
ABSTRACT
THE BOMBAY BLOOD GROUP: HOW DOES IT FIT IN THE HUMAN BLOOD GROUP
By
MAYA DAVIS
Texas Southern University, 2021
Dr. Monica Rasmus
The Bombay blood phenotype is one of the rarest ABO blood group. It is autosomal recessive
allele and occurs due to a point mutation in the FUT1gene on chromosome 19. The H gene
synthesizes the H antigen which is located on the red blood cells (RBCs). This thesis analyzes
the Bombay phenotype, more specifically how it fits in the human blood group. It questions
whether the differences between the Bombay phenotype and the ABO blood group affects its
place as an actual blood group. The goal of this study is to increase the amount of knowledge
regarding the Bombay phenotype and the human blood group system.

ii
Table of Contents
List of Tables ................................................................................................................................. iii
List of Figures ................................................................................................................................ iv
Vita .................................................................................................................................................. v
Dedication ...................................................................................................................................... vi
Acknowledgments......................................................................................................................... vii
Chapter 1 ......................................................................................................................................... 9
Review of Literature ..................................................................................................................... 11
Chapter 2: ...................................................................................................................................... 15
Chapter III ……………………………………………………………………………………….24
Chapter IV ..................................................................................................................................... 30
References ..................................................................................................................................... 37

iii
List of Tables
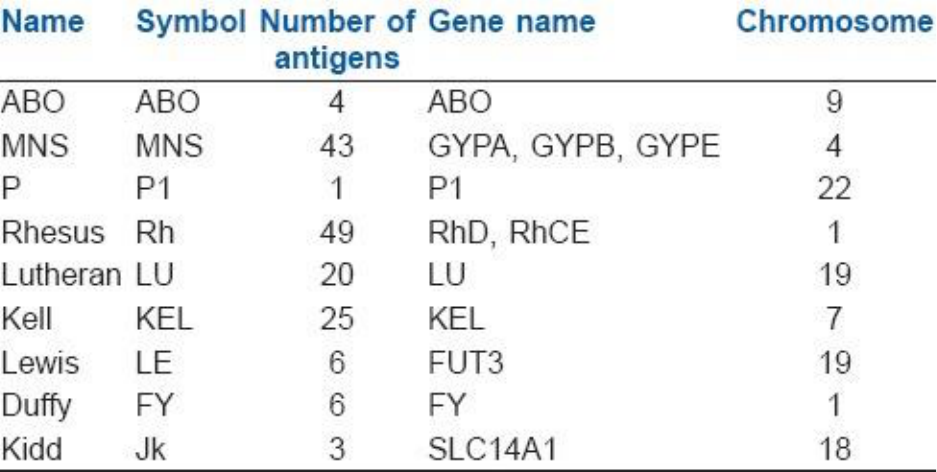
Table 1: Blood Group System ………………………………………………………..20
Table 2: Antibodies and Antigens with corresponding ABO type……………………21
Table 3: Most Common Blood Type by Ethnicity in the US…………………………22
Table 4: Most Rare Blood Type by Ethnicity in the US………….…………………..23
Table 5: ABO Genotyping……………………………………………………………29

iv
LIST OF FIGURES
Page
Figure1: Diagram showing the molecular structure of the ABO (h) antigen system………..19
Figure 2: ABO gene and major A, B, and O alleles …………………………………………27
Figure 3: Showing Synthesis of H, A, and B antigens……………………………………….28
Figure 4: Showing the Structural Component of Blood Group Phenotype………………….36

v
VITA
Maya R. Davis was born in Kingston Jamaica where she resided until she moved to the
United states in 2011. She attended Truman State University in Kirksville Missouri, and in
August 2015 she received the degree of Bachelor of Science in Biology. She entered Texas
Southern University in August 2017 and received a Bachelor of Science degree in Clinical
Laboratory Science in May 2021.

vi
DEDICATION
This thesis is dedicated with love and gratitude to my sister and to all other strong women in
my life, who, have nurtured and contributed greatly to the growth and development of my
character.

vii
ACKNOWLEDGEMENTS
Thank you to my advisor, Dr Monica Rasmus., for providing guidance and feedback throughout
this project. Thanks also to my family, for providing moral support and for providing guidance
and a sounding advice when required.
9
CHAPTER I: INTRODUCTION
The human blood group most commonly includes the ABO blood group system and the
Rh system. Together, these two attributes form the blood group system that most people are
familiar with. The ABO blood group consists of four basics phenotypes which are Type O, A, B,
and AB. Each phenotype can be RhD positive or RhD negative to give a total of eight basic
blood types. The grouping system is based on the premise that individuals have antigens on their
red blood cell membrane that corresponds to the four main blood groups. These antigens are
types of proteins found on the red blood cells. In rare cases, there are individuals who do not
express the H antigen, these individuals are said to have an H antigen deficiency known as the
Bombay phenotype (hh).
The Bombay blood phenotype is one of the rarest ABO blood groups and was discovered
in Bombay, now modern-day Mumbai, by Dr. Y. M. Bhende in 1952. It is transmitted as an
autosomal recessive trait and describes individuals that lack the H antigen on their red blood
cells (RBCs). Bhende and his co-authors published their paper in 1951 after months of research.
The phenotype was further classified into Bombay and para-Bombay phenotype based on the
absence of the H antigen. The Bombay phenotype is mostly found in 1 of 10,000 individuals in
India and parts of the Middle East. Since there is an absence of H antigen expression on the red
cell membrane of the ABO blood group system, blood donations usually have to come from a
suitable relative of patients in need of a blood transfusion. The Bombay phenotype is a result of a
point mutation in the FUT1 gene which is involved in the synthesis of the H antigen. The H
antigen is a precursor to the A and B antigens. Individuals with the Bombay phenotype are H
deficient and therefore cannot synthesize the A or B antigens. The ABH antigens are therefore
10
absent from their red cells. The blood group shows the presence of anti-A, anti-B, and strong
anti-H antibodies in their plasma. Because of this, the Bombay phenotype was initially
recognized as O group.

11
REVIEW OF LITERATIRE
Many people have never heard of the term Bombay phenotype. Most people, however, are
familiar with the ABO human blood group system. The Bombay phenotype is one of the rarest
ABO blood group (Bhende et al,1952). The Bombay phenotype lacks the two genes that encode
for the enzyme to make the H antigen, their genotype is hh and sese. (Watkins & Morgan, 1955).
People having Bombay phenotype inherit the homozygous recessive genotype (hh) instead of the
homozygous dominant (HH) or heterozygous (Hh) genotypes associated with the ABO blood
group system (Awan et al, 2018). Indians have been found to exhibit this phenotype the most.
Bhende and company discovered this blood group in Bombay India after observing that the new
blood group had serum which contained antibodies that attacked the normal ABO red blood cells.
The phenotype is so rare that in India, 1 in 10,000 people have it (Dipta &Hossain, 2011). Bombay
is mostly reported in people of India descent. However, while the phenotype is mostly seen among
Indians and people of Indian descent, this may not necessarily mean it’s not seen in other parts of
the world. In Europe, the prevalence of the Bombay phenotype is 1:10
6
. It is also very rare in
Caucasian with an incidence of 1 in 250,000 (Dipta & Hossain, 2011).
The ABO blood group system is the most popular system and denotes the presence or
absence of one or two antigens on the red blood cells. It was discovered in 1901 by Karl
Landsteiner at the University of Vienna. In 1930, he posthumously received the Nobel Prize for
discovering the blood types (Harmening, 2018). It is used as a means of classifying human blood
and involves two antigens, antigen A and antigen B, and two antibodies, antibody A and
antibody B. The antigens are present on the surface of the red blood cell while the antibody is in
the serum. Within the ABO blood group system there are four basics phenotypes which are Type
O, A, B, and AB. Each blood group can be RhD positive or RhD negative.

12
According to the American Red Cross the most common blood type statistically in the
US is shown in Table 2. Type O negative and O positive blood are constantly in high demands.
Only about 7% of the population are O negative. Approximately 37% of Caucasians are blood
type O positive, but 47% of African Americans are type O positive and 53% of Latin Americans
are type O positive (American Red Cross, n.d.).
Second to the ABO system is the Rh system. The Rh system explains that the red blood
cell has an antigen on its surface called the Rh antigen. The Rh blood group is important because
of the fact that its antigens are highly immunogenic. The Rh status is routinely determined in
persons donating blood. (Dean & Dean, 2005).
While the Bombay phenotype is not popularly known, it is important to note that there
are other blood groups recognized by the International Society of Blood Transfusion (ISBT). In
2019, the International Society of Blood Transfusion (ISBT) have recognized a total of 41
human blood group systems (Storry, 2019). The para-Bombay type is different from the
Bombay phenotype in that the former has H antigens in its secretions, whereas the latter doesn’t.
(Kim et al, 2019).)
Genetic analysis of the Bombay phenotype shows that it is as a result of a homozygous
recessive gene which prevents the development of A, B, and H antigens. (Yunis et al, 1969). It is
as a result of a point mutation in the FUT1 gene, with a deletion of exon 2 on FUT2 (Daniels,
2008). Bombay blood group is easily mistyped as blood group O so proper testing should be
done to detect the Bombay phenotype. Mistyping the Bombay phenotype can lead to an adverse
reaction during blood transfusion. (Nikam et al, 2017)
13
A blood transfusion is a lifesaving routine procedure but for individuals with the Bombay
phenotype it is quite difficult. As demonstrated, the Bombay phenotype lacks the H antigen on
their red blood cells, so transfusion between the ABO blood group can cause a hemolytic
transfusion reaction (Nikam et al, 2017). Individuals with the Bombay phenotype can donate
blood to those individuals that’s a part of the ABO blood group system, but they cannot receive
blood. In Shahshahani and company’s (2013) case report on transfusion reaction with the
Bombay blood group, they found that individuals having the Bombay phenotype are easily
misdiagnosed as the Type O blood group. They noted that a person who has Bombay phenotype
may have a hemolytic transfusion reaction if transfused with the wrong blood. A person having
the Bombay phenotype has to be transfused with someone else of the same phenotype (Knowles,
2006).
Hemolytic transfusion reaction is often associated with the Bombay phenotype. As
demonstrated in Shastry et al, (2013) case report, there can be severe hemolytic disease of the
newborn if the mother is Bombay phenotype. Because of the rarity of the phenotype individuals
with Bombay can receive blood in one of two ways: by doing an autologous blood donation prior
to surgery or transfusion from another Bombay Blood group (Shahshahani et al, 2013). If a
person with the Bombay phenotype gets blood from a donor with the ABO blood type, a
hemolytic transfusion can occur due to the bloods being incompatible. According to the same
case report, HDN is theoretically possible in babies with Bombay phenotype but there are
practically no reports in literature on it (Shastry et al, 2013). It is therefore important that proper
blood grouping takes place.
The Bombay phenotype is a blood group that is very rare. However, further study of the
differences between it and the ABO blood group will lead to better understanding. Specifically,

14
transfusion between both blood groups should be studied in order to learn what makes the
Bombay phenotype incompatible among the ABO blood types and if there is any successful way
to overcome that. Therefore, the following research question is raised
RQ: How does the Bombay phenotype fit in the human blood group?

15
CHAPTER II: THE HUMAN BLOOD GROUP- AN OVERVIEW OF THE ABO BLOOD
TYPE AND THE BOMBAY BLOOD TYPE
The human blood type is a way to classify the human blood based on the presence or
absence of antibodies and antigens, including the Rh factor on the surface of the red blood cells
(RBCs). These antigens are a type of protein found on the red blood cells. As of 2019, the
International Society of Blood Transfusion (ISBT) have recognized a total of 41 human blood
group systems (Storry et al, 2019). Some of these blood groups are highlighted in Table 1. The
blood types in the ABO and RhD system are the most important and known blood group system
as they determine someone’s blood type. The ABO blood group system was discovered in 1901
by Karl Landsteiner at the University of Vienna while he was in the process of trying to figure
out why blood transfusions sometimes cause death and in other cases saves a patient’s life. In
1930, he posthumously received the Nobel Prize for discovering the blood types (Harmening,
2018). The ABO blood group system is a means of classifying human blood based on inherited
genes from both parents. It involves two antigens, antigen A and antigen B, and two antibodies,
antibody A and antibody B. The antigens are present on the surface of the red blood cell while
the antibody is in the serum. The ABO blood group consists of four basics phenotypes which are
Type O, A, B, and AB. Each blood group can be RhD positive or RhD negative. Combining
these two characteristics creates eight basic blood types (O-positive, O-negative, A-positive, A-
negative, B-positive, B-negative, AB-positive, AB-negative).
Whole blood is blood that runs through the veins, it contains erythrocytes, white blood
cells, plasma and platelets. The many components of blood give it its ability to perform various
functions including, transportation of oxygen around the body, forming blood clots to stop
excessive bleeding and carrying antibodies that combat infection. The human blood group is

16
identified by antibodies and antigens in the blood. Antibodies are soldiers that are part of the
bodies defense systems. These antibodies fight against foreign invaders which might pose a
threat to the body. Antigens are protein molecules that are found on the surface of red blood
cells. The four main blood groups defined by the ABO system with the presence or absence of
antibodies and antigens are grouped as follows:
Blood group O – has no antigens, but has both anti-A and anti-B antibodies in its plasma
Blood group A – has A antigens on the red blood cells and has anti-B antibodies in the plasma
Blood group B – has B antigens with anti-A antibodies in its plasma
Blood group AB – has both A and B antigens, but no antibodies
Table 2 shows the possible way antibodies and antigens with corresponding ABO type.
Humans with blood type B will have antigen B on the surface of their red blood cell which will
then prevents them from producing anti-B antibodies. Persons having blood type O do not have
any AB antigens, this makes blood type O universal donors for transfusion as it is not rejected
from others. Individuals having blood type AB do not produce AB antigens which makes them
good receivers for blood transfusion. It is estimated that 5% of the US population has blood type
AB, with 1% having AB negative (AB-) blood and 4% having AB positive (AB+) blood
(American red Cross, n.d.). The AB negative is the least common blood type among Americans
and individuals having this blood type can receive blood from all other negative blood types. The
ABO blood group system is the most important blood group system in human blood transfusion
reactions. O negative blood is routinely used in transfusion for any blood type. It is routinely in
short supply because it is the universally donated blood needed for emergency transfusion
(American Red Cross, n.d.).
17
The Rh system is the second most import blood group system and was discovered in
1940 by Karl Landsteiner and A.S. Weiner. The most important antigen in the Rh system is the
D-antigen. The Rh system explains that the red blood cell has an antigen on its surface called the
Rh antigen. When the antigen is present the individual is termed Rh positive (Rh+). But, if
absent the individuals in this blood group are described as being Rh negative (Rh-). The Rh
blood group is important because of the fact that its antigens are highly immunogenic. It’s solely
for this reason the Rh status is routinely determined in persons donating blood. (Dean & Dean,
2005).
According to the American Red Cross the most common blood type statistically in the
US is shown in the Table 2. Type O negative and O positive blood are constantly in high
demands. Only about 7% of the population are O negative. Approximately 37% of Caucasians
are blood type O positive, but 47% of African Americans are type O positive and 53% of Latin
Americans are type O positive. This indicates the critical role the minority group plays in
meeting the need for blood (American red Cross, n.d.). Table 3 shows the rarest blood types. A
person’s blood type is considered rare if they lack an antigen for which 99% of the population is
positive. If they lack an antigen that 99.99% of the people have, then that blood type is
considered to be extremely rare. To date, the American Red Cross has listed 600 known antigens
which contributes to the nature of blood based on their presence or absence (American Red
Cross, n.d.).
It is important to note that the Bombay phenotype is one of the rarest ABO blood groups.
In the 1950s, Bhende et al. discovered a new blood group in Bombay India (now known as
Mumbai). He described the blood group after observing an individual with an unusual blood type
having a strange reaction to other ABO blood types. (Bhende et al,1952) This new blood group is

18
now called the Bombay phenotype. Dr. Bhende observed that the new blood group had serum
which contained antibodies that attacked the normal ABO red blood cells. The Bombay phenotype
is very rare and reportedly it occurs with a frequency of 1 in 10,000 people in India. (Dipta &
Hossain, 2011). The phenotype is mostly reported in people of India descent. In Europe, the
prevalence of the Bombay phenotype is 1:10
6
(Dean & Dean, 2005).
It is also very rare in Caucasians with an incidence of 1 in 250,000. (Dipta &Hossain,
2011). Because of its failure to express the H antigen on the red cell membrane of the ABO
blood group system, blood donations usually have to come from a suitable relative. Individuals
with Bombay phenotype lack the two genes that encode the enzyme to make the H antigen, their
genotype is hh and sese. (Watkins & Morgan, 1955)
Para-Bombay type and Bombay phenotype are both rare phenotypes that have defects in
producing the H antigen. The para-Bombay type is different from the Bombay phenotype in that
the former has H antigens in its secretions, whereas the latter doesn’t. (Kim et al, 2019).

19
Figure1: Diagram Showing the molecular structure of the ABO (h) antigen system
20
Table 1: Blood Group System

21
Table 2: Antibodies and Antigens with corresponding ABO type.
ABO Blood
Type
Antigen A
Antigen B
Antibody anti A
Antibody anti B
O
N
N
Y
Y
A
Y
N
N
Y
B
N
Y
Y
N
AB
Y
Y
N
N

22
Table 3: Most Common Blood type by Ethnicity in the US
Ethnicity
O positive (%)
A positive (%)
B positive (%)
African American
47
24
18
Latin American
53
29
9
Asian
39
27
25
Caucasian
37
33
9

23
Table 4: Most Rare Blood Type by Ethnicity in the US
Ethnicity
AB negative (%)
B negative (%)
A negative (%)
AB positive
(%)
African American
0.3
1
2
0
Latin American
0.2
1
2
2
Asian
0.1
0.4
0.5
0
Caucasian
1
1
0
3

24
CHAPTER III: THE BOMBAY BLOOD GROUP GENOTYPE- WHAT'S THE DIFFERENCE
BETWEEN THE ABO BLOOD GROUP?
The ABO gene is located on chromosome 9 at the band 9q34.2 and contains 7 exons that
encode a 354-aa glycoprotein. The gene encodes three alleles which are A, B, and O allele.
Chromosome 9 encodes for the A and B glycosyltransferase which are the transferase necessary
for the ABO antigens. The FUT1 gene, is located on chromosome 19q13.3 where the synthesis
of A, B and H antigens occurs. The FUT2 gene is also located on chromosome 19q13.3,
however, it encodes for the transferases essential to the production of the ABO antigens that are
associated with bodily fluids other than blood (Awan et al, 2018).
The rare Bombay blood phenotype occurs in people who inherited two recessive alleles of
the H gene making their genotype hh. These individuals have no H antigen on the surface of their
red cells or in their secretions. In other words, they possess the alleles for either or both of the A
and B alleles, but they are not able to express them. It is a condition that is mainly seen in closed
off communities such as noble families where they inbreed because of their customs. There is a
lack of genetic variety in these types of communities.
This phenotype is a result from homozygosity of a point mutation in the FUT1 gene, with a
deletion of exon 2 on FUT2 (Daniels, 2008). The Tyr316Ter mutation in the coding region of
FUT1introduces a stop codon, leading to a reduction in enzyme that lacks 50 amino acids at the
C-terminal end, causing the enzyme to be inactive. There has to be at least one useful copy of
FUT1 present (H/H or H/h) for the H antigen to be produced on the surface of the red blood
cells. The Bombay phenotype results if both copies of FUT1 are inactive. The H antigen must be
synthesized before the A of B antigen can be made (Dean &Dean, 2005). Chromosome 19
produces glycosyltransferase that add L-fucose to a precursor ingredient to make H antigen on
red cells. H antigen is an essential substance to the A or B transferase which are encoded by the

25
ABO gene (Shahshahani et al, 2013). This A and B transferase converts the H antigen into either
A or B antigen. Blood group A individuals express an α1-3 N-acetylgalactosamine (GalNAc),
and blood group B individuals express an α1-3 galactose (Cooling, 2015). The O allele in type O
individuals, produces a transferase that is inactive. So, group’s O individuals have indolent ABO
genes and only express the H-antigen precursor.
Watkins and Morgan postulated that there are two types of Bombay genotype. They further
go on to state that there is a large number of Lewis positive Bombay individuals. In a report by
Yunis et al (1969), the authors describe a large family, covering three generations that has a
greater number of Bombay individuals than in any other previous studies. The report
demonstrates the inheritance of the Bombay phenotype in offspring from the union of Bombay
phenotype hh and an individual heterozygous Hh at the Bombay locus. The family shows the
suppression of the A-B-O phenotype by way of the Bombay phenotype and also the
heterozygosity at the Lewis Locus. This is consistent with the scheme postulated by Watkins of
the Bombay phenotype having two types of genotype (Yunis et al, 1969).
The main characteristic feature of the Bombay phenotype which is its lack of H antigen
highlights the main difference between the Bombay blood group and the ABO blood group, in
particular the O group. The O blood group contains the highest amount of H antigens among all
the blood phenotypes. Additionally, the Bombay blood group includes anti-H in the plasma
while group O blood does not have anti-H in the plasma. The genomic make-up of the Bombay
blood group is h/h; se/se while the genotype of the O blood group is H/H or H/h and Se/Se or
Se/se. Another difference between Bombay blood group and O blood group is that Bombay
blood group contains two recessive alleles however, the group O blood contains at least a single
dominant H allele. (Dean &Dean, 2005)

26
The similarities that exist between the blood groups are that they are blood phenotypes that
both occur among humans. They are both distinguished by the presence or absence of the H
antigen on the surface of the red blood cells. Both blood groups contain anti-A and anti-B
antibodies in the plasma.

27
Figure 2: ABO gene and major A, B, and O alleles

28
Figure 3: Showing Synthesis of H, A, and B antigens.

29
Table 5: ABO Genotyping
Antigens present of
RBCs
Antibody present in
plasma
Possible Genotype
A
A antigen
Anti-A
AA or AO
B
B antigen
Anti- B
BB or BO
AB
A antigen
B antigen
none
AB
O
None
Anti-A, anti-B, anti-
A, B
OO

30
Chapter IV: THE BOMBAY BLOOD GROUPS – TESTING AND TRANSFUSION
LIMITATIONS
Genetic analysis of the Bombay phenotype shows that it is as a result of a homozygous
recessive gene which prevents the development of A, B, and H antigens. (Yunis et al, 1969). It
shows that the Bombay phenotype is an H antigen deficient phenotype. Bombay blood group is
easily mistyped as blood group O so proper testing should be done to detect the Bombay
phenotype. Mistyping the Bombay phenotype can lead to a transfusion reaction during blood
transfusion.
It is difficult for individuals with the Bombay phenotype to receive blood when there is a
need. Individuals with Bombay can receive blood in one of two ways: by donating their own
blood prior to transfusion or receive it from another Bombay Blood group (Shahshahani, et al
2013). Blood transfusion is a way of adding blood or blood components such as plasma and
platelets to the body. It is a routine medical procedure provided to the recipient through a tube
placed in the vein of the forearm. Blood types are important in transfusion. If you get a
transfusion that’s incompatible with your blood type, your body’s immune response is to fight
the donor’s blood. Allergic reactions are the most common type of transfusion reactions. Allergic
reactions occur when the body reacts to the plasma proteins or other substances in the donated
blood. Usually, the symptoms are mild and include, itching and hives which is treated with
antihistamines. In very rare cases, the reactions can be more severe. (American Cancer Society,
2017). An acute hemolytic transfusion reaction is another form of reaction that is the most serios
type of reaction. It occurs when the blood donor and the recipient blood type do not match. The
reaction occurs when the transfused red blood cells are attacked by the patient’s antibodies
causing the red blood cells to be hemolyzed and release harmful substances into the body’s blood

31
stream. Patients experience acute hemolytic transfusion may have chills, fever, lower back pain
and nausea. In some situations, the reaction can be become deadly if the transfusion is not
stopped. Delayed hemolytic transfusion happens days or weeks after the transfusion. This type of
transfusion occurs in a person who had a transfusion in the past. It involves the body attacking
the antigens on the transfused blood cells days or weeks after the transfusion (American Cancer
Society, 2017).
Hemolytic disease of the newborn could arise in mothers with the Bombay phenotype.
Hemolytic disease of the newborn occurs when the baby’s red blood cells goes through
hemolysis. It occurs due to the mother’s IgG antibodies crossing the placenta leading to
hemolysis (Narang & Jain, 2001). Shastry et al described a rare case of severe hemolytic disease
with a young mother with Bombay phenotype. The mother’s blood is wrongly typed as O
positive. In this case there were two factors which could have caused the hemolytic disease of
the newborn. Firstly, doctors suspected it was because of the anti A present in the mother, as the
baby’s blood group was ‘A’ positive. Secondly, doctors thought the mother was mistyped and
there was the anti H present in the Bombay phenotype mother. The first possibility was ruled out
due to the baby’s incompatibility with the mothers O positive blood. The error in the mother’s
blood group was noted and the hemolysis of the baby’s red blood cells was due to the Oh
phenotype of the mother (Shastry et al, 2013).
Bombay phenotype blood transfusion is complicated given the fact that phenotype lacks
A and B antigens. When individuals with the Bombay phenotype needs a blood transfusion, they
can only receive autologous blood or blood from another Bombay blood group individual. Even
though blood group O has no H antigen, transfusing the red cell blood group O to a Bombay
phenotype can cause a fatal hemolytic reaction. (Shahshahani, et al, 2013)

32
Individuals with the Bombay phenotype can be donors to all ABO blood groups but they
can’t receive blood. They can only accept blood from a Bombay phenotype person. This is
because all ABO donors have the H antigen common in their ABO blood group. This makes the
Bombay phenotype incompatible with ABO donors. Given the rarity of this blood group, anyone
who needs immediate blood transfusion would be unable to be transfused because no blood
would be at the blood bank. Those anticipating the need for this blood would probably have to do
an autologous donation. but this case is not an option when there is an emergency transfusion.
(Nikam et al, 2017).
In a case report by Shahshahani and her co-authors, it was noted how a patient admitted
to the hospital was mistyped and her blood group was thought to be O. A unit of blood group O
was given to the patient during transfusion. The patient had a transfusion reaction which caused
doctors to stop transfusion immediately. Further testing on the patient’s blood revealed that the
patient was not blood type O but actually Bombay phenotype. Bombay phenotype is often
misdiagnosed as the blood group O because of the presence of anti-H in their plasma. A
transfusion reaction between blood group O would result in a hemolytic transfusion reaction.
(Suraci & Mora, 2016).
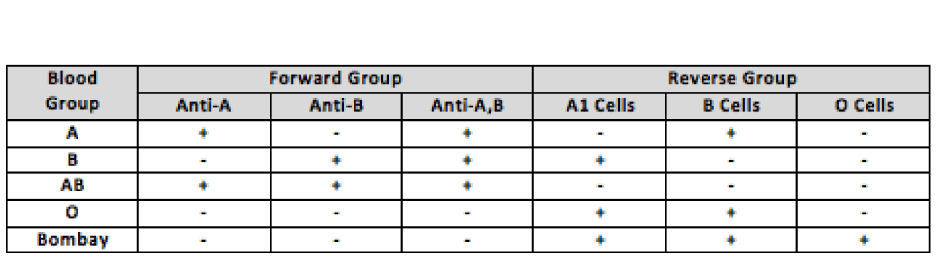
In order to avoid transfusion reactions, it is important to perform both forward and
reverse ABO blood typing. Standard crossmatching and pretransfusion laboratory test should
also be formed in blood banks in the hospitals. (Shahshahani, et al 2013). Table 5 illustrate
forward and reverse grouping with the blood groups. It is shown how, Bombay blood group
would be considered as O group because it doesn’t show any reaction to anti-A and anti-B
antibodies during forward grouping. When it is cross matched with different units of blood O
group, it would show incompatibility (Suraci & Mora, 2016). Therefore, additional test such as

33
reverse grouping has to be performed in order to confirm the Bombay phenotype. It has been
suggested to “routine serum typing or reverse grouping confirmation” along with “O” cell
control in reverse grouping be incorporated in procedures in every blood bank or transfusion
medicine department. (Dipta &Hossain, 2011). In 2019, the Indian express stated that there was
an unofficial registry for Bombay blood group that lists over 350 donors across India. However,
these donors are not always available, in fact, at any time there are only 30 active donors
available to give blood (Barnagarwala, 2019). The Bombay group is generally not stored in
blood banks, mainly because it is rare, and the shelf life of blood is 35-42 days so whenever there
is a demand a patient is required urgently. (Barnagarwala, 2019)
Having the Bombay phenotype does not mean a person suffers from poor immunity or
may be more prone to diseases. Their counts for haemoglobin, red blood cells, platelets, and
white blood cells, are similar to the count of others based on their health index. Because of rarity,
however, they do face problems during blood transfusion. (Barnagarwala, 2019)
The Bombay blood group is the rarest ABO blood group discovered over 60 years ago. It
is rare in India and even rarer globally. Globally the incidence of the phenotype is one in four
million. This blood group is easily mistyped as the ‘O’ blood type because it does not show any
reaction to anti-A and anti-B antibodies just like the normal ‘O’ group. The difference in both
blood groups is that the O group has Antigen H, while the Bombay (hh) group does not. Red
cells of the Bombay group are only compatible with the serum from another Bombay individual.
Individuals with Bombay blood group can donate to all ABO blood group but can only accept
from other Bombay blood group people. The Bombay serum has anti-H is an IgM antibody that
can bind complement and cause red cell lysis. Bombay blood is incompatible with all ABO
34
donors because the H antigen is common to all ABO blood group red blood cells. In context,
cross-matching reverse grouping or serum grouping has to be done to detect this group.
35
Table 3. Forward and reverse Grouping with Blood Types (+) =Agglutination, (-) = No reactivity

36
Figure 4: Showing the Structural Component of Blood Group Phenotype.

37
References
American Cancer Society: Getting a Blood Transfusion. (2017, February 17).
American National Red Cross. (n.d.) Facts About Blood and Blood Types.
https://www.redcrossblood.org/donate-blood/blood-types.html
Awan, S. A., Junaid, A., Khan, S., & Jahangir, S. (2018). Blood Diathesis in a Patient of Rare
Blood Group ‘Bombay Phenotype’. Cureus, 10(10).
Barnagarwala, T. (2019, September 11). Explained: What is bombay blood group, rare and
sought after? The Indian Express. https://indianexpress.com/article/explained/what-is-
bombay-blood-group-rare-and-sought-after-5984653/
Bhende, Y. M., Deshpande, C. K., Bhatia, H. M., Sanger, R., Race, R. R., Morgan, W. T. J., and
Watkins, W. M. 1952. A new blood group character related to the ABO system. Lancet
1:903,
Cooling, L. (2015). Blood groups in infection and host susceptibility. Clinical microbiology
reviews, 28(3), 801-870.
Daniels, G. (2008). Human blood groups. John Wiley & Sons.
Dean, L., & Dean, L. (2005). Blood groups and red cell antigens (Vol. 2). Bethesda, Md, USA:
NCBI.
Dipta, T. F., & Hossain, A. Z. (2011). The Bombay blood group: are we out of
risk? Mymensingh medical journal: MMJ, 20(3), 536-540.
Harmening, D. M. (2018). Modern blood banking & transfusion practices. FA Davis.
https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/blood-
transfusion-and-donation/how-blood-transfusions-are-done.html

38
Kim, M. S., Kim, J. S., Park, H., Chung, Y., Kim, H., Ko, D. H., ... & Oh, H. B. (2019). The
First Case of Para-Bombay Blood Type Encountered in a Korean Tertiary
Hospital. Journal of Korean medical science, 34(39).
Knowles S, Regan F. Blood cell antigens and antibodies: erythrocytes, platelets and
granulocytes. (2006) In: Lewis SM, Bain BJ, Bates I, editors. Practical
Haematology. 10th ed. Churchill Livingstone: Elsevier, Philadelphia, PA, USA;. pp.
481–7
Mitra, R., Mishra, N., & Rath, G. P. (2014). Blood groups systems. Indian journal of
anaesthesia, 58(5), 524.
Narang, A., & Jain, N. (2001). Haemolytic disease of newborn. The Indian Journal of
Pediatrics, 68(2), 167-172.
Nikam, V., Kashid, V., Khapare, J., & Gaikwad, S. (2017). Bombay blood group: An
overview. Inventi Rapid: Pharmacy Practice, 3, 1-2.
Shahshahani, H. J., Vahidfar, M. R., & Khodaie, S. A. (2013). Transfusion reaction in a case
with the rare Bombay blood group. Asian journal of transfusion science, 7(1), 86.
Shastry, S., Lewis, L. E., & Bhat, S. S. (2013). A rare case of hemolytic disease of newborn with
Bombay phenotype mother. Asian journal of transfusion science, 7(2), 153.
Storry, J. R., Clausen, F. B., Castilho, L., Chen, Q., Daniels, G., Denomme, G., ... & Yahalom,
V. (2019). International society of blood transfusion working party on red cell
immunogenetics and blood group terminology: report of the Dubai, Copenhagen and
Toronto meetings. Vox sanguinis, 114(1), 95-102.
Suraci, N., & Mora, M. (2016). Bombay blood phenotype: Laboratory detection and transfusions
recommendations. Int J Blood Transfus Immunohematol, 6, 8-11.

39
Watkins, W. M., Morgan, W. T. J.: (1955) Some observations on the 0 and H characters of
human blood and secretions. Vox Sang. 5:1
Yunis, E. J., Svardal, J. M., & Bridges, R. A. (1969). Genetics of the Bombay
phenotype. Blood, 33(1), 124-132.
