COVID-19 Scientific Advisory Group Rapid
Response Report
June 19, 2020
© 2020, Alberta Health Services,
COVID-19 Scientific Advisory Group
Key Research Question: What is the effectiveness of wearing medical masks, including
home-made masks, to reduce the spread of COVID-19 in the community? [Updated June
19, 2020]
Context
• On June 5
th
, 2020, the WHO, despite a limited evidence base, provided guidance on the
continuous use of medical masks by health workers and caregivers in areas of known or
suspected community transmission regardless of whether direct care to COVID-19 patients is
being provided. In addition they provided guidance to decision makers using a risk based
approach for the use of masks in areas with community transmission of COVID-19 when
physical distancing is difficult (ie. public transit, shops, or other confined or crowded spaces).
• On May 20, 2020, the Public Health Agency of Canada recommended that non-medical masks
be used in settings where it is not possible to maintain a 2-metre physical distance. The federal
transportation minister then mandated mask use on planes, rail transport, and ships.
• The government of Alberta has initiated distribution of 20 million, single-use non-medical masks
to the community which appear to be of high grade (with a 3 layer design, purporting a 96%
filtration rate for particles up to 3 um and Delta-R 1.7 which would meet FFP2 requirements).
• Community mask use is now either encouraged or mandatory in over 80 countries, with many
jurisdictions encouraging but not mandating the use of cloth masks; however, some countries
such as Australia and New Zealand continue to not recommend community masking and have
achieved low rates of COVID activity despite the lack of this particular intervention.
• Shortages of medical (procedure, surgical masks) masks and N95 masks for health care
workers persist globally and nationally.
• With a focus on recovery and relaxation of social distancing in the context of the stabilization of
the initial wave of the pandemic, the general population is returning to community and
workplace settings where social distancing will not always be possible, which is driving interest
in, and controversies around the use of cloth and home-made masks.
Since completion of this report, additional potentially relevant papers have come to attention, to be
reviewed for inclusion in any possible future update of this literature synthesis (added September 3,
2021):
Abaluck, J., Kwong, L.H., Styczynski, A., Haque, A., Kabir, A., et al. (preprint). The impact of community
masking on COVID-19: A cluster-randomized trial in Bangladesh.
https://www.poverty-
action.org/publication/impact-community-masking-covid-19-cluster-randomized-trial-bangladesh
Bundgaard H, Bundgaard JS, Raaschou-Pedersen DET, et al. Effectiveness of adding a mask
recommendation to other public health measures to prevent SARS-CoV-2 infection in Danish mask
wearers. Ann Intern Med. 2020; 18:M20-6817. https://www.acpjournals.org/doi/10.7326/m20-6817
Research Question • 2
Key Messages from the Evidence Summary
• As medical masks are often bundled with other IPC interventions and have variable compliance,
clinical trials on the effectiveness of medical masks have been challenging. Systematic reviews
of randomized controlled trials in health care settings have not demonstrated a significant
reduction in acute respiratory infections, (ARIs), ILIs or laboratory confirmed viral infections with
medical mask use although it is acknowledged there were methodological flaws and smaller
underpowered studies in the data analyzed.
• There is a paucity of clinical evidence in favor of using medical masks in the community, with
multiple randomized trials demonstrating mixed results which when pooled demonstrate no
significant reduction in acute respiratory infections (ARIs), ILIs or laboratory confirmed viral
infections. There are some lower quality studies showing a reduction in viral infection rates in
households, in transmission of viral respiratory infections in the context of mass gatherings, and
in university residences when combined with hand hygiene interventions.
• However, while systematic reviews of randomized clinical trials fail to show significant benefit
with medical mask use in community settings, more observational and case-control studies
(both at higher risk of bias), have suggested that masks are protective.
• The reasons for the lack of significant reduction for ARIs in the randomized trials is complex and
may include: study design, setting, and human factors associated with wearing masks including
low compliance with mask wearing, lack of concomitant hand hygiene, inoculation via the
conjunctiva, frequent facial touching and mask adjustment leading to inoculation events, risk
compensation behaviours, and self-contamination with inappropriate mask doffing. These
possibilities have not been rigorously assessed.
• Laboratory studies investigating the efficacy of masks in filtering viral particles as well as studies
in medical settings with laboratory based endpoints for bacterial respiratory pathogens
(Pseudomonas aeruginosa and Mycobacterium tuberculosis) point to a theoretical benefit to
medical mask use as a form of source control (protecting others from the wearer). There are no
laboratory studies with SARS-CoV-2 and only one looking at other human coronaviruses.
• There are modelling studies and ecological data suggesting a benefit to medical mask use in
the community via a reduction in viral transmission rates (R0) across wide ranges of community
transmission levels. While these models are suggestive, they have significant inherent bias
based on multiple assumptions including assumptions around mask efficacy in preventing
transmission, and bundled interventions.
• Based on lab-based bioaerosol and NaCl aerosol studies, medical masks are superior to
homemade cloth masks, but non-medical masks and optimally constructed home-made masks
may offer some protection in reducing dispersion of droplets. Laboratory-based studies are of
highly variable quality, with only a few studies using industry approved filtration efficiency testing
methods.
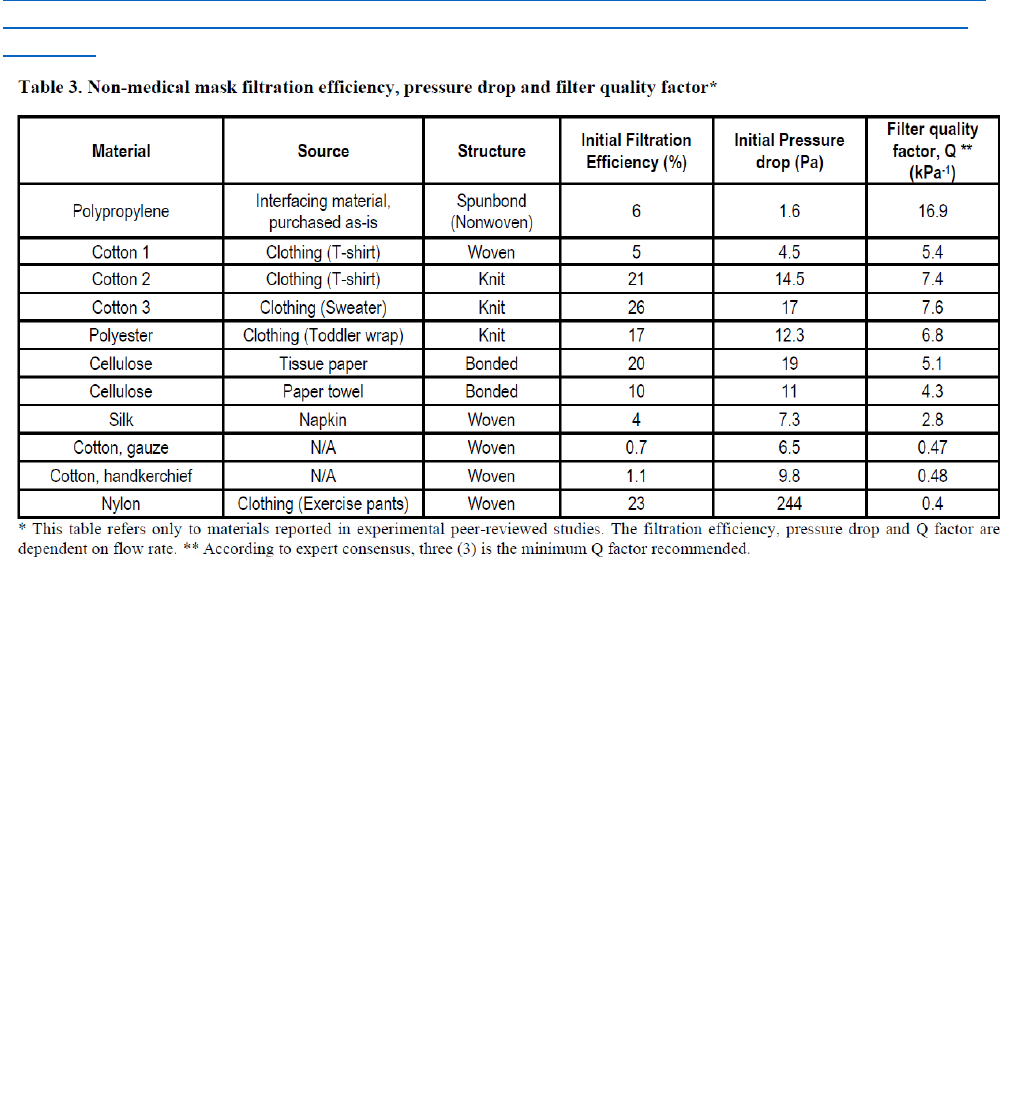
• The newly released guidance from the World Health Organization suggests decision makers
advising on non-medical mask use should take into consideration features of filtration efficiency
(FE), breathability, number (and combination) of materials used, shape, coating and
maintenance of cloth masks. The WHO suggests minimum Q (filter quality factor) score of the
material chosen of 3 (three) based on expert consensus and engineering science and industry
standards. They further suggest an optimal combination of material for non-medical masks
should include three layers:
1) an innermost layer of a hydrophilic material (e.g. cotton or cotton blends);
Research Question • 3
2), an outermost layer made of hydrophobic material (e.g., polypropylene, polyester, or their
blends) and
3) a middle hydrophobic layer of synthetic non-woven material such as polypropylene, or a
cotton layer which may enhance filtration or retain droplets
• There is limited evidence of harms related to community mask wearing with no studies identified
that have systematically looked at potential harms. Such harms could include behavioral
modifications such as risk compensation/non-adherence to social distancing or optimal hand
hygiene practices, self-contamination, induction of facial rashes, and increasing real or
perceived breathing difficulties. There are also concerns about poor compliance or tolerance of
masks in children or those with cognitive challenges and communication difficulties.
• The only clinical study to examine cloth mask efficacy in preventing repiratory virus transmission
was in a healthcare setting, comparing continuous cloth or medical masks use to usual practice.
Among the comparator (usual practice) group, a large percentage of individuals used medical
masks for part of the time. The study had significant methodological issues but did demonstrate
a significantly higher respiratory viral infection event rate of HCW using a 2-ply cotton cloth
masks when compared with the use of standard practice. (Macintyre et al, 2015)
• Pre-symptomatic transmission and asymptomatic transmission of SARS-CoV-2 have been
described but the degree to which they contribute to community spread is unclear, At this point,
there is no direct evidence that the use of a medical or homemade cloth mask or the wider use
of masks in the community significantly reduces this risk. For more information, refer to the
Asymptomatic Transmission of SARS-CoV-2 rapid review.
Committee Discussion
There was agreement that although the evidence base is poor, the use of masks in the community is
likely to be useful in reducing transmission from community based infected persons, particularly those
with symptomatic illness. One member was very concerned, and there was some agreement, that a
focus on mask-use could lead to a reduced sense of personal risk, i.e. risk compensation. There is
some evidence demonstrating less attention to social distancing and hand hygiene as the mainstays of
prevention in a community setting. It was noted that while there is evidence from observational studies
that medical masks may reduce ARIs and ILIs in health care settings, that there is no clinical trial
evidence that use of non-medical or medical masks in the community reduces viral transmission.
There was agreement that there is insufficient information to make a firm recommendation for the use
of home-made (non-medical) masks in the community. In the face of difficulties in quantifying risk of
asymptomatic transmission and potential benefit outweighing the harms of wider use of home-made
masks in the community, several committee members felt strongly that we should carefully balance the
recommendation for community use to reflect the precautionary principle as well as evidence gaps.
One member felt that to achieve the maximum population benefit, the majority of people should be
wearing masks in settings where physical distancing cannot be maintained. To account for these
controversies, which were mostly based on uncertainties in the evidence, a Research Gaps section has
been added.
There was concern that we may be over-emphasizing the potential harm associated with the use of
non-medical masks in the community, and there was general but not unanimous agreement to reduce
this emphasis and focus on the need for systematic research looking at benefits and harms with clinical
outcomes.

Research Question • 4
This update was predominantly based on the WHO revised advice, but it was noted that there is little
new evidence aside from information on filtration efficiency of different home-made masks since our
last update. There remains a lack of data demonstrating benefit of cloth masks as currently used in the
community, beyond lab based filtration studies. There remains a significant disconnect between RCTs
and observational study results of community mask use, and significant confounding and bias in
ecologic trials. Since the last version of this review, there is very little new data except new syntheses
of previous studies, new modeling studies, and some new collations of cloth filtration characteristics.
One reviewer commented on the system level issues with supporting medical and non-medical mask
use in the community as important elements in addition to the patient level harms.
One reviewer highlighted the importance of identifying specific level of guidance and evidence provided
by the updated advice from the WHO. As little additional evidence was highlighted in this review, the
emphasis of the WHO report was discussed: “the process of interim guidance development during
emergencies consists of a transparent and robust process of evaluation of the available evidence on
benefits and harms, synthesized through expedited systematic reviews and expert consensus-building
facilitated by methodologists. This process also considers, as much as possible, potential resource
implications, values and preferences, feasibility, equity, ethics and research gaps” (WHO, June 5,
2020). Therefore more specific description of the document, recommendations and the risk-based
approach to community mask use with consideration of local epidemiology has been incorporated.
(https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-
healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak)
Lastly, committee members felt that the research gaps section should better highlight the remaining
uncertainties regarding mask use in the community, and how they might be addressed. This would
include better information about optimal mask construction, as well as more robust evidence about their
impact on clinically relevant measures of benefit and harm. Finally, additional details about compliance
with medical and non-medical mask use in the community would be helpful.
Recommendations
1. In light of concerns around PPE shortages, medical masks should continue to be prioritized for
HCWs in direct patient care roles. HCWs should continue to wear medical masks whenever
providing direct patient care and whenever social distancing is not possible in health care
settings.
2. In the community, medical mask use should be prioritized for those with any symptoms
suggestive of COVID-19, as a form of source control. Community caregivers of potentially
infectious COVID-19 patients and care providers for those who are more vulnerable to severe
infection in the household setting should also wear medical or well-constructed non-medical
masks as a form of protection.
3. In settings where social distancing cannot be maintained, medical masks or high-quality non-
medical masks should be encouraged as a form of protection for those vulnerable to severe
COVID-19 infection outcomes. Vulnerable populations include those over 60 and those with
comorbidities or immunosuppression.
4. Evaluation of the extent of community transmission of SARS-CoV-2 is required to continually
assess the risks and benefits of community mask use in various situations, although there is
insufficient evidence to recommend specific epidemiologic thresholds for this purpose. This is
consistent with WHO guidance which advises decision makers to apply a risk-based approach
focusing on specific criteria when considering or encouraging the use of masks for the general
public that incorporates consideration of local epidemiology. The WHO encourages use of a
well-constructed non-medical mask, designed according to the available evidence from

Research Question • 5
materials engineering science, as a possible method of reducing risk of transmission of COVID-
19 when social distancing is not possible. Situations where this may be particularly relevant
include: on public transportation, workplaces necessitating close proximity to other workers or
the public, or when entering and exiting public buildings.
5. In light of widespread interest in masks and anecdotal evidence of potentially harmful,
inappropriate use by the public, health officials should widely communicate the need for both
optimal mask construction and mask “etiquette”. It is important to strengthen the messaging that
their use not replace the need for maintaining social distancing and hand hygiene as more
important strategies to prevent transmission of COVID-19; and the need to not touch the mask,
to replace when soiled or wet and ensure appropriate laundering. Current advice on when and
how to wear home-made or non-medical masks is available at:
https://www.albertahealthservices.ca/topics/Page16997.aspx#prev
Research Gaps
1. While there is some additional evidence, there is a need for further research into the optimal
construction and fabric composition of home-made or non-medical masks and their efficacy in
protection against transmission or acquisition of SARS-CoV-2.
2. Currently, we only have theoretical benefit demonstrated in laboratory studies of the filtration
capabilities of cloth masks. Further studies assessing population benefits and harms of home-
made (non-medical) masks are urgently required. These studies should include RCTs that
assess clinical outcomes.
3. Studies evaluating the frequency and compliance of mask use by individuals in clinical and
community settings, potentially using longitudinal surveys and/or contact tracing data would be
of benefit while awaiting more rigorous trial results.
Summary of Evidence
Since the last update on April 21, 2020, the World Health Organization has provided new guidance on
the use of masks in the community. There has also been a significant number of new studies examining
their use. However, there is only one new clinical study. The remainder of the studies have been
multiple new systematic reviews and meta-analyses of previously published clinical studies, modelling
studies, and laboratory-based studies of various homemade materials.
International guidelines and practices for use of masks in the community setting:
World Health Organization guidance on the use of masks in the community
On June 5th, the WHO provided an update to prior guidance from April 6th. 2020.
The process of interim guidance development during emergencies consists of a transparent and robust
process of evaluation of the available evidence on benefits and harms, synthetized through expedited
systematic reviews and expert consensus-building facilitated by methodologists. This process also
considers, as much as possible, potential resource implications, values and preferences, feasibility,
equity, ethics and research gaps (https://www.who.int/publications/i/item/advice-on-the-use-of-masks-
in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-
(2019-ncov)-outbreak).
The primary differences with this update included:
Updated information on transmission from symptomatic, pre-symptomatic and asymptomatic people
infected with COVID-19, as well as an update of the evidence of all sections of this document;

Research Question • 6
• New guidance on the targeted continuous use of medical masks by health workers working in clinical
areas in health facilities in geographical areas with community transmission1 of COVID-19;
• Updated guidance and practical advice for decision-makers on the use of medical and non-medical
masks by the general public using a risk-based approach;
• New guidance on non-medical mask features and characteristics, including choice of fabric, number
and combination of layers, shape, coating and maintenance. (WHO, June 2020)
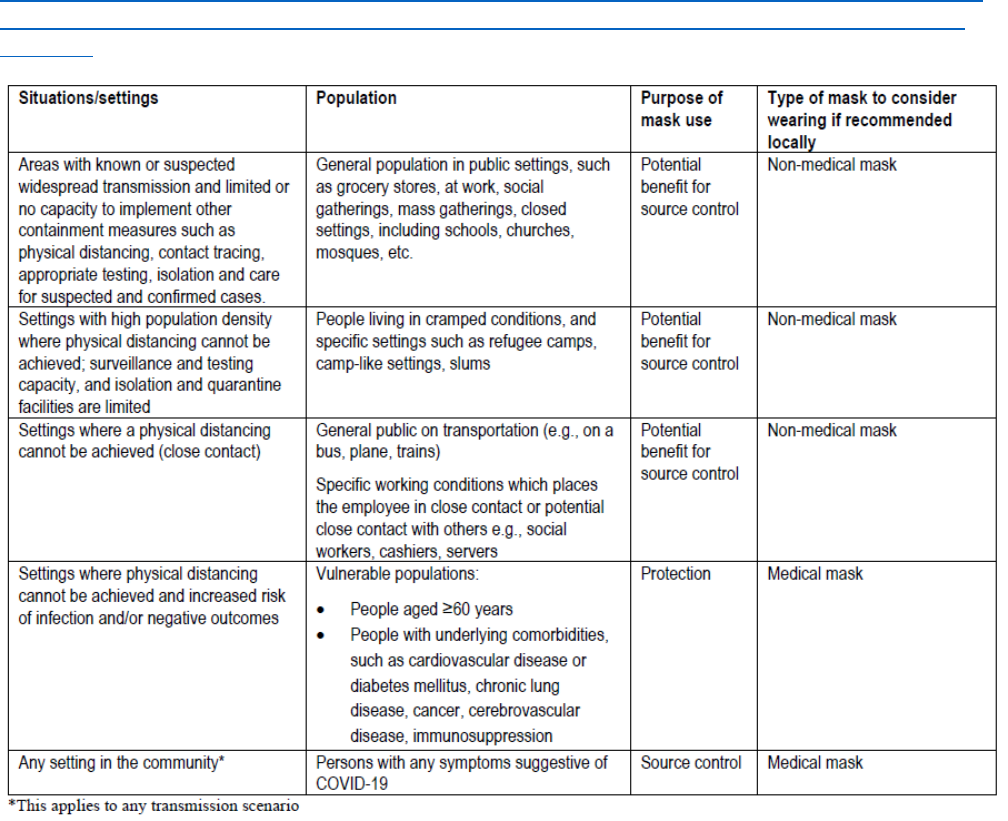
(see Table 1 in the Appendix).
As it relates to the: Targeted continuous medical mask use by health workers in areas of known
or suspected COVID-19 community transmission, the updated WHO guidance document
suggests the following guidance: (WHO, June 5, 2020)
In the context of locations/areas with known or suspected community transmission or intense outbreaks
of COVID-19, WHO provides the following guidance:
• Health workers, including community health workers and caregivers, who work in clinical areas should
continuously wear a medical mask during their routine activities throughout the entire shift; apart from
when eating and drinking and changing their medical mask after caring for a patient who requires
droplet/contact precautions for other reasons;
• According to expert opinion, it is particularly important to adopt the continuous use of masks in
potential higher transmission risk areas including triage, family physician/GP practices, outpatient
departments, emergency rooms, COVID-19 specified units, haematological, cancer, transplant units,
long-term health and residential facilities;
• When using medical masks throughout the entire shift, health workers should make sure that:
• the medical mask is changed when wet, soiled, or damaged;
• the medical mask is not touched to adjust it or displaced from the face for any reason; if this
happens, the mask should be safely removed and replaced; and hand hygiene performed;
• the medical mask (as well as other personal protective equipment) is discarded and
changed after caring for any patient on contact/droplet precautions for other pathogens;
• Staff who do not work in clinical areas do not need to use a medical mask during routine activities
(e.g., administrative staff);
• Masks should not be shared between health workers and should be appropriately disposed of
whenever removed and not reused;
• A particulate respirator at least as protective as a US National Institute for Occupational Safety and
Health-certified N95, N99, US FDA surgical N95, European Union standard FFP2 or FFP3, or
equivalent, should be worn in settings for COVID-19 patients where AGPs are performed (see WHO
recommendations above). In these settings, this includes its continuous use by health workers
throughout the entire shift, when this policy is implemented.
To be fully effective, continuous wearing of a medical mask by health workers, throughout their entire
shift, should be implemented along with other measures to reinforce frequent hand hygiene and
physical distancing among health workers in shared and crowded places where mask use may be
unfeasible such as cafeterias, dressing rooms, etc.
The following potential harms and risks should be carefully taken into account when adopting this
approach of targeted continuous medical mask use, including:
• self-contamination due to the manipulation of the mask by contaminated hands;
• potential self-contamination that can occur if medical masks are not changed when wet, soiled or
damaged;

Research Question • 7
• possible development of facial skin lesions, irritant dermatitis or worsening acne, when used
frequently for long hours
• masks may be uncomfortable to wear;
• false sense of security, leading to potentially less adherence to well recognized preventive measures
such as physical distancing and hand hygiene;
• risk of droplet transmission and of splashes to the eyes, if mask wearing is not combined with eye
protection;
• disadvantages for or difficulty wearing them by specific vulnerable populations such as those with
mental health disorders, developmental disabilities, the deaf and hard of hearing community, and
children;
• difficulty wearing them in hot and humid environments.(WHO, June 5, 2020)
As it relates to the WHO updated Advice to decision makers on the use of masks for the general
public
WHO advises decision makers to apply a risk-based approach focusing on the following criteria when
considering or encouraging the use of masks for the general public:
Taking into account the available studies evaluating pre- and asymptomatic transmission, a growing
compendium of observational evidence on the use of masks by the general public in several countries,
individual values and preferences, as well as the difficulty of physical distancing in many contexts,
WHO has updated its guidance to advise that to prevent COVID-19 transmission effectively in areas of
community transmission, governments should encourage the general public to wear masks in specific
situations and settings as part of a comprehensive approach to suppress SARS-CoV-2 transmission .
WHO advises decision makers to apply a risk-based approach focusing on the following criteria when
considering or encouraging the use of masks for the general public:
1. Purpose of mask use: if the intention is preventing the infected wearer transmitting the virus
to others (that is, source control) and/or to offer protection to the healthy wearer against
infection (that is, prevention).
2. Risk of exposure to the COVID-19 virus:
- due to epidemiology and intensity of transmission in the population: if there is community
transmission and there is limited or no capacity to implement other containment measures such
as contact tracing, ability to carry out testing and isolate and care for suspected and confirmed
cases.
- depending on occupation: e.g., individuals working in close contact with the public (e.g., social
workers, personal support workers, cashiers).
3. Vulnerability of the mask wearer/population: for example, medical masks could be used by
older people, immunocompromised patients and people with comorbidities, such as
cardiovascular disease or diabetes mellitus, chronic lung disease, cancer and cerebrovascular
disease.
4. Setting in which the population lives: settings with high population density (e.g. refugee
camps, camp-like settings, those living in cramped conditions) and settings where individuals
are unable to keep a physical distance of at least 1 metre (3.3 feet) (e.g. public transportation).
5. Feasibility: availability and costs of masks, access to clean water to wash non-medical
masks, and ability of mask wearers to tolerate adverse effects of wearing a mask.
6. Type of mask: medical mask versus non-medical mask

Research Question • 8
Based on these criteria, (Table 1 in appendix) provides practical examples of situations where the
general public should be encouraged to wear a mask and it indicates specific target populations and
the type of mask to be used according to its purpose. The decision of governments and local
jurisdictions whether to recommend or make mandatory the use of masks should be based on the
above criteria, and on the local context, culture, availability of masks, resources required, and
preferences of the population.
Masking recommendations
The following link provides a list of countries recommending or requiring community use of masks:
https://masks4all.co/what-countries-require-masks-in-public/
It is updated daily.
Mask provision
Foreseeing impending medical mask shortages, Taiwan enlisted multiple interventions to try to prevent
them. These included: state-controlled production and distribution of medical masks with daily,
individual, name-based rations of masks (at modest cost) distributed at local drugstore and free
provision of masks for school-aged children. South Korea also implemented state control over
manufacturing and now provides a weekly ration of two masks
(
https://www.nytimes.com/2020/04/01/opinion/covid-face-mask-shortage.html).
In Japan (https://english.kyodonews.net/news/2020/04/67ad0dfcd954-delivery-of-cloth-masks-from-
govt-starts.html), Hong Kong (https://www.qmask.gov.hk/about/), and Singapore
(https://www.gov.sg/article/when-should-i-wear-a-mask) mass-manufactured, re-usable, cloth masks
are being provided to citizens. In Hong Kong, pre-registered, low-income families may also receive 5
disposable medical masks per week for 10 weeks at vending machine dispensers
(
https://finance.yahoo.com/news/world-development-mask-dispensers-live-133000505.html).
The city of Los Angeles is providing garment manufacturers with crude guidelines on sewing non-
medical masks (
https://www.dropbox.com/s/x9myr2t9mhxd4zo/COVID_Mask-Manufacturer-
Packet.pdf?dl=0) that can then be sold to the public.
Current evidence on COVID-19 Transmission:
It is accepted that SARS-CoV-2 is transmitted via droplets (<5 μm) expelled when a patient sneezes or
coughs. However, the exact distance droplets can travel has been called into question (Bourouiba,
2020). Others have also posited the possibility of SARS-CoV-2 transmission through ordinary speech
(Asadi S et al, 2020). There is also increasing concern regarding pre-symptomatic, pauci-symptomatic,
or rarely, asymptomatic transmission of COVID-19, wherein individuals have RT-PCR detectable
SARS-CoV-2 from nasal or throat swabs prior to or without development of symptoms (Bai et al. 2020,
Chan et al. 2020, Pan et al. 2020, Kimball et al. 2020, Wei et al. 2020, and Li et al. 2020). It also
appears that viral loads are highest during the early symptomatic phase (To et al. 2002, Wolfel et al.
2020, and Bai et al. 2020) or even the pre-symptomatic stage. Indeed, He et al. 2020 infer that
infectiousness may peak on or before symptom onset and through modelling, estimate that up to 44%
of secondary cases were infected during the index cases’ pre-symptomatic stage. Therefore, the main
theoretical benefit of masks during the COVID-19 pandemic would be as a form of source control to
minimize dispersion of the expelled viral particles from individuals unknowingly transmitting disease.
For more information, refer to the Asymptomatic Transmission of SARS-CoV-2 Rapid Review
.

Research Question • 9
Clinical studies and systematic reviews examining use of medical masks to prevent
transmission of COVID-19:
One new clinical study has examined masks for prevention of COVID-19 transmission in the
community, specifically, in the household setting. Wang Y et al, 2020 undertook a retrospective study
of 335 people (124 families) to determine characteristics and practices of both the source case and
their contacts that were predictors of secondary transmission. They determined that if one or more
members of the household (either the primary case or their contacts) wore a mask before development
of symptoms, there was a 79% reduction in transmission (OR=0.21, 95% CI: 0.06 to 0.79). In another
study of 105 cases (imported from Wuhan to other centres) and 392 household contacts, the overall
attack rate in households was 16.9%, but was 0% in households of 14 index patients who reportedly
self isolated (used masks, dining separately, and residing alone within the home) upon (not before)
symptom development (Wei Li et al, 2020).
Clinical evidence for the use of medical masks in mixed settings (clinical and community) prior to
COVID-19 has been well summarized in three separate systematic reviews and meta-analyses
(Jefferson et al. 2011, Offeddu et al. 2017, Saunders-Hastings et al, 2017). Offeddu et al. focused
only on health-care settings, Jefferson et al. 2011 and Saunders-Hasting et al. 2017 looked at mixed
settings. All three reviews reported methodologic concerns related to the randomized trials that were
often under-powered and prone to reporting biases. Offeddu et al, did a meta-analysis of RCTs
comparing any mask (medical or N95) to no masks. They found that masks conferred significant
protection against self-reported clinical respiratory illness (RR = 0.59; 95% CI: 0.46–0.77) and
influenza-like illness (RR = 0.34; 95% CI: 0.14–0.82) but only a non-statistically significant effect
against laboratory-confirmed viral infections. A meta-analysis of observational studies noted a
protective effect of medical masks vs. no mask (OR = 0.13; 95% CI: 0.03–0.62) against SARS.
Jefferson et al, 2011 undertook a meta-analysis of seven case-control studies (~50% of participants
were not health care workers) with 3216 participants and found fewer acute respiratory infections with
medical mask use, OR 0.32, 95% CI 0.26 to 0.39. Of all physical interventions (including hand hygiene,
gowns and gloves), masks were the most effective. In a meta-analysis of three case-control studies
(19% of the participants being in a household setting), Saunders-Hastings et al. found that medical
masks provided a non-significant protective effect against pandemic influenza (OR = 0.53; 95% CI
0.16–1.71; I 2 = 48%).
Clinical evidence for the use of masks in the community setting (only) has also been examined, with
three systematic reviews by Brainard et al, 2020 (preprint), MacIntyre et al, 2015, and Barasheed et
al, 2016. Brainard et al, 2020 identified 31 different studies (including pre-post, cross-sectional, case-
control, observational, and randomized controlled trials). 12 studies were RCTs. These authors found
the evidence to be of low to very low certainty and concluded that “the evidence is not sufficiently
strong to support widespread use of facemasks as a protective measure against COVID-19. However,
there is enough evidence to support the use of facemasks for short periods of time by particularly
vulnerable individuals when in transient higher risk situations.” MacIntyre et al. 2015, identified 9 RCTs
of facemasks in diverse settings (households and community), and with varied designs and
interventions (ie. combination hand washing and facemasks). Due to the heterogeneity, no meta-
analysis was undertaken. The results were inconclusive. A copy of the table summarizing these 9
articles is provided in Table 2 of the Appendix. In general, the RCTs included use of a surgical grade
facemask but the observational studies did not provide adequate description of the types of masks
used.
Barasheed et al. 2016, pooled the results of 13 heterogeneously designed studies examining the
effectiveness of medical masks at preventing variably defined acute respiratory infection endpoints

Research Question • 10
arising during the Hajj pilgrimage. Based on studies which the authors deemed to be of “average”
quality, they found a small, statistically significant benefit (RR 0.89, 95% CI 0.84-0.94). However,
pooling of studies of vastly different design may be considered inappropriate from an analytic
perspective and it is possible this small difference disappears when a more appropriate pooling is done.
Since the completion of the last review, multiple new systematic reviews, with or without meta-
analyses, have been completed. They almost exclusively re-examined the studies already included in
the reviews mentioned above.
Any setting:
• Chu et al, 2020 did a systematic review and meta-analysis of observational studies (using
frequentist, Bayesian meta-analysis, and random effects meta-regressions) to look at the impact
of physical distancing, masks, and eye protection. Their analysis was limited to studies of
coronaviruses (SARS-CoV-2, SARS-CoV, and MERS-CoV). They did not identify any
randomized controlled trials. They found any masks (N95, medical mask, or 12-16 layer cotton)
reduced risk of infection (unadjusted n=10,170, RR 0.34, 95% CI 0.26-0.45; adjusted studied
n=2647, aOR 0.15, 95% CI 0.07-0.34) when compared to no mask. When only medical or 12-16
layer cotton masks were compared with no mask, the protective effect was diminished but
persisted (aOR 0·33, 95% CI 0·17–0·61). There was no comparison of medical masks to cotton
masks. When only the 3 community-based studies were included, masks remained protective
(RR 0.56, 95% CI 0.40-0.79). Using the GRADE category of evidence, the findings were
deemed to be of low certainty. This study was limited by the observational nature of the studies
included which are subject to significant bias.
• Jefferson et al, 2020 (pre-print) updated their previous review looking at physical interventions
to stop the spread of respiratory viruses, this time focusing only on randomized and cluster
randomized trials. 14 trials assessed the impact of mask wearing. Looking at general
population, there was no reduction in ILI cases (RR 0.93, 9% CI 0.83 to 1.05) nor in laboratory-
confirmed influenza (RR 0.84, 95% CI 0.61-1.17). No benefit was identified in health care
workers either.
• Liang et al. (pre-print) examined use of any type of mask in any setting in preventing
respiratory virus transmission. In the subgroup of non-HCW, a protective effect was found with a
pooled OR of 0.53 (95% CI=0.36 - 0.79), this effect persisted in both household (OR=0.60, 95%
CI=0.37-0.97) and the non-household settings (OR=0.44, 95% CI=0.33-0.59). The RCTs
included in this study scored 3 or 4/5 on the Jadad scale, but it should be noted that this a
quality assessment tool whose use is discouraged by the Cochrane Collaboration with concerns
of its ability to detect bias.
• MacIntyre R and Chughtai AA, 2020 looked only at randomized controlled trials. Including
eight trials in community settings, and concluded that when masks were used by ill individuals,
their well contacts were protected. Of note, these findings were dissimilar from many others in
that among health care workers in clinical settings, they found that only continual use of
respirators was beneficial, with medical masks found to be less effective and cloth masks were
even less effective than medical masks.
Community settings only:
• Wei et al. (pre-print) did a systematic review and meta-analysis of 8 RCTs examining any type
of mask in the community setting. Masks lowered the risk of developing ILI (pooled RR=0.81,
95% CI: 0.70-0.95).
• In a pre-registered, rapid review using Bayseian analysis, Pereski et al. (pre-print) identified 21
studies examining incidence of ILI (variably reported) in the community. All masks types were
considered. 1/11 RCTs and 6/10 observational studies found that masks reduced incidence of

Research Question • 11
ILI. They found that while RCTs showed a moderate likelihood of a small effect of wearing
medical masks in the community to reduce self-reported ILI, the risk of reporting bias was high.
The evidence for reduction of clinically or lab-confirmed infection was equivocal. By contrast,
observational studies showed that masks reduced incidence of ILI but there was a high risk of
confounding and reporting bias. The difference in the findings between RCTs and observational
studies was also noted previously by Brainard et al.
Cloth masks only:
• Mondal et al. (pre-print) looked at the utility of cloth masks in any setting. They included both
clinical and non-clinical studies, in what can be more accurately described as a scoping review.
They found two clinical studies, only one of which assessed the clinical effectiveness of cloth
masks. This was the study by MacIntyre et al, 2015 which is discussed later in this review. In
the laboratory studies, cloth mask filtration efficiency was highly variable, between 3-95%, likely
reflecting the highly variable materials and measurement techniques.
Laboratory based studies examining use of medical masks to prevent transmission of COVID-
19:
Given the challenges of clinical studies, another approach has been to directly measure the efficacy of
medical masks in both filtering exhaled respiratory viruses and in providing a barrier to entrance of
pathogens.
In the only laboratory study to look at coronaviruses, Leung et al, April 2020 found that coronaviruses
could be detected in respiratory droplets (>5um) and aerosols (<5 uM) in 3/10 (30%) and 4/10
(40%) of samples collected without medical masks, respectively. They did not detect any virus in
respiratory droplets or aerosols collected from participants wearing medical masks.
Multiple other studies have examined the use of masks for preventing spread of other respiratory
pathogens. Milton et al, 2013 found that medical masks reduced influenza viral copy numbers in
exhaled samples by ~3-25 fold (depending on the size of the particle). Johnson et al, 2009 could
detect influenza in all samples of exhaled breath where a mask was not worn but detected no influenza
virus by RT-PCR with medical masks. In two separate studies medical masks reduced the release of
Pseudomonas aeruginosa in patients with cystic fibrosis both when worn for short (Stockwell et
al, 2018) and longer durations (Stockwell et al, 2018). Dharmadhikari et al, 2012, examined the
benefit of medical masks as a form of source control on a multi-drug resistant tuberculosis ward
where exhaust air from patients is delivered to guinea pig exposure chambers. Compared to
patients who did not wear a masks, patients who did wear a mask infected 56% fewer guinea-pigs
(36/90 vs 69/90 infected guinea pigs).
Two studies have examined the effectiveness of medical masks to protect the wearer, as a barrier
against viral bioaerosols. Ma et al, 2020 found that compared with one-layer of polyester, medical
masks blocked 97.15% of avian influenza viral bioaerosols while a 4-layer homemade mask blocked
95.15%. The high efficacy rates of the masks may have been related to the unrealistically tight seals in
the model used. Makison-Booth et al, 2013 realistically adhered masks to the face of a mannequin
and then measured the amount of viable live influenza virus from the air in front and behind of five
different types of surgical masks. They found that medical masks reduced exposure to aerosolized
influenza virus by approximately 6-fold.
Thus, the preponderance of lab-based studies (Milton et al 2013, Johnson et al, 2009, Stockwell et al.
2018, Stockwell et al. 2018, Dharmadhikari et al, 2012, and Leung et al, 2020) suggest the benefit of a
mask is as a method of source control with reduction of the amount of respiratory virus released by

Research Question • 12
exhaled particles. That is, the public would be protected from respiratory spread of infection from the
mask wearer.
Other studies (modelling, ecological, anecdotal, etc) examining use of medical masks to prevent
transmission of COVID-19:
Influenza transmission models:
Brienen et al, 2010 developed a population transmission model to explore the impact of population-
wide mask use on an influenza pandemic. They assumed that the reduction in infection risk would be
proportional to the reduction in exposure to the virus based on particle retention by the mask and mask
coverage (number of people appropriately wearing masks). It is unknown if this assumption is valid.
They concluded that masks could lower the basic reproduction number, at least delaying, if not
containing, an influenza outbreak. A detailed transmission model by Trachet et al, 2009; however was
less optimistic, concluding that while 10% of the population using N95 masks could result in a 20%
reduction in H1N1, even 50% of the population wearing medical masks would only results in a 6%
reduction in number of cumulative cases. In their model, Yan et al, 2019, found that at a population-
level compliance of 50%, all types of masks—except low-filtration surgical mask—could reduce
prevalence of influenza outbreak to <5%. At a compliance rate of 80%, low-filtration surgical masks (not
otherwise defined) could reduce prevalence by 50%.
COVID-19 models: In a model assessing various local interventions, Tian et al, 2020 (preprint)
estimated reductions in the basic reproduction number R0 of SARS-CoV-2 with different interventions.
Assuming masks reduce R0 by a factor (1 − epm)
2
, where e is the efficacy of trapping viral particles
inside the mask, and pm is the percentage of the population that wears masks – for example, if 50% of
the population wears a mask and the mask has a 50% efficacy at trapping particles, R0 could drop to
1.35 (down from ~2.4). It is unknown if this assumption is valid.
Eikenberry et al. 2020 developed a mathematical model that adapted the SEIR model of Breinen et al.
and Trachet et al. to the COVID19 pandemic epidemiologic parameters and then looked at the impact
of varying mask efficacy and compliance rates on transmissions and epidemiologic outcomes (death,
hospitalizations). They found that 80% coverage of masks that are only 20% effective could still reduce
the effective transmission rate by 1/3. Applied to a case study of Washington state, this could translate
into a reduction in mortality of 24-65%. Javid et al, 2020 (pre-print) created a simple, proof of
principle, SIR model, assuming that masks reduced transmission by 8-16%. Like Eikenberry et al.
where there was more mortality benefit seen in areas of lower transmission, Javid et al. noted a more
substantial reduction on deaths when the effective R approached 1. Finally, Worby et al, 2020 (pre-
print) created a SEIRD model to test various strategies for mask allocation (ie. different percentage of
allocation to symptomatic vs asymptomatic individuals; or to the elderly population). First, they found
that the more effective the mask, the lower the population uptake required. That is, deaths could be
reduced by 65% with 15% coverage of a highly effective mask (75%) whereas they would be reduced
by only 10% with 30% coverage with a low effectiveness mask (25% containment). In terms of mask
allocation, they identified that prioritizing the elderly and maintaining a supply for identified infectious
cases is a superior strategy to random distribution.
It should be noted that all the modelling studies listed vary the effectiveness of masks in the model;
however, they do not assume that masks can carry harms that could outweigh benefits.
In an ecologic study, Lo JY et al, 2005 found that in the setting of “community hygienic measures”
promotion during the SARS 2003 epidemic in Hong Kong, where ~76% of individuals were wearing

Research Question • 13
masks, the proportion of positive specimens of other respiratory viruses dropped significantly in 2003. A
similar finding has been noted in Hong Kong since February 2020, where again mask use has
increased with the COVID19 outbreak (Leung et al, 2020). Kenyon et al. (pre-print) compared
countries who had implemented mask use vs no-mask use (as a binary outcome). At the time of the
analysis, 8/49 countries promoted universal mask use. After adjusting for date of the first COVID-19
diagnosis in the country and testing intensity, they found that masking resulted in an average decrease
of 326 cases per 1,000,000 inhabitants (linear coefficient -326, -601 to -51, p=0.021). These studies do
not allow the effect of masks to be separated from other community measures, including social
distancing with school closure, public space closures, hand hygiene, and household hygiene
campaigns. When undertaking ecological comparisons, it should be noted that countries such as New
Zealand, Australia, Denmark, and Switzerland have had success at containment of their epidemics
without the use of universal masking.
There are also two case cluster reports outlining the benefits of community mask use. It is unclear if
medical or non-medical masks were used. Zhang et al, 2013 assessed transmission of influenza A
virus on two flights from the United States to China. None of the 9 influenza-infected passengers,
compared with 47% (15/32) of control-passengers wore a face mask. Unfortunately, this report does
not include any information regarding the location of the other passenger relative to the index case. Liu
et al, 2020 report a case of a SARS-CoV-2 infected male who took two separate buses to return to his
hometown. On the first 2-hour bus ride, he did not wear a mask and 5/39 passengers were infected. By
contrast, on his second ride, a 50-minute ride, he wore a mask and 0/14 passengers were infected.
While Schwartz et al. 2020 do not focus on the use of a mask by the source case, the source case
was masked during a flight from China to Toronto where no SARS-CoV-2 transmissions were identified.
Studies of cloth masks:
Clinical studies
The only clinical study of cloth masks is a cluster randomized trial of cloth masks at all times vs medical
masks at all times (2 masks/8h) vs a standard practice arm in hospitals in Vietnam (Macintyre et al,
2015). In this study, cloth mask users had higher rates of ILI compared with the control arm, RR=6.64,
95% CI 1.45 to 28.65 and more laboratory-confirmed virus, RR=1.72, 95% CI 1.01 to 2.94. Compared
to medical masks, the RR for ILI was 13.25 in the cloth mask arm and 3.8 in the control (mixed) arm. A
possible hypothesis for the worse outcome with cloth masks is that when they become wet, they are
more likely to trap viral particles. Alternatively, there may be inadequate washing of the masks.
However, a methodologic concern was that the control arm consisted of high rates of mask wear.
Specifically, in the control arm, (170/458) 37% used medical masks and (245/458) 53% used a
combination of medical masks and cloth masks, with 24% of control arm participants wearing masks for
more than 70% of working hours (versus 57% of participants in the other 2 arms adherent to masks for
>70% of working hours). This renders the comparison to have been consistent cloth mask use, to
consistent medical mask use, to inconsistent use of any mask type. Therefore, while the study may
have conclusively shown the superiority of medical masks to cloth masks in preventing infection
acquisition in a health-care setting, it cannot be used to reliably evaluate cloth masks to no masks in a
community setting. Given the sudden interest in cloth-mask use, the authors published a response to
their own article on March 30, 2020 (MacIntyre et al. 2020) wherein they state that HCW should not
work without adequate PPE but if they choose to work with a cloth masks, thorough and daily
disinfection is required to prevent potential harms. In another commentary, the same author (MacIntyre
CR and Hasanain SJ, 2020) supports universal masking, stating “There is more evidence supporting

Research Question • 14
face mask use in the community than hand hygiene including in RCTs which compare both
interventions directly,
so it is inconsistent to advocate hand hygiene as a sound principle but not
masks.”
Laboratory based studies
Several contemporary and historical studies have looked at whether homemade masks are able to
reduce the physical spread of droplets by the mask wearer. In a laser-light scattering experiment,
Anfinrud et al. 2020, qualitatively showed that while regular speech resulted in droplets ranging in size
from 20 to 500 µm, a slightly damp washcloth over the mouth could decrease these forward moving
particles. After assessing the filtration performance of a variety of household fabrics (using NaCl
aerosols of smaller size than droplets), Rangesamy et al, 2010 concluded that while markedly
inferior to N95 respirators, the filtration rate of some household materials was comparable to
surgical masks. Davies et al, 2013 found that masks made from cotton t-shirt fabric had a filtration
efficiency of viral particles of ~50% as compared to ~90% for medical masks and tha
t medical masks
were 3 times more effective in blocking transmission than homemade masks. Dato et al. 2006, also
found some protection against an aerosol challenge with the use of a homemade cotton mask.
We identified two studies examining the theoretical benefit of homemade masks in reducing
personal risk of exposure to particles. As previously noted, Ma et al. 2020, found a homemade
mask of one polyester cloth layer and 4 layers of kitchen paper to be as effective as medical
masks in providing protection against avian influenza virus bioaerosols. However, an artificially
tight seal may have been present in this model. van der Sande et al, 2008 found that medical masks
provided about twice as much protection as homemade masks against the entrance of particles.
Notably and unlike other groups, they did not find that masks significantly prevented outward dispersal.
Since the last update, we identified multiple other laboratory-based studies investigating filtration
efficiency, 3 of which were completed since the last update.
Historical studies
• Greene et al, 1961 had volunteers wear muslin and flannel masks (the standard for medical
masks at the time) in a contained chamber. Bacterial recovery on agar sedimentation plates
was dramatically reduced (by 88% to >99% depending on the particle size).
• Quesnel et al, 1975 used a similar chamber to Green et al. and volunteers were asked to try 4
disposable medical masks and one cotton mask. The filtration efficiency of the cotton mask
(after 30 minutes of wear) for larger droplets (>3 μm) >99%.
Air pollution and fine particulate matter (aerosol) studies (<2.5 μm)
• A study by Shakya et al. 2017, that was assessing filtration potential of cloth masks for fine
particulate matter (air pollution related study) noted that the filtration efficiency of three particle
sizes (30, 100, and 500 nm) ranged from 15% to 57%, thus they felt that cloth masks would be
of limited utility for particles<2.5 μm.
• Jung et al, 2014, also assessed a variety of masks for protection against aerosols. Their testing
adhered to the Korean Food and Drug Administration (KFDA) [similar to the European Union
(EU) protocol] and the National Institute for Occupational Safety and Health (NIOSH) protocols.
44 different types of masks were tested. On average, the aerosols used for testing were less
than 2.5 μm. The filtration efficiency of medical masks was only about 60% and only in the 2-
12% range for cloth handkerchiefs. Pressure drop was also measured. They found that “general
masks” and handkerchiefs provided little protection against aerosols.
Research Question • 15
• Jang et al, 2015 [only available in Korean; abstract was reviewed], using polydisperse NaCl
aerosols (0.3~10 μm), compared five commercial cloth masks vs. a respirator. The filtration
efficiencies varied from 9.5-28.5% as compared with 91% by the respirator but increased by
1.7-6.8 times after folding to create multiple layers. Washing once reduced filtration efficiency.
The authors warned that cloth masks were inadequate in protecting against particulate matter.
Bioaerosol and polydisperse NaCl aerosol studies
• Rodriguez-Palacios et al, 2020 (pre-print) used household spray bottles filled with a bacterial
suspension to see whether various textiles could prevent dispersion of the bacterial solution
(which they said mimicked a sneeze) onto agar containing Petri dishes. All the fabrics used,
even in one layer, reduced droplet dispersion to <30cm. As a double layer, they were as
effective as medical masks and reduced droplet dispersion to <10cm. The relevance of this
model is questionable.
• Wang et al, 2020 (pre-print) used industry approved standardized tests to compare 17 different
fabrics against approved medical masks. Testing pressure difference (breathability), particle
filtration efficiency, bacterial filtration efficiency, and resistance to surface wetting, they found
that only 3 materials would pass industry standards. The results showed that three double-layer
materials including double-layer medical non-woven fabric (example, polypropylene) medical
non-woven fabric plus non-woven shopping bag, and medical non-woven fabric plus granular
tea towel could meet all the standards of breathability, particle filtration efficiency (>30%), and
resistance to surface wetting, and were close to the standard of the bacterial filtration efficiency
(>95%).
• Aydin et al, 2020 (preprint) compared one brand of medical mask to a variety of homemade
fabrics to assess for: efficiency of blocking droplets, breathability, weight, hydrophilicity, and
texture. To measure droplet blockage (or filtration) efficiency, they used a metered-dose inhaler
(MDI) loaded with fluorescent beads, of similar size to SARS-CoV-2 virus (70-100nm). A petri
dish covered with the various materials was then held 36mm and 300mm away from the MDI
and the number of fluorescent beads penetrating through to the petri dish were measured. In
this study, even one layer of a 100% cotton t-shirt had 91% efficiency. And while a blend of
cotton and polyester had only 40% efficiency, this increased to 99.98% with 3 layers. They
concluded that multiple fabrics were comparable to a medical mask in terms of filtration and
breathability. However, a 2-3 layer cotton/polyester blend was the closest; despite being far less
hydrophobic. Of note, the materials appear to have been tightly adhered to the petri dish.
• Konda et al, 2020 also tested a variety of household materials. They introduced a polydisperse
NaCl aerosol into a mixing chamber, where it passed through the material being tested (held
down tightly by a clamp). They analyzed particle size with two different particle analyzers and
followed the protocol used for testing face respirators in compliance with the NIOSH 42 CFR
Part 84 test protocol. For droplets >300nm, several materials had filtration efficiency equivalent
to a medical mask (>95% efficiency), including even one layer of a high thread count cotton.
However, the authors recommended a hybrid fabric (cotton + silk) that could leverage both
mechanical and electrostatic properties. Furthermore, the authors found that even small gaps
(hole of 1% surface area) could reduce filtration efficiency by 60%, highlighting the importance
of a tight fit
• Zhao et al, 2020 evaluated common materials using a modified version of the NIOSH standard
test procedure for N95 respirator approval. They used NaCl aerosols (0.075 ± 0.02 μm), without
taking real-world leakage from around the mask into account, to identify the material with the
highest filtration quality factor (Q) – a metric that results from a high filtration efficiency (low
penetration) with low pressure drop. They identified that polypropylene spunbound, a material
Research Question • 16
commonly found in reusable bags, had the optimal Q. While the filtration efficiency was ~6-10%
(which was similar to the other fabrics tested), if it were triboelectrically charged or multiple
layers were added, its filtration efficiency improved without a concomitant increase in pressure.
In fact, as compared with the medical masks they tested (~19-33% filtration efficiency), the five-
layer polypropylene had a filtration efficiency of ~50% with a lower pressure drop.
Though there are now many different laboratory studies to draw from, the variability of the
methodology of the studies and the variability in their findings make their interpretation challenging.
Taken together, these studies suggest that non-medical masks can act as a barrier to outward
dispersion of droplets (but not particles <2.5 μm). For that reason, WHO states that non-medical
masks “should only be considered for source control (used by infected persons) in community
settings and not for prevention”.
Despite the challenges of interpreting non-medical mask studies, a non-medical mask standard has
been developed by the French Standardization Association (AFNOR Group)
(https://www.afnor.org/en/faq-barrier-masks/)
. AFNOR Group defines minimum performance in
terms of filtration (minimum 70% solid particle filtration or droplet filtration) and breathability
(maximum pressure difference of 0.6 mbar/cm2 or maximum inhalation resistance of 2.4 mbar and
maximum exhalation resistance of 3 mbar).
In addition, in its latest interim guidance report (
https://www.who.int/publications/i/item/advice-on-
the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-
the-novel-coronavirus-(2019-ncov)-outbreak), WHO has now provided guidance on the optimal
composition and construction of non-medical masks. They advise that when decision-makers are
providing recommendations on masks, they should take filtration efficiency, breathability, number
and combination of materials used, shape, coating and maintenance into account. Using the filter
quality factor “Q” metric, which is a function of filtration efficiency and breathability (with higher
values being better), they advise the following mask composition:
a) Inner layer of a hydrophilic material (cotton or cotton blend)
b) Outer layer of a hydrophilic material (ie. polypropylene, polyester or blend)
c) Middle hydrophobic layer of a synthetic non-material such as polypropylene or a cotton layer
Table 3 in the Appendix provides a list of different materials with their corresponding filter quality factor
as well as filtration efficiency and breathability.
In terms of fit, they also recommend a tightly-fitted flat-fold or duckbill shape.
(WHO, June 5, 2020)
Theoretical sociological benefits and harms of mask use in COVID-19:
From a sociologic perspective, some have noted that if mask wearing were widespread and not just
limited to those who are feeling ill, it would reduce the stigma associated with their use and increase the
likelihood of their use in ill individuals. Similarly, mask use may act as a visual cue reminding individuals
to maintain physical distance and act as visible signal of social solidarity (preprint, Howard et al. 2020).
In terms of acting as a visual cue, Seres et al, 2020 undertook a field experiment where they
randomized 300 individuals to “exposure” to an individual wearing a mask vs no-mask. Specifically, the
experimenter was randomly assigned to wear a mask or not. Then, they took the last position in line-
ups (ie. a supermarket, store) and noted the distance with which the subsequent customer would stand.
Individuals kept a statistically significantly further distance when someone was wearing a mask.

Research Question • 17
Subsequent survey data suggested this was because it was perceived that a masked person preferred
more distance.
Finally, it is becoming increasingly clear that racial minorities are disproportionately impacted by
COVID-19 (Hooper et al, 2020). In addition to underlying co-morbidities and structural inequalities (ie.
lack of access to healthcare), this discrepancy may be attributed to living conditions and employment.
As Yang, 2020 stated “social distancing is a privilege”. For instance, outside of LTC outbreaks, most
outbreaks in Calgary, Alberta are occurring at warehouses and workplaces
(https://www.alberta.ca/covid-19-alberta-data.aspx#toc-1) where social distancing either cannot be or is
not being enforced. Mandatory masking, with provision of masks and targeted education about mask
hygiene, may be particularly helpful in such settings.
There are also several possible harms associated with widespread mask use. There is concern that
moisture retention could increase the risk of infection which is one possible interpretation of the
McIntyre study. Masks may also increase the frequency with which individuals touch their face. There is
also concern regarding self-contamination of the hands or face with improper donning and doffing
technique. In an observational study of ~10,000 pedestrians in Hong Kong in February 2020, 94% of
individuals wore masks (84% of which were medical masks). However, 13% of individuals wore them
incorrectly, with 5% wearing them inside out or upside-own and 5% wearing them too low (Tam et al,
2020).
The importance of risk-compensation in population-level health interventions has been called into
question (B Pless, 2016). However, the potential harms of masks in creating a false sense of security
and consequent neglect of physical distancing or hand hygiene is raised by the World Health
Organization (WHO, 2020). A recent study by Yan et al, 2020 (pre-print) used smart device location
data to determine the time spent at home and at various public locations before and after mask
mandates were implemented in 36 different states. They accounted for weather patterns, re-openings
orders, and time since stay-at-home orders were implemented. They found that masks mandates were
associated with an increase of 4% (20-30 minutes) of time outside the home per day and they
specifically noted more trips to restaurants. This suggests that for mask to be beneficial, their efficacy in
reducing transmission needs to exceed the increased risk associated with a 4% increase in time away
from home.
Another concern is related to the environmental impact of mass use of medical masks. For instance,
the sheer numbers of disposable masks that would be required in China would be around 900 million
daily and would pose significant disposal challenges (Wang MW et al, 2020). Safe disposal concern
are already arising throughout Asia (https://www.bangkokpost.com/opinion/opinion/1924908/face-mask-
crisis-of-another-design)
Another major concern is the risk of PPE shortages for HCW who are more frequently exposed to
SARS-CoV-2 than the general public. Indeed, there have been shortages globally, with some countries
Date question received by advisory group: March 31, 2020
Date report submitted to committee: April 2, 2020
Date of first assessment: April 3, 2020
(If applicable) Date of re-assessment: June 19, 2020

Research Question • 18
banning or threatening to ban export of medical masks (https://www.cnbc.com/2020/04/03/coronavirus-
trump-to-ban-export-of-protective-gear-after-slamming-3m.html), and with reports of hoarding and price
gouging.
Authorship and Committee Members
This report was written and updated by Leyla Asadi and scientifically reviewed by Elizabeth Mackay
(primary reviewer), Lynora Saxinger (co-chair), and Nelson Lee. The full Scientific Advisory Group was
involved in discussion and revision of the document: Braden Manns (co-chair), John Conly, Alexander
Doroshenko, Shelley Duggan, Andrew McRae, Jeremy Slobodan, James Talbot, Brandie Walker, and
Nathan Zelyas.
© 2020, Alberta Health Services, COVID-19 Scientific Advisory Group
This copyright work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivative
4.0 International license. You are free to copy and distribute the work including in other media and
formats for non-commercial purposes, as long as you attribute the work to Alberta Health Services, do
not adapt the work, and abide by the other licence terms. To view a copy of this licence, see
https://creativecommons.org/licenses/by-nc-nd/4.0/. The licence does not apply to AHS trademarks, logos or content for which
Alberta Health Services is not the copyright owner.
Disclaimer: This material is intended for general information only and is provided on an "as is", "where is" basis. Although
reasonable efforts were made to confirm the accuracy of the information, Alberta Health Services does not make any
representation or warranty, express, implied or statutory, as to the accuracy, reliability, completeness, applicability or fitness
for a particular purpose of such information. This material is not a substitute for the advice of a qualified health professional.
Alberta Health Services expressly disclaims all liability for the use of these materials, and for any claims, actions, demands or
suits arising from such use.

COVID-19 Scientific Advisory Group Rapid
Response Report
June 19, 2020
© 2020, Alberta Health Services,
COVID-19 Scientific Advisory Group
Appendix
The literature search was conducted by Lauren Seal from the AHS Knowledge Resource
Service. The literature search was last updated on May 14, 2020.
Medline/PubMed
1 exp Coronavirus/ or exp Coronavirus Infections/ or coronaviru*.mp. or "corona virus*".mp.
or ncov*.mp. or n-cov*.mp. or COVID-19.mp. or COVID19.mp. or COVID-2019.mp. or
COVID2019.mp. or SARS-COV-2.mp. or SARSCOV-2.mp. or SARSCOV2.mp. or
SARSCOV19.mp. or Sars-Cov-19.mp. or SarsCov-19.mp. or SARSCOV2019.mp. or Sars-
Cov-2019.mp. or SarsCov-2019.mp. or "severe acute respiratory syndrome cov 2".mp. or
"2019 ncov".mp. or "2019ncov".mp. (18987)
2 Masks/ (4203)
3 mask.mp. (28586)
4 masks.mp. (15768)
5 facemask.mp. (1101)
6 "face-mask".mp. (2557)
7 (face adj2 mask*).mp. (3254)
8 2 or 3 or 4 or 5 or 6 or 7 (37583)
9 homemade.mp. (2899)
10 home-made.mp. (2094)
11 "home made".mp. (2094)
12 handmade.mp. (505)
13 "hand made".mp. (346)
14 hand-made.mp. (346)
15 handcraft*.mp. (335)
16 hand-craft*.mp. (321)
17 "hand craft*".mp. (321)
18 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 (6424)
19 8 and 18 (32)
Research Question • 20
20 8 or 19 (37583)
21 1 and 20 (140)
22 limit 21 to last year (19)
CINAHL
S1 (MH "Coronavirus+")
S2 (MH "Coronavirus Infections+")
S3 coronaviru*
S4 "corona virus"
S5 ncov*
S6 n-cov*
S7 COVID-19 OR COVID19 OR COVID-2019 OR COVID2019
S8 SARS-COV-2 OR SARSCOV-2 OR SARSCOV2 OR
SARSCOV19 OR SARS-COV-19 OR SARSCOV-19 OR SARSCOV2019 OR SARS-COV-
2019 OR SARSCOV-2019
S9 "severe acute respiratory syndrome cov 2" OR "severe acute
respiratory syndrome coronavirus*"
S10 "2019 ncov" OR 2019ncov OR Hcov*
S11 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR
S10
S12 (MH "Masks") 2,140
S13 mask OR masks OR facemask OR face-mask OR face N2 mask
OR medical N2 mask OR face N2 cover* 10,693
S14 S12 OR S13 10,693
S15 homemade OR home-made OR "home made" OR handmade OR
hand-made OR "hand made" OR handcraft* OR hand-craft* OR "hand craft*" 2,013
S16 S14 AND S15 10
S17 S14 OR S16 10,693
S18 S11 AND S17 87
S19 S11 AND S17 Limiters - Published Date: 20190101-20201231

Research Question • 21
12
TRIP Pro/Google Scholar/Google/ LitCovid/CEBM/ /Twitter/WHO/Stanford
Medicine/REACTing/Nebraska Medicine COVID-19 resources/CAIC-RT – COVID-19
Capacity Tool/NEJM/ The Oakes Academy Coronavirus Clinical
Collaboration/CochraneLibrary
("covid-19" OR coronavirus OR COVID19 OR “corona virus” OR ncov OR “n-cov” OR “covid-
2019” OR covid2019 OR “SARS-COV-2” OR “sarscov-2” OR sarscov2 OR sarscov19 OR
“sars-cov-19” or “sarscov-19” OR sarscov2019 OR “sars-cov-2019” OR “severe acute
respiratory syndrome”) AND (mask OR facemask OR “face-mask” OR “face mask” OR “face
cover” OR “face covering” OR “homemade mask” OR “home-made mask” OR “handmade
mask” OR “hand-made mask” OR “handcrafted mask” OR “hand-crafted mask”)
(mask OR facemask OR “face-mask” OR “face mask” OR “face cover” OR “face covering” OR
“homemade mask” OR “home-made mask” OR “handmade mask” OR “hand-made mask” OR
“handcrafted mask” OR “hand-crafted mask”)
mask
facemask
face covering
Critical Appraisal
Table 2. Summary of quality assessment results for articles included in this review
Mixed Methods
Appraisal Tool
Criteria:
Reference
Peer
reviewed?
Type of
evidence
Are
there
clear
research
question
s or a
clearly
identified
issue?
Is the
collected
data or
presented
evidence
appropriat
e to
address
the
research
questions
or issue?
1
.
Jefferson T, Del Mar CB, Dooley L, Ferroni E, Al-Ansary LA,
Bawazeer GA, van Driel ML, Nair S, Jones MA,
Thorning S, et al. 2011. Physical interventions to
interrupt or reduce the spread of respiratory viruses.
The Cochrane Database of Systematic Reviews.
2011(7):CD006207.
☒ Yes
Systematic
review and
meta-analysis
☒ Yes
☒ Yes

Research Question • 22
2
.
Offeddu V, Yung CF, Low MSF, Tam CC. 2017.
Effectiveness of masks and respirators against
respiratory infections in healthcare workers: A
systematic review and meta-analysis. Clinical
Infectious Diseases : An Official Publication of the
Infectious Diseases Society of America. 65(11):1934-
42.
☒ Yes
Systematic
review and
meta-analysis
☒ Yes
☒ Yes
3
Saunders-Hastings P, Crispo JAG, Sikora L, Krewski D.
2017. Effectiveness of personal protective measures in
reducing pandemic influenza transmission: A
systematic review and meta-analysis. Epidemics.
20(C):1-20.
☒ Yes
Systematic
review and
meta-analysis
☒ Yes
☒ Yes
4
Brainard J ea. 2020. Facemasks and similar barriers to
prevent respiratory illness such as
COVID-19: A rapid systematic review.
☐ No (pre-
print)
Systematic
review and
meta-analysis
☒ Yes
☒ Yes
5
WHO. Advice on the use of masks in the context of
COVID19. Available at:
https://www.who.int/publications-detail/advice-on-the-
use-of-masks-in-the-community-during-home-care-
and-in-healthcare-settings-in-the-context-of-the-novel-
coronavirus-(2019-ncov)-outbreak .
WHO
guidelines
6
MacIntyre CR, Chughtai AA. 2015. Facemasks for the
prevention of infection in healthcare and community
settings. BMJ : British Medical Journal. 350(apr09
1):h694.
☒
Yes
Review article
☒
Yes
☒
Yes
7
MacIntyre CR, Seale H, Dung TC, Hien NT, Nga PT,
Chughtai AA, Rahman B, Dwyer DE, Wang Q. 2015. A
cluster randomised trial of cloth masks compared with
medical masks in healthcare workers. BMJ Open.
5(4):e006577.
☒ Yes
Cluster
randomzied
trial
☒ Yes
☒ Yes
8
Leung, N.H.L., Chu, D.K.W., Shiu, E.Y.C. et al. Respiratory
virus shedding in exhaled breath and efficacy of face
masks. Nat Med (2020).
https://doi.org/10.1038/s41591-020-0843-2
☒ Yes
Randomzied
lab-based trial
☒ Yes
☒ Yes
9
Davies A, Thompson K, Giri K, Kafatos G, Walker J, Bennett
A. 2013. Testing the efficacy of homemade masks:
Would they protect in an influenza pandemic? Disaster
Medicine and Public Health Preparedness. 7(4):413-8.
☒
Yes
Laboratory
☒
Yes
☒
Yes
1
0
Makison Booth C, Clayton M, Crook B, Gawn JM. 2013.
Effectiveness of surgical masks against influenza
bioaerosols. Journal of Hospital Infection. 84(1):22-6.
☒ Yes
Laboratory
☒ Yes
☒ Yes
Research Question • 23
APPENDIX
Table 1: Situations and types of masks recommended for use in the community (from
the World Health Organization, June 2020 interim guidance “Advise on the use of masks
in the context of COVID-19”)
https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-
home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-
outbreak

Research Question • 24
Table 2. Summary of high level evidence (GRADE guidelines) on facemasks in the
household setting (from: Raina MacIntyre, and Abrar Ahmad Chughtai BMJ
2015;350:bmj.h694)
Research Question • 25
Table 3. Non-medical mask filtration efficiency, pressure drop and filter quality factor*
(from the World Health Organization, June 2020 interim guidance “Advise on the use of
masks in the context of COVID-19” Adapted from Jung et al, 2014 and Zhao et al, 2020)
https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-
home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-
outbreak

Research Question • 26
References
2. Anfinrud P ea. Visualizing speech-generated oral fluid droplets with laser light
scattering. NEJM. 2020. https://www.nejm.org/doi/full/10.1056/NEJMc2007800.
3. Asadi S, Bouvier N, Wexler AS, Ristenpart WD. The coronavirus pandemic and aerosols:
Does COVID-19 transmit via expiratory particles? Aerosol Science and Technology.
2020;ahead-of-print(ahead-of-print):1-
4. http://www.tandfonline.com/doi/abs/10.1080/02786826.2020.1749229. doi:
10.1080/02786826.2020.1749229.
4. Aydin O et al. Performance of fabrics for home-made masks against spread of respiratory
infection through droplets: A quantitative mechanistic study . .
2020. https://doi.org/10.1101/2020.04.19.20071779.
5. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-
19. JAMA. 2020. https://www.ncbi.nlm.nih.gov/pubmed/32083643. doi:
10.1001/jama.2020.2565.
6. Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions: Potential
implications for reducing transmission of COVID-19. JAMA.
2020. https://www.ncbi.nlm.nih.gov/pubmed/32215590. doi: 10.1001/jama.2020.4756.
7. Brainard J ea. Facemasks and similar barriers to prevent respiratory illness such as
COVID-19: A rapid systematic review. . 2020. https://doi.org/10.1101/2020.04.01.20049528.
8. Brienen NCJ, Timen A, Wallinga J, Van Steenbergen JE, Teunis PFM. The effect of mask
use on the spread of influenza during a pandemic. Risk Analysis. 2010;30(8):1210-
1218. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1539-6924.2010.01428.x. doi:
10.1111/j.1539-6924.2010.01428.x.
9. Chan JF, Yuan S, Kok K, et al. A familial cluster of pneumonia associated with the 2019
novel coronavirus indicating person-to-person transmission: A study of a family cluster. The
Lancet. 2020;395(10223):514-523. http://dx.doi.org/10.1016/S0140-6736(20)30154-9. doi:
10.1016/S0140-6736(20)30154-9.
10. Chen X, Ran L, Liu Q, Hu Q, Du X, Tan X. Hand hygiene, mask-wearing behaviors and its
associated factors during the COVID-19 epidemic: A cross-sectional study among primary
school students in wuhan, china. International journal of environmental research and public
health. 2020;17(8):2893. https://www.ncbi.nlm.nih.gov/pubmed/32331344. doi:
10.3390/ijerph17082893.
11. Cheng KK, Lam TH, Leung CC. Wearing face masks in the community during the COVID-
19 pandemic: Altruism and solidarity. The Lancet. 2020. http://dx.doi.org/10.1016/S0140-
6736(20)30918-1. doi: 10.1016/S0140-6736(20)30918-1.

Research Question • 27
12. Cheng VC, Wong S, Chuang VW, et al. The role of community-wide wearing of face mask
for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. Journal of
Infection. 2020. http://dx.doi.org/10.1016/j.jinf.2020.04.024. doi: 10.1016/j.jinf.2020.04.024.
13. Chowell D et al. Sustainable social distancing through facemask use and
testing during the covid-19 pandemic. . 2020. https://doi.org/10.1101/2020.04.01.20049981.
14. Chu D, Akl E, El-Harakeh A, et al. Physical distancing, face masks, and eye protection to
prevent person-person COVID-19 transmission: A systematic review and meta-analysis. SSRN
Electronic Journal. . doi: 10.2139/ssrn.3578764.
15. Clase CM et al. Cloth masks may prevent transmission of COVID-19: An evidence-based,
risk-based approach . . 2020. https://www.acpjournals.org/doi/10.7326/M20-2567.
16. D. F. Johnson, J. D. Druce, C. Birch, M. L. Grayson. A quantitative assessment of the
efficacy of surgical and N95 masks to filter influenza virus in patients with acute influenza
infection. Clinical Infectious Diseases. 2009;49(2):275-
277. https://www.jstor.org/stable/40308667. doi: 10.1086/600041.
17. Dato VM, Hostler D, Hahn ME. Simple respiratory mask. Emerging infectious diseases.
2006;12(6):1033-1034. https://www.ncbi.nlm.nih.gov/pubmed/16752475. doi:
10.3201/eid1206.051468.
18. Davies A, Thompson K, Giri K, Kafatos G, Walker J, Bennett A. Testing the efficacy of
homemade masks: Would they protect in an influenza pandemic? Disaster medicine and
public health preparedness. 2013;7(4):413-
418. https://www.ncbi.nlm.nih.gov/pubmed/24229526. doi: 10.1017/dmp.2013.43.
19. Donald K Milton, M Patricia Fabian, Benjamin J Cowling, Michael L Grantham, James J
McDevitt. Influenza virus aerosols in human exhaled breath: Particle size, culturability, and
effect of surgical masks. PLoS Pathogens.
2013;9(3). https://search.proquest.com/docview/1327739532. doi:
10.1371/journal.ppat.1003205.
20. Eikenberry SE, Mancuso M, Iboi E, et al. To mask or not to mask: Modeling the potential
for face mask use by the general public to curtail the COVID-19 pandemic. Infectious Disease
Modelling. 2020;5:293-308. http://dx.doi.org/10.1016/j.idm.2020.04.001. doi:
10.1016/j.idm.2020.04.001.
21. Esposito S, Principi N. To mask or not to mask children to overcome COVID-19. European
Journal of Pediatrics. 2020. https://search.proquest.com/docview/2401102611. doi:
10.1007/s00431-020-03674-9.
22. Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the
COVID-19 pandemic. The Lancet Respiratory Medicine.
2020. http://dx.doi.org/10.1016/S2213-2600(20)30134-X. doi: 10.1016/S2213-2600(20)30134-
X.

Research Question • 28
23. He X, Lau EHY et al. Temporal dynamics in viral shedding and transmissibility of covid-
19. Nature Medicine. 2020.
24. Howard J ea. Face masks against covid19: An evidence review. .
2020. https://www.preprints.org/manuscript/202004.0203/v1.
25. Jang JY, Kim SW. Evaluation of filtration performance efficiency of commercial cloth
masks. Korean Journal of Environmental Health Sciences. 2015;41(3):203-215. doi:
10.5668/JEHS.2015.41.3.203.
26. Jefferson T, Del Mar CB, Dooley L, et al. Physical interventions to interrupt or reduce the
spread of respiratory viruses. The Cochrane database of systematic reviews.
2011;2011(7):CD006207. https://www.ncbi.nlm.nih.gov/pubmed/21735402. doi:
10.1002/14651858.CD006207.pub4.
27. Kenyon C. Widespread use of face masks in public may slow the spread of SARS CoV-2:
An ecological study. . 2020. https://doi.org/10.1101/2020.03.31.20048652.
28. Keshtkar-Jahromi M, Sulkowski M, Holakouie-Naieni K. Public masking: An urgent need to
revise global policies to protect against novel coronavirus disease (COVID-19). The American
journal of tropical medicine and hygiene.
2020. https://www.ncbi.nlm.nih.gov/pubmed/32323645. doi: 10.4269/ajtmh.20-0305.
29. Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS-CoV-2
infections in residents of a long-term care skilled nursing facility — king county, washington,
march 2020. MMWR. Morbidity and Mortality Weekly Report. 2020;69(13). doi:
10.15585/mmwr.mm6913e1.
30. Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, Guha S. Aerosol filtration
efficiency of common fabrics used in respiratory cloth masks. ACS nano.
2020. https://www.ncbi.nlm.nih.gov/pubmed/32329337. doi: 10.1021/acsnano.0c03252.
31. Leung N, Chu, D.K.W., Shiu, E.Y.C, Milton DK CB. Respiratory virus shedding in exhaled
breath and efficacy of face masks. Nat Med (2020). 2020. https://doi.org/10.1038/s41591-020-
0843-2.
32. Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid
dissemination of novel coronavirus (SARS-CoV2). Science (New York, N.Y.).
2020:eabb3221. https://www.ncbi.nlm.nih.gov/pubmed/32179701. doi:
10.1126/science.abb3221.
33. Liang M et al. Efficacy of face mask in preventing respiratory virus transmission: A
systematic review
and meta-analysis. . 2020. https://doi.org/10.1101/2020.04.03.20051649.
34. Liu X, Zhang S. COVID‐19 : Face masks and human‐to‐human transmission . Influenza
and other respiratory viruses. . https://onlinelibrary.wiley.com/doi/abs/10.1111/irv.12740.

Research Question • 29
35. Lo JYC, Tsang THF, Leung Y, Yeung EYH, Wu T, Lim WWL. Respiratory infections during
SARS outbreak, hong kong, 2003. Emerging infectious diseases. 2005;11(11):1738-
1741. https://www.ncbi.nlm.nih.gov/pubmed/16318726. doi: 10.3201/eid1111.050729.
36. Ma Q, Shan H, Zhang H, Li G, Yang R, Chen J. Potential utilities of mask-wearing and
instant hand hygiene for fighting SARS-CoV-2. Journal of medical virology.
2020. https://www.ncbi.nlm.nih.gov/pubmed/32232986. doi: 10.1002/jmv.25805.
37. MacIntyre CR. COVID-19, shortages of masks and the use of cloth masks as a last
resort. BMJ Open. 2020. https://bmjopen.bmj.com/content/5/4/e006577.responses#covid-19-
shortages-of-masks-and-the-use-of-cloth-masks-as-a-last-resort.
38. MacIntyre CR, Chughtai AA. Facemasks for the prevention of infection in healthcare and
community settings. BMJ : British Medical Journal. 2015;350(apr09
1):h694. http://dx.doi.org/10.1136/bmj.h694. doi: 10.1136/bmj.h694.
39. MacIntyre CR, Seale H, Dung TC, et al. A cluster randomised trial of cloth masks
compared with medical masks in healthcare workers. BMJ Open.
2015;5(4):e006577. http://dx.doi.org/10.1136/bmjopen-2014-006577. doi: 10.1136/bmjopen-
2014-006577.
40. MacIntyre CR, Chughtai AA. A rapid systematic review of the efficacy of face masks and
respirators against coronaviruses and other respiratory transmissible viruses for the
community, healthcare workers and sick patients. International Journal of Nursing Studies.
2020:103629. http://dx.doi.org/10.1016/j.ijnurstu.2020.103629. doi:
10.1016/j.ijnurstu.2020.103629.
41. Makison Booth C, Clayton M, Crook B, Gawn JM. Effectiveness of surgical masks against
influenza bioaerosols. Journal of Hospital Infection. 2013;84(1):22-
26. https://www.clinicalkey.es/playcontent/1-s2.0-S0195670113000698. doi:
10.1016/j.jhin.2013.02.007.
42. Offeddu V, Yung CF, Low MSF, Tam CC. Effectiveness of masks and respirators against
respiratory infections in healthcare workers: A systematic review and meta-analysis. Clinical
infectious diseases : an official publication of the Infectious Diseases Society of America.
2017;65(11):1934-1942. https://www.ncbi.nlm.nih.gov/pubmed/29140516. doi:
10.1093/cid/cix681.
43. Pan Y, Zhang D, Yang P, Poon LLM, Wang Q. Viral load of SARS-CoV-2 in clinical
samples. The Lancet Infectious Diseases. 2020;20(4):411-
412. http://dx.doi.org/10.1016/S1473-3099(20)30113-4. doi: 10.1016/S1473-3099(20)30113-4.
44. Parry J. Covid-19: Hong kong government supplies reusable face masks to all
residents. BMJ. 2020;369:m1880. http://dx.doi.org/10.1136/bmj.m1880. doi:
10.1136/bmj.m1880.
45. Pless B. Risk compensation: Revisited and rebutted. Safety.
2016;2(3):16. https://search.proquest.com/docview/2124776975. doi: 10.3390/safety2030016.

Research Question • 30
46. Raina MacIntyre C, Jay Hasanain S. Community universal face mask use during the
COVID 19 pandemic-from households to travellers and public spaces. Journal of travel
medicine. 2020;27(3). https://www.ncbi.nlm.nih.gov/pubmed/32307526. doi:
10.1093/jtm/taaa056.
47. Rengasamy S, Eimer B, Shaffer RE. Simple respiratory Protection—Evaluation of the
filtration performance of cloth masks and common fabric materials against 20–1000 nm size
particles. The Annals of occupational hygiene. 2010;54(7):789-
798. https://www.ncbi.nlm.nih.gov/pubmed/20584862. doi: 10.1093/annhyg/meq044.
48. Rodriguez-Palacios Aea. Textile masks and surface covers – A ‘Universal droplet reduction
model’ against respiratory pandemics. . 2020. https://doi.org/10.1101/2020.04.07.20045617.
49. Saunders-Hastings P, Crispo JAG, Sikora L, Krewski D. Effectiveness of personal
protective measures in reducing pandemic influenza transmission: A systematic review and
meta-analysis. Epidemics. 2017;20(C):1-20. https://www.clinicalkey.es/playcontent/1-s2.0-
S1755436516300858. doi: 10.1016/j.epidem.2017.04.003.
50. Seres G et al. Face masks increase compliance with physical distancing recommendations
during the COVID-19 pandemic (pre-print). . 2020. https://osf.io/db8sj/.
51. Tam VC, Tam SY, Poon WK, Law HKW, Lee SW. A reality check on the use of face masks
during the COVID-19 outbreak in hong kong. EClinicalMedicine.
2020:100356. http://dx.doi.org/10.1016/j.eclinm.2020.100356. doi:
10.1016/j.eclinm.2020.100356.
52. Tian L ea. Calibrated intervention and containment of the COVID-19 pandemic . .
2020. https://arxiv.org/abs/2003.07353.
53. To KKW et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and
serum antibody responses during infection by SARS-CoV-2: An observational cohort
study. Lancet Infectious Diseases. 2020. https://doi.org/10.1016/S1473-3099(20)30196-1.
54. Tracht SM, Del Valle SY, Hyman JM. Mathematical modeling of the effectiveness of
facemasks in reducing the spread of novel influenza A (H1N1). PloS one.
2010;5(2):e9018. https://www.ncbi.nlm.nih.gov/pubmed/20161764. doi:
10.1371/journal.pone.0009018.
55. van der Sande M, Teunis P, Sabel R. Professional and home-made face masks reduce
exposure to respiratory infections among the general population. PloS one.
2008;3(7):e2618. https://www.ncbi.nlm.nih.gov/pubmed/18612429. doi:
10.1371/journal.pone.0002618.
56. Wang D. et al. Selection of homemade mask materials for preventing transmission of
COVID-19: A laboratory study . . 2020. https://doi.org/10.1101/2020.05.06.20093021.

Research Question • 31
57. Wang Y et al. Reduction of secondary transmission of SARS-CoV-2 in households by face
mask use, disinfection and social distancing: A cohort study in beijing, china . .
. http://press.psprings.co.uk/bmjgh/may/gh002794.pdf.
58. Wang M, Zhou M, Ji G, et al. Mask crisis during the COVID-19 outbreak. European review
for medical and pharmacological sciences.
2020;24(6):3397. https://www.ncbi.nlm.nih.gov/pubmed/32271457.
59. Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic
disparities. JAMA. 2020. https://www.ncbi.nlm.nih.gov/pubmed/32391864. doi:
10.1001/jama.2020.8598.
60a. Wei Li, Bo Zhang, Jianhua Lu, Shihua Liu, Zhiqiang Chang, Cao Peng, Xinghua Liu, Peng
Zhang, Yan Ling, Kaixiong Tao, Jianying Chen, Characteristics of Household Transmission of
COVID-19, Clinical Infectious Diseases, , ciaa450, https://doi.org/10.1093/cid/ciaa450
60. Wei WE LZ, Chiew CJ, Yong SE, Toh MP, Lee VJ. Presymptomatic transmission of SARS-
CoV-2 — singapore, january 23–March 16, 2020. MMWR morbidity and mortality weekly
report. MMWR Morbidity and mortality weekly
report. 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6914e1.htm.
61. Wei WE, Li Z, Chiew CJ, Yong SE, Toh MP, Lee VJ. Presymptomatic transmission of
SARS-CoV-2 - singapore, january 23-march 16, 2020. MMWR. Morbidity and mortality weekly
report. 2020;69(14):411-415. https://www.ncbi.nlm.nih.gov/pubmed/32271722. doi:
10.15585/mmwr.mm6914e1.
62. Worby C CH. Face mask use in the general population and optimal
resource allocation during the COVID-19 pandemic. .
2020. https://doi.org/10.1101/2020.04.04.20052696.
63. World Health Organization. Advice on the use of masks in the context of COVID-
19. https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-
during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-
ncov)-outbreak Web site. https://www.who.int/publications/i/item/advice-on-the-use-of-masks-
in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-
coronavirus-(2019-ncov)-outbreak. Updated 2020. Accessed June 5, 2020.
64. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients
with COVID-2019. Nature. 2020. https://www.ncbi.nlm.nih.gov/pubmed/32235945. doi:
10.1038/s41586-020-2196-x.
65. Yan J, Guha S, Hariharan P, Myers M. Modeling the effectiveness of respiratory protective
devices in reducing influenza outbreak. Risk Analysis. 2019;39(3):647-661. doi:
10.1111/risa.13181.

Research Question • 32
66. Yancy CW. COVID-19 and african americans. JAMA.
2020;323(19):1891. https://www.ncbi.nlm.nih.gov/pubmed/32293639. doi:
10.1001/jama.2020.6548.
67. Yu J, Yen H, Huang H, et al. SARS-CoV-2 viral load in upper respiratory specimens of
infected patients. The New England Journal of Medicine. 2020;382(12):1177-
1179. http://dx.doi.org/10.1056/NEJMc2001737. doi: 10.1056/NEJMc2001737.
68. Zhang L, Peng Z, Ou J, et al. Protection by face masks against influenza A(H1N1)pdm09
virus on trans-pacific passenger aircraft, 2009. Emerging infectious diseases.
2013;19(9):1403-1410. https://www.ncbi.nlm.nih.gov/pubmed/23968983. doi:
10.3201/eid1909.121765.
