
i
Trinity Health,
one of the largest faith-based health care organizations in the nation, reports
excess of revenue over expenses growth of 47.3 percent or $404.9 million to $1.3 billion for the
first nine months of fiscal year 2024; net margin of 6.6 percent
Summary Highlights for the First Nine Months of FY2024 (Nine Months Ended March 31, 2024)
Trinity Health reported significant improvements in operating performance, with operating income before other
items of $69.8 million (operating margin of 0.4 percent and cash flow margin of 5.3 percent) for the nine months
ended March 31, 2024, compared to operating losses before other items of $263.1 million (operating margin
of [1.6] percent and cash flow margin of 3.7 percent) for the nine months ended March 31, 2023. Improvements
were attained in payment rates, same facility patient care volume growth and as a result of several revenue
and cost management initiatives.
Trinity Health continues to take various actions to address current challenges facing the health care industry
in fiscal year 2024. The Corporation is focused on clinical optimization and access; continued focus on the
alignment of operating costs (both labor and non-labor) with revenue; labor stabilization through expansion of
its FirstChoice internal staffing agency, recruitment efforts and clinical prioritization; optimizing revenue
realization utilizing a multifaceted payer strategy to address a challenging payer environment and obtain fair
payment rate increases; and capital prioritization and reallocation of resources to focus on investments
supporting attainment of Mission-critical initiatives. To address labor shortages, the Corporation launched a
new innovative, virtual connected care delivery model using a 3-person team with on-site and virtual nursing
named “TogetherTeam Virtual Connected Care” that is being implemented system-wide and is already active
in 22 hospitals and 58 nursing units, with additional sites slated to go live in the fourth quarter of fiscal 2024.
From these actions, the Corporation is experiencing improvements in patient and employee safety, access to
care, employee retention and patient satisfaction that are helping to improve results of operations. On a same
facility basis, volumes as measured by case mix adjusted equivalent discharges (“CMAEDs”) increased 0.5
percent during the nine months ended March 31, 2024 compared to the same period in the prior fiscal year.
The majority of the Corporation’s revenue is comprised of outpatient and other non-patient revenue. The
Corporation continues to diversify its business segments to gain better position for balanced performance when
individual segments are challenged.
Trinity Health reported growth in operating revenue of 11.4 percent or $1.8 billion to $17.8 billion in the first
nine months of fiscal year 2024 compared to the same period in the prior fiscal year. Revenue growth was
driven by the acquisitions of MercyOne in Iowa on September 1, 2022, North Ottawa Community Health System
(“Grand Haven”) in Michigan on October 1, 2022, and Genesis Health System in Iowa and Illinois on March 1,
2023, (collectively the “Acquisitions”) which contributed $1.0 billion of the increase. This increase was partially
offset by the divestiture of St. Francis Medical Center (“SFMC”) on December 22, 2022, that reduced operating
revenue by $59.3 million compared to the prior year. Excluding the Acquisitions and divestiture of SFMC,
operating revenue increased $863.8 million or 5.8 percent over the prior fiscal year. Net patient service revenue
grew $1.6 billion, or 11.7 percent, or $748.7 million and 5.8 percent excluding the Acquisitions. Same facility
net patient service revenue was positively impacted by improvements in payment rates (inclusive of $146.2
million in new Medicaid provider funding in Iowa and Medicaid rate changes in Michigan, and a $102.8 million
340B remedy lump sum settlement received from CMS under the November 8, 2023 Final Rule), same facility
patient volumes and to a lesser extent case mix.

ii
Other revenue increased $108.1 million, or 8.7 percent, compared to the prior fiscal year on a same facility
basis, primarily driven by $86.9 million of pharmacy revenue, and to a lesser extent gainshare revenue, and
equity in earnings of unconsolidated affiliates. In addition, premium and capitation revenue increased $10.0
million, primarily within the Corporation’s health plans and PACE programs.
Operating expenses increased $1.5 billion to $17.7 billion, or 9.1 percent, for the nine months ended March
31, 2024 compared to the prior fiscal year, with the Acquisitions accounting for $902.9 million of the overall
increase. Excluding the impact of the Acquisitions and divestiture of SFMC, operating expenses for the nine
months ended March 31, 2024, increased $653.0 million, or 4.3 percent. Total operating costs per case (as
measured by CMAEDs) increased 2.7 percent compared to the prior year as the Corporation continues to
tightly manage operating costs amid inflation. On a same facility basis, salaries and wages rose $380.1 million,
or 5.6 percent, inclusive of a 3.7 percent increase in salary rates and a 1.9 percent increase in FTEs, as the
Corporation continues to implement initiatives to address industry wide staffing shortages and wage inflation.
Same facility fiscal year 2024 salary rate increases include a $65 million one-time compensation award
program. Same facility employee benefit costs increased $100.2 million or 8 percent, including a $64.7 million
or 16.9 percent increase in employee health plan costs. Supply costs increased $141.4 million, or 5.3 percent,
on a same facility basis compared to the prior fiscal year, primarily due to increased pharmacy volume.
Although overall supply costs increased, same facility supplies as a percent of net patient service revenue,
excluding the 340B remedy settlement and accrual of the aforementioned Medicaid provider tax changes,
decreased 0.7 percent from prior year. Same facility increases were also reported in interest expense and
other expenses, which includes $55.1M of increased provider tax expense related to the aforementioned
Medicaid provider tax changes.
The Corporation continues to use strong cost controls over contract labor and other operational spending.
Labor stabilization is occurring with investments in its FirstChoice internal staffing agency and TogetherTeam
Virtual Connected Care model. On a same facility basis, contract labor costs decreased $71.3 million, or 25
percent compared to the prior fiscal year. Further expense reductions were seen in purchased services and
medical claims, depreciation and amortization and occupancy.
For the first nine months of fiscal year 2023, other items consisted of $53.9 million in dividend income received
from a cost method investment and an $8.0 million gain for the final settlement from the fiscal year 2022 sale
of Gateway Health Plan, L.P., and Subsidiaries, offset by $82.3 million of restructuring costs related to the
divestiture of SFMC.
The Corporation reported non-operating income of $1.2 billion for the nine months ended March 31, 2024 and
2023. Non-operating income was driven by investment earnings of $853.0 million or 9.1 percent in the first nine
months of fiscal year 2024, compared to earnings of $457.3 million or 5.4 percent during the previous fiscal
year, an increase of $395.7 million. Investment results also drove the $137.7 million improvement in equity in
earnings of unconsolidated affiliates. This was partially offset by a reduction in inherent contributions of $487.7
million primarily related to the fiscal year 2023 acquisitions of Genesis Health System and Grand Haven.
Excess of revenue over expenses for the nine months ended March 31, 2024 was $1.3 billion, net margin of
6.6 percent, compared to excess of revenue over expenses of $856.3 million, net margin of 5.1 percent, for the
nine months ended March 31, 2023.
The Corporation’s balance sheet remains strong after prompt responses to negative impacts from Change
Healthcare’s cyberattack that occurred in February 2024. While the attack did not directly impact the
Corporation’s systems, the event disrupted the billing and collection of patient accounts receivable that grew
$896.8 million as of March 31, 2024 compared to June 30, 2023, or a 19-day use of cash. Responses included

iii
a $600 million draw on liquidity facilities and receipt of Medicare cash advances, amongst others. As of March
31, 2024, days cash of 173 days declined 4 days since June 30, 2023.
Highlights as of and for the nine months ended March 31, 2024, include:
• Total assets of $34.7 billion and net assets of $19.7 billion,
• Operating revenue growth of 11.4 percent to $17.8 billion compared to the same period in the prior
fiscal year, including the impact of the Acquisitions and net of the SFMC divestiture,
• Operating cash flow before other items of $944.8 million, or 5.3 percent operating cash flow margin;
compared to operating cash flow before other items of $596.1 million or 3.7 percent operating cash
flow margin for the nine months ended March 31, 2023,
• Operating income before other items of $69.8 million, or 0.4 percent operating margin; compared to
operating loss before other items of $263.1 million or (1.6) percent operating margin for the nine
months ended March 31, 2023,
• Excess of revenue over expenses of $1.3 billion, net margin of 6.6 percent, compared to excess of
revenue over expenses of $856.3 million, net margin of 5.1 percent for the nine months ended March
31, 2023,
• Unrestricted cash and investments of $10.7 billion; days cash on hand of 173 days compared to 178
days for the year ended June 30, 2023 including the line of credit draws and Medicare cash
advances; excluding these items, days cash on hand is 161 days, or a reduction of 17 days from
June 30, 2023,
• Historical debt service coverage ratio of 3.10x compared to 1.1x required.
TRINITY HEALTH
UNAUDITED QUARTERLY REPORT
As of March 31, 2024, and June 30, 2023, and
For the nine months ended March 31, 2024 and 2023

TRINITY HEALTH
TABLE OF CONTENTS
Page
UNAUDITED CONSOLIDATED FINANCIAL STATEMENTS AS OF
MARCH 31, 2024 AND JUNE 30, 2023 AND FOR THE
NINE MONTHS ENDED MARCH 31, 2024 AND 2023:
Consolidated Balance Sheets (unaudited) 3-4
Consolidated Statements of Operations and Changes in Net Assets (unaudited) 5-6
Summarized Consolidated Statements of Cash Flows (unaudited) 7
Notes to Consolidated Financial Statements (unaudited) 8-26
MANAGEMENT’S DISCUSSION AND ANALYSIS (unaudited) 27-33
LIQUIDITY REPORT (unaudited) 34
FINANCIAL RATIOS AND STATISTICS (unaudited) 35

- 3 -
TRINITY HEALTH
CONSOLIDATED BALANCE SHEETS (UNAUDITED)
(In thousands)
March 31, June 30,
ASSETS 2024 2023
CURRENT ASSETS:
Cash and cash equivalents
924,060$
576,308$
Investments
5,184,250
5,266,635
Security lending collateral
358,247
349,985
Assets limited or restricted as to use - current portion
454,787
430,985
Patient accounts receivable
3,372,384
2,475,557
Estimated receivables from third-party payers
544,852
298,946
Other receivables
430,667
422,689
Inventories 399,135
409,193
Prepaid expenses and other current assets
236,140
225,464
Total current assets
11,904,522
10,455,762
ASSETS LIMITED OR RESTRICTED AS TO USE - noncurrent portion:
Self-insurance, benefit plans, and other
1,189,764
1,052,049
By Board
4,390,982
4,160,166
By donors
645,399
598,003
Total assets limited or restricted as to use - noncurrent portion 6,226,145
5,810,218
PROPERTY AND EQUIPMENT - Net
8,832,768
8,846,497
OPERATING LEASE RIGHT-OF-USE ASSETS 574,980
598,938
INVESTMENTS IN UNCONSOLIDATED AFFILIATES 5,600,268
5,165,540
GOODWILL 942,198
848,078
PREPAID PENSION AND RETIREE HEALTH ASSETS 245,772
232,725
OTHER ASSETS
340,075
322,449
TOTAL ASSETS
34,666,728$ 32,280,207$
The accompanying notes are an integral part of the consolidated financial statements.
(Continued)
As of
- 4 -
TRINITY HEALTH
CONSOLIDATED BALANCE SHEETS (UNAUDITED)
(In thous ands)
March 31, June 30,
LIABILITIES AND NET ASSETS
2024 2023
CURRENT LIABILITIES:
Commercial paper 99,388$ 99,538$
Short-term borrowings 599,415 616,335
Current portion of long-term debt 464,073 245,326
Current portion of operating lease liabilities 142,033 150,878
Medicare cash advances 161,366 -
Accounts payable and accrued expenses 1,848,751 1,551,303
Salaries, wages and related liabilities 1,059,726 1,065,904
Payable under security lending agreements 358,247 349,985
Estimated payables to third-party payers 238,224 286,409
Current portion of self-insurance reserves 302,399 303,658
Total current lia bilities 5,273,622 4,669,336
LONG-TERM DEBT - Net of current portion 7,013,801 6,757,159
LONG-TERM PORTION OF OPERATING LEASE LIABILITIES 515,289 535,888
SELF-INSURANCE RESERVES - Net of current portion 1,219,393 1,151,235
ACCRUED PENSION AND RETIREE HEALTH COSTS 73,470 88,859
OTHER LONG-TERM LIABILITIES 830,245 751,728
Total liabilities 14,925,820 13,954,205
NET ASSETS:
Net assets without donor restrictions 18,491,503 17,176,548
Noncontrolling ownership interest in subsidiaries 539,372 493,440
Total net assets without donor restrictions 19,030,875 17,669,988
Net assets with donor restrictions 710,033 656,014
Total net assets 19,740,908 18,326,002
TOTAL LIABILITIES AND NET ASSETS 34,666,728$ 32,280,207$
The accompanying notes are an integral part of the consolidated financial statements. (Concluded)
As of
- 5 -
TRINITY HEALTH
CONSOLIDATED STATEMENTS OF OPERATIONS AND
CHANGES IN NET ASSETS (UNAUDITED)
NINE MONTHS ENDED MARCH 31, 2024 AND 2023
(In thousands)
2024 2023
OPERATING REVENUE:
Net patient service revenue 15,319,533$ 13,710,230$
Premium and capitation revenue 833,872 832,590
Net assets released from restrictions 22,672 23,315
Other revenue 1,583,483 1,380,539
Total operating revenue 17,759,560 15,946,674
EXPENSES:
Salaries and wages 7,920,260 6,929,400
Employee benefits 1,508,370 1,288,751
Contract labor 278,823 683,743
Total labor expenses 9,707,453 8,901,894
Supplies 3,224,805 2,900,025
Purchased services and medical claims 2,250,545 2,148,270
Depreciation and amortization 668,917 666,497
Occupancy 670,019 635,884
Interest 206,051 192,760
Other 961,928 764,459
Total expenses 17,689,718 16,209,789
OPERATING INCOME (LOSS) BEFORE OTHER ITEMS 69,842 (263,115)
Restructuring costs
- (82,259)
Dividend received from cost method investee
- 53,864
Gain on sale of Gateway Health Plan L.P.
- 8,000
OPERATING INCOME (LOSS)
69,842 (283,510)
NONOPERATING ITEMS:
Investment earnings 853,017 457,334
Equity in earnings of unconsolidated affiliates 433,100 295,360
Change in market value and cash payments of interest rate swaps 9,604 18,157
Other net periodic retirement cost (36,477) (56,655)
Inherent contributions - 484,579
Other, including income taxes (16,366) (2,756)
Total nonoperating items 1,242,878 1,196,019
EXCESS OF REVENUE OVER EXPENSES 1,312,720 912,509
EXCESS OF REVENUE OVER EXPENSES ATTRIBUTABLE
TO NONCONTROLLING INTEREST
(51,481) (56,171)
EXCESS OF REVENUE OVER EXPENSES,
NET OF NONCONTROLLING INTEREST 1,261,239$ 856,338$
The accompanying notes are an integral part of the consolidated financial statements.
(Continued)

- 6 -
CHANGES IN NET ASSETS (UNAUDITED)
NINE MONTHS ENDED MARCH 31, 2024 AND 2023
(In thousands)
2024 2023
NET ASSETS WITHOUT DONOR RESTRICTIONS:
Net assets without donor restrictions attributable to Trinity Health:
Excess of revenue over expenses 1,261,239$ 856,338$
Net assets released from restrictions for capital acquisitions 15,522 13,844
Net change in retirement plan related items - consolidated organizations 50,720 66,223
Net change in retirement plan related items - unconsolidated organizations - 13,567
Purchase of noncontrolling interest in subsidiary (18,448) -
Other 5,923 11,592
Increase in net assets without donor restrictions attributable
to Trinity Health 1,314,956 961,564
Net assets without donor restrictions attributable to noncontrolling interest:
Excess of revenue over expenses attributable to noncontrolling interest 51,481 56,171
Noncontrolling interests attributed to acquisitions 60,658 -
Dividends, distributions and other (66,208) (47,211)
Increase in net assets without donor restrictions
attributable to noncontrolling interest 45,931 8,960
NET ASSETS WITH DONOR RESTRICTIONS:
Contributions:
Program and time restrictions 56,437 40,522
Endowment funds 1,851 1,024
Net investment gains:
Program and time restrictions 22,983 12,162
Endowment funds 10,881 1,386
Net assets released from restrictions (38,194) (37,159)
Acquisitions - 69,732
Other 61 255
Increase in net assets with donor restrictions 54,019 87,922
INCREASE IN NET ASSETS 1,414,906 1,058,446
NET ASSETS - BEGINNING OF YEAR 18,326,002 16,897,308
NET ASSETS - END OF PERIOD 19,740,908$ 17,955,754$
The accompanying notes are an integral part of the consolidated financial statements. (Concluded)

- 7 -
TRINITY HEALTH
SUMMARIZED CONSOLIDATED STATEMENTS OF CASH FLOWS (UNAUDITED)
NINE MONTHS ENDED MARCH 31, 2024 AND 2023
(In thousands)
2024 2023
OPERATING ACTIVITIES:
Increase in net assets 1,414,906$
1,058,446$
Adjustments to reconcile change in net assets to net cash provided by
(used in) operating activities:
Depreciation and amortization 668,917 666,497
Amortization of right-of-use asset 98,047 106,933
Change in net unrealized and realized gains and losses on investments
(816,577) (
386,054)
Change in market values of interest rate swaps (10,190) (24,743)
Undistributed equity in earnings of unconsolidated affiliates (430,014) (284,217)
Inherent contributions related to acquisitions - (484,413)
Loss on transfer of St. Francis Medical Center - 22,842
Gain on sale of Gateway Health Plan L.P. - (8,000)
Dividend received from cost method investee - (53,864)
Loss on purchase of noncontrolling interest in subsidiary 18,448 -
Increase in noncontrolling interest related to acquisitions (60,658) -
Deferred retirement items (7,007) (27,367)
Restricted contributions acquired - (69,732)
Dividends paid attributed to non-controlling interest 50,850 47,161
Other adjustments (30,854) (40,756)
Changes in:
Patient accounts receivable (903,699) (207,502)
Estimated receivables from third-party payers (245,906) 15,415
Prepaid pension and retiree health costs (13,047) (8,702)
Other assets 6,322 (97,766)
Medicare cash advances 161,366 (409,533)
Accounts payable and accrued expenses 311,333 (214,249)
Estimated payables to third-party payers (45,385) (64,122)
Self-insurance reserves and other liabilities (31,733) (129,049)
Accrued pension and retiree health costs (8,383) (9,701)
Total adjustments (1,288,170) (1,660,922)
Net cash provided by (used in) operating activities 126,736 (602,476)
INVESTING ACTIVITIES:
Net sales of investments
594,654 1,836,667
Purchases of property and equipment
(692,736) (642,151)
Change in investments in unconsolidated affiliates
(3,650) (29,488)
Cash proceeds from sale of Gateway Health Plan L.P.
- 8,000
Dividend received from cost method investee - 53,864
Cash used for disposal of St. Francis Medical Center - (14,500)
Net cash used for acquisitions
(57,503) (530,598)
Change in other investing activities
1,867 (4,151)
Net cash (used in) provided by investing activities
(157,368) 677,643
FINANCING ACTIVITIES:
Proceeds from issuance of debt 49,448
366,620
Repayments of debt
(186,559) (169,761)
Net change in commercial paper
(150) (26)
Draws on lines of credit
600,000 -
Dividends paid
(50,850) (47,161)
Proceeds from restricted contributions and restricted investment income
11,343 6,192
Increase in financing costs and other
(979) (2,328)
Net cash provided by financing activities
422,253 153,536
NET INCREASE IN CASH, CASH EQUIVALENTS, AND
RESTRICTED CASH
391,621 228,703
CASH, CASH EQUIVALENTS, AND RESTRICTED CASH -
BEGINNING OF YEAR
736,085 801,155
CASH, CASH EQUIVALENTS, AND RESTRICTED CASH -
END OF PERIOD
1,
127,706$ 1,029,858$
The accompanying notes are an integral part of the consolidated financial statements.

- 8 -
TRINITY HEALTH
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
NINE MONTHS ENDED MARCH 31, 2024 AND 2023
1. ORGANIZATION AND MISSION
Trinity Health Corporation, an Indiana nonprofit corporation headquartered in Livonia, Michigan, and its
subsidiaries (“Trinity Health” or the “Corporation”), controls one of the largest health care systems in the
United States. The Corporation is sponsored by Catholic Health Ministries, a Public Juridic Person of the
Holy Roman Catholic Church. The Corporation operates a comprehensive integrated network of health
services, including inpatient and outpatient services, physician services, managed care coverage, home
health care, long-term care, assisted living care and rehabilitation services located in 27 states. The
operations are organized into Regional Health Ministries, National Health Ministries and Mission Health
Ministries (“Health Ministries”). The Mission statement for the Corporation is as follows:
We, Trinity Health, serve together in the spirit of the Gospel as a compassionate and
transforming healing presence within our communities.
2. SUMMARY OF SIGNIFICANT ACCOUNTING POLICIES
The accompanying unaudited consolidated financial statements have been prepared in accordance with
accounting principles generally accepted in the United States of America (“GAAP”) for interim financial
reporting information. Accordingly, they do not include all of the information and footnotes required by
GAAP for complete financial statements. In the opinion of management, all adjustments considered
necessary for a fair presentation have been included and are of a normal and recurring nature. Operating
results for the nine months ended March 31, 2024 are not necessarily indicative of the results to be expected
for the year ending June 30, 2024.
Principles of Consolidation – The consolidated financial statements include the accounts of the
Corporation, and all wholly-owned, majority-owned, and controlled organizations. Investments where the
Corporation holds less than 20% of the ownership interest are accounted for using the cost method. All
other investments that are not controlled by the Corporation are accounted for using the equity method of
accounting. The equity share of income or losses from investments in unconsolidated affiliates is recorded
in other revenue if the unconsolidated affiliate is operational and projected to make routine and regular cash
distributions; otherwise, the equity share of income or losses from investments in unconsolidated affiliates
is recorded in nonoperating items in the consolidated statements of operations and changes in net assets.
All material intercompany transactions and account balances have been eliminated in consolidation.
Use of Estimates – The preparation of consolidated financial statements in conformity with GAAP requires
management of the Corporation to make assumptions, estimates and judgments that affect the amounts
reported in the consolidated financial statements, including the notes thereto, and related disclosures of
commitments and contingencies, if any.
The Corporation considers critical accounting policies to be those that require more significant judgments
and estimates in the preparation of its consolidated financial statements, including the following:
recognition of net patient service revenue, which includes explicit and implicit price concessions; financial
assistance; premium revenue; recorded values of investments and derivatives; goodwill; evaluation of long-
lived assets for impairment; reserves for losses and expenses related to health care professional and general
liabilities; and risks and assumptions for measurement of pension and retiree health liabilities. Management
relies on historical experience and other assumptions believed to be reasonable in making its judgments and
estimates. Actual results could differ materially from those estimates.

- 9 -
Cash, Cash Equivalents and Restricted Cash – For purposes of the consolidated statements of cash flows,
cash, cash equivalents and restricted cash include certain investments in highly liquid debt instruments with
original maturities of three months or less.
The following table reconciles cash, cash equivalents and restricted cash shown in the statements of cash
flows to amounts presented within the consolidated balance sheets as of March 31 (in thousands):
2024 2023
Cash and cash equivalents $ 924,060 $ 875,451
Restricted cash included in assets limited or restricted as to
use - current portion
Held by trust under bond indenture 222 224
Self insured benefit plans & other 115,890 83,297
By donors 1,681 4,151
Total restricted cash included in assets limited or restricted
as to use - current portion
117,793 87,672
Restricted cash included in assets limited as to use -
noncurrent portion
Self insured benefit plans & other 48,626 27,318
By donors 37,227 39,417
Total restricted cash included in assets limited or restricted
as to use - noncurrent portion
85,853 66,735
Total cash, cash equivalents, and restricted cash shown in
the statements of cash flows
$ 1,127,706 $ 1,029,858
Investments – Investments, inclusive of assets limited or restricted as to use, include marketable debt and
equity securities. Investments in equity securities with readily determinable fair values and all investments
in debt securities are measured at fair value and are classified as trading securities. Investments also include
investments in commingled funds, hedge funds and other investments structured as limited liability
corporations or partnerships. Commingled funds and hedge funds that hold securities directly are stated at
the fair value of the underlying securities, as determined by the administrator, based on readily determinable
market values, or based on net asset value, which is calculated using the most recent fund financial
statements. Limited liability corporations and partnerships are accounted for under the equity method.
Investment Earnings – Investment earnings include interest, dividends, realized gains and losses and
unrealized gains and losses. Also included are equity earnings from investment funds accounted for using
the equity method. Investment earnings on assets held by trustees under bond indenture agreements, assets
designated by the Corporation’s board of directors (“Board”) for debt redemption, assets held for
borrowings under the intercompany loan program, assets held by grant-making foundations, assets
deposited in trust funds by a captive insurance company for self-insurance purposes, and interest and
dividends earned on life plan communities advance entrance fees, in accordance with industry practices,
are included in other revenue in the consolidated statements of operations and changes in net assets.
Investment earnings, net of direct investment expenses, from all other investments and Board-designated
funds are included in nonoperating investment income unless the income or loss is restricted by donor or
law.
Derivative Financial Instruments – The Corporation periodically utilizes various financial instruments
(e.g., options and swaps) to hedge interest rates, equity downside risk and other exposures. The
Corporation’s policies prohibit trading in derivative financial instruments on a speculative basis. The
Corporation recognizes all derivative instruments in the consolidated balance sheets at fair value.
- 10 -
Securities Lending – The Corporation participates in securities lending transactions whereby a portion of
its investments are loaned, through its agent, to various parties in return for cash and securities from the
parties as collateral for the securities loaned. Each business day, the Corporation, through its agent, and the
borrower determine the market value of the collateral and the borrowed securities. If on any business day
the market value of the collateral is less than the required value, additional collateral is obtained as
appropriate. The amount of cash collateral received under securities lending is reported as an asset and a
corresponding payable in the consolidated balance sheets and is up to 105% of the market value of securities
loaned. As of March 31, 2024, and June 30, 2023, the Corporation had securities loaned of $678.5 million
and $698.7 million, respectively, and received collateral (cash and noncash) totaling $695.8 million and
$716.6 million, respectively, relating to the securities loaned. The fees received for these transactions are
recorded in nonoperating investment income in the consolidated statements of operations and changes in
net assets. In addition, certain pension plans participate in securities lending programs with the Northern
Trust Company, the plans’ agent.
The Corporation evaluates the financial condition of its securities lending plan managers and borrowing
institutions to minimize exposure to credit risk. Credit risk is regularly monitored and minimized by Trinity
Health’s managers of the program by selecting borrowers with stringent financial viability standards,
underwriting and approval procedures as set forth by the institution. An established framework is also used
to size borrower credit limits to reduce concentration risk. In addition, the vast majority of parent borrowers
have long-term credit ratings of A or better and short-term ratings of A-1 or better from at least one
nationally recognized statistical rating organization. The Corporation does not expect any credit losses
related to the securities lending arrangement.
Patient Accounts Receivable, Estimated Receivables from and Payables to Third-Party Payers – An
unconditional right to payment, subject only to the passage of time is treated as a receivable. Patient
accounts receivable, including billed accounts and unbilled accounts for which there is an unconditional
right to payment, and estimated amounts due from third-party payers for retroactive adjustments, are
receivables if the right to consideration is unconditional and only the passage of time is required before
payment of that consideration is due. For patient accounts receivable, the estimated uncollectable amounts
are generally considered implicit price concessions that are a direct reduction to patient service revenue and
accounts receivable.
The Corporation has agreements with third-party payers that provide for payments to the Corporation’s
Health Ministries at amounts different from established rates. Estimated retroactive adjustments under
reimbursement agreements with third-party payers and other changes in estimates are included in net patient
service revenue and estimated receivables from and payables to third-party payers. Retroactive adjustments
are accrued on an estimated basis in the period the related services are rendered and adjusted in future
periods, as final settlements are determined.
Assets Limited as to Use – Assets set aside by the Board for quasi-endowments, future capital
improvements, future funding of retirement programs and insurance claims, retirement of debt, held for
borrowings under the intercompany loan program, and other purposes over which the Board retains control
and may at its discretion subsequently use for other purposes, assets held by trustees under bond indenture
and certain other agreements, and self-insurance trust and benefit plan arrangements are included in assets
limited as to use.
Donor-Restricted Gifts – Unconditional promises to give cash and other assets to the Corporation are
reported at fair value at the date the promise is received. Conditional promises to give and indications of
intentions to give are reported at fair value at the date the gift is received. The gifts are reported as support
with donor restrictions if they are received with donor stipulations that limit the use of the donated assets.
When a donor restriction expires, that is, when a stipulated time restriction ends or program restriction is
accomplished, net assets with donor restrictions are reclassified to net assets without donor restrictions and
reported in the consolidated statements of operations and changes in net assets as net assets released from
restrictions. Donor-restricted contributions whose restrictions are met within the same year as received are
reported as contributions without donor restrictions included in other revenue in the consolidated statements
of operations and changes in net assets.
- 11 -
Inventories – Inventories are stated at the lower of cost or market. The cost of inventories is determined
principally by the weighted-average cost method.
Property and Equipment – Property and equipment, including internal-use software, are recorded at cost,
if purchased, or at fair value at the date of donation, if donated. Finance lease right-of-use assets included
in property and equipment represent the right to use the underlying assets for the lease term and are
recognized at the lease commencement date based on the present value of lease payments over the term of
the lease.
Depreciation is provided over the estimated useful life of each class of depreciable asset and is computed
using either the straight-line or an accelerated method and includes finance lease right-of-use asset
amortization and internal-use software amortization. The useful lives of property and equipment range from
2 to 75 years, and finance lease agreements have initial terms typically ranging from 3 to 30 years. Interest
costs incurred during the period of construction of capital assets are capitalized as a component of the cost
of acquiring those assets.
Gifts of long-lived assets such as land, buildings, or equipment are reported as support without donor
restrictions and are excluded from the excess of revenue over expenses, unless explicit donor stipulations
specify how the donated assets must be used. Gifts of long-lived assets with explicit restrictions that specify
how the assets are to be used and gifts of cash or other assets that must be used to acquire long-lived assets
are reported as support with donor restrictions.
Right-of-Use Lease Assets and Lease Liabilities – The Corporation determines if an arrangement is a lease
at inception of the contract. Right-of-use assets represent the right to use the underlying assets for the lease
term and lease liabilities represent the obligation to make lease payments arising from the leases. Right-of-
use assets and lease liabilities are recognized at the lease commencement date based on the present value
of lease payments over the lease term. The Corporation uses the implicit rate noted within the contract,
when available. Otherwise, the Corporation uses its incremental borrowing rate estimated using recent
secured debt issuances that correspond to various lease terms, information obtained from banking advisors,
and the Corporation’s secured debt fair value. The Corporation does not recognize leases, for operating or
finance type, with an initial term of 12 months or less (“short-term leases”) on the consolidated balance
sheet, and the lease expense for these short-term leases is recognized on a straight-line basis over the lease
term within occupancy expense in the consolidated statements of operations and changes in net assets. The
Corporation’s finance leases are primarily for real estate. Finance lease right-of-use assets are included in
property and equipment, with the related liabilities included in current and long-term debt on the
consolidated balance sheet.
Operating lease right-of-use assets and liabilities are recorded for leases that are not considered finance
leases. The Corporation’s operating leases are primarily for real estate, vehicles, and medical and office
equipment. Real estate leases include outpatient, medical office, ground, and corporate administrative office
space. The Corporation’s real estate lease agreements typically have an initial term of 2 to 10 years. The
Corporation’s equipment lease agreements typically have an initial term of 2 to 6 years. The real estate
leases may include one or more options to renew, with renewals that can extend the lease term from 5 to 10
years. The exercise of lease renewal options is at the Corporation’s sole discretion. For accounting purposes,
options to extend or terminate the lease are included in the lease term when it is reasonably certain that the
option will be exercised. Operating lease liabilities represent the obligation to make lease payments arising
from the leases and are recognized at the lease commencement date based on the present value of lease
payments over the lease term.
Certain of the Corporation’s lease agreements for real estate include payments based on common area
maintenance expenses and others include rental payments adjusted periodically for inflation. These variable
lease payments are recognized in occupancy expense, net, but are not included in the right-of-use asset or
liability balances when they can be separately identified in the contract. The Corporation’s lease agreements
do not contain any material residual value guarantees, restrictions, or covenants.
- 12 -
Goodwill – Goodwill represents the future economic benefits arising from assets acquired in a business
combination that are not individually identified and separately recognized
.
Asset Impairments –
Property, Equipment and Right-of-Use Lease Assets – The Corporation evaluates long-lived assets
for possible impairment whenever events or changes in circumstances indicate that the carrying amount
of the asset, or related group of assets, may not be recoverable from estimated future undiscounted cash
flows. If the estimated future undiscounted cash flows are less than the carrying value of the assets, the
impairment recognized is calculated as the carrying value of the long-lived assets in excess of the fair
value of the assets. The fair value of the assets is estimated based on appraisals, established market
values of comparable assets or internal estimates of future net cash flows expected to result from the
use and ultimate disposition of the assets.
Goodwill – Goodwill is tested for impairment on an annual basis or when an event or change in
circumstance indicates the value of a reporting unit may have changed. Testing is conducted at the
reporting unit level. If the carrying amount of the reporting unit goodwill exceeds the implied fair value
of that goodwill, an impairment loss is recognized in an amount equal to that excess. Estimates of fair
value are based on appraisals, established market prices for comparable assets or internal estimates of
future net cash flows.
Other Assets – Other assets include long-term notes receivable, reinsurance recovery receivables, definite-
and indefinite-lived intangible assets other than goodwill and prepaid retiree health costs. The net balances
of definite-lived intangible assets include noncompete agreements, physician guarantees and other definite-
lived intangible assets with finite lives amortized using the straight-line method over their estimated useful
lives, which generally range from 2 to 20 years. Indefinite-lived intangible assets primarily include trade
names, which are tested annually for impairment.
Short-Term Borrowings – Short-term borrowings include puttable variable-rate demand bonds supported
by self-liquidity or liquidity facilities considered short-term in nature.
Medicare Cash Advances – In April 2020, the Corporation requested and received accelerated Medicare
payments of $1.6 billion for its acute care hospitals, which was provided through the Coronavirus Aid,
Relief and Economic Security Act (the “CARES Act”). Claims for services provided to Medicare
beneficiaries began being applied against the Corporation’s cash advances in April 2021.
During the nine
months ended March 31, 2023, the Center for Medicare and Medicaid Services (“CMS”) recouped $409.5
million of the advances. The remaining balance was fully repaid as of June 30, 2023.
Change Healthcare, a subsidiary of UnitedHealth Group and a major clearinghouse for medical claims,
experienced a cyberattack in February 2024. Although the Corporation’s systems were not directly
impacted by this cyberattack, the event disrupted the billing and collection of patients accounts receivable.
As a result, on March 9, 2024, CMS made available accelerated payments to providers and suppliers
experiencing disruptions due to the incident. These advances have been granted in amounts of up to 30 days
of claims payments and will be repaid through automatic recoupment from Medicare for a period of 90
days. The Corporation received $201.0 million of these cash advances of which $39.6 million has been
recouped, with $161.4 million remaining as of March 31, 2024.
Other Long-Term Liabilities – Other long-term liabilities include deferred compensation, asset retirement
obligations, interest rate swaps and deferred revenue from entrance fees. Deferred revenue from entrance
fees are fees paid by residents of facilities for the elderly upon entering into continuing care contracts,
which are amortized to income using the straight-line method over the estimated remaining life expectancy
of the resident, net of the portion that is refundable to the resident.
- 13 -
Net Assets with Donor Restrictions – Net assets with donor restrictions are those whose use by the
Corporation has been limited by donors to a specific time period or program. In addition, certain net assets
have been restricted by donors to be maintained by the Corporation in perpetuity.
Net Patient Service Revenue – The Corporation reports patient service revenue at the amount that reflects
the consideration it is expected to be entitled to in exchange for providing patient care. These amounts are
due from patients, third-party payers (including commercial payers and government programs) and others
and include variable consideration for retroactive revenue adjustments due to settlement of audits,
reviews, and investigations. Generally, the Corporation bills patients and third-party payers several days
after the services are performed or the patient is discharged from a facility.
The Corporation determines performance obligations based on the nature of the services provided. Revenue
for performance obligations satisfied over time is recognized based on actual charges incurred in relation
to total expected charges. The Corporation believes that this method provides a faithful depiction of the
transfer of services over the term of the performance obligation based on the inputs needed to satisfy the
obligation. Generally, performance obligations satisfied over time relate to patients in hospitals receiving
inpatient acute care services, or receiving services in outpatient centers, or in their homes (home care). The
Corporation measures performance obligations from admission to the hospital, or the commencement of an
outpatient service, to the point when it is no longer required to provide services to the patient, which is
generally at the time of discharge or the completion of the outpatient services. Revenue for performance
obligations satisfied at a point in time is generally recognized when goods are provided to our patients and
customers in a retail setting (for example, pharmaceuticals and medical equipment) and the Corporation
does not believe that it is required to provide additional goods and services related to that sale.
Because patient service performance obligations relate to contracts with a duration of less than one year,
the Corporation has elected to apply the optional exemption provided in Financial Accounting Standards
Board (“FASB”) Accounting Standards Codification (“ASC”) 606-10-50-14(a) and, therefore, the
Corporation is not required to disclose the aggregate amount of the transaction price allocated to
performance obligations that are unsatisfied or partially unsatisfied at the end of the reporting period. The
unsatisfied or partially unsatisfied performance obligations are primarily related to inpatient acute care
services at the end of the reporting period. The performance obligations for these contracts are generally
completed when the patients are discharged, which generally occurs within days or weeks from the end of
the reporting period.
The Corporation has elected the practical expedient allowed under FASB ASC 606-10-32-18 and does not
adjust the promised amount of consideration from patients and third-party payers for the effects of a
significant financing component due to the Corporation’s expectation that the period between the time the
service is provided to a patient and the time that the patient or a third-party payer pays for that service will
be one year or less. However, the Corporation does, in certain instances, enter into payment agreements
with patients that allow payments in excess of one year. For those cases, the financing component is not
deemed to be significant to the contract.
The Corporation determines the transaction price based on standard charges for services provided, reduced
by contractual adjustments provided to third-party payers, discounts provided to uninsured and
underinsured patients in accordance with the Corporation’s policy, and implicit price concessions provided
to uninsured and underinsured patients. The Corporation determines its estimates of contractual adjustments
and discounts based on contractual agreements, discount policies and historical experience. The estimate
of implicit price concessions is based on historical collection experience with the various classes of patients
using a portfolio approach as a practical expedient to account for patient contracts with similar
characteristics, as collective groups rather than individually. The financial statement effect of using this
practical expedient is not materially different from an individual contract approach.
- 14 -
Generally, patients who are covered by third-party payers are responsible for related deductibles and
coinsurance, which vary in amount. The Corporation also provides services to uninsured and underinsured
patients, and offers those uninsured and underinsured patients a discount, either by policy or law, from
standard charges. The Corporation estimates the transaction price for patients with deductibles and
coinsurance and for those who are uninsured and underinsured based on historical experience and current
market conditions, using the portfolio approach.
The initial estimate of the transaction price is determined by reducing the standard charge by any contractual
adjustments, discounts, and implicit price concessions. Subsequent changes to the estimate of the
transaction price are generally recorded as adjustments to patient service revenue in the period of the
change. Subsequent changes that are determined to be the result of an adverse change in the payer’s or
patient’s ability to pay are recorded as bad debt expense in other expenses in the statement of operations
and changes in net assets. Agreements with third-party payers typically provide for payments at amounts
less than established charges. A summary of the payment arrangements with major third-party payers is as
follows:
Medicare (Parts A and B) – Acute inpatient and outpatient services rendered to Medicare program
beneficiaries are paid primarily at prospectively determined rates. These rates vary according to a
patient classification system that is based on clinical, diagnostic, and other factors. Certain items are
reimbursed at a tentative rate with final settlement determined after submission of annual cost reports
and audits thereof by the Medicare fiscal intermediaries.
Medicare Advantage (Part C) – Acute inpatient and outpatient services rendered to Medicare
beneficiaries that chose an Advantage plan are paid primarily at prospectively determined rates. These
rates vary according to a patient classification system that is based on clinical, diagnostic, and other
factors.
Medicaid – Reimbursement for services rendered to Medicaid program beneficiaries includes
prospectively determined rates per discharge, per diem payments, discounts from established charges,
fee schedules and cost reimbursement methodologies with certain limitations. Cost reimbursable items
are reimbursed at a tentative rate with final settlement determined after submission of annual cost
reports and audits thereof by the Medicaid fiscal intermediaries.
Medicaid Health Maintenance Organization (HMO) – Reimbursement for services rendered to
Medicaid program beneficiaries that chose an HMO program where payments are based on
prospectively determined rates per discharge, per diem payments, discounts from established charges,
fee schedules and cost reimbursement methodologies with certain limitations.
Other – Reimbursement for services to certain patients is received from commercial insurance carriers,
health maintenance organizations and preferred provider organizations. The basis for reimbursement
includes prospectively determined rates per discharge, per diem payments and discounts from
established charges.
Cost report settlements under these programs are subject to audit by Medicare and Medicaid auditors and
administrative and judicial review, and it can take several years until final settlement of such matters is
determined and completely resolved. Because the laws, regulations, instructions, and rule interpretations
governing Medicare and Medicaid reimbursement are complex and change frequently, the estimates that
have been recorded could change by material amounts.
Settlements with third-party payers for retroactive revenue adjustments due to audits, reviews or
investigations are considered variable consideration and are included in the determination of the estimated
transaction price for providing patient care. These settlements are estimated based on the terms of the
payment agreement with the payer, correspondence from the payer and historical settlement activity,
including an assessment to ensure that it is probable that a significant reversal in the amount of cumulative
revenue recognized will not occur when the uncertainty associated with the retroactive adjustment is
- 15 -
subsequently resolved. Estimated settlements are adjusted in future periods as adjustments become known
(that is, new information becomes available), or as years are settled or are no longer subject to such audits,
reviews, and investigations.
For the nine months ended March 31, 2024, the Corporation accrued $121.6 million for the 340B remedy
lump sum settlement under the Centers for Medicare & Medicaid Services (“CMS”) November 8, 2023
Final Rule related to underpayments in the drug discount program for calendar years 2018 to 2022.
Financial Assistance – The Corporation provides services to all patients regardless of ability to pay. In
accordance with the Corporation’s policy, a patient is classified as a financial assistance patient based on
specific criteria, including income eligibility as established by the Federal Poverty Guidelines, as well as
other financial resources and obligations.
Charges for services to patients who meet the Corporation’s guidelines for financial assistance are not
reported as net patient service revenue in the accompanying consolidated financial statements. Therefore,
the Corporation has determined it has provided implicit price concessions to uninsured and underinsured
patients and patients with other uninsured balances (for example, copays and deductibles). The implicit
price concessions included in estimating the transaction price represent the difference between amounts
billed to patients and the amounts the Corporation expects to collect based on its collection history with
those patients.
Self-Insured Employee Health Benefits – The Corporation administers self-insured employee health
benefit plans for employees. The majority of the Corporation’s employees participate in the programs. The
provisions of the plans permit employees and their dependents to elect to receive medical care at either the
Corporation’s Health Ministries or other health care providers. Patient service revenue has been reduced by
an allowance for self-insured employee health benefits, which represents revenue attributable to medical
services provided by the Corporation to its employees and dependents in such years.
Premium and Capitation Revenue – The Corporation has certain Health Ministries that arrange for the
delivery of health care services to enrollees through various contracts with providers and common provider
entities. Enrollee contracts are negotiated on a yearly basis. Premiums are due monthly and are recognized
as revenue during the period in which the Corporation is obligated to provide services to enrollees.
Premiums received prior to the period of coverage are recorded as deferred revenue and included in
accounts payable and accrued expenses in the consolidated balance sheets.
Certain of the Corporation’s Health Ministries have entered into capitation arrangements whereby they
accept the risk for the provision of certain health care services to health plan members. Under these
agreements, the Corporation’s Health Ministries are financially responsible for services provided to the
health plan members by other institutional health care providers. Capitation revenue is recognized during
the period for which the Health Ministry is obligated to provide services to health plan enrollees under
capitation contracts. Capitation receivables are included in other receivables in the consolidated balance
sheets.
Reserves for incurred but not reported claims have been established to cover the unpaid costs of health care
services covered under the premium and capitation arrangements. The premium and capitation arrangement
reserves are included in accounts payable and accrued expenses in the consolidated balance sheets. The
liability is estimated based on actuarial studies, historical reporting, and payment trends. Subsequent actual
claim experience will differ from the estimated liability due to variances in estimated and actual utilization
of health care services, the amount of charges and other factors. As settlements are made and estimates are
revised, the differences are reflected in current operations.
- 16 -
Other Revenue – Other revenue is recorded at amounts the Corporation expects to collect in exchange for
providing goods or services not directly associated with patient care and recorded over the time in which
obligations to provide goods or services are satisfied. Other revenue includes revenue from the following
sources: grants, retail pharmacy, operating investment income, assisted and independent living, equity in
earnings of unconsolidated affiliates if the unconsolidated affiliate is operational and projected to make
routine and regular cash distributions, incentive revenue, and gainshare recognized under alternative
payment models and ancillary services.
Grant Revenue – Where grants are determined to be contributions, unconditional grants are recognized as
revenue when received. Conditional grants are recognized as revenue when the Corporation has complied
with and substantially met the conditions associated with the grant. For grants that are not contributions,
the Corporation recognizes revenue at the amount that reflects the consideration it is expected to be entitled
to in exchange for providing services under the term of the grant agreement.
Income Taxes – The Corporation and substantially all of its subsidiaries have been recognized as tax-
exempt pursuant to Section 501(a) of the Internal Revenue Code. The Corporation also has taxable
subsidiaries, which are included in the consolidated financial statements. The Corporation includes
penalties and interest, if any, with its provision for income taxes in other nonoperating items in the
consolidated statements of operations and changes in net assets.
Excess of Revenue Over Expenses – The consolidated statements of operations and changes in net assets
includes excess (deficiency) of revenue over expenses. Changes in net assets without donor restrictions,
which are excluded from excess (deficiency) of revenue over expenses, consistent with industry practice,
include the effective portion of the change in market value of derivatives that meet hedge accounting
requirements, permanent transfers of assets to and from affiliates for other than goods and services,
contributions of long-lived assets received or gifted (including assets acquired using contributions, which
by donor restriction were to be used for the purposes of acquiring such assets), net change in retirement
plan related items, discontinued operations and cumulative effects of changes in accounting principles.
Adopted Accounting Pronouncements –
In June 2016, the FASB issued ASU No. 2016-13, “Financial Instruments – Credit Losses (Topic 326)”.
This guidance is intended to align the needs of the users of financial statements related to credit loss
recognition and also address the potential weakness from the delayed recognition of credit losses, resulting
in an overstatement of assets. The amendments replace the current incurred loss methodology, which delays
recognition until it is probable a loss has occurred, with one that reflects expected credit losses and requires
consideration of a broader range of reasonable and supportable information to inform credit loss estimates.
This guidance was effective for the Corporation beginning July 1, 2023. The adoption of this guidance did
not materially impact the Corporation’s financial position, or results of operations. As required, additional
disclosures have been included.
Forthcoming Accounting Pronouncements –
In October 2021, the FASB issued No. 2021-08, “Business Combinations (Topic 805) – Accounting for
Contract Assets and Contract Liabilities from Contracts with Customers”. This guidance was issued to
address the inconsistency in accounting related to recognition of an acquired contract liability and the
payment terms and their effect on subsequent revenue by the acquirer. The amendments in this update
require that the acquirer recognize, and measure contract assets and contract liabilities acquired in a business
combination in accordance with Topic 606, as if it had originated the contracts, generally consistent with
how they were recognized and measured in the acquiree’s financial statements. This guidance is effective
for the Corporation beginning July 1, 2024. The Corporation will apply this guidance in consideration of
any future business combinations that may occur on or after July 1, 2024.

- 17 -
3. INVESTMENTS IN UNCONSOLIDATED AFFILIATES, BUSINESS ACQUISITIONS AND
DIVESTITURES
Investments in Unconsolidated Affiliates – The Corporation and certain of its Health Ministries have
investments in entities that are recorded under the cost and equity methods of accounting. The Corporation’s
share of equity earnings or losses from entities accounted for under the equity method and the classification
on the consolidated statements of operations and changes in net assets for the nine months ended March 31
are as follows (in thousands):
2024 2023
Other revenue 52,332$ 10,528$
Nonoperating Items 433,100 296,935
Total equity in earnings of unconsolidated affiliates 485,432$ 307,463$
The most significant of these investments include the following:
BayCare Health System – The Corporation holds a 50.4% interest in BayCare Health System Inc. and
Affiliates (“BayCare”), a Florida not-for-profit corporation exempt from state and federal income
taxes. BayCare was formed in 1997 pursuant to a Joint Operating Agreement (“JOA”) among the not-
for-profit, tax-exempt members of the Corporation, Morton Plant Mease Health Care, Inc., South
Florida Baptist Hospital, Inc. and BayCare. The Corporation’s participants in BayCare include St.
Anthony’s Hospital, Inc., St. Joseph’s Hospital, Inc., and St. Joseph’s Health Care Center, Inc.
(collectively, the “Trinity Participants”) and certain of their respective Affiliates. BayCare consists of
three community health alliances located in the Tampa Bay area of Florida, including St. Joseph’s-
Baptist Healthcare Hospital, St. Anthony’s Health Care, and Morton Plant Mease Health Care. The
Corporation has the right to appoint nine of the 21 voting members of the Board of Directors of
BayCare; therefore, the Corporation accounts for BayCare under the equity method of accounting. As
of March 31, 2024, and June 30, 2023, the Corporation’s investment in BayCare totaled $4.8 billion
and $4.4 billion, respectively.
Emory Healthcare/St. Joseph’s Health System – The Corporation holds a 49% interest in Emory
Healthcare/St. Joseph’s Health System (“EH/SJHS”). EH/SJHS operates several organizations,
including two acute care hospitals, St. Joseph’s Hospital of Atlanta, and John’s Creek Hospital. As of
March 31, 2024, and June 30, 2023, the Corporation’s investment in EH/SJHS totaled $269.4 million
and $221.5 million, respectively.
Life Flight Network, LLC – The Corporation, through its subsidiary Saint Alphonsus Regional
Medical Center, Inc. holds a 25% interest in Life Flight Network, LLC (“Life Flight”), an Oregon
limited liability company and its affiliates. Life Flight was formed in 2019 pursuant to a JOA. The
members of Life Flight, each owning 25%, are Saint Alphonsus Regional Medical Center, Inc., Legacy
Emmanuel Hospital and Health Center, Oregon Health and Sciences University, and Providence
Health System. Life Flight provides services, including both air and ground ambulance services, in the
Pacific Northwest with 34 bases in Oregon, Washington, Idaho and Montana. The Corporation
accounts for Life Flight under the equity method of accounting. As of March 31, 2024 and June 30,
2023, the Corporation’s investment in Life Flight totaled $78.6 million and $70.5 million, respectively.
Mercy Health Network – The Corporation held a 50% interest in Mercy Health Network, dba
MercyOne, (“MHN”), a nonstock-basis membership corporation with CommonSpirit Health (“CSH”)
,
holding the remaining 50% interest. MHN was the sole member of Wheaton Franciscan Services, Inc.
(“WFSI”) that operates three hospitals in Iowa: Covenant Medical Center located in Waterloo, Sartori
Memorial Hospital located in Cedar Falls and Mercy Hospital of Franciscan Sisters located in
Oelwein. MHN is also the sole member of Central Community Hospital (“CCH”), a critical access
hospital located in Elkader, Iowa. On September 1, 2022, the Corporation completed a transaction
with CSH through which the Corporation acquired CSH’s 50% interest in MHN, and now wholly
owns MHN. See “Acquisitions” subsequently in Note 3 for further information regarding this
transaction. As of March 31, 2024, and June 30, 2023, the Corporation’s investment in MHN totaled
$0, respectively.

- 18 -
Condensed consolidated balance sheets of BayCare, EH/SJHS, and Life Flight are as follows (in
thousands):
Baycare EH/SJHS Life Flight
Total assets 12,629,052$ 965,285$ 400,335$
Total liabilities 2,701,440$ 687,684$ 58,034$
Baycare EH/SJHS Life Flight
Total assets 11,526,730$ 878,549$ 371,904$
Total liabilities 2,616,025$ 603,076$ 61,758$
March 31, 2024
June 30, 2023
Condensed consolidated statements of operations of BayCare, EH/SJHS, Life Flight and MHN are as
follows (in thousands):
Baycare EH/SJHS Life Flight
Revenue, net 4,040,479$ 783,864$ 199,015$
Excess of revenue over expenses 516,976$ 78,018$ 32,155$
Baycare EH/SJHS Life Flight MHN
Revenue, net 3,658,807$ 677,034$ 168,341$ 64,186$
Excess (deficiency) of revenue over expenses 571,666$ 14,510$ 22,370$ (4,236)$
Nine months ended March 31, 2023
Nine months ended March 31, 2024
MHN results are prior to the acquisition date of September 1, 2022, and for the two months ended August
31, 2022.
The following amounts have been recognized in the accompanying consolidated statements of operations
and changes in net assets related to the investments in BayCare, EH/SJHS, Life Flight, and MHN (in
thousands):
Baycare EH/SJHS Life Flight
Other revenue -$ -$ 8,039$
Equity in earnings of
unconsolidated organizations 387,077 47,809 -
Other changes in net assets
without donor restrictions (3,642) - -
Total 383,435$ 47,809$ 8,039$
Baycare EH/SJHS Life Flight MHN
Other revenue -$ -$ 5,593$ (2,077)$
Equity in earnings of
unconsolidated organizations 288,177 6,983 - -
Other changes in net assets
without donor restrictions 15,986 - - -
Total 304,163$ 6,983$ 5,593$ (2,077)$
Nine months ended March 31, 2023
Nine months ended March 31, 2024
MHN results are prior to the acquisition date of September 1, 2022, and for the two months ended August
31, 2022.
- 19 -
Acquisitions:
MercyOne & MHN – On September 1, 2022, the Corporation completed a transaction with CSH through
which (i) the Corporation acquired CSH’s 50% interest in MHN, which is the sole member of WFSI and
the MHN subsidiary that owns and controls CCH, thereby becoming the sole corporate member of MHN,
(ii) MHN became the sole corporate member of Catholic Health Initiatives-Iowa, Corp. d/b/a MercyOne
Des Moines Medical Center (“MercyOne Des Moines”), a regional health care system located in Des
Moines, Iowa, and (iii) Trinity Home Health Services d/b/a Trinity Health At Home, a subsidiary of the
Corporation, acquired certain home care, hospice, and home infusion pharmacy operations from an affiliate
of CSH located in the vicinity of Des Moines (“Iowa Home Care Assets”, and collectively with (i) and (ii),
the “MercyOne Acquisition”). The completion of the acquisition marks a shared commitment to ensuring
access to health care across Iowa. Operating as a part of Trinity Health, MercyOne will retain its name and
brand while enhancing more integrated and unified care in the communities it serves.
The cash paid to CSH in consideration for the MercyOne Acquisition totaled $633.9 million, of which
$613.0 million was paid during the first quarter of fiscal year 2023 and a $20.9 million post-closing
reconciliation adjustment, as stipulated in the definitive agreement, was paid during the third quarter of
fiscal year 2023. Based on final purchase price allocations, goodwill of $27.1 million was recorded on the
consolidated balance sheet as of June 30, 2023.
For the nine months ended March 31, 2024 and 2023, the Corporation’s consolidated statements of
operations and changes in net assets included operating revenue of $1.3 billion and $0.9 billion, operating
losses of $24.6 million and $79.3 million, and deficiency of revenue over expense of $21.1 million and
$62.1 million, respectively, related to the operations of the MercyOne Acquisition.
North Ottawa Community Health System (“Grand Haven”) – The Corporation’s affiliate, Mercy Health
Partners, completed a transaction with Grand Haven under which Mercy Health Partners became the sole
member of Grand Haven on October 1, 2022. Grand Haven and its affiliates operate an acute care hospital,
urgent care center, long-term care facility and provide hospice services in the communities surrounding
Grand Haven, Michigan. The transaction will provide improved access to specialists, primary care and
health care services, while improving care delivery and access close to home in the Corporation’s West
Michigan market. The fair value of identifiable assets acquired exceeded the fair value of liabilities assumed
by $15.4 million which was recorded as an inherent contribution in nonoperating items in the consolidated
statement of operations and changes in net assets for the year ended June 30, 2023.
For the nine months ended March 31, 2024 and 2023, the Corporation’s consolidated statements of
operations and changes in net assets included operating revenue of $52.8 million and $31.6 million,
operating income of $2.5 million and operating loss of $0.9 million, and excess of revenue over expenses
of $2.5 million and deficiency of revenue over expenses of $1.3 million, respectively, related to the
operations of Grand Haven.
Genesis Health System – On March 1, 2023, the Corporation and its affiliate, MHN, completed a
transaction with Genesis Health System, an Iowa nonprofit corporation and Genesis Health System, an
Illinois not-for-profit corporation (together “Genesis”), under which MHN became the sole member of each
and acquired substantially all assets and liabilities except for certain foundation assets, liabilities and net
assets. Genesis and its affiliates operate four acute care hospitals, including two critical access hospitals,
convenient care centers, physician practices, a long-term care facility joint venture, an independent living
facility for seniors and hospice services in the communities in eastern Iowa and western Illinois. The fair
value of identifiable assets acquired exceeded the fair value of liabilities assumed by $468.1 million that
was recorded as an inherent contribution in nonoperating items in the consolidated statement of operations
and changes in net assets for the year ended June 30, 2023. Based on a revised assessment of assets and
liabilities, a $3.3 million reduction to inherent contribution was recorded during the second quarter of fiscal
year 2024 resulting in total inherent contribution of $464.8 million. As part of the transaction the
Corporation also agreed to a capital commitment as further disclosed in Note 4.

- 20 -
For the nine months ended March 31, 2024 and 2023, the Corporation’s consolidated statements of
operations and changes in net assets included operating revenue of $660.9 million and $66.5 million,
operating income of $45.5 million and operating loss of $1.8 million, and excess of revenue over expenses
of $54.9 million and $0.7 million, respectively, related to the operations of Genesis.
Based on final purchase price allocations the summarized balance sheet information is shown below as of
the respective acquisition dates (in thousands):
MercyOne
Acquisition
Grand Haven
Genesis
Estimated fair value of net tangible assets acquired:
Cash 58,987$ 5,665$ 43,112$
Investments, current 90,277 - 2,064
Patient accounts receivable 174,100 5,620 91,254
Other current assets 56,324 2,972 51,957
Assets limited or restricted as to use - noncurrent portion 56,158 2,320 324,487
Property and equipment - net 436,682 22,864 210,292
Operating lease right-of-use assets 95,707 - 47,704
Investments in unconsolidated affiliates 60,783 - 49,079
Other long-term assets 16,630 1,761 19,139
Goodwill 27,064 - -
Previously held investments in unconsolidated affiliates (111,151) - -
Medicare cash advances (19,648) - -
Other current liabilities (156,811) (11,877) (123,015)
Long-term debt - (11,702) (127,415)
Long-term portion of operating lease liabilities (83,570) - (42,429)
Other long-term liabilities (32,218) (2,001) (47,565)
Noncontrolling ownership interest in subsidiaries - - (433)
Net assets with donor restrictions (35,439) (202) (33,434)
Cash paid 633,875$ - -
Inherent contribution 15,420$ 464,797$
The amount of the Corporation’s pro forma revenue, earnings, and changes in net assets, had the MercyOne,
Grand Haven and Genesis acquisitions occurred on July 1, 2021 are as follows for the nine months ended
March 31 (in thousands):
2023
2022
Total operating revenue 16,685,894$
16,892,255$
Excess (Deficiency) of revenue over expenses net of noncontrolling interest 822,713
(24,147)
Change in net assets without donor restrictions 741,854 57,822
Change in net assets with donor restrictions 17,417 (2,494)

- 21 -
Divestiture:
St. Francis Medical Center (“SFMC”) Trenton, N.J. – On December 22, 2022, the Corporation, through
its subsidiary Maxis Health System (“Maxis”), transferred the membership interest of SFMC and certain
subsidiaries as well as $14.5 million of cash, and certain inventory and equipment, to Capital Health
System, Inc. (“Capital”). As a result of this transaction, restructuring costs of $82.3 million were incurred,
primarily related to loss on sale, asset retirement obligations and transition benefits for colleagues during
fiscal year 2023.
For the nine months ended March 31, 2023, the Corporation’s consolidated statements of operations and
changes in net assets included operating revenue of $59.3 million, operating losses of $99.0 million, and
deficiency of revenue over expenses of $103.0 million (inclusive of restructuring costs), related to the
operations of SFMC.
4. PROPERTY AND EQUIPMENT
A summary of property and equipment is as follows (in thousands):
March 31, June 30,
2024 2023
Land 439,100$ 428,858$
Buildings and improvements 11,592,806 11,287,425
Equipment 7,664,371 7,524,260
Finance lease right-of-use assets 95,071 95,329
Total 19,791,348 19,335,872
Accumulated depreciation and amortization (11,777,068) (11,168,290)
Construction in progress 818,488 678,915
Property and equipment - net 8,832,768$ 8,846,497$
In conjunction with the acquisition of Genesis as described in Note 3, the Corporation and MHN committed
to allocate not less than $450 million of capital to Genesis over seven years with the commitment period
ending March 1, 2030. The capital commitment period may be extended up to 18 months under certain
circumstances. The Corporation’s related capital spending for Genesis through March 31, 2024 is $57.9
million.
5. LONG-TERM DEBT AND OTHER FINANCING ARRANGEMENTS
Obligated Group and Other Requirements – The Corporation has debt outstanding under a master trust
indenture dated October 3, 2013, as amended and supplemented, the amended and restated master indenture
(“ARMI”). The ARMI permits the Corporation to issue obligations to finance certain activities. Obligations
issued under the ARMI are joint and several obligations of the obligated group established thereunder (the
“Obligated Group,” which currently consists of the Corporation). Proceeds from tax-exempt bonds and
refunding bonds are to be used to finance the construction, acquisition and equipping of capital
improvements. Proceeds from taxable bonds are to be used to finance corporate purposes or advance refund
tax-exempt bonds. Certain Health Ministries of the Corporation constitute designated affiliates and the
Corporation covenants to cause each designated affiliate to pay, loan or otherwise transfer to the Obligated
Group such amounts necessary to pay the amounts due on all obligations issued under the ARMI. The
Obligated Group and the designated affiliates are referred to as the Trinity Health Credit Group.
Pursuant to the ARMI, the Obligated Group agent (which is the Corporation) has caused the designated
affiliates representing, when combined with the Obligated Group members, at least 85% of the consolidated
net revenues of the Trinity Health Credit Group to grant to the master trustee security interests in their
pledged property which security interests secure all obligations issued under the ARMI. There are several
- 22 -
conditions and covenants required by the ARMI with which the Corporation must comply, including
covenants that require the Corporation to maintain a minimum historical debt-service coverage and
limitations on liens or security interests in property, except for certain permitted encumbrances, affecting
the property of the Corporation or any material designated affiliate (a designated affiliate whose total
revenues for the most recent fiscal year exceed 5% of the combined total revenues of the Corporation for
the most recent fiscal year). Long-term debt outstanding as of March 31, 2024 and June 30, 2023, that has
not been secured under the ARMI is generally collateralized by certain property and equipment.
Commercial Paper – The Corporation’s commercial paper program is authorized for borrowings up to $600
million. As of March 31, 2024, and June 30, 2023, the total amount of commercial paper outstanding was
$99.4 million and $99.5 million, respectively. Proceeds from this program are to be used for general
purposes of the Corporation. The notes are payable from the proceeds of subsequently issued notes and
from other funds available to the Corporation, including funds derived from the liquidation of securities
held by the Corporation in its investment portfolio.
Liquidity Facilities – On September 29, 2022, the Corporation renewed and amended its revolving credit
agreement (“RCAI”), by and among the Corporation and U.S. Bank National Association, which acts as an
administrative agent for a group of lenders under RCAI. RCAI establishes a revolving credit facility for the
Corporation, under which that group of lenders agree to lend to the Corporation amounts that may fluctuate
from time to time. Amounts drawn under the RCAI can only be used to support the Corporation’s obligation
to pay the purchase price of bonds that are subject to tender and that have not been successfully remarketed,
and the maturing principal of and interest on commercial paper notes. Of the $600 million available balance,
the first tranche of $300 million expires on September 26, 2025 and the second tranche of $300 million
expires on September 28, 2026. As of March 31, 2024 and June 30, 2023, there were no amounts
outstanding under RCAI.
On September 29, 2022, the Corporation renewed its three-year general-purpose credit facility (“RCAII”)
of $600 million, with a maturity date of September 26, 2025. The agreement is by and among the
Corporation and U.S. Bank National Association, which acts as an administrative agent for a group of
lenders under RCAII and establishes a revolving credit facility for the Corporation, under which that group
of lenders agree to lend to the Corporation amounts that may fluctuate from time to time. Amounts drawn
under the RCAII can be used for general corporate purposes and working capital needs. On March 19, 2024,
the Corporation executed a draw of $500 million. An additional $100 million draw was executed on March
25, 2024. The draws were executed as a result of the cyberattack on Change Healthcare, which disrupted
the billing and collection of patients accounts receivable and greatly impacted the Corporation’s cash flow
as of March 31, 2024. As of March 31, 2024 and June 30, 2023, there was $600 million and $0 million
outstanding under RCAII, respectively.
Each financial institution providing liquidity support under RCAI and RCAII is secured by an obligation
under the ARMI.
Standby Letters of Credit – The Corporation maintains an arrangement for multiple standby letters of credit
with a financial institution with a capacity available of $90.0 million as of March 31, 2024 and June 30,
2023, respectively. The arrangement supports multiple insurance, unemployment, and other risk liabilities
that total $52.7 million and $63.8 million as of March 31, 2024 and June 30, 2023, respectively. As of
March 31, 2024, and June 30, 2023, there were no draws on the letters of credit.
In addition, the Corporation maintains a two-year arrangement for standby letters of credit with an
additional financial institution in the amount of $50.0 million. The arrangement is for letters of credit that
can relate to multiple insurance, unemployment, and other risk liabilities. There were no letters of credit
issued under this arrangement as of March 31, 2024, and June 30, 2023, respectively.
The banks providing standby letters of credit are not secured by an obligation under the ARMI.
- 23 -
Transactions – In December 2022, the Corporation issued $329.7 million par value in tax-exempt fixed
rate private placement bonds. Proceeds were used to retire $300 million of outstanding taxable commercial
paper obligations issued in connection with the acquisition of MercyOne & MHN as described in Note 3,
and to refinance $29.7 million of outstanding taxable commercial paper obligations in connection with
certain tax-exempt fixed rate hospital revenue bonds.
In January 2023, the Corporation renewed $50.0 million direct placement bonds that were scheduled for
mandatory put in February 2023. In addition, during February 2023, the Corporation renewed $54.7 million
taxable fixed-rate direct placement bonds and converted them to taxable variable-rate direct placement
bonds. This debt obligation was scheduled for mandatory put in February 2023.
On March 1, 2023, the acquisition of Genesis, as described in Note 3, resulted in the assumption of revenue
bonds that totaled $140.7 million. On the acquisition date, Trinity Health issued replacement obligations
under the ARMI in exchange for obligations securing bonds previously issued under the Genesis Master
Indenture (“GMI”). The replacement obligations were accepted by banks previously holding Genesis
revenue bonds. Furthermore, all obligations under the GMI were cancelled and the GMI was discharged.
On June 30, 2023, the Corporation converted the $125.6 million taxable revenue bonds to tax-exempt fixed-
rate bonds.
In September 2023, the Corporation renewed $75.0 million direct placement bonds that were scheduled for
mandatory put in September 2023.
Each series of the referenced bonds is secured by an obligation issued under the ARMI.
6. PROFESSIONAL AND GENERAL LIABILITY PROGRAMS
The Corporation operates a wholly owned insurance company, Trinity Assurance, Ltd. (“TAL”). TAL
qualifies as a captive insurance company and provides certain insurance coverage to the Corporation’s
Health Ministries under a centralized program. The Corporation is self-insured for certain levels of general
and professional liability, workers’ compensation, and certain other claims. The Corporation has limited its
liability by purchasing other coverages from unrelated third-party commercial insurers. TAL has also
limited its liability through commercial reinsurance arrangements.
As discussed in Note 3, on March 1, 2023, the Corporation acquired Genesis Health System, an Iowa
nonprofit corporation, which was the sole member and shareholder of Misericordia Assurance Company,
LTD (“MAC”), a captive insurance company domiciled in the Cayman Islands. Effective March 1, 2023,
TAL policies included the facilities and individuals that were previously insured with MAC. Policies issued
and reinsurance purchased by MAC prior to March 1, 2023 and all losses previous to March 1, 2023, were
assumed by TAL through the merger of MAC into TAL effective as of December 1, 2023.
The Corporation’s current self-insurance program includes $25 million per occurrence with an additional
$5 million ($10 million aggregate) layer for the professional liability and $15 million per occurrence for
general liability as well as $10 million per occurrence for hospital government liability, $5 million per
occurrence for miscellaneous errors and omissions liability and network security and privacy liability, and
$1 million per occurrence for management liability (directors’ and officers’ and employment practices),
and certain other coverages. In addition, through TAL and its various commercial reinsurers, the
Corporation maintains integrated excess liability coverage with separate annual aggregate limits for
professional/general liability and management liability. The Corporation self-insures $750,000 per
occurrence for workers’ compensation in most states, with commercial insurance providing coverage up to
the statutory limits and self-insures up to $500,000 per occurrence for first-party property damage with
commercial insurance providing additional coverage. Privacy and network security coverage in excess of
the self-insurance is also commercially insured.
- 24 -
TAL reinsures a portion of its risks in order to limit its exposure to losses. This reinsurance coverage is in
excess of various attachment points. Reinsurance contracts do not relieve TAL from its obligations to
policyholders. Failure of reinsurers to honor their obligations could result in losses to TAL. Consequently,
TAL evaluates the financial condition of its reinsurers and monitors concentrations of credit risk arising
from similar geographic regions, activities, or economic characteristics of the reinsurers to minimize
exposure to significant losses from reinsurer insolvencies. TAL’s reinsurance contracts are placed with 20
commercial third party reinsurers with A.M. Best ratings of A- or better. Credit risk is minimized by TAL
by monitoring counterparty creditworthiness. TAL manages credit risk on the reinsurance recoverable by
dealing only with reinsurers with good credit ratings.
The liability for self-insurance reserves represents estimates of the ultimate net cost of all losses and loss
adjustment expenses, which are incurred but unpaid at the consolidated balance sheet date. The reserves
are based on the loss and loss adjustment expense factors inherent in the Corporation’s premium structure.
Independent consulting actuaries determined these factors from estimates of the Corporation’s expenses
and available industry-wide data. The Corporation discounts the reserves to their present value and used a
discount rate of 3.0% as of both March 31, 2024 and June 30, 2023. The reserves include estimates of future
trends in claim severity and frequency. Although considerable variability is inherent in such estimates,
management believes that the liability for unpaid claims and related adjustment expenses is adequate based
on the loss experience of the Corporation. The estimates are continually reviewed and adjusted as necessary.
The changes to the estimated self-insurance reserves were determined based upon the annual independent
actuarial analyses.
Claims in excess of certain insurance coverage and the recorded self-insurance liability have been asserted
against the Corporation by various claimants. The claims are in various stages of processing, and some may
ultimately be brought to trial. There are known incidents occurring through March 31, 2024, that may result
in the assertion of additional claims and other claims may be asserted arising from services provided in the
past. While it is possible that settlement of asserted claims and claims which may be asserted in the future
could result in liabilities in excess of amounts for which the Corporation has provided, management, based
upon the advice of legal counsel, believes that the excess liability, if any, should not materially affect the
consolidated financial statements of the Corporation.
7. PENSION AND OTHER BENEFIT PLANS
Deferred Compensation – The Corporation has nonqualified deferred compensation plans at certain Health
Ministries that permit eligible employees to defer a portion of their compensation. The deferred amounts
are distributable in cash after retirement or termination of employment. As of March 31, 2024, and June
30, 2023, the assets under these plans totaled $465.0 million and $380.2 million, respectively, and liabilities
totaled $468.8 million and $385.6 million, respectively, which are included in self-insurance, benefit plans
and other assets and other long-term liabilities in the consolidated balance sheets.
Defined Contribution Benefits – The Corporation sponsors defined contribution pension plans covering
substantially all of its employees. These programs are funded by employee voluntary contributions, subject
to legal limitations. Prior to January 1, 2024 employer contributions to the majority of these plans include
a nonelective contribution of 3% for participants who satisfied certain eligibility requirements, with a
minimum nonelective contribution for certain participants, and varying levels of matching contributions
based on employee service. Effective January 1, 2024, the nonelective contribution was eliminated and the
matching contribution formula changed for most of the plans. The new formula provides 100% match on
the first 3% of eligible compensation plus a 50% match on the next 7% of eligible compensation, regardless
of employee service. Eligibility requirements to receive the matching contribution did not change. The
employees direct their voluntary contributions and employer contributions among a variety of investment
options. Contribution expense under the plans totaled $309.5 million and $282.1 million for the nine-month
periods ended March 31, 2024 and 2023, respectively, which is included in employee benefits in the
consolidated statements of operations and changes in net assets.

- 25 -
Noncontributory Defined Benefit Pension Plans (“Pension Plans”) – The Corporation maintains
qualified Pension Plans that are closed to new participants, and under which benefit accruals are frozen.
Certain nonqualified, supplemental plan arrangements also provide retirement benefits to specified groups
of participants. Certain plans are subject to the provisions of ERISA. The majority of the plans sponsored
by the Corporation are intended to be “Church Plans,” as defined in the Code Section 414(e) and Section
3(33) of the ERISA, as amended, which have not made an election under Section 410(d) of the Code to be
subject to ERISA. The Corporation’s adopted funding policy for its qualified church plans, which is
reviewed annually, is to fund the current service cost based on the accumulated benefit obligations and
amortization of any under or over funding.
Plan Termination – Effective December 31, 2021 the Board approved the termination of the Trinity Health
ERISA Pension Plan (“ERISA Plan”). The ERISA Plan termination included the provision of a pension
lump sum election window that ran from January to March 2023. The ERISA Plan paid $82.5 million in
lump sum payments to the participants who elected such payments within that voluntary lump sum window.
In May 2023, the ERISA Plan irrevocably transferred all future obligations to a third-party insurance
company through the purchase of a group annuity contract. The purchase price of the group annuity contract
was $195.9 million. The plan termination process concluded in fiscal year 2023 resulting in a one-time
settlement charge of $88.4 million which is included in nonoperating items in the consolidated statements
of operations and changes in net assets. Additionally, a $13 million contribution was paid in fiscal year
2023 with an additional contribution of $2.8 million paid in fiscal year 2024 related to final plan termination
costs.
Postretirement Health Care and Life Insurance Benefits (“Postretirement Plans”) – The Corporation
sponsors both funded and unfunded contributory plans to provide health care benefits to certain of its
retirees. All of the Postretirement Plans are closed to new participants. The Postretirement Plans cover
certain hourly and salaried employees who retire from certain Health Ministries. Medical benefits for these
retirees are subject to deductibles and cost sharing provisions. The funded plans provide benefits to certain
retirees at fixed dollar amounts in health reimbursement account arrangements for Medicare eligible
participants.
Components of net periodic benefit expense (income) for the nine-month periods ended March 31 consisted
of the following (in thousands):
8. COMMITMENTS AND CONTINGENCIES
Litigation and Settlements – In November 2018, Mount Carmel Health System (“Mount Carmel”), the
Corporation’s Regional Health Ministry in Central Ohio, discovered sentinel events relating to the clinical
practice by one of its physicians and the related conduct of certain of Mount Carmel’s staff. The physician’s
employment was terminated, and this matter was reported to the authorities. Mount Carmel has been fully
cooperative with the investigations. The matter has been resolved as to the criminal aspects; however, the
civil litigation remains pending. The Corporation believes that this matter will be resolved without material
adverse effect to the Corporation’s future consolidated financial position or results of operations.
Pension Plans Postretirement Plans
2024 2023 2024 2023
Interest cost 220,880$ 222,674$ 2,824$ 2,830$
Expected return on assets (223,124) (214,467) (7,818) (6,804)
Amortization of prior service cost (3,678) (3,093) (260) (410)
Recognized net actuarial loss (gain) 51,900 58,698 (4,247) (2,770)
Net periodic benefit expense (income) 45,978$ 63,812$ (9,501)$ (7,154)$
- 26 -
The Corporation is involved, from time to time, in other litigation and regulatory investigations that may
result in litigation or settlement, arising in the ordinary course of doing business. After consultation with
legal counsel, management believes that these matters will be resolved without material adverse effect on
the Corporation’s future consolidated financial position or results of operations.
Health Care Regulatory Environment – The health care industry is subject to numerous and complex
federal, state and local government laws and regulations. These laws and regulations include, but are not
limited to, matters such as licensure, accreditation, data privacy and security, government health care
program participation requirements, government reimbursement rules for patient services, fraud and abuse
prevention requirements, and requirements for tax-exempt organizations. Both the CARES Act and the
Paycheck Protection Program and Health Care Enhancement Act (“PPPHCE Act”) include Terms and
Conditions as well as attestation to accept related funding. In addition, requirements for accepting, using
and reporting on use of the funds are numerous and the compliance guidance has been subject to periodic
updates by the Department of Health and Human Services. Laws and regulations concerning government
programs, including Medicare, Medicaid, Medicare Advantage, CARES Act and PPPHCE Act, are subject
to varying interpretation. Compliance with such laws and regulations is nuanced and can be subject to future
government review and interpretation as well as significant regulatory enforcement actions, including fines,
penalties, and potential exclusion from government health care programs such as Medicare and Medicaid.
The Corporation and its Health Ministries periodically receive requests for information and notices of
investigations regarding potential noncompliance with those laws and regulations, billing, payment, or
other reimbursement matters; or indicating the existence of whistleblower litigation which, in some
instances, have resulted in the Corporation entering into significant settlement agreements. There can be no
assurance that regulatory authorities will not challenge the Corporation’s compliance with these laws and
regulations. In addition, the contracts the Corporation has with commercial payers also provide for
retroactive audit and review of claims. The health care industry in general is experiencing an increase in
these activities as federal and state governments increase their enforcement activities and institute new
programs and tools designed to identify potential irregularities in reimbursement or quality of patient care.
Based on the information received to date, management does not believe the ultimate resolution of these
matters will have a material adverse effect on the Corporation’s future consolidated financial position or
results of operations. Trinity Health monitors its business activities for compliance with applicable laws
and regulations and operates a values-based ethics and compliance program that is designed to meet or
exceed applicable federal guidelines and industry standards.
9. SUBSEQUENT EVENTS
Management has evaluated subsequent events through May 17, 2024, the date the quarterly report was
issued. The following subsequent event was noted:
On April 10, 2024, the Corporation expanded its general-purpose credit facility RCAII and executed a
draw of $200 million. The funds will be used for general corporate purposes and working capital needs.
The additional draw was completed to increase liquidity due to the continued impact of the Change
Healthcare cyberattack on the Corporation’s balance sheet and cash flows.
******

Discussion and Analysis of
Financial Condition and Results
of Operations for Trinity Health
March 31, 2024
- 28 -
Introduction to Management's
Discussion & Analysis
Trinity Health Corporation, an Indiana nonprofit
corporation headquartered in Livonia, Michigan, and its
subsidiaries (“Trinity Health” or the “Corporation”),
controls one of the largest health care systems in the
United States.
The preparation of financial statements in conformity with
accounting principles generally accepted in the United
States of America requires management of the
Corporation to make assumptions, estimates and
judgments that affect the amounts reported in the
financial statements, including the notes thereto, and
related disclosures of commitments and contingencies, if
any. The Corporation considers critical accounting policies
to be those that require more significant judgments and
estimates in the preparation of its financial statements,
including the following: recognition of net patient service
revenue, which includes explicit and implicit price
concessions; financial assistance; premium revenue;
recorded values of investments and derivatives; goodwill;
evaluation of long-lived assets for impairment, reserves
for losses and expenses related to health care professional
and general liabilities; and risks and assumptions for
measurement of pension and retiree health liabilities.
Management relies on historical experience and other
assumptions, believed to be reasonable under the
circumstances, in making its judgments and estimates.
Actual results could differ materially from those
estimates.
The System uses operating cash flow as a measure of
performance. The System believes aggregate operating
cash flow is important because it provides additional
information about the System’s ability to incur and service
debt and make capital contributions. Operating cash flow
consists of operating income before depreciation and
amortization, asset impairment charges, and interest
expense. Operating cash flow is not a measurement of
financial performance or liquidity under generally
accepted accounting principles. It should not be
considered in isolation or as a substitute for revenue over
expenses, operating income, cash flows from operating
activities or financing activities, or any other measure
calculated in accordance with generally accepted
accounting principles. The items excluded from operating
cash flow are significant components in understanding
and evaluating financial performance.
Certain statements constitute “forward-looking
statements.” Such statements generally are identifiable
by the terminology used such as “plan,” “expect,”
“predict,” “estimate,” “anticipate,” “forecast” or similar
words. The achievement of certain results or other
expectations contained in such forward-looking
statements involve known and unknown risks,
uncertainties, and other factors, many of which the
Corporation is unable to predict or control, that may cause
actual results, performance, or achievements to be
materially different from those expressed or implied by
forward-looking statements.
Economic Impacts and Industry
Trends
Change Healthcare Cyberattack Incident – Change
Healthcare, a major clearinghouse for medical claims,
experienced a cyberattack in February 2024. The attack
did not directly impact the Corporation’s systems, but like
other major HealthCare systems, the event greatly
disrupted the billing and collection of patients accounts
receivable and greatly impacted the Corporation’s
balance sheet and cash flow as of March 31, 2024. Days
cash decreased 4 days from June 30, 2023 to 173 days as
of March 31, 2024, primarily driven by an $896.8 million
increase in patient accounts receivable, a use of 19 days
of cash, partially offset by cash preservation actions. In
March 2024, the Corporation drew $600 million from a
general-purpose liquidity facility. In April 2024, the
Corporation
expanded the general-purpose credit facility
and executed an additional line of credit draw of $200
million to aid in offsetting the decrease in cash collections
and to maintain liquidity needs. Additionally, the
Corporation slowed payments to certain vendors to
further preserve cash. Days in accounts receivable
increased to 56.1 days as of March 31, 2024. The
Corporation continues to monitor cash daily and other
means available such as its commercial paper program
authorized for borrowings of up to $600 million that can
be drawn upon, if necessary, of which $100 million is
currently outstanding.
On March 9, 2024, the Centers for Medicare & Medicaid
Services (“CMS”) made available accelerated payments to
providers and suppliers experiencing disruptions as a

- 29 -
result of the incident. These payments have been granted
in amounts of up to 30 days of average claims payments
and will be repaid through automatic recoupment from
Medicare claims for a period of 90 days. The Corporation
received $201.0 million of these cash advances of which
$161.4 million remained outstanding as of March 31,
2024.
Patient Behavior Trends – Lingering effects of the
global COVID-19 pandemic continue to impact the U.S.
health care industry and the financial condition, results of
operations and cash flows of the Corporation in the first
nine months of fiscal year 2024, although to a much lesser
extent than the same period in fiscal year 2023. Pandemic
driven patient behavior includes a shift from inpatient
care to ambulatory, home health, PACE, urgent care,
specialty pharmacy and digital telehealth care.
Labor and Inflationary Trends –
The Corporation’s
service mix, revenue mix and patient volumes still endure
negative impacts from broad economic factors spurred by
the COVID-19 pandemic, such as reduced consumer
spending, continued inflated costs of labor and supplies,
and the on-going nationwide shortage of nursing and
clinical staff exacerbated by the pandemic. The
Corporation’s response to these ongoing economic
factors continues to require increased labor rates and use
of contract labor staff. However, contract labor costs
during fiscal year 2024, on a same facility basis, are 24.9
percent lower than the prior fiscal year.
Strategies and Response – The Corporation continues
to take various actions utilizing the execution framework
“Run, Evolve and Transform” in fiscal year 2024 to
mitigate the impact on operations from negative ongoing
economic factors.
The Corporation is focused on clinical optimization and
access, revenue growth and diversification opportunities,
labor retention, recruitment, and stabilization, including
utilization of its FirstChoice internal staffing agency to
augment labor stabilization, new care delivery models,
and continued cost reduction plans to mitigate the
challenged economic and industry environment. The
Corporation is focused on optimizing revenue realization
and utilizes a multifaceted payer strategy to address a
challenging payer environment in the health care industry
and obtain fair payment rate increases. The Corporation
also launched a new innovative care delivery model using
a 3-person team with on-site and virtual nursing named
“TogetherTeam Virtual Connected Care” that is being
implemented system-wide and is already active in 22
hospitals and 58 nursing units, with additional sites slated
to go live in the fourth quarter of fiscal 2024. From these
actions, the Corporation is experiencing improvements in
patient and employee safety, access to care, employee
retention and patient satisfaction that are helping to
improve results of operations.
Integration of various fiscal year 2023 acquisitions
remains a focus with improvement initiatives to achieve
common platforms, efficiencies, and to leverage the
system resources of the Corporation. Furthermore, the
Corporation continues to control capital and reallocate
resources to support its operations and clinicians and
remains focused on investments supporting attainment of
Mission-critical initiatives. Actions taken have restored
the Corporation’s historical debt service coverage ratio to
3.1 compared to the 1.1 minimum threshold required for
the rolling twelve-month period ended March 31, 2024.
Acquisitions and Divestiture
The Corporation continually evaluates potential
opportunities for strategic growth as part of the overall
strategic plan. In addition to pursuing growth through
strategic capital investment and organically, at our
Ministries, the Corporation’s approach to strategic growth
includes pursuing prudent mergers, acquisitions, joint
ventures, and portfolio management transactions. As
further described in Note 3 to the unaudited financial
statements, the following material transactions were
undertaken.
MercyOne & Mercy Health Network – On September
1, 2022, the Corporation completed a transaction with
CommonSpirit Health (“CSH”) through which the
Corporation acquired CSH’s 50 percent interest in Mercy
Health Network (“MHN”) and MHN became the sole
corporate member of Catholic Health Initiatives-Iowa,
Corp. d/b/a MercyOne Des Moines Medical Center
(“MercyOne Des Moines”), a regional health care system
located in Des Moines, Iowa. In addition, certain home
care, hospice, and home infusion pharmacy operations
were acquired from an affiliate of CSH located in the
vicinity of Des Moines (collectively the “MercyOne
Acquisition”).

- 30 -
North Ottawa Community Health System (“Grand
Haven”)
– The Corporation’s affiliate, Mercy Health
Partners, completed a transaction with Grand Haven
under which Mercy Health Partners became the sole
member of Grand Haven on October 1, 2022. Grand
Haven and its affiliates operate an acute care hospital,
urgent care center, long-term care facility and provide
hospice services in the communities surrounding Grand
Haven, Michigan.
St. Francis Medical Center (“SFMC”) – On December
22, 2022, the Corporation, through its subsidiary Maxis
Health System, transferred the membership interest of
SFMC and certain subsidiaries as well as $14.5 million of
cash, and certain inventory and equipment, to Capital
Health System, Inc. As a result of this transaction,
restructuring costs of $82.3 million were incurred during
fiscal year 2023, primarily related to loss on sale, asset
retirement obligations and transition benefits for
colleagues.
Genesis Health System – On March 1, 2023, the
Corporation and its affiliate, MHN, completed a
transaction with Genesis Health System, an Iowa
nonprofit corporation and Genesis Health System, an
Illinois not-for-profit corporation (together “Genesis”),
under which MHN became the sole member of each.
Genesis and its affiliates operate four acute care hospitals,
including two critical access hospitals, convenient care
centers, physician practices, a long-term care facility joint
venture, an independent living facility for seniors and
hospice services in the communities in eastern Iowa and
western Illinois.
The acquisitions of MercyOne, Grand Haven, and Genesis,
are collectively referred to as the (“Acquisitions”).
Results from Operations
Operating Income (Loss) Before Other Items
Trinity Health reported significant improvements in
operating performance with operating income before
other items of $69.8 million (operating margin of 0.4
percent and cash flow margin of 5.3 percent) for the nine
months ended March 31, 2024 compared to operating
losses before other items of $263.1 million (operating
margin of [1.6] percent and cash flow margin of 3.7
percent) for the nine months ended March 31, 2023.
Improvements were attained in payment rates, same
facility patient care volume growth and as a result of
several revenue and cost management initiatives that are
improving operations as described above in “Economic
Impacts and Industry Trends – Strategies and Response”
and subsequently in “Revenue.” Quarterly margins
continue to show improvement as illustrated in the chart
below.
On a same facility basis, volumes as measured by case mix
adjusted equivalent discharges (“CMAEDs”) increased 0.5
percent, during the nine months ended March 31, 2024
compared to the same period in the prior fiscal year.
Revenue
Total operating revenue of $17.8 billion increased $1.8
billion, or 11.4 percent, for the nine months ended March
31, 2024 compared to the same period in the prior fiscal
year. Revenue growth was driven by the Acquisitions
which accounted for $1.0 billion of the increase and same
facility net patient service revenue growth. These
increases were partially offset by the divestiture of SFMC
that reduced operating revenue by $59.3 million
compared to prior year. Excluding the Acquisitions and
divestiture of SFMC, on a same facility basis, operating
revenue increased $863.8 million or 5.8 percent over the
prior fiscal year. Net patient service revenue grew $748.7
million or 5.8 percent excluding the Acquisitions. Same
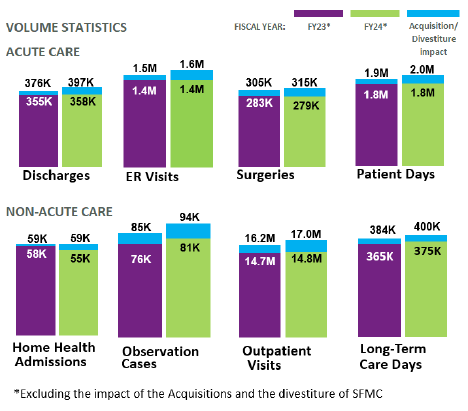
- 31 -
facility net patient service revenue was positively
impacted by improvements in payment rates (inclusive of
a $146.2 million accrual for new Medicaid Provider
funding in Iowa and Medicaid provider tax rate changes in
Michigan and a $102.8 million 340B remedy lump sum
settlement received from the Centers for Medicare &
Medicaid Services (“CMS”) under the November 8, 2023
Final Rule related to underpayments in the drug discount
program for calendar years 2018 to 2022), same facility
patient volumes, and to a lesser extent case mix.
Other revenue increased $108.1 million, or 8.7 percent,
compared to the prior fiscal year on a same facility basis,
primarily driven by $86.9 million of pharmacy revenue and
to a lesser extent, gainshare revenue and equity in
earnings of unconsolidated affiliates. In addition,
premium and capitation revenue increased $10.0 million
primarily within the Corporation’s health plans and PACE
programs. The majority of the Corporation’s revenue is
comprised of outpatient and other non-patient revenue,
and the Corporation continues to diversify its business
segments to gain better position for balanced
performance when individual segments are challenged.
Expenses
Total operating expenses increased $1.5 billion to $17.7
billion or 9.1 percent, for the nine months ended March
31, 2024 compared to the same period in the prior fiscal
year, with the Acquisitions accounting for $902.9 million
or 5.6 percent of the overall increase. Excluding the
impact of the Acquisitions and divestiture of SFMC, on a
same facility basis, operating expenses for the nine
months ended March 31, 2024 increased $653.0 million,
or 4.3 percent. Total operating costs per case (as
measured by CMAEDs) increased 2.7 percent compared to
the prior year as the Corporation continues to tightly
manage operating costs amid inflation. On a same facility
basis, salaries and wages rose $380.1 million, or 5.6
percent, with a 3.7 percent increase in salary rates and a
1.9 percent increase in FTEs, as the Corporation continues
to implement initiatives to address industry wide staffing
shortages and wage inflation. Same facility fiscal year
2024 salary rate increases include a $65.4 million one-
time compensation award program. Same facility
employee benefit costs increased $100.2 million or 8.0
percent, including a $64.7 million or 16.9 percent increase
in employee health plan costs.
Supply costs increased $141.4 million, or 5.3 percent, on a
same facility basis compared to the prior fiscal year,
primarily due to increased pharmacy volume. Although
overall supply costs increased, supplies as a percent of net
patient service revenue, excluding the 340B remedy
settlement and accrual of the aforementioned provider
tax changes, decreased 0.7 percent from prior year. Same
facility increases were also reported in interest expense
and other expenses, which includes $55.1 million of
increased provider tax expense related to the
aforementioned Medicaid provider tax changes.
The Corporation continues to use strong cost controls
o
ver contract labor and other operational spending. Labor
stabilization is occurring with investments in its
FirstChoice internal staffing agency and TogetherTeam
Virtual Connected Care model. On a same facility basis,
contract labor costs decreased $71.3 million, or 24.9
percent, compared to the prior fiscal year. Total contract
labor costs declined $404.9 million or 59.2 percent for the
nine months ended March 31, 2024 compared to the prior
fiscal year. The reduction includes $335.6 million of costs
at MercyOne Des Moines, one of the larger components
of the MercyOne Acquisition, which included costs for
colleagues that were leased from CSH throughout nearly
all of fiscal year 2023. Those costs are included in salaries,
wages, and employee benefits in fiscal year 2024. Further
same facility expense reductions were also seen in
purchased services and medical claims, depreciation and
amortization, and occupancy.
- 32 -
Other Items
For the first nine months of fiscal year 2023, other items
consisted of $53.9 million for a dividend received from a
cost method investment related to a gain on sale realized
by the investee and an $8.0 million gain for the final
settlement from the fiscal year 2022 sale of Gateway
Health Plan, L.P., and Subsidiaries offset by $82.3 million
of restructuring costs related to the divestiture of SFMC,
as noted above. Including other items, operating loss
totaled $283.5 million, with operating margin of (1.8)
percent for the first nine months of fiscal year 2023.
Nonoperating Items
The Corporation reported non-operating income of $1.2
billion for the nine months ended March 31, 2024 and
2023. Non-operating income was driven by investment
earnings of $853.0 million, or 9.1 percent for the first nine
months of fiscal year 2024 compared to earnings of $457.3
million or 5.4 percent during the same period in the
previous fiscal year, an increase of $395.7 million.
Investment returns also drove the $137.7 million
improvements in equity in earnings of unconsolidated
affiliates which totaled $433.1 million for the nine months
ended March 2024. This was partially offset by a reduction
in inherent contributions of $487.7 million primarily
related to the fiscal year 2023 acquisitions of Genesis
Health System and Grand Haven.
Excess of Revenue over Expenses
Excess of revenue over expenses for the nine months
ended March 31, 2024 was $1.3 billion (net margin of 6.6
percent) compared to excess of revenue over expenses of
$856.3 million (net margin of 5.1 percent) for the nine
months ended March 31, 2023. The increase included
improvements in operations and increases in both
nonoperating investment earnings and equity in earnings
of unconsolidated affiliates, partially offset by reductions
in inherent contributions.
Balance Sheet
The Corporation’s balance sheet remains strong after
prompt responses to negative impacts from Change
Healthcare’s cyberattack which include drawing upon
liquidity facilities and receipt of Medicare cash advances,
amongst others, as described above in “Economic Impacts
and Industry Trends – Change Healthcare Cyberattack
Incident.” The Corporation reported total assets of $34.7
billion as of March 31, 2024, which increased $2.4 billion,
or 7.4 percent compared to June 30, 2023. The growth
includes the aforementioned $896.8 million increase in
patient accounts receivable, impacted by Change
Healthcare’s cyberattack. In addition, investments in
unconsolidated affiliates increased $434.7 million, driven
by an increase in the equity method investment in
BayCare Health System. Estimated receivables from third-
party payers increased $245.9 million and includes a
$232.7 million increase in provider tax receivables related
to the Medicaid provider tax changes in Iowa and
Michigan.
Unrestricted cash and investments increased to $10.7
billion as of March 31, 2024, up $494.2 million from June
30, 2023, which includes $600 million of line of credit
draws on the Corporation’s general purpose liquidity
facility. Days cash on hand decreased 4 days since June 30,
2023 to 173 days, heavily impacted by an increase in
patient accounts receivable, an increase in expenses per
day driven by nine months of expenses for the
Acquisitions in fiscal year 2024, and capital expenditures.
The decreases were partially offset by investment
earnings, the $600 million line of credit draws, and
operating cash flows. Excluding the $600 million line of
credit draws and the $161.4 million of Medicare cash
advances net of recoupments, days cash declined 17 days
from June 30, 2023 to 161 days. Net days in accounts
receivable increased by 10.8 days to 56.1 days from June
30, 2023 to March 31, 2024.
Total liabilities of $14.9 billion increased $971.6 million or
7.0 percent compared to June 30, 2023. This increase was
primarily due to a net increase in debt of $458.3 million
due to the line of credit draws, partially offset by principal
payments, along with an increase in accounts payable and
accrued expenses of $297.4 million, as the Corporation
slowed payments to certain vendors and $161.4 million of
Medicare cash advances, net of recoupments. Debt to
capitalization was 31 percent as of March 31, 2024 and
June 30, 2023. Cash to Debt decreased from 132 percent
to 131 percent from June 30, 2023 to March 31, 2024.

- 33 -
Balance Sheet Metrics
Statement of Cash Flows
Cash, cash equivalents and restricted cash increased
$391.6 million during the first nine months of fiscal year
2024. Operating activities provided $126.7 million of cash,
including $161.4 million of Medicare cash advances net of
recoupments, while investing activities used $157.4 million
of cash, including $692.7 million for purchases of property
and equipment, partially offset by $594.7 million of net
sales of investments. Financing activities provided $422.3
million of cash, driven by the $600 million line of credit
draws.

- 34 -
TRINITY HEALTH
Liquidity Reporting
March 31, 2024
($ in millions)
(unaudited)
ASSETS
Daily Liquidity
Money Market Funds (Moody's rated Aaa)
$ 329
Checking and Deposit Accounts (at P-1 rated bank)
368
Repurchase Agreements
-
U.S. Treasuries & Aaa-rated Agencies
-
Dedicated Bank Lines
600
Subtotal Daily Liquidity (Cash & Securities)
$ 1,297
Undrawn Portion of $600 Million Taxable Commercial Paper Program
500
Subtotal Daily Liquidity Including Taxable Commercial Paper Program
$ 1,797
Weekly Liquidity
Exchange Traded Equity
$ 3,451
Publicly Traded Fixed Income Securities Rated at least Aa3 and Bond Funds
1,908
Equity Funds
756
Other
210
Subtotal Weekly Liquidity
6,325
TOTAL DAILY AND WEEKLY LIQUIDITY
$ 8,122
Longer-Term Liquidity
Funds, vehicles, investments that allow withdrawals with less than one-month
notice
1,232
Funds, vehicles, investments that allow withdrawals with one-month notice or
longer
3,321
Total Longer-Term Liquidity
$ 4,553
LIABILITIES (Self-liquidity Variable Rate Demand Bonds & Commercial Paper)
Weekly Put Bonds
VRDO Bonds (7-day)
$ 164
Long-Mode Put Bonds
VRDO Bonds (Commercial Paper Mode)
134
Taxable Commercial Paper Outstanding
100
TOTAL SELF-LIQUIDITY DEBT AND COMMERCIAL PAPER
$ 398
Ratio of Daily and Weekly Liquidity to Self-Liquidity Debt and Commercial Paper
20.41

- 35 -
Trinity Health
Financial Ratios and Statistics (Unaudited)
March 31,
March 31,
2024
2023
Financial Indicators
Liquidity Ratios (as of March 31)
Days Cash on Hand
173
180
Days in Accounts Receivable, Net
56.1
45.2
Leverage Ratios (as of March 31)
Debt to Capitalization
31%
32%
Cash to Debt
131%
132%
Profitability Ratios (For the nine months ended March 31)
Operating Margin before Other Items
0.4%
(1.6%)
Operating Cash Flow Margin before Other Items
5.3%
3.7%
Statistical Indicators (For the nine months ended March 31)
Rounded to nearest thousand
Discharges
397,000
376,000
Patient Days
1,963,000
1,879,000
Outpatient Visits
17,039,000
16,197,000
Emergency Room Visits
1,590,000
1,512,000
Observation Cases
94,000
87,000
Continuing Care
Home Health Admissions
59,000
59,000
Long-term Care Patient Days
400,000
384,000
