
The Costs of Cancer
2020 Edition
Cancer Acti
on
Network
SM

2 American Cancer Society Cancer Action Network The Costs of Cancer 2020
The American Cancer Society Cancer Action Network
SM
(ACS CAN)
is making cancer—and the affordability of cancer care—a top priority
for public officials and candidates at the federal, state and local levels.
ACS CAN is the American Cancer Society’s nonprofit, nonpartisan advocacy affiliate. ACS CAN
empowers advocates across the country to make their voices heard and influence evidence-based
public policy change, as well as legislative and regulatory solutions that will reduce the cancer burden.
This ACS CAN report focuses specifically on the costs of cancer borne by patients in active cancer
treatment as well as cancer survivors. It examines the factors contributing to the cost of cancer care,
the types of direct costs patients face and the indirect costs associated with cancer. To more fully
illustrate what people with cancer actually pay for care, the report also presents scenario models for
several types of cancer and different types of insurance coverage. Finally, the report presents public
policy recommendations for making cancer treatments more affordable for patients, survivors and the
health care system as a whole.
Published October 2020
For more information regarding the methodology of the modeled patient cost scenarios in this report,
and to view additional materials related to this report, please visit www.fightcancer.org/costsofcancer.
This report was supported in part by grants from the Association for Accessible Medicines and
its Biosimilars Council, AbbVie, the Biotechnology Innovation Organization, Boehringer Ingelheim,
Foundation Medicine, Janssen, Merck, Mylan, Pfizer, Sandoz and Sanofi.
Cancer Acti
on
Network
SM

3American Cancer Society Cancer Action Network The Costs of Cancer 2020
National Cancer Costs Projected to Increase Drastically by 2030
$ 250
B
$ 200 B
$ 150 B
$ 100 B
$ 50 B
$ 0 B
2015
$182.6B
2020
$200.7B
2025
$222.2B
2030
$245.6B
34% increase
Source: Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR. Medical Care Costs Associated with Cancer Survivorship in the United States.
Cancer Epidemiol Biomarkers Prev June 10 2020 DOI: 10.1158/1055-9965.EPI-19-1534
Spending on Cancer Care—in 2019 billions of dollars
4%
5%
10%
33%
49%
Medicaid
Medicare
Other
Patient Out-of-Pocket
Costs = $5.6 billion
Private
Insurance
Everyone Pays the Costs of
Cancer Treatment
Introduction
The American Cancer Society (ACS) estimates that roughly 1.8
million new cases of cancer will be diagnosed in the U.S. in 2020
and that more than 16.9 million Americans living today have a
cancer history.
1
As a leading cause of death and disease in the U.S.,
not only does cancer take an enormous toll on the health of patients
and survivors—it also has a tremendous financial impact.
Patient Costs are Unaffordable
For patients and their families, the costs
associated with direct cancer care are staggering.
In 2018 cancer patients in the U.S. paid $5.6
billion out of pocket for cancer treatments,
2
including surgical procedures, radiation
treatments and chemotherapy drugs.
Overall Cancer Costs are Rising
Cancer also represents a significant portion of
total U.S. health care spending. Approximately
$183 billion was spent in the U.S. on cancer-
related health care in 2015, and this amount is
projected to grow to $246 billion by 2030—an
increase of 34%.
These high costs are paid by people with
cancer and their families, employers, insurance
companies and taxpayer-funded public programs
like Medicare and Medicaid.
Source: Data retrieved from the Agency for Healthcare Research and Quality.
Medical Expenditure Panel Survey, 2018. https://meps.ahrq.gov/mepsweb/
*See reference for category definitions.
3
Percentages in chart have been
rounded.

4 American Cancer Society Cancer Action Network The Costs of Cancer 2020
The Costs of Cancer Do Not Impact
All Patients Equally
Because of high costs, many people with cancer
and those who have survived cancer experience
financial hardship, including problems paying bills,
depletion of savings, delaying or skipping needed
medical care, and potential bankruptcy. These
costs and hardships do not impact all cancer
patients equally—there are certain factors that
make a patient more likely to experience
financial hardship:
60%
70%
50%
40%
30%
20%
10%
0%
Ages 18-54
58.9%
Ages 55-64
48.5%
Cancer patients are more likely to experience financial hardship if they are:
Younger
60%
70%
50%
40%
30%
20%
10%
0%
Other Races/
Ethnicities
63.5%
Non-Hispanic Whites
50.9%
People of Color
60%
70%
50%
40%
30%
20%
10%
0%
Less than high
school graduate
69.5%
52.1%
Some college or
more
High school
graduate
51.8%
Less Educated
60%
70%
50%
40%
30%
20%
10%
0%
Low-income
(≤138% FPL)
60.0%
60.5%
High-income
(>400% FPL)
Middle-income
(139-400%FPL)
47.2%
Lower Income
*
FPL = Federal Poverty Level
S
ource: Han X, Zhao J, Zheng Z, de Moor JS, Virgo KS, Yabroff KR. Medical Financial Hardship Intensity and Financial Sacrifice Associated with Cancer in the
United States. Cancer Epidemiol Biomarkers P
rev. 2020;29(2):308-317. doi:10.1158/1055-9965.EPI-19-0460
Note that similar patterns of disparities e
xist in the over-65 population.
% of Individuals with a History of Cancer Reporting at least 1 Ty pe of Financial Hardship, Ages 18-64
The Costs of Cancer Disparities
Cancer and its costs do not impact all
individuals equally. Look for information about
The Costs of Cancer Disparities throughout
this report.

5American Cancer Society Cancer Action Network The Costs of Cancer 2020
Factors Contributing to the Costs of Cancer
With more than 200 different types of cancer, there is no “one
size fits all” cancer treatment—and therefore the costs of cancer
treatment vary significantly from patient to patient. However, there
are several consistent factors that contribute to patients’ overall
costs for their care.
Insurance Status/Type of Insurance Coverage:
Patients without health insurance are responsible
for all of their treatment costs. Some uninsured
patients may qualify for “charity care,” may be able
to participate in drug discount programs to reduce
their costs or may be able to negotiate discounts
with providers. For patients with insurance, the
kind of health insurance the patient has and
the design of their plan are some of the most
important factors in determining the ultimate costs
for patients. Patient costs are often referred to
as cost sharing or an out-of-pocket requirement.
Following are some of the out-of-pocket
components that determine what patients pay:
■
Premium: The monthly amount the patient
pays to stay covered by the insurance plan (in
some cases an employer pays all or part of a
patient’s premiums). Premiums are determined
by a number of factors that differ depending
on type of insurance and can include: age of
the enrollee, where the enrollee lives, how
generous the benefits are (including cost-
sharing amounts listed below) and how much
the plan anticipates it will pay in health care
claims for enrollees. While many enrollees focus
only on premium prices, the other out-of-pocket
costs listed below offer a
more complete picture of
what patients ultimately pay.
For instance, enrollees who
are high utilizers of care—
including those with cancer—
often face a trade-off of
higher premiums for lower
out-of-pocket costs and vice
versa.
■
Deductible: The amount the patient must first
pay out of pocket for care before the insurance
plan will start covering costs. Some plans have
separate deductibles for medical services,
drugs, and/or out-of-network services. High
deductible health plans—defined in 2020 as
plans with a deductible of $1,400 or higher
for individuals or $2,800 for families—are
becoming more prevalent in the U.S.
4
■
Co-payment or Co-pay: A flat fee patients
pay per health care service, procedure or
prescription.
■
Co-insurance: A percentage patients pay
of the total cost of a prescription, service or
procedure. Co-insurance can be unpredictable
because the patient often cannot determine the
total cost of the treatment until arriving at the
pharmacy or receiving a bill after the treatment.
■
Out-of-Pocket Maximum or Out-of-Pocket
Cap: The limit on what a patient must pay each
year before the health plan starts to pay 100%
for covered, in-network benefits. This amount
excludes premiums. Current law establishes
these caps in most private insurance plans.
Caps provide a crucial protection to patients
with high health care costs.
■
In-Network vs. Out-of-Network: Many health
insurance plans have “networks” of doctors,
hospitals, and pharmacies. If a patient goes to
an “in-network” provider, cost sharing is usually
lower because the insurer has negotiated
rates with the provider. Some insurance plans
Current law requires many private
insurance plans to limit annual patient
out-of-pocket spending. The 2020 limit
is $8,150 for an individual plan and
$16,300 for a family plan.
Survivor Views: The Costs of Cancer in
Their Own Words
“I had good insurance through my husband’s
work, but our deductibles were always
high. We met our deductible twice with my
cancers, we have never met it otherwise.
The benefits after meeting the deductible
were nice, but we had to put all of our bills
on payment plans and most would go into
collections even though we were paying
them. When you are paying 8 different bills
for thousands of dollars, and one person is
working with the cost of living and food,
there is little to go around.”
Ovarian Cancer Survivor, Ohio

6 American Cancer Society Cancer Action Network The Costs of Cancer 2020
charge more cost sharing for “out-of-network”
providers, while other plans do not cover out-of-
network providers at all. Out-of-network costs
do not always count towards the patient’s out-
of-pocket maximums.
■
Balance Billing and Unexpected Costs:
Patients may also encounter unanticipated
costs. Their plan may not cover a treatment
they received, they may have used a provider
who was not in-network, or their plan did not
reimburse the provider for the full amount billed
and the patient has to pay the difference (this is
sometimes called “balance billing” or “surprise
billing”). The amount of these surprise bills often
does not count toward the patients’ out-of-
pocket maximum.
Other factors contributing to
costs variations are:
Treatment Plan: The type of treatment (surgery,
radiation, chemotherapy, etc.) and how much
treatment (duration, number of drugs, number
of surgeries, etc.) the patient receives causes
costs to vary significantly. Note that the stage
at which a patient is diagnosed is an important
factor in determining a patient’s treatment plan,
the potential outcome and the treatment costs. In
some cases, doctors and patients have choices
between treatment regimens and can consider
costs in their decision. In other cases, there is only
one treatment option.
Geographic Location: Costs vary based on
where the patient lives and how many providers
are available in that area. Areas that generally
have high costs of living also tend to have higher
treatment costs.
Treatment Setting: Treatment charges are based
on many factors, and the costs to the patient may
differ depending on whether care is delivered in a
hospital, clinic or physician’s office (for example,
many hospitals charge facility fees that increase
costs for patients). Sometimes patients may have
a choice where they receive treatment, but other
times they do not have a choice and must incur
additional cost. Regardless of setting, it is difficult
for patients to obtain price information in order to
make comparisons.

7American Cancer Society Cancer Action Network The Costs of Cancer 2020
Key Terms
■
Medical Benefit: the benefits covered by a health plan. Generally, medical benefits include
coverage for hospital visits, doctor visits and various kinds of tests. In some cases, a health plan
has a separate pharmacy benefit that provides coverage for outpatient prescription drugs
■
Formulary: the list of drugs and pharmacological therapies covered by a health plan.
Formularies often sort drugs into tiers, which are groups of drugs assigned a certain co-pay or
co-insurance.
■
Medicare: the federal government program providing health coverage to Americans age 65
and older, as well as some individuals with disabilities. Medicare has several parts: Part A covers
hospitalization, Part B covers physician and outpatient services (including physician-administered
drugs), and Part D covers oral drugs.
Part C offers private plans that cover hospitalizations, physician and outpatient services. Some
individuals also have a Medigap plan (otherwise known as a Medicare Supplemental plan), which
reduces cost sharing required in Parts A and B.
■
Medicaid: Joint federal-state government program that provides health insurance coverage to
qualifying people with low-incomes, people who are pregnant, children, seniors, and people with
disabilities.
■
Employer-Sponsored Insurance: Health insurance provided through an individual’s employer.
This type of insurance is also usually provided to the individual’s spouse and/or dependents
■
Individual Marketplace Insurance: Insurance purchased by individuals, not offered by
employers or other groups. All individuals have access to either a state-based or federal
Exchange that sells these plans which meet Affordable Care Act standards.
■
Short-Term, Limited-Duration Plan: A private health insurance plan that provides coverage
to policyholders for a period of as little as a month to as long as three years. These plans offer
limited coverage and benefits and are not required to implement the same consumer protections
as other plans.
8 American Cancer Society Cancer Action Network The Costs of Cancer 2020
“Surprise medical billing” or “balance billing” is when an insured
patient is unknowingly treated by an out-of-network provider and is then
billed the difference between what the provider charged and what the
insurer paid. Surprise bills can be significantly higher than the consumer’s
standard in-network cost sharing. They occur most often with ancillary
providers—like anesthesiologists and emergency room physicians.
In an October 2019 survey, ACS CAN asked cancer patients and
survivors about their experiences with surprise bills through its Survivor
Views panel.
5
■
24% of respondents reported having received a surprise bill as a
result of their cancer care.
■
28% of these surprise bills were for $2,000 or higher.
Types of Cancer Treatment Costs
There are traditionally three primary approaches to treating
cancer: surgery, radiation and pharmacological therapy
(including chemotherapy, targeted therapy, hormone therapy
and immunotherapy). Some patients receive all three treatment
modalities, while others receive one or two types. Costs to the
patient vary depending on the type and extent of the treatment.
Surgery: Surgery can be used to remove tumors,
diagnose cancer and/or to find out how far
a cancer has spread. Many people who have
cancer have surgery at least once as part of their
treatment. Surgery can involve multiple medical
providers, hospitals or specialized facilities and
other elements that result in multiple charges
to patients and health insurers. Patients may
be assessed additional facility and other fees
associated with where the surgery is performed.
If a provider is not in-network, a plan may not
cover as much (or any) of the cost for the out-
of-network provider or service. This can lead
the patient to receive unexpected medical bills,
sometimes known as “balance bills” or “surprise
medical bills.” Some insurance plans may require
the patient to pay co-insurance for each service
or a bundle of services, and others have a flat
co-pay per day or per hospital admission. Covered
surgery and associated care are generally
included under a plan’s medical benefit.
Radiation: Radiation therapy uses waves or
high energy particles to destroy or damage
cancer cells. Most patients who receive radiation
treatments do so at a hospital or cancer treatment
facility. Radiation treatment requires complex
equipment and a team of health care providers.
Treatment protocols vary, but some cancer
patients receive radiation daily or several times
a week for many weeks, which contributes to
relatively high patient costs. Patients who have
not yet met their out-of-pocket maximum will
likely be required to pay co-pays per visit or co-
insurance based on the total cost of treatment.
Covered radiation is generally included under a
plan’s medical benefit (or, in the case of Medicare,
under Part B).
Pharmacological Therapy: Medication is a
very common part of cancer treatment. This
can include chemotherapy, targeted therapy,
immunotherapy, hormone therapy and/
or supportive care like pain or anti-nausea
medication. Some of these drugs can be taken as
pills obtained through mail-order or at a pharmacy,
and some are administered intravenously (IV) in
a doctor’s office, clinic or hospital. In most cases,
covered IV drugs are included under a plan’s
medical benefit; while covered drugs taken as
pills or orally and obtained at a pharmacy are
included under a plan’s pharmacy benefit. This
difference is important because cost sharing
is often different for these benefits, and some
plans have separate medical and pharmacy
deductibles. Co-pays and co-insurance are both
common forms of patient cost sharing for drugs.
These tiers are groupings of drugs—like “generic,”
“preferred,” “non-preferred,” and “specialty,” and
sometimes combinations thereof. Each tier has
its own co-pay or co-insurance, which makes
understanding patient out of pocket costs more
complex. Covered pharmacological therapy is
generally included in insurance policies as a
separate pharmacy benefit.
New Therapies: Fortunately, oncology treatment
is a very active area of research and development
for government agencies—such as the National

9American Cancer Society Cancer Action Network The Costs of Cancer 2020
Cancer Institute—as well as for academic and
industry researchers. Decades of significant
investment is resulting in a steady stream of new
treatments becoming available to cancer patients
and their providers. Many of these new treatments
are pharmacological. Some innovations—like
chimeric antigen receptor therapy (CAR-T), which
takes a patient’s own immune system cells and
changes them in a laboratory to attack cancer
cells before re-infusing them
6
—belong in their
own unique category. Some new personalized
therapies require biomarker testing (sometimes
called “genomic testing”) to determine if the
patient has the particular type of cancer the
personalized therapy treats.
Because of the way industry recoups costs for
research and development, a newer treatment
is likely to be more expensive than when it has
been used for many years and competitors
have developed generic or biosimilar versions
of the drug. This often results in higher out-of-
pocket costs for a patient using a new treatment,
especially if they must pay co-insurance, cannot
use copay assistance, or are uninsured. Also, if a
treatment is very new, a patient’s insurance plan
may not have added it as a covered benefit yet or
may consider it ‘experimental.’ In these situations,
a patient may be able to appeal to their insurance
plan for coverage of the treatment–otherwise
their out-of-pocket costs will likely be very high
for an uncovered treatment or a patient may opt
to go without the treatment.
Other Types of Cancer Care Costs: While
surgery, radiation and pharmacological therapy
are the three most common approaches to cancer
treatment, patients may utilize other regimens like
stem cell transplants, hyperthermia, photodynamic
therapy and blood transfusions. Cancer patients
also often need treatments such as supportive or
palliative care, rehabilitative therapy, mental health
services, nutrition counseling and cardiology
consultations as a result of their cancer or
treatments.
7
It is also important to note that these various
forms of treatment require multiple types of health
care personnel. It is very common for people
with cancer to see multiple health care providers
during the course of their treatment, including
primary care doctors, specialists for diseases and
side effects developed as a byproduct of cancer
treatment (like cardiologists, neurologists and
endocrinologists), medical oncologists, radiation
oncologists, surgeons, palliative care specialists,
rehabilitation specialists, physical therapists and
nutritionists. The complexity of cancer treatment
and the necessity of multiple specialists are
large drivers of cancer patient costs. Many health
insurance plans charge higher co-pays or co-
insurance amounts for specialist visits compared
to primary care. Additionally, very specialized
providers are often in short supply, and patients
are sometimes forced to go out-of-network to see
a specialist. This is especially likely for patients
who live in more rural areas.
Rural residents are more likely than their
urban counterparts to have higher rates of
unemployment and lack of health insurance.
10
Survivorship Care Costs: It is also important
to note that even when a person with cancer
has completed their surgery, radiation and/
or chemotherapy, the costs of care do not end
immediately. Many cancer survivors deal with
cancer symptoms and side effects of treatment
months to years after finishing treatment—
sometimes for the rest of their lives. Some cancer
survivors also must take treatments long-term, like
a 10-year regimen of hormone therapy to prevent
breast cancer recurrence. This means many of
the costs discussed in this section, including
for seeing specialist providers like rehabilitation
therapists and psychotherapists, can continue
for years for cancer survivors. In fact, research
shows that annual health care expenditures for
cancer survivors are significantly higher than for
individuals who have never had cancer.
11
Indirect
costs of cancer—explored on the next page—also
often continue into survivorship.
Survivor Views: The Costs of Cancer in
Their Own Words
“One of the most surprising things is the cost
of care AFTER active cancer treatment. I have
lymphedema and the costs are significant,
including various equipment, DME [durable
medical equipment], compression clothing,
and physical therapy. I didn’t realize the costs
would continue after active treatment.”
Breast Cancer Survivor, Arizona
The Costs of
Cancer Disparities
■
Urban areas have
approximately 5
times the number
of oncologists
compared to rural
areas.
8
■
Rural patients have
to travel nearly
twice as long one-
way as urban and
suburban patients
in order to see their
cancer doctor.
9

10 American Cancer Society Cancer Action Network The Costs of Cancer 2020
The Indirect Costs of Cancer
This report focuses on the direct costs of cancer—health care
expenses directly for or related to cancer treatment—but there
are other indirect costs that are just as significant and potentially
problematic for people with cancer and their families.
Survivor Views: The Costs of Cancer in Their Own Words
“ Being diagnosed with cancer six years ago has caused me financial difficulties,
stress, and anxiety. Although I am in remission, I continue to have adverse effects
from my treatment. I spend 2-4 days per week in a doctor’s office and also had to
be treated out of state twice in 2019. Each time I go out of state I am spending a
minimum of $1500. While we are fortunate my husband is well enough to work which
helps pay for my medical bills and expenses, it’s still a financial strain on us.
I am still not able to return to work so we are a one-income family. I don’t know how
others who don’t have a moderate salary are able to afford it. If the ACA [Affordable
Care Act] goes away, I will likely be penalized for my preexisting conditions. I am so
nervous that my medications, physical therapy, treatments, and diabetic supplies will
not be covered.”
Leukemia Survivor, Alaska
Transportation
Some patients have to travel significant distances to
medical appointments and the pharmacy
Lodging
Some cancer patients must travel to receive
treatments, like specialized surgeries, and need a
place to stay near their treatment site
Lost wages or income
Some cancer patients must stop working temporarily
or permanently, or reduce their work schedules
Secondary Effects
Some patients must treat or deal with secondary effects
of cancer or treatment, like fertility treatments, wigs and
cosmetic items, or the cost of special food
Caregiving costs
Some patients may need to pay for help at home to
care for themselves, or for their children
As these are indirect costs, most of them are difficult to quantify and track. But these costs are
significant for people with cancer and their families, adding to the overall costs of cancer care
and also contributing to the “financial toxicity” of cancer.

11American Cancer Society Cancer Action Network The Costs of Cancer 2020
Patient Profiles: Cost Scenarios
Because of the complexity and variation in cancer treatment, it
is difficult to predict the full costs for any individual with cancer
at the time of diagnosis. The following illustrative patient profiles
and associated data represent the typical costs for several
cancer scenarios. The patients are hypothetical, but the treatment
regimens are typical treatments for each specific cancer with the
corresponding actual costs.
Experts at ACS and ACS CAN constructed
profiles of several typical cancer patients. The
types, stages, and details of cancer represented
in these profiles were chosen based on cancer
incidence rates and the need to represent
a diverse set of people with cancer and
experiences. Clinical experts determined the
usual course of treatment for these patients
based on the National Comprehensive Cancer
Network (NCCN) treatment guidelines for each
of the cancers. Estimates for patient out-of-
pocket costs for each of these patients were
based on common insurance scenarios. Note that
some patient profiles were used to run multiple
insurance scenarios for comparison and analysis
purposes—combinations of profiles and insurance
design scenarios that are not reflected in this
section will be discussed in future sections.
All prices and insurance designs are based
on 2020 data. See methodology appendix for
more details, published at www.fightcancer.org/
CostsofCancer.
These patient profiles represent typical scenarios
and timelines. They help illustrate the costs that
cancer patients and health care payers incur for
an individual’s cancer treatments. Note that these
scenarios do not include costs for other health
care treatments unrelated to cancer (for example,
if a patient has asthma, the costs to treat asthma
are not included). Also note that these scenarios
are unable to incorporate all the problems people
with cancer face, including tests that have to be
repeated and delayed timelines.
Shonda—
Pancreatic Cancer
Medicare
Carla—
Breast Cancer
Small Employer, High Deductible Health Plan
Kathy—
Lung Cancer
Individual Market Plan
Brian—
Lymphoma
Short-term Limited Duration Plan
Franklin—
Prostate Cancer
Large Employer Plan
Tom—
Colorectal Cancer
Medicare

12 American Cancer Society Cancer Action Network The Costs of Cancer 2020
Tom—Colorectal Cancer
Medicare
Case Study: Colorectal Cancer—
Medicare Coverage
In January, Tom’s fecal immunochemical test (FIT) test was positive indicating that he might have colon
cancer. His primary care doctor sent him to a gastroenterologist (GI) specialist, who ordered a colonoscopy.
Tom received his colonoscopy at a hospital outpatient center. During the colonoscopy his doctors
discovered 2 adenomatous polyps, which were removed, and a lesion suspicious for colon cancer. The lesion was
biopsied, and Tom was diagnosed with Stage IIB colon cancer.
In February, Tom had blood tests and a CT scan to check for possible spread of the disease.
In March, Tom had colectomy surgery to remove the lesion and surrounding tissue, and a lymphadenectomy to
test if the cancer had spread. Tom’s cancer tissue was also tested to see if he had any biomarkers that
would point his doctors towards the right drug regimen.
In April and May, Tom received chemotherapy to treat his cancer and prevent reoccurrence, and supportive
care drugs, like anti-nausea medication, to ease side effects.
Tom finished his treatments in May and began post-treatment follow-up, including regular doctor’s visits
and blood tests.
Throughout his treatment, Tom met with several practitioners and specialists, including his primary care
doctor, a GI specialist, a surgeon, oncologists, and oncology nurses.
Tom had health insurance coverage through
Medicare and Medigap. His premiums were:
Medicare Part A - $0/month
12
Medicare Part B - $145/month
13
Medigap (Policy G) - $236/month
Medicare Part D - $25/month
Tom’s highest total spending came in April and
May ($767 in April and $612 in May) when some
of his chemotherapy and supportive care drugs
were paid for through his Medicare Part D plan.
Otherwise, Tom’s Medigap plan protected him
from high fluctuating out-of-pocket costs. In total
Tom paid $405 in premiums every month. At the
end of his plan year, he had paid a total of $4,864
in premiums and $568 in cost-sharing—a total
of $5,432—for his cancer care.*
The total health care costs for Tom’s
colorectal cancer treatment in 2020 were
$38,035. Medicare and Tom’s Medigap and
Part D plans paid the vast majority of these
costs—$37,467. If Tom had been uninsured, he
would have been responsible for all of these
costs,** and may have been required to pay them
up-front before treatment.
Even though Tom is no longer in active treatment,
he will still require regular follow-up visits with his
oncologist and primary care physician which add
to his costs in future years.
* Note that these costs only include cancer treatment, and do not include
treatment for other conditions that may have developed as a result of the
cancer treatments and/or any other treatments unrelated to cancer care or
other preventive services.
** Costs for an uninsured patient may be higher than this estimate because
uninsured patients do not benefit from a plan’s negotiated discount rate.
However, some uninsured patients are also able to receive charity care,
which discounts or forgives certain treatment costs.

13American Cancer Society Cancer Action Network The Costs of Cancer 2020
Case Study: Breast Cancer—
Small Employer, High Deductible Health Plan
Year One: Carla has her first mammogram in January to screen for breast cancer. Her doctor sees
something suspicious on the images and sends her for several follow-up tests including blood tests, a
breast MRI, CT scans of her chest and abdomen, ultrasounds of her breasts and lymph nodes, and a diagnostic mammogram.
She then has a core needle biopsy in February, and is diagnosed with stage III breast cancer, with a large
tumor and cancer present in her lymph nodes. Molecular tests reveal her cancer is hormone receptor
negative and human epidermal growth factor receptor 2 (HER2) positive.
Carla’s doctors recommend she start neo-adjuvant (before surgery) chemotherapy right away given the
aggressive nature of her cancer. Before she starts this treatment, she consults with a cardiologist about
the way her treatment can impact her heart and has a chemotherapy port installed.
Carla receives multiple cycles of chemotherapy from March through August, along with supportive care
drugs to address symptoms and side effects like nausea. These treatments are successful in shrinking
her tumors but do not fully eliminate them.
In September Carla has local excision and lymphadenectomy surgery to fully remove the tumors, and then begins
adjuvant (post-surgery) radiation therapy to maximize local control of the cancer. In October she also continues
her HER2-targeted therapy infusions, which started before surgery and will continue for one full year. During these
treatments she continues to have blood tests and visits with her oncologist to monitor her treatment progress.
Year Two: January brings the one-year anniversary of the mammogram that caught her breast
cancer—and Carla continues to receive her HER2-targeted therapy treatments, monitoring blood tests, and visits
with her oncologist. She continues these treatments through June, when she completes a full year of
post-surgery HER2-targeted therapy. In the remaining months of her second year, Carla is tested for
lymphedema—a common side effect of breast cancer treatment—and continues to be monitored by her
oncologist. Because Carla still has most of her breast tissue, she must still have a mammogram every year
to look for cancer recurrence or new cancers.
Throughout her two years of cancer treatments, Carla met with several doctors and specialists,
including her primary care doctor, a medical oncologist, radiation oncologist, cardiologist, and a breast surgeon.
Carla is enrolled in a high-deductible health plan
through her small employer. Carla pays $143 per
month in premiums. Note that Carla’s employer
does not offer an accompanying health savings
account.
Carla is required to pay the full amount of her
high deductible—$6,000—and other cost-
sharing in February, when she undergoes most
of her diagnostic tests. Paying these big bills
the same month she received a serious cancer
diagnosis was a struggle. Fortunately, she hits
her maximum out-of-pocket limit of $8,150 in
February and her expenses level off. At the end of
her first plan year, she had paid a total of $1,712
in premiums and $8,150 in cost-sharing for
her cancer care: an annual total of $9,862.*
Carla’s costs continued in the second year after
her diagnosis: in year two she once again paid
a total of $1,712 in premiums and $8,150 in
cost-sharing for her cancer care.
The total health care costs for Carla’s breast
cancer treatment were $222,981 (over two
years). Carla’s insurance plan paid the vast
majority of these costs—$206,681. If Carla had
been uninsured, she would have been responsible
for all of these costs,** and may have been
required to pay them up-front before treatment.
* Note that these costs only include cancer treatment, and do not include
treatment for other conditions that may have developed as a result of the
cancer treatments and/or any other treatments unrelated to cancer care or
other preventive services.
** Costs for an uninsured patient may be higher than this estimate because
uninsured patients do not benefit from a plan’s negotiated discount rate.
However, some uninsured patients are also able to receive charity care,
which discounts or forgives certain treatment costs.
Carla—Breast Cancer
Small Employer, High Deductible Health Plan

14 American Cancer Society Cancer Action Network The Costs of Cancer 2020
Franklin is enrolled in health insurance through
his large employer. Franklin’s employer
contributes $618 per month towards the
premium, and Franklin pays $169 per month.
Franklin has a relatively small deductible ($500)
and maximum out-of-pocket limit ($3,000),
and he reaches that limit by February, when his
out-of-pocket costs level off. At the end of the
year, he had paid a total of $2,030 in premiums
and $3,000 in cost-sharing for his cancer care—
for an annual total of $5,030.*
The total health care costs for Franklin’s
prostate cancer treatment were $100,557.
Franklin’s employer/insurance plan paid the vast
majority of these costs—$97,557. If Franklin had
been uninsured, he would have been responsible
for all of these costs,** and may have been
required to pay them up-front before treatment.
By the end of the year, Franklin had found a
treatment that seemed to be working to fight his
prostate cancer. He will need to continue taking
this medicine for several years and monitoring his
cancer with blood tests and extra doctor’s visits.
Franklin will continue to pay costs related to his
prostate cancer for years to come.
* Note that these costs only include cancer treatment, and
do not include treatment for other conditions that may have
developed as a result of the cancer treatments and/or any
other treatments unrelated to cancer care or other preventive
services.
** Costs for an uninsured patient may be higher than this
estimate because uninsured patients do not benefit from a
plan’s negotiated discount rate. However, some uninsured
patients are also able to receive charity care, which discounts
or forgives certain treatment costs.
Franklin—Prostate Cancer
Large Employer Plan
The Costs of Cancer Disparities
Compared with white men, African American
men are more likely to develop prostate cancer
and are twice as likely to die from the disease.
14
Case Study: Prostate Cancer—
Large Employer Plan
Franklin has a family history of prostate cancer. As part of his annual physical in January, Franklin receives
a digital rectal exam and his primary care doctor orders a PSA blood test. Franklin’s PSA score from this test
is over 10, indicating possible prostate cancer. Franklin’s doctor orders more blood tests, an MRI, bone scan
and CT scan; and refers him to a medical oncologist.
After having a core biopsy in February, the tests determine that Franklin has locally advanced prostate cancer.
Since Franklin has a life expectancy of more than 10 years, and he has an intermediate risk of his
cancer growing quickly, Franklin chooses to have a radical prostatectomy surgery to remove his prostate and
test his lymph nodes. The cancer is found in his lymph nodes, so his treatment continues with a goal of
stopping its spread to other parts of his body.
In March he begins androgen deprivation therapy (ADT), or hormone therapy, which are pills he takes daily.
Because Franklin also has diabetes, his doctor wanted to prescribe a certain drug for his treatment.
However, Franklin’s insurance coverage requires he try a different drug first.
In April he begins radiation treatments, and regular PSA blood tests and doctor’s visits to monitor his progress.
After 4 months of these treatments, he has a new round of blood tests and a bone scan. These tests
find that his PSA level has already doubled, indicating the treatments are not working, and Franklin is
diagnosed with ‘castration-resistant’ prostate cancer. In August he begins taking the hormone therapy his doctor
originally wanted to prescribe, which stabilizes his cancer and he continues this therapy through the
end of the year.
Throughout the course of his treatment, Franklin saw several doctors and specialists, including his
primary care doctor, a medical oncologist, surgical oncologist, and a radiation oncologist.

15American Cancer Society Cancer Action Network The Costs of Cancer 2020
Shonda—Pancreatic Cancer
Medicare
The Costs of
Cancer Disparities
African Americans
are more likely
to be diagnosed
with cancer at an
advanced stage
compared to white
Americans, and they
also have lower
survival within each
stage—further
reflecting inequalities
in access to and
receipt of high-
quality cancer care.
15
Case Study: Pancreatic Cancer—
Medicare Coverage
Shonda is retired and lives in a rural area near her family. In January she has her annual Medicare
wellness exam with her primary care doctor, where she shares that she has been having stomach pains
and digestive issues. Her doctor recommends some diet changes and schedules a follow-up appointment
in March to see if these changes help.
Unfortunately Shonda is still experiencing symptoms in March, so her doctor orders several
blood tests, followed by a CT scan of her pancreas, an endoscopic ultrasound, and an endoscopic retrograde
cholangiopancreatography (ERCP) procedure. The tests continue in April, when she has a biopsy, and CT scans of
her chest and pelvis. After consulting with a medical oncologist and gastroenterologist, Shonda is diagnosed with
metastatic pancreatic cancer. Surgery is not an option because the cancer has spread, so she prepares to
start systemic therapy. Her tumors are tested for biomarkers, but none are found.
Her doctor tells her that she would be a good candidate for a clinical trial, which would be her choice
for first-line treatment. However, the trial is only offered in a major city that is a 5-hour drive from her
home, and her family is not able to travel that far and care for her while receiving treatment.
Shonda must choose a treatment that is available near her home, so she opts to receive chemotherapy
from her local oncologist. In April she has a port installed and is tested for jaundice in preparation for
her treatment. She also consults with a palliative care specialist to discuss her options for symptom and
side effect control during her upcoming treatments.
In May Shonda begins her chemotherapy treatment at her local hospital that her children must drive her to
a few times a month. Treatment includes supportive care drugs, blood tests, and regular CT scans of her pancreas
to monitor progress. She also meets with her oncologist regularly.
After three months of chemotherapy, a scan shows that the treatment is not working to shrink her
cancer. Shonda and her doctor decide to try another drug, so she begins a 2nd-line chemotherapy treatment.
However, her cancer also does not respond to that treatment, and by November, Shonda’s level of pain
and symptom burden is increasing. She develops blockages in her bile ducts and stomach. In consultation with
a palliative care specialist who has been monitoring her treatment, Shonda decides to choose care that is
focused on her comfort, including regular doses of pain medication and the placement of a gastronomy tube
to allow her to receive nutrition directly.
Shonda had health
insurance coverage
through Medicare
and Medigap. Her
premiums for both were:
Medicare Part A - $0/month
16
Medicare Part B - $145/month
17
Medigap (Policy G) - $236/month
Medicare Part D - $25/month
Shonda’s Medigap plan covered all of her cancer
treatment expenses until May, when she began
taking drugs covered through her Part D plan,
which required cost-sharing. In total Shonda paid
$405 in premiums every month. At the end of
her plan year, she had paid a total of $4,864 in
premiums and $1,767 in cost-sharing for her
cancer care, for an annual total cost of $6,631.*
The total health care costs for Shonda’s
pancreatic cancer treatment in 2020 were
$27,911. Medicare and Shonda’s Medigap and
Part D plans paid the vast majority of these
costs—$26,144. If Shonda had been uninsured,
she would have been responsible for all of these
costs,** and may have been required to pay them
up-front before treatment.
She and her family may decide to move her to
hospice care in the future—which will change how
her cancer and supportive care are paid for.
* Note that these costs only include cancer treatment, and do not include
treatment for other conditions that may have developed as a result of the
cancer treatments and/or any other treatments unrelated to cancer care or
other preventive services.
** Costs for an uninsured patient may be higher than this estimate because
uninsured patients do not benefit from a plan’s negotiated discount rate.
However, some uninsured patients are also able to receive charity care,
which discounts or forgives certain treatment costs.

16 American Cancer Society Cancer Action Network The Costs of Cancer 2020
Kathy—Lung Cancer
Individual Marketplace Plan
Case Study: Lung Cancer—
Individual Marketplace Plan
Kathy smoked previously and met high risk criteria for lung cancer, so she had an annual low-dose CT scan
in January to screen for lung cancer. Her primary care doctor told her the scan was positive for a large
mass in her left lung and referred her to a pulmonologist.
Her pulmonologist ordered a CT scan to confirm the first scan’s results. In February, Kathy had several
blood tests and a lung function test. She then had a lung needle biopsy to test cells from the mass in her lung,
a PET/CT scan, a brain MRI, and was referred to a medical oncologist.
Kathy’s oncologist diagnosed her with an adenocarcinoma of the lung. She was told the cancer was Stage
IV, and it had metastasized to her bones. Because the cancer was too widespread, surgery and
radiation were not treatment options. She also had special biomarker tests on her tumor which showed
she was not a candidate to start with targeted therapy.
In March, Kathy began chemotherapy with an immunotherapy treatment at her doctor’s office. She also had a
consultation with a palliative care specialist to discuss her goals and treatment impact on her work and
family and received supportive care drugs to ease side effects. She also began regular PET scans and blood
tests to monitor the progress of the treatment.
In May, Kathy went to the emergency room and was hospitalized for trouble breathing. She stayed in
the hospital for three days. Kathy and her doctor decided to try a second-line treatment, as her
chemotherapy was not working.
In June, Kathy began receiving a second immunotherapy treatment at her doctor’s office. She continued PET
scans and blood tests to monitor progress. The immunotherapy worked to keep her cancer from spreading
and maintained her quality of life, so Kathy continued the treatment and monitoring through the end of
the year.
Throughout the course of her treatment, Kathy saw several doctors and specialists, including her primary
care doctor, a pulmonologist, a medical oncologist, a palliative care specialist, and the doctors who treated her in
the emergency room.
Kathy bought an
individual health
insurance plan through
her state’s marketplace,
which started in January. The premium for plan
was $840 per month, but she qualified for tax
credits which helped reduce these costs. Kathy
ended up paying $325 per month in premiums.
Kathy finished paying her high deductible
($6,500) in February and hit her out-of-pocket
maximum of $8,150 in March. These costs were
challenging to afford in the span of three months.
Fortunately, after her maximum was met she only
had to pay premiums for the rest of the year. At
the end of her plan year, she had paid out-of-
pocket $3,896 in premiums and $8,150 in cost
sharing for her cancer care,* a total of $12,046.
The total health care costs for Kathy’s
cancer treatment were $140,247. Kathy’s
insurance plan paid the vast majority of these
costs—$132,097. Kathy’s out-of-pocket costs
were significant but if she had been uninsured,
she would have been responsible for all of these
costs,** and may have been required to pay them
up-front before treatment.
At the end of the year, Kathy had found an
immunotherapy that had stabilized her cancer.
Kathy will likely continue to take this treatment
for several more months or years—however long
it works—as well as being monitored for further
cancer spread. Kathy will continue paying costs
for cancer treatments into future years.
* Note that these costs only include cancer treatment,
and do not include treatment for other conditions
that may have developed as a result of the cancer
treatments and/or any other treatments unrelated to
cancer care or other preventive services.
**Costs for an uninsured patient may be higher than this
estimate because uninsured patients do not benefit
from a plan’s negotiated discount rate. However, some
uninsured patients are also able to receive charity
care, which discounts or forgives certain treatment
costs.

17American Cancer Society Cancer Action Network The Costs of Cancer 2020
Brian—Lymphoma
Short-term Limited Duration Plan
Case Study: Lymphoma—
Short-term Limited Duration Plan
Brian works several part-time and freelance jobs and buys the cheapest plan he could find through an
insurance broker website, not understanding that this short-term limited duration plan does not cover a
comprehensive set of benefits or have to follow other patient protections.
Brian noticed that his lymph nodes were swollen and that he was frequently getting unexplained
bruises. In January he went to his primary care doctor, and after ruling out an infection, his doctor ordered
several blood tests followed by a whole-body PET/CT scan, and CT scan of his chest, abdomen and pelvis.
In February, Brian underwent a bone marrow biopsy, and was diagnosed with Stage II diffuse large B-cell
lymphoma, which is a form of Non-Hodgkin Lymphoma. Because Brian may want to father children in the
future, he opts to take fertility preservation measures, which are not covered by his insurance plan. He also
has a chemotherapy port inserted to prepare for his treatments.
In March, Brian begins several cycles of chemotherapy infusions. He also receives supportive care drugs to
treat side effects like nausea.
In April, after his 3
rd
cycle of chemotherapy, Brian has another full body PET/CT scan to check if the
treatment is working. Fortunately, his cancer has shrunk, and he is able to complete treatment in June
without incident and does not require radiation.
Follow-up blood tests show no evidence of cancer, but Brian and his doctors must continue to monitor
for cancer recurrence through imaging and blood tests every 3-6 months for the next 5 years.
Throughout the course of his treatment, Brian saw several doctors and specialists, including his primary
care doctor, a medical oncologist, a hematologist, and a fertility specialist.
Brian is enrolled in a short-term limited duration
(STLD) plan that lasts 12 months. He pays
$156 in premiums every month for this non-
comprehensive coverage. Note that his plan can
also engage in post-claims underwriting, which
means that once he is diagnosed with cancer,
they will likely try to classify it as a pre-existing
condition, not cover any of these costs, or rescind
his coverage entirely.
Brian must pay an extremely high deductible
($12,500—which he meets in February) before
his plan will begin covering part of his cancer
care costs. Once his plan begins covering some
costs, he still must pay multiple thousands of
dollars every month until he completes his active
treatment in June. At the end of the year, he had
paid a total of $1,878 in premiums and $49,782
in cost sharing and costs for uncovered
services, for an annual total of $51,660.*
The total health care costs for Brian’s
Non-Hodgkin’s Lymphoma treatment were
$97,849. While Brian’s STLD plan did pay some
of these costs, it did not cover nearly as many
of the costs that a comprehensive, Affordable
Care Act (ACA)-compliant plan would have paid.
Despite being marketed as an insurance plan,
STLD plans are not considered comprehensive
insurance coverage, and Brian was responsible
for 51% of his cancer costs.
While Brian has finished his active cancer
treatment, he will continue to have tests and
imaging for the next 5 years, so his out-of-pocket
will likely continue to be higher than before he
had cancer. If/when he chooses to have children,
he will likely also have to pay out-of-pocket for
fertility services because of his treatments.
* Note that these costs only include cancer treatment, and do not include
treatment for other conditions that may have developed as a result of the
cancer treatments and/or any other treatments unrelated to cancer care or
other preventive services.

18 American Cancer Society Cancer Action Network The Costs of Cancer 2020
Data Analysis & Key Findings
Comparing Patient Out-of-Pocket Costs—Key Findings
■
Insurance coverage is critical. In each of the
scenarios, patients paid a considerable sum
out-of-pocket for their care but would have paid
significantly higher amounts if they had not had
insurance coverage.
■
The type of insurance a person with cancer
has is an important factor in how much they
will pay out-of-pocket. The type of insurance
a patient has, and that insurance benefit design,
determines how much the patient pays, and in
what form they pay it—e.g. in premiums that
are a fixed monthly amount, in deductibles and
cost sharing that are less predictable, or in
uncovered costs that can be unlimited.
●
In these scenarios, the patient with the large
employer plan pays the least out-of-pocket,
with relatively affordable premiums and cost-
sharing amounts, and a smaller out-of-pocket
maximum that is met early in the year.
●
Patients with a small-employer, high deductible
health plan or individual marketplace plan have
much higher deductibles and maximum out-of-
pocket limits and pay more overall.
●
Patients with Medicare (including Medigap
coverage) pay a high amount every month
in premiums, but lower amounts in co-pays
and co-insurance. In these scenarios, the
patients’ supplemental Medigap plan requires
the highest premiums, but also protects the
patients from paying 20% co-insurance on
many treatments. The majority of Medicare
enrollees have similar supplemental coverage,
but patients who do not have this coverage
pay much higher cost-sharing amounts.
●
The patient with a short-term limited duration
(STLD) plan must pay a much higher
deductible—almost twice as high as any other
deductible in the model—and must pay the
full price for many expenses that are not even
covered by the insurance plan.
■
Out-of-pocket limits help protect cancer
patients. Cancer patients are super-utilizers
of their insurance benefits, and each patient
in the scenarios who had an out-of-pocket
limit reached their maximum quickly. Once the
maximum is reached, patients do not have
to pay cost sharing for in-network, covered
services. This is an important protection for
many privately-insured patients.
The Dangers of Non-Comprehensive Coverage
Brian, who bought a short-term limited duration plan, paid over 4 times as
much as any of the other cancer patients profiled in out-of-pocket costs.
He did not realize that his plan had huge gaps in coverage (for instance it
doesn’t cover any prescription drugs) and now has to go into serious debt
to pay for his cancer treatments.

19American Cancer Society Cancer Action Network The Costs of Cancer 2020
$ 6
0,000
$ 5
0,000
$ 4
0,000
$ 3
0,000
$ 20,000
$ 1
0,000
$ 0
Colorectal
Cancer–
Medicare
Breast Cancer–
Small Employer
High Deductible Plan*
Prostate Cancer–
Large Employer Plan
Pancreatic Cancer–
Medicare
Lung Cancer–
Individual Marketplace
Plan
Lymphoma–
Short-term Limited
Duration Plan
*Annual costs for year 1 of breast cancer treatment
$318
$250
$4,864
$2,150
$6,000
$1,712
$2,500
$2,030
$1,517
$4,864
$1,650
$6,500
$3,896
$36,447
$12,500
$1,878
$500
$835
$250
Total:
$5,432
Total:
$9,862
Total:
$5,030
Total:
$6,631
Total:
$12,046
Total:
$5 1, 660
Uncovered Services
Co-pays & Co-insurance
Deductible
Premiums
Patient Out-of-Pocket Costs Vary Widely, Particularly for
Deductibles and Uncovered Services

20 American Cancer Society Cancer Action Network The Costs of Cancer 2020
$6
0,000
$5
0,000
$4
0,000
$3
0,000
$20,000
$10,000
$0
ACA-Compliant or
Comprehensive Plans
$8,684
$10,747
$6,446
$12,931
$5 1, 660
Medicare Small Employer,
High Deductible
Health Plan
Large Employer
Plan
Short-term Limited
Duration Plan
Individual
Marketplace Plan
Total Annual Costs Paid by Brian, Lymphoma Patient in Each Plan Type
Patient Out-of-Pocket Costs Vary Widely,
Even for the Same Patient
Brian’s out-of-pocket
costs vary from over
$6,000 to almost
$13,000 amongst the
ACA-compliant plans
we included in our
analysis.
His out-of-pocket costs
were over 4 times
higher when he had a
STLD plan that was not
ACA-compliant.
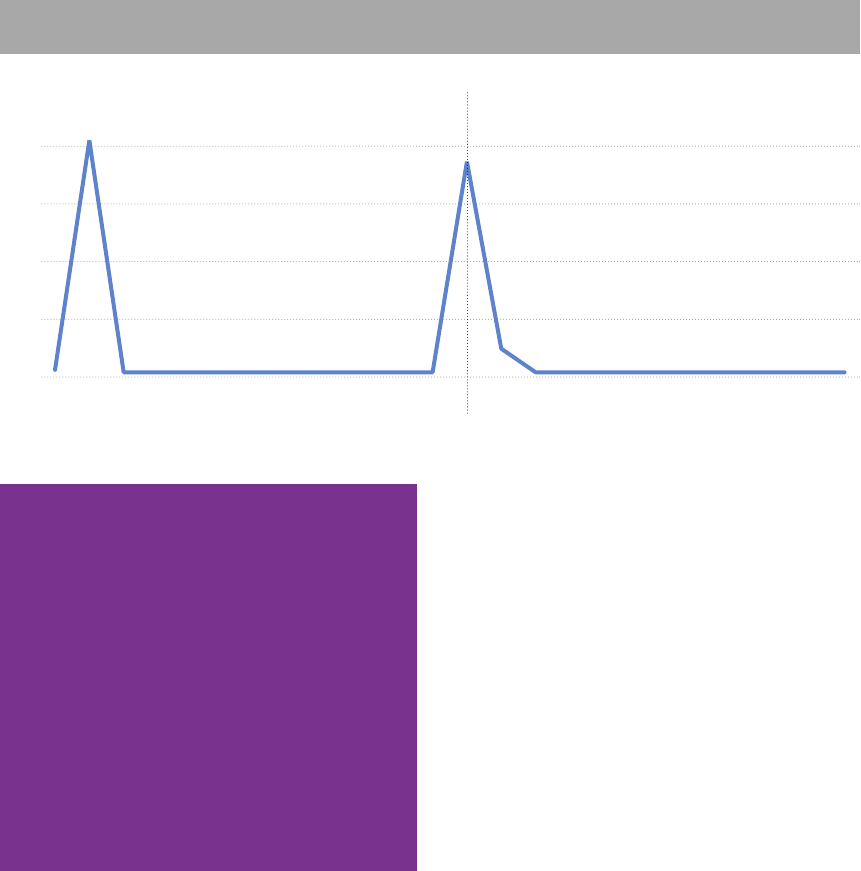
Patient Costs Throughout the Year—Key Findings
■
Out-of-Pocket cancer costs spike quickly.
Almost all of our cancer patients had to pay
several thousands of dollars in the first one to
three months after the
first suspicion of cancer.
Note that many of these
costs were before the
patient was officially
diagnosed—as some
diagnostic tests can be
quite expensive. High
amounts of spending
are required until the
cancer patient meets his
or her deductible and
maximum out-of-pocket
limit (if applicable).
■
Costs spike higher for patients with higher
deductibles and maximum out-of-pocket
limits. Patients with a high deductible or
maximum out-of-pocket limit experience higher
spikes and more uneven month-to-month
spending patterns because a higher amount
of spending is required up-front before the
plan begins covering expenses. This can cause
significant financial hardship for patients who
cannot afford to pay large medical bills all at
once, and can also cause patients to delay tests
or treatments.
19
■
Medicare patients see different spending
patterns. Because a majority of Medicare
enrollees purchase supplemental coverage,
most Medicare patients pay lower cost-sharing
amounts. For the Medicare patients in our
scenarios, their spending did not spike until
they started taking pharmacy drugs—which are
covered through Medicare Part D rather than
their Medigap plan and require cost sharing,
which can often be significant and is not capped.
■
STLD plans play by their own rules (or lack
thereof). Because STLD plans are not required
to have particular maximum out-of-pocket
limits or cover specific services, the spending
pattern under this plan is vastly different. Brian’s
spending spikes much higher, and for a longer
amount of time, than the other patients. This is
because his plan requires a very high deductible,
has a high maximum out-of-pocket limit (note:
some STLD plans do not have such a limit at
all), and does not cover important services like
prescription drugs. Therefore, Brian’s high out-
of-pocket costs never relent until he finishes his
active cancer treatment in July.
The Costs of Cancer Disparities
Could YOUR monthly budget accommodate
a $5,000 (or higher) medical bill? These
spending spikes are hard to afford even for
middle-and high-income people with cancer.
An annual survey shows that 37% of
Americans would NOT be able to cover a one-
time unexpected expense of $400 without
borrowing money or using a credit card that is
not paid off in full at the end of the month. The
survey found that people of color and those
with less education are more likely to have
trouble covering an unexpected expense.
18

21American Cancer Society Cancer Action Network The Costs of Cancer 2020
$ 1
6,000
$ 14,000
$ 12,000
$ 1
0,000
$ 8,000
$ 6,000
$ 4,000
$ 2,000
$ 0
January
February
March
April
May
June
July
August
September
October
November
December
*Monthly costs for year 1 of breast cancer treatment
Brian–Lymphoma–Short-term Limited Duration Plan
Carla–Breast Cancer–Small Employer High Deductible Plan*
Kathy–Lung Cancer–Individual Marketplace Plan
Franklin–Prostate Cancer–Large Employer Plan
Tom–Colorectal Cancer–Medicare
Shonda–Pancreatic Cancer–Medicare
Monthly Patient Out-of-Pocket Spending Spikes Within
1-3 Months of Diagnosis
22 American Cancer Society Cancer Action Network The Costs of Cancer 2020
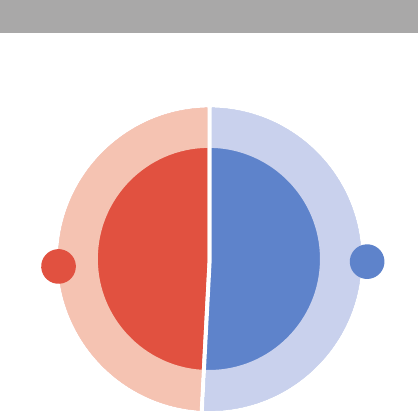
Patient Out-of-Pocket Spending Over Multiple Years—Key Findings
■
The higher costs of cancer can span
multiple years. Carla had an aggressive form
of breast cancer that required several months of
chemotherapy before surgery, and many months
of drug therapy after surgery. Her cancer
experience—and therefore her spending on
cancer treatments—did not fit neatly into a one-
year timeline. Most patients’ cancer treatments
cross plan years. Over the two years we tracked
Carla’s spending on cancer treatments, she
paid her full maximum out-of-pocket amount
twice—resulting in two spending spikes. As
she continues to need follow-up care after her
treatments, she will continue to pay higher costs
for multiple years into survivorship.
Januar
y
April
July
October
Januar
y
April
July
October
Year
1Y
ear 2
$8,000
$6,000
$4,000
$2,000
$0
Two Years of Monthly Out-of-Pocket Costs for Carla, Breast Cancer Patient
When Cancer Treatments Span Multiple Years, Patient Out-of-Pocket
Spending Spikes Multiple Times
The Costs of Cancer Disparities
■
Breast cancer is the most commonly
diagnosed cancer in Hispanic women, and is
also the leading cause of cancer death in this
population.
■
Breast cancer is less likely to be diagnosed
at a local stage in Hispanic women compared
to non-Hispanic white women. Lower rates of
mammography screening and delayed follow-
up on abnormal test results or self-discovered
abnormalities likely contribute to this disparity.
■
Hispanic women are less likely than non-
Hispanic whites to receive appropriate and
timely breast cancer treatment.
Source: American Cancer Society.
20

23American Cancer Society Cancer Action Network The Costs of Cancer 2020
Insurance Coverage Transitions—Key Findings
■
Changing insurance plans mid-year or
mid-treatment can cause spending spikes
and higher total costs. If a cancer patient
must change insurance coverage mid-year or
mid-treatment, they will likely be required to pay
the new plan’s deductible and maximum out-
of-pocket amount—resulting in higher annual
costs for the patient and multiple spikes in
monthly spending. Higher costs also may result
from the new plan covering different benefits
and/or providers. A patient may have to change
their insurance plan mid-year or mid-treatment
if they have:
●
Changed jobs
●
Lost their job, or had to reduce hours to
part-time because of their health, cancer
treatments, or external factors
●
Moved to a new state, and did not have
coverage that transferred to the new state or
had providers located in the patient’s new area
●
Were no longer able to afford paying
premiums
$8,000
$1
0,000
$6,000
$4,000
$2,000
$0
January
February
March
April
May
June
July
August
September
October
November
December
Franklin—Switches Plan Mid-Year
Franklin—Stays in Large Employer Plan All Year
Changing Insurance Mid-Year Causes Higher Costs and Multiple Spikes
Monthly Out-of-Pocket Costs for Franklin, Prostate Cancer Patient
Franklin loses his
job and must
switch to an
Individual
Marketplace Plan
Franklin’s total
annual cost:
$14,580
Franklin’s total
annual cost:
$5,030
The Costs of Cancer Disparities
What if Franklin wasn’t able to afford to enroll in a
marketplace plan right away after he lost his job and
employer-sponsored insurance? A recent study
21
showed:
Disruptions in insurance coverage are common among low-
income populations.
Compared to people whose insurance coverage was
continuous, those with disruptions were less likely to receive
cancer prevention, screening, and treatment.

24 American Cancer Society Cancer Action Network The Costs of Cancer 2020
Types of Cancer Costs—Key Findings
■
Type of cancer and treatment plan cause
huge variation in the source of cancer costs.
For all of the patients included in our analysis,
the majority of their cancer treatment costs
came from drugs, hospital costs, and/or surgical
procedures. This amount varied, however,
depending on the patient’s treatment plan.
■
There are many drivers of the costs of
cancer. While much attention tends to focus on
drug costs, and whether they are rising, other
types of treatments and services drive many of
the costs for people with cancer.
0% 10% 20% 30%40% 50%60% 70%80% 90
%1
00%
Percentage of To tal (Patient & Payer) Costs, Per Treatment Type
Tom—Colorectal Cancer
Carla—Breast Cancer*
Franklin—Prostate Cancer
Shonda—P
ancreatic Cancer
Kathy—Lung Cancer
Brian—Lymphoma
Drugs Radiation Treatments Hospital Costs/Surgical Procedures Doctor's Visits Imaging Tests Laboratory Tests
*Percentage of total costs for 2 years of breast cancer treatment
The Drivers of Cancer Costs Vary Widely Among Patients

25American Cancer Society Cancer Action Network The Costs of Cancer 2020
Spotlight on Drug Costs—Key Findings
■
Patients and payers can save when patients
take biosimilars. In our breast cancer scenario,
Carla underwent drug therapy spanning multiple
years. Under the scenario where she was
able to substitute one of her main drugs for a
biosimilar version, total spending on drugs was
reduced by 21%.
$8
0,000
$6
0,000
$70,000
$5
0,000
$4
0,000
$3
0,000
$20,000
$10,000
$0
$58,906
$74,487
Using Brand-name Drug Using Biosimilar
21%
reduction
Patients and Payers Save With the Use of Biosimilars
Carla, Breast Cancer: Total Expenditures Over 2 Years for Targeted Therapy

26 American Cancer Society Cancer Action Network The Costs of Cancer 2020
0% 10% 20% 30%40% 50%60% 70%80% 90
%1
00%
Percentage of To tal (Patient & Payer) Drug Costs, Per Drug Type
Tom—Colorectal Cancer
Carla—Breast Cancer*
Franklin—Prostate Cancer
Shonda—P
ancreatic Cancer
Kathy—Lung Cancer
Brian—Lymphoma
Physician-administered Anti-cancer Drugs Pharmacy Anti-cancer Drugs Pharmacy Supportive Care Drugs
* Percentage of drug costs for 2 years of breast cancer treatment
Drivers of Drug Costs in Cancer Care Vary Widely
■
The drivers of drug costs in cancer care
vary widely based on the patient’s treatment
plan. Anti-cancer drugs meant to kill cancer
cells or keep them from returning—including
chemotherapy, immunotherapy and hormone
therapy drugs—can be delivered intravenously
in a doctor’s office, or via a pill obtained at the
pharmacy. Supportive care drugs—intended
to help patients with side effects like nausea
and pain—are also an important part of cancer
drug treatment and can come in either form.
Insurance plans often treat drugs differently—
including placing them on different tiers and/or
charging patients different amounts—depending
on these distinctions.

27American Cancer Society Cancer Action Network The Costs of Cancer 2020
Unexpected Problems that Add to
Patient Out-of-Pocket Costs
In each of the modeled scenarios included in this report, analysts
assumed that the cancer patients had no problems using their
insurance benefits, and that each insurance plan covered every
treatment.
22
In reality, many people with cancer encounter problems
that cause delays and complications and further increase their costs.
Below are several common scenarios patients encounter that make
their out-of-pocket costs higher than what was modeled in this
report, or what the patient expected.
No Insurance Coverage
While each patient profiled in this report had
insurance coverage (note: Brian’s STLD plan—
which left many treatments uncovered—is not
considered comprehensive insurance), we know
that millions of Americans are still uninsured.
23
Some of these Americans are diagnosed with
cancer every year. While some uninsured cancer
patients are able to negotiate discounts or qualify
for charitable programs to help pay for their
care, they are never guaranteed treatment. An
uninsured cancer patient is responsible for all
costs of their treatment,
and many forego care due
to cost.
Example: what if Kathy
didn’t have insurance
coverage?
In our scenario, Kathy has
insurance coverage through
her state’s individual
marketplace. At the end of the year in which
she is diagnosed with Stage IV lung cancer, she
has paid over $12,000 in premiums and cost-
sharing—not a small amount. However, if Kathy
were uninsured, she would be responsible for the
entire cost of her cancer care—over $140,000
(or likely higher because she would not benefit
from a plan’s negotiated rates). While she might
be able to negotiate discounts with providers or
receive some charity care, these costs and the
uncertainty of how to pay them would likely to
take a huge toll on Kathy’s financial, emotional
and physical quality of life.
Inadequate Coverage
Some consumers struggle to afford health
insurance premiums, and when shopping for
cheaper premiums may unknowingly enroll in a
plan that has inadequate coverage. Plans like
short-term limited duration insurance—which
despite the name, can last the same amount of
time as other insurance plans—and Association
Health Plans do not have to follow all of the
requirements in the ACA and other regulations.
These plans are missing comprehensive patient
protections, and an enrollee who is diagnosed
with a serious illness like cancer while enrolled in
one of these plans will likely discover that it does
not cover what they expected when purchasing
the plan. Because of this, the patient pays
catastrophically high costs.
$1
50,000
$90,000
$120,00
0
$60,000
$30,000
$0
$140,247
$12,046
With Individual
Marketplace Plan
With No Insurance
Costs are Much Higher for
Uninsured Patients
Annual out-of-pocket costs for Kathy,
lung cancer patient
The Costs of Cancer Disparities
■
Most uninsured people are in low-income
families and have at least one worker in
the family.
■
Adults are more likely to be uninsured
than children.
■
People of color are at higher risk of being
uninsured than non-Hispanic Whites.
24
28 American Cancer Society Cancer Action Network The Costs of Cancer 2020
Example: Brian has a short-term limited
duration plan.
As a young adult who works several part-time
and freelance jobs, Brian was left to find health
insurance on his own. He went online and
bought the cheapest plan he could find through
an insurance broker website, not understanding
that this short-term plan does not cover a
comprehensive set of benefits or have to follow
other patient protections. He knew it had a high
deductible, but he did not expect to need many
health care services this year. Unfortunately, Brian
is diagnosed with lymphoma and discovers that
his plan’s coverage is extremely limited. At the
end of his year of cancer treatments, Brian’s plan
has covered less than half of his cancer treatment
costs. Most significantly, Brian has to pay full price
out-of-pocket for all of his prescription drugs,
because his plan does not cover them. Brian will
be in debt for many years to come because of this
unexpected cancer diagnosis.
51%
49%
STLD Plans Cover Far Fewer Costs
Percentage of costs Brian’s STLD plan covers
compared to costs Brian pays for his
lymphoma treatments
Brian
pays
$49,782
STLD
plan pays
$48,067
Non-Covered Treatments
Health insurance plans do not always cover every
health care service or drug. When plans deny
coverage of certain cancer treatments, patient
out-of-pocket costs can increase considerably
if the patient decides to proceed with their
physician’s recommended course of treatment.
Costs for non-covered services do not count
towards a patient’s out-of-pocket maximum
(where applicable), so patient costs for non-
covered treatments are unlimited and can add up
quickly.
Example: what if Kathy’s individual
marketplace plan does not cover biomarker
testing for her tumor?
When Kathy is diagnosed with lung cancer, her
doctor wants to test her tumors for multiple
biomarkers that could point them towards
effective targeted therapy to treat her cancer.
Thanks to recent therapeutic advances,
several biomarkers are relevant to lung
cancer treatment. However, Kathy’s individual
marketplace plan only covers a test that
evaluates one biomarker. In order to get the full
panel of recommended biomarker tests, Kathy
must pay over $1,500 out-of-pocket. Because
these are charges for uncovered treatments,
this amount also does not count towards Kathy’s
maximum out-of-pocket limit.
Large Deductibles
High deductible health plans (HDHPs) are
becoming more prevalent as consumers seek to
find plans with more affordable premiums, and
employers—facing rising health care costs—want
to have more predictability in what they spend on
employee health care. While HDHPs are required
to cover preventive services with no cost sharing,
and some cover other routine services like primary
care without applying the deductible, all of our
scenarios show that once a patient is suspected
to have cancer, the costs add up quickly and
patients must pay their entire deductible. Often
patients are not expecting these costs—because
they did not expect a serious diagnosis, and/or
they did not fully understand how their HDHP
worked or may not have known the amount of
their deductible.
Example: Carla has a small employer, high
deductible health plan.
Carla’s small employer only offers one option
for health insurance, and it is a high-deductible
health plan. While some employers offer their
employees—or may help fund— a health
savings account, Carla’s employer does not.
When her doctor sees a suspicious spot on her
mammogram, Carla’s doctor orders another
imaging test. As it becomes clear that Carla has

29American Cancer Society Cancer Action Network The Costs of Cancer 2020
an aggressive form of breast cancer, she is sent
for several more scans and tests. Because she
has a high deductible plan, she must pay full price
for these tests out-of-pocket until she meets her
$6,000 deductible. Carla is very worried about
a possible diagnosis of breast cancer, but she
is also a working mother and cannot afford to
pay $6,000 within one month. She must choose
between going into debt to pay these costs—if
her credit card has a high enough limit or she can
borrow from a friend—or delaying these tests and
potentially letting the cancer get worse.
Unpredictable Co-insurance Costs
Once a patient meets their deductible for the year
(as applicable), the primary cost sharing required
are co-pays and co-insurance. Both are fees
that the patient pays when health care services
are delivered, or a prescription is filled. Co-pays
are flat fees, usually defined clearly in a patient’s
insurance documents or formulary. Co-insurance,
however, is a percentage of the total cost of the
treatment or drug that the patient pays. Cancer
patients often have trouble finding out what that
total cost is ahead of time, and therefore cannot
predict the amount of co-insurance they will owe.
Health insurance plans often use co-insurance for
certain types of treatment in their medical benefit,
as well as in the most expensive upper tiers of
their drug formularies.
Example: What if Shonda pays co-insurance
for one of her drugs?
Shonda is dealing with a very serious diagnosis of
pancreatic cancer, and her symptoms and quality
of life get worse throughout the year. Her doctor
prescribes several pills to help with the nausea
that her cancer and chemotherapy cause. One
of these pills is not available as a generic, and
Shonda’s Part D plan charges 28% co-insurance.
But Shonda does not know how much the drug
costs. When her daughter drives to the pharmacy
to pick up her prescription for her, Shonda does
not know how much money to give her daughter
to cover the cost of the drug.
Shonda Pays…
If Shonda Paid a Co-Pay $47
If Shonda Paid Co-Insurance 28% of ??? = ???
Surprise Medical Bills
‘Surprise medical bills’ occur when an insured
patient is unknowingly treated by an out-of-
network provider and is then billed the difference
between what the provider charged and what
the insurer paid. This can happen when a patient
receives emergency care at an out-of-network
facility or non-emergency care at a facility that
is in-network, but the doctor was out-of-network
and the patient did not know. Surprise bills can
be significantly higher than the consumer’s
standard in-network cost sharing, and they do
not count towards a patient’s maximum out-of-
pocket limit (if applicable). They occur most often
with ancillary providers—like anesthesiologists,
assistant surgeons, and emergency room
physicians.
Example: what if Franklin’s anesthesiologist
during his prostatectomy surgery was out-of-
network?
After being diagnosed with advanced prostate
cancer, Franklin’s doctor recommends he have
surgery to remove his prostate. Franklin chooses
to have his surgery at a hospital that is considered
in-network by his insurance plan. After his
successful surgery, Franklin is surprised to receive
a bill for over $2,000 from the anesthesiologist
who worked on his surgery. He is more surprised
to learn that this doctor is out-of-network,
even though his surgery was at an in-network
hospital. Franklin’s insurance plan will only pay
the anesthesiologist its in-network rate, and the
doctor has billed Franklin directly for the rest
30 American Cancer Society Cancer Action Network The Costs of Cancer 2020
of his fee. To add insult to injury, when Franklin
pays this unexpected bill, the amount will not be
counted towards his out-of-pocket maximum.
Unexpected Costs for Preventive/Screening
Services
Almost all insurance plans are required to cover
certain preventive and cancer screening services
with no cost sharing for patients. Believing you
will not need to pay for a service makes you
more likely to seek out the service—and this
is important for preventive services for which
some patients need extra incentive. However,
some patients encounter loopholes in these
requirements that leave them with an unexpected
bill for a service they thought would be free.
Example: what if Tom is charged for his
colonoscopy?
Tom undergoes a screening colonoscopy.
However, in the course of the procedure, polyps
were discovered and removed. If Tom did not
have a Medigap plan, Tom would be surprised
to receive a bill for his colonoscopy because
Medicare considers the removal of polyps to be a
diagnostic procedure—regardless if the procedure
began as a routine screening—because polyps
were found and removed.
25
Tom would be charged
20% co-insurance ($250 in this case) for the
procedure, and he might struggle to pay the bill
on his fixed income.
Problems Using Co-Pay Cards
Some people with cancer need the newest cancer
treatments, and the drug their doctor prescribes
is not yet available in a cheaper generic form. In
most cases, their insurance plan will require much
higher cost-sharing for the brand name drug that
is medically indicated. Because of this, many drug
manufacturers and patient assistance programs
offer co-pay cards or discount programs that
help patients in these situations pay their cost-
sharing amounts and afford their drug treatment.
However, Medicare patients are not eligible
for these discounts because of current federal
government policy. Recently, some private
insurance policies have started to make it harder
for patients to benefit from these discounts, by
not applying the amount the card or assistance
program paid for the drug towards a patient’s out-
of-pocket maximum amount. This plan policy is
known as an “accumulator” adjustment program.
Example: what if Franklin needed to use a co-
pay card for his hormone therapy drug?
When Franklin is diagnosed with advanced
prostate cancer, he must take a hormone therapy
drug for five months. This drug is not available
in generic form, and costs over $10,000 per
month. His insurance plan considers it a specialty
drug, and therefore requires him to pay 50%
co-insurance for the drug until he meets his
maximum out-of-pocket limit. Franklin’s doctor
tells him the drug manufacturer offers a co-pay
card that can help with these costs. The card
covers up to $5,000 of cost-sharing expenses for
patients in Franklin’s situation, and allows Franklin
to pay $50 per month for the prescription, while
the manufacturer covers the rest of his cost-
sharing amount until he reaches his maximum.
Without the co-pay card, Franklin would be
required to pay $3,000 to fill his prescription
in the first month—his entire maximum out-of-
pocket amount. This huge up-front cost may be
challenging for him to afford, and he may decide
to delay or skip this treatment, which could mean
his cancer gets worse. Using the manufacturer
co-pay card, Franklin would only pay $50 to fill
his prescription. The manufacturer would cover
the rest of his co-insurance amount up to his
plan’s $3,000 maximum, and Franklin would
not owe any more money for the prescription
in the following months. However, if Franklin’s
plan uses an ‘accumulator’ adjustment program
to discourage patients from using co-pay cards,
the amount the manufacturer pays towards
his prescription would not count towards his
maximum out-of-pocket limit. This means Franklin
would pay $50 every month for his prescription
until the co-pay card ran out of money in his
second month of taking the drug—at which point
he would have to cover the whole cost of the
prescription.

31American Cancer Society Cancer Action Network The Costs of Cancer 2020
$ 3,000
$ 2,500
$ 2,000
$ 1,500
$ 1,000
$ 500
$ 0
February
March
April
May
June
July
No Co-pay Card
With Co-pay Card
With Co-pay Card in an
Accumulator Plan
$0
$0
$0
$3,000
$50
$50
$0
$0
$2,950
$0
$0
$0
$0
$0
$0
$0
$0
$0
Franklin’s Out-of-Pocket Spending on Hormone Therapy
Franklin’s Costs are Most Affordable When He Can Use a
Co-Pay Coupon as Intended

32 American Cancer Society Cancer Action Network The Costs of Cancer 2020
The worldwide COVID-19 pandemic has created an unprecedented
set of circumstances and challenges for the U.S. health care system.
These challenges are particularly acute for cancer patients, cancer
survivors, and those at risk for cancer—and these challenges have
already, or are likely to, impact the costs of cancer to patients and
the health care system for years to come. The ultimate costs to
cancer patients, cancer survivors, and the health care system of
COVID-19 may likely include:
■
Additional costs associated with delayed
or skipped cancer screenings. Many
individuals at risk for cancer have had their
regular screenings delayed or missed because
of facility closures, recommendations from
health officials prioritizing urgent care and
halting elective procedures, including cancer
screenings , and patient and provider fears and
confusion on the safety of screenings during
a pandemic.
26,27
These delays in screening
can result in cancer that is detected at later
stages, when it is harder and more expensive to
treat.
28,29,30
■
Costs of postponed or missed cancer
treatments. For those who have already been
diagnosed with cancer, delaying or skipping
treatments can cause their cancer to progress
and health outcomes to worsen
31,32
—which may
result in more costly care and more lives lost.
■
Costs of insurance coverage disruptions.
Huge upheavals to our country’s economy
caused by quarantines and other COVID-19
factors have caused many Americans to
lose their jobs or be furloughed. As so many
Americans receive their health insurance
through an employer, this has definitely caused
disruptions to insurance coverage.
33
The data
show that gaps in insurance coverage cause
people to miss screenings and be diagnosed
with cancer at later stages when care is more
expensive.
34
Additionally, individuals who must
switch insurance plans because of these
disruptions will have to pay new cost-sharing
amounts, and their costs will likely rise.
Spotlight in 2020:
The Costs of Cancer and COVID-19
The Costs of Cancer Disparities
People of color have been widely reported to be at increased risk
for hospitalization and the related costs due to COVID-19,
35,36
a
disparity that is likely caused by disparate conditions that existed
before COVID-19, like racial inequalities in insurance coverage and
access to care. Additionally, data are showing that workers who
are people of color are losing their jobs at higher rates than white
workers; and because of these job losses, at least 1 million Asian,
2 million Black, and 3 million Hispanic people are likely to lose their
employer-sponsored health insurance in 2020.
37
Consequently
the increased costs discussed above will hit people of color more
heavily and widen health disparities.

33American Cancer Society Cancer Action Network The Costs of Cancer 2020
According to the National Cancer Institute, medical financial
hardship is a term used to describe problems a patient has related to
the costs of medical care.
38
Financial hardship is also often referred
to as financial toxicity, distress, or burden. These kinds of problems
happen often for cancer patients and survivors—research shows
that individuals with a history of cancer are more likely to experience
financial hardship than those with no cancer history.
39
There are three main types of medical financial hardship:
40
Financial Hardship—How High Costs
Adversely Affect Cancer Patients, Survivors
and their Families
• Trouble paying out-of-pocket expenses
• Trouble paying household bills
• Missed work
• Reduced/lost income
• Medical debt/bankruptcy
• Feelings of distress, stress and worry due to costs of care
• Concern about ability to work and wages/income meeting
necessary expenses
• Taking less or skipping medications because of cost
• Delaying or missing doctor's visits or medical care because of cost
Material
Pshychological
Behavioral

34 American Cancer Society Cancer Action Network The Costs of Cancer 2020
Cancer patient/survivor more likely to experience hardship if:
Importantly, these hardships lead to worse
health outcomes, such as:
• Cancer site, treatment intensity and/or duration
• Later stage at diagnosis, disease progression
• Lower socio-economic status
• People of color
• Younger Age
• Rural residence
• Lack of health insurance coverage
• High cost-sharing levels in a private insurance plan
• Problems with health insurance literacy
41
• Lost income due to time away from work
• Workplace accomodations (or lack thereof)
Younger survivors are more
likely to worry about:
42
Monthly Bills
Retirement
Housing
Standard of Living
Food running out or not lasting
Affording balanced meals
Increased Symptoms
43
Less Satisfaction with care
44
Lower Quality of Life
45
Higher Risk of Dying
46
List of factors adapted from K. Robin Yabroff, Cathy Bradley, and Ya -Chen Tina Shih. Understanding
Financial Hardship Among Cancer Survivors in the United States: Strategies for Prevention and Mitigation.
Journal of Clinical Oncology 2020 38:4, 292-301.
While financial toxicity or
hardship is recognized
as a medical, economic
and societal problem;
providers often find
this toxicity harder to
‘treat’ or address than
physical symptoms and
side effects. As research
continues to show how
financial toxicity affects
cancer patients and
their families—and more
innovative treatments
become available with
higher price tags—
policymakers must
address these problems
through changes in policy.
Lack of action will lead to
wider disparities in cancer
care and outcomes based
on wealth and status.

35American Cancer Society Cancer Action Network The Costs of Cancer 2020
The American Cancer Society Cancer Action Network (ACS CAN)
works to ensure that all people with cancer can afford the right cancer
therapy at the right time, as well as survivorship care, preventive
services and all other required medical care. The affordability of
cancer care—and health care in general—is a multi-faceted problem
that requires multi-faceted solutions.
Ensuring Access to Affordable
Insurance Coverage
The single most important thing policymakers
can do to help cancer patients afford the costs
of cancer is to ensure that everyone has access
to affordable comprehensive health insurance.
American Cancer Society (ACS) research shows
that individuals with health insurance are nearly
twice as likely as those without
it to have access to critical early
detection cancer procedures, and
the uninsured are less likely to get
screened for cancer, are more likely
to be diagnosed with cancer at an
advanced stage and are less likely
to survive that diagnosis than their
insured counterparts.
47,4 8
Having access to insurance coverage means a
patient is 1) not denied enrollment, 2) able to
receive help when needed to understand the
enrollment process and insurance coverage, and
3) able to afford the premiums and cost sharing.
Ensuring access to insurance coverage is
not only an ACS CAN priority, but a priority of
cancer patients and survivors. In a 2020 ACS
CAN Survivor Views survey,
49
respondents
identified access to comprehensive and portable
health insurance as a critical tool in supporting
people with cancer. Over half of cancer patients
and survivors (51%) indicated that ensuring
health insurance covers all needed care was
the priority that would have the greatest
impact in helping people with cancer. The
second most commonly prioritized issue was
ensuring affordable health insurance is available
regardless of job changes (20%) .
Spotlight on ACS CAN Policy Priorities:
Maintain Current Affordable Care Act (ACA)
Patient Protections
All of the patients in our profiles benefited from
ACA protections (except the patient who had a
short-term limited duration plan, which does not
have to follow ACA requirements—the allowance
of which ACS CAN is challenging in the court
system), including the ability to enroll in their
insurance plans, the provision of comprehensive
benefits and limits on their out-of-pocket
spending. The ACA contains critical protections
that provide an essential lifeline for millions who
experience serious illnesses and conditions, like
cancer. Prior to the ACA, individuals who most
needed health insurance coverage—including
those older and sicker who are not yet eligible
for Medicare—often found it difficult, if not
impossible, to obtain health insurance that
covered necessary care at an affordable price.
51
Uninsured patients are less likely to be screened
for cancer and more likely to be diagnosed with
Policy Solutions to Address the Costs of Cancer
The Costs of Cancer Disparities
Black and Hispanic individuals with cancer
are more likely to be uninsured at diagnosis—
although ACA implementation has reduced and
even eliminated some of these disparities.
50
Survivor Views: The Costs of
Cancer in Their Own Words
“My cancer care costs have
completely depleted my savings.
I am no longer able to buy a
house because I cannot afford
any down payment.”
Lymphoma Survivor, Oregon
ACS CAN advocates for public policies that
address the individual and systemic costs of
cancer by:
■
Ensuring access to affordable insurance
coverage for all;
■
Limiting costs by preventing cancer and
detecting it early through the use of
screening and preventive services;
■
Ensuring access to health care services; and
■
Reducing the overall financial impact of
cancer for patients and their families.

36 American Cancer Society Cancer Action Network The Costs of Cancer 2020
later stage disease which is harder to survive and
more costly to treat.
52
Since the law went into effect, individuals with
pre-existing conditions have been better able
to access comprehensive health insurance. The
uninsured rate among nonelderly patients with
newly diagnosed cancer declined substantially,
particularly among low-income people who
resided in Medicaid expansion states—where
it decreased six percent.
53
In addition, there is
already a small but statistically significant shift
that has been found toward early-stage diagnosis
for colorectal, lung, breast and pancreatic cancer
in states that have increased access to health
care through Medicaid because of the ACA.
54
For all these reasons, ACS CAN strongly supports
the continuation of the patient protections in the
ACA. We strongly oppose any efforts to dismantle
the legislation without replacing these protections,
including the current efforts to invalidate the ACA
through the California v. Texas litigation, currently
pending at publication of this report and awaiting
hearing from the Supreme Court of the United
States.
55
Maintain and Expand Access to Medicaid
All of our patient profiles showed the high
costs that an uninsured individual would face if
diagnosed with cancer. However, individuals with
very low incomes are less likely to be provided
insurance coverage through their employer
56
(as applicable), and also are unlikely to be able
to afford paying insurance premiums on their
own. Medicaid is a lifeline for many of these
low-income Americans and maintaining and
expanding access to Medicaid significantly
reduces the costs of cancer for our country’s
most vulnerable cancer patients. To date,
38 states and the District of Columbia have
increased access to their Medicaid programs (or
have passed policies requiring them to do so)
57
,
providing more than nine million individuals and
families access to health care coverage and to
lifesaving tests like mammograms, colonoscopies
and other cancer screenings.
ACS CAN strongly supports and works towards
the expansion of Medicaid eligibility up to 138%
of the federal poverty level (FPL) in every state,
as well as other efforts to ensure low-income
Americans can access the health care they need
through this safety net program. Furthermore,
ACS CAN strongly opposes any efforts to restrict
access to Medicaid or the benefits available to
Medicaid enrollees, including state efforts to:
■
Limit or restrict eligibility (through work or
community engagement requirements, waiving
retroactive eligibility or enrollment caps)
■
Impose cost sharing (premiums, co-payments)
■
Penalize enrollees for non-compliance with
various program or wellness requirements
■
Eliminate and/or restrict benefits/services
■
Place limits on the length of program eligibility
■
Change the financing structure (block grants or
per-capita caps)
Data indicates that these policy proposals,
especially those that limit or restrict eligibility,
will significantly reduce enrollment in the
Medicaid program and deny access to preventive
and treatment services for individuals and
families enrolled in the Medicaid program.
58,59,60
Preservation of eligibility and access to health
care coverage through state Medicaid programs
is critical for continuing to make progress against
cancer for those low-income Americans who
depend on the program for cancer prevention,
early detection, diagnostic, treatment and
survivorship care services.
2020 Federal Poverty Level (FPL)
Individual Family of 4
100% $12,760 $26,200
138% $17,609 $36,156
400% $51,040 $104,800
Source: https://www.healthcare.gov/glossary/federal-poverty-level-fpl/

37American Cancer Society Cancer Action Network The Costs of Cancer 2020
Expand Premium Subsidies for
Marketplace Plans
Kathy, who had Stage IV lung cancer, was insured
through the individual marketplace, and was
fortunate to qualify for subsidies that partially
paid her premiums and made insurance more
affordable. Advanced Premium Tax Credits are
available on a sliding scale for individuals and
families earning between 100 and 400% FPL,
and these subsidies allow many people in this
income bracket to afford enrollment. However,
individuals above 400% FPL and who enroll
through the individual marketplace do not qualify
for subsidies, and many of these individuals and
families struggle to afford their premiums—or
must forego enrollment altogether due to inability
to pay. These middle-income individuals and
families would greatly benefit from the expansion
of these subsidies to include higher incomes.
Additionally, other families do not qualify for
subsidies—and therefore may not be able to
afford premiums—because of what is known as
the “family glitch.” Under the ACA an individual
is eligible for premium subsidies in the individual
marketplace if the amount he/she would have
to pay for their individual employer-sponsored
coverage is more than 9.86% of their household
income. Most employers subsidize the cost of
their employee’s health insurance premiums.
However, this subsidy may be less generous for
family coverage. Even if the employee is paying a
family premium, only the amount of the individual
employee’s coverage is considered for purposes
of calculating eligibility for subsidies. As a result,
families who are paying insurance premiums in
excess of 9.86% of their household income are
ineligible for subsidies.
ACS CAN strongly supports expanding
marketplace premium subsidies by fixing the
family glitch, and by increasing the income range
of individuals and families who are eligible for
subsidies. Federal and/or state policymakers
could create partial subsidies for individuals
earning more than 400% FPL to make premiums
more affordable for individuals who need to enroll
through the individual marketplace.
Other Priorities to Ensure Access to Affordable
Insurance Coverage:
■
Funding outreach and enrollment programs, which
help individuals and families make enrollment
decisions, navigate the enrollment process, and
make them aware of enrollment opportunities in
the first place. Funding outreach and enrollment
programs not only helps the individuals who need
it—these programs also encourage more healthy
individuals to enroll in insurance, improving the
risk pool, lowering premiums for everyone and
ensuring that everyone has access to a doctor or
a hospital when they need it.
■
The creation of reinsurance and risk corridor
programs—at the state or federal level—that
evenly distribute risk and keep premiums in the
individual marketplace from rising.
In the current health care system, ensuring access
to care means ensuring that everyone is able to
enroll in a health insurance plan—whether it be
through their employer, through a government
program like Medicare or Medicaid or through
the individual marketplace. Addressing the
affordability of premiums for these types of plans
is key, but so is taking other measures to make
sure insurance enrollment is truly accessible.
Limiting Costs by Preventing
Cancer and Detecting it Early
Through the Use of Screening
and Preventive Services
Some of the costs of cancer can be avoided
before they ever occur by preventing cancers
from developing in the first place or detecting
cancer at early stages when it is easier to treat.
A substantial proportion of cancers are
preventable,
61
and much of ACS CAN’s work in
prevention focuses on reducing the major risk

38 American Cancer Society Cancer Action Network The Costs of Cancer 2020
factors for cancer: tobacco use, excess weight/
obesity, physical inactivity, poor nutrition and
indoor tanning/sun exposure; as well as advocacy
for critical cancer control programs and increased
access to preventive and evidence-based
screening services. ACS CAN advocates for
evidence-based policies that address these risk
factors and are proven to reduce cancer incidence
and death. Preventing more cancers and detecting
more cancers early requires changes to clinical
settings and services, as well as to communities.
Spotlight on ACS CAN policy priorities:
Stop Unexpected Costs for Preventive and
Screening Services
When Tom’s FIT test was positive, indicating
possible colorectal cancer, his doctor ordered a
follow-up colonoscopy. During the colonoscopy
doctors found and removed polyps that would
have developed into cancer in the future. Tom’s
colonoscopy was a health care service that
both prevented future cancer and screened for
current cancer—and therefore should be provided
with no cost sharing. Most insurance plans are
currently required to cover preventive services and
screenings with no cost sharing. However, Tom’s
scenario includes two loopholes in this policy: 1) his
colonoscopy occurred after a FIT test, and some
insurers apply cost sharing to the patient for a
colonoscopy after a positive stool test; and 2) Tom’s
doctors removed polyps as part of the procedure,
which changes the procedure from a preventive
to a diagnostic procedure under Medicare
policy—meaning Tom will likely wake up to an
unexpected bill for the service. Other loopholes
occur when a cancer survivor finishes his or her
treatment and needs continued screening for
possible cancer recurrence or secondary cancers,
and the insurance policy considers these services
to be diagnostic or follow-up care, instead of the
preventive and screening services that they are.
ACS CAN supports fixing these loopholes
in the coverage of preventive and screening
services to ensure that all these services are truly
provided to all patients with no cost sharing. Free
comprehensive preventive and screening services
will prevent patient and provider confusion,
encourage patients to use preventive and
screening services, and allow all patients to be
able to afford these services.
Other priorities to limit costs by preventing
cancer through the use of screening and
preventive services:
■
Funding that makes evidence-based prevention
and early detection programs available to
those who remain uninsured, including cancer
screenings, HPV vaccines and tobacco
cessation treatments. Targeting these programs
to areas with higher needs or cancer rates is
also crucial.
■
Requiring all Medicaid programs to
comprehensively cover all preventive and
screening services given an ‘A’ or ‘B’ by the U.S.
Preventive Services Task Force with no cost
sharing.
■
Reducing tobacco use and exposure to
secondhand smoke through increasing the price
of tobacco products, implementing smoke-free
policies, funding tobacco control programs and
carefully regulating tobacco products.
■
Promoting healthy eating and active living
through adequately funding evidence-based
programs and supporting strong nutrition
standards and quality physical activity education
in schools.
■
Prohibiting minors’ use of indoor tanning
facilities and properly regulating such facilities.
While the preventive measures discussed above
require some up-front investments, research
shows that these interventions are cost-effective
and that these investments pay off to prevent
cancer and improve the health of communities.
62
,63 , 64, 65, 66, 67, 68
The best way to reduce the costs of
cancer for any individual is to prevent them from
developing cancer in the first place.

39American Cancer Society Cancer Action Network The Costs of Cancer 2020
Ensuring Access to Health Care
Services
Health insurance must provide true access to
care by covering needed services at costs that
are affordable to patients. Making care affordable
includes addressing the underlying costs of
treatments, as well as the cost sharing patients
must pay to receive them.
Spotlight on ACS CAN Policy Priorities:
Address High-Deductible Health Plans
(HDHPs)
Each patient in our scenarios who had a
deductible had to pay it very quickly, and the
higher their deductible, the more patient spending
spiked at the beginning of the patient’s year(s)
in cancer treatment. The IRS defines an HDHP
in 2020 as any plan with a deductible of at least
$1,400 for an individual or $2,800 for a family,
69
and deductibles in the private insurance market
can be much higher. The number of individuals
who enroll in HDHPs also continues to rise
70
—
sometimes because it is their only choice. While
HDHPs are required to cover preventive and
screening services with no cost sharing pre-
deductible, the deductible applies to most other
services—like the diagnosis and treatment of
cancer.
The evidence is mounting that high deductibles
can cause serious problems if an enrollee is
diagnosed with cancer. Studies show that HDHP
enrollment is associated with a decrease in
imaging tests
71
—the tests a patient needs if they
have a positive screening test for suspected
cancer—and that women who were switched to
an HDHP were more likely to experience delays
in diagnostic breast imaging, breast biopsy, early-
stage breast cancer diagnosis, and chemotherapy
initiation.
72
Among individuals with a history of
cancer, HDHPs are associated with more delayed
or foregone care, although these access to care
problems are lessened somewhat if the patient
has a health savings account (HSA).
73
Another
study showed that breast cancer patients with
HDHPs show such delays in care even when
researchers divide patients by income level
74
—
meaning higher incomes do not insulate cancer
patients from the effect of being required to pay
large bills up front for cancer care. Additionally,
having an HDHP has been shown to make a
cancer survivor more likely to experience material,
psychological and behavioral financial hardship
75
—
hardships that can have long and lasting effects
on cancer patients and their families.
For all these reasons, ACS CAN has serious
concerns about the proliferation of HDHPs—
especially among enrollees who have low- and
middle-incomes, may not fully understand the
implications of a high deductible plan and
therefore be ultimately ill-equipped to pay
their deductible. These individuals and families
are likely to experience problems accessing
preventive care, cancer care and other health care
services when they need them. To address these
problems, ACS CAN supports policies that:
■
Ensure that certain health care services are
not subject to the deductible, and therefore
are available for free or lower cost sharing so
patients are not deterred from receiving them.
This includes services that prevent disease,
detect cancer early, and help maintain patient
health.
■
Increase enrollment assistance and financial
navigation services so that potential and current
enrollees can receive help understanding their
insurance benefit and what they will have to pay
up-front for health care services. These services
should be targeted towards low- and middle-
income individuals.
■
Monitor and track the size of deductibles
and study the impact of these deductibles on
enrollees’ access to care and health outcomes.
Prohibit Surprise Medical Billing
When Franklin had surgery to remove his prostate

40 American Cancer Society Cancer Action Network The Costs of Cancer 2020
and check his lymph nodes for cancer, he was
surprised to learn that the anesthesiologist
his in-network hospital provided was actually
out-of-network—and wanted to bill Franklin for
over $2,000. Surprise billing affects millions
of consumers each year, including people with
cancer. In an ACS CAN survey of cancer survivors
conducted in 2019, 24% reported having
received a surprise bill as a result of their cancer
care, and 27% of these bills were for amounts of
over $2,000. The most common services resulting
in surprise bills wre outpatientradiology and
pathology.
76
Recent studies of other populations
confirm that this problem is widespread,
77,78,79
and
amounts of these bills are increasing.
80
Survivor Views: The Costs of Cancer in
Their Own Words
“Charges in the hospital are confusing. You
are visited multiple times a day and night and
you aren’t thinking “Will this person present
a bill?” and “Is this person in my network?”
Why would a hospital employ a provider that
is not in the network? Am I expected to ask
every time someone does a test or a room
visit? That is unreasonable, especially when I
was in ICU and pretty much out of it.”
Multiple Cancer Survivor, Indiana
ACS CAN supports legislative and regulatory
policies at the state and federal level that prohibit
patients from being surprise billed for unexpected
out-of-network care and strongly urges
Congress to pass federal legislation promptly
so that patients across the country can benefit.
Legislation addressing surprise billing should:
1) hold patients harmless, 2) apply protections
to all insurance plans, 3) apply protections to
all surprise bills, 4) apply protections to all care
settings, 5) require transparency in addition to—
and not instead of—surprise billing protections,
6) require additional research and data collection,
and 7) strengthen state protections instead of
weakening them.
81
Stop the Proliferation of Non-Comprehensive
Health Insurance Plans
When Brian, the lymphoma patient, had a short-
term limited duration plan, he had to pay $49,782
out-of-pocket for his treatments—this was by far
the highest amount any of our patients had to pay
under any of the insurance designs we modeled.
Short-term limited duration plans traditionally
have low premiums but fail to provide the kind
of comprehensive coverage an individual would
need if they were diagnosed with a serious
and unplanned disease such as cancer. Issuers
offering short-term limited duration plans are
permitted to engage in medical underwriting,
meaning issuers can deny coverage to people with
pre-existing conditions, charge more based on a
person’s health status, or refuse to cover services
related to an individual’s pre-existing conditions.
They are also permitted to impose lifetime and
annual limits on coverage and are not required to
provide coverage of the ACA’s essential health
benefits. Short-term limited duration plans often
engage in post-claims underwriting (currently
prohibited for ACA-compliant plans), meaning
that once a person is enrolled in coverage if they
submit claims for an expensive service, the issuer
could undertake an investigation to determine
whether the enrollee’s condition constituted a pre-
existing condition. In addition, short-term limited
duration policies can and will end coverage at the
policy’s term, even if the policyholder has gotten
sick and needs coverage to continue.
82
For all of
these reasons, patients enrolled in these non-
comprehensive plans are left extremely vulnerable
to what can be exhorbitantly high out-of-pocket
costs, and all the problems and financial toxicity
such costs cause. Additionally, allowing these
plans into a marketplace negatively impacts
the risk pool and availability and affordability of
ACA-compliant plans by syphoning off younger,
healthier consumers who will be more likely to
purchase cheaper, bare bones plans.
83
ACS CAN urges policymakers to consider
prohibiting the sale, or at the very least limiting
the availability of, short-term limited duration
plans and other non-comprehensive plans. Since
the administration expanded access to short-
term limited duration plans in 2018, there has
been a significant increase in the availability and
coverage length for short-term limited duration
plans. This can be confusing to consumers who
may mistake these plans for comprehensive,
ACA-compliant coverage. Policymakers could
also consider requiring these non-comprehensive
plans to follow the rules that ACA-compliant plans
must follow.

41American Cancer Society Cancer Action Network The Costs of Cancer 2020
Cap Patient Out-of-Pocket Expenses in
Medicare
Our patient profiles showed that patients with
Medicare sometimes have high out-of-pocket
spending throughout the year, particularly
individuals who lack supplemental coverage.
Seniors and disabled Medicare beneficiaries
are often on a fixed income and have trouble
affording these high costs. If patients can’t afford
their cost-sharing, they may skip necessary
doctor’s visits or treatments, or split pills to save
money. As health care costs continue to rise,
patients need the protection of annual maximum
out-of-pocket caps—and while most consumers
have this protection in their employer-sponsored
or private insurance plan, they lose this protection
when they enroll in Medicare.
ACS CAN strongly supports efforts to cap
patient out-of-pocket spending in Medicare.
Several recent federal bills proposed such a
cap in Medicare Part D, which would help many
enrollees with cancer who have high and ongoing
costs for prescription drugs—ensuring that they
are able to take their drugs as needed, improving
their cancer outcomes. ACS CAN encourages
policymakers to enact this Part D cap and
continue finding ways to limit total out-of-pocket
spending for Medicare enrollees by considering
caps in other parts of Medicare (e.g., Part A and
B). This is especially important for those Medicare
enrollees who do not have supplemental or
Medigap coverage that protects them from high
out-of-pocket expenses in Part B. Capping out-
of-pocket spending in Medicare will reduce the
financial toxicity of cancer for Medicare enrollees,
and will give these enrollees more predictability in
their annual expenses, which is especially helpful
to those on fixed incomes.
Ensure Access to Biomarker Testing
Several patients in our profiles received biomarker
testing to determine if certain targeted therapies
would work to fight their cancers. Advances in
precision medicine in cancer have led to targeted
therapies that only work within populations of
cancer patients with very specific biomarkers.
Over the last several years, there has been
a rapid increase in the development of new
targeted therapies across cancer types and the
diagnostics required to determine benefits from
specific therapies. Unfortunately, many patients
who should be tested are not as testing rates lag
behind clinical guideline recommendations, even
years after new biomarkers are recognized and
therapies are developed. In a 2020 ACS CAN
survey, only 39% of cancer survivors reported
having their tumor tested. About one in eight
respondents indicated that biomarker testing was
not covered by their insurance, and 15% of those
who did receive biomarker testing reported paying
more than $500 out-of-pocket for the testing.
84
Insurer coverage is an important factor in provider
uptake and patient access to biomarker testing.
However, coverage of tests differs across health
care payers. To ensure patients have access to
appropriate biomarker testing ACS CAN supports
polices that:
■
Ensure coverage of FDA-cleared or -approved
companion and complementary diagnostics and
all National Comprehensive Cancer Network
(NCCN) guideline-indicated biomarker tests
as necessary to evaluate patient eligibility for a
given targeted therapy.
■
Ensure coverage for tumor-agnostic biomarker
tests as medically appropriate.
As precision medicine shifts the way health
care providers and patients think about cancer
treatments, it will be important to identify barriers
to biomarker testing. Addressing these barriers
will require buy-in from diverse stakeholders
across the health care system.
85
Ensure Working Cancer Patients, Survivors and
Caregivers Have Paid Leave
Each cancer patient in our scenarios had to
spend significant time at doctors’ appointments

42 American Cancer Society Cancer Action Network The Costs of Cancer 2020
and for procedures—and most of them were
working when they were diagnosed. The
National Health Interview Survey (NHIS)
indicates just over 6 million people with a
cancer history were employed in the U.S. in
2018.
86
These individuals want to be productive
employees during treatment and survivorship for
many reasons—not the least of which are that
working brings much needed income and often
health insurance coverage. But cancer treatment
is time consuming. Flexibility to balance
cancer treatment and employment is essential.
Additionally, many caregivers of cancer patients
are working and need these accommodations
as well. Studies show that cancer patients
who have paid leave have higher rates of job
retention and lower rates of financial burden.
87,8 8
Yet not all cancer patients and survivors who
work have access to paid leave. NHIS data
show that only 58% of individuals with a cancer
history over the age of 18 have access to paid
sick leave.
89
ACS CAN supports policies at the national, state
and local levels that increase access to job-
protected paid family and medical leave that can
be used for cancer treatments, survivorship care,
and caregiving as well as other illnesses.
Increase Patient Access to and Use of Generic
and Biosimilar Prescription Drugs
Patients and health care payers can save
money when patients use a generic or biosimilar
alternative to a branded drug. When Carla, the
breast cancer patient in our scenario, used
a biosimilar alternative to her targeted drug
therapy, total expenditures for that drug (what
Carla paid + what her insurer/employer paid)
were decreased by 21%. Savings can be even
bigger when generic alternatives to branded
drugs are available—in fact, generics saved
patients with cancers more than $13 billion in
2019, and savings for the past 10 years total
$87.8 billion.
90
While it is important to continue to incentivize
innovation through research that leads to
development of new drug therapies, diagnostics
and screenings; it is also important that patients
have access to and are prescribed lower cost
drug alternatives when they are available and
medically appropriate for the individual. ACS CAN
supports policy efforts to ensure that biosimilar
and generic drugs are available to patients
either through direct prescription or appropriate
pharmacy substitution of interchangeable
products. Further, ACS CAN encourages
policymakers to explore policies that would
increase access through reducing or eliminating
cost-sharing for patients taking a biosimilar and
incentivize biosimilar utilization through payment
policies. Lastly, we support efforts that remove
artificial barriers to the development and approval
of generics and biosimilars.
Ensure Patients Can Use Co-pay Coupons and
Discounts
In our patient scenarios, Franklin had to take
a drug that did not have a lower cost generic
or biosimilar alternative and used a co-pay
coupon to help him pay the cost of the drug.
These coupons, often distributed through patient
assistance programs, can give patients access to
a life-saving drug that they otherwise could not
afford. Despite these benefits, because of federal
anti-kickback rules, Medicare enrollees are not
allowed to use these programs or coupons—
leaving them vulnerable to high drug costs.
The Costs of Cancer Disparities
For most racial/ethnic groups, female cancer
survivors are more likely than males to report
not adhering to prescribed medications for
financial reasons. However, overall, Hispanics
and African Americans of either sex are more
likely to report medication non-adherence due
to cost than other racial/ethnic groups.
91

43American Cancer Society Cancer Action Network The Costs of Cancer 2020
Additionally, some pharmacy benefit managers,
insurers and/or employers are implementing
“accumulator adjustment programs,” which prevent
the costs that are covered by a patient assistance
program or co-pay coupon from applying
towards the patient’s deductible or out-of-pocket
maximum.
A decision regarding oncology treatment
should be a medical decision between a doctor
and patient. Patient assistance programs help
enrollees to have access to the most appropriate
prescription drugs. Prohibiting the use of these
programs or not counting their support toward
out-of-pocket spending requirements could deny
cancer patients access to medically necessary
prescription drugs. At the same time, these
programs should not be used to steer patients
toward a higher-cost medication when a less
expensive alternative is available, covered and
medically appropriate for an enrollee. ACS CAN
supports policies that ensure patients can use
these coupons to help afford their drugs in
situations where there is no clinically appropriate
alternative.
Survivor Views: The Costs of Cancer in
Their Own Words
“ Even with what is considered decent
Insurance the financial impact of cancer is
crippling. There is a never-ending series of
doctor’s visits and test all adding up to out
of pocket expenses that over multiple years
completely drain you financially. You can’t
even think about making a nonessential
purchase out of fear of the next medical bill
that will popup.”
Breast Cancer Survivor, Michigan
Other priorities to ensuring access to care:
■
Maintaining the Essential Health Benefit (EHB)
coverage requirements for individual and small
group marketplace health insurance plans
■
Maintaining the ACA requirement that all private
insurance plans have a maximum out-of-pocket
limit for patient spending on in-network, covered
services
■
Maintaining the ACA prohibition on annual and
lifetime limits in insurance plans
■
Maintaining and strengthening insurance plan
network adequacy standards so cancer patients
will have access to the providers they need in-
network
■
Requiring insurance plans to maintain robust
formularies with utilization management
practices that are based on clinical evidence
and treatment guidelines and do not prohibit
patients from taking the medication that their
doctor has determined is the right choice for
them. This includes standardizing plans’ prior
authorization processes to 1) make them
electronic, efficient, and easy for patients
and providers to use, and 2) require specific
response times on requests so patients have
timely access to the treatments they need.
■
Requiring that patients have access to an
efficient and timely appeals process in cases
where a cancer patient needs medications or
services that are not covered or are subject
to utilization management tools (such as prior
authorization, step therapy, or quantity limits)
■
Limiting the amount that patients must pay
out-of-pocket for their drugs, including policies
that encourage plans to use only co-pays on
their formularies (which are more transparent
and predictable than co-insurance), policies that
cap cost-sharing amounts for drugs and policies
that cap all out-of-pocket drug spending for the
year
■
Requiring plans to cover oral anti-cancer drugs
with cost-sharing amounts that are comparable
to their coverage of physician-administered
anti-cancer drugs
Addressing the affordability of cancer care—
including the base costs of treatments as well
as the cost sharing and out-of-pocket expenses
patients must pay—is paramount in ensuring true
access to health care.
Reducing the Overall Financial
Impact of Cancer for Patients
and Their Families
Reducing the costs of cancer does not only
mean reducing the actual out-of-pocket costs
for patients—it also means addressing and
preventing the long-term financial impact that
high health care costs have on people with cancer
and their families, and finding ways to help them
plan for and afford the costs they have to pay.

44 American Cancer Society Cancer Action Network The Costs of Cancer 2020
Survivor Views: The Costs of Cancer in
Their Own Words
“ As a single mom, I rely on my employer’s
health care plan for my children’s insurance
and my own. This also means that any out-of-
pocket costs (meeting deductibles, co-pays,
etc.) are solely my responsibility…
The financial toxicity brought on by cancer
and the aftermath of its treatment is
devastating--some months it can equal my
mortgage payment.”
Breast Cancer Survivor, Michigan
Spotlight on ACS CAN Policy Priorities:
Help Patients “Smooth” Their High Out-of-
Pocket Costs
Several patients in our profiles had large ‘spikes’
in their out-of-pocket spending in the 1-2 months
after their first doctor’s visit that led to their
cancer diagnosis. Cancer patients are especially
vulnerable to these spikes because many cancer
treatments and diagnostic tests are high-cost
and scheduled within a short amount of time—
requiring the patient to spend through their
deductible and out-of-pocket maximum quickly.
While many patients have challenges paying
multiple thousands of dollars out-of-pocket over
the course of a year, it is even more challenging
when this amount of spending is required in a
short time—monthly budgets simply can’t afford
these large bills, especially at the same time as
the family is dealing with a life-changing cancer
diagnosis. Large spending spikes like these
greatly contribute to the financial toxicity that
people with cancer face. Many patients would
benefit from having the option to “smooth” out
their payments or spread them out over the
course of the year—much like consumers have
the option to pay for a new car in installments
through a payment plan.
This concept of allowing patients to “smooth”
their out-of-pocket costs has taken hold in the
last few years in encouraging ways. Recent policy
proposals to cap patient out-of-pocket expenses
in Medicare Part D plans also included options
to smooth these costs for Medicare patients that
hit their cap. One way to accomplish this goal is
to systematically identify Medicare patients who
are going to reach the catastrophic drug out-of-
pocket spending level (currently $6,350) in the
span of one or two months, or with one or two
fills of a prescription, and offer these patients
the option to pay their expected annual cost in
monthly, interest-free installments. This kind of
policy could also be applied to other parts of
Medicare, as well as in other types of insurance
plans. Other policies that use ‘smoothing’
principles include policies that cap co-pays/co-
insurance per monthly prescription for cancer
drugs—a policy that has passed in several states.
Additionally, some states have explored requiring
plan issuers to offer a certain number of plan
designs in their marketplaces that only use
co-pays for prescription drugs, rather than co-
insurance that leaves patients vulnerable to high
and unexpected cost spikes. ACS CAN supports
policies that will help patients with high costs
avoid spikes, smooth their costs throughout the
year and hopefully avoid the consequences of
financial toxicity. However, we also note that most
of these ‘smoothing’ solutions explored so far deal
only with pharmacy drug costs. While this is one
category of spending that tends to be high for
cancer patients, it is not the only one. ACS CAN
supports exploring smoothing solutions for all
patient out-of-pocket costs.
Other priorities to reduce the overall financial
impact of cancer:
■
Requiring health care providers to give patients
estimates of their costs for a procedure or
treatment before that treatment occurs so
patients can plan for expenses or ‘shop’ for
providers that may perform the service at a
lower cost
■
Requiring insurance plans to be clear and
transparent about what cost-sharing amounts
are required for drugs—particularly translating
co-insurance to dollar amounts for outpatient
drugs and drugs covered under the medical
benefit– so that patients are not surprised by
charges when they arrive at the pharmacy/
physician’s office
■
Funding programs that provide patients
with financial navigators who can help them
determine how much treatments will cost, how
to plan for these costs and how to best use
their insurance benefits
■
Requiring certain providers—like participants in
the Oncology Care Model
92
—to provide financial

45American Cancer Society Cancer Action Network The Costs of Cancer 2020
navigation services to cancer patients
■
Gathering more information on the options
cancer patients are given to help pay large
medical bills and potential problems—i.e. Are
patients being required to pay high, or any,
interest rates on payment plans? Are all patients
offered these options equally? What happens
when a patient is not able to pay on schedule?
■
Finding ways to help people with cancer and
their families who have significant medical
debt because of their treatment, including
ensuring medical debt does not factor into an
individual’s credit score and potentially creating
debt forgiveness programs for cancer and other
seriously ill patients
ACS CAN is committed to finding policy solutions
that help address the long-term costs of cancer, and
the huge impacts these costs can have all aspects
of cancer patients’ and their caregivers’ lives.
Conclusion
For the millions of Americans diagnosed with
cancer each year, the cost of treating the disease
can be staggering. ACS CAN will continue to
advocate for changes to the health care system
that make care more affordable for cancer
patients, survivors and those at risk for cancer.
Survivor Views:
The Costs of Cancer in Their Own Words
“This treatment has saved my life but now I’m
in debt $365k +..my portion after insurance.
I’ll spend the rest of my life left paying this off.”
Survivor of Multiple Cancers, Colorado
Survivor Views:
The Costs of Cancer in Their Own Words
“Cancer and/or the treatments caused me to have to leave my job
permanently. Going from a double income home to single income was
incredibly difficult on our family. No one should have to worry about
how to pay for services or if they need to stay in a job they cannot
perform any longer to pay for proper medical care. No one should have
to deny a treatment for fear of debt. My diagnosis was 3 years ago and
I am still paying. I am in collections. It is overwhelming and stressful
at a time I need to reduce stress. Very afraid if ACA is repealed I will
become a “pre-existing condition” and be denied insurance.”
Breast Cancer Survivor, Massachusetts

46 American Cancer Society Cancer Action Network The Costs of Cancer 2020
1 Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA A Cancer J Clin. 2020;70(1):7-30. doi:10.3322/caac.21590
2 Data retrieved from the Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey, 2018. https://meps.ahrq.
gov/mepsweb/
3 “Private insurance” includes employer-sponsored, self-funded insurance; as well as fully-insured private plans and expenditures
from Medigap plans. “Other” includes care provided by the Veteran’s Administration or covered by Other Federal, State, or Local
Insurance; Workers’ Compensation; Other Private Insurance; and Other Unknown Insurance.
4 2019 Employer Health Benefits Survey. Kaiser Family Foundation; 2019. https://www.kff.org/report-section/ehbs-2019-section-
8-high-deductible-health-plans-with-savings-option/
5 ACS CAN. Survivor Views: Surprise Billing and Prescription Cost and Coverage Survey Findings Summary. December 4, 2019.
https://www.fightcancer.org/policy-resources/survivor-views-surprise-billing-and-prescription-cost-and-coverage-survey-findings
6 CAR T-Cell Therapy. National Cancer Institute Dictionary of Cancer Terms. https://www.cancer.gov/publications/dictionaries/
cancer-terms/def/car-t-cell-therapy
7 Treatment & Support. American Cancer Society. https://www.cancer.org/treatment
8 Rolleri C. Cancer Care by Zip Code: Examining Geographic Health Disparities in the United States. ASCO Connection.
Published March 7, 2019. https://connection.asco.org/magazine/features/cancer-care-zip-code-examining-geographic-health-
disparities-united-states
9 Rolleri C. Cancer Care by Zip Code: Examining Geographic Health Disparities in the United States. ASCO Connection.
Published March 7, 2019. https://connection.asco.org/magazine/features/cancer-care-zip-code-examining-geographic-health-
disparities-united-states
10 Henley SJ, Jemal A: Rural cancer control: Bridging the chasm in geographic health inequity. Cancer Epidemiol Biomarkers Prev
27:1248-1251, 2018
11 Ekwueme DU, Zhao J, Rim SH, et al. Annual Out-of-Pocket Expenditures and Financial Hardship Among Cancer Survivors Aged
18–64 Years — United States, 2011–2016. MMWR Morb Mortal Wkly Rep. 2019;68(22):494-499. doi:10.15585/mmwr.
mm6822a2
12 Note: most Medicare enrollees, including Tom, do not pay premiums for Part A
13 Note: this represents the ‘standard’ premium for Part B. Higher-income enrollees pay larger amounts.
14 African American Men More Likely to Die from Low-Grade Prostate Cancer. National Cancer Institute Cancer Currents Blog.
Published January 28, 2019. https://www.cancer.gov/news-events/cancer-currents-blog/2019/prostate-cancer-death-disparities-
black-men
15 Cancer Disparities: A Chartbook. American Cancer Society Cancer Action Network; 2018. https://www.fightcancer.org/sites/
default/files/National%20Documents/Disparities-in-Cancer-Chartbook.pdf
16 Note: most Medicare enrollees, including Shonda, do not pay premiums for Part A
17 Note: this represents the ‘standard’ premium for Part B. Higher-income enrollees pay larger amounts.
18 Board of Governors of the Federal Reserve System. Report on the Economic Well-Being of U.S. Households in 2019, Featuring
Supplemental Data from April 2020. Published May 2020. https://www.federalreserve.gov/publications/files/2019-report-
economic-well-being-us-households-202005.pdf
19 Zheng S, Ren ZJ, Heineke J, Geissler KH. Reductions in Diagnostic Imaging With High Deductible Health Plans: Medical Care.
2016;54(2):110-117. doi:10.1097/MLR.0000000000000472
20 https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-hispanics-and-
latinos/cancer-facts-and-figures-for-hispanics-and-latinos-2018-2020.pdf
21 Yabroff KR, et al. Health Insurance Coverage Disruptions and Cancer Care and Outcomes: Systematic Review of Published
Research. JNCI: Journal of the National Cancer Institute. July 2020;112(7): https://doi.org/10.1093/jnci/djaa048
22 With the exception of the short-term limited duration plan analyzed. See methodology appendix for more information.
23 Keisler-Starkey K, Bunch L. Health Insurance Coverage in the United States: 2019. United States Census Bureau; 2020.
https://www.census.gov/library/publications/2020/demo/p60-271.html
24 Kaiser Family Foundation. Key Facts about the Uninsured Population. Published December 13, 2019. https://www.kff.org/
uninsured/issue-brief/key-facts-about-the-uninsured-population/
25 Note that this loophole has been closed in private insurance plans, but not it will take an Act of Congress to make this change for
Medicare enrollees.
26 Ducharme J, Barone E. How the COVID-19 Pandemic has Changed Cancer Care, in 4 Charts. Time Magazine. Published August
28, 2020. https://time.com/5884236/coronavirus-pandemic-cancer-care/
27 Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the Number of US Patients With Newly Identified Cancer Before and
During the Coronavirus Disease 2019 (COVID-19) Pandemic. JAMA Netw Open. 2020;3(8):e2017267. doi:10.1001/
jamanetworkopen.2020.17267
References

47American Cancer Society Cancer Action Network The Costs of Cancer 2020
28 Early cancer diagnosis saves lives, cuts treatment costs. World Health Organization: Newsroom. Published February 3, 2017.
https://www.who.int/news-room/detail/03-02-2017-early-cancer-diagnosis-saves-lives-cuts-treatment-costs
29 Kakushadze Z, Raghubanshi R, Yu W. Estimating Cost Savings from Early Cancer Diagnosis. Data. 2017;2(3):30. doi:10.3390/
data2030030
30 Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the Number of US Patients With Newly Identified Cancer Before and
During the Coronavirus Disease 2019 (COVID-19) Pandemic. JAMA Netw Open. 2020;3(8):e2017267. doi:10.1001/
jamanetworkopen.2020.17267
31 Ohri N, Rapkin BD, Guha C, Kalnicki S, Garg M. Radiation Therapy Noncompliance and Clinical Outcomes in an Urban
Academic Cancer Center. International Journal of Radiation Oncology, Biology, Physics. 2016;95(2):563-570. doi:10.1016/j.
ijrobp.2016.01.043
32 Deek MP, Kim S, Ahmed I, et al. Prognostic Impact of Missed Chemotherapy Doses During Chemoradiation Therapy
for Non–Small Cell Lung Cancer: American Journal of Clinical Oncology. Published online June 2016:1. doi:10.1097/
COC.0000000000000293
33 The COVID-19 Pandemic and Resulting Economic Crash Have Caused the Greatest Health Insurance Losses in American
History. The National Center for Coverage Innovation at Families USA; 2020. https://www.familiesusa.org/resources/the-covid-
19-pandemic-and-resulting-economic-crash-have-caused-the-greatest-health-insurance-losses-in-american-history/
34 Ward E, Halpern M, Schrag N, et al. Association of Insurance with Cancer Care Utilization and Outcomes. CA: A Cancer Journal
for Clinicians. 2008;58(1):9-31. doi:10.3322/CA.2007.0011
35 Karaca-Mandic P, Georgiou A, Sen S. Assessment of COVID-19 Hospitalizations by Race/Ethnicity in 12 States. JAMA Intern
Med. Published online August 17, 2020. doi:10.1001/jamainternmed.2020.3857
36 Garg S, Kim L, Whitaker M, et al. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed
Coronavirus Disease 2019 — COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458-
464. doi:10.15585/mmwr.mm6915e3
37 Sloan C, Duddy-Tenbrunsel R, Ferguson S, Valladares A, Kornfield T. COVID-19 Projected to Worsen Racial Disparities in
Coverage. Avalere Health. Published September 16, 2020. https://avalere.com/press-releases/covid-19-projected-to-worsen-
racial-disparities-in-health-coverage
38 Financial Toxicity. National Cancer Institute Dictionary of Cancer Terms. https://www.cancer.gov/publications/dictionaries/cancer-
terms/def/car-t-cell-therapy
39 Zheng Z, Jemal A, Han X, et al. Medical financial hardship among cancer survivors in the United States. Cancer.
2019;125(10):1737-1747. doi:10.1002/cncr.31913
40 Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR. Financial Hardships Experienced by Cancer Survivors: A Systematic
Review. JNCI J Natl Cancer Inst. 2017;109(2):djw205. doi:10.1093/jnci/djw205
41 Zhao J, Han X, Zheng Z, Banegas MP, Ekwueme DU, Yabroff KR. Is Health Insurance Literacy Associated With Financial
Hardship Among Cancer Survivors? Findings From a National Sample in the United States. JNCI Cancer Spectrum.
2019;3(4):pkz061. doi:10.1093/jncics/pkz061
42 Zheng Z, Jemal A, Tucker-Seeley R, et al. Worry About Daily Financial Needs and Food Insecurity Among Cancer Survivors in the
United States. Journal of the National Comprehensive Cancer Network. 2020;18(3):315-327. doi:10.6004/jnccn.2019.7359
43 Lathan CS, Cronin A, Tucker-Seeley R, Zafar SY, Ayanian JZ, Schrag D. Association of Financial Strain With Symptom Burden
and Quality of Life for Patients With Lung or Colorectal Cancer. JCO. 2016;34(15):1732-1740. doi:10.1200/JCO.2015.63.2232
44 Chino F, Peppercorn J, Taylor DH, et al. Self‐Reported Financial Burden and Satisfaction With Care Among Patients With Cancer.
The Oncologist. 2014;19(4):414-420. doi:10.1634/theoncologist.2013-0374
45 Huang I-C, Bhakta N, Brinkman TM, et al. Determinants and Consequences of Financial Hardship Among Adult Survivors
of Childhood Cancer: A Report From the St. Jude Lifetime Cohort Study. JNCI: Journal of the National Cancer Institute.
2019;111(2):189-200. doi:10.1093/jnci/djy120
46 Ramsey SD, Bansal A, Fedorenko CR, et al. Financial Insolvency as a Risk Factor for Early Mortality Among Patients With Cancer.
JCO. 2016;34(9):980-986. doi:10.1200/JCO.2015.64.6620
47 Ward E, Halpern M, Schrag N, et al. Association of Insurance with Cancer Care Utilization and Outcomes. CA: A Cancer Journal
for Clinicians. 2008;58(1):9-31. doi:10.3322/CA.2007.0011
48 Zhao J, Han X, Nogueira L, Jemal A, Halpern MT, Yabroff KR. Health insurance status and cancer stage at diagnosis and survival
in the United States. JCO. 2020;38(15_suppl):7026-7026. doi:10.1200/JCO.2020.38.15_suppl.7026
49 ACS CAN. Understanding Access to Care During the COVID-19 Pandemic: September 2020 Survey Findings Summary. https://
www.fightcancer.org/sites/default/files/Survivor%20Views%20COVID%20Access%20Polling%20Memo%202020.10.08_Final.
pdf
50 Soni A, Sabik LM, Simon K, Sommers BD. Changes in insurance coverage among cancer patients under the Affordable Care
Act. JAMA Oncol. 2018;4(1):122-24.

48 American Cancer Society Cancer Action Network The Costs of Cancer 2020
51 Doty M, Collins S, Kriss J, Rustgi S. Failure to Protect: Why the Individual Insurance Market Is Not a Viable Option for Most
U.S. Families. The Commonwealth Fund. Published July 21, 2009. https://www.commonwealthfund.org/publications/issue-
briefs/2009/jul/failure-protect-why-individual-insurance-market-not-viable
52 Ward E, Halpern M, Schrag N, et al. Association of Insurance with Cancer Care Utilization and Outcomes. CA: A Cancer Journal
for Clinicians. 2008;58(1):9-31. doi:10.3322/CA.2007.0011
53 Han X, Yabroff KR, Ward E, Brawley OW, Jemal A. Comparison of Insurance Status and Diagnosis Stage Among Patients With
Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act. JAMA Oncol.
2018;4(12):1713. doi:10.1001/jamaoncol.2018.3467
54 Han X, Yabroff KR, Ward E, Brawley OW, Jemal A. Comparison of Insurance Status and Diagnosis Stage Among Patients With
Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act. JAMA Oncol.
2018;4(12):1713. doi:10.1001/jamaoncol.2018.3467
55 Petronio B, Cooper A, Piepenburg C, Rouvelas M, Longstreth J. Amici Curiae Brief in Support of Petitioners and Reversal
by the American Cancer Society et Al. American Cancer Society https://www.fightcancer.org/sites/default/files/National%20
Documents/SCOTUS%20Amici%20Brief%20-%20American%20Cancer%20Society.pdf
56 Rae M, McDermott D, Levitt L, Claxton G. Long-Term Trends in Employer-Based Coverage. Peterson-KFF Health System Tracker;
2020. https://www.healthsystemtracker.org/brief/long-term-trends-in-employer-based-coverage/#item-start
57 Status of State Action on Medicaid Expansion Decision. Kaiser Family Foundation. Published October 1, 2020. https://www.kff.
org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&s
ortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
58 Re: Request to Amend Wisconsin’s Section 1115 BadgerCare Reform Demonstration Project. medicaid.gov. Published June 7,
2017. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/wi/wi-badgercare-
reform-pa.pdf
59 Group VIII Work Requirement and Community Engagement 1115 Demonstration Waiver. medicaid.ohio.gov. https://www.
medicaid.ohio.gov/Portals/0/Resources/PublicNotices/GroupVIII/Detail-GroupVIII-021618.pdf?ver=2018-02-16-092910-683
60 Sommers BD, Goldman AL, Blendon RJ, Orav EJ, Epstein AM. Medicaid Work Requirements — Results from the First Year in
Arkansas. N Engl J Med. 2019;381(11):1073-1082. doi:10.1056/NEJMsr1901772
61 Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA: A Cancer Journal for Clinicians. 2017;67(1):7-30. doi:10.3322/
caac.21387
62 Dilley JA, Harris JR, Boysun MJ, Reid TR. Program, Policy, and Price Interventions for Tobacco Control: Quantifying the Return on
Investment of a State Tobacco Control Program. Am J Public Health. 2012;102(2):e22-e28. doi:10.2105/AJPH.2011.300506
63 2011 Independent Evaluation Report of the New York Tobacco Control Program. RTI International; 2011. https://www.health.
ny.gov/prevention/tobacco_control/docs/2011-09_independent_evaluation_report.pdf
64 Lightwood J, Glantz SA. The Effect of the California Tobacco Control Program on Smoking Prevalence, Cigarette Consumption,
and Healthcare Costs: 1989–2008. Fielding R, ed. PLoS ONE. 2013;8(2):e47145. doi:10.1371/journal.pone.0047145
65 Roux L, Pratt M, Tengs TO, et al. Cost Effectiveness of Community-Based Physical Activity Interventions. American Journal of
Preventive Medicine. 2008;35(6):578-588. doi:10.1016/j.amepre.2008.06.040
66 Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Goodman MJ, Solberg LI. Priorities Among Effective Clinical Preventive
Services. American Journal of Preventive Medicine. 2006;31(1):52-61. doi:10.1016/j.amepre.2006.03.012
67 Maciosek MV, Coffield AB, Flottemesch TJ, Edwards NM, Solberg LI. Greater Use Of Preventive Services In U.S. Health Care
Could Save Lives At Little Or No Cost. Health Affairs. 2010;29(9):1656-1660. doi:10.1377/hlthaff.2008.0701
68 Richard P, West K, Ku L. The Return on Investment of a Medicaid Tobacco Cessation Program in Massachusetts. Verbeek JH, ed.
PLoS ONE. 2012;7(1):e29665. doi:10.1371/journal.pone.0029665
69 High Deductible Health Plan (HDHP). Healthcare.gov Glossary. https://www.healthcare.gov/glossary/high-deductible-health-
plan/
70 Cohen R, Zammitti E. High-Deductible Health Plan Enrollment Among Adults Aged 18–64 With Employment-Based
Insurance Coverage. Centers for Disease Control and Prevention; 2018. https://www.cdc.gov/nchs/products/databriefs/db317.
htm#:~:text=The%20percentage%20enrolled%20in%20an,2007%20to%2018.9%25%20in%202017.
71 Zheng S, Ren ZJ, Heineke J, Geissler KH. Reductions in Diagnostic Imaging With High Deductible Health Plans: Medical Care.
2016;54(2):110-117. doi:10.1097/MLR.0000000000000472
72 Wharam JF, Zhang F, Lu CY, et al. Breast Cancer Diagnosis and Treatment After High-Deductible Insurance Enrollment. JCO.
2018;36(11):1121-1127. doi:10.1200/JCO.2017.75.2501
73 Zheng Z, Jemal A, Banegas MP, Han X, Yabroff KR. High-Deductible Health Plans and Cancer Survivorship: What Is the
Association With Access to Care and Hospital Emergency Department Use? JOP. 2019;15(11):e957-e968. doi:10.1200/
JOP.18.00699
74 Wharam JF, Zhang F, Wallace J, et al. Vulnerable And Less Vulnerable Women In High-Deductible Health Plans Experienced
Delayed Breast Cancer Care. Health Affairs. 2019;38(3):408-415. doi:10.1377/hlthaff.2018.05026

49American Cancer Society Cancer Action Network The Costs of Cancer 2020
75 Zheng Z, Jemal A, Han X, et al. Medical financial hardship among cancer survivors in the United States. Cancer.
2019;125(10):1737-1747. doi:10.1002/cncr.31913
76 Survey: Cancer Patients and Survivors Alter or Delay Care Due to Insurance Barriers. American Cancer Society Cancer Action
Network (ACS CAN) Press Room. Published December 5, 2019. https://www.fightcancer.org/releases/survey-cancer-patients-
and-survivors-alter-or-delay-care-due-insurance-barriers
77 Cooper Z, Scott Morton F. Out-of-Network Emergency-Physician Bills — An Unwelcome Surprise. N Engl J Med.
2016;375(20):1915-1918. doi:10.1056/NEJMp1608571
78 Bai G, Anderson GF. Variation in the Ratio of Physician Charges to Medicare Payments by Specialty and Region. JAMA.
2017;317(3):315. doi:10.1001/jama.2016.16230
79 Garmon C, Chartock B. One In Five Inpatient Emergency Department Cases May Lead To Surprise Bills. Health Affairs.
2017;36(1):177-181. doi:10.1377/hlthaff.2016.0970
80 Sun EC, Mello MM, Moshfegh J, Baker LC. Assessment of Out-of-Network Billing for Privately Insured Patients Receiving Care in
In-Network Hospitals. JAMA Intern Med. 2019;179(11):1543. doi:10.1001/jamainternmed.2019.3451
81 Cancer Patients Need Protection from Surprise Medical Bills. American Cancer Society Cancer Action Network (ACS CAN)
Public Policy Resources. Published August 27, 2019. https://www.fightcancer.org/policy-resources/cancer-patients-need-
protection-surprise-medical-bills
82 Note that former enrollees in STLD plans are not eligible for continuation of coverage through COBRA, like they would be in an
employer-sponsored, ACA-compliant plan.
83 Inadequate Coverage: An ACS CAN Examination of Short-Term Health Plans. American Cancer Society Cancer Action Network
(ACS CAN) Public Policy Resources. Published May 13, 2019. https://www.fightcancer.org/policy-resources/inadequate-
coverage-acs-can-examination-short-term-health-plans
84 Cancer Biomarker Testing: The Key to Unlocking Precision Cancer Therapy. American Cancer Society Cancer Action Network
(ACS CAN). Published 2019. https://www.fightcancer.org/sites/default/files/Biomarker_One_Pager_7.22.20_0.pdf
85 For more information, please visit https://www.fightcancer.org/policy-resources/improving-access-biomarker-testing.
86 2018 National Health Interview Survey (NHIS) Public Use Data Release. National Center for Health Statistics; 2019. https://
www.cdc.gov/nchs/nhis/1997-2018.htm Analysis performed by American Cancer Society Intramural Research team, April 7,
2020.
87 Veenstra CM, Regenbogen SE, Hawley ST, Abrahamse P, Banerjee M, Morris AM. Association of Paid Sick Leave With Job
Retention and Financial Burden Among Working Patients With Colorectal Cancer. JAMA. 2015;314(24):2688. doi:10.1001/
jama.2015.12383
88 Veenstra CM, Regenbogen SE, Hawley ST, Abrahamse P, Banerjee M, Morris AM. Association of Paid Sick Leave With Job
Retention and Financial Burden Among Working Patients With Colorectal Cancer. JAMA. 2015;314(24):2688. doi:10.1001/
jama.2015.12383
89 2018 National Health Interview Survey (NHIS) Public Use Data Release. National Center for Health Statistics; 2019. https://
www.cdc.gov/nchs/nhis/1997-2018.htm Analysis performed by American Cancer Society Intramural Research team, April 7,
2020.
90 IQVIA 2019 for the Association for Accessible Medicines. “Safe, Effective Generic Drugs Help Cancer Patients.” www.
accessiblemeds.org
91 Lee M, Khan MM. Gender differences in cost-related medication non-adherence among cancer survivors. J Cancer Surviv.
2016;10(2):384-393. doi:10.1007/s11764-015-0484-5
92 See https://innovation.cms.gov/innovation-models/oncology-care.
