact with PMI (Dupont, Cochran, & Pillsbury, 2007; Compton, Bahora, Watson,
&Oliva,2008).Additionally,CITcurriculumalsoprovidestrainingforofcersonco-occurringmentalhealthand
substance use disorders that as many as three quarters of PMI experience (Steadman, 2005; Dupont, Cochran,
&Pillsbury,2007).EmpiricalevidenceonCIThasbeenencouragingandsuggeststhatCIT-trainedofcershave
more positive attitudes, beliefs, and knowledge about mental illness, and agencies with CIT programs have lower
arrest rates than other types of diversion programs (Compton, et al., 2008).
Even with the emergence of CIT programs, police agencies struggle to engage with PMI safely in the communities
they serve. To this end, several police departments have partnered with community healthcare providers to
create co-responding police-mental health teams, known alternatively as mobile crisis intervention teams, crisis
outreach and support teams, and ambulance and clinical early response teams (Shapiro et al., 2014). The
generalco-responseteammodelinvolvespartneringaswornpoliceofcerwithamentalhealthprofessional,
although many agencies create three-person teams by adding a medical professional (such as a nurse or
paramedic) or a peer specialist (such as an individual in recovery from mental illness or substance use disorder)
(Hay, 2015). Dozens of such teams currently operate in North America from Los Angeles, California to Halifax,
NovaScotia,andhaveseveralcommongoals,includingdivertingPMIawayfromthecriminaljusticesystemand
increasing consumer access to mental health and substance abuse treatment (Steadman et al., 2001; Shapiro
et al., 2014). However, one important distinction among these co-responding units is the timing of the response:
LITERATURE REVIEW

4
someunitsarerstresponderstothesceneofanemergencywhileotherunitsprovidefollowupafteramental
health or substance abuse crisis.
As these co-response programs are relatively new, only a handful of studies have examined the effectiveness of
thisapproach,thoughresultshavebeengenerallypositiveinndingthatco-responseteamsarecosteffective,
well-receivedbythecommunitiestheyserve,andreduceburdensonthecriminaljusticeandhealthcaresystems.
For example, a 2005 program evaluation of Victoria City (Canada) Police Department’s Integrated Mobile Crisis
Response Team found many positive outcomes, including increased crisis call response rates, decreased reliance
on hospital emergency rooms, and increased information sharing between agencies. The ndings, however,
suggesttheseoutcomesdependedonadequatestafng,appropriatevehicles,sufcientteammembertraining,
a centralized dispatch location, and access to pertinent medical and criminal histories about the PMI served
(Baess, 2005). In 2006, Hartford and colleagues used a mixed-methods approach and reviewed over seven
studiesandftytwopolicedepartmentsurveysfromthreecontinentsaboutpre-bookingdiversionprograms
(includingco-responding police-mental healthteams) and identiedfourkeyelementsthat wereassociated
with positive outcomes: involving all agencies in the program’s development, conducting regular meetings with
program stakeholders, creating a 24/7 no refusal policy for drop off centers, and appointing an individual to
act as a liaison between all agencies involved. A similar 2014 review by Shapiro and colleagues of over twenty
peer-reviewed studies, reports, and dissertations on co-response teams suggested that successful teams created
important bonds between PMI and community mental health resources while lessening the burden on the criminal
justicesystembymakingfewerarrestsandreducingtimeonsceneforrstresponders.
Finally, an evaluation of a mobile police-mental health crisis team in an urban setting by Kirst and colleagues in
2015 found that stakeholders felt that the program was meeting its goals of reducing criminalization of mental
illness and assisting PMI in crisis via positive partnerships between individual team members and their respective
agencies. Despite positive outcomes, however, several barriers to co-response program implementation are
consistently reported throughout the literature. Most importantly, all studies have reported that the lack of
a 24/7 psychiatric drop off location center with a no-refusal policy is a critical barrier to program success.
Additionally, there are recurring issues with role clarity and differences in professional cultures between team
membersascontributingtoimplementationdifculties.

5
TheIndianapolisMCATpilotprojectlaunchedonAugust1,2017asapolice-mentalhealthco-responseteam
modelwiththeadditionofamedicalprofessional.TheIndianapolispilotmodelconsistsofanIMPDpoliceofcer,
an IEMS paramedic, and a mental health clinician from Midtown. MCAT is based in and serves the IMPD East
District. This district was chosen because it ranks high on the Social Disorder Index and has high rates of mental/
emotional911callsandambulancerunsformedicalemergencies.Eachentityinvolvedidentiedacoordinator
withinitsleadershiptodesignandimplementtheMCATprograminconcert.Theseofcialcoordinatorsdeveloped
andimplementedtraining,identiedteammembersfromtheirrespectiveagencies,andmadeproceduraland
logistical decisions with support from the Ofce of Public Health and Safety. In preparation for launch, a
business associate agreement between the Health and Hospital Corporation of Marion County, of which IEMS
and Midtown are part, and IMPD was created to protect personal health information of those with whom the
MCAT teams come in contact.
FourMCAT unitswereformed forthe pilotproject,each working in12-hour shifts,resultingin 24/7 MCAT
availability. MCAT members have unique uniforms identifying them as both MCAT personnel and members of
their respective agencies. The teams operate out of a non-emergent van with an MCAT logo on the outside. Each
teammemberutilizestheirownlaptoptoaccessnecessaryagency-specicinformationandtheMCATvehicle
isadditionallyequippedwithamedicalequipmentbag,automatedexternaldebrillatorandstandardissued
IMPDequipment.MCATmaytransportindividualstoanemergencydepartment,otherassessmentcenter,orjail
when deemed appropriate.
OneaspectoftheMCATthatisespeciallyimportanttonoteisthatitisprimarilyarst-responseunit,nota
follow-upunit.Thus,theMCATmayrespondtothesceneofacrisisattherequestofotherrst-responders,
or self-dispatch upon hearing of a relevant crisis via IMPD or IEMS dispatch radio. However, when necessary,
MCAT may also conduct follow-ups with individuals they previously encountered to encourage linkage with
services.TherolesofMCATteammembersareuidtoallowforthemtoresponddynamically,butgenerally
theofcersensuresecurityatthescene;cliniciansfacilitatementalhealthassessmentsandtreatmentlinkage;
and paramedics address any medical issues, check patient vitals, and perform assessments related to substance
usesymptomswhennecessary.Ofcersandparamedicsareauthorizedtomaneuverthevehicleandanyofthe
three team members may input information regarding runs into the electronic data collection system.
The mission of the MCAT pilot program is to provide a real-time response to individuals in crisis by facilitating
assessment, triage, and linkage with appropriate services. In doing so, MCAT aims to (1) utilize alternatives to
arrests of citizens in behavioral health and substance use crises, when appropriate; (2) seek safe outcomes for
individuals, families, and public safety personnel during a crisis; (3) reduce the overutilization of emergency
services through linking individuals to appropriate support resources; (4) encourage utilization of appropriate
community-based support resources as an alternative to emergency room and inpatient hospitalizations; and (5)
decreasethetimeotherrstresponseunits(i.e.,police,re,andEMS)spendatthesceneofacrisisbyassuming
control when appropriate.
MCAT training was primarily developed by Midtown leadership and included classroom learning, stakeholder
and expert presentations, site visits, and police ride-alongs. Training included the following topics:
INDIANAPOLIS MOBILE CRISIS ASSISTANCE TEAM
6
1. Mental health overview – including CIT training for those who had not yet received it, study of the
mental health and treatment system, language use and stigma, and relevant legislation;
2. First person accounts – including input from individuals with experience in substance use recovery;
3. Legal and Risk management – – including discussion of relevant legal and ethical issues of inter-agency
informationsharingandoverviewofrelevantaspectsofthecriminaljusticesystem;
4. Clinical information – including training related to populations with behavioral health and substance
abuse issues as well as self-care;
5. Special populations – including topics related to persons with developmental disabilities and autism,
personsexperiencinghomelessness,theLGBTQpopulation,olderadults,sextrafckingandprostitution,
veterans, and youth and family issues;
6. IMPD related training–includinguseofforce,situationalawareness,drugandnarcoticidentication,
de-escalation strategies and street safety;
7. IEMS related training–includingrstaid,CPRandnaloxoneuse;
8. Faith-Based community solutions – including introductions to existing programs aimed at assisting
relevant populations; and,
9. Organizational team building.
The MCAT evaluation focused on barriers and facilitators of program implementation as well as outcomes
associated with crisis responses. Barriers are problems, setbacks, challenges or obstacles to program
development or implementation, whereas facilitators are support systems, synergies or bridges that made
program development or implementation easier. The evaluation included qualitative data collection from focus
groupswithMCATmembers,interviewswithkeystakeholders,andeldobservationsduringMCATresponses.
In order to examine MCAT crisis responses, CCJR researchers worked with key stakeholders to identify the
necessary data points and develop data collection protocols. The following types of data were collected for
this evaluation.
Focus Groups
CCJR researchers conducted two semi-structured focus groups with members of the MCAT units. Each focus group
consisted of two teams (six members in each focus group) and lasted approximately 2 hours each. There was
a broad interview guide that was used to facilitate these focus groups in a semi-structured manner, allowing
for diversion and probing when appropriate. One lead researcher guided the focus group and two additional
trained researchers took notes.
STUDY DESIGN

7
Interviews with Stakeholders
CCJR researchers completed nine, one-on-one interviews with MCAT program developers and stakeholders. This
included leadership personnel from IMPD, IEMS, the Indianapolis Department of Public Health & Safety, and
Eskenazi Health. Interviews followed a structured survey guide, were audio recorded, and lasted approximately
one hour each.
Field Observations
TwoCCJRresearchersconductedobservationsofanMCATunitviaa“ride-along”whichlastedapproximately
ve hours. This eld observation began in the MCAT ofce based at the IMPD East District Headquarters.
ResearchersthenaccompaniedtheMCATunitinthevantothreeseparateresponsesandtookeldnoteson
observations.
Qualitative data were transcribed and researchers reviewed transcripts using content analysis to identify
barriers and facilitators to MCAT development and implementation. To establish inter-rater agreement,
researchers individually coded three qualitative sources using NVivo qualitative analysis software, and met
again to discuss emerging themes around barriers and facilitators and to develop coding procedures for the
additionalqualitativesources.Uponindividuallycodingallqualitativematerials,researchersmetanaltimeto
reviewthemajorthemesgleaned.Majorthemesarethoseidentiedbyfourormoreindividualsfromatleast
two different agencies during qualitative data gathering.
Ofcer Survey
Inanefforttotriangulatethesequalitativeresults,researchersalsoconductedasurveyofofcersfromtheIMPD
East District in which MCAT operates. CCJR researchers developed a web-based survey using Qualtrics survey
softwaretosolicitknowledge,attitudesandopinionsofofcerswhosharethedistrictwiththeMCATunits.The
surveywasanonymousandsentviaemailtoapproximately140patrolofcerswhoweregivenonemonthto
complete the survey.
MCAT Response Data
Finally, the research team collected quantitative data on each MCAT crisis response. CCJR researchers developed
a database where MCAT members were responsible for inputting information for each response completed.
MCAT stakeholders assisted in designing these data collection points.
Quantitative data were imported into SPSS for statistical analysis. Analysis largely consisted of descriptive
statistics regarding MCAT responses, but variation in response and outcomes based on key measures were also
examined. To this end, CCJR researchers examined statistically signicant differences using t-tests and Chi-
square difference of proportion tests.

8
BARRIERS TO PROGRAM IMPLEMENTATION
Policies and Procedures
Because the MCAT was established as a pilot program, little was known initially about the ways in which the
teams would most effectively address their behavioral health and substance use agenda. This was made more
problematic with the absence of detailed policies and procedures. As one team member noted,
“We need a clear mission statement; we don’t know whether we’re supposed to be
responding to certain runs or not. Right now we’re all taking different approaches to
these calls. What is our role supposed to be? Because I don’t think we have a clearly
dened role.”
However, leadership was hesitant to limit the ways in which MCAT could respond to emergencies, preferring to
allowforcreativityandexibilityintheirresponse:
“I think putting too many bright line rules on [this program] would probably be
detrimental to it. Because then it’s like when you have these bright line rules and
ofcers are held accountable to these rules they could get in trouble.”
WhilethisuidityallowedforMCATtocontinuouslylearnandadjusttoreal-timeneeds,alackofcleardirection
sometimes led to confusion and variation among the teams, both in this pilot program and previous co-response
programs studied in the literature. As noted by one MCAT stakeholder, “teams are inconsistent as far as their
operationsanddecisionmaking.”
BalancingtheneedsforuidityandconsistencyiskeyforfurtherclarifyingtheroleoftheMCATandcould
lead to greater buy-in from team members. For some, it is unclear whether they can or should perform duties
oftheirtraditionalroleswhileservingasanMCATmember.Greaterdenitionandclaricationofon-the-scene
procedures can help prevent team members from feeling underutilized. Additionally, determining to which
emergency situations MCAT should prioritize responding could lead to more consistency between teams and
greatercondencethatteamsaredoing“whattheyshould.”
Finally, developing common procedures and resources for post-crisis action can increase consistency between
teamsandreduceinefcienciesorconfusionfortheteamsindecidingwheretotakepatients,whotocontact,and
how to follow up. CCJR researchers witnessed evidence of at least one MCAT member who began the process of
consolidating phone numbers, addresses, forms, pamphlets and other resources for MCAT use. Formalizing and
regularly updating this consolidated information should be prioritized.
External Coordination
Inter-agencycoordinationcanbedifcultwhencombiningmultipleagenciesinoneemergencyresponseinitiative,
Inter-agencycoordinationcanbedifcultwhencombiningmultipleagenciesinoneemergencyresponseinitiative,
particularly around the topics of mental health and substance use. A culture shift is necessary for all entities
involved to both understand one another’s initiatives and coordinate a cohesive, appropriate response. IEMS,
IMPD and Midtown have taken strides to successfully coordinate; however, coordinating and communicating
MCAT goals and responsibilities with external actors was a salient barrier that emerged. For example, team
BARRIERS & FACILITATORS TO MCAT IMPLEMENTATION

9
members often recalled being asked who they were, noting that “People don’t know who MCAT is or what they
do.”MCATmembersstatedthatthisoccurredamongfellowofcersintheEastDistrictbutalsoamongotherrst
response agencies. For example, one MCAT stakeholder noted:
“[MCAT leadership] probably could have communicated it a little better amongst
supervisors and ofcers on East District, so they had a better idea. There was a little
confusion about what the responsibilities were. And there were ofcers that really
didn’t know the [MCAT teams] were out there.”
Similar statements were made regarding other community treatment providers. It was suggested that prior to
launch, key stakeholders “should have met with other hospitals before the MCAT program started because they
needtoknowwhoweareandwhywe’rebringinginpatients”andthat“mostpeopledon’tevenknowwhat
MCAT is so I don’t even think that most [doctors] would realize that their patient was brought by MCAT to the
emergencydepartment.”
Therewasalsoaperceivedneedtobetter“market”MCATtothepublicinordertodifferentiatethisprogram
from other initiatives in the East District; one stakeholder explained that other initiatives imbedded in East District
had misconceptions about what MCAT would and wouldn’t do. It is important to involve other actors in the area;
as an MCAT stakeholder advises:
“I would want other agencies to know that you have to be out there selling the
program. When I say out there, I mean other stakeholders in the community and you
have to nd outside partners...It’s not just a police program or a city program or an
EMS program or a clinician program. It is a collaborative approach and I think you
have to have people who understand that.”
By coordinating with other programs and initiatives aimed at helping similar populations, future implementation
efforts might better ensure all stakeholders are aware of the roles of one another. Additionally, it is important to
disseminate coordinated messages to the community and patients receiving MCAT assistance to avoid confusion
about roles and capabilities.
Outpatient Resources
Thedifcultypresentedby alackofoutpatient servicesforpopulationsservedbyMCATsurfacedmultiple
times throughout researcher’s review of both this data and data from previous studies. One MCAT stakeholder
conveyed:
“This is the biggest fear for me; you do all of this work on the front end, but there
are no real services on the back end, so these people aren’t getting the help, because
there are not enough beds or there are not enough mental health professionals that
will work with them, or they don’t have any insurance.”
Addressing the needs of the populations with behavioral health and substance use issues goes beyond responding
to acute emergencies and performing follow up. MCAT team members can provide resources or transport
patients to a hospital or other crisis center, but this does not guarantee the availability of necessary treatment
for people. An MCAT stakeholder suggested that “the city was under the impression that there are places to take
people;therearenot.”Futureimplementationsshouldrstconsiderexpandingtreatmentoptions,

10
“If we are talking about launching this in a thoughtful way in other places, then
making sure that treatment resources are available [is crucial]. You sort of have
to work backwards: if you’re going to go out and nd people who need help, you
probably want to have that help available.”
This was an especially prominent issue in terms of substance abuse treatment. In the midst of an opioid crisis in
Indianapolis, MCAT members noted that they “really don’t have anywhere to send people who need help with
heroinaddiction.”Giventheavailableresources,MCATmemberslamentedthatcrisisresponseswere“goingto
havetocontinuewiththeemergencydepartmentandthejail”butexpressedadesireto“workwithprovidersto
buildrelationshipsandndprovidersthatarewillingtoparticipatewithaclientelethatdoesnothavethebest
resourcesbutwhoaremostinneedoftreatment.”
Limited treatment resources can be a barrier to long-term health for patients, and can also lead to frustration
and burn-out from staff committed to serving people experiencing behavioral health and substance use issues.
For example, as one MCAT member noted, “people come out of [the hospital] not making changes because they
werejustgivenapamphlet,notservices”whileanotherstakeholdersuggestedthat,
“A lot of time and effort and money is being spent on innovative programs when
really probably a lot more time and effort and energy should be spent building the
capacity of our behavioral health system to take care of people.”
Addressing these issues requires bolstering a broader system of behavioral health care beyond the purview of
MCAT,follow-upunits,emergencydepartmentsandrst-responders.
Role Conict and Stigma
Switchingfromatraditionalroletoaspecialunit,particularlyforpoliceofcersandparamedics,wasidentied
asadifcultprocess.SomeMCATmembersexperiencedpersonaldiscomfortwithnewrolesandweremetwith
negative feedback from within their respective agencies, similar to team members in other types of co-response
teamsstudiedintheliterature.Forexample,oneMCATofcersuggestedthat“[Otherofcerssay]we’rejokes
now;wearen’ttherealpolice.”Thistypeofcriticismwasalsoheardfromotherrstresponders;membersstated
that“reghtershavebeenparticularlyresistanttounderstandwhatwedo”andthat“everyambulanceI’verun
intothinkswearetheretodotheirlegwork.”
SomeMCATteammembershaddifcultyadjustingtothenewidentityassociatedwiththeirspecialunitroles.
OnewaythismanifestedwasconcernabouttheMCATuniforms;asoneofcerstated,“thereishonorinyour
uniformandthisMCATuniformisahalfway-policeofceruniform.”
Leadership was aware that certain aspects of a new role as well as riffs with non-special unit personnel might
contribute to team member dissatisfaction or frustration. As one key stakeholder stated,
“One of the most difcult things is coming out of what they are normally doing...
they have all been on the street... so I think that’s an adjustment for them. Any time
law enforcement leaves the rst position (which is street ofcer position and goes to
investigation or something else) it’s often difcult to make that transition.”

11
Leadership also noted that:
“There was a lot of pressure and push back, just culturally within the organization.
Oh, why are you going to a special unit? What are you even going to be doing?
And [ofcers] couldn’t really answer that... It takes a certain type of ofcer with a lot
of self-condence and an open mind.”
Having buy-in from MCAT members is not only crucial for the success of the current program, but also something
to be considered in future implementation efforts. For example, one MCAT team member stated, “I have over 20
yearsofseasonedexperience,IfeellikeIambeingwastedinthatvan.”Effortstocarefullyselect,retainand
motivate team members are important to long-term program success.
FACILITATORS TO PROGRAM IMPLEMENTATION
Initial Citywide Collaboration and Buy-In
As evidenced in the literature, the success of an emergency response team like the MCAT requires buy-in from
many people and agencies who do not necessarily interact with this level of coordination ordinarily. Fortunately,
Indianapolis has multiple years of collaboration between mental health providers and IMPD, has incorporated
CIT training for many ofcers, and has the full support of the Mayor’s Ofce for the MCAT program. For
example, one respondent noted “this is a collaborative approach and you have to have people who understand
thatandcanworkinacollaborativeenvironment.”Anotherstakeholderestablished,
“Even before [MCAT] we had a good relationship with medical services here, a good
relationship with Eskenazi, and a good relationship with mental health workers. So,
from the top down there had been a lot of history and a lot of associations with
individuals who have thought the same way.”
This level of citywide effort in developing multi-agency responses to behavioral health and substance use issues
coupled with dedicated buy-in from agency leadership for development of the MCAT program facilitated a
relatively cooperative implementation and opened avenues for future coordination. Respondents especially noted
supportfromtheMayor’sOfce,asitprovidedaplatformforresourcenegotiationandagencyaccountability.
As one MCAT stakeholder said, “there is going to be push-back any time there is change; having the support
fromthetopiscrucial.”Anotherrespondentassertedthat:
“It has to start from the top down because this is an ask from everybody... there has
to be a return on investment for everybody involved that’s not money...So we have
all of these different moving parts, and when you put the leadership together in a
collaborative way, and these folks all want to solve the same problem, we can sort of
understand, ‘ok I can lose over here if I win over here.”
Programs like MCAT can take advantage of already-existing synergies between agencies, and further combining
efforts can open doors for future collaboration by breaking down communication and coordination barriers. This
allows leadership to leave their agency silos to address common issues in concert. As one respondent expressed,
“MCAT helps with pushing uncomfortable change and having collaboration. It has also helped us look at the
otherwayswecanworktogethertomakeadditionalchanges[tothesystem].”

12
Information Sharing
One of the most salient facilitators of implementation noted by participants in the current and previous studies
wastheabilitytoshareinformationwithinlegalpurview.MCATunitsbenetfromthecombinationofpatient
information from three different entities that serve the same populations. This triangulation of informational
resourcesresultsinagreaterabilitytoaddressaspecicpatientinthemomentofcrisisandlinkorre-engage
them with treatment services. Combining information also helps to identify the patterns and needs of “frequent
yers” of city emergency resources. This facilitator was expressed by multiple stakeholders throughout the
qualitative data. For example:
“It has enabled us to have a deeper understanding of the city enterprise as a whole...
We are able to really have a clear picture of [a patient’s] process through the
system. And we are able to see where we have very distinct weaknesses in our system.
Whether that’s lack of services, lack of support, a lack of communication...”
“There is a Midtown clinician that...is able to link [a patient] back to their treatment
team via our own medical record and communicate that this person is having a
problem, and then you can go in and see [if] this person is getting a follow up from
the treatment team the next day, versus kind of just letting them go.”
Duringeldobservation,researchersrecognizedtheusefulnessofcombiningtheEskenaziandIMPDinformation
systemstoidentifythecorrectaddressofaspecicpatient.OneMCATteammemberstated,“Ilovethatthe
clinician can get on the computer and look up any existing mental health issues that a person has; I’ve never
seenthatbefore.”Stakeholdersrealizedthat,“Combiningthesystemsandsoftwareofthreeagenciescreates
apowerfultool.”
Uponrespondingtoanemergencyscene,ofcersandclinicianscancomparecriminaljusticeandhealthcare
records on their laptops within legal parameters to better prepare the team to respond to a particular patient.
This triangulation can help teams anticipate potential hazards and also allows them to reconnect patients with
treatment services they received in the past when applicable. As one MCAT stakeholder stated,
“We can look at [a situation] from multiple different angles. We can do searches...
We typically try to do our homework when we go out and see somebody, especially
if we have a name ahead of time. Or if it’s on the back end we will look at it after
we get back to the ofce to try to see what has happened with this person in the past.
The police ofcer will go and look at what their record is. Our clinician can look to
see if they are in the Midtown system to see if they have been there before for some
other mental health treatment... and then from the medical side we can see...how many
times they have called in the past few years and now we are putting together a better
picture on things.”
As noted, combining multiple agencies to address emergencies had the unintended consequence of identifying
someofthefrequentyersofcityresources.Whilethesepeoplemayhavebeencontactedindividuallybythe
three agencies involved prior to MCAT, coordinated efforts to identify, record information and support those
individualswerenotasefcientastheycanbethroughMCAT.

13
Team Building
One of the most useful aspects of initial training was the ability for MCAT team members to learn about one
another, adopt useful skills from one another and build relationships. Team members were introduced to the
philosophies, language and procedures of the other agencies involved with MCAT during an almost two-month
training. As one MCAT stakeholder suggested, “It was apparent that each different agency needed to be a little
moreawareoftheotheragenciesinordertoworkmorecloselytogether.”Teammembersfoundthat,“Thebest
part[abouttraining]waslearningoneanother’srole”and“ThetrainingbroughtthisunittogetherandIthinkall
theteamsarefunctioningprettygood.”TheMCATmembersalsonotedthatbeingabletoselecttheirteamswas
a facilitator to program implementation, suggesting that “If we were assigned teams, we may not have been as
successful,butwegottopickourteamsandgetalongbetterforit.”
Researchers observed collegiality among the team members they accompanied during ride-along observations.
The clinician expressed observations of subtle changes in EMS team members’ interaction with persons with
behavioral health issues as a result of collaborating with other MCAT members. This change was also self-
identiedbyIMPDandIEMSmembersoftheMCAT,statingthattheir“mindsetwaschangedbecauseofthe
training.”
TheCCJRsurveyofIMPDEastDistrictofcersyielded63responseswhichisapproximatelya45%response
rate.Respondentswereanaverageageof39(SD=10.49,Range:18to65)andprimarilymale(76%)and
Caucasian(75%).Slightlymorethanhalfofrespondentshadatleastafour-yearcollegedegree(56%)and
had been in law enforcement for an average 13.10 years (SD = 10.39, Range: 1 to 40) with most currently
employedaspatrolofcers(78%).
CCJRresearchersrstaskedrespondentstoevaluatetheirlevelofknowledgeandcontactwiththeMCATteams.
LeadershipmadeeffortstointroducetheMCATteamstoEastDistrictofcersduringroll-call,shortmeetings
thatoccurbeforeeveryshift.However,thismethoddidnotreachallofcersaccordingtothesurveyas29%
of ofcers indicated that theywerenot formally introducedto theMCATprogrambeforeitslaunch. Next,
researchers looked at perceptions regarding the roles and expectations of the MCAT unit before and after
launch.
AsshowninExhibit1,57%statedthatrolesandresponsibilitiessurroundingtheMCATunitweresomewhatclear
orextremelyclearpriortolaunchandatthetimeofthesurvey(mid-lateNovember)84%saidtheroleswere
somewhat or extremely clear. This increased trend in role clarity is likely attributable to the fact that a high
proportionofrespondents,87%,reportedhavingbeenonthesceneofanemergencycallwiththeMCAT.The
surveyalsoallowedforopportunitiesforofcerstoexpress,throughopen-endedquestions,whatwouldmake
theMCATmoreusefultothemasofcersand6respondentsmentionedadesireforclaricationonMCATroles
andthattheseexpectationsbeconsistentbetweenMCATteams.Ofcerssaid,“itwouldbehelpfultoknow
exactlywhatMCATcanandcan’tdo”and“Ijustwantaclearerunderstandingofthesituationstheywill/will
notrespondto.”
IMPD EAST DISTRICT OFFICER SURVEY
14
Researchers also looked at perceptions of MCAT emergency responses. Most survey participants reported
thattheyhadspecicallyrequestedMCATassistanceonascene(83%)and79%reportedthattheMCATunit
arrivesallormostofthetimewhenrequested.DiscussionwithMCATteammembersandeld-observationswith
one team revealed a few reasons why the MCAT does not always arrive when requested. Teams are either
unavailable due to being at the scene of another crisis or cannot arrive fast enough due to their limited ability
totravelquicklyacrossthedistrict.ThesurveyalsorevealedthatEastDistrictofcerswouldlikefortheMCAT
to be more available: in an open-ended question, 17 respondents said the MCAT would be more useful if it was
moreavailable.Oneofcersuggests,“Getmoreofthemworkingatonetime...maybetwoorthreewouldhelp.
Therehavebeenmultipletimeswehaveaskedfor[assistance]wheretheywerealreadyoutonsomething.”
EXHIBIT 1. Clarity of Roles and Expectations of the MCAT Unit
EastDistrictOfcerPerceptions
27%
16%
57%
13%
3%
84%
Unclea r Neu tra l Clear
Percent of Officer Survey Responses
Prior to Launch Now
EXHIBIT 2. Perceptions of MCAT Usefulness
EastDistrictOfcerPerceptions
2%
6%
18%
24%
51%
Not at all useful
Slightly useful
Moderately useful
Very useful
Extremely useful
27%
16%
57%
13%
3%
84%
Unclea r Neu tra l Clear
Percent of Officer Survey Responses
Prior to Launch Now

15
Finally,researcherslookedatperceptionsofMCATusefulness.Overall,EastDistrictofcersndthattheMCAT
isaveryusefulresourcebecauseitallowsofcerstoreturntodutymorequicklyandbecausetheteamprovides
theabilitytobetteraddressmentalhealthcrises.AmajorityofofcersbelievetheEastDistrictisbetterat
responding to mental health crises because of the MCAT. As shown in Exhibit 2, respondents overwhelmingly
ratedtheMCATunitasveryorextremelyusefultothemasofcers(75%).Ofcerrespondentswereasked
toreportthereasonsforwhichtheyndtheMCATtobeuseful.Respondentsweremostlikelytoendorsethe
MCATteamasbeingusefulbecausetheyallowotherofcerstoreturntodutymorequickly(86%);theunique
combinationofanIEMS,IMPD,andclinician(73%);mentalhealthexpertise(64%);abilitytocompletefollow-
up(52%);andadditionalequipmentandresources(49%).Incontrast,respondentswerelesslikelytoviewthe
MCATasusefulforitsabilitytohandlenon-emergencycalls(44%)orprovidesubstanceabuseexpertise(35%).
FocusgroupdatawithMCATmemberssuggeststhatpartofthereasonofcersintheEastDistrictmightnot
perceive the unit as useful in terms of substance abuse is because on the scene of overdose they don’t have the
abilitytoarriveintimetoreviveapersonbeforeotherrst-respondersdoso,andanoverdosepatientisoften
not in a state of mind to engage in discussion about treatment in the moment.
In evaluating the improved ability of the East district to address mental health and substance abuse issues, a
greater proportion of respondents rated East District having a better response to mental health issues due to the
presenceofMCAT(79%)relativetosubstanceuseissues(49%).Aconsiderable89%ofrespondentsbelieved
theMCATunitmetorexceededexpectationssetpriortoitslaunch.Oneofcerstates,“IhonestlythinktheMCAT
crewisdoingaphenomenaljob.”Thisisalsoevidentinthefactthat33%ofofcersindicatedbeinginterested
inservingintheofcerroleontheMCAT.

16
In examining the data on MCAT responses, researchers looked at the characteristics of the people to whom
MCATrespondedandthenproceededtolookatresponseresultschronologically:rstlookingatthereasonfor
the response, then what happened on the scene of a response, and then the outcome of the response. Following
this, researchers examined repeat encounters and differences by teams.
The data used in this analysis come from all MCAT responses that occurred between August 1, 2017 and
December 9, 2017 that were recorded by MCAT team members. During these 19 weeks, there were a total
of 566 responses at approximately 4.4 runs per day. Every day during the study period there was at least 1
response and a day high number of 11 responses. It is also important to note that the 566 MCAT responses
occurredamong488uniqueindividualsas11%oftheresponseswererepeatencounters.
CLIENT DEMOGRAPHICS
Exhibit 3 displays the demographic characteristics among the 488 individuals that MCAT responded to during
thestudyperiod.Morethanhalf(58%)oftheresponseencounterswerewithmalesandmorethanhalf(55%)
wereCaucasian,41%wereBlackorAfricanAmerican,and3%Hispanic.Theaverageageofindividualswith
an MCAT encounter was 38 years and ranged from 10 years old to 90 years old.
QUANTITATIVE DATA ON MCAT RESPONSES
EXHIBIT 3. Demographic Characteristics of MCAT Response Cases
Race/Ethnicity
55%
41%
3%
1%
White Black Hispa nic Other
55%
41%
3%
1%
White
Black
Hispa nic
Other
Female
42%
Male
58%
Gender
N=286 N=210
Average Age
37.9 years old
Standard Deviation: 15.3
17
REASON FOR RESPONSE
MCAT team members were asked to record whether they self-dispatched to a given crisis scene or if another
agencyrequestedtheirresponse.Here,researchersfoundthatnearlytwo-thirds(63%)ofresponseswerethe
resultofMCATself-respondingandtheotherone-third(35%)werefromIMPDrequests;therewere8responses
requested from EMS, 5 from other agencies, and 16 response sources not recorded. MCAT also recorded what
the primary crises were and were able to select all responses that applied from six categories: (1) Suicide or
self-harm attempt or threat (2) Other mental health issues, (3) Overdose or other substance abuse problem, (4)
Domestic violence, (5) Physical health issue, (6) and Gravely disabled. Exhibit 4 shows the frequency that each of
thecategorieswererecordedaswellastheinstancesinwhichonlyonecategorywasrecorded:at59%,mental
healthconcernswerethemostcommonprimaryreasonforresponseandwastheonlycrisistypein37%of
responses. The second most frequent response reason was an overdose or other substance abuse problem which
wasindicated35.4%ofthetimeandwastheonlyreasonforaresponsein23%oftheencounters.Onlyslightly
lessthansubstanceabusewasself-harmorthreatofsuicidewhichwasindicatedin34%oftheencountersand
theonlyresponsereasonindicatedin18%oftheencounters.MCATresponsesfordomesticviolence,physical
health,orgravelydisabledwerelesscommonandtogetherwererecordedin10%ofencountersandeach
recordedastheonlyreasonforaresponseinlessthan2%ofencounters.
Another important point to examine with the MCAT data is whether responses or encounters changed over
time. As shown in Exhibit 5, researchers display the top three kinds of responses (mental health, self-harm,
andsubstanceabuse)duringtherstfourmonthsandfoundsomeuctuationovertimeinthetypesofMCAT
responses. While mental health related calls have remained the most frequent response, the number of self-
harm related responses has increased from 27 to 41. The number of substance abuse related responses started
EXHIBIT 4. Reasons for MCAT Response
Primary Crisis
3%
4%
4%
34%
35%
59%
2%
2%
1%
18%
23%
37%
Domestic violence
Physical Health
Gravely Disabled
Self-H a rm
Overdose or
Substance Abuse
Menta l Hea lth
Percent of runs in which crisis type was indicated
Crisis Type
Only Indication Any Indication

18
high at 50 but decreased during September and October to 29 and 30 respectively and increased to 49 in
November. This is a very limited follow-up period and additional data are needed to further examine these
trends.Thisuctuationmaybeduetothenumberofemergencycallsthatcomethroughforeachcrisistype,the
availability of MCAT to respond, response decisions of MCAT teams, or a combination of these factors.
SCENE OF AN MCAT RESPONSE
When MCATresponded to a crisis scene there were often other emergencyor rst response units already
present:inonly9%ofresponseswasMCATtheonlyunitresponding.IMPDwasalsoonthescenefor85%
ofresponses,EMSat58%ofresponses,andIFDat18%.BothEMSandIMPDwereatthesceneof52%of
responsesandIMPD,EMS,andIFDat16%ofresponses.While generally not the only unit on the scene, in two-
thirds (66%) of encounters, MCAT was able to relieve other emergency or rst response units from the scene.
AmongthoseencounterswhereMCATwasabletorelieveotherunits,63%ofthetimeitwasoneunit(EMS,
IMPD,orIFD),31%ofthetimeitwastwounits,and6%ofthetimeitwasallthreeunits.TheMCATalsoreported
additionalhazardspresentatthescenefor16%oftheencounterswiththemostcommonhazardreportedas
violentbehaviortowardothersbutonlyoccurredin7%ofencounters.Thenextmostcommonhazardreported
wasthepresenceofweaponswhichoccurredin3%ofencounters.
InlookingatthetimespentonthescenethemajorityofMCATencounterswerecompletedinunder90minutes
(88%) with 62% taking an hour or less. For those encounters that took longer to complete,the MCAT was
signicantly more likely have relieved other emergency or rst response units. For example, among those
encountersthatwereoveranhour,80%ofthetimeotheragencieswerereportedashavingbeenrelievedfrom
the scene.
EXHIBIT 5. MCAT Response Types over Time
27
35
48
41
64
69
55
73
50
29
30
49
August September October November
Nu mber of MCAT Runs
Self H a rm Menta l Hea lth Susbtance Abuse

19
MCAT RESPONSE OUTCOMES
OneofthemaingoalsoftheMCATteamistodivertpersonsawayfromjailorincarcerationwhenpossibleand
appropriate, and transport them into needed treatment or services. Following an MCAT encounter, two-thirds of
patients(65%)weretransportedsomewhere,themajorityofwhom(87%)weretransportedtoahospital(33%
weretransportedtoEskenaziHospital).Thismeansthat56%ofallMCATrunsresultedintransportingapersonto
ahospital.In25%ofMCATresponsestherewasanimmediatedetentiondecisionandinnearlyallofthesecases
the MCAT team provided transportation. Exhibit 6 shows the location and outcome of other transports provided by
MCAT.7%ofcrisestowhichMCATrespondedresultedinanarrestandamongthesearrests74%ofthetimeitwas
anIMPDofceralreadyonthescenethatinitiatedanarrest,ratherthananMCATofcer.Infact,MCATonlydirectly
transportedsomeonetojail9timesduringthestudyperiod,orotherwisestated,inlessthan2%ofallencounters.
Therewasnostatisticallysignicantvariationinindividualcharacteristicsorresponsetypeinthelikelihoodtoarrest.
REPEAT ENCOUNTERS
AlargemajorityofindividualsreceivedonlyoneMCATresponse;however,11%oftheoverallsamplereceived
two or more MCAT responses. These repeat encounters involved independent crises and resulting MCAT responses,
they were not follow-ups from a previous response. The average number of responses provided to this sub-
populationrangedfrom2to7encountersandtheaverageamountoftimebetweenindividuals’rstandlast
MCAT encounter was 17 days (M=27.84, SD=27.84). To explore the possibility that individual characteristics
and encounter circumstances can distinguish individuals who receive one MCAT response from individuals who
receivetwoormoreMCATresponses,comparisonsaremadebetweenindividuals’rstMCATresponse.Therst
response was purposely selected as the comparison point as this encounter sets the foundation for sequential
EXHIBIT 6. MCAT Response Outcomes
33%
54%
4%
4%
2%
2%
2%
Eske na z i
Hospit al
Ot her
Hospit al
Residence Reuben
Center
Shelter Other
Crisis
Center
Jail
Percent of MCAT runs resulting in transport
L oc ation
35%
65%
Not Transported
Transported
Did MCAT transport
person in crisis?
When MCAT transported someone,
where were they taken?
56% of all MCAT runs resulted in
transport to a hospital

20
activities. Three factors provide some insights. First, individuals who receive two or more MCAT responses were
more likely to have“gravely disabled” as the primary crisis type with no other crisis classications in their
initial response. Second, a larger proportion of individuals who experienced repeat encounters with MCAT
wererecordedashavingmentalhealthissues(59%)asaprimarycrisisthanindividualswhoreceivedasingle
MCATresponse(45%).Therewerenodifferencesbetweenrepeatandsoleencountersacrosstheremaining
combinations of response categories. Third, a smaller proportion of individuals who received more than one
MCATresponseweretransported(52%)inrelationtoindividualswhoreceivedoneresponse(66%).When
comparing the locations to which individuals are transported, there are no differences between the locations
to which they are delivered that would signal the need for subsequent encounters. In combination, this third
factor provides evidence that it is the decision to transport and not the location to which one is transported that
inuenceswhetheranindividualreceivesarepeatencounter.
Beyond these indicators, there were no other statistically dependable characteristics or circumstances that
enabled an ability to differentiate repeat and sole MCAT encounters. The responding MCAT unit, presence of
emergencyorrstresponseunitsatthescene,existenceofhazardsduringtheencounter,timingoftheencounter,
andactions takenduring the rst encounter did not help to identifyindividuals who wouldreceivemultiple
responses.
DIFFERENCES BY MCAT UNITS
InordertounderstandtheimpactofaspecicMCATunitonresponses,CCJRresearchersexamineddifferences
across the four unique units, referred to hereafter as Unit A, Unit B, Unit C, and Unit D. Researchers also looked
at variation between day and night shifts with Unit A and Unit B as the day shifts and Unit C and Unit D as the
nightshifts.Exhibit8displaysthestatisticallysignicantdifferencesresearchersfoundacrossthesefourunits.
Forexample,asillustratedinExhibit8,UnitAandUnitBweresignicantlymorelikelytoself-dispatchtoacall
whereas Unit C and Unit D were more likely to have been dispatched by IMPD. In terms of the type of calls,
researchers examined those cases where only one type of crisis type was indicated and found that Unit A was
more likely than the other units to respond to a self-harm and mental health related crisis calls but least likely
torespondtoasubstanceabusecall.AsshowninExhibit8,overone-quarter(26%)ofUnitD’sresponseswere
exclusivelysubstanceabuserelatedwhichwassignicantlyhigherthantheotherunits.
EXHIBIT 7. MCAT Repeat versus Single Encounters: Comparison of Transport & Crisis Type
5%
59%
52%
1%
45%
66%
Gravely Disabled
(Only Indicatio n)
Menta l Hea lth
(Only Indicatio n)
Transported
Single Encounters Repeat Encounters

21
Intermsofwhathappenedatthescene,therewerenosignicantdifferencesinthelikelihoodtotransportor
arrest.UnitBwasalsosignicantlymorelikelytorelieveotherrstresponseunitsandalsohadthequickest
responsetimewith23%ofresponseslasting30minutesorlessand72%lastinglessthanhour.Thisrateof
expeditious response was also shared by Unit A. Finally, Unit B was least likely to have had repeat responses.
Researchers also examined differences between shifts that occurred at day and at night and between those
instances where there was a full MCAT team available and those responses where a member of the team was
missing. While there was some variation in encounter characteristics and circumstances by shift and by complete
or incomplete MCAT teams, much of the differences were between units rather than shifts or complete versus
incomplete teams. Moreover, given the data available at this time, researchers cannot say that any of these
congurationswerebetterorworsebutsimplywanttonotethevariabilityinresponsetypesandtimespenton
the scene.
EXHIBIT 8. Variation by MCAT Units
UNIT A UNIT B UNIT C UNIT D
Response Request
MCAT Self Dispatch 51% 72% 66% 59%
IMPD Request 48% 27% 32% 37%
Reason for Response (mutually exclusive)
Self Harm 26% 50% 14% 19%
Mental Health 40% 33% 30% 24%
Overdose or Substance Abuse 12% 15% 18% 26%
Units Relieved
IMPD 41% 67% 58% 65%
IEMS 21% 36% 17% 27%
Any Unit 51% 75% 60% 72%
Response Scene and Outcome
Repeat Encounter 30% 23% 30% 18%
Immediate Detention 17% 36% 17% 26%
Time at Scene
Under 30 Minutes 23% 23% 15% 10%
Under 60 Minutes 69% 72% 48% 59%

22
After a review of the academic literature and a detailed description of the Indianapolis MCAT pilot program, this
studyidentiedanumberofimportantbarriersandfacilitatorstothepilotprogram’simplementation.Interms
of barriers, much like the academic literature on co-response teams, researchers found that ambiguity in terms
ofpoliciesandprocedureswasidentiedasabarrierandmanifesteditselfinanumberofwaysthroughout
theevaluation.Therewasdifcultywithexternalcoordination,inpartbecausetheMCATunitsareunableto
clearlyexpressthepurviewoftheprogramtootherrstresponseandcommunityagencies.Thisbarrierwas
alsoevidentintheEastDistrictsurvey,wherenearlyhalfofofcers(42.8%)statedthattheprogramwasnot
made clear to them prior to launch. This survey suggests that as the MCAT unit became a regular part of the
districtofcers’interactions,theycametobetterunderstanditsroles;however,it’sunclearifthecrystallizationof
these roles actually occurred among the MCAT units themselves. The biggest indicator of a lack of policies and
procedures was in the analysis of the quantitative data where researchers found MCAT units were responding
to different kinds of calls for service. Given the available data and the time of that the pilot program has
been in existence, researchers are not in a position to say which units were operating better or worse; rather,
researcherswouldspeculatethatthisvariationisduetothelackofdelityinprogramimplementationwhich
might be addressed by establishing clear guidelines as part of an MCAT policies and procedures document.
Strong support from city ofcials and key stakeholders was identied as a facilitator towards program
implementation.However,thissupportmightbecodiedandextendedbycreatinganadvisorygroupand/or
program coordinator for the MCAT units. An advisory group and/or program coordinator could communicate
what the goals and guidelines of the MCAT are to other key community stakeholders and agencies, improving
externalcoordination,whichwasidentiedasabarriertoprogramimplementation.Theadvisorygroupor
coordinator could also regularly evaluate the consistency of MCAT responses amongst teams and serve as a
liaisonbetweenteammembersandcityofcialstocentralizecommunication.
Team building was also identied as a facilitator to MCAT implementation. Specically, researchers found
that MCAT members felt training led to a sense of unity among team members. Unfortunately, feelings of
ostracizationfromfellowrstresponderswerealsopresent,asseveralMCATmembersnotedfeelingdiscomfort
in their new roles as a result. However, these feelings are not entirely consistent with the survey in which East
DistrictofcerswereoverwhelminglysupportiveoftheMCATpilotandfeltthatitmetorexceededexpectations.
It is possible that the negative stigma expressed towards MCAT members was an impactful, but relatively rare
event,orwassomethingthatoccurredonlyinitiallyinthepilot.Itisalsoworthnotingthatone-thirdofofcers
surveyedintheEastDistrictwereinterestedinservingasanMCATofcer,whichsuggestsapotentialpoolof
futureMCATofcerteammembers.
ThemostsignicantbarriertosuccessfulimplementationofMCATasawaytodivertpeoplefromthecriminal
justicesystemandintotreatmentserviceswasalackofcommunitytreatmentoptions.Thiswascommonlycited
as source of frustration by the MCAT members, leadership, and the community stakeholders in this study, as well
as participants in previous studies of similar co-response teams. Further research may attempt to follow up with
people who interacted with MCAT to understand the extent of their post-MCAT treatment.
By and large, the most salient facilitator to MCAT implementation was the ability share information in real time
between agencies. MCAT members from IMPD and IEMS regularly noted the advantages to having additional
CONCLUSIONS & FUTURE RESEARCH

23
informationonpersons.Thisinformationallowedthemtolocateindividualsmoreefcientlyandbetterunderstand
uniquetreatmentneeds.Giventheimportanceofthisfacilitator,itisworthexploringhowotherIMPDofcers,
who are not a part a specialized unit, might acquire access to this kind of information. Moreover, it would be
helpfultondawayofacquiringsimilarinformationfromprovidersotherthanMidtown.
Finally, our analysis of preliminary quantitative data from MCAT responses suggests that the program is meeting
itsprimarygoalofdivertingpersonsawayfromjail.Forexample,twothirdsofMCATresponsesresultedin
atransport;nearly90%ofthesepersonsweretransportedtoahospitalorothertreatmentfacilitywhileless
than2%weretransportedtojail.Futurecomparativestudiescandeterminewhetherthisdifferssignicantly
fromothersimilarcrisissituationswhereMCATisnotpresent.Whilethejaildiversiontrendispromising,this
ndingalsoraisesquestionsabouttheaimofMCATtoreducetheutilizationofemergencyservicesandseek
alternatives to hospitalizations given the high rate of transport to hospitals.
Alsonoteworthyisthatintwo-thirdsofallMCATresponsestheywereabletorelieveoneormoreotherrst
response units thereby improving overall emergencysystem efciency by freeing them to respond to other
calls for service. As noted above, there was variability across MCAT units in the kinds of calls they responded
to; however, at this time, researchers cannot determine whether these are meaningful differences that will be
related to outcomes or due to a lack of clear policy and procedure guidelines for MCAT units.
AlsoofnoteweretherepeatMCATencounters.Astheirtimeintheeldincreased,MCATteamscametodiscover
personswhowere“frequentyers”andinsomecasestheMCATmembersreporthavingbecometheprimary
response unit for these persons. While this led to mild frustration among MCAT members, it is also important to
notethatthesefrequentyersweremorelikelytobedisabledandmentallyillthanthepopulationofpeople
involved in only a single MCAT encounter. It might be innovative to accept that, given the nature of the program,
MCAT units are likely to identify these cases and supply them with resources or provide additional interventions.
ThisstudyrepresentsaverybriefsnapshotoftherstvemonthsoftheMCATprogram.Muchmoreresearch
is necessary to fully understand whether the MCAT program is effective in having a long term impact on the
communities it serves. Generally speaking researchers suggest at least three additional types of studies need
to occur to examine program effectiveness. First, data from the MCAT responses need to be linked to other
availabledatasources.Indoingso,researcherswillbeabletolookatchangesincriminaljusticeinvolvement,
the use of IEMS, and potentially treatment engagement. Second, the MCAT responses need to be compared
to similar emergency calls for which MCAT is not present. This would allow researchers to determine whether
the rate of arrest for the MCAT is truly lower than if an MCAT had not responded. Findings in the literature
havesuggestedthatthe arrestrateofPMIissomewherebetween2% and19%,dependingontheofcer
training, the availability of special units to address mental health crises and other factors (Borum and Franz,
2010; Reuland et. al. 2009). Finally, researchers need to better understand the perceptions and experiences
of individuals who are consumers of MCAT services. These individuals could elaborate on how their experiences
with MCAT differ from previous calls for service, whether their experiences had an impact on impressions of
IMPD, IEMS or Midtown, and whether the MCAT response had any short-term or long-term effects on behavioral
health changes and treatment linkage.

24
Adelman, J. (2003). Study in blue and grey. Police interventions with people with mental illness: A review of
challenges. Vancouver: Canadian Mental Health Association, BC Division.
Baess, E.P. (2005). Review of pairing police with mental health outreach services. Unpublished report, Vancouver
Island Health Authority.
Compton, M. T., Bahora, M., Watson, A. C., & Oliva, J. R. (2008). A comprehensive review of extant research on
crisis intervention team (CIT) programs. Journal of the American Academy of Psychiatry and Law, 36, 47-55.
Deane M, Steadman H, Borum R, Veysey B, Morrissey J. (1999). Emerging partnerships between mental health
and law enforcement. Psychiatric Services, 50(1), 99–101.
Dupont, R., Cochran, S., & Pillsbury, S. (2007). Crisis intervention team core elements. Unpublished report,
University of Memphis.
Greene J.C., Caracelli, V.J., & Graham, W.F. (1989). Toward a conceptual framework for mixed-method
evaluation designs. Educational Evaluation and Policy Analysis, 11(3), 255-74.
Hartford, K., Carey, R., & Mendonca, J. (2006). Pre-arrest diversion of people with mental illness: Literature
review and international survey. Behavioral Sciences & The Law, 24(6), 845-856.
Hay, T. (2015). Mental health treatment for delinquent juveniles: A new model for law enforcement-based
diversion. Appalachian Journal of Law, 14(2), 151-168.
Kirst, M., Francombe Pridham, K., Narrandes, R., Matheson, F., Young, L., Niedra, K., & Stergiopoulos, V. (2015).
Examining implementation of mobile, police-mental health crisis intervention teams in a large urban center.
Journal of Mental Health, 24(6), 369-374.
Lamb,H.R.&Grant,R.W.(1982).Thementally-illinanurbancountyjail.Archives of General Psychiatry 39(1),
17-22.
McQuaid,R.(2015,August27).MarionCo.SheriffrunsthelargestmentalillnessfacilityinIndianapolis:thejail.
Retrieved from http://fox59.com/2015/08/27/marion-co-sheriff-runs-the-largest-mental-illness-facility-
in-indianapolis-the-jail/
McQuaid, R. (2017, October 19). Mother alleges son with mental disabilities was denied meds inside Marion
County Jail. Retrieved from http://fox59.com/2017/10/19/mother-alleges-son-with-mental-disabilities-
was-denied-meds-inside-marion-county-jail/
Muntez,M.R.,&Grifn,P.A.(2006).Useofthesequentialinterceptmodelasanapproachtodecriminalization
of people with serious mental illness. Psychiatric Services, 57(4), 544-549.
REFERENCES

25
Shapiro, G. K., Cusi, A., Kirst, M., O’Campo, P., Nakhost, A., & Stergiopoulos, V. (2015). Co-responding police-
mental health programs: a review. Administration and Policy in Mental Health and Mental Health Services
Research, 42(5), 606-620.
Skubby,D.,Bonne,N.,Novisky,M.,Munetz,M.R.,&Ritter,C.(2013).Crisisinterventionteam(CIT)programsin
rural communities: A focus group study. Community Mental Health Journal, 49(6), 756-764.
Steadman,H.J.,&Naples,M.(2005).Assessingtheeffectivenessofjaildiversionprogramsforpersonswith
serious mental illness and co-occurring substance use disorders. Behavioral Sciences & the Law, 23(2), 163-
170.
Stelovich, S. (1979). From the hospital to the prison – Step forward in deinstitutionalization.” Hospital and
Community Psychiatry, 30(9), 618-620.
Swank,G.E.&Winer,D.(1976).Occurrenceofpsychiatric-disorderinacountyjailpopulation.American Journal
of Psychiatry, 133(11), 1331-33.
Taheri,S.(2016).Docrisisinterventionteamsreducearrestsandimproveofcersafety?Asystematicreview
and meta-analysis. Criminal Justice Policy Review, 27(1), 76-96.
Treatment Advocacy Center. (2015). Overlooked in the undercounted: The role of mental illness in fatal law
enforcement encounters. Retrieved from http://www.treatmentadvocacycenter.org/storage/documents/
overlooked-in-the-undercounted.pdf.
Whitmer,G.E.(1980).Fromhospitalstojails - FateofCalifornia’sde-institutionalizedmentally-ill.American
Journal of Orthopsychiatry, 50(1), 65-75.

The IU Public Policy Institute (PPI) delivers unbiased research and
data-driven, objective, expert policy analysis to help public,
private, and nonprot sectors make important decisions that
impact quality of life in Indiana and throughout the nation. As
a multidisciplinary institute within the IU School of Public and
Environmental affairs, we also support the Center for Criminal
Justice Research (CCJR) and the Indiana Advisory Commission on
Intergovernmental Relations (IACIR).
DESIGN BY
Karla Camacho-Reyes, Communications & Graphic Design

27
CENTER FOR CRIMINAL JUSTICE RESEARCH
HORIZONTAL VERSION
CENTER FOR CRIMINAL JUSTICE RESEARCH
VERTICAL VERSION
