
PAGE 1 of 92
Revised 09/2023
2024 Plan Year (January 1-December 31, 2024)
Faculty and Staff Health Plan
Specic Plan Details Document
PROGRAM PROVISIONS FOR:
HEALTH REIMBURSEMENT ACCOUNT
PRIME CARE
CHOICE
PRIME CARE
CONNECT
PRIME CARE
ADVANTAGE
PRESCRIPTION
DRUG BENEFIT
OUT-OF-AREA
Ofce of Human Resources
Suite 300 | 1590 North High Street | Columbus, OH 43201-2190

PAGE 2 of 92
Revised 09/2023
TABLE OF CONTENTS
Introduction ............................................3
Covered Person’s Rights .................................4
Covered Person’s Responsibilities .........................4
Discrimination is Against the Law .........................5
General Plan Provisions ..................................7
Termination of Coverage ................................15
Covered Services .......................................16
Exclusions or Limitations ................................23
The Ohio State University Health Plan, Inc ................25
How Payment Is Determined ............................26
Medical Claims Processing ..............................28
Hospitalization Review .................................32
Coverage Continuation ..................................33
Prescription Drug Benet ...............................35
Medical Coverage Options
Prime Care Advantage .............................42
Prime Care Choice .................................48
Prime Care Connect ................................59
Out-Of-Area ......................................65
Health Reimbursement Account .........................69
Denitions .............................................72
Ohio State Travel Assistance ............................78
Appendix – Claim Determination and Appeal Procedures ...79
YOUR PLAN FOR HEALTH
614-292-4700 or 800-678-6269 (OSU Health Plan)
E-mail: [email protected] or visit yp4h.osu.edu
• Biometric Health Screenings
• Educational Programming
• Personal Health & Well-Being Assessment (PHA)
• Incentive Programs
• Personal and Group Health Coaching Program
• Care Coordination Program
Ohio State Employee Assistance Program (EAP) .. 800-678-6265
• 24/7/365 live connection ..................osuhealthplan.com
Serves faculty, staff and their families
Other Important Contacts
Care Works of Ohio, Inc. .......................888-627-0058
• Workers’ compensation claims assistance
Delta Dental Plan of Ohio ......................800-524-0149
• Customer and Claims Services
• View claims, nd dentist, print ID cards ....toolkitsonline.com
Express Scripts ...............................866-727-5867
• Prescription drugs–retail/home delivery/claims . . express-scripts.com
• Print prescription drug ID cards
Ohio State Travel Assistance
U.S. ...................866-807-6193
International ........01-770-667-0247
Medical care coordination outside Ohio
Ohio State University Health Plan, Inc. ........... 614-292-4700
...........................................800-678-6269
..............................osuhealthplancs@osumc.edu
• Prior authorization of required services and admissions, provider
network inquiries and other medical services
• General benet information and questions . . . osuhealthplan.com
HealthEquity|WageWorks (Flexible Spending Account and HRA
Administrator)Customer Support ...............877-924-3967
Trustmark Health Benets. .....................800-678-6269
• View medical claims ...............myTrustmarkBenets.com
• Print medical ID cards
• COBRA administration
Unum .......................................866-245-3013
• Disability claims assistance
Vision Service Plan (VSP) ......................800-877-7195
• Vision providers and claims assistance ...............vsp.com
THE OHIO STATE UNIVERSITY
Ofce of Human Resources
HR Connection | 614-247-myHR(6947)
1590 North High Street, Suite 300
Columbus, OH 43201-2190
800-678-6010
Fax: 614-292-6235
E-mail: HRConnectio[email protected]
hrconnection.osu.edu
Provides information regarding:
• Certication of state service requests
• Flexible Spending Accounts – Dependent Care and
Health Care
• Health Insurance
• Enrollment
• Verication of coverage
• Life Insurance
• Change of beneciary
• Enrollment
• Retirement Programs
• ARP, OPERS, STRS
•Supplemental Retirement Accounts– 403(b) and 457(b) plans
• Tuition Assistance
• For dependents
• For faculty and staff
• Your Plan for Health, yp4h.osu.edu
Employee and Labor Relations
614-292-2800
Provides information regarding:
• Family/medical leave, sick leave, vacation leave, medical leave,
personal leave, military leave, paid parental leave, organ
donation leave, jury duty/court
Integrated Absence Management and Vocational Service
614-292-3439
800-678-6413
Fax: 614-688-8120
E-mail: id@hr.osu.edu
Available to provide consultation on:
• Department presentations
• Long-term and short-term disability
• OPERS/STRS disability retirement
• Unemployment compensation, 614-688-3578
• Transitional work
• Workers’ compensation
CONTACT INFORMATION
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 3 of 92
Revised 09/2023
INTRODUCTION
This Specic Plan Details document (SPD) describes and establishes important provisions of The Ohio State University Faculty and
Staff Health Plan (the Medical Plan), which provides medical and prescription drug benets to faculty and staff and their eligible
dependents by The Ohio State University and its designated afliates.
ABOUT THIS DOCUMENT
This SPD provides a summary of Ohio State’s medical and prescription drug benets and how you can obtain them.
• You are strongly urged to read this SPD in its entirety. The guidelines dictate how medical claims are processed or considered as
Covered Services under the Medical Plan.
• This SPD is broken down into a number of related sections and is best used by familiarizing yourself with the following:
- The inside front cover – contact information for the services discussed in this SPD, as well as other employee benet programs
maintained by Ohio State.
- The table of contents – the easiest way to navigate this SPD.
- The denitions section – contains a list of important terms used throughout this SPD.
• This SPD also describes your rights and responsibilities as a Covered Person through enrollment in a university-sponsored Medical
Plan. It is important that you have a good understanding of the Covered Services available to you and of the items that are excluded
or limited by the Medical Plan.
ALTERATION OF DOCUMENT
Only the university has the authority to change the coverage and/or terms under the Medical Plans.
TERMS USED IN THIS DOCUMENT
The following terms are used interchangeably throughout this SPD:
• The Ohio State University Faculty and Staff Health Plan Specic Plan Details Document also called Faculty and Staff Health Plan
Specic Plan Details Document, the SPD, or document.
• The Ohio State University Faculty and Staff Health Plan also called the Medical Plans, Ohio State plan, university-sponsored medical
plan and university medical plan.
• Faculty and staff also called you, employee or member.
• The Ohio State University also called Ohio State, the university, the employer and the plan sponsor.
• Ofce of Human Resources also called OHR.
• The Internal Revenue Code of 1986, as amended, also called the Code.
• Other important terms are dened in the “Denitions” section.
COORDINATION OF BENEFITS (COB)
If you or your family members are covered by more than one medical plan, you may not be able to collect benets from both plans.
Each plan may require the covered person to follow its rules or use specic doctors and hospitals, and it may be impossible to comply
with both plans at the same time. Read the rules very carefully, including the “Coordination of Benets” section of this SPD, and
compare these rules with the rules of any other plan that covers you or your family. Pharmacy benets are not coordinated.
OPERATION AND ADMINISTRATION OF THE MEDICAL PLAN
• The Ohio State University is the Plan Sponsor.
• The benets provided under the Medical Plan are paid for directly by Ohio State, which means that the Medical Plan is considered
to be self-funded. Covered employees pay all or part of the cost of providing benets under the Medical Plan through payroll
deductions (i.e., employee contributions) and, if applicable, the employing departments provide the balance.
• Trustmark Health Benets is the university’s third party administrator and COBRA administrator. Trustmark Health Benets is also
referred to as Trustmark. Effective January 1, 2024, Trustmark Health Benets' name will change to Luminare Health. Express
Scripts is the university’s pharmacy benet manager. See page 2 for contact information.
• The Plan Administrator (dened in the “Denitions” section) has the discretionary authority to interpret the Medical Plan in order
to make eligibility and benet determinations as it may determine in its sole discretion. The Plan Administrator also has the
discretionary authority to make factual determinations as to whether any individual is entitled to receive any benets under the
Medical Plan. Benets under the Medical Plan shall be paid only if the Plan Administrator decides in its discretion that a Covered
Person is entitled to them. If any of the authority of the Plan Administrator has been delegated by the Plan Administrator to a
delegate, a reference in this Faculty and Staff Health Plan Specic Plan Details Document to the Plan Administrator shall be deemed
to include a reference to such delegate.
CONTINUED ON PAGE 4
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 4 of 92
Revised 09/2023
COVERED PERSON’S RIGHTS
The university is committed to offering quality medical coverage for its employees and their eligible dependents. As a person
covered by the Medical Plan, you have certain rights that help ensure you and your family members receive quality medical care.
You are expected to be an active participant in your medical care.
AS A COVERED PERSON UNDER THE MEDICAL PLAN, YOU HAVE THE RIGHT TO THE
FOLLOWING:
• Receive and have access to information about the functions of OSU Health Plan, participating medical care providers, terms and
conditions of the Medical Plan, and your rights and responsibilities.
• Receive mental health and substance use disorder treatment consistent with other medical claims and the Mental Health Parity and
Addiction Equity Act and request information from the Plan about relevant claims.
• Fair and respectful consideration and treatment by staff at OSU Health Plan, OHR, Trustmark, Express Scripts, medical care
providers and customer service.
• Condentiality and privacy regarding your medical care matters.
• Receive an explanation of all benets to which you are entitled under the Medical Plan.
• Receive quality medical care through your Medical Plan network in a timely manner and in the most appropriate setting possible.
• Participate with your providers in decision-making about your medical care needs and how best to meet those needs within the
requirements of the Medical Plan.
• Have access to complete and understandable information about your health conditions and the treatments rendered by your medical
care providers.
• Refuse treatment and be informed by your medical care provider or OSU Health Plan of the consequences of such action.
• Be informed of health and wellness, maintenance and preventive programs to help promote and maintain a healthy lifestyle.
• Express concerns and complaints about provider services and administration.
• File a formal appeal, as outlined in the “Medical Claims Processing – Appeal Procedure” and “Prescription Drug – Appeal Procedure”
sections of this SPD.
COVERED PERSON’S RESPONSIBILITIES
For the Medical Plan to work effectively there are certain procedures which you, as a Covered Person, must follow. As a person
covered by the Medical Plan, you have certain responsibilities that will help ensure that you and your family members receive
quality care. You are expected to be an active participant in your medical care.
AS A COVERED PERSON UNDER THE MEDICAL PLAN, YOU HAVE THE RESPONSIBILITY TO:
• Choose a Primary Care Provider who is available to accept new patients and to coordinate medical services as necessary.
• Learn about your coverage options, limitations and exclusions by reviewing the resources available to you.
• Know the rules regarding use of network providers, coverage and Prior Authorization according to the Medical Plan.
• Know how to get information from customer service and/or the Plan Administrator available at osuhealthplan.com.
• Report to OSU Health Plan suspected wrong doing related to medical service and fraud.
• Be a responsible consumer of available health care resources.
• Provide complete, honest and factual information about your medical care status that is needed by providers in order to address your
medical care needs.
• Follow a consensual treatment plan as discussed with and recommended by your medical care providers.
• Listen to and understand the potential consequences that may result should you refuse such treatment.
• Understand your medical and prescription drug benets, as described in this SPD.
• Understand and meet your nancial obligations for copays, annual deductibles, coinsurance and non-covered health-related services,
as indicated in this SPD.
• Provide, when requested, complete and factual information to Trustmark and Express Scripts about any other medical coverage or
insurance benets that you may have.
• Provide, when requested, complete and factual information related to dependency verication.
• Treat other Covered Persons, providers and administrative staff with respect and consideration.
FOR MORE INFORMATION (SEE PAGE 2 FOR CONTACT INFORMATION)
If you have questions when using your medical benets, refer to the following for assistance:
• HR Connection, HRConnection@osu.edu – General benets information, enrollment, eligibility, Publications
• OHR website, hr.osu.edu – Links to provider network listings for the Medical Plan, including network pharmacies
• OSU Health Plan, osuhealthplan.com – Assistance with Prior Authorization of hospital admissions and medical services, provider
listings, general benets information, case management and scheduling of YP4H programming and services
• Third Party Administrator – Trustmark, mytrustmarkbenets.com – Medical claims processing, medical ID card and COBRA
administration
• Pharmacy Benet Manager – Express Scripts, express-scripts.com – Prescription drug claims processing, Prior Authorization for
certain medications, prescription drug ID card
CONTINUED ON PAGE 5
INTRODUCTION
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 5 of 92
Revised 09/2023
DISCRIMINATION IS AGAINST THE LAW
The Ohio State University complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color,
national origin, age, disability, or sex. The Ohio State University does not exclude people or treat them differently because of race, color,
national origin, age, disability, or sex.
The Ohio State University:
• Provides free aids and services to people with disabilities to communicate effectively with us, such as qualied sign language
interpreters and written information in other formats (large print, audio, accessible electronic formats, other formats)
• Provides free language services to people whose primary language is not English, such as qualied interpreters and information
written in other languages.
If you need these services, contact The Ohio State University’s afrmative action and EEO coordinator.
If you believe that The Ohio State University has failed to provide these services or discriminated in another way on the basis of race,
color, national origin, age, disability, or sex, you can le a grievance with:
Afrmative Action and EEO Coordinator
1590 N. High St., Suite 300
Columbus, OH 43201-2190
Phone: 614-292-2800
Fax: 614-292-6199
Email: [email protected]
You can le a grievance in person or by mail, fax, or email. If you need help ling a grievance, the afrmative action and EEO coordinator
is available to help you. You can also le a civil rights complaint with the U.S. Department of Health and Human Services, Ofce for
Civil Rights electronically through the Ofce for Civil Rights Complaint Portal, available at ocrportal.hhs.gov/ocr/portal/lobby.jsf, or by
mail or phone at:
U.S. Department of Health and Human Services
200 Independence Avenue, SW
Room 509F, HMI Building
Washington, D.C. 20201
1-800-868-1019, 800-537-7697 (TDD)
Complaint forms are available at hhs.gov/ocr/ofce/le/index.html.
UPDATING YOUR INFORMATION:
• Inform your departmental human resource contact of any address or name changes or make the change online using Workday at
workday.osu.edu
• Inform HR Connection of any changes you may have in your family status (for example, marriage, divorce, birth or adoption of a
child, dependent child reaching the limiting age, death of a spouse or dependent child) within 30 days of the status
change by using Workday online at workday.osu.edu or by submitting a completed Health Election Form, available at
hr.osu.edu/policies-forms (under Forms - Health Benets -Medical), to OHR.
WHEN RECEIVING COVERED MEDICAL OR PRESCRIPTION DRUG SERVICES:
• Present your medical or prescription drug ID card, as applicable, before receiving medical or prescription drug services.
• At the time of service, you should pay any copay amounts that may apply.
• Notify OSU Health Plan as soon as possible if you are admitted to a hospital, generally within one business day.
• Your health care provider will often le a claim on your behalf. However, if you need to le a medical claim yourself, use the Trustmark
Health Insurance Claim Form found at hr.osu.edu/policies-forms (under Forms - Health Benets – Medical).
• If you need to le a claim for reimbursement of a prescription drug expense go to express-scripts.com for instructions.
• At the time of your provider visit, you should discuss the medical and nancial advantages of generic drugs with your provider.
• Medical and prescription drug claims must be led within 12 months of the date of service.
CONTINUED ON PAGE 6
COVERED PERSON’S RESPONSIBILITIES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

DISCRIMINATION IS AGAINST THE LAW
ATTENTION: If you speak another language, language assistance services, free of charge, are available to you. Call 1-800-264-1552,
Access Code# 80014189.
ATENCIÓN: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 1-800-264-1552, Código de
acceso # 80014189.
注注注注注注注注注注注注注注注注注注注注注注注注注注注注注注1-800-264-1552, 注注注注 # 80014189
ACHTUNG: Wenn Sie Deutsch sprechen, stehen Ihnen kostenlos sprachliche Hilfsdienstleistungen zur Verfügung. Rufnummer:
1-800-264-1552, Zugangscode # 80014189.
注注注注注注: 注注注 注注注 注注注注注 注注注注 注注注注注注 注注注 注注注注注 注注注注注注注注 注注注注注注注 注注注注注注 注注 注注注注注注注. 注注注注 注注注注 1-008-462-2551 注注注 注注注注注注
98141008
Wann du [Deitsch (Pennsylvania German / Dutch)] schwetzscht, kannscht du mitaus Koschte ebber gricke, ass dihr helft mit die englisch
Schprooch. Ruf selli Nummer u: Call 1-800-264-1552, Toegangscode # 80014189.
ВНИМАНИЕ: Если вы говорите на русском языке, то вам доступны бесплатные услуги перевода. Звоните 1-800-264-1552, Код
доступа # 80014189.
ATTENTION : Si vous parlez français, des services d’aide linguistique vous sont proposés gratuitement. Appelez le 1-800-264-1552, Code
d’accès # 80014189.
CHÚ Ý: Nếu bạn nói Tiếng Việt, có các dịch vụ hỗ trợ ngôn ngữ miễn phí dành cho bạn. Gọi số 1-800-264-1552,
mã số truy cập # 80014189.
XIYYEEFFANNAA: Afaan dubbattu Oroomia, tajaajila gargaarsa afaanii, kanfaltiidhaan ala, ni argama. Bilbilaa 1-800-264-1552,
Access Code# 80014189.
注注: 注注注注 注注注注注 注注, 注注 注注 注注注注 注注注 注注注注 注 注注注注. 1-800-264-1552, 注注注 注注
# 80014189, 注注注 注注注 注注注注.
ATTENZIONE: In caso la lingua parlata sia l’italiano, sono disponibili servizi di assistenza linguistica gratuiti. Chiamare il numero
1-800-264-1552, Codice d’accesso # 80014189.
注注注注注注注注注注注注注注注注注注注注注注注注注注注注注注注注注注1-800-264-1552, 注注注注
# 80014189, 注注注注注注注注注注注注注注注注
AANDACHT: Als u nederlands spreekt, kunt u gratis gebruikmaken van de taalkundige diensten. Bel 1-800-264-1552, Toegangscode
# 80014189.
УВАГА! Якщо ви розмовляєте українською мовою, ви можете звернутися до безкоштовної служби мовної підтримки. Телефонуйте
за номером 1-800-264-1552, Код доступу# 80014189.
ATENȚIE: Dacă vorbiți limba română, vă stau la dispoziție servicii de asistență lingvistică, gratuit. Sunați la 1-800-264-1552, Cod de
acces # 80014189.
ATTENTION: If you speak another language, language assistance services, free of charge, are available to you.
Call 1-800-264-1552, Access Code# 80014189.
ATENCIÓN: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 1-800-
264-1552,
Código de acceso # 80014189.
注意:如果您使用繁體中文,您可以免費獲得語言援助服務。請致電 1-800-264-1552, 访问代码 # 80014189
ACHTUNG: Wenn Sie Deutsch sprechen, stehen Ihnen kostenlos sprachliche Hilfsdienstleistungen zur Verfügung.
Rufnummer: 1-800-264-1552,
Zugangscode # 80014189.
ﻢﻗﺮﺑ ﻞﺼﺗ .ﺎﺠﻤﻟﺎﺑ ﻚﻟ ﺮﻓﻮﺘﺗ ﺔﻮﻐﻠﻟ ﺪﻋﺎﺴﻤﻟ ﺎﻣﺪﺧ ﺈﻓ ﺔﻐﻠﻟ ﺮﻛ ﺪﺤﺘﺗ ﺖﻨﻛ :ﺔﻮﺤﻠﻣ1- 008- 462- 2551
ﻮﺧﺪﻟ ﺰﻣ
98141008
Wann du [Deitsch (Pennsylvania German / Dutch)] schwetzscht, kannscht du mitaus Koschte ebber gricke, ass
dihr helft mit die englisch Schprooch. Ruf selli Nummer uff: Call 1-800-264-1552, Toegangscode
# 80014189.
ВНИМАНИЕ: Если вы говорите на русском языке, то вам доступны бесплатные услуги перевода. Звоните
1-800-264-1552,
Код доступа # 80014189.
ATTENTION : Si vous parlez français, des services d'aide linguistique vous sont proposés gratuitement. Appelez
le 1-800-264-1552,
Code d'accès # 80014189.
CHÚ Ý: Nếu bạn nói Tiếng Việt, có các dịch vụ hỗ trợ ngôn ngữ miễn phí dành cho bạn. Gọi số 1-800-264-1552,
mã số truy cập # 80014189.
XIYYEEFFANNAA: Afaan dubbattu Oroomiffa, tajaajila gargaarsa afaanii, kanfaltiidhaan ala, ni argama. Bilbilaa
1-800-264-1552, Access Code# 80014189.
주의: 한국어를 사용하시는 경우, 언어 지원 서비스를 무료로 이용하실 수 있습니다. 1-800-264-1552,
액세스 코드
# 80014189, 번으로 전화해 주십시오.
ATTENZIONE: In caso la lingua parlata sia l'italiano, sono disponibili servizi di assistenza linguistica gratuiti.
Chiamare il numero 1-800-264-1552, Codice d'accesso # 80014189.
注意事項:日本語を話される場合、無料の言語支援をご利用いただけます。1-800-264-1552,
访问代码
# 80014189, まで、お電話にてご連絡ください。
AANDACHT: Als u nederlands spreekt, kunt u gratis gebruikmaken van de taalkundige diensten. Bel 1-800-264-
1552, Toegangscode
# 80014189.
УВАГА! Якщо ви розмовляєте українською мовою, ви можете звернутися до безкоштовної служби мовної
підтримки. Телефонуйте за номером 1-800-264-1552,
Код доступу# 80014189.
ATENȚIE: Dacă vorbiți limba română, vă stau la dispoziție servicii de asistență lingvistică, gratuit. Sunați la 1-
800-264-1552, Cod de acces # 80014189.
1-800-264-1552, # 80014189
ATTENTION: If you speak another language, language assistance services, free of charge, are available to you.
Call 1-800-264-1552, Access Code# 80014189.
ATENCIÓN: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 1-800-
264-1552,
Código de acceso # 80014189.
注意:如果您使用繁體中文,您可以免費獲得語言援助服務。請致電 1-800-264-1552,
访问代码 # 80014189
ACHTUNG: Wenn Sie Deutsch sprechen, stehen Ihnen kostenlos sprachliche Hilfsdienstleistungen zur Verfügung.
Rufnummer: 1-800-264-1552,
Zugangscode # 80014189.
ﻢﻗﺮﺑ ﻞﺼﺗ .ﺎﺠﻤﻟﺎﺑ ﻚﻟ ﺮﻓﻮﺘﺗ ﺔﻮﻐﻠﻟ ﺪﻋﺎﺴﻤﻟ ﺎﻣﺪﺧ ﺈﻓ ﺔﻐﻠﻟ ﺮﻛ ﺪﺤﺘﺗ ﺖﻨﻛ :ﺔﻮﺤﻠﻣ1- 008- 462- 2551
ﻮﺧﺪﻟ ﺰﻣ
98141008
Wann du [Deitsch (Pennsylvania German / Dutch)] schwetzscht, kannscht du mitaus Koschte ebber gricke, ass
dihr helft mit die englisch Schprooch. Ruf selli Nummer uff: Call 1-800-264-1552, Toegangscode
# 80014189.
ВНИМАНИЕ: Если вы говорите на русском языке, то вам доступны бесплатные услуги перевода. Звоните
1-800-264-1552,
Код доступа # 80014189.
ATTENTION : Si vous parlez français, des services d'aide linguistique vous sont proposés gratuitement. Appelez
le 1-800-264-1552,
Code d'accès # 80014189.
CHÚ Ý: Nếu bạn nói Tiếng Việt, có các dịch vụ hỗ trợ ngôn ngữ miễn phí dành cho bạn. Gọi số 1-800-264-1552,
mã số truy cập # 80014189.
XIYYEEFFANNAA: Afaan dubbattu Oroomiffa, tajaajila gargaarsa afaanii, kanfaltiidhaan ala, ni argama. Bilbilaa
1-800-264-1552, Access Code# 80014189.
주의: 한국어를 사용하시는 경우, 언어 지원 서비스를 무료로 이용하실 수 있습니다. 1-800-264-1552, 액세스 코드
# 80014189, 번으로 전화해 주십시오.
ATTENZIONE: In caso la lingua parlata sia l'italiano, sono disponibili servizi di assistenza linguistica gratuiti.
Chiamare il numero 1-800-264-1552, Codice d'accesso # 80014189.
注意事項:日本語を話される場合、無料の言語支援をご利用いただけます。1-800-264-1552,
访问代码
# 80014189, まで、お電話にてご連絡ください。
AANDACHT: Als u nederlands spreekt, kunt u gratis gebruikmaken van de taalkundige diensten. Bel 1-800-264-
1552, Toegangscode
# 80014189.
УВАГА! Якщо ви розмовляєте українською мовою, ви можете звернутися до безкоштовної служби мовної
підтримки. Телефонуйте за номером 1-800-264-1552,
Код доступу# 80014189.
ATENȚIE: Dacă vorbiți limba română, vă stau la dispoziție servicii de asistență lingvistică, gratuit. Sunați la 1-
800-264-1552, Cod de acces # 80014189.
1-800-264-1552,
# 80014189,
ATTENTION: If you speak another language, language assistance services, free of charge, are available to you.
Call 1-800-264-1552, Access Code# 80014189.
ATENCIÓN: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 1-800-
264-1552,
Código de acceso # 80014189.
注意:如果您使用繁體中文,您可以免費獲得語言援助服務。請致電 1-800-264-1552,
访问代码 # 80014189
ACHTUNG: Wenn Sie Deutsch sprechen, stehen Ihnen kostenlos sprachliche Hilfsdienstleistungen zur Verfügung.
Rufnummer: 1-800-264-1552,
Zugangscode # 80014189.
ﻢﻗﺮﺑ ﻞﺼﺗ .ﺎﺠﻤﻟﺎﺑ ﻚﻟ ﺮﻓﻮﺘﺗ ﺔﻮﻐﻠﻟ ﺪﻋﺎﺴﻤﻟ ﺎﻣﺪﺧ ﺈﻓ ﺔﻐﻠﻟ ﺮﻛ ﺪﺤﺘﺗ ﺖﻨﻛ :ﺔﻮﺤﻠﻣ1- 008- 462- 2551
ﻮﺧﺪﻟ ﺰﻣ
98141008
Wann du [Deitsch (Pennsylvania German / Dutch)] schwetzscht, kannscht du mitaus Koschte ebber gricke, ass
dihr helft mit die englisch Schprooch. Ruf selli Nummer uff: Call 1-800-264-1552, Toegangscode
# 80014189.
ВНИМАНИЕ: Если вы говорите на русском языке, то вам доступны бесплатные услуги перевода. Звоните
1-800-264-1552,
Код доступа # 80014189.
ATTENTION : Si vous parlez français, des services d'aide linguistique vous sont proposés gratuitement. Appelez
le 1-800-264-1552,
Code d'accès # 80014189.
CHÚ Ý: Nếu bạn nói Tiếng Việt, có các dịch vụ hỗ trợ ngôn ngữ miễn phí dành cho bạn. Gọi số 1-800-264-1552,
mã số truy cập # 80014189.
XIYYEEFFANNAA: Afaan dubbattu Oroomiffa, tajaajila gargaarsa afaanii, kanfaltiidhaan ala, ni argama. Bilbilaa
1-800-264-1552, Access Code# 80014189.
주의: 한국어를 사용하시는 경우, 언어 지원 서비스를 무료로 이용하실 수 있습니다. 1-800-264-1552,
액세스 코드
# 80014189, 번으로 전화해 주십시오.
ATTENZIONE: In caso la lingua parlata sia l'italiano, sono disponibili servizi di assistenza linguistica gratuiti.
Chiamare il numero 1-800-264-1552, Codice d'accesso # 80014189.
注意事項:日本語を話される場合、無料の言語支援をご利用いただけます。1-800-264-1552, 访问代码
# 80014189, まで、お電話にてご連絡ください。
AANDACHT: Als u nederlands spreekt, kunt u gratis gebruikmaken van de taalkundige diensten. Bel 1-800-264-
1552, Toegangscode
# 80014189.
УВАГА! Якщо ви розмовляєте українською мовою, ви можете звернутися до безкоштовної служби мовної
підтримки. Телефонуйте за номером 1-800-264-1552,
Код доступу# 80014189.
ATENȚIE: Dacă vorbiți limba română, vă stau la dispoziție servicii de asistență lingvistică, gratuit. Sunați la 1-
800-264-1552, Cod de acces # 80014189.
1-800-264-1552,
# 80014189,
ATTENTION: If you speak another language, language assistance services, free of charge, are available to you.
Call 1-800-264-1552, Access Code# 80014189.
ATENCIÓN: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 1-800-
264-1552,
Código de acceso # 80014189.
注意:如果您使用繁體中文,您可以免費獲得語言援助服務。請致電 1-800-264-1552,
访问代码 # 80014189
ACHTUNG: Wenn Sie Deutsch sprechen, stehen Ihnen kostenlos sprachliche Hilfsdienstleistungen zur Verfügung.
Rufnummer: 1-800-264-1552,
Zugangscode # 80014189.
ﻢﻗﺮﺑ ﻞﺼﺗ .ﺎﺠﻤﻟﺎﺑ ﻚﻟ ﺮﻓﻮﺘﺗ ﺔﻮﻐﻠﻟ ﺪﻋﺎﺴﻤﻟ ﺎﻣﺪﺧ ﺈﻓ ﺔﻐﻠﻟ ﺮﻛ ﺪﺤﺘﺗ ﺖﻨﻛ :ﺔﻮﺤﻠﻣ1
-
008
-
462
-
2551 ﻮﺧﺪﻟ ﺰﻣ
98141008
Wann du [Deitsch (Pennsylvania German / Dutch)] schwetzscht, kannscht du mitaus Koschte ebber gricke, ass
dihr helft mit die englisch Schprooch. Ruf selli Nummer uff: Call 1-800-264-1552, Toegangscode
# 80014189.
ВНИМАНИЕ: Если вы говорите на русском языке, то вам доступны бесплатные услуги перевода. Звоните
1-800-264-1552,
Код доступа # 80014189.
ATTENTION : Si vous parlez français, des services d'aide linguistique vous sont proposés gratuitement. Appelez
le 1-800-264-1552,
Code d'accès # 80014189.
CHÚ Ý: Nếu bạn nói Tiếng Việt, có các dịch vụ hỗ trợ ngôn ngữ miễn phí dành cho bạn. Gọi số 1-800-264-1552,
mã số truy cập # 80014189.
XIYYEEFFANNAA: Afaan dubbattu Oroomiffa, tajaajila gargaarsa afaanii, kanfaltiidhaan ala, ni argama. Bilbilaa
1-800-264-1552, Access Code# 80014189.
주의: 한국어를 사용하시는 경우, 언어 지원 서비스를 무료로 이용하실 수 있습니다. 1-800-264-1552,
액세스 코드
# 80014189, 번으로 전화해 주십시오.
ATTENZIONE: In caso la lingua parlata sia l'italiano, sono disponibili servizi di assistenza linguistica gratuiti.
Chiamare il numero 1-800-264-1552, Codice d'accesso # 80014189.
注意事項:日本語を話される場合、無料の言語支援をご利用いただけます。1-800-264-1552,
访问代码
# 80014189, まで、お電話にてご連絡ください。
AANDACHT: Als u nederlands spreekt, kunt u gratis gebruikmaken van de taalkundige diensten. Bel 1-800-264-
1552, Toegangscode
# 80014189.
УВАГА! Якщо ви розмовляєте українською мовою, ви можете звернутися до безкоштовної служби мовної
підтримки. Телефонуйте за номером 1-800-264-1552,
Код доступу# 80014189.
ATENȚIE: Dacă vorbiți limba română, vă stau la dispoziție servicii de asistență lingvistică, gratuit. Sunați la 1-
800-264-1552, Cod de acces # 80014189.
98141008
2551 462 008 1
The Ohio State University Ofce of Human Resources PAGE 6 of 92
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024 Revised 09/2023

PAGE 7 of 92
Revised 09/2023
GENERAL PLAN PROVISIONS
The following terms and conditions apply to all coverage options available under the Medical Plan.
ELIGIBILITY
• Employee holds a Qualifying Appointment. An eligible employee is any faculty or staff member who holds a qualifying
appointment, as determined by The Ohio State University. Details are available at hr.osu.edu/benets/eligibility.
• Employee does not hold a Qualifying Appointment. In addition, an eligible employee is any employee who does not hold a
qualifying appointment but is a “full-time employee.” In general, a full-time employee is an individual who is employed, on average,
for at least 30 hours of service per week. The university uses a look-back measurement method to determine who is a full-time
employee for purposes of coverage under the Medical Plan. The look-back measurement method is based on Internal Revenue
Service regulations under the Patient Protection and Affordable Care Act (PPACA). The look-back measurement method applies to
all university employees.
The look-back measurement method involves three different periods:
- A measurement period for counting an employee’s hours of service. If you are an ongoing employee, this measurement period
(which is also called the “standard measurement period”) ran from October 5, 2022 through October 4, 2023 and determined
your Medical Plan eligibility for the 2024 Plan Year. If you are a new employee who is a variable hour employee, this measurement
period will follow your employment with the university and will last for 11 months.
- A stability period is a period that follows a measurement period. An employee’s hours of service during the measurement period
will determine whether the employee is a full-time employee who is eligible for coverage during the stability period. As a general
rule, the employee’s status as a full-time employee or not a full-time employee is “locked in” for the stability period, regardless of
how many hours the employee works during the stability period, while the employee remains employed. The stability period will
last for 12 months.
- An administrative period is a short period between the measurement period and the stability period when the university performs
administrative tasks, such as determining eligibility for coverage.
Note that special rules apply when employees are rehired by the university or return from an unpaid leave of absence. The rules for
the look-back measurement method are very complex. This is just a general overview of how the rules work. More complex rules may
apply to an employee’s situation. The university intends to follow Internal Revenue Service regulations and any future guidance issued
by the Internal Revenue Service when administering the look-back measurement method.
• If you are an eligible employee, you may cover yourself and those persons who qualify as your eligible dependents. Dependents
can only be enrolled if you are enrolled in coverage. If your spouse or child is an eligible employee, he or she may have employee
coverage or dependent coverage (but not both). If both parents are eligible employees, your children may be covered as dependents
of either (but not both) of you.
• Coverage is not automatic. To cover yourself and your eligible dependents, you must enroll. To enroll in the Medical Plan, use
Workday online at workday.osu.edu or submit a completed Health Election Form, available at hr.osu.edu/policies-forms (under
Forms - Health Benets – Medical). The Medical Plan will not cover a person as both a Covered Employee and dependent or as a
dependent of more than one Covered Employee.
• The university has the ability to rescind (i.e., retroactively terminate) coverage if such coverage was gained due to an individual
(or person seeking coverage on behalf of the individual) performing an act, practice or omission that constitutes fraud or making
an intentional misrepresentation of material fact.
• All Employees and Members of the Employee’s Household: This Medical Plan also provides Employee Assistance Services to all
employees and members of the employee’s household. There is no enrollment necessary, nor are employees charged a premium for
this benet. Please call 800-678-6265 for EAP services.
• All Benets Eligible Employees: This Medical Plan provides you with access to no cost OSU u shots at an on-campus location while
supplies last. For details or to register for an appointment visit osuhealthplan.com/programs-and-services/u-vaccination.
ENROLLMENT
To enroll in the Medical Plan, use Workday online at workday.osu.edu or submit a completed Health Election Form, available at
hr.osu.edu/policies-forms (under Forms - Health Benets – Medical). You must enroll in the desired medical coverage option:
• Within 30 days of appointment in an eligible position as reected in the university’s human resource system (Workday).
• Within 30 days of loss of other eligible coverage.
• During the annual open enrollment period.
• In connection with a qualifying status change as described in the “Change in Coverage Due to Qualifying Status Change” section of
this SPD.
• In connection with an event that provides special enrollment rights as described in “Special Enrollment Rights” below.
• In limited circumstances, you may be eligible to enroll in the Medical Plan on an after-tax basis as described in the “Coverage
Elections Outside an Enrollment Period” section of this SPD.
CONTINUED ON PAGE 8
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 8 of 92
Revised 09/2023
SPECIAL ENROLLMENT RIGHTS
Children’s Health Insurance Program Reauthorization Act of 2009 (CHIPRA)
• CHIPRA provides you and your dependent(s) with special enrollment rights for Medical Plan coverage without having to wait for an
open enrollment period if either of the following occurs:
- You or your dependent(s) are terminated from Medicaid or state Children’s Health Insurance Program (CHIP) coverage as a result
of a loss of eligibility. If so, you must request this special enrollment within 60 days of the loss of coverage.
IMPORTANT NOTE: If you, or your eligible dependent, have a loss of Medicaid or CHIP coverage between March 31, 2023,
and July 31, 2024, you are eligible for a temporary special enrollment period. Details can be found at hr.osu.edu/wp-content/
uploads/20230512-SMM-Coverage-CHIP-Changes.html. For a printed copy of this information call 1-800-678-6010.
- You or your dependent(s) become eligible for a premium assistance subsidy under Medicaid or CHIP. If so, you must request this
special enrollment within 60 days of when eligibility is determined.
• To enroll in the Medical Plan, you and your dependent(s) must be benets-eligible and you must use Workday online at
workday.osu.edu or submit a completed Health Election Form, available at hr.osu.edu/policies-forms (under Forms - Health
Benets - Medical). Documentation of the above event is required.
Health Insurance Portability and Accountability Act of 1996 (HIPAA)
• HIPAA provides you and your eligible dependents with special enrollment rights for Medical Plan coverage without having to wait for
an open enrollment period if either of the following occurs:
- You acquire an eligible dependent after your employment begins as a result of marriage, birth, adoption, or placement for adoption.
- You (or your eligible dependent) were covered under another group health plan or had other health insurance coverage when you
declined coverage under a university Medical Plan and you (or your eligible dependent) lose that other coverage because of loss of
eligibility (other than for failure to pay premiums or termination for cause), termination of employer contributions or exhaustion of
COBRA continuation coverage.
If either of these events occurs, you must request this special enrollment within 30 days of the date of the event.
• To enroll in a university the Medical Plan, you and your dependents must be benets-eligible and you must use Workday online at
workday.osu.edu or submit a completed Health Election Form, available at hr.osu.edu/policies-forms (under Forms - Health Benets
- Medical). Documentation of the above event is required.
EFFECTIVE DATE OF COVERAGE
The effective date for all eligible employees and their eligible dependents will be determined by the university. Coverage will be
communicated to Trustmark and Express Scripts for the purposes of claims administration. Coverage will be
effective on:
• Date of hire or transfer to an eligible appointment as reected in the university’s human resource system (Workday).
• Date of a qualifying status change
• January 1 of a new Plan Year, if the election is made during and as part of the annual open enrollment period
• First day of the employee’s “stability period” as determined by the university. See the “Eligibility” section of this SPD.
ELIGIBLE DEPENDENTS
Spouse
An individual whose marriage to a Covered Employee is recognized by the Internal Revenue Service for federal income tax purposes.
A legally separated spouse is not eligible.
Dependent child
Child of a Covered Employee who meets all of the following eligibility criteria:
1. Has not reached the age limit of 26 (e.g., 26th birthday); except in cases described more fully below, and
2. Fits into one of the following categories:
- The employee’s biological child;
- The employee’s adopted child or child placed with the employee for adoption;
- The employee’s step-child; or
- The child for whom the employee has legal guardianship, or legal custody, and such child is the employee’s tax dependent.
Dependent child coverage beyond the age limit due to disability
A dependent child may be eligible for continued coverage as a dependent child after attaining age 26 if:
• The child is and continues to be incapable of self-sustaining employment by reason of physical handicap or intellectual disability; and
• The child is the employee’s dependent as dened in Section 105(b) of the Code; and
• The child was (1) covered by the Medical Plan when he or she reached the limiting age and the employee makes application for
continuation of coverage to the university within 30 days after the child’s loss of coverage due to reaching the limiting age; or (2)
covered as a dependent under the medical plan of his or her parent’s employer immediately prior to a loss of coverage under such
plan (documentation of prior coverage required) and the employee makes application for continuation of coverage to the university
within 30 days after such loss of coverage occurs. In each case, the employee must provide satisfactory proof of the child’s
incapacity and dependence upon the employee; and
• The employee provides proof of the continuance of such incapacity and dependence upon request by the university.
Consult with a tax advisor with any questions regarding whether or not the child meets the Code requirements.
CONTINUED ON PAGE 9
GENERAL PLAN PROVISIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 9 of 92
Revised 09/2023
The following terms and conditions apply to all coverage options available under the Medical Plan.
Grandfathered Sponsored Dependent (Afdavit of Sponsored Dependency required)
The grandfathered sponsored dependent of a covered employee who meets all of the following criteria:
1. The individual was enrolled in The Ohio State University Faculty and Staff Health Plan as a sponsored dependent as of
December 31, 2016;
2. The individual remains continuously enrolled in The Ohio State University Faculty and Staff Health Plan on and after
December 31, 2016;
3. The individual meets all of the following criteria:
a. The individual resides at the same principal place of abode as the employee and is a member of the employee’s household for the
entire tax year during which grandfathered sponsored dependent coverage is provided;
b. The individual shares a relationship with the employee as dened by one of the following:
- Parent, step-parent, parent-in-law, or person who stood in loco parent is to the employee as a child
- Grandparent or grandparent of the employee’s spouse
- Sibling or sibling-in-law
- Aunt or uncle
- Niece or nephew
- Son or daughter-in-law
- Grandchild or spouse of the employee’s grandchild
- Biological, adopted, step or foster child who is not otherwise eligible for coverage under the terms of the university Medical Plan
- Opposite-sex domestic partner who is unmarried, is not related to the employee by blood to a degree of closeness which would
prohibit marriage in the state in which they legally reside and who has been in a relationship with the employee for at least
six (6) months and intends to remain so indenitely
- Dependent child of an opposite-sex domestic partner (described above);
c. The individual is dependent upon the employee for more than 50% of his or her support. The employee must be able to provide
documentation of such support to OHR or to Trustmark for claims administration, if requested, to verify the dependent status of
this individual.
Support includes:
i. Housing/shelter;
ii. Cost for his or her clothing, food, education, recreation and transportation expenses;
iii. Cost for his or her medical, dental and/or vision care; and
iv. Cost for a proportionate share of other expenses necessary to support the grandfathered sponsored dependent within the
employee’s household (such as food and utilities), but which cannot be directly attributed to that individual;
d. The individual is enrolled in Medicare if he or she is eligible for such coverage. The university’s Medical Plan will be a secondary
payer to Medicare, unless the individual is a family member (not a spouse) who is entitled to Medicare on account of disability; and
e. The individual is the employee’s dependent under Section 152 of the Code, without regard to subsection (d) (1) (B) of Section 152.
Consult with a tax advisor with any questions regarding whether or not the individual meets the Internal Revenue Service
qualications.
Regardless of any other provision in this SPD to the contrary, a grandfathered sponsored dependent must remain enrolled in the
Medical Plan for the entire Plan Year, unless the grandfathered sponsored dependent dies or the grandfathered sponsored dependent
provides proof of obtaining other medical coverage.
CHANGE IN COVERAGE DUE TO A QUALIFYING STATUS CHANGE
• You may enroll in coverage, make changes to your coverage, or disenroll from coverage during the Plan Year (i.e., outside of open
enrollment) only if you experience a qualifying status change. The change in coverage must be consistent with and on account of
the qualifying status change (e.g., you cover your spouse following your marriage). If you wish to change your elections due to a
qualifying status change, the Ofce of Human Resources must receive such change within 30 days of the qualifying status change.
CONTINUED ON PAGE 10
GENERAL PLAN PROVISIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 10 of 92
Revised 09/2023
The following terms and conditions apply to all coverage options available under the Medical Plan.
Qualifying Status Change
• Qualifying status changes include:
- Change in your legal marital status (marriage, death of a spouse (as dened in the Code), divorce, legal separation or annulment);
- Termination of a grandfathered sponsored dependency;
- Change in the number of your dependents (birth, death, adoption or placement for adoption);
- Change in your employment status (termination of employment, commencement of employment, strike, lockout, commencement
of an approved family medical (FML) leave of absence, return from an approved family medical (FML) leave of absence or change in
worksite), or the employment status of your spouse or your dependents that results in the individual becoming eligible, or ceasing
to be eligible, under any cafeteria plan or other employee welfare benet plan of your employer or the employer of your spouse or
dependent;
- Event that causes your dependent to satisfy or cease to satisfy the requirements for coverage due to attainment of age or any
similar circumstances;
- Change in your employment status (termination of employment, commencement of employment, strike, lockout, commencement
of an approved family medical (FML) leave of absence, return from an approved family medical (FML) leave of absence or change in
worksite), or the employment status of your spouse or your dependents that results in the individual becoming eligible, or ceasing
to be eligible, under any cafeteria plan or other employee welfare benet plan of your employer or the employer of your spouse or
dependent;
- Termination of your or your dependent’s Medicaid or Children’s Health Insurance Program (CHIP) coverage as a result of loss of
eligibility (you must submit an election change within 60 days);
- You or your dependent becomes eligible for a premium assistance subsidy under Medicaid or CHIP (you must submit an election
change within 60 days); or
- Entitlement to Medicare or Medicaid.
• In addition, you might be able to make a change under the following circumstances:
- Judgment, decree or order requiring coverage of certain dependents (30-day time limit does not apply);
- Certain leaves of absence;
- Signicant changes in cost of coverage, including a signicant change in medical contributions due to a change in full-time
equivalency;
- Signicant curtailment of coverage;
- If you have a change in employment status during a stability period that is expected to reduce your average hours to less than 30
hours per week, you may drop Medical Plan coverage, provided that you expect to enroll in other health coverage (for example,
through a spouse or the purchase of health insurance);
- Certain changes in or loss of coverage under another plan;
- Certain additions or improvements to benet package options; or
- You, your spouse or dependent enroll in health insurance purchased through the public Marketplace effective other than January 1
in connection with a Marketplace special enrollment event.
Note: Qualifying status change determinations are made by the university in accordance with the provisions of The Ohio State
University Flexible Benets Plan and Internal Revenue Service rules. For questions about what constitutes a qualifying status change,
contact HR Connection at 614-247-myHR(6947), 800-678-6010 or HRConnectio[email protected], or refer to the Life Events section of the
OHR website at hr.osu.edu/life-events.
If a Qualifying Status Change Occurs:
• If a qualifying status change occurs, you must make an election by using Workday online at workday.osu.edu or by submitting a
completed Health Election Form, available at hr.osu.edu/policies-forms (under Forms - Health Benets – Medical). Documentation
may be required for some events. The university must approve any qualifying status change.
• You may make an election in the following ways:
- Use Workday at workday.osu.edu. The election and any required documentation must be submitted through Workday within 30
days of the qualifying status change (except as otherwise noted).
- Complete a Health Election Form, available at hr.osu.edu/policies-forms (under Forms - Health Benets – Medical). The completed
form and any required documentation must be submitted to HR Connection within 30 days of the qualifying status change (except
as otherwise noted).
• Changes in coverage and contributions will be effective as of the date of the qualifying status change. Contributions will be prorated
based on the exact days of coverage because of the qualifying status change.
- If you do not complete and submit a Health Election Form or make an election via Workday at workday.osu.edu within 30 days
(except as otherwise noted above), you will not be allowed to make a change until the next open enrollment period or upon the
occurrence of a future qualifying status change.
Note: A newborn infant must be added within 30 days of the birth. Otherwise the newborn cannot be added until the next open
enrollment period. If coverage is already in effect, you must add the newborn, even if you have family coverage.
Note: Your coverage level and premium contributions may be adjusted based on the qualifying status change. Contributions will be
prorated based on the exact days of coverage because of the qualifying status change.
CONTINUED ON PAGE 11
GENERAL PLAN PROVISIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 11 of 92
Revised 09/2023
Coverage elections for rehires
• If your employment with the university terminates and you are rehired into a benets-eligible position within 30 days after that
termination, you and your eligible dependents will be reinstated with the same elections that you had immediately before your
termination and accumulations for plan features such as annual deductibles and out-of-pocket limits, as well as expenses you had
accumulated towards the Medical Plan’s lifetime maximums, will continue to apply as if there was no loss of coverage. See the
“Health Reimbursement Account (HRA)” section of this SPD for details related to your HRA.
• If your employment with the university terminates and you are rehired into a benets-eligible position more than 30 days after
that termination, you will be able to make new elections as to your coverage levels and coverage options under the Medical Plan.
If you re-enroll within the same Plan Year, plan features such as annual deductibles and annual out-of-pocket maximums, as well
as expenses you had accumulated towards the Medical Plan’s lifetime maximums, will continue to apply as if there was no loss of
coverage. See the “Health Reimbursement Account (HRA)” section of this SPD for details related to your HRA.
COVERAGE ELECTIONS OUTSIDE AN ENROLLMENT PERIOD
Introduction
If you are in an eligible university faculty or staff appointment and an enrollment period, as described in “Enrollment” above (e.g.,
newly eligible, qualifying status change, annual open enrollment), is missed or if coverage under the Medical Plan is terminated by the
university because an otherwise eligible Covered Employee did not take a required action to maintain eligibility (e.g., fully respond to
Dependent Eligibility Verication (DEV), apply timely for continued coverage for a disabled child who has reached the limiting age), the
Covered Employee may elect to participate in the Medical Plan described in this SPD on an after-tax basis by submitting a paper After-
Tax Medical Election Form, which is available by calling 614-247-myHR(6947). After-tax medical coverage elections and changes to
those elections cannot be completed through Workday. COTC employees, OSUP employees, Graduate Associates and Post-Doctoral
Fellows are not eligible for this coverage.
• Eligible employees, as described above, and any eligible dependents of Covered Employees, as described in the “Eligible
Dependents” section of this SPD, may enroll in after-tax medical coverage. However, the following exceptions shall apply to
disabled children who have reached the limiting age and dependents whose coverage has been terminated because the required
documentation was not submitted for DEV:
- Disabled children who have reached the limiting age. An After-Tax Medical Election Form and an Application for Continued
Health Plan Eligibility for Over Age Dependents available by calling 614-247-myHR(6947) must be submitted to OSU Health Plan
for approval. OSU Health Plan will determine if the child was continuously disabled from the date that previous employer medical
coverage ended through the date that after-tax medical coverage has been requested. OSU Health Plan will notify OHR of the
approval or denial. If denied, OSU Health Plan will notify the employee of the denial in writing. If approved, OSU Health Plan will
notify the employee of the approval and effective date in writing.
- DEV. For dependents whose coverage has been terminated because the required documentation was not submitted for DEV, an
After-Tax Medical Election form must be submitted to OHR. In addition, all required documents must be submitted so dependent
eligibility can be conrmed. Coverage will be effective on the date that the required documentation for DEV and the After-Tax
Medical Election Form have been received.
• If an employee has existing coverage under the Medical Plan and then applies for after-tax medical coverage for a dependent(s), the
coverage option elected for after-tax medical coverage must be the same coverage option in which the employee is already enrolled.
• If an employee enrolls in after-tax medical coverage, the employee cannot terminate that coverage for the remainder of the Plan Year,
provided that the employee and, if applicable, his or her dependents remain eligible to participate in the university’s Medical Plan.
Exceptions to this requirement: (1) coverage for an eligible dependent may be terminated if the dependent dies; or (2) the
termination meets the criteria described in the “After-Tax Medical Enrollment Changes During the Plan Year” section below.
After-Tax Medical Enrollment Changes During the Plan Year
• If, after enrolling in after-tax medical coverage, a Covered Employee or his or her dependent experiences a subsequent special
enrollment event, as described in the “SPECIAL ENROLLMENT RIGHTS” section of this SPD, the employee will have the right
to enroll in pre-tax medical coverage and, if desired, be allowed to elect a different coverage option under the Medical Plan on
a pre-tax basis. Any such enrollment changes must meet the requirements of a special enrollment event, including any
deadlines to request special enrollment, and require a completed After-Tax Medical Election Form, which is available by calling
614-247-myHR(6947). After-tax medical coverage cannot be dropped or changed through Workday.
• Regardless of any other provision in this SPD to the contrary, no other enrollment changes to after-tax medical coverage will be
permitted during the Plan Year.
Effective Date of Coverage
• Coverage will be effective on the date that the After-Tax Medical Election Form and all required documents are received by OHR or
OSU Health Plan when an Application for Continued Health Plan Eligibility for Over Age Dependents is being submitted.
• However, there is an exception in limited circumstances if the late enrollment request is to add (1) a newborn child, (2) a newly
adopted child, (3) a child placed for adoption or (4) a child for whom the employee has legal guardianship or legal custody and
such child is the employee’s tax dependent. In that case, if the After-Tax Medical Election form is received by OHR within 90 days
of the event (i.e., birth, adoption or placement), the after-tax medical coverage will be effective as of the date of such event. After-
tax premium contributions will be deducted for the retroactive coverage and will be calculated beginning with the date in which
coverage begins.
CONTINUED ON PAGE 12
GENERAL PLAN PROVISIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 12 of 92
Revised 09/2023
Contributions
• After-tax premium contributions will be charged beginning with the date in which coverage is effective.
• If the employee has existing pre-tax medical coverage, that premium will continue to be deducted on a pre-tax basis in addition to
the after-tax premium contributions.
• The current contribution rates are available by calling 614-247-myHR(6947).
Annual Termination of After-Tax Coverage
• Except in the case of disabled children who have reached the limiting age, after-tax medical coverage will terminate at the end of the
Plan Year. If an eligible employee desires to maintain medical coverage for himself or herself and/or his or her eligible dependents, the
employee must enroll in pre-tax medical coverage for the next Plan Year during the annual open enrollment period.
• Disabled children who have reached the limiting age and who are enrolled in after-tax medical coverage will remain enrolled in the
after-tax medical coverage unless such coverage is waived by the covered employee for the next Plan Year during the annual open
enrollment period. Those children are not eligible to enroll in pre-tax medical coverage during the annual open enrollment period.
CONTINUED ON PAGE 13
GENERAL PLAN PROVISIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 13 of 92
Revised 09/2023
The following terms and conditions apply to all coverage options available under the Medical Plan.
ID CARDS
You will receive a medical ID card shortly after your effective date of coverage. Check your cards to make sure that the information is
correct. If the information is incorrect, contact HR Connection by calling 614-247-myHR(6947). If your medical ID card is lost, stolen,
or you need additional cards, go to mytrustmarkbenets.com to order or print additional cards. To view or print your prescription drug
ID card, go to express-scripts.com. Contact information is available on page 2 of this SPD.
MEDICAL CARE OUTSIDE OHIO OR INTERNATIONALLY
• If you are enrolled in the Medical Plan, you are covered for emergency care outside Ohio and internationally. To determine your
coverage level, carefully read the Schedule of Benets available for your coverage option or contact OSU Health Plan for assistance.
• When paying for international medical services, request that the doctor or hospital complete a description of services provided
translated into English. This is required for your medical coverage reimbursement when you return home. Refer to the “Ohio State
Travel Assistance” section of this SPD for details.
CASE MANAGEMENT
• In order to provide a comprehensive approach to the management of specialized medical care, OSU Health Plan provides and when
necessary requires, case management services. Case management is a collaborative process that assesses, plans, implements,
coordinates, monitors and evaluates resources to promote quality and cost-effective outcomes. To accomplish this, input is obtained
from providers, patients, family members (with patient’s authorization), medical consultants and other sources. Patients are informed
of approved settings for medical treatment options.
• On an exception basis, subject to OSU Health Plan’s case management process, medical benets may be provided for settings and/
or procedures not expressly provided for, but not prohibited by law, rule, or general policy. All requests for case management will be
individually reviewed by OSU Health Plan.
• OSU Health Plan has the right to deny consideration of benets under case management if the use of such services is not clinically
or Medically Necessary . This is inclusive of all services, those normally reviewed by case management, special requests for case
management and any appeals to OSU Health Plan.
PRIVACY OF PROTECTED HEALTH INFORMATION (PHI)
Federal HIPAA regulations restrict how the university and the Medical Plan may use medical information about you and your family.
Permitted Uses and Disclosures
• The Medical Plan may use or disclose PHI to the university, provided that the university does not use or disclose that information
except for the following purposes:
- To perform health plan administrative functions,
- To obtain premium bids for group health insurance, or
- To modify, amend or terminate the plans.
• The Medical Plan may also disclose PHI to the university pursuant to your written authorization.
• All uses and disclosures of PHI must be consistent with HIPAA.
Conditions of Disclosure
• The Medical Plan may disclose PHI to the university only upon receipt of a certication from the university, as plan sponsor of the
Medical Plan, that the plan documents have been amended to incorporate the provisions set forth below and that the university, in
its capacity as plan sponsor, agrees to such provisions.
• The university, as plan sponsor of the Medical Plan, agrees to:
- Not use or further disclose PHI other than as permitted or required by plan documents or as required by law.
- Ensure that any agents or subcontractors to whom it provides PHI received from the Medical Plan agrees to the same restrictions
and conditions that apply to the university with respect to such PHI and that they agree to implement reasonable and appropriate
security measures to protect the information.
- Not use or disclose the PHI received from the Medical Plan for employment-related actions and decisions or in connection with any
other benet or employee benet plan of the university (except to the extent that such other benet or employee benet plans is
part of an organized health care arrangement of which the Medical Plan is a part).
- Report to the Medical Plan any use or disclosure of the information that is inconsistent with the uses or disclosures provided.
- Report to the Medical Plan any security incident of which it becomes aware.
- Make a covered person’s PHI available to them if they request access, in accordance with federal HIPAA regulations.
- Incorporate any approved amendments to a covered person’s PHI requested by the covered person, in accordance with federal
HIPAA regulations.
- Make available an accounting of disclosures of a covered person’s PHI when requested by the covered person, in accordance with
federal HIPAA regulations.
• Make internal practices, books and records relating to the use and disclosure of PHI received from the Medical Plan available to the
Secretary of Health and Human Services for purposes of determining compliance of the Medical Plan with the law.
CONTINUED ON PAGE 14
GENERAL PLAN PROVISIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 14 of 92
Revised 09/2023
• If feasible, return or destroy all PHI received from the Medical Plan that the university still maintains in any form and retain no
copies of information when no longer needed for the purpose for which the disclosure was made. If such return or destruction is not
feasible, limit further uses and disclosures to those purposes that make the return or destruction of the information feasible.
• Ensure adequate separation between the Medical Plan and the university as required by federal law.
Permitted Uses and Disclosures of Aggregate Health Information
• The
Medical Plan
may disclose Aggregate Health Information (see the “Denitions” section of this SPD) to the university, provided
that the Aggregate Health Information is only used by the university for the purpose of:
- Obtaining premium bids for providing health insurance coverage; or
- Modifying, amending, or terminating the
Medical Plan
.
Permitted Uses Enrollment and Disenrollment Information
The
Medical Plan
may disclose enrollment and disenrollment information and information on whether individuals are participating
in the
Medical Plan
to the university, provided such enrollment and disenrollment is only used by the university for the purpose of
performing its administrative functions. Enrollment information held by the university in its capacity as an employer is not PHI.
Security of PHI
The university will implement administrative, physical and technical safeguards that reasonably and appropriately protect the
condentiality, integrity and availability of the electronic PHI that it creates, receives, maintains, or transmits on behalf of the
Medical Plan
.
Adequate Separation Between Plan and Plan Sponsor
• Those employees or other persons under the control of the university involved in performing plan administration functions for, or
on behalf of, the Medical Plan may be given access to and use PHI. Without limiting the generality of the foregoing, such persons
include, without limitation:
- Ohio State University Wexner Medical Center: employees in Payroll who perform administrative functions for the Medical Plan.
- OHR Benets Services: all employees in Benets Services who perform administrative functions for the
Medical Plan
and
employees who review and/or make determinations regarding claims or complaints.
- Payroll Services: employees in Payroll Services who perform administrative functions for the
Medical Plan
.
- Ofce of the Chief Information Ofcer (OCIO): employees who perform administrative functions for the
Medical Plan
.
- Ofce of Legal Affairs: employees who perform administrative functions for the
Medical Plan
.
- Others: any other employee of the university performing plan administration functions for the
Medical Plan
who is designated in
writing by the Privacy Ofcial of the plans as being entitled to access to PHI.
• The employees or other persons described above shall have access to PHI only to the minimum extent necessary to perform plan
administrative functions, unless an individual authorization exists. In the event that any such employees do not comply with these
provisions, the employee shall be subject to disciplinary action by the university for non-compliance pursuant to the discipline
procedures established by the university.
• The separation provided for above will be supported by reasonable and appropriate security measures.
GENERAL PLAN PROVISIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 15 of 92
Revised 09/2023
TERMINATION OF COVERAGE
• Coverage will terminate for the following Covered Person(s) when the following events occur:
- For the covered employee and his or her dependents, when the employee terminates from the university. Coverage will cease on
the employee’s termination date as reected in the university’s human resource system (Workday). Contributions will be prorated
based on the event date and the exact days of coverage prior to termination.
- For the covered employee and his or her dependents, on the last day of the employee’s stability period if the employee is
considered a full-time employee during that stability period, provided that the employee is not eligible for coverage in the next
applicable stability period. Refer to the “Eligibility” section of this SPD.
- For the covered employee and his or her dependents, when the employee transfers to an ineligible appointment, as reected in
the university’s human resource system (Workday), during a stability period if the employee is not considered a full-time employee
during that stability period. Coverage will cease on the date in which the employment status change occurs.
- For the covered employee and his or her dependents, if the employee fails to pay the employee contributions in full. Elected
benets will be terminated for lack of payment. Contributions will be prorated based on the event date and the exact days of
coverage prior to termination.
- For the spouse of the covered employee, upon decree of divorce, dissolution, or legal separation. Coverage will cease on the event
date. If timely notice is provided, premiums will be prorated based on the event date and the exact days of coverage based on the
event date.
- For a dependent child reaching age 26 (other than an eligible disabled child), at the end of the month in which the child reaches
age 26.
- For any other dependent, when the dependent no longer qualies as a dependent. Coverage will cease on the event date. If timely
notice is provided, premiums will be prorated based on the event date and the exact days of coverage based on the event date.
- The Covered Employee is responsible for notifying the university within 30 days of the date of any status change involving the
eligibility of a covered dependent. The university may recover from the employee all damages sustained from losses (including
paid claims and premium costs) and reasonable attorneys’ fees incurred to recover such damages that are brought about as a
result of the employee’s failure to notify the university of status changes which affect dependent eligibility.
• Coverage may be rescinded (i.e., retroactively terminated) if such coverage was gained due to an individual (or person seeking
coverage on behalf of the individual) performing an act, practice or making an omission that constitutes fraud or intentional
misrepresentation of a material fact.
• Coverage may be terminated during an open enrollment period. Coverage will cease on the last day of the Plan Year in which
enrolled.
• Coverage may be terminated due to a qualifying status change. Refer to the “Change in Coverage Due to a Qualifying Status
Change” section of this SPD. Coverage will cease on the date of the qualifying status change if the Health Election Form, available
at hr.osu.edu/policies-forms (under Forms - Health Benets – Medical), is submitted within 30 days of the qualifying status change.
Enrollment changes can also be made by using Workday online at workday.osu.edu within 30 days of the qualifying status change.
Documentation of the status change may be required.
• Upon termination of coverage, individuals may be eligible for coverage continuation as described in the “Coverage Continuation”
section of this SPD. However, if the university is not notied within 60 days of the last day of eligibility and/or coverage the
dependent will not be eligible for coverage continuation as detailed.
• The university will determine when a Covered Person is no longer eligible under the Medical Plan. It is the responsibility of the
university to make determinations as to when coverage will end for a Covered Person and to communicate all terminations of
coverage to Trustmark and Express Scripts.
• Coverage under the Medical Plan will terminate for all Covered Persons on the date on which the Medical Plan terminates or is not
renewed by the university. The university reserves the right to terminate the Medical Plan, in whole or in part, at any time.
Certication of Group Health Plan Coverage
• When your coverage terminates, Trustmark can send a Certicate of Group Health Plan Coverage to you upon request. This
certicate informs you of the length of group health plan coverage and may be required by another employer or health insurance
company prior to providing your health insurance benets. If you would like to request a Certication of Group Health Plan Coverage,
contact Trustmark by calling 800-678-6269.
TERMINATION OF COVERAGE
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 16 of 92
Revised 09/2023
The medical care services that may be covered under the Medical Plan are listed below. For these services and supplies to be
considered covered services, they must be authorized by a physician, rendered and billed by a provider (as dened in the
“Denitions” section of this SPD) and Medically Necessary (as dened in the “Denitions” section of this SPD), except as specied
in this document. (See the description of your specic coverage option for coverage levels and applicable network provider
requirements.)
ACUPUNCTURE
• Acupuncture is used to alleviate pain and to treat certain physical conditions. Acupuncture services and chiropractic care are limited
to a combined maximum benet of $2,000 per Plan Year.
AMBULANCE
• Ambulance service is transportation by a vehicle designed, equipped and used only to transport the sick and injured, when Medically
Necessary :
- From your home, scene of accident or medical emergency to a hospital.
- Between hospitals.
- Between hospital and an extended care facility.
- From a hospital or an extended care facility to your home
1
.
- From your home to an extended care facility, or provider ofce
1
.
• Surface trips must be to the closest local facility that can give covered services appropriate for your condition. If none are available,
you are covered for trips to the closest such facility outside your local area.
• Air transportation is covered when such transportation is Medically Necessary because of a life-threatening injury or sickness and
availability of specialty care. Air ambulance is air transportation by a vehicle designed, equipped and used only to transport the sick
and injured to and from a hospital for inpatient care. Air ambulance services (and ground ambulance services in Ohio) from out-of-
network providers are not subject to balance billing. See Emergency Services Received From Out-of-Network Provider in the How
Payment is Determined section of this document.
BEHAVIORAL (MENTAL) HEALTH SERVICES
All inpatient behavioral (mental) health services require Prior Authorization
1
, unless admitted directly from the emergency room
(notication to OSU Health Plan of hospital admission is then required within one business day) and include the assessment and
treatment of mental and/or psychological disorders and substance abuse.
• Behavioral (mental) health services for the care and treatment of mental illness are covered on an inpatient or outpatient basis.
Substance abuse services for the care and treatment of alcoholism and drug addiction are also covered on an inpatient or outpatient
basis.
• The following services are covered on an inpatient or outpatient basis:
- Individual psychotherapy
- Group psychotherapy
- Psychological testing
- Intensive outpatient behavioral health
- Family counseling – Counseling with family members to assist in your diagnosis and treatment, including marriage counseling
- Convulsive therapy includes electroshock treatment or convulsive drug therapy
• A physician, mental health provider, hospital, specialized hospital, alcoholism treatment facility, or community mental health facility
may provide behavioral (mental) health and substance abuse services.
CHIROPRACTIC CARE
• Chiropractic care is dedicated to the detection and correction of spinal displacement to eliminate interference that can adversely
affect health.
• Chiropractic care and acupuncture services are limited to a combined maximum benet of $2,000 per Plan Year.
CLINICAL TRIALS
The Plan will cover routine patient costs incurred by a qualifying individual who is participating in an approved clinical trial as required
by the Affordable Care Act. For details, see the Experimental and Investigational Services Policy available at osuhealthplan.com (under
Health Plan Tools – Forms and Policies).
CONVENIENT CARE CLINIC
A Convenient Care Clinic is a walk-in health care clinic located in a retail store, supermarket or pharmacy that treats uncomplicated
minor illnesses, injuries or conditions not serious enough for urgent or emergent care. These facilities are staffed with nurse
practitioners and physician assistants who collaborate with physicians to treat minor illnesses and perform some preventive care
services.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 17
COVERED SERVICES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 17 of 92
Revised 09/2023
DENTAL SERVICES
• Expenses for dental work are covered if they are for the prompt repair of an injury to the jaw, sound natural teeth, mouth, or face,
which are required as a result of an accident.
• Dental services are limited to the treatment of the injury that is rendered within 12 months of the injury, or within 12 months of
enrollment in the plan, whichever is later. Injury as a result of chewing or biting is not considered an accidental injury.
• Dental services resulting from an accidental injury are limited to a maximum benet of $3,000 per injury. Prior Authorization
1
is
required.
EMERGENCY CARE
• Emergency care is the service or treatment provided in the outpatient emergency department of a hospital or other facility within
72 hours of the onset of the emergency medical condition. An “emergency medical condition” is dened as a medical condition
that manifests itself by such acute symptoms of sufcient severity, including severe pain, that a prudent layperson with average
knowledge of health and medicine could reasonably expect the absence of immediate medical attention to result in any of the
following:
- Placing the health of an individual, or with respect to a pregnant woman, the health of the woman or her unborn child in serious
jeopardy;
- Serious impairment of bodily functions; or
- Serious dysfunction of a body organ or part.
• If a Covered Person is admitted to a hospital for an emergency care admission, notice of the admission must be provided to OSU
Health Plan as soon as possible after the admission, generally within one business day. The hospital, admitting physician, Covered
Person, or friend/family member of the Covered Person may give notice to OSU Health Plan.
• Emergency care, air ambulance services (and ground ambulance services in Ohio) from out-of-network providers are not subject to
balance billing. See Emergency Services Received From Out-of-Network Provider in the How Payment Is Determined section of this
document.
EXTENDED CARE FACILITY SERVICES
• Covered Services in an extended care facility are the same as those shown in the “Covered Services – Hospitalization Services”
and “Medical Services, Inpatient” sections of this SPD. Refer to your coverage option’s Schedule of Benets, Extended Care Facility
Services, for coverage details.
• Extended care facility services are covered for up to 60 days per Plan Year.
• Prior Authorization
1
is required before receipt of these services.
• Services must be Medically Necessary as a continuation of treatment for the condition for which you were hospitalized.
GENETIC COUNSELING/BRCA
The U.S. Preventive Services Task Force (USPSTF) recommends with a “B” rating to “screen women who have family members
with breast, ovarian, tubal or peritoneal cancer with one of several screening tools designed to identify a family history that may be
associated with an increased risk for potentially harmful mutations in breast cancer susceptibility genes (BRCA 1 or BRCA 2). Women
with positive screening results should receive genetic counseling and, if indicated after counseling, BRCA testing.” There is no cost
to the member for these services when performed by a network provider with Prior Authorization.
1
BRCA testing when Medically
Necessary is covered once per lifetime.
GYNECOLOGICAL (GYN) EXAMINATIONS
Coverage is provided according to each specic coverage option’s Schedule of Benets.
HEALTH AND CANCER RIGHTS ACT OF 1998 (WHCRA) NOTICE
If you have had or are going to have a mastectomy, you may be entitled to certain benets under WHCRA. For individuals receiving
mastectomy-related benets, coverage will be provided in a manner determined in consultation with the attending physician and the
patient, for:
• All stages of reconstruction of the breast on which the mastectomy was performed;
• Surgery and reconstruction of the other breast to produce a symmetrical appearance;
• Prostheses; and
• Treatment of physical complications of the mastectomy, including lymphedema.
These benets will be provided subject to the same deductibles and coinsurance applicable to other benets provided under your
Medical Plan.
If you would like more information on WHCRA benets, contact OSU Health Plan at 614-292-4700.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 18
COVERED SERVICES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 18 of 92
Revised 09/2023
HEALTH/CONTRACEPTIVE COVERAGE
At least one form of women’s contraception in each of the 18 “methods” of contraception outlined in the FDA birth control guide is
covered. For details see the Birth Control Claim Processing Policy available online at osuhealthplan.com under Health Plan Tools
Forms and Policies.
HEARING AIDS AND EAR MOLDS
Coverage is provided for hearing aids and ear molds that are required to improve pure tone hearing ability for causes other than injury
to the ear. The total maximum benet is $1,400 per hearing impaired ear ($2,800 bilateral) every three Plan Years.
• If acute hearing loss is the result of an injury to the ear, then the initial hearing aid and ear mold are covered as part of the prosthetic
appliance benet. See the “Covered Services - Prosthetic Appliances” section of this SPD for further details.
Note: For dependents up to age 12, replacement ear molds that are Medically Necessary due to growth are covered and are not
subject to the maximum benet.
HOME HEALTH CARE SERVICES
• May be provided to you on a part-time basis in your home as a Medically Necessary alternative to inpatient care. A home health care
provider must provide the services according to a physician-prescribed course of treatment that has received Prior Authorization.
1
Covered Services include skilled nursing services, diagnostic services and therapy services.
• Benets are not provided for a nurse who usually lives in the home or is a member of the immediate family.
HOSPICE AND PALLIATIVE CARE
A medical care program providing a coordinated set of services rendered at home, in outpatient settings, or in institutional settings for
Covered Persons suffering from a condition that has a terminal prognosis. A hospice or palliative care must have an interdisciplinary
group of personnel that includes at least one physician and one Registered Nurse (RN), and it must maintain standards of the National
Hospice Organization (NHO) or other appropriate agency and applicable state licensing requirements. Covered Services include, but
are not limited to, room and board, nursing care, respite care, physical/occupational/respiratory therapy and bereavement counseling.
HOSPITALIZATION SERVICES
The following hospitalization services are covered:
• Room and board in a semi-private room containing two or more beds, including meals, special diets and nursing services, other than
private duty nursing services. Coverage includes a bed in a special care unit approved by OSU Health Plan.
• Oral surgery, including the extraction of teeth, if hospitalization is Medically Necessary to safeguard the covered person’s life
or health due to a specic non-dental organic impairment. For these services to be covered, your physician must receive Prior
Authorization.
1
• Ancillary services, such as:
- Operating, delivery and treatment rooms and equipment
- Prescribed drugs
- Anesthesia, anesthesia supplies and services given by an employee of the facility
- Medical and surgical dressings, supplies, casts and splints
- Blood and blood services
- Diagnostic services
- Radiation therapy, intravenous chemotherapy, kidney dialysis, respiratory therapy, physical therapy (as dened below),
occupational therapy (as dened below) and speech therapy (as dened below)
Note: All hospitalizations require Prior Authorization
1
, unless admitted directly from the emergency room (notice of the admission must
be provided to OSU Health Plan as soon as possible following admission, but generally within one business day).
HUMAN ORGAN TRANSPLANTS
• A human organ transplant is, for example, a human heart, heart-lung, liver, kidney, bone marrow, or pancreas transplant. Coverage
will be provided for:
- All Covered Services as applicable to the procedure.
- Expenses related to the acquisition of a human organ. Acquisition includes the preparation, transportation and storage of a
human organ.
• In order to receive benets for human organ transplants, you must contact OSU Health Plan when you learn you are a candidate for
transplant surgery. Prior Authorization
1
will only be granted if the human organ transplant is Medically Necessary.
• No coverage will be provided for services or supplies that are considered by OSU Health Plan to be experimental/investigative (as
dened in the “Denitions” section of this SPD), or that are related to a transplant surgery for which Prior Authorization was not
obtained.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 19
COVERED SERVICES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 19 of 92
Revised 09/2023
IMMUNIZATIONS
Immunizations are a method to trigger your immune system to prevent serious life-threatening diseases. They are an essential part of
wellness programs for all ages.
INFERTILITY TREATMENT
• In order to receive benets for infertility treatment, an obstetrician or gynecologist (OB/GYN) or reproductive endocrinologist must
diagnose the infertility (as dened in the “Denitions” section of this SPD). In addition, coverage is limited to you (the employee) and
your spouse.
• There is a separate lifetime maximum for infertility services. Any prescription medications included in this treatment are applied to
the lifetime maximum.
• All infertility treatments are subject to OSU Health Plan guidelines as outlined in the Schedule of Benets section for your coverage
option. Requires Prior Authorization¹ and specic exclusions apply.
• The Infertility Request Policy is availalbe online at osuhealthplan.com under Health Plan Tools - Forms and Policies.
INJECTION/ADMINISTRATION OF MEDICATIONS
The injection or administration of prescription drugs by a medical professional.
MATERNITY SERVICES
• Coverage for inpatient and outpatient maternity services includes all Covered Services listed under the “Hospitalization Services,”
“Medical Services-Inpatient,” “Medical and Surgical Supplies-Outpatient” and “Outpatient Services” sections of this SPD.
• Statement of Rights Under the Newborns’ and Mothers’ Health Protection Act
- Under federal law, group health plans and health insurance issuers offering group health insurance coverage generally may not
restrict benets for any hospital length of stay in connection with childbirth for the mother or newborn child to less than 48 hours
following a vaginal delivery, or less than 96 hours following a delivery by cesarean section. However, the plan or issuer may pay
for a shorter stay if the attending provider, after consultation with the mother, discharges the mother or newborn earlier.
- Under federal law, plans and issuers may not set the level of benets or out-of-pocket costs so that any later portion of the
48-hour (or 96-hour) stay is treated in a manner less favorable to the mother or newborn than any earlier portion of the stay.
- In addition, a plan or issuer may not, under federal law, require that a physician or other health care provider obtain authorization
for prescribing a length of stay of up to 48 hours (or 96 hours). However, to use certain providers or facilities, or to reduce your
out-of-pocket costs, you may be required to obtain Prior Authorization
1
.
• Only one individual annual deductible must be met for routine maternity services.
MEDICAL AND SURGICAL SUPPLIES – OUTPATIENT
• Syringes, needles, oxygen, surgical dressings, splints and other similar items that serve only a medical purpose are covered. Covered
Services do not include items usually stocked in the home for general use, such as adhesive bandages, thermometers and petroleum
jelly.
• Medical supplies, equipment and appliances must be rented or purchased by an agency or provider approved by OSU Health Plan.
Prior Authorization
1
may be required.
MEDICAL EQUIPMENT
The rental or purchase of medical equipment is covered when prescribed by a physician. Rental costs must not be more than the
purchase price. The equipment must serve only a medical purpose and be able to withstand repeated use. Prior Authorization
1
may be
required.
MEDICAL SERVICES – INPATIENT
The following medical services, when performed by a physician, are covered on an inpatient basis:
• Care and treatment while you are conned in a medical facility.
• One physician visit per day.
• Consultation by another physician when requested by your physician. Staff consultations required by hospital rules are excluded from
coverage.
• Care by two or more physicians during one hospital stay when your condition requires the skills of separate physicians.
• Dental services that are required as a result of injury to the jaws, sound natural teeth, mouth, or face.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 20
COVERED SERVICES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 20 of 92
Revised 09/2023
MEDICATIONS
• Federal legend drugs which are medications that require a prescription under federal law and are approved for general use by the
Federal Drug Administration (FDA).
• Injectable insulin that does not require a prescription is considered to be a Covered Drug.
• Covered over-the-counter medications require a prescription for coverage. See the Prescription Drug Benet section of this SPD for
further details.
NEWBORN CARE
• Coverage for a newborn infant as described in this section is provided only as a covered person under two-person or family
coverage. To have the services covered, you must add the newborn as a covered dependent under your Medical Plan in accordance
with the requirements outlined in the “Change in Coverage Due to a Qualifying Status Change” section of this SPD.
• If single coverage is already in place prior to the birth of the newborn infant, then you must elect employee + child(ren) coverage and
enroll the newborn infant.
• If employee + spouse coverage is already in place prior to the birth of the newborn infant, then you must elect family coverage and
enroll the newborn infant.
• If family or employee + child(ren) coverage is already in place prior to the birth of the newborn infant, you are still required to enroll
the newborn infant.
• Coverage includes:
- Routine nursery care of a newborn infant.
- Inpatient visits to examine a newborn. A physician other than the physician who performed the obstetrical delivery must do the
examination.
Note: To enroll the newborn infant in medical coverage, use Workday online at workday.osu.edu or submit a completed Health Election
Form, available at hr.osu.edu/policies-forms (under Forms - Health Benets – Medical), within 30 days of the date of birth.
NUTRITIONAL SERVICES
Nutritional services are services focused on food/nutrient intake or eating patterns. They can be provided by a licensed and registered
dietician, physician, certied diabetic educator, or within an approved structured program. These services are appropriate when there is
a condition or treatment that is directly inuenced by food and nutrient intake such as diabetes, a malabsorption disorder such as celiac
disease, an eating disorder, or obesity.
OCCUPATIONAL THERAPY
Occupational therapy is the treatment rendered on an inpatient or outpatient basis as a part of a physical medicine and rehabilitation
program to improve functional impairments. It is considered Medically Necessary only if the expectation exists that the therapy will
result in practical improvement in the level of functioning within a reasonable period of time. No benets are provided for diversional,
recreational and vocational therapies (such as hobbies, art and crafts). All outpatient occupational therapy and physical therapy (See
the “Physical Therapy” section of this SPD) services are limited to a combined maximum of 45 visits per Plan Year.
OUTPATIENT SERVICES
The following services are covered on an outpatient basis:
• Blood and blood services, if provided and billed by a hospital or other facility.
• Diagnostic services including laboratory services.
• Home and ofce visits to examine, diagnose, or treat an injury or sickness.
• Outpatient surgical services and supplies; other outpatient visits to examine, diagnose or treat an injury or sickness, including
emergency care and the administration of allergy injections.
• Pre-admission tests and studies required for a scheduled admission as an inpatient.
• Radiation therapy, inhalation therapy, intravenous chemotherapy, kidney dialysis and physical therapy. Occupational, physical and
speech therapy services must be rendered by a licensed therapist.
PERVASIVE DEVELOPMENTAL DISORDER (PDD)
Treatment for the diagnosis of Pervasive Developmental Disorder (PDD) Spectrum including Autism is covered when Medical
Necessity criteria are met. Coverage includes the following:
• Up to 20 hours per week of therapeutic aide services, if criteria are met. Prior Authorization
1
is required.
• Professional services provided by a licensed mental health provider – Refer to each coverage option’s Schedule of Benets for details
on “Behavioral Health Services: Mental Health and Substance Abuse - Outpatient” coverage levels.
• Speech therapy – Refer to each coverage option’s Schedule of Benets for details on “Speech Therapy, Outpatient” coverage levels.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 21
COVERED SERVICES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 21 of 92
Revised 09/2023
• Physical therapy – Refer to each coverage option’s Schedule of Benets for details on “Physical Therapy and Occupational Therapy,
Outpatient” coverage levels.
• Occupational therapy – Refer to each coverage option’s Schedule of Benets for details on “Physical Therapy and Occupational
Therapy, Outpatient” coverage levels.
PHYSICAL THERAPY
• Physical therapy is treatment by physical means including modalities such as whirlpool and diathermy; procedures such as massage,
ultrasound and manipulation; and tests of measurements required to determine the need and progress of treatment. Such treatment
must be given to relieve pain, restore maximum function and to prevent disability following disease, injury, or loss of body part.
Treatment must be for acute conditions where rehabilitation potential exists and the skills of a physician or other professional are
required.
• All outpatient physical therapy and occupational therapy therapy (see the “Occupational Therapy” section of this SPD) services are
limited to a combined maximum of 45 visits per Plan Year.
PREVENTIVE HEALTH CARE (PHYSICAL EXAMINATIONS)
Coverage is provided according to each coverage option’s Schedule of Benets and based on the guidelines in the Preventive Health
Care Guidelines; guidelines (available online at osuhealthplan.com under Health Plan Tools - Forms and Policies).
Note: One physical examination per Plan Year provided for children (age 3 and older) and adults.
PROCEDURES – OUTPATIENT SERVICES
• Performed for primarily diagnostic purposes
• Non-invasive or minimally invasive
• Do not require an operating room environment (e.g., sterile OR setting, or room with specic monitoring or resuscitation equipment)
• Do not require full or prolonged sedation of the patient
• Require no or little post-recovery time for the patient
PROSTHETIC APPLIANCES
Purchase, tting, needed adjustment, repairs and replacements of prosthetic devices and supplies that:
• Replace all or part of a missing body organ and its adjoining tissues.
• Replace all or part of the function of a permanently useless or malfunctioning body organ.
Note: Prior Authorization
1
may be required.
RADIOLOGY
Radiology is the examination of the inner structure and parts of the body using X-rays or other penetrating radiation.
SPEECH THERAPY
• Speech therapy is the active treatment for improvement of an organic medical or developmental condition causing speech
impairment. Treatment must be post-operative or for the convalescent stage of an active illness or disease. The expectation must
exist that the therapy will result in a practical improvement in the level of functioning within a reasonable and predictable period of
time.
• All outpatient speech therapy services are limited to a maximum benet of 20 visits per Plan Year.
SURGICAL SERVICES
• Surgery performed by a physician is covered on an inpatient or outpatient basis. Prior Authorization
1
is required before receipt
of inpatient and certain outpatient surgical services. Refer to the Medical Prior Authorization Guide available online at
osuhealthplan.com under (Health Plan Tools - Forms and Policies) to determine the need for Prior Authorization
1
.
• If two or more surgeries were performed during the same operative session, the following guidelines are normally used to determine
the allowable expense for the claim:
- 100% of the Allowed Amount paid for the rst or primary procedure
- 50% of the Allowed Amount paid for the second and each additional procedure
Note: If you use a surgeon in either the Premier Network or Standard Network, you are not responsible for any balance in excess of
the surgeon’s fee schedule outside of normal deductible and co-insurance limits.
• Reconstructive surgery to restore bodily function. Coverage is limited to medical conditions caused by disease, injury, or birth
defects. Reconstructive surgery does not include any surgery that is specically identied as an exclusion or to correct cosmetic
surgery. Refer to the Medical Prior Authorization Guide available online at osuhealthplan.com under (Health Plan Tools - Forms and
Policies) to determine the need for Prior Authorization
1
.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 22
COVERED SERVICES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 22 of 92
Revised 09/2023
• Second surgical opinion to help determine the need for elective surgery recommended by another physician. Coverage is provided
for the physician’s opinion and related diagnostic services. If the rst and second opinions differ, you may elect to receive a third
surgical opinion, subject to the same provisions as for the second surgical opinion.
• Services of a physician who helps your surgeon in performing covered major surgery when a house staff member, intern, or resident
cannot be present and is Medically Necessary.
TELEHEALTH SERVICES
Telehealth/Electronic consultation services are services in which the healthcare professional and the patient are not at the same site.
Examples include: services delivered by interactive audio/visual devices or other interactive communication platforms. All services are
subject to OSU Health Plan guidelines available here or by calling OSU Health Plan at 800-678-6269.
TEMPOROMANDIBULAR DISORDER (TMD)
TMD is a disease of dysfunction of the joint linking the jawbone and skull and the muscles, nerves and other tissues related to the joint.
TMD Covered Services include diagnostic services, orthotic or orthopedic devices, adjustments to orthotic or orthopedic devices and
therapeutic injection of medication into the TMD. There is a $3,000 maximum lifetime benet for non-surgical procedures. Surgical
procedures for the treatment of TMD are subject to the “Surgical Services” section of this SPD and your coverage option’s Schedule
of Benets.
• No coverage is provided for crowns or for orthodontia (braces) – these services may be covered under your dental care plan.
• Prior Authorization
1
may be required.
TOBACCO CESSATION PROGRAM
Tobacco cessation services are covered through the Medical Plan. Services are paid at 100%. Over-the-counter nicotine replacement
therapy (NRT) and prescription cessation medications (e.g., Chantix) are paid at 100% through the Prescription Drug Benet. See
the Prescription Drug Benet section. A prescription must be obtained from a physician or nurse practitioner for all tobacco cessation
products. Free cessation services can be obtained through Health Coaching at OSU Health Plan by calling 614-292-4700.
URGENT CARE
• Urgent care services are different than emergency medical services. An urgent condition is not life threatening, but may cause
serious medical problems if not promptly treated. Urgent care is dened by the need to treat an unforeseen condition that requires
immediate medical treatment for acute pain, acute infection, or protection of public health.
• Plan members should go to the emergency room for life-threatening medical emergencies.
• Urgent care is not intended for preventive or routine maintenance treatment such as school or annual physicals. These services will
not be covered at urgent care facilities.
• Examples of conditions that require urgent care include: injuries, fever, sudden onset of pain (abdominal pain, severe headache),
broken bones and cuts.
WEIGHT LOSS SURGERY
• Weight loss surgeries include but are not limited to gastric bypass, gastric banding, and gastric reduction. All services are subject to
OSU Health Plan guidelines available at osuhealthplan.com under Health Plan Tools - Forms and Policies (see Weight Loss Surgery
Policy). Prior Authorization
1
is required.
WEIGHT MANAGEMENT PROGRAMS
• Hospital-based/physician-directed programs are reimbursed at 50% coinsurance. The Trustmark Hospital Based/Physician Directed
Weight Loss Claim Form is available at hr.osu.edu/policies-forms under Forms-Health Benets-Medical.
• WW (formerly Weight Watchers™) Core and Premium Programs are reimbursed at 50% coinsurance. The reimbursement is applied
to the month-to-month membership. Membership can be canceled at any time. For more information, or to join, visit
go.osu.edu/weightwatchers.
• Expenses for Weight Management Programs are excluded from the annual out-of-pocket maximum.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
COVERED SERVICES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 23 of 92
Revised 09/2023
BENEFITS ARE NOT PROVIDED FOR SERVICES, SUPPLIES, OR CHARGES:
1. Which are not specied as Covered Services.
2. Which are experimental/investigative (as dened in the “Denitions” section of this SPD), including investigational medical,
surgical, or mental health procedures and pharmacological regimens, as well as associated health services and/or supplies as
dened by the Medical Plan.
3. Which are not Medically Necessary to the care and treatment of any injury, disease, or pregnancy or furnished without
recommendation and approval of a physician acting within the scope of his or her license except for preventive services listed.
4. Which are for injury or sickness (each as dened in the “Denitions” section of this SPD) arising in the course of employment. This
applies whether or not you claim any compensation or recover losses from a third party.
5. For which governmental units provide benets.
6. For injury or sickness (each as dened in the “Denitions” section of this SPD) that occurs as a result of any act of war, declared
or undeclared, when providing service in the armed forces of any country to the extent that such injury or sickness is provided for
through any governmental plan or program.
7. Subject to Section 3923.82 of the Ohio Revised Code, incurred as a result of a covered person’s voluntary involvement or
participation in a felony or an illegal activity, including a riot or act of civil disobedience.
8. For which you have no legal obligation to pay in the absence of this or like coverage.
9. For treatment only to improve appearance.
10. For complications and reconstructive surgery following cosmetic surgery.
11. Received from a member of your immediate family or self-administered/self-prescribed by you for your own benet. Immediate
family is dened as spouse, child, stepchild, parent, sibling, in-laws, or grandparents.
12. For personal hygiene and convenience items, including any item or service requested solely due to member preference.
13. For missed appointments, completion of claim forms, copying or obtaining medical records.
14. For services for custodial care or for services not needed to diagnose or treat an injury or sickness.
15. For reversal of sterilization.
16. For non-therapeutic abortions performed or induced when the life of the mother would not be endangered if the fetus were
carried to term or when pregnancy of the mother was not the result of rape or incest reported to a law enforcement agency (even
if pre-natal testing is covered), including but not limited to pre-and post-procedure diagnostic testing, imaging or surgeries due to
complications subject to Section 9.04 of the Ohio Revised Code.
17. For room, board and general nursing care for hospital admissions mainly for physical therapy or diagnostic studies.
18. For hospitalization for environmental change.
19. For services or supplies incurred prior to your effective date of coverage or after your termination date of coverage except as
otherwise specied in this SPD.
20. For eye examinations for the purpose of prescribing or tting of eye glasses or contact lenses, or for eye examinations for any
occupational condition, ailment or injury arising out of or in the course of employment.
21. For services to correct visual acuity, such as radial keratotomy and corrective refractive surgery.
22. For eye glasses, sunglasses, safety glasses, safety goggles, subnormal vision aids or contact lenses (except for aphakic patients
and soft lenses or sclera shells which are intended for use as corneal bandages or when needed because of an injury to the eye).
23. For services or supplies primarily for educational, vocational or training purposes.
24. For dentistry or dental processes to the teeth, the tissue surrounding the teeth and roots, including orthodontia, except as
otherwise specied in this SPD.
25. For routine dental services, the surgical removal of impacted teeth or residual tooth roots, and endodontal and periodontal surgery.
26. For tooth transplantation including re-implantation from one site to another and splinting and/or stabilization.
27. For transportation or travel other than for use of ambulance services.
28. For medical equipment or appliances for comfort, appearance, weight loss, safety or those for which an acceptable substitute may
be made, even though prescribed by a physician; including but not limited to air conditioners, humidiers, dehumidiers, exercise
equipment, car seats, and strollers.
29. For Replacement or upgrade of medical equipment, including prosthetic devices, that are not out-of-warranty and malfunctioning
or when malfunction is due to misuse, abuse or negligence, regardless of item warranty status. This includes lost or stolen items
and duplicate equipment and supplies.
30. For any service or supply for which the Medical Plan cannot by law provide such benet.
31. For any service or supply for which a charge would not have been made in the absence of eligibility.
32. For any service or supply once the maximum benets have been provided as outlined in the Schedule of Benets for your
coverage option.
33. For charges for herbal medicines, holistic or homeopathic care, including prescribed drugs.
34. For services rendered by a provider who is not specically included in the denition of a physician or specically listed as a
covered provider.
35. For charges in excess of those considered reasonable and customary.
36. For claims led later than 12 months from the date the charge was incurred.
37. For services, supplies or charges for oral or self-injectable medications that are capable of being given outpatient using the
Prescription Drug Benet.
38. For supplements (<50% intake), food, and commercially available milk/soy nutritional powder/liquids, including infant or adult
formula, even if prescribed by a physician.
39. For cord blood donation or storage.
CONTINUED ON PAGE 24
EXCLUSIONS OR LIMITATIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 24 of 92
Revised 09/2023
BENEFITS ARE NOT PROVIDED FOR SERVICES, SUPPLIES, OR CHARGES CONT’D:
40. For chelation therapy unless for the treatment of heavy metal or lead poisoning or blood cleaning therapy.
41. For hospital charges for observation which exceed 48 hours.
42. For routine vitamin injections.
43. For any test solely for the purpose of determining the sex of the fetus.
44. For environmental modications, including but not limited to: air conditioner, air lters, humidiers, vaporizers, heating pads,
wheelchair lifts, ramps, home remodeling.
45. For long-term (greater than 12 months) embryo, sperm, or egg storage.
46. For physicals and other medical services (e.g., vaccines, x-rays, labs, etc.) for administrative requirements such as: immigration,
licensure, adoption, marriage, employment, camp, sports, or school.
47. For outpatient recreational therapy.
48. For living expenses even if related to a medical condition, including independent, assisted, and sober living facilities.
49. For hypnotherapy, music therapy, or remedial reading therapy.
50. For custodial/maintenance care or for services not needed to diagnose or treat an injury or illness.
51. For ambulance services for the convenience of the patient.
52. For educational lectures and counseling.
53. For exercise equipment including but not limited to: bicycles, weights, treadmills, ergometers and gym memberships.
54. For evaluations or treatment mandated by a third party unless considered Medically Necessary (for example, court, employer, or
school), including documentation in the form of reports or summaries of clinical information.
55. For cosmetic services which include but are not limited to: breast enlargement, vaginal rejuvenation procedures including
labiaplasty, wrinkle removal, collagen injections, dermabrasion, hair restoration, electrolysis, hair removal/reduction,
abdominoplasty, liposuction (except when performed as part of Medically Necessary breast cancer reconstruction), excision of
excessive skin of thigh (thigh lift, thighplasty), leg, hip, buttock, arm (arm lift, brachioplasty), forearm or hand, submental fat pad, or
other areas.
56. For services and supplies provided through research studies.
57. For charges for time dedicated to claims resolution.
58. For charges for legal expenses or fees incurred in obtaining medical treatment.
59. For covered charges when there has been an incomplete claims submission.
60. For private duty nursing, homemaking or housekeeping services.
61. For free-standing birthing centers.
62. For home births.
63. For paternity testing.
64. For in-vitro fertilization, articial insemination, assisted reproductive technologies and procedures, and fertility preservation when
either partner has undergone voluntary elective sterilization procedures, or for individuals who are not considered infertile (as
dened in the “Denitions” section of this SPD), or for a Covered Person other than the employee, or spouse. Donor services,
including egg, sperm and embryo.
65. For selective reduction of a pregnancy and any related services, including but not limited to pre- and post-procedure diagnostic
testing, imaging, or surgeries due to complications.
66. For charges for services and supplies which do not conform with generally accepted medical practices,
67. For charges that are not payable by the primary plan covering the patient solely due to the employee/patient’s failure to comply
with that plan’s requirements for cost containment (including but not limited to failure to obtain Prior Authorization, failure to obtain
a second opinion, failure to execute subrogation agreements, etc.).
68. For charges that may be payable by the Medical Plan when a provider or plan participant fails to comply with the Medical Plan’s
request for information.
69. For expenses relating to a medical condition, sickness, or injury, when the covered person receives a prot or wage (other than
employer-based disability payments).
70. For the return of mortal remains in the event of a death away from home.
71. For preventive or routine maintenance treatment such as school or annual physicals received by an urgent care provider or
convenient care clinic.
72. Charges for shipping, handling and tax.
73. Prescriptions for medical marijuana.
74. For services rendered to or for a surrogate or gestational carrier, including, but not limited to, costs for maternity care, if the
surrogate is not a Covered Person.
75. For costs incurred for a fertile woman to achieve a pregnancy as a surrogate or gestational carrier and related costs for the infertile
person, regardless of whether they are a Covered Person. Costs include, but are not limited to, costs for drugs necessary to achieve
implantation, egg retrieval and embryo transfer.
76. For non-emergency use of an emergency room.
77. For services related to treatment of snoring.
78. For services related to athletic performance or enhancement.
79. For services provided by an athletic trainer.
80. For repeat genetic testing for hereditary conditions, including single-site testing or genetic panels.
81. For wigs for androgenetic alopecia (Male/female pattern hair loss).
82. For wheelchairs and other mobility equipment solely for use in the community.
EXCLUSIONS OR LIMITATIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 25 of 92
Revised 09/2023
OSU Health Plan works in partnership with OHR, Trustmark, and Express Scripts to assure access to quality medical and
pharmaceutical care in the most cost-efcient manner.
BEHAVIORAL HEALTH REFERRALS
If mental health or substance abuse treatment is needed, OSU Health Plan can assist in matching patient needs to provider expertise.
OSU Health Plan will take into consideration your cultural, demographic, gender and/or geographic issues when making referrals to
appropriate behavioral health services.
CASE MANAGEMENT
OSU Health Plan provides case management services that promote quality cost-effective medical outcomes. To accomplish this, input
is obtained from sources including providers, patients, family members and medical consultants.
COORDINATION OF MEDICAL COVERAGE WITH SPECIALIST REFERRALS FOR DENTAL AND
VISION SERVICES
When your dental or vision care provider identies necessary specialist care, OSU Health Plan will assist you in locating a specialist
who is part of your university medical, dental, or vision network of providers.
MEDICAL PROVIDER NETWORKS
OSU Health Plan establishes the statewide network in Ohio. This network process includes credentialing of physicians and periodic
quality reviews. OSU Health Plan provides information to members regarding physicians, behavioral health services, other medical
services and case management. A listing of the network providers is available online at osuhealthplan.com/nd-a-provider-search.
PRIOR AUTHORIZATION OF SERVICES
OSU Health Plan determines the Medical Necessity of services and conducts treatment plan reviews for the Medical Plan. Network
providers will obtain Prior Authorization of services for you when necessary. When you use an out-of-network provider, it is your
responsibility to inform the provider when Prior Authorization
1
is required. See Medical Prior Authorization Guide available online at
osuhealthplan.com under Health Plan Tools - Forms and Policies.
THE OHIO STATE UNIVERSITY HEALTH PLAN, INC. (OSU HEALTH PLAN)
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 26 of 92
Revised 09/2023
Payment of the network provider’s fee schedule, provider’s reasonable charge, the Allowed Amount or the actual charge,
whichever is less, will be provided for all Covered Services. All payments will be subject to any applicable annual deductible,
coinsurance, copays, maximum benets and other provisions and limitations and the Schedule of Benets for your coverage option.
ALLOWED AMOUNT
The amount paid for a medical service in a geographic area based on what providers in the area usually accept for the same or similar
medical service. The allowed amount sometimes is used to determine the eligible expenses.
• For out-of-network providers, the Allowed Amount is a fee most frequently accepted for a similar service or medical procedure by
most similarly qualied physicians or other medical care providers in the particular geographic area where the service is rendered or
a fee that has been negotiated with the provider.
• When a charge is submitted to Trustmark on behalf of the university for reimbursement of a Covered Service, payment will be made
for the charge or the Allowed Amount, whichever is less, subject to any applicable coinsurance amounts and other provisions or
limitations of the Medical Plan.
• Unusual circumstances which reasonably require additional time, skill or experience for a provider’s service are taken into
consideration and may result in reimbursement of an amount above the Allowed Amount but not exceeding the actual charge.
Note: Charges that exceed the Allowed Amount may be your responsibility, and do not apply to the annual deductible or annual out-of-
pocket maximum unless stated otherwise in this document. See Emergency Services Received From An Out-of-Network Provider and
Out-of-Network Provider Services Received at a Network Hospital or Ambulatory Surgical Center in the How Payment is Determined
section of this document for exceptions.
ANNUAL DEDUCTIBLE
• The annual deductible is the amount you owe for covered services before the Medical Plan begins to pay. For example, if your annual
deductible is $600, the Medical Plan won’t pay anything until you have met your $600 annual deductible for Covered Services
subject to the annual deductible. The annual deductible may not apply to all services.
• Your annual deductible amount is shown in the Schedule of Benets for your coverage option. Trustmark’s records must show that
you have reached this annual deductible. Therefore, to ensure proper record keeping, you should submit copies of all your bills, even
those that you must pay to meet the annual deductible.
• If the family annual deductible amount is reached then the annual deductible will be waived for all others covered under family
coverage for that Plan Year.
Prescription Drug Benet Annual Deductible
The annual deductible for prescription drug purchases for the Prime Care Advantage, Prime Care Choice and the Out-of-Area coverage
options is $50 per person, $100 per family per Plan Year. These are separate from the Medical Plan’s annual deductible. There is no
separate annual deductible for prescription drug purchases under the Prime Care Connect coverage option.
ANNUAL OUT-OF-POCKET MAXIMUM
The annual out-of-pocket maximum is the most you pay during a Plan Year before the Medical Plan begins to pay 100% of the eligible
expenses for the remainder of the Plan Year with the exception of the excluded services listed below.
• An individual annual out-of-pocket maximum is the maximum amount that each covered person is required to pay in annual out-of-
pocket expense in a Plan Year (includes annual deductibles, copays and coinsurances) with the exception of the excluded services
listed below.
• A family annual out-of-pocket maximum is the maximum amount the family is required to pay in annual out-of-pocket expense
in a Plan Year. If the family limit is satised, the annual out-of-pocket maximum will be waived for all others covered under family
coverage for that Plan Year (See exceptions below.).
• The following services are excluded from the annual out-of-pocket maximum:
- Services and supplies that do not constitute Covered Services
- Any charge in excess of the network provider’s fee schedule, the Allowed Amount or provider’s reasonable charge
- Weight Management Programs
- Penalty for failure to obtain Prior Authorization
• You may submit claims for Covered Services that are not in the same order that you received the Covered Services. Regardless of the
order claims were incurred, the annual out-of-pocket amounts will be applied to Covered Services in the sequence that claims are
submitted and paid.
Note: If you have Out-of-Area coverage and your claim is subject to Balance Billing, the amount that is balance billed will be applied to
your Annual Out-of-Pocket Maximum.
Prescription Drug Benet Annual Out-of-Pocket Maximum
The annual out-of-pocket maximum for prescription drug purchases for the Prime Care Advantage, Prime Care Choice and the Out-of-
Area coverage options is $2,500 per person, $5,000 per family per Plan Year. The annual out-of-pocket maximum for prescription drug
purchases for the Prime Care Connect coverage option is $2,000 per person, $4,000 per family per Plan Year. These are separate from
the Medical Plan’s annual out-of-pocket maximum.
CONTINUED ON PAGE 27
HOW PAYMENT IS DETERMINED
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 27 of 92
Revised 09/2023
COINSURANCE
Your share of the costs of a Covered Service, calculated as a percent (for example, 20%) of the eligible expense for the service. You
may have to pay coinsurance in addition to any annual deductibles you owe, although some Covered Services may not be subject to an
annual deductible. Refer to the Schedule of Benets for your coverage option to see what your coinsurance is for each service.
COMMON ACCIDENT
If two or more family members are hurt in the same accident, only one individual annual deductible must be met for expenses relating
to the accident. This special feature applies to eligible expenses each Plan Year for the same accident.
COPAY / COPAYMENT
A xed amount (for example, $35) you pay for a Covered Service, usually when you receive the service. The amount can vary by the
type of Covered Service. Refer to the Schedule of Benets for your coverage option to see what your copay/copayment is for each
service.
EMERGENCY SERVICES RECEIVED FROM AN OUT-OF-NETWORK PROVIDER
If you have an emergency medical condition and get emergency services from an out-of-network provider or facility, the most the
provider or facility may bill you is your plan’s network cost-sharing amount (such as copayments and coinsurance). You can’t be
balance billed for these emergency services. This includes air ambulance services, ground ambulance services in Ohio, and services
you may get after you’re in stable condition, unless you give written consent and give up your protections not to be balanced billed for
these post-stabilization services.
The plan will pay no less than an amount agreed to by the plan and the provider. If no agreement is reached, the plan will pay the
amount determined by binding arbitration as required by the No Surprises Act. For more information about the No Surprises Act see
the “Your Rights and Protections Against Surprise Medical Bills” notice at hr.osu.edu/notices.
Note: You cannot be balance billed for the difference between the provider’s cost and the plan’s payment.
MAXIMUM BENEFIT LIMITS
• Maximum benet limits are the maximum amount that will be paid for a Covered Service. Refer to the Schedule of Benets for your
coverage option for maximum benet amounts.
• If a Covered Employee elects to change to another coverage option available under the Medical Plan (for example, following a
qualifying status change), any amounts incurred toward a benet limit by a Covered Person under the rst coverage option will apply
under the new coverage option.
Maximum Lifetime Benet Limit
There is no maximum lifetime benet limit for the Medical Plan, unless otherwise indicated for a specic benet.
Infertility Lifetime Benet Limit
The lifetime benet limit for expenses related to the treatment of infertility (as dened in the “Denitions” section of this SPD) and
related prescription drugs is $15,000.
Temporomandibular Disorder (TMD) Lifetime Benet Limit
The benet for the treatment (except surgical procedures) of TMD has a $3,000 maximum lifetime benet limit.
OUT-OF-NETWORK PROVIDER SERVICES RECEIVED AT A NETWORK HOSPITAL OR
AMBULATORY SURGICAL CENTER
When you get services from a network hospital or ambulatory surgical center, certain providers there may be out-of-network. In these
cases, the most those providers may bill you is your medical benet network cost-sharing amount. This applies to emergency medicine,
anesthesia, pathology, radiology, laboratory, neonatology, assistant surgeon, hospitalist, or intensivist services. These providers can’t
balance bill you and may not ask you to give up your protections not to be balance billed. If you get other services at these network
facilities, out-of-network providers can’t balance bill you, unless you give written consent and give up your protections.
PRIOR AUTHORIZATION
Prior Authorization (see the Medical Prior Authorization Guide available at osuhealthplan.com under Health Plan Tools - Forms and
Policies) is notication to OSU Health Plan of a request for benets before receipt of specic services, as outlined in the Schedule of
Benets for your coverage option, or before elective admission to a hospital or facility. Emergency admissions must be authorized as
soon as possible following admission, but generally within one business day. If Prior Authorization is not obtained from OSU Health
Plan, a penalty of 20% of the fee, up to $1,000, per admission or service will be charged. This penalty does not apply toward the
annual deductible or the annual out-of-pocket maximum.
PRE-EXISTING CONDITION LIMITATION
There is no pre-existing condition limitation applied to benets when joining the university’s Medical Plans.
HOW PAYMENT IS DETERMINED
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 28 of 92
Revised 09/2023
When you receive Covered Services, a claim must be led for you to obtain benets. Network providers will le claims for you. If
you need to submit a claim yourself, the claim and appeal procedures are summarized here.
FILING A CLAIM
Claim Forms
Claim forms are available online at hr.osu.edu/policies-forms (under Form - Health Benets - Medical - Trustmark Health Insurance
Claim Form); or from HR Connection by calling 614-247-myHR(6947). Claim forms must be lled out completely and submitted as
indicated on the form.
Initial Claim
Generally, all claims must be submitted within 12 months from the incurred date of service. In certain cases, you may be required to
obtain Prior Authorization for services (refer to this SPD for details on the services requiring Prior Authorization, or go to the Medical
Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies for a list of such
services).
Notice of Determination – If your claim is wholly or partially denied, you will receive a written notice of the decision that will generally
contain:
• Specic reasons for the claim’s denial (including denial codes, as required);
• A description of additional material or information necessary for you to perfect your claim and an explanation of why such
information is necessary;
• Specic references to pertinent plan provisions;
• A statement of your right to request an external review and a description of the plan’s internal appeals and external review
procedures, including your right to request an expedited internal and/or external review in certain circumstances; and
• The availability of, and contact information for, the Ohio Department of Insurance.
• In addition, if an internal rule, guideline or protocol was relied on in making the benet determination, or if the denial is based on
medical necessity, experimental treatment or a similar exclusion or limit, an explanation of such rule or protocol, or the scientic or
clinical judgment used in the determination will be provided in the notice.
Time Frame for Notication – You will be notied of the decision on appeal within certain timeframes established by law. Refer to the
Appendix at the end of this SPD titled “Claims Determination and Appeals Procedures” for additional details.
APPEAL PROCEDURE
If your claim is denied and you wish to have your claim reconsidered, you (or your representative) may appeal. Your appeal must be
received in writing within 180 days after the initial determination. You may submit additional comments, records and documents
related to your claim. You may also, upon request and at no charge, review copies of the documents and information relevant to your
claim. The person who decides the appeal will not be the same individual who decided the claim (or a subordinate of that individual).
Notice of Determination – Notice of the decision will be in writing and will include generally the information detailed above for your
initial claim, as it relates to your appeal.
Time Frame for Notication – You will be notied of the decision on appeal within certain timeframes established by law. Refer to the
Appendix at the end of this SPD titled “Claim Determination and Appeals Procedures” for additional details.
Second-Level Appeal – For post-service claims (see “For More Information” below), if your claim is denied on the rst appeal, you may
ask for a second review. A request for a second review must be submitted, in writing, within 60 days after the date the claim is denied
on the rst appeal. Additional comments, documents or other information relating to your claim should also be submitted. You will be
notied of a decision on your second appeal within 30 days.
External Review – If your appeal is denied, you may be entitled to an independent external review of the denial. External review is
generally limited to denied appeals for medical benets that involve medical judgment (e.g., medical necessity or a determination of
whether a treatment is experimental or investigational). You must request an external review in writing (electronically or verbally if
an expedited review) within 180 days after the notice of determination on appeal. You must generally exhaust (or be deemed to have
exhausted) the plan’s internal claims appeals procedures to be eligible for an external review. You may be eligible for an expedited
external review if the denial could seriously jeopardize your life or health. The assigned independent review organization must provide
written notice of its decision within 30 days after request for a standard review, or within 72 hours for an expedited review.
FOR MORE INFORMATION
The above information provides only a summary of the Medical Plan’s internal claims and appeals and external review procedures. To
review the complete internal claims and appeals and external review procedures refer to the Appendix at the end of this SPD titled
“Claim Determination and Appeals Procedures.”
CONTINUED ON PAGE 29
MEDICAL CLAIMS PROCESSING
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 29 of 92
Revised 09/2023
COORDINATION OF BENEFITS
• All benets provided as described in this document, except prescription drugs obtained under the Prescription Drug Benet, are
subject to coordination of benets (COB). COB determines whether a benet plan is primary or secondary when a Covered Person is
covered by more than one benet plan.
• If you or your family members are covered by more than one medical plan, you may not be able to collect benets from both plans.
Each plan may require you to follow its rules or use specic doctors and hospitals and it may be impossible to comply with both
plans at the same time. Read the rules very carefully and compare them with the rules of any other plan that covers you or your
family.
• In addition to the denitions in the “Denitions” section of this SPD, the following denition of “other contract” applies to this section:
- Any arrangement providing medical care benets or services, including but not limited to: group, blanket, or franchise insurance
coverage; group or individual practice or other prepayment coverage; labor management trusteed plans; union welfare plans;
employer organization plans, or employee benet organization plans; or any tax supported or governmental program.
DETERMINING PRIMARY COVERAGE
• To decide which plan is primary, the university plan must consider both the COB provisions of the other contract and which member
of your family is involved in a claim.
• The primary coverage will be determined by using the rst of the following rules that applies:
Non-Coordinating Plan:
• Another contract with no COB provision is always primary.
Employee:
• The benet plan covering you as an employee, member or subscriber (other than a dependent) is primary.
Children:
• The Birthday Rule – When a dependent is covered by more than one plan of different parents who are not separated or divorced, the
coverage of the parent whose birthday falls earlier in the calendar year (excluding year of birth) is primary.
- If both parents have the same birthday, the plan that covered the parent longer will be primary.
- If a dependent is covered by two benet plans and the non-university contract does not have this COB “birthday” rule, then the
rule of the other contract will determine the primary and secondary contract. If the other contract has a rule based on the gender
of the parent, then the gender rule will determine the primary and secondary contract.
- If a court decree species the parent who is nancially responsible for the child’s medical care expenses, the coverage of that
parent is primary.
- If the court decree states that both parents are responsible for the child’s medical care expenses, then the following rules shall
apply:
1. the plan of the parent whose birthday fails earlier in the calendar year shall be primary; or
2. if both parents have the same birthday, the plan that has covered either parent the longest is primary.
• If there is a court decree that orders joint custody and does not determine primary status for benet coverage, the regular provisions
establishing the primary status for children of active employees will apply.
• Parents separated or divorced – If the parents are separated or divorced, the following rules apply:
- If the parent with custody has not remarried, his or her coverage is primary.
- If the parent with custody has remarried, his or her coverage is primary, the stepparent’s is secondary and the coverage of the
parent without custody pays last.
Former Employee:
• When a plan covers you as an active employee or a dependent of such employee and the other contract covers you as a laid-off or
retired employee or as a dependent of such person, the plan which covers you as an active employee or dependent of such employee
is primary.
• When a person whose coverage is provided under a right of continuation pursuant to federal or state law (such as COBRA) also
is covered under another plan, the plan covering the person as an employee, member or subscriber, or retiree (or as that person’s
dependent) is primary and the continuation coverage is secondary.
Other Situations:
• When the rules above do not apply, the plan that has covered you longer is primary.
COB Payment Process
COB affects benets in the following manner when you are covered by more than one benet plan:
• When this Medical Plan is primary, Trustmark will authorize the payment of benets on behalf of the university without regard to any
other contract.
CONTINUED ON PAGE 30
MEDICAL CLAIMS PROCESSING
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 30 of 92
Revised 09/2023
COB Example 1
Primary OSU (if primary)
Allowed Amount $2,800 2,800
Deductible -$800 -$0
Coinsurance -$400 -$280
Payment $1,600 $2,520
In this example, as the secondary plan, the Ohio State Medical Plan would pay $1,200, which is the total patient responsibility under
the primary plan ($800 deductible and $400 coinsurance). The Medical Plan would pay that amount because it is less than the
amount it would pay if it was the primary plan ($2,520).
COB Example 2
Primary OSU (if primary)
Allowed Amount $2,800 2,800
Deductible -$2,800 -$0
Coinsurance -$0 -$280
Payment $0 $2,520
In this example, as the secondary plan, the Ohio State Medical Plan would pay $2,520, which is the amount the Medical Plan would
pay if it were primary. The Ohio State Medical Plan would pay that amount because it is less than the total patient responsibility
under the primary plan ($2,800 deductible).
ITEMIZED BILL
You have the right to receive a copy of an itemized bill. This bill identies the services and supplies rendered to you. To receive a copy
of the bill, send a written request to the provider from which you have received care. It is in your best interest to exercise this right so
you have a copy of the bill for your personal les.
LIMITATION OF ACTION
No lawsuit can be brought to recover benets unless you have complied with the applicable claims and appeals procedures and
completed the appeal process. Specically, you cannot bring a lawsuit until after the date of the decision on nal appeal. No such
action may be taken later than one year after the time decision on the nal appeal.
PAYMENT OF CLAIMS
• Trustmark reserves the right to make payments to the provider or directly to you. For a network provider, when the provider of
service submits the claim to Trustmark the payment will be issued to the provider. If the member submits the claim and the provider
is not a network provider, then the payment will usually be issued to the member. Payments may not be directed to any other party.
When a service has been rendered, Trustmark will not honor a request to withhold payment of the claim.
• If a covered employee dies or becomes mentally incompetent, any benet owed may be paid to a relative by blood or marriage.
Trustmark, on behalf of the university, would provide the benet to a relative whom it judged to be entitled in fairness to the money.
Any such payment would discharge any obligation to the extent of such payment.
MEDICARE
• When you are covered under the university’s Medical Plan and are also eligible for Medicare due to age, you may:
- Continue your coverage under this Medical Plan (to the extent you remain eligible) and defer enrollment in Medicare.
- Continue your coverage under this Medical Plan and also enroll in Medicare. This Medical Plan would be your primary medical
coverage and Medicare your secondary medical coverage as long as your coverage under this Medical Plan is attributable to
current employment.
- This Medical Plan would be your primary medical coverage and Medicare your secondary medical coverage as long as your
coverage under this Medical Plan is attributable to current employment except when Medicare is required to be primary due to
End-Stage Renal Disease.
- Drop your coverage under this Medical Plan and enroll in Medicare.
• If a grandfathered sponsored dependent is Medicare-eligible, he or she must enroll in Medicare coverage.
• The university’s Medical Plan will always follow the Medicare primary/secondary rules which are then in effect as determined by the
federal government.
CONTINUED ON PAGE 31
• When this Medical Plan is secondary, the following process will be followed. The primary plan pays benets rst. The primary plan
will ignore the fact that the member is covered under a secondary plan and will pay the full eligible benet. The secondary plan pays
next by following these steps:
1. The secondary plan will rst calculate the plan benets.
2. The secondary plan will pay the lesser of:
a. The total patient responsibility (deductible, copay, coinsurance) under the primary plan; or
b. The amount OSU would pay as primary.
MEDICAL CLAIMS PROCESSING
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 31 of 92
Revised 09/2023
SUBROGATION AND REIMBURSEMENT
A Covered Person may incur medical expenses due to an injury or sickness that may be caused by the act or omission of a third
party. Also, a third party (such as an insurance company) may be responsible for payment or agree to compensate a Covered Person
on account of the actions of another person or entity. In such circumstances, the Medical Plan has a right to subrogation and/or
reimbursement, as described below.
Third Party
For purposes of this section, “third party” means any person, entity or organization that is or may be liable or legally responsible to pay
expenses, compensation or damages in connection with a Covered Person’s injury or sickness. A third party includes, but is not limited
to: the party or parties alleged to have caused or that caused the illness or injury or sickness; the insurer, guarantor or other indemnier
of the party or parties alleged to have caused or that caused the illness or injury; a Covered Person’s own insurer (e.g., automobile,
medpay, uninsured/ underinsured motorist, homeowners or other insurance policies); and any other person, entity or organization that
is or may be liable or legally responsible for payment in connection with the illness or injury or sickness.
Subrogation Rights
If a third party is or may be responsible for paying the expense of, or agrees to compensate a Covered Person for, any injury or sickness
covered by this Medical Plan, the Medical Plan has the right to take the Covered Person’s place in recovering payments directly from
the third party. The Medical Plan’s right to do this is called its right of subrogation.
Reimbursement Rights
If a Covered Person receives a settlement or is otherwise compensated by a third party for any injury or sickness covered by this
Medical Plan, the Covered Person is required to reimburse the Medical Plan for the payments made by the Medical Plan. This is called
the Medical Plan’s right of reimbursement.
Amounts Subject to Subrogation and/or Reimbursement
Subject to Section 2323.44 of the Ohio Revised Code:
• All amounts recovered will be subject to subrogation and/or reimbursement.
• In no case will the amount subject to subrogation or reimbursement exceed the amount of benets paid for the injury or sickness
under the Medical Plan and the expenses incurred by the Medical Plan in collecting this amount.
• The Medical Plan has a priority over you and your dependent(s) as to any funds recovered.
• The Medical Plan has a right to recover in full, regardless of how amounts received from a third party may be characterized and
regardless of whether or not the Covered Person (s) have been made whole.
• The Medical Plan has a right to recover in full, regardless of whether the amounts received from a third party are paid directly to the
Covered Person, or placed in a trust or structured settlement for the benet of the Covered Person.
• The Medical Plan’s subrogation and reimbursement rights will not be reduced to reect any cost or attorneys’ fees incurred in
obtaining the compensation unless separately agreed to, in writing, by the university in the exercise of its sole discretion.
• If a Covered Person fails to comply with any of the terms of the Medical Plan governing subrogation and reimbursement, in addition
to any amount the Covered Person owes to the Medical Plan for subrogation and/or reimbursement, the Covered Person will be
liable to the Medical Plan for its reasonable costs to enforce those terms, including but not limited to attorneys’ fees incurred by the
Medical Plan.
Authorization by Covered Person
As a Covered Person under the Medical Plan, you agree to all of the terms of the Medical Plan regarding subrogation and
reimbursement, including, but not limited to, the following:
• You agree that the Medical Plan has rights of subrogation and reimbursement.
• You will promptly refund to the Medical Plan any amount that is subject to the Medical Plan’s rights of subrogation and/or
reimbursement.
• You, your dependent(s) and representative(s) will cooperate fully to help the Medical Plan enforce its rights of subrogation and
reimbursement, and will not do anything that prejudices or impairs those rights.
• You will provide all information needed under the Medical Plan to recover the amount of medical or other benets paid for the injury
or sickness under the Medical Plan and expenses incurred by the Medical Plan in collecting this amount, and execute and deliver any
papers necessary for such recovery.
• The Medical Plan may reduce any future benets otherwise available to you and your dependent(s) under the Medical Plan by the
full amount of the compensation received from the third party.
• You understand and agree that the third party may be sued in order to recover the payments made for you under the Medical Plan.
• You will notify the Medical Plan of any proposed settlement and obtain the Medical Plan’s written consent before signing any release
or agreeing to any settlement. If a Covered Person or the Covered Person’s representative chooses to recover payment from a third
party, the Covered Person or representative must include the amount paid by the Medical Plan in the requested settlement.
MEDICAL CLAIMS PROCESSING
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 32 of 92
Revised 09/2023
PRIOR AUTHORIZATION - HOSPITALIZATION
• Prior Authorization (see the Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools -
Forms and Policies) is a determination made by OSU Health Plan of the Medical Necessity of an inpatient hospital setting and
the appropriate length of stay. Authorization must be obtained for every hospital admission. Prior Authorization for emergency
admissions must be obtained as soon as possible following admission, but generally within one business day.
• If the Covered Person sees a network provider, the network provider is responsible for obtaining the Prior Authorization.
• If the Covered Person is enrolled in a non-network coverage option or uses an out-of-network provider, it is his or her responsibility
to obtain Prior Authorization and to inform the providers that he or she is enrolled in a medical plan that has Prior Authorization
1
requirements.
• In order for OSU Health Plan to conduct a pre-admission review, it must be:
- Provided with information necessary to make a decision as to the Medical Necessity of the admission.
- Informed no later than 10 business days prior to the admission to the hospital, unless the admission is an urgent care admission.
• The hospital, admitting physician, covered person, or any person on the patient’s behalf can give notice to OSU Health Plan of a
hospital admission.
• When the Covered Person contacts OSU Health Plan for Prior Authorization, he or she will need to provide the following
information:
- Name and identication number of the employee
- Name, address, sex and birth date of the patient
- Name, address and telephone number of the admitting physician
- Name, address and telephone number of the admitting hospital
- Date of proposed admission and reason for the admission.
Failure to Receive Prior Authorization
If OSU Health Plan is not informed of a Covered Person’s hospital admission and Prior Authorization
1
is not obtained, payment of
benets by Trustmark for eligible hospital expenses may be reduced, denied, or subject to penalties.
CONTINUED STAY REVIEW
During a Covered Person’s hospital stay, a continued stay review may be conducted. The purpose of this review is to:
• Provide OSU Health Plan with an update as to the Covered Person’s condition/progress.
• If necessary, enable OSU Health Plan to re-evaluate the Medical Necessity of a continued hospital stay.
DISCHARGE PLANNING REVIEW
Review for discharge planning occurs during hospitalization review. The purpose is to:
• Identify patients requiring extended care following discharge.
• Determine the most appropriate setting for continued care, if applicable.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
HOSPITALIZATION REVIEW
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 33 of 92
Revised 09/2023
COBRA
The Consolidated Omnibus Budget Reconciliation Act of 1985 is a federal law commonly referred to as COBRA. COBRA requires that
most employers sponsoring group health plans offer employees and their families the opportunity for a temporary extension of health
coverage (called coverage continuation) at group rates in certain instances where coverage under the plan would otherwise end. This
section is intended to summarize your rights and obligations under the coverage continuation provisions of the law.
Note: COBRA or COBRA-like coverage is available to the employee, spouse and eligible dependents if coverage under the Medical
Plan ends.
EAP: For purposes of the EAP benets, any employee or member of the employee’s household who is not enrolled in the Medical Plan
may continue EAP coverage under COBRA.
Employee
If you are an employee covered by the Medical Plan, you have a right to choose this coverage continuation for up to 18 months if you
lose your group health coverage due to:
• Reduction in your hours of employment that affects benet eligibility; or
• Termination of your employment (for reasons other than gross misconduct on your part).
Coverage may be continued for up to 24 months if you are on a leave of absence for United States uniformed service.
Note: For all other qualifying events (divorce or legal separation or a dependent losing eligibility for coverage as a dependent), you
must notify the Ofce of Human Resources, as provided below, within 60 days after the qualifying event occurs.
Spouse
If your spouse is covered by the Medical Plan, he or she has the right to choose this coverage continuation if group health coverage
under the Medical Plan is terminated for any of the following reasons:
• Coverage may be continued for up to 18 months due to:
- Termination of your employment (for reasons other than gross misconduct); or
- Reduction in your hours of employment that affects benet eligibility.
• Coverage may be continued for up to 24 months if you are on a leave of absence for United States uniformed service.
• Coverage may be continued for up to 36 months due to:
- Death of the Covered Employee (If you enroll in coverage through COBRA as a result of the death of an employee, COBRA
coverage is paid by the university for two months following the date of the Covered Employee’s death.);
- Divorce, or legal separation; or
- Termination of your employment (for reasons other than gross misconduct on your part) or reduction in your hours of employment,
coupled with your entitlement to Medicare benets less than 18 months before your termination of employment or reduction in
hours of employment. In this case, coverage may be continued for up to 36 months from the date of your Medicare entitlement.
Dependent Child/ Other Eligible Individuals as Dened by the University
In the case of a dependent child or other eligible individual as dened by the university (refer to the “Eligible Dependents” section of
this SPD) covered by the Medical Plan, he or she has the right to choose this coverage continuation if group health coverage under the
Medical Plan is terminated for any of the following reasons:
• Coverage may be continued for up to 18 months due to:
- Termination of your employment (for reasons other than gross misconduct) or
- Reduction in your hours of employment that affects benet eligibility.
• Coverage may be continued for up to 24 months if you are on a leave of absence for United States uniformed service.
• Coverage may be continued for up to 36 months due to:
- The death of the Covered Employee (If you enroll in coverage through COBRA as a result of the death of an employee, COBRA
coverage is paid by the university for two months following the date of the Covered Employee’s death.);
- The Covered Employee’s divorce, legal separation, or termination of grandfathered sponsored dependency (university afdavit
required);
- The dependent ceases to meet the eligibility requirements of a dependent ( refer to the “Eligible Dependents” section of this SPD);
or
- Termination of your employment (for reasons other than gross misconduct on your part) or reduction in your hours of employment,
coupled with your entitlement to Medicare benets less than 18 months before your termination of employment or reduction in
hours of employment. In this case, coverage may be continued for up to 36 months from the date of your Medicare entitlement.
Although your eligible dependents other than your dependent children are not “qualied beneciaries” for purposes of COBRA, the
Medical Plan extends COBRA-like continuation rights to such dependents that are equivalent to the rights that a dependent child
would have under COBRA.
Notication
• The employee or a family member is required to complete a COBRA Election Form, available from Trustmark, for a divorce, legal
separation, termination of grandfathered sponsored dependency, or a child ceasing to be an eligible dependent under the Medical
Plan. If such an event occurs, you should notify the Ofce of Human Resource within 60 days of the date the event occurs.
• If such notice is not provided within 60 days, the affected individuals will lose their right to elect coverage continuation under the
Medical Plan with respect to such event.
• When the university is notied that one of these events has happened, or if any other qualifying event occurs, then Trustmark will
notify you and your family of the right to choose coverage continuation.
CONTINUED ON PAGE 34
COVERAGE CONTINUATION
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 34 of 92
Revised 09/2023
Election Period
You have 60 days from the later of (i) the date you lose coverage, as described in the previous section, or (ii) the date Trustmark
provides the COBRA notice (i.e. a COBRA Election Form) to you.
Health Coverage
• If you do not elect coverage continuation, your group health coverage will end on your termination date.
• If you elect coverage continuation, your Medical Plan coverage will continue and will be identical to the same benet as provided
under that plan to similarly situated employees or family members (such as active employees and their dependents).
• You may change your coverage option or coverage level during the university’s annual open enrollment period or at the time of a
qualifying status change.
Disability Extension
If you or anyone in your family covered under the Plan is determined by Social Security to be disabled and you notify Trustmark in a
timely fashion, you and your entire family may be entitled to get up to an additional 11 months of COBRA continuation coverage, for a
maximum of 29 months.
• The disability would have to have started at some time before the 60th day of COBRA continuation coverage and must last at least
until the end of the 18-month period of COBRA continuation coverage.
• You must notify the Ofce of Human Resources within 60 days of the date the individual is determined to be disabled under the
Social Security Act and within 30 days of the date he or she is nally determined not be disabled. (Coverage will end on the rst day
of the month beginning at least 31 days after the covered individual is determined not to be disabled.)
Other Coverage Options
Instead of enrolling in COBRA continuation coverage, there may be other coverage options for you and your family through the Health
Insurance Marketplace, Medicaid, or other group health plan coverage options (such as a spouse’s plan) through what is called a
“special enrollment period.” Some of these options may cost less than COBRA continuation coverage. You can learn more about many
of these options at www.healthcare.gov.
Termination of Coverage Continuation
You are no longer eligible for coverage continuation and may be terminated from the Medical Plan for any of the following reasons:
• The premium for your coverage continuation is not paid on time. (See the “Payment” section below.)
• After rst electing coverage continuation, you become covered under another group health plan that does not contain any exclusion
or limitation with respect to any pre-existing condition.
• After rst electing coverage continuation, you become entitled to Medicare.
• You reach the end of your coverage continuation period.
• In the event that you are receiving extended coverage continuation as a result of your being disabled under the Social Security
Act, your extended coverage continuation may be terminated by the medical plan on the rst day of the month at least 30 days
after a nal determination that you are no longer disabled. You must notify the Medical Plan within 30 days of the date of any nal
determination under the Social Security Act that you are no longer disabled.
• The university no longer provides group health coverage to any of its employees.
Evidence of Insurability (EOI)
It is not necessary for you to show that you are insurable to choose coverage continuation.
Payment
All payments are due by the rst day of each month to Trustmark. The full premium for coverage continuation plus an administrative
charge must be paid. (Although monthly payments are due on the rst day of every month, you will be given a grace period of 30 days
to make each monthly payment. If you pay a monthly payment later than the rst day of the month, but before the end of the grace
period for the coverage period, your coverage may be suspended and then retroactively reinstated when the monthly payment is
received. If you fail to make a monthly payment before the end of the grace period for that month, you will lose all rights to continuation
coverage.) The premium for an extended coverage continuation period due to a total disability may be higher than the premium due for
the rst 18 months.
Changes
Notify Trustmark if there are changes in the following:
• The Covered Person becomes entitled to other group health coverage or Medicare.
• The Social Security Administration determines the Covered Person is no longer disabled.
• The Covered Person’s marital status.
• The Covered Person’s home mailing address.
COVERAGE CONTINUATION
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 35 of 92
Revised 09/2023
PRESCRIPTION DRUG BENEFIT
The Prescription Drug Benet is available to those enrolled in any coverage option available under the Medical Plan.
ELIGIBILITY
You must be enrolled in the Medical Plan.
PRESCRIPTION DRUG ID CARDS
Your prescription drug ID card can be viewed, or printed, by going to express-scripts.com or by using the mobile app.
PROGRAM HIGHLIGHTS
• The Prescription Drug Benet offers three main categories of prescription medications:
- Generic drugs
- Formulary brand name drugs
- Non-formulary brand name drugs
• The Express Scripts National Preferred Formulary can be found online at hr.osu.edu/benets/prescription .
• At the time of your medical visit, you are encouraged to discuss with your health care provider the medical and nancial advantages
of generic and formulary brand name prescription drugs.
• Prescription drug coverage is provided through the Express Scripts Retail Network which includes both preferred and non-preferred
pharmacies. If you utilize a preferred retail pharmacy, you will receive a greater benet than at a non-preferred pharmacy. No
benets are payable if you utilize a pharmacy that is not in the Express Scripts Retail Network. Refer to express-scripts.com or
contact Express Scripts for the location of network pharmacies near you. A nationwide toll free number is located on the prescription
drug ID card.
• You may also receive your prescription drugs through the mail by using Express Scripts Home Delivery.
• Both the retail and Express Scripts Home Delivery are coordinated for complete service (customer service, prescription prole and
annual out-of-pocket charges). The Prescription Drug Benet also provides for the monitoring of your prescriptions for potential drug
interactions and improper drug dosing through a drug utilization review program.
ANNUAL OUT-OF-POCKET MAXIMUM
The annual out-of-pocket maximum is the maximum total amount each Covered Person or family pays toward covered prescription
drug costs in a Plan Year. Once this limit is met, no more prescription drug member cost share is required for the remainder of the Plan
Year, except as indicated below. Refer to the “Prescription Drug Benet – Benet Summary” section of this SPD for details.
• Any medication paid for out-of-pocket that is not covered by the Medical Plan or the Prescription Drug Benet is excluded from
this limit.
• The Prescription Drug Benet annual out-of-pocket maximum is separate from any limits applicable under the Medical Plan.
ANNUAL DEDUCTIBLE
The annual deductible for prescription drug purchases for Prime Care Advantage, Prime Care Choice and Out-of-Area coverage
options is $50 per person, $100 per family per Plan Year. These are separate from your Medical Plan’s annual deductible. There is no
annual deductible for prescription drug purchases under the Prime Care Connect coverage option.
COORDINATION OF BENEFITS (COB)
There is no coordination of pharmacy benets. This Prescription Drug Benet does not cover prescription drugs as a secondary payer.
COVERED DRUGS
• Covered Drugs are medications that require a prescription under federal law and are approved for general use by the Food and Drug
Administration. Prescription drugs must be dispensed for your outpatient use by a licensed pharmacy on or after your coverage
effective date.
• Covered Drugs that are over-the-counter (OTC) drugs require a prescription for coverage under the Prescription Drug Benet and
must be dispensed for your outpatient use by a licensed pharmacy on or after your coverage effective date.
• The administration of prescription drugs is not covered under the Prescription Drug Benet, with the exception of certain vaccines
via the Express Scripts Retail Vaccination Program. The administration of covered and non-covered prescription drugs may be
covered under the Medical Plan.
Note: Under Ohio law, Naloxone may be dispensed for use by an individual if there is reason to believe they are at risk of experiencing
an opioid-related overdose. In that case, the Naloxone will be treated as being dispensed for your outpatient use under the Prescription
Drug Benet.
CONTINUED ON PAGE 36
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 36 of 92
Revised 09/2023
COVERED PERSON’S RESPONSIBILITIES
For the Prescription Drug Benet to work effectively, there are certain procedures, which you, as a Covered Person, must follow. In
general, when receiving prescription drugs:
• If a generic medication is not available or appropriate for your condition, you should discuss formulary options with your health care
provider while referring to a copy of the Express Scripts National Preferred Formulary, available online at hr.osu.edu/benets/
prescription.
• Present your prescription drug ID information to the pharmacist at participating retail pharmacies. You may also contact Express
Scripts directly for the location of the nearest Express Scripts Retail Network pharmacy in the area, or search online at
express-scripts.com.
FORMULARY
The Express Scripts National Preferred Formulary is a list of medications that are chosen based on comparative clinical effectiveness,
safety proles and opportunities to help contain costs. The formulary list used by the university’s Prescription Drug Benet is available
online at hr.osu.edu/benets/prescription.
• Certain medications are excluded from coverage and will be subject to the full retail price. A list of medications excluded
under the Prescription Drug Benet are available on the Express Scripts National Preferred Formulary list online at
hr.osu.edu/benets/prescription.
GENERIC DRUGS
Network pharmacies will dispense a generic equivalent drug whenever possible. Generic drugs, like brand name drugs, are federally
controlled to meet the same standards of composition, safety, strength, purity and quality. If you receive a generic drug, you may pay a
lower amount than if the prescribed drug is on the Express Scripts National Preferred Formulary.
EXPRESS SCRIPTS HOME DELIVERY (EXCLUDES SPECIALTY MEDICATIONS)
With the convenience of home delivery, members taking maintenance medications may receive a 90-day supply of medication per
prescription. Maintenance medications can include those that are used for birth control, hormone replacement therapy, or to treat
asthma, diabetes, high blood pressure, or any chronic health condition. The prescription is sent to the Express Scripts Home Delivery
service where it is subject to the same monitoring parameters as in a local (or retail) pharmacy. The lled prescription is then mailed
to you.
ERECTILE DYSFUNCTION MEDICATIONS
• Covered erectile dysfunction drugs (brand or generic) are subject to a 50% coinsurance with no maximum.
• The Prescription Drug Benet annual out-of-pocket maximum does not apply to erectile dysfunction drugs.
INFERTILITY MEDICATIONS
Infertility medications are subject to the following conditions:
• Excluded from the Prescription Drug Benet’s maximum copay for formulary/non-formulary medications.
• Subject to the infertility lifetime benet limit (see the “How Payment Is Determined – Maximum Benet Limits” section of this SPD).
LOW-COST GENERIC DRUG PROGRAM
Low-Cost Generic Drugs (Home Delivery): A limited list of generic maintenance medications is available through Express Scripts
home delivery at a cost of $10 per 90 day supply. For more information contact OSU Health Plan at 614-292-4700.
OUT-OF-NETWORK PHARMACY
Prescriptions lled at out-of-network pharmacies are not covered unless they are approved by OSU Health Plan due to an emergency
situation. For more information, contact OSU Health Plan.
PHARMACY BENEFIT MANAGER
Express Scripts is the university’s pharmacy benet manager. Express Scripts processes prescription drug claims and provides Prior
Authorization for certain medications.
PRIOR AUTHORIZATION
Your Prescription Drug Benet provides coverage for some medications only if they are prescribed for certain uses. For this reason,
some medications must receive Prior Authorization from Express Scripts before the drugs can be covered under your plan. If your
prescription drug is not approved for coverage under the Prescription Drug Benet, you will be responsible for paying the full cost of
the medication. For more information contact OSU Health Plan at 614-292-4700.
CONTINUED ON PAGE 37
PRESCRIPTION DRUG BENEFIT
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 37 of 92
Revised 09/2023
QUANTITY LEVEL LIMITS (QLL)
Some medications have quantity level limits allowing coverage for an amount of medication consistent with the Prescription Drug
Benet’s intent for the benet. For more information contact OSU Health Plan at 614-292-4700.
SAVEONSP COPAY ASSISTANCE PROGRAM
The Prescription Drug Benet participates in a copay assistance program available through SaveonSP and Express Scripts, which
takes advantage of the funds available from drug manufacturers to lower your cost and the amount the Prescription Drug Benet pays.
Your pharmacy (Accredo, OSU Outpatient Pharmacy, or Nationwide Children’s Hospital Outpatient Pharmacy) will determine whether
your specialty medication is eligible for the SaveonSP copay assistance. If it is, you will be contacted by SaveonSP to enroll and lower
your cost to $0. SaveonSP will only contact you if your specialty medication is eligible for the copay assistance program. If you choose
not to participate in the SaveonSP copay assistance program, you will pay a signicant copay for your specialty medications.
The specialty medications covered by the SaveonSP copay assistance program are considered non-essential health benets, and
any copay expenses will not be applied toward your annual deductible or annual out-of-pocket maximum. If you take a specialty
medication that is not subject to the SaveonSP copay assistance program, your prescription will be subject to the coverage described
in the Prescription Drug Benet Schedule of Benets.
For a full listing of medications or to determine whether a specic medication is part of this program, call SaveonSP at 800-683-1074
or visit https://hr.osu.edu/wp-content/uploads/oe-rx-saveonsp-list.pdf
STEP THERAPY
Step therapy is an authorization review program which requires initial utilization of clinically sound and cost-effective treatment
options before more expensive medications are covered. If a medication is prescribed that does not meet the step therapy criteria, it
may not be covered. Individuals should always consult with their physician about an alternative therapy. For more information contact
OSU Health Plan at 614-292-4700.
VALUE BASED DRUG BENEFIT
Faculty, staff and their dependents who use a preferred pharmacy within the Express Scripts Retail Network and who participate in
the Care Coordination Program are eligible for the Value-Based Drug Benet. If you actively participate in ongoing calls with a Care
Coordinator for management of asthma, chronic obstructive pulmonary disease (COPD), diabetes and heart disease (coronary artery
disease or congestive heart failure), you are considered to be participating in the Care Coordination Program. Refer to Care
Coordination online at osuhealthplan.com under Programs and Services for more details. This benet will reduce or eliminate the
cost of the prescription medications taken specically to treat these chronic conditions. By participating in the Care Coordination
Program, the copay for certain generic drugs taken to treat the chronic condition will be waived and the coinsurance amount for certain
formulary brand-name drugs taken to treat the chronic condition will reduce by 50%. If a member chooses not to use a preferred
pharmacy or not to participate in the Care Coordination Program they will not be eligible for the Value-Based Drug Benet. Members
must also use a preferred pharmacy within the Express Scripts Retail Network in order to receive the Value-Based Drug Benet. Visit
Care Coordination online at osuhealthplan.com under Programs and Services to learn more about the Care Coordination Program.
For More Information
Express Scripts’ contact information is listed on the front of your prescription drug ID card available at express-scripts.com and on
page 2 of this document.
FILING A CLAIM
Claim Forms
• Claim forms are available online at hr.osu.edu (under Policies/Forms-Forms-Health Benets-Prescription Drug Reimbursement
Form).
• Claim forms must be lled out completely and mailed to the address provided on the form.
Initial Claim
All claims must be submitted within 12 months from the incurred date of service. In certain cases, you may be required to obtain Prior
Authorization from Express Scripts for some medications (refer to the Medical Prior Authorization Guide available online at
osuhealthplan.com under Health Plan Tools - Forms and Policies) for a complete list of medications requiring Prior Authorization.
Notice of Determination – If your claim is wholly or partially denied, you will receive a written notice of the decision that will generally
contain:
• Specic reasons for the claim’s denial (including denial codes, as required);
• A description of additional material or information necessary for you to perfect your claim and an explanation of why such
information is necessary;
• Specic references to pertinent plan provisions;
• A statement of your right to request an external review and a description of the plan’s internal appeals and external review
procedures, including your right to request an expedited internal and/or external review in certain circumstances; and
CONTINUED ON PAGE 38
PRESCRIPTION DRUG BENEFIT
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 38 of 92
Revised 09/2023
• The availability of, and contact information for, the Ohio Department of Insurance.
• In addition, if an internal rule, guideline or protocol was relied on in making the benet determination, or if the denial is based on
medical necessity, experimental treatment or a similar exclusion or limit, an explanation of such rule or protocol, or the scientic or
clinical judgment used in the determination will be provided in the notice.
Time Frame for Notication – You will be notied of the decision on appeal within certain timeframes established by law. Refer to the
Appendix at the end of this SPD titled “Claims Determination and Appeals Procedures” for additional details.
APPEAL PROCEDURE
If your claim is denied and you wish to have your claim reconsidered, you (or your representative) may appeal. Your appeal must
be received in writing within 180 days after the initial determination. You may submit additional comments, records and documents
related to your claim. You may also, upon request and at no charge, review copies of the documents and information relevant to your
claim. The person who decides the appeal will not be the same individual who decided the claim (or a subordinate of that individual).
Notice of Determination – Notice of the decision will be in writing and will include generally that information detailed above for your
initial claim, as it relates to your appeal.
Time Frame for Notication – You will be notied of the decision on appeal within certain timeframes established by law. Refer to the
Appendix at the end of this SPD titled “Claims Determination and Appeals Procedures” for additional details.
Second-Level Appeal – For post-service claims, if your claim is denied on the rst appeal, you may ask for a second review. A request
for a second review must be submitted, in writing, within 60 days after the date the claim is denied on the rst appeal. Additional
comments, documents or other information relating to your claim should also be submitted. You will be notied of a decision on your
second appeal within 30 days.
External Review – If your appeal is denied, you may be entitled to an independent external review of the denial. External review is
generally limited to denied appeals for medical benets that involve medical judgment (e.g., medical necessity or a determination of
whether a treatment is experimental or investigational). You must request an external review in writing (electronically or verbally if
an expedited review) within 180 days after the notice on appeal. You must generally exhaust (or be deemed to have exhausted) the
plan’s internal claims appeals procedures to be eligible for an external review. You may be eligible for an expedited external review if
the denial could seriously jeopardize your life or health. The assigned independent review organization must provide written notice of
its decision within 30 days after request for a standard review, or within 72 hours for an expedited review.
FOR MORE INFORMATION
The above information provides only a summary of the Prescription Drug Benet’s internal claims and appeals and external review
procedures. To review the complete internal claims and appeals and external review procedures refer to the Appendix at the end of
this SPD titled “Claim Determination and Appeals Procedures.”
PRESCRIPTION DRUG BENEFIT
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024
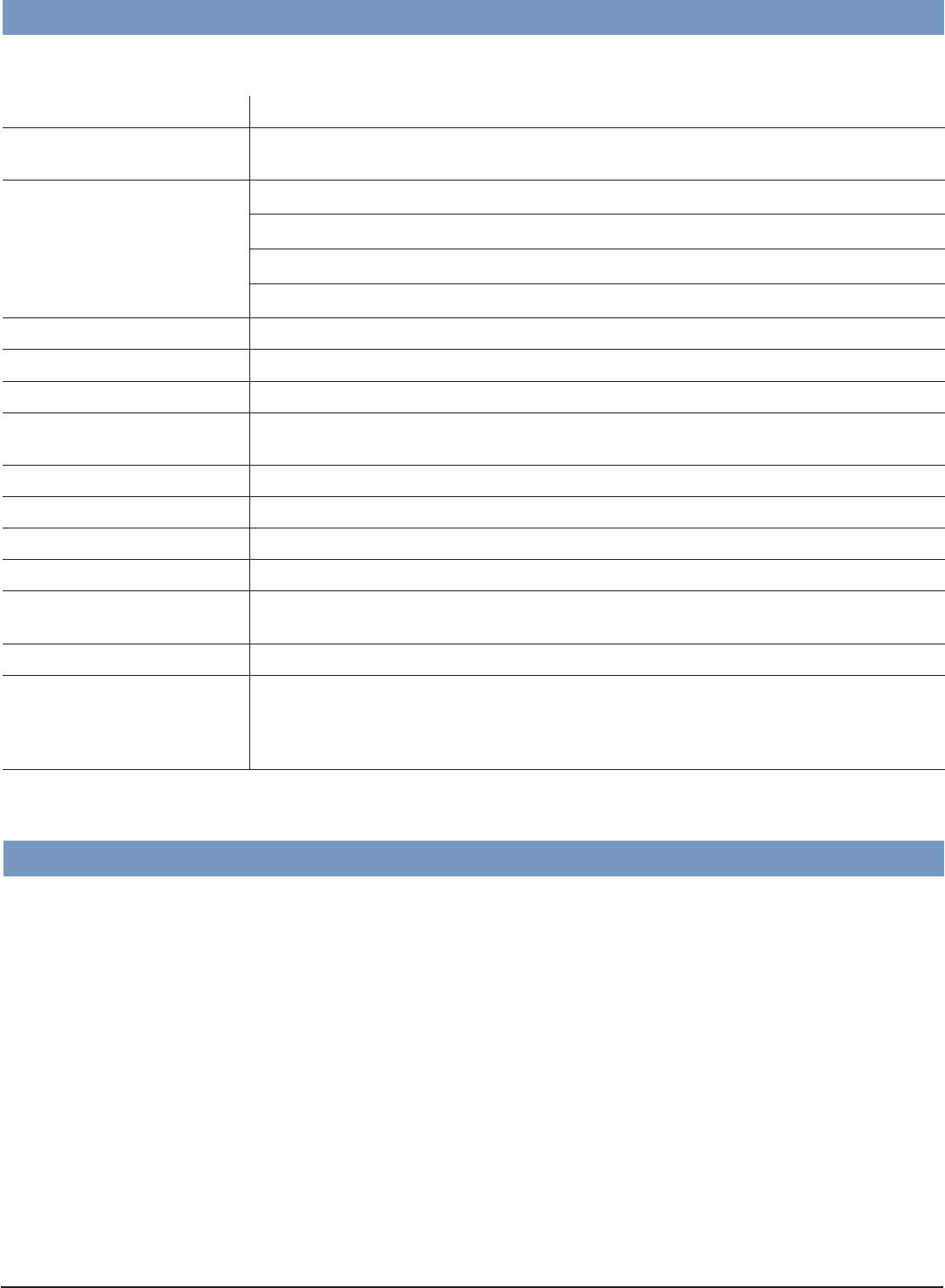
PAGE 39 of 92
Revised 09/2023
The complete pharmacy directory is available online at Express-Scripts.com, where it is regularly updated.
Allergens
Allergy shots
Compound Medications Are not covered if the product lacks documented clinical evidence and FDA approval for
use within compounds
Cosmetic Drugs
Photo-aged skin products
Hair growth products (e.g., Propecia) Injectable cosmetics (e.g., Botox Cosmetic)
Topical treatment products for Onychomycosis (toe nail fungus)
Depigmentation products (e.g., Lustra-AF, Glyquin/XM, Alphaquin HP, Solaquin Forte)
Erectile Dysfunction Drugs
Yohimbine
Durable Medical Equipment
e.g., Wheelchairs, crutches, nebulizers, peak ow meters, ostomy supplies
Diabetic Supplies
e.g., Glucowatch, Alcohol Swabs
Legend Vitamins Legend multivitamins and supplemental agents with OTC equiv. (e.g., Nephrocaps,
Biotin)
Legend Homeopathic Drugs
e.g., Psorzide Ultra, Vertigoheel
Hemophilia Products
e.g., Recombinate
Miscellaneous Exclusions
Medical products and medical supplies
Schedule 1 Drugs
e.g., medical marijuana
Non-Sedating
Antihistamines
e.g., Clarinex and Xyzal
OTC Equivalents
e.g., Hydrocortisone 1% cream, Mentax, Ranitidine 150mg
OTC Products Except insulin, certain diabetic supplies, Nexium 24HR and certain OTC preventive
medications (See Preventive Health Guidelines found at osuhealthplan.com Health Plan
Tools - Forms and Policies for a list of Preventive Medications and Devices, some of
which are OTC and available with no out-of-pocket costs)
Certain other restrictions may apply. Contact Express Scripts for additional information.
PRESCRIPTION DRUG EXCLUSIONS
Your prescription drug coverage does not provide benets for the following:
NETWORK PHARMACIES
PRESCRIPTION DRUG BENEFIT
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 40 of 92
Revised 09/2023
Rev 2023
EFFECTIVE JANUARY 1 – DECEMBER 31, 2024
1 Specic preferred insulin products will be available for a $25 copay per 34-day supply and a $75 copay per 90-day supply through the Express Scripts Patient
Assurance Program only at Preferred Pharmacies.
2 The Prescription Drug Benet annual out-of-pocket maximum is based on benet enrollment and is separate from the medical benet annual out-of-pocket
maximum.
3 Infertility treatment has a combined medical and pharmacy $15,000 lifetime maximum and is limited to a 30-day supply per ll. Prior Authorization from OSU
Health Plan is required.
4 The deductible applies to brand name medications only.
5 Retail90, also known as Smart90, is Express Scripts’ program which allows individuals to ll their prescriptions for up to a 90-day supply via select retail
pharmacies.
6 The Value-Based Drug Benet eligibility is based on actively participating in the Care Coordination Program for management of specic chronic conditions
(asthma, chronic obstructive pulmonary disease (COPD), diabetes, and heart disease). Visit osuhealthplan.com to learn more about the Care Coordination
Program.
7 Non-Formulary Brand Name Drugs are not eligible for the Value-Based Drug Benet.
8 The Value-Based Drug Benet is not available at Non-Preferred Pharmacies.
9 Certain specialty medications are included in the SaveonSP copay assistance program and subject to a different copay structure. While there are copays
associated with each product included in the SaveonSP program, the member copay will be $0. If an individual chooses not to enroll in SaveonSP, they will
be responsible for the prescription drug copay for qualied medications, and the copay amount will not apply to the Prescription Drug Benet out-of-pocket
maximum.
10 In certain cases, the outpatient pharmacy at Nationwide Children’s Hospital may also ll prescriptions under the Specialty Medication Benet. Contact OSU
Health Plan for details.
Preferred
Pharmacy
Non-Preferred
Pharmacy
Home Delivery or
Retail90 Pharmacy
5
Preferred
Pharmacy
Non-Preferred
Pharmacy
Home Delivery or
Retail90 Pharmacy
5
Supply Limitations
up to 30-day
supply
up to 30-day
supply
up to 90-day
supply
up to 30-day
supply
up to 30-day
supply
up to 90-day
supply
Generic Drug $10 copay $20 copay $25 copay $8 copay $18 copay $20 copay
Formulary Brand
Name Drug
30% coinsurance,
up to $100
35% coinsurance,
up to $110
30% coinsurance,
up to $250
30% coinsurance,
up to $40
35% coinsurance,
up to $50
30% coinsurance,
up to $100
Non-Formulary
Brand Name Drug
50% coinsurance,
no maximum
55% coinsurance,
no maximum
50% coinsurance,
no maximum
50% coinsurance,
no maximum
55% coinsurance,
no maximum
50% coinsurance,
no maximum
PRESCRIPTION DRUG BENEFIT
1
PRIME CARE ADVANTAGE
PRIME CARE CONNECTPRIME CARE CHOICE
OUT OF AREA
Annual Out-of-
Pocket Maximum
2,3
$2,500 per person, $5,000 per family $2,000 per person, $4,000 per family
Deductible
4
$50 per person, $100 per family No deductible
VALUED BASED DRUG BENEFIT
6,7,8
PRIME CARE ADVANTAGE
PRIME CARE CONNECTPRIME CARE CHOICE
OUT OF AREA
Preferred
Pharmacy
Home Delivery or
Retail90 Pharmacy
5
Preferred
Pharmacy
Home Delivery or
Retail90 Pharmacy
5
Supply Limitations
up to 30-day supply up to 90-day supply up to 30-day supply up to 90-day supply
Generic Drug $0 $0 $0 $0
Formulary Brand
Name Drug
15% coinsurance,
up to $50
15% coinsurance,
up to $125
15% coinsurance,
up to $20
15% coinsurance,
up to $50
Non-Formulary
Brand Name Drug
50% coinsurance,
no maximum
50% coinsurance,
no maximum
50% coinsurance,
no maximum
50% coinsurance,
no maximum
SPECIALTY MEDICATION BENEFIT
9
FEATURE RETAIL PHARMACY
OSUWMC PHARMACY AND ACCEDO
10
Supply Limitations
up to 30-day supply
Generic Drug
Not Available
20% coinsurance, up to $50
Formulary Brand Name Drug 20% coinsurance, up to $100
Non-Formulary Brand Name Drug
50% coinsurance, no maximum
PRESCRIPTION DRUG BENEFIT – SCHEDULE OF BENEFITS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 41 of 92
Revised 09/2023
PREVENTIVE DRUG LIST
If using a preferred pharmacy and with a prescription, the medications on the preventive list are covered with no out of
pocket cost to the member if eligibility criteria are met.
DRUG CATEGORY ELIGIBILITY CRITERIA
Aspirin Persons younger than 70
Fluoride Persons from 6 months to <17 years
Folic Acid Persons < age 51
Breast Cancer-Primary
Prevention
Subject to Prior Authorization:
• Tamoxifen (generic) • Raloxifene (generic)
• Anastrozole (generic) • Soltamox (Tamoxifen liquid) (brand)
• Exemestane (generic)
Vaccines
See Preventive Health Care Guidelines available online at osuhealthplan.com under Forms and
Downloads
HIV Pre-Exposure Prophylaxis
(PrEP)
Emtricitabine/Tenofovir Disoproxil Fumarate (generic)
Medications used to prepare for
Colonoscopy
Certain bowel preparation agents for persons ≥ 45 years of age
Statins
Low- to moderate-dose statins for persons ≥ 40 years and ≤ 75 years these medications include:
• Atorvastatin ≤ 20mg • Pravastatin ≤ 80 mg
• Fluvastatin ≤ 80 mg • Rosuvastatin ≤ 10 mg
• Lovastatin ≤ 40 mg • Simvastatin ≤ 40 mg
CONTRACEPTIVE COVERAGE
DRUG/DEVICE CATEGORY ELIGIBILITY CRITERIA
Covered products include all FDA-approved 16 contraceptive methods available
through the pharmacy benet. See Preventive Health Care Guidelines available online at
osuhealthplan.com under Forms and Downloads.
Persons < age 51years
TOBACCO CESSATION
DRUG CATEGORY ELIGIBILITY CRITERIA
Prescription and Over-the-Counter products with a physician prescription Person 18 and older.
PRESCRIPTION DRUG BENEFIT – SCHEDULE OF BENEFITS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 42 of 92
Revised 09/2023
PRIME CARE ADVANTAGE
ELIGIBLE EMPLOYMENT
• University faculty and staff with eligible appointments.
• University afliated group employees with eligible appointments at:
- Central Ohio Technical College (COTC)
- Ohio State University Physicians, Inc. (OSUP)
ENROLLMENT
Refer to the “Enrollment” section of this SPD for details. To enroll in this coverage option, use Workday online at workday.osu.edu or
submit a completed Health Election Form, available at hr.osu.edu/policies-forms (under Forms - Health Benets – Medical).
ENROLLMENT CHANGES
Refer to the General Provisions – “Change in Coverage Due to a Qualifying Status Change” section of this SPD.
COVERAGE ACCESS OUTSIDE THE NETWORK AREA
Access to out-of-area coverage is available with special application (online at hr.osu.edu/policies-forms (under Forms - Health Benets
– Medical see Out-of-Area Benet Election Form) to individuals enrolled in Prime Care Advantage who will be living outside Ohio for
at least 30 consecutive days. If the Out-of-Area Benet Election Form is received in our ofce within 30 days of the event (i.e., newly
benets eligible or the date the covered person moved outside the network area), Out-of-Area benets will be effective on the event
date. If the form is completed after 30 days of the event, Out-of-Area benets will be effective on the date the form is received in our
ofce. The form must be renewed annually. Contributions will not change. Examples of circumstances to enroll are:
• You have a dependent child who does not live with you and resides outside Ohio
• You have a dependent who attends college outside Ohio
• You will be outside Ohio on an approved leave of absence or an approved professional leave
• You will be outside Ohio during an off-duty term if you have a nine-month appointment and receive compensation and benets over
a 12-month period
Note: When traveling outside Ohio or the United States, you have access to Ohio State Travel Assistance services. Refer to the Ohio
State Travel Assistance section of this SPD for details.
CONTRIBUTION
The current contribution rates are available online at hr.osu.edu/benets/rates.
COVERED PERSON’S RESPONSIBILITIES
For the Medical Plan to work effectively, you must follow these procedures, when appropriate:
• Coordinate all medical care with your primary care physician.
• Conrm that all providers (physicians, labs, etc.), including those to whom you are referred, are network providers in order to ensure
coverage under the Medical Plan.
• Present your medical ID card to the provider before receiving medical services.
• Notify OSU Health Plan if a physician admits you to a hospital.
• Request Prior Authorization
1
of benets before receipt of certain designated services or elective admission to a hospital or facility.
SPECIAL POINTS TO CONSIDER WHEN USING YOUR PLAN
• When receiving medical services it is important to understand that:
- There are no benets if services are rendered outside the statewide network (except for emergency care services and except as
described above in “Coverage Access Outside Ohio” above). There are two networks—Premier and Standard—and both networks
provide payment for Covered Services based on the network provider’s fee schedule. However, you will receive the highest level of
benet coverage if you use a Premier Network provider.
- All medical treatment should be coordinated through your physician.
• Some services are fully covered while other services require a deductible, coinsurance, or both. When receiving Covered Services
within the network, simply present your medical ID card to your medical service provider.
• This coverage option requires the use of a statewide network of providers.
- When seeking medical care inside Franklin County, the OSU Health Plan network of physicians and facilities must be used. A
current list of network providers is available online at https://osuhealthplan.com/nd-a-provider-search or by contacting OSU
Health Plan at 614-292-4700.
- When seeking medical care outside Franklin County, the Ohio PPO Connect network of physicians and facilities must be used. A
current list of network providers is available online at https://osuhealthplan.com/nd-a-provider-search or by contacting OSU
Health Plan at 614-292-4700.
- If you are traveling outside Ohio or the United States you have access to Ohio State Travel Assistance services. Refer to the “Ohio
State Travel Assistance” section of this SPD for detail.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 43
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 43 of 92
Revised 09/2023
PROVIDER SELECTION
A complete list of network providers is available online at https://osuhealthplan.com/nd-a-provider-search, where it is updated
regularly.
Referrals to Specialists
While you may schedule an appointment directly with a network specialist, some specialists may require a referral from your primary
care physician before making an appointment. Your physician should refer you to a specialist within the network, unless the care you
need is not available within the network. If your physician refers you to a provider outside the network, it is your responsibility to obtain
authorization in advance from OSU Health Plan at 614-292-4700. If your authorization is approved, Covered Services will be paid
according to the network benet.
Note: Following emergency or specialist care, you should notify your primary care physician in order to keep him or her informed of
your medical condition.
HOW PAYMENT IS DETERMINED
Refer to the “How Payment is Determined,” “Exclusions or Limitations” and “Prime Care Advantage – Schedule of Benets” sections of
this SPD for details.
Network
Payments for Covered Services are based upon the network provider’s fee schedule. A member’s cost share (i.e., coinsurance or
deductible) may vary, depending on whether the provider is in the Premier Network or the Standard Network (each as dened in the
“Denitions” section of this SPD). You are not responsible for any balance in excess of the network provider’s fee schedule. In other
words, Covered Services obtained from network providers are not subject to Balance Billing.
Urgent Care
• Payment for covered urgent care services received from network urgent care providers will be based upon the network provider’s fee
schedule. You are not responsible for any balance in excess of the network provider’s fee schedule.
• Urgent care is not intended for preventive or routine maintenance treatment, such as school or annual physicals, and these types of
services will not be covered when received from an urgent care provider.
• Services received from an out-of-network urgent care provider in Ohio will not be covered.
• Urgent care received outside of Ohio will be paid at the network benet.
PRIME CARE ADVANTAGE
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024
PAGE 44 of 92
Revised 09/2023
PRIME CARE ADVANTAGE – SCHEDULE OF BENEFITS
BENEFIT OPTION PROVISIONS
Annual Deductible:
Individual: $550 per person
Family: $1,100 per family
Prescription Drug Benet: A separate deductible of $50 per person, $100 per family
Annual Out-of-Pocket Maximum: Excludes Weight Management Programs and non-Prior Authorization penalty
Individual: $3,000 per person
Family: $6,000 per family
Prescription Drug Benet: A separate limit of $2,500 per person, $5,000 per family applies; see program description
Maximum Benets:
Lifetime: No limit, except as noted for specic benets
Infertility: $15,000 lifetime maximum benet per person, includes prescription drugs used for infertility
Temporomandibular Disorder (TMD): $3,000 lifetime maximum benet per person for all non-surgical TMD covered services
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Acupuncture Services and
Chiropractic Care:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Combined maximum benet of $2,000 per Plan Year
Ambulance Services:
Paid at 80% of network fee schedule after annual deductible, when Medically Necessary
Behavioral Health Services:
Mental Health and Substance
Abuse – Inpatient:
Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Mental Health and Substance
Abuse – Outpatient:
Paid at 80% of network fee schedule no annual deductible
Chiropractic Care and
Acupuncture Services:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Combined maximum benet of $2,000 per Plan Year
Diabetes Education: Paid at 80% of network fee schedule after
annual deductible; no Prior Authorization
Paid at 70% of network fee schedule after
annual deductible; no Prior Authorization
Emergency Room Visits:
Paid at 80% of network fee schedule after annual deductible
Extended Care Facility Services: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Limit of up to 60 days per Plan Year; Prior Authorization
1
required
GYN Examination: One preventive exam per Plan Year paid at
100% of network fee schedule, no annual
deductible; additional diagnostic exams paid
at 80% of network fee schedule, no annual
deductible
One preventive exam per Plan Year paid at
100% of network fee schedule, no annual
deductible; additional diagnostic exams paid
at 70% of network fee schedule after annual
deductible
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 45

PAGE 45 of 92
Revised 09/2023
PRIME CARE ADVANTAGE – SCHEDULE OF BENEFITS
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Hearing Aids:
Paid at 80% of the billed amount after annual deductible 1,400 per hearing impaired ear
($2,800 bilateral) in total benets; every three (3) Plan Years; no network provider restrictions
Hearing Test (Audiometry):
Covered at 100% per the Preventive Health Care Guidelines found at osuhealthplan.com,
Health Plan Tools - Forms and Policies. Diagnostic exams for hearing loss are
covered at 80% (Premier) or 70% (Standard) after deductible.
Ear Molds for Hearing Aids:
Paid at 80% of the billed amount after annual deductible, every three (3) Plan Years, as part of
the$1,400 per hearing impaired ear ($2,800 bilateral) total benet. Note: For dependents up
to age 12, ear molds that are Medically Necessary due to growth are paid at 80% of the billed
amount after annual deductible and are not subject to the maximum benet
Home Health Care Services: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Hospice and Palliative Care: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Hospitalization:
Hospital Charges: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Physician, Surgeon and
Consultation Charges:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Human Organ Transplant:
Hospital Charges: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Physician, Surgeon and
Consultation Charges:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Immunizations:
Paid at 100% of the network fee schedule, no annual deductible; per Preventive Health Care
Guidelines found at osuhealthplan.com under Health Plan Tools - Forms and Policies
Infertility Treatment: Refer to the Schedule of Benets for the service being rendered to
nd specic coverage information.
Paid following diagnosis by a network OB/GYN; subject to OSU Health Plan guidelines
(contact OSU Health Plan for details); $15,000 lifetime maximum benet includes any
prescription drugs used for the treatment of infertility; benet applies to an
enrolled employee or spouse; requires Prior Authorization.
1
Laboratory Services:
Inpatient: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Outpatient: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Maternity Services:
Inpatient: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Professional Services: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 46
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 46 of 92
Revised 09/2023
PRIME CARE ADVANTAGE – SCHEDULE OF BENEFITS
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Medical Equipment and Supplies: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required.
Paid at 90% for qualifying diabetic supplies
when participating in the Value-Based
Drug Benet. Eligibility is based on actively
participating in the Care Coordination
Program. Visit Care Coordination at
osuhealthplan.com to learn more.
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required.
Medications – Outpatient: Paid at 80% of network fee schedule
after annual deductible; for injectable/
oral/intravenous (includes chemotherapy)
medications dispensed on an outpatient
(e.g., providers’ ofce) basis
Paid at 70% of network fee schedule
after annual deductible; for injectable/
oral/intravenous (includes chemotherapy)
medications dispensed on an outpatient
(e.g., providers’ ofce) basis
Medications – Specialty: Paid at 80% of network fee schedule after
annual deductible; specialty medications
for certain conditions are not covered under
the Medical Plan, but are covered under the
Prescription Drug Benet. See:
hr.osu.edu/benets/prescription
Paid at 70% of network fee schedule after
annual deductible; specialty medications
for certain conditions are not covered under
the Medical Plan, but are covered under the
Prescription Drug Benet. See:
hr.osu.edu/benets/prescription
Nutritional Services:
Visit 1 – 3: Paid at 100% of network fee schedule no annual deductible
Visit 4 – 6: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Occupational Therapy and Physical
Therapy, Outpatient:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Combined maximum of 45 visits per Plan Year
Ofce Visits
(includes surgical procedures
performed in the ofce)
(excludes lab and x-ray):
Behavioral Health Provider paid at 80% of network fee schedule, no annual deductible
Convenient Care Clinic (includes University Health Connection)
paid at 100% of network fee schedule no annual deductible
Primary Care Provider (PCP) paid at 100% of
network fee schedule no annual deductible
Specialist paid at 80% of network fee
schedule no annual deductible
All other providers paid at 80% of network fee
schedule after annual deductible
Primary Care Provider (PCP) paid at 70% of
network fee schedule after annual deductible.
Specialist paid at 70% of network fee
schedule, after annual deductible
All other providers paid at 70% of network fee
schedule after annual deductible
Outpatient Services:
See descriptions of covered services for Ofce Visits, Behavioral Health, Laboratory Services,
Occupational Therapy, Physical Therapy, Speech Therapy and Surgical Procedures
Physical Therapy and
Occupational Therapy, Outpatient:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Combined maximum of 45 visits per Plan Year
Pre-Admission Testing: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Prescription Drugs:
See the “Prescription Drug Benet” section of this SPD
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 47
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 47 of 92
Revised 09/2023
PRIME CARE ADVANTAGE – SCHEDULE OF BENEFITS
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Preventive Health Care
(Physical Examinations):
Paid at 100% of network fee schedule no annual deductible, includes related laboratory tests,
per Preventive Health Care Guidelines; charts found at osuhealthplan.com
under Health Plan Tools - Forms and Policies
Note: One physical examination per Plan Year provided for adults
Procedures, Outpatient: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Prosthetic Devices: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required.
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required.
Radiology Outpatient
(X-ray Services):
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Speech Therapy, Outpatient: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Limited to 20 visits per Plan Year
Surgery, Outpatient: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Surgical Services, Second Opinion: Paid at 80% of network fee schedule no
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Telehealth Services:
Telehealth/electronic consultations are covered at the same benet level as the location/
specialty of the provider rendering the service and the type of service rendered (e.g., Premier
Network Primary Care Provider paid at 100% of network fee schedule. Standard Network
Primary Care Provider paid at 70% of network fee schedule after annual deductible.)
Temporomandibular Disorder
(TMD):
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Subject to a lifetime maximum of $3,000 for all non-surgical TMD covered services
Tobacco Cessation:
Tobacco cessation services are covered through the Medical Plan. Services are paid at
100% no annual deductible. Over-the-counter nicotine replacement therapy (NRT) and
prescription cessation medications (e.g., Chantix) are paid at 100% through the Prescription
Drug Benets. A prescription must be obtained from a physician or nurse practitioner for all
tobacco cessation products. Free cessation services can be obtained through Health
Coaching at OSU Health Plan (osuhealthplan.com).
Urgent Care Services:
In Ohio:
Paid at 80% of network fee schedule, no annual deductible; limited to network providers
Outside Ohio:
Paid at 80% of network fee schedule no annual deductible; no network restriction.
Weight Management Programs:
Hospital-based/Physician-directed programs and WW (formerly Weight Watchers™)
programs expenses excluded from annual out-of-pocket maximum
Hospital-based/
Physician-directed Program:
50% of reimbursement of approved billed charges no annual deductible
WW (formerly Weight
Watchers™):
50% reimbursement for Core and Premium Programs no annual deductible
Note:
The reimbursement is applied to the month-to-month membership. Membership can be
canceled at any time. For more information, or to join, visit go.osu.edu/weightwatchers.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 48
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 48 of 92
Revised 09/2023
PRIME CARE CHOICE
ELIGIBLE EMPLOYMENT
• University faculty and staff with eligible appointments.
• University afliated group employees with eligible appointments at:
- Central Ohio Technical College (COTC)
- Ohio State University Physicians, Inc. (OSUP)
ENROLLMENT
Refer to the “Enrollment” section of this SPD for details. To enroll in this coverage option, use Workday online at workday.osu.edu or
submit a completed Health Election Form, available at hr.osu.edu/policies-forms under Forms - Health Benets.
Enrollment Changes
Refer to the “Change in Coverage Due to a Qualifying Status Change” section of this SPD.
COVERAGE ACCESS OUTSIDE THE NETWORK AREA
Access to out-of-area coverage is available with special application (online at hr.osu.edu/policies-forms under Forms - Health Benets
-Out-of-Area Election Form) to individuals enrolled in Prime Care Choice who will be outside Ohio for at least 30 consecutive days. If
the Out-of-Area Benet Election Form is received in our ofce within 30 days of the event (i.e., newly benets eligible or the date the
covered person moved outside the network area), Out-of-Area benets will be effective on the event date. If the form is completed
after 30 days of the event, Out-of-Area benets will be effective on the date the form is received in our ofce. The form must be
renewed annually. Contributions will not change. Examples of circumstances to enroll are:
• You have a dependent child who does not live with you and resides outside Ohio
• You have a dependent who attends a college outside Ohio
• You will be outside Ohio on an approved leave of absence or an approved professional leave
• You will be outside Ohio during an off-duty term if you have a nine-month appointment and receive compensation and benets over
a 12-month period.
Note: When traveling outside Ohio or the United States, you have access to Ohio State Travel Assistance services. Refer to the Ohio
State Travel Assistance section of this SPD for details.
CONTRIBUTION
The current contribution rates are available online at hr.osu.edu/benets/rates.
COVERED PERSON’S RESPONSIBILITIES
For the Medical Plan to work effectively, you must follow these procedures, when appropriate:
• Coordinate all medical care with your primary physician.
• Conrm that all providers (physicians, labs, etc.), including those to whom you are referred, are participating statewide network
providers in order to ensure coverage under the Medical Plan.
• Present your medical ID card to the provider before receiving medical services.
• Notify OSU Health Plan if a physician admits you to a hospital.
• Request Prior Authorization for benets before receipt of specic services or elective admission to a hospital or facility.
SPECIAL POINTS TO CONSIDER WHEN USING THIS COVERAGE
When receiving medical services it is important to understand that:
• Some services are fully covered while other services require a deductible, coinsurance or both. When receiving Covered Services
within the network, simply present your medical ID card.
• In order to receive the network-benet level, you must use network providers. There are two networks – Premier and Standard – and
both networks provide payment for Covered Services based on the network provider’s fee schedule. However, you will receive the
highest level of benet coverage if you use a Premier Network provider.
- When seeking network medical care inside Franklin County, the OSU Health Plan network of physicians and facilities must be
used. A current list of network providers is available online at https://osuhealthplan.com/nd-a-provider-search or by contacting
OSU Health Plan at 614-292-4700.
- When seeking medical care outside Franklin County, the Ohio PPO Connect network of physicians and facilities must be used. A
current list of network providers is available online at https://osuhealthplan.com/nd-a-provider-search or by contacting OSU
Health Plan at 614-292-4700.
- If you are traveling outside Ohio or the United States you have access to Ohio State Travel Assistance services. Refer to the “Ohio
State Travel Assistance” section of this SPD for details.
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 49 of 92
Revised 09/2023
PROVIDER SELECTION
A complete list of network providers is available online at https://osuhealthplan.com/nd-a-provider-search, where it is updated
regularly.
Referrals to Specialists
While you may schedule an appointment directly with a network specialist, some specialists may require a referral from your primary
care physician before making an appointment. Your physician should refer you to a specialist within the network, unless the care you
need is not available within the network. If your physician refers you to a provider outside the network, it is your responsibility to obtain
authorization in advance from OSU Health Plan at 614-292-4700. If your authorization is approved, your Covered Services will be paid
according to network benet.
Note: Following emergency or specialist care, you should notify your primary care physician in order to keep him or her informed of
your medical condition.
HOW PAYMENT IS DETERMINED
Refer to the “How Payment is Determined,” “Exclusions or Limitations,” and “Prime Care Choice Network – Schedule of Benets”
sections of this SPD for details.
Network
Payments for Covered Services obtained from a network provider are based upon the network provider’s fee schedule. A member’s
cost share (i.e., coinsurance or deductible) may vary, depending on whether the provider is in the Premier Network or the Standard
Network (each as dened in the “Denitions” Section of this SPD). You are not responsible for any balance in excess of the network
provider’s fee schedule. In other words, Covered Services obtained from network providers are not subject to Balance Billing.
Out-of-Network
Refer to the “Prime Care Choice Out-of-Network” section of this SPD.
Urgent Care
• Payments for covered urgent care services received from network urgent care providers will be based upon the network provider’s
fee schedule. You are not responsible for any balance in excess of the network provider’s fee schedule subject to applicable
deductible and coinsurance.
• Services received from an out-of-network urgent care provider in Ohio will be covered at the out-of-network benet level. A
complete list of network providers is available online at https://osuhealthplan.com/nd-a-provider-search,
• Urgent care received outside of Ohio will be paid at the network benet level.
• Urgent care is not intended for preventive or routine maintenance treatment such as school or annual physicals and will not be
covered when received from an urgent care provider.
PRIME CARE CHOICE
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 50 of 92
Revised 09/2023
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Acupuncture Services and
Chiropractic Care:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Combined maximum benet of $2,000 per Plan Year
Ambulance Services:
Paid at 80% of network fee schedule after annual deductible, when Medically Necessary
Behavioral Health Services:
Prior Authorization
1
required for inpatient and facility-based behavioral health services
Mental Health and Substance
Abuse – Inpatient:
Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Mental Health and Substance
Abuse – Outpatient:
Paid at 80% of network fee schedule after annual deductible
Chiropractic Care and
Acupuncture Services:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Combined maximum benet of $2,000 per Plan Year
Diabetes Education: Paid at 80% of network fee schedule after
annual deductible; no Prior Authorization
Paid at 70% of network fee schedule after
annual deductible; no Prior Authorization
Emergency Room Visits:
Paid at 80% of network fee schedule after annual deductible
Extended Care Facility Services:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Limit of up to 60 days per Plan Year; Prior Authorization
1
required
GYN Examination: One preventive exam per Plan Year paid at
100% of network fee schedule, no annual
deductible; additional diagnostic exams paid
at 80% of network fee schedule, no annual
deductible
One preventive exam per Plan Year paid at
100% of network fee schedule, no annual
deductible; additional diagnostic exams paid
at 70% of network fee schedule after annual
deductible
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
PRIME CARE CHOICE NETWORK – SCHEDULE OF BENEFITS
BENEFIT OPTION PROVISIONS
Annual Deductible:
Individual: $975 per person
Family: $1,950 per family
Prescription Drug Benet: A separate deductible of $50 per person, $100 per family
Annual Out-of-Pocket Maximum: Out-of-Network annual out-of-pocket expenses apply to the Network Annual Out-of-Pocket
Maximum. However, network annual out-of-pocket expenses do not apply to the Out-of-
Network Annual Out-of-Pocket Maximum
Excludes Weight Management Programs and non-Prior Authorization penalty
Individual: $4,350 per person
Family: $8,700 per family
Prescription Drug Benet: A separate limit of $2,500 per person, $5,000 per family applies; see program description
Maximum Benets:
Lifetime: No limit except as noted for specic benets
Infertility:
$15,000 lifetime maximum benet per person, includes prescription drugs used for infertility
treatment
Temporomandibular Disorder (TMD): $3,000 lifetime maximum benet per person for all non-surgical TMD covered services
CONTINUED ON PAGE 51
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 51 of 92
Revised 09/2023
PRIME CARE CHOICE NETWORK – SCHEDULE OF BENEFITS
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Hearing Aids:
Paid at 80% of the billed amount after annual deductible $1,400 per hearing impaired ear
($2,800 bilateral) in total benets; every three (3) Plan Years; no network provider restrictions
Hearing Test (Audiometry):
Covered at 100% per the Preventive Health Care Guidelines found at osuhealthplan.com,
Health Plan Tools - Forms and Policies. Diagnostic exams for hearing loss are covered at
80% (Premier) or 70% (Standard) after deductible.
Ear Molds for Hearing Aids:
Paid at 80% of the billed amount after annual deductible, every three (3) Plan Years,
as part of the$1,400 per hearing impaired ear ($2,800 bilateral) total benet.
Note: For dependents up to age 12, ear molds that are Medically Necessary due to
growth are paid at 80% of the billed amount after annual deductible and are
not subject to the maximum benet
Home Health Care Services: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Hospice and Palliative Care: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Hospitalization:
Hospital Charges: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Physician, Surgeon and
Consultation Charges:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Human Organ Transplant:
Hospital Charges: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required
Physician, Surgeon and
Consultation Charges:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Immunizations:
Paid at 100% of the network fee schedule, no annual deductible; per Preventive Health Care
Guidelines found at osuhealthplan.com under Health Plan Tools - Forms and Policies
Infertility Treatment: Refer to the Schedule of Benets for the service being rendered to
nd specic coverage information.
Paid following diagnosis by a network OB/GYN; subject to OSU Health Plan guidelines
(contact OSU Health Plan for details); $15,000 lifetime maximum benet includes any
prescription drugs used for the treatment of infertility; benet applies to an
enrolled employee or spouse; requires Prior Authorization.
1
Laboratory Services:
Inpatient: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Outpatient: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Maternity Services:
Inpatient: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
required. See “Maternity Services” in
the Covered Services section for more
information.
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
required. See “Maternity Services” in the
Covered Services section for more
information.
Professional Services: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 52
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 52 of 92
Revised 09/2023
PRIME CARE CHOICE NETWORK – SCHEDULE OF BENEFITS
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Medical Equipment and Supplies: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required.
Paid at 90% for qualifying diabetic supplies
when participating in the Value-Based
Drug Benet. Eligibility is based on actively
participating in the Care Coordination
Program. Visit Care Coordination at
osuhealthplan.com to learn more.
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required.
Medications – Outpatient: Paid at 80% of OSU Health Plan fee schedule
after annual deductible for injectable/
oral/intravenous (includes chemotherapy)
medications dispensed on an outpatient (e.g.,
providers’ ofce) basis after annual deductible
Paid at 70% of OSU Health Plan fee schedule
after annual deductible for injectable/
oral/intravenous (includes chemotherapy)
medications dispensed on an outpatient (e.g.,
providers’ ofce) basis after annual deductible
Medications – Specialty: Paid at 80% of network fee schedule after
annual deductible; specialty medications
for certain conditions are not covered under
the Medical Plan, but are covered under the
Prescription Drug Benet. See: hr.osu.edu/
benets/prescription.
Paid at 70% of network fee schedule after
annual deductible; specialty medications
for certain conditions are not covered under
the Medical Plan, but are covered under the
Prescription Drug Benet. See: hr.osu.edu/
benets/prescription.
Nutritional Services:
Visit 1 – 3:
Paid at 100% of network fee schedule no annual deductible
Visit 4 – 6: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Occupational Therapy and Physical
Therapy, Outpatient:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Combined maximum of 45 visits per Plan Year
Ofce Visits
(includes surgical procedures
performed in the ofce)
(excludes lab and X-ray):
Behavioral Health Provider paid at 80% of network fee schedule, after annual deductible
Convenient Care Clinic (includes University Health Connection)
paid at 100% of network fee schedule no annual deductible
Primary Care Provider (PCP) paid at 100% of
network fee schedule, no annual deductible
All other providers paid at 80% of network
fee schedule after annual deductible
Primary Care Provider (PCP) paid at 70% of
network fee schedule after annual deductible
All other providers paid at 70% of network fee
schedule after annual deductible
Outpatient Services:
See descriptions of covered services for Ofce Visits, Behavioral Health, Laboratory Services,
Occupational Therapy, Physical Therapy, Speech Therapy and Surgical Procedures
Physical Therapy and
Occupational Therapy, Outpatient:
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Combined maximum of 45 visits per Plan Year
Pre-Admission Testing: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Prescription Drugs:
See the “Prescription Drug Benet” section of this SPD
Preventive Health Care
(Physical Examinations):
Paid at 100% of network fee schedule no annual deductible, includes related laboratory tests,
per Preventive Health Care Guidelines; charts found at osuhealthplan.com
under Health Plan Tools - Forms and Policies
Note: One physical examination per Plan Year provided for adults
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 53
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 53 of 92
Revised 09/2023
PRIME CARE CHOICE NETWORK – SCHEDULE OF BENEFITS
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Procedures, Outpatient: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Prosthetic Devices: Paid at 80% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required.
Paid at 70% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required.
Radiology (X-ray Services): Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Speech Therapy, Outpatient: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Limited to 20 visits per Plan Year
Surgery, Outpatient: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Surgical Services, Second Opinion: Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Telehealth Services:
Telehealth/electronic consultations are covered at the same benet level as the location/
specialty of the provider rendering the service and the type of service rendered (e.g., Premier
Network Primary Care Provider paid at 100% of network fee schedule. Standard Network
Primary Care Provider paid at 70% of network fee schedule after annual deductible.)
Temporomandibular Disorder
(TMD):
Paid at 80% of network fee schedule after
annual deductible
Paid at 70% of network fee schedule after
annual deductible
Subject to a lifetime maximum of $3,000 for all non-surgical TMD covered services
Tobacco Cessation:
Tobacco cessation services are covered through the Medical Plan. Services are paid at
100% no annual deductible. Over-the-counter nicotine replacement therapy (NRT) and
prescription cessation medications (e.g., Chantix) are paid at 100% through the Prescription
Drug Benets. A prescription must be obtained from a physician or nurse practitioner for all
tobacco cessation products. Free cessation services can be obtained through Health
Coaching at OSU Health Plan (osuhealthplan.com).
Urgent Care Services:
In Ohio:
Paid at 80% of network fee schedule after annual deductible; limited to network providers
Outside Ohio:
Paid at 80% of the Allowed Amount after annual deductible; no network restriction
Weight Management Programs:
Hospital-based/Physician-directed programs and WW (formerly Weight Watchers™)
programs expenses excluded from annual out-of-pocket maximum
Hospital-based/
Physician-directed Program:
50% of reimbursement of approved billed charges no annual deductible
WW (formerly Weight
Watchers™):
50% reimbursement for Core and Premium Programs no annual deductible
Note: The reimbursement is applied to the month-to-month membership. Membership can be
canceled at any time. For more information, or to join, visit go.osu.edu/weightwatchers.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 54
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 54 of 92
Revised 09/2023
COVERED PERSON’S RESPONSIBILITIES:
For the Medical Plan to work effectively, you must follow these procedures when appropriate:
• Present your medical drug ID card before receiving medical care services.
• Notify OSU Health Plan if a physician admits you to a hospital.
• Request Prior Authorization of benets before receipt of specic services or elective admission to a hospital or facility.
SPECIAL POINTS TO CONSIDER WHEN USING THIS COVERAGE:
• You may visit any physician or go to any facility and receive benets for Covered Services.
• When using an out-of-network provider, you may be required to le claims with Trustmark. See the “Submitting Claims” section
below for further details.
• If you are traveling outside Ohio or the United States you have access to Ohio State Travel Assistance services. Refer to the “Ohio
State Travel Assistance” section of this SPD for details.
HOW PAYMENT IS DETERMINED
Refer to the “How Payment is Determined,” “Exclusions or Limitations,” and “Prime Care Choice Out-of-Network – Schedule of
Benets” sections of this SPD for details.
Payment for Covered Services obtained from an out-of-network provider will never exceed the actual charge for any procedure. All
payments will be subject to any applicable deductible, coinsurance, maximum benets and other provisions and limitations outlined
and the Schedule of Benets.
Submitting Claims
If the out-of-network provider does not submit the claim to Trustmark directly, you must submit an itemized bill or completed claim
form to Trustmark yourself. The address for claims submission is on your medical ID card. Claim forms may be obtained by calling
Trustmark or online at hr.osu.edu/policies-forms (under Form - Health Benets - Medical – Trustmark Health Insurance Claim Form), or
by calling HR Connection at 614-247-myHR(6947).
Claims Payment
Out-of-network claims submitted for payment are considered based on the Allowed Amount. (Refer to the “Denitions” section of this
SPD for additional details.)
Note: Any amount you pay over the Allowed Amount does not apply to your annual deductible or out-of-pocket maximum. Refer to
the “Schedule of Benets” and “Covered Services” section of this SPD for details.
PRIME CARE CHOICE OUT-OF-NETWORK
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 55 of 92
Revised 09/2023
PRIME CARE CHOICE OUT-OF-NETWORK – SCHEDULE OF BENE-
PRIME CARE CHOICE OUT-OF-NETWORK – SCHEDULE OF BENEFITS
BENEFIT OPTION PROVISIONS
Annual Deductible:
Individual: $1,900 per person
Family: $3,800 per family
Prescription Drug Benet: A separate deductible of $50 per person, $100 per family
Annual Out-of-Pocket Maximum: Out-of-Network annual out-of-pocket expenses do apply to the Network Annual Out-of-Pocket
Maximum. However, network annual out-of-pocket expenses do not apply to the Out-of-
Network Annual Out-of-Pocket Maximum
Excludes Weight Management Programs and non-Prior Authorization penalty
Individual: $7,500 per person
Family: $15,000 per family
Prescription Drug Benet: A separate limit of $2,500 per person, $5,000 per family applies; see program description
Maximum Benets:
Lifetime: No limit except as noted for specic benets
Infertility:
$15,000 lifetime maximum benet per person, includes prescription drugs used for infertility
treatment
Temporomandibular Disorder (TMD): $3,000 lifetime maximum benet per person for all non-surgical TMD covered services
Acupuncture Services and
Chiropractic Care:
Paid at 60% of the Allowed Amount after annual deductible for up to a combined maximum
benet of $2,000 per Plan Year; subject to balance billing
Ambulance Services: Paid at 80% of the Allowed Amount after network annual deductible, when Medically
Necessary; subject to balance billing. Air ambulance services and ground ambulance service in
Ohio are not subject to balance billing.
Behavioral Health Services: Prior Authorization
1
required for inpatient and facility-based behavioral health services; subject
to balance billing
Mental Health and Substance
Abuse – Inpatient:
Paid at 60% of the Allowed Amount after annual deductible; Prior Authorization
1
required;
subject to balance billing
Mental Health and Substance
Abuse – Outpatient:
Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing
Chiropractic Care and
Acupuncture Services:
Paid at 60% of the Allowed Amount after annual deductible for up to a combined maximum
benet of $2,000 per Plan Year; subject to balance billing
Diabetes Education: Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing; no Prior
Authorization
Emergency Room Visits: Paid at 80% of the Allowed Amount after network annual deductible; not subject to balance
billing
Extended Care Facility Services:
Paid at 60% of the Allowed Amount after annual deductible; limit of up to 60 days per Plan Year;
Prior Authorization
1
required; subject to balance billing
GYN Examination: Paid at 60% of the Allowed Amount after annual deductible and subject to balance billing
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 56
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 56 of 92
Revised 09/2023
PRIME CARE CHOICE OUT-OF-NETWORK – SCHEDULE OF BENEFITS
BENEFIT OPTION PROVISIONS
Hearing Aids: Paid at 80% of the billed amount after network annual deductible for up to $1,400 per hearing
impaired ear ($2,800 bilateral) in total benets; every three (3) Plan Years; subject to balance
billing
Hearing Test (Audiometry): Covered at 60% of Allowed Amount after annual deductible, subject to balance billing, per the
Preventive Health Care Guidelines found at osuhealthplan.com, Health Plan Tools - Forms and
Policies. Diagnostic exams for hearing loss are covered at 60% after deductible.
Ear Molds for Hearing Aids: Paid at 80% of billed amount after network annual deductible, every three (3) Plan Years, as
part of the $1,400 per hearing impaired ear ($2,800 bilateral) total benet
Note: For dependents up to age 12, ear molds Medically Necessary due to growth are paid
at 80% of billed amount after annual deductible and are not subject to the maximum benet;
subject to balance billing
Home Health Care Services: Paid at 60% of the Allowed Amount after annual deductible; Prior Authorization
1
required;
subject to balance billing
Hospice and Palliative Care: Paid at 60% of the Allowed Amount after annual deductible; Prior Authorization
1
required;
subject to balance billing
Hospitalization:
Hospital Charges:
Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing; Prior
Authorization
1
required
Physician, Surgeon and
Consultation Charges:
Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing
Human Organ Transplant:
Hospital Charges:
Paid at 60% of the Allowed Amount fee schedule after annual deductible; Prior Authorization
1
required
Physician, Surgeon and
Consultation Charges:
Paid at 60% of the Allowed Amount fee schedule after annual deductible
Immunizations: Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing; per
Preventive Health Care Guidelines found at osuhealthplan.com under Health Plan Tools -
Forms and Policies
Infertility Treatment: Paid at 60% of the Allowed Amount after annual deductible and following diagnosis by an OB/
GYN; subject to OSU Health Plan guidelines (contact OSU Health Plan for details); $15,000
maximum benet includes any prescription drugs used for the treatment of infertility; subject to
balance billing; benet applies to an enrolled employee or spouse requires Prior Authorization
1
Laboratory Services:
Inpatient:
Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing
Outpatient:
Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing
Maternity Services:
Inpatient:
Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing; Prior
Authorization
1
required
Professional Services:
Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing
Medical Equipment and Supplies: Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing; Prior
Authorization
1
may be required
Medications – Outpatient: Paid at 60% of the Allowed Amount after annual deductible for injectable/oral/intravenous
(includes chemotherapy) medications dispensed on an outpatient (e.g., providers’ ofce) basis
Medications – Specialty: Paid at 60% of the Allowed Amount after annual deductible; specialty medications for certain
conditions are not covered under the Medical Plan, but are covered under the Prescription
Drug Benet. See: hr.osu.edu/benets/prescription
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 57
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 57 of 92
Revised 09/2023
PRIME CARE CHOICE OUT-OF-NETWORK – SCHEDULE OF BENEFITS
BENEFIT OPTION PROVISIONS
Nutritional Services:
Visit 1 - 3:
Paid at 60% of the Allowed Amount after annual deductible, subject to balance billing
Visit 4 - 6:
Paid at 60% of the Allowed Amount after annual deductible, subject to balance billing
Occupational Therapy and Physical
Therapy, Outpatient:
Paid at 60% of the Allowed Amount after annual deductible for up to a combined maximum of
45 visits per Plan Year; subject to balance billing
Ofce Visits
(includes surgical procedures
performed in the ofce):
Paid at 60% of the Allowed Amount, after annual deductible, subject to balance billing
Outpatient Services:
See descriptions of Covered Services for Ofce Visits, Behavioral Health, Laboratory Services,
Occupational Therapy, Physical Therapy, Speech Therapy and Surgical Procedures
Physical Therapy and
Occupational Therapy, Outpatient:
Paid at 60% of the Allowed Amount after annual deductible for up to a combined maximum of
45 visits per Plan Year; subject to balance billing
Pre-Admission Testing: Paid at 60% of the Allowed Amount after annual deductible; subject to balance billin
Prescription Drugs: See the “Prescription Drug Benet” section of this SPD
Preventive Health Care
(Physical Examinations):
Paid at 60% of the Allowed Amount after annual deductible, subject to balance billing,
includes related laboratory tests, per Preventive Health Care Guidelines; charts found at
osuhealthplan.com under Health Plan Tools - Forms and Policies
Note:
One physical examination per Plan Year provided for adults.
Procedures, Outpatient: Paid at 60% of the Allowed Amount after annual deductible
Prosthetic Devices: Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing; Prior
Authorization
1
may be required
Radiology Outpatient
(X-ray Services):
Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing
Speech Therapy, Outpatient: Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing; limited
to 20 visits per Plan Year
Surgery, Outpatient: Paid at 60% of the Allowed Amount after annual deductible
Surgical Services, Second Opinion: Paid at 60% of the Allowed Amount, after annual deductible; subject to balance billing
Telehealth Services: Telehealth/electronic consultations are covered at the same benet level as the location/
specialty of the provider rendering the service and the type of service rendered (e.g., Premier
Network Primary Care Provider (PCP) paid at 100% of network fee schedule. Standard
Network PCP has a $20 copay. Out-of-Network PCP paid at 60% of the Allowed Amount, after
annual deductible; subject to balance billing.)
Temporomandibular Disorder
(TMD):
Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing; subject
to a lifetime maximum of $3,000 for all non-surgical TMD covered services
Tobacco Cessation: Tobacco cessation services are covered through the Medical Plans. Services are paid at
100% of the Allowed Amount no annual deductible. Over-the-counter nicotine replacement
therapy (NRT) and prescription cessation medications (e.g., Chantix) are paid at 100% through
the Prescription Drug Benet. A prescription must be obtained from a physician or nurse
practitioner for all tobacco cessation products. Free cessation services can be obtained through
Health Coaching at OSU Health Plan (osuhealthplan.com).
Urgent Care Services:
In Ohio:
Paid at 60% of the Allowed Amount after annual deductible; subject to balance billing
Outside Ohio: Paid at 80% of the Allowed Amount after annual deductible; subject to balance billing, no
network restriction
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 58
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 58 of 92
Revised 09/2023
PRIME CARE CHOICE OUT-OF-NETWORK – SCHEDULE OF BENEFITS
BENEFIT OPTION PROVISIONS
Weight Management Programs:
Hospital-based/Physician-directed programs and WW (formerly Weight Watchers™)
programs expenses are excluded from annual out-of-pocket maximum
Hospital-based/ Physician-directed
Program:
50% of reimbursement of approved billed charges no annual deductible
WW (formerly Weight
Watchers™):
50% reimbursement for Core and Premium Programs, no annual deductible
Note:
The reimbursement is applied to the month-to-month membership. Membership can be
canceled at any time. For more information, or to join, visit go.osu.edu/weightwatchers.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024
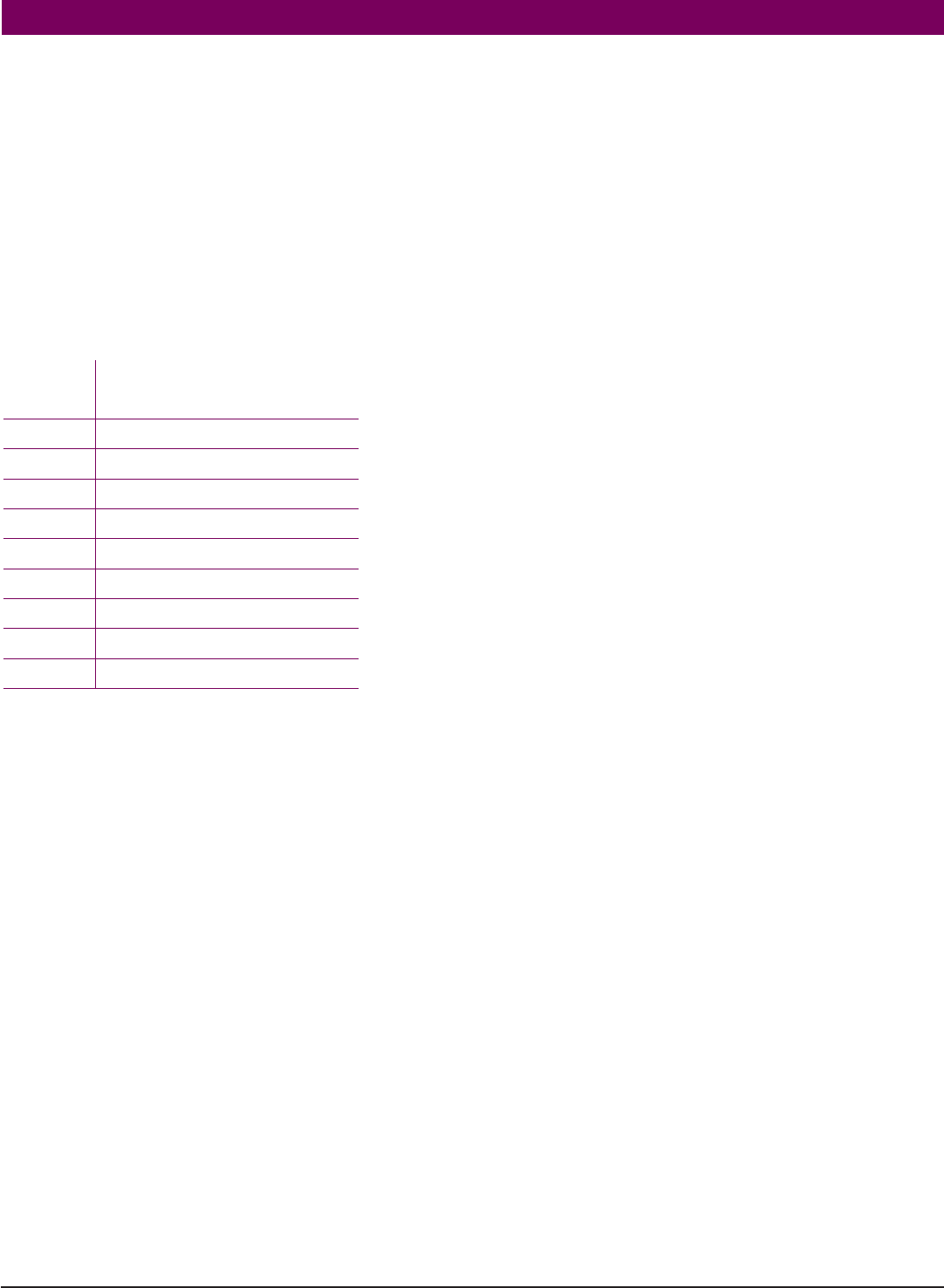
PAGE 59 of 92
Revised 09/2023
PRIME CARE CONNECT
ELIGIBLE EMPLOYMENT
University faculty and staff with eligible appointments (see the “Enrollment” section below).
Note: COTC, OSUP and Graduate Associates are not eligible for this coverage option
ENROLLMENT
To enroll in this coverage option, you must apply during an annual open enrollment period or within 30 days of meeting all of the
following requirements:
• You must be a full-time university employee (75–100% FTE) who is eligible for the full-time medical contribution rate
• You must have a maximum household income level of 225% of the federal poverty level as established annually by the U.S.
Department of Health and Human Services and which was in effect on October 1, 2023. See chart below to determine if you fall
within this level. A change in household income during the Plan Year is not an event that triggers eligibility for enrollment during the
Plan Year. Household income is based on your Adjusted Gross Income (AGI) as indicated on your most recent tax return. If you meet
all of the requirements above and are interested in applying, visit osuhealthplan.com or contact OSU Health Plan at 614-292-4700
or 800-678-6369 to begin the application process. An advocate will perform an initial screening to determine eligibility for Prime
Care Connect coverage and generate an application for you to complete, if requirements are met.
To apply visit ouhealthplan.com or, contact OSU Health Plan at 614-292-4700 or 800-678-6369.
Note: Documentation will be required to conrm household income. Once the application has been submitted and reviewed, an
approval or denial letter will be sent to your home address. To ensure Medical Plan coverage, you are strongly encouraged to enroll in
one of the other coverage options (Prime Care Advantage, Prime Care Choice or Out-of-Area) while waiting to hear if you have been
approved for this coverage.
CHANGE IN ENROLLMENT
Refer to the “Change in Coverage Due to a Qualifying Status Change” section of this SPD for details.
TERMINATION OF COVERAGE
If an event occurs which results in you not meeting all of the enrollment criteria, you must notify OHR and submit a new university
Health Election Form available online at hr.osu.edu/policies-forms (under Forms - Health Benets) within 30 days of the event.
COVERAGE ACCESS OUTSIDE THE NETWORK AREA
Access to out-of-area coverage is available if you permanently reside outside the network area or with special application (online at
hr.osu.edu/policies-forms - see under Forms - Health Benets Out-of-Area Benet Election Form) to individuals enrolled in Prime Care
Connect who will reside outside the network area for at least 30 consecutive days. If the Out-of-Area Benet Election Form is received
in our ofce within 30 days of the event (i.e., newly benets eligible or the date the covered person moved outside the network area),
Out-of-Area network restrictions will not apply effective on the event date. If the form is completed after 30 days of the event, Out-
of-Area network restrictions will not apply effective on the date the form is received in our ofce. The form must be renewed annually.
Contributions will not change. Examples of circumstances to enroll are:
• You have a dependent child who does not live with you and resides outside Ohio
• You have a dependent who attends college outside Ohio
• You will be outside Ohio on an approved leave of absence or an approved professional leave
• You will be outside Ohio during an off-duty term if you have a nine-month appointment and receive compensation and benets over
a 12-month period.
Note: When traveling outside Ohio or the United States, you have access to Ohio State Travel Assistance services. Refer to the “Ohio
State Travel Assistance” section of this SPD for details.
CONTINUED ON PAGE 60
PERSONS
IN FAMILY
MAXIMUM HOUSEHOLD INCOME
BASED ON ADJUSTED GROSS INCOME
(AGI) FROM MOST RECENT TAX RETURN
1 32, 805
2 44,370
3 55,935
4 67,500
5 79,065
6 90,630
7 102,195
8 113,760
9 and up add $11,565 per person
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 60 of 92
Revised 09/2023
COVERED PERSON’S RESPONSIBILITIES
For the Medical Plan to work effectively, you must follow these procedures, when appropriate:
• Coordinate all medical care with your primary physician.
• Conrm that all providers (physicians, labs, etc.), including those to whom you are referred, are network providers in order to ensure
coverage under the Medical Plan.
• Present your medical ID card to the provider before receiving medical services.
• Notify OSU Health Plan if a physician admits you to a hospital.
• Request Prior Authorization of benets before receipt of certain designated services or elective admission to a hospital or facility.
SPECIAL POINTS TO CONSIDER WHEN USING THIS COVERAGE
• When receiving medical services it is important to understand that:
- There are no benets if services are rendered outside the statewide network (except for emergency care services and except
as described above in “Coverage Access Outside Ohio”). There are two networks—Premier and Standard—and both networks
provide payment for Covered Services based on the network provider’s fee schedule. However, you will receive the highest level of
benet coverage if you use a Premier Network provider.
- All medical treatment should be coordinated through your physician.
• Some services are fully covered while other services require a copay or coinsurance. When receiving covered services within the
network, simply present your medical ID card to your medical service provider.
• This coverage option requires the use of a statewide network of providers.
- When seeking medical care inside Franklin County, the OSU Health Plan network of physicians and facilities must be used. A
current list of network providers is available online at osuhealthplan.com/nd-a-provider-search or by contacting OSU Health
Plan.
- When seeking medical care outside Franklin County, the Ohio PPO Connect network of physicians and facilities must be used.
A current list of network providers is available online at osuhealthplan.com/nd-a-provider-search or by contacting OSU Health
Plan.
- If you are traveling outside Ohio or the United States and need travel services, you have access to Ohio State Travel Assistance
services. Refer to the “Ohio State Travel Assistance” section of this SPD for details.
PROVIDER SELECTION
A complete list of network providers is available online at osuhealthplan.com/nd-a-provider-search, where it is updated regularly.
Referrals to Specialists
While you may schedule an appointment directly with a network specialist, some specialists may require a referral from your primary
care physician before making an appointment. Your physician should refer you to a specialist within the network, unless the care you
need is not available within the network. If your physician refers you to a provider outside the network, it is your responsibility to
obtain authorization in advance from OSU Health Plan at 614-292-4700. If your authorization is approved, your medical care covered
services will be paid as determined by the OSU Health Plan.
Note: Following emergency or specialist care, you should notify your primary care physician in order to keep him or her informed of
your medical condition.
HOW PAYMENT IS DETERMINED
Refer to the How Payment is Determined, Exclusions or Limitations and Prime Care Connect – Schedule of Benets sections of this
SPD for details.
Network
Payments for Covered Services are based upon the network provider’s fee schedule. A member’s cost share (i.e., coinsurance, copay,
or deductible) may vary, depending on whether the provider is in the Premier Network or the Standard Network (each as dened in
the “Denitions” section of this SPD). You are not responsible for any balance in excess of the network provider’s fee schedule. In other
words, Covered Services obtained from network providers are not subject to Balance Billing.
Urgent Care
• Payment for covered urgent care services received from network urgent care providers will be based upon the network provider’s fee
schedule. You are not responsible for any balance in excess of the network provider’s fee schedule.
• Urgent care is not intended for preventive or routine maintenance treatment, such as school or annual physicals and these types of
services will not be covered when received from an urgent care provider.
• Services received from an out-of-network urgent care provider in Ohio will not be covered. A complete list of network providers is
available at osuhealthplan.com/nd-a-provider-search, where it is updated regularly.
• Urgent care received outside of Ohio will be paid at the network benet.
PRIME CARE CONNECT
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024
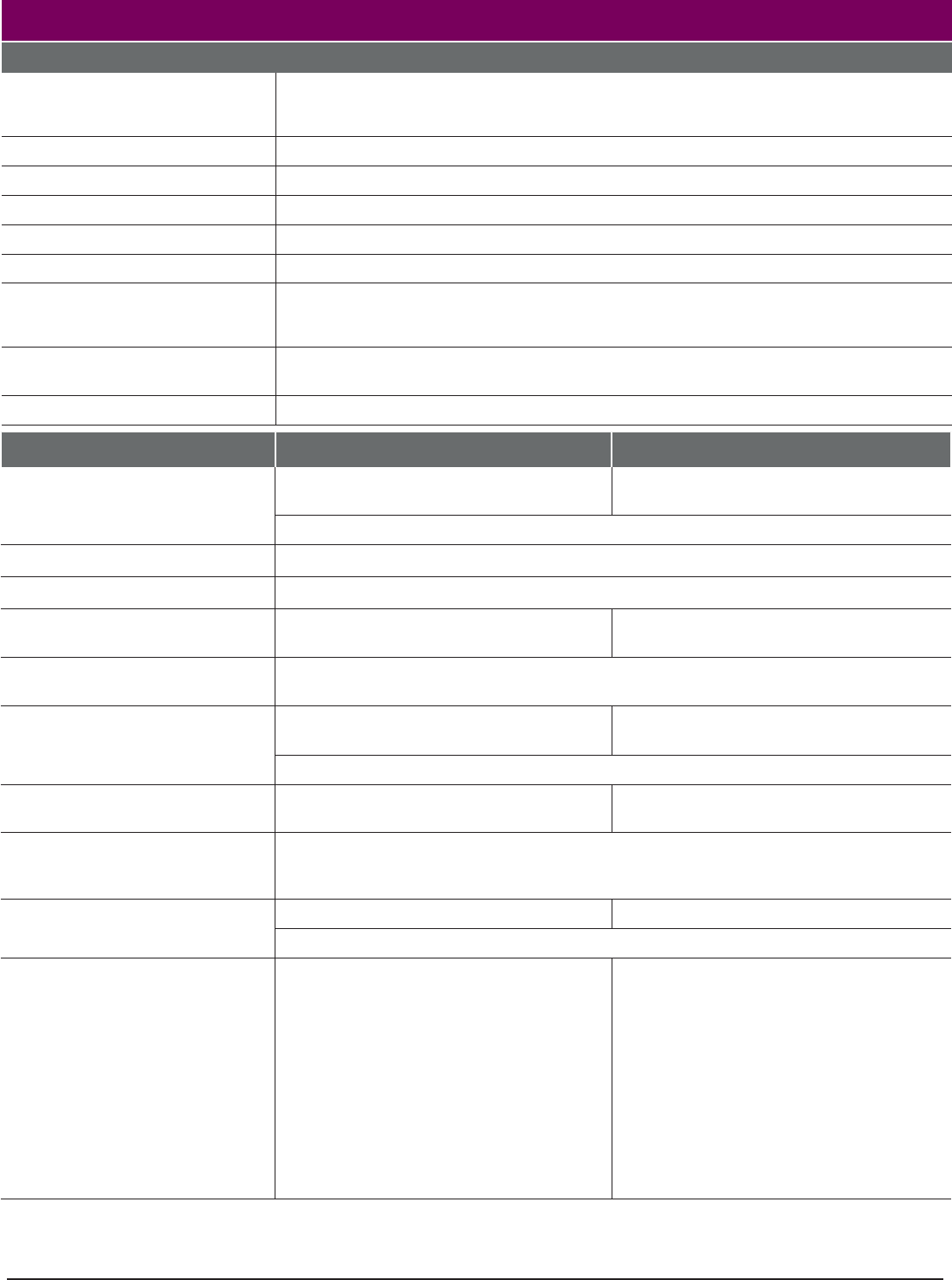
PAGE 61 of 92
Revised 09/2023
PRIME CARE CONNECT – SCHEDULE OF BENEFITS
BENEFIT OPTION PROVISIONS
Annual Deductible:
Individual: $150 per person
Family: $300 per family
Annual Out-of-Pocket Maximum: Excludes Weight Management Programs and non-Prior Authorization penalty
Individual: $1500 per person
Family: $3,000 per family
Prescription Drug Benet: A separate limit of $2,000 per person, $4,000 per family; see program description
Maximum Benets:
Lifetime: No limit, except as noted for specic benets
Infertility:
$15,000 lifetime maximum benet per person, includes prescription drugs used for infertility
treatment
Temporomandibular Disorder (TMD): $3,000 lifetime maximum benet per person for all non-surgical TMD covered services
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Acupuncture Services and
Chiropractic Care:
$20 copay per visit no annual deductible $30 copay per visit no annual deductible
Combined maximum benet of $2,000 per Plan Year
Ambulance Services:
Paid at 100% of network fee schedule no annual deductible when Medically Necessary
Behavioral Health Services:
Prior Authorization
1
required for inpatient and facility-based behavioral health services
Mental Health and Substance
Abuse – Inpatient:
$200 copay per admission
1
; no annual
deductible, Prior Authorization
1
required
$300 copay per admission
1
; no annual
deductible, Prior Authorization
1
required
Mental Health and Substance
Abuse – Outpatient:
Paid at 100% of network fee schedule no annual deductible
Chiropractic Care and
Acupuncture Services:
$20 copay per visit no annual deductible $30 copay per visit no annual deductible
Combined maximum benet of $2,000 per Plan Year
Diabetes Education: Paid at 85% of network fee schedule after
annual deductible; no Prior Authorization
Paid at 75% of network fee schedule after
annual deductible; no Prior Authorization
Emergency Room Visits:
$100 copay per visit no annual deductible
Note: The emergency room copay is waived if the Covered Person is admitted to the hospital
directly from the emergency department. A hospitalization copay will be charged.
Extended Care Facility Services: $50 copay per admission no annual deductible $75 copay per admission no annual deductible
Limit of up to 60 days per Plan Year; Prior Authorization
1
required
GYN Examination: One preventive exam per Plan Year paid at
100% of network fee schedule no annual
deductible; additional diagnostic exams
subject to $20 copay no annual deductible
One preventive exam per Plan Year paid at
100% of network fee schedule no annual
deductible; additional diagnostic exams
subject to $30 copay no annual deductible
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 62
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 62 of 92
Revised 09/2023
PRIME CARE CONNECT – SCHEDULE OF BENEFITS
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Hearing Aids:
Paid at 85% of the billed amount after annual deductible 1,400 per hearing impaired ear
($2,800 bilateral) in total benets; every three (3) Plan Years; no network provider restrictions
Hearing Test (Audiometry):
Covered at 100% per the Preventive Health Care Guidelines found at osuhealthplan.com,
Health Plan Tools - Forms and Policies. Diagnostic exams for hearing loss are
covered at 85% (Premier) or 75% (Standard) after deductible.
Ear Molds for Hearing Aids:
Paid at 85% of the billed amount after annual deductible, every three (3) Plan Years,
as part of the$1,400 per hearing impaired ear ($2,800 bilateral) total benet.
Note: For dependents up to age 12, ear molds that are Medically Necessary
due to growth are paid at 85% of the billed amount after annual deductible and
are not subject to the maximum benet
Home Health Care Services: Paid at 85% of network fee schedule after
annual deductible; Prior Authorization
1
required
Paid at 75% of network fee schedule after
annual deductible; Prior Authorization
1
required
Hospice and Palliative Care:
Paid at 100% of network fee schedule no annual deductible; Prior Authorization
1
required
Hospitalization:
Hospital Charges: $200 copay per admission no annual
deductible; Prior Authorization
1
required
$300 copay per admission no annual
deductible; Prior Authorization
1
required
Physician, Surgeon and
Consultation Charges:
Paid at 100% of network fee schedule no annual deductible
Human Organ Transplant:
Hospital Charges: $200 copay per admission no annual
deductible; Prior Authorization
1
required
$300 copay per admission no annual
deductible; Prior Authorization
1
required
Physician, Surgeon and
Consultation Charges:
Paid at 100% of network fee schedule no annual deductible
Immunizations:
Paid at 100% of network fee schedule no annual deductible; per Preventive Health Care
Guidelines found at osuhealthplan.com under Health Plan Tools - Forms and Policies
Infertility Treatment: Refer to the Schedule of Benets for the service being rendered to
nd specic coverage information.
Paid following diagnosis by a network OB/GYN; subject to OSU Health Plan guidelines
(contact OSU Health Plan for details); $15,000 lifetime maximum benet includes any
prescription drugs used for the treatment of infertility; benet applies to an enrolled
employee or spouse; requires Prior Authorization.
1
Laboratory Services:
Inpatient:
Paid at 100% of network fee schedule no annual deductible
Outpatient: Paid at 85% of network fee schedule no
annual deductible
Paid at 75% of network fee schedule no
annual deductible
Maternity Services:
Inpatient: $200 copay per admission no annual
deductible; Prior Authorization
1
required
$300 copay per admission no annual
deductible; Prior Authorization
1
required
Professional Services:
Paid at 100% of network fee schedule no annual deductible
Medical Equipment and Supplies: Paid at 85% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required.
Paid at 90% for qualifying diabetic supplies
when participating in the Value-Based
Drug Benet. Eligibility is based on actively
participating in the Care Coordination
Program. Visit Care Coordination at
osuhealthplan.com to learn more.
Paid at 75% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 63
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 63 of 92
Revised 09/2023
PRIME CARE CONNECT – SCHEDULE OF BENEFITS
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Medications – Outpatient: Paid at 85% of network fee schedule after
annual deductible for injectable/oral/
intravenous (includes chemotherapy)
medications dispensed on an outpatient
(e.g., providers’ ofce) basis
Paid at 75% of network fee schedule
after annual deductible for injectable/
oral/intravenous (includes chemotherapy)
medications dispensed on an outpatient
(e.g., providers’ ofce) basis
Medications – Specialty: Paid at 85% of network fee schedule after
annual deductible;. Specialty medications
for certain conditions are not covered under
the Medical Plan, but are covered under the
Prescription Drug Benet. See: hr.osu.edu/
benets/prescription
Paid at 75% of network fee schedule after
annual deductible;. Specialty medications
for certain conditions are not covered under
the Medical Plan, but are covered under the
Prescription Drug Benet. See: hr.osu.edu/
benets/prescription
Nutritional Services:
Visit 1 – 3:
Paid at 100% of network fee schedule no annual deductible
Visit 4 – 6: $20 copay per visit no annual deductible $30 copay per visit no annual deductible
Occupational Therapy and Physical
Therapy, Outpatient:
$20 copay per visit no annual deductible $30 copay per visit no annual deductible
Combined maximum of 45 visits per Plan Year
Ofce Visits
(includes surgical procedures
performed in the ofce)
(excludes lab and X-ray):
Behavioral Health Provider paid at 100% of network fee schedule, no annual deductible
Convenient Care Clinic (includes University Health Connection) paid at
100% of network fee schedule no annual deductible
Primary Care Provider (PCP) paid at 100% of
network fee schedule no annual deductible.
All other providers - $20 copay per visit no
annual deductible
Primary Care Provider (PCP) - $20 copay per
visit no annual deductible.
All other providers - $30 copay per visit no
annual deductible
Outpatient Services:
See descriptions of covered services for Ofce Visits, Behavioral Health, Laboratory Services,
Occupational Therapy, Physical Therapy, Speech Therapy and Surgical Procedures
Physical Therapy and
Occupational Therapy, Outpatient:
$20 copay per visit no annual deductible $30 copay per visit no annual deductible
Combined maximum of 45 visits per Plan Year
Pre-Admission Testing: Paid at 85% of network fee schedule no
annual deductible
Paid at 75% of network fee schedule no
annual deductible
Prescription Drugs:
See the “Prescription Drug Benet” section of this SPD
Preventive Health Care
(Physical Examinations):
Paid at 100% of network fee schedule no annual deductible, includes related
laboratory tests, per Preventive Health Care Guidelines; charts found at
osuhealthplan.com under Health Plan Tools - Forms and Policies
Note: One physical examination per Plan Year provided for adults
Procedures, Outpatient: $100 copay per procedure no annual
deductible; copay applies to all outpatient
procedures
$150 copay per procedure no annual
deductible; copay applies to all outpatient
procedures
Prosthetic Devices: Paid at 85% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required
Paid at 75% of network fee schedule after
annual deductible; Prior Authorization
1
may be
required
Radiology (X-ray Services): Paid at 85% of network fee schedule no
annual deductible
Paid at 75% of network fee schedule no
annual deductible
Speech Therapy, Outpatient: $20 copay per visit no annual deductible $30 copay per visit no annual deductible
Limited to 20 visits per Plan Year
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 64
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 64 of 92
Revised 09/2023
PRIME CARE CONNECT – SCHEDULE OF BENEFITS
COVERED SERVICES
PREMIER NETWORK
STANDARD NETWORK
Surgery, Outpatient: $100 copay per visit no annual deductible $150 copay per visit no annual deductible
Surgical Services, Second Opinion: $20 copay per visit no annual deductible $30 copay per visit no annual deductible
Telehealth Services:
Telehealth/electronic consultations are covered at the same benet level as the
location/specialty of the provider rendering the service and the type of service rendered
(e.g., Premier Network Primary Care Provider (PCP) paid at 100% of network fee schedule.
Standard Network PCP has a $20 copay.)
Temporomandibular Disorder
(TMD):
Paid at 85% of network fee schedule after
annual deductible
Paid at 75% of network fee schedule after
annual deductible
Subject to a lifetime maximum of $3,000 for all non-surgical TMD covered services
Tobacco Cessation:
Tobacco cessation services are covered through the Medical Plan. Services are paid at
100% no annual deductible. Over-the-counter nicotine replacement therapy (NRT) and
prescription cessation medications (e.g., Chantix) are paid at 100% through the Prescription
Drug Benets. A prescription must be obtained from a physician or nurse practitioner for all
tobacco cessation products. Free cessation services can be obtained through Health
Coaching at OSU Health Plan (osuhealthplan.com).
Urgent Care Services:
In Ohio:
$35 copay per visit no annual deductible; limited to network providers
Outside Ohio:
$35 copay per visit no annual deductible; no network restriction
Weight Management Programs:
Hospital-based/Physician-directed programs and WW (formerly Weight Watchers™)
programs expenses excluded from annual out-of-pocket maximum
Hospital-based/
Physician-directed Program:
50% of reimbursement of approved billed charges no annual deductible
WW (formerly Weight
Watchers™):
50% reimbursement for Core and Premium Programs no annual deductible
Note: The reimbursement is applied to the month- to-month membership. Membership can be
canceled at any time. For more information, or to join, visit go.osu.edu/weightwatchers.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 65 of 92
Revised 09/2023
ELIGIBLE EMPLOYMENT
• University faculty and staff with eligible appointments.
• University afliated group employees with eligible appointments at:
- Central Ohio Technical College (COTC)
- Ohio State University Physicians, Inc. (OSUP)
ELIGIBLE ZIP CODES
Enrollment in this coverage option is only available to:
• Any eligible employee who lives in a qualifying Ohio zip code
• Any eligible employee living outside the state of Ohio
Note: To determine if you live in a qualifying Ohio zip code, go to the Eligibility by Zip Code at hr.osu.edu/benets/medical (see
Eligibility by Zip Code).
ENROLLMENT
Refer to the “Enrollment” section of this SPD for details. To enroll in this coverage option, use Workday online at workday.osu.edu or
submit a completed Health Election Form, available at hr.osu.edu/policies-forms.
Enrollment Changes
Refer to the “Change in Coverage Due to a Qualifying Status Change” section of this SPD.
CONTRIBUTION
The current contribution rates are available online at hr.osu.edu/benets/rates.
COVERED PERSON’S RESPONSIBILITIES
For the Medical Plan to work effectively, you must follow these procedures, when appropriate:
• Present your medical ID card before receiving medical care services.
• Notify OSU Health Plan if a physician admits you to a hospital.
• Request Prior Authorization
1
of benets before receipt of designated services or elective admission to a hospital or facility.
Note:
You are encouraged to coordinate all medical care with your primary care physician.
SPECIAL POINTS TO CONSIDER WHEN USING THIS COVERAGE
• You may visit any physician or go to any facility and receive benets for Covered Services; however, you may need to pay the costs
for the Covered Services you receive then submit a claim for reimbursement. See the Submitting Claims section below for more
details.
Note: When you are traveling outside Ohio or the United States, you have access to Ohio State Travel Assistance services. Refer to
the Ohio State Travel Assistance section of this SPD for details.
HOW PAYMENT IS DETERMINED
Refer to the “How Payment is Determined,” “Exclusions or Limitations” and “Out-of-Area – Schedule of Benets” sections of this SPD
for details.
Payment for Covered Services will never exceed the actual charge for any procedure. All payments will be subject to any applicable
deductible and/or coinsurance, maximum benet amounts and other provisions and limitations outlined in the Schedule of Benets.
Submitting Claims
If the provider does not submit the claim to Trustmark directly, you must submit an itemized bill or completed claim form to Trustmark
yourself. The address for claims submission is on your medical ID card and the inside front cover. Claim forms may be obtained by
calling Trustmark, or online at hr.osu.edu/policies-forms (see Trustmark Health Insurance Claim Form under the Forms tab – Health
Benets) or by calling HR Connection at 614-247-myHR(6947).
Claims Payment and Balance Billing
Claims submitted for payment are considered based on the Allowed Amount and subject to Balance Billing unless stated otherwise in
this SPD. See “Emergency Services Received from an Out-of-Network Provider” in the “How Payment is Determined” section of this
SPD for details about when a provider cannot balance bill you.
Note: If your claim is subject to balance billing, the amount that is balance billed will be applied to your annual out-of-pocket
maximum.
OUT-OF-AREA
CONTINUED ON PAGE 66
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 66 of 92
Revised 09/2023
CONTINUED ON PAGE 67
OUT-OF-AREA PLAN – SCHEDULE OF BENEFITS
BENEFIT OPTION PROVISIONS
Annual Deductible:
Individual: $550 per person
Family: $1,100 per family
Prescription Drug Benet: A separate deductible of $50 per person, $100 per family
Annual Out-of-Pocket Maximum: Excludes Weight Management Programs and non-Prior Authorization penalty
Individual: $3,000 per person
Family: $6,000 per family
Prescription Drug Benet: A separate limit of $2,500 per person, $5,000 per family applies; see program description
Maximum Benets:
Lifetime: No limit, except as noted for specic benets
Infertility:
$15,000 lifetime maximum benet per person, includes prescription drugs used for infertility
treatment
Temporomandibular Disorder (TMD): $3,000 lifetime maximum benet per person for all non-surgical TMD covered services
COVERED SERVICES
Acupuncture Services and
Chiropractic Care:
Paid at 80% of the Allowed Amount after annual deductible for up to a combined maximum
benet of $2,000 per Plan Year; subject to balance billing
Ambulance Services: Paid at 80% of the Allowed Amount after network annual deductible, when Medically
Necessary; subject to balance billing. Air ambulance services and ground ambulance service in
Ohio are not subject to balance billing.
Behavioral Health Services:
Prior Authorization
1
required for inpatient and facility-based behavioral health services
Inpatient:
Paid at 80% of the Allowed Amount
1
after annual deductible; Prior Authorization
1
required
Outpatient: Paid at 80% of the Allowed Amount after annual deductible, subject to balance billing
Chiropractic Care and
Acupuncture Services:
Paid at 80% of the Allowed Amount after annual deductible for up to a combined maximum
benet of $2,000 per Plan Year; subject to balance billing
Diabetes Education: Paid at 80% of the Allowed Amount after annual deductible; subject to balance billing; no Prior
Authorization
Emergency Room Visits:
Paid at 80% of the Allowed Amount after annual deductible; not subject to balance billing
Extended Care Facility Services: Paid at 80% of the Allowed Amount after annual deductible; limit of up to 60 days per Plan Year;
Prior Authorization
1
required; subject to balance billing
GYN Examination: One preventive exam per Plan Year paid at 100% of the Allowed Amount, no annual deductible
additional diagnostic exams paid at 80% of the Allowed Amount after annual deductible;
subject to balance billing
Hearing Aids: Paid at 80% of billed amount after annual deductible for up to $1,400 per hearing impaired ear
($2,800 bilateral) in total benets; every three (3) Plan Years
Hearing Test (Audiometry): Covered at 100% per the Preventive Health Care Guidelines found at osuhealthplan.com,
Health Plan Tools - Forms and Policies. Diagnostic exams for hearing loss are covered at 80%
after deductible.
Ear Molds for Hearing Aids: Paid at 80% of the billed amount after annual deductible every three (3) Plan Years, as part of
the $1,400 per hearing impaired ear ($2,800 bilaterial) total benet
Note: For dependents up to age 12, ear molds that are Medically Necessary due to growth are
paid at 80% of the billed amount after annual deductible, and are not subject to the maximum
benet.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 67 of 92
Revised 09/2023
OUT-OF-AREA PLAN – SCHEDULE OF BENEFITS
BENEFIT OPTION PROVISIONS
Home Health Care Services: Paid at 80% of the Allowed Amount after annual deductible; Prior Authorization
1
required;
subject to balance billing
Hospice and Palliative Care: Paid at 80% of the Allowed Amount after annual deductible; Prior Authorization
1
required;
subject to balance billing
Hospitalization:
Hospital Charges:
Paid at 80% of the Allowed Amount after annual deductible; Prior Authorization
1
required
Physician, Surgeon and
Consultation Charges:
Paid at 80% of the Allowed Amount after annual deductible, subject to balance billing
Human Organ Transplant:
Hospital Charges:
Paid at 80% of the Allowed Amount after annual deductible; Prior Authorization
1
required
Physician, Surgeon and
Consultation Charges:
Paid at 80% of the Allowed Amount after annual deductible
Immunizations: Paid at 100% of the Allowed Amount no annual deductible; per Preventive Health Care
Guidelines found at osuhealthplan.com under Health Plan Tools - Forms and Policies
Infertility Treatment: Paid at 80% of the Allowed Amount after annual deductible and following diagnosis by an OB/
GYN; subject to OSU Health Plan guidelines (contact OSU Health Plan for details); $15,000
lifetime maximum benet includes any prescription drugs used for the treatment of infertility;
benet applies to an enrolled employee or spouse; subject to balance billing; requires Prior
Authorization
1
.
Laboratory Services: Paid at 80% of the Allowed Amount after annual deductible, subject to balance billing
Maternity Services:
Inpatient:
Paid at 80% of the Allowed Amount after annual deductible, subject to balance billing; Prior
Authorization
1
required
Professional Services:
Paid at 80% of the Allowed Amount after annual deductible, subject to balance billing
Medical Equipment and Supplies: Paid at 80% of the Allowed Amount after annual deductible; Prior Authorization
1
may be
required
Paid at 90% for qualifying diabetic supplies when participating in the Value-Based Drug
Benet. Visit Care Coordination online at osuhealthplan.com under Programs and Services to
learn more.
Medications – Outpatient: Paid at 80% of the Allowed Amount after annual deductible for injectable/oral/intravenous
(includes chemotherapy) medications dispensed on an outpatient (e.g., providers’ ofce) basis
Medications – Specialty: Paid at 80% of the Allowed Amount after annual deductible, subject to balance billing.
Specialty medications for certain conditions are not covered under the Medical Plans, but are
covered under the Prescription Drug Benet. See: hr.osu.edu/benets/prescription
Nutritional Services:
Visit 1 - 3:
Paid at 100% of the Allowed Amount, no annual deductible, subject to balance billing
Visit 4 - 6:
Paid at 80% of the Allowed Amount after annual deductible, subject to balance billing
Occupational Therapy and Physical
Therapy, Outpatient:
Paid at 80% of the Allowed Amount after annual deductible for up to a combined maximum of
45 visits per Plan Year, subject to balance billing
Ofce Visits
(includes surgical procedures
performed in the ofce):
• Primary Care Provider (PCP) paid at 100% of the Allowed Amount no annual deductible.
A PCP is a generalist physician who is designated as a family medicine, general internal
medicine, geriatric medicine or general pediatrics provider. Primary care services can also be
provided by a Primary Care Nurse Practitioner who practices with a PCP, and Convenient
Care Clinics.
• All other practitioners paid at 80% of the Allowed Amount after annual deductible for all
other visits, subject to balance billing
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
CONTINUED ON PAGE 68
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 68 of 92
Revised 09/2023
OUT-OF-AREA PLAN – SCHEDULE OF BENEFITS
BENEFIT OPTION PROVISIONS
Outpatient Services: See descriptions of Covered Services for Ofce Visits, Behavioral Health, Laboratory Services,
Occupational Therapy, Physical Therapy, Speech Therapy and Surgical Procedures
Physical Therapy and
Occupational Therapy, Outpatient:
Paid at 80% of the Allowed Amount after annual deductible for up to a combined maximum of
45 visits per Plan Year; subject to balance billing
Pre-Admission Testing:
Paid at 80% of the Allowed Amount after annual deductible; subject to balance billing
Prescription Drugs:
See the “Prescription Drug Benet” section of this SPD
Preventive Health Care
(Physical Examinations):
Paid at 100% of the Allowed Amount no annual deductible, includes related laboratory tests,
per Preventive Health Care Guidelines; charts found at osuhealthplan.com under Health Plan
Tools - Forms and Policies
Note:
One physical examination per Plan Year provided for adults.
Procedures, Outpatient:
Paid at 80% of the Allowed Amount after annual deductible, subject to balance billing
Prosthetic Devices:
Paid at 80% of the Allowed Amount after annual deductible,
Prior Authorization
1
may be
required
, subject to balance billing
Radiology(X-ray Services):
Paid at 80% of the Allowed Amount after annual deductible, subject to balance billing
Speech Therapy, Outpatient:
Paid at 80% of the Allowed Amount after annual deductible; subject to balance billing; limited
to 20 visits per Plan Year
Surgery, Outpatient:
Paid at 80% of the Allowed Amount after annual deductible, subject to balance billing
Surgical Services, Second Opinion:
Paid at 80% of the Allowed Amount after annual deductible, subject to balance billing
Temporomandibular Disorder
(TMD):
Paid at 80% of the Allowed Amount after annual deductible; subject to a maximum of $3,000
for all non-surgical TMD covered services; subject to balance billing
Tobacco Cessation:
Tobacco cessation services are covered through the Medical Plans. Services are paid at
100% of the Allowed Amount no annual deductible. Over-the-counter nicotine replacement
therapy (NRT) and prescription cessation medications (e.g., Chantix) are paid at 100% through
the Prescription Drug Benet. A prescription must be obtained from a physician or nurse
practitioner for all tobacco cessation products. Free cessation services can be obtained through
Health Coaching at OSU Health Plan (osuhealthplan.com).
Urgent Care Services:
Paid at 80% of the Allowed Amount after annual deductible; subject to balance billing
Weight Management Programs:
Hospital-based/Physician-directed programs and WW (formerly Weight Watchers™) programs
expenses are excluded from annual out-of-pocket maximum
Hospital-based/ Physician-directed
Program:
50% reimbursement of approved billed charges, no annual deductible,
to a combined maximum benet of $1,000 per Plan Year
WW (formerly Weight
Watchers™):
50% reimbursement for Core and Premium Programs, no annual deductible
Note: The reimbursement is applied to the month-to-month membership. Membership can be
canceled at any time. For more information, or to join, visit go.osu.edu/weightwatchers.
1 Prior Authorization (see Medical Prior Authorization Guide available online at osuhealthplan.com under Health Plan Tools - Forms and Policies) of
certain designated services is required to determine Medical Necessity. If Prior Authorization, where indicated, is not obtained from OSU Health Plan,
claims for these services may be denied or a penalty applied consisting of 20% of the fee, up to $1,000 per admission or service. Prior Authorization
penalties do not apply toward the annual deductible or annual out-of-pocket maximum.
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 69 of 92
Revised 09/2023
HEALTH REIMBURSEMENT ACCOUNT (HRA)
A Health Reimbursement Account (HRA) is an employer-funded account that can be used to reimburse eligible health care expenses
(as dened below). Faculty, staff and spouses who are enrolled in the Medical Plan are eligible to earn credits to an HRA.
The HRA program is intended to qualify as a health reimbursement arrangement under Section 105 of the Code and will be
interpreted in a manner consistent with such Code section and the Treasury regulations thereunder. Employees are not permitted
to make contributions to an HRA. Unless required by law, the benets under this HRA are not assignable, alienable or subject to
attachment, execution, garnishment, operation of bankruptcy or insolvency laws, or other legal or equitable process, either voluntarily
or involuntarily.
HealthEquity/WageWorks is the university’s third-party administrator for the HRA.
ELIGIBILITY FOR PARTICIPATION
Faculty, staff and spouses who are enrolled in the Ohio State Medical Plan are eligible to receive credits each calendar quarter
under the HRA by completing wellness activities as part of the Your Plan for Health (YP4H) Incentive Program. Enrolled dependent
children and any enrollee under the age of 18 are not eligible to participate in the HRA. To learn more visit yp4h.osu.edu under
Rewards. HRA Credits will be earned as follows:
REASONABLE ALTERNATIVE STANDARD
Rewards for participating in YP4H may be earned by benets-eligible employees and enrolled spouses. If you think you might be
unable to meet a standard for a reward under YP4H, you may qualify for an opportunity to earn the same reward by different means.
Contact YP4H by emailing [email protected] and YP4H will work with you (and, if you wish, your doctor) to nd a wellness activity with
the same reward that is right for you in light of your health status.
AVAILABILITY OF FUNDS
• Once funds are credited to an employee’s HRA, the employee can submit claims for reimbursement of eligible health care expenses
(as dened below) from the HRA.
• HRA credits may be used to reimburse eligible health care expenses incurred at any time during the Plan Year on or after the
employee’s effective date of participation in the Medical Plan.
• Reimbursements from an HRA will be limited to the then current balance in the HRA.
• The deadline to submit claims for eligible health care expenses incurred during a Plan Year is March 31 of the following Plan Year.
Unused HRA funds will roll over to the next year as long as you are an Ohio State employee carrying a medical plan under The Ohio
State University Faculty and Staff Health Plans (the “Plan”) or medical coverage through COBRA at that time. Beginning in 2023,
the maximum allowable amount of accumulated contributions in your HRA will be $3,900. Any funds over the maximum allowable
amount will be forfeited.
ORDERING OF ACCOUNT REIMBURSEMENTS (HRA and Health Care Flexible Spending Account)
The HRA and the Health Care Flexible Spending Account (HCFSA) offered by the university are separate accounts. Refer to the Flexible
Spending Accounts Specic Plan Details Document for additional details on the HCFSA. An eligible employee may participate in both
an HRA and an HCFSA, subject to the following terms:
• If an incurred health care expense could be reimbursed from either the HCFSA or the HRA, the reimbursement will be paid from the
HCFSA rst.
• All HCFSA funds must be exhausted before HRA funds are used.
Note: If you are a COTC or OSUP employee, contact your benets ofce with questions related to their administration of the ordering
rule.
CONTINUED ON PAGE 70
ACTIVITY LEVELS INCENTIVE
HRA CREDIT AMOUNTS FOR
ENROLLED FACULTY/STAFF & SPOUSE
Achieve Level 1 (2,500 points) Quarterly Reward $10 HRA credit
Achieve Level 2 (5,000 points) Quarterly Reward $20 HRA credit
Achieve Level 3 (10,000 points) Quarterly Reward $30 HRA credit
Achieve Level 4 (25,000 points) Quarterly Reward $40 HRA credit
Complete 2 qualifying activities Bonus $100 HRA credit
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 70 of 92
Revised 09/2023
ACCOUNT ACCESS
• Online Access: You can access your HRA online 24 hours a day, seven days a week. From your online account, you can check your
account balance, track expenses, le a manual claim and set up communication preferences. To access your account, see Helpful
Links at hr.osu.edu/benets/hra.
• EZ Receipts mobile app: With the mobile app, you can manage your account, securely check real-time balances, request a
reimbursement, view transaction details and use your mobile device’s camera to take a picture of any receipt. The EZ Receipts mobile
app is a free download from the Apple App Store and Google Play. To download the mobile app go to the Apple App Store or Google
Play, and search for the EZ Receipts app.
• Call HealthEquity Customer Support at 1-877-924-3967.
USING HRA FUNDS
• If you or a dependent enrolled in your medical coverage incur an eligible health care expense (as dened below), you may be
reimbursed from your HRA by:
- Using your HealthEquity Health Care debit card:
- Present your HealthEquity Health Care card at the point-of-service to directly access your HRA funds when paying for eligible
expenses for you and your eligible dependents. You should retain your receipts for the expenses that you pay for with your
HealthEquity Health Care card, as you are required to substantiate those expenses. If documentation for expenses is requested
and you do not supply documentation upon that request, the expenses will be considered ineligible and you will have to repay
that expense to your HRA. In such case, your HeathEquity Health Care card will be inactive until your account is reimbursed.
- Filling out a HealthEquity Reimbursement Form available online at hr.osu.edu/benets/hra.
- Filing a claim online: to access your account, see Helpful Links at hr.osu.edu/benets/hra. Scan and upload appropriate receipts.
- Filing a claim using the HealthEquity mobile app and using your mobile device to take a photo of appropriate receipts.
As described above, reimbursement from the HRA will occur only after all funds in your HCFSA have been exhausted.
• When ling a claim along with appropriate documentation, you can choose to:
1. “Pay My Provider” and checks will be sent in accordance with payment guidelines or
2. “Pay Me Back” and reimbursement will be made via direct deposit or check. Most claims are processed within one or two
business days after they are received, and payments are sent shortly thereafter.
• Eligible health care expenses for which you are requesting reimbursement must be incurred during the Plan Year, subject to your
eligibility to participate in the HRA.
Important: An eligible health care expense must be incurred before you can be reimbursed from your HRA. You “incur” expenses when
the services giving rise to the claimed expense are rendered, rather than when you are billed or pay for the services.
ELIGIBLE HEALTH CARE EXPENSES
For detailed explanations of these expenses, or for additional information regarding eligible health care expenses, you should review
the list online at hr.osu.edu/benets/hra.
IMPORTANT DATES AND DEADLINES
HRA Plan Year 2024, subject to your eligibility to participate in the HRA:
• Plan Year January 1 – December 31, 2024
• HRA funds will be credited to your account during the Plan Year in which they are earned.
• Incurred Date Window January 1, 2024 – December 31, 2024
- You may use funds in your 2024 HRA for eligible health care expenses if incurred in 2024 by yourself or an eligible dependent
enrolled in the Medical Plan on the date the service was incurred.
• Reimbursement Period January 1, 2024 – March 31, 2025
- You may request reimbursement for eligible health care expenses incurred in 2024 during the reimbursement period. All requests
for reimbursements must be received by HealthEquity no later than March 31, 2025.
• Rollover Period January 1, 2025 – Mid-April, 2025
- During the rollover period HRA funds for 2025 expenses will not be available. By mid-April, 2025, any remaining 2024 HRA funds
(up to the $3,900 maximum) will rollover to your 2025 HRA account, as long as you are a Covered Employee under the Medical
Plan or an employee who has continuation of coverage under COBRA at the time HRA balances are rolled over. You will then have
access to the 2024 rollover funds and any funds credited for 2025. Eligible expenses incurred in 2025 cannot be reimbursed from
the HRA until the prior year’s rollover has occurred and all HCFSA funds have been exhausted.
TERMINATION OF PARTICIPATION
Your account will terminate on the earlier of the following dates:
1. The date on which your coverage under the Medical Plan terminates, unless you elect COBRA continuation coverage.
2. The date on which the HRA program terminates.
HRA balances are not eligible to be transferred to another HRA account, they must remain in the HRA account under which they were
earned. This includes individuals who move from Ohio State medical plan as an employee to another Ohio State medical plan as a
dependent.
CONTINUED ON PAGE 71
HEALTH REIMBURSEMENT ACCOUNT (HRA)
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 71 of 92
Revised 09/2023
CONTINUING HRA PARTICIPATION UNDER COBRA
Even if you are no longer eligible to participate in the HRA, you can continue to access and earn HRA credits for a limited time under
a federal law known as COBRA (Consolidated Omnibus Budget Reconciliation Act). In order to be eligible for COBRA continuation
coverage, you must elect to continue your Medical Plan coverage under COBRA. Refer to the “Coverage Continuation” section of this
SPD for details.
APPEALING A DENIED CLAIM
If you feel your claim was denied in error, you have the right to le an appeal by writing a letter that explains why you believe the claim
should be approved.
Your appeal may be submitted in writing and mailed to:
HealthEquity Claims Appeal Board
PO Box 14034
Lexington, KY 40512
Or, your appeal may be faxed to:
Fax Number: 1-877-220-3248
Your appeal must be received within 180 days of the date you receive the notice of your claim being denied.
You are welcome to submit additional information related to your claim along with your appeal, such as written comments, documents,
records, a letter from your health practitioner indicating medical necessity of the denied product or service, and any other information
you feel will support your claim.
You can request copies of all documents and information related to your denied claim. These will be provided at no charge.
APPEAL REVIEW PROCESS
Your appeal will be reviewed by a person who was not involved with the initial claim denial and who is not a subordinate of any person
who was.
The review will be a fresh look at your claim and appeal without deference to the initial denial and will take into account all information
submitted with your claim and/or appeal.
You will be notied of the decision regarding your appeal in writing by HealthEquity within 30 days of receipt of your written appeal.
AMENDMENT OR TERMINATION OF THE HRA PROGRAM
The university unilaterally reserves the right to amend, modify or terminate the HRA program at any time and for any reason or no
reason. Any termination will be done without prejudice to claims incurred prior to the termination date.
HEALTH REIMBURSEMENT ACCOUNT (HRA)
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 72 of 92
Revised 09/2023
DEFINITIONS
Aggregate Health Information
Information that may be individually identiable health information that:
• Summarizes claim history, claim expenses, or types of claim experienced by individuals for whom the university has provided health
benets under a group medical plan; and
• From which all identiers described above have been deleted. Geographic information need only be aggregated to a ve digit zip
code level.
Alcoholism Treatment Facility
A facility primarily engaged in the treatment of alcoholism or drug addiction. The facility must have in effect plans for utilization and
peer review and programs for rehabilitation or rehabilitation and detoxication of alcoholism. The facility must also be approved,
licensed and certied by the appropriate regulatory authority.
Allowed Amount
The amount paid for a medical service in a geographic area based on what providers in the area usually accept for the same or similar
medical service. The Allowed Amount sometimes is used to determine the eligible expense.
• For out-of-network providers, the Allowed Amount is the fee most frequently accepted for a similar service or medical procedure by
most similarly qualied physicians or other medical care providers in the particular geographic area where the service is rendered or
a fee that has been negotiated with the provider.
• The database used to establish the Allowed Amount is updated on a regular basis, at least annually.
• When a charge is submitted to Trustmark on behalf of the university for reimbursement of a Covered Service, payment will be made
for the charge or the Allowed Amount, whichever is less, subject to any applicable coinsurance amounts and other provisions or
limitations.
• Unusual circumstances which reasonably require additional time, skill or experience for a provider’s service are taken into
consideration and may result in reimbursement of an amount above the normal Allowed Amount but not exceeding the actual
charge.
Ambulatory Health Facility
A facility or distinct part of one that provides services on an outpatient basis in a xed location or specically designed mobile unit and
does not provide overnight accommodations.
Ambulatory Surgical Facility
A facility with an organized staff of physicians that must be accredited by the Joint Commission on the Accreditation of Health Care
Organizations or by the American Osteopathic Association and which:
• Has permanent facilities and equipment for the primary purpose of performing surgical procedures on an outpatient basis;
• Provides treatment by or under the supervision of physicians and nursing services whenever the patient is in the facility;
• Does not provide inpatient accommodations; and
• Is not, other than incidentally, used as an ofce or clinic for the private practice of a physician or other professional.
Ancillary Services
Ancillary services are certain service, supplies and treatment received while a patient is in a hospital:
• Room and board at the hospital’s average semi-private room rate
• Intensive care unit, coronary care unit or other special care units
• Use of operating, delivery, recovery and treatment rooms
• Laboratory and x-ray services
• Anesthesia and its administration by a hospital employee
• Use of incubators and oxygen
• Physical therapy, chemotherapy and radiation therapy
• Drugs and medicines consumed on the premises
• Dressings, supplies and casts
Annual Deductible
• The annual deductible is the amount you owe for covered services before your Medical Plan begins to pay. For example, if your
annual deductible is $600 your Medical Plan benet won’t pay anything until you have met your $600 annual deductible for covered
medical care services subject to the annual deductible. The annual deductible may not apply to all services.
• Your annual deductible amount is shown in the Schedule of Benets for your coverage option under the Medical Plan. Trustmark’s
records must show that you have reached this annual deductible. Therefore, to ensure proper record keeping, you should submit
copies of all your bills, even those that you must pay to meet the annual deductible.
• If the family annual deductible amount is reached then the annual deductible will be waived for all others covered under family
coverage for that Plan Year.
• Refer to the Schedule of Benets for your coverage option to see what your annual deductible is, and whether it applies for each
service.
CONTINUED ON PAGE 73
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 73 of 92
Revised 09/2023
Annual Out-of-Pocket Maximum
The annual out-of-pocket maximum is the most you pay during a Plan Year before your Medical Plan benets begins to pay 100%
of the eligible expenses (for the remainder of the Plan Year). Refer to the Schedule of Benets for your coverage option for more
information on your annual out-of-pocket maximum.
Balance Billing
When a provider bills you for the difference between the provider’s charge and the Allowed Amount. For example, if the provider’s
charge is $100 and the Allowed Amount is $70, the provider may bill you for the remaining $30. A network provider may not balance
bill you for covered services. See “Emergency Services Received from an Out-of-Network Provider” and “Out-of-Network Provider
Services Received at a Network Hospital or Ambulatory Surgical Center” in the “How Payment is Determined” section of this SPD for
details about when an Out-of-Network Provider cannot balance bill you.
Behavioral Health Services
Includes assessment and treatment of mental and/or psychological and substance abuse disorders at any level of care.
Coinsurance
Your share of the costs of a covered health care service, calculated as a percent (for example, 20%) of the eligible expense for the
service. You may have to pay coinsurance in addition to any annual deductibles you owe, although some covered services may not be
subject to an annual deductible. Refer to the Schedule of Benets for your coverage option to see what your coinsurance is for each
service.
Community Mental Health Facility
A facility primarily engaged in the treatment of mental illness, including substance abuse. The facility must have in effect utilization and
peer review plans. The facility must also be approved by the Joint Commission on the Accreditation of Health Care Organizations or
certied by the Department of Mental Health.
Convenient Care Clinic
A walk-in health care clinic located in a retail store, supermarket or pharmacy that treats uncomplicated minor illnesses, injuries or
conditions not serious enough for urgent or emergent care. These facilities are staffed with nurse practitioners and physician assistants
who collaborate with physicians to treat minor illnesses and perform some preventive care services.
Copay/Copayment
A xed amount (for example, $35) you pay for a covered medical care service, usually when you receive the service. The amount can
vary by the type of covered medical care service. Refer to the Schedule of Benets for your coverage option to see what your copay/
copayment is for each service.
Coverage
The payment for Covered Services as specied and limited by this SPD.
Covered Drugs
Medications that require a prescription under federal law and are approved for general use by the Food and Drug Administration.
Prescription drugs must be dispensed for your outpatient use by a licensed pharmacy on or after your coverage effective date.
Covered Employee
The person employed by the university, whose name appears on the medical and prescription ID cards and who is not enrolled as a
dependent.
Covered Persons
The enrolled employee and any enrolled dependents who are eligible for coverage.
Covered Service
A service or supply shown and given by a provider for which benets will be provided. A Covered Service may be subject to an annual
deductible, copay, or coinsurance. To be a Covered Service, services must be:
• Authorized by a physician;
• Medically Necessary except as otherwise specied;
• Consistent with the condition(s) for which the Covered Person was admitted when an inpatient; and,
• Within the scope of the license of the provider performing the service.
CONTINUED ON PAGE 74
DEFINITIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 74 of 92
Revised 09/2023
Custodial Care
Care provided for maintenance of the patient or which is designed to assist the patient in meeting the activities of daily living. Such
care is not provided for its therapeutic value in the treatment of an illness, disease, bodily injury, or condition. Custodial care includes
but is not limited to help in walking, bathing, dressing, feeding, preparation of special diets and supervision over exercises or over self-
administration of oral medications not requiring constant attention of trained medical personnel.
Diagnostic Services
Tests and procedures performed when you have specic symptoms to detect or to monitor your disease or condition. Diagnostic
services include, but are not limited to, the following: X-ray and other radiology services; laboratory and pathology services;
cardiographic, encephalographic and radioisotope tests.
Effective Date of Coverage
The date on which your coverage begins.
Eligible Expenses
Maximum amount on which payment is based for covered medical care services. Eligible expenses do not include expenses in
excess of the network provider’s fee schedule, or, in the case of an out-of-network provider, the lesser of the Allowed Amount or the
provider’s reasonable charge.
Experimental/Investigative
Any healthcare services, supplies, procedures, therapies, or devices not recognized as standard medical care for the condition, disease,
illness, or injury being treated. The determination of whether any of the above is experimental or investigational is based on but not
limited to:
• Applicable governmental regulations, such as FDA approval,
• Available scientic evidence is inconclusive regarding safety and efcacy and there is no clear medical consensus regarding its safety
and/or efcacy; i.e., a lack of an abundance of scientic literature and well-designed clinical trials,
• When the service is not proven to be as safe or effective as alternative accepted treatment or when the service does not improve
health outcomes, or when the service is not proven to be outside the research setting.
Extended Care/Skilled Nursing Facility
A facility providing mainly inpatient skilled nursing and related services to patients requiring convalescent and rehabilitative care.
Such care is given by or under the supervision of physicians. An extended care facility is not, other than incidentally, a place that
provides minimal custodial care, ambulatory or part time care or that provides treatment for mental illness, alcoholism, drug abuse, or
tuberculosis. The Medicare program must certify the extended care facility.
Home Health Care
A facility providing skilled nursing and other services on a visiting basis in your home and is responsible for providing the delivery
of such services under a plan prescribed and approved in writing by the attending physician. A home medical care provider must be
certied by Medicare or accredited by the Joint Commission on the Accreditation of Healthcare Organizations.
Hospital
An institution licensed by the jurisdiction in which it is located and approved by the Joint Commission on the Accreditation of
Healthcare Organizations or certied under Medicare. It must provide inpatient medical care and treatment, a staff of physicians and
nurses, facilities for diagnosis and major surgery, but cannot be mainly a place for the aged or for treatment of alcoholism or drug
addiction. It may include care for mental health.
Infertility
Infertility is the result of a disease (an interruption, cessation or disorder of body functions, systems or organs) of the reproductive tract,
which prevents the conception of a child or the ability to carry a pregnancy to delivery. A birthing person is considered infertile if they
are unable to achieve pregnancy after 12 months or cycles of exposure to sperm if under the age of 35 or 6 months/cycles if over the
age of 35. A birthing person must be premenopausal or experiencing menopause at a premature age and reasonably expect fertility as
a natural state.
Benets are not provided for in-vitro fertilization, articial insemination, assisted reproductive technologies and procedures, when
either partner has undergone voluntary elective sterilization procedures, or for individuals who are not considered infertile according to
the denition.
Injury
An accidental bodily injury caused by external and violent means. Injury to the teeth as a result of biting, chewing, or grinding is not
considered an accidental bodily injury.
CONTINUED ON PAGE 75
DEFINITIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 75 of 92
Revised 09/2023
Inpatient
A covered person admitted to a hospital or other facility as a registered inpatient.
Intensive Outpatient Program (IOP)
A freestanding or hospital-based program that maintains hours of service for at least three hours per day, two or more days per
week. It may be used as an initial point of entry into care, as a step up from routine outpatient services, or as a step down from acute
inpatient, residential care or a partial hospitalization program. An IOP can be used to treat mental health conditions or can specialize in
the treatment of co-occurring mental health and substance use disorder.
Medical and Prescription Drug ID Cards
The cards on which you will be given your identication numbers and that you must present to your medical and prescription drug
providers in order to verify your coverage.
Medical Plan
The Ohio State University Faculty and Staff Health Plan.
Medicare
The program of medical care for the aged and disabled established by Title XVIII of the Social Security Act of 1965, as amended.
Medically Necessary /Medical Necessity
In order for covered services to be paid, the services must be Medically Necessary. This is the criteria used by Trustmark and OSU
Health Plan to determine the medical necessity of medical services explained. To be Medically Necessary, Covered Services must also
be provided at the most appropriate level of care and in the most appropriate type of medical care facility. Only your medical condition
(not the nancial status or family situation, the distance from a facility or any other non-medical factor) is considered in determining
which level of care or type of medical care facility is appropriate. To be Medically Necessary, Covered Services must:
• Be rendered in connection with an injury or sickness;
• Be consistent with the diagnosis and treatment of your condition;
• Be in accordance with the standards of good medical practice;
• Not be considered experimental or investigative; and
• Not be for your convenience or your physician’s convenience.
Note: Any service failing to meet the Medical Necessity criteria will be the Covered Employee’s liability.
Network
A group of providers who have agreed with OSU Health Plan or Ohio PPO Connect to furnish medical care to Covered Persons. This
medical care is furnished in accordance with written agreements the providers enter into with OSU Health Plan or Ohio PPO Connect.
Providers are designated as a member of either the Premier Network or the Standard Network. The Premier Network offers the highest
level of benet coverage.
Network Provider
A physician, provider, or group that has a network service contract in effect with OSU Health Plan or Ohio PPO Connect to provide
services under the statewide network. A network provider may not balance bill you for Covered Services.
Network Provider’s Fee Schedule
The reimbursement amounts as determined by the network provider for payment of Covered Services.
Ohio PPO Connect
The university has contracted with Ohio PPO Connect to allow Covered Persons in network plans to use providers who are part of the
Ohio PPO Connect network when seeking medical services outside of Franklin County. For a complete list of network providers, visit
osuhealthplan.com/nd-a-provider-search.
OHR
Ofce of Human Resources at The Ohio State University.
OSU Health Plan
The Ohio State University Health Plan, Inc.
Out-of-Network Provider
A physician or provider who does not have a network service contract in effect with OSU Health Plan or Ohio PPO Connect.
Outpatient
A covered person who receives medical care or treatment when he or she is not an inpatient.
CONTINUED ON PAGE 76
DEFINITIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 76 of 92
Revised 09/2023
Partial Hospitalization
A type of program used to treat mental illness and substance abuse. In partial hospitalization, the patient continues to reside at home
but commutes to a treatment center up to seven days a week.
Pharmacy
A facility that is a licensed establishment where a pharmacist dispenses prescription drugs under applicable state laws.
Physician
One of these professionals licensed under the applicable state laws:
• Doctor of Medicine (MD)
• Doctor of Osteopathy (DO)
• Podiatrist (DPM)
• Dental Surgeon or Dentist (DDS)
• Chiropractor (DC)
• Doctor of Optometry (OD)
Plan Administrator
The Ohio State University or the person(s) designated by the university as the plan administrator.
Plan Year
January 1 through December 31.
Plan Sponsor
The Ohio State University.
Preventive Health Services
Preventive health services are:
• Services with an “A” or “B” rating from the U.S. Preventive Services Task Force;
• Immunizations for children, adolescents and adults recommended by the Advisory Committee on Immunization Practices of the
Centers for Disease Control and Prevention;
• Preventive care and screenings for infants, children and adolescents as provided for in the comprehensive guidelines supported by
the Health Resources and Services Administration; and
• Additional preventive care and screening for women provided for in the comprehensive health plan coverage guidelines supported
by the Health Resources and Services Administration.
A new recommendation or guideline applies in the rst calendar year beginning on or after the one-year anniversary of the date that
the guideline or recommendation is issued.
The Preventive Health Care Guidelines can be found online at osuhealthplan.com under Health Plan Tools - Forms and Policies.
Primary Care Provider (PCP)
A PCP is a generalist physician who is designated as a family medicine, general internal medicine, geriatric medicine or general
pediatrics provider. This includes primary care services provided by a Primary Care Nurse Practitioner who practices with a PCP.
Prior Authorization
Notication to OSU Health Plan or Express Scripts of a request for benets before receipt of specic services, as outlined in this SPD or
the Schedule of Benets for your coverage option, or before elective admission to a hospital or facility. (See [complete URL] for a list of
services requiring Prior Authorization). Emergency admissions must be authorized within one business day. If Prior Authorization is not
obtained from OSU Health Plan, a penalty of 20% of the fee, up to $1,000, per admission or service will be charged. This penalty does
not apply toward the annual deductible or the annual out-of-pocket maximum.
Prior Authorization Penalty
A benet reduction of 20%, up to $1,000, per admission or service of care will occur when Prior Authorization is not received from
OSU Health Plan before receipt of services or before elective admission to a hospital or facility. This penalty does not apply toward the
annual deductible or the annual out-of-pocket maximum.
CONTINUED ON PAGE 77
DEFINITIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 77 of 92
Revised 09/2023
Protected Health Information (PHI)
Information that is created, received, maintained, or transmitted by the Medical Plan and relates to the past, present, or future physical
or mental health of a Covered Person; the provision of medical care to a Covered Person; or the past, present, or future payment for
the provision of medical care to a Covered Person; and that identies the Covered Person or there is a reasonable basis to believe that
the information could be used to identify the Covered Person. It includes information about living or deceased people. The following
components of a Covered Person’s health information when created, received, maintained, or transmitted by the Medical Plan are also
considered PHI:
• Names
• Street address, city, county, precinct, zip code
• Dates directly related to a covered person (including dates of birth, admission, discharge, death)
• Telephone numbers, fax numbers and electronic mail addresses
• Social Security numbers
• Medical record numbers
• Account numbers
• Certicate/license numbers
• Vehicle identiers, serial numbers and license plate numbers
• Device identiers and serial numbers
• Web Universal Resource Locators (URLs)
• Biometric identiers (including nger and voice prints)
• Full face photographic images or comparable images
• Any other unique identifying number, characteristic or code
• Health plan beneciary ID numbers
• Internet protocol (IP address numbers)
Provider
The facilities or professionals listed below which are licensed and are operating within the scope of that license:
Facility
• Ambulatory health facility
• Ambulatory surgical facility
• Behavioral health day/nightcare center
• Community mental health facility
• Convenient care clinic
• General acute care hospital
• Home medical care provider
• Hospice provider (hospital)
Professional
• Acupuncturist
• Advanced Practice Psychiatric Registered Nurse
• Audiologist
• Certied Nurse Midwife
• Clinical Nurse Specialist
• Independent Chemical Dependency Counselor
• Independent Social Worker (LISW/LPCC)
• Laboratory (must be Medicare approved)
• Marriage and Family Therapist
• Nurse Practitioner
• Occupational Therapist
Schedule of Benets
A separate schedule showing payment information with respect to your Medical Plan coverage option.
Sickness
Any physical disease or mental illness. Pregnancy, premature birth, congenital anomalies and birth anomalies are considered to be
sicknesses.
Specialized Hospital
A facility primarily engaged in providing diagnostic and therapeutic services for the inpatient treatment of mental illness. Such services
must be provided by or under the supervision of an organized staff of physicians. Continuous nursing services must also be provided
under the supervision of a registered nurse.
• Pharmacist
• Physician
• Physician Assistant
• Professional Ambulance Service
• Professional Clinical Counselor
• Physical Therapist
• Psychologist
• Registered or Licensed Dietician
• Registered Nurse Anesthetist
• Speech Pathologist
• Speech Therapist
• Long-term acute care facility
• On-site Birthing Center
• Pharmacy
• Psychiatric facility
• Skilled nursing facility/extended care facility
• Specialized hospital
• Substance abuse treatment facility
• Urgent care facility
DEFINITIONS
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 78 of 92
Revised 09/2023
OHIO STATE TRAVEL ASSISTANCE
Eligibility
Any individual enrolled in medical coverage through The Ohio State University Faculty and Staff Health Plan (the Medical Plan)
automatically has access to Ohio State Travel Assistance services. Travel assistance can be obtained by calling (800) 678-6269,
option 6. Additional Ohio State Travel Assistance information can be found at hr.osu.edu/benets/travel-assistance.
TRAVELING OUTSIDE OHIO
Services Provided by RedpointWTP LLC
Redpoint is a Travel Assistance Company and cannot advise on your health benets or if facilities are in or out-of-network.
24 hour Access to Medical Professionals
When you contact RedpointWTP LLC, you will receive direct access to medical and security experts.
Services Include But Are Not Limited To:
• Medical professional locator
• Telephonic interpretation services
• Medical evacuation
• Transportation to the nearest appropriate medical center
• Medically Necessary repatriation
• Assistance recovering lost or stolen luggage, medications, eyeglasses, wallets or other important documents
• ID theft assistance while traveling
• Dental, legal and bail bond referrals
• Emergency message relay and counseling
• Online pre-trip resources; security and crime alerts, political instability alerts, passport and visa information
• Medical Evacuation
• Mortal Remains Repatriation
For a complete list of all available RedpointWTP LLC services, resources and the Terms of Service, visit LifeBenets.com/travel.
BE AWARE OF YOUR RESPONSIBILITIES
• You are responsible for any out-of-pocket expenses such as deductibles, copayments, and coinsurance in accordance with your
medical coverage.
• You may be required to pay for services and then submit an itemized claim or completed claim form to Trustmark. The
address for claims submissions is on your medical ID card. Claim forms may be obtained by calling Trustmark, or online at
hr.osu.edu/policies-forms (see Trustmark Health Insurance Claim Form under the Forms tab -Health Benets) or by calling
HR Connection at 614-247-myHR(6947).
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 79 of 92
Revised 09/2023
APPENDIX
THE OHIO STATE UNIVERSITY FACULTY AND STAFF HEALTH PLAN CLAIM
DETERMINATION AND APPEAL PROCEDURES
TABLE OF CONTENTS
INTRODUCTION ........................................................................................................80
PRE-SERVICE CLAIMS (NOT INVOLVING URGENT CARE) ..................................................................80
POST-SERVICE CLAIMS .................................................................................................82
URGENT CARE CLAIMS .................................................................................................85
CONCURRENT CARE CLAIMS ...........................................................................................86
RESCISSIONS OF COVERAGE ............................................................................................87
VOLUNTARY EXTERNAL REVIEW PROCESS ..............................................................................88
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 80 of 92
Revised 09/2023
CLAIM DETERMINATION AND APPEAL PROCEDURES
These procedures describe how benet claims and appeals of adverse benet determinations are made under The Ohio State
University Faculty and Staff Health Plan (Plan). You should consult The Ohio State University Faculty and Staff Health Plan Specic
Plan Details (SPD) document for details regarding the benets provided under the Plan.
INTRODUCTION
Types of Claims
The type of claim you make determines the time frame under which a determination is made regarding your claim. There are four
categories of claims, each with somewhat different claim determination and appeal rules. The primary difference is the time frame
within which claims and appeals of adverse benet determinations must be determined:
1. Pre-Service Claim: A “Pre-Service Claim” generally is any claim for a benet where the Plan conditions receipt of the benet, in
whole or in part, on Prior Authorization or approval of the benet in advance of obtaining medical care.
2. Urgent Care Claim: An “Urgent Care Claim” generally is any claim that must be processed on an expedited basis because a delay in
processing could seriously jeopardize the life or health of the patient or the ability of the patient to regain maximum function, or in
the opinion of the physician with knowledge of the patient’s medical condition, a delay would subject the patient to severe pain that
cannot be adequately managed without the care or treatment that is the subject of the claim.
3. Concurrent Care Claim: A “Concurrent Care Claim” generally is any claim involving a decision to reduce or terminate an ongoing
course of treatment or a decision regarding your request to extend a course of treatment beyond what has already been approved.
4. Post-Service Claim: A “Post-Service Claim” generally is any claim that is not an Urgent Care Claim, a Pre-Service Claim or a
Concurrent Care Claim.
Denitions
• Adverse Benet Determination. An “adverse benet determination” means: (1) a denial, reduction, or termination of, or a failure to
provide or make payment, in whole or in part, for, a benet, including as a result of (a) a determination of eligibility to participate in
the Plan; (b) the application of any utilization review; (c) a determination that a health care service or item does not meet the Plan’s
requirements for medical necessity, appropriateness, health care setting, level of care, or effectiveness, including experimental or
investigational treatments; (d) a determination that a health care service is not a covered benet; or (e) the imposition of an exclusion,
including exclusions for pre-existing conditions, source of injury, network, or any other limitation on benets that would otherwise be
covered; or a claim that results in balance billing to the participant following an adjudication between the plan and an out-of-network
provider or facility; and (2) a rescission of your coverage.
• Authorized Representative. Your “authorized representative” means an individual who may act on your behalf with respect to a
benet claim or appeal under these procedures and who is any of the following: (1) a person to whom you have given express,
written consent in the Appointment of Authorized Representative section of an Appeal Form to represent you in an internal appeals
process or external review process of an adverse benet determination; (2) a person authorized by law to provide substituted
consent for you; or (3) a family member or a treating health care professional, but only when you are unable to provide consent. An
authorized representative shall not include a designee of a physician rendering the service for which a bill has been submitted.
• Benets Appeals Committee. For appeals pertaining to enrollment (including eligibility to enroll and to make changes to enrollment),
“Benets Appeals Committee” means the Ohio State University Benets Appeals Committee. For all other appeals, “Benets
Appeals Committee” means OSUHP’s Benets Appeals Committee.
• OSUHP. “OSUHP” means The Ohio State University Health Plan, Inc.
• Rescission of Coverage. A “rescission of coverage” means a cancellation or discontinuance of coverage that has retroactive effect,
but does not include any such cancellation or discontinuance to the extent it is attributable to a failure to pay contributions towards
the cost of coverage on a timely basis. The University shall determine who meets the requirements for eligibility under the Plan.
• Third Party Administrator. “Third Party Administrator” means the University’s third party administrator for medical claims
processing, which is Trustmark Health Benets.
• University. “University” means The Ohio State University.
• You. Any reference to “you” in these procedures includes you and your authorized representative.
Full and Fair Review
In connection with a claim or internal appeal, you will be provided, free of charge, with any new or additional evidence or rationale
considered, relied upon, or generated by the Plan (or at the direction of the Plan) in connection with your claim. Such evidence or
rationale will be provided in advance of the date on which a notice of a nal adverse benet determination is required to be provided, in
order to give you an opportunity to respond prior to that date.
PRE-SERVICE CLAIMS (NOT INVOLVING URGENT CARE)
Consideration of Initial Pre-Service Claim
• Pre-Service Claims must be submitted to OSUHP by completing a Prior Authorization form available at osuhealthplan.com under
Forms and Downloads. If you submit a Pre-Service Claim properly with all necessary information, you will receive written notice of
the claim decision from OSUHP within a reasonable period of time appropriate to the medical circumstances, but not later than 10
days from receipt of the Pre-Service Claim. OSUHP may request a one-time extension of no longer than 10 days for matters beyond
its control if, prior to expiration of the initial 10 day period, you are notied of the circumstances requiring the extension and the date
by which a decision will be rendered.
CONTINUED ON PAGE 81
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 81 of 92
Revised 09/2023
If you le a Pre-Service Claim improperly, you will receive a notice of the improper ling and how to correct it as soon as possible, but
not later than ve days after your Pre-Service Claim is received. Once you receive notice of the improper ling, you then will have 45
days to provide any needed information.
If Your Initial Pre-Service Claim is Denied
If you receive a notice of an adverse benet determination, the notice will set forth:
• Information sufcient to identify the claim or health care service involved, including the name of the health care provider, the date of
service and claim amount, if applicable;
• The specic reason or reasons for the adverse benet determination, including the denial code, such as the claim adjustment reason
code and the remittance advice remark code and each code’s corresponding meaning;
• A description of any additional material or information necessary for you to perfect your claim and an explanation of why the material
or information is necessary;
• Reference to the specic Plan provisions on which the adverse benet determination is based;
• A description of the Plan’s standard, if any, that was used in making the determination;
• A statement of your right to request an external review and a description of the Plan’s internal appeals and external review
procedures and the time limits applicable to such procedures, including information about how to initiate an appeal and an external
review;
• A statement informing you that if your treating physician certies in writing that you have a medical condition for which the time
frame for completion of an expedited review of an internal appeal involving an adverse benet determination would seriously
jeopardize your life or health or jeopardize your ability to regain maximum function, you may le a request for an expedited external
review to be conducted simultaneously with the expedited internal appeal, pursuant to Section 3922.09 of the Ohio Revised Code;
• A statement informing you that if the adverse benet determination involves a denial of coverage based on a determination that the
recommended or requested health care service or treatment is experimental or investigational and your treating physician certies
in writing that the recommended or requested health care service or treatment would be signicantly less effective if not promptly
initiated, you may le a request for an expedited external review to be conducted simultaneously with the expedited internal appeal,
pursuant to Section 3922.09 or 3922.10 of the Ohio Revised Code; and
• The availability of, and contact information for, the Ohio Department of Insurance, who may assist you with the internal appeals and
external review processes.
• If an internal rule, guideline, protocol, or other similar criterion was relied upon in making the adverse benet determination, either
the specic rule, guideline, protocol, or other similar criterion will be provided free of charge to you, or you will be informed that such
rule, guideline, protocol, or other criterion will be provided free of charge to you upon request. If a medical necessity or experimental
treatment or a similar exclusion or limit was relied upon in making the adverse benet determination, either an explanation of the
scientic or clinical judgment for the determination (applying the terms of the Plan to your medical circumstances) will be provided
free of charge to you, or you will be informed that such explanation will be provided free of charge to you upon request.
Mandatory Internal Appeal
• If your initial Pre-Service Claim is denied in whole or in part, you have the right to appeal the adverse benet determination
by sending a written request for review, in a form prescribed by the University, to the Benets Appeals Committee within 180
days following your receipt of notice of the adverse benet determination. Your written request should state why you think your
claim should not have been denied and should include any adverse benet determination notice you received and any additional
documents, records, information or comments you think may have a bearing on your claim. Upon your request, you will be provided,
free of charge, reasonable access to, and copies of, all documents, records and other information relevant to your claim.
• Upon receipt of your request, the Benets Appeals Committee will conduct a review that takes into account all comments,
documents, records and other information submitted by you relating to your claim, without regard to whether such information
was submitted or considered in the initial adverse benet determination. The review will not afford any deference to the initial
adverse benet determination and will be conducted by an individual who is neither the individual who made the adverse benet
determination that is the subject of your appeal, nor the subordinate of such individual.
• If the adverse benet determination was based in whole or in part on a medical judgment (including determinations with regard
to whether a particular treatment, drug or other item is experimental, investigational or not Medically Necessary or appropriate),
the Benets Appeals Committee shall consult with a health care professional who has appropriate training and experience in the
eld of medicine involved in the medical judgment. This health care professional will be neither the individual who was consulted in
connection with the adverse benet determination that is the subject of your appeal, nor the subordinate of such individual. Upon
request, OSUHP will provide the identities of any medical or vocational experts whose advice was obtained on behalf of the Plan
in connection with the adverse benet determination, without regard to whether the advice was relied upon in making the adverse
benet determination.
• The Benets Appeals Committee will notify you of its determination on review within a reasonable period of time appropriate to the
medical circumstances, but not later than 10 days after receipt of your request for review of an adverse benet determination.
If Your Pre-Service Claim is Denied Upon Mandatory Internal Appeal
If your internal appeal is denied (a “nal adverse benet determination”), you will be notied of the following, in a manner to be
understood by you:
• Information sufcient to identify the claim or health care service involved, including the name of the health care provider, the date of
service and claim amount, if applicable;
• A discussion of the determination;
CONTINUED ON PAGE 82
CLAIM DETERMINATION AND APPEAL PROCEDURES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 82 of 92
Revised 09/2023
• The specic reason or reasons for the adverse benet determination, including the denial code, such as the claim adjustment reason
code and the remittance advice remark code and each code’s corresponding meaning;
• Reference to the specic Plan provisions on which the benet determination is based;
• A description of the Plan’s standard, if any, that was used in making the determination;
• A statement that you are entitled to receive, upon request and free of charge, reasonable access to, and copies of, all documents,
records and other information relevant to your claim;
• A statement of your right to request an external review within 180 days after the date of the notice of the nal adverse benet
determination and a description of the Plan’s internal appeals and external review procedures and the time limits applicable to such
procedures, including information about how to initiate an appeal and an external review;
• A statement that if your treating physician certies in writing that you have a medical condition for which the time frame for
completion of a standard external review pursuant to Section 3922.08 of the Ohio Revised Code would seriously jeopardize your
life or health or would jeopardize your ability to regain maximum function, you may le a request for an expedited external review
pursuant to Section 3922.09 of the Ohio Revised Code; and
• The availability of, and contact information for, the Ohio Department of Insurance, who may assist you with the internal appeals and
external review processes.
• If the Benets Appeals Committee relied upon an internal rule, guideline, protocol, or other similar criterion in making the nal
adverse benet determination, either the specic rule, guideline, protocol, or other similar criterion will be provided free of charge to
you, or you will be informed that such rule, guideline, protocol, or other criterion will be provided free of charge to you upon request.
If the Benets Appeals Committee relied upon a medical necessity or experimental treatment or similar exclusion or limit in making
the nal adverse benet determination, either an explanation of the scientic or clinical judgment for the determination (applying the
terms of the Plan to your medical circumstances) will be provided free of charge to you, or you will be informed that such explanation
will be provided free of charge to you upon request.
POST-SERVICE CLAIMS
Filing a Post-Service Claim
• When you receive a covered service, a Post-Service Claim must be led for you to obtain benets under the Plan. Your provider may
le a Post-Service Claim for you. However, if your provider does not le the Post-Service Claim for you, you should le the Post-
Service Claim yourself.
• Claim forms are available: online at hr.osu.edu/policies-forms under Forms - Health Benets - Trustmark Health Insurance Claim
Form; by contacting HR Connection by phone at 614-247-myHR(6947) or (800) 678-6010 or email at HRConnectio[email protected]; or
by contacting the Third Party Administrator.
• Claim forms must be lled out completely and then sent to: Trustmark Health Benets (formerly ), P.O. Box 2310, Mt. Clemens, MI
48046.
• No Post-Service Claims may be submitted more than 12 months from the date of service or supply is provided. Claims led after that
date will not be honored.
• If a Post-Service Claim is submitted, you will receive written notice from the Third Party Administrator reecting the benet
determination within a reasonable period of time, but not later than 30 days following the date the Third Party Administrator
receives the Post-Service Claim, as long as the claim contains all necessary information. The Third Party Administrator may request
a one-time extension of no longer than 15 days for matters beyond its control if, prior to the expiration of the initial 30-day period,
the Third Party Administrator noties you of the circumstances requiring the extension and the date by which the Third Party
Administrator expects to render a decision.
• If additional information is needed to process your Post-Service Claim, you will be notied within the 30-day period and the notice
will specify the required information. Once you receive notice, you then will have 45 days to provide any needed information.
If Your Initial Post-Service Claim is Denied
If you receive a notice of an adverse benet determination, the notice will set forth:
• Information sufcient to identify the claim or health care service involved, including the name of the health care provider, the date of
service and claim amount, if applicable;
• The specic reason or reasons for the adverse benet determination, including the denial code, such as the claim adjustment reason
code and the remittance advice remark code and each code’s corresponding meaning;
• A description of any additional material or information necessary for you to perfect your claim and an explanation of why the
material or information is necessary;
• Reference to the specic Plan provisions on which the adverse benet determination is based;
• A description of the Plan’s standard, if any, that was used in making the determination;
• A statement of your right to request an external review and a description of the Plan’s internal appeals and external review
procedures and the time limits applicable to such procedures, including information about how to initiate an appeal and an external
review;
• A statement informing you that if your treating physician certies in writing that you have a medical condition for which the time
frame for completion of an expedited review of an internal appeal involving an adverse benet determination would seriously
jeopardize your life or health or jeopardize your ability to regain maximum function, you may le a request for an expedited external
review to be conducted simultaneously with the expedited internal appeal, pursuant to Section 3922.09 of the Ohio Revised Code;
CONTINUED ON PAGE 83
CLAIM DETERMINATION AND APPEAL PROCEDURES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024
PAGE 83 of 92
Revised 09/2023
• A statement informing you that if the adverse benet determination involves a denial of coverage based on a determination that the
recommended or requested health care service or treatment is experimental or investigational and your treating physician certies
in writing that the recommended or requested health care service or treatment would be signicantly less effective if not promptly
initiated, you may le a request for an expedited external review to be conducted simultaneously with the expedited internal appeal,
pursuant to Section 3922.09 or 3922.10 of the Ohio Revised Code; and
• The availability of, and contact information for, the Ohio Department of Insurance, who may assist you with the internal appeals and
external review processes.
• If an internal rule, guideline, protocol, or other similar criterion was relied upon in making the adverse benet determination, either
the specic rule, guideline, protocol, or other similar criterion will be provided free of charge to you, or you will be informed that such
rule, guideline, protocol, or other criterion will be provided free of charge to you upon request. If a medical necessity or experimental
treatment or a similar exclusion or limit was relied upon in making the adverse benet determination, either an explanation of the
scientic or clinical judgment for the determination (applying the terms of the Plan to your medical circumstances) will be provided
free of charge to you, or you will be informed that such explanation will be provided free of charge to you upon request.
Mandatory First Level of Internal Appeal
• If your initial Post-Service Claim is denied in whole or in part, you have the right to appeal the adverse benet determination by
sending a written request for review, in a form prescribed by the University, to the Third Party Administrator within 180 days
following your receipt of notice of the adverse benet determination. Your written request should state why you think your
claim should not have been denied and should include any adverse benet determination notice you received and any additional
documents, records, information or comments you think may have a bearing on your claim. Upon your request, you will be provided,
free of charge, reasonable access to, and copies of all documents, records and other information relevant to your claim.
• Upon receipt of your request, the Third Party Administrator will conduct a review that takes into account all comments, documents,
records and other information submitted by you relating to your claim, without regard to whether such information was submitted
or considered in the initial adverse benet determination. The review will not afford any deference to the initial adverse benet
determination and will be conducted by an individual who is neither the individual who made the adverse benet determination that
is the subject of your appeal, nor the subordinate of such individual.
• If the adverse benet determination was based in whole or in part on a medical judgment (including determinations with regard
to whether a particular treatment, drug or other item is experimental, investigational or not Medically Necessary or appropriate),
the Third Party Administrator shall consult with a health care professional who has appropriate training and experience in the eld
of medicine involved in the medical judgment. This health care professional will be neither the individual who was consulted in
connection with the adverse benet determination that is the subject of your appeal, nor the subordinate of such individual. Upon
request, the Third Party Administrator will provide the identities of any medical or vocational experts whose advice was obtained
on behalf of the Plan in connection with the adverse benet determination, without regard to whether the advice was relied upon in
making the adverse benet determination.
• The Third Party Administrator will notify you of its determination on review within a reasonable period of time, but not later than 30
days after receipt of your request for review.
If Your Post-Service Claim is Denied Upon Mandatory First Level of Internal Appeal
If your mandatory rst level of internal appeal is denied, you will be notied of the following, in a manner to be understood by you:
• Information sufcient to identify the claim or health care service involved, including the name of the health care provider, the date of
service and claim amount, if applicable;
• A discussion of the determination;
• The specic reason or reasons for the adverse benet determination, including the denial code, such as the claim adjustment reason
code and the remittance advice remark code and each code’s corresponding meaning;
• Reference to the specic Plan provisions on which the benet determination is based;
• A description of the Plan’s standard, if any, that was used in making the determination;
• A statement that you are entitled to receive, upon request and free of charge, reasonable access to, and copies of, all documents,
records and other information relevant to your claim;
• A statement of your right to request an external review and a description of the Plan’s internal appeals and external review
procedures and the time limits applicable to such procedures, including information about how to initiate an appeal and an external
review;
• A statement informing you that if your treating physician certies in writing that you have a medical condition for which the time
frame for completion of an expedited review of an internal appeal involving an adverse benet determination would seriously
jeopardize your life or health or jeopardize your ability to regain maximum function, you may le a request for an expedited external
review to be conducted simultaneously with the expedited internal appeal, pursuant to Section 3922.09 of the Ohio Revised Code;
• A statement informing you that if the adverse benet determination involves a denial of coverage based on a determination that the
recommended or requested health care service or treatment is experimental or investigational and your treating physician certies
in writing that the recommended or requested health care service or treatment would be signicantly less effective if not promptly
initiated, you may le a request for an expedited external review to be conducted simultaneously with the expedited internal appeal,
pursuant to Section 3922.09 or 3922.10 of the Ohio Revised Code; and
• The availability of, and contact information for, the Ohio Department of Insurance, who may assist you with the internal appeals and
external review processes.
CONTINUED ON PAGE 84
CLAIM DETERMINATION AND APPEAL PROCEDURES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 84 of 92
Revised 09/2023
• If the Third Party Administrator relied upon an internal rule, guideline, protocol, or other similar criterion in making its denial, either
the specic rule, guideline, protocol, or other similar criterion will be provided free of charge to you, or you will be informed that such
rule, guideline, protocol, or other criterion will be provided free of charge to you upon request. If the Third Party Administrator relied
upon a medical necessity or experimental treatment or similar exclusion or limit in making its denial, either an explanation of the
scientic or clinical judgment for the determination (applying the terms of the Plan to your medical circumstances) will be provided
free of charge to you, or you will be informed that such explanation will be provided free of charge to you upon request.
Mandatory Second Level of Internal Appeal
• If you disagree with the Third Party Administrator’s rst level of internal appeal decision, you have the right to request a second level
of internal appeal by sending a written request for review, in a form prescribed by the University, to OSUHP within 60 days following
your receipt of notice of the Third Party Administrator’s decision. Your written request should state why you think your claim should
not have been denied and should include any adverse benet determination notices you received and any additional documents,
records, information or comments you think may have a bearing on your claim. Upon your request, you will be provided, free of
charge, reasonable access to, and copies of, all documents, records and other information relevant to your claim.
• Upon receipt of your request, OSUHP (and in certain cases, the Benets Appeals Committee) will conduct a review that takes
into account all comments, documents, records and other information submitted by you relating to your claim, without regard to
whether such information was submitted or considered in the previous adverse benet determinations . The review will not afford
any deference to the previous adverse benet determinations and will be conducted by an individual who is neither the individual
who made an adverse benet determination that is the subject of your appeal, nor the subordinate of such individual . If OSUHP
determines that all or a portion of your Post-Service Claim should be denied, the Benets Appeals Committee also will conduct a
review of your Post-Service Claim as described in this paragraph.
• If the adverse benet determination was based in whole or in part on a medical judgment (including determinations with regard
to whether a particular treatment, drug or other item is experimental, investigational or not Medically Necessary or appropriate),
OSUHP and, if applicable, the Benets Appeals Committee shall consult with a health care professional who has appropriate training
and experience in the eld of medicine involved in the medical judgment. This health care professional will be neither the individual
who was consulted in connection with the adverse benet determination that is the subject of your appeal, nor the subordinate of
such individual. Upon request, OSUHP and, if applicable, the Benets Appeals Committee will provide the identities of any medical
or vocational experts whose advice was obtained on behalf of the Plan in connection with the adverse benet determination, without
regard to whether the advice was relied upon in making the adverse benet determination.
• OSUHP or, if applicable, the Benets Appeals Committee will notify you of its determination on review within a reasonable period of
time, but not later than 30 days after receipt of your request for review.
If Your Post-Service Claim is Denied Upon Mandatory Second Level of Internal Appeal
If your mandatory second level of internal appeal is denied (a “nal adverse benet determination”), you will be notied of the
following, in a manner to be understood by you:
• Information sufcient to identify the claim or health care service involved, including the name of the health care provider, the date of
service and claim amount, if applicable;
• A discussion of the determination;
• The specic reason or reasons for the adverse benet determination, including the denial code, such as the claim adjustment reason
code and the remittance advice remark code and each code’s corresponding meaning;
• Reference to the specic Plan provisions on which the benet determination is based;
• A description of the Plan’s standard, if any, that was used in making the determination;
• A statement that you are entitled to receive, upon request and free of charge, reasonable access to, and copies of, all documents,
records and other information relevant to your claim;
• A statement of your right to request an external review within 180 days after the date of the notice of the nal adverse benet
determination and a description of the Plan’s internal appeals and external review procedures and the time limits applicable to such
procedures, including information about how to initiate an appeal and an external review;
• A statement informing you that if your treating physician certies in writing that you have a medical condition for which the
time frame for completion of a standard external review pursuant to Section 3922.08 of the Ohio Revised Code would seriously
jeopardize your life or health or would jeopardize your ability to regain maximum function, you may le a request for an expedited
external review pursuant to Section 3922.09 of the Ohio Revised Code; and
• The availability of, and contact information for, the Ohio Department of Insurance, who may assist you with the internal appeals and
external review processes.
• If OSUHP or the Benets Appeals Committee relied upon an internal rule, guideline, protocol, or other similar criterion in making
the nal adverse benet determination, either the specic rule, guideline, protocol, or other similar criterion will be provided free of
charge to you, or you will be informed that such rule, guideline, protocol, or other criterion will be provided free of charge to you upon
request. If OSUHP or, if applicable, the Benets Appeals Committee relied upon a medical necessity or experimental treatment or
similar exclusion or limit in making the nal adverse benet determination, either an explanation of the scientic or clinical judgment
for the determination (applying the terms of the Plan to your medical circumstances) will be provided free of charge to you, or you
will be informed that such explanation will be provided free of charge to you upon request.
CONTINUED ON PAGE 85
CLAIM DETERMINATION AND APPEAL PROCEDURES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 85 of 92
Revised 09/2023
URGENT CARE CLAIMS
Consideration of Initial Urgent Care Claim
• Urgent Care Claims must be submitted to OSUHP by mail to: The OSU Health Plan, 700 Ackerman Road, Suite 1007, Columbus,
Ohio, 43202 or by fax to 614-292-2667. If you submit an Urgent Care Claim, you will receive notice of the benet determination
(in writing or electronically) as soon as possible, taking into account medical exigencies, but not later than 72 hours after OSUHP
receives your claim, unless you fail to provide sufcient information to determine whether, or to what extent, benets are covered or
payable under the Plan. OSUHP will take into account the seriousness of your condition.
• If you fail to provide sufcient information regarding your Urgent Care Claim, OSUHP will notify you as soon as possible, but not later
than 24 hours after receipt of your claim, of the specic information necessary to complete your claim. You will have a reasonable
amount of time, taking into account the circumstances, but not less than 48 hours, to provide the specied information. You will
receive a notice of OSUHP’s determination no later than 48 hours after the earlier of: (1) the Plan’s receipt of the requested specied
information; or (2) the end of the 48-hour period within which you were to provide the additional information.
• OSUHP may provide an oral notice of its determination and then follow up with a written or electronic conrmation within three
days.
If Your Initial Urgent Care Claim Is Denied
If you receive a notice of an adverse benet determination, the notice will set forth:
• Information sufcient to identify the claim or health care service involved, including the name of the health care provider, the date of
service and claim amount, if applicable;
• The specic reason or reasons for the adverse benet determination, including the denial code, such as the claim adjustment reason
code and the remittance advice remark code and each code’s corresponding meaning;
• A description of any additional material or information necessary for you to perfect your claim and an explanation of why the
material or information is necessary;
• Reference to the specic Plan provisions on which the adverse benet determination is based;
• A description of the Plan’s standard, if any, that was used in making the determination;
• A statement of your right to request an external review and a description of the Plan’s internal appeals and external review
procedures and the time limits applicable to such procedures, including information about how to initiate an appeal and an external
review;
• A statement informing you that if your treating physician certies in writing that you have a medical condition for which the time
frame for completion of an expedited review of an internal appeal involving an adverse benet determination would seriously
jeopardize your life or health or jeopardize your ability to regain maximum function, you may le a request for an expedited external
review to be conducted simultaneously with the expedited internal appeal, pursuant to Section 3922.09 of the Ohio Revised Code;
• A statement informing you that if the adverse benet determination involves a denial of coverage based on a determination that the
recommended or requested health care service or treatment is experimental or investigational and your treating physician certies
in writing that the recommended or requested health care service or treatment would be signicantly less effective if not promptly
initiated, you may le a request for an expedited external review to be conducted simultaneously with the expedited internal appeal,
pursuant to Section 3922.09 or 3922.10 of the Ohio Revised Code; and
• The availability of, and contact information for, the Ohio Department of Insurance, who may assist you with the internal appeals and
external review processes.
• If an internal rule, guideline, protocol, or other similar criterion was relied upon in making the adverse benet determination, either
the specic rule, guideline, protocol, or other similar criterion will be provided free of charge to you, or you will be informed that such
rule, guideline, protocol, or other criterion will be provided free of charge to you upon request. If a medical necessity or experimental
treatment or a similar exclusion or limit was relied upon in making the adverse benet determination, either an explanation of the
scientic or clinical judgment for the determination (applying the terms of the Plan to your medical circumstances) will be provided
free of charge to you, or you will be informed that such explanation will be provided free of charge to you upon request.
Mandatory Internal Appeal
• If your initial claim is denied in whole or in part, you have the right to appeal the adverse benet determination by sending a written
request for review, in a form prescribed by the University, to the Benets Appeals Committee within 180 days following your receipt
of notice of the adverse benet determination. Your written request should state why you think your claim should not have been
denied and should include any adverse benet determination notice you received and any additional documents, records, information
or comments you think may have a bearing on your claim. Upon your request, you will be provided, free of charge, reasonable access
to, and copies of all documents, records and other information relevant to your claim.
• Upon receipt of your request, the Benets Appeals Committee will conduct a review that takes into account all comments,
documents, records and other information submitted by you relating to your claim, without regard to whether such information
was submitted or considered in the initial adverse benet determination. The review will not afford any deference to the initial
adverse benet determination and will be conducted by an individual who is neither the individual who made the adverse benet
determination that is the subject of your appeal, nor the subordinate of such individual.
• If the adverse benet determination was based in whole or in part on a medical judgment (including determinations with regard
to whether a particular treatment, drug or other item is experimental, investigational or not Medically Necessary or appropriate),
the Benets Appeals Committee shall consult with a health care professional who has appropriate training and experience in the
eld of medicine involved in the medical judgment. This health care professional will be neither the individual who was consulted in
CONTINUED ON PAGE 86
CLAIM DETERMINATION AND APPEAL PROCEDURES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 86 of 92
Revised 09/2023
connection with the adverse benet determination that is the subject of your appeal, nor the subordinate of such individual. Upon
request, the Benets Appeals Committee will provide the identities of any medical or vocational experts whose advice was obtained
on behalf of the Plan in connection with the adverse benet determination, without regard to whether the advice was relied upon in
making the adverse benet determination.
• In the case of a claim involving urgent care, you may submit a request for an expedited internal appeal either in writing or orally.
All necessary information for the review, including the benet determination on review, may be transmitted between the Plan and
you by telephone, facsimile, or another similarly expeditious method. To proceed with an expedited internal appeal, you or your
authorized representative must contact OSUHP and provide at least the following information:
- Your name;
- The date(s) of the medical service;
- The specic medical condition or symptom;
- The provider’s name;
- The service or supply for which approval of benets was sought; and
- Any reasons why the appeal should be processed on a more expedited basis.
The Benets Appeals Committee will notify you of its determination on review as soon as possible, taking into account the medical
exigencies, but not later than 48 hours after receipt of your request for review of an adverse benet determination. If the Benets
Appeals Committee denies an Urgent Care Claim on review, OSUHP may provide oral notice of that determination, then follow-up with
a written or electronic conrmation within three days.
If Your Urgent Care Claim is Denied Upon Mandatory Internal Appeal
If your internal appeal is denied (a “nal adverse benet determination”), you will be notied of the following, in a manner to be
understood by you:
• Information sufcient to identify the claim or health care service involved, including the name of the health care provider, the date of
service and claim amount, if applicable;
• A discussion of the determination;
• The specic reason or reasons for the adverse benet determination, including the denial code, such as the claim adjustment reason
code and the remittance advice remark code and each code’s corresponding meaning;
• Reference to the specic Plan provisions on which the benet determination is based;
• A description of the Plan’s standard, if any, that was used in making the determination;
• A statement that you are entitled to receive, upon request and free of charge, reasonable access to, and copies of, all documents,
records and other information relevant to your claim;
• A statement of your right to request an external review within 180 days after the date of the notice of the nal adverse benet
determination and a description of the Plan’s internal appeals and external review procedures and the time limits applicable to such
procedures, including information about how to initiate an appeal and an external review;
• A statement informing you that if your treating physician certies in writing that you have a medical condition for which the
time frame for completion of a standard external review pursuant to Section 3922.08 of the Ohio Revised Code would seriously
jeopardize your life or health or would jeopardize your ability to regain maximum function, you may le a request for an expedited
external review pursuant to Section 3922.09 of the Ohio Revised Code; and
• The availability of, and contact information for, the Ohio Department of Insurance, who may assist you with the internal appeals and
external review processes.
• If the Benets Appeals Committee relied upon an internal rule, guideline, protocol, or other similar criterion in making the nal
adverse benet determination, either the specic rule, guideline, protocol, or other similar criterion will be provided free of charge to
you, or you will be informed that such rule, guideline, protocol, or other criterion will be provided free of charge to you upon request.
If the Benets Appeals Committee relied upon a medical necessity or experimental treatment or similar exclusion or limit in making
the nal adverse benet determination, either an explanation of the scientic or clinical judgment for the determination (applying the
terms of the Plan to your medical circumstances) will be provided free of charge to you, or you will be informed that such explanation
will be provided free of charge to you upon request.
CONCURRENT CARE CLAIMS
Consideration of Initial Concurrent Care Claim
• Concurrent Care Claims must be submitted to OSUHP by mail to The OSU Health Plan, 700 Ackerman Road, Suite 1007, Columbus,
Ohio, 43202 or by fax to 614-292-2667. If an ongoing course of treatment was previously approved for a specic period of time or
number of treatments, any reduction or termination of those ongoing treatments before the end of that period of time or number of
treatments will constitute an adverse benet determination. OSUHP must notify you of the adverse benet determination within a
reasonable time period prior to the reduction or termination of the ongoing treatments.
• If you request to extend an ongoing course of treatment and your request is an Urgent Care Claim, OSUHP will decide your request
and notify you of the determination within 24 hours after it is received, provided your request is made at least 24 hours prior to
the end of the approved treatment. If your request for extended treatment is not made at least 24 hours prior to the end of the
approved treatment the request will be treated as an Urgent Care Claim and decided according to the Urgent Care Claim time frames
described above. See Urgent Care Claims beginning on page 85.
CONTINUED ON PAGE 87
CLAIM DETERMINATION AND APPEAL PROCEDURES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 87 of 92
Revised 09/2023
• If your request to extend an ongoing course of treatment is not an Urgent Care Claim, your request will be considered a new claim
and decided according to the Pre-Service Claim or Post-Service Claim time frames described above, whichever is applicable. See
Pre-Service Claims beginning on page 80 or Post-Service Claims beginning on page 82, whichever is applicable.
If Your Initial Concurrent Care Claim Is Denied
If you receive a notice of an adverse benet determination, the notice will set forth:
• Information sufcient to identify the claim or health care service involved, including the name of the health care provider, the date of
service and claim amount, if applicable;
• The specic reason or reasons for the adverse benet determination, including the denial code, such as the claim adjustment reason
code and the remittance advice remark code and each code’s corresponding meaning;
• A description of any additional material or information necessary for you to perfect your claim and an explanation of why the
material or information is necessary;
• Reference to the specic Plan provisions on which the adverse benet determination is based;
• A description of the Plan’s standard, if any, that was used in making the determination;
• A statement of your right to request an external review and a description of the Plan’s internal appeals and external review
procedures and the time limits applicable to such procedures, including if the Concurrent Care Claim is treated as an Urgent Care
Claim, a description of the expedited review process for Urgent Care Claims and including information about how to initiate an
appeal and an external review;
• A statement informing you that if your treating physician certies in writing that you have a medical condition for which the time
frame for completion of an expedited review of an internal appeal involving an adverse benet determination would seriously
jeopardize your life or health or jeopardize your ability to regain maximum function, you may le a request for an expedited external
review to be conducted simultaneously with the expedited internal appeal, pursuant to Section 3922.09 of the Ohio Revised Code;
• A statement informing you that if the adverse benet determination involves a denial of coverage based on a determination that the
recommended or requested health care service or treatment is experimental or investigational and your treating physician certies
in writing that the recommended or requested health care service or treatment would be signicantly less effective if not promptly
initiated, you may le a request for an expedited external review to be conducted simultaneously with the expedited internal appeal,
pursuant to Section 3922.09 or 3922.10 of the Ohio Revised Code; and
• The availability of, and contact information for, the Ohio Department of Insurance, who may assist you with the internal appeals and
external review processes.
• If an internal rule, guideline, protocol, or other similar criterion was relied upon in making the adverse benet determination, either
the specic rule, guideline, protocol, or other similar criterion will be provided free of charge to you, or you will be informed that such
rule, guideline, protocol, or other criterion will be provided free of charge to you upon request. If a medical necessity or experimental
treatment or a similar exclusion or limit was relied upon in making the adverse benet determination, either an explanation of the
scientic or clinical judgment for the determination (applying the terms of the Plan to your medical circumstances) will be provided
free of charge to you, or you will be informed that such explanation will be provided free of charge to you upon request.
Mandatory Internal Appeal(s)
If your initial Concurrent Care Claims is denied in whole or in part, your right to appeal and the process relating to that appeal will be
decided under the Urgent Care Claims provisions (beginning on page 85), the Pre-Service Claims provisions (beginning on page 80) or
the Post-Service Claims provisions (beginning on page 82), whichever is applicable.
RESCISSIONS OF COVERAGE
If Your Coverage Is Rescinded
If you receive a notice of a rescission of coverage, the notice will set forth:
• Information sufcient to identify the claim or health care service involved;
• The specic reason or reasons for the adverse benet determination;
• A description of any additional material or information necessary for you to perfect your claim and an explanation of why the
material or information is necessary;
• Reference to the specic Plan provisions on which the adverse benet determination is based;
• A description of the Plan’s standard, if any, that was used in making the determination;
• A statement of your right to request an external review and a description of the Plan’s internal appeals and external review
procedures and the time limits applicable to such procedures, including information about how to initiate an appeal and an external
review;
• A statement informing you that if your treating physician certies in writing that you have a medical condition for which the time
frame for completion of an expedited review of an internal appeal involving an adverse benet determination would seriously
jeopardize your life or health or jeopardize your ability to regain maximum function, you may le a request for an expedited external
review to be conducted simultaneously with the expedited internal appeal, pursuant to Section 3922.09 of the Ohio Revised Code;
and
• The availability of, and contact information for, the Ohio Department of Insurance, who may assist you with the internal appeals and
external review processes.
• If an internal rule, guideline, protocol, or other similar criterion was relied upon in making the adverse benet determination, either
the specic rule, guideline, protocol, or other similar criterion will be provided free of charge to you, or you will be informed that such
rule, guideline, protocol, or other criterion will be provided free of charge to you upon request.
CONTINUED ON PAGE 88
CLAIM DETERMINATION AND APPEAL PROCEDURES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 88 of 92
Revised 09/2023
Mandatory Internal Appeal
• If your coverage under the Plan is rescinded, you have the right to appeal the adverse benet determination by sending a written
request for review, in a form prescribed by the University, to the Ofce of Human Resources, Benets Services/Appeals, Suite 300,
1590 North High Street, Columbus, Ohio 43201-2190 or by fax (614-292-7813) within 180 days following your receipt of notice of
the adverse benet determination. Your written request should state why you think your coverage should not have been rescinded
and should include any adverse benet determination notice you received and any additional documents, records, information or
comments you think may have a bearing on your claim. Upon your request, you will be provided, free of charge, reasonable access to,
and copies of, all documents, records and other information relevant to your claim.
• Upon receipt of your request, the University’s Ofce of Human Resources will conduct a review that takes into account all comments,
documents, records and other information submitted by you relating to the rescission of your coverage, without regard to whether
such information was submitted or considered in the initial adverse benet determination. The review will not afford any deference
to the initial adverse benet determination and will be conducted by an individual who is neither the individual who made the
adverse benet determination that is the subject of your appeal, nor the subordinate of such individual.
If Your Claim Is Denied Upon Mandatory Internal Appeal
If your internal appeal is denied (a “nal adverse benet determination”), you will be notied of the following, in a manner to be
understood by you:
• Information sufcient to identify the claim or health care service involved;
• A discussion of the determination;
• The specic reason or reasons for the adverse benet determination;
• Reference to the specic Plan provisions on which the benet determination is based;
• A description of the Plan’s standard, if any, that was used in making the determination;
• A statement that you are entitled to receive, upon request and free of charge, reasonable access to, and copies of, all documents,
records and other information relevant to your claim;
• A statement of your right to request an external review within 180 days after the date of the notice of the nal adverse benet
determination and a description of the Plan’s internal appeals and external review procedures and the time limits applicable to such
procedures, including information about how to initiate an appeal and an external review;
• A statement informing you that if your treating physician certies in writing that you have a medical condition for which the
time frame for completion of a standard external review pursuant to Section 3922.08 of the Ohio Revised Code would seriously
jeopardize your life or health or would jeopardize your ability to regain maximum function, you may le a request for an expedited
external review pursuant to Section 3922.09 of the Ohio Revised Code; and
• The availability of, and contact information for, the Ohio Department of Insurance, who may assist you with the internal appeals and
external review processes.
• If the University’s Ofce of Human Resources relied upon an internal rule, guideline, protocol, or other similar criterion in making
the nal adverse benet determination, either the specic rule, guideline, protocol, or other similar criterion will be provided free of
charge to you, or you will be informed that such rule, guideline, protocol, or other criterion will be provided free of charge to you upon
request.
VOLUNTARY EXTERNAL REVIEW PROCESS
If the Plan makes an adverse benet determination with respect to all or any portion of your initial claim or your claim on your
mandatory internal appeal, you may be entitled to obtain an independent external review pursuant to Ohio law by an accredited
independent review organization (IRO) or by the Ohio Department of Insurance.
External Review by an Independent Review Organization
• Generally. External review by an IRO is available only when (1) the adverse benet determination involves a medical judgment or
is based on any medical information, or (2) the adverse benet determination indicates that the requested service is experimental
or investigational (and is not a health care service that is explicitly listed as an excluded benet under the Plan) and your treating
physician certies that one of the following situations is applicable: (a) standard health care services have not been effective in
improving your condition; (b) standard health care services are not medically appropriate for you; or (c) no available standard
health care service covered by the Plan is more benecial than requested health care service; or (3) the adverse determination
involves whether the Plan is complying with the surprise billing and cost-sharing protections under the No Surprises Act and its
implementing regulations. An external review by an IRO may either be standard or expedited.
• Expedited Review. An expedited review is available after an adverse benet determination only if your treating physician certies
that the adverse benet determination involves a medical condition that could seriously jeopardize your life or health if treated
after the time frame of an expedited internal review and you have led a request for an expedited internal review. An expedited
review is available after a nal adverse benet determination if either (1) your treating physician certies that the adverse benet
determination involves a medical condition that could seriously jeopardize your life or health, or would jeopardize your ability to
regain maximum function, if treated after the time frame of a standard external review, or (2) the adverse benet determination
concerns an admission, availability of care, continued stay, or health care service for which you received emergency services but have
yet to be discharged from the facility. An expedited external review may not be provided for a retrospective nal adverse benet
determination.
CONTINUED ON PAGE 89
CLAIM DETERMINATION AND APPEAL PROCEDURES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 89 of 92
Revised 09/2023
• Required Exhaustion of Mandatory Internal Appeals for Standard Review. A standard review (including a standard review involving
experimental or investigational treatment) is not available unless you have exhausted the Plan’s mandatory internal appeal process
described previously. However, exhaustion is not required when: (1) the Plan agrees to waive the exhaustion requirement, (2) you
did not receive a written decision of your internal appeal within the required time frame, (3) an expedited external review is sought
simultaneously with an expedited internal review in accordance with these procedures and applicable state law, or (4) the Plan
fails to adhere to all of the requirements of the internal appeal process, except for de minimis violations that do not cause or are
not likely to cause you prejudice or harm, are for good cause or due to matters beyond the control of the Plan, occur in the context
of an ongoing, good faith exchange of information between the Plan and the covered person and are not reective of a pattern or
practice of non-compliance. Notwithstanding the foregoing, in the case of an adverse benet determination involving a retrospective
review determination made pursuant to a utilization review, you must exhaust the mandatory internal appeals process even if you
do not receive a written decision of your internal appeal within the required time frame and even if the Plan fails to adhere to all
requirements of the internal appeal process.
• Appeal of Denial of Request for External Review for Failure to Exhaust Mandatory Internal Appeals. If the Plan denies your request
for external review on grounds that the mandatory internal appeal process has not been exhausted despite de minimis violations of
that process, you may request written explanation from the Plan and the Plan shall provide its explanation within ten days, including
a specic description of its basis for asserting that the delay should not cause the internal appeals process to be considered
exhausted. You may request review by the Ohio Department of Insurance of this explanation. If the Ohio Department of Insurance
afrms the Plan’s explanation, you may, within 10 days of receipt of the Ohio Department of Insurance’s notice of decision, resubmit
and pursue the internal appeal process.
External Review by Ohio Department of Insurance
You may be eligible for external review by the Ohio Department of Insurance of an adverse benet determination: (1) involving a
contractual issue that did not involve a medical judgment or any medical information or (2) in which emergency medical services have
been determined to be not Medically Necessary or appropriate after an external review by an IRO.
Requesting an External Review
You must request an external review of a nal adverse benet determination, in a form prescribed by the Ohio Department of
Insurance, within 180 days of the date you received notication of the determination. The request must be in writing, except that a
request for an expedited review may be made electronically or orally, provided that you submit written conrmation of the request to
the Plan no later than 5 days after the request is made. When ling a request for an external review, you will be required to authorize
the release of your medical records as necessary to conduct the external review.
Evaluation of a Request for External Review
If your request for external review is complete, OSUHP will send you written notice conrming that your request is complete and
providing you with the name and contact information of the assigned IRO or the Ohio Department of Insurance (as applicable) and a
statement that you may submit additional information for consideration within 10 business days after receipt of the notice, except in
connection with a request for an expedited review (including an expedited review involving experimental or investigational treatment).
If your request for external review is not complete, OSUHP will inform you in writing and specify the additional information you need to
provide. If the Plan determines that the adverse benet determination is not eligible for external review, the Plan will send you written
notice with the reason for the denial and inform you that you may appeal the denial to the Ohio Department of Insurance. The Ohio
Department of Insurance may determine that your request is eligible for external review regardless of the decision by the Plan.
Assignment of Independent Review Organization
If an external review of an adverse benet determination by an IRO is granted, the Ohio Department of Insurance shall assign an IRO
to conduct the external review.
Reconsideration of Adverse Benet Determination by Plan
Except in the case of an expedited external review, the IRO will forward to the Plan, upon receipt, any additional information it receives
from you. The Plan may reconsider its adverse benet determination and provide coverage for the health care service. Reconsideration
will not delay or terminate the external review. If the Plan reverses its previous adverse benet determination, it will notify you, the
assigned IRO and the Ohio Department of Insurance within one day of the decision. The IRO will terminate its review upon receipt of
this notice.
Consideration and Determination of External Review by Independent Review Organization
In addition to the documents and information provided by the Plan relating to its adverse benet determination and any additional
information provided by you, the IRO also will consider, if available and appropriate: (1) your medical records, (2) the attending health
care professional’s recommendation, (3) consulting reports from appropriate health care professionals and other documents submitted
by the Plan, you, or the treating provider, (4) the terms of coverage under the Plan to ensure the decision is not contrary to the terms of
the Plan and (5) the most appropriate practice guidelines, including evidence-based standards and guidelines. The IRO is not bound by
any decisions or conclusions reached by the Plan during its utilization review process or internal appeals process.
CLAIM DETERMINATION AND APPEAL PROCEDURES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 90 of 92
Revised 09/2023
The assigned IRO must provide a written notice of its decision within 30 days after receipt by the Plan of a request for standard
review (including a standard review involving an experimental or investigational treatment) or within 72 hours of receipt by the
Plan of a request for expedited review. This notice will be sent to you, the Plan and the Ohio Department of Insurance. The notice
will include the following information: (1) a general description of the reason for the request for the review, (2) the date the IRO was
assigned, (3) the dates over which the review was conducted, (4) the date the IRO decision was made, (5) the rationale for the IRO’s
decision and (6) references to the evidence or documentation that was used to reach the decision. If the IRO overturns the Plan’s
decision, upon receipt of the notice, the Plan will immediately provide coverage for the health care service.
Any statute of limitations or other defense based upon timeliness is tolled during the time that any properly initiated independent
external review is pending. There is no charge for you to initiate an independent external review. The external review decision
is nal and binding on all parties except to the extent you or the Plan have other remedies available under applicable federal or
state law, or unless the Ohio Department of Insurance determines that, due to the facts and circumstances of an external review,
a second external review is required. You may not le a subsequent request for external review involving the same adverse benet
determination for which you already received an external review decision, except in the event that new medical or scientic evidence
is submitted to the Plan.
CLAIM DETERMINATION AND APPEAL PROCEDURES
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

PAGE 91 of 92
Revised 09/2023
IF YOU HAVE QUESTIONS ABOUT YOUR RIGHTS OR NEED ASSISTANCE
YOU MAY CONTACT:
Ohio Department of Insurance
ATTN:
Consumer Affairs
50 West Town Street, Suite 300
Columbus, OH 43215
800-686-1526 / 614-644-2673
614-644-3744 (fax)
614-644-3745 (TDD)
Contact ODI Consumer Affairs:
https://gateway.insurance.ohio.gov/UI/ODI.CS.Public.UI/Comment.mvc/DisplayCommentSubmission
File a Consumer Complaint:
https://gateway.insurance.ohio.gov/UI/ODI.CS.Public.UI/Complaint.mvc/DisplayConsumerComplaintForm
The Ohio State University Ofce of Human Resources
Faculty and Staff Health Plans Specic Plan Details Document, Effective January 1 – December 31, 2024

