
1
Primary Care Respiratory
Update
Asthma Guidelines in Practice:
a PCRS consensus
Asthma Guidelines in Practice is a PCRS consensus-based article to provide clarity on aspects of
diagnosis, management and monitoring of asthma that are uncertain due to differences between
current national guidelines. The article has been written by Luke Daines (GP and Academic Clinical
Fellow, University of Edinburgh) in conjunction with GP colleagues Noel Baxter, Kevin Gruffydd Jones,
Steve Holmes, Duncan Keeley, nurse colleagues Val Gerrard and Carol Stonham and pharmacist
Deborah Leese. It is based on the recently published PCRS briefing paper (see https://www.pcrs-
uk.org/resource/btssign-british-asthma-guideline-update-july-2019).
Introduction
Asthma is a chronic respiratory condition affecting an estimated 5.4
million people in the UK.
1
Individuals with asthma suffer from wheeze,
shortness of breath, cough and chest tightness, limiting everyday
activities and fulfilment of roles at home and work.
2
In the UK, public sector spending for asthma exceeds £1.1 billion
each year, with the majority of costs (74%) arising from prescriptions
and the estimated 6.4 million primary care consultations that occur
each year.
3
Evidence-based management can maintain good day-
to-day control for most people with asthma and substantially reduce
the risk of asthma attacks.
2
However, knowing which evidence-based strategies to imple-
ment has been made confusing by the presence of multiple guide-
lines for asthma care. In the UK, the National Institute for Health and
Care Excellence (NICE) guideline (published 2017) concentrates on
diagnosis, monitoring and chronic management and incorporates
economic evaluation with interpretation from a multidisciplinary
guideline group.
4
The British Thoracic Society/Scottish Intercollegiate
Guideline Network (BTS/SIGN) guideline (updated 2019) covers all
aspects of asthma care and is led by a multidisciplinary clinical
group.
2
Whilst the evidence considered by the NICE and BTS/SIGN
guideline groups is broadly the same, the methodology used to pro-
duce the guidelines is different, and has resulted in different recom-
mendations.
5
Thankfully, following calls from PCRS (amongst others),
6
an agreement between BTS/SIGN and NICE has been reached,
meaning that future asthma guidelines will be jointly produced.
Asthma diagnosis
• Following a structured clinical assessment, weigh up the prob-
ability that an individual has asthma: use a monitored trial of
treatment if asthma is highly probable; conduct further inves-
tigations (spirometry, peak expiratory flow variability) if an
individual is at intermediate probability.
• Achieving an accurate diagnosis may take time and may
require the comparison of repeated measurements and clini-
cal assessments
• Objective evidence to support an asthma diagnosis should
be sought however likely the diagnosis appears to be.
• The basis for asthma diagnosis should be clearly documented
in medical records.
Asthma management
• Regular inhaled corticosteroid (ICS) is regarded as the foun-
dation of asthma pharmacological treatment.
• When prescribing ICS for children, the starting dose is usually
a ‘very low dose’ and the highest dose is classed as a
‘medium dose’.
• In line with the NICE recommendation, PCRS suggests a trial
of leukotriene receptor antagonists (LTRA) as the first line
add-on therapy to ICS with careful review.
• Maintenance and Reliever Therapy (MART) may be consid-
ered in adults who have a history of asthma attacks despite
medium dose ICS or ICS/LABA (long-acting beta-agonist).
Asthma monitoring
• A regular review of individuals with asthma provides the
chance to assess current symptom control and consider the
future risk of an asthma attack.
• Record asthma control, a measure of lung function, asthma
attacks, oral corticosteroids, absence from work/school and
smoking status at each review.
• Identify the future risk of an asthma attack in all individuals
with asthma: previous asthma attack, poor asthma control
and short-acting beta agonist (SABA) over-reliance increase
the risk substantially.
• Recognise individuals with severe asthma and refer for
specialist review
Key points
Having two UK asthma guidelines has led to conflicting advice and is confusing for clinicians. This article aims to bring
clarity on a number of issues and has been updated in line with the recently released BTS/SIGN 2019 guideline.
OCT+NOV 2019 issue.qxp_Layout 1 18/12/2019 12:30 Page 36
Primary Care Respiratory
Update
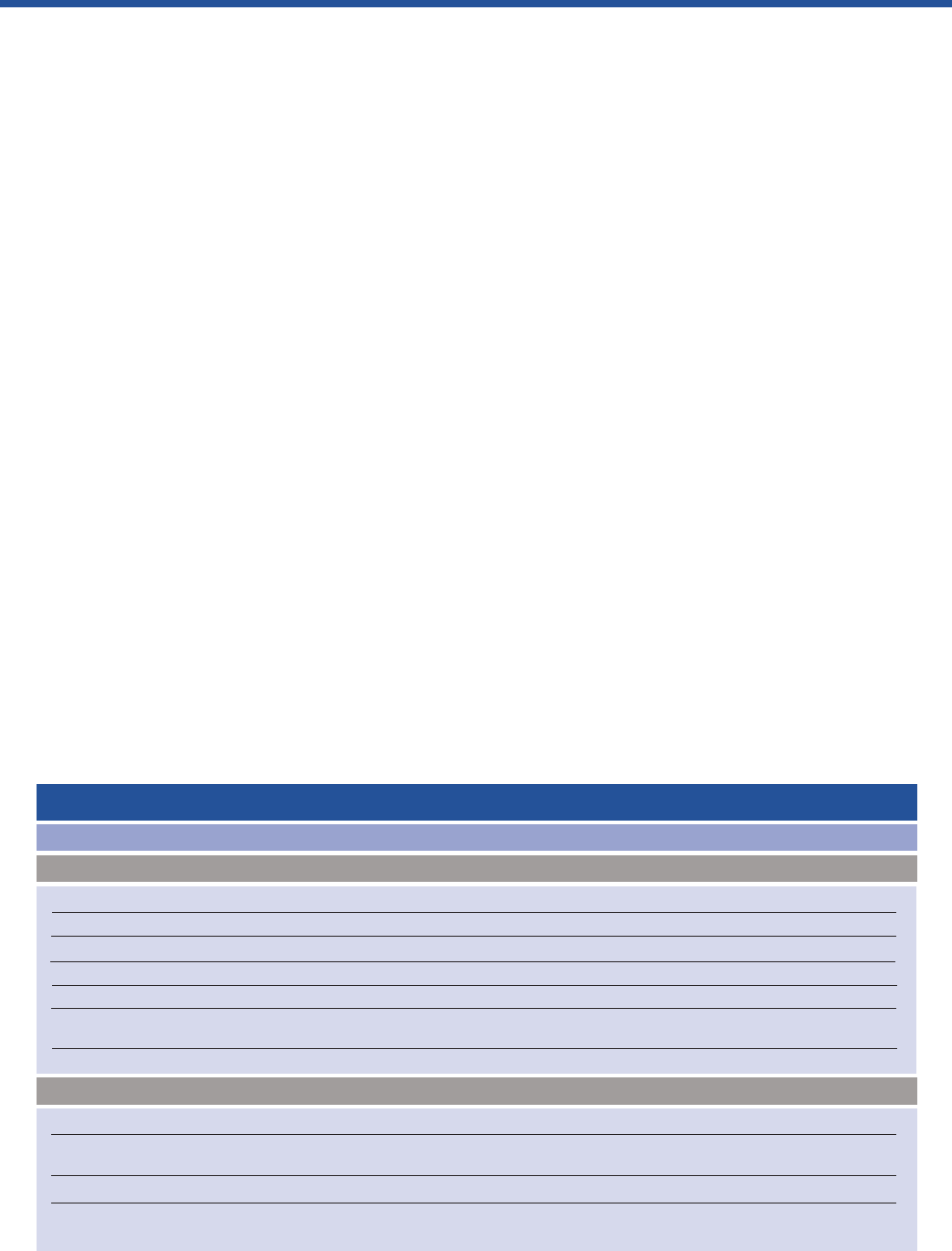
Clinical clue
Predominant cough with no lung function abnormality
Prominent dizziness, light-headedness or peripheral tingling
Recurrent severe ‘asthma attacks’ without objective evidence to confirm
Predominant nasal symptoms without lung function abnormality
Postural and food-related symptoms, predominant cough
Orthopnoea, paroxysmal nocturnal dyspnoea, peripheral oedema,
pre-existing cardiac disease
Crackles on auscultation
Significant smoking history (ie, over 30 pack-years), age of onset over 35 years
Chronic productive cough in the absence of wheeze or breathlessness
New onset in smoker, systemic symptoms, weight loss, haemoptysis
*May also be associated with non-obstructive spirometry.
Table 1:
Clinical features to suggest an alternative diagnosis to asthma in adults
Possible diagnosis
Chronic cough syndromes; pertussis
Dysfunctional breathing
Vocal cord dysfunction
Rhinitis
Gastro-oesophageal reflux disease
Cardiac failure
Pulmonary fibrosis
COPD
Bronchiectasis*, inhaled foreign body*, obliterative
bronchiolitis, large airway stenosis
Lung cancer*, sarcoidosis*
No airflow obstruction
With airflow obstruction
Rationale for PCRS consensus
We look forward to the joint guideline but, in the meantime, we want
to support primary care clinicians who are facing uncertainty due to
conflicting recommendations between the national guidelines. This
article, developed by PCRS members, aims to provide a clear, con-
cise and pragmatic view on the diagnosis, management and moni-
toring of asthma in primary care. It does not attempt to reproduce all
the details contained in each guideline, but instead focuses on the
areas that vary substantially between NICE and BTS/SIGN versions,
offering a workable solution.
Recommendations
Asthma diagnosis
Achieving a clear consensus for the best diagnostic strategy for
asthma is a particular challenge as, on top of economic and imple-
mentation considerations,
4
the definition of asthma is also evolving.
Traditionally a diagnosis of asthma was based on symptoms and
demonstration of variable obstructive airflow on lung function
testing.
2,7
Yet, more recent definitions of asthma include airway
inflammation and airway hyper-responsiveness to incorporate the
subtypes of asthma identified through recent research on genetics
and pathophysiological mechanisms.
2
This changing understanding
of asthma has delivered new ways in which to test and treat for
asthma subtypes and may in the future lead to asthma being ‘de-
constructed’ into distinct ‘treatable traits’.
7,8
Until then, a clear prag-
matic way forward is needed to guide clinicians in non-specialist
settings, where most asthma cases are diagnosed.
8
There is no definitive gold standard test which can categorically
confirm or refute the diagnosis of asthma. Therefore, the diagnosis
of asthma is made clinically following a structured clinical assess-
ment; a careful integration of evidence from a wide variety of
sources.
2,4
Key components of a structured clinical assessment in-
clude a detailed history, examination, review of the patient’s clinical
records and previously completed investigation results (for example,
peak expiratory flow, spirometry, blood eosinophils from a full blood
count).
When taking a history, ask about wheeze, shortness of breath,
cough and chest tightness, the most suggestive symptoms of
asthma.
2,4
Symptoms usually occur in episodes with no (or minimal)
symptoms between episodes.
2
Combinations of symptoms (partic-
ularly wheeze, cough and shortness of breath) occurring in episodes
are more useful for identifying asthma than individual symptoms, par-
ticularly in children.
9
Ask about variability in symptoms through the
day and between seasons. Clarify any triggers that provoke or
worsen symptoms
4
and, in adults, check specifically for work-related
factors. Remember to enquire about personal or family history of
other atopic conditions such as allergic rhinitis or eczema.
4
Informa-
tion from the patient clinical record, including previous respiratory
illnesses, treatments and responses and previous examination
findings (particularly wheeze heard on chest auscultation by a health
professional), can further build the clinical picture.
On auscultation of the chest, asthmatic wheeze tends to be end-
expiratory, scattered and polyphonic. Consider alternative diagnoses
if wheeze is never heard during symptomatic episodes (Table 1).
Remember that respiratory examination may well be normal in an
asymptomatic individual, so it is important not to exclude asthma
solely on examination findings.
4
In addition to a respiratory examina-
tion, check the throat for enlarged tonsils and look out for other signs
of atopic disease such as eczema or rhinitis.
Following a structured clinical assessment, the BTS/SIGN guide-
2
This table is reproduced from SIGN 158 (British guideline on the management of asthma) by kind permission of the Scottish Intercollegiate Guidelines Network
2
OCT+NOV 2019 issue.qxp_Layout 1 18/12/2019 12:30 Page 37

line recommends weighing up the probability that the individual has
asthma based on three categories: high, intermediate and low.
2
If a patient (whether adult or child) has all of the following typical
clinical features, they are considered to have a high probability of
asthma:
2
● Recurrent episodes of symptoms (‘attacks’)
● Wheeze confirmed by a healthcare professional
● A personal or family history of atopy
● A past record of variable airflow obstruction
● No features to suggest an alternative diagnosis (Table 1).
If there is any doubt, the diagnosis should be considered as inter-
mediate probability. Adults and children who have none of the typical
features of asthma or whose symptoms are suggestive of an alter-
native diagnosis have a low probability of asthma.
2
The probability of
asthma informs the next steps in the diagnostic work-up, as demon-
strated in Figure 1.
Even with a careful structured clinical assessment and diagnostic
work-up, the diagnosis of asthma can be challenging, particularly
due to the variable nature of symptoms and lung function over time
and the heterogeneity of presentation. Primary care is ideally placed
to collect, record and appraise the information required to make an
asthma diagnosis and provide continuity to allow repeated assess-
ments over time so that treatment response and natural variation can
be evaluated. Consequently, a diagnostic strategy based on repeated
clinical assessments, supported by objective clinical tests (including
peak expiratory flow monitoring) and sensitively using trials of initiating
and discontinuing therapy is recommended as a practical way
forward.
It is important to refer to specialist services in cases of doubt or
difficulty (Table 2).
Whilst investigating asthma, and until a diagnosis is confirmed,
use the code ‘suspected asthma’.
2,4
Once a diagnosis of asthma has
been made, record the basis for the decision in a single entry in the
person’s medical records, alongside the coded diagnostic entry. The
diagnosis of asthma should ideally be revisited and checked regularly
– especially when you first take over the care of a patient thought to
3
Primary Care Respiratory
Update
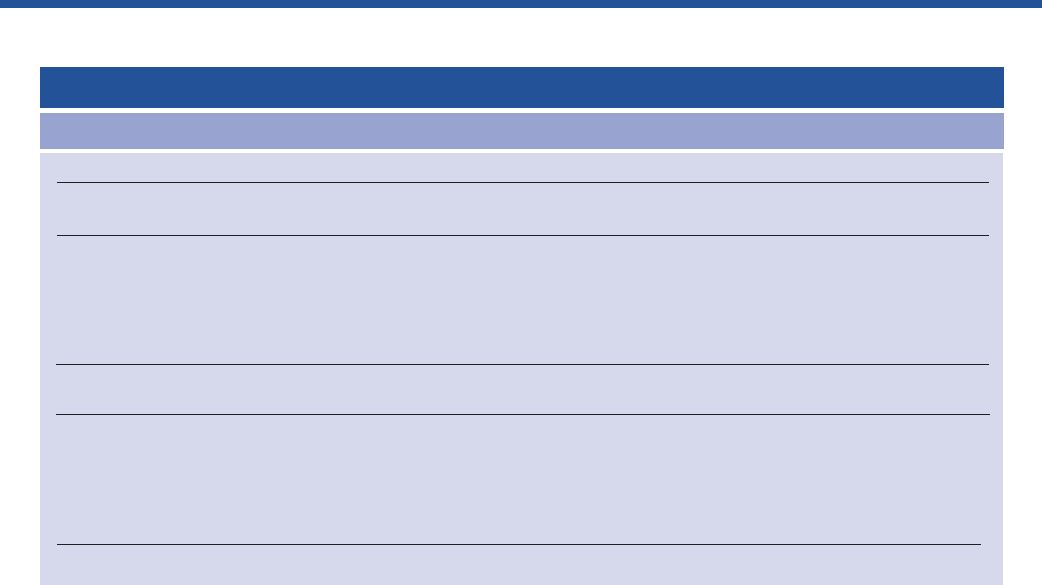
Figure 1 - Diagnostic algorithm for individuals presenting with symptoms suggestive of asthma
†
In children under 5 years and others unable to undertake spirometry in whom there is a high or intermediate probability of asthma, the options are
monitored initiation of treatment or watchful waiting according to the assessed probability of asthma
Presentation with respiratory symptoms: wheeze, cough, breathlessness, chest tightness
†
Adjust maintenance
dose. Provide self-
management. Arrange
on-going review
High probability of
asthma
Code as:
suspected asthma
Initiation of treatment
Good response
Other diagnosis
confirmed
Intermediate probability of asthma
Test for airway obstruction
spirometry + bronchodilator reversibility
Options for investigations are:
Test for variability
●
Reversibility
●
PEF charting
●
Challenge tests
Test for eosinophilic
inflammation or atopy:
●
FeNO
●
Blood eosinophils
●
Skin-prick test, IgE
Low probability of
asthma
Assess response
objectively
(lung function/validated
symptom score)
Poor
response
Investigate/treat for
other more likely
diagnosis
Other diagnosis
unlikely
Structured clinical assessment (from history and examination of previous medical records) look for:
●
Recurrent episodes of symptoms
●
Symptom variability
●
Absence of symptoms of alternative diagnosis
●
Recorded observation of wheeze
●
Personal history of atopy
●
Historical record of variable PEF or FEV
1
Poor
response
Suspected asthma:
Watchful waiting
(if asymptomatic) or
Commence treatment
assess response objec
tively
Good
response
Asthma
This figure is reproduced from SIGN 158 (British guideline on the management of asthma) by kind permission of the Scottish Intercollegiate Guidelines Network
2
OCT+NOV 2019 issue.qxp_Layout 1 18/12/2019 12:30 Page 38

4
Primary Care Respiratory
Update
have asthma. Good documentation is strongly recommended as the
variable nature of asthma can lead to individuals experiencing long
periods without symptoms, leading patients and clinicians to ques-
tion the original diagnosis.
10
Objective tests
Objective tests should be done in all patients old enough to perform
them, as part of an initial diagnostic assessment to support a confi-
dent diagnosis of asthma. Increasing the quality and availability of
objective testing across healthcare is an important policy priority.
Understanding that each diagnostic test available for asthma has
strengths and limitations is therefore valuable in order to use tests
most effectively to build up sufficient evidence so that a differential
diagnosis can be confirmed or refuted correctly.
Tests for demonstrating variability in airflow obstruction
A defining feature of asthma is variable airflow obstruction caused
by airway bronchoconstriction. Yet, demonstrating variable airflow
obstruction can be a challenge as airway physiology may be normal
when an individual with asthma is asymptomatic. This is reflected in
estimates for the negative predictive value of spirometry in adults and
children which varies between 18% and 54%,
2
indicating that more
than half of patients who have a negative result (non-obstructive
spirometry) will have asthma.
11
Therefore, relying on objective tests of airflow obstruction com-
pleted only at a single point of time risks missing asthma, particularly
if the patient is asymptomatic at the time of testing. Instead, testing
for variable airflow obstruction should be repeated over time.
In primary care, peak expiratory flow monitoring and spirometry
with bronchodilator reversibility testing are recommended mea-
sures to demonstrate variable airflow obstruction. When interpret-
ing spirometry, BTS/SIGN recommend the use of lower limit of
normal for FEV
1
/FVC ratio (instead of the fixed ratio of 70%) in
order to avoid the substantial under-diagnosis in children and over-
diagnosis of obstruction in older people.
2,5
Spirometry is a useful
diagnostic test in all patients with suspected asthma, yet if
resources are limited, prioritising those individuals who are consid-
ered intermediate probability is likely to be the best strategy.
Although sometimes undervalued, peak expiratory flow monitoring
can provide useful measurements. The value of peak expiratory
flow monitoring as an important initial test in the assessment of
asthma was discussed in the Spring 2017 edition of Primary Care
Respiratory Update (see https://pcrs-uk.org/peak-flow-and-mi-
crospirometry-support-diagnosis).
Tests for demonstrating eosinophilic inflammation
A positive fractional exhaled nitric oxide (FeNO) test indicates the
presence of eosinophilic inflammation, providing supporting (rather
than conclusive) evidence for an asthma diagnosis. A systematic re-
view of the accuracy of FeNO in diagnosing asthma in adults and
children reported a pooled sensitivity of 65% and specificity of 82%,
indicating that FeNO has a higher potential for ruling in – as opposed
to ruling out – the diagnosis of asthma.
12
In adults, a FeNO reading
of 40 ppb or more should be regarded as a positive test.
2,4
Accurate
Adults
Diagnosis unclear
Suspected occupational asthma (symptoms that improve when patient
is not at work, adult-onset asthma and workers in high-risk occupations)
Poor response to asthma treatment
Severe/life-threatening asthma attack
Prominent systemic features (myalgia, fever, weight loss)
Unexpected clinical findings (eg crackles, clubbing, cyanosis, cardiac
disease, monophonic wheeze or stridor)
Persistent non-variable breathlessness
Chronic sputum production
Unexplained restrictive spirometry
Chest X-ray shadowing
Marked blood eosinophilia
Table 2 Reasons for specialist referral
Children
Diagnosis unclear
Poor response to monitored initiation of asthma treatment
Severe/life-threatening asthma attack
Failure to thrive
Unexplained clinical findings (eg focal signs, abnormal
voice or cry, dysphagia, inspiratory stridor)
Symptoms present from birth or perinatal lung problem
Excessive vomiting or posseting
Severe upper respiratory tract infection
Persistent wet or productive cough
Family history of unusual chest disease
Nasal polyps
Referral for tests not available in primary care
‘Red flags’ and indicators of other diagnoses
Patient or parental anxiety or need for reassurance
This table is reproduced from SIGN 158 (British guideline on the management of asthma) by kind permission of the Scottish Intercollegiate Guidelines Network
2
OCT+NOV 2019 issue.qxp_Layout 1 18/12/2019 12:30 Page 39

interpretation of a FeNO result requires an understanding of the po-
tential confounding factors that may produce false positive and false
negative results (Box 1).
NICE (2017) recommendations for the role of FeNO in the diag-
nosis of asthma are different from those advocated by BTS/SIGN.
2,4
Given the limitations of FeNO, a central role in the diagnostic work-
up of all people suspected of asthma, as advocated by NICE, seems
over-emphasised and may lead to unintended consequences.
Currently, FeNO is not widely available in UK primary care so, if FeNO
is perceived as a required test, referrals to secondary care may
increase, adding to the workload in specialist settings and potentially
de-skilling clinicians in primary care. Cost may be a barrier for indi-
vidual practices adopting FeNO, as ongoing consumables are
required in addition to an initial investment. A future solution might
be for practices to pool resources and develop a locality-based
diagnostic service, as successfully implemented in the Netherlands
and currently being trialled in the UK.
4,15
Despite these concerns, there are clear benefits to be gained
from using FeNO, which could be realised if appropriately imple-
mented. For instance, if an individual has an intermediate probability
of asthma following a structured clinical assessment, a positive FeNO
test increases the probability of asthma, providing further supporting
evidence to confirm or refute a diagnosis. Therefore, in primary care,
PCRS recommend using FeNO as an optional investigation to test
for eosinophilic inflammation in individuals where diagnostic uncer-
tainty remains. Routine use of FeNO testing in adults and children is
not recommended except in specialist respiratory clinics. The
PCRS position statement on FeNO testing is available from
https://www.pcrs-uk.org/resource/feno-testing-asthma-diagnosis.
Diagnosis in children
Confirmation of variable airflow obstruction by objective demonstra-
tion of peak flow monitoring or spirometry with reversibility is desirable
in children old enough to perform these tests. However, the use of
spirometry is not well established in children in primary care and
additional training may be needed to ensure accurate results. If FeNO
is used in children aged 5–16 years, a result of 35 ppb or more is
regarded as a positive test.
2,4
In children under 5 years of age, a diagnosis of asthma is based
on establishing the probability of asthma after an initial structured
clinical assessment.
2
If the probability of asthma is high, a trial of
an inhaled corticosteroid (ICS) using a dosage of 400 μg/day
beclomethasone or equivalent may be considered.
2,16
If a child is
started on a trial of treatment, it should last for 6–8 weeks and be
stopped at the end of the trial.
2,16
If the child has had no response to
treatment and the medication has been taken, the diagnosis of
asthma is unlikely.
16
If symptoms improve with ICS but recur when
stopped, then settle again with reintroduction of treatment, a diag-
nosis of asthma can be made.
16
Where diagnostic doubt persists,
referral for specialist assessment should be considered (Table 2).
Asthma management
Management of asthma should be patient-centred, encouraging and
supporting self-management and making treatment decisions in
partnership with the individual. This should include promoting non-
pharmacological approaches including weight control, encouraging
physical activity and addressing tobacco dependency. Supported
self-management, which includes the provision of an asthma action
plan, improves individual asthma control whilst reducing visits to
unscheduled care.
17
ICS are regarded as the foundation of asthma pharmacological
treatment.
2,5
Therefore, a regular (low-dose) ICS with a short-acting
beta-agonist (SABA) as required is the recommended first-line main-
tenance treatment for adults. In children, once a diagnosis has been
made, the starting dose of ICS is ‘very low dose’ (200 μg/day
beclomethasone or equivalent). If the dose needs to be increased,
be aware that ‘medium dose’ (800 μg/day beclomethasone or equiv-
alent) represents a level of treatment to be used only if referring to
specialist care.
2
If asthma is well controlled there should be little or no need for
SABA.
2
Three or more doses of SABA per week may indicate poor
asthma control and a need to move up treatment. Over-reliance on
SABAs is well established as a risk factor for fatal asthma
18
(see
Monitoring section for further details), therefore anyone prescribed
more than one SABA a month should have their asthma urgently
assessed.
2
Prescribing inhalers by brand name and device ensures that
patients receive the inhaler that the prescriber intends for them.
Prescribing a generic inhaler or not specifying the device should be
avoided as it may result in a patient receiving an inhaler they have
not been taught to use. If prescribing a metered dose inhaler (MDI),
remember to issue with a spacer to increase the efficacy of drug
delivery.
A further consideration when prescribing inhalers is environmen-
tal impact. MDIs have a higher global warming potential than dry
powder inhalers (DPIs),
19
so if there is no obvious clinical reason to
5
Primary Care Respiratory
Update
Box 1 Factors that may confound the accuracy of
fractional exhaled nitric oxide (FeNO) in
making an asthma diagnosis
2,13,14
• Increased levels in men, tall people and those with a diet high
in nitrates (eg, spinach, broccoli)
• Increased levels in individuals with allergic rhinitis exposed
to an allergen (even without respiratory symptoms)
• Increased levels in those with rhinovirus infection (inconsis-
tent effect in those with asthma)
• Lower levels observed in children (N.B. accordingly a lower
reference range is used)
• Reduced levels in cigarette smokers
• Reduced levels by inhaled or oral steroids
OCT+NOV 2019 issue.qxp_Layout 1 18/12/2019 12:30 Page 40

6
Primary Care Respiratory
Update
choose between inhaler types, opt for the lower carbon footprint
DPIs. Remember, however, that any decisions about inhaler choice
should be made on an individual basis between clinicians and patients,
so PCRS warn against any ‘blanket switching’ from MDIs to DPIs.
Add-on therapies
The choice of initial add-on treatment to low-dose ICS remains a
contentious issue and, therefore, was one of the key questions ad-
dressed by the BTS/SIGN 2019 update.
2
To understand why the two
guidelines continue to offer different advice, remember that the NICE
multidisciplinary guideline group considers an economic evaluation
in addition to clinical evidence
4,5
whilst BTS/SIGN make recommen-
dations based purely on a critical appraisal of the literature.
2,5
Adding long-acting beta-agonists (LABA) to ICS alone improves
symptoms, lung function and decreases asthma attacks in adults
and children.
2
In comparison to leukotriene receptor antagonists
(LTRA), LABA are more effective in reducing the number of exacer-
bations,
20
leading BTS/SIGN to recommend LABA as first-line add-
on treatment in adults.
2
If prescribing, LABA should always be issued
in combination inhalers with ICS, reducing the risk of harm from using
LABA as monotherapy
21
and improving the likelihood of adherence
to an additional medication. In children, BTS/SIGN state there is
insufficient evidence to choose between LABA or LTRA as initial add-
on therapy.
2
NICE recommends LTRA as the first-line add-on therapy in
adults and children because the marginal superiority in efficacy of
LABA (noted in adults)
20
is outweighed by its greater cost.
4
As an oral
medication, LTRA may offer an advantage for some for whom an
inhaler is impractical. LTRA also offer treatment benefit for those with
allergic rhinitis.
PCRS supports the value-based approach
22
that NICE used, and
therefore recommend LTRA as the first-line add-on therapy to ICS.
Effectiveness and tolerability should be reviewed in 4–6 weeks. If
LTRA is found ineffective it should be withdrawn, as adding a LABA
on top of a LTRA removes any cost advantage. In children, the use
of a paediatric low-dose ICS with LTRA as first-line add-on treatment
is recommended. If this combination is ineffective, then switch the
LTRA for a LABA.
Ultimately, the decision to opt for LTRA or LABA as initial add-on
therapy should be made after discussion between the clinician and
patient and should take consideration of other factors including
patient preference, adherence (including the potential for additional
prescription costs), concomitant diseases (eg, rhinitis) and risk of ex-
acerbation. Furthermore, there is no need to change the medication
of patients who are already well controlled on ICS/LABA.
Single combination inhaler for maintenance and reliever therapy
Particular types of ICS/LABA combination inhaler may be used to
provide both a regular daily dose and relief from symptoms when
needed, so-called Maintenance and Reliever Therapy (MART). In
comparison with the more traditional fixed daily dosing regimens,
MART may have advantages for some individuals as only one inhaler
is needed and every inhalation contains ICS, reducing the risk of
undertreated airway inflammation.
There are, however, important points to consider with MART.
Firstly, only those inhalers which contain formoterol as the LABA are
suitable for MART, as formoterol has a rapid onset of action. Sec-
ondly, the evidence to support MART is based on trials done on
adults, and whilst there was a reduction in asthma attacks (compared
with standard ICS/LABA treatment), there was no difference to quality
of life, asthma control, lung function or asthma medication use.
23
Thirdly, with limited evidence
23
and no licensed product for under-
12-year-olds, MART is not recommended in children.
In summary, MART may be considered as an option in adults
who have a history of asthma attacks despite medium-dose ICS or
ICS/LABA.
2
To become more widely used, there is a need for better
training and greater clarity on self-management instructions for
MART.
Asthma monitoring
A regular review of individuals with asthma provides the chance to
assess current symptom control and consider the future risk of an
asthma attack. Primary care is best placed to monitor asthma by
staff who are trained, competent and confident, and should be com-
pleted regularly (at least annually in stable patients with a definite
diagnosis) as a pre-planned appointment but also opportunistically.
A more frequent review may be necessary when a diagnosis is first
made, or for those with poor asthma control. At each review, asthma
control, lung function, asthma attacks, oral corticosteroids, absence
from work or school and smoking status should be recorded in the
notes. In children, growth (height and weight centile) should also be
measured.
2
Monitoring asthma symptom control
Asthma control should be assessed using the validated asthma con-
trol questionnaire or asthma control test and are recommended over
the Royal College of Physician’s three questions which has greater
value as a screening test for poor control.
2
Peak flow or spirometry
(or both) should be used to assess lung function. If asthma control is
sub-optimal, check for and address the common causes of poor
asthma control listed in Box 2. For more information on supporting
smokers to quit (be that individuals with asthma or parents/carers of
children with asthma), see the PCRS article on tobacco dependency
(https://www.pcrs-uk.org/sites/pcrs-uk.org/files/TobaccoDepend-
Flier_FINAL.pdf).
Currently there is insufficient evidence from real-life primary care
to support using FeNO routinely to monitor asthma control. However,
it may be an option to support asthma management in people who
are symptomatic despite using ICS as it can help to identify poor
adherence.
OCT+NOV 2019 issue.qxp_Layout 1 18/12/2019 12:30 Page 41

7
Primary Care Respiratory
Update
As well as during a routine review, inhaler technique should be
observed and errors in technique corrected at every opportunity
when there is a deterioration in asthma control, when the inhaler is
changed and if the patient requests a check.
Predicting future risk of asthma attacks
In line with the delivery of personalised asthma care, identifying the
future risk of an asthma attack for children and adults should be
incorporated into any asthma review. In children aged 5–12 years
(Table 3), the factors associated with a greatly increased risk of
asthma attack are persistent asthma symptoms and past history of
asthma attack.
24
School-aged children are at moderately increased
risk if they are over-reliant on SABA, have a co-existing atopic dis-
ease, are vitamin D deficient or from a low-income family.
24
Additional
factors known to slightly increase the risk of asthma attack are
exposure to tobacco smoke, obesity, low parental education and
younger aged children (ie, closer to 5 than 12 years).
24
In adults (Table 4), having a history of previous asthma attacks
is associated with a greatly increased risk of asthma attack.
25
Poor
asthma control and SABA over-reliance are both associated with
a moderately increased risk of an asthma attack.
26
Smoking,
obesity, depression, older age, reduced lung function and female
gender are all associated with a slightly increased risk of a future
asthma attack.
Understanding the factors associated with an increased risk of
attack can help clinicians to know what to enquire about in consul-
tation, but should also lead to proactive care by identifying at-risk
individuals who do not consult regularly (for instance, by searching
the practice record to identify those individuals over-using SABAs).
At-risk individuals should receive targeted care by increasing the
frequency of review, optimising medication choice and adherence
and reviewing self-management strategies. For ideas and tools to
facilitate action on SABA over-reliance, see the work of the Asthma
Right Care Project (https://www.pcrs-uk.org/asthma-right-care).
Severe asthma
When monitoring individuals and weighing up future risk of attack,
have in mind the possibility of severe asthma as such patients require
referral for specialist review. BTS/SIGN define severe asthma as more
than two asthma attacks a year or persistent symptoms with SABA
use more than twice a week despite adequate adherence (>80%)
and therapies beyond initial or add-on controller treatments (ie,
‘specialist therapies’).
2
Severe asthma is increasingly regarded as a
distinct disease entity requiring specialist treatment and is the
subject of a PCRS pragmatic guide for clinicians (available at
Box 2 Common causes of poor asthma control
• Incorrect diagnosis, or co-morbidity that has been missed
• Lack of medication adherence
• Current treatment is unsuitable
• Under-use of ICS or overuse of SABAs
• Inappropriate inhaler technique
• Failure to use a spacer with ICS delivered by a metered dose
inhaler
• Smoking (active or passive) – ideally use a carbon monoxide
meter to monitor smoking
• Exposure to occupational triggers
• Seasonal or environmental factors
• Psychosocial reasons, including ideas and concerns about
asthma/treatment
Level of increased risk
Greatly increased risk
Moderately increased risk
Slightly increased risk
Unclear (evidence limited or equivocal)
Table 3 Factors associated with increased risk of future asthma attacks in school-aged children
Children
• History of previous asthma attacks
• Persistent asthma symptoms
• Suboptimal drug regimen (the ratio of the number of prescriptions for controller
medication to total number of prescriptions for asthma medication <0.5)
• Comorbid atopic/allergic disease
• Low-income family
• Vitamin D deficiency
• Younger age
• Exposure to environmental tobacco smoke
• Obesity
• Low parental education
• Reduced lung function
• Raised FeNO at routine interviews
• Positive skin prick tests
• History of allergen exposure
This table is reproduced from SIGN 158 (British guideline on the management of asthma) by kind permission of the Scottish Intercollegiate Guidelines Network
2
OCT+NOV 2019 issue.qxp_Layout 1 18/12/2019 12:30 Page 42
8
Primary Care Respiratory
Update
https://www.pcrs-uk.org/resource/triggers-referral-poorly-controlled-
and-severe-asthma).
Conclusions
We look forward to the return of a single asthma guideline developed
through the collaboration of NICE and BTS/SIGN. In the meantime,
we have proposed clear guidance to address particular concerns
over conflicting aspects of asthma diagnosis, management and
monitoring that will support non-specialists to continue providing high
quality asthma care.
References
1. Asthma UK. Asthma facts and statistics. Available from: https://www.
asthma.org.uk/about/media/facts-and-statistics/ (accessed August 2019).
2. Scottish Intercollegiate Guidelines Network (SIGN). British guideline on the manage-
ment of asthma. Edinburgh: SIGN; 2019. (SIGN publication no. 158). [cited
17/12/2019]. Available from URL: http://www.sign.ac.uk
3. Mukherjee M, Stoddart A, Gupta RP, et al. The epidemiology, healthcare and
societal burden and costs of asthma in the UK and its member nations: analyses
of standalone and linked national databases. BMC Med 2016;14(1):113.
https://doi.org/10.1186/s12916-016-0657-8
4. National Institute for Health and Care Excellence (NICE). Asthma: Diagnosis, Moni-
toring and Chronic Asthma Management. [NG80]. 2017. https://www.nice.org.uk/
guidance/ng80
5. White J, Paton JY, Niven R, Pinnock H. Guidelines for the diagnosis and manage-
ment of asthma: a look at the key differences between BTS/SIGN and NICE. Thorax
2018 [Epub ahead of print]. https://doi.org/10.1136/thoraxjnl-2017-211189
6. Keeley D, Baxter N. Conflicting asthma guidelines cause confusion in primary care.
BMJ 2018;360:k29. https://doi.org/10.1136/bmj.k29
7. Agusti A, Bel E, Thomas M, et al. Treatable traits: toward precision medicine of
chronic airway diseases. Eur Respir J 2016;47(2):410–19. https://doi.org/
10.1183/13993003.01359-2015
8. Pavord ID, Beasley R, Agusti A, et al. After asthma: redefining airways diseases.
Lancet 2018;391:350–400. https://doi.org/10.1016/ S0140-6736(17)30879-6
9. Yu IT, Wong TW, Li W. Using child reported respiratory symptoms to diagnose
asthma in the community. Arch Dis Child 2004;89(6):544–8. https://doi.org/
10.1136/adc.2003.033688
10. Strachan DP, Butland BK, Anderson HR. Incidence and prognosis of asthma and
wheezing illness from early childhood to age 33 in a national British cohort. BMJ
1996;312(7040):1195–9. https://doi.org/10.1136/bmj.312.7040.1195
11. Schneider A, Gindner L, Tilemann L, et al. Diagnostic accuracy of spirometry in pri-
mary care. BMC Pulm Med 2009;9:31. https://doi.org/10.1186/1471-2466-9-31
12. Karrasch S, Linde K, Rücker G, et al. Accuracy of FENO for diagnosing asthma: a
systematic review. Thorax 2017;72(2):109–16. https://doi.org/10.1136/thoraxjnl-
2016-208704
13. Berry A, Busse WW. Biomarkers in asthmatic patients: has their time come to direct
treatment? J Allergy Clin Immunol 2016;137(5):1317–24. https://doi.org/10.1016/
j.jaci.2016.03.009
14. Bjermer L, Alving K, Diamant Z, et al. Current evidence and future research needs
for FeNO measurement in respiratory diseases. Respir Med 2014;108(6):830–41.
https://doi.org/10.1016/j.rmed.2014.02.005
15. Metting EI, Riemersma RA, Kocks JH, et al. Feasibility and effectiveness of an
asthma/COPD service for primary care: a cross-sectional baseline description and
longitudinal results. NPJ Prim Care Respir Med 2015;25:14101. https://doi.org/
10.1038/npjpcrm.2014.101
16. Bush A, Fleming L. Is asthma overdiagnosed? Arch Dis Child 2016;101:688–9.
https://doi.org/10.1136/archdischild-2015-309053
17. Pinnock H, Parke HL, Panagioti M, et al. Systematic meta-review of supported self-
management for asthma: a healthcare perspective. BMC Med 2017;15(1):64.
https://doi.org/10.1186/s12916-017-0823-7
18. Levy M, Andrews R, Buckingham R, et al. Why asthma still kills: The national review
of asthma deaths (NRAD) confidential enquiry report. Royal College of Physicians,
2014. Available from: https://www.rcplondon.ac.uk/projects/outputs/why-asthma-
still-kills (accessed Aug 2019).
19. Environmental Audit Committee. UK progress on reducing F-Gas emissions inquiry.
House of Commons Environmental Audit Committee, 2018. Available from:
https://www.parliament.uk/business/committees/committees-a-z/commons-se-
lect/environmental-audit-committee/inquiries/parliament-2017/uk-progress-on-re-
ducing-f-gas-emissions-17-19/publications/ (accessed Aug 2019).
20. Chauhan BF, Ducharme FM. Addition to inhaled corticosteroids of long‐acting
beta2‐agonists versus anti‐leukotrienes for chronic asthma. Cochrane Database of
Systematic Reviews 2014;(1). https://doi.org/10.1002/14651858.CD003137.pub5
21. Weatherall M, Wijesinghe M, Perrin K, Harwood M, Beasley R. Meta-analysis of the
risk of mortality with salmeterol and the effect of concomitant inhaled corticosteroid
therapy. Thorax 2010;65(1):39–43. https://doi.org/10.1136/thx.2009.116608
22. Porter ME, Lee TH. The strategy that will fix health care. Harvard Business Review
2013;91(10):1–19.
23. Sobieraj DM. Association of inhaled corticosteroids and long-acting beta-agonists
as controller and quick relief therapy with exacerbations and symptom control in
persistent asthma: a systematic review and meta-analysis. JAMA 2018;319(14):
1485–96. https://doi.org/10.1001/jama.2018.2769
24. Buelo A, McLean S, Julious S, et al. At-risk children with asthma (ARC): a systematic
review. Thorax 2018;73(9):813–24. https://doi.org/10.1136/thoraxjnl-2017-210939
25. Miller MK, Lee JH, Miller DP, Wenzel SE, TENOR Study Group. Recent asthma
exacerbations: a key predictor of future exacerbations. Respir Med 2007;
101(3):481–9. https://doi.org/10.1016/j.rmed.2006.07.005
26. Blakey JD, Price DB, Pizzichini E, et al. Identifying risk of future asthma attacks using
UK medical record data: a Respiratory Effectiveness Group initiative. J Allergy Clin
Immunol Pract 2017;5(4):1015–24.e8. https://doi.org/10.1016/j.jaip.2016.11.007
Level of increased risk
Greatly increased risk
Moderately increased risk
Slightly increased risk
No increased risk
Unclear
(evidence limited or
equivocal)
Table 4 Factors associated with increased risk of future asthma attacks in adults
Children
• History of previous asthma attacks
• Poor control (assess review using objective patient reported control questionnaire such as ACT or ACQ)
• Inappropriate or excessive SABA use
• Older age
• Female
• Reduced lung function
• Obesity
• Smoking
• Depression
• Gender
• Urban residence
• History of anaphylaxis
• Comorbid gastro-oesophageal reflux
• COPD
• Raised FeNO at routine reviews
• Blood eosinophilia
• Poor adherence
This table is reproduced from SIGN 158 (British guideline on the management of asthma) by kind permission of the Scottish Intercollegiate Guidelines Network
2
OCT+NOV 2019 issue.qxp_Layout 1 18/12/2019 12:30 Page 43

9
Primary Care Respiratory
Update
The Primary Care Respiratory Society is a registered charity (Charity Number 1098117) and a company limited by guarantee registered in
England (Company Number 4298947). Vat registration number 866 1543 09. Website https://www.pcrs-uk.org Telephone: 01675 477600.
We are grateful to our corporate supporters (https://www.pcrs-uk.org/corporate-supporters) for their financial support which supports the core
activities of the charity and allows PCRS to make its services either freely available or at greatly reduced rates to its members. PCRS statement
on pharmaceutical funding (shorturl.at/fpvTY)
OCT+NOV 2019 issue.qxp_Layout 1 18/12/2019 12:30 Page 44
