Vaccine Storage and Handling Toolkit
Updated with Mpox Vaccines Storage and Handling Information Addendum
March 29, 2024
MARCH 2024
346940-A
VACCINESTORAGEANDHANDLINGTOOLKITMARCH
Table of Contents
The Vaccine Storage and Handling Toolkit has been updated to address proper storage, handling, transport and emergency handling of
vaccines. The addendum and resources sections are now separate documents. The addendum addresses the proper storage, handling
and transport of the mpox vaccine. The addendum will be updated will be updated as new vaccines are approved and as vaccination
information evolves. Please check the CDC Vaccine Storage and Handling Toolkit website (www.cdc.gov/vaccines/hcp/admin/stor-
age/toolkit/index.html) regularly for the most current version of the toolkit.
Introduction .........................................................................................................................................................................................................3
SECTION ONE: Vaccine Cold Chain ..............................................................................................................................................................5
SECTION TWO: Staff and Training .................................................................................................................................................................7
SECTION THREE: Vaccine Storage and Temperature Monitoring Equipment ......................................................................................9
SECTION FOUR: Vaccine Inventory Management ....................................................................................................................................18
SECTION FIVE: Vaccine Preparation ...........................................................................................................................................................21
SECTION SIX: Vaccine Transport ................................................................................................................................................................. 23
SECTION SEVEN: Emergency Vaccine Storage and Handling...............................................................................................................27
Glossary ............................................................................................................................................................................................................. 29
Disclaimer: This document provides best practices and Centers for Disease Control and Prevention (CDC) recommendations on storage,
handling, and transport of vaccines and diluents. It also provides information on vaccine storage and handling requirements related to
the Vaccines for Children program. Use of trade names and commercial sources in this toolkit is for identification only and does not imply
endorsement by the U.S. Department of Health and Human Services (DHHS), the U.S. Public Health Service (PHS), or CDC.

3
VACCINE STORAGE AND HANDLING TOOLKIT
Introduction
Proper vaccine storage and handling are important factors in preventing and eradicating vaccine-preventable diseases.
Yet, each year, storage and handling errors result in revaccination of many patients and significant financial loss due
to wasted vaccines. Failure to store and handle vaccines properly can reduce vaccine potency, resulting in inadequate
immune responses in patients and poor protection against disease. Patients can lose confidence in vaccines and
providers if they require revaccination because the vaccines they received may have been compromised.
This toolkit provides information, recommendations, and resources to assist you in properly storing and handling
your vaccine supply. The Centers for Disease Control and Prevention (CDC) Vaccine Storage and Handling Toolkit
brings together best practices from the General Best Practice Guidelines for Immunization* product information from
vaccine manufacturers, and results of scientific studies.
Implementing these best practices and recommendations will help protect your patients, safeguard your vaccine
supply, and avoid the unnecessary costs of revaccinating patients and replacing expensive vaccines.
For specific, detailed storage and handling protocols for individual vaccines, always refer to the manufacturer’s product
information vaccines licensed for use in the United States FDA* or contact the manufacturer directly.
Vaccines for Children Program
The Vaccines for Children (VFC) program provides vaccines at no cost to eligible children. VFC providers are
important partners in making sure VFC-eligible children receive viable, properly handled vaccine.
This toolkit provides general background information on many of the VFC storage and handling requirements and
illustrates best practices essential to safeguarding the public vaccine supply.
If you are a VFC provider or receive other vaccines purchased with public funds, consult your state or local
immunization program (referred to throughout this document as “immunization program”
*
) to ensure you are
meeting all mandatory storage and handling requirements that are specific or tailored to your jurisdiction.
You may see vendors use terms such as “VFC-compliant,” “CDC-compliant,” or “satisfies VFC requirements” in their marketing materials
or on their websites. In this context, "compliance" and related terms may lead consumers to incorrectly believe that CDC or the VFC
program has independently assessed and verified the quality of these products. CDC/VFC is not authorized to assess, validate, verify,
or endorse the products or services of private companies. Should you encounter this type of language in vendor marketing materials,
please keep in mind that neither CDC nor the VFC program has validated any product or service for compliance with CDC or VFC
program requirements or standards.
2024 Vaccine Storage and Handling Toolkit Updates
Changes to the 2024 Vaccine Storage and Handling Toolkit Transport System Recommendations for vaccine
transport during any emergency can be found in Emergency Transport Vaccine Storage and Handling.
COVID-19 vaccines are available on the commercial market. Please consult, product inserts and Emergency Use
Authorization (EUA) fact sheets for latest recommendations for storing, handling, and administering all COVID-19
vaccines. If you are a VFC provider or receive other vaccines purchased with public funds, consult your state or
local immunization program (referred throughout this document as “immunization program”) to ensure you are
meeting all mandatory storage and handling requirements that are specific or tailored to your jurisdiction. The
addendum and resources sections are now separate documents. The addendum provides proper storage, handling
and transport of the Mpox vaccine.
* ACIP recommendations: www.cdc.gov/vaccines/hcp/acip-recs/index.html
Manufacturers’ package inserts: Vaccines Licensed for Use in the United States | FDA
Immunization programs: www.cdc.gov/vaccines/imz-managers/awardee-imz-websites.html
4
Introduction
VACCINE STORAGE AND HANDLING TOOLKIT
How to Use the Vaccine Storage and Handling Toolkit
This toolkit outlines CDC recommendations for vaccine storage and handling.
This list shows the icons you will see throughout the toolkit and their meanings:
ICON DESCRIPTION
CDC Recommendation – CDC recommends this as a minimal action to protect your vaccine supply.
CDC Best Practice – CDC recommends best practices as additional actions, practices, and
procedures to enhance protection of your vaccine supply.
Additional CDC vaccine storage and handling information is available at:
• Vaccine storage and handling home page:
www.cdc.gov/vaccines/hcp/admin/storage-handling.html
(sign up for notifications about updates)
• Educational webinars and continuing education for health care providers:
www.cdc.gov/vaccines/ed/courses.html
• Contact information for state/local immunization programs:
www.cdc.gov/vaccines/imz- managers/awardee-imz-websites.html
• E-mail specific questions to CDC: [email protected]v

5
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION ONE: Vaccine Cold Chain
Proper vaccine storage and handling play critical roles in eorts to prevent vaccine-preventable diseases. Vaccines
exposed to storage temperatures outside the recommended ranges may have reduced potency, creating limited
protection and resulting in the revaccination of patients and thousands of dollars in wasted vaccine.
Proper storage and handling begin with an eective vaccine cold chain.
A cold chain is a temperature-controlled supply chain that includes all vaccine-related equipment and procedures. The
cold chain begins with the cold storage unit at the manufacturing plant, extends to the transport and delivery of the
vaccine and correct storage at the provider facility, and ends with administration of the vaccine to the patient.
Vaccine
manufacturing
Vaccine
distribution
Vaccine arrival
at provider facility
Vaccine storage and
handling at provider facility
Vaccine
administration
Manufacturer
responsibility
Manufacturer/
distributor
responsibility
Provider
responsibility
Cold Chain Flowchart
If the cold chain is not properly maintained, vaccine potency may be lost, resulting in an unusable vaccine supply.
Vaccines must be stored properly from the time they are manufactured until they are administered. Potency is reduced
every time a vaccine is exposed to an improper condition. This includes overexposure to heat, cold, or light at any step
in the cold chain. Once lost, potency cannot be restored.
Exposure to any inappropriate conditions can aect potency of any refrigerated vaccine, but a single exposure to
freezing temperatures (0° C [32° F] or colder) can actually destroy potency. Liquid vaccines containing an adjuvant
can permanently lose potency when exposed to freezing temperatures.

6
SECTION ONE: Vaccine Cold Chain
VACCINE STORAGE AND HANDLING TOOLKIT
When the cold chain fails
Ensuring vaccine quality and maintaining the cold chain are shared responsibilities among manufacturers,
distributors, public health staff, and health care providers.
An effective cold chain relies on three main elements:
» Well-trained staff
» Reliable storage and temperature monitoring equipment
» Accurate vaccine inventory management
Results of a cold chain failure can be costly.
1,2,3
General Best Practice Guidelines for Immunization states, “vaccine
exposed to inappropriate temperatures that is inadvertently administered should generally be repeated.”
4
A break in the cold chain can mean extra doses for patients, increased costs for providers, and damage to public
confidence in vaccines.
More importantly, patients refusing revaccination can remain unprotected from serious, vaccine-preventable
diseases.
Vaccine appearance is not a reliable indicator that vaccines have been stored in appropriate conditions. For
example, inactivated vaccines—even when exposed to freezing temperatures—may not appear frozen, giving no
indication of reduced or lost potency.
By following a few simple steps and implementing CDC-recommended storage and handling practices, providers can
ensure patients receive high-quality vaccine that has not been compromised.
1. Department of Health and Human Services, Oce of Inspector General. Vaccines for Children Program: Vulnerabilities in Vaccine
Management, June 2012, oig.hhs.gov/oei/reports/oei-04-10-00430.asp.
2. Gazmararian JA, Oster NV, Green DC, Schuessler L, Howell K, et al. Vaccine storage practices in primary care physician oces: assessment
and intervention. Am J Prev Med 2002;23(4):246–53.
3. Bell KN, Hogue CJR, Manning C, Kendal AP. Risk factors for improper vaccine storage and handling in private provider oces. Pediatrics
2001;107(6):1–5.
4. Centers for Disease Control and Prevention. General Best Practice Guidelines for Immunization, www.cdc.gov/vaccines/hcp/acip-recs/general-
recs/index.html.

7
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION TWO: Staff and Training
Vaccine storage and handling practices are only as eective as the sta that implements them. Sta that is well-
trained in general storage and handling principles and organization-specific storage and handling standard operating
procedures (SOPs) is critical to ensuring vaccine supply potency and patient safety.
Sta Training
All sta members who receive vaccine deliveries as well
as those who handle or administer vaccines should be
trained in vaccine-related practices and be familiar with
your facility’s storage and handling SOPs. If you are a VFC
provider or have vaccines purchased with public funds,
contact your immunization program
*
for specific state
requirements related to training, policies, and procedures.
Storage and Handling SOPs
CDC recommends your facility develop and
maintain clearly written, detailed, and up-to-
date storage and handling standard operating
procedures (SOPs). SOPs will help your facility stay organized, serve as a reference and training tool, and ensure
proper vaccine management. SOPs help ensure proper procedures are followed and problems are identified,
reported, and corrected. SOPs should also provide guidance for emergencies such as equipment malfunctions,
power failures, or natural disasters.
Storage and handling plans and SOPs should contain plans and information for three major areas (see the Vaccine
Storage and Handling SOP Worksheet, (page 35):
• General information—include contact information for vaccine manufacturers, equipment service providers, and
important facility sta, as well as job descriptions, regularly used forms, and sta training requirements
• Routine storage and handling SOPs—include information for all aspects of vaccine inventory management, from
ordering to monitoring storage conditions
• Emergency vaccine storage, handling, and transport SOPs—outline steps to be taken in the event of equipment
malfunctions, power failures, natural disasters, or other emergencies that might compromise vaccine storage
conditions
Worksheets to assist you in developing your organization's routine and emergency SOPs are located in the
resources section.
Train sta on routine vaccine storage and handling and emergency SOPs. Keep SOPs near vaccine storage
units and make sure sta knows where to find them. Document all training completed with dates and participant
names.
Storage and handling training should be completed:
• As part of new employee orientation
• Annually as a refresher for all sta involved in immunization and vaccine storage and handling activities
• Whenever new vaccines are added to inventory
• Whenever recommendations for storage and handling of vaccines are updated
* Immunization programs: www.cdc.gov/vaccines/imz-managers/awardee-imz-websites.html
Online Training Resources
CDC’s You Call the Shots: Vaccine Storage and
Handling
†
is a free, online training module focused
on storage and handling requirements.
Check with your immunization program
*
and
professional organizations to see what vaccine
storage and handling training resources they offer.
†
You Call the Shots: Vaccine Storage and Handling: www.cdc.
gov/vaccines/ed/youcalltheshots.html

8
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION TWO: Staff and Training
Vaccine Coordinator Recommendations
Designate a primary vaccine coordinator. This person
will be responsible for ensuring all vaccines are stored
and handled correctly and should be an expert on your
facility’s storage and handling SOPs.
Coordinator responsibilities should include:
• Ordering vaccines
• Overseeing proper receipt and storage of vaccine
deliveries
• Documenting vaccine inventory information
• Organizing vaccines within storage units
• Setting up temperature monitoring devices
• Checking and recording minimum/maximum temperatures at start of each workday
*
• Reviewing and analyzing temperature data at least weekly for any shifts in temperature trends
• Rotating stock at least weekly so vaccines with the earliest expiration dates are used first
• Removing expired vaccine from storage units
• Responding to temperature excursions (out-of-range temperatures)
• Maintaining all documentation, such as inventory and temperature logs
• Organizing vaccine-related training and ensuring sta completion of training
• Monitoring operation of vaccine storage equipment and systems
• Overseeing proper vaccine transport (when necessary) per SOPs
• Overseeing emergency preparations per SOPs:
— Tracking inclement weather conditions
†
— Ensuring appropriate handling of vaccines during a disaster or power outage
‡
Coordinator responsibilities may be completed by the coordinator or delegated to appropriate sta. Ensure the
coordinator has trained the delegate(s) and documented competency for the specific tasks assigned.
* This is a VFC provider requirement.
† The Federal Emergency Management Agency (FEMA) oers a wide range of information on disaster preparedness: www.fema.gov/. The Center
for Biologics Evaluation and Research (CBER) at the Food and Drug Administration (FDA) oers information concerning the storage and use of
temperature-sensitive biological products that have been involved in a temporary electrical power failure or flood conditions:
www.fda.gov/AboutFDA/CentersOces/OceofMedicalProductsandTobacco/CBER/.
‡ The National Oceanic and Atmospheric Administration (NOAA) provides up-to-date information on U.S. weather conditions:
www.weather.gov/
www.goes.noaa.gov/
Staff Training and
SOP Best Practices
» Review and update SOPs annually.
» Appoint an alternate vaccine coordinator to act
in the absence of the primary coordinator.
» The alternate coordinator, like the primary
coordinator, should be an expert in routine and
emergency SOPs.

9
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION THREE: Vaccine Storage and Temperature Monitoring Equipment
It is important your facility has proper storage and monitoring equipment that is set up correctly, maintained
appropriately, and repaired as needed. This equipment protects patients from inadvertently receiving compromised
vaccine and your facility against costs of revaccinating patients, replacing expensive vaccines, and losing patient
confidence in your practice.
Vaccine Storage Units: Refrigerator and Freezer Recommendations
There are several types of vaccine storage units available. Purpose-built units are specifically designed to store vaccines.
However, household-grade units are also an acceptable option for vaccine refrigeration under the right conditions.
Use purpose-built or pharmaceutical-grade units designed to either refrigerate or freeze. These units can be
compact, under-the-counter style or large.
Purpose-built units, sometimes referred to as “pharmaceutical-grade,” are designed specifically for storage of
biologics, including vaccines. These units often have:
• Microprocessor-based temperature control with a digital temperature sensor (thermocouple, resistance
temperature detector [RTD], or thermistor)
• Fan-forced air circulation with powerful fans or multiple cool air vents promoting uniform temperature and fast
temperature recovery from an out-of-range temperature.
Household-grade units can be an acceptable alternative to pharmaceutical-grade vaccine storage units. As the name
implies, these units are primarily designed and marketed for home use. However, the freezer compartment of this
type of unit is not recommended to store vaccines and there may be other areas of the refrigerated compartment that
should be avoided as well. If your facility provides frozen vaccine, a separate freezer unit is necessary.
Do not store any vaccine in a
dormitory-style or bar-style
combined refrigerator/freezer unit
under any circumstances.
These units have a single exterior
door and an evaporator plate/cooling
coil, usually located in an icemaker/
freezer compartment. These units pose
a significant risk of freezing vaccines,
even when used for temporary storage.
(Note: Not all small storage units are
dormitory- or bar-style units. Compact,
purpose-built units for biologics can be
used to store vaccines.)
Storage unit doors
A door that is not sealed properly or le open unnecessarily not only affects
the temperature in a unit, it also exposes vaccines to light, which can reduce
potency of some vaccines. Consider using safeguards to ensure the doors of
the unit remain closed—for example, self-closing door hinges, door alarms, or
door locks.
Storage Unit Best Practices
To fully ensure the safety of vaccines, equipment
should include a recommended unit with enough
space to accommodate your maximum inventory without crowding.

10
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION THREE: Vaccine Storage and Temperature Monitoring Equipment
Storage Unit Placement
Good air circulation around the outside of the storage unit is important. Place a storage unit in a well-ventilated room,
leaving space between the unit, ceiling, and any wall. Nothing should block the cover of the motor compartment. The
unit should be firm and level, with the bottom of the unit above the floor. Make sure the unit door opens and closes
smoothly and fits squarely against the body of the unit. If not secured properly, unit doors pose a particular risk to
maintaining appropriate internal temperatures of vaccine storage units. Studies find most units work best when placed
in an area with standard indoor room temperatures, usually between 20° C and 25° C (68° F and 77° F). Check the
manufacturer-supplied owner’s manual for additional guidance on placement and spacing.
You may see vendors use terms such as “VFC-compliant,” “CDC-compliant,” or “satisfies VFC requirements” in their marketing
materials or on their websites. In this context, "compliance" and related terms may lead consumers to incorrectly believe that
CDC or the VFC program has independently assessed and verified the quality of these products. CDC/VFC is not authorized to
assess, validate, verify, or endorse the products or services of private companies. Should you encounter this type of language in
vendor marketing materials, please keep in mind that neither CDC nor the VFC program has validated any product or service for
compliance with CDC or VFC program requirements or standards.
Stabilizing Temperatures in New and Repaired Units
It may take 2 to 7 days to stabilize the temperature in a newly installed or repaired refrigerator and 2 to 3 days for a freezer.
Before using a unit for vaccine storage, check and record the minimum and maximum temperatures each workday for
2 to 7 days. If temperatures cannot be recorded digitally, check and record temperatures a minimum of two times each
workday. Once you have 2 consecutive days of temperatures recorded within the recommended range, your unit is
stable and ready for use.
Temperature Ranges
Refrigerators should maintain temperatures between 2° C and 8° C (36° F and 46° F)
*
. Freezers should maintain
temperatures between -50° C and -15° C (-58° F and +5° F). Ultra-cold freezers should maintain temperatures between
-90° C and -60° C (-130° F and -76° F) . Refrigerator or freezer thermostats should be set at the factory-set or midpoint
temperature, which will decrease the likelihood of temperature excursions.
Consult the owner’s manual for instructions on how to operate the thermostat. Thermostats are marked in various
ways and, in general, show levels of coldness rather than temperatures. The only way to know the temperature where
vaccines are stored is to measure and monitor it with a temperature monitoring device.
Temperature Monitoring Device (TMD)
Every vaccine storage unit must have a TMD. An accurate temperature history that reflects actual vaccine
temperatures is critical for protecting your vaccines. Investing in a reliable device is less expensive than replacing
vaccines wasted due to the loss of potency that comes from storage at out-of-range temperatures.
CDC recommends a specific type of TMD called a “digital data logger” (DDL). A DDL provides the most
accurate storage unit temperature information, including details on how long a unit has been operating outside the
recommended temperature range (referred to as a “temperature excursion”). Unlike a simple minimum/maximum
thermometer, which only shows the coldest and warmest temperatures reached in a unit, a DDL provides detailed
information on all temperatures recorded at preset intervals.
Many DDLs use a buered temperature probe, which is the most accurate way to measure actual vaccine temperatures.
Temperatures measured by a buered probe match vaccine temperatures more closely than those measured by
standard thermometers, which tend to reflect only air temperature. However, not all DDLs can measure ultra-cold
temperatures. For accurate ultra-cold temperature monitoring, it is essential to use an air-probe or a probe designed
specifically for ultra-cold temperatures.
Temperature data from a DDL can either be downloaded to a computer using special software or retrieved from a
website. The software or website may also allow you to set the frequency of temperature readings. Reviewing DDL data
is critical for vaccine viability, so it is important to decide whether independent software or a website program works
best for your facility.
* Probes that are permanently embedded in a buer are acceptable as long as the temperature monitoring system for the entire unit can be
calibration-tested.

11
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION THREE: Vaccine Storage and Temperature Monitoring Equipment
Keep the data for 3 years so they can be analyzed for long-term trends and/or recurring problems. Those
receiving public vaccine may need to keep records longer as required by state regulations.
Use a DDL or other appropriate TMD for:
• Each vaccine storage unit
• Each transport unit (emergency or non-emergency)
Have at least one backup TMD in case a primary device breaks or malfunctions.
Use DDLs with the following features:
• Detachable probe that best reflects vaccine temperatures (e.g., a probe buered with glycol, glass beads, sand, or
Teflon®)
*
• Alarm for out-of-range temperatures
• Low-battery indicator
*
• Current, minimum, and maximum temperature display
†
• Recommended uncertainty of +/-0.5° C (+/-1° F)
• Logging interval (or reading rate) that can be programmed by the user to measure and record temperatures at
least every 30 minutes
Use DDLs with a current and valid Certificate of Calibration Testing.
Certificate of Calibration Testing
Calibration testing is done to ensure the accuracy of a temperature monitoring device’s readings against nationally
accepted standards.
A DDL’s Certificate of Calibration Testing should include:
• Model/device name or number
• Serial number
• Date of calibration (report or issue date)
• Confirmation that the instrument passed testing
(or instrument is in tolerance)
• Recommended uncertainty of +/-0.5° C (+/-1° F) or less
To determine if a Certificate of Calibration Testing or Report of Calibration was issued by an appropriate entity, check to
see if the certificate indicates one or more of the following items about calibration testing:
• Conforms to International Organization for Standardization (ISO)/International Electrotechnical Commission (IEC)
17025 international standards for calibration testing and traceability
• Performed by a laboratory accredited by International Laboratory Accreditation Cooperation (ILAC) Mutual
Recognition Arrangement (MRA) signatory body
• Traceable to the standards maintained by the National Institute of Standards and Technology (NIST)
• Meets specifications and testing requirements for the American Society for Testing and Materials (ASTM) Standard
E2877 Tolerance Class F or higher
• Refers to another acceptable accuracy validation method, such as comparison to other traceable reference standards or
tests at thermometric fixed points
Calibration testing should be done every 2 to 3 years or according to the manufacturer’s suggested timeline.
TMDs can experience a “drift” over time, aecting their accuracy. This testing ensures the accuracy of the device
continues to conform to nationally accepted standards.
Mishandling a TMD can aect its accuracy. If a TMD is dropped, hit against the side of a storage unit, or is potentially
damaged in any way, its accuracy should be checked against another calibrated TMD. If there is any question about
accuracy, the device should be replaced or sent for calibration testing.
* Since these devices are typically battery-operated, you should have a supply of extra batteries on hand. If you are storing ultra-cold vaccine,
make sure your DDL is appropriate for ultra-cold monitoring. See the COVID-19 Vaccine Storage and Handling Addendum for more
information.
† Battery changes may aect temperature accuracy and may warrant checking against a known, calibrated TMD. Check with the device’s
manufacturer for specific information on battery changes.

12
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION THREE: Vaccine Storage and Temperature Monitoring Equipment
Monitoring Vaccine Temperature and Vaccine Equipment
Monitoring vaccine storage equipment and temperatures are
daily responsibilities to ensure the viability of your vaccine
supply and the safety of your patients. Implementing routine
monitoring activities can help you identify temperature
excursions quickly and take immediate action to correct
them, preventing loss of vaccines and the potential need for
revaccination of patients.
Power Supply
Even with appropriate equipment and temperature
monitoring practices in place, power disruption can result in
destruction of the entire vaccine supply. Precautions should
always be taken to protect the storage unit’s power supply.
Plug in only one storage unit per electrical outlet to
avoid creating a fire hazard or triggering a safety
switch that turns the power o.
Use a safety-lock plug or an outlet cover to prevent the
unit from being unplugged.
Post “DO NOT UNPLUG” warning signs at outlets and
on storage units to alert sta, custodians, electricians,
and other workers not to unplug units.
Label fuses and circuit breakers to alert people not to
turn o power to a storage unit.
Use caution when using power outlets that can be
tripped or switched o and avoid using:
• Built-in circuit switches (may have reset buttons)
• Outlets that can be activated by a wall switch
• Multi-outlet power strips
If built-in circuit switches, Uninterruptible Power Supply (UPS) unit, or power strip surge protection must be used, make
sure the device is rated to carry the maximum current as specified by the manufacturer of the refrigerator or freezer.
Additionally, consider how the device manages when the power is restored. Whether the device automatically restarts and
allows the equipment to run or has to be manually switched on should be considered and represented in Emergency Plans
and SOPs. Contact the unit manufacturer for any additional questions or guidance regarding circuit switches, power strips,
UPI, or surge protection.
If the entire storage unit is aected by a temperature excursion because of a power supply issue or unit malfunction,
refer to your facility’s emergency SOPs.
Certain types of TMDs have significant limitations
and should not be used to measure temperatures
in a vaccine storage unit. These devices can be
difficult to read and, because they only show the
temperature at the exact time they are checked,
may fail to detect temperatures outside the
recommended range.
CDC does not recommend the following TMDs:
» Alcohol or mercury thermometers, even if placed
in a fluid-filled, biosafe, liquid vial
» Bimetal stem TMDs
» TMDs used for food
» Chart recorders
» Infrared TMDs
» TMDs that do not have a current and valid
Certificate of Calibration Testing
Please note: Some devices sold in hardware and
appliance stores are designed to monitor temperatures
for household food storage. They are not calibrated and
not accurate enough to ensure vaccines are stored within
the correct temperature range. Using these devices can
pose a significant risk of damaging vaccines.

13
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION THREE: Vaccine Storage and Temperature Monitoring Equipment
Organizing and Storing Vaccine
Correctly organizing and placing vaccines in a storage unit
helps prevent conditions that could reduce vaccine potency or
cause vaccine failure.
Store vaccines in their original packaging with lids closed
until ready for administration. Vials and manufacturer-filled
syringes should always be stored in their original packaging.
Loose vials or syringes may be exposed to unnecessary light,
potentially reducing potency, and may be more dicult to
track for expiration dates. They may also impact inventory
management and increase the risk of administration errors
because they may be confused with other vaccines. For
certain purpose-built units, it is recommended that vaccine be
stored outside of the packaging. If this is the case, follow the
manufacturer’s guidance for vaccine storage.
Check and record storage unit minimum and maximum
temperatures at the start of each workday. If your TMD
does not read minimum/maximum temperatures, then check
and record the current temperature a minimum of two times
per workday (at the start and end of the workday).
Record:
• Minimum/maximum temperature
• Date
• Time
• Name of person who checked and recorded the temperature
• Any actions taken if a temperature excursion occurred
If a reading is missed, leave a blank entry in the log.
Food and beverages should never be stored
in the unit with vaccines. If other biologics are
stored in the unit, vaccines should be stored
on the shelf above them.
Temperature Monitoring
Regular checks provide an
opportunity to inspect the
storage unit, reorganize any
misplaced vaccines, and remove any expired
vaccines. Check the temperature each time
vaccines are accessed in the unit.
Review storage unit temperature readings and
review continuous DDL soware or website
information weekly for changes in temperature
trends that might require action.
If there appears to be any fluctuation in
temperature, troubleshoot the problem based
on additional information provided in this
toolkit, manufacturer manuals, and/or your
office storage and handling SOPs.
How to Store Vaccines
Place water bottles on the top shelf and floor and in the door
racks. Putting water bottles in the unit can help maintain stable
temperatures caused by frequently opening and closing unit doors or
a power failure.
Water bottles are not recommended for use with certain
pharmaceutical-grade and purpose-built units. For such units, follow
the manufacturer’s guidance.
do not
unplug
14
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION THREE: Vaccine Storage and Temperature Monitoring Equipment
Organizing and Storing Vaccine
To confirm vaccines are stored correctly and to minimize the risk of administration errors, implement the following
practices:
» Store each type of vaccine or diluent in its original packaging and in a separate container.
» Position vaccines and diluents 2 to 3 inches from the unit walls, ceiling, floor, and door. If using a household-grade
unit, avoid storing vaccines and diluents in any part of the unit that may not provide stable temperatures or
sufficient air flow, such as directly under cooling vents; in deli, fruit, or vegetable drawers; or on refrigerator door
shelves. The instability of temperatures and air flow in these areas may expose vaccines to inappropriate storage
temperatures.
» Label shelves and containers to clearly identify where each type of vaccine and diluent is stored.
» Store vaccines and diluents with similar packaging or names or with pediatric and adult formulations on different
shelves.
» Whenever possible, store diluent with the corresponding refrigerated vaccine. Never store diluent in a freezer.
» Avoid placing or storing any items other than vaccines, diluents, and water bottles inside storage units.
• If other medications and biological products must be stored in the same unit as vaccines, they must be
clearly marked and stored in separate containers or bins from vaccines.
—Potentially contaminated items (e.g., blood, urine, stool) should be properly contained and stored below
vaccines due to risk of contamination from drips or leaks.
—The freezer of a household-grade unit may be used for non-vaccine, medical storage, so long as the use
does not compromise the temperature range within the refrigerator compartment where vaccine is stored.
» Arrange vaccines and diluents in rows and allow space between them to promote air circulation.
» Place vaccines and diluents with the earliest expiration dates in front of those with later expiration dates.

15
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION THREE: Vaccine Storage and Temperature Monitoring Equipment
Temperature Excursions
Temperature excursions or inappropriate storage conditions for any vaccine require immediate action. Any
temperature reading outside the recommended ranges in the manufacturers’ package inserts
*
is considered a
temperature excursion. In general, manufacturers analyze information about the magnitude of the temperature
excursion and the total amount of time that temperatures were out of range, as well as information about the vaccine in
question, to determine whether a vaccine is likely to still be viable.
CDC recommends the following steps in the event of a temperature excursion (see page 38):
1. Any sta who hears an alarm or notices a temperature excursion on the DDL should notify the primary or
alternate vaccine coordinator immediately or report the problem to their supervisor.
2. Notify sta by labeling exposed vaccines "DO NOT USE" and placing them in a separate container apart from
other vaccines (do not discard these vaccines).
3. The vaccine coordinator, supervisor, or if necessary, the person reporting the problem, should begin to document
the event with the following information
†
:
a. Date and time of the temperature excursion
b. Storage unit temperature as well as room temperature, if available (including minimum/maximum temperatures
during the time of the event, if available)
c. Name of the person completing the report and description of the event
‡
:
— General description of what happened
— The length of time vaccine may have been aected, if using a DDL
— Inventory of aected vaccines
— List of items in the unit (including water bottles) other than vaccines
— Any problems with the storage unit and/or aected vaccines before the event
— Other relevant information
4. Implement your facility SOPs to adjust unit temperature to the appropriate range. At a minimum, check the TMD
to make sure it is appropriately placed in the center of the vaccines.
5. Contact your immunization program and/or vaccine manufacturers per your SOPs for further guidance on whether
to use aected vaccines and for information about whether patients will need to be recalled for revaccination.
Be prepared to provide documentation of the event (e.g., temperature log data) to ensure you receive the best
guidance.
6. Complete your documentation of the event, including:
a. Action taken
— What you did with vaccine and how long it took to take action
— Whom you contacted and instructions received
— What you did to prevent a similar future event
b. Results
— Final disposition of aected vaccines (e.g., shortened expiration date per manufacturer, discarded, or returned)
— Other comments
* Manufacturers’ vaccine package inserts: www.immunize.org/fda/. Vaccines under an Emergency Use Authorization (EUA) will provide an EUA
Fact Sheet for Healthcare Providers with this information.
† The Immunization Action Coalition has developed a Temperature Monitoring Log and a Vaccine Storage Troubleshooting Record to support
these activities.
‡ Responses from vaccine manufacturers to events depend on information given by the provider to the manufacturer. If dierent information
about the same event is provided to the same manufacturer, this can lead to dierent recommendations on whether vaccine can be used or
whether patients need to be revaccinated. In addition, each event is unique, and manufacturer recommendations based on existing stability data
cannot be applied to future events that may appear to be similar.

16
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION THREE: Vaccine Storage and Temperature Monitoring Equipment
Regular Maintenance of Vaccine Storage Units and
Temperature Monitoring Devices
Storage units and TMDs need regular maintenance to ensure proper
operation.
Conduct routine maintenance for all vaccine storage units and
related equipment so that your equipment functions at maximum
eciency.
• Check seals and door hinges.
• Clean coils and other components per manufacturer direction.
• Defrost manual-defrost freezers when the frost exceeds either 1 cm or the manufacturer’s suggested limit. Follow
the manufacturer’s instructions. While defrosting, store vaccines temporarily in another unit with appropriate
freezer temperatures.
• Clean the interior of each unit to discourage bacterial and fungal growth. Do so quickly to minimize the risk of a
temperature excursion.
• Test any backup generator quarterly and have it serviced annually.
Never allow vaccines to remain in a
malfunctioning unit for an extended
period of time. If you believe your unit has
failed, implement your emergency SOPs.
Troubleshooting Equipment Problems
Adjusting Storage Unit Temperatures
Storage unit temperatures may need to be adjusted over time. In some situations, thermostats may need to be reset in
summer and winter, depending on room temperature.
Temperature adjustments should be:
• Made by the primary or alternate vaccine coordinator, based on information from the TMD and temperature
monitoring log
• Performed at a time that is not during a busy workday when the unit door is being frequently opened and closed
Remember that temperatures within any storage unit will vary slightly, even with normal use. Therefore, before making
any adjustment:
• Confirm the unit is securely plugged into a power source.
• Check the temperature inside the storage unit.
• Wait 30 minutes, without opening the door, to allow the temperature to stabilize and then check it again to determine
if the thermostat should be adjusted.
If you believe there could be an issue with your TMD, use your backup device to confirm the temperature.
If you confirm that an adjustment is needed:
1. Refer to the owner’s manual for detailed instructions.
2. Make a small adjustment toward a warmer or colder setting by turning the thermostat knob slowly to avoid going
outside the correct temperature range.
3. Once the adjustment is made, allow the temperature inside the unit to stabilize for 30 minutes without opening the
door.
4. Recheck the temperature.

17
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION THREE: Vaccine Storage and Temperature Monitoring Equipment
5. Repeat these steps as needed until the temperature has stabilized
— between 2° C and 8° C (36° F and 46° F) for a refrigerator,
— between -50° C and -15° C (-58° F and +5° F) for a freezer, and
— between -90° C and -60° C (-130° F and -76° F) for an ultra-cold freezer.
6. Consider placing additional water bottles in the unit to help improve temperature stability.
Do not leave vaccines in a storage unit that does not
maintain temperatures within the recommended range.
If you are unable to stabilize the temperature in your unit
within the required range, or temperatures in the unit are
consistently at the extreme high or low end of the range,
your vaccine supply is at high risk. Use your SOPs to
identify an alternative unit with appropriate temperatures
and sucient storage space until the primary unit can be
repaired or replaced.
If you are using a combination storage unit, note
that adjustments to the freezer temperature can
adversely affect the refrigerator compartment
temperature, possibly resulting in frozen vaccines in
the refrigerator.
Repeated Alarm Alerts
If the temperature alarm goes o repeatedly, do not disconnect the alarm until you have determined and addressed
the cause. Do basic checks of the unit door, power supply, and thermostat settings. If the alarm continues to trigger or
the temperature remains out of range, transfer vaccines to a backup unit as directed by your SOPs. A repair technician
should check your equipment to determine the need for repair or replacement.

18
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION FOUR: Vaccine Inventory Management
Proper vaccine inventory management is essential for appropriate vaccine ordering and stock rotation, and ensures
your facility has the vaccines your patients need. Vaccines are expensive, so making sure they are unpacked, stored,
prepared, administered, and transported correctly is critical.
Vaccine Delivery
Scheduling and Receiving Deliveries
Maintaining the cold chain is the first step in vaccine inventory management. Sta members who might accept
vaccine deliveries should be trained to immediately notify the vaccine coordinator or alternate coordinator when
deliveries arrive. Vaccines must always be immediately checked and stored properly upon arrival.
Unpacking Deliveries
Vaccines and diluents must be carefully unpacked, stored at
recommended temperatures, and documented immediately
after they arrive. Do not place an unopened and/or unpacked
shipment box in a vaccine storage unit because the cool packs
shipped with the vaccine may make the packaged vaccine too
cold if placed inside the storage unit.
Never leave a vaccine shipping container unpacked
and unattended. If vaccines and diluents get too
warm, they cannot be used. Be sure all staff knows
that vaccine deliveries require immediate attention.
Immediately examine shipments for signs of damage
and to guarantee receipt of the appropriate vaccine
types and quantities.
• Examine the shipping container and vaccines for signs
of physical damage.
• Check the contents against the packing list to be sure
they match.
— For frozen vaccines, the packing list will show the
maximum time vaccines can be in transit based on
shipment date.
• If the shipment includes lyophilized (freeze-dried)
vaccines, make sure they came with the correct type
and quantity of diluents.
• Immediately check both vaccine and diluent expiration
dates to ensure you have not received any expired or
soon-to-expire products.
• Immediately check the cold chain monitor (CCM), a
device used to monitor vaccine temperatures during
transport (if one was included) for any indication of a
temperature excursion during transit.
Stock Records
Use a stock record to account
for and document every dose of
vaccine. This record will help you keep track of your
inventory and can be in either paper or electronic
form. This record should be updated weekly and
include the vaccine delivery information below:
» Date of delivery and initials of the person who
unpacked the box
» Vaccine and diluent name and manufacturer
» Number and expiration date for each lot
» Number of doses received
» Condition of each vaccine and diluent upon
arrival
» CCM reading if included in the shipping
container
» Number of doses used
» Balance of remaining doses aer subtracting
the amount used
Note: State and local programs that have an
immunization information system (IIS) with vaccine
inventory accounting functions will require VFC
providers to use the IIS to track their inventory.
Vaccine Inventory Accounting
Stock Counts
Stock records are used to determine the type and amount
of vaccines your facility should stock to meet the needs of
your patients. At least once a month and before placing any
vaccine order, count all vaccine and diluent doses to make
sure the number of doses in the storage unit matches the
number of doses documented in the stock record. Always
check expiration dates while counting stock and remove any
expired doses immediately.

19
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION FOUR: Vaccine Inventory Management
Tally sheets can help keep stock records up-to-date. Place tally sheets outside the storage unit door (or another
easily accessible location), and have staff use tick marks to keep a count of every dose removed from the unit.
Tally Sheets
If the numbers in the storage unit do not match the doses documented in the stock record, enter the correct number
based on your count on a separate line below the old balance on your stock record. Make a note next to the new entry
indicating that your count confirmed the new balance and sign it. Use the corrected balance for calculating stock
quantities in the future.
If you receive multiple doses of the same vaccine in the same presentation from the same lot with the same expiration
date, you can document these doses as one entry on the stock record. Indicate the total number of doses received,
regardless of how many vials or syringes the doses came in. For example, if you receive 10 single-dose vials of the same
vaccine with the same lot number and expiration date, you can make a single entry on the stock record, noting that 10
doses were received.
If there are discrepancies between the contents and the packing list or other concerns about the contents, immediately
notify the vaccine manufacturer. If you are a VFC provider or receive vaccines purchased with public funds, contact
your immunization program.
*
Diluents should be documented on a separate stock record and should equal quantities of corresponding vaccines.
At the end of each month, determine the total number of vaccine and diluent doses used that month and the amount
of stock still available. At the end of each year, use your stock record to determine the number of doses received for
the year and add up your monthly dose counts to get a total number of doses used. This information will help you
determine your facility’s needs and guide you in ordering so you can minimize future waste and reduce the need for
transfer and transport of vaccines. It will also help to make sure you have a sucient supply to meet your patients'
needs.
Vaccine Ordering
Order and stock only enough vaccine to meet patient needs.
†
Storing a larger volume than your facility needs can increase the risk of wasting vaccines if they expire before they can
be used or they are compromised in some way (e.g., due to mechanical failure of a storage unit).
Most facilities should also reorder based on patient needs after checking stock count. Vaccine orders usually arrive
within 1 to 2 weeks, but there can be delays. When possible,
avoid placing last-minute or rush orders to lessen the risk of
running out of vaccines.
Stock Rotation and Removal
Vaccine stock should be rotated and checked for
expired doses regularly. Any expired vaccines and
diluents should be removed immediately to avoid
inadvertently administering them. Arrange stock
for each vaccine type so that doses with the earliest
expiration dates are placed in front of those with later
expiration dates.
Contact your immunization program* to find out if expired vaccines purchased with public funds can be returned.
* Contact your immunization program for details about specific state or local regulations impacting this activity.
† An adequate supply of vaccine varies for most providers, facilities, or immunization programs. It is recommended that reordering is done when
stock has been reduced to a 4-week inventory.
Arranging Your Stock
The vaccine coordinator (or other
designated person) should rotate vaccine and
diluent stock at least once a week, as well as each
time your facility receives a vaccine delivery. This will
ensure that vaccines expiring sooner are used first.
20
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION FOUR: Vaccine Inventory Management
Understanding Expiration Dates
All vaccine products, like other medications, have an expiration date,
sometimes referred to as the expiry date. The expiration date is
determined by the manufacturer.
The expiration date is the final day that the vaccine can be
administered. Vaccines past the expiration date should NEVER be used.
Determining when a vaccine or diluent expires is a critical step in
maintaining proper storage and handling. Understanding vaccine
expiration dates can help save your practice time and money.
When the expiration date has only a month and year, the product may be used up to and including the last day of that
month. If a day is included with the month and year, the product may only be used through the end of that day.
In some instances, such as the examples for beyond-use date (BUD) below, vaccines must be used before the
expiration date on the label.
Beyond-Use Dates
Some vaccines have a beyond-use date/time. The Beyond-use date is different from expiration date. The beyond-
use date, or BUD, is the last date or time that a vaccine can be safely used aer it has been moved from one storage
state to another (e.g., frozen to refrigerated) or prepared for patient use. It is a new deadline aer which the product
should not be used. The BUD varies by product and type of transition. This is sometimes also called a beyond-use
time if it falls on the same day at a different time of day.
Unlike the expiration date that is determined by the manufacturer, the BUD is determined by the health care provider
using guidance provided by the manufacturer. The BUD replaces the manufacturer’s expiration date but never
extends it. Always use the earlier date between the two.
Not all vaccine products have a BUD. The package insert or Emergency Use Authorization (EUA) Fact Sheet for
Healthcare Providers will specify if there is a BUD and how to calculate it. Always review this informational material
to determine if a BUD applies. Examples of BUD include:
Reconstituted vaccines have a limited period for use once the vaccine is mixed with a diluent. If a reconstituted
vaccine is not used immediately, follow manufacturer guidance for storage conditions and time limits. Additional
information can be found here.
Multidose vials might have a specified period for use once they have been punctured with a needle. For example, the
package insert may state that the vaccine must be discarded 28 days aer the first puncture with a needle. If the vial
is first punctured on 06/01/2023, the BUD is 06/29/2023. The vaccine should not be used aer the BUD.
Manufacturer-shortened expiration dates may apply when vaccine is exposed to inappropriate storage conditions.
The manufacturer might determine the vaccine can still be used, but will expire on an earlier date than the date on
the label. The BUD should be noted on the vial label along with the initials of the person making the calculation.
Expiration Dates
The vaccine
coordinator (or other
designated person) should remove
expired vaccine and diluent immediately
from the inventory.
Vaccine Disposal
General vaccine disposal guidelines for:
• Expired or compromised vaccine—sometimes unused vaccine and diluent doses, unopened vials, expired vials,
and potentially compromised vaccine may be returned for credit, even if they must be discarded. Contact your
immunization program
*
and/or the vaccine manufacturer for vaccine-specific information.
• Open and broken vials and syringes, manufacturer-filled syringes that have been activated, and vaccine
predrawn by providers—these cannot be returned and should be discarded according to your state requirements.
• Empty vaccine vials—most are not considered hazardous or pharmaceutical waste and do not require disposal in a
biomedical waste container.
†
However, check and comply with your state requirements for disposal.
Medical waste disposal requirements may vary from state to state because they are set by state environmental agencies.
Contact your immunization program
*
or state environmental agency for guidance to ensure your facility’s vaccine
disposal procedures comply with state and federal regulations.
* Contact your immunization program for details about specific state or local regulations impacting this activity.
† While vials are not usually considered hazardous or pharmaceutical waste, an empty RV dispensing tube or oral applicator is considered medical
waste and should be disposed of in a medical waste container.
21
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION FIVE: Vaccine Preparation
Preparing Vaccine for Administration
Vaccine preparation is the final step in the cold chain before administration. Handling vaccines with care is equally as
important as storing them properly.
Vaccine Preparation
» Prepare vaccines in a designated area away from any space where potentially contaminated
items are placed.
» Only prepare vaccines when you are ready to administer them.
» Before preparing the vaccine, always check the:
— Vial to ensure it is the correct vaccine
— Expiration date or beyond-use date/time to ensure it has not passed
» Always check expiration dates and confirm that you have selected the correct vaccine.
» Only administer vaccines you have prepared. This is a quality control and patient safety issue and a best
practice standard of medication administration.
Different types of vaccine vials
Single-Dose Vials
A single-dose vial (SDV) contains one dose and should be used one time for one patient. SDVs do not contain
preservatives to help prevent microorganism growth. Never combine leover vaccine from one SDV with another to
obtain a dose.
Only open an SDV when ready to use. Before you remove the protective cap, always check the vial to make sure you have
the correct vaccine. Once you remove the cap, you must use the vaccine because it may not be possible to determine if
the rubber seal has been punctured. Discard any unused SDVs without a protective cap at the end of the workday.
Multidose Vials
A multidose vial (MDV) contains more than one dose of vaccine. Because MDVs typically contain a preservative to help
prevent the growth of microorganisms, they can be entered or punctured more than once. Only the number of doses
indicated in the manufacturer’s package insert should be withdrawn from the vial. Aer the maximum number of doses
has been withdrawn, the vial should be discarded, even if there is residual vaccine or the expiration date has not been
reached.
MDVs can be used until the expiration date printed on the vial unless the vaccine is contaminated or compromised in
some way or there is a BUD noted in the package insert.
Never use partial doses from two or more vials to obtain a dose of vaccine.
Based on safe injection practices, CDC does NOT recommend the use of vial adapters, spikes, or other vial access
devices when withdrawing vaccine from a multidose vial. Leaving a vial access device inserted into a vial septum provides
a direct route for microorganisms to enter the vial and contaminate the fluid.
Manufacturer-Filled Syringes
A manufacturer-filled syringe (MFS) is prepared and sealed under sterile conditions by the manufacturer. Activate an
MFS (i.e., remove the syringe cap or attach the needle) only when ready to use.
An MFS does not contain a preservative to help prevent the growth of microorganisms. Once the sterile seal has been
broken, the vaccine should be used or discarded by the end of the workday.
22
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION FIVE: Vaccine Preparation
Reconstitution of Vaccine
Lyophilized (freeze-dried) vaccines are in either powder or pellet form and must be mixed with a liquid (diluent) in a
process known as “reconstitution” before being administered.
Diluents vary in volume and composition and are specifically designed to meet volume, pH balance, and the chemical
requirements of their corresponding vaccines. Refer to the manufacturer’s package insert for guidance on storage and
handling.
Diluents are not interchangeable unless specified by the manufacturer.
• Some diluents contain an antigen or an adjuvant needed for vaccine eectiveness. Even if the diluent is composed of
sterile water or saline, use only the diluent supplied with the vaccine to reconstitute it.
Never use a stock vial of sterile water or normal saline to reconstitute vaccines.
Never administer vaccine reconstituted with the wrong
diluent.
• If an incorrectly reconstituted vaccine has already been
administered, contact your immunization program
*
or
the vaccine manufacturer for revaccination guidance.
* Immunization programs: www.cdc.gov/vaccines/imz-managers/
awardee-imz-websites.html
Always check expiration dates on both diluents
and vaccines before reconstituting them.
†
† If you are a VFC provider or have other vaccines purchased
with public funds and must transfer vaccine to another facility
so it can be used before it expires, contact your immunization
program
*
for guidance on vaccine transport.
Predrawing Vaccine
Predrawing vaccines can result in waste if more are drawn up than
needed.
Draw up vaccines only at the time of administration. The
practice of prefilling syringes is discouraged for several reasons.
However, there may be rare instances when the only option is to
predraw vaccine.
If vaccines must be predrawn, adhere to the following best practices:
• Set up a separate administration station for each vaccine type to
prevent medication errors.
• Draw up vaccines only after arriving at the clinic site or mass
vaccination event. Drawing up doses days or even hours before
administering them is not a best practice because general-use
syringes are not designed for storage.
• Each person administering vaccines should draw up no more than
one MDV or 10 doses at one time.
• Once each predrawn dose is prepared, label the syringe with the vaccine name and dosage, the beyond-use date and
time, lot number, and the preparer’s initials. Additional pertinent information can be added, such as age range or
primary or booster dose, as needed.
• Monitor patient flow to avoid drawing up unnecessary doses.
• Predraw reconstituted vaccine into a syringe only when you are ready to administer it. If a predrawn vaccine is not
used within 30 minutes of being reconstituted, follow manufacturer guidance for storage conditions and time limits.
A manufacturer may specify that an unused reconstituted vaccine can only be stored in the vial for a specified
amount of time.
• Predrawn syringes must be stored at the manufacturer-recommended temperatures throughout the clinic day.
• Discard any remaining vaccine in predrawn syringes at the end of the workday.
Never transfer predrawn reconstituted vaccine back into a vial for storage.
As an alternative to predrawing vaccines, use manufacturer-filled syringes for large vaccination clinics.

23
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION SIX: Routine Vaccine Transport
Instruction for routine transport of some vaccine may vary. Carefully review manufacturer guidance for each vaccine
product to ensure the cold chain is maintained.
Transport, as described in this section, involves the movement
of vaccine between providers or other locations over a short
distance and time frame and is appropriate for events such
as o-site clinic or to ensure vaccines that are about to expire
can be used rather than wasted.
General Principles of Transport
Vaccine transport to o-site or satellite facilities is dierent
from both shipping and emergency transport. Shipping
usually involves a professional carrier and a longer distance
and time frame for moving vaccines between locations.
Protecting Your Vaccine Supply
» Vaccine that will be used at
an off-site or satellite facility
should be delivered directly to that facility.
» When delivering to a specific site, adequate
storage equipment and staff should be in
place to provide appropriate oversight.
» If the facility doesn’t have the capacity to
refrigerate the vaccines, then a portable
vaccine storage unit or qualified container
and packout may be used with a DDL.
» If delivery to the specific site is not possible,
then vaccine can be transported in a stable
storage unit and monitored with a TMD.
» If the facility doesn’t have the capacity to
refrigerate the vaccines, then a portable
vaccine storage unit or qualified container
and packout may be used with a DDL.
» Develop an emergency plan or SOPs for
transporting vaccines and include procedures
and protocols for packing and transport.
Vaccine Transport
Vaccines from your supply should not be routinely
transported. In instances where the transport of vaccine
from your supply is necessary, take appropriate precautions
to protect your supply. Vaccines should only be transported
using appropriate packing materials that provide the
maximum protection.
Partially used vials cannot be transferred
between providers OR across state lines.
**
* Contact your immunization program for details about
specific state or local regulations impacting this activity.
The total time for transport alone or transport plus
clinic workday should be a maximum of 8 hours
†
unless guidance from the manufacturer diers (e.g.,
if transport to an o-site clinic is 1 hour each way, the
clinic may run for up to 6 hours).
Use a transport temperature monitoring log to
document temperatures and how long the vaccine is in
the portable storage container.
Transport diluents with their corresponding vaccines
to ensure there are always equal amounts of vaccines
and diluents for reconstitution.
Your facility should have a sucient supply of
materials needed for vaccine transport of your largest
annual inventory. Appropriate materials include:
• Portable vaccine refrigerator/freezer/ultra-cold freezer units (preferred option)
• Qualified containers and packouts
• Coolant materials such as phase change materials (PCMs) or frozen water bottles that can be conditioned
between 4° C and 5° C (39° F and 41° F)
• Insulating materials such as bubble wrap and corrugated cardboard—enough to form two layers per container
TMDs for each container between 4° C and 5° C (39° F and 41° F)
† COVID-19 vaccine transport times may be dierent. Refer to product inserts for vaccine specific information.
24
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION SIX: Routine Vaccine Transport
Soft-sided containers specifically engineered for vaccine transport are acceptable. Do not use commercially available soft-
sided food or beverage coolers because most are poorly insulated and likely to be aected by room or outdoor temperatures.
The same shipping materials the vaccines were initially shipped in should rarely, if ever, be used as they are not meant for
reuse. This could put the cold chain and, ultimately, the viability of the vaccine, at risk.
Transport of Vaccines
It is always safest to have vaccines delivered directly to a facility with a vaccine storage unit ready to receive
the shipment, but this is not always possible. If necessary, vaccines may be transported using a portable vaccine
refrigerator with a temperature monitoring device placed with the vaccines. If a portable vaccine refrigerator is not
available, qualified containers and packouts with a TMD in each container can be used. For transport to an o-site
clinic, bring only what is needed for the workday.
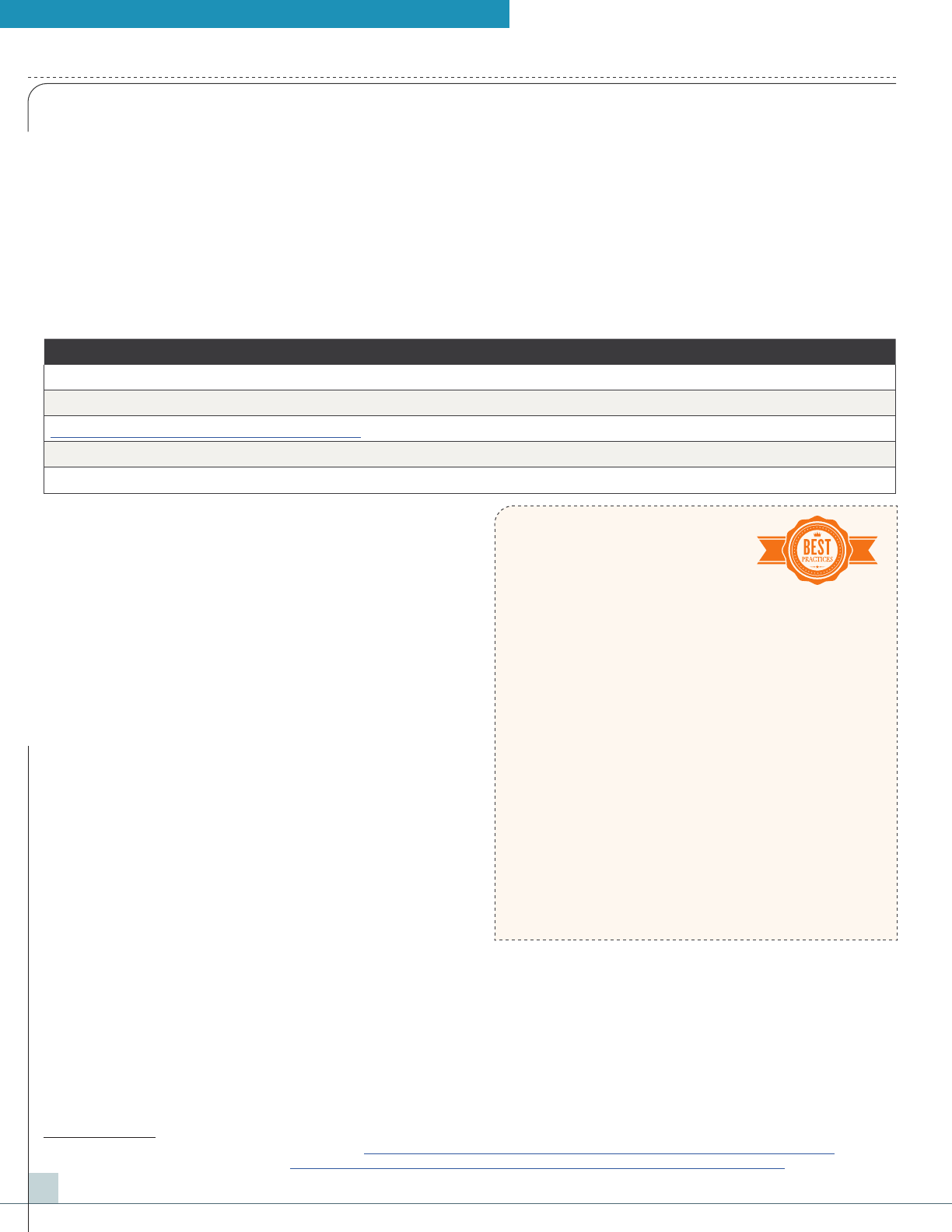
Routine Transport System Recommendations
Container Transport for Off-Site Clinic, Satellite Facility, or Relocation of Stock
Portable Vaccine Refrigerator or Freezer Yes
Qualified Container and Packout Yes
Conditioned Water Bottle Transport System
*
No
Manufacturer’s Original Shipping Container No
Food/Beverage Coolers No
Coolants for Transport
PCMs between 4° C and 5° C (39° F and 41° F) can also be
purchased to maintain proper temperatures. Follow the
manufacturer’s instructions
†
for use to reduce the risk of
freezing vaccines during transport.
Do not use frozen gel packs or coolant packs from
original vaccine shipments to pack refrigerated vaccines.
They can still freeze vaccines even if they are conditioned or
appear to be “sweating.”
Transport Planning and Preparation
Improper packing for transport is as risky for vaccines as a
failed storage unit.
Include vaccine packing and transport protocols in
your routine and emergency storage. At a minimum,
include the following procedures and protocols:
For all sta-facilitated transport:
• Identify trained sta to pack vaccines as well as
primary and backup vehicles and drivers for transport
in advance.
• Consider renting a refrigerated truck if you have a
large quantity of vaccines or need to transport vaccines
an extended distance.
• Take an inventory of your vaccines and record actions to protect the vaccines during transport.
• Open unit doors only when necessary and only after completing all preparation for packing and moving vaccines.
• If using a company or personal vehicle, only transport vaccines inside the passenger compartment (not in the
trunk or bed of a truck, which may be too hot or too cold).
• Move transport containers directly to a vehicle that is already at a comfortable temperature, neither too hot nor too cold.
* Packing Vaccines for Transport during Emergencies: www.cdc.gov/vaccines/hcp/admin/storage/downloads/emergency-transport.pdf
† Manufacturers’ vaccine package inserts: www.fda.gov/vaccines-blood-biologics/vaccines/vaccines-licensed-use-united-states
Transporting mRNA Vaccines
» Transport vials in the tray/
carton whenever possible.
» Protect vials as much as possible from drops,
shocks, and vibration.
» Secure storage containers during transport.
» Protect from light. Avoid exposure to direct
sunlight and ultraviolet light.
If individual vials must be transported:
» Place vials with padding materials like bubble
wrap or similar materials to prevent breaking.
» Keep vaccine vials upright whenever possible.
» Label the container and vials, appropriately
including beyond-use date/time.
» Transport vaccine in vials.
» Refer to the manufacturer package insert for
additional guidance.

25
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION SIX: Routine Vaccine Transport
• Avoid leaving containers in areas where they are exposed to direct sunlight.
• Check vaccine temperature upon arrival at the alternative vaccine storage facility and store vaccines at
recommended temperatures immediately.
• Check with your immunization program
*
for additional guidance and resources on emergency transport of
vaccines, particularly in major emergencies.
Transporting Opened Multidose Vials
If absolutely necessary, a partially used vial may be transported to or from an o-site/satellite facility operated by the
same provider, as long as the cold chain is properly maintained. However, a partially used vial cannot be transferred
from one provider to another or across state lines.
Transporting Predrawn Syringes
CDC recommends transporting vaccine in vials. However, there may be instances when the only option is to transport
predrawn vaccine in a syringe. For example, MFSs are recommended for large vaccination clinics, however, there may
be rare instances when the only option is to predraw vaccine for o-site clinics.
Transporting Diluents
Transport diluents with their corresponding vaccines so there are always equal amounts of vaccines and diluents for
reconstitution. Follow the manufacturer’s guidance
†
for specific temperature requirements.
If diluents stored at room temperature (20° C to 25° C [68° F to 77° F]) are going to be transported with refrigerated
vaccines, they should be refrigerated in advance for as long as possible so they do not raise the container temperature
when placed with refrigerated vaccines.
Never freeze diluents—not even during transport.
Place an insulating barrier like bubble wrap between the diluents and conditioned water bottles or phase change materials.
Transporting Frozen Vaccines
If frozen vaccines must be transported, use a portable vaccine freezer unit or qualified container and packout
that maintains temperatures between -50° C and -15° C (-58° F and +5° F) or -90° C and -60° C (-130° F and -76° F)
for ultra-cold transport.
Follow these steps for transporting frozen vaccines:
• Place a TMD (preferably with a buered probe) in the container as close as possible to the vaccines.
• Immediately upon arrival at the destination, unpack the vaccines and place them in a freezer at a temperature range
between -50° C and -15° C (-58° F and +5° F) or -90° C and -60° C (-130° F and -76° F) for ultra-cold freezer storage.
Any stand-alone freezer that maintains these temperatures is acceptable.
• Record the time that vaccines are removed from the storage unit and placed in the transport container, the
temperature during transport, and the time at the end of transport when vaccines are placed in a stable storage unit.
Do not use dry ice, even for temporary storage
‡
. Dry ice might expose the vaccines to temperatures colder than -50° C (-58° F).
* Immunization programs: www.cdc.gov/vaccines/imz-managers/awardee-imz-websites.html
† Manufacturers’ vaccine package inserts: www.fda.gov/vaccines-blood-biologics/vaccines/vaccines-licensed-use-united-states
‡ The only exception to this is for transport of COVID-19 Vaccine (Pfizer) which can be transported at ultra-cold temperatures using dry ice.

26
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION SIX: Routine Vaccine Transport
Temperature Monitoring During Transport
Regardless of how the vaccine is moved (i.e., car, professional carrier, snowmobile, boat, small plane), if vaccines are
packed by health care provider, the BUD should be applied using manufacturer guidance.
Use a continuous TMD, preferably a DDL with the capability to measure minimum/maximum temperatures, for
monitoring and recording temperatures while transporting vaccines:
• The TMD should have an accuracy of +/-0.5° C (+/-1° F).
• Place buered probe material in a sealed vial directly with the vaccines.
• Keep the TMD display on top of vaccines so you can easily see the temperature.
• Record the time and minimum/maximum temperature at the beginning of transport.
Temperature Monitoring after Transport
Immediately upon arrival at the destination, vaccines should be stored in an appropriate storage unit with a
TMD. Be sure to follow these guidelines for monitoring and recording storage unit temperature:
• If the device displays minimum/maximum temperatures, this information should be checked and recorded.
• If the device does not display minimum/maximum temperatures, then the current temperature should be
checked and recorded a minimum of two times (at the start and end of the workday).
If vaccines cannot be stored in an on-site storage unit, they should be kept in the portable vaccine storage unit using
the following guidance:
• If using a DDL that records minimum/maximum temperatures, only check and record temperatures each time
the portable vaccine storage unit is opened. If the TMD measures current temperatures only, place the probe as
close as possible to the vaccines, and check and record temperatures hourly.
• Keep the container closed as much as possible.
• For o-site clinic use, remove only one multidose vial or 10 doses at a time for preparation and administration
by each person administering vaccines.

27
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION SEVEN: Emergency Transport Vaccine Storage and Handling
Instructions for handling vaccine products during an emergency may be dierent from those for other vaccines.
Carefully review this section as well as the manufacturer guidance to ensure the vaccine cold chain is maintained
during an emergency.
Emergencies like equipment failures, power outages, severe
weather conditions, or natural disasters usually happen without
warning and may compromise vaccine storage conditions. In
addition to vaccine transport planning, you should make plans to
prepare for emergencies.
*
Vaccine Transport During Emergencies
Emergency transport usually involves relocating vaccines
to protect them when a facility’s ability to store vaccines is
compromised (e.g., because of power loss). Depending on the
situation, some general principles of vaccine transportation
recommendations may be the same, but there are also some
dierences such as:
• A system using conditioned water bottles can be used during
emergency situations.
• Manufacturers’ original shipping containers may also be used
as a last resort in an emergency situation.
• Hard-sided insulated containers or Styrofoam™ (Use in
conjunction with the Packing Vaccines for Transport during
Emergencies
†
tool can be used only in an emergency.
*The Center for Biologics Evaluation and Research (CBER) at the Food and Drug Administration (FDA) oers information concerning the storage
and use of temperature-sensitive biological products that have been involved in a temporary electrical power failure or flood conditions:
www.fda.gov/BiologicsBloodVaccines/SafetyAvailability/ProductSecurity/ucm147243.htm.
† Packing Vaccines for Transport during Emergencies: www.cdc.gov/vaccines/hcp/admin/storage/downloads/emergency-transport.pdf
Vaccines may remain inside a nonfunctioning
unit as long as appropriate temperatures are
maintained. Monitor your DDL to determine
when additional action should be taken.
If an alternative vaccine storage
facility is not available
If you cannot find an alternative vaccine
storage facility within a reasonable distance,
or if you cannot reach your alternative facility,
you can use portable vaccine refrigerator/
freezer units (if power source is available),
qualified containers and packouts, or a hard-
sided insulated container or Styrofoam™ using
the Packing Vaccines for Transport during
Emergencies tool. Always place a TMD with
the vaccines and carefully monitor the TMD to
ensure vaccines remain within the appropriate
temperature range. Temporary storage
containers should remain closed, and vaccines
can only be stored safely for as long as the
containers are validated to maintain proper
storage temperatures.
The Packing Vaccines for Transport during
Emergencies tool
†
describes a system in which
properly conditioned frozen water bottles
can be used as a coolant when transporting
vaccines during emergency situations.
Container
Transport for Off-Site
Clinic, Satellite Facility, or
Relocation of Stock
Portable Vaccine Refrigerator
or Freezer
Yes
Qualified Container
and Packout
Yes
Conditioned Water Bottle
Transport System
†
Yes
Manufacturer’s Original
Shipping Container
Yes
(last resort only)
Food/Beverage
Coolers
No

28
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION SEVEN: Emergency Transport Vaccine Storage and Handling
Emergency Equipment Backup Options
Alternative Storage Facility
No piece of vaccine storage equipment is infallible. At
some point, equipment will fail because of a power outage,
breakdown, or normal wear and tear.
Establish a working agreement with at least one
alternative storage facility even if you have a generator
as backup equipment. Make sure you have 24-hour access
to this facility. Hospitals, long-term care facilities, state
depots, the Red Cross, fire stations, packing plants, grocery
stores, funeral homes and commercial pharmacies are
some of the facilities that may be able to assist you.
Ensure the alternative storage facility has a dedicated unit
or shared space that can maintain temperatures at the
appropriate range. Note that shared spaces may not be able to
maintain temperatures at the recommended ranges for your
vaccine supply.
Your facility may also choose to have a backup storage unit so
that vaccine may not have to be packed and/or moved to an
alternative storage facility if the primary storage unit fails.
Temperature monitoring at alternative storage sites:
Vaccine temperature should be maintained when stored at an alternative facility during an emergency. Temperatures
should be monitored and documented in temperature logs when storing vaccines during an emergency. Sometimes
getting temperature logs before an emergency is not feasible. However, provider should confirm that the emergency
unit can maintain the required vaccine temperature range between 2-8°C. This could be completed by locating the
specifications for the make/model of the storage unit online.
Accessing Your Building after Hours
Ensure the alternative storage facility has a dedicated unit or shared space that can maintain temperatures at the
appropriate range. Note that shared spaces may not be able to maintain temperatures at the recommended ranges for your
vaccine supply.
Emergency situations can arise outside of normal business hours, so maintain a relationship with your facility’s building
manager and/or security sta. Ensure all sta members are familiar with emergency SOPs, including after-hours roles and
responsibilities.
Your facility’s storage and handling SOPs should include instructions for accessing your vaccine storage units
when the building is closed, with a building map/diagram and locations of:
• Spare batteries
• Flashlights
• Keys
• Locks
• Circuit breakers
• Emergency transport equipment and materials
Keep information on after-hours building access and security procedures with SOPs and with building management
and security sta, if appropriate, and also make sure relevant sta has copies of this information available at home.
Generators and backup battery
power sources
Having an on-site generator prevents the need to
transport vaccines to an alternative storage facility
during a power outage.
» Keep sufficient fuel on hand to continuously run
the generator for at least 72 hours.
» A generator should be tested quarterly and
serviced annually.
A backup battery power source can be used in lieu
of a generator.
» Backup battery power sources should be tested
quarterly and serviced annually.
» Check the manufacturer’s guide for testing.
29
VACCINE STORAGE AND HANDLING TOOLKIT
SECTION SEVEN: Emergency Transport Vaccine Storage and Handling
Power Outages
Monitoring Unit Temperature during a Power Outage
If your storage unit has an external temperature monitoring
display that you can check without opening the unit door, take the
following steps:
• Record room temperature (if possible) and the temperature
inside the unit as soon as the power goes out.
• Record minimum and maximum temperatures reached inside
the unit during the outage.
• Temperature excursions should be avoided, if possible, by using emergency plans and SOPs for transport and
alternative storage. However, if temperatures have fallen outside of the recommended range, follow your procedures
for temperature excursions.
If you cannot monitor the temperature inside the unit without opening the door and you do not have an alternative
facility with power where the vaccines can be stored or other emergency vaccine storage SOPs, wait until power is
restored and then take the following steps:
• Record the room temperature (if possible) and the temperature inside the unit.
• If using a DDL, document the length of time the power was o and the minimum and maximum temperatures during
that period.
• If temperatures inside the unit have already fallen outside of the recommended range, follow your procedures for
temperature excursions. Even if an excursion has occurred, move your vaccines to an alternative storage unit or
location where they can be stored at appropriate temperatures, if possible. Make sure to separate and mark these
vaccines “Do NOT Use” until a decision can be made about whether the vaccines can still be used.
During a power outage, only open the
storage unit door if:
» Power is restored.
» It is determined that the vaccines need to
be packed in separate storage containers
and/or transported to an alternative
storage facility.
30
VACCINE STORAGE AND HANDLING TOOLKIT
Glossary
Buffered temperature probe Temperature probe designed to prevent false readings by protecting
the thermometer from sudden changes in temperature that can
occur when opening a refrigerator door. A probe is “buffered” by
immersing it in a vial filled with liquid (e.g., glycol, ethanol, glycerin),
loose media (e.g., sand, glass beads), or a solid block of material (e.g.,
Teflon®, aluminum).
Beyond-use date (BUD) The date or time aer which a vaccine should not be administered,
stored, or transported. The BUD should never exceed the
manufacturer’s original expiration date.
Calibration Professional measurement of the accuracy of a temperature
monitoring device’s readings against nationally accepted standards.
Cold chain monitor (CCM) Generally, a single-use device that monitors the temperature inside
a vaccine shipping container. CCMs should be thrown away aer
being checked. CCMs are stored in a separate compartment of the
shipping container (a CCM may not be included when vaccines are
shipped directly from the manufacturer).
Conditioned water bottles Frozen water bottles that have been submerged under lukewarm
water until the ice block inside can spin freely.
Digital data logger (DDL) An electronic device that records data digitally over time or in
relation to location either with a built-in or external instrument or
sensor.
Diluent A diluting agent (e.g., a liquid) added to reconstitute lyophilized
vaccine before administration. Manufacturers of these vaccines also
supply the matching diluent.
Dormitory-style (bar-style) storage
unit
A combination refrigerator/freezer unit with one exterior door and
an evaporator plate (cooling coil), which is usually located inside an
icemaker compartment (freezer) within the refrigerator. These units
have been shown to pose a significant risk of freezing vaccines, even
when used for temporary storage.
Fan-forced air circulation Technology using powerful fans or multiple cool air vents inside the
unit that promote uniform temperature and fast temperature
recovery.
Household-grade storage unit A storage unit that is primarily sold for home use.
Lyophilized Freeze-dried; usually referring to a vaccine that is freeze-dried into a
powder or wafer.
Minimum/maximum temperature A vaccine storage unit’s coldest and warmest temperature readings
during a set period of time.
31
VACCINE STORAGE AND HANDLING TOOLKIT
Glossary
Phase change materials (PCMs) Engineered packing supplies that help control container
temperatures during vaccine transport or shipping.
Portable vaccine storage unit A type of powered refrigerator or freezer unit specifically designed
for use during vaccine transport. These are passive units that require
a power source to function. Please note that some active units are
“qualified” to maintain desired temperatures for a set amount of time
in the event of a power loss.
Potency A vaccine’s strength or effectiveness; in the context of this toolkit,
potency refers to a vaccine’s response to environmental conditions.
Presentation Type of packaging for a vaccine (e.g., single-dose vial, multidose vial,
manufacturer-filled syringe, etc.).
Purpose-built /pharmaceutical-grade
unit
Unit that are specifically designed to store vaccines.
Qualified container and packout A type of container and supplies specifically designed for use
when packing vaccines for transport. They are containers that are
“qualified” through laboratory testing under controlled conditions
to ensure they achieve and maintain desired temperatures for a set
amount of time.
Standard operating procedures
(SOPs)
A set of step-by-step instructions compiled by an organization to
help workers carry out complex routine or emergency operations.
SOPs aim to achieve efficiency, quality output, and uniformity of
performance, while reducing miscommunication and preventing
failure to comply with industry regulations and best practices.
Stand-alone storage unit A storage unit that operates independently of any other device or
system for its desired function (i.e., a refrigerator that only functions
as a refrigerator or a freezer that only functions as a freezer).
Temperature excursion Any temperature reading that is outside the recommended range for
vaccine storage as defined in the manufacturer’s package insert.
Tolerance Compliance with nationally accepted standards for the calibration
limits of temperature monitoring equipment. The equipment can
either be considered “in” or “out” of tolerance.
Traceability An unbroken chain of measurements and associated uncertainties.
Uncertainty The quantification of the doubt about the measurement result.
