
On July 12, 2018, the Centers for Medicare and Medicaid Services (CMS) released the proposed
2019 Medicare physician fee schedule and quality payment program, combining these 2 rules
for the first time. This occurred in a milieu of changing regulations that have been challenging
for interventional pain management specialists. The Affordable Care Act (ACA) continuous to be
amended by multiple administrative changes. This July 12th rule proposes substantial payment
changes for evaluation and management (E&M) services, with documentation requirements, and
blending of Level II to V CPT codes for E&M into a single payment. In addition, various changes in
the quality payment program with liberalization of some metrics have been published. Recognizing
that there are differing impacts based on specialty and practice type, as a whole interventional
pain management specialists would likely see favorable reimbursement trends for E&M services
as a result of this proposal. Moreover, in comparison with recent CMS final ruling, this proposed
rule has relatively limited changes in procedural reimbursement performed in a facility or in-office
setting.
CMS, in the new rule, has proposed an overhaul of the E&M documentation and coding system
ostensibly to reduce the amount of time physicians are required to spend inputting information into
patients’ records. The new proposed rule blends Level II to V codes for E&M services into a single
payment of $93 for office outpatient visits for established patients and $135 for new patient visits.
This will also have an effect with blended payments for services provided in hospital outpatients.
CMS also has provided additional codes to increase the reimbursement when prolonged services are
provided with total reimbursement coming to Level V payments. Interventional pain management-
centered care has been identified as a specialty with complexity inherent to E&M associated with
these services.
Among the procedural payments, there exist significant discrepancies for the services performed
in hospitals, ambulatory surgery centers (ASCs), and offices. A particularly egregious example
is peripheral neurolytic blocks, which is reimbursed at 1,800% higher in hospital outpatient
department (HOPD) settings as compared with procedures done in the office. The majority of
hospital based procedures have faced relatively small cuts as compared with office based practice.
The only significant change noted is for spinal cord stimulator implant leads when performed in
office setting with 19.2% increase. However, epidural codes, which have been initiated with a
lower payment, continue to face small reductions for physician portion.
This review describes the effects of the proposed policy on interventional pain management
reimbursement for E&M services, procedural services by physicians and procedures performed in
office settings.
Key words: Physician payment policy, physician fee schedule, Medicare, Merit-Based Incentive
Payment System, interventional pain management, regulatory tsunami, Medicare Access and CHIP
Reauthorization Act of 2015
Pain Physician 2018: 21:415-432
Health Policy
Reframing Medicare Physician Payment Policy
for 2019: A Look at Proposed Policy
From:
1
Pain Management Center
of Paducah, Paducah, KY;
2
Spine
Pain Diagnostics Associates,
Niagara, WI;
3
Millennium Pain
Center, Bloomington, IL, and
University of Illinois, Urbana-
Champaign, IL;
4
LSU Health
Science Center, New Orleans,
LA; and
5
Massachusetts General
Hospital and Harvard Medical
School, Boston, MA
Additional Author Affiliation
Information on P. 428.
Address Correspondence:
Laxmaiah Manchikanti, MD
2831 Lone Oak Road
Paducah, KY 42003
E-mail: [email protected]
Disclaimer: There was no
external funding in the
preparation of this manuscript.
Conflict of interest: Dr.
Benyamin is a consultant for
Medtronic. Dr. Kaye is a speaker
for Depomed, Inc. and Merck..
Dr. Hirsch is a consultant for
Medtronic.
Manuscript received: 08-15-2018
Revised manuscript received:
09-04-2018
Accepted for publication:
09-06-2018
Free full manuscript:
www.painphysicianjournal.com
Laxmaiah Manchikanti, MD
1
, Vijay Singh, MD
2
, Ramsin M. Benyamin, MD
3
,
Alan D. Kaye, MD, PhD
4
, Vidyasagar Pampati, MSc
1
, and Joshua A. Hirsch, MD
5
www.painphysicianjournal.com
Pain Physician 2018; 21:415-432 • ISSN 1533-3159

www.painphysicianjournal.com 417
Pain Physician: September/October 2018: 21:415-432
416 www.painphysicianjournal.com
Reframing Medicare Physician Payment Policy for 2019
and intensity, whereas changes in service utilization
were not associated with a statistically significant
change (23). The data also showed that changes in
disease prevalence of instance were essentially associ
-
ated with spending reductions of 2.4% or $28.2 billion
(23). Even then, disability continues to escalate, along
with opioid related deaths, which continue to increase
at epidemic rates (24-26). It was also postulated that
a nominal decrease in health care cost based on price
reductions and cost calculation methodology of services
with site-of-service differentials by Medicare and oth
-
ers, and multiple policy changes, may have led to the
unintended consequences of limiting access to medi
-
cally needed services (2-4,27,28).
In a press release from July 2018, in the form of
a letter to physicians from CMS Administrator, Seema
Verma, the administration understandings of the is
-
sues facing provider communities and Medicare were
described (29). Administrator Verma highlighted the
following:
Years of eduction, training, and hard work, as well
as the expertise of physicians, are not utilized ap
-
propriately, but instead, they are being forced to
spend far too much of their time on burdensome
and often mindless administrative tasks.
Wasteful tasks imposed on physicians have been
draining energy and taking time away from pa
-
tients, from reporting on measures that demand
that physicians follow complicated and redundant
processes, to documenting lines of text that don’t
add value to patient’s medical record, to hunting
down records and faxes from other physicians and
sifting through them.
The systems have taken the most brilliant students
and put them to work clicking through screens
and copying and pasting, with 42% of physicians
reporting burnout.
Doctor/patient relationship has been deteriorating
and patients are not being put first.
Physicians should be able to deliver care to pa
-
tients, not sitting at a computer screen.
Administrator Verma blamed Washington for many
of the frustrations with the current system, as policies
that have been put forth as solutions either have not
worked or have moved health care in the opposite di
-
rection. In fact, she stated that electronic health records
that should make it easier for physicians to record notes
and achieve interoperability. Amazingly, the govern
-
ment spent $30 billion to encourage their uptake, turn-
T
he Centers for Medicare and Medicaid Services
(CMS) released its proposed 2019 Medicare
Physician Fee Schedule on July 12, 2018, with
the comment period ending September 10, 2018 (1). As
opposed to prior iterations, the 2019 Medicare physician
fee schedule (MPFS) and quality payment program
(QPP) proposed rule is the first year that the 2 rules
have been combined. This rule also is accompanied by
multiple fact sheets including ones on changes to the
quality payment program and physician fee schedule
proposals for 2019. In many ways, these changes reflect
the philosophy of the Trump administration. This is in
contrast to the 2017 proposed rule at which time the
Obama administration had declared the success of
the Patient Protection and Affordable Care Act (ACA)
with significant progress towards solving longstanding
challenges facing the US health care system related
to access, affordability, and quality of care (2-8). As
we have described in the past, reducing health care
expenditures with increased access to affordable
insurance coverage and improvement in quality have
been the cornerstones of multiple legislative efforts and
regulations including the ACA (4-18). Despite the fact
that there are clear examples of program success, the
effectiveness of ACA in achieving some of its primary
goals has been questioned (5,8). There has been a net
increase in the number of individuals with insurance;
a portion of which is attributable to the expansion of
Medicaid. Moreover there likely has been a reduction
in costs; however, with diminished access for many
who were previously insured and concerningly without
corresponding improvement in the quality of care
(4,5,8).
National health expenditures (NHEs) have grown
with expenditures reaching $3.3 trillion in 2016, which
is equivalent a 17.9% share of the gross domestic
product (GDP) (19). Medicare spending also reached a
historic $672.1 billion with a share of 20.36% of total
NHEs, while Medicaid spending grew almost as high as
Medicare to $565.5 billion in 2016, and a 17.1% share
of total NHE (19). The Trump administration started
with plans to repeal the ACA, which have not material
-
ized even with multiple legislative attempts through
Congress leaving it as the law of the land (20,21). The
statistics showing expenditures in the United States
reveal that the US spent $87.6 billion on back and neck
pain with an additional $95.9 billion on musculoskel
-
etal disorders in 2013 (22). Further, the same authors
also showed that the major reason for the increase in
expenditures was related to changes in service price
ing this tool into a serious distraction from patient care
due to the inability to exchange records between sys
-
tems and the increasing requirements for information
that must be documented. Administrator Verma prom
-
ised that CMS is committed to turning the tide and has
launched “Patients Over Paperwork” initiative, under
which they have been working to reduce the burden
of unnecessary rules and requirements. CMS indicates
that is has thus proposed an overhaul of the evaluation
and management (E&M) documentation and coding
system ostensibly to dramatically reduce the amount of
time physicians have to spend in putting unnecessary
information into patient’s records. Administrator Verma
also described multiple other changes that are reflected
in this proposed rule including a major reduction of the
documentation burden for E&M office visit code, .new
payments for physician services that are not part of a
face-to-face office visit and some easements in the qual
-
ity payment program
The proposed policy favorably affects interven
-
tional pain management’s reimbursement for E&M ser-
vices, procedural services by physicians and procedures
performed in office settings.
Background
Medicare establishes a physician fee schedule for
services furnished by physicians and other practitioners
in all sites of services, including office visits, surgical pro
-
cedures, diagnostic tests, therapy services, and multiple
specified preventive services. Payments are based on the
relative resources typically used to furnish the service.
Relative value units (RVUs) are applied to each service
for physician work, practice expense, and malpractice.
These RVUs become payment rates through application
of a conversion factor. Payment rates are calculated to in
-
clude an overall payment update specified by the statute.
The impact of the Medicare physician fee schedule
is enormous for interventional pain physicians. The
Medicare fee schedule affects not only fee-for-service
Medicare, but also Medicare Advantage Plans, a large
number of Medicaid plans, and a significant proportion
of private payers. Since 2016, interventional pain man
-
agement has suffered significant losses in multiple areas
of payments, not only for physician payments, but also
facility payments for in-office procedures and ambula
-
tory surgery centers. Further, the opioid epidemic has
also become a focus affecting interventional techniques
in that interventional techniques might appropriately
be considered in lieu of prescriptions opioids (24-26,30-
40). Manchikanti et al (2) demonstrated significant
declines in payment rates in 2017, which continued
through 2018, despite multiple efforts by American
Society of Interventional Pain Physicians (ASIPP) and
others to avoid these reductions. This is likely resulting
in reductions in utilization of interventional techniques
as shown in Appendix Table 1 and Appendix Figs. 1-4
(33-39). Opioid prescriptions are down but deaths
continue to increase concurrent with a decline in in
-
terventional techniques as shown in Appendix Figs. 5
and 6 (24-32).
Even prior to the proposed rule, interventional
techniques have been facing a multitude of issues de
-
spite demonstration of clinical and cost effectiveness
due to improper evidence synthesis (41-58). Based on
the available data, CMS is proposing updated pricing
recommendations for supply and equipment items cur
-
rently used as direct practice expense (PE) inputs. These
data were derived from market research resources and
methodologies including field surveys, aggregate data
-
bases, vendor resources, market scans, market analysis,
physician substantiation, and statistical analysis. CMS
is proposing to update supply and equipment pricing
over a 4-year phase-in.
Physician Payment uPdate
The proposed rule updates physician payment
schedule conversion factor from $35.9996 to $36.0463,
reflecting a statutory update of 0.25%, offset by a
budget neutrality adjustment of -0.12%, resulting in a
0.13% update.
Evaluation and Management Services
Payments
CMS proposed to collapse payment for office and
outpatient visits to a single blended payment for office
visits, Level 2 to 5 for new patients (CPT 99202-99205)
with a single payment of $134.45 and for established
patient office visits with a single payment for Levels
2-5 (CPT 99212-99215) into a single payment of $92 as
shown in Table 1.
In addition, new codes would be created to pro
-
vide additional payments to office visits of $5, $14 and
$67, with multiple procedure adjustment with reduc
-
tion when an E&M visit is furnished in combination
with a procedure on the same day (Table 2). Physicians
will be allowed to choose their method of documenta
-
tion, among the following options:
1995 or 1997 E&M guidelines for history, physical
examination, and medical decision making (cur
-
rent framework for decision making, which is the

www.painphysicianjournal.com 419
Pain Physician: September/October 2018: 21:415-432
418 www.painphysicianjournal.com
Reframing Medicare Physician Payment Policy for 2019
current framework for documentation)
Medical decision making only.
Physician time spent face-to-face with patients.
It seems that some physicians will continue to
document and report among the 5 levels of codes. CMS
will only require documentation to support the medical
necessity of the visit and to support a Level 2 CPT visit
code. In order to report an established office visit to
Medicare, physicians need to document medical neces
-
sity and then one of the following:
Two of the 3 components:
1) Problem-focused history that does not include
a review of systems or a past, family or social
history;
2) A limited examination of the affected body
area or organ system; and
3) Straightforward medical decision making mea
-
sured by minimal problems, review, and risk; or
Time personally spent by billing practitioner face-
to-face with the patient.
However, CMS is soliciting comments on what time
disproportionately care for patients with complex needs
would face a fee cut for Levels 4 and 5 visits, despite the
add-on payment. Further, physicians in nonprocedural
specialties whose revenue derives largely from these vis
-
its as shown in Appendix Fig. 7 could find this cut unten-
able. Figures 1 and 2 compare the interventional pain
management, pain management, and parent specialties
compared with internal medicine and overall specialties.
As illustrated earlier, interventional pain management
would see an increase with added benefit of reduced
documentation, facilitating increased patient time.
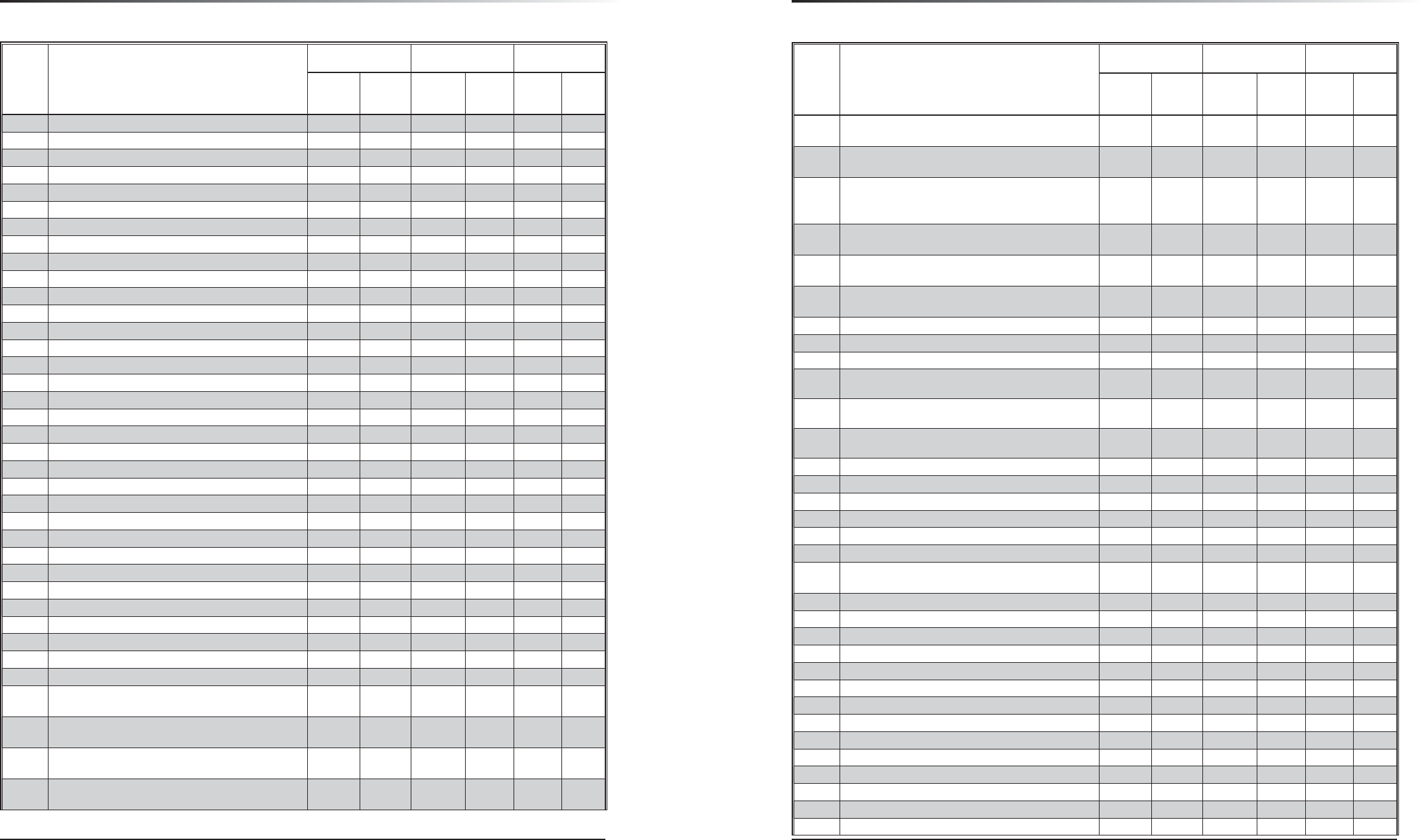
Table 1. Proposed blended payment schedule for office and outpatient based evaluation and management visits.
Physician Office
Payments
Hospital Outpatient Payments
Established Patients 2018
2019
Proposed
2018 2019 Proposed
Physician Facility Total Physician Facility Total
Level 1 – CPT 99211 $21.96 $24.15 $9.36
$113.68
$123.04 $9.73
$115.76
$125.49
Level 2 – CPT 99212 $44.64
$91.92
$25.92 $139.60
$65.60 $181.36
Level 3 – CPT 99213 $74.16 $52.20 $165.88
Level 4 – CPT 99214 $109.44 $79.92 $193.60
Level 5 – CPT 99215 $147.60 $113.04 $226.72
New Patients
Level 1 – CPT 99201 $45.36 $43.26 $27.36
$113.68
$141.04 $25.59
$115.76
$141.35
Level 2 – CPT 99202 $76.32
$134.45
$51.48 $165.16
$102.37 $218.13
Level 3 – CPT 99203 $109.80 $78.12 $191.80
Level 4 – CPT 99204 $167.40 $131.76 $245.44
Level 5 – CPT 99205 $210.60 $172.08 $285.76
Table 2. Proposed additional payment codes in 2019 physician payment rule.
• Proposing ~$5 add-on payment to recognize additional resources to address inherent complexity in E&M visits associated with primary care
services.
• Proposing ~$14 add-on payment to recognize additional resources to address inherent visit complexity in E&M visits associated with certain
non-procedural based care.
• Proposing ~$67 add-on payment for a 30 minute prolonged E&M visit.
should be required if this is the documentation selec-
tion with multiple options being considered. One op-
tion being 10 minutes (CPT defined typical time) or 16
minutes which is a weighted average of all established
office visits.
An impact analysis with additional payment accu
-
racy adjustments was performed by CMS as shown in
Table 3. For 2019, multiple specialties may face a reduc
-
tion. For some specialties, it is rather significant and it
is thus easy to understand their concern. Obstetrics and
gynecology will be the major beneficiary with overall
4% increase, followed by nurse practitioners of 3%.
Interventional pain management will see less than 3%
increases. Anesthesiology and physical medicine and
rehabilitation specialties will see minimal changes to
overall payments.
Song and Goodson (59) analyzed the CMS proposal
to reform office visit payments. Overall they had a nega
-
tive opinion about collapsing of the codes and also the
resultant adverse consequences. As shown in Appendix
Fig. 7, they postulated that these changes may benefit
by removing physicians’ incentive to spend time with
patients who have complex needs. Thus, physicians who
Specialty
Allowed
Charges
(in
millions)
Estimated
Potential
Impact of
Valuing Levels
2-5 Together,
with Additional
Adjustments
Nephrology $2,285
Minimal change to
overall payment
Neurosurgery $812
Nuclear Medicine $50
Ophthalmology $5,542
Oral/Maxillofacial Surgery $57
Orthopedic Surgery $3,815
Other $30
Pathology $1,151
Pediatrics $64
Physical Medicine $1,120
Plastic Surgery $387
Radiology $4,898
Thoracic Surgery $360
Vascular Surgery $1,132
Allergy/Immunology $240
Less than 3%
estimated decrease
in overall payment
Audiologist $67
Hematology/Oncology $1,813
Neurology $1,565
Otolaryngology $1,220
Pulmonary Disease $1,767
Radiation Oncology and
Radiation Therapy Centers
$1,776
Rheumatology $559 -3%
Dermatology $3,525 -4%
Podiatry $2,022 -4%
TOTAL $93,486 0%
Table 3 Specialty-specific impacts including payment accuracy adjustments.
Specialty
Allowed
Charges
(in
millions)
Estimated
Potential
Impact of
Valuing Levels
2-5 Together,
with Additional
Adjustments
Obstetrics/Gynecology $664 4%
Nurse Practitioner $3,586 3%
Obstetrics/Gynecology $664
Less than 3%
estimated increase
in overall payment
Nurse practitioner $3,586
Hand Surgery $202
Interventional Pain Management $839
Optometry $1,276
Physician Assistant $2,253
Psychiatry $1,260
Anesthesiology $1,995
Minimal change to
overall payment
Cardiac Surgery $313
Cardiology
Chiropractor $789
Colon and Rectal Surgery $168
Critical Care $334
Emergency Medicine $3,196
Endocrinology $482
Family Practice $6,382
Gastroenterology $1,807
General Practice $461
General Surgery $2,182
Geriatrics $214
Infectious Disease $663
Internal Medicine $11,173
Interventional Radiology $362
Multispecialty Clinic/Other
Physicians
$141
Other Evaluation and Management Proposals
1. When physicians report an E&M service and a pro-
cedure on the same date, CMS proposes to imple-
ment a 50% multiple procedure payment reduc-
tion to the lower paid of the 2 services. However,
this policy is not consistent with current valuation
of procedures commonly performed with office
visits, as duplicative resources have already been
removed from the underlying procedures. It ap
-
pears CMS proposed this policy to offset payment
increases to dermatology and other specialties that

www.painphysicianjournal.com 421
Pain Physician: September/October 2018: 21:415-432
420 www.painphysicianjournal.com
Reframing Medicare Physician Payment Policy for 2019
often report lower level office visit codes in con-
junction with minor procedures.
2. In addition, CMS will add $5 to each office visit per
-
formed for primary care purposes via a new code
GPC1X visit complexity inherent to E&M associated
with primary medical care services. In addition, rel
-
evant to interventional pain management, CMS
identified multiple specialties including interven
-
tional pain management that often report higher
level office visits and noted that potential reduction
in payment. To offset this loss, CMS proposes to add
$14 to each office visits performed by the specialists
in the following specialties via a new code GCGOX
visit complexity inherent to E&M (Table 2). The fol
-
lowing specialties have been identified:
Allergy/immunology
Cardiology
Endocrinology
Hematology/oncology
Interventional pain management-centered care
Neurology
Obstetrics/gynecology
Otolaryngology
Rheumatology
Urology
A new prolonged service code will be implemented
to add on to any office visit lasting more than 30 min
-
utes beyond the office visit (i.e., hour-long visits in total.
It is reported by:
Code GPR01, prolonged evaluation and man
-
agement or psychotherapy services(s). with a
payment rates of $67 (Table 2).
An interventional pain management physician
currently reporting 99205 and spending more than 60
minutes with a patient would be paid $211. Under the
proposed new method, the interventional pain physi
-
cian would report 99202-99205, depending on their
documentation selection ($134), plus GCG0X ($14), plus
GPR01 ($67), for a combined payment of $215.
CMS will implement new codes and payment for re
-
mote monitoring and inter-professional consultations.
3. Medicare would pay physicians for their time when
they reach out to beneficiaries via telephone or
other telecommunication devices to decide wheth
-
er an office visit or other service is needed. CMS
also proposes to pay for the time it takes physicians
to review a video or image sent by a patient seek
-
ing care or diagnosis for an ailment.
Fig. 1 2016 Medicare E&M services by level of service – new patient visits.
Fig. 2. 2016 Medicare E&M services by level of service – established patient visits.
Practice Expense Relative Values
Based on the Protecting Access to Medicare Act
of 2014 (PAMA), CMS initiated a market research to
update the direct PE inputs for supply and equipment
pricing for calendar year (CY) 2019.
Proposed Additional Calculation for
Evaluation and Management Services
CMS determines the proportion of indirect PE al-
located to a service by calculating a PE per hour based
upon the mix of specialties that bill for a service. How
-
ever, a wide range of specialties bill for E&M services
and the change into one payment level will have an ef
-
fect on PE per hour for many specialities. To address this
issue, CMS is proposing to create a single PE per hour
value for E&M visits of $136.34, based on an average
of the PE per hour across all specialties that bill E&M
codes, weighted by the volume of those specialties al
-
lowed charge for E&M services.
creation of a Bundled ePisode of
c
are for management and counseling
t
reatment for suBstance use disorders
Due to the available evidence suggesting that
routine counseling, either associated with medication-
assisted treatment (MAT) or on its own, can increase the
effectiveness of treatment for substance use disorder,
the federal guidelines for opioid treatment programs
describe that MAT and wraparound psychological and
support service can include the following services (60):
• Physical examination and assessment
• Psychological assessment
• Treatment planning
• Counseling
• Medication management
• Drug administration
• Comprehensive care management and supportive
services
• Care coordination
• Management of care transition
• Individual and family support services
• Health promotion
CMS now believes that making a separate payment
for a bundled episode of care for management and
counseling for substance use disorders could be effec
-
tive in preventing the need for more acute services (61).
Medicare pays for one-third of opioid related hospital
stays, and Medicare has seen the largest annual increase

www.painphysicianjournal.com 423
Pain Physician: September/October 2018: 21:415-432
422 www.painphysicianjournal.com
Reframing Medicare Physician Payment Policy for 2019
in the number of these stays over the past 2 decades.
CMS is requesting comments on whether the counsel
-
ing portion and other MAT components could also be
provided by qualified practitioners “incident” to the
services of the billing physician who would administer
or prescribe any necessary medications and manage the
overall care, as well as supervise any other counselors
participating in the treatment.
Professional liaBility insurance
r
elative values
CMS is seeking specific comments on ways to
improve how specialties in the state-level raw rate fil
-
ings data are cross walked for categorization into CMS
specialty codes in order to develop the specialty-level
risk factors and the professional liability insurance (PLI)
RVUs. At present CMS is proposing to add 28 codes
identified as low-volume services to the list of codes
for anticipated specialty assignment. These codes are
reported with the -26 modifier and were submitted by
the RUC. In the addendum for the CY2019 malpractice
risk factors and premium amounts by specialty, CMS
cross walked non-MD-DO specialties to the lowest
MD-DO risk factor specialty, allergy immunology. The
RUC also has consistently maintained that a risk factor
linked to a physician specialty is too high for many of
the non-physician health care professions.
In addition, cardiothoracic surgery and neurosur
-
gery, specialties with high PLI costs, are proposed to
receive positive impacts to payments related to their
insurance costs for 2019.
gloBal surgery data collection
The Medicare Access and CHIP Reauthorization Act
of 2015 (MACRA) required CMS to implement a process
to collect data on post-operative visits and use these
data to assess the accuracy of global surgical package
valuation.
CMS currently bundles payments for postoperative
care within 10 or 90 days after many surgical proce
-
dures. Historically, CMS has not collected data on how
many postoperative visits are actually performed dur
-
ing the global period. In the year 2017 FFS final rule,
CMS adapted a policy to collect postoperative visit
data (62). Consequently, CMS required practitioners in
groups with 10 or more practitioners in 9 states includ
-
ing Florida, Kentucky, Louisiana, Nevada, New Jersey,
North Dakota, Ohio, Oregon, and Rhode Island to use
the no pay CPT code 99024 for the postoperative fol
-
low-up visit, normally included in the surgical package,
to indicate that an E&M service was performed during a
postoperative period for reasons related to the original
procedure to report postoperative visits. However, this
has not affected practitioners who only practice with
fewer than 10 practitioners. There have been multiple
data reporting utilizing CPT 99024 in anesthesiology.
The proportion of practitioners reporting CPT code
99024 in anesthesiology is 29%, pain management is
40%, and interventional pain management is 33%. Fur
-
ther, these were variable for 10-day and 90-day global
period. In the future, CMS may add or increase physi
-
cian payment work value based on this data.
2019 Potentially misvalued codes list
CMS continues to propose a list of potentially misval-
ued codes for review by the RUC and possible adjustment.
Historically, the RUC and CMS has identified 2,086 services
through 20 different screening criteria for further review
by the RUC since 2006 (63-66). The RUCs efforts for 2009 to
2018 have resulted in $5 billion for redistribution within
the Medicare Physician Payment Schedule.
Potentially misvalued codes are identified in the
following categories:
• Codes that have experienced the fastest growth
• Codes that have experienced substantial changes
in practice expense
• Codes that describe technologies or surveys within
an appropriate time period (such as 3 years) after the
relative values are initially established for such codes
• Codes which are multiple codes that are frequently
billed in conjunction with furnishing a single service
• Codes with low relative values, particularly those
that are often billed multiple times for a single
treatment
• Codes that have not been subject to review since
implementation of the fee schedule
• Codes that account for the majority of spending
under the fee-for-service (FFS)
• Codes for services that have experienced a sub
-
stantial change in the hospital length of stay or
procedure time
• Codes for which there may be a change in the typi
-
cal site of service since the code was last valued
• Codes for which there is significant difference in
payment for the same service between different
sites of service
• Codes for which there may be anomalies in relative
values within a family of codes
• Codes for services when there may be efficiencies
when a service is furnished at the same time as
other services
• Codes with higher intraservice work per unit of
time
• Codes with high PE RVUs
• Codes with high cost supplies
• Codes as determined appropriate by the secretary
Apart from CMS identifying the misvalued codes,
the public and stakeholders, including insurers, may
nominate potentially misvalued codes for review by
submitting the code with supporting documentation
by February 10 of each year.
Payment for interventional Pain
m
anagement Procedures
In the proposed rule, the physician payment sched-
ule conversion factor is updated to $36.0463 from the
previous factor of $35.9996. This is a reflection of the
statutory update of 0.25%. However, this is offset by
the budget neutrality adjustment of 0.12% and so the
actual update result is only 0.13%
The physician payment schedule is mostly without
significant changes in payment rates for procedures,
without major changes for more commonly performed
procedures, while some procedures have seen signifi
-
cant increases; consequently, it is a mixed bag. Table 4
shows the 2019 proposed physician payment rates
comparing them to the 2018 final rates. The schedule
shows the rates for facility and non-facility; facility rates
when a physician performs the procedure in an ASC or
hospital; whereas, non-facility rates include the facility
expense portion of the office. An extended schedule
is available on the ASIPP website under Physician Fee
Schedules at http://www.asipp.org/Fee-Schedules.html.
Based on the available literature (28,33-39), an
overwhelming majority of interventional techniques
are performed in outpatient settings, either in physi
-
cians’ offices, hospital outpatient departments (HOP-
Ds), or ambulatory surgery centers (ASCs). In 2012, the
Medicare Payment Advisory Commission (MedPAC)
recommended that if the same service can be safely
performed in different settings, a prudent purchaser
should not pay more for that service in one setting
than in another (27,67). The Office of Inspector General
(OIG) also has expressed a similar approach (68); how
-
ever, because of hospital acquisition of practices and
increased levels of payments which is costing more for
Medicare. More and more procedures are performed in
an HOPD setting, essentially in an office setting which
is most likely similar to offices utilized outside, but paid
at 300% more than in-office procedures and over 80%
more than in ASCs. Further, for some procedures there
is such a dramatic difference that hospitals are paid at
2,000% as shown in Table 5 (1,68).Thus, the same pro
-
cedures are provided in an office is reimbursed at a rate
of $14-$20 with continued reductions in 2019, which
were initiated in 2017. These rates are inadequate for
these procedures which must be performed in sterile
fashion following the guidance set by the Centers for
Disease Control and Prevention (CDC).
With the continued decline in reimbursement ini
-
tiated in 2017, percutaneous adhesiolysis (CPT 62263
and 62264) continue to be the subject of comments
in the past and continue to face declines. Once again,
the fee schedule shows a 0.9% to 2.4% reduction for
non-facility settings and a reduction of 1.5% to 4.9%
for facility setting. CPT 62263 involving multiple per
-
cutaneous epidural adhesiolysis sessions, 2 or 3 days,
is performed very infrequently or rarely. However, CPT
62264 is commonly performed (38), though its utiliza
-
tion is declining rapidly as shown in Appendix Fig. 3.
and Appendix Table 2. The reimbursement is reduced
0.9% in a non-facility setting and 1.5% in a facility set
-
ting. Even though there is no significant difference for
the facility portion of the work involved to perform the
procedure in a non-facility setting, there is a significant
difference in reimbursement of $426.43 versus $597.65.
The saga related to epidural injections with and
without fluoroscopy which started in 2017 continues.
Overall, the reimbursement changed with an increase
of 0.1% to 0.8% for non-facility services; whereas,
it declined by 1.6% to 2.1% when the procedure is
performed in a facility setting. The reimbursement
rates continue to be inadequate with elimination of
separate payment for fluoroscopy, leading potentially
to a shift of procedures to the more highly reimbursed
transforaminals rather than interlaminars. Inter
-
laminars have declined significantly over the past few
years though there are other confounding factors at
play with regards to this migration (Appendix Fig. 2
and Appendix Table 3) (34,37). Ironically, there are
meaningful increases for continuous epidural injec
-
tions which are never performed in chronic pain man-
agement settings and carry different codes when they
are performed in obstetric anesthesia.
There are significant reductions for electronic
analysis of programmable pump (CPT 62367), electronic
analysis of programmable pump with reprogramming
(CPT 62368) with 8.1% and 6.8% reductions for non-
facility performance, whereas, these reductions are
2.8% and 4% in a facility setting.
www.painphysicianjournal.com 425
Pain Physician: September/October 2018: 21:415-432
424 www.painphysicianjournal.com
Reframing Medicare Physician Payment Policy for 2019
Table 4. 2019 proposed physician payment rates compared to 2018 rates.
CPT Description
2018 (CF=35.9996)
2019 Proposed
(CF: 36.0463)
% of change from
2018
Non-
Facility
(Office)
Facility
(ASC/
HOPD)
Non-
Facility
(Office)
Facility
(ASC/
HOPD)
Non-
Facility
(Office)
Facility
(ASC/
HOPD)
20526 Injection, therapeutic, carpal tunnel $79.56 $59.76 $79.30 $59.84 -0.3% 0.1%
20550 tendon sheath, ligament injection $54.36 $40.68 $53.35 $40.01 -1.9% -1.6%
20551 Tendon origin/insertion $62.28 $44.28 $53.71 $40.73 -13.8% -8.0%
20552 Single or multiple trigger point(s), 1 or 2 muscle group(s) $56.52 $39.24 $55.87 $38.57 -1.1% -1.7%
20553 Single or multiple trigger point(s), 3 or more muscle groups $65.16 $44.64 $64.88 $44.34 -0.4% -0.7%
20600 Small joint injection $49.32 $36.72 $47.58 $35.69 -3.5% -2.8%
20605 Intermediate joint injection $51.84 $38.88 $50.46 $37.85 -2.7% -2.7%
20610 Major joint injection $61.92 $47.88 $61.28 $47.94 -1.0% 0.1%
22510 Vertebroplasty (Thoracic) $1,727.62 $453.24 $1,816.73 $454.90 5.2% 0.4%
22511 Vertebroplasty (Lumbar) $1,705.66 $423.72 $1,797.27 $426.07 5.4% 0.6%
22512 Vertebroplasty - Additional $978.47 $216.72 $933.24 $217.00 -4.6% 0.1%
22513 Percut kyphoplasty, thor $7,328.08 $541.43 $7,090.67 $541.06 -3.2% -0.1%
22514 Percut kyphoplasty, thor $7,293.52 $503.99 $7,063.99 $503.57 -3.1% -0.1%
22515 Percut kyphoplasty, Additional $4,415.35 $233.64 $4,106.76 $234.30 -7.0% 0.3%
22534 Percut kyphoplasty, lumbar $379.08 $382.45 0.9%
22869 Insj stablj dev w/o dcmprn $551.81 $471.49 -14.6%
22870 Insj stablj dev w/o dcmprn add-on $142.56 $128.32 -10.0%
27093 Injection procedure for HIP arthrography – without anesthesia $191.88 $72.72 $207.99 $72.45 8.4% -0.4%
27095 Injection procedure for HIP arthrography – with anesthesia $252.00 $86.40 $277.20 $86.51 10.0% 0.1%
27096 Injection procedure for Sacroiliac joint, arthrography $163.08 $86.40 $162.57 $85.07 -0.3% -1.5%
27279 Arthrodesis sacroiliac joint $725.61 $719.99 -0.8%
62263 Percutaneous epidural adhesiolysis - 2 or 3 days $612.35 $329.40 $597.65 $313.24 -2.4% -4.9%
62264 Percutaneous epidural adhesiolysis – 1 day $430.20 $245.88 $426.43 $242.23 -0.9% -1.5%
62268 Percutaneous aspiration, spinal cord cyst or syrinx $267.84 $266.38 -0.5%
62270 Spinal puncture, diagnostic $162.36 $81.00 $153.92 $80.74 -5.2% -0.3%
62272 Spinal puncture, therapeutic $208.08 $86.76 $202.58 $87.23 -2.6% 0.5%
62273 Epidural, blood patch $178.20 $117.36 $176.27 $116.07 -1.1% -1.1%
62284 Injection procedure myelography $194.76 $91.08 $203.66 $91.56 4.6% 0.5%
62287 Disc decompression $595.43 $592.24 -0.5%
62290 Diskography each level: lumbar $334.08 $175.32 $344.60 $172.30 3.2% -1.7%
62291 Diskography each level: C/T $331.92 $173.52 $330.91 $165.45 -0.3% -4.6%
62320 Cervical or Thoracic interlaminar epidural; without fluoro $170.28 $103.32 $165.45 $100.93 -2.8% -2.3%
62321 Cervical or Thoracic interlaminar epidural; with fluoro $253.80 $110.88 $254.13 $108.50 0.1% -2.1%
62322
Lumbar or sacral (caudal) interlaminar epidural
injection(s); without fluoro
$159.84 $89.64 $155.00 $87.59 -3.0% -2.3%
62323
Lumbar or sacral (caudal) interlaminar epidural
injection(s); with fluoro
$250.56 $102.60 $252.68 $100.93 0.8% -1.6%
62324
Cervical or thoracic continuous interlaminar epidural
Injection(s),; without fluoro
$149.04 $93.60 $148.51 $93.72 -0.4% 0.1%
62325
Cervical or thoracic continuous interlaminar epidural
Injection(s),; with fluoro
$225.72 $108.00 $238.99 $110.66 5.9% 2.5%
Table 4 (cont.). 2019 proposed physician payment rates compared to 2018 rates.
CPT Description
2018 (CF=35.9996)
2019 Proposed
(CF: 36.0463)
% of change from
2018
Non-
Facility
(Office)
Facility
(ASC/
HOPD)
Non-
Facility
(Office)
Facility
(ASC/
HOPD)
Non-
Facility
(Office)
Facility
(ASC/
HOPD)
62326
Lumbar or sacral (caudal) continuous interlaminar epidural
Injection(s),; Without fluoro
$156.96 $92.88 $153.20 $91.56 -2.4% -1.4%
62327
Lumbar or sacral (caudal) continuous interlaminar epidural
Injection(s),; With fluoro
$230.04 $98.64 $238.27 $99.49 3.6% 0.9%
62350
Tunneled intrathecal or epidural catheter for long-term
medication administration via an external pump or
implantable reservoir; w/o laminectomy
$414.36 $410.21 -1.0%
62355
Removal or previously implanted intrathecal or epidural
catheter
$278.28 $277.20 -0.4%
62360
Implant or replacement of device for intrathecal or epidural
drug infusion; subcutaneous reservoir
$323.64 $328.74 1.6%
62361
Implantation or replacement of device for epidural drug
infusion; non-programmable pump
$448.56 $454.90 1.4%
62362 Implant spine infusion pump $398.52 $395.07 -0.9%
62365 Remove spine infusion device $307.80 $306.75 -0.3%
62367 Electronic analysis of programmable pump $43.56 $26.28 $40.01 $25.23 -8.1% -4.0%
62368
Electronic analysis of programmable pump with
reprogramming
$58.68 $36.36 $54.79 $35.33 -6.6% -2.8%
63650
Implant neuroelectrodes (NA=National price is Not
Available)
$1,353.23 $425.88 $1,613.43 $418.50 19.2% -1.7%
63655
Implant neuroelectrodes (NA=National price is Not
Available)
$866.51 $877.37 1.3%
63661 Remove spine eltrd perq aray $602.27 $335.88 $620.36 $332.71 3.0% -0.9%
63662 Remove spine eltrd plate $875.87 $888.54 1.4%
63663 Remove spine eltrd perq aray $809.63 $467.27 $824.74 $459.23 1.9% -1.7%
63664 Remove spine eltrd plate $911.87 $919.90 0.9%
63685 Implant neuroreceiver $376.92 $372.00 -1.3%
63688 Revise/remove neuroreceiver $387.36 $384.61 -0.7%
64400
Injection, anesthetic agent; Trigeminal nerve, any division
or branch
$134.64 $74.52 $138.78 $74.62 3.1% 0.1%
64402 Facial nerve $144.72 $85.68 $155.00 $88.31 7.1% 3.1%
64405 Greater occipital nerve $105.48 $65.88 $85.43 $54.43 -19.0% -17.4%
64408 Vagus nerve $119.16 $88.92 $116.43 $85.43 -2.3% -3.9%
64410 Phrenic nerve $158.40 $87.12 $161.49 $87.95 2.0% 1.0%
64413 Cervical plexus $130.68 $84.24 $129.77 $84.35 -0.7% 0.1%
64415 Brachial plexus $121.32 $67.32 $122.56 $67.77 1.0% 0.7%
64417 Axillary nerve $132.84 $72.72 $136.98 $73.17 3.1% 0.6%
64418 Suprascapular nerve $120.24 $64.08 $97.33 $58.76 -19.1% -8.3%
64420 Intercostal, single $114.48 $69.48 $113.91 $69.57 -0.5% 0.1%
64421 Intercostal, multiple, regional block $154.80 $95.04 $158.24 $93.72 2.2% -1.4%
64425 Ilioinguinal, Iliohypogastric $137.52 $96.84 $140.58 $97.33 2.2% 0.5%
64430 Pudendal nerve $140.76 $83.16 $147.79 $82.19 5.0% -1.2%
64445 Sciatic nerve $140.76 $75.24 $141.66 $75.34 0.6% 0.1%
64450 Other peripheral nerve or branch $82.08 $46.80 $77.86 $45.42 -5.1% -3.0%

www.painphysicianjournal.com 427
Pain Physician: September/October 2018: 21:415-432
426 www.painphysicianjournal.com
Reframing Medicare Physician Payment Policy for 2019
Table 4 (cont.). 2019 proposed physician payment rates compared to 2018 rates.
CPT Description
2018 (CF=35.9996)
2019 Proposed
(CF: 36.0463)
% of change from
2018
Non-
Facility
(Office)
Facility
(ASC/
HOPD)
Non-
Facility
(Office)
Facility
(ASC/
HOPD)
Non-
Facility
(Office)
Facility
(ASC/
HOPD)
64479 Cervical transforaminal epidural injections $240.48 $136.08 $247.28 $133.37 2.8% -2.0%
64480 Cervical transforaminal epidural injections add-on $115.92 $65.16 $121.84 $64.52 5.1% -1.0%
64483 L/S transforaminal epidural injections $223.20 $115.92 $229.98 $113.91 3.0% -1.7%
64484 L/S transforaminal epidural injections add-on $94.32 $53.64 $98.41 $52.27 4.3% -2.6%
64490 C/T facet joint injections, 1st Level (Old 64470) $193.68 $109.44 $190.32 $107.06 -1.7% -2.2%
64491 C/T facet joint injections, 2nd Level (Old 64472) $95.40 $62.28 $95.16 $61.28 -0.2% -1.6%
64492 C/T facet joint injections, 3rd Level $96.12 $63.00 $95.52 $62.00 -0.6% -1.6%
64493 Paravertebral facet joint or facet joint nerve; L/S, 1st Level $175.68 $93.60 $174.46 $91.92 -0.7% -1.8%
64494 Paravertebral facet joint or facet joint nerve; L/S, 2nd Level $88.20 $53.64 $87.95 $52.27 -0.3% -2.6%
64495 Paravertebral facet joint or facet joint nerve; L/S, 3rd Level $88.20 $54.36 $87.59 $52.99 -0.7% -2.5%
64505 Injection, anesthetic agent; sphenopalatine ganglion $112.32 $93.60 $121.12 $96.60 7.8% 3.2%
64510
Injection, anesthetic agent; Stellate ganglion (cervical
sympathetic)
$130.32 $75.96 $133.37 $75.34 2.3% -0.8%
64520
Injection, anesthetic agent; lumbar or thoracic
(paravertebral sympathetic)
$191.88 $83.52 $205.82 $83.99 7.3% 0.6%
64530
Injection, anesthetic agent; celiac plexus, with or without
radiologic monitoring
$192.96 $93.96 $202.58 $93.36 5.0% -0.6%
64600
Destruction by neurolytic agent, trigeminal nerve;
supraorbital, infraorbital, mental, or inferior alveolar branch
$416.52 $234.00 $439.76 $237.91 5.6% 1.7%
64605
Destruction by neurolytic agent, trigeminal nerve; second
and third division branches at foramen ovale
$559.07 $351.00 $585.03 $353.25 4.6% 0.6%
64610
Destruction by neurolytic agent, trigeminal nerve; second
and third division branches at foramen ovale under
radiologic monitoring
$762.83 $509.39 $803.11 $518.71 5.3% 1.8%
64612
Chemodenervation of muscle(s); muscle(s) innervated by
facial nerve (eg, for blepharospasm, hemifacial spasm)
$137.16 $121.32 $139.14 $122.56 1.4% 1.0%
64620 Destruction by neurolytic agent, intercostal nerve $210.24 $177.84 $208.35 $176.63 -0.9% -0.7%
64630 Destruction by neurolytic agent; pudendal nerve $236.16 $197.64 $242.59 $195.73 2.7% -1.0%
64633 Destroy cerv/thor facet jnt $429.12 $232.56 $418.14 $227.09 -2.6% -2.4%
64634 Destroy c/th facet jnt addl $192.96 $70.56 $187.80 $69.57 -2.7% -1.4%
64635 Destroy lumb/sac facet jnt $424.44 $229.32 $415.25 $224.93 -2.2% -1.9%
64636 Destroy l/s facet jnt addl $175.32 $61.56 $170.86 $59.84 -2.5% -2.8%
64640
Destruction by neurolytic agent; other peripheral nerve or
branch
$135.72 $96.12 $136.26 $95.52 0.4% -0.6%
64680
Destruction by neurolytic agent, with or without radiologic
monitoring; celiac plexus
$309.96 $168.84 $324.42 $166.17 4.7% -1.6%
It appears that CMS has recognized the importance
of implanting of neuroelectrodes by increasing the
reimbursement for non-facility setting by 19.2%; how
-
ever, at the same time it reduces physician reimburse-
ment by 1.7%.
Facet joint nerve blocks and facet joint neuro-
lytic procedures are facing reductions in the range of
1.5% to 3%; however, increases for nerve blocks and
sympathetic blocks, especially in non-facility setting is
appreciable.
Table 5 Schedule of facility 2019 proposed payments for soft tissue and intraarticular injections in multiple settings.
Office
Overhead
ASC HOPD
% of HOPD over
Office Overhead
20600 Small joint injection $11.90 $21.97 $248.68 1991%
20605
Intermediate joint injection $12.62 $23.41 $248.68 1871%
20550 tendon sheath, ligament injection $13.34 $23.41 $248.68 1765%
20551 Tendon origin/insertion $12.98 $24.13 $248.68 1816%
20552 Trigger point(s), 1 or 2 muscle group(s) $17.30 $30.25 $248.68 1337%
20553 Trigger point(s), 3 or more muscle groups $20.55 $35.29 $248.68 1110%
20526 Injection, therapeutic, carpal tunnel $19.47 $39.25 $248.68 1178%
64640
Destruction by neurolytic agent; other peripheral
nerve or branch
$40.64 $87.86 $772.30 1800%
Finally, CMS continues to provide inadequate
reimbursement for peripheral neurolytic procedures
(CPT 64640) of $136.26 for non-facility and physician
reimbursement of $95.52. These procedures require
blockade of multiple nerves with expensive equip
-
ment; however, CMS continues to consider this as a
single procedure and thus reimburses inadequately.
This procedure should be reimbursed similar to other
radiofrequency neurotomy procedures such as facet
joint neurotomy (CPT 64633-64637). There is substantial
evidence showing the effectiveness of peripheral nerve
blocks in managing chronic knee pain, hip pain, among
multitude of other conditions. The code is often uti
-
lized to report sacroiliac joint neurotomy procedures.
Thus, reflecting the HOPD rates, these reimbursement
patterns must be addressed and increased. The proce
-
dure also carries an extremely low reimbursement in
ASC settings. Similarly, though not to the same extent,
another procedure the neurolytic block of pudendal
nerves (CPT 64630) also carries a low reimbursement of
$242.59 in a non-facility setting and $195.73 in a facility
setting. The neurolytic procedure of intercostal nerve
also faces the same path with $208.35 for non-facility
setting and $176.63 for facility setting. Consequently, it
is time for CMS while making so many changes to make
the appropriate changes for the future.
recognizing communication technology-
Based services
CMS is proposing to pay separately for 2 newly de-
fined physicians’ services furnished using communica-
tion technology including brief communication in tech-
nology-based service i.e., virtual check-in (HCPCS code
GVCI1) and remote evaluation of recorded video and/or
images submitted by the patient (HCPCS code GRAS1).
This is expected to increase efficiency for practitioners
and convenience for beneficiaries. Both services of brief
communication technology-based service and remote
evaluation of recorded video and/or images may be
used to assess the patient visit needs.
In addition, CMS also has proposed to pay sepa
-
rately for new coding describing chronic care remote
physiologic monitoring (CPT codes 990X0, 990X1, and
994X9) and interprofessional internet consultation with
multiple CPT codes 994X6, 994X0, 99446, 99447, 99448,
and 99449.
discontinuation of functional status
r
ePorting requirements for outPatient
t
heraPy
The proposed payment rule for 2019 will discon-
tinue the functional status reporting requirements
for services furnished on or after January 1, 2019 for
outpatient therapy. Since January 1, 2013, as required
by the Middle Class Tax Relief and Jobs Creation Act of
2012, all providers of outpatient therapy services have
been required to include functional status information
on claims for therapy services. The data was collected
using a non-payable HCPCS G-codes and modifiers to
describe a patient’s functional limitation and severity
at periodic intervals during outpatient therapy services.
Since the Bipartisan Budget Act of 2018 repealed the
therapy caps, these requirements served no purpose.
quality Payment Program
The proposed changes to quality payment pro-
gram (QPP) aim to reduce clinician burden, focus on
outcomes, and promote intraoperability of electronic
health records by removing Merit-based Incentive Pay
-
ment System (MIPS) process-based quality measures

Reframing Medicare Physician Payment Policy for 2019
www.painphysicianjournal.com 429
Pain Physician: September/October 2018: 21:415-432
428 www.painphysicianjournal.com
references
1. Department of Health and Human Ser-
vices, Centers for Medicare & Medicaid
Services. 42 CFR Parts 405, 410, 414, 414,
415 and 495. [CMS–1693–P] Medicare
Program; Revisions to Payment Policies
Under the Physician Fee Schedule and
Other Revisions to Part B for CY 2019;
Medicare Shared Savings Program Re-
quirements; Quality Payment Program;
and Medicaid Promoting Interoperabili-
ty Program. Proposed rule. July 27, 2018.
2. Manchikanti L, Kaye AD, Hirsch JA.
Proposed Medicare physician payment
schedule for 2017: Impact on interven-
tional pain management practices. Pain
Physician 2016; 19:E935-E955.
3. Manchikanti L, Singh V, Hirsch JA. Fa-
cility payments for interventional pain
management procedures: Impact of
proposed rules. Pain Physician 2016;
19:E957-E984.
4. Obama B. United States health care re-
form: Progress to date and next steps.
JAMA 2016; 316:525-532.
5. Manchikanti L, Helm S 2nd, Benya-
min RM, Hirsch JA. A critical analysis
of Obamacare: Affordable care or insur-
ance for many and coverage for few?
Pain Physician 2017; 20:111-138.
6. Manchikanti L, Hirsch JA. Repeal and re-
place of Affordable Care: A complex, but
not an impossible task. Pain Physician
2016; 19:E1109-E1113.
7. Bauchner H. The Affordable Care Act
and the future of US health care. JAMA
2016; 316:492-493.
8. Cannon MF. Is Obamacare harming
quality? (Part 1). Health Affairs Blog, Jan-
uary 4, 2018.
www.healthaffairs.org/do/10.1377/
hblog20180103.261091/full/
9. Hirsch JA, Leslie-Mazwi TM, Barr RM,
McGinty G, Nicola GN, Silva E 3rd,
Manchikanti L. The bundled payments
for care improvement initiative. J Neu-
rointerv Surg 2016; 8:547-548.
10. Hirsch JA, Nicola G, McGinty G, Liu RW,
Barr RM, Chittle MD, Manchikanti L.
ICD-10: History and context. AJNR Am
J Neuroradiol 2016; 37:596-599.
11. Manchikanti L, Hammer M, Benyamin
RM, Hirsch JA. Physician Quality Re-
porting System (PQRS) for intervention-
al pain management practices: Chal-
lenges and opportunities. Pain Physician
2016; 19:E15-E32.
12. Hirsch JA, Harvey HB, Barr RM, Dono-
van WD, Duszak R Jr, Nicola GN, Schae-
fer PW, Manchikanti L. Sustainable
growth rate repealed, MACRA revealed:
Historical context and analysis of recent
changes in Medicare physician payment
methodologies. AJNR Am J Neuroradiol
2016; 37:210-214.
13. Hirsch JA, Leslie-Mazwi TM, Barr
RM, McGinty G, Nicola GN, Patel AB,
Manchikanti L. The Burwell roadmap. J
Neurointerv Surg 2016; 8:544-546.
14. Hirsch JA, Leslie-Mazwi TM, Nicola GN,
Bhargavan-Chatfield M, Seidenwurm
DJ, Silva E, Manchikanti L. PQRS and
the MACRA: Value-based payments have
moved from concept to reality. AJNR Am
J Neuroradiol 2016; 37:2195-200.
15. Manchikanti L, Helm S 2nd, Benya-
min RM, Hirsch JA. Merit-Based In-
centive Payment System (MIPS): Harsh
choices for interventional pain manage-
ment physicians. Pain Physician 2016;
19:E917-E934.
16. Hirsch JA, Leslie-Mazwi TM, Patel AB,
Rabinov JD, Gonzalex RG, Barr RM, Nic-
ola GN, Klucznik RP, Prestigiacomo CJ,
Manchikanti L. MACRA: Background,
opportunities and challenges for the
neurointerventional specialist. J Neuroin-
terv Surg 2016; 8:868-874.
17. Hirsch JA, Rosenkrantz AB, Ansari SA,
Manchikanti L, Nicola GN. MACRA 2.0:
Are you ready for MIPS? J Neurointerv
Surg 2017; 9:714-716.
18. Golding LP, Nicola GN, Ansari SA,
Rosenkrantz AB, Silva Iii E, Manchikanti
L, Hirsch JA. MACRA 2.5: the legislation
moves forward. J Neurointerv Surg 2018
Jul 4. [Epub ahead of print].
19. Hartman M, Martin AB, Espinosa N,
Catlin A, The National Health Expendi-
ture Accounts Team. National health care
spending in 2016: Spending and enroll-
ment growth slow after initial coverage
expansions. Health Aff (Millwood) 2018;
37:150-160.
20. Hirsch JA, Rosenkrantz AB, Nicola GN,
Harvey HB, Duszak R Jr, Silva E 3rd, Barr
RM, Klucznik RP, Brook AL, Manchikanti
L. Contextualizing the first-round failure
of the AHCA: Down but not out. J Neuro-
interv Surg 2017; 9:595-600.
21. Hirsch JA, Rosenkrantz AB, Allen B,
Nicola GN, Klucznik RP, Manchikanti L.
AHCA meets BCRA; timeline, context,
and future directions. J Neurointerv Surg
2018; 10:205-208.
22. Dieleman JL, Baral R, Birger M, Bui AL,
Bulchis A, Chapin A, Hamavid H, Horst
C, Johnson EK, Joseph J, Lavado R, Lom-
sadze L, Reynolds A, Squires E, Campbell
M, DeCenso B, Dicker D, Flaxman AD,
Gabert R, Highfill T, Naghavi M, Night-
ingale N, Templin T, Tobias MI, Vos T,
Murray CJ.. US spending on personal
health care and public health, 1996-
2013. JAMA 2016; 316:2627-2646.
23. Dieleman JL, Squires E, Bui AL, Camp-
bell M, Chapin A, Hamavid H, Horst
C, Li Z, Matyasz T, Reynolds A, Sadat
N, Schneider MT, Murray CJL. Factors
associated with increase in US health
care spending, 1996-2013. JAMA 2017;
318:1668-1678.
24. Manchikanti L, Kaye AM, Knezevic
NN, McAnally H, Trescot AM, Blank S,
Pampati V, Abdi S, Grider JS, Kaye AD,
Manchikanti KN, Cordner HJ, Gharibo
CG, Harned ME, Albers SL, Atluri S,
Aydin SM, Bakshi S, Barkin R, Benyamin
RM, Boswell MV, Buenaventura RM,
Calodney AK, Cedeno DL, Datta S, Deer
TR, Fellows B, Galan V, Grami V, Hansen
H, Helm S 2nd, Justiz R, Koyyalagunta
D, Malla Y, Navani A, Nouri K, Pasupule-
ti R, Sehgal N, Silverman SM, Simopou-
los TT, Singh V, Slavin KV, Solanki DR,
Staats PS, Vallejo R, Wargo BW, Wata-
nabe A, Hirsch JA. Responsible, safe,
and effective prescription of opioids for
chronic non-cancer pain: American So-
ciety of Interventional Pain Physicians
(ASIPP) guidelines. Pain Physician 2017;
20:S3-S92.
25. National Institute on Drug Abuse. Over-
dose death rates. September 2017.
www.drugabuse.gov/related-topics/
trends-statistics/overdose-death-rates
26. Manchikanti L, Sanapati J, Benyamin
RM, Atluri S, Kaye AD, Hirsch JA. Re-
framing the prevention strategies of the
opioid crisis: focusing on prescription
opioids, fentanyl, and heroin epidemic.
Pain Physician 2018; 21:309-326.
27. Manchikanti L, Benyamin RM, Falco
FJE, Hirsch JA. Recommendations of the
Medicare Payment Advisory Commis-
sion (MedPAC) on the health care deliv-
ery system: The impact of interventional
pain management in 2014 and beyond.
Pain Physician 2013; 16:419-440.
28. Manchikanti L, Pampati V, Hirsch JA.
Cost calculation methodology exac-
erbates site-of-services differential by
10- to 18-fold for soft tissue and joint
injections in hospital outpatient depart-
ments. IPM Reports 2017; 1:183-189.
29. Letter to Doctors from CMS Admin-
istrator Seema Verna, Department of
Health & Human Services, Centers for
Medicare and Medicaid Services.
and overhauling the MIPS. Quality payment program is
a subject of a separate manuscript.
conclusion
The proposed fee schedule includes seismic shifts
for E/M services, which is garnering significant atten
-
tion in the medical community. Interventional pain
management continues to face many challenges in the
present environment. It is important for IPM specialists
to understand the multitude of changes in the regula
-
tions including the proposed fee schedule so as to pre-
serve interventional pain management into the future.
Acknowledgments
The authors wish to thank Bert Fellows, MA, Direc-
tor Emeritus of Psychological Services, Pain Manage-
ment Center of Paducah, for manuscript review, and
Tonie M. Hatton and Diane E. Neihoff, transcriptionists,
for their assistance in the preparation of this manu
-
script. We would like to thank the editorial board of
Pain Physician for its review and criticism in improving
the manuscript.
Author Affiliations
Dr. Manchikanti is Medical Director of the Pain
Management Center of Paducah, Paducah, KY, and
Clinical Professor, Anesthesiology and Perioperative
Medicine, University of Louisville, Louisville, KY, and
Professor of Anesthesiology-Research, Department
of Anesthesiology, School of Medicine, LSU Health
Sciences Center, New Orleans, LA.
Dr. Singh is Medical Director, Spine Pain Diag
-
nostics Associates, Niagara, WI
Dr. Benyamin is Medical Director, Millennium
Pain Center, Bloomington, IL, and Clinical Assistant
Professor of Surgery, College of Medicine, University
of Illinois, Urbana-Champaign, IL.
Dr. Kaye is Professor, Program Director, and
Chair, Department of Anesthesiology, and Professor,
Department of Pharmacology, LSU Health Science
Center, New Orleans, LA.
Vidyasagar Pampati is a Statistician at the Pain
Management Center of Paducah, Paducah, KY.
Dr. Hirsch is Vice Chief of Interventional Care,
Chief of NeuroInterventional Spine, Service Line
Chief of Interventional Radiology, Director Inter
-
ventional and Endovascular Neuroradiology, Massa-
chusetts General Hospital; and Associate Professor,
Harvard Medical School, Boston, MA.
aPPendix
To access complete article with live links to Appendix Tables and Figures:
http://www.painphysicianjournal.com/current
Click Here for All Appendix Tables and Figures

Reframing Medicare Physician Payment Policy for 2019
Pain Physician: September/October 2018: 21:415-432
430 www.painphysicianjournal.com
www.painphysicianjournal.com 431
30. H.R. 5804. Post-Surgical Injections as an
Opioid Alternative Act. Introduced May
15, 2018.
31. National Institute on Drug Abuse. Over-
dose death rates. August 2018
www.drugabuse.gov/related-topics/
trends-statistics/overdose-death-rates
32. IQVIA Institute for Human Data Science
Study. Medicine use and spending in
the U.S. A review of 2017 and outlook for
2022. April 2018.
www.iqvia.com/institute/reports/med-
icine-use-and-spending-in-the-us-re-
view-of-2017-outlook-to-2022
33. Manchikanti L, Pampati V, Hirsch JA.
Utilization of interventional techniques
in managing chronic pain in Medicare
population from 2000 to 2014: An analy-
sis of patterns of utilization. Pain Physi-
cian 2016; 19:E531-E546.
34. Manchikanti L, Soin A, Mann DP, Bak-
shi S, Pampati V, Hirsch JA. Reversal of
growth of utilization of interventional
techniques in managing chronic pain
in Medicare population post Affordable
Care Act. Pain Physician 2017; 20:551-567.
35. Manchikanti L, Pampati V, Hirsch JA.
Retrospective cohort study of usage
patterns of epidural injections for spi-
nal pain in the US fee-for-service Medi-
care population from 2000 to 2014. BMJ
Open 2016; 6:e013042.
36. Manchikanti L, Hirsch JA, Pampati V,
Boswell MV. Utilization of facet joint
and sacroiliac joint interventions in
Medicare population from 2000 to 2014:
Explosive growth continues! Curr Pain
Headache Rep 2016; 20:58.
37. Manchikanti L, Soin A, Mann DP, Bak-
shi S, Pampai V, Hirsch JA. Comparative
analysis of utilization of epidural proce-
dures in managing chronic pain in the
Medicare population: Pre and post Af-
fordable Care Act. Spine (Phila Pa 1976)
2018; [Epub ahead of print].
38. Manchikanti L, Pampati V, Benyamin
RM, Hirsch JA. Declining utilization of
percutaneous epidural adhesiolysis in
Medicare population: Evidence-based
or over-regulated? IPM Reports 2018;
2:9-18.
39. Manchikanti M, Manchikanti L, Kaye
AD, Pampati V, Hirsch JA. Usage pat-
terns of sacroiliac joint injections – A
comparative evaluation of pre and post
Affordable Care Act in Medicare popula-
tion. IPM Reports 2018; in press. HOLLY
ADD PAGE NUMBERS
40. H.R. 6138. ASC Payment Transparency
Act of 2018. June 19, 2018.
41. Chou R, Hashimoto R, Friedly J, Fu R,
Dana T, Sullivan S, Bougatsos C, Jarvik
J. Pain Management Injection Therapies
for Low Back Pain. Technology Assess-
ment Report ESIB0813. (Prepared by the
Pacific Northwest Evidence-based Prac-
tice Center under Contract No. HHSA
290-2012-00014-I.) Rockville, MD:
Agency for Healthcare Research and
Quality; July 10, 2015.
www.cms.gov/medicare/coverage/de-
terminationprocess/downloads/id98ta.
pdf
42. Manchikanti L, Knezevic NN, Boswell
MV, Kaye AD, Hirsch JA. Epidural injec-
tions for lumbar radiculopathy and spi-
nal stenosis: A comparative systematic
review and meta-analysis. Pain Physician
2016; E365-E410.
43. Grider JS, Manchikanti L, Carayan-
nopoulos A, Sharma ML, Balog CC,
Harned ME, Grami V, Justiz R, Nouri
KH, Hayek SM, Vallejo R, Christo PJ. Ef-
fectiveness of spinal cord stimulation in
chronic spinal pain: A systematic review.
Pain Physician 2016; 19:E33-E54.
44. Helm II S, Racz GB, Gerdesmeyer L,
Justiz L, Hayek SM, Kaplan ED, El Ter-
any MA, Knezevic NN. Percutaneous
and endoscopic adhesiolysis in manag-
ing low back and lower extremity pain:
A systematic review and meta-analysis.
Pain Physician 2016; 19:E245-E282.
45. Farber SH, Han JL, Elsamadicy AA, Hus-
saini Q, Yang S, Pagadala P, Parente B,
Xie J, Lad SP. Long-term cost utility of
spinal cord stimulation in patients with
failed back surgery syndrome. Pain Phy-
sician 2017; 20:E797-E805.
46. Cho JH, Lee JH, Song KS, Hong JY,
Joo YS, Lee DH, Hwang CJ, Lee CS.
Treatment outcomes for patients with
failed back surgery. Pain Physician 2017;
20:E29-E43.
47. Helm II S, Simopoulos TT, Stojanovic M,
Abdi S, El Terany MA. Effectiveness of
thermal annular procedures in treating
discogenic low back pain. Pain Physician
2017; 20:447-470.
48. Manchikanti L, Helm S 2nd, Pampati V,
Racz GB. Cost utility analysis of percu-
taneous adhesiolysis in managing pain
of post-lumbar surgery syndrome and
lumbar central spinal stenosis. Pain
Pract 2015; 15:414-422.
49. Manchikanti L, Pampati V, Kaye AD,
Hirsch JA. Cost utility analysis of cervi-
cal therapeutic medial branch blocks in
managing chronic neck pain. Int J Med
Sci 2017; 14:1307-1316.
50. Manchikanti L, Pampati V, Kaye AD,
Hirsch JA. Therapeutic lumbar facet
joint nerve blocks in the treatment of
chronic low back pain: Cost utility analy-
sis based on a randomized controlled
trial. Korean J Pain 2018; 31:27-38.
51. Boswell MV, Manchikanti L. Appropri-
ate design and methodologic quality as-
sessment, clinically relevant outcomes
are essential to determine the role
of epidural corticosteroid injections.
Commentary RE: Chou R, Hashimoto
R, Friedly J, Fu R, Bougatsos C, Dana
T, Sullivan SD, Jarvik J. Epidural corti-
costeroid injections for radiculopathy
and spinal stenosis: A systematic review
and meta-analysis. Ann Intern Med 2015;
163:373-381. Evid Based Med 2016; 21:89.
52. Manchikanti L, Boswell MV, Kaye AD,
Helm II S, Hirsch JA. Therapeutic role of
placebo: Evolution of a new paradigm
in understanding research and clinical
practice. Pain Physician 2017; 20:363-386.
53. Manchikanti L, Hirsch JA, Falco FJ, Bo-
swell MV. Management of lumbar zyg-
apophysial (facet) joint pain. World J Or-
thop 2016; 7:315-337.
54. Levine AB, Parrent AG, MacDougall KW.
Stimulation of the spinal cord and dor-
sal nerve roots for chronic groin, pel-
vic, and abdominal pain. Pain Physician
2016; 19:405-412.
55. Manchikanti L, Falco FJE, Pampati V,
Cash KA, Benyamin RM, Hirsch JA. Cost
utility analysis of caudal epidural injec-
tions in the treatment of lumbar disc
herniation, axial or discogenic low back
pain, central spinal stenosis, and post
lumbar surgery syndrome. Pain Physi-
cian 2013; 16:E129-E143.
56. Manchikanti L, Pampati V, Benyamin
RM, Hirsch JA. Cost utility analysis of
lumbar interlaminar epidural injections
in the treatment of lumbar disc hernia-
tion, central spinal stenosis, and axial or
discogenic low back pain. Pain Physician
2017; 20:219-228.
57. Manchikanti L, Hirsch JA, Kaye AD, Bo-
swell MV. Cervical zygapophysial (facet)
joint pain: Effectiveness of intervention-
al management strategies. Postgrad Med
2016; 128:54-68.
58. Manchikanti L, Manchikanti KN, Ghar-
ibo CG, Kaye AD. Efficacy of percuta-
neous adhesiolysis in the treatment of
lumbar post surgery syndrome. Anesth
Pain Med 2016; 6:e26172.
59. Song Z, Goodson JD. The CMS proposal
to reform office-visit payments. N Engl J
Med 2018 [Epub ahead of print].
60. King VL, Brooner RK, Peirce JM, Kolod-
ner K, Kidorf MS. A randomized trial of
Web-based videoconferencing for sub-
stance abuse counseling. J Subst Abuse
Treat 2014; 46:36-42.
61. Owens PL, Barrett ML, Weiss AJ, Wash-
ington RE, Kronick R. Hospital Inpatient
Utilization Related to Opioid Overuse
Among Adults 1993-2012. Statistical
Brief #177. Healthcare Cost and Utiliza-
tion Project (HCUP). August 2014. Agen-
cy for Healthcare Research and Quality,
Rockville, MD.
www.hcup-us.ahrq.gov/reports/stat-
briefs/sb177-Hospitalizations-for-Opi-
oid-Overuse.jsp
62. Department of Health and Human Ser-
vices, Centers for Medicare & Medicaid
Services. 42 CFR Parts 405, 410, 411, 414,
417, 422, 423, 424, 425, and 460. [CMS-
1654-CN2] Medicare Program; Revisions
to Payment Policies Under the Physi-
cian Fee Schedule and Other Revisions
to Part B for CY 2017; Medicare Advan-
tage Bid Pricing Data Release; Medicare
Advantage and Part D Medical Loss Ra-
tio Data Release; Medicare Advantage
Provider Network Requirements; Ex-
pansion of Medicare Diabetes Preven-
tion Program Model; Medicare Shared
Savings. Proposed Rule. November 18,
2016.
63. Hirsch JA, Leslie-Mazwi TM, Nicola GN,
Barr RM, Bello JA, Donovan WD, Tu R,
Alson MD, Manchikanti L. Current pro-
cedural terminology: A primer. J Neuro-
Intervent Surg 2015; 7:309-312.
64. Hirsch JA, Silva E 3rd, Nicola GN, Barr
RM, Bello JA, Manchikanti L, Donovan
WD. The RUC: A primer for neurointer-
ventionalists. J Neurointerv Surg 2014;
6:61-64.
65. Hirsch JA, Donovan WD, Leslie-Mazwi
TM, Nicola GN, Manchikanti L, Silva E
3rd. Component coding and the neu-
rointerventionalist: A tale with an end. J
Neurointerv Surg 2013; 5:615-619.
66. Donovan WD, Leslie-Mazwi TM, Silva E
3rd, Woo HH, Nicola GN, Barr RM, Bel-
lo JA, Tu R, Hirsch JA. Diagnostic carotid
and cerebral angiography: A historical
summary of the evolving changes in
coding and reimbursement in a com-
plex procedure family. J Neurointerv Surg
2014; 6:712-717.
67. Medicare Payment Advisory Commis-
sion. Report to the Congress. Medicare
Payment Policy. Washington, DC: Med-
PAC. March 2017.
http://medpac.gov/docs/default-source/
reports/mar17_entirereport.pdf
68. Department of Health and Human Ser-
vices, Centers for Medicare & Medic-
aid Services. 42 CFR Parts 416 and 419.
[CMS–1695–P] Medicare Program: Pro-
posed Changes to Hospital Outpatient
Prospective Payment and Ambulatory
Surgical Center Payment Systems and
Quality Reporting Programs; Requests
for Information on Promoting Interop-
erability and Electronic Health Care In-
formation, Price Transparency, and Le-
veraging Authority for the Competitive
Acquisition Program for Part B Drugs
and Biologicals for a Potential CMS In-
novation Center Model. Proposed Rule.
July 31, 2018.
