
Best Practices for Nutrition,
Food Service and Dining in
Long Term Care Homes
A Working Paper of the Ontario LTC Action Group
2019
www.dietitians.ca
l
www.dietetistes.ca
© Dietitians of Canada. 2019. All rights reserved.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE ii
Acknowledgements
The Ontario LTC Action Group provided their expertise and input to this revision of Best Practices. The leadership of these
individuals is gratefully acknowledged for the 2019 revision:
Dale Mayerson RD – research Julie Urbshott RD
Karen Thompson RD – editor Tara Pfab RD
Sharon Armstrong RD Stacey Scaman RD
Alicia Marshall RD Julie Cavaliere RD
Natalie Naor RD Carol Donovan RD
Monique Pigeon RD Leslie Whittington-Carter RD
Thanks to Dr. Heather Keller for review and guidance, and to Jennifer Buccino for supporting the project.
The leadership of these individuals is gratefully acknowledged for the 2013 revision:
Christine Barker RD
Julie Cavaliere RD
Mary Fitzpatrick RD, Past Chair of the LTCAG and lead on the 2007 version
Margaret Leaver-Power RD
Dale Mayerson RD
Marsha Rosen RD
Karen Thompson RD
Leslie Whittington-Carter RD

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE iii
Table of Contents
ORGANIZATION AND ADMINISTRATION .......................................................................................................... 2
!
MENU PLANNING .......................................................................................................................................... 4
!
STANDARDIZED FOOD PRODUCTION ............................................................................................................ 10
!
NUTRITION AND HYDRATION CARE ............................................................................................................... 12
!
MEAL SERVICE AND PLEASURABLE DINING .................................................................................................. 34
!
CONTINUOUS QUALITY IMPROVEMENT (CQI) ............................................................................................... 42
!
CONCLUSION ............................................................................................................................................. 43
!
Comments / Questions / Concerns ............................................................................................................. 43
!
Sample Forms and Policies ......................................................................................................................... 44
!
RESOURCES and SELECTED REFERENCES ..................................................................................................... 58
!

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE iv
Acronyms used in this document:
BMI Body Mass Index
CHO Carbohydrates
CQI Continuous Quality Improvement
CSNM Canadian Society of Nutrition Managers
DRI Dietary Reference Intakes
EHR Electronic Health Record
GI Gastrointestinal
HACCP Hazard Analysis and Critical Control Points
LTC Long Term Care
MD Doctor of Medicine
NCP Nutrition Care Process
NM Nutrition Manager
OSNM Ontario Society of Nutrition Management
OT Occupational Therapist
PEN Practice Based Evidence in Nutrition
POA Power of Attorney
PES Problem, Etiology and Signs and Symptoms
PT Physiotherapist
QI/RM Quality Improvement/Risk Management
RAI-MDS Resident Assessment Instrument - Minimum Data Set
RD Registered Dietitian
RHA Resident Home Area
RN Registered Nurse
SDM Substitute Decision Maker
SLP Speech Language Pathologist
Introduction
Best practices in the nutrition, food service and dining program incorporate the home’s vision and mission and
provide systems and processes to:
• Support, promote and respect residents’ rights, safety, security, comfort, choice, autonomy and decision-
making
• Recognize that quality nutrition, hydration and pleasurable dining enhance the “quality of life” and the
“quality of care” for residents in LTC
• Embrace a holistic approach, recognizing that food, beverages and pleasurable dining influence residents’
psychological and social well-being as well as their physical well-being
• Take into account residents’ past history and how their history influences their food preferences and how we
address their nutritional needs
• Recognize that the ability to feed oneself is a basic component of an individual’s feeling of self-worth and
autonomy and therefore incorporates a supportive and restorative dining component to maintain, support
and/or regain residents’ self-feeding skills
• Embrace both interprofessional collaboration and an interdisciplinary care team approach to support
residents’ health and well-being
Ongoing consultation with the residents, family, substitute decision makers/powers of attorney (SDM/POA) and
members of the LTC home/facility’s interdisciplinary care team is required to ensure best practices continue to meet or
exceed residents’ needs and expectations and continue to reflect the home’s philosophy of care.
Best practices for the nutrition, food service and dining program recognize that quality nutrition, hydration and dining
is achieved by meeting the goals of these five components:
• Organization and Administration
• Menu Planning
• Food Production
• Nutrition and Hydration Care
• Meal Service and Pleasurable Dining
BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 2
ORGANIZATION AND ADMINISTRATION
Best practices ensure that the nutrition, food service and dining program is organized and administered to effectively
and safely provide resident-focused nutrition care and services that reflect the mission and philosophy of the home, meet
current residents’ needs and expectations and are in keeping with professional practice, standards of care, applicable
governing/ministry acts, regulations, and directives.
Best practices require that protocols, policies, procedures and tools for administration and organization include, as a
minimum, processes for developing and implementing the following:
Mission, Goals and Objectives
• A program or department mission/vision/philosophy statement reflecting the home’s mission statement
• Specific, timely and measurable long-term goals
• Specific, timely and measurable short-term objectives
Human Resources
• Effective allocation of resources and utilization review
• Staffing qualifications required to provide a quality program, including:
- Registered dietitian (RD): member in good standing of the provincial regulatory body
- Nutrition manager (NM): member in good standing of the Canadian Society of Nutrition Management and/or
provincial alternative
- Cooks: qualified, with appropriate trade papers
- Food/Nutrition department employees: have completed or are enrolled in a recognized Certified Food Service
Worker Training program that is completed within 3 years of hire date
• Adequate and consistent staffing pattern improves communication with and between residents and staff and
help to know residents and their wishes
• Written job descriptions and job routines defining the overall roles, functions and specific duties of each
position as well as timeframes for completion of duties
Staff Education
• Frequency of training is determined by home priorities, by audit and survey results and other feedback
• All home staff receive orientation to food and nutrition services upon hire
• Staff involved in meal and snack service receive education/training on nutrition and hydration. Topics may
include:
- Basic therapeutic diets
- Food texture
- Fluid consistency
- Food safety
- Customer service/hospitality training
- Knowledge of dementia and responsive behaviours
- Ability to recognize, report and document signs and symptoms of dysphagia

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 3
- Eating assistance
- Person/relationship-centered care
- Promoting and improving the mealtime experience
• All Food/Nutrition Staff receive education/training on topics such as:
- Food safety, temperature control, dining service, nutrition related health concerns and other topics as
needed
- Proper preparation, testing and storage of all levels of texture modified foods and thickened fluids to ensure
production of food and fluids consistent with developed texture expectations
Sanitation and Safety
• Policies/protocols for all staff involved in food handling/dining service
• Housekeeping and sanitation programs to ensure the provision of safe food in a safe, sanitary environment
• Preventative Maintenance Program for all equipment used in meal preparation and service as well as
equipment required for clinical assessment and monitoring of residents’ nutrition and hydration care
Communication
Interdisciplinary and Interdepartmental Communication includes:
• Effective communication and documentation processes and tools that provide new information to
interdisciplinary care team members. This may include recent memos, minutes of recent team meetings,
dining room concerns relating to production guidelines, recipes, quantities and other pertinent information.
• Accountability by all appropriate team members for reading the previous communications back to the last
shift they worked and for reporting/documenting any incidents or concerns that occurred during their shift.
• Accountability for taking and documenting corrective actions as required and for following communications
as provided.
• Policies to ensure that privacy is maintained in all communication in adherence with federal and provincial
laws.
• Development of interdisciplinary programs involving nutrition, hydration and dining; e.g. bowel management
and continence, skin and wound care, etc.
• Representation of the Nutrition and Food Service Department by the dietitian, NM or delegate at resident care
conferences, and interdisciplinary care team meetings including: Medical/Professional Advisory,
Palliative/End of Life Care, Accreditation, Wound Care, Dysphagia, Restorative Care, Pharmacy and
Therapeutics, QI/RM (Quality Improvement/Risk Management), Infection Control, Occupational Health and
Safety and other meetings/committees as appropriate.
Protocols, Policies, Procedures and Tools
• Policies exist that support the components of Food Service and Dining Programs
- Organization and Administration
- Menu Planning
- Food Production
- Nutrition and Hydration Care
- Meal Service and Pleasurable Dining
BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 4
MENU PLANNING
The master menu is planned so that residents are provided with appetizing foods and fluids appropriate for their health
and personal requirements, cultural and religious needs/practices and quality of life. Menu planning encompasses all
foods and beverages to be provided daily to residents. The master menu includes a minimum of three meals, three
additional beverage opportunity passes and two snacks daily.
Menus accommodate residents’ nutrition and hydration needs and preferences as much as possible.
Types of Menus
• Cycle menus are planned and revised on a regular basis, at least annually. Menu is 3 to 4 weeks per cycle for
optimal variety, unless otherwise requested by residents.
• There is a menu for mid-morning drink, mid-afternoon snack and drink, and evening snack and drink that are
included in the menu cycle. Snacks are considered as opportunities to promote hydration and nutrition, through
nutrient dense offerings.
• All menus for meals and snacks include therapeutic and texture modified food and fluid options.
• An emergency non-selective menu plan is in place, covering 3 days at a minimum. Texture modifications are
considered by including as many foods as possible that are appropriate for multiple textures.
• In addition, food and beverages are available for residents on a 24-hour basis.
Menu and Meal Evaluation
• Residents, family members, SDM/POA, other designated parties and appropriate team members are consulted
and involved in the menu planning and approval process to ensure menus reflect current residents’ social, ethnic,
cultural and religious practices and needs.
• A residents’ food committee can be established for planning and approving cycle menus and special occasion
menus.
• Residents’ preferences and appetites are routinely assessed. This assessment could include: information from
residents’ satisfaction questionnaires, Residents’ Council and/or Food Committee comments, results of dining
audits, feedback from front line Food/Nutrition and Nursing staff, as well as plate waste records in the menu
planning and evaluation process.
• Regular observations by dietitian, NM and dining room staff and informal conversations with residents are
important components of the evaluation process.
Menu Planning Standards, Guidelines and Considerations
Menus are:
• revised a minimum annually, with adjustments made for seasonal preferences (Spring/Fall).
• designed to provide adequate nutrition, variety and choice for all residents.
• assessed, documented and planned, based on residents’ preferences regarding variety and frequency of menu
items. Variety guidelines may be developed and reviewed with the residents prior to each revision.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 5
• planned to meet DRIs and balance and/or control the amount of sugars, sodium and fats in the diet so that fewer
interventions are required to help maintain good health and control disease. Menus include adequate dietary
fibre and fluids.
• relatively consistent in Calories from day to day, served at consistent times, with controlled portions and
generally small servings of desserts.
• planned using meal day patterns and portion sizes for both food and fluids for all textures.
• planned to include fresh seasonal foods and local foods, in keeping with budget limitations and availability.
• feasible from a labour and production perspective, based on collaboration between the dietitian and NM.
Therapeutic and Texture Modified Menus
It is widely accepted that the quality of life of older residents in LTC homes may be enhanced by a liberalized dietary
approach. In keeping with current practice, standard therapeutic diet menus are created using the regular menu as a
base, and are used as needed, based on the dietitian and interdisciplinary care team’s assessment.
• The dietitian, in collaboration with the interdisciplinary care team, bases therapeutic menus on the needs of the
resident population, i.e. types of therapeutic diets, texture-modified foods, modified fluid consistencies, specific
snacks and supplements required
• Therapeutic and texture modified menus follow the regular menu as closely as possible to provide similar choice,
variety and palatability, based on the dietitian’s professional judgment to maximize intake and quality of life.
• Therapeutic diets are sufficiently flexible to allow for liberalization where appropriate; some residents may prefer
to follow a more tightly controlled therapeutic diet and this option should also be available.
• Residents with dementia and other similar conditions may benefit from finger foods. These options can facilitate
increased oral intake, independence and self-feeding. Finger foods may be considered a type of texture
modification.
• The menu is developed with consistent ilar levels of carbohydrates and calories over meals and from day to day
to help stabilize blood glucose levels without further limiting or restricting the diet.. This means that the menu
offers similar levels of CHO for each breakfast, similar CHO for lunches and similar CHO for suppers. Meals for all
residents are consistent in Calories from day to day, served at consistent times, with controlled portions and
generally small servings of desserts.
• The dietitians and NM in each home collaborate to ensure modifications made to the menu are feasible each
day from a labour and production perspective.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 6
IDDSI
The International Dysphagia Diet Standardisation Initiative (IDDSI) promotes standardization of food textures and fluid
consistencies to maintain safety for individuals with dysphagia. IDDSI provides a methodology to ensure that foods and
fluids are prepared in a standardized way to provide more consistent foods and fluids to residents. Their goal is to avoid
confusion and serious, sometimes fatal, outcomes of LTC residents receiving different textures when moving between
different healthcare settings. LTC homes should connect with their local hospitals and other community partners to learn
whether they are changing to IDDSI protocols, in order to ensure that residents are safe when transferred to hospital
emergency or when admitted as an inpatient.
IDDSI
IDDSI graphic: The International Dysphagia Diet Standardisation Initiative 2016 @http://iddsi.org/framework/.Attribution is NOT
PERMITTED for derivative works incorporating any alterations to the IDDSI Framework that extend beyond language translation.
Refer to the IDDSI website at www.iddsi.org for a detailed explanation of the specific descriptions for each of the food
and fluid textures, as well as tools and training aids.
IDDSI is a voluntary standard that has been supported internationally for use with residents with dysphagia. Significant
time and resources are required from the entire care team, specifically the dietitian and Nutrition Manager, to implement
IDDSI.
In deciding on the use of IDDSI it is important to remember that the food and fluid textures cannot be modified in any
way. Residents, however, have the right to refuse the texture defined by IDDSI, such as the use of gelled bread for all
textures except the regular texture. (e.g. Level 4 minced & moist; allow bread [which is considered a Level 6 regular
texture).

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 7
Options for LTC homes to consider in the implementation of IDDSI:
• Consider the most simplified option of educating staff so they can identify and safely use food and fluid textures
of food manufacturers who are using IDDSI terminology.
• Decide to partially or gradually implement IDDSI. This may involve implementing only the IDDSI levels that best
meet the residents’ needs and keeping some of the home’s previous textures names and descriptions. If the LTC
home decides to select this option, it is important to remember to have references available for staff to translate
an IDDSI diet order to the LTC home diet order. This may be needed on admission of a new resident or a return
from hospital where the IDDSI diets are being used.
• Decide to wholly implement IDDSI and use the new terminology in every aspect of care and service, including
menus, recipes, assessments and Nutrition and Hydration Care Plans, in order to be in step with other health
care facilities in the community.
Initial Plan
For individual homes, the process to work towards aligning with IDDSI may include developing and articulating:
• A clear understanding of the IDDSI requirements and how to use these guidelines in providing safe food and
fluid textures
• A map of current food textures and fluid consistency with the IDDSI framework
• The feasibility of adopting this framework either in part or in whole (including naming conventions)
• An action plan with responsibilities and timelines specified
Food Preparation
• All recipes for pureed and minced foods and for all thickened fluids are revised using specified testing methods
as needed to meet IDDSI parameters. There is clear and consistent terminology for the naming of food and fluid
textures for recipes and menus, and a description of each texture is readily available for all staff.
• Standardization of mincing and pureeing equipment and methods are improved in the home. Standardized
(IDDSI specified) testing methods are used to ensure the foods and fluids meet the criteria for the named level
of IDDSI diet at point of service.
• A review of all purchased texture modified foods is completed using the standardized testing methods to
determine whether they meet new criteria. Suppliers are consulted to determine their plans to change to IDDSI
terminology.
Communications / Training
• An approved, standardized dysphagia screening tool is used that includes IDDSI terminology to identify and
determine resident risk of dysphagia
• Intensive training for Cooks and Food Service Workers is provided on preparation and testing of products.
• Awareness training for all LTC home staff involved in meal or snack time assistance, regardless of the degree of
implementation of IDDSI
• Changes are communicated to residents and families prior to implementation. See http://iddsi.org/resources/
for communication tools.
• Relevant policies and procedures are revised and staff are educated on these changes.
BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 8
• Changes are incorporated into the quality improvement program.
Nutrient Analysis
A well-developed menu provides foods that are nutrient dense, taking into account guidelines for adequate Calories,
protein, dietary fibre, healthy fats, sodium, vitamins and minerals. Since many residents are unable to consume large
quantities, the nutrient density of menu choices is very important.
• A nutritional analysis is completed each time a new or updated menu is introduced and at a minimum, on an
annual basis. Pureed menus in particular are evaluated to ensure that they provide adequate Calories, protein,
fibre and other nutrients.
• Nutrient analysis of the menu is completed using appropriate software. Manual analysis of the menu is not
recommended due to the extensive time required and likelihood for inaccuracy.
• Note: nutrient analysis of the menu is only accurate if product specifications, recipes, and portion sizes are
followed. Standard production and service systems must be in place to ensure that the planned menu is
prepared and served accurately.
• Generally nutrient analysis of the menu includes all items that could be chosen by the residents (first choice
analyzed separately from second choice). It is recognized that most residents will not consume all of the foods
and beverages that are included on the menu, and that an individual resident’s intake will differ from the analysis
of the total menu.
• Due to the time commitment required for analysis and adjustment of the menu, specific time allocation is
required for the dietitian so that other responsibilities can also be completed.
• The menu is planned to meet the home’s residents’ needs, and is based on the current Canada’s Food Guide
and Dietary Reference Intakes (DRI). Note: guidance on applying CFG to healthcare menu planning is expected
from Health Canada.
• Where it is identified that the menu does not meet the DRI, a plan is developed for appropriate changes to be
made as soon as possible, and if not possible, then on the next version of the menu. Note: it is challenging to
attain the RDA for several nutrients (e.g. vitamin D and E) for the older age group from food alone.
Menu Approval
• As part of the evaluation, the dietitian evaluates and approves all menus, including therapeutic and texture
modified variations and ensures that there is evidence of menu consultation with residents.
• The dietitian completes a menu approval tool (see sample in forms section), signs off and ensures the NM and
home administrator each have a copy of the completed tool.
Protocols, Policies, Procedures and Tools
• Standardized recipes and portion sizes are developed and used consistently for each menu item. This includes
all foods and fluids that are modified in texture or consistency.
• There is a policy and procedure to address development of individualized menus when the needs of a resident
cannot be met by the standard, therapeutic or texture modified menus. Examples may include gluten free,
vegetarian, multiple food allergies/intolerances, or complex renal diets. When several residents follow a similar

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 9
diet (e.g. vegetarian) then a standard menu may be considered. Individualized menus may be needed for
therapeutic and texture-modified combinations or other multiple diet types.
• There is a policy and procedure that addresses the needs of residents who request cultural- or religious-specific
food choices. This may include parameters for choice and variety, resident and family input, cost responsibilities,
etc.
• There is a policy and procedure that defines alternate portion sizes such as smaller or larger portions for
residents who require or request them. This provides clear directions to staff and ensures accuracy in assessment
by the dietitian and documentation in the nutrition and hydration care plan.
• Weekly and daily menus are posted in a common area in or near the dining room for residents and families to
see. Font size is as large as is possible and practical.
• Financial analysis of menus allows decisions to be made so that menu includes optimal amounts of healthy
options with adequate protein sources. Menu cost per resident per day at least meets the Ministry of Health and
Long Term Care funding envelope for raw food.
• Education about basic therapeutic diets, food texture and fluid consistency modification is provided to all
Interdisciplinary Care Team members. The importance of following the therapeutic menu in the delivery of quality
nutrition and hydration care is emphasized.
Menu planning is a complex process and requires the development of a plan with specific steps. See sample menu
implementation policy in the Resources section.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 10
STANDARDIZED FOOD PRODUCTION
All food and beverages are prepared and provided in a clean, safe environment using methods that consistently result in
nutritious, safe and personally acceptable meals for residents.
Purchasing/Receiving/Storing
Processes for food production ensure all menu items and food products are purchased, received, stored, prepared and
served to:
• Ensure appropriate food product selection considering quality, cost and acceptance by residents
• Prevent contamination, spoilage and food-borne illness
• Retain maximum nutritive value, flavour, colour, texture and appearance
• Enhance effective standardized food production
• Ensure delivery of all residents’ meals, snacks and special snacks in the correct location in a timely fashion
• Consistently result in personally acceptable and visually appealing meals and snacks for all residents
Forecasting and Planning
Standardized food production guidelines are available that indicate all food and beverages provided daily to residents.
These include a minimum of three meals, two snack and three beverage opportunities/passes, menu items for all regular
and therapeutic diets, texture modified meals, modified fluid consistencies, special snacks and nutritional supplements.
These reflect the home’s current resident population’s needs and numbers in sufficient quantities to meet residents’
requirements and expectations.
Recipes
Standardized recipes are used to prepare all food and beverages for all textures and fluid consistencies and include:
• Item name and number
• Ingredient quantities by weight, measure, volume or count
• Portion size, yield and appropriate serving utensil
• Panning information
• Method or procedure for combining ingredients
• Time and temperatures for cooking or baking
• Heating and chilling requirements at various stages of production and requirements for monitoring temperatures at
these stages as required (i.e. HACCP guidelines)
• Final internal temperatures of foods
• Production time and time required for panning/baking/heating and serving/holding
• Methods for adjusting recipe yields if required

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 11
• The initial recipe also includes instructions on how to texture modify all items, i.e. size to cut pieces prior to
processing, when to add liquid and/or thickening agent, what type of liquid to add, how to return to safe, palatable
temperatures. If a separate recipe is needed for texture-modified foods, it is noted on the original recipe.
• Instructions for texture modified items identifies whether measuring and/or processing takes place before or after
product is fully cooked
• Final portion size for texture modified products should be consistent with regular products.
Protocols, Policies, Procedures and Tools
Policies and procedures for food production include as a minimum:
• HACCP principles, including time and temperature guidelines for food purchasing, preparation, holding, service and
storage
• Purchasing procedures including ordering, receiving, food storage and delivery
• Standardized food production guidelines including portion control
• Procedures for taste testing
• Procedures for taking and documenting food temperatures, sanitation and regular calibration of thermometers
• Guidelines for safe operation of equipment
• Employee health and safety in the kitchen and food service areas
• Cleaning guidelines and schedules for production, service and ware washing areas and equipment
• Procedures for waste management, may include topics such as recycling, compost, solid waste, liquid waste,
hazardous waste e.g. broken glass

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 12
NUTRITION AND HYDRATION CARE
The most appropriate nutrition care and interventions for each resident are provided in the least restrictive and most
effective manner. The dietitian, in consultation with the resident, family, SDM/POA and interdisciplinary care team, plans
the most effective nutrition interventions that will meet the residents’ health and personal goals. All interdisciplinary front
line staff are fully trained to understand their individual roles in all aspects of nutrition and hydration care.
Consent to Treatment
Dietitians have a legal and professional responsibility to obtain consent for treatment when practicing dietetics, and to
provide residents with clear and complete information relating to the risks, benefits and consequences of giving or
refusing consent. Residents are then able to make informed decisions regarding any treatment done for a therapeutic,
preventative, palliative, diagnostic, or health related purpose; this includes a course or plan of treatment. Consent is
informed and is given by the resident voluntarily and directly if the resident is capable. Lack of informed consent may
constitute negligence or battery. Written blanket consent forms are not valid. The consent must come from a person,
not a piece of paper, unless it is an emergency.
If possible, include all discussions about key areas such as modified textured diets, thickened fluids, enteral feeding etc.,
earlier on in the admission process as some residents may be capable at time of admission but incapable after decline
occurs. Ensure these are well documented as part of the resident’s medical record. These documented responses may
aid the SDM or POA in making these nutrition and hydration decisions that will reflect the desire of the resident.
Processes are established for receiving consent to treatment, to ensure residents are appropriately informed about their
care.
How to determine whether resident is capable:
• A capable resident gives consent directly, and does not redirect the dietitian to a family member to make a
decision. residents may be able to make decisions about certain aspects of their lives and not others.
Members of the interdisciplinary care team determine whether an individual resident is deemed “capable”
to understand information that is provided for decision-making. Residents are deemed capable if they are
able to:
• Understand the information that is relevant to making a decision about the treatment, admission,
or personal assistance service as the case may be, and
• Appreciate the reasonably foreseeable consequences of a decision or lack of decision
• To obtain consent, the health professional and the resident discuss nutrition interventions and the reasons
for them. The health professional provides ample time and clear explanations and repeats up to three times,
in three different ways to explain the nutrition intervention or plan fully. Education, good observational
skills, strong advocacy and consistent relationships with caregivers enable a resident with impaired
decision- making capacity to make choices for their nutrition care.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 13
Resident deemed capable
• The information about the treatment preferences and/or decision is discussed amongst the team, including the
resident (and POA/SDM if agreeable to the resident) and only then an agreed-upon choice is made.
• If the resident is sufficiently informed about the risks and benefits of acceptance (informed consent) or refusal
(informed refusal) of a proposed intervention or treatment and refuses, the dietitian respects the resident’s
decision. Each capable resident has the right, once properly informed, to refuse treatment or recommendations
and disregard clinical advice, and not be labelled as “non-compliant”.
• When a resident makes a “risky” decision, the plan of care is adjusted to honour informed choice and provide
supports available to mitigate the risks. The dietitian will follow the prescribed protocol for advising
Administration and/or Director of Care/Nursing when there is a risk situation.
Resident deemed not capable
• If the dietitian believes the resident is not capable, s/he can ask for informed consent from the resident’s power
of attorney for care. If there is no POA, then informed consent is given by the resident’s specified substitute
decision maker (SDM).
• It is important that the dietitian and care team educate the POA or SDM on the same recommendations, risk and
benefits to allow them to make an informed decision regarding the plan of care for the resident. It is important
to ensure that the SDM or POA is acting in the best interest of the resident and not making decisions based on
their own desires or preferences. Involving the care team and other disciplines such as social work, may be
advisable.
Documentation
The dietitian documents each step of the process in detail, being specific and including trials, agreements and refusals
for care or treatment. The agreed upon plan of care is then revised and monitored to make sure the home is best meeting
the resident's needs.
Nutrition Care Process (NCP)
Standard nutrition care process is a systematic approach for dietitians to consistently address practice-related nutrition
problems and uses a client-centered framework that clarifies the dietitian’s role. NCP provides uniform documentation of
nutrition care services, and therefore improves client outcomes by clearly identifying nutrition problems through
diagnosis and choosing specific interventions to resolve each one. Use of well-designed, customized computerized
systems supports a more consistent and efficient NCP.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 14
NCP includes:
- Nutrition assessment - collection and documentation of information such as food or nutrition-related history,
biochemical data, anthropometric measurements, results of medical tests and procedures, and other
relevant data and history
- Nutrition diagnosis - the naming of specific problem that requires intervention, or a PES statement, which is
composed of three distinct components: the problem (P), the etiology (E), and the signs and symptoms (S).
The format for the nutrition diagnosis statement is problem (P) related to etiology (E) as evidenced by signs
and symptoms (S). The use of PES statements standardizes and summarizes main nutrition problems or
issues that will be targeted through intervention.
- Nutrition interventions - interventions aimed at alleviating the signs and symptoms of the diagnosis
- Nutrition monitoring and evaluation - determination if the resident has achieved, or is making progress
toward, the planned goals
Learn more about the Nutrition Care Process Standardization at https://www.dietitians.ca/Dietitians-Views/Health-
Care-System/NCP-and-IDNT.aspx
Nutrition Assessment, Care Planning, Monitoring
Initial and Ongoing Assessment Process
Processes are established for initial and ongoing nutrition assessments and screening, to identify nutrition risk issues
that require dietitian intervention. These can include the following criteria and steps:
• Interdisciplinary care team collects basic information within 24 hours of admission that allows safe and
appropriate meal service (e.g. food allergies and/or intolerances, food texture and fluid consistency
requirements, assistive devices)
• Communication with other care providers (e.g. primary health care, homecare, acute care, retirement home)
to determine history and previous nutrition interventions
• Nutrition manager or other team member collects basic dietary information for each resident during the first
week of admission and observation period; e.g. food likes and dislikes
• Interdisciplinary care team completes the RAI-MDS or equivalent assessment of resident
• Dietitian completes a timely nutrition assessment that identifies resident’s nutrition, hydration and dining
needs and nutrition and hydration risk issues. Time frames may be based on home’s policy or RAI-MDS
requirements
The Nutrition Assessment
The nutrition assessment uses biochemical & physical measurements and clinical analysis including, but not limited
to:
• Current height and weight status and historical weight data if available
• Current diet, food texture, fluid consistency
• Dietary history and current documented food and fluid intake
• Vitamin or mineral supplements
• Use of herbal supplements or other complementary and alternative medicine

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 15
• Need for and use of oral nutritional supplements
• Relevant conditions and diagnoses, including those known to be of particular risk to this population
• Physical and cognitive functioning
• Self-feeding ability and need for assistance
• Skin integrity
• GI/bowel function/issues
• Significant lab values
• Medications and potential food-drug interactions
• Dentition, chewing or swallowing concerns
• Allergies and/or food intolerances
• Preferences and food practices related to culture and/or religion
• Daily nutritional requirements
Care Planning
• The Dietitian consults with the interdisciplinary care team and resident, to develop an individualized Nutrition
and Hydration Care Plan, to maintain/restore/optimize nutrition health and hydration status
• The Nutrition and Hydration Care Plan indicates problem/focus, interventions, interdisciplinary care team
member(s) responsible for providing interventions, desired outcomes, expected reassessment date and
resident’s (SDM/POA/s if appropriate) response to the plan
• Interdisciplinary care team implements the Nutrition and Hydration Care Plan
• Reassessment of each resident’s Nutrition and Hydration Care Plan, is completed quarterly, at a minimum,
and whenever there is a significant change in status and/or a referral for reassessment by a member of the
interdisciplinary care team
• Mechanisms are in place for monitoring and documenting each resident’s response to the Nutrition and
Hydration Care Plan and interventions that includes the following:
• Observe and document each resident’s food and fluid intake at every opportunity for intake at
every meal, beverage, snack, med pass and social activities throughout the day
• Take and record each resident’s weight, monthly as minimum, and more often as documented
according to need
• Processes and communication systems for referral to the dietitian whenever concerns are noted
regarding food/fluid intake and/or weight
• Mechanisms are in place to evaluate each resident’s response to the Nutrition and Hydration Care Plan.
Interventions are modified as required including interdisciplinary reassessment of each resident based on
individual nutrition risk issues, nutrition care needs and change in health status
• Therapeutic diets, texture and fluid consistencies, as ordered by the dietitian and/or doctor, are recorded in
the residents’ charts and communicated to the interdisciplinary care team, as per the home’s policies
• Residents are assessed by the dietitian and interdisciplinary care team to determine the support, supervision,
encouragement, and assistance required with intake of food and beverages at meal and snack-times to
promote safety, comfort, independence and dignity in eating and drinking, which include the following:

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 16
• Determine appropriate seating and positioning
• Determine those residents who would benefit from assistive devices, and types and amount of
assistance required to support and maintain self-feeding skills
• Determine the need for a Restorative Dining Program, with individual goals established for each
resident participating in such a program
• Adapt the meal times and dining environment as deemed appropriate
Liberalized Diets
Nutrition care is planned to maximize food and fluid intake and to enhance quality of life. A liberalized approach to diets
removes restrictions that may reduce residents’ food choices. Diabetic diets, lower sodium diets, and other restrictive
diets can potentially limit food choices and reduce resident food and fluid intake. In the LTC setting, it is generally
accepted that the effects of malnutrition due to decreased food intake may be a greater risk to the resident than the
benefits provided by the therapeutic diet.
Based on the dietitian’s professional judgment:
• A regular diet is provided for residents for meals and snacks, unless the resident prefers a restrictive diet or it is
essential to resident’s wellbeing and diet acceptance. Residents with clearly identified concerns may require
specific focused and individualized changes to the regular menu in order to maintain optimal health. A few
examples include residents who are: undergoing dialysis; have CHF but are not cachectic; younger or newly
diagnosed with a condition managed by diet; challenged with keeping in glycemic control with medication alone;
lactose intolerant or require a gluten-free diet.
• As part of the nutrition assessment, medications are reviewed with the physician/care team as a means to control
health concerns rather than limiting food and fluid intake.
• Residents’ previous eating patterns and their wishes to follow or not follow a specific diet to manage a health
condition are respected when determining the dietary approach. This is resident-centered care that is promoted
in LTC with the hope that it will lead to better quality of life for all residents.
• Where it is the preference of the resident or the SDM, diet restrictions are eliminated or minimized to provide
optimal variety, which in turn may lead to increased nutrient intake, and more pleasure from meals. These
strategies may have the potential to improve nutritional status, weight maintenance or weight gain and quality
of life. Unwarranted diet restrictions in LTC can lead to skin breakdown, risk of falling, and increased confusion.
A wider variety of available foods is meant to help reduce these health concerns.
• Education and discussion are provided on the liberalized diet approach with residents/SDM regarding the
resident’s individualized nutrition assessments, monitoring, and care planning. This is essential to the residents’
ongoing nutritional health and will focus on any areas of concern. Staff and families who are accustomed to
dietary restrictions may benefit from discussion and education on the liberalized diet approach in order to
understand the benefits.
• All staff are fully aware of any individualized menu changes that are based on the nutritional assessment and
are documented in the Nutrition and Hydration Care Plan. This will support accuracy in serving and is an
important part of ensuring that residents receive the appropriate foods at meals specific for their individual
needs. Liberalized approach to therapeutic diets may mean an increase in individualized interventions, which
requires staff education and systems to monitor.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 17
Common Nutrition and Hydration Care Challenges In LTC
Unplanned Weight Changes
• Unplanned weight loss in seniors is correlated with increased morbidity and mortality, functional decline,
increased rates of hospitalization leading to increased infections, pressure ulcers, falls and bone fractures.
Weight loss can be related to mental changes, eating challenges (e.g. shortness of breath, chewing difficulties),
cognitive decline (e.g. extensive oral processing of food), physical disabilities (e.g. eating challenges), and acute
medical problems (e.g. cachexia associated with CHF), and can also be affected by depression, loss of social
networks, and chronic illness. Aging and medications can change the smell and taste of food or depress appetite.
• Fluid intake and hydration status may also be responsible for fluctuations in body weight from month to month
and should be considered as part of the nutrition assessment.
• To prevent or manage unintended weight loss, there are policies in place that includes assessment and
monitoring, and interventions.
Policies and procedures are available to describe:
• when and how monthly weights are taken and documented, and when a re-weigh will be conducted.
• when and how wheelchairs are weighed and labeled
• the referral process to dietitians for residents with unplanned weight change.
• the calibration of weigh scales.
Key points for the dietitian related to weight changes:
• Monitor weight a minimum of monthly and upon return from hospital stay
• Reweigh when weight is up or down more than 2 kg from previous month
• Address any unplanned weight change up or down of 5% in one month, 7.5% in 3 months and/or 10% in 6
months
• Work with the interdisciplinary care team to establish root cause
• Take immediate action after unplanned weight loss is identified
• Determine level of nutrition risk and need for further follow-up
• Document in progress notes
• Update Nutrition and Hydration Care Plan and implement interventions
• Communicate any changes to NM and Food/Nutrition Staff for immediate implementation at point of service.
Assessment and Monitoring
• Standardized processes are in place for taking and recording accurate weights by nursing on admission, monthly,
and upon return from hospital unless otherwise specified in the care plan.
• Standardized processes are in place to record heights and to report methods used for obtaining height
measurement. There are several methods to calculate estimated height while standing or lying down, such as
ulna length and demi-span. See http://www.rxkinetics.com/height_estimate.html for detailed information.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 18
• Maintain a record of all residents’ heights and weights on admission that is taken by nursing, and include
methods of measurement.
• Monitor all residents’ weights monthly, using standardized protocol, and more frequently for identified residents.
• There is a process for referring any resident with unplanned weight change, confirmed by reweigh, of 5% change
in one month, 7.5% in three months or 10% over 6 months, if weight drops below 40 kg or if BMI is greater than
35. The dietitian completes a nutrition assessment for these residents.
• Residents are re-weighed if weight changes are significant from previous month (more than 2 kg) or if resident
has returned from hospital.
• Monitor each resident’s food and fluid intake and use this information to frequently monitor and evaluate
resident’s status as needed.
Interventions
• Initiate appropriate nutrition interventions (e.g. modifying the resident’s diet based on the resident’s current
diet/menu and documented energy intake) in consultation with the resident, family, SDM/POA and interdisciplinary
care team in order to better meet individual resident’s needs.
• Identification of unplanned weight loss should lead to early intervention, which may correct reversible nutritional
deficits. Examples of early interventions include:
• Assistance with eating or assistive devices to increase independence
• More liberalized diet to increase food and fluid variety
• Focus on food preferences, appropriate food consistency, snacks
• Changing meal environment to remove distractions or barriers to intake (ensure it is an unhurried, social,
and well-lit environment)
• Family involvement with visits or assistance at meal times
• Assessment for depression and dementia
Causes of weight loss in older adults – MEALS ON WHEELS mnemonic (widely used in research literature)
https://www.timeofcare.com/weight-loss-mnemonic-meals-on-wheels/
M
edications (e.g., digoxin, theophylline, SSRIs, antibiotics)
E
motional (e.g., depression, anxiety)
A
lcoholism, older adult abuse
L
ate life paranoia or bereavement
S
wallowing problems
O
ral factors (tooth loss, xerostomia)
N
osocomial infections (e.g., tuberculosis, pneumonia)
W
andering and other dementia-related factors
H
yperthyroidism, hypercalcemia, hypoadrenalism
E
nteral problems (e.g., esophageal stricture, gluten enteropathy)
E
ating problems
L
ow salt, low cholesterol, and other therapeutic diets
S
ocial isolation, stones (chronic cholecystitis)

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 19
9 Ds of Weight Loss in the Elderly
https://www.aafp.org/afp/2014/0501/p718.html
Dementia, dentition, depression, diarrhea, disease [acute and chronic], drugs, dysfunction [functional disability],
dysgeusia, dysphagia
Hydration
• Dehydration is estimated to be present in almost half of long term care residents. Inadequate fluid intake may
lead to increased risk of: constipation, falls, longer time for wound healing, acute confusion, decreased kidney
function, and increased hospitalizations.
• Classic signs and symptoms of dehydration include: dry mucous membranes, cracked lips, furrowed tongue,
sunken eyes, decreased salivation, decreased skin turgor, rapid pulse, weakness, and decrease in orthostatic
blood pressure.
• Risks for dehydration are greater at times of acute illness, which include fever, vomiting and diarrhea.
Dehydration concern is also greater for residents who are unable to feed themselves or have impaired cognition
and functional status. Depression and loneliness may also be psychological risks associated with dehydration.
• Prevention of dehydration can be achieved with a minimum of 1,500 to 2,400 mL/day of fluid from food or
liquids for adults weighing from 50 to 80 kg, based on the formulas listed below.
Assessment and Monitoring
• Signs and symptoms and risk factors of dehydration are identified as part of the assessment process.
• For individualized assessments, there are several calculations that can be used to estimate daily fluid
requirement:
• 25 to 30 mL fluid/kg body weight
• 1 mL fluid/Calorie needed
• 1000 mL fluid for first 10 kg actual body weight
+ 50 mL/kg for next 10 kg actual body weight
+ 15 mL/kg for each additional kg over 20 kg
• An accurate record is kept of each resident’s fluid intake on a daily basis.
• Fluid intake records are regularly monitored and compared with a resident’s estimated fluid requirements in
order to identify risk of dehydration who require referral to the dietitian.
• Laboratory values that may be indicators of dehydration include:
Serum osmolality > 295 mOsmol - most accurate test of dehydration
Urea:creatinine ratio> or = 0.15
Elevated Na
For more information, see: Woodward M. 2013. Guidelines to Effective Hydration in Aged Care Facilities. Heidelburg
Repatriation Hospital, Australia. Page 4 – 5
https://www.mcgill.ca/familymed/files/familymed/effective_hydration_in_elderly.pdf

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 20
Interventions
Staff may increase hydration using the following strategies:
• Regular rounds with a hydration cart
• Offer drinks that are known to be preferred by residents
• Offer drinks before/after bathing, toileting, brushing teeth, social activities
• Encourage drinks at each meal and snack - at each meal include water, milk, choice of juice, choice of tea
or coffee, according to the individuals’ preferences
• Encourage at least 60 ml drink at each med pass
• Identify at-risk residents (e.g. confused, refusing fluids, febrile, on diuretics) so they can be more closely
monitored
• Record fluids at meals and snacks and at med-pass and supplement intake to check for daily adequate
intake
• Assess independent intake as well as fluids offered by staff
• Develop hydration program with all staff participating, e.g. “Sip and Go”
• Educate all staff on signs, symptoms and risk factors related to dehydration, and the importance of working
together as a team to identify and immediately treat dehydration, as well as continual provision, monitoring and
recording of fluid intake.
• Hypodermoclysis (administration of isotonic fluids via a subcutaneous infusion) can be a convenient and cost-
effective alternative to hospitalization. For mild rehydration or the prevention of dehydration. This requires a
Physician’s order.
Policy Development
• A policy exists on hydration, including the times, quantities and provision of beverages throughout the day.
• Hot weather policies for hydration exist.
• Procedures are established for monitoring and documenting signs and symptoms of dehydration for each
resident.
• Procedures for documentation and corrective actions are established when fluid intake does not meet resident’s
requirements or when there is a change in the resident’s hydration status. Corrective action includes referral to
the dietitian.
• Policies are in place to manage residents with consistently low fluid intake that do not exhibit clinical signs of
dehydration or have refused interventions to increase fluid intake. Policy includes these key points:
• Establish/calculate individual fluid needs upon admission and a minimum of quarterly.
• Ensure a system to monitor fluid intake is established and anyone at risk of dehydration is identified and
immediate action is taken even if the dietitian is not onsite.
• Ensure there is a system in place to immediately notify the dietitian, NM and Food/Nutrition staff if a resident
is at risk of dehydration.
• Ensure use of a referral tool that includes dehydration.
• Work with the interdisciplinary care team to establish root cause of low fluid intake or dehydration.
• Take immediate action, implement individual interventions.
• Continue to monitor until stabilized.
• Document in progress notes and update the Nutrition and Hydration Care Plan.
• Communicate any changes to the NM and Food/Nutrition staff for implementation at point of service.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 21
Skin and Wound Care
• Poor dietary intake and increased metabolic needs can lead to malnutrition, which presents a risk for skin
breakdown. Residents who require skin and wound care management include those that may be at risk of skin
breakdown, may have already developed skin breakdown, or may have delayed wound healing.
• Nutrition considerations for skin health at initial screening and ongoing nutrition assessments include potential for
weight loss, potential for dehydration, need for assistance with meals and snacks, and overall food and fluid intake.
• The dietitian participates as a member of the interdisciplinary skin and wound care team to contribute to the overall
program for skin health and the development and implementation of best practice protocols. This includes referral
to the dietitian for all levels of pressure ulcers and other skin wounds for assessment, care planning and
establishment of hydration and nutrition interventions.
Assessment and Monitoring
• There is a process to screen nutritional status for each resident, at admission and with each quarterly assessment
that includes risk of developing or worsening skin breakdown. Referrals are sent to dietitian as required.
• Dietitian collaborates with the interdisciplinary care team to identify residents at risk of developing or worsening
skin breakdown, and a referral is sent to the dietitian for nutrition assessment and care planning.
• RD assesses each resident’s adequacy of total nutrient intake, with awareness of nutrients affecting skin health,
such as Calories, protein, fluids, micronutrients. Goals can include:
• 30 to 35 Calories per kilogram body weight
• 1 to 1.5 grams protein per kilogram body weight
• 25 to 30 ml fluids per kilogram body weight
• Additional fluids are provided in the presence of elevated ambient temperature, fever, vomiting, diarrhea,
profuse sweating, and significant fluid loss from wounds.
Interventions
• Interventions are established to address the resident’s increased needs for energy, protein, fluid and
vitamins/minerals, to promote wound healing.
• An individualized Nutrition and Hydration Care Plan is developed for residents at risk of developing or having
worsening skin breakdown.
• Fortified or nutrient dense foods and/or oral nutritional supplements may be provided between meals if
nutritional requirements are not being achieved through meals and regular snacks. An example of a fortified
food is the use of skim milk powder blended into milk, to provide extra Calories, protein and micronutrients.
• For those who require assistance with eating, food, fluid and/or supplement is provided at a time when
assistance is available.
• A vitamin/mineral supplement may be provided when dietary intake is poor or when deficiencies are confirmed
or suspected.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 22
Policy Development
Policies, procedures and protocols are developed for the Interdisciplinary Skin and Wound Care Team, including referral
to the RD for all levels of pressure ulcers and other skin wounds for assessment, care planning and establishment of
hydration and nutrition interventions. This includes the following key points:
• Establish / calculate resident’s skin status upon admission and a minimum of quarterly.
• Ensure a system to monitor skin integrity is established and anyone at risk of skin breakdown is identified and
immediate action is taken even if the RD is not onsite.
• Ensure there is a system in place to immediately notify the RD, NM and Food/Nutrition Staff if a resident is at
risk of skin breakdown including skin tears as per MOHLTC regulations.
• Work with the Interdisciplinary Health Care Team to establish root cause.
• Take immediate action.
• Implement individual interventions.
• Continue to monitor until wound is cleared.
• Determine level of nutrition risk and need for further follow-up
• Document in Progress Notes.
• Update Nutrition and Hydration Care Plan.
• Communicate any changes to NM and Food/Nutrition Staff for implementation at POS
• Policy includes notation that referral to RD may not be required for simple skin tears or stage 1 wounds, in order to
avoid over-referrals and inefficient use of the RD’s time.
Dysphagia
• Eating and swallowing are complex behaviors involving more than 30 nerves and muscles interacting together
in precision. Stroke, dementia, Parkinson’s disease, or other conditions/illnesses can cause decreased
swallowing function.
• The RD will have gained knowledge and skill to competently perform an assessment on residents’ swallowing
ability for solids and liquids. This includes identifying, analyzing, and evaluating potential risks related to feeding
and swallowing, as well as proper body positioning, and the risk of malnutrition. As with all areas of practice,
the RD is aware of his/her own limitation of skills, and continues to seek out education opportunities to continue
to learn about all aspects of dysphagia. Further education and resources can be obtained through Dietitians of
Canada and the College of Dietitians of Ontario.
• Assessment, planning, monitoring and follow up are best managed with the Interdisciplinary Care Team working
together for the benefit of the resident. A team approach is optimal, with every discipline, as well as families and
SDMs included in the assessment results, to maintain and optimize nutrition, hydration, safety, and, ultimately,
quality of life for the resident. The RD participates as a member of the Interdisciplinary Care Team, which
conducts swallowing assessments, reviews all recommendations for texture modification, thickened fluids or
enteral feeding and is responsible for approval of such recommendations.
• All aspects of assessment, planning, monitoring and follow up are documented in the resident plan of care and
health record.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 23
Assessment and Monitoring
• RD conducts the swallowing assessment as well as a nutrition assessment to address other food and nutrition
concerns. SLP may conduct the swallowing assessment depending on the nature of the swallowing disorder and
the perceived risk.
• Swallowing assessments are completed in the resident’s normal meal location and in the resident’s usual body
position for eating and drinking to determine dysphagia risk and how best to manage swallowing challenges.
Note: videofluoroscopy or fibre-optic endoscopic evaluation of swallowing is needed for diagnosis.
• The assessment may include trials of different texture modifications. RD consults with resident and/or SDM/POA
as part of the assessment.
• RD consults, communicates and collaborates with:
• Resident and family
• Nursing staff and the attending Physician on relevant diagnosis, behaviours and patterns of eating
• SLP for dysphagia assessment and interventions or videofluoroscopy for detailed swallow study and
diagnosis
• PT or OT for appropriate provisions for eating and positioning of residents for safe dining, if required.
• Food and fluid intakes are monitored to determine if there is a need for diet modification or nutritional
supplements.
Interventions
• Food and fluid modifications are important interventions for swallowing safety. This is where a decision is made
about the specific food texture and fluid consistency that is required. IDDSI protocols are recognized as the gold
standard for texture management for dysphagia.
• Residents have the right to refuse texture recommendations. The RD works with the resident, family and
healthcare team collaboratively to create a safe feeding plan that is accepted by all.
• Food molds or food piping are considered for every day or for special occasions at the point of service, to
enhance the appearance of pureed foods. Attention is also given to providing quality, appealing minced and
moist food products.
• Education of staff and families to recognize signs of dysphagia and to report and document registered nursing
staff, so the RD can be contacted
• Staff and families are trained to safely assist residents whenever eating and drinking, and how to monitor
residents’ feeding, chewing and swallowing abilities
• Negative perceptions and opinions toward texture modified foods can lead to poor intake by residents. All staff
has the opportunity to taste-test texture modified foods so that negative perceptions can be changed.
Policy Development
Policies exist for all of the above aspects of dysphagia care and menu planning and include IDDSI terminology.
• Documented protocols for texture modifications are developed and followed.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 24
• Purchased, prepared texture modified foods and modified consistency fluids are appropriate for residents’
needs.
• Broth, gravy or sauces for flavor are used instead of water for in-house pureed foods. Taste testing occurs to
monitor flavor.
• Encourage food-based thickeners primarily, since commercial thickeners have been shown to suppress the base
flavours in food.
• Standardized recipes and menus are in place, providing information on how to modify textures appropriately.
• Staff is aware of the resident’s current diet, texture and fluid consistency order, and individualized Nutrition and
Hydration Care Plan.
Diabetes
• Type 2 diabetes is a disease in which the pancreas does not produce enough insulin, or the body’s cells do not
properly use the insulin it makes. The majority of frail senior residents with diabetes in LTC have type 2 diabetes.
• Although tight glycemic controls through diet may prevent complications of diabetes in younger adults, targets
for glycemic control for older adults are more generous to avoid hypoglycemia. It has been hypothesized that a
restrictive diet may result in decreased food intake leading to unintentional weight loss and under-nutrition for
these residents.
• Concerns of complications such as renal and eye diseases become apparent only after many years of sustained
hyperglycemia and therefore are not considered to be a priority for most residents.
Assessment and Monitoring
• RD assesses residents individually to determine who may require a diabetic diet prescription e.g. residents with
Type 1 diabetes, younger residents with Type 2 diabetes, or fluctuating blood glucose levels.
• Resident and SDM preferences for diet prescription are respected
• There is a process for all staff to identify those residents who have diabetes to ensure food and fluid intake at
meals and snacks are monitored.
• Blood glucose control for all residents is managed with appropriate medications. Hemoglobin A1c is checked
every 3 to 6 months. A level of 7.1 to 8.5% is considered acceptable for frail, elderly residents with stable blood
glucose levels. For most frail elderly, the effects of hypoglycemia are a greater risk than hyperglycemia.
• Frail older residents of LTC remain at higher risk of hypoglycemia due to their advanced age, multiple
comorbidities, polypharmacy, hypoglycemia unawareness and impaired renal function and inadequate food
intake.
• Cognitive dysfunction in older people with diabetes has clearly been identified as a significant risk factor for the
development of severe hypoglycemia. As such, hypoglycemia is a more immediate concern than hyperglycemia
and should be reported to nursing staff immediately.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 25
Interventions
• Most experts agree that using medication rather than dietary changes to control blood glucose, blood lipid levels,
and blood pressure can enhance the joy of eating and reduce the risk of malnutrition for older adults in long
term care.
• Interventions are individualized in consultation with the resident and based on individual needs, personal
preferences and medical complications and comorbidities, e.g. kidney disease, liver failure, obesity.
• A more strictly regulated diet may be beneficial for functionally independent older people with diabetes who
have a life expectancy of greater than 10 years.
• A more strictly regulated diet may be considered for residents who are younger or who have Type 1 diabetes; a
more traditional diabetes diet with CHO restrictions may be of benefit to manage high blood glucose levels and
reduce the risk of micro and macrovascular complications. The RD as part of the care team in consultation with
the resident and family should make this determination.
• Residents with insulin resistance may show some improvement with a small amount of weight loss.
• Resident education may be helpful for those who are able to choose their own meals. Any physical activity can
also help to moderate high blood glucose levels.
• Staff watch for signs and symptoms of hypoglycemia and report immediately to nursing staff who will provide
treatment following the 15/15 rule: Provide 15 g of quickly absorbing carbohydrate and check blood glucose
level in 15 minutes. This may be 15 ml of sugar or honey stirred into a small glass of water or 125 ml of apple
juice. If blood glucose level is still low, repeat the process. Providing more than 15 g of CHO at one time will
result in blood glucose quickly rising to dangerously high levels. If there are more than 2 hours before the next
meal, provide a CHO-protein snack.
Policy Development
• Policies exist for management of blood glucose levels including risk of hypoglycemia, and staff education to
monitor diabetes for the frail elderly population and for the higher risk and/or younger residents.
• Policies exist for monitoring food and fluid intake at meals and snacks and for management of hypoglycemic
episodes.
Constipation Management
An international panel of experts defines chronic constipation as two or more of the following:
• Straining during at least 25% of defecations
• Straining and hard stools are often the predominant symptoms in the elderly.
• Lumpy or hard stools in at least 25% of defecations
• Sensation of incomplete evacuation for at least 25% of defecations
• Sensation of anorectal obstruction/blockage for at least 25% of defecations
• Manual maneuvers to facilitate at least 25% of defecations (e.g. digital evacuation, support of the
pelvic floor)
• Fewer than three defecations per week
Rome III diagnostic criteria http://www.theromefoundation.org/assets/pdf/19_RomeIII_apA_885-898.pdf

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 26
Older adults in long term care are at increased risk for constipation. Causes of complications may include:
• Diminished functional and cognitive ability in the frail elderly
• Immobility, poor food intake and dehydration
• Gastrointestinal transit time may be slower in the frail elderly, particularly in those who are bed-bound.
• Medications such as antihypertensives, opioid analgesics, calcium-channel blockers, antidepressants, oral iron
supplements and antidiarrheal agents are frequently used medications that can lead to constipation.
• See Beers List for more information on medications with side effects of constipation: Beers List 2015 for Canada -
http://bcbpsd.ca/docs/part-1/PrintableBeersPocketCard.pdf
Complications of constipation include:
• Symptoms of irritability or aggression
• Constipation leading to fecal impaction can present with anorexia, nausea and pain associated with functional
decline.
• Excessive straining can trigger fainting, or coronary or cerebral ischemia. Left untreated, constipation can lead to
more serious and painful conditions such as hemorrhoids, fissures and fecal impaction, leading to hospitalization.
Assessment and Monitoring
• An Interdisciplinary Team approach to planning bowel and bladder protocols is necessary, so that food, fluid and
fibre are the first means of intervention.
• Some residents may have become dependent on laxatives after years of chronic use. Depending on the severity of
the dependence, it may not be possible to relieve constipation with dietary means. The Interdisciplinary Care Team
establishes reasonable goals in this situation.
• Documentation by the Interdisciplinary Care Team, through monitoring of residents’ food and fluid intake and bowel
function, will help maintain and improve residents’ bowel function.
Interventions
• Consistent and routine toileting is promoted each day.
• The gastrocolic reflex, which results in a mass peristalsis of the gut, is strongest when the stomach is empty. For this
reason, breakfast is viewed to be the “triggering meal”, and toileting is suggested 5 to 15 minutes after the triggering
meal. Residents should place their feet on a small step stool instead of on the floor to straighten the anorectal
junction, and be allowed adequate time and privacy for bowel movements. Bedpans should be avoided.
• It is especially important to set a consistent defecation time for residents with cognitive impairment and depression
because they are at high risk to delay defecation.
• RD provides individualized interventions, in consultation with the resident and family, based on individual needs
and preferences. These may include use of fibre, especially soluble fibre such as oats and flax that has been shown
to be effective for constipation.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 27
• Fibre is added gradually to avoid flatulence, cramping and bloating, and distention. Increasing fibre is not advised
in a person who is immobile or bedbound, especially with limited fluid intake; this is to avoid impaction or
obstruction. Loose bran should be avoided as it absorbs too much liquid and could worsen constipation.
• Gradually increase fibre intake to 20–30 grams/day from fruits, vegetables, and legumes. Other food items include
flax flour, pea flour, and commercial or in-house high fibre products.
• Provide fibre supplements such as “power puddings”, “fruit spread” and fibre-dense commercial products. These
products have been used successfully to increase fibre intake in combination with a high fibre diet.
• Provide adequate fluids to manage constipation. An intake of 1500 mL fluid per day is normally cited as the
minimum amount of fluid required for normal physiological functioning of the body. Individual estimation of fluid
requirements is calculated for each resident.
• Fruits such as apples; pears; stone fruits, such as peaches, apricots and nectarines; and dried fruits, such as prunes,
dates and raisins contain sorbitol and may help manage constipation.
• Probiotics in the elderly may both shorten bowel transit time and soften stools, most likely by the increased short
chain fatty acid concentration.
Policy Development
Policies include:
• Bowel management as part of initial nutrition assessment and ongoing screening and /or assessments.
• Responsibilities of the Interdisciplinary Care Team in the management of constipation.
Nutrition Supplements and Food First Approach
• The concept of the Food First approach is to enhance quality of life for residents by normalizing their food and fluid
intake. This promotes the pleasure of providing foods and fluids over commercial nutritional supplements to meet
nutritional needs. This is often a first approach but requires evaluation on an individual basis.
• Residents receive protein and micronutrients and other food components (e.g. fibre, phytochemicals etc.) to
maintain or improve muscle mass and strength, as well as immune status, skin integrity, promote wound healing,
bone health, normalize blood pressure and achieve an appropriate weight. Nutrients are most potent when they
come from food, as they include many beneficial naturally occurring substances, such as carotenoids, flavonoids,
fibre, minerals, and antioxidants that are not in most supplements. There may be less need for medications for
constipation with a food first approach and possibly less waste of food/fluids and of oral nutritional supplements,
leading to better cost management.
• An adequate intake of all nutrients is important for the prevention of nutritional deficiencies and malnutrition. If
residents are not eating sufficient food provided at meals and regular snacks, then additional Calories, protein and
other nutrients are encouraged as required through individualized snacks, fortified food items and/or oral nutritional
supplements, according to residents’ health and nutritional status.
• Studies involving frail elderly have shown that adding flavor enhancers to food may improve intake, which may in
turn positively affect immune function. Flavour enhancement can include the addition of spices, herbs, salt or any

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 28
addition that intensifies the flavor or aroma of food and may compensate for taste losses that may accompany
aging.
• Research indicates that increasing feeding support and assistance provided to residents can lead to an increased
food intake. On the other hand, oral nutritional liquid or pudding supplements may require less time to prepare and
possible less time to assist residents to eat.
Assessment and Monitoring
• As part of the Nutrition Assessment, the reason for sub-optimal intake is assessed and addressed. As appropriate,
RD consults with Interdisciplinary Care Team, resident, and/or POA/SDM to discuss underlying concerns affecting
intake.
• It is helpful to know the preferred food and fluid items of the individual resident so those foods/fluids can be
fortified. It is also beneficial to know the optimal time of day to provide these fortified items to individual residents
to improve consumption.
• Food and fluid intake is documented for all residents daily and the record is monitored regularly to identify poor
intake so residents can be referred to the RD prior to weight loss occurring
• Whether using fortified foods or supplements, intake is recorded and effectiveness assessed in the health care
record.
• All nutrition interventions are monitored and re-evaluated regularly for acceptance and effectiveness, and
discontinued when results are achieved or if resident refuses.
Interventions
RD consults with Interdisciplinary Care Team, resident, POA/SDM to discuss interventions that would be best suited to
the preferences and needs of the resident.
• Food is offered before supplements - give a little extra at meal and snack times and provide preferred foods.
• Providing food and fluids that give residents extra Calories and protein without increasing overall food/fluid volume,
are generally better tolerated and may provide a significant benefit for residents’ overall health.
• Extra staff time may be needed to prepare fortified foods and to assist residents to eat them. Research shows that
increasing feeding support and assistance provided to residents increases food intake.
• Fortified foods are offered at meals or snacks or may be implemented during additional scheduled snacks.
• Desirable and Calorie dense foods (e.g. ice cream, cheese) are available in the Resident Home Area for provision
between meals and scheduled snacks if the resident indicates interest in eating.
• A commercial supplement may be offered if the fortified foods do not have the desired results. Begin with small
volumes to supplement fortified foods and overall intake and increase only as required to achieve desired results.
• A 2.0 kcal/ ml supplement can be considered to decrease volume while increasing nutrition. This can be provided
at the end of a meal, or at snack time or with medication pass.
• Supplements are discontinued when the resident’s oral intake at meals and snacks improves, and/or when the
resident achieves goal weight.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 29
• If the resident has significant eating challenges, continuous sleeping or severely reduced appetite that suggest end
of life, consider if comfort feeding is the appropriate option.
Policy Development
A policy exists that outlines the decision-making process and education for the Interdisciplinary Care Team, and the meal,
snack, medication pass and comfort feeding options available to the residents who require these.
Dementia/Responsive Behaviours
• As dementia progresses, difficulties in communication and thought processes become increasingly prevalent and
may result in responsive behaviours.
• According to the Alzheimer’s Society of Ontario (www.alzheimers.ca), responsive behaviours follow these principles:
• All personal expressions (words, gestures, actions) have
meaning
.
• Personal expressions communicate
meanings, needs and concerns
.
• To understand their meaning, you must consider
the factors influencing his behaviour
(physical, emotional
and environmental elements etc.).
• “Personal expression” is a term used to describe the actions, words and gestures of people living with dementia
that express their needs, but may appear to others as an unreasonable or un-called for response. To understand
their meaning, consider the factors influencing the behaviour (physical, emotional and environmental elements
etc.).
• Personal expressions are the result of the inability to communicate effectively one’s needs due to changes in the
brain affecting memory, judgment, orientation, mood and behavior. These expressions may also result from mood
disorders such as depression, personality disorders, adjustment disorder, and delusions. Expressions often include
reactions of frustration, grief and loss, as well as expressions of loneliness.
• Many residents with dementia cannot communicate verbally about pain or discomfort related to chewing or
digestive function. In the dining room, the Interdisciplinary Care Team needs to be alert to changes in appetite,
difficulty with self-feeding and/or complete unawareness of food when being served.
• These residents will be at risk for weight loss, malnutrition, dehydration and potentially dysphagia. Ability to
communicate may depend on the level of cognitive and physical impairment that can impact how care is received
or provided, and are can be exhibited as agitation, wandering and pacing, and apathy.
• Specific behaviours and Interventions that may affect intake include:
• Agitation - Redirect resident’s attention and remain calm.
• Sundowning (behavior change later in the day) - Discourage napping at the dining table, restrict caffeine
after lunch, provide reassurance, offer a favourite item to hold.
• Constant unwarranted requests for attention and help - Provide reassurance, e.g. tell resident that someone
will be there soon.
• Wandering - Provide foods that resident can safely eat while walking. Encourage resident to come back to
the dining room.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 30
• Verbal outbursts - Listen, empathize, reassure; then try to redirect or distract resident. Do not directly
disagree with the resident as this may add to the resident’s agitation.
• Aggression - Watch for a sudden increase in movement to indicate anxiety and respond in a supportive
manner with a gentle voice. Speak slowly and use repetition.
Assessment and Monitoring
• Dementia and personal expressions are discussed and documented as part of the initial assessment and ongoing
nutrition assessment.
• Food and fluid intake are monitored and recorded since they can be significantly affected by dementia and
responsive behaviors
Interventions
• Interventions for eating and drinking are based on individual needs and may include:
• Seat resident at a dining table that will minimize or eliminate distractions.
• Seat with other residents that will provide a calming effect and minimize agitation.
• Finger foods may be helpful for residents who wander.
• Ask if you can support them with eating by cutting their food.
• General guidelines for approaching residents include:
• Approach from the resident’s front not from behind.
• Speak to the resident at eye level as much as possible.
• Address resident by preferred name.
• Be respectful and polite at all times.
• Use simple words, short phrases and gentle calm tone.
• Give time to respond; suggest words.
• Show empathy and caring if distressed
• Create a rapport with families in order to help understand residents’ individual needs and work together to develop
interventions that are successful.
• Be creative and flexible, and support residents’ retained abilities while preserving dignity and resident rights.
• Interact with residents by prompting and praising appropriate mealtime behaviours.
• Training programs can provide staff with improved knowledge, attitudes and supportive behaviours relating to
mealtime assistance for people with dementia.
For Additional Information and Support
• Behaviour Supports Ontario provides case management and mobile interdisciplinary behavioural support outreach
teams that provide support to staff of LTC homes in Ontario. http://www.behaviouralsupportsontario.ca/
• P.I.E.C.E.S. is a best practice learning and development initiative for LTC staff that is available across Ontario and
many other locations. It provides an approach to understanding and enhancing care for individuals with complex
and cognitive/mental health needs and behaviour changes. http://pieceslearning.com/

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 31
Enteral Feeding (Tube Feeding)
• Enteral nutrition is used to provide appropriate nutrition support to residents who have a functioning
gastrointestinal tract but are not able to meet their nutritional needs orally.
• Enteral nutrition may be needed due to severe protein-energy malnutrition, head or neck conditions, critical
illness, stroke, dementia and other reasons.
• Enteral feeding can vary according to placement location of the tube into the GI tract, type of formula required
based on medical condition, and planned feeding regimen. Preference is for a closed system to reduce the risk
for infection.
• Enteral feeding in advanced dementia is generally not recommended. Family or SDM is provided with
information on potential risks and benefits to allow an informed decision. The interprofessional team may need
to get consultation from an ethicist or clergy person to support family members.
Assessment and Monitoring
• Provide advance notice of admission of residents requiring enteral feeding so the home is properly equipped
and able to provide for the residents’ needs.
• Residents who are admitted to the home on enteral feedings are assessed promptly upon admission by the RD.
Requirements for Calories, protein and fluids are calculated and documented and diet order is adjusted as
required.
• Periodic interdisciplinary assessment regarding transition back to oral feeds is considered, where appropriate.
• Signs and symptoms of intolerance, intake, weight and pertinent lab values are monitored to best determine
optimal formula, volume of formula and fluid and rates of flow.
• Each resident is monitored on every shift by Interdisciplinary Care Team members to evaluate their progress and
condition, checking for symptoms of intolerance to the formula or administration method and for
signs/symptoms of dehydration.
Interventions
• Enteral feeding orders and routines are written by the MD or RD, specifying formula product name, total volume,
method of delivery, rate of delivery, times of feeding, and volumes and times of required water flushes, and type
of pump used.
• Where transition to oral feeding is planned, the Interdisciplinary Care Team in conjunction with the RD initiates
and develops a comprehensive plan for transition including specific guidance for all staff and clear monitoring
protocols.
• Nutrition and hydration care is provided for residents receiving enteral feeding that is managed by the
Interdisciplinary Care Team and overseen by the RD, with input/support from appropriate referring source or
previous providers, when applicable.
• Specialized products and feeding protocols are recommended based on resident’s medical condition.
Policy Development
Protocols, policies, procedures and tools are in place to support:
• Effective implementation and management of the enteral feeding program, including responsibilities for
assessment, monitoring and care planning

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 32
• The types of formulas, and feeding pumps
• Staff training for administering enteral feeds
End of Life Care
• Residents continue to receive food and fluids in the end of life phase, but the emphasis is on quality of life and
symptom relief rather than active nutritional therapy or prolonging life.
• Conversations and education about end-of-life issues are initiated early with the resident in the diagnostic and
treatment stages rather than waiting until the dying process has begun. Family is included if the resident wishes
this, or if the resident is not capable. Families should understand the physiological progression at end of life.
• Hydration interventions may be limited as artificial hydration may lead to suffering, restricted movements and
prolonging the dying process due to increasing pulmonary secretions, increased urinary output, nausea,
vomiting, and edema.
• Benefits of dehydration in the dying process include reduced lung secretions/less coughing, reduced edema or
ascites, reduced nausea and vomiting, and less urine output. Symptoms of dry mouth can be managed with ice
chips, lip balm, and moistened swabs.
• Tube feeding for people with dementia at end of life has not been shown to confer any benefit regarding
nutritional status, reduction of pressure sores, mortality risk or survival time, although this may depend on the
resident’s mental and physical status and expected duration of life.
• The resident’s expressed desire for care at the end of life is the primary guide for determining the extent of
nutrition and hydration interventions and the focus is on quality for life and symptom relief.
Assessment
• The RD functions as part of the Interdisciplinary Care Team, which includes the resident and/or next of kin/SDM,
when formulating plans for end of life care. The team must take into account the cultural, social, psychological
and spiritual needs and wishes of the resident.
• Frequent monitoring is needed to ensure that interventions are meeting the needs of the resident and family.
resident’s status and individual needs and wishes can change quickly.
Interventions
• Providing “comfort feeding” and oral hydration may be therapeutic for residents. A “comfort feeding only” diet
order offers an alternative to NPO orders. This diet order can include foods and fluids that the resident prefers
and therefore provides the resident with the comfort and pleasure of eating, without consideration of diet,
weight, and nutritional status.
• Meal Time Interventions may include:
• Careful and slow hand feeding when the resident is alert and in a safe body position (upright with chin tuck)
minimizes the risk of choking or aspiration.
• The resident is provided with one small teaspoon or one small bite of food at a time, while watching for
swallowing to take place. There may be a gradual decrease in intake as end of life approaches.
• If the resident is coughing or has shortness of breath, wait until normal breathing has resumed and the
resident confirms that he/she is ready to restart feeding.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 33
• When good mouth care is undertaken, residents do not suffer the ill effects of terminal dehydration, which
may reduce the consideration for hypodermoclysis or intravenous therapy.
• Other strategies may include discontinuing orders for monthly weights, vitamin/mineral supplements, and
nutritional supplements unless request by the resident or family to continue.
• Staff training includes:
• Understanding and managing end of life care.
• Supportive and non-coercive eating assistance techniques.
• How to support residents and family during this time as well as the ethical challenges regarding this care.
Policy Development
Policies and procedures are in place that outline the processes for managing End of Life care for individual residents.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 34
MEAL SERVICE AND PLEASURABLE DINING
• All residents are provided with a pleasurable and supportive dining environment for all meals, beverages and
snacks so they consume and enjoy the foods and fluids they are offered and thereby receive quality nutrition
care appropriate for their medical condition(s), personal needs, and quality of life.
• Dining is influenced by the physical and psychosocial environments. Dining rooms are smaller and have
adequate light and temperature, good flow for pathways and include furniture and other features like entryways,
that support a calm and efficient dining service. The psychosocial environment includes the interactions that
happen among residents and team members that are social and resident- and relationship centered. Canadian
research indicates that living in a dementia specific care area and providing resident-centred care supports food
intake. Some studies have also suggested that this environment can impact social interactions and promote
food intake, as well as reduced distress for those living with dementia.
• Policies, procedures, job descriptions and work schedules all reinforce the provision of a pleasurable and
supportive dining experience.
• Processes for meal service/pleasurable dining include:
• Relaxed, supportive dining environment
• Organized meal service
• Meeting residents’ nutrition and hydration care needs
• Food and beverage choices
• Food and beverages at safe and palatable temperatures
• Medications and treatments before mealtime
• Supportive/restorative dining programs
• Dining supervision
Relaxed, Supportive Dining Environment
• Residents enjoy their meals and may eat more in a physical environment that is comfortable and supports a
positive dining experience.
• The physical environment has an important impact on the dining experience of LTC residents, supporting them
to thrive in their environment by increasing social interaction, reducing agitation, with the goal of improving
energy intake and nutritional status.
• Dining rooms are clean, including tables, chairs, walls, floors, window coverings and ledges.
• Dining rooms are peaceful and cheerful with appropriately set table and seasonal décor.
• Tablecloths/placemats are clean and used to enhance the home-like atmosphere of dining rooms.
• Each dining room has adequate equipment to provide effective meal service, including adequate supply of
dishware, glassware and cutlery, assistive eating/drinking devices, adjustable height dining room tables,
comfortable dining room chairs and appropriate seating for Interdisciplinary Care Team members assisting
residents.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 35
• Contrasting colours are used for table coverings/placemats and dishes to help residents with poor vision to
identify what is being served.
• Dining rooms are well lit, so that residents can see well without the distortion of glare.
• Noise level is as low as possible. Use rubber spatulas to scrape plates, keep voices low for task focused staff-
staff conversations. Ensure all cart wheels are quiet.
• Food aroma is an integral part of dining and is considered in the meal set up prior to serving.
• Wheelchairs fit under tables appropriately. Walkers are out of the way and any clutter from walking paths in the
dining room is cleared to ensure a safe route for residents and team members. This also enhances residents’
feelings of autonomy and inclusion.
• A mix of table sizes may be provided for optimal socialization and to create more walking space in the dining
room for residents and for staff.
• A dining room that includes or overlooks a garden/green space, and includes items of interest (such as a clock
and/ or artwork) make the area more home-like and may enhance intake.
• All aspects of dining, including table settings, condiments, music, and noise level are evaluated and adapted to
meet resident needs and desires. Music volume is low and TV is turned off.
Organized Meal Service
Type of Service and Timing
• Encourage dining room service that is tailored to residents’ needs. Alternative types of service are
accommodated under special circumstances and are documented in the Nutrition and Hydration Care Plan.
• Meal service is at regular intervals during the day, with a full breakfast available until at least 0830 hours for
residents who choose to sleep late, and the evening meal is not offered before 1700 hours, unless otherwise
determined and based on the wishes and needs of the majority of residents, as documented in the residents’
Council minutes.
• Meals are provided in a relaxed, skilled and unhurried manner, generally over 45 minutes to 1 hour, to promote
residents’ enjoyment, safety, comfort, independence and dignity in eating and drinking. Flexible dining may
include a longer time frame for meal service.
• Temporary tray and isolation tray service are provided according to established home policy and as documented
in the Nutrition/Hydration Care Plan. Ensure the need is evaluated on an ongoing basis and that the resident’s
safety is maintained, with supervision and assistance provided as necessary
Point of Service Tools
• The seating plan is developed and updated regularly so that residents are seated with suitable tablemates to
promote socialization.
• Residents requiring support and assistance are seated together when appropriate, at tables of four, with two
residents requiring complete assistance (not to be called “feeders”). Seating one staff member at each table may
provide optimal meal time supervision and best utilizes staff.
• Standard, modified and individual menus are the basis of what is prepared and served and are important
communication tools.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 36
• Ensure that this information is available for easy access by the staff plating and serving meals, ensuring that
resident’s privacy is respected.
• Instruct staff on the importance of adherence to any therapeutic diet needs, including the use of portion control
and correct serving.
• Documentation of family members’ information about well-liked foods and food preferences if residents are
unable to express themselves.
• Resident diet, meal and snack service information that corresponds with the resident care plan may include
additional information about how the resident will be served to best meet his/her dining/eating/nutrition needs.
• This resource is readily available to all staff at the point of food and beverage service and provides clear
directions to staff providing care and service, ensuring at all times that the resident’s right to privacy is respected.
• Document for residents who might be resting or away during the regular snacks or when beverages are offered
so that the snacks and beverages can be provided at a time more suitable to their individual needs.
• Staff is aware of the importance of providing feedback to RD/NM on the level of acceptance and success of
nutrition interventions.
• The order of the “table by table” service is rotated on a regular basis to allow all residents the opportunity to be
served first. Homes may elect to identify dining room tables with numbers or other identifiers to facilitate an
organized meal service.
Dining Procedures and Activities
Before the Meal
Provide residents with encouragement and assistance as they arrive in the dining room ready for an enjoyable dining
experience. This may include:
• Residents are addressed as they wish, e.g. first name, Mr., Ms. or Mrs.
• Provide resident assistance with washing hands prior to assisting to the dining room. Hand sanitizer may be
appropriate for some residents, however hand washing is required to remove visible dirt. Hand sanitizer may be
contraindicated for residents due to skin concerns.
• Residents are assisted to the dining room according to their Plan of Care, e.g. independently, walking program,
wheelchair, walker, cane.
• Residents arrive in the dining room no more than 20 minutes in advance of dining service starting.
• Residents are properly groomed and dressed and wearing any needed sensory aids, e.g. hearing aids, glasses,
dentures etc.
• Appropriate support and assistance is provided so the resident is seated comfortably at the dining room table.
• Seat residents according to the seating plan.
• Position residents for safety and comfort, sitting as upright as possible, close to the dining tables, with chin
tucked to enable safe swallowing.
• Before the meal begins, offer the resident clothing protection (not referred to as “bibs”) such as cloth napkins or
aprons, as preferred by the resident/family and documented in the Nutrition and Hydration Care Plan. Residents
are asked if they wish assistance with the clothing protector before placing them on residents. Sufficient paper
napkins are available to avoid using the protector to wipe the mouth of residents who require eating assistance.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 37
• As a comfort measure, warm washcloths may be provided for residents before/after eating, with assistance
provided for those residents who need help.
Service of the Meal
• Residents are encouraged to socialize and eat at a pace that provides time to eat slowly and chew carefully to
maintain their independence and safety whenever possible. Residents are not rushed from the dining room for
cleanup or to convenience team members in their tasks.
• A team approach is used to provide meals and assistance to promote continuous flow of meal courses so that
residents experience an appropriately paced meal service.
• For residents who may wander or be impatient, finger foods can be provided that can be easily picked up and
eaten with the hands. If resident is impatient between courses or will leave if not actively involved in eating,
consider providing all courses at the same time. Document this in the Nutrition and Hydration Care Plan.
• As much as possible provide table-by-table service.
• When serving the meal plates, provide sufficient warning if the food is hot.
• Encourage residents to make as many mealtime decisions as possible for themselves (e.g. what beverage they
would like, etc.).
• As much as possible meals are served course by course; however, staff supports resident requests to make
changes to usual course-by-course service, e.g. tea served at same time as soup or dessert served at beginning
of meal, etc.
• Residents are given ample time to complete one course before the next is offered, and dirty dishes are removed
before providing the next course.
• Second helpings are offered, unless contraindicated in the Nutrition and Hydration Care Plan.
• Food and fluid intake is monitored during meals. This information is noted and communicated to those
documenting the intakes.
• Residents may request a smaller or larger than standard portion and this request is supported by the serving
staff. The size of meal that the resident wants is provided, with opportunity for second helpings.
• Staff listens to residents and support individual requests such as gravy on the side, extra condiments or
condiments not on menu, etc.
Providing Assistance at Mealtime
• Staff is seated (never standing) with appropriate eye contact, when assisting residents who require complete
assistance. Inform residents of the food they are about to eat. Talk about the smell and taste of the different
foods being offered, so that the resident can identify what they are eating. Involve the resident in social
conversation, even if they are unable to verbally respond.
• Use cues or reminders, improved peer support, timely and appropriate feedback, timely and consistent follow
up for all team members and volunteers who assist in improving resident intake at meals.
• Avoid mixing foods together unless it is otherwise indicated in the Nutrition and Hydration Care Plan.
BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 38
After the Meal
• As required, residents may be asked if they wish to be assisted to wash their hands and/or remove food particles
from face and clothing when they have finished eating.
• Food and fluid intake is documented.
• Tables are cleared and cleaned after all or almost all residents have finished eating and have left the dining area.
Residents’ Nutrition and Hydration Care Needs
• Ensure there is an organized system to provide nutrition care at meals as well as between meal snacks and
beverage passes, according to each resident’s needs which include the following:
• Staff has ready access to residents’ nutrition and hydration information, including the
binder/roster/computerized system of resident dietary-related needs and wishes.
• Interdisciplinary care team members verify pertinent information provided for each resident prior to
every meal service delivery, by referring to the binder/roster/ computer system.
• Regular tables are assigned to team members so they become familiar with the residents and their
personal needs including therapeutic diets, food textures, fluid consistencies and preferences in dining.
• There is an established process to ensure all dining room point of service materials are current at all
times.
• Staff is aware of the importance of adherence to any therapeutic diet needs, including the use of portion
control and correct serving equipment.
• Staff recognizes that receiving correct food items enhances the feeling of control and personal worth to
residents, as well as their satisfaction with meals and ultimately, their intake.
• Service staff portion and plate meals based on point of service information so they are visually appealing
to the residents.
• Document those residents who might be resting or away during the regular snacks or when beverages
are offered so that the snacks and beverages can be provided at a time more suitable to their individual
needs.
• Meal time training includes:
• Use of all point of service tools in use in the service of meals and snacks
• Emotional and physical support and conversation with staff and volunteers, to make meal times an
enjoyable experience that has purpose and meaning.
• Consistent staff to improve communication and knowledge of residents’ needs and wishes.
• Use of the power of observation, resident history and continual monitoring of resident choices in order
to become aware of resident preferences.
• Cross-training so all staff is familiar with dining room routines. Staff is fully engaged in making the dining
process successful.
• All disciplines and departments need to be involved to successfully implement changes in dining
practices and the mealtime environment.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 39
Food and Beverage Choices
• Residents are provided with a choice of food and beverages based on the posted and communicated menu
and in a manner suitable to each resident’s ability and/or limitations e.g. visual, verbal or written.
• Offering of choice includes the following:
• Ask residents for their meal and beverage preferences.
• Offer all the planned menu choices – including beverages, entrées, vegetables, desserts and their
alternates - for all regular, therapeutic and texture-modified diets. Post alternatives to planned menu
choices before meal service, as necessary.
• Ensure all menu items are prepared, provided and ready to be served at the same time for all diet types
required for the home’s residents and served course by course.
• Offer beverages and confirm preferences (even when known) as residents arrive for meals, with a team
member providing appropriate beverages.
• Offer menu choices by various team members, table by table, so all residents are offered all their
choices.
• Rotate the order of the “table by table” service on a regular basis to allow all residents the opportunity
to be served first.
• Provide visual choice (e.g. “show plates”) for residents. For those with limited communication, watch for
eye movements or focusing on a specific dish as a potential indicator of preference.
• Some residents may respond better to having a choice offered in an alternate way, e.g. verbal, use of
likes and dislikes, a family marked menu, etc. This is documented in the Resident’s Plan of Care.
• Use i-Pads or other methods of displaying meal choices as an alternative to show plates to save money
and avoid food waste.
• Display the menu choices in regular texture, but provide the meal to residents requiring texture modified
foods in the manner modified to meet their individual needs. Explain that the meal items will be provided
in the texture that has been planned to best meet residents’ needs.
• Relay resident choices to the Food/Nutrition staff plating the meals by table number and by resident
name so Food/Nutrition staff can portion the meals based on each resident’s information in the dining
binder/roster.
Food and Beverages at Safe and Palatable Temperatures
Policies and Procedures are in place to ensure that food and beverages for meal times and snack and beverage
service are provided at safe, comfortable and palatable temperatures. These policies and procedures include the
following:
• Maintain correct food temperatures. Hot foods are maintained at a minimum temperature of 60 degrees Celsius
throughout meal service, and cold foods at a maximum of 4 degrees Celsius throughout meal service.
• Provide appropriate equipment to transport and hold hot and cold food at safe temperatures both for meal and
snack service.
• Take and record temperatures of both hot and cold food and beverages at the point of service. Thermometers
are sanitized between foods and calibrated regularly for accuracy.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 40
• Take corrective action if holding temperatures are found not to be at the correct level, prior to or during meal
service, as the problem is identified.
• Ensure plating and delivering meals to residents requiring assistance with eating occurs when staff are present
to provide assistance.
• Include information on what temperatures provide resident safety, comfort and meal satisfaction and how this
“comfortable” temperature is achieved as a part of staff orientation.
Medications and Treatments at Mealtime
Practices for medications and treatments at mealtime recognize each resident’s right to respect, dignity and privacy and
that medication may also affect the taste and enjoyment of food.
• Medications are not mixed in food or fluid that is served as part of the meal without prior documented approval
from resident/POA/SDM.
• Whenever possible, medications are provided as residents arrive and leave the dining room so the dining
experience is not interrupted with medications; this also allows for more Nursing supervision and assistance
during dining.
• Medications are not given in the dining room during meal service unless indicated on the resident’s care plan.
• Any medications that are provided in the Dining Room are administered in a manner that ensures residents can
safely swallow and are not disruptive to the dining experience.
• Staff provide medications in a discrete manner to preserve resident dignity.
• Staff is seated to administer a medication that requires crushing or mixing with food for residents who need
assistance, so resident is properly positioned to swallow.
• A medication mixed in a sweet food (that is not one of the menu items or part of the actual meal, e.g. applesauce),
is not provided when the resident is eating the savoury portion of their meal.
• No treatments are administered in the dining room unless otherwise indicated in a resident’s Care Plan.
Supportive/Restorative Dining
• Supportive Dining is an overarching principle that supports dining and eating/assisting practices that work
towards creating an environment that supports and promotes all residents for safety, comfort, independence
and dignity in eating and drinking. Encouraging residents to make decisions for themselves and to eat more
independently enhances dining pleasure, strengthens memory and enhances mental health.
• The goal of Restorative Dining is to return or maintain an individual to their highest practicable physical, mental
and psychological functional level and well-being. It is not a separate entity but is integrated into routine
dining/assisting that is organized, planned, documented, monitored and evaluated. Staff is trained in the tasks
and techniques that promote resident involvement in the activities of dining.
• Residents are provided with food and fluids at meal and snack times in an environment that supports and
promotes their safety, comfort, independence and dignity in eating and drinking.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 41
• The Interdisciplinary Care Team is trained to watch for signs that a resident’s needs are changing (recognizing
that all residents require some assistance from time to time), such as: eating less, tiring more readily, and
needing meat and other foods to be cut for them.
• Each resident is assessed for assistive devices to encourage more dining independence - assistive cutlery,
special drinking glasses/mugs, plates, guards, mat, etc. Assistive devices are clean, in good condition and ready
for the resident at each meal.
• Staff use appropriate seating while assisting residents, to ensure safe feeding techniques, maintain eye contact,
inform residents of the food they are about to eat and involve the resident in communication.
• All plans and interventions for restorative dining are discussed with and approved by residents and/or SDM/POA.
• The level of support and/or assistance that each resident requires is given, e.g. cueing, encouragement, cutting
food, intermittent assistance, hand over hand assistance or full assistance. Prompt the resident to eat by placing
cutlery or cup in the resident’s hand.
• Fatigue is monitored during the meal as the resident may require enhanced assistance at the end of the meal to
ensure adequate intake.
• Refer to physiotherapy/occupational therapy if resident is not able to sit properly or safely at the table. Referral
to OT can also be made for assistive eating devices.
Dining Supervision
• Residents are monitored and supervised during dining, including meals, snacks and other food-related activities
to promote residents’ safety, comfort, independence and dignity in eating and drinking, to monitor residents’
overall response to the dining program and to monitor each resident’s nutritional well-being.
• Provide monitoring/supervision of residents by a member of the Interdisciplinary Care Team.
• Ensure the Nutrition Manager, Dietitian and Registered Nursing staff, as well as other Food/Nutrition and Nursing
Team members, have responsibility for the monitoring and management of the quality of the dining program and
its benefits and risks.
• Assure that one Interdisciplinary Care Team member, trained to handle risk situations such as choking, illness
and other response protocols, is assigned to be present at all times while residents remain in the dining room.
• Complete meal time audits on a regular basis to ensure the dining program provides a safe and pleasurable
dining experience.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 42
CONTINUOUS QUALITY IMPROVEMENT (CQI)
Best Practices require a strong Continuous Quality Improvement (CQI) program consisting of quality improvement, risk
management and utilization review. This program strives to:
• Meet and exceed the continually changing needs and expectations of residents
• Take appropriate corrective actions, as required, to effectively utilize and deliver services
• Prevent, or reduce and control actual or potential risks, to the safety, security, welfare, health and reputation of
residents, all levels of staff and the home
The CQI program may follow a cycle of assessing, planning, implementing and of monitoring, evaluating and improving
in order to develop the Protocols, Policies, Procedures and Tools needed to drive the organization and delivery of the
Nutrition, Food Service and Dining Program that can be used by both the Departmental and Interdisciplinary Care Teams.
The CQI program monitors, evaluates and improves the quality of care through:
• Communication and documentation among Interdisciplinary Care Team members on the effectiveness of the
program
• Consistent monitoring and supervision of the dining and snack programs to ensure residents receive nutrition
care as planned and to provide ongoing evaluation of the effectiveness of this care.
• Regular review and updating of each resident’s Nutrition and Hydration Care Plan so goals and interventions
remain current and effective
• Appropriate corrective actions taken and documented as required.
• Use of consistent and effective methods of measuring performance, e.g. resident satisfaction surveys, employee
performance appraisals, budget review, resident weights, accurate food and fluid records, monitoring of RAI-
MDS quality indicators
• Evaluation of the effectiveness of protocols, policies, procedures and tools and revisions as required
• Education and training to team members involved in the organization and administration process of all of the
above
The Education Program consists of:
• Education on Interdepartmental and Interdisciplinary Protocols, Policies, Procedures and Tools
• Inclusion in the planned orientation program for all new employees to ensure all Interdisciplinary Care Team
members know and understand their importance and role in the Nutrition, Hydration and Dining Program
• Regularly scheduled educational programs and updates on the Nutrition, Food Service and Dining Program for
all Interdisciplinary Care Team members based on their assessed learning needs and changes in the program
• Additional educational opportunities, as needs and opportunities arise such as Nutrition Month activities
• Team members belong to appropriate professional and educational associations and networks, which may
include Dietitians of Canada (DC), PEN membership, DC Gerontology Network, CSNM, and OSNM.
• Access to current resources for training and support

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 43
CONCLUSION
Best Practices for Nutrition, Food Service and Dining in LTC Homes:
• Ensure all guidelines, protocols, policies, processes, and interventions are based on promoting and
supporting residents’ health, safety, comfort, rights and quality of life, as well as their autonomy and
involvement in decision making regarding their care and services.
• Promote Interprofessional Collaboration and an Interdisciplinary Care Team to provide the maximum
benefit of the Nutrition, Hydration and Dining Program for the resident.
• Respect the resident and team’s time and effort by using audits, surveys and data to improve the quality
of the Nutrition, Food Service and Dining Program.
• Standardize processes that work well and use the information obtained from audits and surveys and team
input to improve processes that are not effective.
• Modify protocols, policies, processes and tools based on information collected and documented by the
team.
• Use the results of published evidence and of applied research and studies performed by the team and
peers to improve current practices.
• Continually strive to improve the quality of care and services, maximize the effective use of resources and
reduce the potential of risk to residents, team and home.
• Provide appropriate orientation and ongoing education so the whole team understands and promotes the
entire Nutrition, Food Service and Dining Program effectively.
Comments / Questions / Concerns
We welcome your feedback about this document. Please let us know if you have found it helpful and feel free to send us
any specific comments, questions or concerns you may have about the content.
Please contact the current Chair of the Ontario LTC Action Group (see Dietitians of Canada website (www.Dietitians.ca).

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 44
Sample Forms and Policies
Dietitian Referral Form Sample
Requested by: ______________________ Unit: ______ Date: _______________
Intake Concerns
¨ Change from usual pattern in food / fluid intake for two of the three meals over a period of seven
days
¨ Refusal to eat / drink (> 3 consecutive meals)
¨ Leaves 25% or more of food for two of the three meals over a period of seven days
¨ Leaves 25% or more of fluid for two of the three meals over a period of seven days
¨ Intake from one of the four food groups restricted (vegetables and fruit, grain products, milk and
alternatives, meat and alternatives)
¨ Change in self-feeding ability affecting intake
Medical Conditions / Symptoms
¨ Altered skin integrity including skin breakdown, pressure ulcers, skin tears or wounds (not rashes or
bruises)
¨ Episodes of hyper / hypoglycemia
¨ Constipation
¨ Newly diagnosed diabetes or residents who are newly prescribed insulin
¨ Palliative care
¨ Signs and symptoms of dehydration (e.g. decreased/absent urine output, decreased tears, dry eyes,
poor oral health, dry chapped lips, dry mouth, etc.)
¨ Undesirable, unplanned, progressive weight change (>5% in one month, >7.5% in 3 months and/or
10% in 6 months or any other change that compromises the residents’ health status
¨ Swallowing disorder, aspiration pneumonia, GI concerns, vomiting and/ or diarrhea lasting more than
72 hours, abdominal distention
¨ Return from hospital with changes in diet or deviation from normal lab values
¨ New tube feed or concerns with tube feed
¨ Other, specify: ____________________________________________________
Referral Received by:
Name and designation: ___________________________________________
Signature: ___________________________________________
Comments: ___________________________________________
Completed: Progress Note Diet Order Diet Book Care Plan

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 45
Nutrition Assessment Sample
o Annual Assessment Resident Name, Age, Room #DOB, DOA
o Significant Changes in Status
o High nutrition risk monitoring
o Assessment by Referral
Anthropometric Measures and Physical Observations:
Current height (cm) (MDS: K2) Current weight (kg) (MDS: K2) Usual body weight (kg)
________________________ _______________________ __________________________
Physical signs of nutrition status (RAI/MDS: H, K, L, I, M, P)
________________________________________________________
Reference weight range for height/age/sex (kg)
________________________________________________________
Resident’s goal weight range (kg) ____________________
BMI ____________________
Medical Information:
Change in condition/diagnosis (RAI/MDS: B, C, D, E, G, I, M, O,P)
___________________________________________________________________________________
RAI output score CPS: ____ DRS: _____ CHESS: ____ Pain: _____ ISE: ______ PURS: ________
Medication with nutritional implications (including those with drug nutrient interactions affecting food intake,
enjoyment, absorption, vitamins/minerals (MDS:O, U - optional)
___________________________________________________________________________________
Laboratory Data (RAI/MDS: P9)
___________________________________________________________________________________
Gastrointestinal - problem (RAI/MDS: H, L, I, O) Managed by:
____________________________________ _______________________________
Skin - nutritional related problem (RAI/MDS: M, P) Managed by:
____________________________________ _______________________________
Chewing Concerns and Oral Status (RAI/MDS: I, J, K, L, P)
o No o Yes, reason Managed by:
____________________________________ _______________________________
Weight History % change
Current ______ kg ________
30 days ago _______kg ________
90 days ago _______kg ________
180 days ago ______kg ________
1 year ago _______ kg ________
Comment:
BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 46
Swallowing Concerns (RAI/MDS: I, K, L, P)
o No o Yes, reason Managed by:
____________________________________ _______________________________
Sensory Deficit Affecting Nutritional Intake (RAI/MDS: B, C, D)
o No o Yes, reason Managed by:
____________________________________ _______________________________
Diet History
Intake: o Good o Fair o Poor
Food and fluid preferences/changes
___________________________________________________________________________________
Comments/Specific Eating Patterns:
__________________________________________________________________________________
___________________________________________________________________________________
___________________________________________________________________________________
Current Diet and Meal Observation (RAI/MDS: A1 of H, I, J, K, M)
Regular Therapeutic Diet: Supplement
________________________________________ Daily bid tid qid
Other/individual menu __________________________ Food Allergies _________________________
Additional dietary needs ________________________ Food Intolerances ______________________
Diet Texture Fluid Consistency
____________________________________ _______________________________
Snacks o Bulk o Individual
___________________________________________________________________________________
Meal Observation and Evaluation
Eating ability: (RAI/MDS: G, P)
o Independent o Supervision o Limited assistance o Extensive assistance o Total dependence
Eating behaviour (RAI/MDS: E) Assistive feeding devices (RAI/MDS: K)
BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 47
____________________________________ _______________________________
Estimated Daily Nutrition Requirements (RAI/MDS: B, K, M, I, H, N, G)
Energy kcal / day: ________________ Protein g / day: ____________ Fluid cc / day: _____________
Estimated daily Caloric intake: _______________ Estimated daily protein intake: _____________
Estimated food intake: o >75 - 100% o 50 - 75% o <50%
Estimated fluid intake: oMore than 1500 ml (>75% fluid intake)
o1000 - 1500 ml (50 - 75% fluid intake)
o< 1000 ml (< 50% fluid intake)
Changes in last 90 days: Adequacy to meet needs:
____________________________________ ______________________________
Comments:
__________________________________________________________________________________
__________________________________________________________________________________
__________________________________________________________________________________
Summary of Nutrition Assessment Analysis
Nutrition Risk Status: o High o Moderate o Low
Goals/Recommendations appropriate: o Yes o No
Comments:
__________________________________________________________________________________
__________________________________________________________________________________
__________________________________________________________________________________
Non-Triggered RAP Identification
It is important not to duplicate the documentation in the RAP assessment summary and care plan. This section is to identify
actual or potential non-triggered RAP problem only. Goals and care plan interventions are to be stated in the care plan
document)
Signature/Status Date Completed Year - Month - Day
____________________________________ ______________________________

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 48

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 49

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 50

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 51
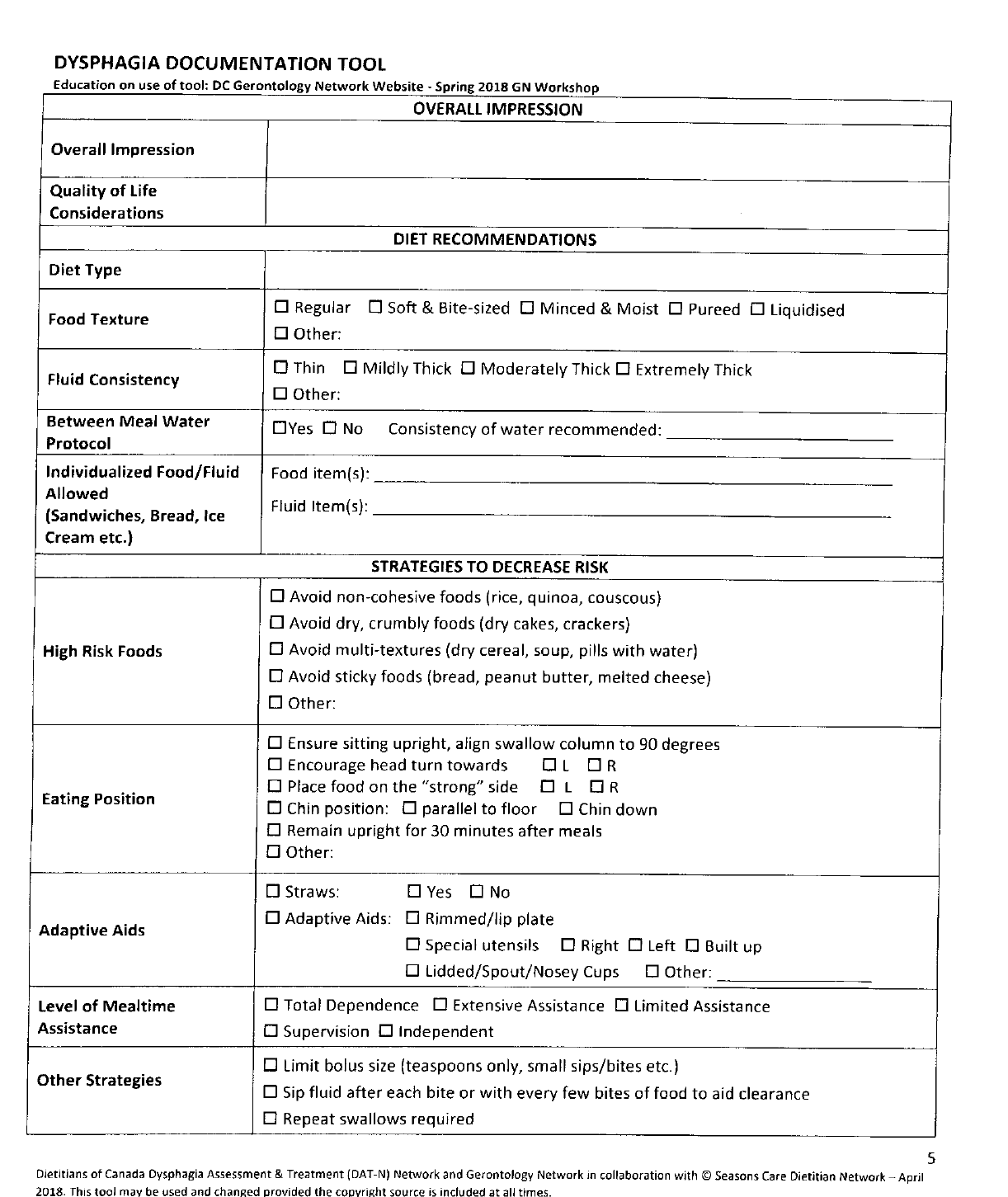
BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 52

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 53
BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 54
Sample Policy on Menu Planning
POLICY:
A menu cycle shall be established by the food and nutrition services for Residents.
PURPOSE:
1. To provide nutritionally adequate and personally acceptable meal choices for residents; with
minimum 1800 ml fluid per day
2. To provide a variety of food from highest quality ingredients this is suitable for the population
being served.
3. To provide a plan for efficient and economic use of food, supplies and labour.
4. To provide menus in accordance with Canada's Food Guide, current best practices, LTC Homes
Act and regulations and DRIs (Dietary Reference Intakes).
PROCEDURE:
1. The Dietitian and/or Nutrition Manager considers the optimal length of time (number of weeks)
for the menu cycle and the start date of the menu. The Residents Council must approve this
decision.
2. The Dietitian and/or Nutrition Manager develops the regular menu for residents, including
alternate choices and snacks, using feedback provided by the Residents, Families and Staff of
the Home. The committee also considers the special days, including holiday meals, special
functions, barbecues, etc., that are upcoming in the menu.
3. The Dietitian reviews and approves the draft menu. The draft menu is reviewed using Canada’s
Food Guide and a nutritional analysis is completed and checked with the DRIs for selected
nutrients.
4. Residents Council and/or Family Council and/or Resident Food Committee review the draft
menu. Recommendations by Residents’ Council and/or Resident Food Committee are
recorded in the minutes for those committees.
5. The Dietitian and/or Nutrition Manager updates the menu with the recommended revisions and
then reviews the updated menu with the Cooks for issues regarding production and equipment.
6. Once finalized, the draft regular resident menu is expanded to include texture modified and
therapeutic diets as well as portion sizes for all food items served. This will be reviewed and
approved by the Registered Dietitian.
7. The Dietitian and/or Nutrition Manager then develops the snack menu every day for the full
menu cycle, which includes a morning drink, an afternoon snack and drink and an evening
snack and drink.
BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 55
8. The Dietitian and/or Nutrition Manager keeps a file of the current master menu. The file
includes: current menu cycle for meals and snacks, full therapeutic menus, minutes of
Residents Council, Family Council and Food Committee showing that the menu has been
reviewed, letter from Dietitian showing approval of the nutrient and fluid content of the menu
and any other documentation related to the menu planning process. This file is kept for
Ministry inspectors to view as requested.
9. The Nutrition Manager develops or obtains standard recipes for all menu items, including
texture modified foods and fluid consistencies and snack menu.
10. The Nutrition Manager creates daily production sheets to match the menus, to help instruct staff
on what to prepare for each meal and snack.
11. The Dietitian adjusts the nutrient analysis for the updated menu including snacks.
12. The Nutrition Manager conducts a cost analysis and make adjustments as needed.
13. The Nutrition Manager posts menus in common areas and at point of service.

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 56
Nutrition and Dietary Services Satisfaction Questionnaire
To be completed as an in person interview by FSM or designate. The questions should be
used as an outline. Further space is provided for additional information.
YES NO
MEALS
Do you enjoy the meals you are served? □ □
Does the food taste good? □ □
Does your food look good? □ □
Are your hot foods served hot? □ □
Are your cold foods served cold? □ □
Are you usually getting enough to eat? □ □
Do you eat most of the food you receive at meals? □ □
SERVICE
Are those who serve your food pleasant and friendly? □ □
Are you offered two choices for lunch and supper? □ □
Do you receive the assistance you need at meal times? □ □
Are you given enough time to finish your meals? □ □
Are your suggestions about meals dealt with in a satisfactory way? □ □
Do we meet your personal food preferences? □ □
ENVIRONMENT
Is your table set properly and neatly? □ □
Is the dining room clean and inviting? □ □
Comments regarding meal or service:
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
____________________________________
BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 57
Food And Nutrition Services Quality And Performance Indicators
# of Nutrition Referrals received monthly - To identify trends in # of Nutrition Referrals to assess
workload impact
Average # Days to complete Nutrition Referrals received monthly - Calculate # days required
to complete each Nutrition Referral, averaged on a monthly basis. Set realistic goal target
according to RD days on-site weekly
% High Nutrition Risk Residents - Prevalence of residents at High Nutritional Risk as a
determination of acuity trends - % of residents at High Nutritional Risk based on results of the
Nutrition/Hydration Risk Identification Tool 2015 as of the last day of each month.
% Residents with Significant Weight Change assessed - Ensure timely nutritional assessment
for significant weight changes - % residents with significant weight loss/gain who were assessed by
a member of the Nutrition Care Team as of the last day of each month. Significant weight change
identified by unplanned weight loss/gain of: 5% in 1 month, 7.5% in 3 months, 10% in 6 months.
Performance Indicator goal - 100% significant weight changes assessed monthly
% completion RD Wound Reviews – Ensure residents with wounds are regularly assessed by
RD on a monthly basis - Monthly random audit of X # of residents with wounds from each resident
home area to determine if monthly nutritional assessments were completed as of the last day of
each month. Determine % completion. Performance indicator goal 90% of wounds assessed
monthly until healed
% RD High Nutrition Risk Reviews - Ensure that high nutrition risk residents are regularly
assessed by RD on a monthly basis. Monthly random audit of X # of residents at high nutritional
risk from each resident home area to determine if monthly nutritional assessments were completed
as of the last day of each month. Determine % completion. Performance indicator goal 90% of high
nutritional risk residents assessed monthly
# of residents requiring partial and total feeding assistance - Prevalence of residents requiring
partial or total feeding assistance calculated as of the last day of each month by resident home
area - Determine # and % of residents requiring partial or total feeding assistance due to staff
impact
Satisfaction - % Resident and SDM Satisfaction – Annual satisfaction and Quality of Life Survey.
BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 58
RESOURCES and SELECTED REFERENCES
RESOURCES
Bruyere Continuing Care - Pleasurable Dining Training
https://clri-ltc.ca/emodules/pleasurable_dining_EN/player.html
Schlegel-UW Research Institute for Aging
Making Mealtimes Matter
https://www.youtube.com/watch?v=wPfaQztS-mQ
Research Institute for Aging (RIA), Choice + Program
https://www.youtube.com/user/SchlegelUWRIA
https://the-ria.ca/resources/choice-checklists/
Mealtime Satisfaction Questionnaire
Research Institute for Aging (RIA), http://www.the-ria.ca/products-resources/msq/
Research Institute for Aging (RIA), other resources for nutrition and aging
http://www.the-ria.ca/products-resources/nutrition-aging/
Choice + Program
http://www.the-ria.ca/products-resources/choice/
The Lantern Project Australia
http://thelanternproject.com.au/
Anyone interested in The Lantern Project can contact Cherie Hugo via email at [email protected].

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 59
SELECTED REFERENCES
Menu Planning
Vucca V, Keller HH, Morrison HM, Duncan AM, Duizer LM, Carrier N, Lengyel CO, Slaughter SE (2017). Nutritional quality
of regular and pureed menus in Canadian long term care homes: an analysis of the Making the Most of Mealtimes (M3)
project. The Journal of Nutrition Health & Aging, 1-7, 2018
INDI Fact Sheet (Irish Dietitians)
https://www.indi.ie/fact-sheets/fact-sheets-on-nutrition-for-older-people/509-good-nutrition-for-the-older-person.html
Recipes
Molt, M.K. (2018).Food for Fifty, 14
th
edition. Pearson Publishing,
https://www.pearson.com/us/higher-education/program/Molt-Food-for-Fifty-14th-Edition/PGM332697.html
13
th
edition, free download - https://multi-drain.ca/DOC-ID/food-for-fifty-13th-edition
IDDSI
http://www.iddsi.org
Cichero JAY, Lam P, et al. (2017). Development of International Terminology and Definitions for Texture-Modified Foods
and Thickened Fluids Used in Dysphagia Management: The IDDSI Framework. Dysphagia (2017) 32:293–314
Published online: 2 December 2016 - open access at Springerlink.com
Consent
Pioneer Network website
https://www.pioneernetwork.net/wp-content/uploads/2016/10/The-New-Dining-Practice-Standards.pdf
Social Care Institute for Excellence website
https://www.scie.org.uk/dementia/living-with-dementia/difficult-situations/refusing-help.asp
College of Dietitians of Ontario website
https://www.collegeofdietitians.org/Web/Members/Professional-Standards-Guidelines/Consent.aspx

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 60
Liberalized Diets
Stewart L - article in Nutrition Care Systems
https://www.nutritioncaresystems.com/liberalizing-diets-in-long-term-care/
https://www.pioneernetwork.net/wp-content/uploads/2016/10/The-New-Dining-Practice-Standards.pdf
https://www.nutritioncaresystems.com/does-a-diagnosis-automatically-mean-a-diet-order/
Academy of Nutrition and Dietetics (2018). Position of the Academy of Nutrition and Dietetics: Individualized Nutrition
Approaches for Older Adults: Long-Term Care, Post-Acute Care, and Other Settings
https://www.eatrightpro.org/-/media/eatrightpro-files/practice/position-and-practice-papers/position-
papers/individualizednutritionapproachesforolderadults.pdf?la=en&hash=2F38FDB728F4CAD73BED1CB94908893D
948B25ED
Weight Changes
Nutrition Care Systems website
https://www.nutritioncaresystems.com/weight-changes-and-nutritional-challenges-in-the-elderly/Nutrition
Hydration
Practice-Based Evidence in Nutrition (PEN) website
http://www.pennutrition.com/KnowledgePathway.aspx?kpid=7997&trid=7975&trcatid=38
Skin and Wounds
Nutrition in Pressure Ulcer Prevention and Treatment
http://www.npuap.org/wp-content/uploads/2014/08/Quick-Reference-Guide-DIGITAL-NPUAP-EPUAP-PPPIA-
Jan2016.pdf
Registered Nursing Association of Ontario - Pressure Injuries Best Practice Guidelines
http://rnao.ca/sites/rnao-ca/files/Pressure_Injuries_BPG.pdf
Dysphagia
PEN Competencies for Dysphagia Assessment and Management in Dietetic Practice June 2017 - The Alliance of
Canadian Dietetic Regulatory Bodies
https://daa.asn.au/wp-content/uploads/2016/07/ACI-97-DAA.pdf

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 61
Niezogoda H, Keller HH, Steele C, Chambers LW (2014). What should a case-finding tool for dysphagia in long-term
care Residents with dementia look like? J Am Med Dir Assoc. 2014 Apr; 15(4): 296–298.
Diabetes
Diabetes Canada Clinical Practice Guidelines 2018 website for Older Adults
http://guidelines.diabetes.ca/cpg/chapter37
http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf
Constipation
Eat Well Nutrition Service website
http://eatwellnutrition.com.au/2014/05/06/dietary-management-constipation/
Health in Aging website
http://www.healthinaging.org/resources/resource:eldercare-at-home-constipation/
Food First/Supplements
Pioneer Network website
https://www.pioneernetwork.net/wp-content/uploads/2016/10/Flexible-Dining-Tip-Sheet-1.pdf
Nutrition Care Systems website
https://www.nutritioncaresystems.com/fortifying-enhancing-foods/
Keller HH, Carrier N, Slaughter SE, Lengyel C, Steele CM, Duizer L, Morrison J, Brown KS, Chaudhury H, Yoon MN, Duncan
AM, Boscart V, Heckman G, Villalon L. Prevalence and Determinants of Poor Food Intake of Residents Living in Long-
Term Care. J Am Med Dir Assoc. 2017 Nov 1;18(11):941-947.
Dementia/Responsive Behaviours in Dining
Health Quality Ontario website
www.hqontario.ca
Alzheimer’s Society Canada website
http://www.alzheimer.ca/en/on/We-can-help/Resources/Shifting-Focus/Examples-of-responsive-behaviour/Agitation
St. Christopher’s Episocopal Church website
http://www.stchristophers.org.uk/wp-content/uploads/2015/10/practice-development-
1.EoLJ_.Vol4_.No1_.Dementia.pdf

BEST PRACTICES FOR NUTRITION, FOOD SERVICE, AND DINING IN LTC HOMES
2019
DIETITIANS OF CANADA
I
PAGE 62
Alzheimer’s Association website (U.S.)
https://www.alz.org/care/alzheimers-food-eating.asp
End of Life Care
Today’s Dietitian website
http://www.todaysdietitian.com/newarchives/082508p68.shtml
Dining
Pioneer Network Food and Dining Clinical Standards Task Force (August 2011). New Dining Practice Standards
https://www.pioneernetwork.net/wp-content/uploads/2016/10/The-New-Dining-Practice-Standards.pdf
Enhancing the mealtime experience for older adults in long-term care
https://choice.the-ria.ca/enjoyment/
Restorative Dining
Pioneer Network website
https://www.pioneernetwork.net/wp-content/uploads/2016/10/Enhancing-the-Quality-of-Nursing-Home-Dining-
Assistance-Symposium-Paper.pdf
INDI Fact Sheet (Irish Dietitians)
https://www.indi.ie/fact-sheets/fact-sheets-on-nutrition-for-older-people/516-feeding-strategies-in-dementia.html
https://www.indi.ie/fact-sheets/fact-sheets-on-nutrition-for-older-people/997-dementia-the-dining-experience.html
