
Guidelines for
Living Donor Kidney
Transplantation
United Kingdom Guidelines
www.bts.org.uk
© British Transplantation Society
March 2018
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
Fourth Edition
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
2
CONTENTS
1 INTRODUCTION AND OBJECTIVES 5
1.1 Introduction 5
1.2 Scope of the Guidelines 6
1.3 Process of Writing and Methodology 6
1.4 Editorial Committee 7
1.5 Contributing Authors 7
1.6 Disclaimer 10
1.7 Declarations of Interest 11
1.8 Grading of Recommendations 11
1.9 Abbreviations 12
2 LEGAL FRAMEWORK 15
2.1 The Human Tissue Act 2004 15
2.2 The Human Tissue Authority (HTA) 16
2.3 The European Union Organ Donation Directive 16
2.4 Consent for the Removal of Organs from Living Donors 17
2.5 Types of Living Kidney Donation Permitted by the Legislation 17
2.6 Requirements for Transplants involving a Living Donor 19
2.7 Prohibition of Commercial Dealings in Human Material 20
2.8 Reimbursement of Expenses 21
2.9 Exceptional Circumstances 21
2.10 The Human Tissue (Scotland) Act 2006 22
3 ETHICS 26
3.1 Ethics 26
3.2 Key Ethical Principles in Living Donor Transplantation 26
3.3 The Recipient Perspective 27
3.4 The Donor Perspective 28
3.5 The Transplant Team Perspective 29
3.6 Expanding the Living Donor Pool 30
3.7 The Child or Young Person as a Living Donor 30
3.8 The British Transplantation Society (BTS) Ethics Committee 30
4 SUPPORTING AND INFORMING THE POTENTIAL DONOR 32
4.1 Confidentiality 33
4.2 Informing the Potential Donor 34
4.3 Informed Consent for Living Kidney Donation 35
4.4 Donor Identity 39
4.5 Patient Advocacy 40
4.6 Independent Translators 42
4.7 Psychological Issues 42
4.8 Death and Transplant Failure 45
5 DONOR EVALUATION 48
5.1 Introduction 48
5.2 Donor Evaluation: Summary 52
5.3 ABO Blood Grouping and Crossmatch Testing 58
5.4 Medical Assessment 59
5.5 Assessment of Renal Function 66
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
3
5.6 Donor Age 79
5.7 Donor Obesity 85
5.8 Hypertension in the Donor 90
5.9 Diabetes Mellitus 98
5.10 Cardiovascular Evaluation 105
5.11 Proteinuria 110
5.12 Non-Visible Haematuria 116
5.13 Pyuria 123
5.14 Infection in the Prospective Donor 125
5.15 Nephrolithiasis 139
5.16 Haematological Disease 146
5.17 Familial Renal Disease 151
5.18 Donor Malignancy 159
6 SURGERY: TECHNICAL ASPECTS, DONOR RISK AND
PERI-OPERATIVE CARE 171
6.1 Introduction 172
6.2 Assessment of Renal Anatomy 173
6.3 Peri-Operative Mortality 176
6.4 Peri-Operative Morbidity 177
6.5 Long-Term Mortality 178
6.6 Pre-operative Care and Preparation 179
6.7 Donor Nephrectomy 181
7 HISTOCOMPATIBILITY TESTING FOR LIVING DONOR
KIDNEY TRANSPLANTATION 191
7.1 Assessment of Donor-Recipient HLA Mismatch Status 193
7.2 Identification and Characterisation of Alloantibodies 194
7.3 Pre-transplant Donor-Recipient Crossmatch Test 196
7.4 Selection of Suitable Donor-Recipient Pairs 198
7.5 Antibody Incompatible Living Donor Transplantation 199
8 EXPANDING THE DONOR POOL 202
8.1 Paired/Pooled Living Donation 203
8.2 Altruistic Donation (Directed and Non-directed) 210
8.3 Antibody Incompatible Donation 219
8.4 Appendix: Mental Health Assessment of Altruistic Kidney Donors 222
9 LOGISTICAL CONSIDERATIONS 235
9.1 Reimbursement of Living Donor Expenses 235
9.2 Donors who are Non-UK Residents 237
9.3 Prisoners as Living Donors 238
9.4 Appendix: Template Letter for Potential Overseas Donors 243
10 DONOR FOLLOW-UP AND LONG-TERM OUTCOME 247
10.1 Long-Term Outcome Following Living Kidney Donation 248
10.2 Arrangements for Follow-up 251
10.3 The Unsuitable Donor 255
10.4 Pregnancy following Kidney Donation 256
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
4
11 RECIPIENT OUTCOME AFTER LIVING DONOR KIDNEY
TRANSPLANTATION IN ADULTS 260
11.1 Living versus Deceased Donor Transplantation 261
11.2 Extended Criteria Living Donors 261
11.3 Transplantation versus Dialysis 262
11.4 High Risk Recipients 263
12 RECURRENT RENAL DISEASE 267
12.1 Introduction 268
12.2 Diabetic Nephropathy 269
12.3 Primary Focal Segmental Glomerulosclerosis 269
12.4 IgA Nephropathy 270
12.5 Membranous Nephropathy 271
12.6 Amyloidosis 272
12.7 Systemic Lupus Erythematosus 273
12.8 ANCA Associated Systemic Vasculitis 273
12.9 Goodpasture’s Disease 274
12.10 Alport Syndrome 274
12.11 Mesangiocapillary Glomerulonephritis 275
12.12 Haemolytic Uraemic Syndrome 277
12.13 Primary Hyperoxaluria 278
12.14 Cystinosis 279
13 LIVING DONOR KIDNEY TRANSPLANTATION IN CHILDREN 284
13.1 Introduction 284
13.2 Donor Selection 285
13.3 Recipient Considerations 286
13.4 Surgery 287
14 APPENDIX 291
14.1 Conflicts of Interest 291
14.2 Search Strategies 292
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
5
1 INTRODUCTION AND OBJECTIVES
1.1 Introduction
Kidney transplantation from a living donor, when available, is the treatment of choice
for most patients with end stage renal disease, offering optimum patient and graft
survival and reduced time on the national transplant waiting list. Living donor
transplantation also offers a proportion of complex recipients the opportunity to
benefit from a transplant that they might otherwise not have received from the
deceased donor waiting list; or, through the UK Living Kidney Sharing Schemes
(UKLKSS), a better quality or better matched kidney than might otherwise have been
available.
For all these reasons, and the opportunity to expand the kidney donor pool, living
kidney donation has been actively promoted in the UK over the last 20 years. At the
time of writing, approximately 1 in 3 kidney transplants performed in the UK are from
living donors. The latest national statistics show that there were 998 living kidney
donor transplants in the UK in 2016-17 (1). Of 926 adult donor transplants, 484 were
related, 442 were unrelated, 18 were HLA incompatible, 65 were ABO incompatible,
109 were paired/pooled, and 81 were altruistic donor transplants. 36% of the
patients transplanted from living donors were transplanted pre-emptively,
i.e. without a need for dialysis (1).
The expansion of the UKLKSS has represented a significant change in practice
since the last edition of this guideline, not least by reducing the need for HLA- and
ABO-incompatible transplantation. In parallel, increasing confidence in the safety of
living kidney donation has permitted the expansion of the potential donor pool; to
date, the oldest living kidney donor in the UK was aged 85.
Nonetheless, it must be recognised that living kidney donation carries some risk.
The welfare of the donor remains paramount, and vigilance in donor care and
management is essential to ensure that appropriate safeguards are in place to
protect individuals and to inspire public confidence. These guidelines are intended
to act as a resource for the transplant community, and to underpin best practice in
living donor kidney transplantation.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
6
1.2 Scope of the Guidelines
This guidance relates only to living donor kidney transplantation and reflects a
growing body of evidence, incorporating aspects of clinical practice that are relevant
to both adult and paediatric settings. These include the ethical and medico-legal
aspects of donor selection, medical and pre-operative donor evaluation,
identification of high risk donors, the management of complications, and expected
outcome. Scenarios that present an increased level of risk to the potential recipient,
such as antibody incompatible transplantation, recurrent disease and
transplantation in the context of other co-morbidities, are also included. Guidance is
provided on the most appropriate investigations to be considered to assist clinical
decision-making, and the best surgical approaches when faced with different clinical
scenarios.
1.3 Process of Writing and Methodology
The original ‘UK Guidelines for Living Donor Kidney Transplantation’ were
commissioned by the British Transplantation Society (BTS) and the Renal
Association (RA) as part of a wider initiative to develop ‘Best Practice’ guidance for
clinicians involved in transplantation. Initially published in 2000 (2) and revised in
2005 (3) and 2011 (4), the guidelines have achieved international repute. This fourth
edition has used the framework of previous editions but has been significantly
updated in the light of new data and changing practice. It has been produced with
wide representation from UK colleagues and professional bodies involved in both
donor and recipient management and in consultation with patient representatives.
In updating these guidelines, areas of interest were identified with input from
clinicians and patient representatives. A systematic review of the relevant literature
and synthesis of the available evidence was undertaken by selected relevant clinical
experts. This was followed by peer group appraisal and expert review. Draft
proposals were amended by the editorial committee and the appropriate levels of
evidence added to recommendations. Wider consultation with the transplant
community was undertaken by e-mail. The penultimate draft of the document was
placed on the BTS website in January 2018 for a six week period of open
consultation, to which professional groups, patients and other authorities were
actively encouraged to contribute. The final document was posted in March 2018.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
7
Where available, these guidelines are based on published evidence, and the
evidence and recommendations have been graded for strength except where the
published studies are descriptive. With a handful of exceptions, conference
presentations have not been included and the publication cut-off date for evidence
was July 2017.
It is anticipated that these guidelines will next be revised in 2023.
1.4 Editorial Committee
Dr Peter A Andrews MD FRCP
Consultant Nephrologist & Clinical Lead for Transplantation, SW Thames Renal &
Transplantation Unit, St Helier Hospital, Surrey
Reader in Renal Medicine, University of London
Chair of BTS Standards Committee
Ms Lisa Burnapp RN MA
Consultant Nurse, Living Donor Kidney Transplantation, Guy’s & St Thomas’ NHS
Foundation Trust, London
Lead Nurse - Living Donation, Organ Donation and Transplantation, NHS Blood and
Transplant (NHSBT)
1.5 Contributing Authors
Dr Peter Andrews MD FRCP, Consultant Nephrologist & Reader in Renal Medicine,
SW Thames Renal & Transplantation Unit, St Helier Hospital, Surrey
Dr Richard Baker PhD FRCP, Consultant Nephrologist, St. James’s University
Hospital, Leeds
Prof Simon Ball PhD FRCP, Consultant Nephrologist, Queen Elizabeth Hospital,
Birmingham
Dr Kate Bramham PhD MRCP, Consultant Nephrologist, King’s College Hospital,
London
Mr Tim Brown FRCS, Consultant Transplant Surgeon, Belfast City Hospital, Belfast.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
8
Ms Lisa Burnapp RN MA, Lead Nurse, Living Donation, NHS Blood and Transplant
& Consultant Nurse, Living Donor Kidney Transplantation, Guy’s & St Thomas’
NHS Foundation Trust, London
Prof Jamie Cavenagh MD FRCP FRCPath, Consultant Haematologist, Barts and
the London NHS Trust, London
Mr Marc Clancy PhD FRCS, Consultant Transplant Surgeon, Queen Elizabeth
Hospital, Glasgow
Dr Aisling Courtney MPhil FRCP, Consultant Nephrologist, Belfast City Hospital,
Belfast
Dr Sam Dutta, MS FRCS, Consultant Transplant Surgeon, Nottingham City
Hospital, Nottingham
Dr Robert Elias MD FRCP, Consultant Nephrologist, King’s College Hospital NHS
Foundation Trust, London
Dr Anthony Fenton MRCP, Speciality Registrar, Queen Elizabeth Hospital,
Birmingham
Prof Susan Fuggle DPhil FRCPath, Consultant Clinical Scientist, Oxford Transplant
Centre, Oxford
Mr Keith Graetz DM FRCS, Consultant Transplant and General Surgeon,
Wessex Kidney Centre, Portsmouth
Dr Siân Griffin PhD FRCP, Consultant Nephrologist, University Hospital of Wales,
Cardiff
Dr Brendan Healy MRCP MRCPath, Consultant in Microbiology and Infectious
Diseases, University Hospital of Wales, Cardiff
Dr Rachel Hilton PhD FRCP, Consultant Nephrologist, Guy’s & St Thomas’ NHS
Foundation Trust, London
Dr Gareth Jones PhD FRCP, Consultant Nephrologist, Royal Free Hospital, London
Dr Graham Lipkin MD FRCP, Consultant Nephrologist, University Hospitals
Birmingham NHS Foundation Trust, Birmingham
Dr Adam Mclean DPhil FRCP, Consultant Nephrologist & Transplant Physician,
West London Renal & Transplant Centre, London
Prof Nizam Mamode MD FRCS, Professor of Transplant Surgery, Guy’s & St
Thomas’ NHS Foundation Trust, London
Ms Hanna Maple PhD MRCS, SpR in Transplant Surgery, Guy’s & St Thomas’ NHS
Foundation Trust, London
Dr Stephen Marks MRCP FRCPCH, Reader and Consultant in Paediatric
Nephrology, Great Ormond Street Hospital for Children NHS Foundation Trust,
London

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
9
Dr Emma K Montgomery MRCP, Consultant Nephrologist, Freeman Hospital,
Newcastle
Dr Peter Nightingale PhD, Statistician, University Hospitals Birmingham NHS
Foundation Trust, Birmingham
Mr Jonathan Olsburgh PhD FRCS(Urol), Consultant Transplant & Urological
Surgeon, Guy’s & St Thomas’ NHS Foundation Trust, London
Professor Michael Peters MD FMedSci, Professor of Applied Physiology, Brighton
and Sussex Medical School, Brighton
Dr Michael Picton PhD FRCP, Consultant Nephrologist, Manchester Royal
Infirmary, Manchester
Dr Stephen Potts FRCPsych FRCPE, Consultant in Transplant Psychiatry, Royal
Infirmary of Edinburgh, Edinburgh
Dr Nicola Price DPhil FRCPath, Consultant Virologist, University Hospital of Wales,
Cardiff
Dr Richard Sandford PhD FRCP, Honorary Consultant in Medical Genetics,
University of Cambridge, Cambridge
Dr Alastair Santhouse FRCP FRCPsych, Consultant Psychiatrist in Psychological
Medicine, South London and Maudsley NHS Foundation Trust, London
Prof Neil Sheerin PhD MRCP, Professor of Nephrology, Newcastle University,
Newcastle
Ms Lisa Silas RN MSc, Advanced Nurse Practitioner, Living Kidney Donation, ABO
and Recipient Workup, Guy’s & St Thomas’ NHS foundation Trust, London
Ms Karen Stevenson PhD FRCS, Consultant Transplant Surgeon, Queen Elizabeth
Hospital, Glasgow
Dr Craig Taylor PhD FRCPath, Director of Histocompatibility and Immunogenetics,
Cambridge University Hospital NHS Foundation Trust, Cambridge
Dr Raj Thuraisingham MD FRCP, Consultant Nephrologist, Barts and the London
NHS Trust, London
Dr Nicholas Torpey PhD FRCP, Consultant Nephrologist, Addenbrooke’s Hospital,
Cambridge
Dr Caroline Wroe, Consultant Nephrologist, PhD MRCP, South Tees Hospitals NHS
Foundation Trust, Middlesborough
Contributions to draft versions of this guideline were also made by the following:
Prof Derek Manas, Professor of Transplant Surgery, Newcastle
Dr Liset Pengel, Peter Morris Centre for Evidence in Transplantation, London
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
10
Dr Mysore Phanish, Consultant Nephrologist, St Helier Hospital, Surrey
Ms Jan Shorrock, donor representative, ‘Give a Kidney’ charity
The following made helpful comments at the consultation stage which have been
incorporated into the final version of the guidelines:
Prof Paul Cockwell, Consultant Nephrologist, Queen Elizabeth Hospital,
Birmingham
Prof Colin Geddes, Consultant Nephrologist, Queen Elizabeth University Hospital,
Glasgow
Ms Tess Harris, Chief Executive Officer, Polycystic Kidney Disease Charity
Ms Jessica Porter, Head of Regulation, on behalf of the Human Tissue Authority,
London
Dr Kerry Tomlinson, Consultant Nephrologist, Royal Stoke University Hospital,
Stoke-on-Trent
Mr Ray Trevitt, Living Donor Coordinator, Barts and the London NHS Trust, London
Prof Chris Watson, Professor of Transplant Surgery, Addenbrooke’s Hospital,
Cambridge
We also thank contributors to earlier editions of this guideline, some of whose work
remains unchanged in this edition, but who have been previously acknowledged.
1.6 Disclaimer
This document provides a guide to best practice, which inevitably evolves over time.
All practitioners need to undertake clinical care on an individualised basis and keep
up to date with changes in the practice of clinical medicine.
These guidelines represent the collective opinions of a number of experts in the field
and do not have the force of law. They contain information/guidance for use by
practitioners as a best practice tool. The opinions presented are subject to change
and should not be used in isolation to define the management for any individual
patient. The guidelines are not designed to be prescriptive, nor to define a standard
of care.
The British Transplantation Society and the Renal Association cannot attest to the
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
11
accuracy, completeness or currency of the opinions contained herein and do not
accept any responsibility or liability for any loss or damage caused to
any practitioner or third party as a result of any reliance being placed on the
guidelines or as a result of any inaccurate or misleading opinion contained therein.
1.7 Declarations of Interest
Editors, authors and contributors have worked to the standards detailed in the BTS
Clinical Practice Guideline accessible at:
http://www.bts.org.uk/MBR/Clinical/Guidelines/Current/Member/Clinical/Current_
Guidelines.aspx (7).
Declarations of interest are listed in an appendix to this document.
1.8 Grading of Recommendations
In these guidelines, the GRADE system has been used to rate the quality of
evidence and the strength of recommendations (4). This approach is consistent with
that adopted by KDIGO in its recent guidance relating to renal transplantation, and
also with guidelines from the European Best Practice Committee, and from the
Renal Association.
For each recommendation the quality of evidence has been graded as one of:
A (high)
B (moderate)
C (low)
D (very low)
For each recommendation, the strength of recommendation has been indicated as
one of:
Level 1 (we recommend)
Level 2 (we suggest)
Not graded (where there is not enough evidence to allow formal grading)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
12
These guidelines represent consensus opinion from experts in the field of
transplantation in the United Kingdom. They represent a snapshot of the evidence
available at the time of writing. It is recognised that recommendations are made
even when the evidence is weak. It is felt that this is helpful to clinicians in daily
practice and is similar to the approach adopted by KDIGO (5).
1.9 Abbreviations
The following abbreviations are used in this document:
ABPM Ambulatory Blood Pressure Monitoring
ABOi ABO Incompatible
ACR Albumin: Creatinine ratio
ADPKD Autosomal Dominant Polycystic Kidney Disease
AIT Antibody Incompatible Transplantation
ADC Altruistic Donor Chain
AML Angiomyolipoma
BMI Body Mass Index
BTS British Transplantation Society
CKD Chronic Kidney Disease
CMV Cytomegalovirus
CTS Collaborative Transplant Study
DAD Directed Altruistic Donor
DDD Dense Deposit Disease
DSA Donor-Specific antibody
DTT Dithiothreitol
DVT Deep Vein Thrombosis
EBV Epstein-Barr Virus
eGFR Estimated Glomerular Filtration Rate
ESRD End Stage Renal Disease
EUODD European Union Organ Donation Directive
ECD Expanded Criterion Donor
ERAS Enhanced Recovery After Surgery
FSGS Focal Segmental Glomerulosclerosis
GMC General Medical Council
GFR Glomerular Filtration Rate
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
13
HBV Hepatitis B Virus
HCV Hepatitis C Virus
HEV Hepatitis E Virus
HIV Human Immunodeficiency Virus
HLA Human Leucocyte Antigen
HLAi HLA Antibody Incompatible
HTA Human Tissue Authority
HTLV Human T Lymphotrophic Virus
HUS Haemolytic Uraemic Syndrome
IA Independent Assessor
IFG Impaired Fasting Glucose
KDIGO Kidney Disease: Improving Global Outcomes
LD Living Donor
LDC Living Donor Co-ordinator
LDKMR Living Donor Kidney Matching Run
LDKT Living Donor Kidney Transplantation
MCGN Mesangiocapillary Glomerulonephritis
MDT Multi-Disciplinary Team
mGFR Measured Glomerular Filtration Rate
METS Metabolic Equivalents
MDS Myelodysplastic Syndrome
MGUS Monoclonal Gammopathy of Uncertain Significance
NDAD Non-Directed Altruistic Donor
NHSBT NHS Blood and Transplant
NICE National Institute for Health and Care Excellence
NTNT Non-Transfusion Dependent Thalassaemia
ODT Directorate of Organ Donation and Transplantation
OGTT Oral Glucose Tolerance Test
PANVH Persistent Asymptomatic Non-Visible Haematuria
PCR Protein: Creatinine Ratio
PNVH Persistent Non-Visible Haematuria
PPD Paired/Pooled Donation
RCC Renal Cell Carcinoma
SaBTO Advisory Committee on the Safety of Blood, Tissues and Organs
SCD Standard Criterion Donor
SCT Sickle Cell Trait
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
14
TBMN Thin Basement Membrane Nephropathy
UKLKSS UK Living Kidney Sharing Schemes
VTE Venous Thromboembolism
References
1. NHS Blood and Transplant. Annual report on living donor kidney transplantation.
Report for 2016/17. https://nhsbtdbe.blob.core.windows.net/umbraco-
assets-corp/5706/annual-report-on-living-donor-kidney-transplantation-
2016_17.pdf
2. British Transplantation Society / Renal Association. United Kingdom Guidelines
for Living Donor Kidney Transplantation, 2000.
3. British Transplantation Society / Renal Association. United Kingdom Guidelines
for Living Donor Kidney Transplantation, Second Edition, 2005.
4. British Transplantation Society / Renal Association. United Kingdom Guidelines
for Living Donor Kidney Transplantation, Third Edition, 2011.
http://www.bts.org.uk/transplantation/standards-and-guidelines/
5. Uhlig K, Macleod A, Craig J, et al. Grading evidence and recommendations for
clinical practice guidelines in nephrology. A position statement from Kidney
Disease: Improving Global Outcomes (KDIGO). Kidney Int 2006; 70: 2058-65.
6. Kidney Disease Improving Global Outcomes (KDIGO) Transplant Work Group:
KDIGO clinical practice guideline for the care of kidney transplant recipients. Am
J Transplant 2009; 9(S3): S1-S157.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
15
2 LEGAL FRAMEWORK
Recommendations
All transplants performed from living donors must comply with the
requirements of the primary legislation (Human Tissue Act 2004 and
Human Tissue (Scotland) Act 2006), which regulate transplantation and
organ donation across the United Kingdom. (Not graded)
All transplant centres performing living organ donation must be
licensed by the Human Tissue Authority in line with the requirements
of the European Union Organ Donation Directive which sets out the
minimum requirements for the Quality and Safety of Organs for
Transplantation. (Not graded)
Consent for the removal of organs from living donors, for the purposes
of transplantation, must comply with the requirements of the Human
Tissue Act 2004, and the Mental Capacity Act 2005 in England and
Wales, and the Mental Capacity Act 2016 in Northern Ireland. Consent
in Scotland must comply with the Human Tissue (Scotland) Act 2006
and the Adults with Incapacity (Scotland) Act 2000. (Not graded)
The Human Tissue Act 2004 is the primary legislation regulating transplantation in
England, Wales and Northern Ireland (1). Separate legislation, the Human Tissue
(Scotland) Act 2006, applies in Scotland (2).
2.1 The Human Tissue Act 2004
The Human Tissue Act (2004) sets out the licensing and legal framework for the
storage and use of human organs and tissue (excluding gametes and embryos) from
the living and for the removal, storage and use of human organs and tissue from the
deceased. It permits authorised activities to be carried out for certain scheduled
purposes. The Act covers seven scheduled purposes requiring general consent, one
of which is transplantation, and this incorporates living donor transplantation (3).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
16
Authorised activities, including transplantation, are only lawful if done with
‘appropriate consent’ (4). Unauthorised dealings may result in offences, which carry
penalties (5). The Human Tissue Authority (HTA) issues Codes of practice
applicable to those working in England, Wales and Northern Ireland, which establish
guidelines for practice, particularly with regard to the meaning and extent of
‘appropriate consent’ (6,7).
2.2 The Human Tissue Authority (HTA)
The Human Tissue Authority (HTA) was established as the regulatory body under
the Human Tissue Act 2004 (8). The HTA regulates the removal, storage, and use
of human bodies, organs and tissue from the deceased and the storage and use of
human organs and tissue (excluding gametes and embryos) from the living (9,10).
The HTA is responsible for assessing all applications for organ donation from living
people. This involves an independent assessment process. All donors and
recipients see an Independent Assessor (IA) who is trained and accredited by the
HTA and acts on behalf of the HTA to ensure that the donor has given valid consent,
without duress or coercion, and that reward is not a factor in the donation. If the HTA
is satisfied on these matters then approval for the living donation will be given. Clear
guidance about the roles and responsibilities of the transplant team and
Independent Assessors in the context of living donation is published and regularly
updated by the HTA (11).
2.3 The European Union Organ Donation Directive
The European Union Organ Donation Directive (EUODD) came into effect in August
2012 (12). The EUODD was implemented to standardise systems and processes
across all member states to improve the quality and safety of human organs
intended for transplantation. It is the first pan-European regulatory framework
governing the donation and transplantation of organs from the living and deceased
and includes common standards for the procurement, transportation, traceability,
characterisation and follow-up of living donors across the EU.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
17
The HTA is the Competent Authority for the UK under the EUODD. Every
transplanting hospital is licensed by the HTA to perform specified activities related
to the donation and/or implantation of a donated organ (13).
2.4 Consent for the Removal of Organs from Living Donors
Seeking consent for the removal of organs from living donors, for the purposes of
transplantation, is the responsibility of the treating clinician. Part of the HTA’s
statutory assessment process is to ensure that the donor has given valid consent
(14). The common law, the Mental Capacity Act 2005, and the Mental Capacity Act
(Northern Ireland) 2016 also apply for minors and those who lack capacity to give
valid consent (15,16).
Following the UK Supreme Court judgment in Montgomery v Lanarkshire Health
Board [2015] (17), the HTA revised its guidance on valid consent in living organ
donation. The clinician responsible for the living donor is required to give the HTA
explicit assurance that the person intending to donate understands both the generic
and specific material risks of donation. This includes information about generic risks
to which a) any reasonable person or all donors would attach significance, as well
as b) information about individual risks to which the person consenting to donation
is likely to attach significance (e.g. a clinical reason such as pre-existing
hypertension or a non-clinical consideration such as a lifestyle or occupational
hazard that is specific to the donor) (see also Chapter 4).
2.5 Types of Living Donation Permitted by the Legislation
In September 2012, the HTA published a revised legal framework, which specifies
the types of relationships that are permitted between the living donor and recipient
under the Human Tissue Acts (11,14).
1. Directed donation
Also known as ‘specified donation’ in EU member states, a form of donation
where a healthy person donates an organ or part of an organ to a specific

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
18
recipient with whom they have a genetic or pre-existing emotional relationship.
This includes:
(i) Genetically related donation: where the potential donor is a blood relative
of the potential recipient;
(ii) Emotionally related donation: where the potential donor has a relationship
with the potential recipient; for example, spouse, partner, or close friend;
2. Paired or pool donation
A form of living donation where donor-recipient pairs are involved in a linked
‘exchange’. A healthy person, donor ‘A’, from one donor-recipient pair donates
an organ to recipient ‘B’ in another pair, whose donor then donates to recipient A
in a reciprocal arrangement. The donors are not genetically related or known to
their respective recipients. ‘Paired donations’ involve two pairs in an exchange
and ‘pooled donations’ include a series of paired donations, each of which is
linked to another in the same series (see Chapter 8).
3. Non-directed altruistic donation
Also known as ‘unspecified donation’ in EU member states, a form of living
donation whereby an organ or part of an organ is donated by a healthy person to
an unknown recipient, i.e. someone they have never met and who is not known
to them.
4. Directed altruistic donation
A form of living donation whereby an organ or part of an organ is donated by a
healthy person and contact between the donor and recipient has been made
because the recipient requires a transplant. Within the HTA framework, these
donors are categorised as follows:
(i) Genetic relationship and no established emotional relationship (e.g. donors
who have not seen their relative for many years; relative with whom there
has been no contact previously)
(ii) No pre-existing relationship between donor and recipient before the
identification of the recipient’s need for a transplant (e.g. contact through
social networking or media campaigns)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
19
2.6 Requirements for Transplants Involving a Living Donor
Restrictions on living donor transplants and requirements for information about
transplant operations are set out in Part 2, sections 33 and 34 of the Human Tissue
Act 2004 respectively (18) and sections 9-14 of the Regulations (14). It is an offence
to remove or use an organ from the body of a living person for transplantation unless
the requirements of the Human Tissue Act 2004 and the Regulations are met.
The Regulations require that all living donations for organ transplantation must be
approved by the HTA before donation can take place and, before giving approval,
the HTA must be satisfied that:
1. No reward has been, or will be, given;
2. Consent to removal for the purpose of transplantation has been given (or
removal for that purpose is otherwise lawful);
3. An Independent Assessor (IA) has conducted separate interviews with the
donor (and if different from the donor, the person giving consent) and the
recipient (or the person acting on behalf of the recipient) and submitted a
report of their assessment to the HTA. With the exception of non-directed
altruistic donors (NDADs), a joint IA interview with donor and recipient is also
required by the HTA.
In cases of directed genetically or emotionally related donation, the HTA requires
that evidence of relationship is provided to confirm that the relationship between
donor and recipient is as stated. At the time of writing, the decision on whether a
transplant proceeds must be made by an HTA panel of at least three members in all
cases where there is perceived to be a higher regulatory risk. These include:
Paired and pooled donation
Non-directed altruistic living donation
Directed altruistic donation cases where the donor is non-resident in the UK
Certain directed donation cases where the donor has an economic
dependence on the recipient
If the organ donor is a child
If the organ donor is an adult who lacks capacity
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
20
The HTA provides an out-of-hours emergency telephone approval service via the
executive but this is rarely required in the case of LDKT and must only be used in
cases of directed donation where there is an urgent clinical need.
The HTA also requires the living donor to specify how they wish their donated organ
or part organ to be used should it not be possible to transplant it into the intended
recipient. The donor is asked to explicitly consent to one of the following options:
implantation into another recipient, re-implantation back into the donor, research, or
disposal of the organ. Typically, this consent is taken during discussion with the
surgeon and the donor’s wishes are recorded in the referral letter prior to the
independent assessment for the HTA.
2.7 Prohibition of Commercial Dealings in Human Material
Section 32 of the Human Tissue Act 2004 prohibits commercial dealings in human
material, including organs for transplantation (19). Unless designated by the HTA to
carry out such activity, a person is committing an offence if they:
1. Give, offer or receive any type of reward for the supply or offer of supply of
an organ or part of an organ;
2. Look for a person willing to supply an organ or part of an organ for reward;
3. Offer to supply an organ or part of an organ for reward;
4. Initiate or negotiate any arrangement involving the giving of a reward for the
supply of, or for an offer to supply, an organ or part of an organ for
transplantation;
5. Take part in the management or control of any type of group whose activities
consist of or include the initiation or negotiation of such arrangements;
6. Cause to be published or distributed, or knowingly publish or distribute, any
type of advertisement inviting people to supply, or offer to supply, an organ
or part of an organ for reward, or indicate that the advertiser is willing to
initiate or negotiate any such arrangements.
The following terms apply:
- ‘Transplantable material’ is defined in Part 3, sections 9 and 10 of the
regulations and includes living donor liver lobes for transplantation (20);
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
21
- ‘Relevant Material’ is material, other than gametes, which consists of or
includes human cells;
- ‘Advertisement’ includes any form of advertising for reward, whether to the
public generally, to any section of the public, or individually to selected
persons;
- ‘Reward’ means any description of financial or other material advantage.
In March 2015, the UK signed the Council of Europe Convention against Trafficking
in Human Organs (21). This provides the first internationally agreed legal definition
of trafficking in human organs, identifying the activities that ratifying States must
criminalise in their national laws. It also includes provisions to deter these practices
and to protect victims.
2.8 Reimbursement of Expenses
The Human Tissue Act 2004 (22) allows donors to receive reimbursement of
expenses, such as travel costs and loss of earnings, which are reasonably
attributable to and directly result from donation (see section 14.1).
2.9 Exceptional Circumstances
2.9.1 Children
The Human Tissue Act 2004 defines a child as a person under 18 years old (22). In
England and Wales the legal position regarding consent by minors (under the age
of 18 years) to medical treatment is determined in case law by ‘Gillick’ (23). It could
be argued that organ donation is not, prima facie, in the best interests of the minor
as a potential donor, nor is it therapeutic treatment. However, if the young person is
‘Gillick competent’ (understands fully what is proposed and is capable of making a
choice in his/her best interests) in principle, he or she may be able to consent to
donation. However, children should only be considered as living organ donors in
exceptionally rare circumstances. As a minimum, good practice demands that
parental consent is always obtained and, even if there is parental consent to
donation, that an advanced ruling be sought from the Court before proceeding. The
use of a living organ from a child can only proceed with Court approval followed by
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
22
approval from an HTA panel (22). In Scotland, living donation of solid organs from
children is not permitted under the Human Tissue (Scotland) Act 2006 (see 3.10)
2.9.2 Adults without Mental Capacity
In England, Wales and Northern Ireland, the removal of an organ or part organ from
an adult who lacks the capacity to consent to such a procedure requires court
approval (14). Following court approval donation may then only proceed if the case
is approved by an HTA panel. In Scotland, living donation from adults without mental
capacity is not permitted under the Human Tissue (Scotland) Act 2006 (see 3.10)
2.10 The Human Tissue (Scotland) Act 2006
The purpose of the 2006 Act (2) is to make provision for activities involving human
tissue in the context of transplantation, research and education, its removal,
retention and use following post-mortem examinations, and for the purposes of the
Anatomy Act (1984), which is incorporated into the 2006 Act. Provisions of the
Human Tissue (Scotland) Act are based on ‘authorisation’ (24) rather than
‘appropriate consent’ as in the Human Tissue Act 2004 (3), but the principles in each
Act are essentially the same.
The 2006 Act stipulates that the removal and use of organs, parts of organs or tissue
from the body of a living person for use in transplantation constitutes an offence
unless certain conditions are satisfied, including that the donor must give consent,
without coercion or reward, for the removal of organs to take place. Restrictions on
transplants involving living donors are set out in section 17 of the 2006 Act (25).
These provisions are supplemented by the Human Organ and Tissue Live
Transplants (Scotland) Regulations 2006 (the Scottish Live Transplants
Regulations) (26) Prohibitions of commercial dealings in parts of a human body for
transplantation are set out in section 20 of the 2006 Act (27).
Under arrangements made between the Scottish Executive and the HTA, potential
living donors are assessed by the HTA to ensure that there is no evidence of
coercion or financial reward, as in other UK countries. The 2006 Act also permits
kidney paired exchange programmes and altruistic donation.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
23
Exceptional Circumstances
Under Scottish legislation children are defined as persons who have not yet reached
the age of 16 years. The principle of competency of children under 16 years to
consent to procedures is incorporated into Age of Legal Capacity Act (Scotland)
1991 (28) which states that ‘A person under the age of 16 years shall have legal
capacity to consent on his own behalf to any surgical, medical or dental procedure
or treatment where, in the opinion of a qualified medical practitioner attending him,
he is capable of understanding the nature and possible consequences of the
procedure or treatment’. The Children (Scotland) Act 1995 endorsed this principle.
The Adults with Incapacity (Scotland) Act 2000 governs adults without capacity to
make their own decisions in Scotland (29).
The Human Tissue (Scotland) Act 2006 prohibits the donation of non-regenerative
tissue such as kidneys and liver lobes by minors (under 16 years of age) and adults
lacking capacity (30).
References
1. Human Tissue Act 2004.
www.opsi.gov.uk/acts/acts2004/ukpga_20040030_en_1
2. The Human Tissue (Scotland) Act 2006.
www.opsi.gov.uk/legislation/scotland/acts2006/asp_20060004_en_1
3. The Human Tissue Act 2004. Part 1 of Schedule 1 of the 2004 Act.
http://www.opsi.gov.uk/acts/acts2004/40030--e.htm#sch1
4. Human Tissue Act 2004, section 3.
5. Human Tissue Act 2004, section 5.
6. Human Tissue Act 2004, section 26.
7. Human Tissue Authority Codes of Practice on Donation of Solid Organs and
Tissue www.hta.gov.uk/sites/default/files/files/HTA%20Code%20F_0.pdf
8. Human Tissue Act 2004, Part 2, sections 13-15.
9. The Human Tissue Authority. www.hta.gov.uk
10. The Human Fertilisation and Embryology Authority www.hfea.gov.uk.
11. Guidance for Transplant Teams and Independent Assessors (including
Scotland) www.hta.gov.uk/regulated-sectors/living-donation-approvals
12. Directive 2010/45/EU of the European Parliament and of the Council of 7 July
2010. www.hta.gov.uk/_db/_documents/EUODD_Directive_August_2011.pdf
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
24
13. Organ Donation Directive - The Human Tissue
Authority.http://www.hta.gov.uk/organdonationdirective.cfm
14. Human Tissue Act 2004 (Persons who Lack Capacity to Consent and
Transplants) Regulations 2006. www.opsi.gov.uk/si/si2006/20061659.htm
15. Mental Capacity Act 2005.
www.opsi.gov.uk/acts/acts2005/ukpga_20050009_en_1
16. Mental Capacity Act 2016 www.legislation.gov.uk/nia/2016/18/enacted
17. Montgomery v Lanarkshire Health Board [2015] UKSC 11.
www.supremecourt.uk/decided--
cases/docs/UKSC_2013_0136_Judgment.ppdf
18. Human Tissue Act 2004 Part 2, section 33-34.
http://www.opsi.gov.uk/acts/acts2004/ukpga_20040030_en_4#pt2-pb5-l1g32
19. Human Tissue Act 2004 Part 32.
www.opsi.gov.uk/acts/acts2004/ukpga_20040030_en_4#pt2-pb6
20. Human Tissue Act 2004 Part 3, section 54.
www.opsi.gov.uk/acts/acts2004/ukpga_20040030_en_5#pt3-pb2-l1g54
21. www.declarationofistanbul.org/resources/recommended-reading/the-council-
of-europe-convention-against-trafficking-in-human-organs.
22. Human Tissue Act 2004 Part 2.
http://www.opsi.gov.uk/acts/acts2004/ukpga_20040030_en_4#pt2-pb5-
23. Gillick v West Norfolk & Wisbech Area Health Authority and Department of
Health & Social Security (1985).
24. The Human Tissue (Scotland) Act 2006, sections 6-10
www.opsi.gov.uk/legislation/scotland/acts2006/asp_20060004_en_2#pt1-pb2-
l1g6
25. The Human Tissue (Scotland) Act 2006, section 17.
www.opsi.gov.uk/legislation/scotland/acts2006/asp_20060004_en_3#pt1-pb3
26. Human Organ and Tissue Live Transplants (Scotland) Regulations 2006 (the
Scottish Live Transplants Regulations).
www.oqps.gov.uk/legislation/ssi/ssi2006/ssi_20060390_en_1
27. The Human Tissue (Scotland) Act 2006, section 20.
www.opsi.gov.uk/legislation/scotland/acts2006/asp_20060004_en_3#pt1-pb5-
l1g20
28. Age of Legal Capacity Act (Scotland) 1991.
http://www.legislation.gov.uk/ukpga/1991/50/contents
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
26
3 ETHICS
Recommendations
All health professionals involved in living donor kidney transplantation
must acknowledge the wide range of complex moral issues in this field
and ensure that good ethical practice consistently underpins clinical
practice. The BTS has an Ethics Committee to provide additional
support and advice if required. (Not graded)
Regardless of potential recipient benefit, the safety and welfare of the
potential living donor must always take precedence over the needs of
the potential transplant recipient. (Not graded)
Independence is recommended between the clinicians responsible for
the assessment and preparation of the donor and the recipient, in
addition to the Independent Assessor for the Human Tissue Authority.
(Not graded)
3.1 Ethics
Living donor transplantation has become a well-established practice in the UK,
contributing more than a third of all organ transplants, of which 97% are LDKT. (1).
By its nature, living donor organ transplantation raises a wide range of complex
ethical issues. As transplant programmes continue to expand, all health
professionals involved in living donor transplantation must be familiar with the
general principles that underpin and are applicable to good ethical practice (2-7).
3.2 Key Ethical Principles in Living Donor Transplantation
Altruism has been the basis of organ donation in the UK from the outset and is
understood as a selfless gift to others without expectation of remuneration (8).
Altruistic giving may be to strangers or take place within the context of family or other
relationships. Altruism reinforces the philosophy of voluntary and unpaid donation
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
27
and solidarity between donor and recipient. There are some concerns that altruism
may be compromised by hidden coercive pressures: for example, the expectation
that a family member will donate an organ to help another family member in need of
a transplant (9). These pressures may be exacerbated if there is a sense of urgency
to transplant a recipient who, for example, is deteriorating rapidly.
Autonomy is the right of an individual to self-determination. Autonomy underpins
our entitlement to control our own body, because it is ‘ours’. Valid consent must be
given by the living donor before an organ can be removed; a primary aim is that
such decisions are freely and autonomously made to offset concerns about coercion
and ‘undue inducement’ that undermine valid consent.
Beneficence refers to actions that promote the wellbeing of others. In medicine this
means taking actions that serve the best interests of patients.
Dignity is often associated with the Kantian concept of the inherent dignity or special
status of the human body where dignity and price are mutually incompatible: the
maintenance of human dignity requires human beings to be beyond negotiable price
(10). Thus, any form of financial payment or ‘commodification’ of bodies or body
parts violates human dignity, even if the person concerned does not feel in any way
degraded. The opposing view is that degradation is dependent upon each person’s
own perception of what is degrading (11).
Non-maleficence is the principle of ‘doing no harm’ and it is based on the
Hippocratic Oath maxim ‘abstain from doing harm’.
Reciprocity refers to providing benefits or services to another as part of a mutual
exchange. For example, reciprocity underpins paired/pooled LDKT in which
donor/recipient ‘pairs’ enter into a reciprocal arrangement with each other, and also
domino donation in which an organ or part of an organ from a living donor may be
donated for the benefit of another as part of a therapeutic procedure for the donor.
3.3 The Recipient Perspective
The rationale for LDKT and the risk versus benefit to the recipient are detailed
elsewhere in these guidelines. In terms of outcome, a living donor kidney transplant
would almost always be the preferred option, with better transplant and patient
survival than for deceased donation. The added recipient benefits include the option
for planned pre-emptive transplantation and more opportunities for a successful
transplant through the UK living kidney sharing schemes (UKLKSS) and antibody
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
28
incompatible transplantation (AIT) programmes (see Chapter 8: Expanding the
Donor Pool). For children, living donation offers a unique opportunity for early
transplantation and to minimise disruption to growth, development and school.
Regardless of recipient benefit, living donation can only be justified if the interests
of the donor are given primacy. The safety and welfare of the potential living donor
must always take precedence over the needs of the potential transplant recipient.
3.4 The Donor Perspective
Donating a kidney involves a detailed process of investigation, major surgery, and
a significant period of recovery. Whilst there are documented overall benefits for the
individual donor and wider society, living donor surgery entails risk, which includes
a small risk of death (see Chapter 6). In addition, removal of a kidney will inevitably
cause physical harm to the donor and the potential life-long impact on health and
well-being must be fully considered for every individual. This conflicts with the
concept of non-maleficence and the maxim ‘first, do no harm’ and is often used as
an argument against living organ donation. However, other moral considerations,
such as individual autonomy, also contribute to an individual’s decision and
motivation to donate and despite the lack of physical benefit for donors, they often
describe a psychological gain in knowing that their gift has provided an opportunity
to transform the life of a relative, friend or stranger (12). It could be argued that a
potential living donor may be psychologically harmed if his/her donation, for
whatever reason, does not take place.
The principle of autonomy provides a legitimate basis for supporting living donation.
Living donor surgery is morally acceptable when carried out with ‘informed consent,
freely given’ but establishing ‘informed consent freely given’ can be problematic.
While all living donor programmes expect potential donors to be given an
appropriate, detailed description of the risks of donation, it is much less clear that all
such donors will listen. There is a well-described tendency for some people to decide
that they wish to donate at an early stage and then to be impervious to or oblivious
of any suggestion that they should make a more informed decision following
counselling (13). The consent may be real, but whether it is truly informed may be
questionable (see Chapter 4: Informing the Donor).

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
29
The only person who can know that consent is ‘freely given’ is the living donor. While
it may be possible to identify the donor who has come under overt pressure or
coercion, from either the recipient or from other family members, more subtle
pressures may not be revealed and/or remain undetected by health care
professionals. These may make it difficult or impossible for a potential donor not to
proceed through the assessment process.
It is important to recognise that the concept of ‘Informed consent, freely given’ will
vary according to the donor-recipient pair involved. In most situations, the motives
and autonomy of the donor will be beyond question but, in others, it can be more
difficult to establish that consent is both informed and voluntary. For this reason, a
multi-disciplinary team (MDT) approach is recommended in the assessment and
preparation of all donors and independence between the clinicians responsible for
the donor and the recipient is strongly recommended. Once the clinical assessment
is complete, the Independent Assessor for the Human Tissue Authority (see Chapter
2) provides an additional safeguard for the potential donor.
3.5 The Transplant Team Perspective
The collective transplant MDT is responsible for informing the potential donor of the
risks associated with living kidney donation. When the MDT has concerns about the
suitability of a potential donor and feels that proceeding with donation is
inappropriate, the team is under no obligation to proceed.
Members of the transplant team have individual rights as well as professional
responsibilities. If a fully informed potential living donor wishes to proceed with a
course of action that involves risks that go beyond that which individuals or the team
find acceptable or appropriate, they are under no obligation to proceed. Referral for
a second opinion may be appropriate in such circumstances (see section 5.2).
The transplant team has an obligation to utilise organs for transplantation to
maximise benefit for the whole patient pool. An area of controversy in living kidney
donation is when to remove patients from the national transplant list for a deceased
donor kidney if they have a potential donor/s undergoing assessment. The risks to
the individual recipient, the potential donor and the ‘greater good’ to the pool of
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
30
patients waiting for a kidney must be considered in coming to a decision. See
Chapter 4 for further discussion and recommendations.
3.6 Expanding the Living Donor Pool
The options for living donor kidney transplantation in the UK have expanded rapidly
over the years in line with technological advances, changes in the legal framework
and development of clinical practice. There are unique ethical considerations
associated with these developments, which are discussed in Chapter 8.
3.7 The Child or Young Person as a Living Donor
Minors (under the age of 18 years) should rarely, if ever, be considered as potential
living donors because of concerns about autonomy and the validity of consent from
young people in this situation.
In living donor kidney transplantation, some regard the use of an identical twin as
an acceptable child donor, on the basis that the outcome for the recipient twin is
exceptional and because the relationship between identical twins is so close that
restoring the health of the recipient confers major psychological benefit for the donor
(14). This view is highly controversial and has been challenged (15,16). The British
Medical Association has previously expressed the view that ‘it is not appropriate for
live, non-autonomous donors (minors) to donate non-regenerative tissue or organs’
(17). The most compelling argument for not using a child donor in this context is
their ability to fully understand the risks and give valid consent to donation.
3.8 The British Transplantation Society (BTS) Ethics Committee
The BTS Ethics Committee is a subcommittee of the BTS Council. Healthcare
professionals responsible for living donor organ transplantation are encouraged to
contact the Chairman of the BTS ethics subcommittee (via [email protected]k) if they
would like help or advice relating to ethical aspects of a particular living donor
recipient pair.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
31
References
1. NHS Blood and Transplant, Annual Activity Report, 2015/16. www.odt.nhs.uk
2. Price D. Human tissue in transplantation and research: a model legal and
ethical donation framework. Cambridge University Press, 2009.
3. Price D. Legal and ethical aspects of organ transplantation. Cambridge
University Press, 2000.
4. Plant WD, Akyol MA, Rudge CJ. The ethical dimension to organ transplantation
in transplantation surgery (2
nd
Edn). Ed Forsythe JLR. WB Saunders London,
2002.
5. Ross LF, Glannon W, Josephson MA. Should all living donors be treated
equally? Transplantation 2002; 74: 418-21.
6. Kahn J, Matas AJ. What’s special about the ethics of living donors?
Transplantation 2002; 74: 421-2.
7. Truog RD. The ethics of organ donation by living donors. N Engl J Med 2005;
353: 444-6.
8. Titmuss RM. The gift relationship: from human blood to social policy. London:
Allen and Unwin, 1970.
9. Scheper-Hughes N. The tyranny of the gift: sacrificial violence in living donor
transplants. Am J Transplant 2007; 7: 507-11.
10. Cohen CB. Selling bits and pieces of humans to make babies: the gift of the
Magi revisited. J Med Philos 1999: 24; 288-306.
11. Daar AS. Paid organ donation - the grey basket concept. J Med Ethics 1988;
24: 365-8.
12. Clarke A, Michell A, Abraham C. Understanding donation experiences of
unspecified (altruistic) kidney donors. Br J Health Psychol 2013; 19: 393-408.
13. Russell S, Jacob RG. Living related organ donation: the donor’s dilemma.
Patient Educ Couns 1993; 21: 89-99.
14. WHO guiding principles on human cell, tissue and organ transplantation.
Transplantation 2010; 90: 229-33.
15. Curran WJ. Kidney transplantation in identical twin minors - justification is done
in Connecticut. N Engl J Med 1972; 287: 26-7.
16. Hollenburg NK. Altruism and coercion: should children serve as kidney donors?
N Engl J Med 1977; 296: 390-1.
17. Medical ethics today: its practice and philosophy. London: BMJ Books, 1998.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
32
4 SUPPORTING AND INFORMING THE POTENTIAL DONOR
Recommendations
The living donor must be offered the best possible environment for
making a voluntary and informed choice about donation. The
transplant team must provide generic information that is relevant to all
donors as well as specific information that is material to the person
intending to donate. This includes information about the assessment
process and the benefits and risks of donation to the individual donor.
(B1)
Independent assessment of the donor and recipient is required by
primary legislation (Human Tissue Act 2004). (Not graded)
To achieve the best outcome for donor, recipient and transplant, the
boundaries of confidentiality must be specified and discussed at the
outset. Relevant information about the recipient can only be shared
with the donor if the recipient has given consent and vice versa. Both
the recipient and donor must be informed that it is necessary and usual
for all relevant clinical information to be shared across the transplant
team in order to optimise the chance of a successful outcome for the
transplant. (B1)
Ideally, the recipient will discuss relevant information with their donor,
or allow it to be shared. If the recipient is not willing to disclose
information, then the transplant team must decide whether it is
possible to communicate the risks and benefits of donating
adequately, without needing to disclose specific medical details. (Not
graded)
Separate clinical teams for donor and recipient are considered best
practice but healthcare professionals must work together to ensure
effective communication and co-ordination of the transplant process
without compromising the independence of either donor or recipient.
It is essential that an informed health professional who is not directly
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
33
involved with the care of the recipient acts as the donor advocate in
addressing any outstanding questions, anxieties or difficult issues,
and assists the donor in making a truly autonomous decision. (B1)
Support for the prospective donor, recipient and family is an integral
part of the donation/transplantation process. Psychological needs
must be identified at an early stage in the evaluation to ensure that
appropriate support and/or intervention is initiated. Access to
specialist psychiatric/psychological services must be available for
donors/recipients requiring referral. (B1)
4.1 Confidentiality
Both the donor and recipient have a right to a confidential relationship with their
respective clinicians. Clinical teams have a duty to respect that right. Highlighting
this aspect of LDKT is of particular importance because the uniqueness of the donor-
recipient scenario creates a novel proximity between all parties involved and can
generate ethical challenges and uncertainty (1-3).
It is important that boundaries are made explicit from the outset and that there are
realistic expectations on both sides about what information can be shared and what
is confidential to each individual. It may be assumed that both parties have an equal
right to information about one another, but information can only be shared if the
respective party gives express consent. It is advisable to have this discussion at an
early stage to avoid any possible misunderstanding or breach of confidentiality and
to ensure that the wishes of both donor and recipient are known to each other and
to their respective clinical teams.
The same principles are applied to keeping and maintaining clinical records for
recipients and donors. A separate clinical record must be maintained for each party.
There are no grounds for amalgamating complete recipient and donor records or for
maintaining joint clinical documentation. Nor is it best practice to file copies of results
or correspondence relating to the potential donor in the potential recipient’s notes,
or vice versa.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
34
It is necessary for clinical teams to share information that is directly relevant to the
management or performance of the kidney transplant. Examples include HLA
mismatching/cross matching results, CMV/EBV status (for post-transplant
prophylaxis or monitoring) and recipient diagnosis (for consideration of
recurrent/hereditary disease that might impact on graft or patient survival). It is
accepted that essential information will be shared between clinical teams in the best
interests of both parties when it has a direct bearing on the outcome of the transplant
or donation (e.g. renal vasculature, renal function) and is material to the decision-
making process. Access to such information must be made available via the
transplant centre for the purposes of long-term follow-up.
Information regarding a donor’s identity and his or her genetic relationship with the
potential recipient may become available during the living donor work-up process.
There may be occasions when this information, quite unexpectedly, identifies that a
genetic relationship has been misattributed. The potential personal, social and
cultural implications of this for both donor and recipient may be devastating and the
effects of receiving such information should not be underestimated. Donors and
recipients may or may not wish to be informed. Both donor and recipient must be
informed about the possibility of this before the work-up is started. It may be helpful
to seek their views on disclosure of information that is not directly relevant to
transplantation at that point. Particular care is required to ensure that material is not
inadvertently shared in such circumstances (see section 4.4).
If a potential donor wishes to withdraw from the transplant process at any time, the
primary responsibility of the donor assessment team is to support him/her to do so.
4.2 Informing the Potential Donor
The General Medical Council (GMC) is explicit about the responsibility of registered
doctors when seeking informed consent (4). Central to the validity of the process is
the respect by the medical practitioner for the right of the individual to exercise
autonomy and the provision of information in the form that allows them to make an
informed decision (see Chapter 3: Ethics).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
35
4.3 Informed Consent for Living Kidney Donation
4.3.1 A Summary of Key Points to be Discussed with a Potential Donor
General points about process, consent and confidentiality:
1. For a living donor to give valid consent for donation, he/she must be properly
informed about the generic risks (for all donors) and any specific, individual
risks (for them) (see section 4.3.5 and Chapter 2).
2. Informed consent must be sought before progressing to each stage of the
pathway.
3. Information must be given about what will be shared amongst the transplant
team and the GP.
4. Information must be given about what will not be shared with the potential
recipient, unless explicit consent is given to do so.
5. It should be explained that the tests might throw up unexpected findings that
may or may not be relevant to donating a kidney. These findings might
include:
a. Information about the genetic relationship with the recipient.
b. Medical or anatomical findings of uncertain significance that might
require further assessment or referral to another specialty.
6. It should be emphasised that the donor can withdraw from the process at
any time up until the time of surgery.
Specific points about process and possible outcomes:
1. Risks of donation (generic and specific).
2. Nature of surgical procedure and length of stay in hospital.
3. Potential graft loss in the recipient.
4. Requirement for HTA assessment.
5. Reimbursement of expenses.
6. Requirement for annual review.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
36
4.3.2 Understanding what is Involved
The need for valid consent for kidney donation must be explained to the potential
donor. An explanation of the concept of living kidney donation must be provided and
a clear definition of the donor assessment pathway. There is a significant
commitment involved in attending investigations and consultations and it is
important that the donor understands what is expected of them.
Submitting to a number of medical tests can generate uncertainty and anxiety. Even
when there are no concerns raised by the tests, the process may be stressful. There
is also a chance that tests will uncover an ‘incidental finding’. Although the finding
of significant pathology in potential donors is low, one study of 1597 potential donors
found that the incidence of proven malignancy discovered by CT scan was 0.1% (5).
The same study reported that the proportion of people having CT scans that
identified an ‘incidentaloma’ was 17% (5). In another study of 175 potential donors,
CT scan revealed a ‘potentially significant extra-renal finding’ in 28% (6).
Information about the process of kidney donation must also include an explanation
of proposed follow-up. Follow-up is recommended to ensure the safety of the
donor’s health and to facilitate data collection for monitoring outcomes via the
National Transplant Registry maintained by NHS Blood and Transplant. It is
important that potential donors are aware of the reasons and plans for follow-up
after donation (see Chapter 10).
Ideally, both verbal and written information about living kidney donation must be
provided.
4.3.3 Information about Likely Outcomes for the Kidney
Although the surgical risks associated with nephrectomy are independent of the
identity of the recipient, the likelihood of the transplant being successful may be
material to the donor’s decision to donate or not. Providing information about the
likelihood of success is an integral part of the consent process. The prospective
living donor must be given a realistic estimate of the likelihood of successful
transplant outcome. Factors that increase the risk of recipient mortality or morbidity
and/or graft survival require open discussion with the donor (e.g. pre-emptive
transplantation vs time on dialysis, recurrent disease, positive viral serology, age,
immunological complexity).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
37
It is only possible to provide the donor with specific information which is relevant to
the outcome of the transplant if the potential recipient agrees to such information
being shared. If the recipient is unwilling for this information to be shared, the
transplant team must decide whether this impinges on the ability of the donor to give
valid consent. There may be occasions where it is possible to communicate the risks
and benefits of donating without needing to disclose specific medical details. There
may, on the other hand, be occasions when the medical team feels that disclosure
of a specific diagnosis is essential. The team must be able to articulate clearly why
that is the case (7-9). It is then imperative that the recipient understands that
reluctance to disclose information directly impinges on the ability of a donor to give
valid consent, and that as a consequence it may not be possible to progress to
surgery.
Where there is insufficient evidence available to give comprehensive information
regarding the likelihood of successful transplantation, this fact must be shared so
that both donor and recipient have realistic expectations about possible outcomes
(see Chapter 11). These discussions with donor and recipient are best performed at
an early stage of assessment in separate consultations so that each has the
opportunity to speak openly and freely with health professionals and so that
expectations can be appropriately managed.
4.3.4 Independence of Decision
Valid consent for surgery must be informed and freely given and the clinician
responsible for obtaining consent must be satisfied that the prospective donor has
the ability to make a competent and cogent decision. As above, the potential donor
must be seen separately, in the absence of the prospective recipient and their family,
on at least one occasion during the donor assessment process and be assured that
their views concerning kidney donation, as well as their medical and social history
will be treated in strict confidence. It is imperative that language barriers do not get
in the way of this consultation (see section 4.6).
The potential donor must be provided with a balanced view of the advantages and
disadvantages of living donor transplantation. It should be made clear from the
outset that the potential donor may withdraw at any stage in the donation process
without having to provide an explanation for his or her decision. He or she must be
allowed adequate time to reflect on the decision to donate. If the donor decides not
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
38
to proceed, this decision must be respected and should not be regarded as a failure
but as a natural result of the education process. If additional emotional support is
required, this may be addressed within the transplant hub, the referring centre, or in
the primary care setting, and does not necessarily require referral to a mental health
professional. However, access to specialist psychologist or psychiatrist must be
available if necessary (see section 4.7).
If the prospective donor is unable to donate for a clinical reason, this can cause
distress for both donor and recipient and may be associated with negative feelings
of failure, anger or guilt, which could lead to depression or other negative
psychological outcomes. The need for emotional support must be anticipated and
adequately provided for in this situation (see section 4.7).
The decision regarding whether or not to proceed with living kidney donation can be
stressful for both donor and recipient, and their respective family and friends. If
several family members are contemplating donation, the decision-making process
as to which donor should proceed be may be complex. The healthcare team can
assist by identifying and addressing the relevant issues at an early stage so that all
parties can make a choice that is as fully informed as possible.
4.3.5 The Responsibility of the Donor Surgeon
The surgeon performing living donor nephrectomy has a particular responsibility
under his/her duty of care to ensure that the donor fully understands the potential
risks and long-term effects of the operation (4). It is recommended that a
combination of verbal and written information is given to the potential donor and that
the areas detailed in Chapter 6 of this document are specifically addressed. The risk
of death associated with living donor nephrectomy and the risks of short and long-
term complications must be fully explained. Following recent developments in case
law (Montgomery), the clinician responsible for the living donor is required to give
the HTA explicit assurance that the person intending to donate understands both
the generic and specific material risks of donation. This includes information about
generic risks to which any reasonable person or all donors would attach significance,
as well as information about individual risks to which the person consenting to
donation is likely to attach significance (10) (also see section 2.4).

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
39
4.4 Donor Identity
The significance of donor identity in the context of informed consent is the subject
of much debate. Information regarding a donor’s identity and their genetic
relationship with the potential recipient of their donation may become available
during the living donor transplant work-up. There may be occasions when this
information, quite unexpectedly, identifies that a genetic relationship has been
misattributed. For example, cases of misattributed paternity have come to light when
HLA typing has inadvertently disclosed the lack of genetic relationship between a
father and a child at an early stage in the assessment process. To date, there has
been no consistency in how such cases have been handled by healthcare
professionals in terms of disclosure to both parties (11-13). While cases of
misattributed paternity are most common, other unexpected findings may be
identified; for instance, sibling pairs and children born to young teenage mothers
who have been raised in the belief that another relative in the family is their mother.
The Human Tissue Authority (HTA) has previously issued guidance that encourages
transplant teams to take responsibility for informing the donor of this possibility
(i.e. that HLA typing may identify cases of misattributed genetic identity) and to seek
consent for or against disclosure of donor identity in the event that the HLA typing
does not support the claimed genetic relationship (14).
The above must not be confused with the role of the Independent Assessor who,
under the HTA Current Codes of Practice has a responsibility, with appropriate
evidence, to confirm the claimed relationship between donor and recipient (15). This
does not mean that the Independent Assessor is responsible for establishing that
claimed genetic relationships are real. It is the responsibility of the clinical teams to
establish such genetic relationships and to provide any relevant information to the
Independent Assessor in confidence, as part of the assessment process.
The principle of seeking donor consent before HLA testing is attractive as a risk
management strategy, particularly where there may be social and/or cultural
considerations, but it must also extend to the recipient as both parties are
inextricably linked in the context of living kidney donation. There is potential for
conflict within the relationship and within the wider family if the donor and recipient
make different decisions about disclosure, with the result that one is party to
information that the other is not. However, appropriate discussion with the recipient
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
40
and donor/s involved allows the underlying principle of valid consent to be upheld
provided that all parties understand the implications of testing and the advantages
and disadvantages of agreeing to consent for disclosure.
This is a difficult and controversial area because the relevance of genetic identity
may be questioned in the context of a loving relationship where the perceived
identity of the donor has never been at issue. There are also implications for the
wider family and the impact on family dynamics. There is no ‘one size fits all’ answer
and each case will need to be judged on its own merits. However, prior discussion
and consent are important to help minimise the assumptions being made about the
information that donors and recipients wish to know in the event of an issue arising.
One study has estimated that misattributed paternity will be found in approximately
0.25% to 0.5% of all living kidney donations (12). Given the high likelihood that
transplant centres will come across this issue from time to time, transplant teams
should determine in advance how they will approach a finding of misattributed
genetic identity.
4.5 Patient Advocacy
It has always been considered best practice for the potential donor to be given an
opportunity to meet separately with a party who is independent of the transplant
team and this is reflected in the UK legislative framework. To comply with the
Regulations and Codes of Practice of the HTA, every donor-recipient pair must be
assessed by an appropriately trained and accredited third party (the Independent
Assessor) (15) (see Chapter 2).
In addition to this, it is essential that an informed health professional who is not
directly involved with the care of the recipient acts as the donor advocate in
addressing any outstanding questions, anxieties or difficult issues, and assists the
donor in making a truly autonomous decision. Separation of the donor and recipient
clinical teams is also considered to be best practice, although it is recognised that
this may not be possible at all stages of the donor pathway, particularly around the
time of donation/transplantation.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
41
Transplant teams must be aware that potential donors might be subject to significant
pressure to donate, especially in cases where there is an expectation or sense of
obligation. Such examples include when a potential recipient is unsuitable for
inclusion on the deceased donor waiting list but the risk of a planned living donor
transplant is considered acceptable, or if someone is the only potential donor. When
a donor does not wish to donate but is concerned that refusal may result in family
conflict, the donor advocate can assist with discussions to limit damage to family
relationships (16).
If at all possible, it is preferable to encourage open and honest discussion between
the donor and recipient from the outset. Pre-emptive discussion is helpful in ensuring
that both parties are fully informed about how information will be handled by their
respective healthcare teams and to minimise the risk of future conflict. Multi-
disciplinary meetings are essential to ensure appropriate information is shared and
to facilitate the parallel management of both donor and recipient pathways and
underpin best practice. This is particularly pertinent when the donor and recipient
clinical teams are working independently of one another.
Not all recipients wish to accept living donation, but there is a tendency on the part
of healthcare professionals and/or family members to assume that they will.
Provided that their decision is an informed choice, it should be respected. In such
cases, the recipient may need support and guidance to refuse the offer without
causing the potential donor distress or relationship conflict. Where potential
recipients have formed good relationships within the transplant team, sufficient
support may be available but an independent third party offers a different dimension
and an environment in which there is potentially less pressure and more opportunity
for free expression concerning acceptance of the kidney. This is especially important
in the case of young adults (17).
While the outcome of LDKT, particularly pre-emptive transplantation, is superior to
that of deceased donor kidney transplantation (see Chapter 11), some recipients
may choose to remain on the national deceased donor transplant waiting list for
other reasons such as family, work and lifestyle considerations. If a potential
recipient has a living kidney donor who is healthy and keen to proceed to donation,
it is usually appropriate to recommend that the potential recipient is suspended from
the deceased donor transplant waiting list until living donation proceeds or the
potential donor is deemed unsuitable. The decision whether to remain on the waiting
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
42
list or not must be made jointly between the donor and recipient, and in discussion
with their clinical teams, so that the risks and benefits are clear. Ultimately, all
decisions of this nature are made on a case-by-case basis. However, it is usually
inappropriate for a patient to remain on the deceased donor waiting list once the
donor has been fully assessed and deemed suitable to proceed, unless there are
extremely strong competing arguments.
4.6 Independent Translators
There is a rich cultural and ethnic diversity within the UK and a high proportion of
donors for whom English is not their first language. Novel presentations of both
verbal and written information, even when translated, often do not help individual
donors to acquire the depth and breadth of knowledge they need to be an informed
kidney donor. This may mean that they are vulnerable to coercion. Independent
translators are a requirement under the HTA Codes of Practice (18) to ensure that
the interests of the potential donor are protected and, as a matter of best practice,
they must be used where there are difficulties in communicating freely with both
parties. The translator must be unknown to both the donor and recipient and
competent to discuss the implications and associated risks of donor nephrectomy
and the post-operative recovery process. The translator must have sufficient
knowledge and skill to accurately translate complex discussions and to understand
the nature and subtlety of the conversation in order for the donor to make the right
decision. In the absence of face-to-face translation, telephone translation can be
helpful.
4.7 Psychological Issues
Psychological problems are infrequent after donation and most donors experience
increased self-esteem, whilst donor and recipient relationships are enhanced. The
majority of donors express no regrets after donation (19,20). However, it is essential
to identify pre-existing or potential mental health issues that might arise for the
prospective donor, to ensure that these are appropriately addressed. An opportunity
to explore any concerns in confidence must be offered as an integral part of the
assessment process, including aspects related to the donor assessment process,
family relationships and decision-making. The purpose of such an assessment is to
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
43
identify the level of support or intervention that may be required so that appropriate
arrangements can be made, including referral to a mental health professional if
necessary. A full psychological or psychiatric assessment is recommended if there
is concern about the suitability of a donor on mental health grounds; for example, if
there is evidence of previous or current mental illness, active substance abuse,
dependence on prescribed medication, self-harming behaviour, or significantly
dysfunctional family relationships, particularly between recipient and donor. Such an
assessment is valuable in establishing when it is unsuitable to proceed to donation
on these grounds (21). The EPAT tool provides a structured approach to initial
psychosocial assessment, which can be performed by any member of the multi-
disciplinary team and could help to identify potential areas of concern (22).
Psychological support for the donor may be provided by a variety of healthcare
professionals who have the necessary knowledge and skills to deal with a range of
psychological and social needs. Most transplant centres have designated personnel
(usually a transplant co-ordinator or nurse specialist) who play a key role in
organising the assessment and surgery for donor and/or recipient. Such individuals
often become closely acquainted with the donor and their families and may be best
placed to provide the necessary support, even in the context of adverse events
before or following transplantation. Other centres have dedicated social workers,
counsellors, psychologists and psychiatrists, or access to such colleagues, to whom
patients can be referred for specialist intervention and additional support.
The development of peer support/patient befriending programmes whereby patients
who have experienced living donor transplantation offer support and guidance to
donors and recipients who are considering this option, has also become an
established and effective part of clinical practice in some centres, providing a
complementary approach to that of healthcare professionals (23).
Although not mandated by the HTA, formal mental health assessment for all non-
directed altruistic donors is recommended best practice (24) (see Chapter 8).
Not all genetically and/or emotionally related donors and recipients will require
referral to a mental health professional but a clear, stratified framework for
psychological care must be in place to ensure that needs are accurately identified
and appropriately met and that there is access to a range of specialist services for
patients who may need to be referred. A ‘tiered approach’ to delivering support and
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
44
psychological services is an appropriate model in the context of living kidney
donation (25).
There is some evidence that, by merely presenting the option of living donation, the
potential donor is immediately placed under an unwarranted moral burden and may
feel in a ‘no win’ situation (26). While this may be true for some people and it may
not be possible for the donor to avoid these pressures completely, a supportive
environment that encourages discussion can relieve the strain and facilitate
decision-making.
Sibling decision-making has been reported as one of the most complex areas (23).
Motivational factors such as altruism, manipulation of familial relationships, coercion
and covert pressure are reported (see Chapter 3). Donor advocacy is essential in
these situations to ensure that donors feel supported to make the right decision for
them (see section 4.5).
Donors and recipients need to be made aware that psychological problems have
been reported after donation (27). These usually focus around the gift exchange
elements of donation: recipients suffer psychological distress from feelings of
indebtedness, which they can never repay; and donors exhibit proprietary interest
in the health, work and private life of the recipient that can damage relationships.
Discussion is recommended before surgery to pre-empt difficulties that might arise
at a later date. In terms of psychological care, the impact of living donor
transplantation for donor and recipient must be considered within the context of the
wider family network to ensure effective support and intervention.
After donation, kidney donors generally consider that organ donation was a positive
experience and regret about having donated is low (20,28). Although most donors
report a better quality of life after donation compared to the general population, a
small minority have experienced reduced quality of life, higher levels of fatigue and
relationship changes (29). These appear to be associated with a pre-donation higher
body mass index (BMI), smoking, and higher expectations regarding health
consequences. Depression and fatigue after donation may be more prevalent in
females (28). Potential donors must be made aware of these possible outcomes and
must be followed up appropriately if they arise after donation.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
45
4.8 Death and Transplant Failure
LDKT is increasingly considered the treatment of choice for recipients with higher
baseline comorbidity. An increased risk of post-operative co-morbidity, transplant
failure and death is likely and the appropriate management of expectations is an
essential part of the pre-transplant preparation for all parties concerned.
Death is a rare complication of transplant surgery, but can occur (see Chapters 6 &
11). Bereavement support in these cases must be provided by qualified,
independent counsellors and continue in the community for as long as required.
Early graft failure is likely to result in feelings of profound loss for many donors and
recipients. Emotional support must be accessible to all patients and their families,
up to and including referral to a mental health professional.
References
1. Tong A, Chapman JR, Wong G, Craig JC. Living kidney donor assessment:
challenges, uncertainties and controversies among transplant nephrologists
and surgeons. Am J Transplant 2013; 13: 2912-23.
2. Reese PP, Boudville N, Garg AX. Living kidney donation: outcomes, ethics, and
uncertainty. Lancet 2015; 385: 2003-13.
3. Elias R, Iqbal R. Ethics of transplantation in Handbook of Kidney and Pancreas
Transplantation. MacPhee and Fronek eds. Wiley-Blackwell 2012: 447-59.
4. General Medical Council. Consent: patients and doctors making decisions,
2008.
www.gmc-uk.org/guidance/ethical_guidance/consent_guidance_index.asp
5. Tan N, Charoensak A, Ajwichai K, et al. Prevalence of incidental findings on
abdominal computed tomography angiograms on prospective renal donors.
Transplantation 2015; 99: 1203-7.
6. Maizlin Z, Barnard SA, Gourlay WA, Brown JA. Economic and ethical impact of
extrarenal findings on potential living kidney donor assessment with computed
tomography angiography. Transpl Int 2007; 20: 338-42.
7. Elias R. Confidentiality and consent in living kidney transplantation: is it
essential for a donor to know that their recipient has HIV disease? Clin Ethics
2009; 4: 202-7.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
46
8. Rodrigue JR, Ladin K, Pavlakis M, Mandelbrot DA. Disclosing recipient
information to potential living donors: preferences of donors and recipients,
before and after surgery. Am J Transplant 2011; 11: 1270-8.
9. Hizo-Abes P, Young A, Reese PP, et al. Donor Nephrectomy Outcomes
Research (DONOR) Network. Attitudes to sharing personal health information
in living kidney donation. Clin J Am Soc Nephrol 2010; 5: 717-22.
10. Montgomery v Lanarkshire Health Board [2015] UKSC 11
www.supremecourt.uk/decidedcases/docs/UKSC_2013_0136_Judgment.pdf
11. Meadow J, Thistlethwaite JR Jr, Rodrigue JR, Mandelbrot DA, Ross LF. To tell
or not to tell: attitudes of transplant surgeons and transplant nephrologists
regarding the disclosure of recipient information to living kidney donors. J Clin
Trans Res 2015; 29: 1203-12.
12. Young A, Kim SJ, Gibney EM, et al. Donor Nephrectomy Outcomes Research
(DONOR) Network. Discovering misattributed paternity in living kidney
donation: prevalence, preference, and practice. Transplantation 2009; 87:
1429-35.
13. Schroder NM. The dilemma of unintentional discovery of misattributed paternity
in living kidney donors and recipients. Curr Opin Organ Transplant 2009; 14:
196-200.
14. Human Tissue Authority. Absence of presumed genetic relationship,
recommendation by letter, 21/06/2010 (n/a on website 13/08/10).
15. Human Tissue Authority. Code of Practice 2, Donation of solid organs for
transplantation, living organ donation version 14.0. Updated: July 2014
Scheduled review date: July 2016. www.hta.gov.uk
16. Jacobs C, Johnson E, Anderson K, Gillingham K, Matas A. Kidney transplants
from living donors: how donation affects family dynamics. Adv Renal Replace
Ther 1998; 5: 89-97.
17. Franklin P, Crombie A. Live related renal transplantation: psychological, social
and cultural issues. Transplantation 2003; 76: 1247-52.
18. Human Tissue Authority. Code of Practice 1, Consent, general provisions,
revised Sept 2009; 60-1.
19. Fehrman-Ekholm I, Brink B, Ericsson C, Elinder CG, Dunér F, Lundgren G.
Kidney donors don’t regret: follow-up of 370 donors in Stockholm since 1964.
Transplantation 2000; 69: 2067-71.
20. Maple H, Chilcot J, Burnapp L, et al. Motivations, outcomes, and characteristics
of unspecified (nondirected altruistic) kidney donors in the United Kingdom.
Transplantation 2014; 98: 1182-9.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
47
21. Potts SG. Transplant Psychiatry J R Coll Physicians Edinb 2009; 39: 331-6.
www.rcpe.ac.uk/sites/default/files/potts.pdf
22. Massey EK, Timmerman L, Ismail SY, et al. ELPAT Psychosocial Care for
Living Donors and Recipients Working Group; ELPAT living organ donor
psychosocial assessment tool (EPAT: from ‘what’ to ‘how’ of psychosocial
screening- a pilot study. Transplant Int 2017. doi: 10.1111/tri.13041
23. Benefits of peer support in people with chronic kidney disease.
https://www.kidney.org/sites/default/files/docs/02-10-
4196_ebb_benefitsprofessionalflyer.pdf
24. Human Tissue Authority. Guidance for transplant teams and Independent
Assessors, March 2015.
https://www.hta.gov.uk/sites/default/files/Guidance_to_Transplant_Teams_an
d_Independent_Assessors%20(1)_0.pdf
25. British Renal Society. The renal team: a multi-professional renal workforce plan
for adults and children with renal disease. Recommendation of the National
Renal Workforce Planning Group, 2002.
26. Russell S, Jacob R. Living-related organ donation: the donor’s dilemma. Patient
Educ Couns 1993; 21: 89-99.
27. Fox RC, Swazey JP. Spare parts. Oxford University Press, 1992.
28. Sommerer C, Feuerstein D, Dikow R, et al. Psychosocial and physical outcome
following kidney donation - a retrospective analysis. Transplant Int 2015; 28:
416-28.
29. de Groot IB, Stiggelbout AM, van der Boog PJM, Baranski AG, Marang-van de
Mheen PJ for the PARTNER-study group. Reduced quality of life in living kidney
donors: association with fatigue, societal participation and pre-donation
variables. Transplant Int 2012; 25: 967-75.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
48
5 DONOR EVALUATION
5.1 INTRODUCTION
The primary goal of the donor evaluation process is to ensure the suitability of the
donor and to minimise the risk of donation. This involves identifying
contraindications to donation and potential clinical (physical and psychosocial) risks.
To ensure that the evaluation is comprehensive, potential donors must be assessed
according to an agreed, evidence-based protocol which includes multi-disciplinary
input and discussion. Investigations must be undertaken in a logical sequence so
that the potential donor is protected from unnecessary, particularly invasive,
procedures until the appropriate stage of assessment. There is good agreement
about the recommended routine screening tests and supplementary investigations
that may be required to assess the suitability of an individual donor (1). Use of
evidence-based guidelines to ensure a consistent approach to the assessment and
preparation of living donors has become increasingly important as the criteria for
donor acceptance have extended and clarity about individual donor risk is
paramount (1,2).
The same best practice principles apply to the assessment and preparation of all
donors. Special consideration must be given to donors who are non-resident in the
UK, and plan to donate to an NHS-entitled recipient, as well as to donor-recipient
pairs who travel to the UK for the purposes of LDKT. These are discussed in more
detail in Chapter 9.
The timing of donor assessment will vary according to individual clinical
circumstances. In many cases, donor evaluation will only be undertaken once the
suitability of the potential recipient for transplantation has been established.
However, where the likelihood of recipient contraindications is low, it may be
appropriate to start the donor work-up in parallel to the recipient assessment to
maximise the chance of pre-emptive transplantation and avoid unnecessary delay.
It is important to respect the confidentiality of the donor and to maintain a clear
separation of the interests of the donor and recipient (see Chapter 4). This is best
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
49
achieved by ensuring that separate physicians and/or clinical teams assess the
donor and recipient before donation and transplantation.
Throughout the evaluation, good communication with the donor’s GP is
recommended to confirm past and present medical history and to reveal any
undisclosed issues that might influence the decision to donate. It is recommended
that non-UK resident donors who plan to donate to NHS-entitled recipients are
registered as temporary patients at the recipient’s GP practice for the duration of
their stay in the UK. Written consent is recommended from the donor before
disclosure of information or contact with his/her GP. If the donor has previously
donated (e.g. a lobe of liver), consent to contact the previous donating centre is also
recommended to confirm the outcome of the previous donation and any physical or
psychosocial issues relevant to subsequent donation (3).
There are no absolute rules about when a recipient should be suspended from the
active national deceased donor waiting list if they have a potential living donor under
assessment, and the approach taken will vary according to individual
circumstances. Plans are best made after discussion with the individual donor and
recipient, but the recipient benefit from receiving a living donor compared with a
deceased donor transplant must be made explicit. Another consideration is the
optimal management of the national waiting list, although this must never take
precedence over the potential recipient’s or donor’s best interests.
The evaluation of potential living donors is resource intensive and a proportion of
those who volunteer as donors will not be suitable to proceed for a variety of clinical
and non-clinical reasons. The earliest possible triage of unsuitable donors will help
to maximise benefit, minimise risk and manage expectations for donors, recipients
and their families. Strategies must also be in place to offer appropriate emotional
support and clinical follow-up for potential donors who are found to be unsuitable.
The option of a second opinion must always be available to donors and recipients.
A pathway to facilitate referral for a second opinion has been agreed by the LDKT
2020 strategy implementation group and is shown in Table 5.1.1.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
50
References
1. KDIGO Clinical Practice Guideline on the Evaluation and Care of Living Kidney
Donors. Transplantation 2017; 101: 8S-1.
http://kdigo.org/wp-content/uploads/2017/07/2017-KDIGO-LD-GL.pdf
2. (CD-P-TO), Council of Europe: Long-term outcome of living kidney donation
position paper of the European Committee on Organ Transplantation Transplant
International, 2015 Steunstichting ESOT 29 (2016) 129-31.
http://onlinelibrary.wiley.com
3. BTS/BASL UK Guidelines for Living Donor Liver Transplantation, 1st Edition,
July 2015.
https://bts.org.uk/wp-content/uploads/2016/09/03_BTS_LivingDonorLiver-1.pdf
4. Living Donor Kidney Transplantation 2020: a UK Strategy.
https://www.odt.nhs.uk/odt-structures-and-standards/key-strategies/living-
donor-transplantation-strategy-2020/

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
51
Table 5.1.1 Initiating a Second Opinion for a Living Donor or Recipient of a
Living Donor Kidney Transplant
Donor or recipient referred/self-
referred for assessment in a
referring nephrology unit
Donor or recipient referred/self-
referred for assessment in a
transplant centre
Donor and/or recipient
assessment stopped
Donor/recipient referred for 2
nd
opinion to
another transplant centre/s:
Consultant to consultant written referral
Copied to the living donor co-ordinators
in both centres and relevant MDT
members in referring team
If donor and/or recipient unsuitable, decision discussed:
1. At transplant multi-disciplinary meeting (in collaboration with the
transplant centre if referral originates in referring nephrology unit, according
to type of contraindication +/- donor/recipient preferences)
2. With donor and/or recipient and second opinion offered:
Routinely if categories 2 or 3 apply
Exceptionally if category 1 applies (depending upon type of
contraindication +/- donor/recipient preferences
Follow-up consultation +/-
management plan arranged
Donor and/or recipient may be considered unsuitable because they:
1. Have an absolute contraindication to donation/transplantation according to
UK Guidelines (i.e. general comorbidity or kidney specific issue)
2. Have a relative contraindication to donation/transplantation according to
UK Guidelines
3. Do not meet transplant centre-specific criteria for acceptance of referral
(e.g. age; comorbidity; complex anatomy; body mass index; immunological
risk)
Transplant centre/s for 2
nd
opinion may be:
Within/adjacent to the region (ease of
access for the donor/recipient)
Identified for specific knowledge or
expertise and willing to accept referrals
for 2
nd
opinions
2
nd
opinion decision relayed within 2-4 weeks of referral:
In writing to referring consultant, copied to the living donor co-ordinators and
relevant MDT members in both centres
Decisions maybe reviewed by the Chair +/- NHSBT Kidney Advisory Group
via the Chair on request
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
52
5.2 DONOR EVALUATION: SUMMARY
Recommendations
In cases of directed donation (to a known recipient) the likely suitability
of the potential recipient for transplantation must be established before
starting donor assessment. If additional recipient assessment is
required, unnecessary delay should be avoided. Non-invasive
assessment of the donor may be undertaken in this phase. (Not graded)
As far as possible, donor assessment is planned to minimise
inconvenience to him/her and to avoid unnecessary barriers to
proceeding. Flexibility in terms of timescales, planning consultations,
attending for investigations and date of surgery is helpful. (Not graded)
Donor assessment must be planned to ensure that it is focused, logical
and coherent. Good communication with the donor and involvement of
the wider multi-disciplinary team is essential and is achieved most
effectively if a designated co-ordinator leads the organisation of the
assessment process. The results of investigations must be relayed
accurately and efficiently to the potential donor. Unsuitable donors
must be identified at the earliest possible stage of assessment. (Not
graded)
A policy must be in place to manage prospective donors who are found
to be unsuitable to donate and appropriate follow-up and support must
be made available. (Not graded)
The organisational aspects for donor evaluation will vary between
centres, according to available resources and personnel, but the same
principles apply for all donors. An agreed donor assessment protocol
must be in place that is tailored to the needs of the individual. Table
5.2.1 shows a suggested best practice model with an audit standard for
donor evaluation. (Not graded)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
53
To facilitate pre-emptive transplantation, donor evaluation must start
sufficiently early to allow time for more than one donor to be assessed
if required. Information must be provided at an early stage and
discussion with potential donors and recipients will usually be started
when the recipient eGFR is approximately 20 mL/min or when the
recipient is expected to require renal replacement therapy within 12-18
months. Recipient and donor assessment can then be tailored
according to the rate of decline of recipient renal function, disease
specific considerations and individual circumstances. (B2)
The evaluation of a potential donor should be undertaken within an 18
week pathway, assuming there are no logistical issues such as donor
unavailability. There may, of course, be pauses if the recipient’s
transplant assessment is complicated or if the recipient’s renal
function remains satisfactory. A suggested timeline for donor work-up
is presented in Table 5.2.1
References
1. NHS England Service Specification, Adult Kidney Transplantation.
https://www.england.nhs.uk/wp-content/uploads/2017/05/service-spec-adult-
kidney-transplant-service.pdf
2. West Midlands Clinical Network and Clinical Senate. Transplant First end of
project report, September 2016. https://www.thinkkidneys.nhs.uk/kquip/wp-
content/uploads/sites/5/2017/04/End_of_Project_Report_-
_Transplant_First_v1.pdf
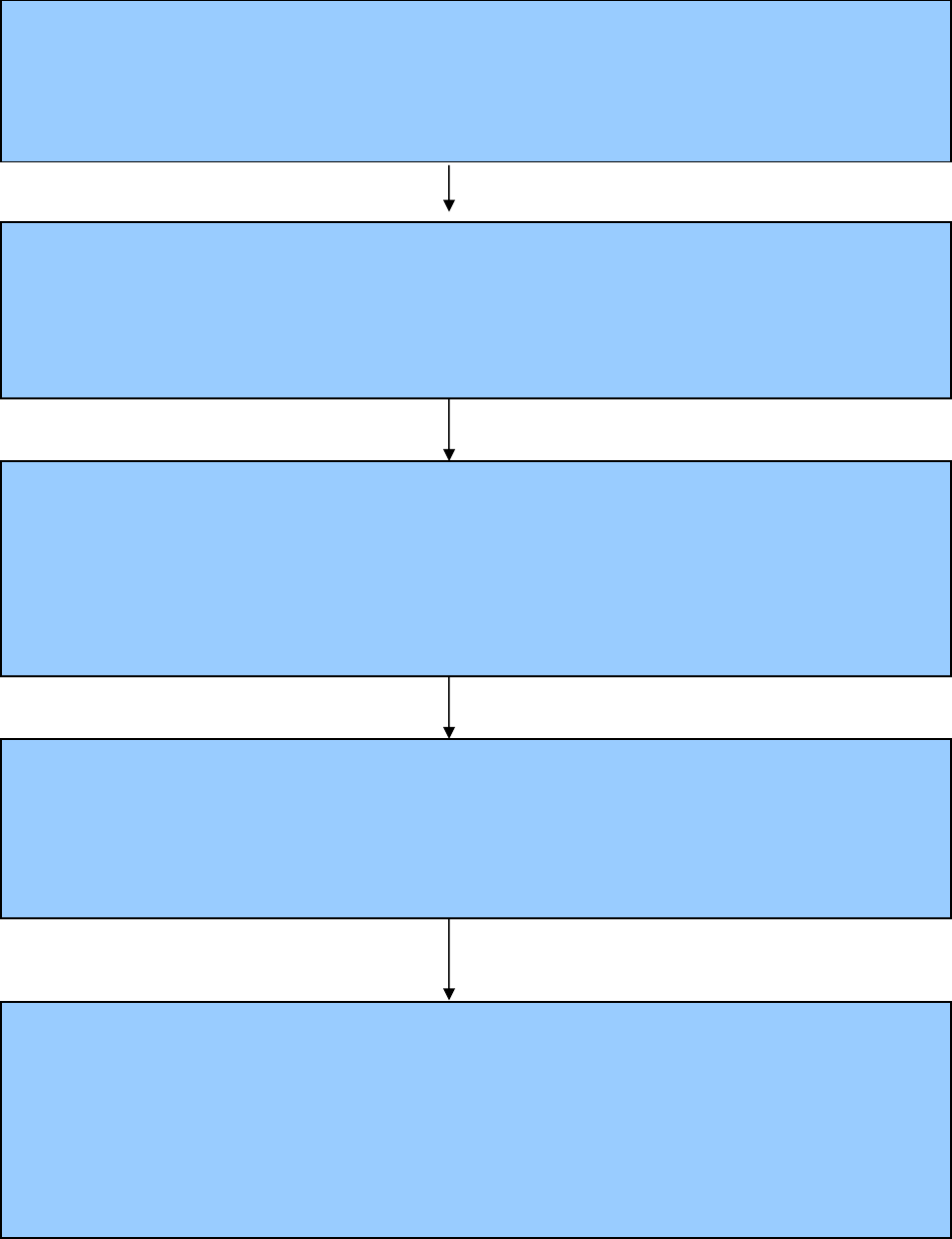
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
54
Table 5.2.1 Donor Evaluation: Summary and Organisational Chart
(directed donor-recipient pair)
Within 2-4 weeks of referral (4)*
Weeks 0-2
Weeks 2-4
Weeks 4-8
Early education & discussion with all potential transplant recipients +/- potential donors about
optimal options for transplantation.
RATIONALE: To promote planned, pre-emptive LD transplantation as the
treatment of choice for suitable transplant recipients
To minimise time on dialysis for suitable recipients
ABO compatibility +/- HLA sensitisation (if indicated) confirmed. Primary contra-indications
identified from donor(s) past and present medical history*. Routine blood & urinalysis tests.
* Donor screening questionnaire (Appendix 5.2) with telephone or face to face triage
RATIONALE: To initiate early triage of unsuitable donors
To identify potential incompatibility issues (ABO/HLA)
Donor evaluation is planned with the prospective donor, in a timely manner, to an agreed
protocol & in accordance with the availability of local resources. Emphasis should be placed
upon a coherent, Consultant-led service with a logical progression of assessment using ‘gold
standard’ investigations, multidisciplinary input & excellent communication between all parties.
A designated LD co-ordinator is considered optimal.
RATIONALE: To provide a clinically effective service based upon the best
evidence available & national best practice guidelines
Potential donor(s) identified.
LD co-ordinator facilitates initial discussion with potential donor(s) +/- recipient & other family
members as appropriate. If more than one potential donor, the most appropriate should be
identified, taking into account possible social, psychological and medical risk factors.
RATIONALE: To minimise evaluation of multiple donors & maximise best use of
resources
To ensure that the donor can give valid consent for donation
Establish recipient fit for transplantation & start appropriate pre-transplant assessment as per
local protocol [see section 5.1]
RATIONALE: To optimise management of recipient & donor expectation
To avoid unnecessary investigative assessment/inconvenience for the
prospective donor(s) if transplantation cannot proceed
To ensure that the recipient can give valid consent

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
55
Within 2 weeks of investigations (10)
Weeks 8-10
Weeks 11
Week 18
Results review by members of the MDT & feedback to the donor.
RATIONALE: To ensure continuity & keep the donor informed
Suitable donor & recipient pair referred for final pre-
operative discussion with Consultant Nephrologist and
Transplant Surgeon, & Independent Assessment for Human
Tissue Authority. Date of transplant or management plan via
the UKLKSS agreed
RATIONALE: To ensure transplant can legally
proceed & that both donor & recipient
can provide valid consent for surgery
Final cross match within the 7-10 days before Tx + routine
pre-op investigations/pre-admission visit*
RATIONALE: To ensure transplant can safely proceed*
* only applies to UKLKSS pairs once matched
OPERATION/ready to list in UKLKSS
LD co-ordinator maintains contact with donor & facilitates
life-long follow-up arrangements
RATIONALE: To provide continuing support to
the donor & inform the UK Living
Donor Registry
If donor unsuitable, follow-up
arranged.
RATIONALE:
To offer opportunity to discuss
results & arrange appropriate
follow up

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
56
APPENDIX 5.2 DONOR HEALTH QUESTIONNAIRE
PLEASE ANSWER ALL QUESTIONS
Name:
Date of birth:
Address:
E mail:
Telephone number:
Name of person requiring transplant (if known):
Date of birth:
Address:
Relationship to you (if any):
Have you ever been in hospital? Yes No
If yes, please give details
Have you had any operations? Yes No
If yes, please give details
Do you attend your GP regularly? Yes No
If yes, please give details
Are you on any regular medication? Yes No
If yes, please give details
Do you take:
The contraceptive pill Yes No
Hormone replacement therapy (HRT) Yes No
Aspirin Yes No
Do you have any allergies? Yes No
If yes, please give details
What is your height? _____
What is your weight? _____
Have you been diagnosed with any of the following?
High blood pressure Yes No
Diabetes Yes No
Angina / heart disease Yes No
Stroke Yes No
Kidney stones Yes No
Cancer Yes No
Blood clot Yes No
Bleeding from the bowel Yes No
Depression or mental health issues Yes No
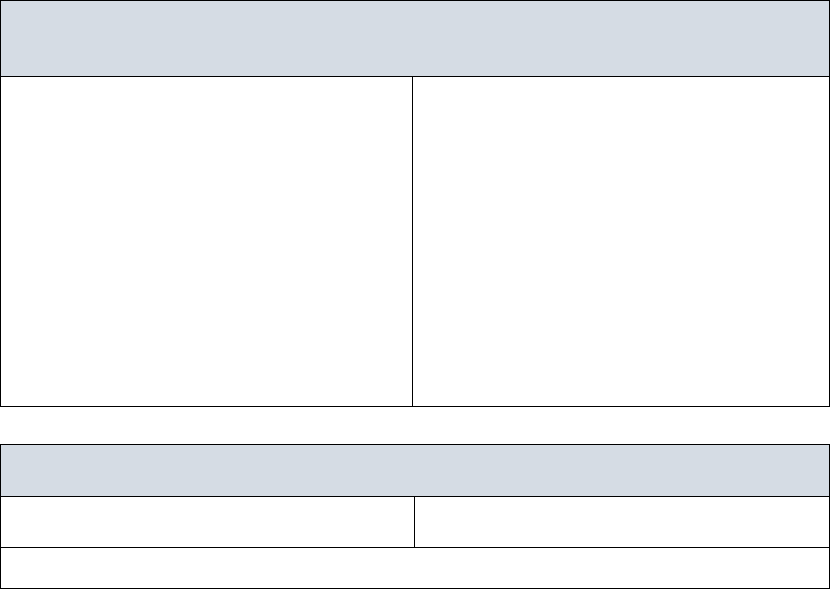
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
57
When was your last smear test (women only)? ------------
When was your last mammogram (women over 50)? ------------
Have you participated in the National Bowel Screening
Programme (over 60 years only)? ------------
Do you smoke? Yes No
Have you ever injected recreational drugs? Yes No
How many units of alcohol do you drink on average per week? ------------
Have you travelled outside Europe/North America
within the past 12 months? Yes No
Have any of your family members (close blood relatives) been diagnosed with?
Diabetes Yes No
Kidney failure Yes No
Cancer Yes No
Early onset heart disease/failure Yes No
Are you willing for us to contact your GP and
review your medical records if necessary? Yes No
I have completed these questions to the best of my knowledge:
Signature: …………………………………….. Date:
Please provide the following details so that we can register you in our hospital
system
GP Details
Name:
Address:
Telephone number:
Next of Kin
Name:
Relationship:
Address:
Telephone number:
For hospital use only
Date received:
Date reviewed:
Comment/special instructions:
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
58
5.3 ABO BLOOD GROUPING AND CROSSMATCH TESTING
Recommendations
A compatible ABO blood group and human leucocyte antigen (HLA)
transplant offers the best opportunity for success. (A1)
Where ABO or HLA incompatibility is present, alternative options for
transplantation must be discussed with the donor and recipient,
including paired/pooled donation and antibody incompatible
transplantation. Antibody incompatible transplantation must only be
performed in a transplant centre with the relevant experience and
appropriate support. (A1) (see Chapters 7 and 8)
ABO blood grouping is an important early screening test as it identifies if a (directed)
donor is blood group compatible or incompatible with his/her intended recipient at
an early stage. Alternatively, in non-directed donation, it provides information that
will be used to allocate the kidney to a suitable recipient. ABO blood group testing
may be undertaken by the GP, nephrologist, specialist nurse, or at a transplant
assessment clinic.
Initial HLA typing +/- crossmatch testing is performed once the blood group status
is established, in accordance with the recommendations in Chapter 7. For non-
directed donors, HLA typing provides essential information for kidney allocation
purposes, but crossmatching is only performed once a potential recipient has been
identified in the UK Living Kidney Sharing Schemes (UKLKSS) or on the national
transplant list (see Chapter 8).
If the directed donor is not blood group compatible with his/her recipient, an
alternative donor may be sought or options for paired pooled donation and/or
antibody incompatible transplantation can be considered. See Chapters 7 and 8.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
59
5.4 MEDICAL ASSESSMENT
It is important to manage the expectations of the donor from the outset and to be
clear about the difference between a healthy individual and a suitable donor. For
example, an otherwise healthy person with one kidney or short renal vessels may
be unsuitable to donate. The assessment may reveal previously undiagnosed
disease, and potential donors must be warned of this possibility. A previously
unrecognised condition may impact on future life insurance or specialist
employment. Conversely, early detection of a health problem, which might otherwise
have gone undiagnosed, may benefit the donor.
A full past and present medical history must be taken and the areas listed in Tables
5.4.1 must be addressed and followed up where required. The history aims to
identify any risk of latent or current infection in the donor that could be transmitted
to the recipient by a kidney allograft (see Table 5.4.2 and section 5.14), or any past
or present condition that could impact on the safety of the donor at the time of
surgery or in the long-term. These aspects are discussed in detail throughout
Chapter 5. A thorough clinical examination must be performed, taking particular
account of the cardiovascular and respiratory systems and including the
assessments listed in Table 5.4.3.
A psychosocial assessment is recommended for all donors with appropriate referral
to a mental health professional as required (see Chapters 4 and 8). The EPAT tool
provides a structured approach to initial psychosocial assessment which can be
performed by any member of the multi-disciplinary team and which can help to
identify potential areas of concern. A particular issue is the assessment of mental
and physical health in the potential donor with a history of substance or drug abuse.
Such potential donors should always receive formal psychiatric assessment. For
non-directed donors, assessment by a mental health professional is recommended
in all cases and a structured assessment process has been developed in the UK to
assist this (appended to Chapter 8).
Donor assessment will usually be arranged by a specialist transplant/living donation
nurse, supported by a clinician. The clinician will undertake the medical examination
of the potential donor and, if possible, should not be directly involved in the care of
the intended recipient. Table 5.4.4 details the routine screening investigations that
are recommended for the potential donor.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
60
Reference
1. Massey EK, Timmerman L, Ismail SY, et al. The ELPAT living organ donor
psychosocial assessment tool (EPAT): from ‘what’ to ‘how’ of psychosocial
screening- a pilot study. Transpl Int 2017 Aug 29. doi: 10.1111/tri.13041.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
61
Table 5.4.1
Summary of Key Points of Importance in the Medical +/- Family History of a
Potential Kidney Donor
Haematuria/proteinuria/urinary tract infection
Difficulty in passing urine, including urgency, frequency, dysuria
History of peripheral oedema
Gout
Nephrolithiasis
Hypertension
Diabetes mellitus, including family history
Ischaemic heart disease/peripheral vascular disease/other atherosclerosis
Cardiovascular risk factors
Thromboembolic disease
Sickle cell and other haemoglobinopathies
Weight change
Change in bowel habit
Previous jaundice
Previous or current malignancy
Systemic disease which may involve the kidney
Chronic infection such as tuberculosis
Family history of a renal condition that may affect the donor
Smoking
Current or prior alcohol or drug dependence
Mental health history
Obstetric history
Residence abroad
Previous medical assessment e.g. for life insurance
Previous anaesthetic problem
History of back or neck pain and trauma
Results of national screening programme tests e.g. cervical smear, mammography,
colorectal screening

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
62
Table 5.4.2
History with respect to Transmissible Infection
Previous illnesses
Jaundice or hepatitis
Malaria
Previous blood transfusion
Tuberculosis / atypical mycobacterium
Family history of tuberculosis
Family history of Creutzfeldt-Jakob disease, previous treatment with natural growth
hormone, or undiagnosed degenerative neurological disorder
Specific geographical risk factors: e.g. fungi and parasites, tuberculosis, hepatitis,
malaria, worms
Increased risk of HIV, HTLV1 and HTLV2, Hepatitis B and C infection
Haemophiliac or sexual partner of haemophiliac
High risk sexual behaviour
History of infectious hepatitis or syphilis
History of intravenous drug use
Tattoo or skin piercing within last 6 months
Sexual partner of an individual with positive serology
Sexual partner of drug addict
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
63
Table 5.4.3
Points of Particular Importance when Undertaking Clinical Examination of a
Potential Kidney Donor
Abdominal fat distribution
Blood pressure
Body mass index
Dipstick urinalysis
Evidence of self-harm
Examination for abdominal masses or herniae
Examination for scars or previous surgery
Examination for lymphadenopathy
Examination / history of regular self-examination of the breasts
Examination / history of regular self-examination of the testes
Examination of the cardiovascular and respiratory systems
Mental health
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
64
Table 5.4.4
Routine Screening Investigations for the Potential Donor
Urine
Dipstick for protein, blood and glucose (at least twice)
Microscopy, culture and sensitivity (at least twice)
Measurement of protein excretion rate (ACR or PCR)
Blood
Haemoglobin and blood count
Coagulation screen (PT and APTT)
Thrombophilia screen (where indicated)
Sickle cell trait (where indicated)
Haemoglobinopathy screen (where indicated)
G6PD deficiency (where indicated)
Creatinine, urea and electrolytes
Isotopic or other reference test for measurement of GFR
Liver function tests
Bone profile (calcium, phosphate, albumin and alkaline phosphatase)
Urate
Fasting plasma glucose
Glucose tolerance test (if family history of diabetes or fasting plasma glucose
>5.6 mmol/L)
Fasting lipid screen (if indicated)
Thyroid function tests (if strong family history)
Pregnancy test (if indicated)
Virology and infection screen (see section 5.14)
Hepatitis B and C
HIV
HTLV1 and 2 (if appropriate)
Cytomegalovirus
Epstein-Barr virus
Toxoplasma
Syphilis
Varicella zoster virus (where recipient seronegative)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
65
HHV8 (where indicated)
Malaria (where indicated)
Trypanosoma cruzi (where indicated)
Schistosomiasis (where indicated)
Cardiorespiratory system (see section 5.10)
Chest X-ray
ECG
ECHO (where indicated)
Cardiovascular stress test (as routine or where indicated)

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
66
5.5 ASSESSMENT OF RENAL FUNCTION
Recommendations
Measurement of Renal Function
Initial evaluation of donor candidates should be using estimated
glomerular filtration rate (eGFR), expressed as mL/min/1.73m
2
computed from a creatinine assay standardised to the International
Reference Standard. (B1)
GFR must subsequently be assessed by a reference measured method
(mGFR) such as clearance of
51
Cr-EDTA,
125
iothalamate or Iohexol
performed according to guidelines published by the British Society of
Nuclear Medicine. (B1)
Differential kidney function, determined by
99m
TcDMSA scanning is
recommended where there is >10% variation in kidney size or
significant renal anatomical abnormality. (C1)
Advisory GFR Thresholds for Donation
Pre-donation mGFR should be such that the predicted post-donation
GFR remains within the gender and age-specific normal range within
the donor’s lifetime. Recommended threshold levels are defined in
Table 5.5.2. (B1)
The risk of end-stage renal disease (ESRD) after donation is no higher
than that of the general population. However, there is a very small
absolute increased lifetime risk of ESRD following donation for which
the potential donor must be consented. (D2)
The decision to approve donor candidates whose renal function is
below the advisory GFR threshold or who have additional risk factors
for the development of ESRD should be individualised and based on
the predicted lifetime incidence of ESRD. (D2)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
67
The renal function requirements of the intended recipient, based upon
the absolute GFR of the donor, are relevant to the decision to donate
(in a directed donation) and to the acceptance of a kidney offer from a
non-directed donor or within the UK Living Kidney Sharing Schemes.
(Not Graded)
Monitoring of Kidney Donor
The donor must be offered lifelong annual assessment of renal function
including serum creatinine, estimation of urine protein excretion and
blood pressure measurement. (B1)
5.5.1 Initial Assessment of Donor Renal Function
The initial assessment of renal function in potential living kidney donors is by
measurement of serum creatinine. This is most commonly performed by an estimate
of glomerular filtration rate (eGFR
cr
) using the Chronic Kidney Disease Epidemiology
Collaboration (CKD-EPI) equation and employing a creatinine assay with calibration
traceable to standardised reference material. A correction factor must be applied to
eGFR
cr
values estimated for people of African-Caribbean or African family origin
(multiply eGFR
cr
by 1.159)
(1).
Screening identifies potential living donors with evidence of existing CKD (eGFR
cr
<45 mL/min) who may be saved further investigation as potential kidney donors and
who may require investigation in their own right. However, there is significant
imprecision of eGFR
cr
around the normal range, making it unsuitable as a marker of
renal function without confirmation (1).
More detailed assessment of potential donor function requires an accurate
measurement of GFR using a reference standard measure such as clearance of
inulin,
51
Cr-EDTA,
125
I-iothalamate or iohexol
(1). This is used to inform potential
donors of the long-term risks of donation and potential recipients of the anticipated
level of kidney function being transplanted.
51
Cr-EDTA is the most widely available
reference test. Recent data show a significant coefficient of variation of
51
Cr-EDTA
measured GFR in potential living kidney donors across UK centres (2). The
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
68
technique must be performed strictly according to guidelines of the British Society
of Nuclear Medicine (3).
Divided Renal Function
Divided renal function, measured by combining
51
Cr-EDTA and
99m
Tc-DMSA, can
be helpful in decision-making where there is a size disparity between the two
kidneys (>10%) in a potential donor, if renal function is close to the acceptable
threshold for donation, or when there is anatomical abnormality or complexity. If
suitable for transplantation, the kidney with lower function is usually donated. Some
centres choose to perform split function testing routinely on all donors, although the
evidence for doing so is limited (4).
5.5.2 What is a Safe Threshold Level of Kidney Function to Donate?
A safe threshold level of pre-donation kidney function is one that leaves sufficient
function after donation to maintain the donor in normal health (or minimal absolute
reduction of health) without affecting lifespan. This requires a definition of normal
renal function and of the normal range of age-related change in renal function in
healthy adults over time.
It is reasonable to assume that a threshold which leaves the donor with normal age-
related kidney function after donation is safe. This assumption must be supported
by long-term post-donation health outcomes of kidney donors. These outcomes
include:
Early post donation kidney function after compensation of the residual
kidney
Lifetime rate of decline in kidney function after donation
Any increased risk of ESRD and long-term mortality, as well as any impact
on other non-renal health outcomes when compared to a matched equally
healthy comparator population
It is important to recognise the limitations of the current evidence base (5). Most
series reporting long-term post-donation outcomes comprise mainly Caucasian
donors who have been normotensive, non-diabetic and normo-albuminuric. The
mean age at donation of the cohorts has been around 45 years and the lower

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
69
threshold for donation a GFR >80 mL/min/1.73m
2
. The current practice of living
donation includes donors outside these criteria.
Normal Kidney Function & Change in Kidney Function with Aging
Recent data accurately define gender and age-specific mean and normal ranges for
measured GFR in over 3000 healthy potential UK living kidney donors. Data on
glomerular filtration rate measured by
51
Cr-EDTA clearance in donors at two large
UK centres were amalgamated with patient level data from a recent study of GFR in
over 1800 potential donors from 15 UK centres (6,7). This study conclusively
indicates that renal function corrected for BSA is significantly higher for men than
women after age 40 years. GFR in this normal population remains stable in both
sexes until aged around 40 years and then declines each decade at a rate of
6.6 mL/min/1.73m
2
for men and 7.7 mL/min/1.73m
2
in women.
Table 5.5.1 Age and Gender-Specific GFR based on almost 3000 Healthy
Potential UK living kidney donors
Age
(years)
Measured GFR
(mL/min/1.73m
2
)
Male
Female
20-29
100 (74-126)
98 (72-125)
30-34
100 (74-126)
98 (72-125)
35
99 (73-126)
98 (72-125)
40
96 (70-122)
94 (68-121)
45
93 (67-119)
91 (64-117)
50
90 (63-116)
87 (60-113)
55
86 (60-112)
83 (56-109)
60
83 (57-109)
79 (52-105)
65
80 (54-106)
75 (48-101)
70
76 (50-102)
71 (44-97)
75
73 (47-99)
67 (40-94)
80
70 (44-96)
63 (36-90)

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
70
Figure 5.5.1 Mean and Lower Normal Values (-2SD) for GFR Determined in
Almost 3000 Healthy UK Potential Living Kidney Donors (6)*
* The mean fall in GFR each decade after 40years is 6.6 mL/min/1.73m
2
for men
and 7.7 mL/min/1.73m
2
in women
Early changes to Renal Function Following Living Kidney Donation
Following kidney donation there is a compensatory increase in function in the
remaining kidney in male and female donors across a broad age range. By three
months, remnant kidney clearance increases to a mean GFR of around 65-75% of
pre-donation renal function. In 22 studies where it was described, the average
decrement in GFR after donation was 26 mL/min/1.73m
2
(range 8-50) (7).
Long-Term Loss of GFR in Kidney Donors
The rate of decline in renal function following kidney donation appears to be no
higher, and it is likely that it is lower, than in the healthy general population. It
appears reasonable and cautious to employ the cross-sectional age-related decline
in renal function in the normal population to predict renal function after donation in
the long term. The recommended age-related GFR thresholds for donation in this
0
20
40
60
80
100
120
140
20 30 40 50 60 70 80
GFR (mL/min/1.73 m
2
)
Age (Years)
Male
Female
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
71
guideline ensure that predicted renal function will remain within the lower limit of
normal GFR with aging.
Measurement of kidney function was performed on a selected group from 2,949 (out
of a total of 3,404) patients who had donated over a 40 year period in a single US
centre (selection criteria for donation, GFR >80 mL/min/1.73m
2
). Most donors
(85.5%) had a clearance of >60 mL/min/1.73m
2
on follow-up, and none were
<30 mL/min/1.73m
2
. In a small representative sample of donors, the rate of decline
of renal function was 0.6 +/- 3.8 mL/min/1.73m
2
/y, this being measured with two
samples three years apart an average of 12 years after donation. A caveat is that
the population was predominantly Caucasian (9). In a prospective study of GFR in
203 donors and healthy matched controls, residual renal function continued to
improve in donors over three years post-donation, whereas controls had the
expected age-related decline in function (10). Analysis of 9229 UK kidney donors
selected according to previous (2011) UK Guidelines (1-10 year follow-up)
demonstrates the expected fall in eGFR from baseline to 1 year post-donation
(35%). Thereafter, renal function remained stable up to 5 and 10 years across all
donor age ranges (20-70 years), albeit numbers by 10 years were small (11).
5.5.3 Is Donation Associated with an Increased Risk of End-Stage Renal
Disease, Cardiovascular Disease or Death?
Decreased GFR in the general population is associated with an increased risk of
adverse outcomes including ESRD, cardiovascular disease and death. This
increase becomes apparent with a GFR between 60-75 mL/min/1.73m
2
as
compared to GFR >90 mL/min/1.73m
2
and rises exponentially thereafter (1).
The incidence of ESRD in living kidney donors appears to be similar to or lower than
that seen in the unselected general population despite a reduction in GFR (12). This
is reassuring but not unexpected. Two recent studies compared the post-donation
risks of ESRD with carefully matched healthy controls. Muzaale compared the
outcome of 96,000 kidney donors in the USA over a maximum follow-up of 15 years
(mean 9 years) with matched healthy controls. The donor population was 75% white,
25% obese and 22% had a pre-donation eGFR <80 mL/min. The estimated risk of
ESRD 15 years post-donation was 31 per 10,000 compared to 4 per 10,000 in

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
72
matched controls. The increased risk was far greater in high risk donor populations
such as African American donors, 75 per 10,000. The estimated lifetime risk of
ESRD was 90 per 10,000 in donors, 326 per 10,000 in the general population, and
14 per 10,000 in matched healthy non-donor controls (13). A second study included
1,901 Norwegian donors compared with healthy matched controls and
demonstrated a similar increased risk of ESRD after kidney donation (14).
Donors may be reassured that the absolute increase life time risk of GFR
<30 mL/min/1.73m
2
or ESRD is very small (<1%) for the populations included in this
study. The absolute risk for young donors over a lifetime, particularly with additional
risk factors for ESRD is likely to be more significant.
Figure 5.5.2 Estimated Lifetime Risk of End-Stage Kidney Disease in
Matched but Unscreened Non-Donors, Living Kidney Donors
and Matched Healthy Controls (12)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
73
5.5.4 Individualisation in Discussion of the Risks of ESRD
Physicians are faced with advising potential donors how to proceed when they have
additional adverse factors associated with an increased lifetime risk ESRD. Factors
and compounding risks include:
Measured GFR just below the guideline threshold
Ethnic groups at higher risk (African Caribbean or South Asian origin (by
inference))
Hypertension, obesity and/or (pre) diabetes
A recent US study is helpful in counselling these potential donors (14). Outcome
data of almost 5 million participants from seven US cohorts followed for 4-16 years
enabled 15 year and lifetime risk projections for the incidence of ESRD in non-
donors. This was based on baseline clinical and demographic factors in people who
did not donate. An online calculator allows estimation of the risk of ESRD using 10
clinical and demographic factors (www.transplantmodels.com/esrdrisk).
Hypertension, obesity (BMI >30 kg/m
2
), smoking status, eGFR 60-89
mL/min/1.73m
2
and abnormal urine albumin excretion independently increased the
long-term risks of ESRD by 1.35, 1.16, 1.76, 1.63 and 2.94 fold respectively.
The actual risk of ESRD in almost 53,000 living donors was then compared with the
risk of the matched population. The 15 year observed risk of ESRD for donors was
3.5 to 5.3 times greater than the expected risk, and was higher for blacks compared
with Caucasians and in men compared with women. The risk of ESRD was greatest
for younger patients of black ethnicity. The absolute increased lifetime risk of ESRD
may be helpful in counselling potential donors with risk factors including those below
threshold GFR as defined above. The data also support donation from some older
donors who have additional risk factors such as hypertension but whose lifetime risk
of ESRD is low.
Three retrospective observational studies compared mortality among living kidney
donors in comparison with healthy non-donors (8-10). Two studies (one from the
United States with a follow-up of up to 12 years and one from Canada with a median
follow-up of 6.5 years) revealed a lower risk of death in donors compared to healthy
non-donors whilst the third study suggested a possible small increase. Garg et al
conducted a study of living kidney donors in the province of Ontario, Canada, who
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
74
donated between 1992 and 2009 (8). A total of 2028 donors and 20,280 matched
non-donors were followed for a median of 6.5 years (maximum 17.7 years). The risk
of death and cardiovascular events was lower and the risk of death-censored
cardiovascular events was the same in the donors as compared with the healthy
matched population. The quality of the evidence is considered poor. There is no
clear evidence that donation reduces long-term survival (5) (see section 10.1).
5.5.5 Advisory Threshold Measured GFR Considered Safe for Donation
The age and gender-specific GFRs that are considered safe to donate are defined
in Table 5.5.2. Long term outcome studies demonstrate a very small absolute
increased risk of ESRD in large donor populations with mGFR in excess of
80 mL/min/1.73m
2
where the mean age at donation was around 40-50 years.
However, these series contain only small numbers of young donors (13,14).
A threshold GFR >80 mL/min/1.73m
2
appears safe for donation in the 35 year and
above age range.
Given the extended expected lifetime risk of over 60 years for a 20-year-old,
recommendations for minimum GFR in younger donors are more conservative.
Grams demonstrated an increased absolute lifetime risk in younger donors with
GFR <90 mL/min/1.73m
2
, particularly those with additional risk factors (15).
A threshold for donation of >90 mL/min/1.73m
2
has therefore been set for those
<30 years.
For those >45 years the threshold renal function is predicated on post-donation GFR
(75% of pre-donation function) remaining above the lower limit of the age and
gender-specific normal range described above (-2SD below mean). At all age and
gender-specific GFR thresholds, predicted post-donation renal function in the long
term is based cautiously on loss of GFR each decade after age 40 of
6.5 mL/min/1.73m
2
for men and 7.9 mL/min/1.73m
2
in women. As such, if the
thresholds given in table 5.5.2 and Figures 5.5.3 and 5.5.4 below are adopted, renal
function will be expected to remain within the normal range up to age 80.
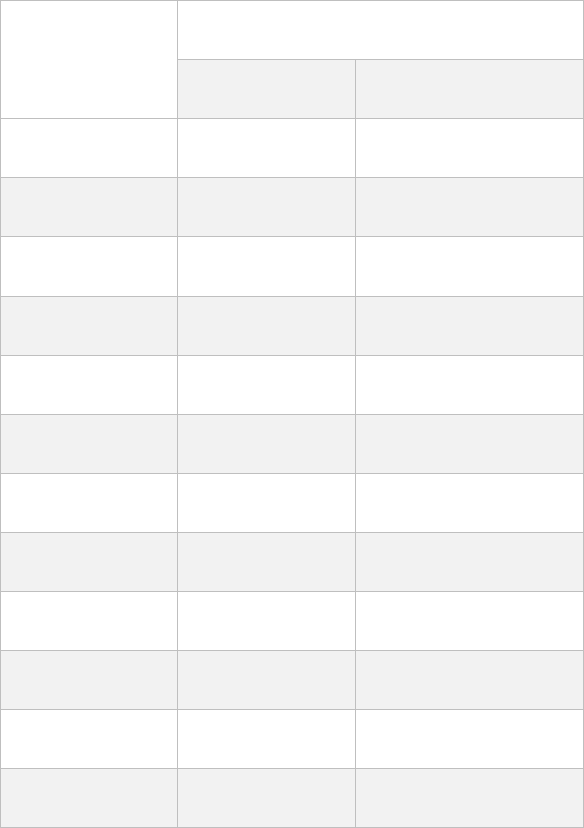
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
75
Table 5.5.2 Advisory Threshold GFR Levels Considered Acceptable for
Living Kidney Donation*
Age (years)
Threshold GFR (mL/min/1.73m
2
)
Male
Female
20-29
90
90
30-34
80
80
35
80
80
40
80
80
45
80
80
50
80
80
55
80
75
60
76
70
65
71
64
70
67
59
75
63
54
80
58
49
*Where the potential donor GFR lies just below these thresholds or there are
additional factors for the development of ESRD, the decision on suitability for
donation should be based on a discussion of the lifetime risk of ESRD without
donation. www.transplantmodels.com/esrdrisk

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
76
Figure 5.5.3 Advisory Threshold GFR Considered Acceptable for Donation
in Males
Figure 5.5.4 Advisory Threshold GFR Considered Acceptable for Donation
in Females
0
20
40
60
80
100
120
140
20 30 40 50 60 70 80
GFR (mL/min/1.73 m
2
)
Age (years)
0
20
40
60
80
100
120
140
20 30 40 50 60 70 80
GFR (mL/min/1.73 m
2
)
Age (years)

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
77
5.5.6 Research Recommendation
Prospective monitoring of post-donation outcomes compared with matched healthy
controls, particularly amongst ethnic minority donors, those with GFR lower than
current BTS recommendations, and those with co-morbidities.
References
1. National Institute for Health and Care Excellence (2014). Chronic kidney disease
in adults: assessment and management. NICE guideline (CG182).
2. Peters AM, Howard B, Neilly MD, et al. The reliability of glomerular filtration rate
measured from plasma clearance: a multi-centre study of 1,878 healthy potential
renal transplant donors. Eur J Nucl Med Mol Imaging 2012; 39: 715-22.
3. Fleming JS, Zivanovic MA, Blake GM, Burniston M, Cosgriff PS. British Nuclear
Medicine Society. Guidelines for the measurement of glomerular filtration rate
using plasma sampling. Nucl Med Commun 2004; 25: 759-69.
4. KDIGO Living Donor Guidelines, 2016.
www.kdigo.org/clinical_practice_guidelines/LivingDonor/KDIGO
5. Lam NN, Lentine KL, Levey AS, Kasiske BL, Garg AX. Long-term medical risks
to the living kidney donor. Nat Rev Nephrol 2015; 11: 411-9.
6. Peters AM, Perry L, Hooker CA, et al. Extracellular fluid volume and glomerular
filtration rate in 1878 healthy potential renal transplant donors: effects of age,
gender, obesity and scaling. Nephrol Dial Transplant 2012; 27: 1429-37.
7. Lipkin G, Fenton A, Montgomery E, Nightingale P, Peters M, Wroe C. Age and
gender-specific normal range for GFR in over 2500 potential UK live kidney
donors; implications for selection and outcomes of live kidney donors.
https://bts.org.uk/wp-content/uploads/2016/09/BTS_Abstract_pdf_2016.pdf.
8. Garg AX, Muirhead N, Knoll G, et al. Proteinuria and reduced kidney function in
living kidney donors: a systematic review, meta-analysis, and meta-regression.
Kidney Int 2006; 70: 1801-10.
9. Ibrahim HN, Foley R, Tan L, et al. Long-term consequences of kidney donation.
N Engl J Med 2009; 360: 459-69.
10. Kasiske BL, Anderson-Haag T, Israni AK, et al. A prospective controlled study
of living kidney donors: three-year follow-up. Am J Kidney Dis 2015; 66: 114-24.
11. Krishnan N, Bradbury L, Lipkin GW. Comparison of baseline GFR levels by age
bands with 1 year, 5 year and 10 year outcomes in live donors - UK cohort study.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
78
https://bts.org.uk/wp-content/uploads/2016/09/BTS_Abstract_pdf_2016.pdf.
12. Segev DL, Muzaale AD, Caffo BS, et al. Perioperative mortality and long-term
survival following live kidney donation. JAMA 2010; 303: 959-66.
13. Muzaale AD, Massie AB, Wang MC, et al. Risk of end-stage renal disease
following live kidney donation. JAMA 2014; 311: 579-86.
14. Mjoen G, Hallan S, Hartmann A, et al. Long-term risks for kidney donors. Kidney
Int 2014; 86: 162-7.
15. Grams ME, Sang Y, Levey AS, et al. Kidney-failure risk projection for the living
kidney-donor candidate. N Engl J Med 2016; 374: 411-21.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
79
5.6 DONOR AGE
Recommendations
Old age alone is not an absolute contraindication to donation but the
medical work-up of older donors must be particularly rigorous to
ensure they are suitable. (A1)
Both donor and recipient must be made aware that the older donor may
be at greater risk of peri-operative complications and that the function
and possibly the long-term survival of the graft may be compromised.
This is particularly evident with donors >60 years of age. (B1)
The young and the old raise different issues with respect to consideration as
potential living kidney donors (1). The ethical barriers to the use of minors and young
people as living donors are addressed in Chapter 3.
5.6.1 The Young Donor
Most programmes do not consider donors aged <18 years and consider an age of
18-21 years as a relative contraindication to donation. Younger donors, even if
without risk factors for kidney disease at the time of evaluation, may still develop
diabetes, hypertension, obesity, immunologically mediated disease or other renal
risk factors, and have more time for these risk factors to progress to CKD and
ultimately ESRD. This is supported by OPTN data which show that most of the
donors that have been placed on the transplant waiting list had donated between
the ages of 18 and 34 years and developed ESRD >15 years after donation (2).
Careful psychological assessment is recommended before donation.
5.6.2 The Older Donor
In the last five years there has been a significant increase in the number of living
donations in the UK from the 60-69 and >70 year groups. Donors above 60 years of
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
80
age need careful consideration with respect to the increased risk of peri-operative
complications, existing comorbidities and residual function post-donation, and also
the long-term transplant outcome in the recipient associated with reduced donor
GFR and potential donor vasculopathy.
5.6.3 Donor Complication Rates Related to Age
Much of the change in attitude towards accepting older donors is due to the wide
and almost universal use of laparoscopic kidney donation in the UK and the resultant
reduction in morbidity and improved recovery. Although peri-operative outcomes
such as operative time, blood loss and length of stay are shown in some recent
studies to be no different from younger donors in carefully selected donors above
60 years (3-5), caution should be exercised in the evaluation, operation and post-
operative management of the older donor.
Considering 80,347 living kidney donors in the US between 1st April 1994 and 31st
March 2009, Segev et al demonstrated poorer 12 year survival for donors aged >50
years as compared to donors <40 years of age, with donors >60 years having worse
survival than those aged 50-59 years (6). However, the long-term risk of death was
no higher for older living donors than for age- and comorbidity-matched NHANES III
participants, the poorer survival therefore not being clearly attributable to kidney
donation. Jacobs has argued that age should not preclude laparoscopic donation on
review of the outcome of a series of 738 consecutive laparoscopic living donor
nephrectomies performed in Maryland (7). In keeping with this, some centres report
higher laparoscopic nephrectomy rates in donors >50 years (8).
Pre-donation cardio-respiratory function should be carefully assessed in older
donors. Most centres perform a stress echocardiogram and/or myocardial perfusion
scan if indicated. Respiratory function tests may be indicated in smokers and those
with airway disease. Cardiopulmonary exercise testing, and in particular the
definition of the anaerobic threshold, has been validated as a predictor of post-
operative complications, particularly in elderly patients. If available, it may be of
particular use in the assessment of elderly donors (9).
Screening of serum PSA is mandatory in males above 55 years. Although a mildly
elevated PSA may not preclude donation, a rising PSA over time may be of concern
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
81
and there should be a low threshold for formal urological review. In women, an up-
to-date mammogram and relevant history should be reviewed. In all patients, there
should be a careful review of bowel function, incorporating the results of up-to-date
population screening tests such as tests for faecal occult blood. Social, family and
psychological support for elderly donors should be provided, particularly in the case
of altruistic donation.
5.6.4 Graft Outcome from Older Donors
Renal function declines progressively with age and kidneys from older living donors
have reduced function (10). Matas et al reported the outcome of 2,540 living donor
kidney transplants in their centre and documented worse outcome when the donor
was >55 years of age (11). In one study, 5 year graft survival after living donor
transplantation was 76% for kidneys from donors >60 years (n=241) and 79% for
kidneys from donors aged <60 years (n=518). However, serum creatinine levels
remained significantly lower in the recipients of kidneys from younger donors, and
graft survival was significantly better beyond 5 years after transplantation (12).
An extensive study recently demonstrated poorer outcomes for kidneys from donors
>59 years of age in 3,142 transplants performed in the UK between 2000 and 2007
(13). This is in keeping with a Scandinavian study demonstrating no effect of donor
age on transplant outcome when all donors aged >50 years were considered, but
poorer outcomes in the subgroup with donor age >65 years (14).
More recently, using the UNOS data from 1994 to 2012, 250,827 kidney transplant
recipients were categorised by donor status: standard criteria donor (SCD),
expanded criteria donor (ECD), or living donor (LD); and by donor age: <60, 60-64,
65-69, ≥70 years. 92,646 of the transplants studied from living donors, with 4.5% of
the recipients (4,186) transplanted with older LD kidneys. Transplant recipients with
older LD kidneys had significantly lower graft and patient survival compared to
younger LD recipients. Compared to SCD recipients, graft survival was decreased
in recipients with living donors 70 years or older, but patient survival was similar.
Older LD kidney recipients had better graft and patient survival than ECD recipients
(15).

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
82
Overall, the use of older kidney donors appears to be an equivalent or beneficial
alternative to awaiting deceased donor kidneys (15). Donor GFR has been
demonstrated to be an important determinant of transplanted kidney function (16)
and it has been suggested that donor function rather than age may be the most
important determinant of outcome, although not all studies have confirmed this (14).
Older donors are more likely than younger donors to be excluded from donating on
the basis of problems discovered during the medical evaluation. However, each
case should be considered on individual merit and if the older donor is judged fit
after rigorous medical evaluation, and if the renal function of the donor is normal
after correction for age and gender, there is no compelling evidence for excluding
donation on the basis of chronological age alone (17,18).
5.6.5 Long Term Risk for Older Donors
Older donors with potential risk factors for kidney disease, such as hypertension or
diabetes, are less likely than younger donors to have enough time for such risk
factors to lead to progressive kidney disease, or for any kidney disease that
develops to affect life expectancy (19).
5.6.6 Summary
Most US transplant programs currently do not have an upper age limit for accepting
donors and are more flexible in applying exclusion criteria for renal risk factors in
older donors (20). UK practice also tends to this conclusion. Younger potential
donors with borderline risk factors should be subjected to stringent exclusion criteria
(21).
References
1. Jones J, Payne WD, Matas AJ. The living donor risks, benefits, and related
concerns. Transplant Rev 1993; 7: 115-28.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
83
2. Gibney EM, King AL, Maluf DG, Garg AX, Parikh CR. Living kidney donors
requiring transplantation: focus on African Americans. Transplantation 2007;
84: 647-9.
3. Dols LF, Kok NF, Roodnat JI, et al. Living kidney donors: impact of age on long-
term safety. Am J Transplant 2011; 11: 737-42.
4. Jacobs SC, Ramey JR, Sklar GN, Bartlett ST. Laparoscopic kidney donation
from patients older than 60 years. J Am Coll Surg 2004; 198: 892-7.
5. Neipp M, Jackobs S, Jaeger M, et al. Living kidney donors >60 years of age: is
it acceptable for the donor and the recipient? Transpl Int 2006; 19: 213-7.
6. Segev DL, Muzaale AD, Caffo BS, et al. Perioperative mortality and long-term
survival following live kidney donation. JAMA 2010; 303: 959-66.
7. Jacobs SC, Cho E, Foster C, Liao P, Bartlett ST. Laparoscopic donor
nephrectomy: the University of Maryland 6-year experience. J Urol 2004; 171:
47-51.
8. Johnson SR, Khwaja K, Pavlakis M, Monaco AP, Hanto DW. Older living donors
provide excellent quality kidneys: a single center experience (older living
donors). Clin Transplant 2005; 19: 600-6.
9. Hall A, Older P. Clinical review: How to identify high-risk surgical patients. Crit
Care 2004; 8: 369-72.
10. Sumrani N, Daskalakis P, Miles AM, Hong JH, Sommer BG. The influence of
donor age on function of renal allografts from live related donors. Clin Nephrol
1993; 39: 260-4.
11. Matas AJ, Payne WD, Sutherland DER, et al. 2,500 living donor kidney
transplants: a single-center experience. Ann Surg 2001; 234: 149-64.
12. Kahematsu A, Tanabe K, Ishikawa N, et al. Impact of donor age on long-term
graft survival in living donor kidney transplantation. Trans Proc 1998; 30: 3118-
9.
13. Fuggle SV, Allen JE, Johnson RJ, et al. Kidney Advisory Group of NHS Blood
and Transplant. Factors affecting graft and patient survival after live donor
kidney transplantation in the UK. Transplantation 2010; 89: 694-701.
14. Oien CM, Reisæter AV, Leivestad T, Dekker FW, Line PD, Os I. Living donor
kidney transplantation: the effects of donor age and gender on short- and long-
term outcomes. Transplantation 2007; 83: 600-6.
15. Englum BR, Schechter MA, Irish WD, et al. Outcomes in kidney transplant
recipients from older living donors. Transplantation 2015; 99: 309-15.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
84
16. Hawley CM, Kearsley J, Campbell SB, et al. Estimated donor glomerular
filtration rate is the most important donor characteristic predicting graft function
in recipients of kidneys from live donors. Transpl Int 2007; 20: 64-72.
17. Kumar A, Kumar RZ, Srinadh ES, et al. Should elderly donors be accepted in
liverelated renal transplant programs? Clin Transplant 1994; 8: 523-6.
18. Lezaic V, Djukanov L, Blagojevic-Lazik R, et al. Living related kidney donors
over 60 years old. Transpl Int 1996; 9: 109-14.
19. Steiner RW. ‘Normal for now’ or ‘at future risk’: a double standard for selecting
young and older living kidney donors. Am J Transplant 2010; 10: 737-41.
20. Mandelbrot DA, Pavlakis M, Danovitch GM, et al. The medical evaluation of
living kidney donors: a survey of US transplant centers. Am J Transplant 2007;
7: 2333-43.
21. Kher A, Mandelbrot DA. The living kidney donor evaluation: focus on renal
issues. Clin J Am Soc Nephrol 2012; 7: 366-71.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
85
5.7 DONOR OBESITY
Recommendations
Otherwise healthy overweight patients (BMI 25-30 kg/m
2
) may safely
proceed to kidney donation. (B1)
Moderately obese patients (BMI 30-35 kg/m
2
) must undergo careful pre-
operative evaluation to exclude cardiovascular, respiratory and kidney
disease. (C2)
Moderately obese patients (BMI 30-35 kg/m
2
) must be counselled about
the increased risk of peri-operative complications based on
extrapolation of outcome data from very obese donors (BMI >35 kg/m
2
).
(B1)
Moderately obese patients (BMI 30-35 kg/m
2
) must be counselled about
the long-term risk of kidney disease and be advised to lose weight
before donation and to maintain their ideal weight following donation.
(B1)
Data on the safety of kidney donation in the very obese (BMI >35 kg/m
2
)
are limited and donation should be discouraged. (C1)
In 2013 over a quarter of adults in England were classified as obese (BMI >30 kg/m
2
)
(1). In the general population, obesity is associated with increased morbidity and
mortality. For a BMI of 30-35 kg/m
2
, the median life expectancy is reduced by 2-4
years and for a BMI of 40-45 kg/m
2
, it is reduced by 8-10 years, which is comparable
with the effects of smoking (2). In comparison with individuals of normal weight,
overweight and obese individuals are at increased risk of hypertension,
hypercholesterolemia, insulin resistance and diabetes, heart disease, stroke, sleep
apnoea and certain cancers (3).
Obesity is considered a relative contra-indication to living kidney donation because
of the increased risk of surgical complications and the adverse impact of obesity on
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
86
renal function in the longer term. The presence of obesity in kidney donors is
associated in some studies with an increase in peri-operative complications,
although these are mostly relatively minor in nature. In a single centre retrospective
study of 553 consecutive hand-assisted laparoscopic living kidney donations, those
with a high BMI (≥35 kg/m
2
, n=58) had longer operative times (mean increase 19
minutes), more minor peri-operative complications (mostly wound complications),
but the same low rate of major surgical complications (conversion to open
nephrectomy or re-operation) and a similar length of stay (2.3 vs 2.4 days) as low
BMI (<25 kg/m
2
) donors (4). In a retrospective cross-sectional analysis of 6,320
cases, obesity was identified in only 2% of donors but was an independent predictor
of donor risk; 28.3% of obese patients had complications compared with 18.2% of
non-obese patients (5). In another retrospective analysis of 3,074 living kidney
donors from 28 US centres during 2004 and 2005, 2.4% of donors were obese and
obesity was associated with an increase in peri-operative complications (odds ratio
1.92), but no peri-operative mortality (6).
A systematic review and meta-analysis of ten studies, including that by Heimbach
et al (4), examined 484 obese living donors with a mean BMI of 34.5 kg/m
2
at
donation (range 32-39 kg/m
2
) and reported no deaths. It found statistically significant
(but clinically insignificant) differences in operative time, blood loss and hospital stay
between obese and non-obese donors (7). A further meta-analysis in 2013 of nearly
6000 laparoscopic donor nephrectomies showed a significant increase in
conversion to open surgery as the only morbidity risk that was significantly increased
in the obese donor (absolute risk 2.7% versus 1.5%, odd ratio 1.69) (8). According
to a recent cohort study of all (80,347) living donors during a 15-year period in the
US, 22.6% were obese (BMI ≥30 kg/m
2
) but obesity was not associated with a
statistically significant difference in surgical mortality (9). Similar findings were
supported by US Registry Analysis of 14,964 living donors, of whom a moderate
proportion were obese (10).
Overall, these data suggest that laparoscopic donor nephrectomy is an increasingly
safe procedure in the otherwise healthy obese kidney donor and does not result in
a high rate of major peri-operative complications.
The principal concern for the obese living donor is the possibility that donation may
have an adverse effect on long-term kidney function. Obesity associated
co-morbidities such as hypertension, diabetes and the metabolic syndrome may
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
87
compromise future kidney function. In addition, data suggest that obesity is
independently associated with a higher risk of developing end stage kidney disease
(11). Focal glomerulosclerosis and obesity-related glomerulopathy (glomerular
enlargement and mesangial expansion) with associated proteinuria have been
described in patients with severe obesity (12) and may be reversible with weight
loss. Obesity is also a risk factor for renal insufficiency after unilateral nephrectomy.
At 10 years post-nephrectomy, 60% of patients whose BMI was >30 kg/m
2
at the
time of nephrectomy developed proteinuria (>3 g/day) and 30% developed renal
insufficiency (creatinine clearance <70 mL/min) (13). These data suggest that
nephrectomy in obese patients increases the risk of developing proteinuria and/or
renal insufficiency.
Individual risk for developing obesity increases with time, both in the general
population and in living kidney donors. Weight gain post-donation is a common
observation, particularly in those who are overweight before donation (14). At mean
follow-up of 12 years post-donation, a higher BMI was associated with both
hypertension and a GFR that was lower than 60 mL/min/1.73m
2
(15). In a recent
retrospective analysis, kidney function in 98 obese (BMI >30 kg/m
2
) and non-obese
(BMI <30 kg/m
2
) patients who donated a kidney 5 to 40 years previously was similar,
though both donor groups had reduced kidney function compared with BMI-matched
two-kidney control subjects (16). Obesity was associated with a higher risk of
hypertension and dyslipidaemia in both donors and controls. In a study of 39 African
American living kidney donors 4 to 10 years post-donation, 8 subjects whose BMI
was >35 kg/m
2
had a significantly greater fall in eGFR than those with BMI <35 kg/m
2
(40 and 28 mL/min/1.73m
2
respectively) (17). However, in a different retrospective
cohort study using OPTN data from 5,304 donors among whom 40% were
overweight (BMI >25 kg/m
2
), 18% were obese (BMI >30 kg/m
2
) and 5% were very
obese (BMI >35 kg/m
2
), the decline in eGFR from baseline and percentage change
in creatinine at 6 months did not differ significantly across the three groups (18). In
a more recent study of 36 obese living kidney donors 7 years post-donation, 47%
had an eGFR below 60 mL/min/1.73m
2
, 42% were hypertensive and 19% had
microalbuminuria (19). There was no control group in this study.
These findings support the current practice of accepting otherwise healthy
overweight (BMI 25-30 kg/m
2
) and moderately obese (BMI 30-35 kg/m
2
) donors,
although there are few studies that address long-term health outcomes for the very
obese (BMI >35 kg/m
2
). Pre-donation counselling should include a careful
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
88
discussion of the uncertain long-term risks of donation in obese individuals along
with advice about weight maintenance following donation.
References
1. Statistics on obesity, physical activity and diet: England, 2010. NHS Health and
Social Care Information Centre, March 2015.
http://www.hscic.gov.uk/catalogue/PUB16988
2. Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific
mortality in 900 000 adults: collaborative analyses of 57 prospective studies.
Lancet 2009; 373: 1083-96.
3. Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS. Association of
hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity:
findings from the national health and nutrition examination survey, 1999 to 2004.
J Am Coll Surg 2008; 207: 928-34.
4. Heimbach JK, Taler SJ, Prieto M, et al. Obesity in living kidney donors: clinical
characteristics and outcomes in the era of laparoscopic donor nephrectomy. Am
J Transplant 2005; 5: 1057-64.
5. Friedman AL, Cheung K, Roman SA, Sosa JA. Early clinical and economic
outcomes of patients undergoing living donor nephrectomy in the United States.
Arch Surg 2010; 145: 356-62.
6. Patel S, Cassuto J, Orloff M, et al. Minimizing morbidity of organ donation:
analysis of factors for perioperative complications after living-donor
nephrectomy in the United States. Transplantation 2008; 85: 561-5.
7. Young A, Storsley L, Garg AX, et al. Health outcomes for living kidney donors
with isolated medical abnormalities: a systematic review. Am J Transplant 2008;
8: 1878-90.
8. Lafranca JA, Hagan SM, Dols LF, et al. Systematic review and meta-analysis of
the relation between donor body mass index and short-term donor outcome of
laparoscopic donor nephrectomy. Kidney Int 2013; 83: 931-9.
9. Segev DL, Muzaale AD, Caffo BS, et al. Perioperative mortality and long-term
survival following live kidney donation. JAMA 2010; 303: 959-66.
10. Lentine KL, Lam NN, Axelrod D, et al. Perioperative complications after living
kidney donation: a national study. Am J Transplant 2016; 16: 1848-57.
11. Hsu CY, McCulloch CE, Iribarren C, Darbinian J, Go AS. Body mass index and
risk for end-stage renal disease. Ann Intern Med 2006; 144: 21-8.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
89
12. Kambham N, Marcowitz GS, Valeri AM, Lin J, D'Agati VD. Obesity related
glomerulopathy; an emerging epidemic. Kidney Int 2001; 59: 1498-509.
13. Praga M, Hernandez E, Herrero JC, et al. Influence of obesity on the appearance
of proteinuria and renal insufficiency after unilateral nephrectomy. Kidney Int
2000; 58: 2111-8.
14. Torres VE, Offord KP, Anderson CF, et al. Blood pressure determinants in living-
related renal allograft donors and their recipients. Kidney Int 1987; 31: 1383-90.
15. Ibrahim HN, Foley R, Tan L, et al. Long-term consequences of kidney donation.
N Engl J Med 2009; 360: 459-69.
16. Tavakol MM, Vincenti FG, Assadi H, et al. Long-term renal function and
cardiovascular disease risk in obese kidney donors. Clin J Am Soc Nephrol
2009; 4: 1230-8.
17. Nogueira JM, Weir MR, Jacobs S, et al. A study of renal outcomes in African
American living kidney donors. Transplantation 2009; 88: 1371-6.
18. Reese PP, Feldman HI, Asch DA, Thomasson A, Shults J, Bloom RD. Short-
term outcomes for obese live kidney donors and their recipients. Transplantation
2009; 88: 662-71.
19. Nogueira JM, Weir MR, Jacobs S, et al. A study of renal outcomes in obese
living kidney donors. Transplantation 2010; 90: 993-9.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
90
5.8 HYPERTENSION IN THE DONOR
Recommendations
Blood pressure must be assessed on at least two separate occasions.
Ambulatory blood pressure monitoring or home monitoring is
recommended if blood pressure is high, high normal or variable, or the
potential donor is on treatment for hypertension. (C2)
We suggest that a blood pressure <140/90 mmHg is usually acceptable
for donation. (C1)
Prospective donors must be warned about the risk of developing
donation-related hypertension, particularly if in a high-risk group.
Blood pressure measurement is part of annual donor monitoring. (C1)
Potential donors with mild-moderate hypertension that is controlled to
<140/90 mmHg (and/or 135/85 mmHg with ABPM or home monitoring)
with one or two antihypertensive drugs and who have no evidence of
end organ damage may be acceptable for donation. Acceptance will be
based on an overall assessment of cardiovascular risk and local policy.
(C1)
It is recommended that potential donors with hypertension are
excluded from donation if: (C1)
o Blood pressure is not controlled to <140/90 mmHg on one or two
antihypertensive drugs
o Evidence of end organ damage (retinopathy, left ventricular
hypertrophy, proteinuria, previous cardiovascular disease)
o Unacceptable risk of future cardiovascular risk or lifetime
incidence of ESRD
All living kidney donors must be encouraged to minimise the risk of
hypertension and its consequences before and after donation by
lifestyle measures including stopping smoking, reducing alcohol
intake, frequent exercise and, where appropriate, weight loss. (C1)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
91
It is recommended that donors who are diagnosed with hypertension
during assessment or who develop hypertension following donation
are managed according to British Hypertension Society guidelines.
(B1)
Hypertension is one of the commonest reasons for declaring a potential kidney
donor medically unsuitable (1). Sub-clinical, hypertensive nephrosclerosis may be
present at the time of donation. In addition, an increase in blood pressure after
donation may increase future cardiovascular risk or predicted lifetime incidence of
ESRD above an acceptable level. As with other aspects of living donation, each
case needs to be considered individually, bearing in mind that many potential donors
may be willing to accept a higher risk of developing hypertension than their
transplant professionals (2).
5.8.1 Definition of Hypertension in the Donor
There is a general consensus from the Joint National Committee on Prevention,
Detection and Treatment of High Blood Pressure (3), British Hypertension Society
(4) and European Society of Hypertension (5) that adults with a blood pressure
above 140/90 mmHg should be considered hypertensive. All guidelines agree that
a blood pressure above 140/90 mmHg requires further assessment and/or
treatment.
In addition, it is evident that the risk of cardiovascular disease increases with blood
pressure values that are still within the normal range. The Joint National Committee
reports that cardiovascular risk doubles for every 20/10 mmHg rise in blood pressure
above 115/75 mmHg. This has in part led to the recognition of the risk of ‘high
normal’ blood pressure and the need to monitor this patient group (4). There is no
evidence that ‘high normal’ blood pressure is a contra-indication to donor
nephrectomy but these donors should be informed of the high lifetime risk of
developing hypertension irrespective of nephrectomy, and therefore the need for
follow-up.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
92
5.8.2 Method of Blood Pressure Measurement
Most of the large population based studies of cardiovascular risk have relied upon
office blood pressure measurements. There is no evidence to suggest that office
blood pressure measurements are a less accurate predictor of cardiovascular risk
in potential donors undergoing nephrectomy and therefore this method should be
used for the standard measurement of blood pressure. 20-25% of the population will
exhibit ‘white coat’ hypertension (6). In this situation, 24-hour ambulatory blood
pressure monitoring (ABPM) or home readings may be useful. In addition 10-30%
of the population may have a normal office blood pressure but demonstrate
hypertension with ABPM or home readings (masked hypertension) (7).
The British Hypertension Society define hypertension when daytime ABPM or
average home blood pressure is >135/85 mmHg (8). In a study of 238 potential
donors, 36.7% were classified as hypertensive based on office measurements.
However, this proportion decreased to 11% when ABPM was used for assessment.
This discrepancy was most marked in older donors (9). These data would support
the use of ABPM in the assessment of potential donors with hypertension based on
office measurements. Ozdemir et al suggested that ABPM was more sensitive at
identifying hypertension in potential donors than office blood pressure
measurements (10). However, there is little evidence to support the routine use of
ABPM to assess potential donors who are normotensive on initial office blood
pressure measurements.
5.8.3 Risk of Developing Hypertension Post-Donation
The reported incidence of hypertension after unilateral nephrectomy varies
significantly from 9-75% (11-14). Several larger studies with varying duration of
follow-up suggest that approximately one third of donors will develop hypertension
(15-17). Although this rate is high, these studies do not quote the incidence of
hypertension in control populations and therefore it is not possible to determine
whether there is any excess risk attributable to unilateral nephrectomy. Even if
controlled data were available, it would not account for screening during donor
selection.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
93
A large database study from the US which involved 3,698 donors concluded that the
rate of hypertension in donors was similar to that of the general population (18). In
contrast, a similar study from Ontario suggested that donors were more frequently
diagnosed with hypertension (16.3% vs 11.9%) (18). Several small studies have
also suggested an increase in the incidence of hypertension after unilateral
nephrectomy when compared to a control population (14,19,20). However, other
studies have failed to reproduce this finding (16,21,22). In addition, no difference
was found when the incidence of hypertension was compared in kidney donors and
their siblings (23).
Two meta-analyses have considered the effect of unilateral nephrectomy on
hypertension. The first in 1995 reported a small increase in both systolic and
diastolic pressures post-nephrectomy (2.4 and 3.1 mmHg respectively) but no
increase in the incidence of hypertension compared to controls (24). A more recent
meta-analysis performed in 2006 reported a weighted mean increase in blood
pressure of 7 mmHg systolic and 5 mmHg diastolic (25).
It is clear that the risk of developing hypertension after kidney donation is influenced
by pre-donation characteristics including pre-donation blood pressure, body mass
index and age (16,17). Data on the effect of race on donor outcomes are more
limited. The available data suggest higher rates of hypertension in black donors after
donation, paralleling the observed prevalence in the general population (26).
However several large studies have suggested that hypertension is more prevalent
in black donors that in matched non-donor controls (27,28). Similar changes in blood
pressure were seen in Hispanic donors (27).
Higher risk groups should be warned of the higher risk of developing hypertension
and the need for monitoring. Although there is no direct evidence to support a lower
acceptable blood pressure threshold in younger potential donors, the advice given
to such patients should take account of donor age in the assessment of long-term
donor risk.
5.8.4 Pre-existing Hypertension in the Donor
There is relatively little information on the influence of nephrectomy in patients with
pre-existing hypertension. However, it is generally accepted that the presence of
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
94
hypertensive end organ damage (left ventricular hypertrophy, retinopathy,
proteinuria) (29,30), uncontrolled hypertension, or hypertension that requires more
than two drugs to achieve adequate control are contraindications to donor
nephrectomy. Since it is unlikely that donor nephrectomy will be performed in these
circumstances, evidence to support this practice will not be generated in the living
donor setting.
Evidence is also sparse for potential donors who present with less severe
hypertension and it is difficult to draw definite conclusions from the available
literature (reviewed by Young et al) (31). This scenario will become increasingly
common as older donors are considered. In a series by Textor et al (published only
in abstract), 58 patients with hypertension controlled on 1 or 2 agents underwent
nephrectomy (32). There were no increased risks to the donor identified (renal
function, proteinuria and hypertension). In a smaller series of patients reported by
the same group, 24 patients with hypertension (>140/90 mmHg) underwent donor
nephrectomy. Pre-existing donor hypertension did not have an adverse effect on
outcome with no evidence of higher blood pressure or renal injury after nephrectomy
(33). These reports suggest that potential donors with mild or moderate
hypertension should be considered suitable for nephrectomy, particularly if the blood
pressure is controlled with non-pharmacological methods and 1 or 2
antihypertensive agents.
Potential donors with hypertension should have this confirmed by either repeated
office measures or ABPM. If confirmed, non-pharmacological interventions should
be recommended and drug treatment started if required. If adequate blood pressure
control is achieved or if the long-term cardiovascular risk is deemed acceptable by
both patient and assessor, the donor may proceed to nephrectomy.
5.8.5 Management of Hypertension following Donor Nephrectomy
Hypertension will develop in at least 30% of patients following unilateral
nephrectomy. Several studies have reported longitudinal data on patients after
unilateral nephrectomy including renal function, albuminuria and blood pressure.
The data are conflicting with some reports suggesting that hypertension after
nephrectomy is associated with the development of renal complications (21), but
this has not been confirmed by others (12,34). Hypertension in this context should
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
95
be managed according to the standard guidelines of the British Hypertension
Society (4).
5.8.6 Conclusion
All potential donors should be carefully assessed for the presence of hypertension
which, if present, may exclude donation. However, donation may be possible in the
presence of controlled hypertension with no evidence of end organ damage. All
donors should be warned that blood pressure may rise after donation. Blood
pressure should be monitored regularly after donation and lifestyle should be
modified to minimise the risk of hypertension and future cardiovascular disease.
References
1. Fehrman-Ekholm I, Gabel H, Magnusson G. Reasons for not accepting living
kidney donors. Transplantation 1996; 61: 1264-5.
2. Young A, Karpinski M, Treleaven D, et al. Differences in tolerance for health
risk to the living donor among potential donors, recipients, and transplant
professionals. Kidney Int 2008; 73: 1159-66.
3. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint
National Committee on prevention, detection, evaluation, and treatment of high
blood pressure: the JNC 7 report. JAMA 2003; 289: 2560-72.
4. Williams B, Poulter NR, Brown MJ, et al. British Hypertension Society guidelines
for hypertension management 2004 (BHS-IV): summary. Br Med J 2004; 328:
634-40.
5. 2003 European Society of Hypertension - European Society of Cardiology
guidelines for the management of arterial hypertension. J Hypertens 2003: 21:
1011-53.
6. Pickering TG, James GD, Boddie C, et al. How common is white coat
hypertension? JAMA 1988; 259: 225-8.
7. Stergiou GS, Asayama K, Thijs L, et al. Prognosis of white-coat and masked
hypertension: international database of home blood pressure in relation to
cardiovascular outcome. Hypertension 2014; 63: 675-82.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
96
8. British Hypertension Society. Hypertension in adults: diagnosis and
management. 2011. Available from: http://www.nice.org.uk/guidance/cg127/
chapter/Introduction.
9. Textor SC, Taler SJ, Larsonet TS, et al. Blood pressure evaluation among older
living kidney donors. J Am Soc Nephrol 2003; 14: 2159-67.
10. Ozdemir N, Guz G, Sezer S, et al. Ambulatory blood pressure monitoring in
potential renal transplant donors. Nephrol Dial Transplant 2000; 15: 1038-40.
11. Anderson CF, Velosa JA, Frohnert PP, et al. The risks of unilateral
nephrectomy: status of kidney donors 10 to 20 years postoperatively. Mayo Clin
Proc 1985. 60: 367-74.
12. Eberhard OK, Kliem V, Offner G, et al. Assessment of long-term risks for living
related kidney donors by 24-h blood pressure monitoring and testing for
microalbuminuria. Clin Transplant 1997; 11: 415-9.
13. Miller IJ, Suthanthiran M, Riggio RR, et al. Impact of renal donation. Long-term
clinical and biochemical follow-up of living donors in a single center. Am J Med
1985; 79: 201-8.
14. Saran R, Marshall SM, Masden R, Keavey P, Tapson JS. Long-term follow-up
of kidney donors: a longitudinal study. Nephrol Dial Transplant 1997; 12: 1615-
21.
15. Fehrman-Ekholm I, Elinder CG, Stenbeck M, Tyden G, Groth CG. Kidney
donors live longer. Transplantation 1997; 64: 976-8.
16. Ibrahim HN, Foley R, Tan L, et al. Long-term consequences of kidney donation.
N Engl J Med 2009; 360: 459-69.
17. Torres VE, Offord Kp, Anderson CF, et al. Blood pressure determinants in living-
related renal allograft donors and their recipients. Kidney Int 1987; 31: 1383-90.
18. Garg AX, Prasad GV, Thiessen-Philbrook HR, et al. Cardiovascular disease
and hypertension risk in living kidney donors: an analysis of health
administrative data in Ontario, Canada. Transplantation 2008; 86: 399-406.
19. Watnick TJ, Jenkins RR, Rackoff P, Baumgarten A, Bia MJ. Microalbuminuria
and hypertension in long-term renal donors. Transplantation 1988; 45: 59-65.
20. Hakim RM, Goldszer RM, Brenner BM. Hypertension and proteinuria: long-term
sequelae of uninephrectomy in humans. Kidney Int 1984; 25: 930-6.
21. Fehrman-Ekholm I, Duner F, Brink B, Tyden G, Elinder CG. No evidence of
accelerated loss of kidney function in living kidney donors: results from a cross-
sectional follow-up. Transplantation 2001; 72: 444-9.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
97
22. Goldfarb DA, Matin SF, Braun WE, et al. Renal outcome 25 years after donor
nephrectomy. J Urol 2001; 166: 2043-7.
23. Williams SL, Oler J, Jorkasky DK. Long-term renal function in kidney donors: a
comparison of donors and their siblings. Ann Intern Med 1986; 105: 1-8.
24. Kasiske BL, Ma JZ, Louis JA, Swan SK. Long-term effects of reduced renal
mass in humans. Kidney Int 1995; 48: 814-9.
25. Boudville N, Prasad GV, Knoll G, et al. Meta-analysis: risk for hypertension in
living kidney donors. Ann Intern Med 2006; 145: 185-96.
26. Nogueira JM, Weir MR, Jacobs S, et al. A study of renal outcomes in African
American living kidney donors. Transplantation 2009; 88: 1371-6.
27. Lentine KL, Schnitzler MA, Xiao H, et al. Racial variation in medical outcomes
among living kidney donors. N Engl J Med 2010; 363: 724-32.
28. Doshi MD, Goggins MO, Li L, Garg AX. Medical outcomes in African American
live kidney donors: a matched cohort study. Am J Transplant 2013; 13: 111-8.
29. Abramowicz D, Cochat P, Claas FH, et al. European Renal Best Practice
Guideline on kidney donor and recipient evaluation and perioperative care.
Nephrol Dial Transplant 2015; 30: 1790-7.
30. Ierino F, Kanellis J. The CARI guidelines. Donors at risk: haematuria.
Nephrology (Carlton) 2010; 15 Suppl 1: S111-3.
31. Young A, Storsley L, Garg AX, et al. Health outcomes for living kidney donors
with isolated medical abnormalities: a systematic review. Am J Transplant 2008;
8: 1878-90.
32. Textor SC. Hypertensive living renal donors have lower blood pressures and
urinary microalbumin one year after nephrectomy. Am J Transplant 2003; 3
(Abstract).
33. Textor SC. Atherosclerotic renal artery stenosis: how big is the problem, and
what happens if nothing is done? J Hypertens Suppl 2005; 23: S5-13.
34. Praga M, Hernandez E, Herrero JC, et al. Influence of obesity on the
appearance of proteinuria and renal insufficiency after unilateral nephrectomy.
Kidney Int 2000; 58: 2111-8.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
98
5.9 DIABETES MELLITUS
Recommendations
All potential living kidney donors must have a fasting plasma glucose
level checked. (B1)
A fasting plasma glucose concentration between 6.1-6.9 mmol/L is
indicative of an impaired fasting glucose state and an oral glucose
tolerance test (OGTT) should be undertaken. (B1)
Prospective donors with an increased risk of type 2 diabetes because
of family history, a history of gestational diabetes, ethnicity or obesity
should also undergo an OGTT. (B1)
If OGTT reveals a persistent impaired fasting glucose and/or an
impaired glucose tolerance, then the risks of developing diabetes after
donation must be carefully considered. (B1)
Consideration should be given to the use of a diabetes risk calculator
to inform the discussion of potential kidney donation. (B2)
Consideration of patients with diabetes as potential kidney donors
requires very careful evaluation of the risks and benefits. In the
absence of evidence of target organ damage and having ensured that
other cardiovascular risk factors such as obesity, hypertension or
hyperlipidaemia are optimally managed, diabetics can be considered
for kidney donation after a thorough assessment of the lifetime risk of
cardiovascular and progressive renal disease in the presence of a
single kidney. (Not graded)
5.9.1 Diagnosis of Diabetes and the Oral Glucose Tolerance Test
All prospective donors should have a fasting plasma glucose measurement to
exclude diabetes. A fasting venous plasma glucose of >7.0 mmol/L indicates
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
99
diabetes (6). Fasting plasma glucose values of between 6.1 and 6.9 mmol/L indicate
impaired fasting glucose (IFG). In the context of living donation, impaired fasting
glucose is an indication for a standard 2-hour oral glucose tolerance test (OGTT). A
2-hour glucose value of equal to or greater than 11.1 mmol/L indicates diabetes (6).
A 2-hour value between 7.8 and 11.1 mmol/L indicates impaired glucose tolerance
(IGT) (1).
Impaired fasting glucose
Impaired fasting glucose is not a distinct clinical entity but rather indicates a
significantly increased risk for the development of diabetes and adverse health
outcomes in the future. The overall prevalence of IFG is around 5%. The
reproducibility of the test is not good: around 51-64% of patients with IGT will
continue to have IGT if the test is repeated, around 30% will be reclassified as
normal, and around 10% will be reclassified as having diabetes. Of Europeans with
IFG, around 6.6% will at the same time fulfil the criteria for diabetes whilst 18.9% of
South-Asians with IFG will have diabetes, as defined by the OGTT limits. An
individual with IFG has an 4.7 fold increased annualised relative risk of developing
diabetes and the annualised relative risk of adverse health outcomes is 1.19-1.28
times higher than someone with a normal fasting plasma glucose (1).
Impaired glucose tolerance
Impaired glucose tolerance was initially defined in terms of an increased future risk
of diabetes, but it is now appreciated that it is also associated with an increased risk
of premature mortality and increased cardiovascular risk. The overall prevalence of
IGT is around 10%, is higher in ethnic minority groups, and increases with age.
There is moderate reproducibility of the test result with 33-48% remaining
unchanged on repeat testing, 39-46% reclassified as normal and 6-13% reclassified
as in keeping with diabetes. If present, the annualised relative risk of a patient
developing diabetes is 6 times higher compared to those with a normal test result
and all-cause mortality is 1.48 times higher (1).
HbA1c
Diabetes may also be diagnosed based upon HbA1c criteria, a result >48 mmol/mol
(6.5%) being sufficient to diagnose diabetes if confirmed by repeat testing (2). An
HbA1c <48 mmol/mol (6.5%) may be used to predict the future likelihood of
developing diabetes; for example, an HbA1c result of 42-48 mmol/mol (6.0-6.5%)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
100
indicates a 5-year incidence risk of diabetes of 25-50%, 20 times higher than that
associated with a HbA1c of 31 mmol/mol (5%). An OGTT should be strongly
considered when the HbA1c is in this range. It is reasonable to consider HbA1c
values between 39 and 46 mmol/mol (5.7% and 6.4%) as identifying individuals with
pre-diabetes, and at increased risk of developing diabetes and cardiovascular
disease in the future (3).
5.9.2 Risk of Type 1 Diabetes
Type 1 diabetes presents predominantly in childhood and early adulthood and 50%
of cases have presented by the age of 20 years (4). The incidence of type 1 diabetes
in adults is less than 1 in 10,000 (4). First degree relatives of an individual with type
1 diabetes have a 15-fold increased risk of developing the disease. Moreover, the
relatives of type 1 diabetics with diabetic nephropathy appear to be at increased risk
of nephropathy should they subsequently develop diabetes (5). However, because
type 1 diabetes is relatively uncommon and most cases have presented before the
age at which living donation is under consideration, there is little need for concern
even when there is a family history of type 1 diabetes. It may sometimes be difficult
to determine from the history whether an affected family member had type 1 or type
2 diabetes. As a working definition, type 1 diabetes is characterised by onset below
the age of 30 years and a requirement for insulin treatment from the time of
diagnosis.
5.9.3 Risk of Type 2 Diabetes
Type 2 diabetes is predominantly a disease of later life and in 50% of cases is
clinically unrecognised (6). The crude prevalence of undiagnosed disease in the
Caucasian population is 2.3% (7). Individuals who have a family history (first degree
relative) of type 2 diabetes are at higher risk of developing the disease (relative risk
3.0). The prevalence of type 2 diabetes is much higher than for type 1 diabetes and
the absolute risk of developing the disease is high (lifetime risk 38%) (8). The
combination of a positive family history and obesity (BMI >30 kg/m
2
) places an
individual at very high risk of diabetes in later life (9). Individuals from South Asia
and the Caribbean are at increased risk of type 2 diabetes, independent of age and
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
101
obesity. A history of gestational diabetes is an independent risk factor for later
diabetes.
Individuals at high risk of type 2 diabetes because of a positive family history,
gestational diabetes, and/or obesity should undergo an OGTT. For individuals with
a normal OGTT, the risk of developing type 2 diabetes within 5 years is around 1%
and is modulated by ethnicity and obesity.
5.9.4 Risk Calculators
The OGTT can be used either to diagnose diabetes or to predict the risk of
developing diabetes in the future. More recently, risk calculators have been
developed that use data for a particular individual to give an estimated risk for that
individual for the development of diabetes over the subsequent 10 years. The use
of such calculators has been advocated when making therapy decisions and when
discussing those decisions with patients (QDiabetes
®
-2015 risk calculator:
http://qdiabetes.org) (10). Such calculators may usefully be used in the assessment
of kidney donors and discussion of the results may be part of the assessment
process.
5.9.5 Impaired Fasting Glucose and Kidney Donation
In a small study, 45 donors with impaired fasting glucose were matched with 45
donors with a normal fasting glucose at the time of donation and followed for a
median duration of 10.4 years. Those with IFG appeared to do well, when compared
with donors with a normal fasting glucose. Urine albumin excretion and MDRD
eGFR were similar in both groups. Almost 60% of the donors with IFG had a normal
fasting glucose at follow-up, but significantly more had developed diabetes (15.6%
vs 2.2%) (11).
5.9.6 Diabetes and Kidney Donation
Traditional guidance has suggested that individuals with diabetes should not donate
a kidney. However, in an observational study of 444 donors from a single Japanese
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
102
centre that has accepted subjects with an abnormal OGTT, including a small number
with diabetes, no difference was found in the rate of immediate post-operative
complications or survival at 20 years between the glucose tolerant and intolerant
groups. Through self-reporting of status at follow-up, no major diabetic
complications were observed in the glucose intolerant group (12).
Consideration of a diabetic as a potential donor requires a thorough evaluation of
the risks and benefits of donation and transplantation, for both the donor and
recipient. Specifically, a careful search should be made for any evidence of target
organ damage and assessment of cardiovascular risk factors such as obesity,
hypertension and hyperlipidaemia. The age of the donor, donor GFR, and the
relationship to the potential recipient are critical factors. After exclusion of pre-
existing diabetic nephropathy, possibly including renal biopsy, the potential risk of
development of diabetic nephropathy should be discussed with the potential donor
(13,14).
5.9.6 Risk of Diabetes Causing ESRD in Living Kidney Donors
An important consideration for a potential kidney donor is the risk of developing
nephropathy should they subsequently develop type 2 diabetes. There is a sharp
increase in the incidence of type 2 diabetes after the age of 50 and the median age
at diagnosis is around 60 years. Less than 1% of Europeans with type 2 diabetes
develop ESRD but the incidence is higher in other ethnic groups (15). There is,
however, a 50% cumulative incidence of proteinuria after type 2 diabetes has been
present for 20 years (16) which may become an issue for kidney donors who have
an above average life expectancy and who may expect to live into their 80s (17).
In a large survey of living kidney donors in the United States, Ibrahim et al found
that the self-reported prevalence of diabetes was 5.2% in the 2,954 patients who
responded. The vast majority of kidney donors where white, about 50% were
genetically related to the recipient. The eGFR and the rate of decline of eGFR were
not significantly different between diabetic and matched non-diabetic donors. In this
study, 11 donors developed ESRD requiring dialysis or transplantation, of which
none were due to diabetic kidney disease (18).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
103
Similar reassurance comes from a review from the Organ Procurement and
Transplantation Network and the Center for Medicare and Medicaid Services
databases. These identified 126 cases of ESRD post-kidney donation from 56,458
living donors across the USA between 1987 and 2003. The median time to ESRD
after donation was 10.4 years and glomerulonephritis was considered to be the
cause in 33%, hypertension in 25%, and diabetes in 9% (19).
In conclusion, diabetic nephropathy in a kidney donor is not common during the
follow-up periods reported in the published literature. It is, however, quite possible
that this may not be the case with longer follow-up, particularly in younger donors
and in minority ethnic groups (20).
References
1. World Health Organisation (WHO) / International Diabetes Federation:
Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia,
2006.
http://www.who.int/diabetes/publications/Definition%20and%20diagnosis%20o
f%20diabetes_new.pdf
2. WHO: Use of glyclated haemoglobin (HbA1c) in the diagnosis of diabetes
mellitus http://www.who.int/diabetes/publications/diagnosis_diabetes2011/en/
3. Diabetes Care 2015; 38 (Suppl 1): S8-16.
4. Green A, Gale G. The aetiology and pathogenesis of IDDM - an epidemiological
perspective. In: Williams R, Papoz L, Fuller J, eds. Diabetes in Europe. London:
John Libbey & Company Ltd, 1994; 11-20.
5. Seaquist ER, Goetz FC, Rich S, Barbosa J. Familial clustering of diabetic kidney
disease: evidence for genetic susceptibility to diabetic nephropathy. N Engl J
Med 1989; 320: 1161-5.
6. Harris MI. Undiagnosed NIDDM: clinical and public health issues. Diabetes
Care 1993; 16: 642-57.
7. Williams DRR, Wareham NJ, Brown DC, et al. Glucose intolerance in the
community; the Isle of Ely Diabetes Project. Diabetic Med 1995; 12: 30-5.
8. Pierce M, Keen H, Bradley C. Risk of diabetes in offspring of parents with non-
insulin dependent diabetes. Diabetic Med 1995; 12: 6-13.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
104
9. Morris RD, Rimm DL, Hartz AJ, Karlhoff RK, Rimm AA. Obesity and heredity in
the etiology of non-insulin-dependent diabetes mellitus in 32,662 adult white
women. Am J Epidemiol 1989; 130: 112-21.
10. Hippisley-Cox J, Coupland C, Robson J, Sheikh A, Brindle P. Predicting risk of
type 2 diabetes in England and Wales: prospective derivation and validation of
QDScore. Br Med J 2009; 338: b880.
11. Chandran S, Masharani U, Webber AB, Wojciechowski DM. Prediabetic living
kidney donors have preserved kidney function at 10 years after donation.
Transplantation 2014; 97: 748-54.
12. Okamoto M, Suzuki T, Fujiki M, et al. The consequences for live kidney donors
with preexisting glucose intolerance without diabetic complication: analysis at a
single Japanese center. Transplantation 2010; 89: 1391-5.
13. Simmons D, Searle M. Risk of diabetic nephropathy in potential living related
kidney donors. Br MedJ 1998; 316: 846-8.
14. Kasiske BL, Ravenscraft M, Ramos EL, Gaston RS, Bia MJ, Danovitch GM.
The evaluation of living renal transplant donors: clinical practice guidelines.
JASN 1996; 7: 2288-313.
15. Fabre J, Balant LP, Dayer PG, Fox HM, Vernet AT. The kidney in maturity onset
diabetes mellitus: a clinical study of 510 patients. Kidney Int 1998; 35: 681-7.
16. Borch-Johnsen K. Renal disease in diabetes. In: Williams R, Papoz L, Fuller J,
eds. Diabetes in Europe. London: John Libbey & Company Ltd, 1994; 56-60.
17. Fehrman-Ekholm I, Elinder CG, Stenbeck M, Tyden G, Groth CG. Kidney
donors live longer. Transplantation 1997; 64: 976-8.
18. Ibrahim HN, Kukla A, Cordner G, Bailey R, Gillingham K, Matas AJ. Diabetes
after kidney donation. Am J Transplant 2010; 10: 331-7
19. Cherikh WS, Young CJ, Kramer BF, Taranto SE, Randall HB, Fan PY. Ethnic
and gender related differences in the risk of end-stage renal disease after living
kidney donation. Am J Transplant 2011; 11: 1650-5.
20. Steiner RW, Ix JH, Rifkin DE, Gert B. Estimating risks of de novo kidney
diseases after living kidney donation. Am J Transplant 2014; 14: 538-44.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
105
5.10 CARDIOVASCULAR EVALUATION
Recommendations
There is no evidence to support the routine use of stress testing in the
assessment of the potential donor at low cardiac risk. (C2)
Potential kidney donors with a history of cardiovascular disease, an
exercise capacity of <4 metabolic equivalents (METS) or with risk
factors for cardiovascular disease should undergo further evaluation
before donation. (C2)
For higher risk potential donors, stress testing is recommended by
whichever method is locally available or by CT calcium scoring . (C2)
Discussion with and/or review by cardiologists, anaesthetists and the
transplant MDT is recommended as part of the clinical assessment of
donors with higher cardiovascular and peri-operative risk. (D2)
Cardiovascular assessment before donation has two purposes. First, it identifies
prospective donors with higher than average risk of peri-operative complications
who may be unsuitable for donation. Second, it provides an opportunity to assess
the cardiovascular risk factors of a donor, to consider the long-term effects of kidney
donation, and to act to reduce the progression of cardiac disease.
5.10.1 Role of Screening Electrocardiogram
Electrocardiography complements the clinical assessment and may indicate the
presence of pre-existing ischaemic heart disease or cardiomyopathy. The latter is
important as cardiomyopathies, particularly hypertrophic cardiomyopathy (incidence
1:500), are the most common cause of sudden cardiac death in apparently healthy
young people (1). Particular attention needs to be given to the presence of
pathological Q waves (>25% R wave height), left bundle branch block, voltage
criteria for left ventricular hypertrophy, pathological T wave changes, and atrial
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
106
arrhythmias. Any abnormality should trigger formal assessment, which is likely to
include echocardiography and a cardiology opinion. A normal electrocardiogram,
whilst reassuring, does not exclude coronary artery disease.
5.10.2 Screening Patients with Established Overt Cardiac Disease
Every attempt should be made to ensure that potential living kidney donors are not
exposed to significant or unavoidable risk. As such the threshold for refusal on
health grounds must be relatively low and the presence of overt cardiac disease will
exclude most individuals as potential donors. The specific issues surrounding
hypertension and diabetes are dealt with elsewhere (sections 5.8 and 5.9).
In terms of cardiac disease, a detailed history and examination should be carefully
focused to uncover existing problems. It is important that further assessment is
sought for those individuals excluded due to symptoms or signs of existing disease.
This will usually be involve referral to a cardiologist so that current best practice may
be ensured.
5.10.3 Screening for Occult Cardiac Disease
Although there are challenges with the management of overt disease, it is even more
difficult to produce clear guidance for asymptomatic individuals. As the positive
predictive value of any test is dependent upon the risk within the population being
studied, there is a significant danger that screening of low risk individuals will
produce a large number of false positive results. This will expose potential living
kidney donors to unnecessary anxiety and result in further investigation which may
be invasive or use ionising radiation. Some potential donors who would have been
at low risk of complications will withdraw, or be withdrawn from the donation process
for no justifiable cause. Further testing will also lead to an additional economic
burden upon the healthcare system.
There are various methods to estimate cardiovascular risk in people without known
disease (for example QRISK 2 (2) and the Framingham Coronary Heart Disease
Risk Score (3)). These risk calculators variably use factors such as age, smoking
status, presence of hypertension or diabetes, family history and cholesterol to
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
107
predict the risk of a new cardiovascular event over a period of time, usually 10 years.
Although this will identify higher risk potential donors, there is no evidence to support
a specific risk threshold above which further investigation is required or donation
should not occur. Each case should be considered individually. The most commonly
used method to predict peri-operative cardiovascular risk, the Lee index, includes
factors such as previous ischaemic heart disease, congestive cardiac failure and
diabetes and is therefore not applicable to the low risk donor population (4).
Assessment of functional capacity, either by self-reporting of exercise capacity or
measured by cardiopulmonary exercise testing, can predict peri-operative
cardiovascular mortality and long-term outcomes (5,6). The ability to undertake
activities that require more than 4 METS, for example moderate cycling and jogging,
is associated with a low peri-operative risk. There are no data to support a level of
functional status, reported or measured, that either requires further evaluation or
excludes donation. However, a functional capacity of >4 METS and without the
cardiovascular risk factors listed above would predict a low risk of peri-operative
cardiovascular events.
If potential donors have a high predicted risk of cardiovascular disease and/or poor
functional capacity, further evaluation should be undertaken. However, there are no
data to inform the most appropriate method to detect or exclude coronary artery
disease in an asymptomatic population. Whichever method of stress testing is used
is likely to give false positive results in this population, and the negative predictive
value will be unknown.
CT coronary calcium scoring can be used to assess risk of coronary atherosclerotic
disease. Using this technique in an asymptomatic individual, a coronary calcium
score of zero effectively excludes significant coronary atherosclerosis and obviates
the need for further structural or functional assessments The technique has recently
been recommended by NICE as the most appropriate screening technique in
patients presenting to a rapid access chest pain clinic in whom the clinical suspicion
of significant coronary atherosclerosis is low (7). It should be re-emphasised,
however, that no evidence currently exists to support the hypothesis that donor
candidates at low risk of cardiac events should undergo additional pre-operative
cardiac evaluation before donation (8).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
108
5.10.4 Screening for Non-Coronary Pathology
A combination of clinical assessment and 12 lead surface ECG has a reasonable
sensitivity for the detection of non-coronary cardiac pathology. There is an extensive
literature on the pre-participation screening of high performance athletes and in this
group of young, fit people there is little incremental benefit from routine
echocardiography. However, this may not be true in an older cohort. Currently there
is no consensus regarding the definition of a “high risk” cohort and the role of routine
echocardiography in potential living kidney donors who have no clinical or
electrocardiographic abnormalities is unclear.
5.10.5 Conclusion
There is no evidence to support cardiac stress testing or invasive testing in potential
donors at low cardiac risk. However, a low threshold should be set for formal cardiac
investigation and for the exclusion of individuals at higher risk. As well as
determining suitability for donation, the assessment process should provide an
opportunity to identify and correct recognised cardiovascular risk factors. The choice
of stress test will be influenced by local service provision. CT coronary calcium
scoring may be an alternative way of stratifying coronary risk.
References
1. Maron BJ, Shirani J, Poliac LC, Mathenge R, Roberts WC, Mueller FO. Sudden
death in young competitive athletes. Clinical, demographic, and pathological
profiles. JAMA 1996; 276: 199-204.
2. Hippisley-Cox J, Coupland C, Vinogradova Y, et al. Predicting cardiovascular
risk in England and Wales: prospective derivation and validation of QRISK2. Br
Med J 2008; 336: 1475-82.
3. D'Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk
profile for use in primary care: the Framingham Heart Study. Circulation 2008;
117: 743-53.
4. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective
validation of a simple index for prediction of cardiac risk of major noncardiac
surgery. Circulation 1999; 100: 1043-9.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
109
5. Reilly DF, McNeely MJ, Doerner D, et al. Self-reported exercise tolerance and
the risk of serious perioperative complications. Arch Intern Med 1999; 159:
2185-92.
6. Snowden CP, Prentis JM, Andreson Hl, et al. Submaximal cardiopulmonary
exercise testing predicts complications and hospital length of stay in patients
undergoing major elective surgery. Ann Surg 2010; 251: 535-41.
7. NICE guideline. Chest pain of recent onset: assessment and diagnosis. June
2016. https://www.nice.org.uk/guidance/gid-cgwave0827/documents/short-
version-of-draft-guideline
8. Lam NN, Lentine KL, Garg AX. Renal and cardiac assessment of living kidney
donor candidates. Nat Rev Nephrol 2017; 13: 420-8.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
110
5.11 PROTEINURIA
Recommendations
Urine protein excretion needs to be quantified in all potential living
donors. (B1)
A urine albumin/creatinine ratio (ACR) performed on a spot urine
sample is the recommended screening test, although urine
protein/creatinine ratio (PCR) is an acceptable alternative. (A1)
ACR >30 mg/mmol, PCR >50 mg/mmol, albumin excretion >300 mg/day
or protein excretion >500 mg/day represent absolute contraindications
to donation. (C2)
The significance of moderately increased albuminuria (ACR 3-30
mg/mmol) and proteinuria (PCR 15-50 mg/mmol or 24-hour urine
protein 150-500 mg/day) has not been fully evaluated in living kidney
donors. However, since the risk of CKD and cardiovascular morbidity
increase progressively with increasing albuminuria or proteinuria such
levels are a relative contraindication to donation. (C2)
Proteinuria should be quantified in all potential living kidney donors. Increased
urinary protein excretion is a marker of kidney damage, reflecting either increased
glomerular permeability (albuminuria) or decreased tubular reabsorption (low
molecular weight proteinuria). Proteinuria may also be a manifestation of conditions
other than kidney disease such as lymphoproliferative disorder (overflow
proteinuria) or lower urinary tract disease (post-renal proteinuria).
Proteinuria is an important risk factor for both chronic kidney disease (1,2) and
cardiovascular morbidity and mortality (3). In particular, proteinuria predicts both the
progression of CKD and cardiovascular events in patients with established CKD,
established cardiovascular disease, and patients with diabetes (3,4). Proteinuria
also predicts the development of CKD and cardiovascular disease in those without
medical co-morbidities.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
111
A recent meta-analysis based on data from nearly five million healthy people
identified from seven general population cohorts in the US found that each 10-fold
increase in urinary ACR was associated with three times the risk of ESRD over a
median follow-up of 4 to 16 years, although this finding was not statistically
significant (5). The projected risk of ESRD was higher among people with additional
risk factors, including middle age, male gender, black ethnicity and smokers, than
among those without additional risk factors.
5.11.1 Methods of Testing for Proteinuria
Historically, abnormal proteinuria has been defined as the excretion of more than
150 mg of total protein per day. However, early renal disease may be reflected by
lesser degrees of proteinuria, and particularly by increased albuminuria. The normal
rate of albumin excretion is <10 mg per day in healthy young adults and increases
with age and with increased body weight. Persistent albumin excretion between 30
and 300 mg/day is termed moderately increased albuminuria (formerly known as
"microalbuminuria") and in non-diabetic patients is associated with an increased risk
of cardiovascular disease (3). An albumin excretion >300 mg/day is considered
overt proteinuria or severely increased albuminuria (formerly known as
"macroalbuminuria"), and is the level at which the standard urine dipstick becomes
positive. It should be noted that the standard urine dipstick primarily detects albumin
and is relatively insensitive to non-albumin proteins. Furthermore, the dipstick is
insensitive to low levels of albumin excretion with a lower limit of detection of
approximately 10-20 mg/dL. Thus patients with moderately increased albuminuria
or low molecular weight proteinuria may be missed if this is the sole method of
detection.
The gold standard for measurement of protein excretion is a 24-hour urine collection,
but this is cumbersome for patients and often collected inaccurately. Hence the urine
albumin /creatinine ratio (ACR) or protein /creatinine ratio (PCR) in a spot urine
sample are now the preferred methods as both correlate well with 24-hour urinary
protein excretion and overcome inaccuracies related to incomplete urine collection.
Both are supported by Kidney Disease: Improving Global Outcomes (KDIGO) (6) as
appropriate methods to aid in the diagnosis of chronic kidney disease, but ACR is
preferred by both KDIGO and the National Institute for Health and Care Excellence
(NICE) as it has greater sensitivity than PCR for low levels of proteinuria (7). Table

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
112
5.11.1 provides a summary of the comparative values detected using these
screening methods.
Table 5.11.1 Expressions of Urinary Protein Concentration and their
Approximate Equivalents and Clinical Correlates
(adapted from reference 5)
Albuminuria
category
Dipstick
reading
PCR
(mg/mmol)
Total
protein
(mg/24h)
ACR
(mg/mmol)
Albumin
excretion
(mg/24h)
Normal to
mildly
increased
(A1)
Negative
to trace
<15
<150
<3
<30
Moderately
increased
(A2)
Trace to +
15-50
150-500
3-30
30-300
Severely
increased
(A3)
+ or
greater
>50
>500
>30
>300
5.11.2 Assessment of Proteinuria in Living Donors
There is uncertainty regarding the threshold of proteinuria that precludes kidney
donation. In 2005 the Amsterdam Forum concluded by consensus that a 24-hour
urinary protein excretion of >300 mg is a contraindication to donation (8). According
to a 2007 survey among US transplant centres, the most common exclusion criterion
for kidney donors was 300 mg/day proteinuria, but almost as many centres were
using a protein excretion of 150 mg/day as a cut-off (9).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
113
Albumin excretion >30 mg/day (ACR >3 mg/mmol) is associated with an increased
risk for complications of CKD. A meta-analysis by the CKD Prognosis Consortium
demonstrated associations of an ACR >3 mg/mmol or reagent strip +1 protein with
a subsequent risk of all-cause and cardiovascular mortality, kidney failure, acute
kidney injury, and CKD progression in the general population and in populations with
increased risk for CVD (3,10,11). ACR is associated with an increased risk of
mortality linearly on the log-log scale, without threshold effects. For this reason,
although the significance of moderately increased albuminuria has not been fully
evaluated in living kidney donors, raised albumin excretion would currently
constitute at least a relative contraindication to donation, although other risk factors
for ESRD may be taken into account. Severely increased proteinuria (ACR >30
mg/mmol, PCR >50 mg/mmol, albumin excretion >300 mg/day, or protein excretion
>500 mg/day) constitute an absolute contraindication to donation.
Orthostatic proteinuria should not be considered as a contraindication to donation.
Orthostatic proteinuria appears benign (12), but a confident diagnosis requires an
ACR on a spot urine sample voided immediately after waking.
There are few studies examining either the renal or cardiovascular outcome for living
kidney donors who have donated despite pre-existing low level proteinuria. In many
donors there is a modest increase in urine protein excretion after nephrectomy, the
majority of whom have no evidence of accelerated GFR loss over time (13-16). In
one study, five donors with low-grade proteinuria (mean 210 mg in a 24 hr urine
collection) were more likely to have significant proteinuria 20 years or more after
donation (>800 mg/day), although without significant loss of kidney function (17). A
review of 1,519 living kidney donors in Japan identified eight who developed ESRD
(18). Of these, only two had pre-donation proteinuria, both of whom developed
cardiovascular disease, hypertension and ESRD 6 and 16 years after donation. A
recent US study among 4,650 living donors found that by 7 years post-donation,
after adjustment for age and sex, greater proportions of black compared with white
donors had chronic kidney disease (12.6% vs 5.6%), proteinuria (5.7% vs 2.6%) or
nephrotic syndrome (1.3% vs 0.1%), suggesting the need for more stringent risk
stratification among black donors (19).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
114
References
1. Iseki K, Ikemiya Y, Iseki C, Takishita S. Proteinuria and the risk of developing
end-stage renal disease. Kidney Int 2003; 63: 1468-74.
2. Halbesma N, Kuiken DS, Brantsma AH, et al. Macroalbuminuria is a better risk
marker than low estimated GFR to identify individuals at risk for accelerated
GFR loss in population screening. J Am Soc Nephrol 2006; 17: 2582-90.
3. Matsushita K, van der Velde M, Astor BC, et al. Association of estimated
glomerular filtration rate and albuminuria with all-cause and cardiovascular
mortality in general population cohorts: a collaborative meta-analysis. Lancet
2010; 375: 2073-81.
4. Brantsma AH, Bakker SJ, de Zeeuw D, et al. PREVEND study group. Extended
prognostic value of urinary albumin excretion for cardiovascular events. J Am
Soc Nephrol 2008; 19: 1785-91.
5. Grams ME, Sang Y, Levey AS, et al. Kidney-failure risk projection for the living
kidney-donor candidate. N Engl J Med 2016; 374: 2094-5.
6. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group.
KDIGO 2012 Clinical practice guideline for the evaluation and management of
chronic kidney disease. Kidney Int Suppl 2013; 3: 1-150.
7. National Institute for Health and Care Excellence (2014). Chronic kidney
disease in adults: assessment and management. NICE guideline (CG182).
https://www.nice.org.uk/guidance/cg182
8. Delmonico F. Council of the Transplantation Society. A report of the Amsterdam
Forum on the care of the live kidney donor: data and medical guidelines.
Transplantation 2005; 79 (6 Suppl): S53-66.
9. Mandelbrot DA, Pavlakis M, Danovitch GM, et al. The medical evaluation of
living kidney donors: a survey of US transplant centers. Am J Transplant 2007;
7: 2333-43.
10. Gansevoort RT, Matsushita K, van der Velde M, et al. Lower estimated GFR
and higher albuminuria are associated with adverse kidney outcomes. A
collaborative meta-analysis of general and high-risk population cohorts. Kidney
Int 2011; 80: 93-104.
11. van der Velde M, Matsushita K, Coresh J, et al. Lower estimated glomerular
filtration rate and higher albuminuria are associated with all cause and
cardiovascular mortality. a collaborative meta-analysis of high-risk population
cohorts. Kidney Int 2011; 79: 1341-52.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
115
12. Springberg PD, Garrett LE Jr, Thompson AL Jr, et al. Fixed and reproducible
orthostatic proteinuria: results of a 20-year follow-up study. Ann Intern Med
1982; 97: 516-9.
13. Fehrman-Ekholm I, Dunér F, Brink B, et al. No evidence of accelerated loss of
kidney function in living kidney donors: results from a cross-sectional follow-up.
Transplantation 2001; 72: 444-9.
14. Garg AX, Muirhead N, Knoll G, et al. Donor Nephrectomy Outcomes Research
(DONOR) Network. Proteinuria and reduced kidney function in living kidney
donors: a systematic review, meta-analysis and meta-regression. Kidney Int
2006; 80: 1801-10.
15. Gossmann J, Wilhelm A, Kachel HG, et al. Long-term consequences of live
kidney donation follow-up in 93% of living kidney donors in a single transplant
center. Am J Transplant 2005; 5: 2417-24.
16. Ibrahim HN, Foley R, Tan L, Rogers, et al. Long-term consequences of kidney
donation. N Engl J Med 2009; 360: 459-69.
17. Goldfarb DA, Matin SF, Braun WE, et al. Renal outcome 25 years after donor
nephrectomy. J Urol 2001; 166: 2043-7.
18. Kido R, Shibagaki Y, Iwadoh K, et al. How do living kidney donors develop end-
stage renal disease? Am J Transplant 2009; 9: 2514-9.
19. Lentine KL, Schnitzler MA, Garg AX, et al. Race, relationship and renal
diagnoses after living kidney donation. Transplantation 2015; 99: 1723-9.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
116
5.12 NON-VISIBLE HAEMATURIA
Recommendations
All potential living donors must have reagent strip (dipstick) urinalysis
performed on at least two separate occasions. (B1)
Two or more positive tests, including trace positive, is considered as
persistent non-visible haematuria (PNVH). (B1)
If PNVH is present, perform urine culture and renal imaging to exclude
common urologic causes including infection, nephrolithiasis and
urothelial carcinoma. (A1)
If no cause is found, perform cystoscopy in patients age >40 years to
exclude bladder pathology. (B1)
If no cause is found and the donor still wishes to donate, then a kidney
biopsy is recommended if haematuria is 1+ or greater on dipstick
testing. (B1)
Glomerular pathology precludes donation, with the possible exception
of thin basement membrane disease. (B1)
For donors with persistent asymptomatic non-visible haematuria
(PANVH) and a family history of haematuria or X-linked Alport
syndrome, a renal biopsy (B1) and referral to a clinical geneticist are
recommended. (B2)
Non-visible haematuria is the preferred term (replacing microscopic haematuria) for
blood identified in a urine sample either by microscopy or by reagent strip analysis.
Non-visible haematuria is a common finding in the general population, may indicate
either urological or renal parenchymal disease, and must be carefully evaluated in
prospective living kidney donors.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
117
5.12.1 Detection of Non-Visible Haematuria
Non-visible haematuria is routinely detected using semi-quantitative reagent strips.
A reagent strip ‘trace positive’ result corresponds to 1-5 red cells/l, while >10 red
cells/l are conventionally considered to be significant in urological practice (1). In
the UK urine microscopy is not recommended to confirm the presence of haematuria
(2) and indeed often produces false negative results, although the detection of
dysmorphic red cells and red cell casts may be useful to identify glomerular
haematuria. Potential living donors must have reagent strip urinalysis performed on
at least two occasions not related to fever, menstruation or exercise. If two out of
three consecutive tests are positive then the donor is considered to have persistent
non-visible haematuria.
Non-visible haematuria is present in 1-21% of the general population, the
prevalence increasing with age (3-7). Most patients are asymptomatic with no
urologic symptoms, no proteinuria and normal renal function. Subsequent urine
testing is often normal. Such transient haematuria is generally considered
insignificant, although with little supporting evidence from longitudinal studies. In
one report including 432 patients with normal urological investigation who were
followed for 5.8 +/- 4.4 years, haematuria disappeared in 44%, none of whom
developed proteinuria or renal impairment (8). In a smaller study of 49 patients
investigated for non-visible haematuria, those in whom haematuria disappeared all
had a normal kidney biopsy (9).
5.12.2 Persistent Asymptomatic Non-Visible Haematuria (PANVH)
PANVH is present in about 25% of those with an initial positive test (3-10)
and, in
two single centre reports, 2.7% and 8.3% of potential living kidney donors in the US
and Japan respectively (11,12). Malignant disease of the urinary tract, present in 3-
5% of patients overall (13,14), is rare under the age of 40 but diagnosed in up to
10% of those aged >60. In patients with normal urological investigations, kidney
biopsy is frequently abnormal. In a UK-based study of 165 patients, 77 (46%) were
found to have glomerular pathology, most commonly IgA nephropathy, mesangial
proliferative glomerulonephritis without IgA deposition, or thin basement membrane
nephropathy (15). Similar pathology has been demonstrated in a Dutch study where
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
118
29 out of 49 biopsies were abnormal (9), a Korean study in which only 10 out of 156
biopsies were normal (16), a Japanese study in which all of 56 biopsies were
abnormal (17), and in a US study of potential living donors with PANVH in which 8
out of 10 biopsies were abnormal (11).
Longitudinal studies have confirmed the importance of PANVH. In the Dutch study
of 49 patients, those with a normal biopsy developed neither proteinuria nor
worsening renal function during 11 years of follow-up. In contrast, proteinuria
(10 patients), hypertension (14) and worsening kidney function (4) were found in the
29 patients with an abnormal biopsy (9). In a Japanese study of 242 living donors,
8.3% had PANVH before donation and 15.3% following donation. None were
investigated with a kidney biopsy, but the presence of haematuria predicted the
development of proteinuria during a median follow-up of 2.3 years (12). In a similar
study including patients from the Japanese general population, 10% of those with
PANVH developed proteinuria over a median follow-up of 5.8 years (8).
The above supports current practice that persistent asymptomatic non-visible
haematuria should be investigated in potential living kidney donors, both to exclude
urological disease and to identify glomerular pathology that would preclude
donation. However, there remain uncertainties: in particular, the relevance of low
levels of haematuria (‘trace’ positive), and the importance of thin basement
membrane nephropathy (TBMN) merit further discussion.
5.12.3 ‘Trace’ Microscopic Haematuria
A reagent strip ‘trace positive’ result corresponds to 1-5 red cells/µL (1). Existing
studies rarely, if ever, distinguish between the degrees of non-visible haematuria
recorded on dipstick testing. As the incidence of significant disease following the
investigation of trace positive haematuria is no different to that of control
populations, recent primary care (2) and Urology guidelines in the UK have
recommended that trace non-visible haematuria be considered a normal variant
(18). However, glomerular pathology has been reliably identified in potential living
donors using thresholds of even 1 or 3 red cells/l (11,12). No studies have directly
addressed the threshold below which investigation of the potential donor is
unnecessary, and a balance must be struck between the risk of missing significant
renal disease in a potential donor, against the inconvenience and risk of biopsy.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
119
High degrees of non-visible haematuria (1+ or greater) mandate biopsy before
donation, but trace haematuria is at present a relative indication.
If, after counselling, the prospective donor with non-visible haematuria remains
committed to donation and a kidney biopsy is performed, histological evaluation
must include immunofluorescence or immunohistochemistry, and electron
microscopy.
Considerable evidence also suggests that cystoscopy is of limited value in the
investigation of non-visible haematuria below the age of 40 years, especially in
women, and this is reflected in current UK guidelines (18). Risk factors for uro-
epithelial cancer should be assessed including donor age, smoking history,
exposure to aniline dye, analgesics or cyclophosphamide, and pelvic irradiation. In
younger asymptomatic patients, it is reasonable to discuss the risk/benefit ratio of
cystoscopy with the prospective donor. Above the age of 40 years, however, the
increased incidence of urological disease mandates a full urological assessment,
including cystoscopy.
5.12.4 Thin Basement Membrane Nephropathy
Thin basement membrane nephropathy (TBMN) is an autosomal dominant disorder
often associated with mutations in either the COL4A3 or COL4A4 genes (encoding
the 3 and 4 chains of type 4 collagen). Individuals in whom both alleles of either
gene are abnormal may have autosomal recessive Alport syndrome, and TBMN can
be regarded as the carrier state for this condition. TBMN is present in 10-50% of
patients biopsied for PANVH
(9,11,15,16) and although often considered a benign
diagnosis may carry some risk of progression. Both proteinuria (10-20% of patients)
and renal impairment (5%) have been described (19-21), often associated with
additional pathological abnormalities including FSGS
(21,25) or IgA nephropathy
(22,23)
(both of which would preclude donation). A recent study of Greek-Cypriot
families with familial haematuria identified COL4A3 or COL4A4 mutations in 16/57
families (28.1%), and in this population 10/87 (11.5%) heterozygous patients
developed ESRD (24, 25).
Many individuals with TBMN but otherwise normal investigations have undoubtedly
donated kidneys, either knowingly
(11) or unknowingly (12), and although adverse
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
120
outcomes have not been reported these donors must be made aware of uncertainty
over long-term safety. Recently published consensus guidelines recommend a renal
biopsy (to exclude FSGS-like lesions associated with progression to ESRD) and
referral to a clinical geneticist for genetic testing, especially when donating to a
family member with unexplained kidney failure or where there is a family history of
sensori-neural deafness or haematuria (26 - see also section 5.17 Familial Renal
Disease). Referral to a geneticist is mandatory in potential donors of Cypriot origin.
TBMN must be distinguished from the carrier state of X-linked Alport syndrome
(XLAS - caused by mutations in the COL4A5 gene encoding the α5 chain of type 4
collagen), which is associated with a 5-20% risk of progressive renal impairment
(27,28) and generally considered to prohibit donation (26). A recent study describing
six XLAS carriers who donated kidneys to their affected children supports this view
(29). A decline in kidney function of between 25% and 60% was observed in four of
the six donors over 2-14 years of follow-up, although in no case was creatinine
clearance <40 mL/min. Four of the six developed microalbuminuria or proteinuria
and four developed hypertension. Some have argued that, if no other donor can be
found, women with XLAS who are over the age of 45, have normal kidney function,
no proteinuria and no hearing deficiency (both risk factors for progression to end-
stage kidney disease) might be considered as donors after appropriate counselling
(26,30). Involvement of a clinical geneticist and renal biopsy would be mandatory in
the screening of such a potential donor.
References
1. Freni SC, Heederik GJ, Hol C. Centrifugation techniques and reagent strips in
the assessment of microhematuria. J Clin Pathol 1977; 30: 336-40.
2. Chronic kidney disease in adults: assessment and management. NICE
guideline CG182 (2014): www.nice.org.uk/guidance/cg182
3. Topham PS, Jethwa A, Watkins M, Rees Y, Feehally J. The value of urine
screening in a young adult population. Fam Pract 2004; 21: 18-21.
4. Mohr DN, Offord KP, Owen RA, Melton LJ. Asymptomatic microhematuria and
urologic disease: a population based study. JAMA 1986; 256: 224-9.
5. Messing EM, Young TB, Hunt VB. Home screening for haematuria: results of a
multiclinic study. J Urol 1992; 148: 289-92.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
121
6. Froom P, Ribak J, Benbassat J. Significance of microhematuria in young adults.
Br Med J 1984; 288: 20-2.
7. Vivante A, Afek A, Frenkel-Nir Y, et al. Persistent asymptomatic isolated
microscopic hematuria in Israeli adolescents and young adults and risk for end-
stage renal disease. JAMA 2011; 306: 729-36
8. Yamagata K, Kobayashi M, Koyama A. A long-term follow up study of
asymptomatic haematuria and/or proteinuria in adults. Clin Nephrol 1996; 45:
281-8.
9. Nieuwhof C, Doorenbos C, Grave W. A prospective study of the natural history
of idiopathic non-proteinuric haematuria. Kidney Int 1996; 49: 222-5.
10. Jaffe JS, Ginsberg PC, Gill R, Harkaway RC. A new diagnostic algorithm for the
evaluation of microscopic haematuria. Urology 2001; 57: 889-94.
11. Koushik R, Garvey C, Manivel C, Matas AJ, Kasiske B. Persistent,
asymptomatic microscopic hematuria in prospective kidney donors.
Transplantation 2005; 80: 1425-9.
12. Kido R, Shibagaki Y, Iwadoh K, et al. Persistent glomerular haematuria in living
kidney donors confers a risk of progressive kidney disease in donors after
heminephrectomy. Am J Transplant 2010; 10: 1597-604.
13. Khadra MH, Pickard RS, Charlton M, Powell PH, Neal DE. A prospective
analysis of 1,930 patients with haematuria to evaluate current diagnostic
practice. J Urol 2000; 163: 524-7.
14. Edwards TJ, Dickinson AJ, Natale S, Gosling J, McGrath JS. A prospective
analysis of the diagnostic yield resulting from the attendance of 4020 patients
at a protocol-driven haematuria clinic. BJU Int 2006; 97: 301-5.
15. Topham PS, Harper SJ, Furness PN, Harris KPG, Walls J, Feehally J.
Glomerular disease as a cause of isolated microscopic haematuria. Q J Med
1994; 87: 329-35.
16. Kim BS, Kim YK, Shin YS, et al. Natural history and renal pathology in patients
with isolated microscopic haematuria. Korean J Intern Med 2009; 24: 356-61.
17. Hoshino Y, Kaga T, Abe Y, et al. Renal biopsy findings and clinical indicators of
patients with hematuria without overt proteinuria. Clin Exp Nephrol 2015; 19:
918-24.
18. Kelly JD, Fawcett DP, Goldberg LC. Assessment and management of non-
visible haematuria in primary care. Br Med J 2009; 338: 227-32.
19. Savige J, Rana K, Tonna S, Buzza M, Dagher H, Wang YY. Thin basement
membrane nephropathy. Kidney Int 2003; 64: 1169-78.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
122
20. Auwardt R, Savige J, Wilson D. A comparison of the clinical and laboratory
features of thin basement membrane disease (TBMD) and IgA
glomerulonephritis (IgA GN). Clin Nephrol 1999; 52: 1-4.
21. van Passen P, van Breda Vriesman PJ, van Rie H, Tervaert JW. Signs and
symptoms of thin basement membrane nephropathy: a prospective regional
study on primary glomerular disease - the Limburg Renal Registry. Kidney Int
2004; 66: 909-13.
22. Cosio FG, Falkenhein ME, Sedmark DD. Association of thin glomerular
basement membrane with other glomerulopathies. Kidney Int 1996; 46: 471-4.
23. Berthoux FC, Laurent B, Alamartine E, Diab N. A new subgroup of primary IgA
nephritis with thin glomerular basement membrane (GBM): syndrome or
association. Nephrol Dial Transplant 1996; 11: 558-61.
24. Papazachariou L, Demosthenous P, Peri M, et al. Frequency of
COL4A3/COL4A4 mutations amongst families segregating glomerular
microscopic haematuria and evidence for activation of the unfolded protein
response. Focal and segmental glomerulosclerosis is a frequent development
during ageing. PLoS ONE 2014; 9: e115015.
25. Voskarides K, Damianou L, Neocleous V, et al. COL4A3/COL4A4 mutations
producing focal segmental glomerulosclerosis and renal failure in thin basement
membrane nephropathy. J Am Soc Nephrol 2007; 18: 3004-16.
26. Savige J, Gregory M, Gross O, Kashtan S, Ding J, Flinter F. Expert guidelines
for the management of Alport syndrome and thin basement membrane
nephropathy. J Am Soc Nephrol 2013; 24: 354-75.
27. Kashtan CE. Alport syndrome and the X chromosome: implications of a
diagnosis of Alport syndrome in females. Nephrol Dial Transplant 2007; 22:
1499-505.
28. Jais J, Knebelmann B, Giatras I, et al. X-linked Alport Syndrome: natural history
and genotype-phenotype correlations in girls and women belonging to 195
families: A ‘European Community Alport Syndrome Concerted Action’ Study. J
Am Soc Nephrol 2003; 14: 2603-10.
29. Gross O, Weber M, Fries JW, Muller GA. Living donor kidney transplantation
from relatives with mild urinary abnormalities in Alport syndrome: long-term risk,
benefit and outcome. Nephrol Dial Transplant 2009; 24: 1626-30.
30. Kashtan CE. Women with Alport syndrome: risks and rewards of kidney
donation. Nephrol Dial Transplant 2009; 24: 1369-70.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
123
5.13 PYURIA
Statement of Recommendation
Prospective donors found to have pyuria can only be considered for
donation if it can be demonstrated that the pyuria is due to a reversible
cause, such as an uncomplicated urinary tract infection. (C1)
Pyuria is defined as the presence of 10 or more white cells/mm
3
in a urine specimen,
three or more white cells per high-power field of unspun urine, a positive result on
Gram’s staining of an unspun urine specimen, or a urinary dipstick test that is
positive for leukocyte esterase (1). Sterile pyuria is defined as the persistent
presence of white cells in the urine in the absence of bacteria.
Sterile pyuria is relatively common, affecting 13.9% of women and 2.6% of men (2)
and can occur in patients who have already taken antimicrobials, or where there is
infection with atypical organisms. These include sexually transmitted infections such
as gonorrhoea and chlamydia, genital herpes and herpes zoster, human papilloma
virus and HIV infections; genitourinary tuberculosis; fungal infections such as
candidiasis; and parasitic infections such as trichomoniasis and schistosomiasis.
Other causes of sterile pyuria include inflammatory and autoimmune conditions
such as systemic lupus erythmatosus, Kawasaki’s disease and analgesic
nephropathy, or urological conditions such as stones, foreign bodies and stents. For
a more complete list of causes see reference 3.
The cause of the pyuria must be established before a potential donor proceeds for
further assessment (3).
In a retrospective study of 86 living kidney donors whose procedures were over 1
year ago (mean 17.24 ± 5.04 months), pyuria was found in 7 (8.1%). The cause and
longer-term outcome for these patients was not reported (4).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
124
References
1. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of
healthcare-associated infection and criteria for specific types of infections in the
acute care setting. Am J Infect Control 2008; 36: 309-32.
2. Alwall N, Lohi A. A population study on renal and urinary tract diseases: II:
urinary deposits, bacteriuria and ESR on screening and medical examination of
selected cases. Acta Med Scand 1973; 194: 529-35.
3. Wise GJ, Schlegel PN. Sterile pyuria. N Engl J Med 2015; 372: 1048-54.
4. Azar SA, Nakhjavani MR, Tarzamni MK, et al. Is living kidney donation really
safe? Transplant Proc 2007; 39: 822-3.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
125
5.14 INFECTION IN THE PROSPECTIVE DONOR
Recommendations
Screening for infection in the prospective donor is essential to identify
potential risks for the donor from previous or current infection and to
assess the risks of transmission of infection to the recipient. (B1)
Active HBV and HCV infection in the donor are usually
contraindications to living donor kidney donation; however, donors
with evidence of active viral replication may be considered under some
circumstances. (B1)
The presence of HIV or human T lymphotrophic virus (HTLV) infection
is an absolute contraindication to living donation. (B1)
Screening for HBV, HCV and HIV infection must be repeated within 30
days of donation. (Not graded)
All potential donors should be provided with dietary advice regarding
avoidance of HEV infection, and screening should be undertaken for
HEV viraemia by nucleic acid testing within 30 days of donation. (Not
graded)
The CMV status of donor and recipient must be determined before
transplantation. When the donor is CMV positive and the recipient is
CMV negative, the donor and recipient must be counselled about the
risk of post-transplant CMV disease. (B1)
The EBV status of donor and recipient must be determined before
transplantation. When the donor is EBV positive and the recipient is
EBV negative, the donor and recipient must be counselled about the
risk of developing Post Transplant Lymphoproliferative Disease. (B1)
Potential donors must be screened by history for travel or residence
abroad to assess their potential risk for having acquired endemic
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
126
infections and appropriate microbiological investigations instigated if
indicated. (Not graded)
5.14.1 Introduction
Potential living donors undergo careful screening for infectious diseases. This allows
both for identification and treatment, and minimisation of any risk associated with
transmission between donor and recipient. In many cases, donation is possible
following resolution of infection, although on specific occasions recipient monitoring
and prophylaxis might be recommended following transplantation.
The same principles that apply to deceased donors and blood donors should be
applied to the screening of living donors (1-3). Expert advice is provided on a
national basis by the Advisory Committee on the Safety of Blood, Tissues and
Organs (SaBTO) (3). All risk assessments are regularly reviewed and amended if
new relevant evidence becomes available.
Global travel and the increasing number of donors from all areas of the world has
necessitated that consideration be given to geographically relevant infections, with
which the transplant team may be unfamiliar (4). In these cases, the involvement of
a Consultant with relevant expertise should be sought to guide appropriate
assessment and investigations.
Identification of current or previous infection in the prospective donor is an important
aspect of donor evaluation. The presence of any active infection usually precludes
donation. Apart from the implications for the potential donor, a number of infections
may be transmitted by organ transplantation. Those that are of established clinical
significance are listed in Table 5.14.1.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
127
Table 5.14.1 Infections of Established Clinical Significance in
Transplantation
Viral
Herpes group viruses
Cytomegalovirus (CMV or HHV 5)
Epstein-Barr virus (EBV or HHV4)
Herpes simplex virus (HSV or HHV1 and HHV2)
Varicella-zoster virus (VZV or HHV3)
Kaposi Sarcoma virus (KSKV or HHV8)
Human immunodeficiency virus (HIV-1 and HIV-2)
Human T lymphotrophic virus (HTLV-1 and HTLV-2)
Hepatitis B virus (HBV)
Hepatitis C virus (HCV)
Hepatitis E virus (HEV)
West Nile Virus (WNV)
Bacterial
Atypical mycobacterial infections
Mycobacterium tuberculosis
Syphilis
Fungal and parasitic
Toxoplasmosis
Coccidiomycosis
Malaria
Schistosomiasis
Trypanosoma cruzi
Strongyloides
Prion-associated
Creutzfeldt-Jakob disease (CJD)
Variant Creutzfeldt-Jakob disease (vCJD)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
128
5.14.2 Evaluation of the Prospective Donor
A detailed clinical history is important and must include a psychosocial and sexual
history to define at-risk behaviour (see Table 5.4.2 in section 5.4). Prospective
donors who were born or lived in geographical areas outside the UK where there is
a high prevalence of certain infections may require additional evaluation (5). During
routine physical examination of the donor, examination of the chest and
reticuloendothelial system may reveal evidence of infection. The routine screening
investigations already outlined in Table 5.4.4 in section 5.4 include those ordinarily
required to exclude infection in the prospective donor. Particular attention should be
paid to the possibility of past tuberculosis when examining the chest X-ray. A mid-
stream urine should be cultured and examined by microscopy on at least two
occasions. If sterile pyuria is detected the cause must be identified. The presence
of eosinophilia may indicate chronic parasite infection.
The serological tests that should be performed on the prospective donor are listed
in Table 5.14.2. SaBTO recommendations state that a blood sample taken up to 30
days before organ donation is considered to meet the requirements for testing, as
long as the donor’s risk status has not changed in the time between the sample
being taken and the donation. Infections can be transmitted by both blood
transfusion and organ donation during the incubation period of the relevant organism
and before a serological response has been mounted, and is discussed further
below. Serology should not, therefore, be regarded as a substitute for a detailed
psychosexual and medical history exploring potential risk factors.
Routine testing for viral infection may, if a positive result is obtained, raise complex
ethical problems. It is important that there is full discussion with the prospective
donor before testing for viral infection, particularly for hepatitis B virus (HBV),
hepatitis C virus (HCV), and human immunodeficiency virus (HIV). A strategy for
dealing with a positive result should be formulated before testing.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
129
Table 5.14.2 Serological Testing of Donor
Routine tests for all donors
HbsAg and HBcAb
HCV IgG
HIV 1/2 Ab / HIV Ag combination assay (minimum 4
th
generation assay)
HTLV 1/2 Ab
Treponema pallidum Ab
CMV IgG
EBV IgG
Toxoplasma gondii IgG
Consider in selected cases
*Coccidiomycosis antibody
*Malaria blood film
*Schistosomiasis antibody, urine microscopy
*Trypanosoma cruzi antibody
*Strongyloides stercoralis antibody
*West Nile Virus antibody/RNA
*Where clinically indicated e.g. specific endemic (geographical) risks
5.14.3 Viral Infections in the Prospective Donor
Hepatitis B
All prospective living donors should be tested for both Hepatitis B surface antigen
(HBsAg) and Hepatitis B core antibody (HBcAb). If the HBcAb is positive, the donor
should be tested for the presence of HBV DNA and Hepatitis B surface antibody
(HBsAb). If HBsAb is >100 iU/L and HBV DNA is not detected, the infectious risk of
the donor is low.
There are a substantial number of reports of kidneys transplanted from HBsAg
negative/DNA undetectable, HBcAb positive deceased donors in which there have
been a low risk of HBV seroconversion and no excess risk of graft failure or short-
term morbidity (6-9). In the context of living donation, donors who are HBcAb alone
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
130
(with negative HBsAg and undetectable DNA in blood) can therefore donate. The
prospective recipient will ideally have been effectively immunised against HBV,
although immunization can be repeated post-transplant if a suboptimal antibody
response has been made. The addition of anti-viral drugs may be considered,
especially in recipients with a low HBsAb response to vaccination. Under these
circumstances, advice from specialists with appropriate expertise should be sought
and the donor and recipient should be fully informed. Further discussion is available
in the BTS Guidelines for Hepatitis B in Solid Organ Transplantation (10).
Most transplant units would not consider potential donors with evidence of active
HBV viral replication. If it is necessary to consider a potential donor who is HBsAg
positive (or in whom HBV DNA is detected), then advice should be sought from a
specialist with appropriate expertise (10).
Hepatitis C
Active hepatitis C in the donor is a relative contraindication to living donation, not
only because of the risk of transmitting HCV to the recipient but also because of the
risk of glomerular disease in the donor (11,12). The risk of HCV transmission from
an HCV RNA positive donor approaches 100% if transplanted into a naïve recipient
(13). All potential donors should have HCV antibody testing performed and, if
positive, HCV RNA should be checked. If the donor is consistently RNA negative,
then transplantation may be considered, even into a naïve recipient. However, the
risks entailed must be carefully explained to both donor and recipient. In these
exceptional circumstances, the likely life expectancy of the recipient and the risks of
remaining on dialysis may be deciding factors.
Advances in anti-viral agents and vaccination may influence such decisions in the
future. Effective anti-viral therapy resulting in sustained virological response for HCV
has recently become available. As such, if donation from a HCV-infected donor was
the only option for a life-preserving transplant then a risk/benefit analysis would be
appropriate and advice from a specialist with appropriate expertise should be
sought. The risks entailed must be carefully explained to both donor and recipient.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
131
Hepatitis E
Hepatitis E is an RNA virus with enteric transmission and was previously considered
an endemic infection in developing countries. However, an increasing number of
infections have been reported in the UK and the virus is now considered endemic in
Europe. HEV infections are usually relatively asymptomatic in healthy individuals,
but can lead to chronic hepatitis and liver cirrhosis in infected solid organ transplant
recipients (14,15).
BTS guidelines published in April 2017 recommend that all solid organ donors,
including living donors, are screened for HEV in line with the UK Advisory Committee
for the Safety of Blood, Tissues and Organs (SaBTO) (16). It is recommended that
potential living donors are provided with dietary advice regarding avoidance of HEV
infection (from undercooked meat, particularly pork products) and that screening
with a single sample HEV-Nucleic Acid Amplification Test (NAAT) be undertaken
within 30 days of organ donation as part of routine assessment. If HEV viraemia is
detected, donation should be deferred until laboratory testing confirms spontaneous
resolution of HEV infection (plasma and stool HEV RNA not detected).
Human immunodeficiency virus (HIV) and Human T Lymphotrophic virus
The presence of HIV or HTLV infection is an absolute contraindication to living
donation. HTLV is known to be endemic in Africa, the Caribbean and Japan but
HTLV serology must be performed for all prospective donors, regardless of country
of origin (3). Kidney donation should not be undertaken if significant doubt remains
about the possibility of HTLV infection in the donor.
High risk donors and window period infection
Behavioural risk information obtained from potential living donors is generally more
reliable than the collateral history obtained for deceased donors. If there is any doubt
about the acquisition of a blood borne virus that might be transmitted to the recipient,
consideration should be given to delaying the transplant to allow for the “window
period” to have passed and repeat testing performed. The “window period” for a
pathogen is the time between infection and detection by a specific testing method.
NAAT shortens the window period for blood borne viruses relative to serology and
therefore may decrease the risk of transmitting disease from a serologically negative
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
132
donor (17). The period of observation should be at the discretion of the transplant
centre, based on an individual risk analysis and discussion with a specialist with
appropriate virological expertise.
Cytomegalovirus (CMV)
CMV infection is the most commonly encountered clinically significant viral infection
after kidney transplantation and may cause significant morbidity and mortality,
particularly if the recipient is heavily immunosuppressed (18). It also increases the
risk of chronic graft dysfunction as well as post-transplant lymphoproliferative
disorder (PTLD) and opportunistic infection.
CMV disease may result from reactivation of latent infection or because of primary
infection transmitted by a kidney from a CMV positive donor. For CMV and other
viral infections, primary infection is generally more severe than reactivation and the
recipients most at risk are those who are CMV seronegative and receive a kidney
graft from a CMV seropositive donor. Matching CMV seronegative recipients with
CMV seronegative donors is an effective strategy for reducing the risk of CMV
infection but is rarely practicable in the context of living donor kidney transplantation.
Either CMV prophylaxis or pre-emptive therapy with close monitoring of viral loads
should be offered to all recipients except those who are CMV seronegative in receipt
of a graft from a CMV seronegative donor (19). In all other combinations, the donor
and recipient should be informed about the increased risk of CMV disease before
the transplant is performed.
Epstein Barr virus (EBV)
Primary EBV infection is most likely to occur in EBV negative paediatric recipients
who receive a kidney from an EBV positive donor. EBV infection increases the risk
of post-transplant lymphoproliferative disorder (PTLD) and this risk is increased
further if the recipient is given lymphocyte depleting immunosuppressive therapy.
When the donor is EBV positive and the recipient EBV negative, clinical vigilance is
required following transplantation to detect PTLD as early as possible. However,
PTLD can also occur in recipient EBV positive antibody patients, and occasionally
in those who are negative.
Additional potentially significant viral infections (no routine screening)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
133
Human Herpes Virus 8 (HHV8)
HHV8 may be transmitted by organ transplantation and is associated with an
increased risk of Kaposi sarcoma (20). However, there is no evidence to support
screening of potential organ donors.
West Nile Virus
West Nile Virus (WNV) was first reported in the USA in the New York area in 1999,
and has since become endemic in widespread regions of the US. Since 2002, at
least nine instances of donor-derived infection to solid organ transplant recipients
have been reported following deceased donation. There is the potential for
transmission from a living donor, although no cases have been reported to date.
Interpretation of serological results is complex, and exclusion of infection at the time
of donation requires nucleic acid testing. Expert advice should be sought if there are
concerns when assessing a donor from an endemic area (21).
5.14.4 Bacterial Infections in the Prospective Donor
The risk of transmission of a bacterial infection from a healthy living donor is
extremely small. If a specific bacterial microbiological diagnosis has been made,
then a course of appropriate antibiotic is likely to be effective in preventing
transmission.
Urine should be sent for culture from all potential donors. Asymptomatic bacteriuria
is relatively common, especially in women. If the potential donor is male or there is
a personal or family history of urinary tract infection, appropriate imaging of the
kidneys to assess for cortical scarring should be performed.
The main risk of inadvertent transmission of a bacterial infection comes from
mycobacteria (both M. tuberculosis, MTB, and atypical species). As of September
2012, 30 cases of potential or proven donor-derived tuberculosis had been
described in solid organ transplant recipients (22). Four of these had been from
living donors.
Up to 30% of the world’s population is infected with MTB, although this proportion is
much lower in the UK. After initial infection, most people do not develop active
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
134
tuberculosis, but the organism persists in the body - this is referred to as latent TB,
and can be transmitted by transplantation.
Donors should initially be screened for mycobacterial infection on the basis of their
history. Particular high risk factors include: country of birth and any previous
prolonged periods (>3 months) spent in a country with high prevalence; previous
close contact with individuals known to be infected; or working with high risk groups
(prison inmates, the homeless, those with alcohol or other substance abuse).
Screening should include a careful history, including ethnic origin and country of
upbringing, and any previous exposure to TB. A chest X-ray may be suggestive of
previous disease. Tuberculin skin testing or interferon gamma release assay may
be considered for donors at risk of latent infection, although diagnostic tests for
latent TB are limited in sensitivity (23). In cases of concern, discussion with a
Consultant with appropriate expertise is recommended. The risk of transmission is
minimal if the infection has been identified and fully treated, and is not a
contraindication to subsequent donation.
Transmission of syphilis has been reported in the UK to two recipients from a
deceased donor with a past history of treated disease (24). Donation may be
considered after treatment, with informed consent and post-transplant monitoring of
the recipient. If a recipient is considered to be at risk of syphilis transmission from
the donor, prophylactic treatment should be given (2.5 MU benzathine penicillin im
single dose, or doxycycline 100 mg po for 14 days, or 1 g azithromycin po single
dose) in line with British Association for Sexual Health and HIV guidelines (25).
Involvement of a specialised clinic in genitourinary medicine is recommended.
5.14.5 Fungal and Parasitic Infections in the Prospective Donor
A living donor is unlikely to transmit a fungal infection if otherwise in good health.
However, this possibility should be borne in mind when assessing donors from areas
where fungal infections are endemic. Toxoplasma gondii, Coccidioidomycosis,
Strongyloides stercoralis, Trypanosoma cruzi (the causative agent of Chagas
disease) and malaria can be transmitted by a renal transplant (21). In most of the
reported cases, transmission has been from living unrelated donor transplantation
taking place abroad.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
135
Coccidioidomycosis is a fungal infection caused by Coccidioides species endemic
to the southwestern United States, where it presents a challenge for transplant
recipients (26). In this area, up to 8% recipients may develop infection, usually in
the first year following transplantation.
Infection with Strongyloides stercoralis results from skin penetration by larvae and
thus may after walking in soil with faecal contamination. It typically occurs in rural
agricultural regions with poor sanitation. Adult worms can live for up to 5 years, and
autoinfection is an important source of prolonged infection even when the individual
is no longer living in an endemic area. Symptomatic infection with Strongyloides is
more common in the immunocompromised (27).
We suggest screening the following groups: those who were born or lived in tropical
or subtropical countries where sanitation conditions are poor, those with
unexplained eosinophilia and travel to an endemic area and those with a prior history
of Strongyloides infection. Initial screening is by serology, which may indicate
current or past infection. If positive, an opinion from a Consultant with appropriate
expertise should be sought. Donation may proceed after treatment of the donor with
an appropriate agent, such as ivermectin.
Trypanosoma cruzi
Endemic areas for T. cruzi include parts of Mexico and most of Central and South
America, and transmission has been reported following living organ donation (28).
Initial screening of donors from these areas is by serology. Donation may be
considered after appropriate treatment.
Other infections are either transmitted rarely (occasional case report) or may be
considered a possible risk but there have been no reports of donor derived infection.
5.14.6 Prion-Associated Diseases in the Prospective Donor
CJD and vCJD
There is no screening test currently available for CJD or vCJD. No cases of
transmission by organ transplantation have been reported, although there has been
transmission of vCJD infection via transfusion of red blood cells (4 cases) and from
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
136
the plasma used to produce factor VIII (one case) (3). Donor deferral issues
concerning the potential for transmission of vCJD are complex, and are detailed in
the UK blood transfusion and SaBTO guidelines (2,3). Donation is contraindicated
from individuals with a personal or family history of CJD or vCJD (unless considered
not at risk following genetic counselling). Circumstances requiring an individual
assessment, taking into consideration the level of risk or exposure, expected benefit
of transplantation and the availability of alternative donors include: history of blood
transfusion since 1980; history of receipt of dura mater graft; and history of receipt
of human pituitary derived growth hormone or gonadotrophin.
5.14.7 Summary
Provided a careful history is obtained and appropriate screening tests performed,
the risk of transmission of infection from a healthy living donor is very small. Should
there be any uncertainties concerning potential risk, the advice of a Consultant with
appropriate expertise in infectious diseases, microbiology, virology or hepatology
should be sought, to maintain the health and safety of both donor and recipient.
References
1. Standards for solid organ transplantation in the United Kingdom. British
Transplantation Society 2003; ISBN 0 9542221-2-1.
2. UK Blood Transfusion & Tissue Guidelines. Donor selection guidelines.
www.transfusionguidelines.org.uk
3. Guidance on microbiological safety of human organs, tissues and cells used in
transplantation, Advisory Committee on the Safety of Blood Tissues and
Organs (SaBTO), February 2018.
https://www.gov.uk/government/groups/advisory-committee-on-the-safety-of-
blood-tissues-and-organs
4. Martin-Davila P, Fortun J, Lopez-Velez R, et al. Transmission of tropical and
geographically restricted infections during solid-organ transplantation. Clin
Microbiol Rev 2008; 21: 60-96.
5. Kidney disease: improving global outcomes (KDIGO). Clinical Practice
Guideline on the evaluation and follow-up care of living kidney donors.
www.kdigo.org
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
137
6. Satterthwaite R, Ozgu I, Shidban H, et al. Risks of transplanting kidneys from
hepatitis B surface antigen-negative, hepatitis B core antibody-positive donors.
Transplantation 1997; 64: 432-5.
7. Madayag RM, Johnson LB, Bartlett ST, et al. Use of renal allografts from donors
positive for hepatitis B core antibody confers minimal risk for subsequent
development of clinical hepatitis B virus disease. Transplantation 1997; 64:
1781-6.
8. De Feo TM, Grossi P, Poli F, et al. Kidney transplantation from anti-HBc+
donors: results from a retrospective Italian study. Transplantation 2006; 81: 76-
80.
9. Kirchner VA, Liu PT, Pruett TL. Infection and cancer screening in potential living
donors: best practices to protect the donor and recipient. Curr Transpl Rep
2015; 2: 35-42.
10. BTS Guidelines for Hepatitis B in Solid Organ Transplantation
https://bts.org.uk/guidelines-standards/
11. Johnson RJ, Gretch DR, Yamabe H, et al. Membranoproliferative
glomerulonephritis associated with hepatitis C virus infection. N Engl J Med
1992; 328: 465-70.
12. Stehman-Breen C, Willson R, Alpers CE, Gretch D, Johnson RJ. Hepatitis C
virus-associated glomerulonephritis. Curr Opin Nephrol Hypertens 1995; 4:
287-94.
13. Pereira BJ, Milford EL, Kirkman RL, et al. Prevalence of hepatitis C virus RNA
in organ donors positive for hepatitis C antibody and in the recipients of their
organs. N Engl J Med 1992; 327: 910-5.
14. Kamar N, Dalton HR, Abravanel F, Izopett J. Hepatitis E infection. Clin Microbiol
reviews 2014; 27: 116-38.
15. Vassallo D, Husain MM, Greer S, McGrath S, Ijaz S, Kanigicherla D. Hepatitis
E infection in a renal transplant recipient. Case Reports in Nephrology 2014:
86547.
16. British Transplantation Society. Guideline: Hepatitis E and solid organ
transplantation, 1
st
Edition, April 2017.
https://bts.org.uk/wp-content/uploads/2017/06/BTS_HEV_Guideline-FINAL.pdf
17. Humar A, Morris M, Blumberg E et al. Nucleic acid testing (NAT) of organ
donors: is the “best” test the right test? A consensus conference report. Am J
Transplantation 2010: 10: 889-99.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
138
18. Van Son WJ, The TH. Cytomegalovirus infection after organ transplantation: an
update with special emphasis on renal transplantation. Transpl Int 1989; 2: 147-
64.
19. Guidelines for the prevention and management of cytomegalovirus disease
after solid organ transplantation. British Transplantation Society, 2002. ISBN:
0954222105.
https://bts.org.uk/wp-content/uploads/2016/09/14_BTS_CMV_3RDE-1.pdf
20. Regamey N, Tamm M, Wernli M, et al. Transmission of human herpesvirus 8
infection from renal transplant donors to recipients. N Engl J Med 1998; 19:
1358-63.
21. Levi ME, Kumar D, Green M, et al on behalf of the AST ID Community of
Practice. Considerations for screening live kidney donors for endemic
infections: a viewpoint on the UNOS policy. Am J Transplant 2014; 14: 1003-
11.
22. Morris MI, Daly JS, Blumberg E, et al. Diagnosis and management of
tuberculosis in transplant donors: a donor-derived infections consensus
conference report. Am J Transplant 2012; 12: 2288-300.
23. Subramanian AK. Tuberculosis in solid organ transplant candidates and
recipients: current and future challenges. Curr Opin Infect Dis 2014; 27: 316-
21.
24. Cortes NJ, Afzali B, MacLean D, et al. Transmission of syphilis by solid organ
transplantation. Am J Transplant 2006; 6: 2497-9.
25. Kingston M, French P, Higgins S, et al. UK national guidelines on the
management of syphilis 2015. Int J STD AIDS 2016; 6: 421-46.
26. Blair JE, Mulligan DC. Coccidioidomycosis in healthy persons evaluated for liver
or kidney donation. Transpl Infect Dis 2007; 9: 78-82.
27. Roxby AC, Gottlieb GS, Limaye AP. Strongyloidiasis in transplant patients. Clin
Infect Dis 2009; 49: 1411-23.
28. Huprikar S, Bosserman E, Patel G, et al. Donor-derived Trypanosoma cruzi
infection in solid organ recipients in the United States, 2001-2011. Am J
Transplant 2013; 13: 2418-25.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
139
5.15 NEPHROLITHIASIS
Recommendations
In the absence of a significant metabolic abnormality, potential donors
with a limited history of previous kidney stones, or small renal stone(s)
on imaging, may still be considered as potential kidney donors. Full
counselling of donor and recipient is required along with access to
appropriate long-term donor follow up. (C2)
Potential donors with metabolic abnormalities detected on screening
should be discussed with a specialist in renal stone disease. (C2)
In appropriate donors with unilateral kidney stone(s) the stone-bearing
kidney can be considered for donation (if vascular anatomy and split
kidney function permit) in order to leave the donor with a stone-free
kidney after donation. (C2)
5.15.1 Incidence, Natural History and Management of Renal Stones
In the UK, symptomatic renal stones are common with a prevalence of around 3-
5%. The use of CT to evaluate potential kidney donors has led to increased
detection of asymptomatic kidney stones, which are generally small (4 mm) and
present in about 5% of potential kidney donors undergoing non-contrast CT scan.
The lifetime risk of recurrent kidney stones is an important consideration in
evaluating the suitability for kidney donation. There are few data on the lifetime risk
specific to the kidney donor population. However, data relating to risk of further stone
episodes are available for people who present with a symptomatic kidney stone
(overall 50% chance of developing a further stone within 5 years) and a risk
prediction tool exists (1). Risk prediction tools do not yet exist for asymptomatic
stone formers, but ≥1 stone at presentation confers an increased risk of metabolic
risk factors and future stone episodes (1).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
140
Most renal stones (75%) are composed predominantly of calcium oxalate. In
symptomatic patients who undergo metabolic evaluation (who may be a selected
group), a metabolic abnormality (e.g. hypercalciuria, hyperoxaluria, or
hypocitraturia) may be detected in over 50% (2,3). The remaining 25% of stones are
composed of uric acid, pure calcium phosphate, cysteine or struvite (magnesium
ammonium phosphate, also called infection stones) (2,4). Uric acid stones are often
associated with a history of gout, ileostomy, diarrhoea or with the metabolic
syndrome, in all of which the urine is acidic. Calcium phosphate stones may occur
with hypercalciuria and are the predominant stone type formed by patients with a
low urinary citrate and distal renal tubular acidosis. Cystine stones are always
associated with cystinuria and people with these stones should not donate a kidney.
Infection stones are commonly associated with an anatomical abnormality and
people with these stones should not donate a kidney unless the anatomical
abnormality is easily correctable.
Most asymptomatic stones found in potential donors are small (<5 mm). Small
stones usually pass spontaneously but can occasionally cause ureteric obstruction
leading to acute renal failure in patients with a single kidney. Small kidney stones
can be treated using less invasive treatment modalities e.g. flexible uretero-
renoscopy. However, for the general population, the evidence that treating small
asymptomatic stones is superior to simply observing them is mixed (6), with about
25% becoming symptomatic in 5 years and 3% developing painless silent
obstruction (7). Upper or middle pole stones are more likely to become symptomatic
and also to pass spontaneously.
It is recognised that the natural history of small asymptomatic stones detected during
a donor work-up may be very different to stones presenting with clinical features or
described in the existing urological literature. A recent study of 1,957 potential
kidney donors evaluated at the Mayo Clinic from 2000 to 2008 reported that 3% had
past symptomatic stones, while 11% had radiographic stones detected on screening
(11). In this study, asymptomatic stone formers were not characterised by older age,
male gender, hypertension, obesity, metabolic syndrome, abnormal kidney function,
hyperuricaemia, hypercalcaemia or hypophosphataemia. One conclusion is that
asymptomatic stone formers may lack the co-morbidities found in symptomatic
stone formers and that different mechanisms may be involved in asymptomatic
versus symptomatic stone formation.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
141
Perhaps reflecting the above, there is a lack of evidence to guide decision making
and a lack of unanimity between the current recommendations regarding stone size
cut-off (12-14). On balance, it is likely that the risks of recurrent stone formation are
low in asymptomatic potential kidney donors. However, in the absence of a reliable
evidence base, a degree of caution is warranted.
Large or staghorn stones can commonly lead to chronic renal damage (2) and are
usually associated with infection or a significant metabolic abnormality and people
with these stones should not be considered as donors.
In transplant recipients, the long-term risks associated with a small stone transferred
from the donor kidney appear low (6,7).
5.15.2 Assessment of Potential Donors
Imaging
The use of CT for renal vascular imaging has increased the detection rate of
asymptomatic kidney stones. Where CT is not used routinely for vascular imaging
and a stone is suspected from USS or MRI, a non-contrast CT KUB is advisable to
determine the number, size and location of suspected stones.
If a probable stone is identified on imaging, a urological and radiological review
should be undertaken. The number, size, position and density of the potential stones
should be considered; as should the presence of any underlying structural renal
abnormality. A CT IVU may be useful in these circumstances. A DMSA scan is
useful if renal scarring is suspected and will give an estimate of split renal function.
Biochemical Assessment
A full metabolic and imaging screen should be carried out before donation on
potential donors with a history of stone disease or radiological evidence of a current
stone. This screen should include 24-hour urine collections for calcium, oxalate,
citrate and urate, and early morning pH assessment. This will require two separate
urine collections as calcium, oxalate and citrate analyses require an acidified
collection, whereas electrolytes, urate and pH are measured in a plain urine
collection. Urine creatinine should be measured on each collection as an internal

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
142
marker of completeness and the 24 hour urine volume should be noted. A pH
measurement on an early morning urine sample is useful, together with a qualitative
cystine screen for cystinuria (8), followed, if positive, by a 24-hour collection for
cystine concentration. Serum calcium (adjusted for albumin level) and urate should
be measured. A metabolic screen (urine and plasma biochemistry) may also be
indicated in potential donors with a significant family history of stone disease or with
significant risk factors for the development of stones e.g. inflammatory bowel
disease.
In patients with previous calculus disease, where a stone has been retrieved,
biochemical stone analysis is also of value.
5.15.3 Proceeding to Donation
There is an increasing literature of single centre units utilising donors with small
unilateral kidney stones. If a significant and uncorrectable metabolic abnormality is
identified then kidney donation is contra-indicated (9). However, donation may be
considered in potential donors with minor or correctable metabolic abnormalities e.g.
isolated hypocitraturia, isolated hypercalciuria, isolated hyperuricosuria, particularly
if the history of calculus disease is very limited. Donation may be considered where
factors that have previously put the patient at risk of stone formation e.g. diet or
medication, have been successfully modified, urine pH has been corrected to normal
(preferably using a pH meter rather than dipstick testing), and 24 hr urine levels
have demonstrated to a return to the normal range. In such cases, careful
counselling of the donor is mandatory before surgery. It is recommended that advice
is obtained from a clinician with a specific interest in this field. A history of a previous
infection-related (struvite) or cystine renal stone is generally considered a contra-
indication to donation.
In potential donors who have a history of previous stones but no metabolic
abnormality, proceeding with donation should be considered providing the number,
size and frequency of previous stones has been low.
Potential donors found to have small stone(s) on imaging, or cases where there is
uncertainty as to whether there is a true calculus or parenchymal calcification, may
be suitable to donate. In all cases, the results of the metabolic screen, donor age,
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
143
and history of previous stone formation should be considered, and donation should
only take place after full counselling of the donor and recipient. Both need to be
aware of the limited data regarding long-term outcomes in these circumstances (10).
The smaller the stone bulk and the older the potential donor, the lower is risk
associated with proceeding to donation.
If donation proceeds, it is preferable to remove the kidney containing the suspected
calculus. If the stone is very small it may be left in situ at the time of transplantation.
However, it is relatively straight forward, with urological input and modern flexible
ureterorenoscopes, to inspect the collecting system and remove any confirmed
stones ex vivo, before implanting the donor kidney (15,16).
Leaving the donor with a single kidney containing a possible small stone is
undesirable, but may be considered in exceptional circumstances, e.g. strong
anatomical reasons to remove the contralateral kidney. Full counselling of the donor
is required in this situation and appropriate close long-term follow-up of the donor is
necessary.
People with bilateral kidney stones should in general not be considered as kidney
donors. This situation both suggests an inherent metabolic or anatomical
abnormality and would leave the individual with a single kidney containing a stone
placing them at significant risk of a future stone event in a solitary kidney.
5.15.4 Follow Up
All management decisions need to take into consideration the potential follow-up
requirements, with particular reference to donors from overseas.
Donors who have a past history of stones and those who have donated a stone-
bearing kidney should be counselled about symptoms of renal/ureteric colic and
anuria and information should be provided regarding the availability of local
urological expertise. Donors should also be advised to maintain a high fluid intake
for life (at least 2.5 litres of fluid per day) and also (where appropriate) to continue
any medication prescribed to reduce the risk of future stone formation. Regular
follow-up imaging e.g. annual or biennial renal ultrasound may be advisable, and
regular re-assessment of the metabolic profile should be considered.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
144
Potential donors deemed unsuitable to donate because of stone disease should be
referred to a local urologist for further management.
References
1. Rule AD, Lieske JC, Li X, et al. The ROKS nomogram for predicting a second
symptomatic stone episode. J Am Soc Nephrol 2014; 25: 2878-86.
2. Coe FL, Keck J, Norton ER. The natural history of calcium urolithiasis. JAMA
1977; 238: 1519-23.
3. Johri N, Cooper B, Robertson W, Choong S, Rickards D, Unwin R. An update
and practical guide to renal stone management. Nephron Clin Pract 2010; 116:
c159-71.
4. Spivacow FR, Negri AL, Del Valle EE, Calvino I, Zanchetta JR. Clinical and
metabolic risk factor evaluation in young adults with kidney stones. Int Urol
Nephrol 2010; 42: 471-5.
5. Sayer JA. The genetics of nephrolithiasis. Nephron Exp Nephrol 2008; 110:
e37-43.
6. Burgher A, Beman M, Holtzman JL, Monga M. Progression of nephrolithiasis:
long-term outcomes with observation of asymptomatic calculi. J Endourol 2004;
18: 534-9.
7. Dropkin BM, Moses RA, Sharma D, et al. The natural history of nonobstructing
asymptomatic renal stones managed with active surveillance. J Urol 2015; 193:
1265-9.
8. Martin G, Lipke MC, Sharfuddin A, Govani M, Sundaram P. Asymptomatic
unilateral urolithiasis in living donor transplant kidneys. Urology 2007; 70: 2-5.
7. Ho KLV, Chow G. Prevalence and early outcome of donor graft lithiasis in living
renal transplants at the Mayo Clinic. J Urol 2005; 173: S439 abstract 1622.
8. Singh SK, Agarwal MM, Sharma S. Medical therapy for calculus disease. BJU
Int 2011; 107: 356-68.
9. Kasiske BL, Ravenscraft M, Ramos EL, Gaston RS, Bia MJ, Danovitch GM.
The evaluation of living renal transplant donors: clinical practice guidelines: Ad
Hoc Clinical Practice Guidelines Subcommittee of the Patient Care and
Education Committee of the American Society of Transplant Physicians. J Am
Soc Nephrol 1996; 7: 2288-313.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
145
10. Strang AM, Lockhart ME, Amling CL, Kolettis PN, Burns JR. Living renal donor
allograft lithiasis: a review of stone related morbidity in donors and recipients. J
Urol 2008; 179: 832-6.
11. Lorenz EC, Lieske JC, Vrtiska TJ, et al. Clinical characteristics of potential
kidney donors with asymptomatic kidney stones. Nephrol Dial Transplant 2011;
26: 2695-700.
12. Kälble T, Alcaraz A, Budde K, et al. European Urology Association Guidelines.
Renal transplantation 2009.
www.uroweb.org/gls/pdf/Renal%20Transplantation%202010.pdf
13. Delmonico F. A report of the Amsterdam Forum on the care of the live kidney
donor: data and medical guidelines: Council of the Transplantation Society.
Transplantation 2005; 79 (S6): S53-66.
14. Rydberg J, Kopecky KK, Tann M, et al. Evaluation of prospective renal donors
for laparoscopic nephrectomy with multisection CT: the marriage of minimally
invasive imaging with minimally invasive surgery. Radiographics 2001; 21:
S223-36.
15. Rashid MG, Konnak JW, Wolf JS, et al. Ex vivo ureteroscopic treatment of
calculi in donor kidneys at renal transplantation. J Urol 2004; 171: 58-60.
16. Olsburgh J, Thomas K, Wong K, et al. Incidental renal stones in potential live
kidney donors: prevalence, assessment and donation, including role of ex vivo
ureteroscopy. BJU Int 2013; 111: 784-92.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
146
5.16 HAEMATOLOGICAL DISEASE
Recommendations
Donor anaemia needs to be investigated and treated before donation.
(A1)
A haemoglobinopathy screen must be carried out in patients with non-
Northern European heritage or if indicated by the full blood count. (A1)
Careful consideration needs to be given to the use of potential donors
with haemoglobinopathies. (B1)
Advice from a consultant haematologist is recommended for
haematological conditions not covered in this guideline. (Not graded)
5.16.1 Introduction
Haematological abnormalities can be associated with increased risk to either or both
of the donor and recipient in living donor kidney transplantation. A targeted history
should be obtained from the donor, with specific enquiry about anaemia, venous
thromboembolism (VTE), and any family history of haemoglobinopathy. All donors
should have a full blood count and clotting screen as part of their assessment.
Attention should be paid to the haemoglobin concentration, total and differential
white count, and the mean corpuscular volume (MCV and MCH).
Abnormalities of any of the above will require further investigation. In addition,
haemoglobinopathy screening needs to be carried out in potential donors of non-
northern European heritage or where indicated by the MCV to screen for
haemoglobinopathies. If there is a history of VTE, a thrombophilia screen should
also be undertaken in the donor.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
147
5.16.2 Red Cell Disorders
Anaemia
Anaemia (WHO classification Hb <130 g/L for men and <120 g/L for women) should
be fully investigated and treated before organ donation.
Sickle cell disease and sickle cell trait
Sickle cell disease is an absolute contraindication to living kidney donation, with as
many as 5-20% of patients developing CKD in their lifetime
(1). In addition, the risks
of general anaesthetic are much greater in this population.
The situation is more complex in potential donors with sickle call trait (SCT). There
is a high incidence of urine concentrating abnormalities in such patients. In addition,
visible and non-visible haematuria are well described, often as a result of papillary
necrosis. There is epidemiological evidence to suggest that SCT is associated with
a higher risk of progression to end stage renal disease, a higher incidence of CKD
and albuminuria, and a more rapid deterioration in renal function. This is equally true
for Hb AS and Hb AC (2,3). What is not clear is whether those without albuminuria
are at increased risk. In addition, the peri-operative risks may be higher in patients
with SCT, including complications such as venous thromboembolism (4). Individuals
with SCT are also at increased risk of renal medullary carcinoma.
There are few data on the safety of kidney donation in individuals with SCT. A survey
of US Transplant centers found that 37% would or might exclude patients on the
basis of having SCT (5). On balance, SCT should not be an absolute
contraindication to kidney donation, but donors wishing to proceed need to be
counseled about the possible risks with input from a haematologist with an interest
in sickle cell disease. Careful screening for the presence of existing renal
involvement is required, with particular attention to a history of macroscopic
haematuria.
Thalassaemia
Patients with thalassaemia can be categorised into those with transfusion
dependent thalassaemia (TDT), non-transfusion dependent thalassaemia (NTDT)
(including haemoglobin H disease, a form of alpha thalassaemia) and thalassaemia
trait (thalassaemia carriers). Only the latter can be considered for living kidney
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
148
donation as even individuals with NTDT periodically require transfusion and often
suffer with iron overload and associated medical sequelae. There have been a few
reports of minor tubular dysfunction in some patients with thalassaemia trait but
there is no other reported association with renal disease (6).
Other haemoglobin variants
Other haemoglobinopathies may be encountered when screening donors of non-
northern European heritage and in general should not pose a problem with kidney
donation except where they form part of a compound heterozygote with Hb S (e.g.
Hb SC, Hb ES, etc). Such patients behave like patients with sickle cell disease and
therefore should not be accepted as living kidney donors. There is also some
evidence that individuals with Hb CC and Hb AC may at increased risk of developing
CKD (3).
Red cell membrane disorders
These include hereditary spherocytosis and hereditary eliptocytosis, inherited
haemolytic anaemias of variable severity. Some of these patients undergo
splenectomy to ameliorate anaemia. Renal function is not significantly impaired in
these conditions and organ donation is acceptable in mild forms where treatment
has not been required. Advice from the treating haematologist should be sought.
5.16.2 White Cell Disorders
Monoclonal gammopathy of uncertain significance (MGUS)
MGUS is a plasma cell proliferative disorder that is characterised by a plasma cell
content of <10% in the bone marrow, a monoclonal band of ≤30 g/L on protein
electrophoresis, and the absence of end organ damage in the form of
hypercalcaemia, renal insufficiency, anaemia or bone lesions (7). MGUS occurs in
2% of the population over the age of 50 years. There is a small year-on-year risk of
transformation to myeloma or AL amyloid (1-2% per year) (8).
MGUS per se does not cause end organ disease and individuals with this condition
could with caution be considered as living kidney donors. However, such a decision
has to be taken with great care and following discussion with the donor and their
haematologist. Potential donors with MGUS need to be aware of the potential risk
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
149
of progression to malignant B cell disorders which may adversely affect their
remaining kidney; and also that they will have a lower GFR following donation, which
may limit their treatment options should their MGUS transform into a malignant
condition. Although the risk of disease transmission is considered negligible, the
potential recipient should also be counselled re a potential increased risk associated
with donation.
Myelodysplasia
Myelodysplastic syndromes (MDS) are a range of conditions resulting from
abnormal clonal proliferation of bone marrow derived stem cells. As such there is a
theoretical possibility of carry-over in a donor kidney to the recipient. In addition to
the risk of transformation into acute myeloid leukaemia, patients with MDS are also
at increased risk of premature death, especially as a result of cardiac disease (9).
The presence of MDS should be considered a strong contraindication to donation.
5.16.3 Clotting Disorders
Patients with a history of VTE can be classified into high, medium and low risk as
per the AT9 Guidelines (10) whereby the risk of an event is >10%, 5-10% or <5%
respectively. The risk of VTE in the low risk group (on warfarin) following a procedure
is less than 0.2% irrespective of the use bridging anticoagulation peri-procedure.
However, those receiving bridging anticoagulation are more likely to have bleeding
complications. These data should inform discussion with potential donors in this
category and may represent a relative contraindication to donation but, in general,
the risks should be discussed with a haematologist.
References
1. Shaw C, Sharp CC. Could sickle cell trait be a predisposing risk factor for CKD?
Nephrol Dial Transplant 2010; 25: 2403-5.
2. RP Naik, VK Derebail, ME Grams, et al. Association of sickle cell trait with
chronic kidney disease and albuminuria in African Americans. JAMA 2014; 312:
2115-25.
3. Derebail VK, Nachman PH, Key NS, et al. High prevalence of sickle cell trait in
African Americans with ESRD. J Am Soc Nephrol 2010; 21: 413-7.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
150
4. Austin H, Key NS, Benson JM, et al. Sickle cell trait and the risk of venous
thromboembolism among blacks. Blood 2007; 110: 908-12.
5. Reese PP, Hoo AC, Magee CC. Screening for sickle trait among potential live
kidney donors: policies and practices in US transplant centers. Transpl Int 2008;
21: 328-31.
6. Cetin T, Oktenli C, Ozgurtas T, et al. Renal tubular dysfunction in beta-
thalassemia minor. Am J Kidney Dis 2003; 42: 1164-8.
7. Berenson JR, Anderson KC, Audell RA, et al. Monoclonal gammopathy of
undetermined significance: a consensus statement. J Haematol 2010; 150: 28-
38.
8. Kyle RA, Therneau TM, Rajkumar SV, et al. A long-term study of prognosis in
monoclonal gammopathy of undetermined significance. N Engl J Med 2002;
346: 564-9.
9. Goldberg SL, Chen E, Corral M, et al. Incidence and clinical complications of
myelodysplastic syndromes among United States Medicare beneficiaries. J Clin
Oncol 2010; 28: 2847-52.
10. Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management
of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis,
9th ed: American College of Chest Physicians Evidence-Based Clinical Practice
Guidelines. Chest 2012; 141 (2 Suppl): e326-50.
11. Clark NP, Witt DM, Davies LE, et al. Bleeding, recurrent venous
thromboembolism, and mortality risks during warfarin interruption for invasive
procedures. JAMA Intern Med 2015; 175: 1163-8.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
151
5.17 FAMILIAL RENAL DISEASE
Recommendations
All potential transplant recipients must have a detailed family history
recorded and confirmation where possible of the diagnosis in other
family members with known kidney disease. This may aid diagnosis for
the recipient, clarify any mode of inheritance and identify at risk
relatives. (A1)
When the cause of kidney failure in the recipient is due to an inherited
condition, appropriate tests - including genetic testing if available - are
recommended to exclude genetic disease in the potential donor. (A1)
Many inherited kidney diseases are rare, so involvement of clinical and
laboratory genetics services must be considered at an early stage to
assess likely risks to family members and the appropriate use of
molecular genetic testing. (B1)
When renal failure in the recipient is due to an inherited renal disease, where there
is a family history of renal disease, or where the primary disease is unknown, it is
important to thoroughly investigate genetically related potential donors to assess
their risk of developing renal disease (1,2). The diagnosis of many familial renal
diseases still relies on a high index of suspicion coupled with biochemical,
radiological and histological investigations. It may also be revealed only through a
detailed pedigree, which must be obtained for all individuals with renal disease who
are being considered for transplantation. Genetic testing for a wide range of
inherited renal diseases is now available through the NHS (see below) resulting in
more families also having a genetic diagnosis.
A significant proportion of patients with ESRD will have a family history of renal
disease. In such cases, confirmation of all diagnoses within the family is essential
to identify whether there is a clinically significant genetic predisposition to renal
disease that may be relevant to potential donation (3). Information on constructing
a pedigree can be obtained via the National Genetics Education and Development
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
152
Centre (www.genomicseducation.hee.nhs.uk). However, in most cases the family
history is due to polygenic influences such as diabetes, certain types of
glomerulonephritis and hypertension for which no additional genetic testing or
screening is required above that recommended for routine donor evaluation (3).
A negative family history does not exclude a primary renal genetic disease. With the
exception of autosomal dominant polycystic kidney disease (ADPKD), most familial
renal diseases are rare in the nephrology clinic. Where the diagnosis is a known
genetic disease or the family history is suggestive of a monogenic (Mendelian)
disease, the pedigree will aid in the identification of the mode of inheritance (typically
autosomal dominant, autosomal recessive or X-linked) and the identification of at
risk relatives. This information is important to clarify the lifetime risk to a genetically
related potential donor of developing significant renal disease.
The genetic basis of many familial renal diseases has been elucidated, providing
the opportunity to use molecular investigations for diagnostic testing in the
recipient and predictive testing in the potential living related donor (4). Genetic
testing may also aid the prediction of the likelihood of disease recurrence in the
transplanted kidney, e.g. in atypical haemolytic uraemic syndrome (aHUS) and
steroid resistant nephrotic syndrome (SRNS). The UK Genetic Testing Network
(www.ukgtn.nhs.uk) provides information on all tests currently available through
the NHS and links to other sources of information such as GeneReviews
(www.ncbi.nlm.nih.gov/sites/GeneTests) and OMIM (www.ncbi.nlm.nih.gov/omim).
As genetic testing may be offered to individuals and families, involvement of clinical
genetics services or specialist renal genetics services should be considered at an
early stage to support the donor assessment team. This will be of value in identifying
risks to family members and for the type and use of genetic testing for diagnostic
and exclusion purposes. Details of all UK genetics centres can be found on the
British Society of Human Genetics website (www.bsgm.org.uk/information-
education/genetics-centres/).
It should also be noted that molecular testing can take in excess of 3 months and,
with the increasing use of gene panels containing many genes, the likelihood of
identifying a genetic variant that requires further interpretation is increased. This
should be considered when planning donor evaluation and screening. Bespoke
genetic testing may also be available for some families through the use exome
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
153
testing or whole genome sequencing, even if the test is not currently listed on
the UKGTN. Projects such as the 100,000 Genomes project may facilitate the
latter and further necessitates interaction with genetic services at an early stage
of donor/recipient evaluation www.genomicsengland.co.uk/the-100000-genomes-
project/.
Autosomal Dominant Conditions
In autosomal dominant (AD) diseases, first-degree relatives are at 50% risk of
carrying the familial mutation although variable penetrance and expression,
common in many genetic diseases, may suggest some at risk family members are
unaffected or that the recipient represents a de novo mutation. At risk relatives must
be carefully evaluated for specific disease manifestations and consideration given
to genetic testing to definitively clarify risk and therefore suitability as a potential
donor.
Autosomal Recessive Conditions
In autosomal recessive (AR) disease, unless there is a family history of
consanguinity, only siblings have a significant risk of developing disease (25%).
Parents will be obligate gene carriers and second degree relatives will be at 50%
risk of also being gene carriers. For most AR diseases, carrier status will have no
important clinical sequelae and individuals may be considered as potential donors.
One exception is AR Alport syndrome (see section 5.12 Non-Visible Haematuria).
In this disease, which accounts for ~15% of Alport syndrome cases, carriers may
manifest non-visible haematuria as a consequence of thin basement membrane
disease due to mutation of the COL4A3 or COL4A4 genes (5). It remains unclear
what the risk of progression to proteinuria and renal impairment is for carriers, but
this has been described (6,7). Molecular testing can be used to confirm the
diagnosis in the affected individual and carrier status in parents and other relatives.
This will also have benefit in distinguishing AR from X-linked Alport syndrome. It is
currently unclear whether mutation carriers who do not have non-visible haematuria
on repeat testing can be donors. Despite this uncertainty, carriers with no renal
abnormality by age 45 might be considered as donors in a similar manner to X-linked
Alport syndrome.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
154
X-Linked Conditions
X-linked (XL) conditions should be considered in pedigrees where there are isolated
or several affected males. In X-linked conditions such as XL Alport syndrome and
Dent Disease, female carriers may manifest a phenotype as severe as males, or
very minor abnormalities with a low likelihood of disease progression. In XL Alport
syndrome, female carriers may develop ESRD (see section 5.12, Non-Visible
Haematuria). The majority, >95%, will develop non-visible haematuria by adulthood
but have a life-time risk of progressive renal disease of 5-20%. Gene testing for both
conditions is available and is important for diagnostic confirmation and the carrier
testing of other female family members. Therefore careful evaluation of renal
function, possibly including renal biopsy, may be indicated in X-linked diseases to
provide accurate risks for potential female donors who have been shown to be
carriers.
In all familial renal diseases, a genetically related potential donor can be offered
predictive genetic testing if the familial mutation has been identified. This should
only be offered by experienced individuals, usually via a regional clinical genetics
service, because of the potential impact of identifying clinical or genetic status to an
otherwise clinically asymptomatic individual. Any person found to carry the familial
mutation would normally be excluded as a potential donor if this predicted
development of disease, and should also be referred for appropriate follow-up.
Genetic testing is currently available for diseases where a mutation has a high
probability of predicting development of disease. This is largely confined to
Mendelian diseases as discussed above. However, genetic determinants of
complex diseases have also been identified. These tend to be associated with a
much smaller predictive value of developing disease and are relevant to populations
and not families. A particular example is the association of APOL1 gene variants
which account for some of the excess risk of chronic and ESRD in persons of African
ancestry, including FSGS. Currently there are no prospective data on which to base
recommendations for APOL1 genetic testing and screening for what are also
common variants in the normal population (8,9).
Disease status in an at-risk potential donor may also be determined by clinical
assessment without genetic testing. This requires the use of appropriate screening
tests and is straightforward for diseases such as ADPKD where robust criteria for
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
155
the use of ultrasound and MRI screening have been produced (10). For some
diseases such as UMOD associated nephropathy (OMIM 162000), the only
abnormality may be a reduction in fractional excretion of urate (FE
ur
), or in Dent
Disease the carrier status may only be revealed by measuring low molecular weight
proteinuria.
Conditions in which renal dysfunction may be inherited and transplantation indicated
for renal replacement therapy include the following:
Autosomal dominant: ADPKD; Renal cysts and diabetes; Von Hippel Lindau
disease; Familial haemolytic uraemic syndrome; Familial
FSGS; Tuberose sclerosis complex; UMOD associated
nephropathy (autosomal dominant tubulointerstitial
disease); Nail patella syndrome
Autosomal recessive: ARPKD; Alport syndrome; Familial nephrotic syndrome,
renal ciliopathies including nephronophthisis
X-linked: Alport syndrome; Fabry disease; Dent disease
Polygenic: VUR; FSGS, IgA nephropathy
In the majority of these conditions, the presence of disease in the potential donor
precludes transplantation.
ADPKD
The most common inherited renal disease is ADPKD, which affects 1:1000-1:2000
individuals and is responsible for ~10% of UK patients receiving renal replacement
therapy. The diagnosis of ADPKD in someone at 50% risk of being affected is based
on the following recently revised ultrasound criteria (11):
Three or more unilateral or bilateral cysts in individuals aged 15-39 years
At least two cysts in each kidney for individuals aged 40 to 59 years
At least four cysts in each kidney for individuals aged >60 years
A negative renal ultrasound beyond the age of 40 years excludes disease. Between
the ages of 20-40 years, a negative ultrasound should be followed by a CT or MRI
scan. Criteria for the diagnosis or exclusion of disease using CT or MRI have
recently been published with a total of >10 cysts being sufficient for diagnosis
and <10 cysts being sufficient to exclude disease (10). An analysis of the UNOS
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
156
database indicates better graft survival from genetically unrelated donors in ADPKD
(12). As genetic testing for ADPKD is available via the UKGTN, this may permit more
accurate disease exclusion for donors when combined with radiological screening.
Indeed, many units would not use a kidney from a relative under 30 years of a patient
with ADPKD who had even just one renal cyst without mutation screening. Genetic
testing may therefore be helpful where equivocal imaging studies do not allow formal
exclusion of the diagnosis. Guidelines for the use of genetic testing for living related
donors have been published and advice is also available via the UKGTN (2,13).
Reflux Nephropathy
Vesico-ureteric reflux on the other hand is a condition where the genetic basis is
unclear but where family studies show a high sibling recurrence risk and significant
risk of inheritance (14). It affects around 1-2% of infants and is one of the most
common reasons for transplantation in young adults. A careful search for evidence
of reflux or its consequences should be undertaken in relatives being considered as
donors. A history of childhood enuresis or urinary tract infection is common in
affected individuals. Nuclear medicine scanning can detect renal scars and this can
be used to look for indirect evidence of reflux in potential donors. Genetic testing is
currently unavailable.
Sources of Information
The following websites may be consulted for up-to-date guidance regarding genetic
disease and testing:
UK Genetic Testing Network (www.ukgtn.nhs.uk)
OMIM (www.ncbi.nlm.nih.gov/omim)
GeneReviews (www.ncbi.nlm.nih.gov/sites/GeneTests)
United Network for Organ Sharing (www.unos.org)
British Society of Human Genetics (www.bshg.org.uk)
National Genetics Education and Development Centre
(www.geneticseducation.nhs.uk)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
157
References
1. Kasiske BL, Ravenscraft M, Ramos EL, Gaston RS, Bia MJ, Danovitch GM.
The evaluation of living renal transplant donors: clinical practice guidelines. Ad
Hoc Clinical Practice Guidelines Subcommittee of the Patient Care and
Education Committee of the American Society of Transplant Physicians. J Am
Soc Nephrol 1996; 7: 2288-313.
2. Lentine KL, Kasiske BL, Levey AS, et al. KDIGO clinical practice guideline on
the evaluation and care of living kidney donors, 2017. Transplantation 2017;
101 (8S); S1-109.
3. Freedman BI, Volkova NV, Satko SG, et al. Population-based screening for
family history of end-stage renal disease among incident dialysis patients. Am
J Nephrol 2005; 25: 529-35.
4. Hildebrandt F. Genetic kidney diseases. Lancet 2010; 375: 1287-95.
5. Savige J, Gregory M, Gross O, Kashtan C, Ding J, Flinter FJ. Am Soc Nephrol
2013; 24: 364-75.
6. Marcocci E, Uliana V, Bruttini M, et al. Autosomal dominant Alport syndrome:
molecular analysis of the COL4A4 gene and clinical outcome. Nephrol Dial
Transplant 2009; 24: 1464-71.
7. Pierides A, Voskarides K, Athanasiou Y, et al. Clinico-pathological correlations
in 127 patients in 11 large pedigrees, segregating one of three heterozygous
mutations in the COL4A3/COL4A4 genes associated with familial haematuria
and significant late progression to proteinuria and chronic kidney disease from
focal segmental glomerulosclerosis. Nephrol Dial Transplant 2009; 24: 2721-9.
8. Riella LV, Sheridan AM. Testing for high-risk APOL1 alleles in potential living
kidney donors. Am J Kidney Dis 2015; 66: 396-401.
9. Kopp JB, Winkler CA, Nelson GW. MYH9 genetic variants associated with
glomerular disease: what is the role for genetic testing? Semin Nephrol 2010;
30: 409-17.
10. Pei Y, Hwang YH, Conklin J, et al. Imaging-based diagnosis of autosomal
dominant polycystic kidney disease. J Am Soc Nephrol 2015; 26: 746-53.
11. Pei Y, Obaji J, Dupuis A, et al. Unified criteria for ultrasonographic diagnosis of
ADPKD. J Am Soc Nephrol 2009; 20: 205-12.
12. Futagawa Y, Waki K, Gjertson DW, Terasaki PI. Living-unrelated donors yield
higher graft survival rates than parental donors. Transplantation 2005; 79:
1169-74.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
158
13. Huang E, Samaniego-Picota M, McCune T, et al. DNA testing for live kidney
donors at risk for autosomal dominant polycystic kidney disease.
Transplantation 2009; 87: 133-7.
14. Cordell HJ, Darlay R, Charoen P, et al. Whole-genome linkage and association
scan in primary, nonsyndromic vesicoureteric reflux. J Am Soc Nephrol 2010;
21: 113-23.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
159
5.18 DONOR MALIGNANCY
Recommendations
Careful history taking, clinical examination and investigation of
potential donors are essential to exclude occult malignancy before
kidney donation, particularly in older (age >50 years) donors. (B1)
Active malignant disease is a contraindication to living donation but
donors with certain types of successfully treated low-grade tumour
may be considered after careful evaluation and discussion. (B1)
Donors with an incidental renal mass lesion must have this diagnosed
and managed on its own merit (out with discussion of kidney donation)
with appropriate referral to a Urology Specialist in line with the ‘2-week
wait’ pathway. (A1)
Contrast enhanced renal CT scan, ultrasound and / or MRI can usually
distinguish between benign lesions such as angiomyolipoma (AML) or
malignancy such as renal cell carcinoma (RCC). Review by a specialist
uroradiologist is recommended. (C1)
Bilateral AML and AML >4 cm generally preclude living kidney donation
although occasionally unilateral large (>4 cm) AML can be used if ex
vivo excision of the AML appears to be straightforward.
An incidental, unilateral solitary AML <4 cm with typical characteristic
CT criteria does not usually preclude donation.
A kidney with an AML <1 cm may be considered for donation or left in
situ in the donor’s remaining kidney.
Kidneys containing a single AML between 1 and 4 cm can be
considered for donation depending on its position, consideration of
whether ex vivo excision of the AML is straightforward, or whether it
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
160
can be left in situ in the recipient and followed with serial ultrasound
imaging. (C1)
Donors with an incidental small (<4 cm) renal mass that appears on
imaging to be a RCC must be seen in a specialist Urology clinic and be
offered standard of care treatment options, including partial and radical
nephrectomy. Renal function permitting, if the person wishes to
consider radical nephrectomy, ex-vivo excision of the small renal mass
with subsequent donation of the reconstructed kidney can be
considered on an individual basis with specific caveats, full MDM
discussion and appropriate informed consent from the donor and
recipient. (D2)
The accidental transmission of malignant disease from donor (deceased or living)
to a recipient by kidney transplantation is well described and was relatively common
before stringent donor criteria were enforced (1-7). Two types of donor-derived
malignancies are possible: inadvertent transfer of tumour tissue (donor transmitted),
and de-novo malignancy arising after transplantation in donor-derived tissue (donor
derived). In a US registry review of 154 cadaveric donors with known cancer,
transmission occurred in 45% of recipients (70/154 donors to 103 recipients),
although these risks may be exaggerated as they come from a voluntary reporting
registry (6). More recent reports from both sides of the Atlantic suggest that
transmission is much less common but still occurs (8-11). To minimise this risk, care
must be taken during evaluation of the potential living donor to ensure that a past
medical history of malignant disease is recorded and that symptoms consistent with
undiagnosed malignancy are identified.
It is worth stating that outcomes after transplantation should be compared to
outcomes when remaining on dialysis, a condition with a high morbidity and
mortality. This has led some to question whether previous tumours with low grade
and slowly progressive biology should be considered in individual cases after
discussion with the oncology MDT. Unfortunately, we do not know the biology of
such tumours under the influence of immunosuppressive drugs. As an example it
has been possible to transplant kidneys from unrelated donors with small renal cell
carcinomas (<3 cm) with a very low risk of recurrence (12-14). Others have
highlighted the low risk of renal transplantation from donors with successfully treated

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
161
low grade and localised prostate cancer (15). Registry data in the UK has
demonstrated that donors in the UK with a past history of high risk cancer have
donated organs with very low risk of transmission (16).
During clinical examination, the possibility of occult malignancy should be borne in
mind and care taken to exclude the presence of potentially malignant skin lesions,
abdominal masses, breast lumps, testicular swelling and lymphadenopathy.
Screening procedures applicable to the general population should be up to date e.g.
cervical screening, mammography, faecal occult blood for colorectal malignancy. A
chest X-ray and imaging of the renal tract should be carried out, and urine analysis
to look for haematuria. Cross sectional imaging of the kidneys may reveal incidental
adrenal masses. Evidence suggests that these are extremely unlikely to be
malignant and if causing clinical concern can be removed at the same time as
nephrectomy with minimal morbidity (17). Other tests such as PSA, tumour markers
or screening for aortic aneurysm are not necessary unless indicated on the basis of
history, clinical examination or routine investigation. It should be remembered that
the risk of malignancy increases with age and that this effect is particularly marked
over the age of 50; at least 75% of cancer cases are diagnosed in those over 65
years old (18).
Figure 5.18.1 Age at First Diagnosis with cancer
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
162
If the potential donor has a history of treated malignant disease, there are no reliable
data from which to accurately predict the risk of tumour transmission to the recipient.
The situation is further complicated by wide variations in the natural history of
different primary tumours. Registry data relating to tumour transmission from
cadaveric donors indicate that certain tumours seem to be particularly high risk,
e.g. lung, breast, and colonic carcinomas, as well as lymphoma and metastatic
melanoma (2,8,10,11). There should be a low threshold to exclude any potential
donor with a history of these cancers, although some potential donors with treated
disease, no evidence of recurrence, long follow-up and favourable histology may be
considered following careful oncology review. In contrast, other registry data have
documented no evidence of tumour transmission, especially when most tumours
were non-melanoma skin cancers or low-grade malignancies (19,20). Advice
adapted from the Amsterdam Forum for Living Donation in 2005 (21) is shown in
Table 5.18.1.
The biology of the tumour should be considered and discussed with the relevant
expert oncology team. There is universal agreement that tumours with a propensity
to late recurrence, e.g. advanced breast cancer, lung cancer, malignant melanoma
and sarcoma are an absolute contraindication to organ donation (22-24),
irrespective of the tumour-free interval. For other types of malignancy, it has been
suggested that consideration for donation may be appropriate if there is no evidence
of tumour recurrence after ten years (5). Factors such as the natural history of the
disease, the grade, stage and site of the tumour and the disease-free interval must
all be taken into account when assessing the risk of transmission. An attempt to
grade tumours into categories of risk was published in 2011 by the Donor
Transmission Advisory Committee (DTAC) in the United States (see Figure 5.18.2)
(25,26).

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
163
Table 5.18.1 Previous Cancer and Fitness for Living Donation
Recommendation
Type of Cancer
Strong or absolute
contraindication
Malignant melanoma
Testicular cancer
Renal cell carcinoma >3 cm
Choriocarcinoma
Haematological malignancy
Lung cancer
Breast cancer
Sarcoma
Possible donation
Treated cancer with high probability of cure
after 5-10 years (favourable classification and
staging) e.g.
Colon cancer (Dukes’ A >5 years ago)
Non-melanoma skin cancer
Carcinoma-in-situ of the cervix or vulva
Localised low grade prostate cancer with
curative treatment, minimum cancer-free
period of 5 years
Renal cell carcinoma <3 cm
Breast cancer Stage I, hormone receptor-
negative, curative surgery, minimum
cancer-free period of 5 years
Ovarian cancer following curative surgery
and minimum cancer-free period of 10
years
Small low grade thyroid cancers
Low grade CNS tumors (WHO Grade 1 &
2)

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
164
If a donor with previously treated malignant disease is to be considered, it is
important that the consent process includes a detailed discussion of risk with both
the donor and the recipient. It should be made clear that transmission of malignant
disease cannot be completely excluded (21). It is also important to consider the
possibility that should a potential donor develop recurrent malignancy, the presence
of a solitary kidney may in certain situations be a major disadvantage, either
because it may be affected directly by recurrent disease or indirectly by the
additional treatment (e.g. chemotherapy) required.
Figure 5.18.2 DTAC Risk Categorisation
5.18.1 Small Renal Mass, including Angiomyolipoma and Renal Cell
Carcinoma
Classic angiomyolipoma (AML) is a triphasic, benign neoplasm composed of mature
adipose tissue, smooth muscle and thick walled blood vessels (27) and can occur
as an incidental finding in donor work-up. Diagnosis of an AML can usually be made
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
165
by imaging without recourse to biopsy; however, it is important to discriminate
classic AML from the uncommon subtype of epitheloid AML, which may have a
malignant phenotype. A specialist uroradiologist should review all cases.
Two large series (29 and 33 patients) observed the natural history of isolated AML
(not as part of tuberous sclerosis complex) followed for approximately two to four
years (28-30). Small (<4 cm) isolated AMLs, detected incidentally, showed a low
risk of increase in size during long-term follow-up. 92% of renal AMLs showed no
radiographic changes, serious complications or new renal or extra-renal lesions
during follow-up. Such patients may be followed conservatively by ultrasonography
every 2 years. AML more than 4 cm in diameter at presentation were more likely to
have significant growth.
For living kidney donors, bilateral AML preclude donation. In unilateral disease,
generally only the affected kidney should be considered for donation. However, if
the AML is <1 cm, the affected kidney may be considered for donation, or in a male
donor can be left in situ in the donor’s remaining kidney. In contrast, it would not be
appropriate to leave an AML in the single remaining kidney of a female of
childbearing age due the risk of increase size and rupture during pregnancy (31). If
an AML is 4 cm or larger, donation should only be contemplated if excision of the
AML is possible, because of the risk of subsequent symptoms. This approach has
been published as case reports describing either in or ex vivo excision of AML of
varying sizes from living donors with a successful outcome (32-35).
If the AML is small, for example 1 cm or less, and its position makes removal
particularly difficult, then implantation of the AML-bearing kidney followed by bi-
annual ultrasound surveillance is reasonable (36).
Donors with an incidental renal mass that appears on imaging to be a renal cell
carcinoma must be seen urgently in a specialist urology clinic. The incidental renal
mass must be diagnosed and managed on its own merit, outwith discussion of
kidney donation, and referred to the appropriate Urology Specialist in a time frame
in keeping with the 2-week wait pathway. Contrast enhanced renal CT scan,
ultrasound and / or MRI are usually able to characterise whether the renal mass
might be a renal cell carcinoma (RCC). The imaging must be reviewed by a
specialist uroradiologist.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
166
Standard of care treatment options depend on the size and location of the renal
mass and include partial nephrectomy and radical nephrectomy. Most people with
an incidental small (<4 cm) renal mass will be counselled toward partial
nephrectomy to preserve renal function, and occasionally minimally invasive
techniques such as radio-frequency ablation or cryotherapy may be indicted.
Most potential kidney donors have excellent renal function and lack co-morbidity in
order to be considered for donor nephrectomy. If the potential donor wishes to
consider radical nephrectomy as opposed to partial nephrectomy, ex vivo excision
of the small renal mass with subsequent donation of the reconstructed kidney can
be considered on a case-by-case basis with specific caveats and after full MDM
discussion; and with appropriate informed consent from the donor and recipient pair
(37-41). Case series from 2005-15 totalling around 60 living donor / recipient pairs
have recently been summarised in a systematic review (42). There are also two
case reports from UK units: one involving the management of a small renal mass
found at the time of donor nephrectomy; and the second in recipients who were at
high immunological risk (43,44). A small survey of UK transplant recipients,
nephrologists and transplant surgeons were supportive of this approach (45).
These approaches should permit transplantation without transmission of donor
malignancy and minimise intervention in the donor, but do require careful case-by-
case discussion. Specific issues requiring careful consideration are:
i) Consideration of percutaneous biopsy in the donor. Histopathological
assessment of biopsy for SRM has become much more widely used and with
improved sensitivity and specificity. It allows diagnosis of whether a SRM is
a RCC, often the subtype of RCC (e.g. clear cell or papillary RCC) and
exclusion of high nuclear grade (Fuhrman 4) RCC.
ii) What is the chance in the donor of bilateral non-synchronous RCC? This is
rare but more likely if there is a family history of RCC or if there is a papillary
RCC. Such patients are likely to be counselled against donation.
iii) A negative chest CT scan (not chest X-ray) is required for donation to be
considered.
iv) Is the recipient appropriate to receive a kidney that will have ex-vivo excision
and reconstruction of a potentially malignant SRM? This may not be
appropriate due to age of recipient, immunological risk or surgical risks from
reconstruction, e.g. bleeding if recipient requires anticoagulation.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
167
v) Will frozen section pathology be needed at the time of ex-vivo excision of the
SRM and reconstruction?
vi) What imaging follow-up will be arranged for both donor and recipient?
References
1. Birkeland SA, Storm HH. Risk for tumor and other disease transmission by
diseases in organ donors. Transplantation 2002; 74:1409-13.
2. Buell JF, Beebe TM, Trofe J, et al. Donor transmitted malignancies. Ann
Transplant 2004; 9: 53-6.
3. Martin DC, Rubini M, Rosen VJ. Cadaveric renal homotransplantation with
inadvertent transplantation of carcinoma. JAMA 1965; 192: 752-4.
4. Matter B, Zukoski CF, Killen DA, Ginn E. Transplanted carcinoma in an
immunosuppressed patient. Transplantation 1970; 9: 71-4.
5. Penn I. Donor transmitted disease: cancer. Transplant Proc 1991; 23: 2629-31.
6. Penn I. Transmission of cancer from organ donors. Ann Transplant 1997; 2: 7-
12.
7. Wilson RE, Hager EB, Hampers CL, Corson JM, Merrill JP, Murray JE.
Immunologic rejection of human cancer transplanted with a renal allograft.
N Engl J Med 1968; 278: 479-83.
8. Desai R, Collett D, Watson CJ, Johnson P, Evans T, Neuberger J. Cancer
transmission from organ donors-unavoidable but low risk. Transplantation
2012; 94: 1200-7.
9. Desai R, Collett D, Watson CJ, Johnson P, Evans T, Neuberger J. Estimated
risk of cancer transmission from organ donor to graft recipient in a national
transplantation registry. Br J Surg 2014; 101: 768-74.
10. Ison MG, Hager J, Blumberg E, et al. Donor-derived disease transmission
events in the United States: data reviewed by the OPTN/UNOS Disease
Transmission Advisory Committee. Am J Transplant 2009; 9: 1929-35.
11. Ison MG, Nalesnik MA. An update on donor-derived disease transmission in
organ transplantation. Am J Transplant 2011; 11: 1123-30.
12. Brook NR, Gibbons N, Johnson DW, Nicol DL. Outcomes of transplants from
patients with small renal tumours, live unrelated donors and dialysis wait-listed
patients. Transpl Int 2010; 23: 476-83.
13. Flechner SM, Campbell SC. The use of kidneys with small renal tumors for
transplantation: who is taking the risk? Am J Transplant 2012; 12: 48-54.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
168
14. Musquera M, Perez M, Peri L, et al. Kidneys from donors with incidental renal
tumors: should they be considered acceptable option for transplantation?
Transplantation 2013; 95: 1129-33.
15. Dholakia S, Johns R, Muirhead L, Papalois V, Crane J. Renal donors with
prostate cancer, no longer a reason to decline. Transplant Rev (Orlando) 2016;
30: 48-50.
16. Desai R, Collett D, Watson CJ, Johnson PJ, Moss P, Neuberger J. Impact of
cytomegalovirus on long-term mortality and cancer risk after organ
transplantation. Transplantation 2015; 99: 1989-94.
17. Arpali E, Aslan A, Scalea J, et al. Living kidney donors with adrenal
incidentalomas: are they appropriate donors. Urology 2016; 87: 100-5.
18. Cancer Research UK: Cancer Incidence by Age: 2012-2014.
http://www.cancerresearchuk.org/health-professional/cancer-
statistics/incidence/age - heading-Zero
19. Feng S, Buell JF, Cherikh WS, et al. Organ donors with positive viral serology
or malignancy: risk of disease transmission by transplantation. Transplantation
2002; 74: 1657-63.
20. Kauffman HM, McBride MA, Delmonico FL. First report of the United Network
for Organ Sharing Transplant Tumor Registry: donors with a history of cancer.
Transplantation 2000; 70: 1747-51.
21. Delmonico F. A report of the Amsterdam Forum on the care of the live kidney
donor: data and medical guidelines. Transplantation 2005; 79: S53-66.
22. Strauss DC, Thomas JM. Transmission of donor melanoma by organ
transplantation. Lancet Oncol 2010; 11: 790-6.
23. Thoning J, Liu Y, Bistrup C, et al. Transmission of angiosarcomas from a
common multiorgan donor to four transplant recipients. Am J Transplant 2013;
13: 167-73.
24. Xiao D, Craig JC, Chapman JR, Dominguez-Gil B, Tong A, Wong G. Donor
cancer transmission in kidney transplantation: a systematic review. Am J
Transplant 2013; 13: 2645-52.
25. Nalesnik MA, Woodle ES, Dimaio JM, et al. Donor-transmitted malignancies in
organ transplantation: assessment of clinical risk. Am J Transplant 2011; 11:
1140-7.
26. Zhang S, Yuan J, Li W, Ye Q. Organ transplantation from donors (cadaveric or
living) with a history of malignancy: review of the literature. Transplant Rev
(Orlando) 2014; 28: 169-75.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
169
27. Halpenny D, Snow A, McNeill G, Torreggiani WC. The radiological diagnosis
and treatment of renal angiomyolipoma - current status. Clin Radiol 2010; 65:
99-108.
28. Steiner MS, Goldman SM, Fishman EK, Marshall FF. The natural history of
renal angiomyolipomata. J Urol 1993; 150: 1782-6.
29. De Luca S, Terrone C, Rossetti SR. Management of renal angiomyolipoma: a
report of 53 cases. BJU Int 1999; 83: 215-8.
30. Chen A, Scherr D, Eid JF. Renal transplantation after in vivo excision of an
angiomyolipoma from a living unrelated kidney donor. J Urol 2000; 163: 1859.
31. Preece P, Mees B, Norris B, et al. Surgical management of haemorrhaging
renal angiomyolipoma in pregnancy. Int J Surg Case Rep 2015; 7C: 89-92.
32. Bissada NK, Bissada SA, Fitts C, Rajagopalan PR, Nelson R. Renal
transplantation from living related donor after excision of angiomyolipoma of the
donor kidney. J Urol 1993; 150: 174-5.
33. Johannes JR, Doria C, Lallas CD. In vivo partial nephrectomy of
angiomyolipoma with concurrent transplantation. Can J Urol 2008; 15: 4184-7.
34. Hetet JF, Rigaud J, Blancho G, Renaudin K, Bouchot O, Karam G. Renal
transplantation after excision of an angiomyolipoma on living donor kidney.
Prog Urol 2004; 14: 205-6.
35. Sener A, Uberoi V, Bartlett ST, Kramer AC, Phelan MW. Living-donor renal
transplantation of grafts with incidental renal masses after ex-vivo partial
nephrectomy. BJU Int 2009; 104: 1655-60.
36. Fritsche L, Budde K, Rogalla P, Turk I, Neumayer H-H, Loening SA. Successful
living related kidney transplantation despite renal angiomyolipoma in situ. J Urol
1999; 162: 480-1.
37. Buell JF, Hanaway MJ, Thomas M, et al. Donor kidneys with small renal cell
cancers: can they be transplanted? Transplant Proc 2005; 37: 581-2.
38. Mannami M, Mannami R, Mitsuhata N, et al. Last resort for renal transplant
recipients, ‘restored kidneys’ from living donors/patients. Am J Transplant 2008;
8: 811-8.
39. Nicol DL, Preston JM, Wall DR, et al. Kidneys from patients with small renal
tumours: a novel source of kidneys for transplantation. BJU Int 2008; 10: 188-
92.
40. Brook NR, Gibbons N, Johnson DW, Nicol DL. Outcomes of transplants from
patients with small renal tumours, live unrelated donors and dialysis wait-listed
patients. Transpl Int 2010; 23: 476-83.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
170
41. Musquera M, Pérez M, Peri L, et al. Kidneys from donors with incidental renal
tumors: should they be considered acceptable option for transplantation?
Transplantation 2013; 95: 1129-33.
42. Lugo-Baruqui A, Guerra G, Arocha A, Burke GW, Ciancio G. Use of kidneys
with small renal tumors for transplantation. Curr Urol Rep 2016; 17: 3.
43. Bycroft JA, Benaragama KS, Green A, Lindsey B, Nicol DL. Incidental renal cell
carcinoma identified during laparoscopic live-related donor nephrectomy. JRSM
Short Rep 2010; 1: 32.
44. Ali AM, Rajagoppal P, Sayed A, Hakim N, David T, Papalois P. Transplant of
kidneys with small renal cell carcinoma in incompatible, heavily
immunosuppressed recipients. Ann R Coll Surg Engl 2012; 94: e189-90.
45. Khurram MA, Sanni AO, Rix D, Talbot D. Renal transplantation with kidneys
affected by tumours. Int J Nephrol 2011; 2010: 529080.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
171
6 SURGERY: TECHNICAL ASPECTS, DONOR RISK AND
PERI-OPERATIVE CARE
Recommendations
Work-up for living kidney donation may include direct or indicative
evaluation of split renal function with the kidney with poorer function
selected for nephrectomy irrespective of vascular anatomy (see
Chapter 5.5). (C2)
Work-up for living kidney donation must include detailed imaging
confirming the vascular anatomy of both donor kidneys and
information about the renal parenchyma and collecting systems. Either
CTA or MRA can be used as current evidence indicates little difference
in accuracy. (B1)
Multiple renal arteries or kidneys with anatomical anomalies are not
absolute contraindications to donation. Decisions must be made on an
individual basis as part of a multi-disciplinary team evaluation. (B2)
All living donors must receive adequate thromboprophylaxis. Intra-
operative mechanical compression and post-operative compression
stockings, along with low molecular weight heparin, are recommended.
(A2)
All living donor surgery must be performed or directly supervised by a
Consultant surgeon with appropriate training in the technique. (C1)
Pre-operative hydration with an overnight infusion and/or a fluid bolus
during surgery improves cardiovascular stability during laparoscopic
donor nephrectomy. (B2)
Pre- and peri-operative intravenous fluid replacement with Hartmann’s
solution is preferred to 0.9% Saline. (B2)
Laparoscopic donor surgery (fully laparoscopic or hand-assisted) is
the preferred technique for living donor nephrectomy, offering a
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
172
quicker recovery, shorter hospital stay and less pain. Mini-incision
surgery is preferable to standard open surgery. (B1)
Haem-o-lok clips are not to be used to secure the renal artery during
donor nephrectomy following a report of an adverse event involving
this technique.(C2)
Patients undergoing living donor nephrectomy are likely to benefit
from the management approaches widely used in “enhanced recovery
after surgery” (ERAS) programmes. (D2)
6.1 Introduction
Living donor nephrectomy is a major surgical operation. This Chapter covers the
pre-operative care and preparation, including the anatomical assessment of the
donor, the nephrectomy, and the early post-operative care of the donor.
Responsibility for the donor lies ultimately with the surgeon performing the donor
nephrectomy but optimal peri-operative care depends on an effective
multidisciplinary approach that includes key contributions from medical, nursing,
anaesthetic, theatre and ward staff. The importance of effective communication
between different team members cannot be over emphasised.
Transplant units should have a written protocol detailing the peri-operative
preparation and post-operative care of kidney donors. This should be reviewed
regularly and updated where necessary. The consent of the donor to undergo
nephrectomy is made on the understanding that the operation will be performed by
an experienced and competent surgeon and that all possible steps will be
undertaken to reduce the incidence of peri-operative complications. Transplant units
should regularly audit outcomes from living donor nephrectomy.
The risks associated with donor nephrectomy vary in accordance with factors
identified in the course of pre-operative assessment and can be divided into peri-
operative risks and the long term risks of life with a single kidney. The majority of
donor nephrectomies in the UK are now performed laparoscopically, but this section
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
173
will consider both the laparoscopic and open operation (including mini-incision),
since all are still performed.
6.2 Assessment of Renal Anatomy
The use of kidneys with anatomical anomalies is now considered only a relative
contraindication to donation by most experienced transplant centres. Relevant
anatomical anomalies may include renal cysts, pelvi-ureteric junction obstruction,
solitary stones <1 cm, duplex ureteric system, and multiple arteries and veins.
Despite initial caution in the use of kidneys with multiple vessels, retrospective
reports from multiple centres have shown that kidneys with multiple renal artery or
vein anomalies, such as circumaortic or retroaortic renal veins, have not been
associated with an increased risk of complications in experienced hands (1,2).
6.2.1 Initial Evaluation
Renal imaging prior to donor nephrectomy can be performed using several
modalities including ultrasound (US), catheter angiography (CA), digital subtraction
angiography (DSA), computed tomography (CT), and magnetic resonance
angiography (MRA). All imaging modalities have both strengths and weaknesses.
The preferred modality is one that can best assess the renal parenchyma, the
urinary drainage system and the presence or absence of variant renal vascular
anatomy, and which best identifies anatomical factors predictive of complications
during the transplant procedure.
Renal anatomy should be assessed during the donor evaluation to confirm the
presence of two kidneys of normal size and to exclude abnormalities such as
hydronephrosis, pelvi-ureteric obstruction, renal cysts and nephrolithiasis. The
simplest non-invasive investigation is an abdominal ultrasound. Although an IVU is
considered to be useful by some, this involves submitting the donor to radiation and
equivalent imaging can be achieved as part of a subsequent evaluation by CT or
MRI (see below).
The rationale for this initial imaging is to confirm equality or near equality of renal
size and function between the two native kidneys, ensuring that the donor will retain
adequate renal function after surgery. A difference in size of 2 cm or more between
the kidneys indicates the possibility of a significant difference in GFR between the
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
174
two kidneys (a difference in function of more than 10% may be considered
significant). In such cases, a split function isotope scan or equivalent split function
measurement should be performed. Many units chose to perform such a study for
all potential donors. Usually the kidney with significantly lower function is selected
for nephrectomy, irrespective of vascular anatomy.
The interpretation of multiple cystic lesions in a potential living kidney donor requires
careful assessment. Multiple renal cysts may indicate polycystic kidney disease,
although 11% of individuals over the age of 50 will have one or more simple renal
cysts. In such a situation, a detailed family history is crucial and in those with a family
history of polycystic kidney disease under the age of 40 years, the presence of two
or more cysts (unilateral or bilateral) indicates autosomal dominant polycystic
disease (ADPKD) (3). It should be noted that a negative scan in this age group is
associated with a 4% false negative rate, and even the presence of a single cyst is
of sufficient concern that advice should be sought regarding genetic testing (section
5.17). For those aged 40 to 59 years, the absence of at least two cysts in each
kidney gives a 100% negative predictive value for ADPKD, whilst for those older up
to four cysts are acceptable in each kidney. It is, however, important to be aware
that polycystic disease can arise from spontaneous mutations and that a family
history may not always be evident.
Kidneys with large simple cysts (>2 cm) are likely to be suitable for donation but
should undergo review in a multidisciplinary meeting including a radiologist, and may
require further cross-sectional imaging.
6.2.2 Vascular Anatomy
Approximately 25% of potential donors will have multiple arteries to one kidney and
around 7% will have multiple vessels to both kidneys (4). A donor kidney with a
single renal artery should, whenever possible, be chosen for transplantation to
minimise the risk of vascular complications in the recipient procedure; similarly,
single renal veins are usually preferred. If both kidneys have single vessels, the left
is usually selected as the longer renal vein on this side facilitates implantation.
Multiple renal arteries have been associated with an increased incidence of
complications in the recipient in some studies but do not adversely influence patient
or graft survival (1,2). It is acceptable to use a kidney with multiple renal arteries
and/or veins for transplantation, provided that the surgeon responsible has the
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
175
necessary experience in implanting and where necessary, reconstructing, the
vasculature of the kidney. Decisions should be made on a case-by-case basis
supported by input from an MDT (5). Imaging is often helpful to identify early arterial
bifurcation and short renal arteries prior to the donor nephrectomy, and to anticipate
the need for additional vascular reconstruction.
6.2.3 Anatomical and Vascular Evaluation
Prior to donor nephrectomy, all donors should undergo a detailed evaluation of
vascular and ureteric anatomy by appropriate imaging, usually CT or MR scanning.
Since these investigations have a small but defined risk for donors and are relatively
costly, they are usually performed as the final investigation during the process of
donor evaluation. Definition of arterial anatomy is important to select the most
appropriate kidney for donation. CT has been shown to have a high (98%)
correlation with operative findings (6-11). MR angiography may also be used,
although the sensitivity at detecting accessory arteries may be lower (8,9,11). Both
modalities can be used to assess venous anatomy, although variations in venous
drainage such as duplex or retro-aortic renal veins or large lumbar veins are not
normally considered as contraindications to donation on that side. Similarly,
assessment of ureteric anatomy and exclusion of nephrolithiasis can be performed
with either modality, and a duplex ureter is not normally considered to be a
contraindication to donation.
Although several case series have been published comparing the use of CT
angiography with MR angiography in the preoperative assessment of living kidney
donors, there appears to be little difference in characterising the renal vasculature
before donation (10,11). It is important to recognise that local preference and
facilities may affect the preferred imaging modality, and this is perfectly acceptable
in light of published evidence.
Nephrolithiasis is considered separately (see section 5.15).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
176
6.3 Peri-operative Mortality
In the USA, good data from retrospective studies show that the peri-operative
mortality is approximately 1 in 3,000 after open living donor nephrectomy (12-15).
More recently, a large study of over 80,000 donors in the US - including significant
numbers of laparoscopic donations - considered all donors reported using the
national mandatory reporting system and showed the 90 day mortality to be a very
similar 3.1 in 10,000 donations (95% CI 2.0-4.6), despite increasing age and obesity
in the donor population (16). Mortality was higher in men than in women (5.1 vs 1.7
per 10,000 donors), in black vs white and Hispanic individuals (7.6 vs 2.6 and 2.0
per 10,000 donors), and in donors with hypertension vs those without hypertension
(36.7 vs 1.3 per 10,000 donors). The longer term risk of death is addressed below.
In the UK, a study published in 2007 of 2,509 donors showed no peri-operative
deaths based on complete Registry data including 601 laparoscopic cases (17).
Before 1998, two known peri-operative donor deaths had been reported in the UK.
One was due to myocardial infarction and one to pulmonary embolus (17) with at
least one further death occurring in 2011 also due to myocardial infarction.
Since the inception of the UK Transplant Living Donor Registry in 2000, a number
of further deaths have been reported following living donor nephrectomy but beyond
the perioperative period. Causes of death have included myocardial
infarction/ischaemic heart disease and malignancy. Although occurring within the
first year after surgery, case reviews have not considered it likely that these events
have been directly related to the process of donation.
The most common causes of death after living donation are pulmonary emboli,
hepatitis and cardiac events (myocardial infarction and arrhythmia) (13,19,21). It has
been pointed out that these death rates are comparable with the annual risk of dying
in a road traffic accident in the USA (0.02%) (15); the corresponding risk for the UK
is 0.33%. Such analogies should be used with caution. Although most potential
donors are accepting of the risks associated with surgery, it must always be
emphasised that there is a small but measurable risk which cannot be eliminated.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
177
6.4 Peri-operative Morbidity
Until 2015, many studies of morbidity after donor nephrectomy had not provided
definitive estimates of the rates of typical post-donation complications as non-
standard, differing classifications were used, and most large published series were
from single centres of excellence. In 2015, Lentine et al combined data from the
United States Transplant Registry with records from a consortium of 97 hospitals
performing living donor kidney transplantation. Data from 14,964 living donors
performed from 2008-12 showed an overall incidence of 16.8% for any perioperative
complication. Complications were formally graded using the Clavien-Dindo
classification (22) with 8.8% of donors manifesting a Clavien 2 complication, 7.3%
a Clavien 3 and 2.5% the most severe (life-threatening) Clavien 4. Complications
included respiratory, cardiac, infections, hernia/wound complications, thrombosis,
bleeding, and most commonly gastrointestinal.
This series included predominantly laparoscopic (including hand-assisted) donor
surgeries but also 2.4% robotically performed nephrectomies and 3.7% open donor
procedures. Only 1 complication (the most severe) was considered for each donor
and multivariate analysis showed that obesity and African American ethnicity were
associated with increased risk of complications, whilst higher annual centre volume
was associated with lower rates of complications.
Earlier reported peri-operative complication rates for living donor nephrectomy had
been summarised for a large number of single centre studies (15). The mean overall
complication rate was estimated at 32% and the major peri-operative complication
rate at 4.4%. The estimated ‘major complication’ rate in a survey by Bay and Hebert
(14) was 1.8%, whereas the American Society of Transplant Physicians (ASTP)
survey (12) reported that 22 out of 9,692 (0.23%) kidney donors experienced
‘potentially life-threatening or permanently debilitating’ complications.
In the UK, analysis of Registry data with mandatory reporting has shown the major
morbidity rate after laparoscopic donor nephrectomy to be 4.5%, and 5.1% for open
nephrectomy (no significant difference) (17). The rate of any morbidity was 10.3%
for laparoscopic surgery and 15.7% for open surgery (p=0.001). In a review of
10,828 living donor nephrectomies performed in the USA between January 1999
and June 2001, reoperation rates were 0.4% for open donors and 1% and 0.9% for
hand-assisted and non-hand-assisted laparoscopic surgery respectively (p=0.001)

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
178
(23). Complications not requiring reoperation were 0.3%, 1% and 0.8% respectively
(p=0.02). However, this study was based on a retrospective survey of transplant
centres with a 73% response rate.
Randomised controlled trials comparing open mini-incision (MODN) and
laparoscopic donor nephrectomy (LDN) have not thus far had sufficient statistical
power to allow an adequate comparison of complication rates between these
techniques. However, comparison of the latest reported complication rates in the
USA with historical series suggests that complication rates in laparoscopic donor
nephrectomy are not significantly higher than those observed with open surgery.
Specific complications that require special mention in pre-operative planning and
counselling include wound related problems such as sepsis, hernia and chronic
pain; the impact of conversion from laparoscopic to open surgery (1-3%); blood loss
and the requirement for blood and blood products (which donors may find
unacceptable e.g. Jehovah’s Witnesses); and finally the cosmetic consequences,
especially of open surgery.
Irrespective of the type of incision, wound pain is a major source of anxiety for the
donor. The incidence of prolonged wound pain following laparoscopic surgery is
difficult to determine but a figure of 3.2% should be regarded as realistic (23). A
small number of patients may require referral to a pain clinic. A recent UK centre
report of 123 donors undergoing open nephrectomy reported that 12% of donors
experienced chronic disabling pain and 14% neuropathic pain (24).
6.5 Long-Term Mortality
The donor must be counselled about the life-long risks of donation in the context of
their own health, age and ethnic background before giving consent for donation.
(See Chapters 5.5 and 10).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
179
6.6 Pre-operative Care and Preparation
6.6.1 General Considerations
Living donor surgery must be carried out by a team with adequate expertise, and in
an environment where donors are regularly cared for. A Consultant anaesthetist with
experience of managing such patients should be present. It is recommended that a
transplant unit should undertake at least 20-30 living donor operations per year to
ensure that adequate expertise is maintained, and should regularly audit its results.
Each donor surgeon should maintain up-to-date surgical experience, and should
also audit his or her individual results.
6.6.2 DVT Prophylaxis
Deep venous thrombosis (DVT) and pulmonary embolism (PE) remain major causes
of morbidity and mortality after major surgery, and living kidney donors are no
exception to this. They should be classified as “medium risk‟ patients, even if
undergoing laparoscopic surgery, and the NICE approved thromboprophylaxis
policy should be followed (25). This entails applying the DH risk assessment tool to
all donors on admission and grading the “relative risk‟ of venous thromboembolism
(VTE), which includes the potential risk of bleeding and which will help to inform the
best form of prophylaxis. Factors such as age >60 years, dehydration, known
thrombophilia, obesity (BMI >30 kg/m
2
), personal history or first- degree relative with
a history of VTE, use of HRT, use of oestrogen-containing contraceptive therapy,
and varicose veins with phlebitis must all be taken into account. Details are available
at http://guidance.nice.org.uk/CG92.
The relative risk of VTE with laparoscopic versus open donor nephrectomy
procedures has not yet been investigated in depth. Based on the pathophysiology
of VTE, factors that may heighten the risk with laparoscopy are the duration of the
procedure (>90 minutes), patient positioning, and the effect of the
pneumoperitoneum. Conversely, shorter hospital stays and more rapid post-
operative mobilisation should decrease the risk (26). Typically this will mean the use
of pneumatic mechanical compression during surgery and both TED stockings and
LMWH from surgery until discharge (27).
Early mobilisation (on the first post-operative day) is recommended. Donors with a
personal history of DVT or PE who undergo surgery are at high risk of developing
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
180
further venous thromboembolism (30% within 5 years) and should be screened to
exclude significant thrombophilia, as should any potential donors with a family
history (first or second degree relative) of VTE. A case series of 130 living donors
who were prospectively screened identified laboratory evidence of thrombophilia in
6.9% of donors and were managed with intensified and prolonged prophylaxis. (28).
In such cases, donation may not be precluded but advice should be sought from a
haematologist (29). Any donors deemed high risk should have prolonged
prophylaxis following discharge for at least 7 to 14 days.
6.6.3 Prophylactic Antibiotics
There is little published evidence to support the use of prophylactic antibiotics in
donor surgery, although many centres have historically used a single dose of
antibiotic at induction.
A randomised controlled trial has recently been reported in abstract form (30). 293
living kidney donors across five UK transplant centres were randomised 1:1 to either
placebo or a single dose of intravenous co-amoxiclav at the time of surgery. The
primary endpoint was the occurrence of any infection at 30 days following surgery.
Antibiotic administration led to a significant reduction in postoperative infection (41.4%
placebo v 26.6% antibiotic, p=0.006), with much of this related to a reduced incidence
of surgical site infection (21.4% placebo v 11.9% antibiotic, p=0.023). Overall the
administration of prophylactic antibiotics reduced the odds of developing postoperative
infection by 50% (CI 31-82%). Following the full publication of this trial and given the
limited downsides, the use of antibiotic prophylaxis is likely to become routine practice
in laparoscopic living donor nephrectomy.
6.6.4 Consent and Site Marking
The law on informed consent has changed following a Supreme Court judgment.
Doctors must now ensure that patients are aware of any “material risks” involved in
a proposed treatment, and of reasonable alternatives, following the judgment in the
case Montgomery v Lanarkshire Health Board (see Chapter 2).
The judgment describes this in terms of “materiality”: “A material risk is one that a
reasonable person in the patient’s position is likely to attach significance to, or if the
doctor is or should reasonably be aware that their patient would be likely to attach
significance to it.” The key is to understand what matters - or is likely to matter - to
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
181
the individual patient.
The GMC guidance ‘Good medical practice and Consent: patients and doctors
making decisions together’ should be followed. Central to this is the principle that
the relationship between a doctor and a patient should be a partnership based on
openness, trust and communication (31).
Standard practice for major surgery is to seek written consent before admission, and
to reconfirm this on admission for surgery. The site should be marked and confirmed
with the patient before leaving the ward for theatre. The appropriate imaging must
be available in theatre and standard safety checks, usually involving the WHO
checklist (32), should be performed before the start of surgery.
6.6.5 Blood Transfusion
Blood is rarely needed during donor nephrectomy, but when it is the case it may be
needed urgently. All donors should be “group and saved‟ and surgery should only
take place where adequate facilities for the provision of urgent blood products are
available. All donors should be counselled about the potential risk of bleeding and
the use of blood and blood products, especially donors with specific religious
affiliation such as Jehovah’s Witnesses. Where blood transfusion is refused or
contraindicated, the use of a cell saver may be indicated.
6.7 Donor Nephrectomy
6.7.1 General Considerations
Living donor surgery is a unique sub-discipline of general surgery. Patients are
selected for their fitness rather than the presence of a morbidity that requires
surgical intervention. Donor surgery, other than the potentially significant
psychological benefits of performing an act of altruism, can only lead to the potential
for harm. Therefore, it is imperative, for the patient and the UK living donor transplant
programme in its entirety, that careful consideration and effort goes into maximising
each donor experience.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
182
6.7.2 Type of Surgery
The vast majority of donor nephrectomy in the UK is carried out using minimally
invasive techniques, either fully laparoscopic or hand assisted, using a trans- or
retro-peritoneal approach to the kidney. A number of studies have attempted to
demonstrate superiority of one technique over another, but the differences or
advantages between the techniques are small and surgery should be performed
using whichever technique the operating surgeon has been trained to perform safely
(33).
A number of vascular stapling devices are available for surgeons to use. The choice
of which device to use is down to surgeon preference.
Discussion at the BTS Chapter of Surgeons meeting, London 2014, reached
consensus that Haem-o-lok clips were not to be used to secure the renal artery
during donor nephrectomy following a report of an adverse event involving this
technique.
6.7.3 Preferred Kidney and Vasculature
The left kidney is usually preferred, assuming both kidneys have equal numbers of
arteries, due to the greater length of the left renal vein. One randomised trial
comparing right and left laparoscopic donor nephrectomy showed no difference in
complication rates but a shorter operating time for right nephrectomy.
The decision on the side of donor nephrectomy should be documented and ideally
made at a multi-disciplinary meeting which includes a review of the vascular
imaging. The potential donor should be informed of any increased risk associated
with this decision. When assessed in the context of a paired exchange programme,
the donor and recipient surgeons should communicate directly to discuss which
kidney is selected for nephrectomy.
6.7.4 Peri-operative Considerations
Multi-modal strategies to enhance recovery after Donor Nephrectomy
Since the 1990s, Henrik Kehlet, a surgeon working in Denmark, has advocated
strategies to address and attenuate the surgical stress response (34,35). These
Enhanced Recovery After Surgery (ERAS) Pathways are well established in several
surgical sub-disciplines, notably colorectal surgery, and have been demonstrated to
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
183
reduce post-operative morbidity, mortality and the length of post-operative hospital
stay (36-38). The role of Enhanced Recovery pathways has yet to be established in
donor nephrectomy; however, the enhanced recovery principles eschewed by other
surgeons performing major intra-abdominal surgery are readily transferrable to
donor nephrectomy. As such, several units in the UK are now adopting these
strategies.
6.7.5 Pre-operative Psychological Preparation
A very simple and key intervention of an Enhanced Recovery pathway is that of pre-
operative preparation. A number of stages in the donor assessment pathway allow
for expectation management, and repeated education at each of these steps aids
with information retention.
Information given to the potential donor should be detailed and should concentrate
on each step of their pre- and post-operative journey. Emphasis should be placed
on what is expected of the patient so that they may aid their own recovery, and the
reasons for each recommendation. The pre-operative consent process should be
performed by the operating surgeon and not be rushed.
6.7.6 Peri-operative Fasting and Insulin Resistance
Guidelines surrounding peri-operative fasting in non-emergency surgical cases (in
patients with no history of gastric emptying disorders) recommend fasting for six
hours for solids (including milk in tea or coffee) and two hours for clear liquids
(40,41).
Overnight fasting has been demonstrated to increase insulin resistance associated
with the surgical stress response, presumably as an adaptation to increase the
bioavailability of glucose for consumption during the ‘fight or flight’ response. Insulin
resistance is related to increased peri-operative morbidity and length of hospital stay
for patients undergoing cardiac and major gastro-intestinal surgery.
Reversing the ‘fasting’ state of the patient by administration of an oral carbohydrate
drink pre-operatively can increase insulin sensitivity by 50%, a state which continues
into the post-operative period. A recent Cochrane analysis of randomised controlled
trials looking at pre-operative carbohydrate loading prior to major abdominal surgery
suggests that there is a more rapid recovery with administration of a carbohydrate
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
184
drink rather than traditional fasting regimens (42). There have been no studies to
date looking at the effect of insulin resistance in donor nephrectomy; however,
extrapolating the results achieved from gastrointestinal surgery, it would seem
reasonable to consider pre-operative carbohydrate loading in patients undergoing
donor nephrectomy. Nutricia Pre-op has been designed and validated for this
purpose. The pre-operative dosing regimen is 4 x 200 mL cartons between 9 pm
and midnight before the operation with a further 2 x 200 mL 2 hours pre-operatively.
In addition, allowing clear fluids up to 2 hours pre-operatively improves patient
comfort by reducing thirst and allows black tea or coffee to be consumed by habitual
caffeine drinkers who may be susceptible to withdrawal headache.
Post-operative fasting should be avoided and early and unrestricted resumption of
fluid and solid food is recommended in the immediate post-operative period.
6.7.7 Peri-operative fluid requirements
The surgical stress response initiates a well-documented cascade of hormonal
pathways leading to a diminished ability of the patient to excrete sodium and water.
Traditional pre-operative intravenous fluid regimens using 0.9% Saline have been
demonstrated to lead to significant fluid retention and weight gain, the development
of hyperchloraemic acidosis, renal oedema, reduced renal blood flow and reduced
renal cortical perfusion, even in healthy volunteers (43). The use of 0.9% Normal
Saline has been demonstrated to lead to inferior surgical outcomes in
gastrointestinal and orthopaedic surgery with increased rates of pulmonary
complications, post-operative Ileus, anastomotic dehiscence and delayed post-
operative recovery. Peri-operative complications in gastrointestinal surgery increase
when the post-operative weight gain exceeds 2.5 kg, reflecting a net fluid gain of
2,500 mL of fluid (44,45). A number of units within the UK follow aggressive pre-
operative intravenous fluid regimens for living donors, with or without the addition of
diuretic agents. Evidence from one randomised control trial (46) and one series has
demonstrated improved cardiovascular stability and reduced sub-clincal renal injury
respectively when such pre-operative hydration strategies are applied (47). Other
units within the UK perform donor nephrectomy restricting intravenous fluid therapy
to Hartmann’s solution given intra-operatively only, aiming for a ‘near 0 fluid
balance.’
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
185
Whilst there are no comparative studies to inform on best practice, outcomes for
donor and recipients from units in the UK are satisfactory. However, with mounting
evidence to suggest that 0.9% Normal Saline is detrimental to patient outcome, and
may indeed contribute to renal dysfunction, the use of this solution in donors cannot
be recommended. Hartmann’s solution is the recommended intravenous fluid of
choice.
6.7.8 Post-operative Analgesia
Adequate analgesia is paramount to achieving excellent outcomes. However,
balancing the level of analgesia with the unwanted side effects of analgesic agents
requires thought, observation and an individual, tailored approach to each patient.
Epidural Anaesthesia
Epidural anaesthesia can achieve excellent post-operative analgesia as well as
significantly attenuate the surgical stress response. In early Enhanced Recovery
protocols, epidural anaesthesia was the preferred method of choice to minimise the
use of opiates in the peri-operative period. However, the side effects (hypotension,
headache, potential for infection, urinary retention, reduced mobility) are well
documented and other opiate sparing strategies have now superseded epidural use.
There is now little place for epidural use within the domain of donor nephrectomy,
especially when performed laparoscopically (48,49).
In-Dwelling Nerve Catheters
The anatomical basis of the nerve supply to the abdominal wall has been well
described. Blockade of the nerve supply to the wound with local anaesthesia is
therefore a very straightforward and attractive option as an ‘opiate sparing’
technique.
Indwelling nerve catheters have been in use for around 15 years and can provide
safe and effective analgesia to a variety of surgical wounds in the thorax and
abdomen as well as upper and lower limbs. Their use as a potential ‘opiate sparing’
strategy within Enhanced Recovery programs is gaining popularity. Their use in
donor nephrectomy surgery is novel but they have been shown to reduce opiate
requirements in hand assisted laparoscopic donor nephrectomy (using an upper
abdominal transverse extraction scar) and in fully laparoscopic donor nephrectomy
(using a Pfannenstiel incision to extract the donor kidney) (50-55).

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
186
The On-Q pain buster device has a well-documented safety record. Correct
anatomical placement of the catheter is paramount to achieving success and there
is a short learning curve to achieve expertise of use. A bolus of 30 mL 0.25%
levobupivacaine is introduced on the operating table followed by a continuous
infusion of 0.125% levobupivacaine at 6-10 mL/hr. The infusion can be administered
via an elastomeric pump or a battery run infusion pump (52).
Opiates
Opiates are an effective analgesic and remain a common treatment of post-
operative pain control worldwide. However, the short term side effects of this class
of medication are significant. Drowsiness, nausea, vomiting, pruritis and lack of
appetite all work against the principles of Enhanced Recovery surgery aiming for
early mobilisation and return to oral intake. More recently, multimodal strategies
have been attempting to introduce ‘opiate sparing’ regimens to ameliorate the early
unwanted side effects of these drugs (55).
Despite these drawbacks, many units in the UK use intravenous patient controlled
opiate administration strategies to good effect. Opiates also have an effective role
for breakthrough pain when opiate sparing strategies have not been effective.
References
1. Hsu TH, Su LM, Ratner LE, Trock BJ, Kavoussi LR. Impact of renal artery
multiplicity on outcomes of renal donors and recipients in laparoscopic donor
nephrectomy. Urology 2003; 61: 323-7.
2. Chedid ME, Muthu C, Nyberg SL, et al. Living donor kidney transplantation
using laparoscopically procured multiple renal artery kidneys and right kidneys.
J Am Coll Surg 2013; 217: 144-52.
3. Pei Y, Obaji J, Dupuis A, et al. Unified criteria for ultrasonographic diagnosis of
ADPKD. J Am Soc Nephrol 2009; 20: 205-12.
4. Weinstein SH, Navarre RJ, Loening SA, Corry RJ. Experiences with live donor
nephrectomy. J Urol 1980; 124: 321-3.
5. Kälble T, Lucan M, Nicita G, et al. EAU guidelines on renal transplantation. Eur
Urol 2005; 47: 156-66.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
187
6. Rajamahanty S, Simon R, Edye M, Butt K, Eshghi M. Accuracy of three-
dimensional CT angiography for preoperative vascular evaluation of
laparoscopic living renal donors. Endourol 2005; 19: 339-41.
7. Lewis GR, Mulcahy K, Brook NR, Veitch PS, Nicholson ML. A prospective study
of the predictive power of spiral computed tomographic angiography for defining
renal vascular anatomy before live-donor nephrectomy. BJU Int 2004; 94: 1077-
81.
8. Kim JC, Kim CD, Jang MH, et al. Can magnetic resonance angiogram be a
reliable alternative for donor evaluation for laparoscopic nephrectomy? Clin
Transplant 2007; 21: 126-35.
9. Israel GM, Lee VS, Edye M, et al. Comprehensive MR imaging in the
preoperative evaluation of living donor candidates for laparoscopic
nephrectomy: initial experience. Radiology 2002; 225: 427-32.
10. Arévalo Pérez J, Gragera Torres F, Marín Toribio A, Koren Fernández L,
Hayoun C, Daimiel Naranjo I. Angio CT assessment of anatomical variants in
renal vasculature: its importance in the living donor. Insights Imaging 2013; 4:
199-211.
11. Gluecker TM, Mayr M, Schwarz J, et al. Comparison of CT angiography with
MR angiography in the preoperative assessment of living kidney donors.
Transplantation 2008; 88; 1249-56.
12. Bia MJ, Ramos EL, Danovitch GM, et al. Evaluation of living renal donors. The
current practice of US transplant centers. Transplantation 1995; 60: 322-7.
13. Najarian JS, Chavers BM, McHugh LE, Matas AJ. 20 years or more of follow-
up of living kidney donors. Lancet 1992; 340: 807-10.
14. Bay WH, Hebert LA. The living donor in kidney transplantation. Ann Intern Med
1987; 106: 719-27.
15. Kasiske BL, Ravenscraft M, Ramos EL, Gaston RS, Bla MJ, Danovitch GM.
The evaluation of living renal transplant donors: clinical practice guidelines.
J Am Soc Nephrol 1996; 7: 2288-313.
16. Segev DL, Muzaale AD, Caffo BS, et al. Perioperative mortality and long-term
survival following live kidney donation. JAMA 2010; 303: 959-66.
17. Hadjianastassiou VG, Johnson RJ, Rudge CJ, Mamode N. 2509 living donor
nephrectomies, morbidity and mortality, including the UK introduction of
laparoscopic donor surgery. Am J Transplant 2007; 7: 2532-7.
18. Bakran A. Postal survey of living donor kidney transplant units. Presented at the
symposium “Meeting the challenges of live donation”. Royal College of
Physicians, 21 April 1998.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
188
19. Bennett AH, Harrison JH. Experience with living familial renal donors. Surg
Gynecol Obstet 1974; 139: 894-8.
20. Lentine KL, Lam NN, Axelrod D,
et al. Perioperative complications after living
kidney donation: a national study. Am J Transplant 2016; 16: 1848-57.
21. Uehling DT, Malek GH, Wear JB. Complications of donor nephrectomy. J Urol
1974; 111: 745-6.
22. Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of
surgical complications: five-year experience. Ann Surg 2009; 250: 187-
96.
23. Matas AJ, Bartlett ST, Leichtman AB, Delmonico FL. Morbidity and mortality
after living kidney donation, 1999-2001: survey of United States transplant
centers. Am J Transplant 2003; 3: 830-4.
24 Owen M, Lorgelly P, Serpell M. Chronic pain following donor nephrectomy - a
study of incidence, nature and impact of chronic post nephrectomy pain. Eur J
Pain 2010; 14: 732-4.
25. NICE Guidance on VTE. www.nice.org.uk/guidance/CG92.
26. Kakkar AK. Prevention of venous thromboembolism in general surgery. In:
Colman RW, Clowes AW, George JN, Goldhaber SZ, Marder VJ,
eds. Hemostasis and thrombosis: basic principles and clinical practice. 5th ed.
Philadelphia, PA: Lippincott, Williams & Wilkins; 2006: 1361-7.
27. Roderick P, Ferris G, Wilson K, et al. Towards evidence-based guidelines for
the prevention of venous thromboembolism: systematic reviews of mechanical
methods, oral anticoagulation, dextran and regional anaesthesia as
thromboprophylaxis. Health Technol Assess 2005; 9: iii-iv, ix-x, 1-78.
28 Biglarnia A, Bergqvist D, Johansson M, Wadstrom J. Venous thromboembolism
in live kidney donors - a prospective study. Transplantation 2008: 86: 659-61.
29. British Society for Haematology (BSCH) Guidelines. Investigation and
management of heritable thrombophilia, 2001.
www.bcshguidelines.com/guidelinesMENU.asp
30. Ahmed Z, Uwechue R, Kessaris N, Mamode N. Prophylaxis of wound infections
- antibiotics in renal donation (POWAR): a multicentre UK double blinded
placebo controlled randomised controlled trial. American Transplant Congress.
(abstract) 2018.
31. General Medical Council: Good medical practice and consent: patients and
doctors making decisions together. http://www.gmc.uk.org/guidance/ethical_
guidance/consent_guidance_index.asp
32. WHO's patient-safety checklist for surgery. Lancet 2008: 372; 1148-9.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
189
33. Dols LF, Kok NF, Ijzermans JN. Live donor nephrectomy: a review of evidence
for surgical techniques. Transplant Int 2010; 23: 121-30.
34. Kehlet H, Mogensen T. Hospital stay of 2 days after open sigmoidectomy with
a multimodal rehabilitation programme. Br J Surg 1999; 86: 227-30.
35. Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-
track surgery. Ann Surg 2008; 248: 189-98.
36. Lassen K, Coolsen MM, Slim K, et al. Guidelines for perioperative care for
pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®)
Society recommendations. World J Surg 2013; 37: 240-58.
37. Varadhan KK, Lobo DN, Liunqqvist O. Enhanced recovery after surgery: the
future of improving surgical care. Crit Care Clin 2010; 26: 527-47.
38. Fearon, KCH, Ljunqqvist O, Von Meyenfeldt M, et al. Enhanced recovery after
surgery: a consensus review of clinical care for patients undergoing colonic
resection. Clin Nutr 2005; 24: 466-77.
39. Dwyer AJ, Tarassoli P, Thomas W, Porter P. Enhanced recovery program in
total hip arthroplasty. Indian J Orthop 2012; 46: 407-12.
40. Smith I, Kranke P, Murat I, et al. Perioperative fasting in adults and children.
Eur J Anaesthesiol 2011; 28: 556-69.
41. Ljunqqvist O. Modulating postoperative insulin resistance by preoperative
carbohydrate loading. Best practice & research. Best Pract Res Clin
Anaesthesiol 2009; 23: 401-9.
42. Awad S, Varadhan KK, Ljunqqvist O, Lobo DN.. A meta-analysis of randomised
controlled trials on preoperative oral carbohydrate treatment in elective surgery.
Clin Nutr 2013; 32: 34-44.
43. Chowdhury AH, Cox EF, Francis ST, Lobo DN. A randomized, controlled,
double-blind crossover study on the effects of 2-L infusions of 0.9% saline and
plasma-lyte(R) 148 on renal blood flow velocity and renal cortical tissue
perfusion in healthy volunteers. Ann Surg 2012; 256: 18-24.
44. Shaw AD, Bagshaw SM, Goldstein SL, et al. Major complications, mortality, and
resource utilization after open abdominal surgery. Ann Surg 2012; 255: 821-9.
45. Varadhan KK, Lobo DN. A meta-analysis of randomised controlled trials of
intravenous fluid therapy in major elective open abdominal surgery: getting the
balance right corrigendum. Proc Nutr Soc 2010; 69: 488-98.
46. Mertens zur Borg IR, Bi Base M, Verbrugge S, Ijzermans JN, Gommers D.
Comparison of three perioperative fluid regimes for laparoscopic donor
nephrectomy: a prospective randomized dose-finding study. Surg Endosc 2008;
22: 146-50.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
190
47. Aitken E, Vesey A, Glen J, Clancy M. Neutrophil-gelatinase associated lipocalin
(N-GAL) to assess perioperative acute kidney injury in hand-assisted
laparoscopic donor nephrectomy: a pilot study. Indian J Transplant 2015; 9:
168-9.
48. Kehlet H, Rung GW, Callesen T. Postoperative opioid analgesia: time for a
reconsideration? J Clinl Anesth 1996; 8: 441-5.
49. Carli F, Kehlet H, Baldini G, et al. Evidence basis for regional anesthesia in
multidisciplinary fast-track surgical care pathways. Reg Anesth Pain Med 2011;
36: 63-72.
50. Chelly JE, Ghisi D, Fanelli F. Continuous peripheral nerve blocks in acute pain
management. Br J Anaesth 2010; 105 S1: i86-96.
51. Beaussier M, El’Ayoubi H, Schiffer E, et al. Continuous preperitoneal infusion
of ropivacaine provides effective analgesia and accelerates recovery after
colorectal surgery. Anesthesiology 2007; 107: 461-8.
52. Baig MK, Zmora O, Derdemezi J, Weiss EG, Noqueras JJ, Wexner SD. Use of
the ON-Q pain management system is associated with decreased
postoperative analgesic requirement: double blind randomized placebo pilot
study. J Am Coll Surg 2006; 202: 297-305.
53. Stephenson B, McGrogan D, Pattenden C,Brown T, Iston N. Outcomes after
hand-assisted laparoscopic donor nephrectomy can be improved by an
enhanced recovery after surgery programme. Oral presentation, British
Transplantation Society, Bournemouth, 2015.
https://bts.org.uk/wp-content/uploads/2016/09/BTS_Abstract_pdf_2015.pdf
54. Brown T, et al. Use of wound infiltration catheters for enhanced recovery in fully
laparoscopic live donor nephrectomies. Oral presentation, Enhanced Recovery
after Surgery UK, Edinburgh, 2015.
55. White PF. The changing role of non-opioid analgesic techniques in the
management of postoperative pain. Anesthesia & Analgesia 2005; 101: S5-
S22.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
191
7 HISTOCOMPATIBILITY TESTING FOR LIVING DONOR KIDNEY
TRANSPLANTATION
Recommendations
Initial assessment of donor and recipient histocompatibility status
must be undertaken at an early stage in living donor kidney transplant
work-up to avoid unnecessary and invasive clinical investigation. (B2)
Screening of potential living donor kidney transplant recipients for
clinically relevant antibodies is important for ensuring optimal donor
selection and graft survival. (A1)
Antibody screening is especially important when potential living donor
transplant recipients undergo reduction or withdrawal of
immunosuppression. (B2)
Post-transplant antibody monitoring must be undertaken according to
the BSHI/BTS guidelines. (B1)
Transplant units and histocompatibility laboratories must agree an
evidence-based protocol to define antibody screening and crossmatch
results that constitute a high immunological risk to transplantation.
(B2)
When possible, the HLA type(s) of partners/offspring of female
recipients who have had previous pregnancies should be determined
to aid immunological risk assessment for repeat paternal HLA
mismatches in women with low level DSA. (B1)
A pre-transplant serum sample collected within 14 days of the planned
date for transplantation must be tested in a sensitive antibody
screening and donor crossmatch assay and transplantation should not
usually be performed if the crossmatch test is positive, unless the
antibody is shown to be indicative of acceptable immunological risk.
(A1)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
192
Changes in immunosuppression during the transplant work-up must
be notified to the histocompatibility laboratory and additional antibody
screening and donor-recipient crossmatch tests must be undertaken
as indicated. (B1)
HLA matching may be preferred when there is an option of selecting
between living donors, particularly to reduce the possibility of
subsequent sensitisation. This is important for younger recipients
where repeat transplantation may be required. However, it is
recognised that other donor factors will be taken into account. (B1)
For patients with an ABO/HLA incompatible and/or a poorly HLA
matched living donor, consideration should be given to entry into the
UK living kidney sharing scheme (UKLKSS) to identify a more suitable
donor. (B2)
The histocompatibility laboratory must issue an interpretive report
stating the donor and recipient HLA mismatch, recipient sensitisation
status and crossmatch results, and define the associated
immunological risk for all living donor-recipient pairs. (A1)
Policies defining the histocompatibility requirements for living donor kidney
transplantation should be jointly established between the clinical transplant team
and the consultant histocompatibility scientist in each centre. There are three
components to the histocompatibility assessment: determination of donor-recipient
HLA mismatch status; identification of alloantibodies in patient serum that could be
potentially harmful to a transplanted organ; and confirmation of antibody
compatibility by performing a donor-recipient crossmatch. The results of these
investigations provide an immunological risk assessment, which together with
clinical information provide guidance on the suitability of a particular living kidney
donor-recipient pair for transplantation. These guidelines are applicable to ABO
blood group compatible, HLA antibody compatible transplants and are to be read in
conjunction with the BSHI/BTS ‘Guidelines for the Detection and Characterisation
of Clinically Relevant Antibodies in Allotransplantation’ (1). The BTS has separate
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
193
guidelines for ABO Blood Group and HLA Antibody Incompatible (HLAi)
Transplantation (2).
Initial assessment of donor and recipient histocompatibility status should be
undertaken at an early stage in the donor work-up to avoid unnecessary and
invasive clinical investigations. Histocompatibility assessments and interpretation of
test results should only be undertaken in an appropriately accredited laboratory (e.g.
United Kingdom Accreditation Service (UKAS) / European Federation for
Immunogenetics (EFI)) by scientists with specialist training in Histocompatibility &
Immunogenetics, as demonstrated by FRCPath or equivalent level qualification and
experience. The onus is on the referring centre to provide accurate information and
donor and recipient samples necessary to fulfil these guidelines.
7.1 Assessment of Donor-Recipient HLA Mismatch Status
In the absence of preconditioning protocols, the choice of a living donor is restricted
by the requirement for ABO blood group compatibility.
HLA typing of the recipient and all potential living donors should be performed using
DNA-based methods to at least two digit (low) resolution for HLA-A, -B, -C, -DR and
-DQ and the donor-recipient mismatch determined. In addition, for patients known
to have HLA-DP specific alloantibodies, donor and recipient HLA-DP typing should
be performed. The level of donor and recipient HLA compatibility is usually
expressed as an HLA-A, -B and -DR mismatch grade determined from the number
of donor HLA specificities at each locus that are absent in the recipient. A donor and
recipient with no HLA-A, -B, -DR incompatibilities is denoted ‘0.0.0’, whereas a fully
mismatched combination is denoted ‘2.2.2’. In the case of transplants between
siblings there is a 1 in 4 chance of inheriting the same two HLA-bearing parental
haplotypes, a 1 in 2 chance of sharing one parental haplotype and a 1 in 4 chance
of sharing no parental haplotypes.
In the case of genetically related donors, ABO blood group and HLA typing results
can indicate the nature of the familial relationship. Informed consent must therefore
be obtained by the referring centre from both the recipient and all genetically related
potential donors before these tests are undertaken (see section 4.3).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
194
Selection of the most suitable donor for a particular recipient is complex and the
HLA mismatch grade will be considered together with other factors such as donor
and recipient age, sensitisation status and alternative options for transplantation,
both now and in the future (see also section 7.4 and Chapter 11).
7.2 Identification and Characterisation of Alloantibodies
Pre-transplant antibody screening
The presence of pre-transplant HLA-specific antibodies that are reactive against
mismatched donor HLA is potentially harmful to a transplanted kidney and therefore
a policy for the detection of such antibodies must be rigorously implemented.
Immunological sensitisation can arise through exposure of the potential recipient to
allogeneic tissue bearing foreign HLA, such as transfusion of blood products,
pregnancy (including miscarriage and terminated pregnancy), and previous
transplantation. HLA-specific alloantibodies can also arise naturally through cross-
reactivity with pathogens, when they are termed idiopathic antibodies.
Particular attention should be paid to low-level donor HLA-specific antibodies
(normally classified as low immunological risk) in patients previously exposed to that
same HLA specificity through previous transplantation or, in female patients,
pregnancy. In these cases there is the risk of an anamnestic response that is often
refractory to baseline induction immunosuppression.
It is essential for the laboratory to have accurate information about the timing and
nature of all potential allosensitisation events throughout the patient’s lifetime.
Recent and past potential allosensitisation events, including recent infections, must
be documented by the referring clinical team and reported to the histocompatibility
laboratory. Recipient serum samples must be obtained for HLA-specific antibody
screening at least every three months, and additional samples collected at 14 and
28 days after transfusion of any blood products.
Potential recipients listed for repeat transplantation who are receiving
immunosuppression while under assessment for living kidney transplantation are at
high risk of de novo sensitisation, particularly if the baseline immunosuppression is
changed, reduced or withdrawn. For patients with a failing/failed transplant,
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
195
consideration should be given to the potential benefits of immunosuppression
reduction/withdrawal and the risks of developing de novo HLA-specific
allosensitisation that could severely restrict future options for transplantation. It is
the responsibility of the clinical team to notify the histocompatibility laboratory of
such changes and additional serum samples should be obtained for HLA-specific
antibody screening at four weeks after any change in immunosuppression.
Recipient sera must be tested for HLA-specific alloantibodies according to the
BSHI/BTS guidelines (1) and HLA specificities to which the patient is sensitised
should be identified. In cases where HLA-DP-specific antibodies are detected in
recipient serum, donor-recipient HLA-DP status and potential HLA-DP-specific
antibody incompatibility should be determined. Recipients that have donor HLA-
specific antibodies (unacceptable mismatches) identified in recent and/or past
(historic) serum samples should have a formal immunological risk assessment
based on donor HLA type, antibody levels, priming source and duration in
consultation with the clinical team and, where appropriate, may be considered for
HLAi transplantation. These discussions should take place at the earliest
opportunity, to avoid delay and unnecessary investigation.
In many cases, the living donor kidney transplant work-up may be prolonged and it
is not uncommon for a year or more to elapse between the initial histocompatibility
assessment and the planned operation. During this period, the antibody
compatibility status of the potential recipient and donor(s) must be monitored and
any changes in the patient’s antibody profile should be reported to the transplant
team. The recipient must have contemporary antibody screening results available
using samples obtained within three months of the transplant operation. Any
potential alloantibody priming events that occur within one month of the latest
antibody screening sample, or after the sample collection date could change the
donor-recipient antibody compatibility status and will obviate all previous results.
Post-transplant antibody screening
Monitoring of HLA-specific antibodies in recipient serum after the transplant
operation can provide helpful prognostic information for the diagnosis of antibody-
mediated rejection and help guide post-transplant rejection treatment, antibody
reduction therapy and choice of maintenance immunosuppressive therapy. Post-
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
196
transplant antibody monitoring should be undertaken according to the BSHI/BTS
guidelines (1).
7.3 Pre-transplant Donor-Recipient Crossmatch Test
A prospective pre-transplant donor-recipient crossmatch test is performed to confirm
the presence or absence of donor HLA-specific alloantibodies. The results can only
be interpreted in conjunction with knowledge of pre-transplant alloantibody priming
events, donor-recipient HLA mismatches and pre-transplant antibody screening
results. In the case of donor-recipient combinations where donor HLA-specific
antibodies are present in recipient serum, the crossmatch test can provide
information about antibody levels and the associated immunological risk (3). Pre-
formed donor HLA-specific antibodies present in recipient serum can cause
hyperacute and acute rejection and there should be close liaison between the
histocompatibility laboratory and the clinical team.
Living kidney donor crossmatch tests should be carried out according to the
BSHI/BTS Guidelines for the Detection and Characterisation of Clinically Relevant
Antibodies, and tested using lymphocytes isolated from donor peripheral blood (1).
Because of the opportunity for planned living donor transplant work-up, a virtual
crossmatch is not acceptable. Living donor crossmatch testing is usually carried out
at the time of first referral. The final crossmatch must always be undertaken using a
serum sample obtained within 14 days of the planned operation date. This time
frame minimises the risk of a change in recipient antibody status, but any potential
alloantibody priming event around the time of the final crossmatch will obviate the
results.
The selection of recipient serum samples for crossmatch and choice of target cell
type (i.e. donor peripheral blood lymphocytes, isolated donor T lymphocytes and/or
B lymphocytes) and the technique used (complement dependent lymphocytotoxicity
[CDC] and/or flow cytometric [FC] crossmatch) will depend on previous alloantibody
priming events and pre-transplant antibody screening results, and should conform
to the BSHI/BTS guidelines (1). It is recommended that allosensitised recipients with
pre-formed HLA class I- and/or class II-specific alloantibodies and recipients
awaiting repeat transplantation should undergo donor T lymphocyte (for HLA class
I sensitised patients) or T and B lymphocyte (for HLA class II sensitised patients)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
197
flow cytometric crossmatching as a minimum. Undertaking a CDC donor T and B
lymphocyte crossmatch using untreated and dithiothreitol (DTT) treated recipient
serum can provide further information for risk stratification (3). Result interpretation
and acceptable immunological risk stratification should be undertaken according to
local policy and BSHI/BTS guidelines. A positive donor lymphocyte crossmatch test
performed using DTT treated sera by CDC carries a high immunological risk of
hyperacute and acute humoral rejection and constitutes a veto to transplantation,
unless an effective HLAi strategy is used to minimise the risk of graft failure.
Careful consideration must be given to the sensitisation status and crossmatch
results for proposed transplants where recipient allosensitisation priming has
previously occurred through exposure to the donor HLA, either directly (e.g.
offspring donor to mother) or indirectly (shared donor HLA haplotype in
spousal/partner donation to female recipient following pregnancy, or repeat
transplants using a second related donor). The occurrence of an anamnestic
immune activation of latent donor alloantigen-specific lymphocytes and uncontrolled
graft rejection has been observed following crossmatch negative male to female
spousal transplantation and this risk may be pre-empted and minimised by using
sensitive antibody screening methods, appropriate crossmatch techniques and
tailored immunosuppression.
A further important consideration relates to patients undergoing living donor kidney
transplant assessment following a previous failed or failing kidney transplant that
remains in situ. Such patients often have immunosuppression reduced or withdrawn
during the period of clinical work-up, because of a desire to reduce unnecessary
medication. This is frequently associated with the development of de novo HLA-
specific antibodies to the allograft which cause a previously unexpected positive
crossmatch and which then preclude future transplantation from an HLA-
mismatched living donor. Consideration must be given to the relative risk of
maintaining recipient immunosuppression during the donor work-up, the benefit of
immunosuppressive drug reduction or withdrawal, and the risk of de novo
allosensitisation. A reduction or stopping of immunosuppression within one month
of the planned operation date is contraindicated and may delay or preclude
transplantation. As a minimum, this would necessitate additional antibody screening
and donor-recipient crossmatch tests to be undertaken using a current serum
sample obtained within 24 hours before the transplant operation.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
198
7.4 Selection of Suitable Donor-Recipient Pairs
The presence of donor-specific HLA antibodies or a positive crossmatch in a
sensitised patient is a contraindication to transplantation unless desensitisation
protocols are employed. In a sensitised patient, a well matched donor is more likely
to be antibody compatible than a poorly matched donor. Transplants between
siblings offer the best opportunity for a well matched graft because of familial
inheritance of HLA genes. As described above, kidney transplants from offspring to
the mother or from a father to the mother of his children should be approached with
caution, but where HLA sensitisation is excluded and a negative crossmatch
achieved, transplant outcomes are equivalent to those for other non-HLA identical
living donor transplants (4,5).
A widely cited publication of the experience of living unrelated spousal donor kidney
transplantation in North America showed that graft survival rates for such transplants
was equivalent to that of HLA-mismatched living related donor kidney transplants
(5). This equates with the current UK experience (see Chapter 11). The
Collaborative Transplant Study (CTS) found a significant reduction in graft survival
when living donor kidney transplants were mismatched at HLA-A, -B and -DR (4).
CTS analysis of more than 5,000 living unrelated donor transplants performed
between 1995 and 2002 showed a highly significant influence of HLA matching on
graft survival (6), but survival of even the worst matched kidneys was better than
seen in deceased donor transplantation. However, a more recent analysis of the UK
Transplant registry of living donor kidney transplants performed between 2000 and
2007 did not show an influence of HLA matching on transplant outcome (7).
A key point is that when a poorly matched kidney transplant fails because of
rejection, the recipient is at high risk of becoming highly sensitised (1), restricting
options for repeat transplantation. This is particularly relevant for paediatric
recipients and young adults who are likely to require re-transplantation within their
lifetime and for whom avoiding sensitisation, particularly to common antigens, is
important. Children are often registered on the transplant list with mismatched
parental HLA specificities listed as unacceptable to avoid sensitisation against these
prospective living donors. In contrast, in the context of older spouse couples where
a second transplant is unlikely, the risk of sensitisation is not a major concern.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
199
For patients with an ABO/HLA incompatible and/or a poorly HLA matched, living
donor, consideration should be given to entry into the UK living kidney sharing
scheme (UKLKSS) to identify a more suitable donor (8).
7.5 Antibody Incompatible Living Donor Transplantation
Antibody incompatible transplantation (AIT) may be an option for some patients who
have a potential living donor where there is a specific immunological barrier to
transplantation. Such transplantation falls into two categories: ABO incompatible
transplantation, where transplantation occurs across an ABO blood group barrier
(e.g. from a blood group B donor to a blood group O recipient); and HLA-
incompatible transplantation, where the recipient has high titres of antibodies
against one or more specific HLA antigens present in the donor.
Both forms of transplantation are established in the UK and contribute to the
expansion of the living donor pool. (see section 8.3). Close liaison between clinicians
and histocompatibility laboratories is obviously critical for such transplantation,
which should be concentrated in units with particular expertise.
The BTS has published specific guidelines on antibody incompatible transplantation,
which should be referred to (2). The following summary points are derived from
these guidelines:
Recommendations (Not graded)
Antibody incompatible transplantation (AIT) should only be undertaken
after prior consideration of entry of the donor-recipient pair into the UK
Living Kidney Sharing Schemes (UKLKSS) (see Chapter 8).
AIT should be considered as part of an ongoing structured programme,
and should not be performed on an occasional basis.
To initiate a programme, a unit should be able to demonstrate a
demand of at least five cases a year and appropriate support from
clinical transplant, plasmapheresis and histocompatibility teams. An
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
200
AIT programme requires funding for additional staff and consumables,
and all programmes should receive Commissioner support.
There is insufficient evidence to make precise recommendations for
treatment protocols, but units should have a written protocol based on
best published practice. This should include recommendations on
prevention, diagnosis and treatment of antibody mediated rejection.
Protocols that follow the above can be regarded as established
treatment and do not require Ethics Committee approval as research
procedures. However, the standard of consent should include detailed
written information which describes the risks of the procedure. The
transplant donor should receive equivalent information to the
recipient, so they are aware of the risks of the procedure to the
recipient, whether it results in a transplant or not. Potential recipients
and donors should be aware of their treatment choices, especially the
option of exchange (pooled/paired) transplantation.
Laboratories should be able to define antibodies to the standard
defined in the BSHI/BTS document ‘Guidelines for the Detection and
Characterisation of Clinically Relevant Antibodies in Solid Organ
Transplantation’. Sensitive and rapid techniques for the measurement
of donor-specific HLA antibody levels must be available.
If ABOi transplantation is to be performed, blood group antibody titres
need to be measured, with differentiation between A1 and A2
subgroups of recipient blood group A (when appropriate) and
discrimination between IgG- and IgM-specific ABO antibodies. In living
donor transplantation, a 7 day per week service with same day turn-
around time is required.
AIT results in an improved quality of life when compared to dialysis.
Additionally, many patients receiving antibody incompatible
transplants may have no other chance of a transplant. Transplantation
is cost effective over time with a saving of about £15,000 per annum
compared to dialysis when averaged over a 10 year period
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
201
Every patient undergoing AIT should be audited on a local and national
basis, with the national audit through the AIT Registry.
The UK AIT Registry will define the optimal dataset to be collected, and
will be able to report AIT activity against benchmark outcome data from
international reports and the national dataset of renal transplantation.
References
1. Guidelines for the detection and characterisation of clinically relevant antibodies
in allotransplantation. British Society for Histocompatibility and Immunogenetics
and British Transplantation Society, 2015.
www.bts.org.uk/wp-content/uploads/2016/09/06_BTS_BSHI_Antibodies-1.pdf
2. British Transplantation Society, Guidelines for Antibody Incompatible
Transplantation, 3
rd
Edition, 2015.
www.bts.org.uk/wp-content/uploads/2016/09/02_BTS_Antibody_Guidelines-
1.pdf
3. Taylor CJ, Kosmoliaptsis V, Summers DM, Bradley JA. Back to the future:
application of contemporary technology to longstanding questions about the
clinical relevance of human leukocyte antigen-specific alloantibodies in renal
transplantation. Human Immunol 2009; 70: 563-8.
4. Opelz G. Impact of HLA compatibility on survival of kidney transplants from
unrelated live donors. Transplantation 1997; 64: 1473-5.
5. Terasaki PI, Cecka JM, Gjertson DW, Cho YW. Spousal and other living donor
transplants. In: Clinical Transplants 1997. Eds Cecka JM, Terasaki PI. UCLA
Tissue Typing Laboratory, Los Angeles, USA, pp 269-84.
6. Collaborative Transplant Study Newsletter 2004; 2, May 1.
www.ctstransplant.org
7. Fuggle SV, Allen JE, Johnson RJ, et al. Factors affecting graft and patient
survival after live donor kidney transplantation in the UK. Transplantation 2010;
89: 694-701.
8. Kosmoliaptsis V, Gjorgjimajkoska O, Sharples LD, et al. Impact of donor
mismatches at individual HLA-A, -B, -C, -DR and -DQ loci on the development
of HLA-specific antibodies in patients listed for repeat renal transplantation.
Kidney Int 2014; 86: 1039-48.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
202
8 EXPANDING THE DONOR POOL
Recommendations
Coherent organisational and clinical practices are essential between
transplant centres to optimise the UK Living Kidney Sharing Schemes
(UKLKSS) and to maximise the number of potential transplants that
proceed. (B1)
To maximise transplant opportunities within the UKLKSS, donors and
recipients must only be included in a matching run if:
o Their clinical assessment and histocompatibility screening are
complete and up to date. (B1)
o If matched, they are available to attend for crossmatch testing
and proceed to surgery within the designated timeframes. (B1)
o Relevant complex donor considerations identified in the ‘pre-
run’ and donor HLA and age preferences have been discussed
and agreed with the recipient. (B1)
o They understand their roles and responsibilities with respect to
other donors and recipient pairs in the schemes with whom they
may be matched. (B1)
The default for all non-directed altruistic kidney donors (NDADs) is to
donate into an altruistic donor chain (ADC) within the UKLKSS
provided that there is no higher priority patient on the national
transplant list. (B1)
All altruistic donors (non-directed and directed) must undergo formal
mental health assessment with a mental health professional before
donation. (C1)
Living kidney donors who are antibody incompatible with their
recipient must have all the options and risks explained to them,
including donation into the UKLKSS and antibody removal. (C1)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
203
As a minimum, donors must be made aware that a compatible
transplant has the best chance of success and direct antibody
incompatible transplant is associated with higher short- and long-term
risk, if that is what is proposed. (C1)
The UK Living Kidney Sharing Schemes (UKLKSS) were established after the
introduction of the Human Tissue Acts in September 2006 (see Chapter 2), and the
first transplants were performed in 2007. The UKLKSS enables kidneys donated
from living donors to be shared across the UK to maximise the number of transplant
opportunities and include:
Paired/pooled donation
Altruistic donor chains
8.1 Paired/Pooled Living Donation
Paired/pooled donation (PPD) allows the exchange of kidneys between donor-
recipient pairs so that recipients who are Human Leucocyte Antigen (HLA) or ABO
blood group incompatible with their donors can receive a compatible transplant.
Compatible donor-recipient pairs may also enter the scheme to achieve a better
HLA- or age-matched transplant, or to optimise other relevant factors such as a
discrepancy in BMI. The entry of such donor-recipient pairs increases the transplant
opportunities for all recipients who are waiting within the UKLKSS. Exchanges are
identified between two (paired) or three (pooled) pairs (Figure 8.1).
The paired/pooled scheme requires careful co-ordination and administration to
ensure that the use of kidneys is optimised and maximum patient benefit is
achieved.
Registration in the Scheme
Only donor-recipient pairs who have been fully evaluated and are suitable to
proceed to donation/transplantation can be registered into the paired/pooled
scheme and entered into the quarterly living donor kidney matching runs (LDKMR).
Results of clinical investigations and up-to-date histocompatibility and

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
204
Figure 8.1 Exchange Options within the UKLKSS
immunogenetics (H&I) testing must be available before donor-recipient pairs are
confirmed for inclusion in each matching run. At a minimum, relevant clinical
investigations for registered donors and recipients must be repeated annually, or
more frequently as clinically indicated, if they remain unmatched in the scheme.
The deadline for registration of potential pairs with NHS Blood and Transplant
(NHSBT) is usually three weeks before the quarterly matching run with the
opportunity to suspend or activate pre-registered pairs (positively confirm inclusion)
up to seven days before the run. Deadline dates for registration and dates of LDKMR
are published in advance by NHSBT. Recipients must be registered with maximum
acceptable donor age and any specific HLA match requirements. However, these
limitations can reduce the chances of a match and must be discussed with the
recipient. Recipients can also be registered with ‘extended criteria’ for acceptable
HLA and ABO blood group mismatches to increase the options for transplantation
(e.g. a low risk ABOi transplant in preference to a higher risk HLAi transplant). Such
preferences must be agreed before registration and confirmed before inclusion in
each matching run to avoid exchanges not proceeding due recipient withdrawal after
the matching run.
Nominated contacts from the living donor co-ordinator team at each transplant
centre and/or referring hub are responsible for ensuring that all eligible pairs are
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
205
registered and that information is complete and up to date. Each H&I laboratory also
has nominated contacts for the schemes to co-ordinate scientific information for
donor-recipient pairs. Key responsibilities for the nominated living donor co-
ordinator contacts include:
Close collaboration with the H&I key contacts to ensure recipient HLA antibody
screening is up to date, unacceptable antigens are registered, and donor HLA
preferences are specified before confirmation of inclusion in each matching
run.
Close collaboration with clinical colleagues to ensure that donor and recipient
assessments are up to date and complete before confirmation of inclusion in
a matching run.
With the exception of multiple donors for one recipient, ensuring that donor-
recipient pairs are assessed by an Independent Assessor and approved by
the HTA before inclusion in the matching run.
Particular donor information that is relevant to the acceptance of a kidney by
a recipient centre must be cited with the registration according to the agreed
clinical criteria, which include complex vascular or non-vascular anatomy,
relevant medical history, and absolute GFR for all complex potential donors.
Contact with both donor and recipient individually to confirm their commitment
to enter/remain in the scheme and to ensure that no issues have emerged
since the last matching run that might preclude them. It is particularly important
that donor-recipient pairs understand the implications and expectations of
participation in the scheme and the impact of late withdrawal (after pairs have
been matched) on other pairs should they decide not to proceed. This should
not override their right to withdraw consent at any time, but must be discussed
in advance to minimise the risks.
Collation and confirmation of information to register and positively confirm
inclusion of relevant pairs in the scheme at the notified times.
Matching Runs and Scoring Systems
There are four matching per year, at quarterly intervals. Each matching run identifies
all potential matches within the pool according to a scoring system developed in
collaboration with experts in matching algorithms at the University of Glasgow.
Scoring is necessary to optimise the number of transplants overall and the best
transplant option for a single recipient from multiple possibilities. The number of
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
206
transplants and the scores of different possibilities are optimised over all options
involving both 2-way and 3-way exchanges and altruistic donor chains. Identification
of possible matches takes into account any donor age or HLA restrictions specified
at the time of registration. Typically there are approximately 250 pairs in any one
matching run and up to 70 transplants may be identified.
Scoring is based on the:
Calculated level of sensitisation (to promote matches for sensitised patients
where such are identified)
Waiting time in the scheme (after the first matching run)
HLA mismatch level of the potential transplant (to promote good matching
where possible)
Age difference between the two donors, which is a tie-breaker to optimise
outcome
The scheme continues to evolve. For example, a restriction on blood group O donor
kidneys only being allocated to blood group O recipients has been removed to
maximise transplant opportunities for highly-sensitised HLA recipients. Current
matching arrangements, statistics related to the scheme, and on-line resources to
support clinical decision-making can be found at www.odt.nhs.uk (1-3).
One week before each matching run, a ‘pre-run’ is performed to identify any potential
matches between complex donors (see above) and the recipients in the scheme.
Transplant teams are requested to review the potential matches for their patients
and discuss with them if they wish to be included with the potential donor in the final
matching run. This pre-run and the discussions with clinical teams and recipients
before the actual matching run is finalised are essential to minimise the number of
potential transplants that may not proceed.
When a matching run has taken place, NHSBT notifies the nominated scheme leads
with a report specifying all the donor-recipient pairs that have been successfully
matched. The nominated scheme leads in transplanting centres are responsible for:
Liaising with local referring units and donor-recipient pairs to inform them that
they are in a potential match, pending initial crossmatch between all pairs.
Recipients must be reminded that they are automatically suspended from the
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
207
national transplant list until confirmation of the initial crossmatch test. The
initial crossmatch must be arranged as soon as possible after the matching
run so that it is reported within a maximum of 14 days after the notification of
identified transplants. In the event of a positive crossmatch, the recipients from
the provisionally matched group are reinstated on the national transplant list
unless an alternative match within the same group can proceed. Transplant
centres are responsible for reinstating recipients on the national transplant list.
Liaising with local leads and living donor co-ordinators in the other
participating centres to arrange initial crossmatching, exchange of donor
information, scheduling of surgery, and pre-admission requirements, including
Independent Assessment and HTA approval if this has not been completed
prior to registration in the schemes (see Chapter 5). Transport arrangements
for essential samples and organs before and on the day of the transplant
should be co-ordinated via NHSBT transport or an equivalent courier service
to ensure ‘door to door’ collection and delivery.
Updating the LKD Schemes Co-ordinators within NHSBT of the progress of
the matched group, including the outcomes of crossmatch results, prompt
reporting of problems, e.g. non-proceeding transplants, delay to the scheduled
dates of surgery, and response to requests for further information (including
the investigation of incidents and action to prevent future risk or recurrence).
Liaising with the wider in-centre teams to facilitate arrangements for
admission, co-ordinating the start of simultaneous donor lists on the day of
surgery, and ensuring colleagues are updated and informed throughout the
process. Designated weeks of surgery are scheduled within 8 weeks of the
notification of the outcome of the matching scheme and dates are included in
the annual timetable distributed by NHSBT. All participating transplant centres
in the UK are requested to ‘ring-fence’ operating lists within the ‘sharing period’
to accommodate as many exchanges as possible. This is important to reduce
delay and to incentivise donor-recipient pairs and non-directed altruistic
donors (NDADs) to enter into the scheme.
Special considerations
The expectations of donor-recipient pairs entering the paired/pooled scheme must
be managed. The potential benefit from a compatible living donor transplant must
be balanced with realistic information about the likelihood of being matched, tailored
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
208
to their individual circumstances (e.g. degree of sensitisation, blood group
mismatch, etc.). In addition to the latest statistical information and decision-making
aids related to the scheme available at www.odt.nhs.uk, the NHSBT ‘Incompatible
Pairs’ calculator enables clinicians to assess the likelihood of a particular
incompatible donor-recipient being matched in the scheme (3).
Approximately 25% of identified transplants will not proceed due to reasons that
cannot be foreseen before the matching run, i.e. positive crossmatch or
clinical/social considerations for either the donor or recipient. The schemes are
formally monitored by the Directorate of Organ Donation and Transplantation (ODT)
within NHSBT to identify when transplants do not proceed due to modifiable reasons
and to make recommendations for remedial action to reduce the risk of recurrence.
Donors and recipients need to be aware of how the scheme works, the registration
requirements, and their responsibilities as participants within it. There are some key
considerations:
Before confirming inclusion in each matching run, donor-recipient pairs must
agree, if matched, to be available for crossmatch testing and to proceed to
surgery within the designated timeframes.
All incompatible donor-recipient pairs are entitled to know the treatment
choices that are available to them. Practices vary between centres but,
increasingly in HLA or high titre ABO blood group incompatible scenarios, up
to 3 or 4 matching runs (1 year) in the paired-pooled scheme are often
recommended before considering other interventions. An annual review of all
unmatched donor-recipient pairs in the scheme is recommended to ensure
that appropriate treatment options are reconsidered.
Multiple donors with different HLA types and blood groups can be assessed
and registered for a single recipient, to increase potential for matching.
Recipients can be registered with ‘extended criteria’ for both HLA and ABO
matching to facilitate a lower risk transplant (see above).
Compatible donor-recipient pairs are eligible for the scheme and benefit the
whole UKLKSS by increasing the donor-recipient pool. For individual
recipients, this is recommended if an improved age or HLA match might be
achieved (e.g. for children or young adults).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
209
Registration in the paired scheme does not preclude listing for a deceased
donor kidney.
Recipients considering antibody removal treatment must be suspended from
the paired scheme if such treatments are initiated using agents (e.g.
Rituximab
®
) that could influence the interpretation of a crossmatch with a
paired donor.
Donors from outside the UK for NHS recipients, non-UK donor-recipient (non-
NHS entitled) pairs, and privately funded pairs can be included in the UKLKSS
if they meet the requirements for registration and inclusion and the timeframes
involved to avoid impact on other pairs in the scheme. Such cases are
reviewed on an individual basis. In the case of private patients or non-NHS
entitled donor-recipient pairs, the terms of participation in the schemes must
be made explicit and it is recommended that they are referred and managed
in collaboration with a NHS multi-disciplinary transplant team that is familiar
with the schemes.
Donor-recipient pairs must be made aware of the implications of late
withdrawal on other matched pairs and encouraged to carefully consider this
before registration in the scheme and at the time of each subsequent matching
run.
Although simultaneous donor surgery is the default position for all matched
donor-recipient pairs, non-simultaneous surgery may be the preferred option
to overcome logistical complexities and to facilitate timely transplantation. If
this approach is adopted, although the risk of a recipient missing out on a
transplant opportunity is low, donor-recipient pairs must be consented to
ensure that they understand the possible risks involved.
If a paired/pooled recipient misses out on a transplant and his/her donor has
donated but all the exchanges cannot be completed, he/she can be prioritised
for transplantation from either a living or deceased donor, according to their
preference. Details are available from https://www.odt.nhs.uk/living-donation/
Transplants and Outcomes
It is usual for the retrieved kidneys to travel between donor and recipient hospitals,
but arrangements for donors and recipients to move can be made if all parties agree.
Usually, donor operations start simultaneously at the induction of general
anaesthesia for the donors, with contact either directly between the donor surgeons
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
210
or indirectly via the living donor co-ordinators to ensure that both operations proceed
and that the kidneys are dispatched to the recipient hospital at the expected time.
However, there is flexibility for centres to stagger the start time of donor surgery
within the same day or on adjacent days to accommodate matched transplants
within the scheduled sharing weeks (see also section 8.2).
To streamline the transplant process and minimise delay at implantation, the
retrieved kidney should be prepared in the retrieval centre so that it is ready for
implantation into the recipient on arrival. If a kidney cannot be transplanted into the
intended recipient on the day of surgery and the donor has consented to the option
of transplantation into an alternative recipient (see HTA consent, Chapter 2), the
kidney is re-offered to all UK centres via NHSBT according to the offering process
for a deceased donor kidney.
Five-year transplant survival rates (not censored for patient death) are comparable
for paired donation transplantation and other forms of living donor transplantation
(2).
Anonymity
The scheme relies upon anonymity between matched donor and recipient pairs to
avoid disclosure of identity before donation-transplantation (4). All members of the
transplant team need to be vigilant about the exchange of information and conscious
of the confidentiality issues involved to avoid inadvertent disclosure. This is
particularly challenging when two or more pairs are matched within the same centre
and consideration needs to be given to the admission arrangements, proximity of
operating theatres, and where donor-recipient pairs are cared for during their
inpatient stay. Anonymity can be broken with the consent of all parties, usually
initiated by the recipient, after the exchange transplant has been performed and it is
recommended that this is facilitated through the respective living donor co-
ordinators.
8.2 Altruistic Donation (Directed and Non-directed)
Increased public awareness since 2011 has led to more people volunteering to be
considered for altruistic kidney donation and this is a valuable means of expanding
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
211
the donor pool. Five year transplant survival rates (not censored for patient death)
are comparable for recipients of non-directed altruistic donor kidneys with other
forms of living donor transplantation
(2).
Terminology
The Human Tissue Authority (HTA) classifies the different types of altruistic living
organ donation according to whether the donation is made to a specific individual or
to a stranger (4).
Donation to a specific individual: Directed Altruistic Donation
The HTA defines two categories of directed altruistic donor (DAD)
1. Where there is no genetic relationship or established emotional relationship
between the donor and recipient (e.g. distant family member who has not
seen their potential recipient for many years; relative with whom there has
been no contact previously; friend of a friend)
2. Where there is no pre-existing relationship between the donor and recipient
before the identification of the recipient’s need for a transplant (i.e. contact
is made through a third party such as through social networking, media
campaign, Facebook, bespoke website, local newspaper)
This is a challenging and controversial area in living organ donation. To provide a
framework for an approach to the management of DAD referrals, the British
Transplantation Society (BTS) has published specific guidelines to support clinical
practice (5).
It is particularly important to manage the expectations of category 2 DAD donors
and their potential recipients so that both sides are clear about the likelihood of
finding a suitable donor through social media/media appeals. More guidance is
available at https://www.organdonation.nhs.uk//about-donation/living-donation/ and
https://www.nhsbt.nhs.uk/get-involved/promoting-donation-hub/download-digita
Donation to unspecified individuals: Non-Directed Altruistic Donation
Non-directed altruistic donors (NDAD) donate an organ to an individual who is
unknown to them. These donations account for approximately 10% of all living
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
212
kidney donations in the UK (1). Different names are used to describe this type of
donation within the transplant literature (e.g. altruistic, anonymous, non-directed,
“Good Samaritan”, unspecified). To remain consistent with the terminology used in
the Human Tissue Act 2004 and by the Human Tissue Authority (4), the term Non-
directed Altruistic Donation is used by the BTS and within these guidelines.
From January 2018, provided that there is no patient with higher priority on the
national transplant list to whom their kidney could be allocated, all NDADs donate
into the paired / pooled scheme to create altruistic donor chains (ADCs) of up to
three transplants. The NDAD is used to ‘prime’ a chain of transplants between two
or more donor-recipient pairs to maximise transplant opportunities within the
UKLKSS. The remaining organ from the paired donor at the end of the chain is
donated to the best-matched recipient on the national waiting list (see Figure 8.2).
Options to use the last paired donor as a ‘bridge donor’ to initiate an ADC in the next
LDKMR may be considered for the future.
Assessment of Directed Altruistic and Non-Directed Altruistic Donors
Directed altruistic donors (DADs) and Non-Directed altruistic donors (NDADs) must
complete the same living donor assessment as required for directed donors, with
the additional requirement of a formal mental health assessment (see Chapter 8,
Appendix 1).
Registration and Allocation
Most DADs donate directly to an identified, compatible recipient and will proceed as
per directed donations within a single centre or by agreement between two centres.
If a DAD is incompatible with their recipient, they may also enter the paired/pooled
scheme as donor-recipient pair, provided that they can meet the requirements of the
scheme and are aware of their roles and responsibilities within it (see section 8.1).
Once they have been fully evaluated and HTA approved, all NDADs are registered
with NHSBT. Registration is facilitated by the living donor co-ordinator in the
referring centre or in the transplant centre where the donor assessment and/or donor
surgery will be performed.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
213
Figure 8.2 Allocation Options for NDAD Kidneys
The allocation of NDAD kidneys, including altruistic donor chains identified in the
living donor kidney matching run and the possible default to a high priority patient
on the national transplant list, must be discussed with all NDADs at an early stage
of assessment so that the arrangements and timeframes for donation are clear.
If an altruistic donor chain falls through, the NDAD can choose to donate directly to
the waiting list to avoid further delay to their donation, or wait for the next quarterly
matching run (2).
Once a NDAD has been matched to a recipient (through a chain or directly via the
waiting list), the living donor co-ordinators in donor and recipient centres liaise to
arrange the initial crossmatching, exchange of donor information, scheduling of
surgery and pre-admission arrangements. The following principles of best practice
are established:
Specific donor information that is relevant to the acceptance of a kidney by a
recipient centre must be cited with the registration according to the agreed
clinical criteria, which include complex vascular or non-vascular anatomy,
relevant medical history and absolute GFR for all complex donors.
LDKT 2020 PAG, July 2017
KSS
pairs
The Game-changers?
Direct to Waiting List Short AD Chain (ADC) Long ADC
2007 2012 April 2015
AD
D1
R1
WL
AD
D1
R1
D2
R2
WL
AD
WL
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
214
Donors must be made aware that they cannot request specific dates for donor
surgery but that every effort will be made to accommodate their donation
within the shared weeks of surgery attached to each matching run. In
exceptional circumstances only, if a donor is unable to donate within the
shared weeks of surgery, this must be specified in the special considerations
at registration to allow other centres to accept/decline an offer for a potential
recipient.
For donations into the UKLKSS, the same principles that apply to the
paired/pooled scheme (detailed in section 8.1) are applicable to NDADs
entering into an altruistic donor chain.
Receiving an altruistic donor offer to a recipient on the national transplant list
After an offer of a kidney from a NDAD has been made for a recipient on the national
transplant list from NHSBT, the living donor co-ordinators are responsible for liaising
with appropriate colleagues to facilitate the transplant process according to local
arrangements.
Key considerations:
The timing of donor-recipient surgery is negotiated between the participating
centres, but consideration should be given to the preferences of the donor and
the expectations of both donor and recipient in scheduling a date.
Before accepting an offer in principle and before informing the potential
recipient, the following must be identified as a priority: recipient clinical issues;
suitability of offer for the intended recipient; and centre logistics. Once the
recipient has been informed about the offer, it can cause unnecessary distress
if it is not appropriate to proceed. The donor will also be subjected to delay if
the decision to accept is prolonged.
Initial crossmatching between donor and recipient should be facilitated so that
it is reported within fourteen days of the offer being made unless exceptional
circumstances apply.
Transport arrangements for essential samples (crossmatching) and organs on
the day of transplant should be co-ordinated via NHSBT transport or an
equivalent courier service to ensure door-to-door collection and delivery.
Costs are met by the recipient centre.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
215
If the donor and recipient are within the same centre, the recipient and donor
co-ordinators should liaise with the wider in-centre team regarding
arrangements for admission, in-patient stay, and surgery and ensuring
colleagues are informed about the anonymity requirements.
Specific Considerations in Directed and Non-directed Altruistic Donation
Psychosocial assessment
A formal mental health assessment by a mental health professional (psychiatrist or
psychologist) remains a mandatory stage in the work-up of both DADs and NDADs.
Research into non-directed altruistic donation has demonstrated that there is no
significant difference in psychosocial outcomes between those donating to a
stranger and those donating to someone that they know (6). The same study also
showed that a mental health history in NDADs does not prohibit donation, nor does
it increase the likelihood of adverse post-operative outcome.
There are currently no data regarding the sensitivity or specificity of mental health
assessments or whether they can be safely removed without an increase in pre- or
post-operative mental health problems within these donor subsets, yet there are still
large numbers of potential altruistic donors who are screened out for a variety of
psychosocial reasons (7). Given the positive psychosocial outcomes reported after
NDAD in the UK and the reliance on positive outcomes to further expand the
programme, it is prudent for formal mental health assessments to remain best
practice until further evidence is available. The UK and Ireland Group of Renal
Transplant Psychiatry has produced a Consensus Guidance Statement on the
Mental Health Assessment of Altruistic Donors as a framework for assessment
(Appendix 1, Chapter 8).
Age
An issue commonly discussed within the field of directed and non-directed altruistic
donation is that of age: particularly young adults aged between 18-25 years.
Separate from considerations about long-term health, the majority of concerns relate
to whether younger donors may be more likely to regret their decision. There is no
evidence to suggest that this is the case. A helpful discussion with younger donors
may include questions regarding why it is important to them that they donate now
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
216
and whether it is something that they would consider at a later point in their life. A
period of time to reflect on the decision may also be encouraged.
Donor motivation
Research into non-directed donation has dispelled many pre-existing concerns
regarding donor motivation. Donors have been found to be most commonly
motivated by a desire to help another individual, and that donation would make a
significant impact on someone in need with minimal inconvenience to themselves.
NDADs are most commonly made aware of altruistic donation through the media or
through researching other forms of donation. Religious motivations are relatively
uncommon (6).
Social support
One area in which conventional directed donors and DADs/NDADs appear to differ
is social support; the perception of being cared for and supported by those around
us. A number of studies have demonstrated that NDADs commonly do not
experience the same level of social support as conventional directed donors. The
loved ones of those choosing to donate altruistically are not always fully supportive
of the donation, principally due to a lack of understanding regarding the motivations
behind the donation and fears related to complications. Some donors may also
choose not to tell their loved ones about their decision to donate until quite late into
their work-up.
Anecdotally, a lack of social support has been shown to be a significant reason
behind altruistic donors withdrawing from the donation process. Therefore, the issue
should be raised with all directed altruistic and non-directed altruistic donors during
the early stages of their work-up and they should be encouraged to notify their loved
ones of their decision to become a donor. This is so that issues specific to social
support can be identified early and addressed as necessary.
Anonymity
Anonymity between NDADs and their recipient prior to surgery is required (4,8). All
members of the transplant team need to be vigilant about the exchange of
information and conscious of the confidentiality issues involved to avoid inadvertent
disclosure, particularly when a donor is matched to a recipient within the same
centre. Although this is not as logistically challenging as the paired/pooled situation,
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
217
similar consideration needs to be given to admission arrangements, the proximity of
operating theatres, and where the donor and recipient are cared for during their in-
patient stay.
After the transplant has been performed, anonymity can be broken with the consent
of both parties and it is recommended that this is facilitated through the respective
living donor co-ordinators.
Donor expectations
There are particular considerations about the lack of proximity between the donor
and recipient that are unique to NDADs. It is essential for the expectations of all
NDADs to be carefully explored during the assessment process, so that there are
realistic expectations about feedback and contact after transplantation. NDADs
should be prepared for how they would feel should they hear nothing from or about
their recipient, or should they find out that the transplant was unsuccessful. Their
expectations of the process should also be clearly elicited alongside the
psychological impact of unmet expectations.
NDADs differ considerably on how much contact they would like with the recipient
after donation. UK NDADs have found that 50% of donors received a card or letter
after donation and of those who didn’t, the majority “would have liked or maybe
would have liked” to receive one (87%). This implies that the majority of NDADs
would like to hear something from the recipient. A large number had found out
whether the donated kidney had worked, and only a minority regretted finding out
this information. Further contact was minimal with the majority of donor-recipient
pairs never meeting in person (6).
Donors with terminal illnesses
Enquiries have been made from individuals with terminal illnesses who wish to
donate a kidney before they die and a handful of transplants from such donors have
now taken place. It is important for each case to be considered on an individual
basis with regular involvement of the multidisciplinary team. In the absence of
additional physical risks (to either the donor or the recipient) or psychological
contraindications, there is no reason why donations from these individuals should
not take place (9). Transplant centres must accept that whilst these donors may be
passed as fit to donate, they are inherently different from other types of NDADs and
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
218
as a result may have additional healthcare needs which have implications on
resources, such as nursing and social care.
Logistical considerations
The NDAD scheme differs from the UKLKSS in that there is no specific requirement
for the recipient to be automatically suspended from the national transplant list when
an offer of a kidney has been made, or even when the initial crossmatch has been
performed. It is nearly always in the best interests of the recipient to receive a kidney
from a living donor and so consideration should be given to the relative risk of
removing the potential recipient from the national waiting list whilst finalising the
arrangements for transplantation against the possibility that the transplant will not
occur. There is also the potential for disruption to the donor if the recipient is offered
a kidney from an alternative donor during this period, as the option of proceeding
with a different recipient may be refused.
As a minimum standard, discussion must be initiated with the recipient about
suspension from the national list at the time of the offer, and again following the
outcome of initial crossmatching. The recipient transplant centre is then responsible
for notifying that decision to NHSBT.
If a kidney is offered to a recipient and the date of surgery is subsequently
postponed, a decision has to be made about re-offering the kidney, depending upon
the reason for the delay. Without betraying confidential information, this decision
should involve the donor as he or she may be willing to reschedule for the same
recipient if it is a problem that is likely to resolve. If it is a more permanent issue,
clinical or otherwise, it may be advisable to re-offer the kidney with the donor’s
agreement. If a kidney cannot be transplanted into the intended recipient on the day
of surgery, it is re-offered to all UK centres via NHSBT according to the offering
process for a deceased donor kidney.
To streamline the transplant process and minimise delay at implantation, the
retrieved kidney should be appropriately prepared in the retrieval centre so that it is
ready for implantation into the recipient on arrival.
Donor reimbursement for paired/pooled and altruistic donors
Special considerations for donors within these groups have been identified and are
addressed in Chapter 9.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
219
8.3 Antibody Incompatible Living Donor Transplantation
Antibody incompatible transplantation (AIT) accounted for 2.5% (n=27) of living
donor transplants in the UK in 2016-17 (1). The decline in activity in the past five
years may be due to the development of the UKLKSS and the improved transplant
opportunities through the schemes, as well as the better outcomes from HLA-
compatible transplants. The BTS has published specific guidelines on antibody
incompatible transplantation (10). These are also summarised in section 7.5.
Such transplantation falls into two categories: ABO incompatible transplantation
(ABOi), where transplantation occurs across an ABO blood group barrier (e.g. from
a blood group B donor to a blood group O recipient); and HLA-incompatible
transplantation (HLAi), where the recipient has antibodies against one or more
specific HLA antigens present in the donor resulting in a positive flow cytometric or
CDC crossmatch.
Compared with ‘compatible’ transplants, both categories of AIT carry increased risks
and it is important that the donor is aware of these and of the alternatives to AIT. In
general, ABOi carries a small (1-2%) additional risk of early accelerated antibody
mediated rejection but otherwise has short and long term results which are
comparable with compatible transplantation (11-13). However, HLAi carries an
increased risk of severe rejection, serious morbidity from infection due to increased
immunosuppression, and death (14-16). These risks should ideally be discussed
with the donor and recipient together, prior to transplantation. As a minimum, the
donor must be aware that the transplant is high risk and that the long term outcome
may be suboptimal.
Options for antibody incompatible living donor pairs are listed below:
i) Deceased donor transplantation - i.e. the recipient remains on the waiting
list and does not proceed with LDKT
ii) Entry of the pair into the UKLKSS
iii) Direct antibody incompatible transplantation
iv) Acceptance of a lower risk antibody incompatible transplant within the
UKLKSS (e.g. ABOI rather than HLAi)
Discussions around these options are complex and depend on a number of factors,
but pairs are in general encouraged to enter the UKLKSS in the first instance. The
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
220
‘Incompatible Pairs Living Donor Kidney Application’ available at www.odt.nhs.uk
(3) provides information on how long pairs can expect to wait for a transplant based
on the characteristics of the pair. It should be used to inform discussions with the
donor-recipient pair and to determine a strategy in which alternative approaches can
be considered over time.
Sources of Information
NHS Blood and Transplant www.odt.nhs.uk or www.organdonation.nhs.uk
Human Tissue Authority www.hta.gov.uk
British Transplantation Society, Standards & Guidelines
https://bts.org.uk/guidelines-standards/
References
1. Organ Donation and Transplantation annual activity report 2016/17.
https://www.odt.nhs.uk/statistics-and-reports/annual-activity-report/
2. https://www.odt.nhs.uk/living-donation/living-donor-kidney-transplantation/
3. Incompatible pairs living donor kidney application, 2015
https://www.odt.nhs.uk/living-donation/tools-and-resources/
4. Human Tissue Authority. Guidance to transplant teams and Independent
Assessors March 2015. https://www.hta.gov.uk/policies/guidance-transplant-
teams-and-independent-assessors
5. British Transplantation Society. Directed altruistic organ donation, June 2014.
https://bts.org.uk/wp-content/uploads/2016/09/16_BTS_Directed_Altruistic_2-
1.pdf
6. Maple H, Chilcot J, Burnapp L, et al. Motivations, outcomes and characteristics
of unspecified (non-directed altruistic) kidney donors in the United Kingdom.
Transplantation 2014; 98: 1182-9.
7. Nadkarni A, Schartau P, Burnapp L, et al. Assessing potential nondirected
altruistic kidney donors: a case note audit. Br J Renal Med 2012; 17: 19-23.
8. Human Tissue Authority, Code A: Guiding principles and the fundamental
principle of consent and Code F: donation of solid organs and tissues for
transplantation https://www.hta.gov.uk/hta-codes-practice-and-standards-0
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
221
9. Rakke YS, Zuidema WC, Hilhorst MT, et al. Seriously ill patients as living
unspecified kidney donors: rationale and justification. Transplantation 2015; 99:
232-5.
10. British Transplantation Society. Guidelines for antibody incompatible
Transplantation, 3
rd
Edition, 2015.
https://bts.org.uk/wp-content/uploads/2016/09/02_BTS_Antibody_Guidelines-
1.pdf
11. Opelz G, Morath C, Süsal C, Tran TH, Zeier M, Döhler B. Three-year outcomes
following 1420 ABO-incompatible living-donor kidney transplants performed
after ABO antibody reduction: results from 101 centers. Transplantation 2015;
99: 400-4.
12. Barnett AN, Manook M, Nagendran M, et al, Tailored desensitization strategies
in ABO blood group antibody incompatible renal transplantation. Transpl Int
2014; 27: 187-96.
13. Montgomery RA, Berger JC, Warren DS, James NT, Montgomery RA, Segev
DL. Outcomes of ABO-incompatible kidney transplantation in the United States.
Transplantation 2012; 93: 603-9.
14. Bentall A, Cornell LD, Gloor JM, et al. Five-year outcomes in living donor kidney
transplants with a positive crossmatch. Am J Transplant 2013; 13: 76-85.
15. Montgomery RA, Lonze BE, King KE, et al. Desensitization in HLA-incompatible
kidney recipients and survival. N Engl J Med 2011; 365: 318-26.
16. Couzi L, Manook M, Perera R, et al. Difference in outcomes after antibody-
mediated rejection between ABO-incompatible and positive cross-match
transplantations. Transpl Int 2015; 28: 1205-15.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
222
8.4 APPENDIX TO CHAPTER 8
MENTAL HEALTH ASSESSMENT OF ALTRUISTIC KIDNEY DONORS:
CONSENSUS GUIDANCE STATEMENT
BACKGROUND
Altruistic kidney donation (aka non-directed, anonymous, Good Samaritan,
unspecified), previously well-established elsewhere, first became legal in the UK in
2006.
The relevant regulatory body, the Human Tissue Authority (HTA) at first mandated
a psychiatric assessment of all potential donors before invasive investigation, but
said little about the purpose and nothing about the process of such assessment. It
also recommended that psychiatric assessments be made available to Independent
Assessors (IAs), who are individuals trained and appointed by them who undertake
final donor assessments before a date for surgery is set.
The HTA requirement for mandatory psychiatric assessment was withdrawn in 2012
on legal advice, but the BTS and NHS-BT do still recommend it, albeit without further
elaboration. (The HTA further recommend that the only information to go to the IA
is a referral letter from the transplant co-ordinator. It does not specifically exclude
the sending of other background information, including psychiatric assessment
where these have been undertaken, but it does not see a need for it).
After a slow initial take-up, altruistic donor numbers currently account for
approximately 10 % of all living donors.
Practice varies widely across the UK in regard to:
- The proportion of donors referred for mental health assessment
- The professional affiliation of the assessor
- The nature of the assessment
Anecdotally, up to 20-30% of potential donors are turned down on mental health
grounds. Some donors have reported the process of mental health assessment as
intrusive and unwelcome ("worse than the angiogram").
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
223
There is therefore a clear need to attempt standardisation of these assessments in
an effort to reduce unjustified variation in practice, improve acceptability to donors,
and justify decisions to decline donors, preferably on a growing evidence base.
In recognition of this need, a consensus guidance workshop was convened in
London in March 2015 by the UK and Ireland Transplant Psychiatry and Psychology
Group, an informal multidisciplinary network covering most of the mental health
professionals undertaking this work.
Draft guidance was developed and circulated before the workshop, and then used
as a basis for detailed discussion on the day, with follow-up comment by e-mail. This
document is the outcome of that process. It is the hope of the group that the
guidance it contains will be helpful to clinicians in the field and the relevant clinical
and regulatory bodies.
QUESTIONS
1. Which potential donors should be referred?
2. Who should undertake assessments?
3. At what stage of work-up?
4. With what information to hand?
5. What is the purpose of assessment?
6. How should it be undertaken?
7. To whom should the report be sent?
8. What are the follow-up requirements
- for those who go on to donate?
- for those who are declined on mental health grounds?
9. Should reports be collated centrally as a research resource?
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
224
1 Which potential donors should be referred?
The HTA's originally mandated requirement and the continuing recommendations
from NHSBT and BTS reflect concerns in the transplant community that a significant
proportion of potential donors might come forward as a result of mental disorder
which they were not well placed, as transplant clinicians, to identify or assess.
Accumulating clinical experience has reduced, but not abolished, this concern.
Given the high rates of psychopathology reported in altruistic donors and the
frequency of declining donation on mental health grounds, there are clear risks
which are best addressed by ensuring all altruistic donors undergo mental health
assessment.
Recommendation
There is clear, emphatic consensus among mental health clinicians
working in the field that ALL potential altruistic donors should be
referred for mental health assessment.
2 Who should undertake assessments?
Transplant centres' access to mental health specialists varies widely across the UK,
as it does in other countries. Some centres specifically fund or part-fund embedded
psychiatrists, psychologists or nurse specialists (though few will have direct access
to more than one such type of mental health clinician). Others have service level
agreements which establish routes of referral to specific individuals with dedicated
funding streams, while some still fall back to generic mental health services
allocated according to the patients’ address or GP. But however the mental health
services to individual transplant centres are aligned and funded, they need to work
in broadly the same way.
Any mental health clinician working in this field should be able to assess motivation,
capacity and mental disorder (including substance misuse and personality disorder),
though there are different emphases in training and clinical practice across the
disciplines. What is more important than the professional affiliation of the assessing
mental health clinician is their familiarity with transplantation procedures,
timescales, risks and outcomes. Competencies matter more than formal roles.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
225
Recommendations
Mental health assessments of potential altruistic donors can be
undertaken by any suitably qualified and sufficiently senior mental
health clinician (whether psychiatrist, psychologist, social worker,
counsellor or nurse specialist) who is sufficiently familiar with
transplant procedures, risk and outcomes, ideally because they are
embedded within or affiliated to transplant services.
Centres with access to more than one type of clinician can direct
referrals accordingly (for example preferring that potential donors with
a history of mental disorder treated by medication see a psychiatrist,
rather than psychologist, initially). Some cases may require
assessment by more than one professional.
3 At what stage of work-up?
Transplant units usually undertake initial donor screening via a transplant co-
ordinator, who provides information (verbal, written and via DVD) about the process
(including the risks), gathers a basic health history, takes baseline blood samples,
and makes contact with the GP to confirm the history. If this does not identify obvious
contraindications (and in a significant minority it will), patients are then usually seen
by a transplant physician and/or surgeon, who emphasises again the nature of the
risks involved. Referral for mental health assessment is usually undertaken at this
stage, and definitely before any invasive investigation (such as renal biopsy or
angiography), in order to ensure that potential donors who might be excluded on
mental health grounds are not exposed to undue risk.
Recommendation
Referral for mental health assessment of potential altruistic donors
should be made after initial screening, clinical assessment, and
provision of information by the transplant team, but before any
investigations which carry risk. However, to avoid delay in the
assessment process and in discussion with the donor, it may be
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
226
appropriate to perform mental health assessment in parallel with
physical assessment.
4. With what information to hand?
One risk of making mental health assessments mandatory is that referrals may be
perfunctory, when instead they should set out clearly any particular causes for
concern. These might, for example, arise from a potential donor’s age, a history of
contact with mental health services or treatment for mental disorder in primary care,
psychological symptoms evident at initial assessment, or doubts about the nature of
the motivation involved.
Transplant teams routinely request information from potential donors’ GPs which
may be relevant to donor’s suitability on medical and mental health grounds.
Information regarding the latter is clearly relevant to the mental health assessment
and normally passed on with the referral, but it is open to the mental health clinician
receiving the referral to request further background information from GPs and
mental health services (e.g. discharge summaries, outpatient letters) before and
after seeing the potential donor. Such requests are an integral part of mental health
assessment, and any reluctance by potential donors to grant them is relevant to their
suitability to proceed as donors.
Recommendation
Referral information should include, at a minimum, a clear description
of any specific mental health concerns or a statement that there are
none. Where concerns relate to past episodes of treatment, available
details obtained from the GP should be forwarded to the referee. Mental
health clinicians receiving referrals should be free to gather further
information directly if they judge it relevant, either on referral or after
interview. Potential donors should be advised by the referrer that this
gathering and sharing of information will happen (just as it would if
they had a cardiac history and were being referred for cardiology
assessment), and should be asked to agree to it.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
227
5. What is the purpose of assessment?
The HTA's (now withdrawn) mandatory requirement was vague about the purpose
of mental health assessment, and the NHSBT and BTS recommendations say little
more. Clinicians in the field identify several overlapping purposes, some specifically
psychiatric (i.e. related to the subset with mental disorder), others psychological
(applying to all donors). They include:
• To confirm the donor’s capacity (i.e. their ability to understand, remember and
weigh up the information presented to them, and to then make and convey
their decisions).
• To explore motivation. This is particularly important in cases of altruistic
donation. Where significant concerns about motivation emerge, they may
amount to reasons for exclusion from donation.
• To explore resilience and available practical and emotional support, including
the views of significant others.
• To explore expectations. This is mainly a role for transplant co-ordinators, but
drawing out the expectations of altruistic donors bring may help prevent and
manage “post-donation blues”.
• To identify those who bring additional risks of mental health complications
(e.g. relapse of a recurrent condition) during assessment and after surgery
and who therefore may require specific mental health treatment in the peri-
operative and post-operative period. In some cases, these potential risks may
be sufficient to contraindicate donation.
• To clarify the appropriate route by which to access specialist mental health
services for follow-up in the event of mental health problems arising after
donation (or exclusion from donation).
• To identify those whose wish to donate arises from mental disorder, and who
should therefore be excluded from donation. While few living related kidney
donors are excluded on mental health grounds, anecdotal evidence suggests
the proportion rises for altruistic non-directed donors, the main reasons being
personality disorder, substance misuse, and recurrent depression.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
228
It should be made explicit at the outset that mental health assessment of altruistic
donors is not intended to be therapeutic (although it may identify a need for
treatment), but is an integral part of the whole process of assessing altruistic donors.
Confirming capacity, clarifying support, and (less explicitly) exploring motivation are
also in part the remit of the HTA's IA assessment, though in that context the main
focus in assessing motivation is to consider any evidence of coercion, duress or
financial incentive.
Where a mental health assessment has covered these areas it is therefore important
the conclusions should be available to the IA.
Recommendation
The multiple potential purposes of mental health assessment listed
above should be acknowledged, together with their overlap with each
other and with the IA role. Referral should, where possible, clarify the
purpose(s) for which referral is made. Mental health clinicians should
clarify the specific purpose(s) they have addressed in their
assessment.
6. How should it be undertaken?
Different disciplines approach mental health assessment in different ways. None
should be expected to radically depart from their usual methods in this context, and
each is free to use whatever methods they judge appropriate to answer the
questions put to them in the referral.
Assessment will always involve a clinical interview with the potential donor. This may
be supplemented with standardised instruments (questionnaires, structured
interviews) as judged appropriate by the assessor. For example, a clear cut clinical
diagnosis of current depression may suffice for the purpose of the assessment, or
the assessor may judge it necessary to supplement this with the use of recognised
depression scales (HAD, BDI etc.).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
229
Assessment may necessitate interviews with informants such as partners or other
next of kin, according to the judgment of the assessor. Issues arising may require
repeat interviews with potential donors.
A referral suggesting the possibility of cognitive impairment (and thus possible
impaired capacity) will normally require a clinical interview, a standardised
assessment (e.g. ACE-III and/or other instruments), and a third party interview which
itself may need to be standardised.
Assessments will vary widely depending on the questions to be answered and their
underlying complexity. Some will be straightforward, requiring no standard scales or
third party interviews, and should be possible within the customary one-hour
interview. Others will be more complex and require multiple elements spread over
more than one appointment. It is unlikely any such assessment should take more
than three hours in total.
Recommendation
The nature of the assessment should be tailored to the referral
question, the clinical circumstances, and the professional background
of the assessor. Repeat interviews, third party interviews, standardised
questionnaires and structured assessments may all be necessary, but
the only element of assessment required in all cases is a clinical
interview
7. To whom should the assessment report be sent?
The report should obviously go the referrer and the GP, as well as to any mental
health services with which the donor has had, or may foreseeably require, contact.
Some renal services share all correspondence (including mental health referral
letters) with patients, including potential donors, but this is not standard practice in
all units. Mental health services also vary in the degree to which they routinely share
assessment letters with patients.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
230
The mental health assessment of a potential altruistic donor may draw upon
information which has not previously have been shared with the donor. The
conclusion of the report should not be automatically shared, even if this is usual
practice.
Given the identified overlap between some aspects of mental health assessment
and the IA assessment, reports should be forwarded to the IA with the HTA referral
when donor work-up reaches that point.
Recommendation
As a minimum, the assessment report should go to the referring
clinician in the transplant team, the GP, and any mental health services
with which the potential donor is in (or may foreseeably require) follow
up. Reports may also go directly to the patient, where this is consonant
with practice in local mental health and renal services. The report
should also be forwarded to the HTA-IA in due course. The patient
should be informed about, and consent to, this dissemination of
information.
8 What are the follow-up requirements for those who go on to donate,
and for those who are declined on mental health grounds?
Mental health assessment may identify vulnerabilities in potential donors which are
not so great as to prevent donation, but which bring identifiable risks such as a
relapse of depression in the event of medical complications.
Pre-donation assessment should seek to identify the appropriate routes to specialist
mental health services for such donors. In the short term, this might be a referral
back to the assessing mental health clinician in the transplant service; for problems
arising in longer term follow-up, this may mean a referral (back) to local generic
mental health teams. Altruistic donors will normally be followed up annually for life
by transplant clinics, sometimes at a distance from the patients' home. Clinicians
need signposting guidance if follow-up identifies emerging mental health problems.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
231
This issue is more acute for those turned down on mental health grounds, especially
as the decision to decline them may intensify distress and heighten risk. Where such
potential donors are in current follow-up with mental health services, those services
should be informed promptly (with copies to the GP) of the decision and the reasons
for it. Where they have been in recent follow-up, and may need to be seen again,
the assessor should also inform the mental health services (copied to the GP).
Where there is no current or recent mental health follow-up, the GP should be
informed promptly and advised of the potential need to refer the donor on. If the
clinical urgency is requires it, the assessing clinician may need to refer the donor
directly.
Recommendation
Assessing clinicians should identify routes to mental health follow-up
for those who may need it in the short- or long-term after donation. For
potential donors who are declined there should be direct liaison with
relevant mental health services and the GP.
9 Should reports (or data extracted from them) be collated routinely for
purposes of audit, clinical governance and research? If so, what
elements form the core data set?
There is a strong case for the central collation of data abstracted from mental health
reports, in order to better understand the issues raised and to relate outcomes to
factors identified at assessment. There is at present no obvious candidate body to
undertake such collation; however it is to be done, the task requires agreement on
a standard minimum data set, and there is nothing to prevent data being collected
locally under a standard national template. The first step is therefore to agree a core
data set which should quickly and easily codeable (5 minutes, no free text), and
ideally should take up no more than one A4 page.
(There is also a case for a central mechanism to identify donors who, after being
declined by one transplant centre on mental health or other grounds, approach other
centres. These two aims can probably not be met by the same central service,
especially as the first will require removal of patient-identifiable information while the
later relies on it).

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
232
Proposed Minimum Data Set
Assessor
Professional affiliation (social worker, psychiatrist, psychologist, nurse therapist,
counsellor, other)
Number of appointments
Total time taken
Method: clinical interview
Plus standardised instruments
Plus collateral informant interview
Demographics
Age
Gender
Postcode (for DepCat scores)
Employment status (f/t, p/t, u/e, retired, student, etc.)
Marital status / domestic circumstances
Any dependent children? Number, ages
Mental Health History
Treatment
G/P, O/P, I/P, detention
Current, recent, remote (?df),
Drugs, specific psychological Rx, supportive
Diagnosis
Current, Recent, Remote (?df),
ICD-11, DSM-V codes
Any history of self-harm or factitious disorder?
Current psychological symptoms
Evident, subclinical, absent
Mood, anxiety, psychotic
Cognitive impairment
Evident (ACE-III score), subclinical, absent

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
233
Capacity
Intact, impaired, borderline
Alcohol and substance (mis)use
Substance (s)
Dependent, harmful, hazardous, non-problematic
Current, recent, remote
Significant family psychiatric history
Forensic history
Current/previous probation or prison
Pending proceedings
Motivation
General altruism
Consistent with other behaviour (blood & bone marrow donor, charity, community,
volunteering etc.)
Inconsistent
Specific trigger
Bereavement
Other
Attitude of family
Supportive, opposed, indifferent, unaware
Decision
No specific mental health concerns
Donation contraindicated on mental health grounds
Donation not contraindicated but additional measures required
Donation deferred pending mental health intervention

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
234
Mental Health Follow-up
Already in place with relevant service
New need identified and acted on
With assessor
Not specifically required but routes of referral identified
Outcome
Donation declined on mental health grounds
Donation declined on other grounds
Donor withdrew
Donation pending
Donation progressed
- post-donation MH problems: Y/N/unknown
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
235
9 LOGISTICAL CONSIDERATIONS
Recommendations
Wherever possible, the aim is to ensure that the financial impact on the
living donor is cost neutral by the reimbursement of legitimate
expenses incurred as a direct result of the preparation for and/or act of
donation. There are clear policies across the four UK countries to
ensure that claims are settled in full and in a timely manner (B1)
Donors who are non-UK residents present unique logistical
challenges. To ensure that the process is clinically effective and to
comply with Visa and Immigration requirements, there is an agreed
entry visa application process and maximum duration of stay in the UK
(six months) for the donor. Visa extensions will only be considered in
exceptional or unforeseen circumstances. (B1)
9.1 Reimbursement of Living Donor Expenses
The reimbursement of legitimate expenses to a living donor, including loss of
earnings that are directly attributable to the organ donation, is supported by the
Health Departments in all four UK countries and forms part of national
commissioning arrangements. NHS England has combined its separate kidney and
liver policies to provide a single pathway. The policy has been developed in
conjunction with both clinicians and commissioners, is compatible with the policies
in each of the other UK countries, and sets out the framework and responsibilities
of those involved in achieving a successful claim (1). Reimbursement does not
contravene the current UK legislation under the Human Tissue Act 2004, which
forbids payment for supplying a human organ, provided that the donor does not gain
any financial advantage as a result (see section 3.8).
The policy is underpinned by some key principles:
Individual claims must be settled within a specified timeframe to prevent
unnecessary financial hardship to the donor as a consequence of the
donation
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
236
Claims are settled by the recipient Commissioning Authority on a case-by-
case basis according to agreed criteria
Early identification of potential claims is essential during the donor
assessment period to facilitate timely settlement
Whenever possible, claims should be submitted before the date of donation,
but claims can be considered retrospectively if there are genuine reasons
why they have not been notified previously
Donor expectations must be appropriately managed about the nature and
size of claims that will be approved
Donors must be provided with appropriate and specific information about the
criteria for application at an early stage of the assessment process, in
particular the need for supporting evidence, the approval processes, and the
timeframes
Alternative sources of reimbursement, e.g. statutory sick pay, must be
declared when a donor applies for reimbursement
9.1.1 Reimbursement of Expenses within the UK Living Kidney Sharing
Schemes and for Non-directed altruistic kidney donors
In cases of paired/pooled donation and non-directed altruistic donation, living donor
kidneys are exchanged across the UK between different transplant centres and may
cross country borders with different mechanisms of donor reimbursement. Once
exchanges have been identified and dates of surgery are scheduled, there is limited
time to obtain prior approval for donor reimbursement from the recipient’s
commissioners.
In cases of paired/pooled donation, an application to the local recipient
Commissioners should be made by the donor at the time of registration into the
scheme (as for a direct living donation). This facilitates prior approval of anticipated
expenses and timely reimbursement when the transplant proceeds. Reciprocity
between each donor/recipient pair involved in an exchange means that the costs to
the local commissioners are equitable.
In cases of non-directed altruistic donation, there is no direct reciprocity between
the donor and recipient transplant centres unless the kidney is allocated by chance
to a local recipient through the national allocation schemes. However, any recipient
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
237
in the UK may be a potential beneficiary of such a kidney and so the accepted
mechanism for donor reimbursement is by application to the recipient’s
commissioners. If a non-directed donor donates into an altruistic donor chain,
expenses should be reimbursed by the commissioners for the recipient on the
national transplant list, i.e. at the end of the chain. This leaves the local
arrangements for the paired donors and recipients in the middle of the chain
unaffected (see above).
9.2 Donors who are Non-UK Residents
Donors who are non-UK residents present logistical challenges. Policies have been
jointly developed to facilitate the entry of genuine donors into the UK for the
purposes of donation to either an NHS entitled recipient or to a private patient. The
current immigration rules provide a clear process for consideration of Entry Visa
applications and define the supporting information that is required to support the
donor application, including a letter from the recipient’s transplant centre/referring
nephrology unit, using an agreed template (see Appendix to Chapter 9) to clinically
endorse the application (2). Using a template letter ensures that the application is
recognised by Visa and Immigration personnel in individual posts (embassies) and
processed correctly. Posts in individual countries are responsible for approving and
issuing Entry Visa applications. Appeals on compassionate grounds may be
considered on a case-by-case basis if supporting evidence is available. Please
contact NHSBT for further advice. Non directed altruistic donors and directed
altruistic donors that fall into category 2 within the HTA’s revised legal framework
(i.e. where donor and recipient have no pre-existing relationship, having met only
for the purposes of living donor transplantation) are not considered for donation in
the UK or eligible to apply for a UK Entry Visa (3).
Potential non-resident donors must be provided with clear and comprehensive
information about their rights and entitlements whilst in the UK for the purposes of
organ donation. Before coming to the UK, prospective donors must be provided with
a letter which explains that the costs associated with treatment to donate a kidney
will be covered by the NHS, including those costs related to immediate post-
operative complications (see Appendix 9). However, it must be made clear that any
medical or dental treatment outside of the donor process (such as the detection of
previously unsuspected malignancy) would not be covered by the NHS and that any
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
238
treatment would require payment in person or through medical insurance, or that
the donor would need to return to his/her country of residence for treatment.
Successful applicants will be issued with a six-month visa under the visitor rules,
during which time they must be assessed and prepared for donation, undergo donor
nephrectomy and return to their country of origin following initial post-operative
recovery. It is the responsibility of clinical teams to ensure that, pending unforeseen
circumstances, donors comply with the terms of the Entry Visa and that extensions
to stay in the UK are only applied for in exceptional circumstances.
The Council of Europe (CoE) identified some core principles to underpin the
evaluation and protection of non-resident donors, including national oversight, a
regulatory framework and clear clinical and organisational pathways (4,5). These
same principles are also relevant to donor-recipient pairs who wish to travel to the
UK for the purposes of LDKT and are managed within the private sector. Tables
9.2.1 and 9.2.2 summarise the information requirements and a best practice model
for clinicians working with donors who are non-resident in the UK and wish to donate
to a NHS entitled recipient in the UK.
Potential recipients are discouraged from travelling outside the UK to receive a
transplant. As the national focal point for transplant-related crimes, NHSBT is
responsible for collecting registry data for all LDKTs that take place outside the UK.
Transplant centres are required to submit annual data to NHSBT so that this activity
is monitored and accurately captured within the UK Registry.
9.3 Prisoners as Living Donors
In response to a small number of offers from prisoners to donate an organ
altruistically, the British Transplantation Society (BTS) has collaborated with the
relevant agencies to produce guidance for clinicians who receive requests to
consider offers of living organ donation from this source, for both family members
and unknown recipients. The guidance provides a framework for management of
such referrals, with particular emphasis on the logistical aspects that need to be
addressed along the clinical pathway (6).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
239
Useful website sources of information:
NHS Blood and Transplant www.odt.nhs.uk; www.organdonation.nhsbt.nhs.uk
Visas and Immigration www.gov.uk/apply-uk-visa
Human Tissue Authority www.hta.gov.uk
References
1. NHS England, Policy for reimbursement of living organ donors, August 2017.
https://www.england.nhs.uk/publication/commissioning-policy-reimbursement-
of-expenses-for-living-donors/
2. Visas and immigration, routes for living organ donors. November 2014.
https://www.gov.uk/search?q=living+organ+donors
3. UK guidelines for directed altruistic donation. British Transplantation Society,
2014. https://bts.org.uk/wp-
content/uploads/2016/09/16_BTS_Directed_Altruistic_2-1.pdf
4. Council of Europe, Guide to the Quality and Safety of Organs for
Transplantation, 6
th
Edition https://www.edqm.eu/en/organ-tissues-cells-
transplantation-guides-1607.html
5. Council of Europe, Resolution CM/Res (2017)1. On principles for the selection,
evaluation, donation and follow-up of the non-resident living organ donors.
https://www.edqm.eu/sites/default/files/cmres_2017_1-
on_principles_for_selection_eval_donation_and_follow_up_of_nrld.pdf
6. UK Guidelines for living organ donation from prisoners. British Transplantation
Society, 2014. https://bts.org.uk/wp-
content/uploads/2016/09/04_BTS_Donation_Prisoners-1.pdf

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
240
Table 9.2.1
Information Requirements for Assessment of Non-UK Living Donors Before
Travel to the UK
Information
Minimum requirement
Desirable
1. Personal details
Name
Date of birth
Address
Nationality
Occupation
Email address
Telephone number
Passport number
and country of
issuance
2. Relationship to
recipient
Description of
relationship
Documentary
evidence
Letter from elder/post
3. Medical History
Medical and surgical
history
Including yes/ no for
diabetes, hypertension,
kidney disease
Medication history
Documentation by a
medical professional
Full family history
4. Physical status
Weight
Height
Blood pressure
Full physical
examination by local
doctor
5. Investigations
Urine dip
Creatinine
FBC
Fasting blood glucose
HIV, Hep B and Hep C
U&E, LFT, Bone
PCR or ACR
Haemoglobin electro
MSU
6. H&I
Blood group
Virtual or wet
crossmatch

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
241
Table 9.2.2
Summary Flowchart for Assessment of Non-UK resident Living Donors for
NHS Entitled Recipients
Action
Responsible
Person/s
1. Recipient contacts living donor co-ordinator (LDC)
with potential non-UK resident donor
Recipient
2. Recipient provided with medical questionnaire
letter/proforma, blood pack for virtual cross match
and information pack with link to relevant web
sites e.g. NHSBT, HTA, Visas and Immigration
LDC
3. Donor investigations and medical review
arranged in own country. Copies of results and
completed donor medical questionnaire returned
back to LDC
Donor
4. Donor blood drawn for virtual cross match and
either sent by courier or returned with potential
recipient
Donor +/- recipient
5. Medical questionnaire, blood results and virtual
cross match reviewed in transplant
centre/referring unit and decision made whether
donor appears to be suitable
Multi-disciplinary
team (MDT)
6. Donor contacted directly (or through recipient if
not able to contact directly) to relay results and
suitability after MDT discussion
LDC
7. Supporting letter for donor Entry Visa application
(if required) provided by transplant/medical team
using agreed template (see Appendix 9.4)
LDC/donor clinician
8. Donor Entry Visa attained and LDC informed
about estimated date of arrival in the UK
Donor +/- recipient
9. Donor registered in transplant centre/referring unit
and investigations arranged to start as soon as
possible after donor arrives in UK
LDC

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
242
10. On arrival, donor passport, Entry Visa and
incoming airline ticket are copied and retained in
the donor record for monitoring purposes (e.g.
Home Office tracking)
LDC
11. Donor assessed medically and surgically, as per
usual protocol. If suitable, independent
assessment and donation date arranged
MDT and HTA
Independent
Assessor (IA)
12. Donor progresses to donation. Donor is offered
immediate follow-up in the transplant centre.
MDT
13. When recovered and before expiry of Entry Visa,
the donor is discharged back to country of origin
with written information about recommended life-
long follow-up. Donor should be given contact
details in the UK +/- country of origin, in case of
medical issues when he/she returns home
MDT
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
243
9.4 APPENDIX TO CHAPTER 9
Template Letter for Potential Overseas Donors to Support Entry Visa
Applications to the UK
Trust headed paper
[include contact details for living donor coordinator]
[Name and address (in country of residence) for non-resident potential donor]
Hospital No/ID
NHS No
Date of Birth
Dear [Donor’s name]
RE: PROPOSED LIVING KIDNEY DONATION FOR
UK RECIPIENT: (NAME, HOSPITAL ID, DOB, ADDRESS IN UK)
I am writing to you because you have volunteered to be assessed as a living kidney
donor for your [relationship donor to recipient].
Thank you for the medical information that you have provided. To make sure that you
can safely donate a kidney and understand everything that you need to know about it,
you will need to complete your assessment in the United Kingdom (UK). We are
pleased to accept you for further donor assessment at [’X’] Hospital, [Name of
City/Town/UK].
We have planned appointments for you starting from [Day, Date]. You now need
to apply for a UK Entry Visa to start as close to this date as possible. Please do not
book your travel arrangements until your visa has been issued. This letter tells
you what to do to apply for your visa and to arrange your travel to the UK. Please read
it carefully before you make your plans.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
244
Next Steps:
1. Your application to travel to the UK
To travel to the UK to be a kidney donor, you can apply for a Standard Visitor Visa and
stay for up to 6 months. You need to comply with UK immigration requirements and
apply to your local British Diplomatic Mission, stating that you plan to donate an organ
to your relative. Your relative, the potential recipient of your kidney, must be a
resident in the UK and entitled to kidney transplant treatment on the National
Health Service (NHS). He/she must check this with the hospital in the UK before you
submit an application, otherwise it will not be valid.
You will find all the information you need to apply for your visa on the UK Visas and
Immigration website at: https://www.gov.uk/standard-visitor-visa or at your local British
Diplomatic Mission. To make sure that your application can be processed quickly
and has the best chance of success, you must make sure that you include all
the information that is requested – your visa will be refused if there is missing
information.
You need to apply for your visa a minimum of 4 weeks (maximum 12 weeks) before
you plan to travel to the UK. Your visa is only valid for 6 months from the date it is
issued. To make the most of your time in the UK, please contact us to discuss
the best date to attend the hospital before you apply for your visa. This date
must be included on the visa application form.
2. Your medical testing and donation in the UK
To complete the kidney donation process within your 6-month visa, your medical
assessment, operation and recovery in the UK must be planned ahead. Once your
assessment is complete, we will confirm if you are able to donate and check that you
still wish to go ahead. You will need to recover in the UK after donation for up to 4
weeks before you travel back to your own country.
You must arrange to stay with your family in the UK throughout your stay or find
suitable accommodation before you arrive (you will have to provide evidence of this in
your visa application to travel to the UK). When you are sent home from hospital, it is
important that you live with someone who can support you whilst you recover from
your operation.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
245
3. Your checklist
To help us plan everything as smoothly as possible for you, you can help us by:
1. Making sure that you have discussed with the hospital when you wish to travel to
the UK before submitting your application. This is very important – if you do not
check with the hospital first, you will not have enough time in the UK to complete the
assessment, donate a kidney and recover from the operation before you need to travel
home again. Your visit to the UK will be wasted.
2. Following the guidance on the https://www.gov.uk/standard-visitor-visa website
when applying for your visa so that you include all the information that is requested
before you submit your application. Incomplete information is the most common
reason for visas to be refused.
3. Attaching this letter to your visa application and submitting it with all your other
supporting information to your local British Diplomatic Mission, where an Entry
Clearance Officer will deal with it. If your application is approved, it will start on the
date that you requested in your application, as agreed with the hospital in the UK.
Please keep a copy of all these documents - you will need them when you travel to the
UK.
4. It is your responsibility to let us know if there is any delay in submitting your
visa application or in approving it so that we know when to expect you to arrive.
Contact details are at the top of this letter.
Costs
It is important that you know which costs and expenses are covered during your visit.
The costs of your medical treatment to donate a kidney (donor assessment, donor
operation and out-patient appointments) are covered by the NHS whilst you are in the
UK. Once you return home at the end of the 6-month period, you are not entitled to
NHS care in your own country.
Whilst you are in the UK, any medical or dental treatment outside of the donor process,
is not covered by the NHS and, if you do not have medical insurance, you would be
expected to pay for this yourself or return to [Country of residence for donor] for
treatment. You are, therefore, advised to obtain medical insurance before you travel.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
246
You can apply for reimbursement of expenses (e.g. travel) due to the donation process
from the NHS. You will need to keep a record and receipts of expenses. We can give
you the information that you need to make a claim once you arrive in the UK.
Please ensure that you and your family have read this letter and understand all the
information before applying for a visa. I will be coordinating your donor assessment at
the hospital. Please contact me directly or through your recipient if you have any
questions.
Yours sincerely
Living Donor Coordinator/member of Transplant/Referring team
cc: [potential recipient]
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
247
10 DONOR FOLLOW-UP AND LONG-TERM OUTCOME
Recommendations
Counselling and consent of potential living kidney donors must include
acknowledgement that the baseline risk of ESRD is increased by
donation (see also section 5.5). (A1)
Discussion with potential donors must be informed by those factors
known to increase ESRD risk post-donation, including donor age, sex,
race, BMI, and a family history of renal disease (see also sections 5.6-
5.9). (A1)
Risk calculators predicting lifetime ESRD risk may help inform the
consent process. (C2)
The risk of ESRD in living donors mandates lifelong follow-up after
donor nephrectomy. For donors who are resident in the UK, this can
be offered locally or at the transplant centre according to the wishes of
the donor, but such arrangements must secure the collection of data
for submission to the UK Living Donor Registry. (B1)
Donors who are non UK residents and travel to the UK to donate
(privately or to a NHS entitled recipient) are not entitled to NHS follow-
up but must be given advice about appropriate follow-up before
returning to their country of origin. (C1)
Potential donors who are unable to proceed to donation must be
appropriately followed up and referred for further investigation and
management as required. (B1)
Women must be informed of a greater risk of pregnancy-induced
hypertension following kidney donation. (A1)
Close monitoring of blood pressure, creatinine and foetal well-being is
advisable in kidneys donors during pregnancy. (C1)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
248
Kidney donors may be offered Aspirin 75 mg daily for pre-eclampsia
prophylaxis. (D2)
There is no evidence to support the benefits of right or left
nephrectomy to prevent pregnancy induced hydronephrosis. (Not
graded)
Births after kidney donation should be reported to the Living Donor
Registry as ‘a significant medical event’ at each annual review. (Not
graded)
10:1 Long Term Outcome Following Living Kidney Donation
The continued success of living donation depends upon ensuring the safety and
excellent long-term outcomes of the donor. In particular, donors must be reassured
that the risk both of developing progressive CKD and of premature cardiovascular
death remain low following nephrectomy. Studies in Sweden (1,2) and the USA (3-
5) have demonstrated that longevity remains greater and the risk of developing
ESRD remains lower in cohorts of donors when compared to the general population.
Although favourable outcomes in donors when compared to the general population
provide reassurance, such studies are not able to determine whether donor
nephrectomy increases the risk of adverse outcomes when compared to pre-
donation risk. To do so would require a control group of those assessed as able to
donate, but who did not – a group that is not readily available. Two recent studies
(6,7) have compared donors to ‘healthy non-donor’ controls in an attempt to address
this question.
Muzaale et al reported the long-term follow-up of 96,217 donors who had donated
a kidney in the USA between 1994 and 2011, and compared outcomes to a control
group of 20,024 participants in the NHANES III study (6). Median follow-up was 7.6
years for donors and 15 years for matched healthy non-donors. ESRD developed in
99 kidney donors at a mean of 8.6 years after donation, compared to 36 non-donors.
The estimated risk of developing ESRD at 15 years post-donation was 30.8 per
10,000 for donors and 3.9 per 10,000 in the control group (p<0.001). The risk was
higher in black compared to non-black donors (74.7 vs 22.7, p<0.001). The lifetime
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
249
risk of ESRD was estimated as 14 in 10,000 non-donors, 90 in 10,000 donors, and
326 in 10,000 of the US general population. The same authors previously reported
that the risk of long-term mortality was not increased in donors compared to controls
(5)
Subsequent analyses of up to 133,824 US living kidney donors between 1987 and
2015 identified male sex (hazard ratio (HR) 1.88), black race (HR 2.96), first-degree
biologic relationship to the recipient (HR 1.70), BMI (HR 1.61 for each 5 kg/m
2
) and
age (HR 1.4 for each 10 years in non-black donors) as risk factors for ESRD in the
donor population (8). ESRD in the first 10 years post-donation (10 in 10,000 donors)
was predominantly caused by glomerulonephritis; whilst by 25 years post-donation
ESRD (85 in 10,000 donors) was predominantly attributed to diabetes and
hypertension (9).
Mjoen et al reported long-term renal function, and both cardiovascular and all-cause
mortality, in 1901 donors who had donated in Norway between 1963 and 2007 and
compared the outcomes to 32,621 non-donors who could have been considered for
donation over the same period (7). The median follow-up was 15.1 years for donors
and 24.9 years for non-donors. The hazard ratio for all-cause death was 1.3 for
donors when compared to controls, 1.4 for cardiovascular death, and 11.38 for
ESRD. Importantly, the substantial HR for ESRD reflected only 9 cases of ESRD
developing at a median of 18.7 years post-donation, with immunologic renal disease
accounting for 7 of these cases.
Methodological concerns have been raised regarding both studies. In the US report
(6), 9,364 of the 20,024 NHANES III participants were considered as potential
donors. Each of these 9,364 controls was matched to multiple donors. Thus, if ESRD
were by chance under-represented in the much smaller control group then the risk
of ESRD in the donors would be falsely amplified. In this context, it is of note that
none of the white control group developed ESRD. In the Norwegian study (7), the
control group was drawn from the HUNT1 study that included subjects from a single
county (Nord Trondelag), which is a largely rural area with several small towns. The
control group was younger than the donors and less likely to smoke. Perhaps most
importantly, 80% of the Norwegian donors were first-degree relatives of their
recipient, and all cases of ESRD were in this group. Similarly, 84% of ESRD cases
in US donors occurred in the 67.6% of donors biologically related to their recipient.
In contrast, the majority of the controls were unlikely to have had a family history of
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
250
renal disease. Accordingly it is possible that the background risk of ESRD in the
control groups underestimates the pre-donation risk of ESRD in donors.
Notwithstanding these concerns, the US and Norwegian studies are important. Both
provide comprehensive data on large cohorts of living kidney donors with long-term
follow-up, and for the first time provide accurate predictions of the risk of ESRD
following donation. Both are reassuring, indicating that the lifetime risk of ESRD after
kidney donation is low, occurring in less than 1:200 donors (0.5%). However, it
appears clear that, for an individual at low baseline risk, donating a kidney does
increase the risk of later developing ESRD. This risk remains substantially less than
that in the general (unscreened) population. By contrast, it is not clear that kidney
donation has a detrimental effect on long-term cardiovascular or all-cause mortality,
with conflicting results from the US (5) and Norwegian (7) studies.
Both studies identify that the increase in ESRD risk in donors is largely due to
genetic and immunologic factors. The most potent risk factor for ESRD is black race,
identified both in the US study and in previous reports from the USA (6,10). The
estimated ESRD risk at 15 years post-donation was 74.7 and 22.7 per 10,000 in
black and white donors respectively (6). It is not clear if the excess risk in black
donors is related to the future development of hypertension, socio-economic factors,
or to a genetic predisposition to ESRD, possibly including at-risk APOL1
polymorphisms (11). At present there is no evidence to support APOL1 genetic
testing, but black donors must be counselled with due regard to the increased risk
of developing ESRD. This is especially important for young black donors, in whom
the cumulative risk of ESRD is greatest.
Donor age is also an important consideration. The risk of ESRD is less in young
when compared to older donors when followed for a fixed period of time. In the US
study the 15 year ESRD risk was 29.4 per 10,000 donors aged 18-39, 17.4 for those
aged 40-49, 54.6 for ages 50-59 and 70.2 for those aged >60, with statistical
significance when those aged <50 are compared to those aged >50 (6). However,
the cumulative time post-donation is necessarily longer in young donors. For
example a 20-year-old donor may have 60 years to accumulate the complications
of donor nephrectomy, whereas a 60-year-old donor only 20 years. Thus the lifetime
risk of ESRD is greater in young donors. This is particularly important since immune-
mediated renal disease (the commonest cause of ESRD in donors) has a peak
incidence in middle age. Young donors must be counselled accordingly.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
251
Risk calculators provide a means of estimating ESRD risk both at baseline (12) and
post-donation (8). It is not clear that such calculators can be applied to the UK
population, but they may be useful in illustrating risk to potential donors.
In summary, living kidney donation remains a safe and acceptable surgical
procedure. Recent studies have provided evidence to estimate ESRD risk in donors,
demonstrated a numerically small increase in ESRD risk, and identified those
groups at particular risk (black donors, young donors, donors genetically related to
patients with ESRD, donors with increased BMI). Importantly, the absolute risk of
ESRD in donors remains low when compared to the general population. This data
must inform donor assessment and consent, and emphasises the importance of
long-term donor follow-up.
10.2 Arrangements for Follow-up
Early follow-up of the donor is recommended, within the first few weeks after
surgery, to ensure that he or she is supported and is making appropriate progress
following the operation. This includes the monitoring of kidney function and the early
detection of problems such as infection and poor wound healing.
All centres have arrangements in place for immediate and life-long follow-up of living
donors. The minimum standard includes a follow-up appointment within four to six
weeks after donation at the transplant centre and an annual review thereafter, either
at the transplant centre, the referring nephrology unit or in primary care. Additional
reviews are arranged if clinically indicated. Within a maximum of twelve weeks, it is
anticipated that the donor will have made a full recovery and returned to normal
activities.
A survey of UK transplant centres in 2016 (13) demonstrated wide variations in
regional practice with 56% of transplant centres performing life-long donor follow-up
in 80-100% of previous donors ‘in-centre’ with face-to-face appointments. Living
donor co-ordinators perform 80% of life-long follow-up with nephrologists or
surgeons performing the remaining 20%. A minority of transplant centres and
referring units refer donors back to primary care for annual review and the majority
of these only do so after the first anniversary (or subsequent anniversary)
appointments. Telephone or virtual clinics are rarely used. Most non-UK resident
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
252
donors are lost to follow-up unless individual arrangements are put in place once
they have returned to their countries of origin.
Long-term annual follow-up provides an opportunity for specific clinical review as
well as a general health and wellbeing check, including psychosocial aspects (see
Figure 10.1). The European Organ Donation Directive (EUODD) specifies the
requirement for life-long donor follow-up data to be collected on all living organ
donors (14) and this principle is embedded in the UK Living Donor Registry
administered by NHSBT (2). While not all donors wish to return for regular review,
many welcome the continuing support and interest in their welfare.
There are some logistical challenges in achieving life-long follow-up for all donors,
particularly for non-UK residents and/or those who are not NHS entitled. This is
especially the case in countries where living donor transplantation is not an
established practice or where individuals pay for healthcare. These donors must be
provided with written advice about appropriate annual monitoring. Depending upon
the country, it may be possible to put the donor in contact with a local hospital or
nephrology/transplant service to facilitate annual review.
In the event of an unsuccessful transplant, it is particularly important to provide
adequate emotional as well as physical support for the donor, including access to
counselling facilities and psychological support.
Latest statistics show variation in the quantity and completeness of donor follow-up
data contributed to the UK Registry data between transplant centres (16). Figure
10.2 provides a template toolkit, which has been developed by the Living Donor
Kidney Transplantation 2020 (LDKT 2020) Strategy Implementation Group as a
flexible resource for clinical teams to plan and improve the consistency of life-long
follow-up. A donor reported outcome measures (DROM) survey is under
development and will be available in 2018.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
253
Figure 10.1 Pathway for Follow Up After Living Donor Nephrectomy
Referral to donor follow-up
clinic for lifelong annual review
Re-appointment in surgical or
medical review clinic
Life-long donor follow-up
Rationale: To provide continuing support to the donor & inform
the UK Living Donor Registry
Annual review subject to review according to clinical need
Performed at local transplant/referring centre or GP
Relevant research/audit data collated & data returned to UK
Transplant Living Donor Registry by LD co-ordinator
Annual review to include assessment of:
General health & lifestyle
Wound +/- complications
Medication
Renal profile
Full blood count
Dipstick urinalysis +/- mid-stream urine +/- albumin/creatinine ratio
Blood pressure; referral to GP for 24 hr ABPM / treatment if
indicated
Weight & BMI
Appropriate referral to be made if further nephrological, urological or
surgical opinion is indicated. GP referral to be made for unrelated health
problems
Upon discharge from the ward, donors must be provided with:
Appropriate advice about wound care, pain relief & general
rehabilitation
Prescribed medication & wound dressings as required
Medical certificate to cover the period of inpatient stay
EPR discharge summary for GP
Contact numbers for the living donor co-ordinator team
Routine follow-up appointment in surgical OPD clinic with
operating surgeon (when possible)

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
254
Figure 10.2 Toolkit to Support Centres to Provide Lifelong Donor Follow Up
Return Data to the UK Registry*
TOOLKIT: PART 1 - ELEMENTS AND REQUIREMENTS
ELEMENT
WHO
REQUIREMENT
Clinical Standard
What is best for
the donor?
BTS/RA UK
Guidelines for
LDKT
Annual follow-up
Clinical Review Registry
Data
Donor Reported Outcome
Measures (DROMs)
Legal Standard
What is required
by law?
EU Organ Donation
Directive
Human Tissue
Authority
Annual follow-up
UK Registry
What informs best
practice?
UK Registry
NHS Blood and
Transplant
Pan EU Registry
Collection of outcome data
1,2,5,10 and every 5 years
thereafter
TOOLKIT: PART 2 - WHERE TO PERFORM FOLLOW UP AND BY WHOM
WHERE?
BY WHOM?
1. Transplant Centre: Minimum year 1 +/-
1
st
anniversary appointment if returning to
referring unit/GP, or lifelong if donor
originated in transplant centre wishes to
stay
2. Referring nephrology centre: All donors
before or after 1
st
anniversary
appointment
3. Primary Care (GP): Donor choice, after
1
st
anniversary appointment
4. Non-UK Countries: By local arrangement
+/- written referral
Appropriately qualified
healthcare professional
Nurse-led after discharge
from medical/surgical review
clinic
Face to face
Telephone
Telemedicine

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
255
TOOLKIT: PART 3 - HOW TO PERFORM FOLLOW-UP
HOW
• Annual review in month of nephrectomy anniversary (tailored to clinical
need in 1
st
year)
• Transplant centre responsible for return of data from Tx centre and GP
• Referring units responsible for return of own data
• Electronic/paper submission of annual data to NHSBT within 3/12 of
anniversary (EU Registry uploaded from NHSBT Registry)
• Ensure all donors are given a positive choice about where/how they
are followed up and decision is recorded and reviewed at each visit
• Administrative processes in place in transplant centres & referring
centres to support clinics and correspondence, i.e.
• Maintaining local databases re donor preference for follow-up,
anniversary appointment dates
• Reminder appointment letters to donor +/- GP for anniversary
visits
• Receipt and return of donor data from GP & non-UK resident
donors
* developed and approved by the LDKT 2020 Strategy Implementation Group
10.3 The Unsuitable Donor
It is essential to provide appropriate care and follow-up for people who start the
donor assessment process but who do not subsequently donate. If the person is
unsuitable to donate because of health concerns, appropriate arrangements must
be made for any necessary further investigation and management. A donor who is
unsuitable for other reasons (for example a positive crossmatch) may need
emotional support to manage feelings of failure or guilt about the recipient and any
subsequent adverse outcomes should they occur (see Chapter 5).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
256
10.4 Pregnancy following Kidney Donation
Many kidney donors are women of child bearing age and accurate assessment of
potential pregnancy complications after donation is needed to inform decision
making. Early small studies (including 39 and 23 pregnancies) did not identify any
increased risk of pregnancy complications in women after donation (17,18).
However, larger survey and population studies have reported higher rates of
hypertensive complications during pregnancy. Comparison of pregnancy outcomes
pre- and post-donation in 326 donors from the Norwegian Birth Registry identified
that pre-eclampsia occurred more frequently after donation (5.7%) than before
donation (2.6%), but the absolute numbers affected were low (19). Similarly, the
incidences of pre-eclampsia and gestational hypertension were higher (5.5% and
5.7% respectively) after donation compared to pre-donation (0.8% and 0.6%
respectively) in a survey study of 1085 donors reporting 3213 pregnancies from
Minnesota (20). However, the rate of pre-donation pre-eclampsia in these studies
may be low due to selection bias, as women with a history of pre-eclampsia may
have been advised not to donate.
In the Minnesota study, post-donation pregnancies were also more likely than pre-
donation pregnancies to be complicated by fetal loss (19.2% v 11.3%), gestational
diabetes (2.7% v 0.7%), and delivery before 36 weeks gestation (26.3% vs 15.4%)
(20). There were no differences in pre-pregnancy eGFR between women with and
without complications post-donation. Greater maternal age after donation may
contribute to worse outcomes; however, the mean maternal age at pregnancy after
donation was 28.8 ± 5.5 years and is therefore unlikely to exclusively explain these
differences. These findings have not been confirmed by other studies.
More recently, a Canadian population study compared pregnancy outcomes in 131
pregnancies in 85 kidney donors with 510 healthy non-donor women selected from
the general population matched for demographics and number of previous
pregnancies (21). In keeping with previous findings, the rates of gestational
hypertension or pre-eclampsia (11%) were higher in kidney donors compared to
non-donors (5%). Again this study is limited by the small number of women affected
and the diagnosis of pre-eclampsia was determined by coding rather than by clinical
criteria. Importantly, there were no differences between the mode of delivery,
gestation at delivery or birth weight (i.e. features of poor placental function
associated with pre-eclampsia) between kidney donors and matched controls.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
257
It is recommended that women are informed of a potential greater risk of pregnancy
induced hypertension following kidney donation which may require specialist
antenatal care, but it does not appear to lead to adverse outcomes for either mother
or offspring. Close monitoring is advisable in donors during pregnancy, with
monitoring of blood pressure, creatinine and fetal well-being. Although direct
evidence of benefit is lacking, kidney donors can be offered Aspirin 75 mg daily for
pre-eclampsia prophylaxis (22). There is a theoretical risk of increased
complications in women with a single right kidney due to pregnancy-induced
hydronephrosis but there is no evidence at present to support a preference for right
or left nephrectomy.
Women who develop pre-eclampsia, particularly in those with early onset disease,
are more likely to develop long term health consequences (e.g. hypertension,
cardiovascular disease) than women with normal blood pressure during pregnancy
(23). Pre-eclampsia occurs in late pregnancy in the majority of kidney donors, but
the risk of future cardiovascular disease in kidney donors who develop pre-
eclampsia is unknown. Within the UK, there is an opportunity to report births post-
donation to the Living Donor Registry as ‘a significant medical event’ at each annual
review (24). This should be encouraged in order to improve the evidence base.
References
1. Fehrman-Ekholm I, Elinder CG, Stenbeck M, et al. Kidney donors live longer.
Transplantation 1997; 64: 976-8.
2. Fehrman-Ekholm I, Norden G, Lennerling A, et al. Incidence of end stage renal
disease among live kidney donors. Transplantation 2006; 82: 1646-8.
3. Najarian JS, Chavers BM, McHugh LE, Matas AJ. 20 years or more of follow-
up of living kidney donors. Lancet 1992; 340: 807-10.
4. Ibrahim HN, Foley R, Tan L, et al. Long-term consequences of kidney
donation. N Engl J Med 2009; 360: 459-69.
5. Segev DL, Muzaale AD, Caffo BS, et al. Perioperative mortality and long-term
survival following live kidney donation. JAMA 2010; 303: 959-66.
6. Muzaale AD, Massie A, Wang MC, et al. Risk of end-stage renal disease
following live kidney donation. JAMA 2014; 311: 579-86.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
258
7. Mjoen G, Hallan S, Hartmann A, et al. Long-term risks for kidney donors.
Kidney Int 2014; 86: 162-7.
8. Massie AB, Muzaale AD, Luo X, et al. Quantifying post-donation risk if ESRD
in living kidney donors. J Am Soc Nephrol 2017; 28: epub ahead of print.
9. Anjum S, Muzaale AD, Massie AB, et al. Patterns of end-stage renal disease
caused by diabetes, hypertension, and glomerulonephritis in live kidney
donors. Am J Transplant 2016; 16: 3540-7.
10. Lentine KL, Schnitzler MA, Xiao H, et al. Racial variation in medical outcomes
among living kidney donors. N Engl J Med 2010; 363: 724-32.
11. Parsa A, Kao L, Xie D, et al. APOL1 risk variants, race, and progression of
chronic kidney disease. N Engl J Med 2013; 369: 2183-96.
12. Grams ME, Sang Y, Levey AS, et al. Kidney failure risk projection for the living
donor candidate. N Engl J Med 2016; 374: 411-21.
13. Survey of life-long donor follow-up practice in UK Transplant Centres, LDKT
2020 Strategy Implementation Group, (presented April 2016).
14. Directive 2010 /45/EU of the European Parliament and of the Council of 7 July
2010.
http://www.hta.gov.uk/_db/_documents/EUODD_Directive_August_2011.pdf
15. Living Donor Registry. http://www.odt.nhs.uk/uk-transplant-registry/
16. Living Donor Kidney Transplantation Centre Specific Report, 2016/17.
https://www.odt.nhs.uk/statistics-and-reports/organ-specific-reports/
17. Jones JW, Acton RD, Elick B, Granger DK, Matas AJ. Pregnancy following
kidney donation. Transplant Proc 1993; 25: 3082.
18. Buszta C, Steinmuller DR, Novick AC, et al. Pregnancy after donor
nephrectomy. Transplantation 1985; 40: 651-4.
19. Reisaeter, AV, Roislien, J, Henriksen, T, Irgens, LM, Hartmann, A. Pregnancy
and birth after kidney donation: the Norwegian experience. Am J Transplant
2009; 9: 820-4.
20. Ibrahim HN, Akkina SK, Leister E, et al. Pregnancy outcomes after kidney
donation. Am J Transplant 2009; 9: 825-34.
21. Garg AX, Nevis IF, McArthur E, et al. Gestational hypertension and pre-
eclampsia in living kidney donors. N Engl J Med 2015; 372: 124-33.
22. National Institute of Clinical and Health Excellence: Hypertension in
pregnancy: the management of hypertensive disorders during pregnancy.
2010.
23. Mol BW, Roberts CT, Thangaratinam S, Magee LA, de Groot CJ, Hofmeyr GJ.
Pre-eclampsia. Lancet 2015; 387: 999-1011.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
260
11 RECIPIENT OUTCOME AFTER LIVING DONOR KIDNEY
TRANSPLANTATION IN ADULTS
Recommendations
Graft and patient survival after living donor kidney transplantation
should be within the national range of expected outcomes. (A1)
Transplant centres should regularly audit secondary outcomes and
should reappraise practice if their results are not comparable with
other units. (B1)
Where a recipient is considered to be at high risk, transplantation
should only proceed if, in the view of the team of professionals
involved, there is an expectation that the patient is likely to survive with
a functioning transplant for more than 2 years. (C2)
Patients at higher risk of complications and a poor outcome, due to
immunological status or co-morbidities, should be considered for
transplantation when the clinical team regard the risk / benefit ratio to
be favourable. Due process will include careful consideration of the
likely outcome for that individual without transplantation. The potential
donor must be fully appraised of the issues. A summary of these
discussions (between the clinical team and the donor-recipient pair)
should be documented in the clinical records and a copy should also
be given to the donor and recipient. (C2)
Continuous and careful consideration of recipient outcomes is an important aspect
of any living donor kidney transplant programme. This section will consider the
outcomes in:
Living versus deceased donor transplantation
Extended criteria living donors
Living donor transplantation versus dialysis
High risk recipients
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
261
11.1 Living versus Deceased Donor Transplantation
It is long established that recipients of living donor kidney transplants have superior
graft and patient survival compared to those from deceased donor organs. Pre-
mortal renal injury is avoided, donors are generally healthier, cold ischaemic times
are shorter, and operative conditions for the recipient are optimised in an elective
setting. Additionally, it is often possible to arrange pre-emptive transplantation or
minimisation of dialysis duration.
The UK Transplant Registry, managed by the Organ Donation and Transplant (ODT)
division of National Health Service Blood and Transplant (NHSBT) authority,
provides contemporaneous supportive data (1).
For example, 10 years after transplantation, 75% of adults who received their first
(kidney only) deceased brainstem death donor transplant in 1998-2000 were still
alive. This compares to 90% of those transplanted in the same period with a first
kidney transplant from a living donor. Hence, there was a 20% improvement in 10-
year patient survival with living versus deceased donation for those transplanted in
that period (1).
The annual activity reports provided by ODT also allow for the comparative
assessment of graft and patient outcomes for individual centres. Such comparative
national audit is of great value and necessitates an ongoing commitment to data
return from each centre (see Chapter 10).
11.2 Extended Criteria Living Donors
The persistent disparity between the number of patients waiting for a kidney
transplant and the organs available from the deceased donor pool, coupled with
increasing familiarity of the outcomes for living donors and their recipients, has led
the transplant community to consider potential donors who would previously been
discounted due to demographic characteristics or medical issues.
The areas of uncertainty related to short and long-term outcomes for the donor in
medically complex volunteers is covered in detail in other sections of these
guidelines.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
262
In terms of recipient outcome, consideration must be given to the alternative options:
the likelihood of receiving a standard or extended criteria deceased donor
transplant, the outcome of such a transplant, the morbidity and potential mortality
risk while waiting for a suitable deceased organ, the suitability / risks associated with
emergency versus elective surgery, the likely outcome of this living donor organ in
comparison with projected life expectancy of this individual etc.
The literature is sufficiently developed to advocate transplantation from older living
donors for at least a cohort of patients (see section 5.6.4 for detailed discussion). In
a similar manner, the appropriateness of giving what may be a ‘non-ideal’ living
donor kidney (due to function, matching, co-morbidities) to a patient must be
considered on an individual basis for the particular recipient. Entry of a donor-
recipient pair into the UK Living Kidney Sharing Scheme (UKLKSS) should be
considered when it may be possible to achieve a better living donor option,
particularly in terms of age or matching for younger recipients. As of 31 Dec 2016,
66 compatible pairs were registered in the UKLKSS; in 12 pairs the age difference
between donor and recipient exceeded 20 years; in 58 pairs the HLA mismatch was
level 4 (2). It is expected that in due time, more data on outcomes for recipients from
more complex donors will be available to guide decision-making.
11.3 Transplantation versus Dialysis
It must be remembered that the long-term outcome for patients on maintenance
dialysis therapy remains limited. The decision for a recipient is seldom between a
‘sub-optimal’ and an ‘ideal’ living donor kidney transplant. The alternative to living
donor transplantation, of whatever quality, is to remain on dialysis waiting for a
suitable deceased donor organ.
The quality of deceased donor kidneys now available for transplantation in the UK
must also be taken into consideration. For example, a living donor kidney may be
declined for a recipient on the basis of age but, in 2016-17, 36% of all deceased
donors in the UK were at least 60 years old (1).
The duration of dialysis therapy before transplantation remains an important
(potentially modifiable) factor in long-term survival after transplantation. Of those
listed for kidney transplantation in the UK in 2011-12, 56% had received a transplant
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
263
after 3 years, 6% had been removed from the waiting list and 5% had died while
waiting (1). This is another important issue when considering potential living donor
transplant options.
11.4 High Risk Recipients
The success of a transplant programme cannot be judged solely by recipient and
graft survival, but in the outcomes for the entire end-stage renal disease (ESRD)
population. A conservative approach to risk is more likely to result in excellent graft
and patient survival after transplantation, but potentially be associated with inequity
of access to transplantation for patients at higher anaesthetic, surgical or
immunological risk and an increased risk of death on the waiting list. A measure of
the approach of individual units to risk is less easily measured than survival
outcomes in those transplanted. The proportion listed for transplantation is one such
measure. Of note, the Access to Transplantation and Transplant Outcome Measure
(ATTOM) national observational study has identified significant disparities in age,
ethnic, socio-economic and geographical factors living donor transplant utilisation
(3).
For the purpose of this guideline, a high-risk recipient is defined as a potential
recipient of a kidney transplant who is at a significantly higher risk of death,
complications or graft failure because of pre-existing co-morbidity or immunological
status. Statistically, this equates to an expected outcome that is outside the 95%
confidence interval for graft and patient survival in the UK. There is currently no
robust, clinically applicable scoring system upon which to base this assessment of
risk. Although models are likely to be developed in due course (4,5), it is recognised
that with the uncertainty of prediction tools there is on-going dependency on the
clinical judgement of the transplant professionals involved.
Living donor kidney transplantation can provide opportunity for individuals whose
peri-operative risks for an emergency procedure are considered unacceptably high,
but who may be suitable for an elective transplant. The advantages include:
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
264
Optimisation of the recipient
Availability of senior staff from across the multidisciplinary team (surgeons,
anaesthetists and intensivists, H&I scientists, nursing staff in theatre and
ward, nephrologists etc.)
Pre-transplant immunosuppression or immunomodulation
Good quality organ with low risk of delayed graft function
The key issue is that, whilst these patients may expect a relatively poorer outcome
from transplantation compared with individuals considered to be at standard risk,
their outcome may be better than it would be if they remained on dialysis. Pre-
existing cardiovascular disease, pulmonary disease, obesity and diabetes all affect
survival of patients whether they have a transplant or are dialysis dependent (6,7).
The premise of undertaking higher risk living donor transplantation is already
established. Antibody incompatible transplants, for example, are excluded from the
survival analysis on living donor kidney transplant outcomes in the annual NHSBT
report as the survival rates are not as good as antibody compatible transplants.
However, for some patients, such a transplant represents the only option for dialysis
independency.
Given the insufficient data available to give clear guidance on this issue to individual
high-risk recipients, risk assessment in each case must, by default, be based on
combined expert opinion. Careful consideration of all higher risk living donor
transplants must be in a multi-disciplinary meeting, with clear documentation of
discussions.
In a similar manner, the risks and likely outcomes must be conveyed to both the
donor and recipient. Although such discussion is applicable to living donation in
general, it is particularly important for the high risk recipient where the risk of an
adverse outcome is greater than for standard transplantation.
The following are recommended when considering potential higher risk recipients:
If it is unlikely that the patient would survive with a functioning graft for at
least 2 years, then living donor transplantation should not be considered
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
265
The risks and benefits of living donor transplantation must be described
along with other management options (deceased donor transplantation,
dialysis, maximal conservative care)
It must be established what the recipient wants and expects from
transplantation in terms of quality and extension of life
If considering living donor transplantation, particularly for patients who are
high risk due to established co-morbidities, the goal should be pre-emptive
transplantation
The donor must be fully appraised of the risks and the potentially poor
outcome for the recipient
The details of the final understanding must be compliant with the NHS
consent process, and documentation of the issues must be given to both the
donor and recipient
If agreement cannot be achieved within a particular transplant centre e.g.
because of differences in opinion on the degree of risk, the option of referral
to another transplant centre for a second opinion must be discussed with the
potential recipient and donor
It is important that the decision to transplant high risk recipients is not influenced by
undue concern about outcome data. It is not possible to set national standards for
transplant outcomes in this group given the patient heterogeneity and unit variation
in definition of high risk. It is recommended that each centre maintains detailed
records of relevant clinical features for each high risk recipient. This will be useful
for internal or external review, and may be valuable for future audit.
It is recommended that, for all living donor transplants, data are also collected locally
by each unit. There are many parameters that are not currently reported centrally
but which are important measures of service provision that should be audited
regularly. The following list is not exhaustive:
Delayed graft function
Return to theatre
Urological complications
Acute rejection
Infective complications
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
266
Transplant artery stenosis
Renal function at 1 and 5 years
References
1. UK Transplant Registry annual activity reports and organ specific reports.
https://www.odt.nhs.uk/statistics-and-reports/annual-activity-report/
2. Mumford L. Compatible pairs in the UK living kidney sharing schemes.
Presented at NHSBT Renal Transplant Services meeting 2017.
3. Wu DA, Robb ML, Watson CJE, et al. Barriers to living donor kidney
transplantation in the United Kingdom: a national observational study. Nephrol
Dial Transplant 2017; 32: 890-900.
4. Li B, Cairns JA, Robb ML, et al. Predicting patient survival after deceased donor
kidney transplantation using flexible parametric modelling. BMC Nephrol 2016;
17: 51-61.
5. John Hopkins University School of Medicine Transplant Models: Kidney
transplant candidacy calculator for older patients.
www.transplantmodels.com/candidate65
6. UK Renal Registry annual report 2015.
https://www.renalreg.org/reports/2015-eighteenth-annual-report/
7. Fuggle SV, Allen JE, Johnson RJ, et al. Factors affecting graft and patient
survival after live donor kidney transplantation in the UK. Transplantation 2010;
89: 694-701.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
267
12 RECURRENT RENAL DISEASE
Summary of Recommendations
A wide range of diseases that cause renal failure may recur in a
transplanted kidney. This is important to consider when determining
the optimal treatment strategy for a recipient and when counselling
both donor and recipient on the relative risks and benefits of living
donor transplantation. The risks of recurrence, the consequences for
transplant function, and the time-course of any deterioration must all
be considered. A discussion of the effects of immunosuppression and
transplant failure on morbidity and mortality may also be appropriate.
(B1)
The risks of recurrent disease are high in FSGS and MCGN. In these
diseases, the presence of specific adverse clinical features may
indicate living donor transplantation should be avoided, even where a
donor is available. This will require careful assessment and
deliberation with all interested parties. (B2)
In atypical HUS potential de novo disease in a related donor needs to
be addressed directly. The risks of recurrent disease in the recipient
need to be mitigated through regulated approval and consideration of
the use of an inhibitor of complement activation, currently eculizumab.
(A1)
In patients with risks related to underlying activity such as SLE or
systemic vasculitis, adequate disease control and an appropriate
period of quiescence are important to ensure optimal outcomes. (B1)
Recommendations for individual diseases follow in the following text.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
268
12.1 Introduction
Many native kidney diseases can recur following transplantation and may result in
allograft failure. These include systemic disorders of metabolism and
glomerulonephritis (1, 2). The reduction in acute rejection associated with modern
immunosuppression means that recurrent disease is now an important cause of
graft dysfunction and/or failure (3). The likelihood and consequences of recurrence
are therefore important when assessing and counselling living donor-recipient pairs.
In many diseases, the published literature on recurrent disease post-transplantation
consists largely of case series. These give only a limited quantification of risk as
they are confounded by ascertainment bias since there is an interaction between
the indication for biopsy and the consequences of disease recurrence (2). Large
registry studies provide a better estimation of risk; however, they too require careful
interpretation because disease rates will be influenced by diagnostic practice and
convention in the contributing centres (4-7). This is particularly important when
considering heterogeneous disease processes such as FSGS (2).
These issues are considered in the following discussion of individual diseases. This
is an evolving field and it may be necessary to review source data or seek specialist
advice to estimate risk and decide upon the optimal treatment for individual cases.
For example, previous reports of an association between living kidney donation and
the recurrence of glomerulonephritis, particularly in zero mismatched donor-
recipient pairs, have either been unconfirmed (6) or not so clear-cut as to definitely
preclude transplantation (8,9).
There is increasing definition of single genes associated with familial FSGS, which
may in fact present as sporadic disease. This has implications for assessment of
any related donor but also improves quantification of the risk of disease recurrence.
In atypical haemolytic uraemic syndrome (HUS) the risk of unrecognised genetic
susceptibility to disease in the donor and in the recipient is now well recognised and
has significantly influenced clinical practice with respect to the assessment of any
donor (10). Similarly, the availability of eculizumab, an inhibitor of complement C5
cleavage has changed practice with respect to the prevention of disease recurrence
in the recipient (10).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
269
12.2 Diabetic Nephropathy
Histological recurrence of diabetic nephropathy is relatively common following renal
transplantation (11). The time required for recurrent diabetic disease to cause
significant graft dysfunction is long and it is therefore not a contraindication to living
donor transplantation. Living donor transplantation significant benefits with respect
to both patient and graft outcomes (12-14). Where appropriate, the balances of risk
and benefit should also be compared with the option of combined kidney and
pancreas transplantation from a deceased donor.
Recommendation
Type 1 and type 2 diabetes are not contraindications to living donor
transplantation, irrespective of whether they are the underlying cause
of renal failure. Both the donor and recipient should be counselled
regarding the increased risks associated with surgery.
12.3 Primary Focal Segmental Glomerulosclerosis
Recurrent focal segmental glomerulosclerosis (FSGS) is a significant problem
following renal transplantation and is estimated to occur in 20% to 50% of cases
(1,2,15). This wide range in reported frequency of recurrence is likely to reflect
heterogeneity in the underlying diagnoses associated with FSGS. The histological
description of FSGS in the context of proteinuria and renal failure frequently occurs
as a non-specific finding in many forms of kidney disease, including transplantation.
This secondary FSGS may complicate the interpretation of undifferentiated reports
of recurrence in transplantation.
Primary FSGS, characterised by the nephrotic syndrome, is associated with a high
risk of disease recurrence in the transplant, particularly if there is:
End stage renal failure at a young age, particularly during adolescence (5,15-
17)
Rapid progression to end stage renal failure (18)
Recurrent disease in a previous transplant (5,6,19)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
270
In these situations the rate of graft loss secondary to recurrent disease may be
significantly above 50%. This generalisation is, however, not true in familial forms of
FSGS, which can have an early presentation and rapid course of deterioration but
have a relatively low risk for disease recurrence (20-24). This is also true of sporadic
forms of FSGS in which a genetic diagnosis is nevertheless established. A
contemporary strategy for age-stratified identification of genetic causes of FSGS is
therefore recommended (20). The detail of this strategy is likely to evolve with
increased availability of genetic data.
Even primary FSGS presenting with the nephrotic syndrome seems not to be a
single disease entity, and this may account for differences in the rate of recurrence
in different groups. For example, there is evidence that recurrent disease is more
common in whites than blacks (25), pointing towards genetic heterogeneity and
potential future risk stratification (25,26).
Recurrent primary FSGS generally occurs in the first 6 months following
transplantation, an important point if transplant recipients are not to be incorrectly
labelled as having recurrent disease. The very rare recurrence of nephrotic
syndrome consequent upon de novo antibody formation to a nephrin determinant
absent in the recipient in congenital nephrotic syndrome of the Finnish type is an
exception to this generalisation (22).
There is now sufficient information to believe that previous suggestions of a
relationship between HLA matching and risk of recurrence are not a concern, but
probably arose from co-linearity with other risk factors (26,27).
Recommendations
Living donor kidney transplantation is a reasonable option in patients
with primary FSGS. Both the donor and recipient need to be specifically
counselled about the risk of recurrent disease, which may occur early
and result in rapid graft loss. In those in whom a genetic aetiology has
been established the risk of recurrent disease is low but not absent. A
potential living related donor must also be investigated for evidence of
the same genetic abnormality.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
271
Transplantation in an individual with unequivocal evidence of graft
loss secondary to recurrent disease constitutes a high risk of
subsequent failure such that some centres consider this a
contraindication to repeat transplantation (28). In this context, living
donor transplantation should be considered only in special
circumstances and after careful discussion between the multi-
professional team, the donor and the recipient. Equally it is incumbent
upon that team to assess the circumstances of the original graft failure
with absolute rigor. The risk of recurrence is low when the previous
graft did not fail due to recurrent disease.
12.4 IgA Nephropathy
Histological evidence of recurrent IgA nephropathy commonly occurs in
transplanted kidneys, but is less frequently of clinical significance. It may be
associated with transient, but more commonly slowly progressive transplant
dysfunction. The prevalence of graft loss due to recurrent IgA disease was 2.8% in
the report of Briganti and colleagues, which gave an estimated 10-year incidence of
graft loss of 9.7% (7). The importance of recurrent disease may be reducing in the
context of modern immunosuppression (29).
Recommendation
The risk of recurrent disease does not contraindicate living donor
transplantation in IgA nephropathy. Both the donor and recipient
should be counselled regarding the risks of recurrent disease.
12.5 Membranous Nephropathy
The recurrence rate of idiopathic membranous nephropathy has been reported as
29% in the first 3 years post-transplantation with a corresponding graft survival of
52% at 5 years and 38% at 10 years (30,31). In the report of Briganti and colleagues,
recurrent membranous nephropathy was responsible for 12.5% of the 40.1% of
failed transplants at 10 years (7).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
272
Recurrent disease may relate to the persistence of antibody to PLA2 receptor but
this remains to be proven (32). At the time of transplantation, approximately 50% of
patients have detectable antibody and its presence is associated with recurrent
disease; however, the correspondence is imperfect and at present there is no
evidence to suggest that this should alter the approach to treatment. Living donation
seems not to be a risk factor for recurrent disease.
Recommendation
This risk of recurrent disease does not contraindicate living donor
transplantation in membranous nephropathy. Both the donor and
recipient should be counselled regarding the risks of recurrent
disease.
12.6 Amyloidosis
In patients with amyloidosis, the underlying cause, disease activity, response to
treatment and extra-renal involvement will inform the strategy for renal
transplantation. Initial assessment will usually involve the National Amyloidosis
Centre. Living donor kidney transplantation is a reasonable treatment option in some
circumstances, after adequate control of the underlying disease has been achieved
(33,34). The donor and recipient need to be counselled regarding the additional risks
arising from recurrent renal disease and the additional mortality associated with the
underlying disease and its treatment.
Recommendation
Patients with amyloidosis should be discussed with the National
Amyloidosis Centre before progressing to living donor transplantation.
Patients with AA amyloidosis should have effective disease control
before surgery.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
273
12.7 Systemic Lupus Erythematosus
Recurrence of lupus nephritis within a transplant is said to be low. The risk of
recurrence is higher in young black females and is associated with a high rate of
graft loss (35), although this is not always directly attributable to disease activity.
The treatment of active lupus should be optimised before transplantation, although
it is recognised that serological markers of disease, native renal histology and
duration of dialysis are poor predictors of recurrent disease. The presence of anti-
phospholipid antibodies is a risk factor for thrombotic complications following
transplantation. Where these are present, this should be discussed with the donor
and recipient before transplantation and increased peri-operative anti-thrombotic
prophylaxis should be considered.
Recommendation
The overall risks associated with recurrent disease are small in SLE
and living donor transplantation is safe in quiescent disease. Both the
donor and recipient should be counselled regarding the risks of
recurrent disease. (B2)
12.8 ANCA Associated Systemic Vasculitis
The risk of recurrent disease in ANCA associated systemic vasculitis (AASV) is
small when patients are transplanted in remission: reportedly between 1% and 2.8%
per year of patient follow-up The consequences of recurrence may, however, be
significant, with increased mortality and graft loss (36).
There is a particular risk associated with kidney transplantation less than 1 year
following the induction of remission because of increased recipient mortality. Living
donor transplantation should therefore usually take place after 1 year of disease
quiescence, although this should be balanced against the potential risks of staying
on dialysis (37). Although the detection of ANCA is a risk factor for disease
recurrence, a persistently positive ANCA is a common finding and is not a
contraindication to transplantation if unaccompanied by clinical disease.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
274
Recommendation
The risks associated with recurrent disease are small and the
outcomes of transplantation good, therefore AASV does not
contraindicate living donor transplantation if the aforementioned
criteria are met. Both the donor and recipient should be counselled
regarding the risks of recurrent disease.
12.9 Goodpasture’s Disease
Recurrent renal disease is rare following a diagnosis of Goodpasture’s disease
provided the recipient no longer produces anti-glomerular basement membrane
antibodies. Transplantation should be delayed for at least 6 months following the
disappearance of anti-GBM antibodies and for 12 months following presentation
(38,39).
Recommendation
The risks associated with recurrent disease are small and the
outcomes of transplantation good, therefore Goodpasture’s disease
does not contraindicate living donor transplantation if the
aforementioned criteria are met. Both the donor and recipient should
be counselled regarding the risks of recurrent disease.
12.10 Alport Syndrome
De novo anti-GBM disease is reported in approximately 5% of patients with Alport
syndrome and despite treatment may result in transplant failure (40). It is reported
to occur mainly in patients with a juvenile type X-linked Alport syndrome and
truncation mutations of the COLIVA5 gene. When a patient has lost one transplant
due to post-transplant anti-GBM disease, repeat transplantation is difficult because
of the high risk of recurrence. The decision to proceed should be considered only
after careful discussion between the multi-professional team, the donor, and the
recipient.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
275
Recommendation
The overall risks associated with Alport syndrome are small and the
outcomes of transplantation good, therefore Alport syndrome does not
contraindicate living donor transplantation. Both the donor and
recipient should be counselled regarding the risks of de novo anti-GBM
disease. (B2)
12.11 Mesangiocapillary Glomerulonephritis
There has been a significant change in the description of mesangiocapillary
glomerulonephritis (MCGN) based upon improved understanding of the
mechanisms underlying its pathogenesis. MCGN may be associated with
predominant deposition of monoclonal or polyclonal immunoglobulin. This may be
secondary to haematological, autoimmune or infectious disease with a small
number of ‘idiopathic’ cases. MCGN may also be associated with dysregulated
activation of the alternate pathway of complement encompassed in the term C3
glomerulopathy (41). C3 glomerulopathy may be divided on the basis of electron
microscopic appearance into Dense Deposit Disease (DDD) and C3
glomerulonephritis. Assessment of these diseases is described in detail elsewhere.
In patients with C3 glomerulopathy, detailed complement testing should be
performed to identify any underlying complement abnormality as it may inform the
risk of recurrence. The identification of genetic complement regulatory abnormalities
in a proband also has implications for other family members who may be affected.
The description of outcomes following transplantation has until recently relied upon
histological differentiation primarily reporting on MCGN class I and II. These provide
much of the context for the reported literature and the recommendations that follow,
albeit with additional insights provided by contemporary understanding of C3
glomerulopathy.
Type I MCGN has been reported to recur in between 33% and 48% of renal allograft
recipients after four years. The mean graft survival following recurrence is 40 months
(8) and the risk of recurrence in a subsequent graft may be as high as 80% (9). The
risk of graft loss in patients with recurrent type 1 MCGN is therefore around 15% at
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
276
5 years. This represents a significant cause of transplant failure (7,8,42). The risk of
recurrence may be higher in living donor transplantation (8,9). It may be that the risk
of secondary MCGN is low following successful control of the underlying disease.
On the other hand, this histological classification includes a significant mix of cases,
some with immunoglobulin deposition and others with C3 glomerulonephritis. In
these cases it is thought that the likelihood of recurrent disease in C3
glomerulonephritis is likely to be high and comparable to that of DDD.
DDD (Type II MCGN) is the primary glomerulonephritis most likely to recur after
renal transplantation and does so in virtually all cases. The outcome after
transplantation is variable. In 75 patients reported by the North American Pediatric
Renal Transplant Cooperative Study, 5 year graft survival was 65.9% and 34.1% in
living and deceased donor transplantation respectively (42). Poor outcome has been
associated with heavy pre-transplant proteinuria and increased glomerular
proliferation (43).
Recommendations
Type I and II MCGN do not contraindicate living donor transplantation.
However, the risk of recurrent disease and subsequent graft loss is
sufficiently high that transplantation should only be undertaken
following careful discussion between the multi-professional team, the
donor and the recipient. This is particularly the case if there is an
identified abnormality of a soluble complement regulatory protein.
Transplantation in an individual with unequivocal evidence of graft
loss secondary to recurrent C3 glomerulopathy constitutes a high risk
of subsequent failure such that some centres consider this a
contraindication to repeat transplantation (44)
Among patients with genetic abnormalities in complement proteins or
with an unknown cause of C3 glomerulopathy, a comparison with
atypical HUS suggests that consideration should be given to avoiding
living related donors in whom similar genetic mutations may
predispose to the future development of C3 glomerulopathy after
nephrectomy (44)
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
277
12.12 Haemolytic Uraemic Syndrome
The recommendation for renal transplantation in HUS has changed significantly
since the previous edition of these guidelines because effective therapy has become
available for the treatment and prevention of recurrent disease in atypical HUS. In
England, use of this medication, eculizumab, is co-ordinated through a national
expert centre. There remain, however, important considerations with respect to the
recipient and donor. The principles of this management are discussed in a
publication from 2009: ‘Clinical Practice guidelines for the management of atypical
haemolytic uraemic syndrome in the United Kingdom’ (10). Additional information
relevant to the use of eculizumab has been prepared by the national expert centre
and is accessible through rarerenal.org. Further advice on genetic testing and
evaluation of potential donors is available through the aHUS National Service
(contact details on rarerenal.org).
HUS may be associated with infection, most commonly with diarrhoea caused by
verocytotoxin producing coliforms. It may also occur in association with disorders of
complement regulation, most commonly of genetic origin. Rarely, it may occur in
other settings including HIV infection, malignancy, pregnancy, connective tissue
disease and with certain medication.
Patients presenting with atypical HUS or wishing to be considered for transplantation
should be assessed in accordance with the aforementioned guidelines and the
national expert centre. The rate of recurrence following transplantation is high in
patients known to have mutations in Factor H or gene re-arrangements involving
Factor H or Factor H related proteins, gain of function mutations in Factor B or C3,
or who have lost a previous transplant due to disease recurrence. The risk of
recurrence is intermediate for mutations of factor I, in the presence of autoantibodies
against factor H, and when mutations of uncertain functional significance or when
no mutation or autoantibody is detected. Patients carrying an MCP (CD46) mutation
but no additional mutation in factor H, factor I, factor B and C3 or an anti-factor H
autoantibody have a low risk of recurrence after transplantation (10).
Living unrelated transplantation may therefore be considered after appropriate
counselling of donor and recipient. Patients at low risk do not require prophylaxis
with eculizumab but should be warned of the possibility of recurrence and monitored
closely. In patients at medium or high risk of recurrence it is recommended that
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
278
treatment with eculizumab be offered, although the necessary duration of treatment
is uncertain.
Living related renal transplantation should normally be avoided in atypical HUS
because there is a risk of disease occurring in the donor, even in the absence of a
currently recognised mutation. In exceptional circumstances, living related donation
may be considered after all known mutations have been excluded in the donor and
the risks of HUS in the donor have been carefully discussed.
In patients in whom the underlying cause has unequivocally been attributed to
Shiga-toxin, the recurrence rate is low and living donor transplantation may be
considered (40).
Recommendations
Living related renal transplantation should be avoided in atypical HUS
unless the cause of the disease in the recipient is known and this has
been excluded in the donor. Even then related donors may be at a
greater risk of aHUS and should be warned of this risk.
In patients in whom the underlying cause has unequivocally been
attributed to Shiga-toxin, the recurrence rate of HUS is low and living
donor transplantation may be considered.
12.13 Primary Hyperoxaluria
Primary hyperoxaluria is a rare condition that requires careful assessment and
specialist advice to optimise management. Living donor kidney transplantation is a
treatment option in certain circumstances, whereas in others combined liver and
kidney transplantation is preferred (45).
Primary hyperoxaluria type 1 is generally treated with combined liver and kidney
transplantation (46,47) or early liver transplantation alone (48). However, some
groups in North America have advocated early living donor kidney transplantation,
particularly if there is evidence of pyridoxine responsiveness (49) in particular in
patients homozygous for the G170R mutation (50).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
279
Primary hyperoxaluria type 2 has been treated successfully with kidney
transplantation alone. This is ideally pre-emptive, therefore living donor
transplantation is a reasonable treatment option (51).
Recommendation
In appropriately selected cases, living donor kidney transplantation is
a reasonable treatment option in primary hyperoxaluria. Both the donor
and recipient should be counselled regarding the risks of recurrent
disease.
12.14 Cystinosis
The outcome of living donor transplantation in cystinosis is primarily determined by
extra-renal complications, which can be mitigated by long-term treatment with
cysteamine (52).
Recommendation
Cystinosis is not a contra-indication to living donor transplantation.
However, both donor and recipient should be counselled regarding the
long-term extra-renal complications related to disease progression.
References
1. Choy BY, Chan TM, Lai KN. Recurrent glomerulonephritis after kidney
transplantation. Am J Transplant 2006; 6: 2535-42.
2. Golgert WA, Appel GB, Hariharan S. Recurrent glomerulonephritis after renal
transplantation: an unsolved problem. Clin J Am Soc Nephrol 2008; 3: 800-7.
3. El-Zoghby ZM, Stegall MD, Lager DJ, et al. Identifying specific causes of kidney
allograft loss. Am J Transplant 2009; 9: 527-35.
4. Hariharan S, Adams MB, Brennan DC, et al. Recurrent and de novo glomerular
disease after renal transplantation: a report from Renal Allograft Disease
Registry (RADR). Transplantation 1999; 68: 635-41.
5. Briggs JD, Jones E. Recurrence of glomerulonephritis following renal
transplantation. Scientific Advisory Board of the ERA-EDTA Registry. European
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
280
Renal Association-European Dialysis and Transplant Association. Nephrol Dial
Transplant 1999; 14: 564-5.
6. Cibrik DM, Kaplan B, Campbell DA, Meier-Kriesche HU. Renal allograft survival
in transplant recipients with focal segmental glomerulosclerosis. Am J
Transplant 2003; 3: 64-7.
7. Briganti EM, Russ GR, McNeil JJ, Atkins RC, Chadban SJ. Risk of renal
allograft loss from recurrent glomerulonephritis. N Engl J Med 2002; 347: 103-
9.
8. Lorenz EC, Sethi S, Leung N, Dispenzieri A, Fervenza FC, Cosio FG. Recurrent
membranoproliferative glomerulonephritis after kidney transplantation. Kidney
Int 2010; 77: 721-8.
9. Andresdottir MB, Assmann KJ, Hoitsma AJ, Koene RA, Wetzels JF. Recurrence
of type I membranoproliferative glomerulonephritis after renal transplantation:
analysis of the incidence, risk factors, and impact on graft survival.
Transplantation 1997; 63: 1628-33.
10. Taylor CM, Machin S, Wigmore SJ, Goodship TH. Clinical practice guidelines
for the management of atypical haemolytic uraemic syndrome in the United
Kingdom. Br J Haematol 2010; 148: 37-47.
11. Hariharan S, Smith RD, Viero R, First MR. Diabetic nephropathy after renal
transplantation. Clinical and pathologic features. Transplantation 1996; 62: 632-
5.
12. Young BY, Gill J, Huang E, et al. Living donor kidney versus simultaneous
pancreas-kidney transplant in type I diabetics: an analysis of the OPTN/UNOS
database. Clin J Am Soc Nephrol 2009; 4: 845-52.
13. Poommipanit N, Sampaio MS, Cho Y, et al. Pancreas after living donor kidney
versus simultaneous pancreas-kidney transplant: an analysis of the organ
procurement transplant network/united network of organ sharing database.
Transplantation 2010; 89: 1496-503.
14. Reese PP, Israni AK. Best option for transplant candidates with type 1 diabetes
and a live kidney donor: a bird in the hand is worth two in the bush. Clin J Am
Soc Nephrol 2009; 4: 700-2.
15. Ingulli E, Tejani A. Incidence, treatment, and outcome of recurrent focal
segmental glomerulosclerosis posttransplantation in 42 allografts in children--a
single-center experience. Transplantation 1991; 51: 401-5.
16. Moroni G, Gallelli B, Quaglini S, et al. Long-term outcome of renal
transplantation in patients with idiopathic membranous glomerulonephritis
(MN). Nephrol Dial Transplant 2010; 25: 3408-15.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
281
17. Baum MA, Ho M, Stablein D, Alexander SR. Outcome of renal transplantation
in adolescents with focal segmental glomerulosclerosis. Pediatr Transplant
2002; 6: 488-92.
18. Schachter M, Monahan M, Radhakrishnan J, et al. Risk of recurrent focal
glomerulosclerosis (RFSGS) in the renal allograft J Am Soc Nephrol 2007; 18:
683A.
19. Stephanian E, Matas AJ, Mauer SM, et al. Recurrence of disease in patients
retransplanted for focal segmental glomerulosclerosis. Transplantation 1992;
53: 755-7.
20. Santín S, Bullich G, Tazón-Vega B, et al. Clinical utility of genetic testing in
children and adults with steroid-resistant nephrotic syndrome. Clin Journal Am
Soc Nephrol 2011; 6: 1139-48.
21. Ghiggeri GM, Aucella F, Caridi G, et al. Posttransplant recurrence of proteinuria
in a case of focal segmental glomerulosclerosis associated with WT1 mutation.
Am J Transplant 2006; 6: 2208-11.
22. Becker-Cohen R, Bruschi M, Rinat C, et al. Recurrent nephrotic syndrome in
homozygous truncating NPHS2 mutation is not due to anti-podocin antibodies.
Am J Transplant 2007; 7: 256-60.
23. Kuusniemi AM, Qvist E, Sun Y, et al. Plasma exchange and retransplantation
in recurrent nephrosis of patients with congenital nephrotic syndrome of the
Finnish type (NPHS1). Transplantation 2007; 83: 1316-23.
24. Weber S, Gribouval O, Esquivel EL, et al. NPHS2 mutation analysis shows
genetic heterogeneity of steroid-resistant nephrotic syndrome and low post-
transplant recurrence. Kidney Int 2004; 66: 571-9.
25. Abbott KC, Sawyers ES, Oliver JD, et al. Graft loss due to recurrent focal
segmental glomerulosclerosis in renal transplant recipients in the United States.
Am J Kidney Dis 2001; 37: 366-73.
26. Nehus EJ, Goebel JW, Succop PS, Abraham EC. Focal segmental
glomerulosclerosis in children: multivariate analysis indicates that donor type
does not alter recurrence risk. Transplantation 2013; 96: 550-4.
27. Holmberg C, Jalanko H. Congenital nephrotic syndrome and recurrence of
proteinuria after renal transplantation. Pediatr Nephrol 2014; 29: 2309-17.
28. Ghiggeri GM, Carraro M, Vincenti F. Recurrent focal glomerulosclerosis in the
era of genetics of podocyte proteins: theory and therapy. Nephrol Dial
Transplant 2004; 19: 1036-40.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
282
29. Moroni G, Longhi S, Quaglini S, et al. The long-term outcome of renal
transplantation of IgA nephropathy and the impact of recurrence on graft
survival. Nephrol Dial Transplant 2013; 28: 1305-14.
30. Cosyns JP, Couchoud C, Pouteil-Noble C, Squifflet JP, Pirson Y. Recurrence
of membranous nephropathy after renal transplantation: probability, outcome
and risk factors. Clin Nephrol 1998; 50: 144-53.
31. Moroni G, Gallelli B, Quaglini S, Banfi G, Montagnino G, Messa P. Long-term
outcome of renal transplantation in adults with focal segmental
glomerulosclerosis. Transpl Int 2010; 23: 208-16.
32. Stahl R, Hoxha E, Fechner K. PLA2R autoantibodies and recurrent
membranous nephropathy after transplantation. N Engl J Med 2010; 363: 496-
8.
33. Lachmann HJ, Gillmore JD. Renal amyloidosis. Br J Hosp Med (Lond) 2010;
71: 83-6.
34. Leung N, Griffin MD, Dispenzieri A, et al. Living donor kidney and autologous
stem cell transplantation for primary systemic amyloidosis (AL) with
predominant renal involvement. Am J Transplant 2005; 5: 1660-70.
35. Contreras G, Mattiazzi A, Guerra G, et al. Recurrence of lupus nephritis after
kidney transplantation. J Am Soc Nephrol 2010; 21: 1200-7.
36. Little MA, Hassan B, Jacques S, et al. Renal transplantation in systemic
vasculitis: when is it safe? Nephrol Dial Transplant 2009; 24: 3219-25.
37. Goceroglu A, Rahmattulla C, Berden AE, et al. The Dutch Transplantation in
Vasculitis (DUTRAVAS) Study: outcome of renal transplantation in
antineutrophil cytoplasmic antibody-associated glomerulonephritis.
Transplantation 2016; 100: 916-24.
38. Netzer KO, Merkel F, Weber M. Goodpasture syndrome and end-stage renal
failure--to transplant or not to transplant? Nephrol Dial Transplant 1998; 13:
1346-8.
39. Kluth DC, Rees AJ. Anti-glomerular basement membrane disease. J Am Soc
Nephrol 1999; 10: 2446-53.
40. Browne G, Brown PA, Tomson CR, et al. Retransplantation in Alport post-
transplant anti-GBM disease. Kidney Int 2004; 65: 675-81.
41. Pickering MC, D'Agati VD, Nester CM, et al. C3 glomerulopathy: consensus
report. Kidney Int 2013; 84: 1079-89.
42. Braun MC, Stablein DM, Hamiwka LA, Bell L, Bartosh SM, Strife CF.
Recurrence of membranoproliferative glomerulonephritis type II in renal
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
283
allografts: The North American Pediatric Renal Transplant Cooperative Study
experience. J Am Soc Nephrol 2005; 16: 2225-33.
43. Little MA, Dupont P, Campbell E, Dorman A, Walshe JJ. Severity of primary
MPGN, rather than MPGN type, determines renal survival and post-
transplantation recurrence risk. Kidney Int 2006; 69: 504-11.
44. Barbour S, Gill JS. Advances in the understanding of complement mediated
glomerular disease: implications for recurrence in the transplant setting. Am J
Transplant 2015; 15: 312-9.
45. Cochat P, Hulton SA, Acquaviva C, et al. Primary hyperoxaluria Type 1:
indications for screening and guidance for diagnosis and treatment. Nephrol
Dial Transplant 2012; 27: 1729-36.
46. Brinkert F, Ganschow R, Helmke K, et al. Transplantation procedures in
children with primary hyperoxaluria type 1: outcome and longitudinal growth.
Transplantation 2009; 87: 1415-21.
47. Hoppe B, Latta K, von Schnakenburg C, Kemper MJ. Primary hyperoxaluria -
the German experience. Am J Nephrol 2005; 25: 276-81.
48. Kemper MJ. The role of preemptive liver transplantation in primary
hyperoxaluria type 1. Urol Res 2005; 33: 376-9.
49. Scheinman JI. Liver transplantation in oxalosis prior to advanced chronic kidney
disease. Pediatr Nephrol 2010; 25: 2217-22.
50. Lorenz EC, Lieske JC, Seide BM, et al. Sustained pyridoxine response in
primary hyperoxaluria type 1 recipients of kidney alone transplant. Am J
Transplant 2014; 14: 1433-8.
51. Kemper MJ, Conrad S, Muller-Wiefel DE. Primary hyperoxaluria type 2. Eur J
Pediatr 1997; 156: 509-12.
52. Gahl WA, Balog JZ, Kleta R. Nephropathic cystinosis in adults: natural history
and effects of oral cysteamine therapy. Ann Intern Med 2007; 147: 242-50.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
284
13 LIVING DONOR KIDNEY TRANSPLANTATION IN CHILDREN
Recommendations
Pre-emptive living related renal transplantation is the gold standard
therapy for children with end-stage renal disease. (2C)
The aim should be for children to receive a renal transplant from a
blood group compatible well-matched donor, although ABO and/or
HLA incompatible renal transplantation is feasible in children. (2C)
Every effort should be made to minimise HLA mismatches (especially
with common antigens) to reduce the risk of future sensitisation. (2D)
All children with stage 4 and 5 chronic kidney disease should be
assessed by a multi-disciplinary team, including a paediatric
nephrologist, transplant surgeon, anaesthetist and urologist (where
appropriate) prior to renal transplantation. (Not graded)
In general, children who are ≥10 kg in weight are suitable to receive a
kidney from an adult living donor. (2C)
13.1 Introduction
Pre-emptive living related renal transplantation is the gold standard therapy for
children with end-stage renal disease (ESRD) (1). The aim should be for children to
receive a blood group compatible well-matched donor minimising HLA mismatches
(to reduce the risk of future sensitisations), although ABO and/or HLA incompatible
renal transplantation is feasible in children (2-6). All children with Stage 4 and 5
chronic kidney disease (CKD) should be assessed by a multi-disciplinary team,
including a paediatric nephrologist, transplant surgeon, anaesthetist and urologist
(where appropriate) prior to transplantation.
When transplanting children from living donors, there are some specific issues that
require consideration. This Chapter highlights some of the key areas that warrant
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
285
special mention, primarily in the context of donor selection, recipient considerations,
the transplant operation, and peri-operative management.
13.2 Donor Selection
Parents are the usual source of living donor kidneys for children. However, any
suitable adult may be considered as a potential donor, including unrelated and
altruistic donors, who may come forward from the UK Living Kidney Sharing Scheme
(UKLKSS) (2).
The following issues require particular consideration in children:
HLA mismatching
As children are likely to require re-transplantation during their lifetime, every effort
should be made to minimise HLA mismatches (especially with common antigens) to
reduce the risk of future sensitisation (see Chapter 7) (3). One parent may
fortuitously be better than a one haplotype match, or may mismatch on less common
antigens and therefore be the preferred donor. The involvement of an expert in
histocompatibility is critical in advising upon such decisions.
ABO incompatible transplantation
This should be considered when an ABO compatible transplant is not available,
including after consideration of UKLKSS. Younger children tend to have lower
antibody titres and there may be reduced risk, although ABO incompatible
transplantation should only be performed in centres with appropriate support for the
additional treatment required (4,5).
HLA incompatible transplantation
This should be considered when a highly sensitised patient has not been able to
receive a transplant (usually retransplant as highly sensitised from previous
transplant) via a deceased donor, living donor or via the UKLKSS. However, it
should only be performed in centres with appropriate support for the additional
treatment required (6).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
286
Immunisations and infection
Children are less likely to have been exposed to infectious agents and, where
possible, should be immunised before transplantation to reduce the subsequent
infection risk (7). This risk may be reduced by considering the use of less
immunosuppression for children who receive a well-matched kidney.
Special note should be made that many children are EBV naïve at the time of
transplantation, with no currently available vaccination, whereas most adult donors
are EBV positive. When available, the use of an EBV negative kidney donor should
be considered to reduce the risk of post-transplant lymphoproliferative disorder.
Social aspects
Choosing a donor must include assessment of the psychosocial aspects of the
family. It should be noted that parental donors may be cared for in a different hospital
from the recipient and clear plans should be made for supporting the donor, the
recipient, and other family members during the post-operative period.
13.3 Recipient Considerations
The commonest causes of ESRD in children are congenital anomalies of the kidney
and urinary tract, with renal dysplasia and/or reflux and/or obstructive uropathy in
over half of cases; obstructive uropathy accounts for 18% of cases (8). All children
should be seen by a paediatric urologist with appropriate urological investigation
(including flow studies and video-urodynamics) before living donor transplantation.
The most appropriate timing of any urinary tract reconstructive surgery should be
discussed between the transplant surgeon and paediatric urologist (9).
Glomerular disease accounts for 10% of children with ESRD (8). This group includes
a number of conditions that may recur after the transplant. Specific advice for these
conditions is detailed in Chapter 12. In children, the most common of these is
primary FSGS. Pre-transplant genetic studies may identify those at risk of disease
recurrence in the transplant and provide additional information to inform the
selection and consent process of potential living donors (10).
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
287
In children, particularly those requiring dialysis in infancy, there is a risk of
thrombosis of major intra-abdominal vessels and this requires careful evaluation
before surgery (11).
13.4 Surgery
In general, children who are ≥10 kg in weight (and occasionally even less) are
suitable to receive a kidney from an adult living donor, and this may be retrieved by
laparoscopic surgery (12,13). In small children, the kidney is usually placed in the
right side of the abdomen. The intra-peritoneal approach allows access to the mid-
aorta and inferior vena cava (IVC) for attachment of the donor renal vessels. Some
transplant surgeons prefer the extra-peritoneal approach to the great vessels. This
decision is usually dictated by the size of the recipient but there are other factors
that may influence this, including the presence of a thrombosed IVC or other
anatomical abnormalities (14).
In children, standard abdominal closure following transplantation onto the iliac
vessels (or onto the aorta and IVC in those closer to the minimum weight) may
compromise graft perfusion. On table Duplex scanning is valuable in assessing
organ perfusion after wound closure (15). In the presence of high intra-abdominal
compartment pressure compromising renal perfusion, delayed closure or a porcine
dermal collagen graft inserted as a patch closure of the abdominal muscle may be
considered (16).
The implantation of an adult kidney into a paediatric recipient requires close
cooperation between the paediatric nephrology, transplant surgical and anaesthetic
teams with intensive care involvement in smaller and/or ventilated children (17).
Meticulous attention needs to be paid to the child’s intravascular volume status.
When the aortic and inferior vena cava clamps are released, the transplanted organ
and lower extremities fill with blood, potentially resulting in severe hypovolaemia
unless adequate volume loading has taken place. Washout of the organ
preservation fluid into the child’s circulation may reduce core temperature and
produce severe hyperkalaemia. Careful monitoring and replacement of ongoing fluid
loss is required, remembering that the urine output from both the native and donor
kidney may be significant. The surgical and anaesthetic team should note a target

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
288
blood pressure for adequate renal perfusion during the surgical procedure which
should guide the post-operative management.
In the early post-operative phase, particular attention should be paid to fluid and
electrolyte balance because of the large volumes of urine that can be passed, and
these should be replaced with regular monitoring of renal function, urine and plasma
electrolytes and blood sugar levels. Central venous pressure (CVP) monitoring is
mandatory and the CVP should be maintained at 6-10 mmHg in the spontaneously
breathing patient, with intravenous normal saline or by the administration of an
alternative colloid to correct hypovolaemia. Elective ventilation may be considered
in young children for the first 24 to 48 hours after transplantation to allow optimal
control of fluids and blood pressure over this critical period.
Where intra-peritoneal surgery has taken place, a post-operative ileus may develop
and the child may not be able to start feeds or enteral medication. Rarely, careful
consideration should be given to administering immunosuppressive agents via the
intravenous route where it is possible and safe to do so. The risk of vascular
thrombosis is greater in this group than in larger/adult recipients and the use of anti-
platelet therapy may be appropriate (11).
It may be necessary to perform the donor and recipient procedures in separate
hospitals and, provided that the kidney is transported safely and efficiently between
the two centres to minimise the cold ischaemia time, there is no impact on the
incidence of primary graft function. Consideration should be given to the
geographical separation of the donor and recipient during the post-operative period
and the emotional impact that this may have on the donor, recipient and carers.
Provision should be made using webcam technology (such as FaceTime or Skype),
to facilitate contact between the donor, child and their carers.
References
1. Murray P, Pankhurst L, Marks SD. Are we performing enough pre-emptive
paediatric renal transplants? A national and single centre study. Pediatr Nephrol
2015; 30: 1708.

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
289
2. Mumford L, Marks SD, Ahmad N, Maxwell H, Tizard J. UK paediatric renal
transplantation: a review of changing practice and improved outcomes. Pediatr
Nephrol 2012; 27: 1807.
3. Marks SD, Hudson A, Pankhurst L, Fuggle S. The effect of HLA mismatching on
deceased and living donor renal allograft outcomes in paediatric recipients in the
United Kingdom. Pediatr Transplant 2013; 17 (Suppl 1): 60.
4. Stojanovic J, Mamode N, Adamusiak A, et al. Outcomes of ABO incompatible
kidney transplantation in children. Pediatr Nephrol 2015; 30: 1558.
5. Mamode N, Marks SD. Maximising living donation with paediatric blood group
incompatible renal transplantation. Ped Nephrol 2013; 28: 1037-40.
6. Marks SD, Adamusiak A, Stojanovic J, et al. Successful paediatric HLA
incompatible renal transplantation. Pediatr Nephrol 2015; 30: 1719.
7. Mencarelli F, Marks SD. Non-viral infections in children after renal
transplantation. Ped Nephrol 2012; 27: 1465-76.
8. Hamilton AJ, Braddon F, Casula A, et al. Demography of patients receiving renal
replacement therapy in paediatric centres in the UK in 2014. UK Renal Registry
18
th
Annual Report 2015; 4; 1-12. Accessed 19 Jan 2016:
https://www.renalreg.org/wp-content/uploads/2015/12/Chapter-04_v2.pdf
9. Taghizadeh AK, Desai D, Ledermann SE, et al. Renal transplant or bladder
augmentation first ? A comparison of complications and outcomes in children.
BJU Int 2007; 100: 1365-70.
10. McCarthy HJ, Bierzynska A, Wherlock M, et al on behalf of RADAR, the UK
SRNS Study Group. Simultaneous sequencing of 24 genes associated with
steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol 2013; 8: 637-8.
11. Al Midani A, Koffman G, Taylor J, Marks SD. Extraperitoneal transplantation. A
safe approach with a low surgical complication rate for transplanting children
under 21 kg: a single centre study. Pediatr Nephrol 2007; 22: 1478.
12. Chandak P, Sivaprakasam R, Stojanovic J, et al. Is there a difference in patient
and graft survival in children weighing <20 kg versus those weighing >20 kg at
time of renal transplantation? Pediatr Transplant 2015; 19 (S1): 144.
13. Chandak P, Kessaris N, Durkan A, et al. Is laparoscopic donation safe for
paediatric recipients? A study of 85 paediatric recipients comparing open and
laparoscopic donor nephrectomy. Nephrol Dial Transplant 2012; 27: 845-9.
14. Chandak P, Turner S, Callaghan C, et al. Successful renal transplantation in
complex small paediatric recipients with vascular anomalies. Pediatr Transplant
2015; 19 (S1): 140.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
290
15. Wiebe S, Kellenberger CJ, Khoury A, Miller SF. Early Doppler changes in a renal
transplant patient secondary to abdominal compartment syndrome. Pediatr
Radiol 2004; 34: 432-4.
16. Pentlow A, Smart NJ, Richards SK, Inward CD, Morgan JD. The use of porcine
dermal collagen implants in assisting abdominal wall closure of pediatric renal
transplant recipients with donor size discrepancy. Pediatr Transplant 2008; 12:
20-3.
17. Goh C, Hume-Smith H, Marks SD. What is the optimal perioperative blood
pressure and fluid management of paediatric renal transplant recipients? Pediatr
Nephrol 2015; 30: 1720.
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
291
14 APPENDIX
14.1 Conflicts of Interest
The authors make the following statements in relation to potential conflict of interest
related to this guideline:
Dr Peter Andrews None
Dr Richard Baker None
Prof Simon Ball Travel support from Astellas. Research support and
honorarium from Oxford Immunotec
Dr Kate Bramham None
Mr Tim Brown No details available
Ms Lisa Burnapp Advisory board membership for Chiesi, medical
advisor to the ‘Gift of Life’ donor information booklet
sponsored by Astellas and Sandoz
Prof Jamie Cavenagh No details available
Mr Marc Clancy Research grants from Astellas. Advisory board
Sandoz. Speaker fees from Astellas and Sandoz.
Educational meeting sponsorship from Astellas and
Sanofi. Research collaboration Cytori
Dr Aisling Courtney None
Dr Sam Dutta None
Dr Robert Elias Support to attend conferences from Janssen and
funding for a shared decision making network from the
Association of Renal Industries
Dr A Fenton None
Prof Susan Fuggle Honoraria and support to attend conferences from
Astellas
Mr Keith Graetz None
Dr Siân Griffin None
Dr Brendan Healy None
Dr Rachel Hilton Research grants, honoraria and/or support to attend
conferences from Astellas, Genetech, Novartis,
Oxford Immunotec, and Roche
Dr Gareth Jones None
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
292
Prof Graham Lipkin None
Dr Adam Mclean Research funding from Astellas, invited delegate at
Astellas, Novartis-funded meetings
Prof Nizam Mamode Payment for consultancy work from Alexion
Pharmaceuticals, and unrestricted educational grants
from Astellas and Glycorex
Ms Hannah Maple Co-applicant on an NIHR study further investigating
the topic of altruistic donation
Dr Stephen Marks Principal investigator in randomised controlled trials
with Novartis and Astellas but no direct payments
Dr E Montgomery None
Dr P Nightingale None
Mr Jonathan Olsburgh None
Dr Michael Picton None
Dr Stephen Potts None
Dr Nicola Price None
Dr Richard Sandford None
Dr Alastair Santhouse Expenses (but not lecture fees) from Novartis and
the World Transplantation Congress
Prof Neil Sheerin None
Ms Lisa Silas None
Ms Karen Stevenson No details available
Dr Craig Taylor None
Dr Raj Thuraisingham None
Dr Nicholas Torpey None
Dr Caroline Wroe None
14.2 Search Strategies
Authors of this guideline have notified the following search strategies:
Dr Peter Andrews PubMed search, review of national guidelines and
NICE website, review of ODT and UNOS websites
Dr Richard Baker PubMed search, review of national and
international guidelines
BTS/RA Living Donor Kidney Transplantation Guidelines 2018
293
Prof Simon Ball Combinations of recurrent disease, transplant,
kidney, and renal alone or along with one of the
following: mesangiocapillary glomerulonephritis, C3
glomerulopathy, haemolytic uremic syndrome, HUS,
FSGS, focal segmental glomerulosclerosis,
Goodpasture’s disease, ANCA , systemic lupus
erythematosus, SLE , IgA nephropathy, IgA disease,
membranous nephropathy, diabetic nephropathy,
hyperoxaluria, oxalosis, cystinosis, Alport, inherited
nephropathy
Dr Kate Bramham None
Mr Tim Brown No details available
Ms Lisa Burnapp Search strategies for my sections are largely covered
by the general statements that include guideline
review but, specifically, also include direct on-line
search for specific policies, guidance and statistics
from national and global donation and transplantation
organisations and PubMed
Prof Jamie Cavenagh No details available
Mr Marc Clancy PubMed, NHSBT website and direct online searches
Dr Aisling Courtney PubMed, NHSBT website
Dr Sam Dutta PubMed
Dr Robert Elias We searched PubMed through to 01 September 2015,
using keywords "HIV", "transplant", "transplantation",
"consent", "informed consent", "confidentiality" and
"ethics". We also searched reference lists of review
articles, relevant studies, and clinical practice
guidelines. We considered all systematic reviews,
randomised controlled trials, observational cohort
studies, ethics reports and case reports looking at
people with HIV infection treated with kidney and/or
pancreas transplantation. Our search was limited to
articles in English and studies conducted in adult
humans. One study published in 2016 was added at
editorial review
Dr A Fenton Search strategy-Pub Med, references from related
articles, review of BTS, EBPG, KDIGO guidelines

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
294
Prof Susan Fuggle All relevant articles and review of national guidelines
Mr Keith Graetz Online, PubMed, NICE, OVID
Dr Siân Griffin A literature search was performed using PubMed to
identify the relevant evidence. Related guidelines
were also considered (Guidelines for Hepatitis E and
Solid Organ Transplantation, first edition, BTS 2017;
Guidance on the microbiological safety of organs,
tissues and cells used for transplantation, Advisory
Committee on the Safety of Blood. Tissues and
Organs (SaBTO) 2011 and KDIGO Clinical Practice
Guideline on the Evaluation and Follow-Up Care of
Living Kidney Donors, draft 2015)
Dr Brendan Healy As per Dr Griffin
Dr Rachel Hilton I searched PubMed through to 01 November 2016
using the keywords "proteinuria", “albuminuria”,
“pyuria”, “living donor”, "kidney", “renal”, "transplant"
and "transplantation". I considered all systematic
reviews, randomised controlled trials, observational
cohort studies and case reports looking at living
kidney donors. I also searched reference lists of
review articles, relevant studies, and clinical practice
guidelines. Specifically, I looked at European Best
Practice guidelines (2013) on donor and recipient
evaluation and perioperative care and also the KDIGO
chronic kidney disease guidelines (2012). My search
was limited to articles in English and studies
conducted in humans
Dr Gareth Jones NHSBT website and BTS guidelines
Prof Graham Lipkin All relevant articles from PubMed and review of latest
versions of KDIGO+EBPG guidance
Dr Adam Mclean 1) PubMed searches using "Kidney Transplantation"
(Mesh Terms) AND "Living Donors" (Mesh Terms)
AND "Obesity" (Mesh Terms), and equivalent (All
Fields) search
2) PubMed searches using "Kidney Transplantation"
(Mesh Terms) AND "Living Donors" (Mesh Terms)

BTS/RA Living Donor Kidney Transplantation Guidelines 2018
295
AND "Risk Factors" (Mesh Terms) and equivalent
(All Fields) search
Prof Nizam Mamode PubMed search, along with NHSBT website
Ms Hannah Maple Search strategy adapted from PhD
Dr Stephen Marks Search strategies are covered by the general
statements that include guideline review but,
specifically, also include direct on-line search for
specific policies, guidance from national and
international transplantation organisations, and
PubMed
Dr E Montgomery Search strategy: PubMed, references from related
articles, review of BTS, EBPG, KDIGO guidelines
Dr P Nightingale Search strategy: PubMed, references from related
articles, review of BTS, EBPG, KDIGO guidelines
Mr Jonathan Olsburgh PubMed search using the search terms kidney
transplant, kidney donor, donor nephrectomy, ex-vivo
ureteroscopy, kidney stones
Prof Michael Peters Search strategy: PubMed, references from related
articles, review of BTS, EBPG, KDIGO guidelines
Dr Michael Picton PubMed search
Dr Stephen Potts I did not use a formal search strategy
Dr Nicola Price As per Dr Griffin
Dr Richard Sandford PubMed and NCBI website search, review of current
national guidelines, review of UNOS, UKGTN, BSHG
and genetics education websites as stated
Dr Alastair Santhouse As per Dr Elias
Prof Neil Sheerin Hypertension search on PubMed using terms
hypertension, living donor, kidney donation
Ms Lisa Silas As per Dr Elias
Ms Karen Stevenson No details available
Dr Craig Taylor All relevant articles and review of national guidelines.
Dr Raj Thuraisingham PubMed search
Dr Nicholas Torpey No details available
Dr Caroline Wroe PubMed, references from related articles, review of
BTS, EBPG, KDIGO guidelines

