
The author(s) shown below used Federal funds provided by the U.S.
Department of Justice and prepared the following final report:
Document Title: Delivery and Evaluation of Sexual Assault
Forensic (SAFE) Training Programs
Author(s): Debra Patterson, Ph.D., Stella Resko, Ph.D.,
Jennifer Pierce-Weeks, RN, Rebecca Campbell,
Ph.D.
Document No.: 247081
Date Received: June 2014
Award Number: 2010-NE-BX-K260
This report has not been published by the U.S. Department of Justice.
To provide better customer service, NCJRS has made this Federally-
funded grant report available electronically.
Opinions or points of view expressed are those
of the author(s) and do not necessarily reflect
the official position or policies of the U.S.
Department of Justice.

Delivery and Evaluation of Sexual Assault Forensic (SAFE) Training Programs
2010-NE-BX-K260
FINAL REPORT
March 28, 2014
Principal Investigator: Debra Patterson, Ph.D., Assistant Professor
School of Social Work, Wayne State University
Detroit, MI 48202
Phone: (313) 577-5942
Email: [email protected]
Co-Investigator: Stella Resko, Ph.D., Assistant Professor
School of Social Work, Wayne State University
Detroit, MI 48202
Phone: (313) 577-4445
Email: [email protected]
Project Director: Jennifer Pierce-Weeks, RN, SANE-A, SANE-P
International Association of Forensic Nurses
6755 Business Parkway
Suite 303
Elkridge, MD 21075
Phone: (410) 626-7805 ext. 107
Consultant: Rebecca Campbell, Ph.D., Professor
Department of Psychology, Michigan State University
East Lansing, MI 48824-1116
Phone: (517) 432-8390
Email: [email protected]
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
ii
ABSTRACT
This study evaluated the effectiveness of the IAFN SAFE training that used an innovative blended
learning approach, which included a didactic portion online over a 12-week time period and a two-day
simulated clinical skills workshop. Healthcare clinicians (e.g., registered nurses) from across the United
States were enrolled in the training (N=198). We conducted an outcome evaluation using a mixed methods
approach to assess if the training was effective with training completion, knowledge attainment, and
knowledge retention three months post-training. Students completed a Web-based survey prior to the
training to examine three factors that may impact training completion: student characteristics, motivation,
and external barriers. To assess if there was a significant increase in the students’ knowledge, we utilized a
one-group pre-test post-test design where we assessed students’ knowledge attainment for all 12 online
modules. To examine students’ knowledge retention, students took an online post-training exam three
months following the training. Qualitative interviews were conducted with the clinical instructors to
understand their pedagogical approach and challenges to teaching clinical skills. In addition, we
interviewed students until we reached saturation of the major themes (N=64) about their post-training
experiences and struggles of applying their knowledge and skills into their practice.
Regarding training completion, the findings show that 79.3 percent of the enrolled students
completed the SAFE training. Utilizing hierarchical logistic regression, the study also found that students
were more likely to complete the training when they were interested in the training because of the two-day
clinical component. Students who work in rural communities were more likely to complete the training than
students from urban and suburban communities.
Regarding knowledge attainment, the results showed that the mean post-test scores were
significantly greater than the mean pre-test scores for all 12 online modules. On over 40% of the modules,
the students exhibited at least a 25% knowledge gain. Using a multiple linear regression model, we found
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
iii
that knowledge attainment was positively associated with students who have a reliable Internet connection,
students who were drawn to the training because it was no cost to them, and those with higher levels of
motivation. Lower knowledge gains were significantly related to students who reported more work/personal
barriers and those who were drawn to SAFE practice because they or someone close to them has personal
experience with sexual assault. Lower knowledge gain also was marginally linked with students who
reported less comfort with computers.
Regarding knowledge retention, the results indicate that students experienced a reduction of
knowledge from 77.92% at post-test to 68.83% at the follow-up exam with a 9.17% loss of knowledge.
Using multiple linear regression, the analysis found that knowledge retention was higher for students who
were drawn to the training because of the clinical training, and somewhat higher for students with more
nursing experience. Knowledge retention was significantly lower for those who have taken a prior online
course, and somewhat lower for students drawn to forensic nursing because of an experience with sexual
assault.
The qualitative interviews suggested that the clinical training helped clarify, broaden, or solidify the
content covered in the online modules. Most students identified utilizing many approaches they learned in
the training with their post-training patients. Some students indicated that they encountered challenges
since they began practicing as SAFEs such as feeling less prepared to provide care for some patient
populations (e.g., males), and having limited access to trained preceptors.
In conclusion, the evaluation’s overall assessment is that the IAFN SAFE training curriculum and
blended training model offers a strong foundation that can be built upon to meet the diverse learning needs
of clinicians across the country.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

iv
TABLE OF CONTENTS
Executive Report
1
I. Overview
9
II. Review of Relevant Literature
13
A. The Importance of Sexual Assault Forensic Nurse Examiners
13
B. Online Training as a Solution to SAFE Shortage
15
C. Limitations of Online Learning
17
D. Blended Learning: A Comprehensive Training Approach
19
III. The Current Research Project: Evaluation of the IAFN Training
21
A. Training Design and Implementation
21
B. Multi-Study Project Design: Concurrent Triangulation Mixed Methods Design
27
C. Quantitative Evaluation Aims
28
D. Qualitative Evaluation Aims
33
IV. Quantitative Evaluation Aims
35
Evaluation Question 1: What Factors Predict Training Completion/Attrition?
35
A. Methods
1. Research Design
35
2. Sampling
36
3. Procedures for Data Collection
39
4. Measures
41
5. Analytic Plan
43
B. Results
1. What Predicts Training Completion?
45
2. When did Attrition Occur?
49
Evaluation Question 2: Is There a Significant Increase in the Students’ Knowledge upon Completion
of the Training Modules?
52
A. Methods
1. Research Design
52
2. Sampling
52
3. Procedures for Data Collection
54
4. Measures
55
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

v
5. Analytic Plan
57
B. Results
1. Do Students’ Attain Knowledge?
58
2. What Predicts Knowledge Attainment?
60
Evaluation Question 3: Among those who Completed the Training, did the Participants Retain their
Knowledge 3 Months Post-Training?
63
A. Methods
1. Research Design
63
2. Sampling
64
3. Procedures for Data Collection
66
4. Measures
66
5. Analytic Plan
67
B. Results
1. Do Students Retain Knowledge of SAFE Practice?
68
2. What Predicts Knowledge Attainment Over Time?
69
V. Qualitative Evaluation Aims
73
A. Methods
1. Research Design
73
2. Sampling
74
3. Procedures for Data Collection
76
4. Measures
76
5. Analytic Plan
77
B. Results
Evaluation Question 4: How did the Clinical Training Contribute to Students’ Knowledge?
78
1. Instructors’ Pedagogical Approach.
79
2. Developing Sexual Assault Patient Care Skills
81
3. Developing Medical Forensic Exam Skills
87
4. Instructors’ Challenges and Recommendations
95
Evaluation Question 5: What were the Students’ Post-Training Experiences with Applying their
Knowledge?
99
1. Application of Skills with Post-Training Patients
99
2. Students’ Remaining Challenges with Patient Care
102
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

vi
3. Students’ Remaining Challenges with the Medical Forensic Exam
107
4. Students’ Experience and Needs when Encountering Delayed Practice
112
VII. Discussion of Findings
116
A. Summary of Cross-Study Findings and Implications
116
1. Findings from Evaluation Question #1: What factors predict training completion?
117
2. Findings from Evaluation Question #2: Is There a Significant Increase in the Students’
Knowledge upon Completion of the Training Modules?
124
3. Findings from Evaluation Question #3: Did the students retain knowledge?
129
4. Findings from Evaluation Question #4: How did the Clinical Training Contribute to
Students’ Knowledge?
133
5. Findings from Evaluation Question #5: What were the Students’ Post-Training
Experiences with Applying their Knowledge?
136
6. Evaluator Guidance for Incorporating Recommendations
143
B. Project Strengths, Limitations, and Implications for Future Research
150
C. Conclusions
154
VIII. References
156
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

vii
APPENDICES
Appendix A: Project Staff
175
Appendix B: Dissemination
177
Appendix C: Data Collection Instruments
178
Appendix D: Modules
230
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

viii
LIST OF FIGURES
Figure 1: Creswell et al.’s (2003) Concurrent Triangulation Mixed Methods Design
28
Figure 2: Kaplan Meier Curve Illustrating Training Completion Over Time
51
Figure 3: Mean Increase in Knowledge from Pre-test to Post-test
60
Figure 4: Mean Increase in Knowledge from Pre-test to Post-test to three Month Follow-up
69
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

ix
LIST OF TABLES
Table 1: Overview of the Evaluation Aims
29
Table 2 (Question 1): Students’ Descriptive Statistics
40
Table 3 (Question 1): Inter-correlations among Multivariate Predictor Variables for Training
Completion Analyses
44
Table 4 (Question 1): Bivariate Cross-tabulations and Chi-squared Tests Assessing the Relationship
between Training Completion and Study Variables
47
Table 5 (Question 1): Bivariate Logistic Regression Analysis Predicting Training Completion
48
Table 6 (Question 1): Hierarchical Logistic Regression Predicting Training Completion
49
Table 7 (Question 1): Cox Proportional Hazards Model Predicting time to Attrition
50
Table 8 (Question 2): Students Descriptive Statistics
53
Table 9 (Question 2): Descriptive Statistics and t-test Results for Knowledge Attainment on Online
Modules
60
Table 10: Inter-correlations among Knowledge Attainment Multivariate Predictor Variables
61
Table 11 (Question 2): Bivariate Regression Analysis Predicting Knowledge Attainment
62
Table 12 (Question 2): Multiple Linear Regression Predicting Knowledge Attainment
63
Table 13 (Question 3): Descriptive statistics for Independent and Dependent Variables
65
Table 14 (Question 3): Inter-correlations among Knowledge Retention Multivariate Predictor
Variables
70
Table 15 (Question 3): Change in Knowledge Scores from Pre-test to Three Months Post-Training
71
Table 16 (Question 3): Bivariate Regression Analysis Predicting Knowledge Gains at Three Months
Post-Training
71
Table 17 (Question 3): Multiple Linear Regression Predicting Knowledge Retention
73
Table 18 (Question 4 & 5): Descriptive Statistics of Students Participation in the Qualitative
Interviews
75
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
1
EXECUTIVE SUMMARY
Sexual assault forensic examiner (SAFE) programs provide post-assault services to sexual assault
survivors that include medical forensic evidence collection, as well as patient-centered care to meet their
acute healthcare and emotional needs. Unfortunately, many victims do not have access to SAFE patient
care because there is a shortage of SAFE-trained clinicians across the United States. Limited access to
education has repeatedly been identified as a major contributor to the shortage of SAFE-trained clinicians,
especially in smaller communities. This project sought to address this shortage by delivering and evaluating
a comprehensive SAFE training developed by the International Association of Forensic Nurses (IAFN).
The IAFN SAFE training used an innovative blended learning approach: Students took a didactic
portion online over a 12-week time period and also attended a two-day clinical skills workshop. The 12-
week online structure allows students to learn the core content of SAFE practice without interfering with
their work schedule. The two-day clinical skills workshop was taught in a laboratory that simulates a clinical
setting with live models (gynecological teaching associate [GTA]) that allowed students to develop clinical
skills through repeated practice. To assess if the training was effective, we conducted an outcome
evaluation using a mixed methods approach, including quantitative pre-post training and qualitative
interviews with instructors and students.
The first evaluation question examined how many students completed the training and what
predicted training completion. This study used Web-based surveys that students (N=198) completed prior
to the training to examine three factors that may impact training completion and the timing of attrition:
student characteristics, motivation, and external barriers. The findings show that 79.3 percent of the
enrolled students completed the SAFE training, which is higher than completion rates for online courses in
general and substantially higher for free continuing education courses. Utilizing hierarchical logistic
regression, the study also found that students who were interested in the training because of the two-day
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
2
clinical component also were more likely to complete the training. Further, students who work in rural
communities were more likely to complete the training than students from urban and suburban
communities. In terms of when attrition occurred, we found that the instantaneous probability of attrition for
a participant who was motivated by the two-day clinical workshop was roughly a third of the probability for
those who were not interested in the two-day clinical workshop. The instantaneous probability of attrition for
those students that worked in a rural community was roughly a third of the probability for those who worked
in an urban or suburban community. The study also found that students who were interested in the training
because of its online nature were more likely to complete more of the training.
The second evaluation question examined if there was a significant increase in the students’
knowledge by utilizing a one-group pre-test post-test design where we assessed students’ knowledge
attainment for all 12 online modules. Students completed a weekly online pre-test before beginning each
training module and then a post-test upon completion of the module. The results showed that the mean
post-test scores were significantly greater than the mean pre-test scores for all 12 online modules. On over
40% of the modules, the students exhibited at least a 25% knowledge gain. The modules with high
knowledge gains included forensic science, ethics, and self-care (35.85%), photography (29.80%), medical
forensic history and physical (25.48%), evidence collection (25.63%), anogenital exam (23.93%), and the
justice system & testifying (20.75%). The modules with the lowest knowledge gains were medical
management module (15.86%), documentation (14.92%), program and operational issues (14.11%), and
patient centered, coordinated team approach (9.33%). We also examined the predictors of knowledge
attainment. Using a multiple linear regression model, we found that knowledge attainment was positively
associated with a reliable Internet connection, students who were drawn to the training because it was no
cost to them, and those students with higher levels of motivation. By contrast, lower knowledge gains were
significantly related to students who reported more work/personal barriers and those who were drawn to
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
3
SAFE practice because they or someone close to them has personal experience with sexual assault. Lower
knowledge gain also was marginally linked with students who reported less comfort with computers.
The third evaluation question sought to understand if the student retained their knowledge, which
was examined using an online post-training survey given to students three months following the training
and subsequently analyzed using repeated measures ANOVA. Our findings suggest that students
experienced a reduction of knowledge from 77.92% at post-test to 68.83% at the follow-up exam with a
9.17% loss of knowledge. Using multiple linear regression, the analysis found that knowledge retention was
somewhat higher for students with more nursing experience. Alternatively, students who have taken a prior
online course experienced significantly less knowledge retention. In addition, students who were drawn to
forensic nursing because of an experience with sexual assault was somewhat associated with less
retention of knowledge.
SAFE clinical skills are not commonly taught in a simulated laboratory setting. Thus, we wanted to
gain a more in-depth picture of the unique contributions of the clinical training with preparing clinicians for
SAFE practice. Therefore, the fourth evaluation question utilized a qualitative framework to understand the
instructors’ pedagogical approach to teaching clinical skills. In addition, we conducted qualitative interviews
to examine the students’ perceptions of the patient care and medical forensic exam skills gained from the
clinical component in the SAFE training, and how the clinical training contributed to their skill development.
Students who completed the entire training (i.e., online and clinical) were the target sample for the
qualitative interviews. We interviewed students until we reached saturation of the major themes (N=64).
The qualitative interviews also examined the fifth evaluation question: how students applied their gained
knowledge and skills into their practice with their post-training patients, along with any remaining struggles
that they encountered post-training. Furthermore, we explored the challenges experienced by a subset of
students following the training: those who are still waiting to examine their first patient (N=28 or 44% of all
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
4
students interviewed). In particular, we examined how students feel about not practicing, and if they
believed the delay will affect their abilities to practice as SAFEs.
The instructors indicated that their pedagogical approach began with creating an environment
conducive to learning by treating the students with respect and patience. The instructors began each skill
station by inquiring about the students’ clinical background to assess their learning needs. The instructors
also demonstrated components of SAFE practice, which provided students with a clear picture of the exam
process and to see the exam practiced correctly. While the students practiced different components of the
exam process with the GTAs, the instructors provided guidance and feedback. Instructors also suggested
that they promoted students’ clinical reasoning by having students’ articulate the rationale of their decisions
during the exam process. Together, the instructors believed that these different instructional methods
helped students to feel more confident with their skills by the end of the clinical training.
Because a patient-centered approach is important to the sexual assault patients’ wellbeing as well
as their participation in prosecution, we wanted to understand whether the students understood the concept
of patient-centered care. Prior to the training, several students said they had perceived the SAFE role only
as an evidence collector and identified forensic collection as their primary purpose with sexual assault
patients. By emphasizing that the well-being of the patient is paramount to SAFE practice, the training
helped students learn to see their SAFE role as an important part of the sexual assault patient’s healing. In
the qualitative interviews we asked students to describe different aspects of the SAFE role. The majority of
participants described some version of patient-centered care such as approaching sexual assault patients
with compassion and a non-judgmental attitude, and restoring a sense of control by providing them with
choices. While the entire training helped students understand the importance of patient-centered care, the
majority of students indicated that the clinical training played a stronger role in helping them learn how to
provide this model of care. The interviewed students explained that the hands-on practice and instructor
feedback were beneficial because they helped students conceptualize their approach with the patients’
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
5
comfort level in mind. Students reported that the realistic nature of the mock scenarios portrayed by the
GTAs was particularly beneficial to learning how to foster comfort during the exam and how to empower
sexual assault patients. By following the GTA’s cues (e.g. allowing or not allowing certain procedures
similar to how a patient may react), students were given practice on how to follow the needs of the patient,
which is a critical component of patient-centered care. In addition, observing the instructors demonstrate
the forensic exams and patient interactions helped students learn how to avoid re-traumatizing sexual
assault patients.
Another priority of the training was to help students attain the examination and evidence collection
skills needed to perform a competent sexual assault medical forensic examination. Overall, the majority of
students reported the clinical training substantially contributed to their knowledge and development of
medical forensic skills (e.g., history taking, conducting pelvic exams with a speculum). The GTAs’ realistic
portrayals of sexual assault patients were important in developing students’ skills, particularly with history
taking and pelvic speculum exams. During the pelvic exams, the instructors taught the students how to
identify abnormalities or injury using visualization and equipment. Students also learned about and were
able to practice photographing injuries and practice the Toluidine blue dye application and the Foley
catheter techniques. As a result of these instructional activities, the majority of students noted that they left
the training feeling confident enough to begin practicing.
For students who have had patients since the training, we asked them to describe a couple of post-
training cases and to describe how they approached or interacted with these patients. Students identified
utilizing many approaches they learned in the training to enhance their patients’ sense of safety, including
using a slower, gentler approach combined with non-threatening tone of voice and body language,
following the patients’ needs and allowing them to tell their story without interruption to build patient-
provider trust and rapport. Students also described offering their patients detailed explanations, validating
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
6
their experiences and avoid making any blaming or judgmental statements. Students reported this
approach appeared to help their sexual assault patients feel safe during the exam process.
We were also interested in understanding the quality of the students’ medical forensic evidence
documentation for exams with sexual assault patients following the training. Thus, the qualitative interviews
inquired if the students had received feedback from an experienced colleague or supervisor regarding their
documentation with sexual assault patients. Overall, we found that most students were not provided
feedback about their documentation from a supervisor or colleague. Some of the students who did receive
feedback were provided with brief remarks that they had done a good job with their documentation, while
others who do not have SAFEs in their institutions sought feedback from their department supervisors and
were told their documentation was detailed and thorough. A smaller number of students were provided with
feedback from trained SAFEs who indicated that the students’ documentation was of high quality.
The qualitative interviews also inquired about students’ remaining challenges they have
encountered since they began practicing as SAFEs. Although the clinical training included the practice of
patient interaction skills, many interviewed students expressed fear of re-traumatizing patients. Many
students also felt less prepared to provide care for male patients, patients with disabilities, and patients who
exhibit strong or absent emotional reactions. Students who practice in rural and low-resource SAFE
programs also continue to struggle with patient care due to their unique settings and challenges. For
example, some students reported they do not have local victim advocacy groups, which has resulted in
their role expanded to include the type of emotional support often provided by advocates. As a result, they
were less confident in their patient comfort skills. The students also identified several areas of struggle with
the medical forensic exam and documentation. Although the clinical training included several practice
opportunities, many students reported feeling unprepared for some aspects of the medical forensic exam
such as using the colposcope. Some students expressed a lack of confidence in the quality and accuracy
of their evidence collection because they have not received feedback from a SAFE in their institutions.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
7
Overall, the students believed that more practice opportunities during the clinical training would have let
them refine their skills.
Lastly, the interviews examined the challenges of those students who are still waiting to examine
their first patient. Many of the students who had not performed an exam remained committed to being a
SAFE. These students said they stayed motivated by keeping up with information and seeking out
educational opportunities. In addition, students found community groups (local IAFN chapter) to keep
abreast of SAFE topics while connecting to other SAFEs. Several students said they would be able to
perform an exam because the skills they learned in the training would be quickly remembered and
incorporated into their practice. However, several students said they would approach their first exam with
less confidence than they would had they performed their first exam immediately following the training.
Despite this decreased confidence, these students still expressed their continued interest in pursuing SAFE
work.
In conclusion, the evaluation identified many successes of the training. The majority of students
completed the training. Students exhibited high knowledge gains in the online modules pertaining to
forensic science, ethics, and self-care; photography; medical forensic history and physical; evidence
collection; anogenital exam; and justice system and testifying. Further, students experienced a fairly high
level of knowledge retention in comparison to the rates reported in prior research. As common with the
initial development of a training, the evaluation identified many challenges and recommendations. Students
experienced lower knowledge gains in multiple online modules, including those focusing on medical
management; documentation, program and operational issues; and patient-centered, coordinated team
approach. Several students indicated that these lengthy modules could be improved by breaking them into
subsections, as well as adding homework assignments that would allow instructors to provide formative
feedback on student progress. Many students in the qualitative interviews indicated that the clinical training
helped clarify, broaden, or solidify the content covered in the online modules. Finally, the evaluation
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
8
identified distinct learning needs of students with less healthcare experience and from rural communities,
which will require some modifications to the training. For example, these students believed that additional
practice time during the clinical training, as well as post-training supports (e.g. refresher training), would
have helped them feel more prepared to practice as SAFEs. These challenges and recommendations
notwithstanding, the evaluation’s overall assessment is that the IAFN developed a comprehensive SAFE
training curriculum that has the potential to meet the diverse learning needs of clinicians across the country.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

9
I. Overview
National epidemiological data suggest that at least 17% of women will be sexually assaulted in
their adult lifetimes (Tjaden, & Thoennes, 1998, 2006); however, most victims/survivors do not report to law
enforcement (Bureau of Justice Statistics, 2007). Overall, approximately 18% of reported sexual assaults
are prosecuted (Campbell, 2008a; Spohn, 2008). When rape victims/survivors seek professional help after
an assault, they are most likely to be directed to the medical system, specifically hospital emergency
departments (ED) (Resnick et al, 2000). Over the years, both researchers and rape victim advocates have
noted numerous problems with this ED-based approach to post-assault health care and forensic collection
(Martin, 2005; Campbell & Martin, 2001; Campbell & Bybee, 1997). Many ED physicians are reluctant to
perform the rape exam (Martin, 2005), and most lack training specifically in forensic evidence collection
procedures (Littel, 2001). As a result, many rape kits collected by ED doctors are done incorrectly and/or
incompletely (Littel, 2001; Sievers, Murphy, & Miller, 2003). Additionally, emerging research indicates that
many rape victims are retraumatized by post-assault ED exams, which often leave them feeling more
depressed, anxious, blamed, and reluctant to seek further help (Campbell et al., 2001; Campbell et al.,
1999; Campbell & Raja, 1999; Campbell, 2005). These negative experiences have the unintended effect of
decreasing victims’ willingness to participate in law enforcement investigations and legal prosecution
(Campbell, 1998).
To address these problems, communities have implemented Sexual Assault Forensic Examiner
(SAFE) Programs
1
. These programs employ specially trained clinicians, usually nurses (rather than hospital
emergency department physicians) to provide comprehensive psychological, medical, and forensic services
for sexual assault victims (DOJ, 2004, 2006). SAFE programs can be a vital resource to victims as well as
the legal community, with prior research suggesting that these programs have improved the response
1
For purposes of this report, we will primarily refer to the medical personnel as SAFEs to be inclusive of all medical disciplines.
In addition, we will use the term “sexual assault” to reflect the broader range of contact and non-contact sexual offenses
including rape (see Koss & Achilles, 2008).
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
10
towards victims by meeting their acute healthcare and emotional needs, as well as the quality of medical
forensic evidence collection and documentation (Cabral, Campbell, & Patterson, 2011; Derhammer,
Lucente, Reed, & Young, 2000; Ledray & Simmelink, 1997; Sievers et al., 2003). This fundamental shift
has had a positive impact on the prosecution of rape cases (Campbell, Patterson, & Bybee, 2012; Crandall
& Helitzer, 2003). Therefore, it is critical that patients have access to SAFE clinicians, as they provide a
bridge between healthcare and legal systems.
Unfortunately, many victims do not have access to SAFE patient care because there is a shortage
of SAFE-trained clinicians across the United States. Limited access to training has repeatedly been
identified as a major contributor to the shortage of SAFE-trained clinicians, especially in smaller
communities. As recently as December 2009, IAFN’s SAFEta Project Coordinator noted that in the course
of delivering specific technical assistance around the National Protocol for Sexual Assault Medical Forensic
Examinations of Adults/Adolescents, many rural and tribal areas are still struggling to find and provide
SAFE training for healthcare providers (K. Day, personal communication, May 1, 2010). The structure of
SAFE courses also may limit accessibility to training for some clinicians. Per the IAFN’s Sexual Assault
Nurse Examiner Educational Guidelines, this included 40 hours of didactic education followed by
recommended clinical activities that complement the didactic content. Traditionally, SAFE courses are
taught in-person over the course of one week, with students fulfilling their clinical hours following the
didactic education by performing pelvic exams at healthcare clinics with patients who are seeking routine
gynecological care. This is followed by the students practicing SAFE-related skills with sexual assault
patients under the supervision of a preceptor. The traditional one-week didactic course structure requires
training participants to incorporate training schedules into their personal and professional lives. Often, this
means that students are using vacation time and are paying for travel expenses out of pocket, which may
not be possible for all interested clinicians. Even when clinicians are able to complete the didactic training,
they may experience difficulty with obtaining necessary post-didactic clinical hours, which may prevent
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

11
trained clinicians from practicing as SAFEs. Attrition may be problematic as many trainers estimate that
roughly half of those who complete the training will actually practice as a forensic examiner
2
.
The purpose of this current project was to develop and evaluate a comprehensive sexual assault
medical-forensic examination training program that would reduce students’ barriers to accessing and
completing SAFE training. This project enabled IAFN to create and implement standardized, accessible
SAFE training on a national level by utilizing a blended training structure. Blended training incorporates
online and face-to-face modalities within a training by placing the didactic component of training online
while the face-to-face component focuses on skill building. The SAFE training taught a patient-centered
approach, the examination and evidence collection skills needed to perform a competent sexual assault
medical-forensic examination, and to impart knowledge of the criminal justice process to enable effective
courtroom testimony.
Most SAFE training is conducted in a classroom setting, during a one-week timeframe with a series
of PowerPoint presentations and minimal hands-on activities. However, spacing the content over a longer
timeframe rather than a truncated amount of time can improve knowledge retention (Bell et al., 2008). In
addition, an active learning approach has been shown to be substantially effective for learning clinical skills
(Stefanski & Rossler, 2009). The IAFN SAFE blended training was designed so that students took the
didactic portion online over a twelve-week time period through a series of modules. The bulk of the didactic
course was completed on the students’ own schedules, which increases accessibility to high-quality training
for rural and remote clinicians, and those who cannot leave their employment for a week-long training.
Obtaining clinical education has been a challenge for many clinicians who have completed the didactic
portion of SAFE training. Many communities have no experienced SAFEs with whom clinicians can train, or
2
Anecdotal conversations with trainers including Susan Chasson, Jenifer Markowitz, Jennifer Pierce Weeks, Kim Day and Carey
Goryl, also based on the number of SANE/SAFE courses listed in IAFN’s training calendar averaged annually and the number of
memberships to IAFN generated from these classes.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
12
simply have too few patients to obtain clinical competency. The IAFN training addressed these barriers by
providing a face-to-face two-day clinical skills workshop following the didactic series. The workshop
provided students with the opportunity to gain critical clinical skills as students were provided hands-on
experience through multiple case scenarios with gynecologic teaching associates (GTAs). Moreover, the
workshop provided an opportunity for participants to form a valuable network of mentors and peers to
provide support and assistance. The blended course was offered three times to allow for a manageable
course size to ensure that students’ learning needs were met. This course was available to clinicians at no
cost.
To assess if the training was effective, an outcome evaluation using a mixed methods approach
was conducted. First, the evaluation examined training completion, including the percentage of students
who completed the training and the factors that contributed to their completion. Second, the evaluation
assessed whether students attained knowledge through pre-test/post-tests and the factors that contributed
to knowledge attainment. We also conducted qualitative interviews with students to understand how the
clinical training contributed to their knowledge of patient and medical forensic exam skills. In addition,
qualitative interviews were conducted with the instructors to understand how they approached the clinical
training, challenges that they encountered during the training, and recommendations for future trainings.
Third, students’ retention of their knowledge was evaluated through a post-training exam approximately
three months following the training. Furthermore, qualitative interviews were conducted with students to
explore how the students applied their gained knowledge and skills into their practice following the training.
In addition, the interviews explored any challenges that the students encountered post-training, and their
recommendations for future trainings.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

13
II. Review of Relevant Literature
A. The Importance of Sexual Assault Forensic Examiners
Sexual Assault Forensic Nurses Examiner (SANE/SAFE) Programs emerged in the 1970s and now
number close to 600 programs throughout the United States (IAFN, 2013). Examiners in these programs
provide extensive psychological, medical, and forensic services for rape victims. The goal of SAFE
programs is to provide supportive care to victims while improving prosecution rates. SAFE programs strive
to improve prosecution by providing: 1) better-quality medical forensic evidence collection by specially
trained healthcare clinicians; 2) case consultation for law enforcement officials to increase their
understanding of medical evidence findings; and 3) expert witness testimony (Littel, 2001).
Research has found that SAFE programs can contribute to increased reporting and prosecution
rates for sexual assault cases (Campbell, Patterson, & Bybee, 2012). Campbell and colleagues (2008)
identified that SAFE practice can positively impact criminal justice outcomes through increased
engagement of sexual assault patients in the investigative and prosecution process (Patterson & Campbell,
2010). In particular, SAFEs help their patients begin the process of reinstating control over their bodies and
lives by not pressuring them to report to law enforcement. They emphasize that it is the victims’ choice and
SAFEs are there to care for them whatever they decide (Campbell, Greeson, & Patterson, 2011; Campbell,
Patterson, Adams, Diegel, & Coats, 2008). This attention to helping survivors heal indirectly affects their
willingness to participate in legal prosecution. When survivors are not as traumatized, they are more willing
and capable of participating in the prosecution process. In addition, survivors often have questions about
the medical forensic exam and the process of criminal prosecution. When forensic examiners provide
patients with this information, victims have more hope for and confidence about their legal cases, which
also indirectly contributes to increased victim participation (Campbell, Patterson, Bybee, & Dworkin, 2009).
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
14
Competent medical/forensic care can also provide victims with greater confidence in the criminal
justice system as a result of effective collaboration between SAFEs and colleagues in law enforcement and
prosecution (Campbell, Patterson, & Cabral, 2010). Clinical education on the medical forensic exam
process helps cultivate and enhance clinicians’ skills as expert witnesses and teaches effective trial
preparation in collaboration with prosecutors.
Numerous case studies suggest that SANEs are a vital resource to police and prosecutors (see
Campbell, Patterson, & Lichty, 2005 for a review). SAFE programs give law enforcement personnel and
prosecutors state-of-the-art forensic evidence to document crimes of sexual assault. The evidence
collected by the SAFE is typically sent to the state crime lab for analysis and the results are forwarded to
the prosecutor’s office. For example, research has shown that medical forensic evidence (MFE)
significantly predicts increased case progression, even after accounting for other characteristics that
traditionally have stunted case progression (e.g., use of alcohol). As such, the quality of the documentation
is paramount to successful legal outcomes. High-quality documentation also increases the likelihood that
law enforcement and prosecutors will utilize this documentation in their work. Detailed documentation may
suggest investigational leads that law enforcement could pursue to further develop a case. Prosecutors are
more inclined to charge cases when quality MFE documentation exists and often utilize this documentation
as a tool for plea bargaining when appropriate (Campbell et al., 2009). Two NIJ-funded, quasi-experimental
pre-post studies found that prosecution rates significantly increased after the implementation of SAFE
programs (Campbell, Bybee, Ford, Patterson, & Ferrell, 2009; Crandall & Helitzer, 2003). These results
suggest SANE programs may be effective in addressing the under-prosecution of sexual assault.
Overall, the emerging literature has suggested that SAFE programs play a critical role in improving
the response towards sexual assault victims, as well as prosecution rates. Despite the importance of SAFE
programs, there is a shortage of trained SAFEs in many communities often due to lack of accessible
training. This may be particularly true for less populated, geographically dispersed areas such as smaller
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

15
cities, rural communities, and tribal lands where access to training has been limited (Roberts, Brannan, &
White, 2005). In addition, remote/rural locations often struggle with competency due to limited or
nonexistent local expertise and low patient volume. Consequently, many victims across the United States
do not have access to quality patient care and expert medical forensic evidence collection following a
sexual assault.
B. Online Training as a Solution to SAFE Shortage
Online training may be a viable solution to increasing the number of trained SAFEs. Online training
has gained popularity and acceptance as a legitimate educational forum for providing high quality
healthcare training (Allen, & Seaman, 2010; Miller, Devaney, Kelly, & Kuehn, 2008; Ruiz, Mintzer, &
Leipzig, 2006). In addition, online training addresses a common barrier for many clinicians – family and
work responsibilities – of participating in professional training (Gormley, Costanzo, Lewis, Slone, & Savage,
2012). Online training is flexible and convenient and thus, time and costs associated with travel are
eliminated (Johnston, 2007). As such, online training increases accessibility to those living in remote areas
or those would have had to take time off from their jobs for training to attend a week-long classroom
training (Welsh, Wanberg, Brown, & Simmering, 2003; Pratt, 2002). Additionally, online training increases
the opportunity for students to have national experts serve as their instructors (Miller, Devaney, Kelly, &
Kuehn, 2008).
The extant literature has examined satisfaction and effectiveness with online learning among
practicing and student nurses, physicians, and other healthcare professionals. This literature suggests that
many healthcare students have characterized their online learning experience as primarily satisfactory
(Atack, 2003; Atack & Rankin, 2001; Bloom & Hough, 2003). In particular, students appreciate the flexibility
in scheduling and reduced travel, as well as the self-directed and self-pacing nature of online learning
(Roberts, Brannan, & White, 2005; Salyers, 2005). Students believed that this reduction in travel time could
be devoted to learning course concepts (Bello et al., 2005). Learners also expressed satisfaction with
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
16
online courses when they were provided with opportunity to share information, ask questions, and receive
feedback from other students and the instructor (Atack, Rankin, & Then, 2005; Johnson, Hornik, & Salas,
2008). Additionally, students find online training satisfactory because it provides multiple types of activities
for learning, such as recorded lectures, case studies, links to articles, patient interviews, and interactive
videos (Atack , Rankin, & Then, 2005; Zhang, Zhou, Briggs, & Nunamaker, 2006).
In terms of effectiveness, the overwhelming majority of studies have found online learning to be
effective in increasing knowledge across a wide variety of topics and healthcare learners (e.g., registered
nurses, medical and nursing students, physicians) (Cook et al., 2008; Smith, Silva, Covington, & Joiner,
2013; Stone, Barber, & Potter, 2005; US Department of Education, 2010). Furthermore, research has
suggested that online learning is effective for improving healthcare professional’s competencies, which
yields better patient care (Atack, Rankin, & Then, 2005; Schneiderman, Corbridge, & Zerwic, 2009).There
have been fewer studies examining knowledge retention following the training. These studies found the
degree of knowledge retention has been correlated positively to course satisfaction, student motivation, and
the amount of time spent with the online material (Metcalf, Tanner, & Buchanan, 2010; Naidr et al, 2004). In
addition, opportunity to discuss course content among students and with the instructor on discussions
boards has been linked to successful learning outcomes (Johnston, 2007; Means, Toyama, Murphy, Bakia,
& Jones, 2010).
Many studies have compared the effectiveness of online learning to the traditional face-to-face
classroom setting among healthcare learners, and found them to be equally effective with attaining
knowledge (Bello et al., 2005; Buckley, 2003; Day, Smith, & Muma, 2006; Hugenholtz, Croon, Smits, van
Dijk, & Nieuwenhuijsen, 2008; Jeffries et al., 2003; Leasure et al., 2000; Pratt, 2002; Salyers, 2005;
Walters, Raymont, Galea, & Wheeler, 2012; Woo & Kimmick, 2000). Although the majority of studies
suggest that online learning is neither inherently superior nor inferior to face-to-face learning (Cook et al.,
2008), a few studies have suggested that online learning produces modestly better learning outcomes
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

17
(Bandla et al., 2012; Means, Toyama, Murphy, Bakia, & Jones, 2010). Alternatively, a couple of studies
found mixed results with the online participants yielding higher scores than face-to-face learners on some
topics taught in the course but lower scores on other topics (Jang, Hwang, Park, Kim, & Kim, 2005;
Johnston, 2008). There is a dearth of research examining knowledge retention between these two learning
modalities, but a couple of studies tracked their participants’ pass rates for national certification exams and
found mixed results. For example, Hansen-Suchy (2011) found no significant differences in certification
exam scores for medical laboratory technicians and first time pass rates between online and face-to-face
learners. However, Johnston (2008) found that the exam scores for the patient care section of the
American Registry of Radiologic Technologists certification exam were higher for face-to-face learners than
for those online learners. Taken together, this research suggests that online and face-to-face modalities
produce similar learning outcomes in general, but each modality may provide learning conditions favorable
for particular topics.
C. Limitations of Online Learning
Although effective, online learning has its challenges. While research has suggested that the
majority of healthcare students find online learning satisfactory, some students may find this learning
modality less satisfying or more challenging. For example, students who have less comfort and experience
with computers would have difficulty maneuvering an online learning management system and would
require more technological guidance (Atack, Rankin, & Then, 2005). In addition, students may misperceive
online courses as easier and underestimate the amount of time needed to maintain the course expectations
(Johnston, 2007). Some students prefer the face-to-face learning experience because it offers opportunity
for direct interaction and opportunity to receive answers to their questions in real-time (Bandla et al, 2012;
Day, Smith, & Muma, 2006). Therefore, some students may experience feelings of isolation in an online
course, particularly if there is limited opportunity for students to interact with each other or receive feedback
from the instructor (Atack & Rankin, 2001; Johnston, 2007).
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
18
Another common challenge is that fewer students complete online courses. Research has
compared attrition rates between online and face-to-face settings, and found that online courses tend to
have higher attrition rates, often exceeding the classroom by 10%-20% (American Association of Colleges
of Nursing, 2010; Gilmore & Lyons, 2012). Attrition can be particularly challenging for free continuing
education courses because students may not be serious about completing the course (Stone, Barber, &
Potter, 2005). For example, Walters and colleagues (2012) reported a 53.1% completion rate for a
continuing education medical course. Gyorki et al. (2013) found a similar completion rate of 55.3% of those
who began the continuing education course but also noted an even earlier risk of attrition. Of those who
enrolled in the training, only three-quarters actually started the course.
Why are attrition rates higher for online courses? While student demographics and course
satisfaction have not been found to influence attrition substantially, lack of time, low motivation, and job
changes appear to contribute to attrition rates (Martinez, 2003; McMahon, 2013; Patterson & McFadden,
2009). For example, students who had more family responsibilities or worked full-time were more likely to
drop a course (Angelino, Williams, & Natvig, 2007; Willging & Johnson, 2009). Furthermore, students were
less likely to complete a course when they experienced personal and family problems such as health
concerns or death of a family member (Perry, Boman, Care, Edwards, & Park, 2008). Further, students with
less motivation may drop an online course because it requires more self-discipline and self-pacing than
traditional courses (Atack, 2003). Additionally, students may not complete a course if they realize that the
training no longer fits with their career aspirations (Perry, Boman, Care, Edwards, & Park, 2008).
Finally, clinical skills are complex and difficult to teach so it is unclear if online courses are
conducive for learning these complex skills (Rowe, Frantz, & Bozalek, 2012). Research has suggested that
online healthcare learners have additional needs that are typically addressed in the traditional face-to-face
classrooms, such as time to practice new skills (Atack & Rankin, 2001; Gilmore & Lyons, 2012). Blended
learning (also termed “hybrid”) may be a solution to address some of the challenges of online learning by
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

19
combining the online modality with the face-to-face setting (Means et al., 2010). This approach allows
students to gain new knowledge online while practicing new skills in the face-to-face setting.
D. Blended Learning: A Comprehensive Training Approach
Blended learning is a fairly new training approach in healthcare (Makhdoom, Khoshhal, Algaidi,
Heissam, & Zolaly, 2013), but it might be particularly advantageous because students receive the benefits
of both the online and face-to-face learning modalities. For example, most blended learning models places
the primary content in the online component, which allows healthcare students to learn the core content at
a flexible pace, reducing the common training barriers of work and family responsibilities (Gormley,
Costanzo, Lewis, Slone, & Savage, 2012). When students gain a solid knowledge of the content online, it
optimizes the time allotted for students to practice new skills during the face-to-face component (Bradley et
al., 2007; Lehmann, Bosse, & Huwendiek, 2010). Additionally, the face-to-face interaction provides
opportunity for students to interact with other students and ask questions of the instructor while they are
practicing skills (Gormley, Costanzo, Lewis, Slone, & Savage, 2012). Together, the blended learning model
provides a richer learning experience that meets the varied needs of students (Wild, Griggs, & Downing,
2002). Consequently, healthcare students who participate in blended learning tend to report feeling more
motivated and satisfied than those in an online or face-to-face only training (Bradley et al., 2007; Sung,
Kwon, & Ryu, 2008).
There have been few studies examining the effectiveness of blended learning for clinical
healthcare training (Rowe, Frantz, & Bozalek, 2012), but the existing research suggests favorable
outcomes. In a systematic review, Rowe and colleagues (2012) report that blended learning can enhance
clinical competencies such as history taking, performing examinations, documentation, and clinical
reasoning. Other studies have examined the effectiveness of blended learning to the traditional face-to-face
setting, and found that students who participated in blended training had significantly higher mean scores
(Makhdoom, Khoshhal, Algaidi, Heissam, & Zolaly, 2013; Means, Toyama, Murphy, Bakia, & Jones, 2010;
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
20
Stewart, Inglis, Jardine, Koorts, & Davies, 2013; Pereira et al., 2007; Sung, Kwon, & Ryu, 2008). Only one
study has examined knowledge retention of healthcare students who participated in a blended training, and
they found that students retained their knowledge two to four weeks following the training (Karamizadeh,
Zarifsanayei, Faghihi, Mohammadi, & Habibi, 2012). Blended learning may yield stronger effects because
students receive additional learning time and materials within two learning contexts, which increases the
likelihood of meeting the diverse learning needs of students (Means et al, 2010; Stewart, Inglis, Jardine,
Koorts, & Davies, 2013). Furthermore, the classroom learning likely reinforces the content learned online,
which can facilitate knowledge retention (Bradley et al., 2007).
Overall, blended learning addresses many of the common barriers to accessible training by placing
most of the students’ learning time online, but it also addresses some of the challenges with exclusive
learning online. As such, blended learning may be a viable option for increasing the accessibility of SAFE
training while advancing the students’ clinical skills. A clinical component of the training allows students to
have earlier exposure to gaining clinical skills essential for SAFE practice, which may be particularly
important for new SAFEs working in geographically dispersed communities where there are low volumes of
sexual assault patients. In this case, students might experience a delay in applying their new knowledge
and skills while they are waiting for their first sexual assault patient. In addition, there is a shortage of
nursing preceptors in these areas, including preceptors who have training as SAFEs (Elfrink, Kirkpatrick,
Nininger, & Schubert, 2010). This shortage may prevent new SAFES from receiving adequate clinical
experience to gain core competencies. Thus, a clinical component of a SAFE training may circumvent
these issues by helping students develop their foundational clinical skills. However, there is a dearth of
research on whether a blended training model is effective in developing the knowledge and skills essential
for competent SAFE practice.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

21
III. The Current Research Project: Evaluation of the IAFN SAFE Blended Training
A. Training Design and Implementation
1. Training Development. In accordance with best practices for online learning, the training was
developed through a peer review process (Ruiz, Mintzer, & Leipzig, 2006). In 2011, two focus groups were
convened in order to develop the online curriculum for the Sexual Assault Forensic Examiner
adult/adolescent training. The first focus group was comprised of community-based advocates, detectives,
prosecutors and crime lab analysts from across the United States. The second focus group was comprised
of SANE-A board certified Sexual Assault Nurse Examiners, advanced practice nurses and physicians from
across the United States. Under the facilitation of the Project Director and the assistance of a curriculum
specialist, the focus groups reviewed existing curriculum in conjunction with the International Association of
Forensic Nurses Sexual Assault Nurse Examiner Education Guidelines. The curriculum was edited to the
approval of both groups and formatted utilizing the American Nurses Credentialing Center format for
continuing education activities, and content expert presenters for specific topics were identified.
The full online curriculum was separated into twelve distinct modules. Current bibliographic
references for each module were compiled along with participant handout material that would be utilized in
the presentation material. Content experts developed specific PowerPoints for their presentations based on
the agreed upon curriculum, and created an audio recording of their lectures. This allowed students to view
PowerPoint slides while hearing the lecture. The project director in conjunction with the curriculum
consultant developed pre-test and post-test questions for each individual module to be completed by
course participants within the Learning Management System.
All finalized recorded content was transcribed and formatted into Shareable Content Object
Reference Model (SCORM) for the web-based e-learning system. Content was then loaded and launched
from the Digital Ignite Learning Management System. The Digital Ignite SCORM compliant Learning
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

22
Management System (LMS) housed the online training and discussions during course delivery. Each
participant's progress was tracked by the LMS, and participation was tracked online by the Project Director.
Each online module included a pre-test and post-test for participants, tracking their before and after
knowledge of content. The LMS was able to support a variety of learning formats including Flash, streaming
video and audio narrations, and various reading assignments and materials hosted internally. The
evaluations of each module and the overall course were also housed and tracked internally within the LMS.
The clinical skills lab curriculum was developed from a previously implemented clinical skills
training launched on the East Coast over 10 years ago, and was based on a precepted competency
assessment of SAFE-trained nurses working in rural communities with low volumes of sexual assault
patients. This existing one-day curriculum was expanded to a curriculum that would allow for one day of
training, including hands-on demonstration with live simulated patients, in the technical aspects of the
examination (evidence collection, speculum use, culture collection, Foley catheter, Toluidine blue dye and
colposcope use, photography and history taking). Day one was followed by a second day of training where
the precepted students performed mock complete sexual assault medical forensic examinations using live
simulated patients while being taught and evaluated by preceptors. The live clinical skills lab curriculum
was reviewed and revised by the medical expert focus group in keeping with the necessary clinical skills
acquisition expected of practicing Sexual Assault Forensic Examiners, whether they are registered nurses
or advanced practice providers, according to the IAFN SANE Education Guidelines.
2. Quality Assurance. During the in-person focus groups, nationally recognized experts from the
fields of advocacy, law enforcement, prosecution, medical and criminalistics (forensic science) gathered to
review, revise and approve the online and live clinical skills curriculum in keeping with the IAFN SANE
Education Guidelines and national protocols. The Project Director and curriculum expert outlined the
objectives in keeping with Bloom's Taxonomy of Educational Objectives, including the six categories of
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

23
knowledge, comprehension, application, analysis, synthesis and evaluation. The content was then outlined
and sequenced with timeframes for completion, and all objectives were evaluated by participants.
3. Didactic Online Content. SANE training can look very different from one state to another, and
while the IAFN Education Guidelines are specific with regard to content that must be covered, how that
content is covered across jurisdictions is less clear. It was necessary that the content be generalizable
across jurisdictions, and that the students be able to pull out state- or territory-specific information
whenever necessary. Additionally, there are considerable differences between delivering an online versus
live audience training. It was important to utilize instructors that understood the absence of the live student,
and were willing and able to engage with students in different formats (i.e. email, online discussions) to
address any content questions that arose.
Therefore, Didactic Content Instructors were chosen across a wide geographic distribution based
on their extensive work in their area of expertise (SANE Practice, advocacy, investigation, criminalistics
[forensic science], prosecution) and for their known training ability. Because students would be attending
from all over the country, a mix of instructors was chosen from around the United States to represent the
larger country rather than a specific location. Many of the chosen instructors were from the original
curriculum development focus groups. Below is a summary of the content covered in the modules.
a) SAFE training introduction. The participants were introduced to the online learning management
system, logging in, how to negotiate completion of the pre-tests and post-tests, managing both the content
and handout materials, and troubleshooting technology issues. This module also introduced participants to
the SAFE field, including its history and the role of the SAFE.
b) Module I: Dynamics. The participants were given a basic introduction to the prevalence,
incidence and misconceptions that surround rape, sexual assault and abuse in the adult and adolescent
populations. An overview of the varying needs of specific patient populations (e.g., males, military, prison
population, LGBTQ, disabilities, etc.) were covered during this module.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
24
c) Module II: Forensic science, ethics and self-care. This module provided the fundamental basis
for the work as a sexual assault examiner, including evidence-based practice, the role of the sexual assault
examiner in the care of the patient who has experienced sexual violence, and the ethical implications of
practice. Additionally, recognizing the impact of trauma on the health and well-being of the examiner is
paramount to ensuring the ability to continue providing services. This module provided a baseline
understanding of what impact compassion fatigue can have, and how a plan may be devised to counter or
address that impact.
d) Module III: Patient-centered, coordinated team approach. While the focus of this training is on
the healthcare response to sexual assault and its implications on the patient’s long-term health and well-
being, it is only one component of a larger response with multiple service providers. Each responder to
sexual assault plays a different role, and it is best practice to assure that this approach is coordinated and
streamlined as much as possible to provide a comprehensive, holistic, healing process for the patient. This
module of the training explained the roles of the various responders to sexual assault. Striving to have a
coordinated, multidisciplinary team approach may be another area where the examiner is expected to
provide leadership at the community level. Recognition of the roles of different responders is an important
concept for the examiner.
e) Module IV: History and physical. The medical forensic history is one of the fundamental
components of the examination. It is from that history that important details of the assault may emerge
(e.g., relationship between victim and assailant, suspected drug or alcohol-facilitated assault), the plan of
care is developed, and evidence collection proceeds. In this module, the examiner recognized the
importance of developing and integrating the proper communication skills necessary to formulate the plan
of care. The module also covered how to gather a history when drug- and alcohol-facilitated sexual assault
is suspected, and how to complete a thorough physical assessment of the patient. This assessment
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
25
includes the head-to-toe assessment process, normal development and anatomy, identification of common
non-genital injuries that may be associated with sexual violence.
f) Module V: Anogenital exam. The assessment of the anogenital area is one of the capstones of
the medical forensic examination. This module included information for the participant on preparing the
patient for the genital examination and on the identification of the structures of the normal male and female
genitalia. Introduction to anatomical variants and disease processes that can be encountered during the
examination were also be presented. Examination techniques and adjuncts that can help facilitate
visualization of the genital anatomy and structures were detailed.
g) Module VI: Photography. This module focused on photography that can be utilized during the
medical forensic examination of the patient who has experienced sexual violence. Photographic
documentation of injury and visible evidence can help to augment the written documentation of the
examination. Taking photographs of the areas of the patient’s body that were involved in the sexual assault
are a routine part of the examination process. The participant must also recognize the purpose of
photography in the medical forensic examination, as well as privacy and storage of images.
h) Module VII: Evidence collection. The collection of forensic samples during the examination is
another critical component of the medical forensic evaluation in the acute patient. Recognizing basic
forensic principles and applying them along with the medical forensic history that has been obtained from
the patient will guide the evidence collection process. These forensic principles and evidence collection
techniques, including those pertaining to drug- and alcohol-facilitated sexual assaults, were the focus of this
module.
i) Module VIII: Documentation. This module focused on the proper use of medical documentation
following sexual assault care, including gathering a verbatim history, documenting using quotations from
the patient, objective versus subjective notes, incorporating implementation of treatment and referrals.
Timing of documentation, the electronic record and storage and release issues were discussed.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

26
j) Module IX: Medical management. The medical management of the patient who has experienced
sexual violence is the focus of this module. The health consequences of sexual violence were covered
including acute health needs (e.g., prophylaxis treatment for sexually transmitted infection (STI), injury
treatment, HIV post-exposure prophylaxis and pregnancy prevention) to long-term issues (e.g., counseling,
psychological consequences). It is imperative that the examiner remain focused on treating and preventing
the sequelae from the sexual assault.
k) Module X: Program and operational issues. Institutions may or may not have formalized
programs in place. Working with and establishing formal SANE/SAFE programs may be an expectation of
some facilities and may fall to the trained examiner. This module explored various models of care delivery
that sexual assault programs can operate under, and offered a foundational emphasis for program
development and a glimpse into sustainability issues that programs face.
l) Module XI: Justice system. Examiners will be called upon to provide testimony in court as either
fact and/or expert witnesses. This module focused on providing an overview of the different criminal court
systems that the examiner may be called to interact with, including federal, tribal, civil and state court
systems. This module provided information for the examiner on how the examiner may be called upon to
ethically testify in multiple courtroom venues about the findings from the medical forensic examination.
4. Clinical Content. Clinical Skills Workshop Instructors were chosen from a long-running, high-
volume forensic nurse examiner program in the city where the live clinical skills training was taking place.
All of the clinical instructors/preceptors were practicing SANE's, most with SANE-A and SANE-P
certification. All had been trained as Sexual Assault Forensic Examiners and had extensive experience
taking care of this patient population in rural, tribal and urban programs throughout the country. The
preceptors all had experience training newly hired SANEs in performing all functions of the job. Several
preceptors had experience training in the simulation lab environment, and the project director who
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

27
supervised all the clinical skills trainings had more than 10 years of experience utilizing a simulation lab and
the live model approach to training.
Module XII: Clinical skills workshop. This live, 16-hour session occurred over the course of two
days in a simulated teaching lab in a Colorado hospital. The clinical skills workshop began with a brief
orientation to provide an overview of the workshop. The students were divided into small groups and
rotated through the different skill stations throughout the two days. Each clinical skill station was taught by a
trained SAFE instructor (preceptor) and included a live model (gynecological teaching associate [GTA]) as
a simulated patient. In addition, a professional photographer with healthcare experience instructed students
on how to use a camera to document injuries. Each GTA role-played a patient scenario such as an
adolescent patient, a patient who was sexually assaulted by an intimate partner, a patient who experienced
a drug-facilitated sexual assault, and a patient who was sexually assaulted by a stranger. Instructors
demonstrated how to interact with patients in a compassionate, empowering manner, and how to perform
medical forensic exams and various techniques. Subsequently, students were provided opportunities to
practice with GTAs while receiving feedback from instructors and GTAs. This process provided students
the opportunity to be trained and practice the necessary skills to provide sexual assault care. The students
convened at the end of each day so the project director could answer any outstanding questions, address
practice issues, and share resources. The skills stations included: a) history-taking and documentation, b)
evidence collection, c) Foley catheter visualization of the hymen, d) Toluidine dye application and removal,
e) speculum insertion and removal, f) bimanual exam performance, g) digital photography, and h)
colposcopic visualization.
B. Multi-Study Project Design: Concurrent Triangulation Mixed Methods Design
In this project we used a multi-study, mixed methods design to examine whether this blended
approach would be an effective learning modality to train SAFEs. We used a concurrent triangulation mixed
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

28
methods design to address the research aims (Creswell, Plano Clark, Gutmann, & Hanson, 2003) (see
Figure 1).
FIGURE 1: Creswell et al.’s (2003) Concurrent Triangulation Mixed Methods Design
In this design, the quantitative and qualitative components of the study are considered equal and parallel.
This design is characterized by separate collection and analysis of quantitative and qualitative data. The
purpose of this design is to gain a complete understanding of the training by capitalizing on the strengths of
each method. In this study, the quantitative components allowed us to determine rates of training
completion and knowledge attainment, and the factors associated with those rates. However, we wanted to
capture the processes that occurred during the clinical training to understand how those processes linked
to students’ learning, which is better understood by qualitative methods. Furthermore, qualitative methods
allowed us to gather an in-depth understanding of students’ experiences and challenges after the training
when they returned to their communities to practice. As common in this design, the two methods were
integrated during the final interpretation phase of the study.
C. Quantitative Evaluation Aims
Quant Data
Collection and
Analysis
INTERPRETATION
OF
ENTIRE
ANALYSIS
Qual Data
Collection and
Analysis
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

29
Table 1 provides an overview of the evaluation aims. The first column displays the evaluation
framework while the second column identifies the evaluation questions within that framework. The second
column explains the sub-themes examined for each evaluation question.
Table 1: Overview of the Evaluation Aims
Evaluation Component
Evaluation Questions
Sub-Questions/Themes
Quantitative Aims
Question 1: What Factors Predict Training
Completion/Attrition?
What Predicts Training
Completion?
When did Attrition Occur?
Question 2: Is There a Significant Increase
in the Students’ Knowledge upon
Completion of the Training Modules?
Do Students’ Attain
Knowledge?
What Predicts Knowledge
Attainment?
Question 3: Among Those who Completed
the Training, did the Participants Retain
their Knowledge 3 Months Post-Training?
Do Students Retain
Knowledge of SAFE
Practice?
What Predicts Knowledge
Attainment Over Time?
Qualitative Aims
Question 4: How did the Clinical Training
Contribute to Students’ Knowledge?
Instructors’ Pedagogical
Approach
Developing Sexual Assault
Patient Care Skills
Developing Medical Forensic
Exam Skills
Instructors’ Challenges and
Recommendations
Question 5: What were the students’ post-
training experiences with applying their
knowledge?
Application of Skills with
Post-Training Patients
Students’ Remaining
Challenges with Patient
Care
Students’ Remaining
Challenges with the Medical
Forensic Exam
Students’ Experience and
Needs when Encountering
Delayed Practice
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
30
Student attrition is a major concern for online learning, with rates of completion around 55% for free
continuing education courses (Stone, Barber, & Potter, 2005). The first evaluation question sought to
understand whether attrition would be a similar disadvantage of the online SAFE course, and therefore an
ineffective way to address the SAFE shortage. Furthermore, our aim was to examine the predictors of
attrition because this could guide the selection process of applicants for future SAFE trainings. Finally, the
risk of attrition may change over the course of the training. That is, factors associated with early withdrawal
may be different than later withdrawal of the course (Park and Choi 2009). Thus, we focused on when
attrition occurred during the online training and identified variables that may be associated with the timing of
attrition.
Drawing from the literature, we examined three key areas that prior research has shown to
influence training completion. First, we wanted to understand if students’ characteristics and computer
experience influenced attrition. While most research has not found student demographics to be related to
attrition, it is still possible that student characteristics influence training completion (Park, 2007). Because
online training participation requires some familiarity with and ease of using computers, it is possible that
that anxiety with using computers could lead to participant attrition (Gormley, Costanzo, Lewis, Slone, &
Savage, 2012; Perry, Boman, Care, Edwards, & Park, 2008; Willging & Johnson, 2009). Thus, we
assessed the participants’ comfort and experience with computers as a potential factor of training attrition.
Furthermore, we inquired about access to Internet connectivity as it is essential for success in online
learning (Atack, 2003).
Second, students’ motivation to complete the training can be influenced by factors before they
even participate in the training (Gegenfurtner, Veermans, Festner, & Gruber, 2009). Students’ motivation is
particularly important for retention in online learning (Park, 2007; Welsh, Wanberg, Brown, & Simmering,
2003) and thus, we included items to assess intrinsic motivation when students began the training.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
31
Students also may not complete a course if it does not fit with their career interests (Perry, Boman, Care,
Edwards, & Park, 2008), so we inquired about the reasons students were interested in forensic nursing.
Finally, the extant literature has suggested that family and work responsibilities played a strong role
in training attrition (Angelino, Williams, & Natvig, 2007; Willging & Johnson, 2009). Therefore, we asked the
students about external barriers that could impact their participation in the training, including time
constraints, work load, supervisory support for training attendance, and family obligations.
The second evaluation question determined to what extent students learn the course content. It is
recommended that assessment of knowledge is ongoing throughout a training, especially because prior
studies have found that online learning can be more and less effective for particular topics (Jang, Hwang,
Park, Kim, & Kim, 2005; Johnston , 2007; Reeves, 2000; Wild, Griggs, & Downing, 2002). Thus, our first
aim was to assess whether students attained knowledge during each training module. To assess the
participant’s knowledge, the study used a one-group pre-test/post-test design (Shadish, Cook and
Campbell, 2002), which involved students completing a weekly online pre-test before completing each
training module and then a post-test upon completion of the module. For this study, it was not feasible to
compare our participants to those who already have been trained through other mechanisms. Many types
of SAFE trainings exist with some nurses being trained by national experts and some by local nurses.
Therefore, we would not be able to account for all of the variation in the training content and delivery
methods for a comparison group. Furthermore, we would not be able to determine if the trainings attended
by a comparison group contributed to the knowledge of the SAFEs or if their experience and post-training
supervision contributed to their skill set. Given the lack of feasibility of using a comparison group, we chose
to use the one-group pre-test/post-test design because it provided the most rigorous research design
without a comparison group In order to address potential validity issues throughout the project, students
were asked if they attended other trainings or read materials not provided by the IAFN training.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
32
Because prior research has suggested numerous factors that may influence knowledge attainment,
students also completed a post-training online survey to examine their effort; their perceptions of what
helped them learn; and recommendations for improving the training. This information, along with the data
collected in the pre-training survey (demographics, motivation) allowed us to exam the factors that impact
knowledge attainment. These factors were grouped into four broad categories: a) trainee characteristics
and control variables; b) motivation; c) external barriers; and d) characteristics related to the training. We
also wanted to understand if students’ characteristics and computer experience influenced knowledge
attainment. Research has suggested that novice online learners may experience challenges with learning
the technology, which could have a negative impact on learning the course content (Atack, Rankin, & Then,
2005). In addition, students’ who do not have reliable access to the Internet may have less success with
online courses (Hylton, 2006). We also wanted to assess factors outside of the training because students
reading non-assigned material or attending additional SAFE trainings might influence their knowledge
attainment.
Students’ motivation and external barriers also may impact knowledge attainment (Johnston, 2007;
Metcalf, Tanner, & Buchanan, 2010; Naidr et al, 2004). Thus, the variables used to examine training
attrition were included in the analysis for this study. Additionally, students’ effort in the training might
influence their success in the course (Metcalf, Tanner, & Buchanan, 2010; Naidr et al, 2004). Thus, we
examined if students’ knowledge attainment was impacted by efforts such as reading the course material,
completing the homework, and participating in the discussion boards. On a similar note, online learning
poses a unique challenge as it requires students to be self-directed and self-pace their learning (Zhang,
Zhou, Briggs, & Nunamaker, 2006). If students fall behind with the weekly modules, this could impact their
learning. So we examined whether the students completed the training on time and if this influenced their
success. Finally, students’ perceptions of the training might impact their success in the course (Metcalf,
Tanner, & Buchanan, 2010; Naidr et al, 2004). The post-training survey asked students about multiple
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

33
components of the training, including if they had adequate time to learn the material, whether the
discussion boards were helpful, and if the topics were covered adequately. In addition, we asked if they
were satisfied with the training and if it met their expectations. Together, this component of the evaluation
will help explain if the online modality is effective for students to gain the knowledge essential for competent
SAFE practice.
The third evaluation question determined to what extent students retain their knowledge after the
training. Prior research has noted that students may not retain all of the knowledge originally attained
during the training (Bell et al., 2008; Naidr et al., 2004). Therefore, students’ retention of their knowledge
was evaluated through a post-training exam approximately three months following the training. For the
three-month follow-up exam, participants answered 32 questions that were randomly selected from the pre-
tests/post-tests from the 12 modules. We used a subset of questions on the follow-up exam with the
anticipation that the reduced length would lead more students to complete the test in its entirety. All
students who completed the SAFE training (i.e. 12 online modules and two-day clinical workshop), and the
three-month post-training survey, which included the follow-up exam, were included in this analysis
(N=142). Because prior research has suggested that factors that influence knowledge attainment also may
impact knowledge retention, the analysis included the same variables that were in included in the analysis
for knowledge attainment: a) student characteristics and control variables; b) motivation; c) external
barriers; d) characteristics related to the training; e) computer experience and reliable access to the
Internet; g) student effort during the online training; and h) satisfaction with the training.
D. Qualitative Evaluation Aim
Because clinical simulation laboratory training is uncommon with SAFE training, the fourth
evaluation question sought to gain a more in-depth picture of the unique contributions of the clinical training
with preparing clinicians for SAFE practice. The traditional SAFE training model is taught over the course of
one week, primarily through lectures and minimal or no hands-on practice. Students in these trainings
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

34
typically practice SAFE-related skills (e.g., interacting with traumatized patients, medical forensic exam
techniques, speculum insertion) following the didactic training while providing services for actual patients.
Students usually begin practicing with wellness patients followed by sexual assault patients under the
supervision of a preceptor. If the new SAFEs work in geographically dispersed areas with low patient
volume, it may take a while before they can achieve competency and/or they may not have a preceptor
who specializes in SAFE practice. Alternatively, the clinical component of the IAFN SAFE blended training
allotted 16 hours of hands-on practice with gynecologic teaching associates (GTAs). Given this unique
feature of the training, we wanted to hear from students and the clinical instructors to gain insight about the
unique contributions of the clinical training. Therefore, we also utilized a qualitative framework to
understand the instructors’ pedagogical approach to teaching clinical skills. In addition, we conducted
qualitative interviews to examine the students’ perceptions of how the two-day clinical workshop contributed
to their patient care and medical forensic exam skills. Students who completed the entire training (i.e.,
online and clinical) were recruited for this component of the evaluation study. We interviewed students until
we reached saturation of the major themes (N=64).
We also wanted to evaluate how students applied their knowledge and skills with actual sexual
assault patients. The original plan involved the students asking their adult
3
patients to complete a survey
about their experience with the new SAFE, and to submit their medical forensic chart for a subject matter
expert review (with permission from the patient). We had planned to continue this component of the
evaluation for the first three months following the training because it would be difficult to attribute the
students’ performance to the training for a longer period of time. However, we found that most students had
not had an opportunity to examine adult patients within those three months, either because they only had
examined adolescent patients or have not had any patients. Of the students who did not have sexual
assault patients during that time frame, many worked in institutions that had a low volume of patients, and
3
The institutional review board required the eligibility criteria to be limited to adult patients.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

35
some students experienced delays due to community barriers such as problems with sexual assault
patients being referred to their institutions.
Still, we wanted to know how the students applied their gained knowledge and skills into their
practice with patients, along with any challenges that they encountered post-training. Therefore, we
decided to interview students later in the course of this evaluation project, allowing for more time for
students to have patients. The fifth evaluation question focused on gaining an in-depth perspective of how
the training prepared students for SAFE practice, and their recommendations for future trainings. In
addition, we asked students to discuss their perceptions of the best way to approach or interact with sexual
assault patients. For students who eventually had opportunity to work with sexual assault patients, we
asked them to discuss a case that went well and one that did not go well, and the ways in which the training
did and did not prepare them for those cases. Together, these qualitative aims provided a clearer in-depth
picture of the unique contributions of the clinical training with preparing clinicians for SAFE practice.
IV. Quantitative Evaluation Aims
Evaluation Question #1: What Factors Predict Training Completion/Attrition?
A. Methods
1. Research Design. A quantitative survey design was used to examine how many participants
completed the training and what factors predicted training completion. All participants who signed up for the
SAFE training (N=198) completed an online survey that assessed factors potentially related to retention or
attrition of participants. The survey was administrated prior to the start of the training and addressed a
range of topics including internet access, level of ease with computers, motivation to learn, and work
responsibilities. A total of 198 participants completed the pre-training survey and 79.3 percent (152 out of
the 198 students) continued on to complete the SAFE training. This section describes the results of these
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

36
pre-training surveys, identifies the factors that may have influenced training completion, and identifies
factors that may have influenced when attrition occurred.
Because there is a dearth of literature about student attrition for SAFE training, the development of
the quantitative survey was based off of the student attrition literature for healthcare in general. However,
we wanted to understand if there may be reasons unique to SAFE students or SAFE practice that might
contribute to student attrition. Therefore, in addition to this quantitative survey design, we also utilized a
qualitative framework to explore the clinical instructors’ perceptions of attrition specific to SAFE training.
This allowed us to augment the quantitative findings by gaining a deeper insight into the issues impacting
attrition. It is important to note that the instructors had not met the students who had dropped out of the
training before the clinical training occurred. Thus, we did not interview them about the reasons that the
students in this study dropped out of the training because the instructors only met those who completed the
online training. However, their experience in the field could lend insight into the reasons that clinicians who
participate in SAFE training in general do not transition into SAFE practice.
2. Sampling . The target audience for this training was registered nurses (RN), nurse practitioners
(NP), physician assistants (PA), and physicians, which is consistent with IAFN’s Sexual Assault Nurse
Examiner Educational Guidelines, the National Protocol for Sexual Assault Medical Forensic Examinations
of Adults/Adolescents, and the National Training Standards for Sexual Assault Medical Forensic
Examiners. Research has indicated that attrition rates can be high for continuing education courses
because professionals may “window shop” online trainings out of curiosity and may not be serious about
completing the course (Stone, Barber, & Potter, 2005). As such, the training candidates had to complete an
application to be considered for the training. The application requested background information to aid the
selection process including a) professional background; b) whether they have taken a SAFE training; c)
their intent to practice post-training and program/community background information; d) if they have reliable
access to the Internet; and e) if they can/will commit to the two-day clinical training and training evaluation.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
37
Finally, the application included an open-ended question about why the applicants wanted to participate in
the training. The application was accessible on the IAFN web site from July 5, 2011 to September 1, 2011.
The training was publicized on the IAFN website, and through announcements by IAFN and the
affiliations of the Subject Matter Experts involved in this project. The training project team actively promoted
the course through email announcements to the IAFN electronic database (over 10,000 individual
contacts), web announcements, and printed materials disseminated by the 32 IAFN Chapters, State Sexual
Assault Coalitions and the project’s Organizational Partners (e.g., Forensic Health Online). All electronic
advertisements included a link to the application web page. In addition, the Project Director held a listening
session webinar marketed to Statewide SANE Coordinators to address state specific training concerns in
relation to the web-based course.
There were 626 clinicians who applied for the training. Applicants were eligible for the training if
they a) had not completed a SANE/SAFE training; b) were not certified as SANEs/SAFEs through state
entities; c) intended to join or start a SANE/SAFE program in their community; d) were willing to participate
in the evaluation and two-day clinical training; e) practiced in the United States; and f) had reliable access
to the Internet. Finally, clinicians working in rural areas and tribal lands were considered a higher priority
because one of the aims of this project was to increase accessibility to high-quality didactic and clinical
training for this population.
A two-stage process was utilized to select the training participants. First, applicants were
eliminated automatically if they had completed a previous SAFE training (didactic or clinical) or were
certified as SANEs/SAFEs (N=87). Second, the evaluation coordinator read the applications in detail and
noted those who did not meet the eligibility criteria, which included those who a) had no intention or vague
plans for joining or starting a SAFE program (N= 68); b) unwilling to participate in the evaluation or two-day
clinical component of the training (N=12); and c) did not practice in the United States (N= 1). Together, this
yielded 168 applicants who did not meet the training criteria. To assess the reliability of the selection
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

38
procedures, 30% of the applications were randomly selected and reviewed by the PI to determine if the
same cases were excluded based on the criteria for eligibility (100% agreement). Next, the evaluation team
and the Project Director discussed the procedures for selecting the applicants from the list of those who
met the eligibility criteria. Given the goal of increasing access to training for those working in rural and tribal
lands, it was determined that applicants from major metropolitan urban areas
4
would be excluded because
they have more accessibility to SAFE training in their regions (N=150). This yielded a sample of N=308
applicants who were invited to participate in the training. Students were divided into three cohorts, with the
first cohort starting the training in January 2012 (referred to as Course 1), the second cohort starting in April
2012 (Course 2), and the third cohort starting in July 2012 (Course 3). It is important to note that there were
no differences in the content or the pedagogical approach among these courses, but rather the division of
students into three courses allowed for a manageable cohort size. The applicants were assigned to one of
the three courses based on geography and least likely weather interference of travel for the two-day clinical
training based on time of year.
Of the 308 participants who originally accepted the invitation, only 200 participants started the
training
5
. The applicants who originally accepted, but had subsequently opted out of the training did not
participate in the evaluation. Therefore, the reasons that these applicants declined to begin the training
were not collected. However, many applicants communicated with the Project Director and/or the
Evaluation Coordinator about their reasons for not starting the training. The most commonly cited reasons
included a) the availability of a SAFE course that began sooner; b) the inability to acquire a support letter
by their intuition, which was required by Wayne State University’s Institutional Review Board (IRB); and c)
4
Clinicians who worked in smaller urban areas were included in the training.
5
Participants were considered to start the training if they completed the pre-training survey. This “intent to treat” approach is
common in medical research that examines attrition and considers someone who took the initial steps to participate even if they
dropped out in the beginning of the training on because they at some point had an intention of being trained (Newel, 1992).
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

39
personal circumstances that interfered with their ability to participate in the training (e.g., pregnancy, death
in family). Of the 200 students in the training, two did not consent to the evaluation even though they
originally expressed willingness in their applications. This yielded a final sample for the evaluation as
N=198.
Descriptive information about the sample is provided in Table 2 (next page). Of the participants
who started the training, the mean age was 40.63 years, with a range of 21 years to 65 years old (1.5%
missing data). The participants’ education background varied with 36.5% having an associate’s degree,
42.1% having a Bachelor’s degree, and 21.3 % having a graduate degree (.005% missing data). The
average years of nursing experience was 12.49, with a range of 6 months to 41 years (4% missing data
6
).
Slightly more than half of the participants described their community as rural with the rest of the participants
identifying their community as suburban (22.8%) or urban (26.9%). The majority of students worked full-
time.
3. Procedures for Data Collection. Because attrition is common with online courses, we asked students to
complete a survey prior to beginning the training. One month prior to the training, the students received an
email to inform them that they would be receiving an email that would link them to the online training. Three
weeks prior to the commencement of the online training, all of the students were emailed a link to an online
survey housed by Zoomerang. All of the participants completed the survey prior to beginning the training.
The data were downloaded from Zoomerang and imported into IBM SPSS Statistics software 20 (IBM,
2011).
6
The wording of the survey item inquired about nursing experience rather than healthcare experience and thus, participants who
were not nurses (e.g., physicians) did not respond. In addition, a few participants provided a range (e.g., “30+ years,” “more than
20”) that could not be entered as a precise measure and thus, were coded as missing data. Typically, these ranges were higher
the mean years of experience and thus, it is estimated that the mean years of experience would be slightly higher if these
imprecise responses could have been included in the descriptive analyses.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

40
Table 2: Evaluation Question 1 Students’ Descriptive Statistics (N=198)
Variable
Percent/Mean
Course
One
39.9
Two
32.3
Three
27.8
Highest Level of Education
Associate Degree
36.5%
Bachelor’s Degree
42.1%
Graduate Degree
21.3%
Work Setting
Urban/Suburban
49.7%
Rural
50.3%
Current Employment
Unemployed
1.5%
Employed Part-time
11.1%
Employed Full-time
87.4%
Previous online class
72.7%
Reasons for Interest in Forensic Nursing
Professional
Personal experience
Community/organizational need
Personal learning/enrichment
Humanitarian
41.4%
11.1%
20.2%
6.1%
14.1%
Reasons for Participating in Training:
No cost to student
Most training is online
Two-day clinical training (in person)
IAFN-sponsored training
72.7%
80.3%
55.1%
57.6%
Plans Following Training
Apply for job with a SAFE program
Begin working in an established SAFE program
(offered position but not conducting exams)
Continue working in established SAFE program
(already conducting SAFE exams)
Start new SAFE program
39.4%
24.2%
11.6%
27.3%
Reliable Internet Access
82.8%
Age (in years)
40.6 (9.9)
Nursing Experience (in years)
12.5 (9.8)
Comfort with Computers
Intrinsic Motivation
Work/Personal Barriers
19.3 (4.3)
15.1 (8.6)
17.2 (2.0)
Note: Standard deviation in parentheses
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

41
4. Measures. Training completion was the dependent variable. This variable was measured as a
dichotomous variable (coded as 1 = completed the training or 0 = did not complete the training). The
second set of analyses focused on the timing when attrition occurred for those participants who dropped
out of the training. Participants could not continue to the next training module until they took the post-test.
Therefore, we attributed the timing of attrition to the time point where the participant missed the post-test.
For example, when a student completed post-test one and two but did not complete post-test three, attrition
was recorded as occurring at time three.
The independent variables included numerous factors that could lead to attrition and also impact
the timing of attrition. These factors were grouped into three broad categories: a) student characteristics
and control variables; b) motivation; and c) external barriers.
a) Student characteristics and control variables. Student characteristics included age (in years),
nursing experience (in years), highest level of education (associate degree, bachelor’s degree or graduate
degree), current employment status (1= employed, 0 = unemployed), community where they work/plan to
work (rural = 1, urban/suburban = 0), previous experience with online classes (1 = yes, 0 = no) and comfort
with computers. Comfort with computers was assessed with the following questions rated on a 5 point
Likert-type scale (adapted from O’Connell, Doverspike, Gilliken, & Meloun, 2001): 1) I usually get very
anxious about using a computer; 2) I’m not the type to do well with computers; 3) I have a lot of confidence
when it comes to working with computers; 4) I like working with computers; and 5) the online course will
take less time than a traditional course in a classroom. Responses on the Likert-type scales ranged from 1
(strongly agree) to 5 (strongly disagree), with two of the questions reverse scored (question 1 and 2).
Summing the scores for these five items yields a comfort with computers index with a possible range of 5-
25. Students were assigned to one of the three courses (Course 1,2, or 3) based on geography and least
likely weather interference of travel for the two-day clinical training based on time of year. There were no
differences in the content or the pedagogical approach among these courses, but rather the division of
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
42
students into three courses allowed for a manageable cohort size. Training course (Course 1, 2, or 3) was
included as a control variable in order to take account of any differences in training across the three
courses.
b) Motivation variables. Participants were asked an open-ended question about the reason they
were interested in forensic nursing. Responses to this question were coded into five broad categories. Five
dichotomous variables were created based on these categories: professional interest (e.g., being a SAFE is
a career goal), personal experience (e.g., student indicates that she/he is a survivor or knows a survivor),
community/organizational need (e.g., need a SAFE program or more SAFEs in existing program), personal
learning/enrichment (e.g., “I love to learn”), and humanitarian (e.g., “I believe in this cause”) (coded 1 = yes,
0 = no). We then asked which of the following factors impacted their interest in this specific training: no cost
to student, most of the training is online, the two-day in-person clinical training, and IAFN-sponsored
training. Participants were able to select all categories that were applicable (responses for the four
variables were coded as 1 = yes, 0 = no). How participants planned to use the training in their future work
was assessed with a question that asked participants what best describes their plans following the training
(response categories: apply to work in an already established SAFE program; have already been offered
position in established SAFE program and will begin conducting exams after the training; currently
conducting exams at an already established SAFE program; and starting a new SAFE program). Four
dichotomous variables were created based on these response categories (coded 1 = yes, 0 = no).
Intrinsic motivation for participating in the training was measured using a summative scale based
on the following five items (adapted from Noe & Wilk, 1993): 1) I will try to learn as much as I can from this
course; 2) I am interested in learning the training material; 3) I am willing to invest the effort to improve
skills and competencies related to becoming a forensic nurse; 4) I will get more from this training than most
people; and 5) I am motivated to learn the skills needed to be a forensic nurse examiner. Participants rated
each of these items on a Likert-type scale that ranged from 1 (strongly agree) to 5 (strongly disagree).
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

43
Intrinsic motivation was measured by a summation of the ratings for five items implying a possible range of
5-25.
c) External barriers. Participants were asked four questions about external barriers that could
impact their participation in the training. These items addressed time constraints, work load, supervisory
support for training attendance, and family obligations. Individual items were scored from 1 (strongly agree)
to 5 (strongly disagree). Summing the scores for the individual items yields an external barrier index with a
possible range of 4-20. Because most of the training was online, we also asked participants if they have
good Internet connectivity. Responses were dichotomized to indicate if the participant had good Internet
connectivity (good internet connectivity coded as 1 and all others coded 0).
5. Quantitative Analytic Plan. Prior to conducting the substantive quantitative data analysis, raw
data were examined statistically and graphically to verify data quality, potential outliers, and distributional
problems that required transformations or alternative methods. Listwise deletion was used to handle
missing data for this analysis given the low levels of missing data for each participant (five participants
missing one or more items) (Tabachnick & Fidell, 2013). This resulted in an analytic sample of 193
participants. Data were aggregated across the three training courses to maximize sample size.
a). What Predicts Training Completion? Binary logistic regression was used to determine what
factors predict training completion. Following Hosmer and Lemeshow’s (2000) approach to variable
selection for logistic regression, we first conducted bivariate analyses and examined the pair-wise
association between independent variables and the dependent variable. Pearson’s chi-squared test
statistics were calculated for categorical independent variables (e.g. employed vs. unemployed) while
bivariate logistic regression models were calculated for continuous variables with many integer values (e.g.
age). A significance level of p < 0.15 was used as the initial cut-off point to select independent variables
that were further analyzed through hierarchical logistic regression. This liberal screening criterion required a
critical review during the model building, but provided greater assurance that all of the important variables
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
44
were retained for further analysis (Hosmer & Lemeshow, 2000). If an independent variable met the
screening criterion in bivariate analyses for the dependent variable, it was considered for inclusion in the
hierarchical logistic regression models.
Variable entry for the logistic regression analysis was approached from a hierarchical perspective,
with predictors organized into conceptually meaningful blocks that were entered sequentially. This
approach allowed us to examine the contribution of variables in later blocks, controlling for the effects of
variables in earlier blocks (Hosmer & Lemeshow, 2000). Specifically, this analysis allowed us to test the
effects of: 1) student characteristics; 2) motivation, controlling for the effects of student characteristics; 3)
external barriers controlling for the effects of student characteristics and motivation; 4) the unique
contribution of variables in each conceptual block relative to the other blocks; and 5) the overall
predictability of training completion. The logistic regression analyses were conducted with IBM SPSS
Statistics software 20 (IBM, 2011). Correlational analyses were conducted with the variables to investigate
potential problems with multicollinearity (Menard 2002) (See Table 3 for summary of the correlations
among all independent variables in the final multivariate model).
Table 3: Inter-correlations among Multivariate Predictor Variables for Training Completion Analyses
(N=193)
Variable
1
2
3
4
5
6
7
8
1. Course 1
1
2. Course 2
0.56
1
3. Rural community
0.27
-0.25
1
4. Nursing experience (in years)
0.05
-0.03
0.04
1
5. Intrinsic motivation
0.05
0.02
0.12
0.13
1
6. Motivation: Two-day clinical training
0.09
-0.09
0.18
0.11
0.14
1
7. Motivation: Most of training is online
0.12
-0.09
0.04
0.06
0.09
0.37
1
8. Reliable internet access
0.14
-0.06
0.04
0.05
0.30
0.04
0.13
1
b). When did Attrition Occur? Survival analysis examines and models the time it takes for events to
occur. The Cox proportional-hazards (Cox PH) regression model is currently one of the most widely used
methods of survival analysis (Kleinbaum, 2005). For this study, we used the Cox PH model to analyze
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
45
when attrition occurred, and identify variables that may be associated with the timing of attrition. Survival
models consist of two basic parts. The first part is the underlying hazard function that describes how the
hazard (or risk) changes over time at baseline levels of covariates. In this problem we examine how the risk
of attrition changes as the participants progressed through the training modules. The second part of the
survival model consists of the effect parameters that describe how the hazard (risk) varies in response to
explanatory covariates. The Cox PH model gives an expression for the hazard at time t for an individual
with a given specification of a set of explanatory variables. This model has the following specification:
h(t,X) = h
0
(t) exp( ),
X = (X
1
,…,X
i
…X
P
), (explanatory variables)
The Cox model formula says that the hazard at time t is the product of two quantities. The first of these,
h
0
(t), is the baseline hazard function. The second quantity is the exponential expression, e to the linear sum
of βi Xi , where the sum is over the P explanatory X variables, where the βi ‘s are fit by maximum likelihood
estimation. The Cox proportional hazards model was fit using the “Survival” package, within R statistical
software (R Development Core Team, 2012; Therneau, 2013).
B. Results
1. What Predicts Training Completion?
a. Bivariate Associations. Tables 4 and 5 (pages 47 and 48, respectively) provide information on
the bivariate relationships between training completion and both the student characteristics/control
variables, motivation and external barriers. Three of the student characteristics/control variables met the p
< 0.15 significance criteria and were retained for possible inclusion in the logistic regression model: training
course (p = 0.104), working in a rural community (p = 0.031) and years of experience in nursing (p = 0.101).
Although age did not meet the initial significance criteria, it was retained as a control variable for the
multivariate logistic regression due to its relationship with years of experience in nursing. None of the other
student characteristic variables met the criteria for significance at the 0.15 level (employment, highest level
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
46
of education, previous online class experience, and comfort with computers). Thus, these variables were
not retained for the multivariate analysis.
When focusing on the motivation measures, two variables were below the 0.15 cut-off point. One of
these variables focused on a reason the participant enrolled in the training: the two-day, in-person clinical
training (p = 0.021). Intrinsic motivation, measured on the 5-item scale, was also retained for the
hierarchical logistic regression (p = 0.070). The other motivation measures did not meet the 0.15 criteria
and were excluded from the hierarchical logistic regression model: motivation in forensic nursing
(professional, personally experience with sexual assault, community/organizational need, personal
learning/enrichment, and humanitarian), reasons for participating in the training (no cost to student, most of
training is online and IAFN sponsored), and plans following the training (apply for a job with a SAFE
program, begin working in an established program, continue working in established program, or start a new
SAFE program).
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

47
Table 4: Bivariate Cross-tabulations and Chi-squared Tests Assessing the Relationship between
Training Completion and Study Variables (N=193)
Variable
Df
p
Student Characteristics & Control Variables
Course
3.95
2
0.139
Employed
0.30
1
0.587
Rural community
Highest level of education
Previous online class
5.37
0.02
0.65
1
1
1
0.020
0.992
0.422
Motivation
Reasons for Interest in Forensic Nursing
Professional
Personal
Community/organizational need
Personal learning/enrichment
Humanitarian
0.39
0.82
1.94
1.32
0.75
1
1
1
1
1
0.533
0.775
0.164
0.252
0.385
Reasons for Participating in Training:
No cost to student
Most training is online
Two-day clinical training
(in person)
IAFN-sponsored training
1.23
1.66
5.37
0.86
1
1
1
1
0.267
0.197
0.021
0.355
Plans Following Training
Apply for job with a SAFE program
Begin working in an established SAFE program
(offered position but not conducting exams)
Continue working in established SAFE program
(already conducting SAFE exams)
Start new SAFE program
0.44
0.15
0.93
0.10
1
1
1
1
0.507
0.701
0.335
0.747
External Barriers
Reliable Internet Access
1.47
1
0.225
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

48
Table 5: Bivariate Logistic Regression Analysis Predicting Training Completion (N=193)
Variable
B
SE of B
p
OR (95% CI)
Student Characteristics & Control Variables
Age
Nursing Experience (in years)
Comfort with Computers
Motivation
Intrinsic Motivation
External Barriers
Work/Personal Barriers
0.02
0.03
0.01
0.14
0.06
0.02
0.02
0.04
0.08
0.74
0.282
0.101
0.846
0.070
0.426
1.02 (0.98-1.06)
1.03 (0.99-1.08)
1.01 (0.93-1.09)
1.15 (0.99-1.35)
1.06 (0.92-1.23)
b. Hierarchical Logistic Regression Results. Results of the binary logistic regression models are
presented in Table 6 (page 49). Training attrition was regressed on the following variables: training course,
rural community, nursing experience (in years), motivated by two-day clinical training and intrinsic
motivation. The variables were entered in three hierarchal blocks. The first block contained the control
variables and student characteristics (training course, rural community, nursing experience). The second
block contained the motivation variables (motivated by two-day clinical training and intrinsic motivation). A
third block was not included in the hierarchical regression because none of the external barrier variables
met the initial criteria for inclusion in the multivariate model (p < .15).
Model 1, which included the control variables and student characteristics was statistically
significant (10.42, df = 4, p =.03). One variable in model 1 were significant at the 0.05 alpha level.
Community type was significantly associated with training completion. Participants who worked in a rural
community were significantly more likely to complete the training. Model 2, the full model, was statistically
significant, indicating that the predictors as a set reliably distinguished between those who completed the
training and those who did not. (χ² = 14.41, df = 6 p = .025).The Hosmer and Lemeshow test for goodness
of fit was not significant and also indicated adequate fit for the full model (p= 0.55). In model 2, two
independent variables were significantly associated with training completion at the 0.05 alpha level.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

49
Consistent with the results from model 1, community type was a statistically significant predictor of training
completion. For students who worked in rural communities, the odds of training completion were 88%
higher (OR[0.59] = 1.81; p = .031). Participants who were interested in the training because of the two-day
in person clinical workshops were significantly more likely to complete the training. Interest in the two-day
clinical workshop was associated with a 77% increase in the odds of training completion (OR[0.57] = 1.77;
p = .039).
Table 6: Hierarchical Logistic Regression Predicting Training Completion (N=193)
Variable
B
SE of B
P
OR (95% CI)
Model 1
Course 1*
Course 2*
Rural community
Nursing experience (in years)
Model 2
Course 1*
Course 2*
Rural community
Nursing experience (in years)
Motivation: Two-day clinical training
Intrinsic motivation
0.67
0.28
0.72
0.03
0.65
0.28
0.59
0.03
0.57
0.02
.46
.43
.38
.02
.46
.44
.39
.02
.28
.02
0.142
0.514
0.048
0.136
0.163
0.522
0.031
0.235
0.039
0.257
1.96 (0.80-4.80)
1.33 (0.057-3.11)
2.07 (1.01-3.39)
1.03 (0.99-1.07)
1.91 (0.77-4.73)
1.33 (0.56-3.15)
1.81 (1.11-4.51)
1.03 (0.98-1.07)
1.77 (1.04-3.71)
0.86 (0.94-1.07)
*For the training course variable, Course 3 was the comparison group.
2. When did Attrition Occur?
a) Cox Proportional Hazard Model. Results of the Cox Proportional Hazard Model are presented in
Table 7 (next page). At the 0.05 alpha level, two independent variables were found to be statistically
significant indicators of increased attrition risk. Interest in the training because of the in-person two-day
clinical workshop was associated with a lower instantaneous attrition hazard rate compared to those who
were not motivated by the two-day clinical workshop. For any given time during the training, a participant
who was motivated by the two-day clinical workshop had an instantaneous attrition hazard ratio of -0.99
(Exp(B)=0.35). The probability of early attrition for those who were not motivated by this factor was 2.86
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

50
times greater than for those who were motivated by the two-day clinical workshop. Similarly, an interest in
the training because it was online was significantly associated with a lower instantaneous attrition hazard
ratio compared to those who were not motivated by the online nature of the training. For any given time
during the training, participants who were interested in the online nature of the training had an
instantaneous attrition hazard ratio of -0.74 (Exp(B)=0.37). Thus, those participants who were not
interested in the training because of its online nature had a probability of attrition that was 2.7 times greater
than those who were motivated by the training’s online nature. One additional variable, community type,
was a marginally significant predictor of the instantaneous rate of attrition. At the 0.10 alpha level, working
in a rural community was associated with a lower instantaneous rate of attrition compared to the rate for
those who worked in urban or suburban communities. For any given time point in the training period, the
probability of early attrition for those that worked in an urban or suburban community was 2.94 times
greater than those who worked in a rural community (HR[-0.58] = 0.56, p=.09).
Table 7: Cox Proportional Hazards Model Predicting time to Attrition (N=193)
Variable
B
Exp (B)
SE of B
p
Rural community
Motivation: Most of training is online
Motivation: Two-day clinical training
Nursing Experience (in years)
Reliable internet access
-0.58
-0.74
-0.99
0.58
-0.03
0.34
0.37
0.35
0.53
0.02
0.34
0.02
0.02
0.04
0.53
0.093
0.045
0.005
0.274
0.106
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

51
Figure 2: Kaplan Meier Curve Illustrating Training Completion over Time
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

52
Evaluation 2: Is There a Significant Increase in the Students’ Knowledge upon Completion of the
Training Modules?
A. Methods
1. Research Design. A quantitative framework was used to examine if the training enhanced the
students’ knowledge to competently practice as SAFEs. This study used a one-group pre-test/post-test
design (Shadish, Cook and Campbell, 2002) to assess the participant’s knowledge prior to each training
module and afterward. The one-group pre-test/post-test design provided the most rigorous research design
without a comparison group. For this study, it was not feasible to compare our participants to those who
already have been trained through other mechanisms. Many types of SAFE trainings exist with some
nurses being trained by national experts and some by local nurses. Therefore, we would not be able to
account for all of the variation in the training content and delivery methods for a comparison group.
Furthermore, we would not be able to determine if the trainings attended by a comparison group
contributed to the knowledge of the SAFEs or if their experience and post-training supervision contributed
to their skill set. Given the lack of feasibility of using a comparison group, we chose to use the one-group
pre-test/post-test design. In order to address potential validity issues throughout the project, students were
asked if they attended other trainings or read materials not provided by the IAFN training. These items were
included as control variables in the analyses.
2. Sampling. All students who completed the SAFE training (i.e. the online modules and two-day
clinical workshop) and had no missing data on the independent variables were included in the analysis for
the second evaluation question (N=151). Demographics of these students were provided in Table 8 (next
page). The mean age of those who completed the training as 41.18 years, with a range of 24 years to 65
years old. At the start of the training, most participants (86.1%) were employed full-time. The participants’
education background varied with 35.3% having an associate’s degree, 43.3% having a Bachelor’s degree,
and 21.3% having a graduate degree. The average years of nursing experience was 13.22, with a range of
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
53
6 months to 41 years. Fifty-five percent of the students described their community as rural with the rest of
the participants identifying their community as suburban or urban (45%).
Table 8: Question 2 Students’ Descriptive Statistics (N=151)
Variable
Percent/Mean
Course
One
44.4
Two
30.5
Three
25.2
Highest Level of Education
Associate Degree
35.3%
Bachelor’s Degree
43.3%
Graduate Degree
21.3%
Work Setting
Urban/Suburban
45%
Rural
55%
Current Employment
Unemployed
1.3%
Employed Part-time
12.6%
Employed Full-time
86.1%
Previous online class
72.2%
Reasons for Interest in Forensic Nursing
Professional
Personal
Community/organizational need
Personal learning/enrichment
Humanitarian
42.7%
11.3%
21.9%
4.6%
15.9%
Reasons for Participating in Training:
No cost to student
Most training is online
Two-day clinical training (in person)
IAFN-sponsored training
74.2%
83.4%
60.9%
59.6%
Plans Following Training
Apply for job with a SAFE program
Begin working in an established SAFE program
(offered position but not conducting exams)
Continue working in established SAFE program
(already conducting SAFE exams)
Start new SAFE program
37.7%
25.2%
12.6%
27.2%
Reliable Internet Access
82.8%
Read additional materials
23.2%
Attended additional trainings
9.3%
Performed pelvic exams prior to training
29.1%
Performed pelvic exams following training
Test completed on time
58.3%
68.9%
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

54
Age (in years)
41.18 (10.18)
Nursing Experience (in years)
13.22 (10.33)
Comfort with Computers
Intrinsic Motivation
Work/Personal Barriers
Effort
19.4 (4.3)
16.1 (8.1)
12.2 (2.2)
6.5 (2.4)
Perception of training
10.1 (5.0)
Note: Standard deviation in parentheses
3. Procedures for Data Collection. The training entailed two main components: twelve online
training modules and a two-day in-person clinical workshop. Before the training began, participants
completed a pre-test for the first module (Introduction to SAFE). After receiving instruction on how to
navigate through the online learning management system, the participants completed the first module. This
module presented information on the history and role of the SAFE. After the participants completed the
introduction module, an online post-test was given to all participants to assess knowledge gain on the
introductory content.
A similar pattern of completing a pre-test, participating in the online training module and then
completing a post-test existed for the other eleven training modules. Students were asked to complete a
weekly online pre-test before completing each training modules. Upon completion of each of these
modules, the pre-test exams were re-administered to participants online as a post-test. The pre-tests/post-
tests for each module varied in length, including from 6 to 40 questions per module (M = 12 questions, SD
= 9.65). Participants were required to complete the modules in a sequential order. Once participants began
a training module, they were not able to continue on to the next module until the module and its associated
post-test were completed. The purpose of the pre-tests and post-tests was to examine if the training
enhanced the participants’ knowledge upon completing each module.
Most of the questions had one correct answer and was scored as correct or incorrect. Some of the
questions had multiple correct answers in which students were instructed to check all of the correct
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

55
answers. For this type of question, each answer was considered a test item. In the example below, there
are five possible answers that could be checked as correct and each was treated as a test item. The
correct answers are A, D, and E. If a student checked A, it was scored as correct. If the student did not
check A, then it was scored as incorrect. If B was checked, it was scored as incorrect while it was scored
as correct if it was not checked. This method of scoring allowed for a precise measurement of the students’
knowledge.
Tanner Staging is (choose all that apply):
A. A tool used to assess secondary sex characteristic development
B. Divided into 4 phases for males and 5 for females
C. Used to estimate chronological age
D. Divided into 5 phases
E. Based upon developmental changes in Caucasians
The pre-tests and post-tests were taken by students in the learning management system. Data was
retrieved from the system by downloading each student’s scores for the pre-test and post-test of each
module, and entering them into SPSS. This process was necessary because the learning management
system did not treat a multiple answer question (check all that apply) as multiple items, which would have
yielded a less precise measure.
Three months after the training, participants completed an online post-training survey to examine
the effort of the students (e.g., if they read the assigned readings); students’ perceptions of what helped
them learn; and recommendations for improving the training.
4. Measures. We assessed whether there was increased knowledge based on the percentage of
correct answers on each pre-test and post-test
7
(See Appendix C). The training project team worked in
collaboration with the evaluators to develop the pre-tests/post-tests for each module (12 pre-tests/post-
tests in total). Students’ level of knowledge was assessed with recognition and recall of concepts, and
7
Students were required to take the post-tests to obtain continuing education unit (CEUs). Similar to most continuing education
courses, students were allowed to take the post-test more than once. The student’s score for the evaluation utilized the score
from the first time that the student took the post-test for each module.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
56
knowledge of how and when to apply knowledge to different case scenarios. Knowledge was rated through
multiple-choice, true-false, and multiple answer (check all that apply) questions.
A paired-samples t-test was conducted to compare the total number of correct answers on all of
the pre-tests and the total number of correct answers on all of the post-tests. As part of the t-test, change
scores were calculated by subtracting the number of correct pre-test questions from the number of correct
post-test questions. The independent variables included numerous factors that could impact knowledge
and skills attainment. These factors were grouped into four broad categories: a) student characteristics and
control variables; b) motivation; c) external barriers and d) characteristics related to the training. Factors a-c
were taken from the pre-training online survey (see page 179) except the control variables. In order to
assess for outside influences, this evaluation aim included additional variables that were collected during
the follow-up survey. In particular, we included measures of whether participants read any additional non-
assigned training materials (1 = yes, 0 = no) or attended additional forensic examiner trainings (1 = yes, 0 =
no) during the course of the study. In addition, we assessed participants’ experience conducting pelvic
exams both prior to (1 = yes, 0 = no) and after the training (1 = yes, 0 = no). The follow-up survey also asked
participants about their efforts during the training, which was measured using a summative scale based on
four items from the online post-training survey. These questions, rated on a scale from 1 (strongly agree) to
5 (strongly disagree), asked if the participant: 1) read all of the materials assigned for the course; 2) did the
recommended homework, 3) read the postings in the weekly discussion board, and 4) put a good deal of
effort into learning the material. Summing the ratings on the four questions resulted in a scale with a
possible range of 4-20.
Characteristics related to the training characteristics is the fourth broad category included in the
analysis for the second evaluation question. Participants’ perceptions of the training were measured on a
scale created by using six questions from the online post-training survey. These questions assessed
whether students felt 1) they had enough time to learn the material, 2) the topics were covered adequately,
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

57
3) the weekly discussion board helped them understand the material better, 4) the online training met their
expectations, 5) they learned a considerable amount during the training, and 6) whether they were satisfied
with the amount they learned in the course. These individual items were rated from 1 (strongly agree) to 5
(strongly disagree). Summing the scores for the individual items yields an index with a possible range of 6-
30. A final variable was used to assess whether or not participants completed the training on time (coded 1
= yes, 0 = no).
5. Analytic Plan
a). Do Students’ Knowledge of SAFE Practice Increase from the Weekly Pre-test to Post-test?. A
series of paired sample t-tests were used to assess change in participants’ level of knowledge for each of
the 12 online didactic modules. This approach takes into account the repeated measures data structure.
The pre-tests could affect the degree of success on the post-tests and the paired samples t-test allows the
pre-test scores to be parceled out of variability in the post-test scores. Because the training included 12
modules, this analysis required 12 t-tests. In order to compensate for the multiple comparisons, a
Bonferroni correction was used to maintain the Type I error rate. This correction allowed us to maintain a
family-wise error rate of p<.05 and required a stronger level of evidence to be observed in order for an
individual comparison to be deemed “significant” (Tabachnick & Fidell, 2013).
b). What Predicts Knowledge Attainment? Simple linear regression and multiple linear regression
were used to examine which factors were associated with increased knowledge attainment. The dependent
variable was an overall change score that was calculated by subtracting the total number of correct pre-test
questions from the total number of correct post-test questions. Similar to the approach used to assess
knowledge gain, this analysis takes account of how pre-tests could affect the degree of success on post-
tests. This approach also builds on our assessment of whether there was a gain in knowledge and helps us
assess factors that were associated with a gain in knowledge.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

58
Before proceeding with the multivariate analysis, all variables were examined for both univariate
and multivariate outliers and indications of normality. No problematic outliers were detected. There were a
few instances where minor normality issues were detected (e.g. skewed or kurtotic variables) and data
transformations were evaluated (e.g. square root and log transformations). Although the transformations
resulted in some improvements to normality, the additional complexity of interpretation led us to retain the
original untransformed variables. Correlational analysis indicated that there were a number of significant
correlations among the independent and dependent variables; however, the magnitude of these
correlations was modest (See Table 10 on page 61 for summary of correlations among independent
variables in the final multivariate model).
B. Results
1. Does Students’ Knowledge of SAFE Practice Increase from the Weekly Pre-test to Post-test?
Paired samples t-tests were conducted to evaluate whether the participants knowledge increased from the
pre-tests to the post-tests for the 12 training modules. Descriptive statistics and results of the repeated
measure t-tests are presented in Table 9 on page 60 (see pre-test and post-test columns). Average pre-test
scores for each module ranged from 43.43% (module 2) to 81.01% (module 1). Average post-test scores
for each module ranged from 74.55% (module 9) to 95.36% (module 1).The results of the repeated
measures t-tests with Bonferroni corrections indicated that mean post-test scores were significantly greater
than the mean pre-test scores for each of the 12 training modules (p<.0001 for every module).
Although there was a significant gain in knowledge in each module, the gains did vary to some
extent (see Figure 3 and Paired Differences Column in Table 9). On over 40% of the modules, the students
exhibited at least a 25% knowledge gain. The greatest gains in knowledge were seen in module 2 (Mean
gain = 35.85; SD= 21.83), module 6 (Mean gain = 29.80; SD=23.85) and the introduction module (M gain
=28.13; SD=22.37). Module 2 addressed forensic science, ethics and self-care, while the introduction
addressed the history and role of the SAFE. Module 6 covered content on using photography in medical
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

59
forensic exams. Although the knowledge gains on modules 3 (team approach), 10 (operational issues) and
1 (dynamics of sexual assault) were also statistically significant; the average increases on these modules
were smaller. The average knowledge gain was 9.33% for module 3 (SD=14.14) and 14.11% for module 10
(SD=14.06). These modules included content on a patient-centered team approach (module 3) and
program and operational issues (module 10). While gain scores for module 1 (dynamics of sexual assault)
also were lower than many of the other modules (M=14.35%; SD=14.53), it is noteworthy that the high
initial pre-test scores (M=81.01%; SD=12.18) on this module left less room for improvement.
2. What Predicts Knowledge Attainment? Simple linear regression and multiple linear regression were
used to identify factors associated with knowledge attainment upon completion of the SAFE training. For
this analysis we first examined the descriptive characteristics of the knowledge change scores and
conducted pair-wise comparisons using simple linear regression. We then conducted a multiple linear
regression model using a backward elimination approach. This approach was used because of the large
number of independent variables and the exploratory nature of the study. We examined four broad
categories of independent variables: 1) student characteristics and control variables; 2) motivation
variables; 3) external barriers and 4) training characteristics.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

60
Table 9: Descriptive Statistics and t-test Results for Knowledge Attainment on the Online Modules
(N=151)
Pre-test
Post-test
Paired Difference
Variable
M
SD
M
SD
M
SD
95% CI
t
Introduction
50.66
18.44
79.58
15.05
28.91
21.83
25.41-32.43
16.28
Module 1
81.01
12.18
95.36
9.84
14.35
14.53
12.01-16.69
12.13
Module 2
43.43
18.87
79.28
20.58
35.85
22.67
32.21-39.50
19.44
Module 3
66.89
11.18
76.21
12.45
9.33
14.14
7.05-11.60
8.11
Module 4
56.06
12.94
81.54
13.69
25.48
15.19
23.03-27.92
22.61
Module 5
54.79
9.55
78.72
13.36
23.93
15.37
21.46-26.40
19.13
Module 6
49.83
17.26
79.64
18.75
29.80
23.75
25.98-33.62
15.97
Module 7
51.26
14.71
76.89
15.80
25.63
19.78
22.45-28.81
15.46
Module 8
74.98
10.67
89.89
10.83
14.92
14.83
12.53-17.30
15.92
Module 9
58.69
8.26
74.55
12.95
15.86
12.06
13.92-17.80
16.17
Module 10
69.25
11.72
83.36
13.31
14.11
14.06
11.85-16.37
12.34
Module 11
70.29
8.99
91.04
10.76
20.75
12.49
18.73-22.77
20.35
Degrees of Freedom =150 for each test; Knowledge gains were significant for all modules at p < .0001.
Figure 3.Mean Increase in Knowledge from Pre-test to Post-test (N=151)
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

61
Table 10: Inter-correlations among Knowledge Attainment Multivariate Predictor Variables (N=151)
Variable
1
2
3
4
5
6
1. Comfort with computers
1
2. Intrinsic motivation
0.45
1
3. Reasons for Interest in SAFE:
Personal Experience
0.11
0.23
1
4. Reasons for Participating in Training:
No cost to student
0.10
-0.07
-0.76
1
5. Reliable Internet Access
0.37
0.56
0.23
-0.01
1
6. Work/Personal Barriers
0.52
0.35
0.16
0.01
0.41
1
Results of the simple linear regression are presented in Table 11 (next page). Three variables were
statistically significant at the 0.05 alpha level. Participants who planned to apply for a job with a SANE
program and those with interest in SAFE practice as a result of personal experiences had significantly
lower knowledge attainment (p= 0.024 and p= 0.006, respectively). In contrast, participants who planned to
start a SANE program had significantly higher knowledge attainment (p=0.012). One additional variable,
whether participants were motivated by the training having no cost, was marginally significant (p=0.073).
Results of the multiple linear regression model are presented in Table 12 (page 63). Only one
variable significant at the bivariate level remained statistically significant in the multiple regression model.
Intrinsic motivation (p=0.001), an interest in SAFE practice because of personal experiences (p=.003),
reliable Internet access (p=.030), and work/personal barriers (p=.038) all significantly contributed to the
multivariate model, F(6,128 =4.101, p<.001, R² = 0.16). These variables accounted for approximately 16%
of the variance in the knowledge gain. The final model indicates that higher levels of motivation and a
reliable Internet connection were significantly associated with an increase in knowledge. Participants who
reported interest in SAFE practice due to a personal experience and those with increased work/personal
barriers experienced significantly less gains in knowledge. Two additional variables, comfort with
computers and whether participants were motivated by the training having no cost, were marginally
significant predictors of knowledge attainment (p= 0.066 and p=0.054, respectively).
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

62
Table 11: Bivariate Regression Analysis Predicting Knowledge Attainment (N=151)
Variable
B
SE
β
t
p
Student Characteristics & Control Variables
Age
0.54
0.06
0.07
0.91
0.367
Nursing experience (in years)
0.06
0.06
0.08
1.04
0.302
Highest level of education*
Graduate Degree
0.18
1.46
0.10
0.12
0.904
Associate Degree
-1.94
1.25
-0.12
-1.55
0.124
Currently employed
1.99
4.43
0.04
0.45
0.650
Rural community
-0.63
1.21
-0.04
-0.52
0.603
Previous online class
-2.09
1.33
-0.13
-1.58
0.117
Comfort with computers
-0.07
0.15
-0.04
-0.45
0.657
Course**
One
1.87
1.20
0.12
1.55
0.123
Two
-0.65
1.30
-0.04
-0.50
0.615
Read additional materials
0.22
1.45
0.12
1.52
0.879
Attended additional trainings
-0.58
2.06
-0.02
-0.28
0.780
Performed pelvic exams prior to training
-1.65
1.31
-1.04
-1.26
0.211
Performed pelvic exams following training
-0.92
1.27
-0.06
-0.72
0.470
Motivation
Intrinsic motivation
0.32
0.28
0.09
1.12
0.265
Effort during training
-0.35
0.26
-0.11
-1.35
0.180
Reasons for Interest in SAFE practice:
Professional
Personal experience
Community/organizational need
Learning/enrichment
Humanitarian
1.10
-5.35
1.09
0.48
-0.27
1.21
1.91
1.47
2.76
1.66
0.07
-0.22
0.06
-0.01
-0.01
0.91
-2.81
0.74
-0.17
-0.16
0.366
0.006
0.460
0.862
0.870
Reasons for Participating in Training:
No cost to student
Most training is online
Two-day clinical training
IAFN-sponsored training
2.48
-2.34
1.45
-0.92
1.37
1.57
1.22
1.22
0.14
-0.12
0.09
-0.06
1.80
-1.49
1.18
-0.75
0.073
0.138
0.238
0.450
Plans Following Training:
Apply for job with a SAFE program
Begin working in an established SAFE program
(offered position but not conducting exams)
Continue working in established SAFE program
(already conducting SAFE exams)
Start new SAFE program
-2.77
-0.10
0.26
3.37
1.22
1.34
1.82
1.33
-0.18
-0.01
0.01
0.20
-2.27
-0.07
0.14
2.54
0.024
0.950
0.888
0.012
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

63
Table 11 (continued)
Variable
B
SE
β
t
P
External Barriers
Reliable Internet Access
1.38
1.58
0.07
0.88
0.382
Work/Personal Barriers
-0.16
0.26
-0.05
-0.62
0.538
Training Characteristics
Perception of the Training
-.080
0.13
-0.05
-0.59
0.554
Test completed on Time
-0.97
1.31
-0.06
-0.74
0.461
*For Education, Bachelor’s degree was the comparison group.
***For the training course variable, Course 3 was the comparison group.
Table 12: Multiple Linear Regression Predicting Knowledge Attainment
Variable
B
SE
Β
T
p
95% CI
Comfort with computers
-0.34
0.18
-0.19
-1.86
0.066
-0.70 to 0.022
Intrinsic Motivation
1.33
0.40
0.34
3.31
0.001
0.54 to 2.12
Reasons for Interest in SAFE:
Personal Experience
-6.01
1.96
-0.26
-3.07
0.003
-9.88 to -2.14
Reasons for Participating in Training:
No cost to student
2.85
1.46
0.16
1.95
0.054
-.05 to 5.74
Reliable Internet Access
4.83
2.20
0.22
2.20
0.030
0.48 to 9.18
Work/Personal Barriers
-0.75
0.36
-0.22
-2.10
0.038
-1.46 to -0.04
Evaluation Question 3: Among Those who Completed the Training, did the Participants Retain their
Knowledge Three Months Post-training?
A. Methods
1. Research Design. Research has suggested that students may not retain all of the knowledge
originally attained during the training (Bell et al., 2008; Goldstein & Ford, 2002; Naidr et al., 2004).
Therefore, a quantitative framework was used to examine whether participants were able to retain the
knowledge learned during the IAFN SAFE training. Our analysis of knowledge attainment indicated that, by
the end of the training, participants had significantly improved their knowledge of how to collect sexual
assault forensic evidence and provide appropriate healthcare for sexual assault patients. The current study
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

64
builds on that analysis and examines whether this improvement was maintained at approximately three
months after the training. To examine knowledge retention rates, we used a one-group longitudinal design
to examine changes in the participants’ knowledge from the pre-test to the post-test and to the three month
follow-up interview. A strength of this research design is that it provides the opportunity to observe changes
in knowledge over time by accommodating multiple time points. For examining predictors of knowledge
retention, linear regression models are used to examine factors associated with improved knowledge
retention at the three month follow-up exam.
2. Sampling. Descriptive characteristics comparing the participants who completed the SAFE
training (N=151) and those that completed the training as well as the three month follow-up exam (N=138)
can be found in Table 13 on the next page (91% response rate). Although 8.6% of participants who
completed the SAFE training did not complete the follow-up exam, the two samples were similar with
regard to age, years of nursing experience, educational attainment, employment level (i.e. full-time, part-
time or unemployed) and work setting (i.e. rural vs. urban/suburban). On average, participants who
completed the three month follow-up exam were 41 years old (SD=10.22) and had 13 years of experience
in nursing (SD=10.40). At the start of the training, most of the participants (85.9%) were employed full-time.
Just over half of the participants (54.2%) reported working in rural settings.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

65
Table 13: Question 3 Descriptive Statistics for Independent and Dependent Variables
Participants who
Completed the Training
(N=151)
Participants who
Completed the 3 Month
Follow-up (N=138)
Variable
%/Mean
%/Mean
Course
One
44.4%
44.4%
Two
30.5%
31.0%
Three
25.2%
24.6%
Highest Level of Education
Associate Degree
35.3%
37.6%
Bachelor’s Degree
43.3%
41.8%
Graduate Degree
21.3%
20.6%
Work Setting
Urban/Suburban
45%
45.8%
Rural
55%
54.2%
Current Employment
Unemployed
1.3%
1.4%
Employed Part-time
12.6%
12.7%
Employed Full-time
86.1%
85.9%
Previous online class
72.2%
73.8%
Reasons for Interest in Forensic Nursing
Professional
Personal
Community/organizational need
Personal learning/enrichment
Humanitarian
42.7%
11.3%
21.9%
4.6%
15.9%
41.8%
10.6%
22.7%
5.0%
17.0%
Reasons for Participating in Training:
No cost to student
Most training is online
Two-day clinical training (in person)
IAFN-sponsored training
74.2%
83.4%
60.9%
59.6%
75.4%
82.4%
57.7%
59.9%
Plans Following Training
Apply for job with a SAFE program
Begin working in an established SAFE program
(offered position but not conducting exams)
Continue working in established SAFE program
(already conducting SAFE exams)
Start new SAFE program
37.7%
25.2%
12.6%
27.2%
34.5%
26.1%
14.1%
28.2%
Reliable Internet Access
82.8%
83.7%
Read additional materials
23.2%
23.9%
Attended additional trainings
9.3%
10.6%
Performed pelvic exams prior to training
29.1%
31.2%
Performed pelvic exams following training
Test completed on time
58.3%
68.9%
63.4%
69.7%
Age (in years)
41.18 (10.18)
40.98 (10.22)
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

66
Nursing Experience (in years)
13.22 (10.33)
13.10 (10.40)
Comfort with Computers
Intrinsic Motivation
Work/Personal Barriers
Effort
19.4 (4.3)
16.1 (8.1)
12.2 (2.2)
6.5 (2.4)
19.4 (4.5)
15.7 (8.3)
12.1 (2.3)
6.5 (2.4)
Note: Standard deviation in parentheses
3. Procedures for Data Collection. As described earlier, participants completed a pre-test and post-
test on each of the 12 didactic training modules (12 pre-tests and 12 post-tests in total) while they
participated in the online training. The purpose of these tests was to examine if the training enhanced the
participants’ knowledge upon completing each module. Three months after the training, the students were
emailed a link to an online survey housed by Zoomerang. The survey had four primary purposes: a) to
assess student satisfaction with the online and clinical components of the training; b) to capture the effort
they devoted to the training (e.g., reading assigned readings); c) their recommendations for the training;
and d) a comprehensive follow-up exam to assess their knowledge retention. The data were downloaded
from Zoomerang and imported into IBM SPSS Statistics software 20 (IBM, 2011).
4. Measures. The dependent variable to asses retention rates was the percentage of correct
answers on the knowledge and skill assessment tests that were administered at pre-test, post-test, and the
three-month survey. On each of these tests, knowledge was rated through multiple-choice and true-false
questions. The follow-up exam was designed to examine if the participants retained their knowledge after
the training was over. For the three-month follow-up test, participants answered 32 questions that were
randomly selected from the pre-tests/post-tests from the 12 modules. We used a subset of questions on the
follow-up test with the anticipation that the reduced length would lead more students to complete the test in
its entirety. All students who completed the SAFE training (i.e. 12 online modules and two-day clinical
workshop), and the three-month post-training survey, which included the follow-up exam, were included in
this analysis (N=138).The dependent variable to examine the predictors of retention was change scores
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

67
that were calculated by subtracting the number of correct pre-test questions from the number of correct
follow-up test questions.
The independent variables utilized to examine knowledge attainment were included in the analysis
to examine predictors of knowledge retention (see page 41 & 56). To recap, these factors were grouped
into four broad categories: a) students characteristics and control variables; b) motivation; c) external
barriers and d) training characteristics. These measures were taken primarily from the pre-training online
survey and the post-training survey that was administered following completion of the training.
5. Analytical Plan
a) Do Students Retain Knowledge of SAFE practice? A repeated-measures analysis of variance
(ANOVA) was used to assess change in participants’ level of knowledge over three time points: the pre-
tests administered before the modules, the post-tests administered after completion of the training modules
and the three month follow-up exam. The repeated-measures ANOVA is one of the most commonly used
statistical approaches for longitudinal data (Tabachnick & Fidell, 2013). One advantage to using the
repeated-measures ANOVA is that we are able to partition out and eliminate variability due to individual
differences. Repeated-measures ANOVA differs from standard ANOVA in that standard ANOVA is based
upon an assumption of independence, and therefore it does not model the correlation structure between
the repeated-measures. In repeated measures ANOVA, repeated-measures of the outcome (i.e. scores on
the tests) are regressed on a time variable (i.e. the data collection time point) yielding an average intercept
(level of the outcome at time = 0; e.g., pre-test) and slope-over-time (average change in the outcome
across one unit of time). As the repeated-measures ANOVA excludes all cases with missing data, only
participants who completed the training and follow-up survey could be included in this analysis (N=138).
b) What Predicts Knowledge Attainment Over Time? Simple linear regression and multiple linear
regression were used to examine which factors were associated with increased knowledge attainment at
the three-month follow-up point. The dependent variable was an overall change score that was calculated
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

68
by subtracting the total number of correct pre-test questions from the total number of correct three-month
follow-up questions, the implication being that an observed value of zero on this scale signifies no retention.
This analysis incorporates models similar to those used in assess knowledge attainment, which helped us
assess factors that were associated with retaining knowledge over time.
Before proceeding with the multivariate analysis, all variables were examined for both univariate
and multivariate outliers and indications of normality. No problematic outliers were detected. There were a
few instances where minor normality issues were detected (e.g. skewed or kurtotic variables) and data
transformations were evaluated (e.g. square root and log transformations). Although the transformations
resulted in some improvements to normality, the additional complexity of interpretation led us to retain the
original untransformed variables. Correlational analysis indicated that there were a number of significant
correlations among the independent and dependent variables; however, the magnitude of these
correlations was generally modest (See Table 14 on page 70 for a summary of the correlations among all
independent variables in the final multivariate model).
B. Results
1. Do Students Retain Knowledge of SAFE Practice? A repeated measures ANOVA was
conducted to evaluate the participants’ knowledge of forensic nursing at each of the three time points (i.e.,
pre-test, post-test and the three month follow-up exam). Mauchly’s test of sphericity indicated that the
assumption of sphericity had been met (χ
2
(2) = 5.4, p = 0.060)
8
. Results of the repeated measures ANOVA
indicate that test scores differed significantly between time points, (F(2, 282) = 443.26, p < 0.001). Post-hoc
comparisons using the Bonferroni test were used to examine which specific means differed. Consistent with
our earlier analysis, the post-hoc tests indicate there was a significant increase in test scores from pre-test
(M=58.65 SD=5.47) to post-test (M=80.77 SD=9.22) (See Figure 4). Post-hoc comparisons further indicate
8
Mauchly’s Test of sphericity tests for the equivalence of the hypothesized and the observed variance/covariance patterns.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
69
there was a significant increase when comparing scores from the pre-test (M=58.65 SD=5.47) to the three
month follow-up test (M=67.24 SD=9.21). However there was also a significant difference between post-
test scores (M=77.92 SD=8.84) and three-month follow-up scores (M=68.83 SD=9.17). Taken together,
these results suggest that while some knowledge was lost over time, a lasting gain in knowledge among
the participants resulted from this training.
Figure 4. Mean Increase in Knowledge from Pre-test to Post-test to three Month Follow-up (N=138)
0
10
20
30
40
50
60
70
80
90
Pre-Test Post-Test 3 Month Follow
up
Mean Test Score
2. What Predicts Knowledge Attainment Over Time? Simple linear regression and multiple linear
regression were used to identify factors associated with knowledge retention three months following the
completion of the SAFE training. For this analysis we first examined the descriptive characteristics of the
change scores and conducted pair-wise comparisons using simple linear regression. We then conducted
multiple linear regression following a backward elimination approach. This approach was used because of
the large number of independent variables and the exploratory nature of the study. We examined four
broad categories of independent variables: 1) student characteristics and control variables; 2) motivation
variables; 3) external barriers and 4) training characteristics. Post-test scores were included in this analysis
to control for the loss of knowledge from posttest to the three-month follow-up test.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

70
Change scores from pre-test to the three month follow up test ranged from -18.2 to 31.1 (Mean =
8.6; standard deviation = 8.8). Most participants (83.3%) demonstrated a gain in knowledge during this time
period (See Table 15). At three months following the training, only small proportions of participants
demonstrated decreases in knowledge (10.9%) or knowledge levels within one point above or below their
pre-test score (5.8%). Results of the simple linear regression are presented in Table 16 (next page). Nine
variables were statistically significant at the 0.05 alpha level. Additional years of age and experience in
nursing were associated with greater knowledge gains at three months following the training (p= 0.031 and
p= 0.046, respectively). Higher post-test scores were also associated with significantly greater gains in
knowledge at three months following the training. Participants who were motivated to participate in the
training because it was free (p= 0.046), primarily online (p= 0.038), and included a two-day in-person
clinical workshop (p= 0.005) had significantly greater gains in knowledge at three months following the
training. Participants who planned to start a SANE program and had participated in the first course of the
training also had significantly higher knowledge gains (p=0.009 and p=0.038, respectively). In contrast,
participants with previous experience taking an online class had significantly lower gains in knowledge at
three months following the training (p=0.005).
Table 14: Inter-correlations among Knowledge Retention Multivariate Predictor Variables (N=138)
Variable
1
2
3
4
1. Nursing experience (in years)
1
2. Previous online class
-0.08
1
3. Reasons for Interest in Forensic Nursing:
Personal Experience
0.11
-0.06
1
4. Reasons for Participating in Training:
Two-day clinical training (in person)
0.08
0.10
0.06
1
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

71
Table 15: Change in Knowledge Scores from Pre-test to Three Months Post-Training (N=138)
%/Mean(Standard Deviation)
Decrease in knowledge score
10.9%
Knowledge score remained the same*
5.8%
Increase in Knowledge score
83.3%
Overall mean change in knowledge
8.6 (8.8)
*A knowledge score was considered the same if the 3 month follow-up score was within one point above or
below the pretest score.
Table 16: Bivariate Regression Analysis Predicting Knowledge Retention at Three Months Post-
Training (N=138)
Variable
B
SE
β
t
p
Student Characteristics & Control Variables
Age
0.16
0.07
0.18
2.17
0.031
Nursing experience (in years)
0.14
0.07
0.17
2.01
0.046
Highest level of education*
Graduate Degree
1.11
1.84
0.05
0.61
0.546
Associate Degree
0.40
1.54
0.01
0.03
0.979
Currently employed
1.00
6.28
0.01
0.16
0.874
Rural community
1.60
1.48
0.09
1.08
0.280
Previous online class
-4.71
1.64
-0.24
-2.87
0.005
Comfort with computers
-0.13
0.17
-0.06
-0.74
0.459
Course**
One
3.08
1.47
0.18
2.10
0.038
Two
-3.11
1.58
-0.16
-1.97
0.051
Read additional materials
1.18
1.73
0.06
0.68
0.497
Attended additional trainings
0.34
2.41
0.01
0.14
0.887
Performed pelvic exams prior to training
-1.10
1.61
-0.06
-0.68
0.497
Performed pelvic exams following training
0.23
1.54
0.01
0.15
0.881
Post-test score
0.16
0.08
0.10
2.06
0.041
Motivation
Intrinsic motivation
-0.01
0.09
-0.01
-0.14
0.893
Effort during training
0.14
0.31
0.01
0.05
0.964
Reasons for Interest in Forensic Nursing:
Professional
Personal
Community/organizational need
Learning/enrichment
Humanitarian
-0.15
-5.35
1.09
0.48
-0.27
1.51
1.91
1.47
2.76
1.66
-0.01
-0.22
0.06
-0.01
-0.01
-0.10
-2.81
0.74
-0.17
-0.16
0.922
0.072
0.969
0.977
0.480
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

72
Table 16 continued:
Variable
B
SE
β
t
p
Reasons for Participating in Training:
No cost to student
Most training is online
Two-day clinical training
(in person)
IAFN-sponsored training
2.48
-2.34
1.45
-0.92
1.37
1.57
1.22
1.22
0.14
-0.12
0.09
-0.06
1.80
-1.49
1.18
-0.75
0.046
0.038
0.005
0.968
Plans Following Training:
Apply for job with a SANE program
Begin working in an established SANE program
(offered position but not conducting exams)
Continue working in established SANE program
(already conducting SAFE exams)
Start new SANE program
-2.23
-2.72
-1.70
4.27
1.55
1.67
2.12
1.61
-0.12
-0.14
-0.07
0.22
-1.44
-1.63
-0.80
2.66
0.152
0.106
0.425
0.009
External Barriers
Reliable Internet Access
-1.59
2.00
-0.67
-0.79
0.430
Work/Personal Barriers
2.32
1.60
0.12
1.45
0.538
Training Characteristics
Perception of the Training
-0.02
0.16
-0.01
-0.10
0.924
Test completed on Time
2.32
1.60
0.12
1.45
0.149
*For education, Bachelor’s degree was the comparison group.
***For the training course variable, Course 3 was the comparison group.
Results of the multiple linear regression are presented in Table 17 (next page). Previous
experience with an online class (p=0.015) and an interest in forensic nursing because of the clinical in-
person training (p=.006) all significantly contributed to the multivariate model, F(4,134 =5.16, p<.001, R² =
0.16). These variables accounted for approximately 16% of the variance in the knowledge gains at three
months following the training. The final model indicates that participants who were motivated by the two-
day in-person clinical workshop retained significantly more knowledge from the training. Participants who
reported previous experience with online classes experienced significantly less retention of knowledge.
One additional variable, a personal interest in forensic nursing, was a marginally significant predictors of
knowledge retention (p= 0.077).
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

73
Table 17: Multiple Linear Regression Predicting Knowledge Retention
Variable
B
SE
β
t
p
95% CI
Post-test Score
0.09
0.08
0.10
1.18
0.242
-0.06 to -0.25
Nursing experience (in years)
0.11
0.69
0.12
1.52
0.130
-0.03 to 0.24
Previous online class
-4.04
1.64
-0.20
-2.47
0.015
-7.28 to -0.81
Reasons for Interest in Forensic Nursing:
Personal Experience
-4.14
2.32
-0.15
-1.78
0.077
-8.72 to -0.45
Reasons for Participating in Training:
Two-day clinical training (in person)
3.99
1.43
0.22
2.79
0.006
1.16 to 6.82
V. Qualitative Evaluation Aims
A. Methods
1. Research Design. We wanted to gain a more in-depth picture of the unique contributions of the
clinical training with preparing clinicians for SAFE practice. Therefore, this study utilized a qualitative
framework to examine the students’ perceptions of what they learned from the clinical component in the
SAFE training, and how the clinical training contributed to those learning outcomes. Because clinical
instructors can have a substantial influence on students’ learning (Reeves, 2000), the PI interviewed the
instructors to understand their instructional approach to teaching complex skills, and the rationale behind
their approach. In addition, these qualitative interviews explored the clinical instructors’ challenges and
recommendations for the clinical training. We were interested in understanding their perceptions because
teaching students complex skills can be challenging. Further, the clinical component of the training is an
innovative approach to SAFE training so these insights could help inform future trainings.
We also interviewed students to examine how students applied their gained knowledge and skills
into their practice with their post-training patients, along with any challenges that they encountered post-
training. Furthermore, we examined the challenges experienced by a subset of students following the
training. As noted in the current study section, many students had not performed an exam within the three
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

74
months following the training. This section focuses on students who are still waiting to examine their first
patient, including a few students who attended Course 1, which ended nearly a year when these interviews
occurred. As such, we examined how students feel about not practicing, and if they believed it affects their
abilities to practice as SAFEs.
2. Sampling.
a) Instructors. Each two-day clinical training was taught by at least four clinical instructors, a
photography instructor, and the project director for a total of N=11 instructors for the entire project. The PI
contacted the instructors to request their participation in this study, and ten agreed. One instructor did not
respond to multiple requests to arrange an interview (91% participation). Nine of the instructors were
female and one was male. No other demographic data was collected.
b) Students. Students who completed the entire training (i.e., online and clinical) were the target
sample for this study. The evaluation coordinator contacted all of the students who completed the training
to schedule an interview if they agreed to participate in the study. Participant recruitment and interviewing
continued until the sample size allowed for saturation, whereby the same themes were repeated, with no
new themes emerging among participants (N=64) (Starks & Trinidad, 2007). This is a reasonable sample
size for a qualitative study examining a phenomenon in-depth (Creswell, 2013). Descriptive information
about the sample is provided in Table 18 (next page). Their average age of the interview participants was
40.67 years old, with a range of 26 to 65 years old. The students’ educational level varied: 32.8% had an
associate’s degree, 48.4% had a bachelor’s degree, and 18.8% had a master’s degree. The students had
12.33 years of nursing experience on average with a range of six months to 41 years. More than half of the
participants were from a rural area (53.1%). There were no statistically significant differences in student
characteristics and knowledge attainment rates between students who did and did not participate in the
qualitative interviews.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

75
Table 18: Descriptive Statistics of Students Participation in the Qualitative Interviews
Students who Completed
the Training (N=151)
Students who Participated
in the Qualitative Interview
(N=64)
Variable
%/Mean
%/Mean
Course
One
44.4%
42.2%
Two
30.5%
31.3%
Three
25.2%
26.6%
Highest Level of Education
Associate Degree
35.3%
32.8%
Bachelor’s Degree
43.3%
48.4%
Graduate Degree
21.3%
18.4%
Work Setting
Urban/Suburban
45%
46.9%
Rural
55%
53.1%
Current Employment
Unemployed
1.3%
1.6%
Employed Part-time
12.6%
12.5%
Employed Full-time
86.1%
85.9%
Age (in years)
41.18 (10.18)
40.67 (10.32)
Nursing Experience (in years)
13.22 (10.33)
12.33 10.96)
Note: Standard deviation in parentheses
We also explore the challenges of a subset of the qualitative interviews: those students who have
not performed their first exam with a sexual assault patient (N=28 or 44% of all students interviewed). The
reasons that the students have not examined their first patient varied: a) personal reasons such a personal
crisis or moved (N=4); b) institutional barriers such as low patient volume or management issues (N=14); c)
community barriers such as problems with the referral process (N=6); and four students who experienced
institutional and community barriers. Despite these barriers, all but two students expressed their
commitment to practicing as a SAFE. The average age of the subset of students who did not have their first
patient was 42.68 years old, with a range of 26 to 65 years old. Their educational levels differed, with
35.7% having an associate’s degree, 35.7% with a bachelor’s degree, 25% with some graduate school, and
3.6% with a master’s degree. The students had 14.79 years of nursing experience on average with a range
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

76
of six months to 38 years. Many students were from rural areas (64.3%), while 17.9% were from suburban
communities, and 17.9% were from urban areas.
3. Procedures for Data Collection. The instructor interviews were conducted after the completion of
the training. This allowed the instructors to reflect on their approach over the course of the project. The
instructors were interviewed by the PI by phone. Team meetings were held to discuss emerging themes to
address in subsequent interviews. The length of the interviews ranged from 30 to 90 minutes, with an
average of 48 minutes. The student interviews were conducted by phone by the evaluation coordinator.
The length of the interviews ranged from 25 minutes to 68 minutes, with an average of 46 minutes.
Ongoing weekly team meetings were held to discuss emerging themes to address in subsequent
interviews. The interviews were tape recorded with permission and transcribed. Transcripts were checked
for errors.
4. Measures.
a) Instructors. The semi-structured qualitative interviews with the instructors explored five main
topics: 1) the instructors’ perceptions of student training attrition; 2) the instructors’ approach to teaching
SAFE skills to students; 3) areas in which students struggled during the clinical training and the instructors’
strategies to mitigate those struggles; 4) factors that influenced students to succeed during the clinical
training; and 5) lessons learned and overall recommendations for future trainings (see Appendix C for
interview protocol).
b) Students. The semi-structured qualitative interviews with the students explored five main areas
(see Appendix C for interview protocol). To ground the interview, students were asked whether they have
had opportunity to examine sexual assault patients. If the students did not have opportunity to practice as
SAFEs, follow-up questions were asked to understand any barriers or obstacles to practicing. Second, the
interview inquired about the students’ perceptions of the clinical training, including the impact of the training
on their knowledge, skills, and feelings of preparedness. In addition, students were asked to provide
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

77
feedback about the instructors and the content covered during the clinical training. Third, the post-training
survey indicated that students would have liked more information about documentation and thus, the
qualitative interviews inquired about what they would have liked covered more in-depth about
documentation, and what was helpful about the information covered on documentation. For students who
have examined sexual assault patients, they were asked to describe the feedback that they have received
from a supervisor or experienced SAFE about the quality of their documentation. Fourth, the post-training
surveys indicated that the participants would have liked more information about interacting with sexual
assault patients. Therefore, the interviews asked the students what was helpful about the training with
learning about how to interact with patients and what they would have liked covered more in-depth. Finally,
we wanted to understand how the training has shaped the students’ perceptions about how to approach
sexual assault patients. Thus, we asked the participants what they believed was the best way to approach
and interact with sexual assault patients. For students who have worked with sexual assault patients, we
asked them to discuss an experience with a patient that went well and how the training did or did not help
them with those patients. Then we had the students describe an experience with a patient that did not go
as well and how the training did or did not help with those patients. Furthermore, they were asked to
describe the feedback that they have received from a supervisor or experienced SAFE about the quality of
their documentation. If the students did not have opportunity to practice as SAFEs, follow-up questions
were asked to understand any barriers or obstacles to practicing.
5. Analytic Plan. Data analysis proceeded in a two-phase process. First, consistent with Strauss
and Corbin’s (1990) method of “open coding,” and Miles and Huberman’s (2013) concept of “data
reduction,” two analysts independently read the transcripts and identified a preliminary list of themes
mentioned by participants. The analysts compared themes, discussed and clarified the meaning of the
thematic codes, and revised the coding framework until there was consensus. Once the coding framework
was finalized, the transcripts were independently coded by the two analysts. Because of the larger sample
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

78
size for the student interviews, a coding matrix was created and updated each time a set of ten transcripts
were coded. The coding matrix included a summary of major findings of the codes along with
corresponding memos. The memos consisted of insights about the data and emerging concepts, arising
questions, and areas that need further exploration. Writing these memos consistently throughout the coding
process helped the analysis move from a descriptive to an explanatory understanding of the data.
In the second phase of data analysis, we used Erickson’s (1986) analytic induction method, which
is an iterative procedure for developing and testing empirical assertions in qualitative research (see also
Patton, 2002). A key advantage of this method is that it elevates the analyses from the descriptive level (the
first phase) to an explanatory focus. In this approach, an analyst reviews all of the data multiple times with
the goal of arriving at a set of assertions that are substantiated based on a thorough understanding of all of
the data. The next task is to establish whether each assertion is warranted by going back to the data and
assembling confirming and disconfirming evidence. The analyst must look for five types of evidentiary
inadequacy: 1) inadequate amount of evidence; 2) inadequate variety in the kinds of evidence; 3) faulty
interpretative status of evidence (i.e., doubts about the accuracy of the data due to social desirability bias);
4) inadequate disconfirming evidence (i.e., no data were collected that could disconfirm a key assertion);
and 5) inadequate discrepant case analysis (i.e., no cases exist that are contrary to a key assertion)
(Erickson, 1986, p. 140). Assertions are revised or eliminated based on their evidentiary adequacy until a
set of well-warranted assertions remain.
B. Results
Evaluation Question 4: How did the Clinical Training Contribute to Students’ Knowledge?
The results will begin with a summary of the clinical instructors’ pedagogical approach, and then
we will discuss how the clinical training contributed to the students’ patient and medical forensic exam
skills. The training aimed to help students understand the importance of the patient-centered care approach
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

79
including how to provide compassionate care and empower sexual assault patients. During the qualitative
interviews, we asked students to describe the best approach when working with sexual assault patients to
help us assess if the students still understood the core concepts of patient-centered care. Thus, one area
will examine student perceptions of patient-centered care, and how the training helped students understand
this concept. In addition to providing patient-centered care, another priority of the training was to help
students attain the examination and evidence collection skills needed to perform a competent sexual
assault medical forensic examination. Thus, the next area of the results will focus on how the training
assisted students’ development of these skills. Although the students indicated that the clinical training was
instrumental in their skill development, the instructors did encounter a few challenges. Thus, the results will
conclude with a description of these challenges.
1. Instructors’ Pedagogical Approach. Although there were slight variations at times, all of the
instructors employed five overarching approaches to teaching clinical skills: They created a non-threatening
learning environment, assessed students’ learning needs, demonstrated/modeled clinical skills, allowed
hands-on practice, and fostered critical thinking.
a) Non-Threatening Learning Environment. The instructors aimed to create a non-threatening
learning environment because many of the students expressed feeling anxious about practicing medical
forensic exams on GTAs. Thus, the instructors said that creating a non-threatening environment during the
clinical training was the first step in facilitating learning and allaying student fears. The instructors tried to
foster a sense of student camaraderie so that anxious students could connect to others with the same fears
and uncertainties. Students who were feeling particularly unsure of themselves would be made aware that
there were others in their cohort who felt the same way. The project director also divided students into
smaller groups for the hands-on practice segment of the training (i.e., skill stations), directing them to assist
their classmates by offering advice or support if needed. The instructors also were accessible and amiable,
allowing students to ask questions without judging or criticizing them. As a result of these efforts, several
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
80
students said they were able to feel more comfortable with practicing the exam, and noted that the
instructors’ friendliness and patience helped them feel less anxious.
b) Assessing learning needs. Clinical training instructors faced the challenge of having to teach
students with a diverse array of backgrounds and experiences. Some students were from rural areas,
which may have different practice concerns than those in urban areas. Other students had more practice
experience or differing levels of education. To address these differences, students were assigned to a
smaller group with others with similar backgrounds when possible. The instructors began their skills
stations by asking students about their backgrounds and practice areas as a mechanism to gauge their
learning needs. This helped them provide information that may be salient to particular students’ needs.
c) Demonstrated/modeled skills. According to both instructors and students, an effective way of
learning the forensic exam was by first observing it being done by a trained professional. Students were
able to see how an ideal exam should look before attempting to practice it on their own. Instructors
demonstrated how to approach a sexual assault patient, speculum insertion, the pelvic exam, evidence
collection techniques, and patient interviewing. Most students said they found this aspect of the clinical
training helpful because it gave them direction on how to perform their own exams. Instructors thought that
demonstrating exam techniques helped students feel calmer about practicing on their own. For example,
one instructor explained that by demonstrating her particular process students would mimic her technique,
but would eventually find their own styles once they became more comfortable performing exams.
c) Practice with gynecological teaching associates (GTAs). The instructors noticed that students
felt more relaxed and confident after they were able to practice the forensic exam on their own. Students
could practice on a live person while the instructors guided them or corrected their technique. Instructors
also pointed out anatomical landmarks and allowed students to repeat an aspect of the exam if needed.
The instructors noted that the utilization of GTAs provided students with the opportunity to hone their skills
before using them on actual sexual assault patients.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

81
d) Fostering critical thinking. An important component to SAFE practice is the ability to critically
assess each situation, tailoring approaches to meet the needs of a variety of patients. Though observing
and practicing provide students with the tools to learn technical aspects of the exam, instructors also had to
teach students how to make sound clinical decisions that were in the best interests of their patients. The
primary way instructors achieved this was by providing rationale for each aspect of the exam and then
having students provide rationale when they began practicing on their own. By asking students why they
were performing a particular exam technique or using certain phrasing during the interview, instructors
were prompting them to think in-depth before taking action.
2. Developing Sexual Assault Patient Care Skills
a). Patient-centered Care. Because a patient-centered approach is important to the patients’
wellbeing as well as their participation in prosecution, we wanted to understand whether the students
understood the concept of patient-centered care. The interviews revealed that the training’s focus on this
patient-centered philosophy was an important realization for students. Prior to the training, several students
said they had perceived the SAFE role only as an evidence collector and identified forensic collection as
their primary purpose with sexual assault patients. Some of the students had performed forensic exams as
part of their position in emergency departments prior to receiving training. These students described their
approach prior to the training as cold and methodical with a strong focus on following the instructions on the
rape kit box. The purpose, these students explained, was to aid law enforcement with forensic evidence
collection.
By emphasizing that the well-being of the patient is paramount to SAFE practice, the training
helped students learn to see their SAFE role as an important part of the sexual assault patient’s healing. In
the qualitative interviews we asked students to describe different aspects of the SAFE role. An
overwhelming number of participants described some version of patient-centered care. For example, some
students talked about approaching sexual assault patients with compassion and a non-judgmental attitude.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
82
Many students described SAFEs as helping give control back to patients by providing them with choices
and following their needs. In the following quote, a student discusses the concept of patient-centered care:
I thought that my most important job was to collect the evidence so that I could serve the
patient better. After the course, I realize that my first job was to take care of the patient and
then worry about collecting the evidence, I mean the evidence collection is important, but
serving that patient’s emotional needs and taking care of them as a patient is the most
important thing I could ever do for them. I realize when you do your documentation, your
documentation actually comes out better cause you are focusing on the patient, you’re
actually listening to what they say… [Student 20053].
As these quotes demonstrate, the training raised most students’ awareness of the emotional needs of their
patients. They no longer view their role as evidence collectors. Overall, the training was successful in
clarifying the majority of students’ perceptions of SAFE practice and underscoring the importance of patient
care taking precedence over medical forensic evidence.
The qualitative interviews also suggested that most students had a strong understanding of the two
important components of patient-centered care: compassionate care and patient empowerment, which will
be discussed next.
b). Compassionate Care. A large number of students had several years of experience caring for
patients in general, and many identified that treating patients compassionately is an important aspect of
medical care. Both components of the training helped all of the students understand that the emotional
vulnerability of sexual assault patients makes compassionate care all the more important to the patient-
provider relationship. In the following quote, a student describes how compassionate care can improve
sexual assault patients’ outcomes and facilitate their healing process.
I think it’s important to be empathic, but they are in the state like we all are... our behavior
and actions are state-dependent, and our responses to things and they are in a state that
you have to be... and it can go anyway. It’s as if... I don’t know... I don’t think firecracker is
the right word. But they can go... they are like a raw nerve. And can respond any way. And
the experience can be made so much worse or so much more healing based on how you
experience them and they experience you [Student 10050].
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
83
As noted above, students perceive compassionate care, and their role as a SAFE, as particularly important
to the long-term health and well-being of sexual assault patients.
While the entire training helped all of the students understand the importance of compassionate
care, the majority of students indicated that the clinical training played a stronger role in helping them learn
the process of fostering patient comfort and how to avoid re-traumatizing patients. During the clinical
training, students practiced taking mock patient histories from the GTAs while receiving guidance and
feedback from clinical instructors. Most of the students noted that the practice and feedback helped them
refine their language with sexual assault patients.
But when I went to the clinical, you know, when I actually did a role play interview with one
of the models, you know, when they start, the instructor would stop you and say, “Maybe
put it this way,” “You have to be more sensitive,” or whatever. So pointed out things that I
was doing wrong that I didn’t think I was doing wrong, was helpful [Student 30037].
In addition, the mock scenarios helped most students understand how certain words or phrases, like “your
story” or “alleged,” may be perceived as accusatory, offensive, or judgmental. As a result, most students
noted that they learned how to communicate with patients in a sensitive manner without causing further
emotional distress.
I think just at the clinical day it was interesting to see when the instructors would go
through, you know, this is what I would say. They would not just say this is what I would
say, they would say listen. I am going to talk to you like you're the patient. So just listening
to how they would say okay. My hand is here. Saying I'm going to put my hands on you.
Just the way that they phrased things that they were doing, that was helpful because I
never have thought about rephrasing what I was going to say to somebody. That was very
helpful to kind of think of it from their perspective of how you should talk to a patient to
make them more comfortable with what you're doing so they maintain a sense of control in
the situation [Student 20019].
The instructors’ modeling taught students the importance of careful wording and how rephrasing can help
make a patient feel more comfortable.
c). Empowering Sexual Assault Patients. Key to empowering care is the concept of giving control
or power back to an individual who has had it taken away, as in the case of a sexual assault victim. Thus,
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
84
SAFE practice aims to restore some of the control that was lost as a result of sexual assault, and therefore
empower the victim to take an active role in her or his own healing process (Campbell, Patterson, Adams,
Diegel, & Coats, 2008). The clinical training sought to impart this idea to the students through observation
and practice empowering care in simulated scenarios. Many students found this helpful because they were
able to remember the information when they could observe it and then practice it. In other words, practicing
empowering care at the clinical training transformed what was abstract didactic online information into a
tangible reality. As a result, many of the students interviewed were able to articulate the importance of
giving control back to traumatized patients, and also indicated it was one of the primary purposes of their
interaction with patients. In the following quote, a student explains the importance of empowerment:
Let them discuss their feelings and allow them to feel like they’re in control. Once this
[sexual assault] happens, they feel like they have lost all their control and they have no
power or anything [Student 20032].
The primary way these students described how to give sexual assault patients back their control is
by explaining and offering choices throughout the forensic exam. Students described various ways this
happens, whether it is introducing oneself and explaining what the forensic exam is, giving the patient the
opportunity to refuse any part of the exam, or explaining every step of the exam as it is occurring. For
example, many students described asking the patient for permission throughout every part of the exam,
frequently asking “Is this okay?” and allowing the patient to say yes or no. Many students who mentioned
explaining the exam process and offering choices as priorities noted how it gave patients more control and
ownership of the exam and therefore, more control of their own bodies. Below, a student describes this
process:
Explain who you are, what you are there to do. Explaining that they have rights and if at
any time if they are uncomfortable say stop. Just let them have control. … So they can
kind of gain control back of their body after being sexual assaulted, they feel like they lose
control, but they've got to understand that they do have control of their own body, and what
I'm doing is they can say yea or nay at any time. It doesn’t have to be done; it’s their
choice [Student 3006].
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
85
Many students also mentioned that giving the patient choices extends beyond the exam. The patient can
choose whether to report the assault to law enforcement, for instance, or decide if she or he wants an
advocate present for the exam. Many students also talked about patient education as a form of
empowering care. These students explained that providing patients with knowledge about STDs,
medications, reporting and options for follow-up care is, in essence, giving patients more power over their
healthcare. The following quote explains this idea:
What options we can give to the patient in that this is what we can do for you? You have
the choice on what you would like to have done. If any part of the exam is uncomfortable
and you want us to stop, we’ll stop right there. And so just educating the patient on STDs
and birth control. There are so many things that we need to talk to the patient about. I think
if we approach the patient as a nurse knowing what options they have so we can give
them that information and they can make a good decision for themselves [Student 20018].
Several students also mentioned how it was important that a SAFE communicates that they believe the
patient and does not judge the circumstances that may have surrounded the assault. For instance, one
student talked about how her professional role dictates that she put her personal values and biases aside
when caring for patients. In other words, even if she felt judgmental about a particular case, her
identification as a professional SAFE kept those feelings from entering into her patient interaction. Because
sexual assault patients are vulnerable to being blamed or not believed by other formal and informal
supports when it comes to the circumstances of their assaults (Campbell, 2005), this aspect of
professionalism can be especially empowering. This idea is illustrated by the following quote:
I think just based on from when I started, you have to go in... I’m trying to figure how to say
this... unbiased, I guess, for lack of a better word. I learned real quick when [inaudible]
can’t judge somebody. You have to go in with it to do your job, trying to help them through
it, get them through it. Yet, several of mine have been false claims. But that’s not for me to
judge. Get in there. Do what you’ve got to do. Help and support them where you need to
help them and get them through it the best you can. And, like I said, it’s not for me to
judge, it’s not for me to decipher [Student 2006].
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
86
Through practicing patient interactions with GTAs, many students reported that they not only
learned the importance of offering empowering care, but learned the steps to offering it. By following the
GTA’s cues (e.g. feedback, allowing or not allowing certain procedures), students were given practice on
how to follow the needs of the patient, which is a critical component of empowering care. Below, a student
explains this idea:
And what I really came away with was giving them their control back of their body. Asking
them, “Is it ok, if I do this?” They say “yes” or “no” and that was really pivotal in many
aspects of nursing. “Is it ok if I do this?” You know, but especially it is allowing them to say,
“Yes, it’s ok.” Because of course they feel like they’ve just lost control of their own body,
being assaulted [Student 10016].
In addition, most students described how walking through simulated cases helped them
understand the words to say and the context in which to say them. For example, one student described
learning how the wording of phrases like “I’m going to touch your leg” can revivify traumatic feelings
depending on the situation. Practicing these interactions is what most students described as being
particularly memorable about learning empowering techniques (e.g. giving control back, giving patient
choices). The following quote illustrates how these students learned empowering care by walking through
scenarios and practicing with mock patients:
Just that the patients really have control of the whole exam. How to initially walk into a
room. What options we can give to the patient in that this is what we can do for you? You
have the choice on what you would like to have done. If any part of the exam is
uncomfortable and you want us to stop, we’ll stop right there. And so just educating the
patient on STDs and birth control. There are so many things that we need to talk to the
patient about. I think if we approach the patient as a nurse knowing what options they have
so we can give them that information and they can make a good decision for themselves
[Student 20018].
Probably most effective for learning empowering care were the instructors themselves. The
majority of students described how they learned empowering care by observing the empowering actions of
their instructors. Not only could they observe instructors acting in an empowering way to the GTAs, but they
were the recipients of this same behavior in the learning setting. Most students repeatedly used words like
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

87
“professional,” “confident” and “non-judgmental” when speaking about the instructors. Interestingly,
“professional” and “confident” were also terms most students used to describe the qualities they believed
an ideal SAFE clinician should possess.
3. Developing Medical Forensic Exam Skills. Overall, the majority of students reported the clinical
training substantially contributed to their knowledge and development of medical forensic skills, including
history taking, conducting pelvic exams with a speculum, identifying injuries with equipment and evidentiary
techniques, accurate documentation, and photographing injuries. This section will discuss the unique
benefits of learning forensic skills in a simulated clinical setting, and the medical forensic skills gained
during the clinical training.
a) Unique Benefits of Clinical Training. All of the students noted that the online training provided a
foundation of their understanding of medical forensic exams, but the clinical training advanced their
knowledge and skills to a level that made them feel confident and prepared to practice with sexual assault
patients. These feelings of preparedness were developed through multiple activities during the clinical
training. The students observed the instructors demonstrate how to take a history with GTAs, perform
pelvic exams, identify injuries with and without equipment, and collect and document medical forensic
evidence. Students were then given the opportunity to practice exams with mock patients while receiving
guidance and helpful feedback from experienced SAFEs. The majority of students noted that practicing all
aspects of the medical forensic exam during the clinical training contributed substantially to their skillset:
The actual hands-on, going step-by-step I thought was critical. Otherwise, you’re not
exactly sure … what it would look like in a real situation. So just having that experience
showing you how to work through the process, I thought was really helpful. To see it on-
line, you know, you read through some parts quicker and you might be missing something
you don’t think is as important. But when you’re actually doing the exam with someone,
they line out each step so you understand why you’re doing what you’re doing [Student
10073].
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
88
The majority of students also noted that practicing the exam with GTAs under the supervision of
experienced instructors helped them feel more confident in their forensic abilities.
The clinical training was absolutely a necessity for sure…it just gives you a little more
confidence, and it gives you – it helps to really train you in life situations as to how to go
about interacting with the patient, how to physically do things…It’s not until you go and
start doing the clinicals that you are able to apply and learn in a different way and be able
to hone your skills and just really figure out how you are going to do it and get yourself
together in a professional way so that you can approach it without looking like you’re
nervous all the time [Student 10041].
These students noted that the clinical training was particularly impactful because the training setting was
similar to a hospital emergency department, and the GTAs role played realistic scenarios. Together, the
clinical training set the tone of a realistic practice experience. The majority of students also indicated that
practicing with GTAs maximized their ability to learn because they could learn how to conduct exams
without fear of harming sexual assault patients.
b) History Taking. The GTAs’ realistic portrayals of sexual assault patients were important in
developing students’ history taking skills, particularly with their terminology. For example, students who
role-played with a GTA playing the part of a teenage girl had to use the vernacular common to adolescents.
If the student used terminology that a teenager might not understand, the GTAs would provide feedback
about their wording and how it could be confusing to a younger patient. In the following quote, one student
describes how the GTAs’ feedback enhanced her history taking skills.
We would say the word “ejaculate” and they were like, “If you’re fifteen years old. You
might not know what that means if you’re the victim.” So I like that, it was like we were
given a little sensitivity training, to not talk in big nursing terms, for even something as
simple as that word. They might not know what that means. Or they might call semen a
different word that you and I as a nurse haven’t heard about. So I liked that there was
sensitivity training in there. It seemed to me to be more open-minded. When I went into the
room to see the model and she was explaining that when I repeated what I had to say
back to her or interact with her, I was using her terms, not big nursing medical terms
[Student 20024].
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
89
As noted above, receiving feedback from the GTAs helped the majority of students refine their history-
taking skills with sexual assault patients. As a result, these students noted that they learned to use
language that the patient can easily understand. This practice and feedback also helped the majority of
students recognize the importance of using simple, concise language in their charting.
All of the students also learned that the patient’s history was important because it guided the
medical forensic exam. Prior to the training, some students had collected medical forensic evidence for the
sexual assault kit as part of their role in the emergency department. They shared that their approach was to
follow the instructions in the kit step-by-step without regard for the patient’s history. Thus, the kit rather than
the patient history dictated their process:
One of the things that I think we were doing at our facility was trying to do every swab in
our kit, whether it was necessary or not. So the knowledge that I and [colleague] do the
patient history and then let your history guide your exam. You know, if all there was
intercourse, they didn’t lick them or didn’t touch them or anything like that, then why are
you doing swabs? What are you swabbing? I mean, there wasn’t… so you have to let your
exams decide what swabs to even obtain. I think that was the biggest part, which is great
for the patient. They’re not having to sit there and endure all of that [Student 20012].
As noted above, the clinical training fostered the majority of students’ critical thinking skills when making
decisions about the medical forensic exam. In addition, these students were able to see the connection
between the patient’s history and decisions of what to collect during the medical forensic exam.
c) Fostering patient comfort during the medical forensic exam. Another skill that all of the students
learned during the clinical training was how to foster patient comfort while they were performing the medical
forensic exam. The instructors helped students understand how easily a sexual assault patient could be re-
traumatized during the pelvic exam and modeled different techniques to foster patient comfort during the
invasive aspects of medical forensic exam. In the following quote, a student describes why it was helpful to
observe the instructors’ explanation and interaction with mock patients.
I think when I watched the instructors, when they actually did an exam and showed us first,
it was kind of like how they... just watching them and the way they talked to them, and the
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
90
way they would seem to make that patient feel more comfortable in that situation. And I
think this comes to mind. Like when you’re actually doing the internal exam for a sexual
assault patient, they made us understand that this person has just been sexually assaulted
and now you’re going to stick a speculum into them and you know, when they’ve just been
assaulted, that could be very upsetting. So they just kind of talked to them and the way
they talked to them and told them how they were going to perform the exam and what they
were going to do and talked them through it. So I think that’s probably the thing I learned
the most, just watching them do that and interact with the patient [Student 30037].
As indicated above, observing the instructors helped all of the students understand the importance of
explaining the medical forensic exam to sexual assault patients, and how doing so can help patients
maintain a sense of control and feel more comfortable throughout the process.
In addition to the instructors, the GTAs had an important role by providing feedback and guidance
during the mock exams. For example, the GTAs would tell the students if the position of the speculum was
uncomfortable. Because the GTAs served as mock patients multiple times, they understood their bodies
well enough to provide this specific feedback, which the majority of students found helpful:
I just thought of the fact that we had live models for those exams, it was the first time, in
having done a lot of pelvic exams, it was the first time that I felt the person was being
completely honest about how uncomfortable the exam was or tolerable. Usually you ask a
patient. You check in with them constantly. How are you doing? Is this okay? Now I am
going to do this. You know, women are pretty tolerant. No. No. It’s fine. Just go ahead. I've
done this a million times. Just go ahead and do it. Those live models actually said you
know what? You are pushing too hard on this side. That was really interesting to have an
honest respondent during a pelvic exam. That's pretty unique [Student 30038].
Feedback from the GTAs prompted all of the students to conceptualize the exam from the patients’
perspective and helped them develop a slower, gentler approach.
The clinical training also gave all of the students the opportunity to practice the pelvic exam on
multiple GTAs of varying ages and body types. This was particularly helpful because all of the students
learned to gauge which speculum size and insertion method to use based on patients’ body type or size,
and how to vary their technique to promote patient comfort. The following quote discusses the benefit of
practicing with a diverse array of anatomies.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
91
We had a real young girl. We had an older woman. Then we had kind of a middle, who
was very skinny. So you got three different body types, three different ages, three different
sets of areas to examine…of different…one non-childbirth, one multiple childbirths, one
non-childbirth, but older. So it gave me a huge amount of knowledge over a short period of
time [Student 20020].
By performing exams with GTAs who had different body types, the majority of students felt more confident
and prepared to perform medical forensic exams in a gentle manner to a wide range of patients.
d) Identifying Injuries with Equipment and Evidentiary Techniques. While practicing the pelvic
exams, the instructors taught the students how to identify abnormalities or injury using visualization and
equipment. Many students believed that examining the GTAs was particularly beneficial with learning how
to identify abnormalities and injury.
I guess my learning style is it’s easier for me to remember how to do things and
procedures if I see them visually, but also it was nicer to see in that clinical setting, actually
being able to work with live subjects that you could get a better feel for what the genitalia
landmarks are that you are looking for as opposed to just looking at the diagram. That was
very helpful [Student 20019].
All of the students also believed that examining multiple GTAs allowed them to see variations of
genitalia, which provided a broader range of what was normal and abnormal. Students also observed the
instructors collecting evidence before practicing it on their own, including assessing injuries using
equipment such as the colposcope. The students also learned to use other techniques to visualize injuries,
including Toluidine blue dye and the Foley catheter. This practice was helpful to all of the students who
were new to performing pelvic exams, as well as advanced practitioners who perform pelvic exams as part
of their ongoing practice:
They had one day where it was skills and then the next day we did more scenario types.
So for me, sure I knew how to do a pelvic, but I got to use the colposcope. I got to use the
T-blue dye, which I had never used before. So all of those things were super helpful, to
have the scenarios and to have people who actually do it on a daily basis, as opposed to,
“Oh yes, I’ve never done this, but I teach it all the time,” [Student 10059].
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
92
As noted above, the instructors’ guidance while students practiced increased the majority of students’
sense of competency with the use of forensic equipment during MFE exams. In addition to demonstrating
techniques to collect evidence, most students noted that instructors provided the rationale behind their
approach and use of the techniques.
Like when they’re talking to the person they say, “Then next I usually will go like this, or I’ll
do this.” And they actually did it. And then if we can say, “Well, why did you do it like that
instead of this?” And they can answer. To me, that’s really helpful because it’s as if hands-
on I get to ask and they are showing me from experience how they do it and why they do it
[Student 10073].
By providing the rationale, the majority of students were able to gain a deeper knowledge of these
techniques by understanding how to use them, as well as when they should be utilized. Some students
reported understanding the rationale was helpful to their retention of forensic knowledge and skills.
Furthermore, some students found it helpful to observe multiple instructors who approached the
medical forensic exam with nuanced variations. In particular, these students indicated that these variations
provided them with multiple examples of the exam, which allowed them to determine the approach that
would work best for them.
I liked having the instructor there and seeing how they do it and what they would do. Each
of them had just a little different trick and you can see different ways of doing the same
thing and decide, “OK, this is what works best for me. This is what I’m most comfortable
doing,” [Student 10011].
By seeing demonstrations of multiple techniques and approaches, all of the students were able to try out
multiple approaches and select the one that worked best for them.
e) Forensic and Injury Documentation. Another major focus of the training was learning
documentation. During the clinical training, students practiced documentation while history taking and
practicing the medical forensic exam with GTAs. Many students indicated that they learned best through
hands-on practice and thus, the clinical training played a stronger role in learning documentation skills.
I think actually filling them out [chart] because that’s what we did for our clinical, at least
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
93
the one I went to. It was far more beneficial, to me, than watching it on-line. The on-line
course did help with getting an idea and feel for things, but like I said, I’m a hands-on
learner. It’s easier for me to do it to learn than it is to watch somebody else. But the on-line
portion did give me a basis to work from [Student 30055].
And the paperwork, that was pretty intimidating…And just being able to practice and not be
right in the heat of the moment with a case that could go to court. That was very beneficial
to get my hands on it and kind of get used to the process a little bit more… [Student
10054].
As noted, all of the students gained documentation skills because the clinical training provided a hands-on
opportunity in a low-risk situation; students could practice documentation without fear of legal
repercussions or negatively impacting a sexual assault patients’ case if they made a mistake. The majority
of students also noted that the instructors’ feedback contributed to their learning because it helped them
understand what they did well and the mistakes they had made.
It was nice to have someone go over it with me. I mean, the lecture on-line was good too.
But it was nice to actually do it, you know, kind of role play at being the documenter. And
then having someone go over it and be like, “No, that’s wrong and this is why.” It was nice
to have someone proofread it and then tell me why I need to change the way I did
something, instead of just reading. Like I said, I like the hands-on better, so it was better
for me. I liked getting this feedback. The feedback helped a lot [Student 10054].
The clinical instructors also provided students with examples to demonstrate how easy it is to make a
mistake or alter patients’ statements when collecting the patients’ history. The following quote illustrate this
point:
We saw how easy it was to make a mistake. They were talking about she was on a porch
drinking beer, but the nurse had written some beer, which was left; was it one beer or was
it a whole bunch of beer? So just a simple twisting of the words or a simple mistake could
throw the whole thing off so drastically, so that was helpful because they really tried to
reinforce that [Student 3005].
As indicated above, receiving instructors’ feedback and seeing examples of inaccurate documentation
helped all of the students understand the importance of accurate forensic documentation and how errors
might negatively impact a sexual assault patient’s case. Most of the students also noted that refining their
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
94
documentation skills was helpful because healthcare documentation is often more subjective and far less
detailed.
f) Photography and injury documentation. During the clinical training, a healthcare clinician who
also is a professional photographer taught students about photography and how to use an array of cameras
to document injuries. The instructor provided students with general information about the cameras’ buttons
and functions, including helpful information such as how to adjust the flash. The instructor also provided
students with specific information, such as how to take an orientation picture to effectively document the
size and appearance of sexual assault patients’ injuries. Additionally, the instructor demonstrated how to
document injuries by modeling photography with “injured” manikins. After observing the instructor, students
were given the opportunity to practice their photography skills. During the students’ practice, the instructor
provided helpful feedback to improve the quality of their pictures. According to the majority of students, the
hands-on practice and feedback made a substantial contribution to their understanding of photography and
its use in documenting injuries:
And he was really good at explaining how to do this with a very expensive camera vs. a
basic camera. How to do it with... you know... you go to a facility that’s not your normal
facility, and they say you have to use their equipment. And this is what you get. Here’s how
to approach that. Here’s how to look at this. Here’s how to do this angle [Student 20020].
Then he would look at the photos after we were done. He said, “You know what? You
need to do this. Or try this.” Like little neat things, like if you wanted to tone down the flash,
you could put a handkerchief over it or kleenex, and if you can’t figure out your buttons on
it, just put your finger over it. [Student 20034].
As indicated above, the hands-on practice of photography and the instructor’s feedback helped the majority
of students tailor their approach to capture optimal pictures of sexual assault patients’ injuries to
incorporate into their documentation.
g) Understanding their State Rape Kits. Because this was a national training, the students all came
from states that had their own policies and protocol pertaining to sexual assault, as well as their own unique
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

95
sexual assault kits. Prior to the clinical training, students were asked to bring sexual assault kits from their
states or facilities. The project director discussed the variations between kits and referred students to their
facilities for specific questions about the rationale of their kits’ contents. Most students found it helpful to
hear about the kit differences as it allowed students to understand how their facility’s documentation and
evidence collection could be improved. The following quote portrays the helpfulness of reviewing kits and
learning the current best practices:
We don’t have fingernail clippers in our kit. We don’t have a large piece of paper that you
spread out, so when they take off their clothes, any of the trace evidence that may be lost
when they change their clothes, in order to set up their clothes so you don’t have to touch
it and then you wrap everything back up in there. We don’t have that in our kit. I’m trying to
think what else ... There were actually several things. Those are the two I can remember
off the top of my head, because we didn’t have that, I wished that we had [Student 20034].
As noted above, reviewing kit differences increased all of the students’ understanding of rape kits and
exposed them to different approaches to forensic documentation and evidence collection. Furthermore, this
review helped most students identify problems, such as missing paperwork or outdated methods of
evidence collection. Finally, reviewing the states’ rape kits gave many students the confidence to ask their
program or crime laboratory the rationale behind the outdated documentation or evidence collection
practices.
4. Instructors’ Challenges and Recommendations. All of the instructors identified three primary
challenges experienced with teaching the clinical training: a) being unaware of the content taught online; b)
the diversity of approaches among instructors with teaching the medical forensic exam; and c) teaching the
medical forensic exam to students who have different sexual assault evidence kits from their home states.
In addition, we highlight the instructors’ recommendations for selecting instructors to teach future clinical
trainings.
a) Unaware of Online Content. The majority of the instructors did not view the online modules, and
some believed that it would have been beneficial in order to have a better sense of the online content. For
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
96
example, some of the instructors felt that seeing the modules would have provided a clearer understanding
what online content was covered. By being aware of the online content, these instructors believed that they
would have a better sense of the students’ knowledge base as they entered the clinical training. This would
allow the instructors to reinforce the critical areas covered in the online training while avoiding any
unnecessary redundancy.
It was important so that I knew how to tailor my teaching. What the content was on-line
should be reflected in the content and experience they were getting in clinicals, and so I
knew what knowledge level the participants were coming in with to help me teach
better…Do they understand the steps in a forensic exam? Have they been given didactic
or classroom content on how to obtain a history from a patient? Have they been given
rationale on why we collect some evidence in cases where we might not collect that same
evidence in a different case? So that you know what needs to be reinforced. You know
what needs to be addressed a little bit more than other areas [Instructor 106].
As indicated above, a few instructors believed that seeing the online modules would have allowed the
instructors to tailor their teaching style, thus creating more consistency in the teaching method from the
online training to the clinical training.
b) Diverse Approaches to Teaching the Exam. Most SAFEs have nuances in their approach to the
medical forensic exam process. These nuances are often a result of their training and professional
experience, as well as the unique nature of their clinical setting and patient needs. All of the instructors
suggested that these nuances may have been slightly problematic when teaching the clinical training. In
particular, the inexperienced students had some confusion when they saw each instructor approach the
medical forensic exam in a slightly different way.
For some people it’s good that they hear different ways of doing it and they can
incorporate all of that and choose to develop their practice from that-from all of those
sources but for other people it’s difficult hearing different ways of doing it and they would
just like-they would just want to be like “tell me how to do it right, tell me how to do it
correctly and that’s the way I wanna do it” [Instructor 110].
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
97
Two potential solutions were recommended to mitigate student confusion. One solution was having a brief
instructor orientation prior to the clinical training with the goal of establishing a consistent foundation for
teaching the exam.
… as an instructor I was aware of what the instructor next door was teaching. You know,
because of the students coming through. So I do wonder too if there would be a good
meeting for... like just before, to meet with the instructors and say, “This is the technical
way that we’re going to teach this” [Instructor 104].
All of the instructors noted that it is beneficial for students to observe variations among instructors because
it allows students to identify the process that would work best with their clinical setting and patient
population. However, many instructors believed that the inexperienced students needed to observe an
exact exam process before they would be able to integrate any variations into their understanding of the
exam process. Therefore, another recommendation was to teach an exact process first by having all of the
students observe a full exam together by one instructor. Once students are able to learn an exact process,
they would be ready to learn about the variations that exist among healthcare clinicians.
c) Sexual Assault Kit Differences among States. Students were told to bring their states’ sexual
assault kits to the clinical training. The goal was to have students review their state kits to become familiar
with them during the training. This posed particular challenges during the clinical training because most of
the state kits had different paperwork and protocols. In addition, the kits had varied evidence collection
practices and, in some cases, included outdated practices. As noted earlier, inexperienced students
preferred an exact approach and thus, this wide range of kits may have been confusing to students. In
addition, the kit differences was challenging for the instructors to address during the training because it was
important for students to practice the core components of the exam.
Well, I think I would assume it was a challenge for the students because we were mainly
using our Colorado kits. And the students, some of them, did bring their home state kits
with them, but I don’t know how often those were actually used, or whether it was more
they would be looking at their kit as we were explaining our Colorado kit. Like I said, the
principles of how you collect evidence should be universal, but you know, the different
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
98
steps, like the consent forms, all sound different. Some of the reporting issues are
different. Things like that I don’t know how that could be addressed in each state
[Instructor 103].
As this instructor notes, this is a challenge to teaching at a national training level because it requires the
instructors to be familiar with different state protocols. Thus, the majority of instructors believed it would
have been beneficial to learn more about state differences. The instructors handled these kit differences by
having a dialogue about why some kit items or protocols are considered outdated. Furthermore, the
instructors provided guidance to the students about talking with their local crime laboratories about the
rationale to include or exclude particular items in their state kits.
d) Selection of the Instructors is Important. Instructors appeared to play an important role with
students developing their skillsets at the clinical training. Thus, we wanted the instructors’ viewpoint of who
would be an appropriate candidate to teach the clinical training. The majority of instructors believed that
those with many years of experience and who still practice would serve as the best instructors because
they need to answer a wide range of questions given the diversity of students’ backgrounds, experiences,
and patient populations. Experienced instructors also may be better equipped to articulate the rationale
involved in multiple decision points with SAFE practice. Furthermore, instructors who have a wealth of
experience share stories that keep the students more engaged in learning and benefit from hearing real-life
successes and mistakes.
I think the instructors have to be processing and seeing a fair amount of patients in order
to be able to teach these students. And have a good knowledge base. ... you can’t have a
nurse that’s just... who does some clinicals once in a while, and has a little bit. I mean, they
really need to have a fair amount of expertise so they can share that with the students.
And be able to answer questions that come up, because there are tons of questions that
come up. You don’t have to know the answer to every question. But I think if you’re a
nurse that has been an instructor that has seen several different types of patients... I feel
like I have such a broad spectrum of patients that I’ve seen that I’m able to answer a lot of
questions, because we see so many patients [Instructor 107].
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

99
In addition to experience, instructors must have patience and be encouraging, but also direct
students to practice even when they are experiencing anxiety about practicing the exams. On occasion,
some instructors would spend the time allotted to their skill station by answering questions and
demonstrating the exam rather than requiring students to practice. While this can enhance students’
knowledge, it places students in a passive learning stance rather than having an active role. The quote
below explains why passive learning is problematic for students learning SAFE practice.
They would actually buy into the idea, and sometimes you get this when you’re live
precepting with actual assault victims and nurses, is, “No, no. I want to watch you do it.”
You know, so those instructors that allowed themselves to sort of be led down that road,
instead of having the students practice, I prefer that not happen. The ones that I would
want back over and over again explained the rationale to the students all the time, had the
students explain the rationale to them as they were doing something, so that they had
them saying out loud what was being done and why… You can teach someone to do task
X, Y and Z, but they are either learning the rationale or they’re not. And it’s definitely been
my experience that, if nurses after a certain period of orienting and precepting cannot
explain to me why they’re doing what they’re doing, they’re not getting it. So the instructors
who are assisting those students along in describing what they’re doing and why they’re
doing what the rationale is behind it, are the best instructors [Instructor 101]
As noted, instructors need to focus most of the time on having students practice the exam and articulate
their rationale for the decisions made during that practice. This learning process prepares students to
practice autonomously, which is common in most SAFE program settings.
Evaluation Question 5: What were the students’ post-training experiences with applying their
knowledge?
1. Application of Skills with Post-Training Patients.
a) Compassionate Care Skills. We were interested in understanding if the students implemented a
compassionate care approach with their patients once they began practicing. For students who have had
patients since the training, we asked them to describe a case that went well and one that did not go well so
we could understand their approach with the sexual assault patients. All of the students identified utilizing
many approaches they learned in the training, including using a slower, gentler approach combined with
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
100
non-threatening tone of voice and body language. They also described taking time to build rapport and trust
between the patient and provider; and respecting patient modesty by asking others to leave the room
during the exam or covering the patient with a sheet to limit exposure:
Well, definitely tone of voice, choosing your words wisely, making sure you’re not
displaying any sense of opinion. Treating them as a whole, rather than just someone to do
an exam on [Student 30053].
Additionally, all of these students reported creating a soothing environment, such as securing a private
room with dim lighting and attending to patients’ needs by offering warm blankets, and food and drink. A
student explained how to create a comfortable and safe environment for patients below:
Soothing voice, blankets, calmness, initially a little bit lower light not just stark white, and
just like a reassurance that, “We’re here to help you and help get you through this,” and let
them know that, “Down the road, there is still going to be help for you,” rather than, “This is
what’s going to happen tonight. Bye bye. See ya.” You know, that there is a future after
this event [Student 10036].
Many students also noted ways that they enhanced their patients’ sense of safety, such as following the
patients’ needs and allowing them to tell their story without interruption to build patient-provider trust and
rapport. These students reported trust, reassurance, and a comfortable environment appeared to help their
sexual assault patients feel safe during the exam process. In the following quote, a student explained how
she ensures safety with sexual assault patients:
When we do our exams, our doors are shut and our curtains are closed. There is also a
note on the outside of the door that says there is a procedure in progress. So the patient
knows from the very beginning that nobody is allowed in that room at all. The fact just
covering them up and making them feel comfortable and letting them know that it’s okay if
they say no. Nothing is going to happen to them, or nothing is going to change the fact that
I’m there to take care of them if they say no. I think that has a lot to do with it too [Student
30039].
b) Empowering Care Skills. During the study’s interview process, students were asked to describe
a case they either observed or performed that went well. This was to garner their perceptions of what
components go into an exemplary forensic exam. Most students described cases that included some
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
101
elements of empowering care. For example, these students described offering their patients detailed
explanations, validating their experiences and leaving out questions that may seem blaming or judgmental
(e.g. questions about what the patient was wearing, why they put themselves in a particular situation, etc.).
Many students believed that judgment is to be left out of the interaction with the patient, instead focusing on
education and offering informed choices:
I never made a single remark about, “What on earth did you do? Going to someone’s
house, you know, and doing this kind of thing?” But she was so beside herself. There was
no judgment on my part. I took detailed notes about everything that she said. And I
supported her and then followed up with her [Student 10050].
This student was able to acknowledge her personal opinions without letting those feelings get in the way of
empowering patient care. Based on the majority of students’ descriptions, it is evident that students were
able to integrate patient care skills learned in the training, such as compassionate care and fostering
patient empowerment, into their post-training care of sexual assault patients.
c) Students’ Documentation. We were also interested in understanding how students applied their
medical forensic knowledge and skills in their practice with sexual assault patients following the training.
Thus, the qualitative interviews inquired if the students had received feedback from an experienced
colleague or supervisor regarding their documentation with sexual assault patients. Overall, we found that
most students were not provided feedback about their documentation from a supervisor or colleague. Some
of the students who did receive feedback were provided with brief remarks that they had done a good job
with their documentation, while others who do not have SAFEs in their institutions sought feedback from
their department supervisors.
When I did the first exam and turned it in, my one boss and my educator both said they
hadn’t realized how in depth and how vast an actual sexual assault exam can get. They
would have never even thought about doing half the things I did in the exam. And that was
when I started saying, “We need a specific packet for this.” That was what brought it all to
the forefront with that. They were like, “You know, we figured that what we had would
suffice. There’s a lot more to it. I said you should also take consider a referral out to a
social worker and a psych for treatment down the road. It doesn’t just stop here [Student
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

102
20020].
Although the supervisor and educator were not SAFEs, their feedback indicated that the student’s
documentation was detailed and thorough. A smaller number of students were provided with feedback from
trained SAFEs who indicated that the students’ documentation was of high quality:
Their feedback was good. Yeah, it was very good. She said, “You were concise and to the
point. You didn’t add anything extraneous. You just wrote what you needed to write down
and really wrote down, again, what that victim stated,” [Student 10016].
Well, like I said before, she [supervisor] is not a very complimentary person, and she was
very complimentary on the very first one I did. She came to me and said excellent job.
There is nothing to correct at all. She said she was impressed [Student 20063].
The few students who we able to receive feedback from trained SAFEs and non-SAFEs have indicated that
their documentation is meeting the institutions’ expectations with some minor exceptions. For example, one
student was informed to write “not collected” on envelopes rather than leaving it blank.
2. Students’ Remaining Challenges with Patient Care. We were also interested in understanding
students’ remaining challenges and recommendations after completing the training, specifically in regards
to patient care. Although the clinical training included the practice of patient interaction skills, many
students lack confidence in providing care and fostering comfort with sexual assault patients. Based on
qualitative interviews, these students’ struggles with patient care include fear of re-traumatizing patients as
well as caring for patients with unique needs (e.g., male patients). Many students who practice in rural and
low-resource SAFE programs also continue to struggle with patient care due to their unique settings and
challenges. Students’ remaining struggles and recommendations are outlined in further detail below.
a) Fear of re-traumatizing patients. Some students are still fearful of re-traumatizing sexual assault
patients. Specifically, students said they are afraid they might say something insensitive or offend patients
with their wording of questions:
I kinda felt we’re rushing through the interview process and – cause that seemed like the
most important part for me. I wanted to get my wording down so I can talk to my patients
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
103
and not be nervous…that’s the thing I’m most nervous about is offending somebody you
know; saying the wrong thing [Student 3003].
It is interesting to note that this fear seems to be more prevalent for students who do not work in
emergency departments (EDs) as students who work in EDs were less likely to have concerns about
upsetting their patients. This may be because students who work in EDs have previous experience with
traumatized patients or patients in crisis, and are therefore less anxious about interacting with them.
I don’t know what other nurses' specialties were entering this program, but I’m an ER
nurse and we see that in our psych patients. We see that in our patients who just lost...
whose family member just coded. We see emotional, physical traumas every day in my
field, so I treat everyone the same, meaning that yes, I will be more empathetic to one,
more comforting to another. You can see. The non-verbals will tell you where they stand
and how they are handling their stress. Everybody handles stress differently. And you have
to identify these flags and treat them appropriately [Student 20047].
Many students with the aforementioned struggles would have liked additional opportunities to
observe instructors interact with GTAs and then engage in hands-on practice with GTAs. Namely, many
students felt less confident with conducting the patient interviews and would have liked to observe the
instructors demonstrate more mock interviews. These students felt more practice would have let them
refine their techniques before treating actual patients, as illustrated in the following quote:
I guess the big thing was the interview process. I think that was a key concept. I think we
could have had a little bit more time with it … We didn’t really get to practice that and I
think that is where you make your biggest connection with the patient. It is just hearing
other people, I guess, how they have done this since they have much more experience
than us…the words that they use to communicate with our patients, and it would have
been really helpful to go over that a few more times or even have like a mock interview
thing where we could at least taken it home and molded it to how we want to process
[Student10066].
b) Managing Biases. A few students were concerned about ambivalent feelings they might have
toward SA patients and how to manage those feelings so as not to let it negatively impact patient
interaction. While this was not a common occurrence, a couple students seemed surprised by these
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
104
feelings as they found it difficult not to judge a sexual assault patient’s decisions prior to the assault. Below,
a student talks about this conflict:
Ambiguous, and feelings of like, “How did you get here and why?” And not just how do you
avoid blaming that person, even just... not outwardly, but internally… And not blaming. I
mean, even though you know no matter what happened, it’s hard not to feel like, in your
mind, on the outside, but even I think the first time I did one by myself, it was... it affected
like whether or not I was going to collect something, because she didn’t... yeah, so just
trying to be neutral at all points, I think. You just have to practice that too. But I know we
did talk about it at the training. And more reminders about that, the feelings [Student
10010].
These students thought it would have helped them understand some of these conflicting feelings if they
heard more about the instructors’ personal experiences with patients. In general, these students reported
they liked hearing about the clinical instructors’ experiences and getting advice from those who have been
through a wide variety of clinical situations. But it seems that these students would have had less anxiety
about patient interaction if they heard stories about some of the mistakes instructors may have made in the
field.
I think I would have learned a lot. You know, you learn by other people's mistakes kind of
thing or their weird interactions. It's the same kind of thing. I think I would have learned a
little bit more [Student 30015].
c) Male patients. Some students stated they felt unprepared to approach, comfort, interact, and
perform exams on male sexual assault patients. This may be because male sexual assault patients are
less common and students had little to no previous experience treating them. Below, a student discusses
her feeling of anxiety in regard to treating male sexual assault patients:
Like I said, the only thing that I wish had been covered more was the aspect of a male
because that is something that happens. You don't think it does, but it does, and how to
approach them because it is different. They are different. Men are different from women.
Emotionally they are different. This situation is completely different. The areas of assault
are different. The ways of assault are different. You know, there's a lot of difference, and I
wished we could have approached that [Student 20063].
As demonstrated above, some students were concerned about interacting with male sexual assault
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
105
patients because they may present differently than female patients. Sexual assault patients’ demeanor,
trauma reactions, and exam needs may be subject to gender differences, according to these students.
These students recommended the clinical training include hands-on practice with male GTAs, including the
opportunity to role-play clinical scenarios, collect evidence, and perform exams.
d) Patients with strong or absent emotional reactions. Many students stated it was challenging to
provide patient-centered care to patients with strong or absent emotional reactions. This includes, for
example, patients who present with flat affects or, by contrast, patients who have strong emotional
reactions who are inconsolable. These students said they were particularly concerned about approaching,
comforting, and interacting with these patients without causing the patient further emotional distress. These
students reportedly felt ill-equipped to establish rapport with these patients, and also were unsure of how to
obtain consent or conduct an exam when a patient is highly emotional or withdrawn. The following quote is
from a student who discusses this challenge:
Whereas the ones [patients] that really bothered me the most are the ones who don’t
interact with you at all. They just lay there, don’t want to answer any questions. That to me
is more emotional than anything, I think, because they are shut off. And the ones that are
yelling or screaming or crying or something, at least there’s some emotion that you can
react to. You can’t react to anything if there’s nothing. That’s the hardest for me. Do you
just continue to do this? Even though they’ve given consent… [Student 10028].
Many of these students would have liked additional opportunities to practice scenarios with GTAs exhibiting
strong or absent emotional reactions. Further, these students recommended additional opportunities to
observe instructors interact in these scenarios in order to learn words and phrases to comfort the patient or
de-escalate highly charged situations. Additionally, they suggested online modules should include
interactive scenarios of patients’ reactions and have the student identify how to manage reactions and
promote comfort with their patients.
e) Patients with disabilities. Some students also wanted more information about patients with
special needs such as those with cognitive, psychiatric, or physical disabilities. Based on qualitative
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
106
interviews, these students stated they felt underprepared to meet the potentially complex needs of this
patient population. Similar to their feelings about patients with strong or absent reactions, some students
were also concerned about obtaining consent and explaining patients’ rights to patients with disabilities. For
example, one student talked about caring for a patient with dissociative personality disorder and how
difficult it was to attend to the patient’s medical and evidence collection needs while also having to attend to
a severe psychiatric disorder. Below, another student describes the challenges she faced in this respect:
But at the same time, I think, “Gosh, am I just not very good at directing people who maybe
need a little more direction, particularly in the history taking. So I guess maybe wish that
the training had covered the history taking a little bit more. I guess that’s what it amounts
to, because I think even in the situation of that first patient I told you about, it’s not
necessarily just about the history taking. But it still is that period of time where you’re just
getting to know the client and you’re hearing what happened. How do you hear a
particularly challenging client or a client that has challenges particularly related to mental
illness or other mental impairments due to drugs or intoxication? [Student10049].
Students who reported such struggles did not provide specific recommendations as to how the training
could address their concerns. Overall, students with these concerns would have liked additional information
on how to meet the needs of patients with disabilities.
f) Rural and low-resource SAFE programs. Many students from rural and low-resource SAFE
programs reported having difficulty providing patient-centered care due to their unique setting and practice
challenges. Many students from these practice settings reported not having private rooms or pelvic beds for
their sexual assault patients. The lack of resources hinders students’ ability to promote patient comfort and
poses challenges to maintaining patient privacy or ensuring patient safety. For example, low-resource
programs may be less likely to have a private room for sexual assault exams. Further, some students
practicing in rural or low-resource SAFE programs reported they do not have local victim advocacy groups.
Because of this lack of advocacy services, these students found their role expanded to include the type of
emotional support often provided by advocates. As a result, they were less confident in their patient comfort
skills and concerned about how their increasingly supportive role might alter their role as objective forensic
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

107
examiners. As such, these students would have liked more information about addressing their patients’
emotional and follow-up needs.
Students from rural SAFE programs also face unique challenges, particularly in regards to privacy
and confidentiality. Many students from rural SAFE programs, for instance, reported it is common for sexual
assault patients to be personally acquainted with their medical providers. Students said patients in this
situation may feel uncomfortable due to risks to confidentiality and may be more reluctant to report assaults
or be less forthcoming with SAFEs. Many students recommended the clinical training include additional
opportunities to practice scenarios more likely to occur in rural areas, which may help students feel more
prepared and comfortable in their SAFE roles.
3. Students’ Remaining Challenges with the Medical Forensic Exam. Many students identified
several areas of struggle with the medical forensic exam and documentation. Although the clinical training
included several practice opportunities, many students lack confidence in their role as a SAFE and are
fearful that their mistakes may compromise a case. Based on the qualitative interviews, many students’
remaining struggles include certain aspects of the medical forensic examinations, documentation, and CJS
involvement in sexual assault cases. Students’ challenges and training recommendations will be described
next.
a) Medical forensic evidence (MFE) exam. A significant number of students reported feeling
unprepared for some aspects of the MFE exam because they did not feel that they had enough time to
practice using equipment such as the colposcope. As a result, several students reported that it has been
challenging to incorporate this equipment into their MFE exam with post-training patients:
I work with a different camera and it’s on a tripod and it’s not on a colpo. So in the clinical
training, we used a colposcope to take vaginal pictures, which is different than using a
regular camera and tripod. So yeah, I would have loved to have been able to... like I still
have a hard time doing genital exams and taking a photo with a digital camera. You know,
it’s not an easy thing. So there are things like that that I wish that I could have had more
practice with…how to fill your kit correctly. Like I still, “OK, what tape am I really allowed to
use here?” [Student 10059]
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
108
These students could have benefitted from more practice with different types of equipment and procedures
that would be germane to what they would encounter when they began practicing post-training.
Secondly, some students continue to lack confidence in the quality and accuracy of their evidence
collection because they have not received feedback from a SAFE or their crime lab. Some of the students
were surprised that their local crime lab has never provided them with feedback about the completion and
accuracy of their kits. These concerns were particularly salient for SAFEs working in low-resource or rural
programs who do not have an active sexual assault response team (SART).
We don’t have actual set people, and that’s what’s hard. It’s really getting… because I
don’t know that, whenever I’m handing over this evidence if it’s getting followed up. I would
like to have touched more on that in class situation. Like maybe have brought the whole
SART team in and explain the whole procedure and explain what each person’s
responsibility is…I would like to have seen the whole, entire process. That would have
been awesome. Not just the exam [Student 10018].
A few students also expressed confusion about their local protocols such as where to submit the blood and
urine specimens for toxicology. It would have helped, they said, if the training had included a speaker from
a crime lab to gain a better understanding of how to submit toxicology samples, enhance evidence
collection, and maintain the chain of custody with sexual assault kits. A few students would have liked to
have seen how the kit is processed in the crime lab.
I think that we’ve just touched the tip of forensics with what we’re doing. I think it would be
helpful to know the entire process of running a kit through a crime lab. To me, it would just
kind of complete the picture of why I’m collecting this and why it’s important to collect it a
certain way [Student 10011].
Furthermore, many students desired some guidance about how to reach out and collaborate with their local
crime laboratory and law enforcement agencies to better understand their community protocol.
e) Documentation. Many students reported they were uncertain of the accuracy of their forensic
documentation because they have not had the opportunity to perform many exams post-training and did not
have a trained SAFE to provide feedback.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
109
I felt that the information I got on documentation, the on-line stuff, was pretty thorough,
was pretty... I mean, I think why I lack in it and why I’ve had problems with it was not being
able to do it enough. You know, if there was maybe more examples or more opportunities
to do actual written exam documentation, I think that would have been a beneficial part of
the course that we didn’t really get to do [Student 20020].
Many students believed that they could have benefitted from more coverage of documentation in
the training to help them feel more prepared and confident. For example, students would have liked the
online training to incorporate additional examples of good and weak documentation. Many students also
suggested that the online training incorporate documentation homework whereby students are shown
pictures of anatomy with a range of injuries, and the students would have to document the injuries on a
body map.
They’re meaning documentation of injury because we got so used to looking at what was
normal that when injury came about, it was kind of like, “Oh. What is that? Is that a bruise?
Is that an abrasion? And maybe showing more slides of actual non…like not normal,
compared to normal…Like maybe during the on-line stuff having a picture put up and then,
“Ok, what do you see?” And then having like a multiple choice, and, “Ok, that’s an
abrasion.” And then having it say, “Nope. This is what it is and this is why this is what it is,”
[Student 10071]
In addition, some students believed that it would help to hear audio recordings of mock patients and have
to document the patient narratives, then receive feedback from the project director.
Many students said that their uncertainties about documentation could have been mitigated if the
clinical training included more opportunities to practice documenting the patient narrative with GTAs.
Several students also expressed they struggle to identify and document injuries related to a sexual assault,
such as identifying the difference between a laceration and an abrasion. A student discusses this challenge
in the quote below:
I honestly really do honestly wish I had had a little bit more training in looking for vaginal
injury and using the Toloudine blue and using the colposcope because…so many more of
the majority of rapes that I see are somebody that’s a person they have had sex with in the
past, somebody that they are in a dysfunctional relationship with…So those are going to
be harder to find areas of trauma, but I want to be able to find the slightest little piece of
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
110
evidence, because if you can’t find anything, that’s really going to hurt them if they are
trying to press charges [Student 10041].
Many students lack confidence in their knowledge of the proper medical terminology used to describe injury
(e.g., ecchymosis) and anatomical terms (e.g., posterior fourchette). These students said they would have
liked more time during the clinical training to practice identifying a range of injuries and anatomical
landmarks. In addition to practice, they would have liked more feedback from the clinical instructors as to
the quality of their injury documentation.
f) States’ rape kits. A large group of students were unable to obtain their states’ rape kits before
attending the clinical training. These students reported it was difficult to learn about documentation and
evidence collection specific to their states’ rape kits without having access to their own. They reported it
was challenging to learn a new skill using unfamiliar paperwork and then transfer their knowledge to their
own program’s forms. Many students recommended the training include every state’s rape kit so that
students could learn how to perform sexual assault kits with their own materials. In addition, many students
recommended the clinical training incorporate an experienced SAFE’s review of each student’s kit so they
could learn the current best practices or how to enhance their collection of medical forensic evidence.
g) The role of CJS. Many students experienced challenges with the criminal justice system
personnel and wanted more information about how to work with them cooperatively while keeping their
patients’ needs a priority. For example, some students reported feeling rushed or pressured by law
enforcement while they performed the exam. As a result of being rushed, they reported missing important
aspects of documentation or the exam. The following quote illustrates one student’s challenge in working
with law enforcement.
No. Most of it is that I am ... you know, when you’re in the middle of doing the exam on the
patient and then the police are hounding you to get the box, that I’m doing it too quickly,
and then afterwards I’m like, “Oh my gosh.” When I review it I say, “I should have done
this. I should have documented that. I forgot to document this.” Things like that [Student
10059].
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

111
A few students recommended the clinical training include discussions about the best approaches to
developing professional relationships with their local law enforcement agencies and prosecutors.
Some students reported still being confused by the different sexual assault laws and statutes
between states. These students reported feeling overwhelmed by the amount of information provided in the
online module that covered various states’ sexual assault laws.
And it sort of felt like I was, instead of just getting a taste of what was there, I felt like I was
trying to learn the whole legal system. And sort of I could see where feeling like you had
more knowledge, you just, in that sense, I felt I was less confident [Student 1009].
Even though many students understand how difficult it is to address each student’s concerns at a national
training, they would have liked if the training could have directed them to resources within their particular
states where they could have gone for more information.
Finally, most students are particularly fearful of testifying in court because they are afraid that their
mistakes might weaken the case or damage their credibility as a SAFE. These students would have liked
the clinical training to provide an opportunity to practice testifying at a mock trial.
Yes. I think a mock trial is really important, if it’s possible. Just because it puts that
together and to listen. If you can really get a prosecuting attorney to listen to how they try
to break down their credentials and ruffle your feathers and to watch some of the
experience that goes into trial. I would think if you had never seen that and then you were
called to trial, they could just chew you up and spit your out. I think that would be a
valuable addition, if at all possible [Student 10016].
4. Students’ Experience and Needs when Encountering Delayed Practice. More than half of the
students interviewed reported performing or observing at least one forensic exam following the IAFN
training. However, a sizable minority of students had not yet performed nor observed any exams. These
students were not practicing because of personal reasons (e.g. relocation or change in employment status),
low patient volume at their practice sites, and resistance from their institutions or communities (e.g. state
regulations or lack of awareness about SAFE services). Most of the non-practicing students stated they
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
112
remain committed to SAFE practice and were attempting to access opportunities to practice the skills they
learned in the training. In this section, we explore the post-training experiences of students who
encountered delays with practicing as a SAFE. We will begin by explaining the barriers that students faced
with practicing, and how this delay impacted the students. This will be followed with a discussion of the
additional needs of students who encountered delayed practice.
a) Barriers to Practice. Most of the time, students were not practicing for reasons outside their
control. Many students were employed in rural areas with low-patient volumes and simply had not had the
opportunity to examine a sexual assault patient. Some students, meanwhile, described considerable
resistance from their institutions and/or communities. For example, several of these students described a
pervasive lack of awareness about sexual assault that prevented administrators or community members
from seeing the need for SAFE services. For these students, systemic resistance and a lack of awareness
have been the major obstacles to practice.
Some institutional obstacles are procedural; that is, some students said their institutions do not
have policies or protocols in place to treat sexual assault patients or poor administrative support precludes
a program from being established. Other obstacles are because of rigid state or community regulations on
SAFE practice. For example, two students had not practiced nearly a year after the training because state
officials were uncertain whether the IAFN training fulfilled the particular education requirements of those
states. Another student reported that officials are procrastinating about allocating money to fund a program
in her state. Some students said they were surprised by these challenges, saying that they mistakenly
thought they would return from the training and transition seamlessly into practice. Below, a student
discusses her surprise at the difficulties she faces in regard to beginning practice:
Yeah, I guess I left there 10 foot tall and bulletproof thinking that I could start something no
matter what, but I didn't realize all the legalistic parts of it. You can't do it without
somebody to back you or somebody that's in this area that's done it. I don't see being able
to leave Colorado and come back and do sexual assault exams by yourself [Student
20049].
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
113
b) Effects of not Practicing. Given that approximately 44% of the students had not performed their
first exam, we wanted to know how delayed practice impacted students’ feelings of confidence and/or
motivation. This section will look at how students feel about not practicing, and if they believed it affects
their abilities to practice as SAFEs.
Motivation. Many of the students who had not performed an exam remained committed to
eventually starting SAFE practice. These students said they stayed motivated by keeping up with
information and seeking out educational opportunities. This includes students attending a community
seminar about sexual assault or reading and studying the subject. For example, one student said she will
often re-read some of the course materials and notes she took during the training. The following quote
offers another example of how through self-guided learning a student can stay motivated and less anxious
about practicing:
It hasn’t because I’ve always been learning about it. I’ve still been studying on it even
though it’s been taking a while to get me into the clinical setting [Student 3003].
Several students also found encouragement from colleagues at their institutions or by linking up
with community groups that addressed SAFE issues. These students found that having regular contact with
experienced SAFEs or those interested in SAFE practice helped them stay interested as well. One non-
practicing student, for instance, explained how physicians at her hospital let her observe and assist with
SAFE exams in order to keep her skills and knowledge fresh while she waits to become certified in her
state.
In addition, several students found community groups that supported their interest, such as a local
chapter of the IAFN. This gave students regular access to up-to-date SAFE knowledge while connecting to
others with the same area of interest. The following quote discusses how community resources can support
clinicians while they wait to start practicing:
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
114
However, I think it’s really key to continue education throughout the year. If you’re in a rural
hospital, especially, what we have in [Nearby city] and [Nearby city] is our SANE program
down in the metro area, they allow SANE nurses from the rural areas to come in and
shadow the busy hospitals. I did do that this past winter, in January.… To have maybe a
larger metro hospital having these shadow programs for the rural hospitals is fabulous. It’s
– an awesome experience, I learned a lot [Student 20018].
Anticipation. Several students expressed positive feelings about the prospect of practicing. These
students, while acknowledging they would be nervous during their first exam, looked forward to practicing
and believed they would be able to recall the training information easily. During the interviews, students
who had not performed exams were asked whether they would perform a SAFE exam if called upon that
same day. This question was meant to gauge students’ perceptions of their own abilities and whether they
felt prepared to begin SAFE practice. Several students said they could perform an exam because the
information and skills they learned in the training would be quickly remembered and incorporated into their
practice. A student discusses this in the following quote:
I do feel like I certainly learned that, and it would all jog back pretty darned quick. The
pelvic is a maneuver. I could look at a YouTube in 15 minutes and get refreshed on that.
So it is truly no different than looking in someone’s ears or eyes. … So no, they gave me a
lot of confidence at that training. And we’re almost a year out. [Student 10073].
A few students said that they believed the delay in practice would give them a different approach once they
started practicing. For example, a student explained that had she started practicing immediately following
the training she would have been overconfident. The delayed practice, she believed, had made her more
careful and thoughtful about performing exams.
Confidence. In contrast, several students who had not yet started practice mentioned they had
decreased confidence about practicing than they would have had they begun practice immediately
following the clinical training. However, they did not indicate that this affected their desire to practice as
SAFEs. Instead, they acknowledged they would have less confidence going into their first exams, but
believed they would eventually overcome it in order to begin practicing. Some of these students stated they
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
115
would probably ask that a supervisor or colleague shadow their first exam to ensure everything was being
done correctly. Below, two students talk about how their confidence has been affected by not practicing:
I definitely am not as confident as when I first came out, of course. But as far as
confidence goes, that builds with practice, which I don’t have any of. So I definitely
wouldn’t say, “No, I can’t do it.” I might do it with a doctor that’s done it before, helping me
[Student 10028].
I definitely, especially now, you know, every day that passes that we’re away from the
training, I feel like I’m not as good as I should be [Student 10058].
Both students linked their lack of confidence with their lack of practice following the training. Most of the
students who reported a lack of confidence said that they would likely have more needs once they start to
practice. For example, many students said they would have to observe a SAFE exam a few times before
attempting to perform one on their own, or they would want a preceptor to oversee their first few exams.
While many students believed that they would be able to recall the training information easily, some were
concerned about losing the finer details. Some were concerned about losing the information they were
taught in the training, including whether they would be able to identify genital landmarks or perform
speculum insertion.
c) Post-training Needs. Some students suggested a couple of ways in which the IAFN or the
training itself could assist them post-training. Several students said they would have liked more educational
opportunities post-training. For example, students who had not started practicing yet were concerned about
forgetting information and suggested that the IAFN could offer regular “refresher” courses as a way to keep
up their skills and knowledge:
I would like to... I don’t know... there should be some kind of refresher or something, I
think, for us in the rural communities who do not see the cases like they do in the inner
cities [Student 10028].
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

116
These students were not specific in their suggestions, meaning they did not outline curriculum needs or
offer ideas on what online platform to use. Rather, their suggestions were more general, voicing an overall
concern about retaining knowledge and skills while they await practice opportunities.
A few students would also have liked the IAFN or, more specifically, the clinical instructors, to have
checked in with them post-training. Ongoing support seemed to be particularly salient for students who
were either struggling to start practicing or were located in more isolated geographic areas where there was
not an established support system. In the following quote, a student explains how follow-up is particularly
important for her because she does not receive any feedback at her rural facility:
But I don’t know, some follow up in the year, you know, like maybe that could just be a
requirement of the training, I don’t know. But in a year, you kind of go through an
evaluation or support, you know, kind of situation where you review your cases or review
your technique or get a booster of training or something like that. It would be helpful for
me, I know, because I don’t get a lot of feedback from my facility itself. And you certainly
don’t get feedback from your patients or anything like that. I mean, you may get some
feedback from the legal system eventually. But that’s pretty delayed and down the road, if
it ever happens at all [Student 10010].
This student wanted some sort of evaluation or review to ensure she is providing adequate and appropriate
SAFE care for her patients.
VI. DISCUSSION OF FINDINGS
A. Summary of Cross-Study Findings and Implications
Blended training has great potential to address the SAFE shortage across the United States,
especially in communities with limited access to SAFE training. In this project we used a multi-study, mixed
methods design to examine whether this blended approach would be an effective learning modality to train
SAFEs. We analyzed quantitative surveys, pre- and post-tests, and a post-training follow-up test to
evaluate immediate and longer-term learning outcomes. Further, we conducted qualitative interviews with
the clinical instructors and students who completed the training to explore how the clinical training
contributed to the students’ learning outcomes, and the processes that occurred during the clinical training
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
117
that contributed to those outcomes. Taken together, this project evaluated the effectiveness of this blended
learning modality to understand if and how this approach prepared healthcare clinicians for competent
SAFE practice. It is important to understand whether blended training is effective because SAFEs have a
critical role in promoting healthcare outcomes of sexual assault victims and collecting high quality medical
forensic evidence, both of which have been linked to improved prosecution rates. This section will begin
with a discussion of the key findings and implications across the five evaluation questions included in this
project, and conclude with an examination of the strengths and limitations of this project. In the discussion
section, we will provide potential explanations for the findings and the students’ recommendations, as well
as offer our recommendations when applicable.
1. Findings from Evaluation Question #1: What Factors Predict Training Completion/Attrition?
The first aim of the study was to understand whether student attrition would be a concern for this
blended learning approach by examining how many students completed the training and what predicted
training completion. This is has been shown to be a particular challenge for no-cost continuing education
courses, where the rate of completion has been approximately 55% (Stone, Barber, & Potter, 2005). If the
clinicians do not complete the training, they cannot become SAFEs, and thus the blended learning modality
would not be considered effective for improving the SAFE shortage. Thus, it is important to understand
whether students complete this training and the reasons behind why some did not complete it. However,
there is a dearth of research on student attrition of SAFE training regardless of training modality. Therefore,
we drew upon the literature focused on training attrition of adult learners, especially healthcare clinicians.
This literature suggested three major factors that influence training completion: student characteristic
including familiarity with, access to, and ease of using computers; student motivation (e.g., intrinsic
motivation, reasons for interest in SAFE practice); and barriers to training completion (e.g., work and family
obligations, time constraints, supervisory support for training participation).
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

118
1. What Predicts Training Completion? We utilized a quantitative survey design to examine how
many participants completed the training and what factors predicted training completion. We were
concerned that students who dropped out of the training would not continue to participate in the evaluation
so we administered an online survey to all enrolled students prior to the training that covered a range of
factors that the literature suggested was associated with attrition. The findings showed that 79.3 percent of
the enrolled students completed the SAFE training, which is higher than completion rates for online courses
in general and substantially higher for free continuing education courses.
a) Predictors of training completion. The results from the hierarchical logistic regression analysis
indicated that clinicians who were interested in the training because of the two-day clinical component were
more likely to complete the training. Further, students who work in rural communities were more likely to
complete the training. These findings are different than prior research examining the completion of other
types of courses, which suggests that access and familiarity with computers, student motivation, and fewer
external barriers, such as work and family obligations, leads to training completion (Angelino, Williams, &
Natvig, 2007; Atack, 2003; Gegenfurtner, Veermans, Festner, & Gruber, 2009; Gormley, Costanzo, Lewis,
Slone, & Savage, 2012; Perry, Boman, Care, Edwards, & Park, 2008; Park, 2007; Welsh, Wanberg, Brown,
& Simmering, 2003; Willging & Johnson, 2009). One reason for this difference may be that the significant
predictors of training completion in this study (interested in the clinical component and type of community)
are not commonly included in training studies because they are primarily relevant to this specific training.
However, the extant literature on online training completion may provide some insight into the reasons that
these particular factors influenced the students to complete the training.
b) Interest in clinical training. Being drawn to the training because of the clinical component was a
significant predictor of training completion, so the students may have been motivated to complete the online
training so they could attend the clinical training. There are a couple of reasons these students may have
wanted to attend the clinical component of the training. The students who participated in the qualitative
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
119
interviews indicated that they preferred “hands-on” learning and the opportunity to ask questions and
receive immediate feedback while they practiced. Furthermore, the students may have been drawn to the
clinical training because of the clinical instructors’ extensive experience, especially because of the shortage
of qualified preceptors (Elfrink, Kirkpatrick, Nininger, & Schubert, 2010). Approximately half of the
interviewed students indicated that they did not have a trained SAFE available for a preceptorship and thus,
they viewed the clinical training as critical to the development of their clinical skills. The clinical training may
have served as a motivator for completing the online training because it was a prerequisite to participating
in the clinical training.
c) Community type. The findings also indicate that students who work in rural programs were more
likely to complete the training. Prior research has not found differences in the perceptions of online learning
between clinicians who work in rural and urban areas (Karaman, 2011). However, clinicians from rural
communities struggle to obtain continuing education because there are fewer healthcare trainings available
locally and access to such trainings requires travel (Baernholdt & Mark, 2009). Furthermore, workplace
budget constraints, lack of administrative support, and staff shortages prevent access to training for those
in rural communities (Bolin, Peck, Moore, Ward-Smith, 2011; Stroth, 2010). Therefore, students from rural
communities may have viewed the SAFE training as a rare opportunity to access training, especially
because online training mitigates the common barriers to participating in training for rural clinicians (Penz,
D’Arcy, Stewart, Kosteniuk, Morgan, & Smith, 2007). Additionally, clinicians in rural hospitals commonly find
they have to be proficient in multiple specialties and have a variety of responsibilities in several
departments as compared to clinicians in urban hospitals (Roberge, 2009; Stroth, 2010). Therefore, the
rural clinicians may have been expected to provide acute care for sexual assault patients prior to the
training, which may have motivated them to complete the training so they can become proficient in their
care of future patients.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

120
On the other hand, because urban and suburban areas often have more continuing education
opportunities like SAFE training, clinicians in these programs may not have viewed dropping out of the
training as a missed opportunity because they could attend a local training. Urban and suburban institutions
also have higher patient volumes than rural programs, and it may have been possible that the students
needed to receive training quicker in order for the institution to meet the demands of the patient volume
(Roberge, 2009; Pong & Russel, 2003). A few of the interviewed students noted that their institutions were
confused by the length of the training because the traditional SAFE training model is one week of didactic.
It is possible that some of the students from urban and suburban communities needed the training to have
a shorter duration. In addition to needing a shorter course because of work concerns, some students simply
learned at a faster pace than others and would have liked more flexibility when moving through the
modules. To address this issue, we recommend that future IAFN SAFE trainings provide more flexibility
with students completing the modules at a quicker pace.
2. When did Attrition Occur? We also examined the risk of attrition over the course of the training.
This is a less examined area of training attrition, but it is possible that the factors associated with early
withdrawal may be different than later withdrawal of the course (Park & Choi 2009). Therefore, we
examined the factors associated with the timing of when attrition occurred. The Cox Proportional Hazard
Model found somewhat similar results as the first part of this evaluation question. For any given time during
the training, the odds of remaining in the training were greater for a participant who was motivated by the
two-day clinical workshop compared to those who were not interested in the two-day clinical workshop.
Community type was a marginally significant predictor with attrition being lower for those that worked in a
rural community than those who worked in an urban or suburban community.
The study also found that students who were interested in the training because of its online nature
were more likely to complete more of the training relative to those who were not. The factors that draw
students to online training may have been a motivator to complete more of the training but not necessarily
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

121
enough to complete the training. For example, students who are drawn to online learning prefer learning at
a flexible pace, which also reduces the common training barriers of work and family responsibilities
(Gormley, Costanzo, Lewis, Slone, & Savage, 2012). Still, students who are interested in online training
sometimes misperceive online courses as easier and underestimate the amount of time needed to maintain
the course expectations (Johnston, 2007). Taken together, the flexible pace may have contributed to these
students completing more of the training, but their underestimation of the time commitment may have
prevented some students from completing the entire training.
2. Findings from Evaluation Question #2: Is There an Effect of the Training on Students’
Knowledge?
The aim of the second evaluation question was to determine what extent students learn the course
content. It is important to understand if/which modules yield low knowledge gains because they can be
revised to maximize learning. Furthermore, it is important to understand what factors may influence higher
or lower gains of knowledge. Similar to attrition, there is a dearth of research on knowledge attainment
rates and predictors for SAFE training. As such, we drew upon the literature focused on knowledge
attainment of adult learners, primarily in the healthcare field. Prior research indicated four major factors that
influence knowledge attainment: a) student characteristics and prior computer experience; b) motivation; c)
external barriers such as work and family obligations; and d) characteristics related to the training. Further,
we also wanted to assess factors outside of the training because students reading non-assigned material or
attending additional SAFE trainings might influence their knowledge attainment.
1. Is There a Significant Increase in the Students’ Knowledge upon Completion of the Training
Modules? The second evaluation question assessed whether students attained knowledge during the
twelve online training modules. The study used a one-group pre-test/post-test design (Shadish, Cook and
Campbell, 2002), which involved students completing a weekly online pre-test before completing each
training module and then a post-test upon completion of the module. This design has been recommended
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
122
for the assessment of online courses because online learning can be more and less effective for particular
topics (Jang, Hwang, Park, Kim, & Kim, 2005; Johnston, 2007; Reeves, 2000; Wild, Griggs, & Downing,
2002). The results showed that the mean post-test scores were significantly greater than the mean pre-test
scores for all 12 online modules. On over 40% of the modules, the knowledge gains exceeded 25%. Prior
studies have found a broad range of knowledge gains for healthcare professionals participating in online
courses, from 9% to 42.5%, with an average of 24% (Bell et al, 2008; Bello et al., 2005; Hugenholtz, Croon,
Smits, van Dijk, & Nieuwenhuijsen, 2008; Jang, Hwang, Park, Kim, & Kim, 2005; Jeffries et al., 2003;
Metcalf, Tanner, & Buchanan, 2010; Schneiderman, Corbridge, & Zerwic, 2009; Stone, Barber, & Potter,
2005). Thus, 40% of the modules are similar or above the average rates of knowledge attainment.
a) Higher knowledge gains. The module with the greatest knowledge gain was the forensic
science, ethics, and self-care (35.85%), which focused on the fundamental work of the SAFE, including the
role in the care of the patient and the ethical implications of practice. The rest of the modules with high
gains in knowledge focused primarily on the medical forensic exam, including the modules on photography
(29.80%), medical forensic history and physical (25.48%), evidence collection (25.63%), anogenital exam
(23.93%), and the criminal justice system (20.75%). Although the students scored well in these modules,
some of the interviewed students reported feeling less confident with identifying injuries, and distinguishing
between normal genitalia and anatomical variants and disease process. These students stated that they
would have liked the online modules to include more opportunity to view pictures of genitalia and practice
identifying injuries, and anatomical structures. In addition, although students had higher knowledge gains
with the justice system and testifying, the interviewed students noted that they would have liked opportunity
to practice testifying through mock trials during the two-day clinical training, which would boost their
confidence with courtroom testimony. It is important to note that these students believed that they had
attained a strong foundational knowledge, which was also shown in their post-test scores, but they wanted
additional opportunities to learn the material deeply. Therefore, we recommend that future trainings
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
123
incorporate additional practice, case study reviews, and repetition of the content into the online modules to
advance their knowledge and skillset, which has been found in prior research (Johnson, Hornik, & Salas,
2008; Wild, Griggs, & Downing, 2002).
b) Lower knowledge gains. The modules with lower knowledge gains included those pertaining to
medical management (15.86%), documentation (14.92%), program and operational issues (14.11%), and
patient-centered, coordinated team approaches (9.33%). The qualitative interviews may shed some light on
these lower gains. The medical management module covered the health consequences of sexual violence,
including acute health needs (e.g., prophylaxis treatment for sexually transmitted infection (STI), injury
treatment, and pregnancy prevention) to long-term issues (e.g., counseling). Some of the interviewed
students indicated that this module was quite lengthy, which led to them feeling overwhelmed and confused
by the content. When students perceive the amount of material as cumbersome, they often have less
engagement with learning, which result in lower knowledge gains (Svirko & Mellanby, 2008). In general,
they believed that they learned better with shorter modules, and recommended that longer modules be
broken into subsections to help them grasp the material better. They also believed this would help them
plan their online learning time better. Additionally, some students did not believe that all of the content was
relevant to SAFE work. Understanding the relevance of the training content plays an important role in
knowledge attainment because students are more engaged when they understand the relevancy (Guthrie &
Schwoerer, 1996). Thus, the students who believed that some of the content was irrelevant to SAFE
practice may have been less engaged with this module. We recommend that IAFN assess the medical
managment module to determine if all of the content is relevant to SAFE work. Any material that is not
relevant should be removed to allow students to focus on the core content. If all of the content is deemed
relevant, then the module should begin with an explanation of how the content is relevant to SAFE practice.
Further, the medical management module should be broken into subsections that ideally do not extend
beyond twenty minutes (Pomales-García & Liu, 2006).
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
124
The documentation module focused on documenting the medical forensic evidence and the
patient’s history accurately and thoroughly. One reason that student scores in this module may have been
low is that this type of documentation was new for students. Many of the interviewed students described
MFE documentation as requiring a great amount of detail in comparison to the documentation used in their
current and prior clinical work. As such, many of these students wanted more opportunities to practice
documentation and receive feedback to understand if they were using terminology correctly and
documenting accurately. Given the students’ feedback and the lower knowledge gains for this module, we
recommend that the documentation module incorporate additional homework to practice documentation
and provide feedback to help students gauge the accuracy of their documentation.
The program and operational issues module discussed various models of care delivery used by
SAFE programs, and SAFE program development and sustainability issues. This module may have not felt
relevant to those who were joining an established SAFE program and do not have aspirations to manage a
SAFE program. Therefore, it is possible that those students were less engaged with this module.
Interestingly, those students who were developing new programs desired more information on program
development than what was provided. Because the training is content-intensive, we recommend that IAFN
consider including only content in this module that is relevant to a new SAFE. Material that is not relevant to
a new SAFE could be offered as an elective module at the end of or after the training. This would allow
students who encounter program development and sustainability issues to benefit from the module at a
time when it is most relevant to them. Finally, students had low test scores in the patient-centered,
coordinated team care module, which explained the multidisciplinary team approach to sexual assault,
including each responder’s role. Interestingly, the interviewed students noted that it was the clinical training
that helped them understand the role of other disciplines. It is possible that the students did not understand
the relevance of the information so early into the training as this was the third module in the online series.
Most clinicians do not collaborate with the criminal justice system as part of their daily work and thus, the
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

125
importance of this module may have not been recognized by students so early in the training. Now that the
students are in the field and are trying to forge relationships with other disciplines, they realize the
importance of this content. Based on their field experiences, they recommended that this module include
approaches to developing professional relationships with the criminal justice system, as well as how to
work cooperatively with law enforcement while keeping their patients’ needs a priority. This balance
between responsibilities to patients and collaborations with the criminal justice is a common challenge for
SAFEs, including those with extensive experience. Thus, this topic is important to include in the module
(Campbell, Greeson, & Patterson, 2011). Because these challenges were not realized until the students
began practicing, we recommend that this module occur later in the course or be covered at graduated
levels across the course. For example, students could learn about the basic roles early in the course, but
learn about how to collaborate with system personnel towards the end of the training or even offer an
additional module once they begin practicing.
2. What Predicts Knowledge Attainment? The second evaluation question also examined the
predictors of knowledge attainment. The results from the multiple linear regression analysis found that
higher knowledge gains were significantly associated with higher levels of motivation and a reliable Internet
connection. Students who were drawn to the training because it was no cost to them was linked somewhat
to higher knowledge gains. On the other hand, lower knowledge gains were significantly related to students
who reported more work/personal barriers and those who were drawn to forensic nursing because they
have personal experiences with sexual assault. Lower knowledge gain also was marginally linked with
students who reported less comfort with computers during the pre-training survey.
a) Comfort with computers. Access to reliable Internet has been linked to students’ success for
online courses (Hylton, 2006). In addition, discomfort with computers has been linked to less success
because there can be a steep learning curve to maneuvering a learning management system, which may
detract these students from learning the content (Atack, Rankin, & Then, 2005; Hylton, 2006). The project
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
126
director fielded many questions about the learning management system through emails, phone calls, and
the discussion board, which seemed to resolve the technology issues that some students experienced.
However, those who felt less comfortable with computers may have continued to have difficulty acclimating
to online learning despite the assistance provided. This evaluation utilized a scale to measure students’
comfort with computers. We recommend that IAFN consider having future students answer the items on
this scale (see page 180 in Appendix C) to allow the project director to identify individuals who may struggle
with online learning, and subsequently contact them by email or phone to address their specific
technological challenges.
b) External barriers. Additionally, work and personal barriers (e.g., work and family responsibilities)
also can impede learning if students do not have adequate time to spend with the course material. Success
with online courses tends to require six to ten hours a week, but many students underestimate the amount
of time needed (Alexander, Polyakova-Norwood, Johnson, Christensen, & Loquist, 2010; Chio, 2012).
Similar to recommendations in the literature, some students suggested providing a course schedule that
outlines the time duration of each module, which would allow students to reserve specific time to engage
with course work and stay on-track (Alexander, Polyakova-Norwood, Johnson, Christensen, & Loquist,
2010). In addition to providing a course schedule, we recommend that IAFN inform students upfront of the
weekly time commitment, which would allow them to determine whether they have adequate time to commit
to the training and plan accordingly.
c) Motivation. Motivation to learn also has been linked to successful course performance (Frankola,
2001; Gegenfurtner, Veermans, Festner, & Gruber, 2009; Howard, Noe, & Wang, 2006; McMahon, 2013;
Welsh, Wanberg, Brown, & Simmering, 2003). Student motivation is particularly important because of the
self-directed and self-paced nature of learning for online courses (Zhang, Zhou, Briggs, & Nunamaker,
2006). Thus, less motivated students may experience temptation to postpone online course work or be less
engaged while going through the modules (Baptista-Nunes & McPherson, 2002). The IAFN SAFE training
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
127
engaged in many activities shown to foster student engagement and have been linked to increased
knowledge attainment. For example, the online instructors provided pictures and a brief introduction of
themselves, which can help students feel connected to their instructors (Atack & Rankin, 2001). In addition,
the online training incorporated audio of the instructors providing a lecture that followed on-screen text and
visual information (e.g., pictures of anatomy), which is similar to instructional methods utilized in a
traditional classroom (Sitzmann, Kraiger, Stewart, & Wisher, 2006). The integration of audio and visual
modalities was noted by students to be helpful with learning the content. Prior research also has found that
audio-video integration contributes to student engagement and greater knowledge gains than utilizing
visual or audio information alone (Derouin, Fritzsche, & Salas, 2005; Wild, Griggs, & Downing, 2002). In
addition, student engagement and success are enhanced with a variety of instructional approaches
(Means, Toyama, Murphy, Bakia, & Jones, 2010). For instance, the SAFE training students found the
online audio interviews with patients talking about how SAFE patient care impacted them particularly
powerful. This type of real-life scenario activity has been shown to promote learning as well (Metcalf,
Tanner, & Buchanan, 2010). Thus, we recommend that the IAFN continue to utilize these instructional
approaches.
Although IAFN utilized many instructional methods that have been linked to student engagement
and course success, students who began the training with lower motivation to learn may require additional
activities. We recommend that IAFN incorporate into future trainings additional strategies that have been
found effective with increasing engagement of less motivated students. One strategy is to increase
instructor-to-student and student-to-student communication and discussion (Baptista-Nunes & McPherson,
2002). The types of instructor-to-student communications found to increase student engagement include
the instructors individually contacting students early on in the course and when students exhibit lower levels
of online activity (Angelino, Williams, & Natvig, 2007). Providing feedback on homework is another way to
help students feel engaged and has been strongly linked to course success (Atack & Rankin, 2001;
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
128
Johnson, Hornik, & Salas, 2008; Sitzmann, Kraiger, Stewart, & Wisher, 2006). In other words, two-way
interaction provides stronger course outcomes than one-way interactions, which means that course sizes
must be manageable for this communication and feedback to occur (Atack, 2003; Machtmes & Asher,
2000). It is important to note that the SAFE project director did engage and communicate with students,
which they indicated was helpful and satisfactory. However, the interviewed students expressed a need for
additional homework assignments where they could receive feedback, which we will address in more detail
later in this section.
Collaborative learning among students also improves their engagement and course performance
compared to students working in complete isolation (Means, Toyama, Murphy, Bakia, & Jones, 2010; U.S.
Department of Education, 2010). The most common method of developing collaborative learning is posting
weekly questions to foster discussion (Baptista-Nunes & McPherson, 2002). The SAFE training provided
discussion board forums, but some of the students indicated the students’ discussion focused primarily on
providing each other with support. Some students found this support helpful while others would have
preferred more structured discussion boards that spurred conversations about the content. This suggests
that the SAFE students have two needs --- support and content discussion – with both playing an important
role in fostering engagement and motivation. Thus, we recommend two types of discussion board forums:
one that provides students with a virtual space to offer each other support and another that provides
discussion threads with the specific aim of advancing their understanding of the content.
d) Personally affected. The current study also showed that students who were drawn forensic
nursing because of personal experience with sexual assault (as a survivor or as an informal support) had
lower gains. This variable also was marginally related to knowledge retention so it merits additional
investigation. While this finding has not been examined in online learning research, prior research has
suggested that those who have been exposed to intimate violence with and without post-traumatic stress
have more difficulty with sustaining auditory attention, have delayed free recall, and poorer working
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
129
memory (Jenkins, Langlais, Delis, Cohen, 1998; Stein, Kennedy, & Twamley, 2002). However, it is
important to note that students were not asked if they had experienced a sexual assault. Instead, these
students volunteered this information when asked an open-ended question of why they were interested in
the forensic nursing. Thus, it is possible that there were other survivors in this training, but they were drawn
to forensic nursing for other reasons. The instructors who were interviewed noted that this training can
intensify emotions for survivors. It may be possible that the content of online modules and the clinical
training provoked emotional reactions strong enough to impede their knowledge attainment and retention.
One of the interviewed students noted that they observed another student who appeared a bit shaken from
listening to a GTA role-playing an abducted survivor. After hearing the story conveyed by the GTA, the
student walked out of the room feeling shocked by the story. While it is unknown if this student was a
survivor, this does suggest that the clinical training might be triggering emotions for some students, which
might make it difficult for them to learn. Although the scenario may have been upsetting, SAFEs do
encounter sexual assault patients who have experienced abduction, along with other forms of violence.
Thus, this finding should not imply that the scenarios should be different for future training. However, the
students may need some forewarning that the scenarios might provoke emotion and suggestions for how
they can handle this during the clinical training. Furthermore, we recommend that the instructors share how
they have handled their own emotional reactions when working with sexual assault patients, especially
when they began their SAFE careers. Understanding how a SAFE training impacts survivors merits
additional research, particularly because this work may appeal to survivors who want to make a difference.
Therefore, it would be beneficial to understand survivors’ needs as they participate in a SAFE training and
how to maximize their learning.
3. Findings from Evaluation Question # 3: Did the students retain their knowledge?
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

130
Prior research has noted that students may not retain all of the knowledge originally attained during
the training (Bell et al., 2008; Naidr et al., 2004). Therefore, the third evaluation question examined to what
extent students retain their knowledge after the training.
1. Among those who Completed the Training, did the Participants Retain their Knowledge? We
assessed students’ retention of their knowledge through a post-training test approximately three months
following the training. There is limited research on knowledge retention rates of blended learning because
this training approach is fairly new in healthcare (Makhdoom et al., 2013). Karamizadeh and colleagues
examined the rate of knowledge retention of students who participated in a blended healthcare training. In
this study, they compared pre-test scores to test scores measured two to four weeks following the training,
and found a significant increase pre-test to a two- to four-week post-test, suggesting that knowledge can be
retained for a short period of time following a training course. A few studies have examined knowledge
retention for a longer prior of time for healthcare online courses. They found that knowledge loss was
common and sometimes high with a range of 26.4% to 100% of knowledge loss when tested three months
or longer (Bell et al., 2008; Naidr et al., 2004). This suggests that a fair amount of knowledge can be lost
following a continuing education course.
In the current study, we examined knowledge retention with the same factors utilized to assess
knowledge attainment. Using repeated measures ANOVA, the study found that the students experienced a
reduction of knowledge from 77.92% at post-test to 68.83% at the follow-up exam with a 9.17% loss of
knowledge. In comparison to the rates reported in prior research, this rate of knowledge loss for the IAFN
SAFE blended training appears fairly low. The clinical training, in particular, may have played a role in
supporting knowledge retention. Many students in the qualitative interviews indicated that the clinical
training helped clarify, broaden, or solidify the content covered in the online modules. Thus, it appears that
the clinical training reinforced the content learned online, which can facilitate knowledge retention (Bradley
et al., 2007; Kaddura, 2010; Means et al, 2010; Stewart, Inglis, Jardine, Koorts, & Davies, 2013). The
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

131
extant literature suggests that engaging in simulated training, such as utilizing GTAs, can help students
retain knowledge because it provides an opportunity for students to have an active role in learning (Elfrink,
Kirkpatrick, Nininger, & Schubert, 2010; Kneebone, Scott, Darzi, & Horrocks, 2004). In addition, immediate
feedback from the instructors plays an important role in identifying gaps in the learner’s knowledge and
skills, which can help students’ progress as they learn from their mistakes (Kaddura, 2010; (Stefanski &
Rossler, 2009).
2. What Predicts Knowledge Retention? We also examined predictors of knowledge retention. The
results from the multiple linear regression analysis found that the students who were drawn to the training
because of the two-day clinical training experienced more retention of knowledge. In addition, knowledge
retention was somewhat higher for students with more experience. Alternatively, students who have taken
a prior online course experienced significantly less retention of knowledge. Students who were drawn to
forensic nursing because of an experience with sexual assault had somewhat less retention of knowledge.
a) Interest in clinical training. Being drawn to the training because of the clinical component was a
significant predictor of knowledge retention. Valuing the hands-on component of the clinical training may
have influenced students’ knowledge retention. The training literature suggests that transferring knowledge
to the workplace can occur when students perceive the course as valuable and useful because they tend to
engage more in learning the content (Gegenfurtner, Veermans, Festner, & Gruber, 2009; Johnson, Hornik,
& Salas, 2008). In the pre-training survey, some students noted that they were particularly interested in
learning medical forensic evidence (MFE) exam skills, which is a large component of the clinical training.
Further, the students who participated in the qualitative interviews noted that they preferred “hands-on”
learning methods, which suggests that these students may learn better and retain more from an active
applied instructional modality Elfrink, Kirkpatrick, Nininger, & Schubert, 2010; Kneebone, Scott, Darzi, &
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
132
Horrocks, 2004). Together, this might suggest that the students perceived the clinical training as valuable,
which led to deeper engagement in the clinical training and, subsequently, to knowledge retention.
b) Nursing experience. Clinicians with less experience are often in the stage of exploring their
career options, which can result in leaving a department, an institution, or even the healthcare field (Pool,
Poell, & ten Cate, 2012). In comparison, experienced clinicians tend to have more career and
organizational commitment. This commitment to one’s career and organization has been linked to
transferring knowledge to the workplace (Gegenfurtner, Veermans, Festner, & Gruber, 2009). Further,
experienced clinicians have fewer training opportunities to help them broaden their skills (De Lange et al.,
2010; Pool, Poell, & ten Cate, 2012; Taylor and Urwin, 2001). The excitement of learning new skills may
have been motivating to the experienced students, which is related to higher degrees of knowledge
retention (Metcalf, Tanner, & Buchanan, 2010; Naidr et al, 2004).Taken together, this unique opportunity to
advance their skills and provide a needed service in their institution may have motivated the experienced
clinicians to invest in their skill set by reinforcing and applying their learning following the training. In the
current study, students with less experience were less likely to complete the training and had less
knowledge retention. As such, we recommend that inexperienced clinicians be provided with additional
supports during and after the training to be successful. For example, post-training mentoring may be useful
in helping inexperienced clinicians with the transition into the SAFE role (see page 149 for specific
suggestions for mentoring).
c) Previous online courses. Students who have taken a prior online course had significantly less
knowledge retention. One possible reason for this finding is that students may have underestimated the
time commitment based on their prior experience with online courses. The pre-training survey asked the
students if they believed that an online course would take less time than a traditional course. Of those
students who have taken an online course, the majority either thought it would take less time than a
traditional course, or were uncertain if it would take less time or not. Students who have realistic
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

133
perceptions of a training including time commitment are more likely to retain and utilize their knowledge in
the workplace (Gegenfurtner, Veermans, Festner, & Gruber, 2009). Thus, it may be possible that the prior
courses taken by these students were less rigorous and required less time in comparison to the IAFN
training. By underestimating the time commitment, students may have engaged in surface learning, which
is a quick approach to learning in which students learn enough to do well on tests (Chambers, 2013).
However, a deeper approach to learning, where the goal is to understand the material, is essential for
knowledge retention. As mentioned earlier, we recommend that future students be provided with a detailed
syllabus that outlines the time duration of each module might be helpful so students can arrange time when
they will be most engaged with the material (Alexander, Polyakova-Norwood, Johnson, Christensen, &
Loquist, 2010). In addition, we suggest that time commitments and expectations be included in future
training applications and advertisements to help students determine if their personal schedule permits time
to be effectively engaged with the course content. Furthermore, homework that requires active learning
may help students engage in deeper learning (Chambers, 2013).
4. Findings from Evaluation Question # 4: How did the clinical training contribute to students’
knowledge?
1. How did the Clinical Training Impact Students’ Understanding of SAFE Concepts? To assess if
students understood the core concepts of patient-centered care, we asked the students who were
interviewed to describe the best approach when working with sexual assault patients. The students
appeared to have solid understanding of the importance of providing patient-centered care for their
patients’ well-being. Furthermore, they understood that the patient-centered approach creates a non-
threatening environment for survivors to disclose the assault, which improves history taking and
subsequently the MFE exam. In terms of the medical forensic exam, the students believed that the clinical
training contributed substantially to their knowledge and skill set. They reported that the training enhanced
their history taking skills and helped them document the patient narratives in an objective manner. Many
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

134
believed that the training improved their communication skills, including using terminology understandable
to patients. Many students noted that they felt competent conducting medical forensic exams, including
speculum insertion, allowing the patient history to guide the exam, identifying and documenting injury, and
utilizing multiple evidence collection techniques and equipment. Students also believed that they were
better at taking pictures of injuries.
2. How did the Clinical Training Facilitate Student Learning? The effectiveness of clinical skills
trainings is strongly related to the process and strategies utilized by instructors (Elfrink, Nininger, Rohig, &
Lee, 2009). The interviews with the clinical instructors and students revealed that the clinical training and
instructors utilized many strategies that have been shown to be effective in enhancing students’ learning
(Wild, Griggs, & Downing, 2002). First, students’ anxiety about attending the clinical training was
addressed. Many students and instructors noted that the students were anxious when they entered the
training. This level of anxiety is common among students participating in a clinical skills training because
their learning occurs in the presence of others (Elfrink, Nininger, Rohig, & Lee, 2009). Similar to past
research, the greatest contributor of their anxiety was the fear of conducting pelvic exams due to the
personal nature of the exam and fear of causing harm to the mock patients (Pugh, Obadina, & Aidoo, 2009;
Seago, Ketchum, & Willett, 2012). High levels of anxiety and low self-confidence is problematic in the
learning environment because they can impede a student’s ability and effort to learn (Klein, 2006;
Lundberg, 2008). The instructors and director utilized multiple strategies found to be effective with creating
a non-threatening environment such as treating the students with respect and patience, offering
encouragement, and facilitating a sense of camaraderie (Elfrink, Nininger, Rohig, & Lee, 2009; Haffer &
Raingruber 1998; Jeffries, 2005; Lundberg, 2008).
The clinical training also incorporated many pedagogical approaches that have been found to be
effective with learning clinical skills. The instructors began each skill station by inquiring about the students’
clinical backgrounds to assess their learning needs. This assessment was important because the students
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
135
had varied backgrounds – some had no experience conducting pelvic exams; others had extensive
experience with pelvic exams in their roles as advanced clinician practitioners or physicians. Further, some
students had experience interacting with patients dealing with multiple types of physical or emotional
trauma while others did not. Thus, this assessment informed the instructors of areas that might require
additional practice (McGaghie, Issenberg, Petrusa, & Scalese, 2010). The instructors also demonstrated
components of SAFE practice (e.g., history taking, empowering compassionate care, MFE collection),
which provided students with a clear picture of the exam process. This allowed the students to be exposed
to exemplary practice, which can be particularly helpful for those with little experience (Goodman, & Wood,
2004). However, modeling is less effective than students practicing the exam process themselves, so most
instructors had students swiftly proceed to practicing with the GTAs (O’Connor, 2006).
Students practiced different components of the exam process with the GTAs while the instructors
provided guidance and feedback. GTAs have been found to improve student performance with exams, and
reduce student anxiety about performing pelvic exams with actual patients (Baillie, & Curzio, 2009; Seago,
Ketchum, & Willett, 2012; Theroux & Pearce, 2006). Students often practiced one component of the exam
at a time, which is a method particularly effective with inexperienced clinicians (van Gog, Sluijsmans,
Brinke, & Prins, 2010). Instructors also promoted students’ clinical reasoning by having them articulate the
rationale of their decisions during the exam process, which can help students develop autonomous
decision-making (Kaddoura, 2010; Parker & Myrick, 2010).
Feedback also played an important role with students’ skill development. The GTAs helped
students feel less fearful about conducting pelvic exams by providing them with feedback about whether
the speculum was hurting them or not. Because many students worried that inserting a speculum would
hurt the GTA, receiving their feedback of when it did and did not hurt boosted their confidence and lowered
their anxiety about performing the exams. It is important to point out that actual patients typically do not
provide this type of feedback even when asked and thus, the GTAs’ feedback provided an invaluable
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

136
insight into the patient perspective (Theroux & Pearce, 2006; Vessey & Huss, 2002). Instructors also
provided immediate feedback while the students were conducting the exam, which is often inappropriate to
do with actual patients because the feedback may decrease patients’ confidence with their provider.
Immediate feedback is critical to skill development because students can receive corrective guidance as
mistakes are occurring or validation for when they are performing well (Ellis & Davidi, 2005; McGaghie,
Issenberg, Petrusa, & Scalese, 2010). This allows students to have a clear understanding of their learning
progress and needs. These pedagogical approaches instilled confidence in most students, which is
important because students who lack confidence are more prone to performing poorly and making clinical
errors (Smith et al., 2001; Wolf, Colahan, Costello, Warwick, Ambrose, & Giardino, 1998).
5. Findings from Evaluation Question # 5: What were the students’ post-training experiences with
applying their knowledge?
1. Students Application of SAFE Skills with Post-training Patients. For those who had the
opportunity to work with sexual assault patients, we also asked them to describe how they approached and
interacted with their post-training patients. The students described treating their patients in a
compassionate manner, which involved treating them with respect and dignity, showing empathy instead of
judgment or blame, and building rapport and trust. Students also described empowering their patients by
explaining the exam process and offering them choices throughout their interactions. The qualitative
interviews also sought to understand how students applied their medical forensic knowledge and skills in
their practice with sexual assault patients following the training. We inquired if the students had received
feedback from an experienced colleague or supervisor on their documentation with post-training sexual
assault patients. We found that feedback about documentation was uncommon. Several students noted
that they did not have trained SAFEs in their institutions to provide feedback. Still, these students did seek
feedback from non-SAFE clinicians, and most received brief positive remarks. Only a small number of
students were provided with feedback from trained SAFEs who indicated that the students’ documentation
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

137
was of high quality and, for the most part, met their institutions’ expectations. Feedback is essential for
students to grow their skills. Therefore, we recommend that students receive post-training mentoring and
support if they do not have an available SAFE-trained preceptor (see page 149 for specific
recommendations on mentoring). In addition, we reiterate our earlier recommendation of incorporating
homework into the online documentation module so students can advance their documentation skills.
2. What Challenges did Students Experience after the Training? Overall, the students were
satisfied with the training and found the clinical training incredibly impactful. However, some of the students
encountered challenges following the training, which often were linked to delays in practice, their prior
clinical experiences, and/or community types. For instance, 44% of the interviewed students were still
waiting to examine their first patient or had examined only a couple of patients because they either worked
in institutions with low patient volumes or they were starting new programs. This delay in practice posed
challenges for some students with maintaining confidence and retaining their knowledge and skills.
Similar to most SAFE trainings, the students in the IAFN training included clinicians with a range of
experiences and clinical backgrounds (e.g., emergency medicine, midwifery, gynecology), and these
differences created diverse learning needs. The IAFN SAFE training also drew students from multiple types
of communities (e.g., rural, urban), which posed a unique challenge of training students with community-
specific needs, such as working in institutions that do not have SAFE-trained clinicians to serve as
preceptors or that have a low volume of patients. Below, we will identify when the students’ challenges
were linked to delayed practice, prior clinical experience and background, and/or their type of community.
a) Patient interactions. Interacting with patients and taking a patient history are important
components of healthcare but require complex skills, including strong questioning techniques, the ability to
translate medical terminology into lay terms for patients, and developing non-verbal communication
(McKenna, Innes, French, Streitberg, & Gilmour, 2011). History taking for SAFE practice can be
challenging because it is more detailed and requires engaging traumatized patients in longer dialogue than
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
138
the typical patient. As one instructor noted, “you cannot fake rapport” when you are a SAFE because you
spend a long time with the patient. Thus, it is not surprising that some students experienced challenges
with this important component of SAFE practice. In particular, these students were afraid of re-traumatizing
patients by saying something that might offend them.
Students made several suggestions for the clinical training that might help bolster their confidence
with patient interaction skills. For example, they wanted to understand how one asks indelicate questions
during the history taking. These students also desired more understanding of how to start the conversation
with patients during the initial point of contact. As such, these students indicated that they would have
benefitted from additional opportunities during the training to practice the initial conversation with the GTAs,
as well as taking a patient history. The students who felt less confident in these interpersonal skills included
those who have had few or no sexual assault patients. As prior studies have suggested, confidence is
primarily acquired in the clinical setting as they experience success with their patients (Lundberg, 2008;
Weaver, 2011). In addition, students who do not have experience in emergency medicine expressed feeling
less confident with interacting with sexual assault patients. It may be possible that students who have
experience in emergency medicine are used to working with patients experiencing an acute crisis or trauma
and thus, interacting with sexual assault patients does not feel intimidating.
Students who have had patients indicated that they had different types of learning needs than
those students who have not had patients. Some of these students wanted the training content and clinical
scenarios to be expanded to additional populations, such as patients with disabilities. In particular, they
wanted to understand and practice how to empower and obtain consent from patients with disabilities
appropriately. Some students also wanted a male GTA at the clinical training because they believed that
male sexual assault patients might respond to or interact with SAFEs differently than female patients. Some
students suggested that during the training the GTAs role-play more challenging situations such as patients
with a flat affect or exhibiting strong emotions like anger or heavy sobbing. This would have allowed
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
139
students to practice responding to patients with a range of emotional reactions. Additionally, GTAs would
often break character during the role plays in order to provide feedback. A few students would have
preferred the GTAs stay in character while the students were practicing.
When considering the aforementioned students’ recommendations, we believe it is important to
consider the core differences between students who have and have not had opportunities to practice.
Students who have had no or few patients struggled with less confidence about their ability to interact with
patients. Although these students have healthcare experience, a new role can induce feelings of anxiety
and being overwhelmed, but these feelings often dissipate when clinical experience occurs in this new role
(Neal-Boylan, 2006). The anxiety leading up to and during that first exam can be overwhelming. SAFEs
tend to gain confidence after they have completed their first exam because they have the opportunity to
work through their anxiety. In addition, receiving positive feedback from the patient or a preceptor builds
confidence (Seng, Sanubol, & Johnson County SANE Team, 2004). Although additional practice during the
training might bolster their confidence, acquiring practice with patients likely will mitigate their anxiety as it
has appeared to do so for the SAFE students who have had patients. In contrast, the students who have
had patients post-training recommended more advanced topics such as working with a patient with strong
emotional reactions. This raises the question of whether these students would have been ready to learn
about these advanced topics prior to working with sexual assault patients. When considering that those
without patients recommended additional practice of the core content (e.g., history taking), it is likely that
some students may not be ready for advanced practice opportunities. We offer additional recommendations
on how to address these diverse needs at the end of this discussion section.
Students from rural programs also had an additional need specific to the unique context of rural
healthcare that they wished had been addressed more in-depth. Specifically, students gained a strong
understanding of the sensitive nature of sexual violence, which raised concern that survivors in their
community would not seek help. Survivors in rural areas do have unique barriers to accessing services
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
140
(Eastman & Grant-Bunch, 2007). Pressure to remain silent prevents rural survivors from seeking help
because they fear their community and family reactions. These survivors often worry that service providers
will gossip about their assault if they seek help, which would lead to their community becoming aware of
their victimization. This fear makes it difficult for survivors to trust service providers enough to disclose
(Logan, Evans, Stevens, & Jordan, 2005). Given this concern, the rural students wanted the training to
cover how to address this problem. In addition, the students noted that they were more likely to know their
patients personally, and wanted to hear from those working in rural programs about how to address
confidentiality with sexual assault patients in a manner that would mitigate the patients’ concerns.
Furthermore, rural communities have fewer social service agencies in the community, but healthcare
providers also lack adequate training on how to address the emotional needs of their patients (Allen, 2012).
Some of the students from the rural programs noted that they do not have advocacy programs and thus,
they believed additional training was necessary to guide them on how to address their patients’ emotional
needs in the absence of advocacy services.
These findings suggest that the IAFN training needs to provide additional information to meet the
unique needs of students from rural programs. We recommend that Module I (dynamics) or Module IV
(History) include an elective subsection that provides information about how to address the unique barriers
of survivors in rural communities with accessing services, as well as how to address confidentiality with
sexual assault patients. Furthermore, we believe that students from rural programs could benefit from slight
modifications to the scenarios utilized during the clinical training. In particular, the scenarios enacted by the
GTAs could be changed to include situations specific to rural programs. For example, the scenario of the
adolescent patient could be modified for the rural students to be an adolescent patient who lives in close
proximity of the SAFE clinician. This would allow the rural students to practice addressing these region-
specific issues surrounding confidentiality. In addition, the students from rural programs who do not have
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
141
advocacy may benefit from extended practice on how to meet their patients’ emotional needs within the
scope of SAFE practice.
b) Medical forensic exam. Although many students entered the training with anxiety about
conducting pelvic exams with speculums, only a few students noted that they would have wanted more
practice of speculum insertion. This might suggest that the majority of students have gained confidence in
their skills with conducting pelvic exams. Although it is important to note that some students from rural
communities reported that their hospitals do not have pelvic beds (i.e., beds with stirrups), which made it
more challenging to conduct the exams because the training used pelvic beds. We recommended that the
clinical training include a discussion of how to conduct the exam using a regular patient bed without
compromising the quality of the evidence collection but still promoting patient comfort. Furthermore, we
suggest that students who do not have pelvic beds in their home institutions practice the exam without the
stirrups. Although practicing pelvic exams without stirrups may require extended practice time, these
students will be more prepared to conduct pelvic exams with the equipment constraints that they will
encounter in their home institutions (McGaghie, Issenberg, Petrusa, & Scalese, 2010).
In terms of the medical forensic aspects of the exam, some students felt less confident with the
quality of their evidence collection and documentation skills. These students were primarily those who have
not received feedback about the quality of their exam or documentation because they do not have a
preceptor. These students worried that they were not collecting evidence accurately and needed a SAFE to
help them determine whether their injury assessment was thorough and accurate. Some students were
also worried about documenting the MFE accurately and lacked confidence in their knowledge of medical
terminology and anatomy. In addition, those who experienced delayed practice also felt less confident
about conducting the MFE exam. While they believed that they would be able to recall the information
learned in the training, they were concerned that they were losing the nuanced details of conducting the
exam. The students who lacked confidence in their MFE exam skills recommended that the training provide
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
142
more opportunities to practice evidence collection, such as swabbing, documenting, and preserving
evidence (e.g., bagging, sealing, & labeling). Students also wanted more practice on assessing injuries with
and without equipment (e.g., colposcope) and techniques (e.g., Foley catheter). In addition, students
wanted to practice taking photographs of injuries on GTAs, as well as the manikin.
While the students recommended additional practice during the training, it appears that the
absence of feedback from SAFE-trained preceptors in their institutions has been a challenge. In fact,
approximately half of the interviewed students -- primarily those in rural and low-volume institutions --
indicated that they did not have preceptors. This shortage of preceptors can be common in rural institutions
(Allen, 2012; Macleod, Misner, Banks, Morton, Vogt, & Bentham, 2008). However, feedback is critical for
new SAFEs because it helps the clinician have a clear understanding of their clinical strengths and learning
needs (Boehm & Bonnel, 2010). This indicates that new SAFEs need supports that extend beyond the
training. Although trainings typically provide learning activities within a bounded time frame, we suggest
that IAFN consider providing post-training learning or mentoring activities to support the post-training skill
development of students without SAFE-trained preceptors (see pages 149-150 for specific
recommendations).
c) Sexual assault evidence kits. The difference in the quality of the sexual assault kits across the
country has both implications for the training and implications that extend beyond the training. IAFN staff
were aware of the variation among the state kits, but it was not until students brought their kits to the
clinical training that they realized how outdated some kits had become. Kits with outdated practices can
impact the quality of evidence collection and subsequently the prosecution of cases, as well as pose health
risks to some patients (e.g., flossing teeth routinely without assessing for the risk of HIV exposure)
(Department of Justice, 2013). Therefore, we recommend that IAFN propose a national initiative to update
and create more uniformity of the kits across the country.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

143
The differences among the kits also posed challenges for the instructors and students because it
was confusing for each student to use their own kits. Because some of the kits were outdated, the
instructors had to help students understand what is considered current and outdated practices. Although
the students found this helpful, these discussions reduced the time allotted to practice. In order to make the
process run smoother, the instructors primarily used the Colorado kit for the skill stations. While this
reduced confusion during the skill stations, the students who learned to practice with the Colorado kit had
to transition back to their kits when they returned to their institutions, which they found challenging. In order
for students to transfer their newly acquired skills from the clinical training to their SAFE programs, we
recommend that the clinical training conditions (e.g., kit) be as similar to the students’ institutions as
possible (Healy, Wohldmann, Parker, & Bourne, 2005; McGaghie, Issenberg, Petrusa, & Scalese, 2010).
The students also recommended that the instructors guide them as they practiced the exam with
their state kits. Becoming familiar with their own kits can help students develop a routine, which may reduce
the likelihood of missing evidence or overlooking key information (Seng, Sanubol, & Johnson County SANE
Team, 2004). In order for this recommendation to be followed, the instructors indicated that they would
need more understanding of the differences among all of the state kits to feel more prepared. In addition,
we believe that the students should be familiar with their state kits prior to the clinical training. Thus, we
suggest that students receive a homework assignment in which they explore their kits prior to the clinical
training. This might occur with a module to inform them of the common kit contents, of kit contents that
might be considered outdated, and an explanation of why some practices are considered current while
others are deemed outdated. This homework might free up time in the clinical training for students to
engage in additional practice. However, some students had difficulty accessing their kits, so we
recommend that IAFN provide them with specific instructions on how to access a kit.
6. Evaluator Guidance for Incorporating Recommendations:
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
144
As noted earlier, there was a varied set of recommendations from students, which appears linked
to their clinical backgrounds, post-training challenges, and community types. Because of the diverse needs
of the students, it might be difficult to incorporate all of the recommendations within a two-day clinical
training and continue to meet the core needs of every student. For example, students without patients
would have liked additional practice of the core content, while those with experience would have liked more
advanced practice scenarios. By adding additional practice time of the core content, there would not be
time for students to practice advanced scenarios. On the other hand, students who wanted additional
practice of the core content may not be ready to practice advanced scenarios. Therefore, incorporating one
group’s recommendations may have less benefit for another group. While there is not a clear solution, we
offer a number of options for consideration when making changes that would occur before, during, and after
the clinical training to satisfy the learning needs of the majority of students.
a) Prior to training. The most frequent recommendation by students was to provide additional
practice opportunities. To maximize the time allotted to practice, some activities may need to occur prior to
the training (Lehmann, Bosse, & Huwendiek, 2010). For example, many students entered the clinical
training with many questions based on the content that they learned from the online modules, which
reduced hands-on practice time. Therefore, we recommend that the project director provide a phone
discussion prior to the clinical training to address some of these questions. Because of the students’ varied
schedules, more than one discussion session may need to be offered. An alternative option would be for
students to submit their questions, and the answers could be provided through a podcast or asynchronous
webinar. In either case, the goal is to address as many of the students’ questions prior to the training to free
up time for practicing.
We also suggest that students receive homework during multiple modules that allows them to
practice some components of SAFE practice. We believe that future students would be receptive to
homework because many of the students in the current study indicated that it would have been helpful to
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
145
their development, especially if they had received feedback. Some students suggested having a mock
patient case where they would hear a SAFE conducting a history taking so they could practice documenting
the patient narrative. This assignment could also provide pictures that would allow them to document
injuries on a body diagram. We also suggest including homework that focuses on patient interactions in
which students could choose among multiple case studies that ask students how they would handle
patients presenting with different emotional reactions (e.g., flat affect, anger displayed towards the
provider). Some of these case scenarios could be unique to the students’ type of community, such as a
SAFE in a rural program who knows the patient. By encouraging students to choose the case studies that
best reflect a situation that they would most likely encounter, the homework would be more relevant,
engaging, and beneficial to their learning (Means, Toyama, Murphy, Bakia, & Jones, 2010; Zhang, Zhou,
Briggs, & Nunamaker, 2006). Further, these homework assignments may help the students feel more
prepared prior to entering the clinical training so they will feel ready to begin practicing quicker.
Although these activities may help students feel more prepared, they would require more of a time
commitment, which may be a challenge for students with more external barriers (e.g., work and family
responsibilities). In addition, students’ needs may vary with these learning activities. For example,
inexperienced students would benefit from homework where they practice identifying anatomical structures.
However, this assignment may have less benefit for students who perform frequent pelvic exams in their
current practice, such as gynecologists and midwives. Thus, we recommend that students in future
trainings have some control of choosing which supplemental learning activities to complete so their unique
learning needs can be met (Means, Toyama, Murphy, Bakia, & Jones, 2010; Zhang, Zhou, Briggs, &
Nunamaker, 2006). Students may experience even more engagement and success if they choose the
learning activities that are most meaningful to their development (Johnston, 2007).
Preparing the instructors also might help save time during the clinical training. The majority of
instructors noted that they had not seen the online modules, which made it difficult for some to determine
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
146
what content would need to be introduced or just reinforced. Some of the instructors were offered the
chance to view the online modules, but they did not due to time constraints. One possible solution is to
provide the instructors with a curriculum outline for each module that details the module content and
learning objectives. This may provide them with a stronger sense of what the content covered in the online
modules. Still, the instructors should be strongly encouraged or required to review the modules to prepare
them for the clinical training.
b) During the training. The instructors were concerned that each instructor’s nuanced approach to
the training may have been confusing because students asked many questions during the skill stations
about the differences among the instructors. In particular, the instructors believed that the nuanced
approaches may have been particularly confusing for the students with less nursing experience in general,
as well as those new to conducting pelvic exams. When clinicians are in the beginning stages of learning a
new role, they rely on basic principles, and they have less tolerance for nuances and variations of rules
(Benner, 2001). Still, students observing multiple clinicians who have slightly different approaches can
contribute to their understanding that there are many correct ways to approach the exam and clinical
decisions (Jeffries, 2005; Lewenson & Truglio-Londrigan, 2008). Therefore, we do not recommend that the
instructors try to have one single approach during the entire training, especially because the students will
be working in their institutions with other SAFEs who will have their own unique approaches. Instead, we
endorse the instructors’ recommendation that the students observe one instructor demonstrate one exact
process of the entire exam (e.g., from greeting to discharging the patient) before entering the skill stations.
This would allow the students to see the exam process, understand the rationale, and help them
understand the standards that they should apply to their own exams. We also propose an additional
solution of having an exact process demonstrated in an online module. This could consist of a SAFE
interacting and taking a patient history with a GTA, and then performing the exam on a manikin. Some
students noted that the exam process was not fully understood until they participated in the clinical training.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
147
By placing this demonstration online, students might gain a deeper understanding of the entire exam
process earlier, and this would save time that could be allotted to more practice. In addition, students would
be informed that each SAFE has a nuanced approach to the exam so they are not confused when they see
a different approach during the clinical training. This process may reduce confusion among the students
and subsequently, reduce the number of questions about these differences.
Another solution for maximizing practice time rests with the instructors’ teaching styles. It is
common for students who lack confidence to defer practice opportunities to other students or ask many
questions to delay practice (Lundberg, 2008). Therefore, these students need an assertive instructor to
encourage and direct them to engage in the practice activity. While most of the instructors guided students
into practice in a timely manner, a few instructors spent most of the skill station time answering the
students’ questions. We recommend that the project director have a pre-clinical training orientation to
provide the instructors with clear expectations of their role, as well as guidance about how to encourage
anxious students to practice. By moving all of the students into practicing quicker, the students are more
likely to receive additional practice time. By maximizing the practice time of the core content, students may
feel ready for an advanced scenario during the final skill station.
Students acquire competency through repeated practice of new skills (Kneebone, Scott, Darzi, &
Horrocks, 2004). However, the type of clinical skills that need practice varies depending on the students’
clinical backgrounds. Students who have competency with conducting pelvic exams and speculum insertion
would benefit from moving quickly into the medical forensic component of the exam. Furthermore,
experienced clinicians often exhibit higher levels of critical thinking and decision-making skills and thus,
they may need less time to understand the rationale of the MFE exam components (Fero, Witsberger,
Wesmiller, Zullo, & Hoffman, 2009; Hatcher et al., 2006). As such, we recommend that experienced
students receive more advanced scenarios once they have practiced the core MFE exam skills (Parker &
Myrick, 2010). We also suggest gradually increasing the complexity of the scenarios to help experienced
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
148
students remain engaged and advance their skills (van Gog, Sluijsmans, Brinke, & Prins, 2010). On the
other hand, we recommend that inexperienced students’ practice time focus on the basics of pelvic exams,
the components of the MFE exam, and patient care.
We propose two potential solutions for the training to meet both groups of students’ needs while
creating an efficient learning environment. One solution is to schedule some training sessions specifically
for experienced students, which would allow them to practice more complex situations during most of the
clinical training (Kneebone, Scott, Darzi, & Horrocks, 2004). Another solution is to continue with the current
training structure; placing the advanced students together into the small groups, but prepare the GTAs to
play out their assigned scenario with multiple layers of complexity. For example, one of the scenarios
involved the GTA playing an adolescent patient. The inexperienced students would be provided with a
basic scenario with the GTA playing the adolescent as cooperative and without complex issues. The
experienced students could be provided with an advanced scenario involving the GTA playing an angry
adolescent who is uncertain about consenting to the exam. In this latter solution, the inexperienced
students could advance to more complex scenarios when they are ready.
c) Post-training. Some students reported that they needed support following the training,
particularly those who experienced a delay with practicing and those who do not have SAFE-trained
preceptors. Students who experienced delays in practice were concerned about knowledge retention,
especially around the details of the exam. We recommend that the IAFN create an online refresher module
or allow access to the modules for an extended period of time. A few students suggested having a quiz that
provides immediate scoring so they could assess their knowledge and help them maintain confidence in
their skill set. This type of follow-up training has been found to be effective with reinforcing recently attained
knowledge (Bell et al, 2008). Although an online refresher module would benefit those who are still waiting
for their first patient, we also believe that SAFEs in low-patient volume institutions may benefit from these
post-training reinforcement activities as well.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
149
Clinicians new to SAFE practice require more support and supervision as they achieve
competency (Benner, 2001). However, approximately half of the interviewed students did not have a SAFE-
trained preceptor, supervisor, or colleague to provide this support and supervision. Thus, it is unsurprising
that these students recommended that IAFN provide post-training supports such as an assessment of their
work (e.g., documentation review), and having an instructor contact them to offer guidance and support.
While these requests are beyond the scope of the training, the IAFN has provided post-training support
when feasible. The lack of SAFE-trained preceptors raises the concern that many SAFEs may be working
in isolation, which could have negative effects on their knowledge retention and confidence (Boswell,
Lowry, & Wilhoit, 2004). Further, these clinicians may be more prone to burnout and turnover (Allen, 2012;
Laschinger et al. 2001; Roberge, 2009). To mitigate these effects of professional isolation, we recommend
that IAFN consider implementing a post-training mentoring program for new SAFEs without SAFE-trained
preceptors, supervisors, or colleagues.
Professional mentoring entails an experienced clinician fostering a supportive relationship and
offering guidance to a clinician who is trying to achieve a higher level of competence (Marrelli, 2004).
Mentors can serve as sounding boards, assist with problem solving, and provide feedback on challenging
cases (Mills, Francis, & Bonner, 2008). Although mentoring typically occurs by pairing an experienced
clinician with a new clinician, this type of mentoring may be cost prohibitive. Thus, we suggest the more
feasible solution of an experienced clinician mentoring a small group of SAFEs rather than individual
mentoring. While mentoring often focuses on support and professional learning (Macleod, Misner, Banks,
Morton, Vogt, & Bentham, 2008), it also could be useful for students who are starting a new SAFE program.
For example, an experienced SAFE could provide guidance about the challenges of implementing such a
program. Mentoring has been found to promote job satisfaction and career commitment while reducing
feelings of isolation for the new clinician and subsequently improving the quality of care for patients
(Harrington, 2011). Furthermore, mentors often benefit from the experience as they gain new insights from
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

150
the mentoring experience. These activities also may reduce isolation and prevent burnout (Maslach &
Leiter, 2008), and subsequently reduce the problem of SAFE shortage.
B. Project Strengths, Limitations, and Implications for Future Research
The purpose of this project was to develop and evaluate a comprehensive sexual assault medical-
forensic examination training program that would reduce students’ barriers to accessing and completing
SAFE training. IAFN designed a standardized comprehensive curriculum with the guidance of nationally
recognized experts from the fields of advocacy, law enforcement, prosecution, medicine and criminalistics
(forensic science). Further, they were successful with increasing healthcare clinicians’ access to SAFE
training, especially those from communities who have had limited access to SAFE training historically.
The goal of the evaluation study was to examine if a blended learning modality effectively produces
the essential competencies for clinicians to provide high quality sexual assault patient care. There is a
dearth of literature examining the impact of SAFE trainings on the clinicians’ knowledge and skills. Thus,
this project provided the first comprehensive examination of SAFE training effectiveness. Comparing the
effectiveness of the IAFN-blended SAFE training to existing classroom trainings was not feasible because
many types of SAFE trainings exist across the country with some nurses being trained by national experts
and some by local nurses. It would not have been possible to account for all of the variation in the training
content and delivery methods for a comparison group. Thus, we used several strategies in combination to
determine the effectiveness of the IAFN SAFE training.
In our quantitative components, we used a survey design to gather data about the students prior to
the training so we could understand who would end up completing or dropping out of the training. This
study also used a one-group pre-test/post-test design to assess the participant’s knowledge prior to each
training module and afterward. This design provided the most rigorous research design without a
comparison group. A follow-up exam was also utilized to assess whether students retained their
knowledge. Together, the quantitative components of this study provided the first comprehensive
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
151
assessment of the effectiveness of the SAFE training. The clinical component of the IAFN training is a
unique feature of the training as most SAFE trainings utilize didactic instructional methods. Thus, we added
qualitative data to gain a deeper understanding of the clinical component of the training from the
perspectives of the clinical instructors and students who completed the training. These data allowed us to
understand both the process and outcomes of the clinical training, as well as the students’ experiences
following the training. Together, we have been able to provide a broader understanding of what factors
contributed to students’ success, and how SAFE trainings can address the variety of learning needs among
its diverse student population.
Despite these strengths, there are several limitations of the project that merit examination. First,
this study did not have a comparison group of students (e.g., those who attended a traditional SAFE
training) to examine the unique contributions of the blended learning approach on increasing students’
knowledge. Therefore, there may be other factors related to knowledge attainment and retention not
accounted for in this study. We were able to control for some potential validity issues, including if the
students were exposed to SAFE content not provided by the IAFN training. Still, there may have been other
threats to internal validity that may have not been assessed, such as workplace factors that may have
inhibited or promoted knowledge attainment or retention. However, it may be difficult to design an “ideal”
study that can adequately address these limitations because standardization of SANE/SAFE curricula does
not exist. What is taught in one educational program may be unrelated, or worse, antithetical to what is
taught in another. Thus, comparative studies would have to compare two different curricula using the same
instructional methods, or compare two different instructional methods using the same curricula. For
example, a future study could compare knowledge retention of students who participated in the IAFN online
didactic training to students who participate in the online didactic and clinical components the IAFN SAFE
training to understand the unique contributions of each component with knowledge retention. Alternatively,
a future study could compare knowledge retention of students who participated in a traditional classroom to
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
152
students who participate in the online didactic, with both trainings incorporating the IAFN curriculum and
clinical component.
Second, the variables utilized in the quantitative models all accounted for a small percentage of the
variance. It appears that other factors beyond the scope of this study played a role in the students’
knowledge and retention. For example, the students’ self-efficacy, time management skills, and their ability
to self-pace through the online modules may influence knowledge attainment but were not included in this
study (Angelino, Williams, & Natvig, 2007;Sitzmann, 2010). Additionally, the bivariate analysis for
knowledge retention showed that those students who participated in Course 1 had higher knowledge
retention, although this was not significant in the multivariate analysis. A closer examination of the students
who attended these three courses did not show significant differences among the students. Thus, it is likely
that other factors beyond this study played a role in Course 1 students’ higher levels of retention. For
example, Course 1 students were able to participate in the training soon after the application process while
the students from other courses had to wait. Students and instructors may have had more enthusiasm
during Course 1 because they were participating in the first national IAFN course. Together, this
enthusiasm may have played a role in knowledge retention in ways that were not captured in this study.
Finally, the findings of this study may only be generalized to students who attend a blended
training, and taught by instructors with a high level of SAFE and teaching expertise. The students who were
interviewed indicated that the clinical component of the training clarified, reinforced, and expanded the
knowledge learned in the online didactic training. Thus, if future students do not attend the clinical
component, their knowledge retention rates may not be as high as those who do. In addition, this training
was free to students, which may have played a role in the students’ attrition, knowledge attainment, and
knowledge retention rates. It may be possible that students would be less likely to drop out of the training if
they or their institutions were charged. Furthermore, students’ knowledge attainment and retention rates
might differ if the students or institutions had to financially invest in the students’ development. In addition,
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
153
because the goal of the training was to increase access to training for those working in rural areas,
applicants from major metropolitan urban areas were excluded because they have more accessibility to
SAFE training in their regions. Therefore, the findings cannot suggest whether the IAFN SAFE training
would be effective with preparing SAFEs to work in major metropolitan urban communities.
Future research on the effectiveness of SAFE training can advance these findings by addressing
these limitations. In addition, future research can build upon the findings of this project. The current study
found that some students fared better than others with completing the course, and attaining and retaining
knowledge. For example, students from rural communities were more likely to complete the training, but
they had unique challenges when they returned to their institutions to practice as SAFEs. In particular, the
students from rural communities were more likely to experience a delay in practice. Although our study did
not find a significant difference in knowledge retention between rural and urban/suburban students around
the three month post-training timeframe, it would be informative to examine knowledge retention for a
longer period of time to understand if these students can retain their knowledge when they experience
longer delays in practice. Furthermore, it would be helpful to understand what promotes or impedes their
knowledge retention when students experience long practice delays. In addition, our qualitative interviews
with the students raised the concern of the limited number of SAFE-trained preceptors in rural communities,
which means that many new SAFEs have to practice in geographic isolation. Given these challenges,
additional research is needed to understand the longer-term needs of new SAFEs from rural communities
with maintaining their competencies, as well as with practicing in isolation.
There also appears to be different learning needs for students across the lifespan of their
healthcare careers. Students with less healthcare experience retained less knowledge than those with
experience. Further, they reported more challenges when they began practicing, particularly with feeling
confident. These differences merit additional investigation. What strategies might be effective for enhancing
their knowledge retention?
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

154
Furthermore, there is limited research that examines what helps students transfer their knowledge
and skills into their work setting (Weaver, 2011). What helped students maintain their knowledge? Was the
opportunity to provide patient care the driving factor for knowledge retention or did other factors play a role?
Do preceptors play a role with promoting or impeding knowledge retention and if so, how? Alternatively, it
would be helpful to understand the conditions that contribute to knowledge loss and whether there are
strategies to prevent that loss.
Finally, this project raised concerns about the variations of sexual assault evidence kits across the
country, including outdated practices. In part, these variations may be a result of limited research to guide
our understanding of the best evidentiary practices for victims’ well-being and the prosecution of sexual
assault cases. Additional research is sorely needed to understand what medical forensic evidence
practices lead to the best victim, evidentiary, and prosecution outcomes. For instance, how do these
differences among the kits differentially impact case decision-making by prosecutors, judges, or jurors?
How do these variations among kit documentation forms differentially influence how crime laboratories
analyze the kits? Which contents of the kits are considered too invasive by victims? Together, answering
these research questions can provide states with the knowledge to make informed decisions to improve
their sexual assault kits.
C. Conclusion
In conclusion, the evaluation identified many successes of the training. The majority of students
completed the training and exhibited high knowledge gains in several of the online modules, specifically
those focusing on forensic science, ethics, and self-care; photography; medical forensic history and
physical; evidence collection; anogenital exam; and the justice system and testifying. Further, students
experienced a fairly high level of knowledge retention in comparison to the rates reported in prior research.
Many students in the qualitative interviews indicated that the clinical training helped clarify, broaden, or
solidify the content covered in the online modules. However, the evaluation identified many challenges and
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
155
recommendations. Students experienced lower knowledge gains in multiple online modules including those
pertaining to medical management, documentation, program and operational issues, and patient-centered,
coordinated team approach. Several students indicated that these lengthy modules could be improved by
breaking them into subsections. Finally, the evaluation identified distinct learning needs of students with
less healthcare experience and from rural communities, which will require some modifications to the
training. For example, these students believed that additional practice time during the clinical training, as
well as post-training supports (e.g., refresher training) would have helped them feel more prepared to
practice as SAFEs. Overall, the IAFN developed a comprehensive SAFE training curriculum that offers a
strong foundation that can be built upon to meet the diverse learning needs of clinicians across the country.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

156
VIII. References
Alexander, J., Polyakova-Norwood, V., Johnson, L., Christensen, P., & Loquist, R. (2010). Collaborative
development and evaluation of an online nursing course. Distance Education, 24(1), 41-56.
Allen, J. C. (2012). Field training for rural public health nurses. Public Health Nursing Cambridge, 29(5),
473-477.
Allen, I.E., & Seaman, J. (2010). Class differences: Online education in the United States, 2010. Retrieved
from The Sloan Consortium website:
http://sloanconsortium.org/sites/default/files/class_differences.pdf
Al-Qahtani, A. Y. & Higgins, S. E. (2013). Effects of traditional, blended and e-learning on students'
achievement in higher education. Journal of Computer Assisted Learning, 29(3), 220-234.
American Association of Colleges of Nursing (2010). The future of higher education in nursing: 2010 annual
report. Washington, DC: Author. Retrieved from http://www.aacn.nche.edu/publications/annual-
reports/ar2010.pdf
Angelino, L. M., Williams, F. K., & Natvig, D. (2007). Strategies to engage online students and reduce
attrition rates. The Journal of Educators Online, 4(2), 1-14.
Atack, L. (2003). Becoming a web-based learner: Registered nurses' experiences. Journal of Advanced
Nursing, 44(3), 289-297.
Atack, L., & Rankin, J. A. (2001). A descriptive study of registered nurses' experiences with web-based
learning. Journal of Advanced Nursing, 40(4), 457-465.
Atack , L., Rankin, J. A., & Then , K. L. (2005). Effectiveness of a 6-week online course in the Canadian
triage and acuity scale for emergency nurses. Journal of Emergency Nursing, 31(5), 436-441.
Baernholdt, M. & Mark, B. A. (2009). The nurse work environment, job satisfaction and turnover rates in
rural and urban nursing units. Journal of Nursing Management, 17(8), 994-1001.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

157
Baillie, L. & Curzio, J. (2009). Students’ and facilitators’ perceptions of simulation in practice learning.
Nurse Education in Practice, 9(5), 297-306.
Bandla, H., Franco, R. A., Simpson, D., Brennan, K., McKanry, J., & Bragg, D. (2012). Assessing learning
outcomes and cost effectiveness of an online sleep curriculum for medical students. Journal of
Clinical Sleep Medicine 8(4), 439-443.
Baptista-Nunes, M., McPherson, M., 2002. No lectures on campus: can e-learning provide a better learning
experience? In: Proceedings of the Second IEEE International Conference on Advanced Learning
Technologies (ICALT’03) IEEE Computer Society, Available from:
<http://lttf.ieee.org/icalt2002/proceedings/t1404_icalt124_End.pdf>, pp. 442–447.
Bell, D. S., Harless, C. E., Higa, J. K., Bjork, E. L., Bjork, R. A., Bazargan, M., & Mangione, C. M. (2008).
Knowledge retention after an online tutorial: A randomized educational experiment among resident
physicians. Journal of General Internal Medicine, 23(8), 1164-1171.
Bello, G., Pennisi, M., Maviglia, R., Maggiore, S., Bocci, M., Montini, L., & Antonelli, M. (2005). Online vs.
live methods for teaching difficult airway management to anesthesiology residents. Intensive Care
Medicine, 31(4), 547-552.
Benner, P. E. (2001). From novice to expert: Excellence and power in clinical nursing practice. Upper
Saddle River, N.J: Prentice Hall.
Bloom, K. C. & Hough, M. C. (2003). Student satisfaction with technology-enhanced learning. Computers,
Informatics, Nursing, 21(5), 241-246.
Boehm, H., & Bonnel, W. (2010). The use of peer review in nursing education and clinical practice. Journal
for Nurses in Professional Development, 26(3), 108-115.
Bolin, T., Peck, D., Moore, C., & Ward-Smith, P. (2011). Competency and educational requirements:
Perspective of the rural emergency nurse. Journal of Emergency Nursing, 37(1), 96-99.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

158
Boswell, S., Lowry, L. W., & Wilhoit, K. (2004). New nurses' perceptions of nursing practice and quality
patient care. Journal of Nursing Care Quality, 19(1), 76-81.
Bradley, C., Erice, M., Halfer, D., Jordan, K., Lebaugh, D., Opperman, C, & Stephen, J. (2007). The impact
of a blended learning approach on instructor and learner satisfaction with preceptor
education. Journal for Nurses in Professional Development, 23(4), 164-170.
Buckley, K. M. (2003). Evaluation of classroom-based, web-enhanced, and web-based distance learning
nutrition courses for undergraduate nursing. The Journal of nursing education, 42(8), 367.
Bureau of Justice (2007). Criminal victimization, 2006. NCJ Document No: 219413. Washington, DC:
Author Retrieved from: http://bjsdata.ojp.usdoj.gov/content/pub/pdf/cv06.pdf
Cabral, G., Campbell, R., & Patterson, D. (2011). Adult sexual assault survivors’ experiences with sexual
assault nurse examiners (SANEs). Journal of Interpersonal Violence, 26(18), 3618-3639.
Campbell, R. (1998). The community response to rape: Victims' experiences with the legal, medical, and
mental health systems. American Journal of Community Psychology, 26(3), 355-379.
Campbell, R. (2008). The psychological impact of rape victims. American Psychologist, 63(8), 702-717.
Campbell, R. (2005). What really happened? A validation study of rape survivors' help-seeking experiences
with the legal and medical systems. Violence and Victims, 20(1), 55-68.
Campbell, R. & Bybee, D. (1997). Emergency medical services for rape victims: Detecting the cracks in
service delivery. Women’s Health, 3(2), 75-101.
Campbell, R., Bybee, D., Ford, J. K., Patterson, D., & Ferrell, J. (2009). A systems change analysis of
SANE programs: Identifying mediating mechanisms of criminal justice system impact. Washington,
DC: National Institute of Justice.
Campbell, R., Greeson, M., & Patterson, D. (2011). Defining the boundaries: How sexual assault nurse
examiners (SANEs) balance patient care and law enforcement collaboration. Journal of Forensic
Nursing, 7(1), 17-26.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
159
Campbell, R. & Martin, P. Y. (2001). Services for sexual assault survivors: The role of rape crisis centers.
Renzetti, C. M., Edleson, J. L, & Bergen, R. K. (Ed.). Sourcebook on Violence against Women (pp.
223-242). Thousand Oaks, CA: Sage Publications, Inc.
Campbell, R., Patterson, D., Adams, A. E., Diegel, R., Coats, S. (2008). A participatory evaluation project to
measure SANE nursing practice and adult sexual assault patients’ psychological well-being.
Journal of Forensic Nursing, 4(1), 19-28.
Campbell, R., Patterson, D., & Bybee, D. (2012). Prosecution of adult sexual assault cases: A longitudinal
analysis of the impact of a sexual assault nurse examiner program. Violence against Women,
18(2), 223-244.
Campbell, R., Patterson, D., Bybee, D., & Dworkin, E. R. (2009). Predicting sexual assault prosecution
outcomes: The role of medical forensic evidence collected by sexual assault nurse examiners.
Criminal Justice and Behavior, 36(7), 712-727.
Campbell, R., Patterson, D., Cabral, G. (2010). Using ecological theory to evaluate the effectiveness of an
indigenous community intervention: A study of sexual assault nurse examiner (SANE) programs.
American Journal of Community Psychology, 46(3-4), 263-276.
Campbell, R., Patterson, D., Lichty, L. F. (2005). The effectiveness of sexual assault nurse examiner
(SANE) programs: A review of psychological, medical, legal, and community outcomes. Trauma,
Violence, and Abuse, 6(4), 313-329.
Campbell, R. & Raja, S. (1999). Secondary victimization of rape victims: Insights from mental health
professionals who treat survivors of violence. Violence and Victims, 14(3), 261-275.
Campbell, R., Sefl, T., Barnes, H. E., Ahrens, C. E., Wasco, S. M., & Zaragoza-Diesfeld, Y. (1999).
Community services for rape survivors: Enhancing psychological well-being or increasing trauma?
Journal of Consulting and Clinical Psychology, 67(6), 847-858.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

160
Campbell, R., Wasco, S. M., Ahrens, C. E., Sefl, T., & Barnes, H. E. (2001). Preventing the “Second Rape”:
Rape survivors’ experiences with community service providers. Journal of Interpersonal Violence,
10(12), 1239-1259.
Chambers, D. (2013). Deep learning & real connections: Designing an online subject that requires higher
order thinking and real collaboration. Journal of Education and Learning, 13, 3847-3857.
Chio, K. S. (2012). Effective practices in providing online, in‐service training to health professionals in
low‐resource settings. International Journal of Training and Development, 16(3), 228-234.
Corbridge, S. J., McLaughlin, R., Tiffen, J., Wade, L., Templin, R., & Corbridge, T. C. (2008). Using
simulation to enhance knowledge and confidence. The Nurse Practitioner, 33(6), 12-13.
Cook, D. A., Levinson, A. J., Garside, S., Dupras, D. M., Erwin, P. J., & Montori, V. M. (2008). Internet-
based learning in the health professions: A meta-analysis. The Journal of the American Medical
Association, 300(10), 1181-1196.
Cox, D. R., & Oakes, D. (2001). Analysis of survival data. London: Chapman and Hall.
Crandall, C. & Helitzer, D. (2003). Impact evaluation of a Sexual Assault Nurse Examiner (SANE) Program.
Washington, DC: National Institute of Justice.
Creswell, J. W. (2013). Research Design: Qualitative, quantitative and mixed methods approaches (4
th
edition). Thousand Oaks, CA: Sage Publications, Inc.
Creswell, J. W., Plano Clark, V. L., Gutmann, M. L., & Hanson, W. E. (2003). Advanced mixed methods
research designs. In A. Tashakkori & C. Teddlie (Eds.), Handbook of Mixed Methods in Social and
Behavioral Research (pp. 209–240). Thousand Oaks, CA: Sage.
Day, D., Smith, B., & Muma, R. D. (2006). The effectiveness of online courses in physician assistant
education. The Journal of Physician Assistant Education, 17(3), 33-36.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
161
De Lange, A. H., Taris, T. W., Jansen, P., Kompier, M. A., Houtman, I. L., & Bongers, P. M. (2010). On the
relationships among work characteristics and learning‐related behavior: Does age matter? Journal
of Organizational Behavior, 31(7), 925-950.
Department of Justice (2004). A national protocol for sexual assault medical forensic examinations:
Adults/adolescents. Washington, DC: Author.
Department of Justice (2006). National training standards for sexual assault medical forensic examiners.
Washington, DC: Author.
Department of Justice (2013). A national protocol for sexual assault medical forensic examinations:
Adults/adolescents. Washington, DC: Author.
Derhammer, F., Lucente, V., Reed, J. F., & Young, M. J. (2000). Using a SANE interdisciplinary approach
to care of sexual assault victims. Joint Commission Journal on Quality and Patient Safety, 26(8),
488-496.
Derouin, R. E., Fritzsche, B. A., & Salas, E. (2005). E-learning in organizations. Journal of
Management, 31(6), 920-940.
Dyess, S. M. & Sherman, R. O. (2009). The first year of practice: New graduate nurses' transition and
learning needs. Journal of Continuing Education in Nursing, 40(9), 403-410.
Eastman, B. J., & Bunch, S. G. (2007). Providing services to survivors of domestic violence: A comparison
of rural and urban service provider perceptions. Journal of Interpersonal Violence, 22(4), 465-473.
Elfrink, V. L., Kirkpatrick, B., Nininger, J., & Schubert, C. (2010). Using learning outcomes to inform
teaching practices in human patient simulation. Nursing Education Perspectives, 31(2), 97-100.
Elfrink, V. L., Nininger, J., Rohig, L., & Lee, J. (2009). The case for group planning in human patient
simulation. Nursing Education Perspectives, 30(2), 83-86.
Ellis, S., & Davidi, I. (2005). After-event reviews: Drawing lessons from successful and failed
experience. Journal of Applied Psychology, 90(5), 857-871.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
162
Erickson, F. (1986). Qualitative methods in research on teaching. In M.C. Wittrock (3
rd
Ed.), Handbook of
Research on Teaching (pp. 119-161). New York, NY: Macmillan.
Fero, L. J., Witsberger, C. M., Wesmiller, S. W., Zullo, T. G., & Hoffman, L. A. (2009). Critical thinking ability
of new graduate and experienced nurses. Journal of Advanced Nursing, 65(1), 139-148.
Frankola, K. (2001). Why online learners drop out. Workforce-Costa Mesa, 80(10), 52-61.
Gegenfurtner, A., Veermans, K., Festner, D., & Gruber, H. (2009). Integrative literature review: Motivation
to transfer training: An integrative literature review. Human Resource Development Review, 8(3),
403-423.
Gilmore, M., & Lyons, E. M. (2012). Nursing 911: An orientation program to improve retention of online RN-
BSN students. Nursing Education Perspectives, 33(1), 45-47.
Goldstein, I. & Ford, J.K. (2002). Training in organizations (4
th
ed.). Belmont, CA: Wadsworth.
Goodman, J. S., & Wood, R. E. (2004). Feedback specificity, learning opportunities, and learning. Journal
of Applied Psychology, 89(5), 805-809.
Gormley, D. K., Costanzo, A. J., Lewis, M. R., Slone, B., & Savage, C. L. (2012). Assessing nurses’
continuing education preferences in rural community and urban academic settings. Journal for
Nurses in Staff Development, 28(6), 279-284.
Guthrie, J. P., & Schwoerer, C. E. (1996). Older dogs and new tricks: Career stage and self-assessed need
for training. Public Personnel Management, 25(1), 59-72.
Gyorki, D. E., Shaw, T., Nicholson, J., Baker, C., Pitcher, M., Skandarajah, A., & Mann, G. B. (2013).
Improving the impact of didactic resident training with online spaced education. ANZ Journal of
Surgery, 88(6), 477-480.
Haffer, A. G., & Raingruber, B. J. (1998). Discovering confidence in clinical reasoning and critical thinking
development in baccalaureate nursing students. The Journal of Nursing Education, 37(2), 61-70.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

163
Hansen-Suchy, K. (2011). Evaluating the effectiveness of an online medical laboratory technician
program. Clinical Laboratory Science: Journal of the American Society for Medical
Technology, 24(1), 35-40.
Harrington, S. (2011). Mentoring new nurse practitioners to accelerate their development as primary care
providers: A literature review. Journal of the American Academy of Nurse Practitioners, 23(4), 168-
174.
Hatcher, B., Bleich, M.R., Connolly, C., Davis, K., Hewlett, P.O. & Hill, K.S. (2006). Wisdom at work: The
importance of the older and experienced nursing in the workplace. Washington, DC: Robert Wood
Johnson Foundation.
Healy, A. F., Wohldmann, E. L., Parker, J. T., & Bourne, L. E. (2005). Skill training, retention, and transfer:
The effects of a concurrent secondary task. Memory & Cognition, 33(8), 1457-1471.
Hosmer, D. W., & Lemeshow, S. (2000). Interpretation of the fitted logistic regression model (2
nd
ed.) Applied Logistic Regression (pp. 47-90). Hoboken, N. J.: John Wiley & Sons, Inc.
Howard, K., Noe, R., & Wang, C. (2006). Motivation to learn and course outcomes: The impact of delivery
mode, learning goal orientation and perceived barriers and enablers. Personnel Psychology, 59(3),
665-702.
Hugenholtz, N. I., de Croon, E. M., Smits, P. B., van Dijk, F. J., & Nieuwenhuijsen, K. (2008). Effectiveness
of e-learning in continuing medical education for occupational physicians. Occupational
Medicine, 58(5), 370-372.
Hylton, M. E. (2006). Online versus classroom-based instruction: A comparative study of learning outcomes
in a diversity course. The Journal of Baccalaureate Social Work, 11(2), 102-114.
IAFN (2013). Data base of the International Association of Forensic Nurses, retrieved September 1, 2013
from http://www.forensicnurse.org.
IBM Corporation (2011). IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

164
Jang, K. S., Hwang, S. Y., Park, S. J., Kim, Y. M., & Kim, M. J. (2005). Effects of a Web-based teaching
method on undergraduate nursing students' learning of electrocardiography. The Journal of
Nursing Education, 44(1), 35-39.
Jeffries, P. R. (2005). A frame work for designing, implementing, and evaluating simulations used as
teaching strategies in nursing. Nursing Education Perspectives, 26(2), 96-103.
Jeffries, P. R., Woolf, S., & Linde, B. (2003). Technology-based vs. traditional instruction: A comparison of
two methods for teaching the skill of performing a 12-lead ECG. Nursing Education
Perspectives, 24(2), 70-74.
Jenkins, M. A., Langlais, P. J., Delis, D., & Cohen, R. (1998). Learning and memory in rape victims with
posttraumatic stress disorder. American Journal of Psychiatry, 155(2), 278-279.
Johnson, R. D., Hornik, S., & Salas, E. (2008). An empirical examination of factors contributing to the
creation of successful e-learning environments. International Journal of Human-Computer
Studies, 66(5), 356-369.
Johnston, J. (2007). The effectiveness of online instruction: A literature review. The Canadian Journal of
Medical Radiation Technology, 38(2), 17-21.
Johnston , J. (2008). Effectiveness of online instruction in the radiologic sciences. Radiologic Technology,
79(6), 497-506.
Kaddoura, M. A. (2010). New graduate nurses' perceptions of the effects of clinical simulation on their
critical thinking, learning, and confidence. Journal of Continuing Education in Nursing, 41(11), 506-
516.
Karaman, S. (2011). Nurses’ perceptions of online continuing education. BMC Medical Education, 11(86),
1-6.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

165
Karamizadeh, Z., Zarifsanayei, N., Faghihi, A. A., Mohammadi, H., & Habibi, M. (2012). The study of
effectiveness of blended learning approach for medical training courses. Iranian Red Crescent
Medical Journal, 14(1), 41-44.
Klein, H. J., Noe, R. A., & Wang, C. (2006). Motivation to learn and course outcomes: The impact of
delivery mode, learning goal orientation, and perceived barriers and enablers. Personnel
Psychology, 59(3), 665-702.
Kleinbaum, D. G., & Klein, M. (2005). Survival Analysis: A Self-Learning Text (2
nd
ed). New York: Springer.
Kneebone, R. L., Scott, W., Darzi, A., & Horrocks, M. (2004). Simulation and clinical practice:
Strengthening the relationship. Medical Education, 38(10), 1095-1102.
Laschinger, H. K. S., Shamian, J., & Thomson, D. (2001). Impact of magnet hospital characteristics on
nurses' perceptions of trust, burnout, quality of care, and work satisfaction. Nursing
Economics, 19(5), 209-219.
Leasure, A. R., Davis, L., & Thievon, S. L. (2000). Comparison of student outcomes and preferences in a
traditional vs. World Wide Web-based baccalaureate nursing research course. The Journal of
Nursing Education, 39(4), 149-154.
Ledray, L. E., & Barry, L. (1998). SANE expert and factual testimony. Journal of Emergency Nursing, 24(3),
284-287.
Ledray, L. E., & Simmelink, K. (1997). Efficacy of SANE evidence collection: A Minnesota study. Journal of
Emergency Nursing, 23(1), 75-77.
Lehmann, R., Bosse, H. M., & Huwendiek, S. (2010). Blended learning using virtual patients and skills
laboratory training. Medical Education, 44(5), 521-522.
Leiter, M. P., Jackson, N. J., & Shaughnessy, K. (2009). Contrasting burnout, turnover intention, control,
value congruence and knowledge sharing between Baby Boomers and Generation X. Journal of
Nursing Management, 17(1), 100-109.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

166
Leiter, M. P., & Laschinger, H. K. S. (2006). Relationships of work and practice environment to professional
burnout: Testing a causal model. Nursing Research, 55(2), 137-146.
Lewenson, S. B., & Truglio-Londrigan, M. (2008). Decision-making in nursing: Thoughtful approaches for
practice. Sudbury, MA: Jones & Bartlett Publishers.
Littel, K. (2001). Sexual assault nurse examiner (SANE) programs: Improving the community response to
sexual assault victims. Washington DC: US Department of Justice.
Logan, T. K., Evans, L., Stevenson, E., & Jordan, C.E. (2005). Barriers to services for rural and urban
survivors of rape. Journal of Interpersonal Violence, 20(5), 591-616.
Lundberg, K. M. (2008). Promoting self-confidence in clinical nursing students. Nurse Educator, 33(2), 86-
89.
Machtmes, K., & Asher, J. W. (2000). A meta‐analysis of the effectiveness of telecourses in distance
education. American Journal of Distance Education, 14(1), 27-46.
Macleod, M. L., Misener, R. M., Banks, K., Morton, A. M., Vogt, C., & Bentham, D. (2008). " I'm a Different
Kind of Nurse": Advice from nurses in rural and remote Canada. Canadian Journal of Nursing
Leadership, 21(3), 40-53.
Makhdoom, N., Khoshhal, K. I., Algaidi, S., Heissam, K., & Zolaly, M. A. (2013). ‘Blended learning’ as an
effective teaching and learning strategy in clinical medicine: A comparative cross-sectional
university-based study. Journal of Taibah University Medical Sciences, 8(1), 12-17.
Marrelli, T. M. (2004). Why mentoring is important. Home Health Care Management & Practice, 16(2), 122-
123.
Martin, P. Y. (2005). Rape work: Victims, gender, and emotions in organization and community context.
New York, N.Y.: Routledge.
Martinez, M. (2003, July 14). High attrition rate in e-learning: Challenges, predictors, and solutions. The
eLearning Developers Journal, 1-7.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

167
Maslach, C., & Leiter, M. P. (2008). Early predictors of job burnout and engagement. Journal of Applied
Psychology, 93(3), 498-512.
McGaghie, W. C., Issenberg, S. B., Petrusa, E. R., & Scalese, R. J. (2010). A critical review of
simulation‐based medical education research: 2003–2009.Medical Education, 44(1), 50-63.
McKenna, L., Innes, K., French, J., Streitberg, S., & Gilmour, C. (2011). Is history taking a dying skill? An
exploration using a simulated learning environment. Nurse Education in Practice, 11(4), 234-238.
McMahon, M. (2013). A study of the causes of attrition among adult on a fully online training course. Irish
Journal of Academic Practice, 2(1), 1-25.
Means, B., Toyama, Y., Murphy, R., Bakia, M., & Jones, K. (2010). Evaluation of evidence-based practices
in online learning: A meta-analysis and review of online learning studies. Washington, DC: U.S.
Department of Education Office of Planning, Evaluation, and Policy Development Policy and
Program Studies Service. Retrieved from www.ed.gov/about/offices/list/opepd/ppss/reports.html.
Menard, S. (2002). Applied logistic regression analysis (2
nd
ed.). Thousand Oaks, CA: Sage.
Metcalf, M. P., Tanner, T. B., & Buchanan, A. (2010). Effectiveness of an online curriculum for medical
students on genetics, genetic testing and counseling. Medical Education Online, 15, 1-12.
Miles, M. B., Huberman, A. M., & Saldaña, J. (2013). Qualitative data analysis: A methods sourcebook (3
rd
ed.). Thousand Oaks, CA: Sage Publications, Inc.
Miller, L. C., Devaney, S. W., Kelly, G. L., & Kuehn, A. F. (2008). E-mentoring in public health nursing
practice. The Journal of Continuing Education in Nursing, 39(9), 394-399.
Mills, J., Francis, K., & Bonner, A. (2008). Walking with another: rural nurses' experiences of
mentoring. Journal of Research in Nursing, 13(1), 23-35.
Naidr, J. P., Adla, T., Janda, A., Feberova, J., Kasal, P., & Hladikova, M. (2004). Long-term retention of
knowledge after a distance course in medical informatics at Charles University Prague. Teaching
and Learning in Medicine, 16(3), 255-259.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

168
Neal-Boylan, L. (2006). An analysis of the difference between hospital and home healthcare nurse job
satisfaction. Home Health Care Nurse, 24(8) 505-512.
Newel D. J. (1992). Intention-to-treat analysis: Implications for quantitative and qualitative
research. International Journal of Epidemiology, 21, 837–41.
Noe, R. A., & Wilk, S. L. (1993). Investigation of the factors that influence employees' participation in
development activities. Journal of Applied Psychology, 78(2), 291-302.
NVivo qualitative data analysis software; QSR International Pty Ltd. Version 10, 2012.
O’Connell, M. S., Doverspike, D., Gillikin, S., & Meloun, J. M. (2001). Computer anxiety: Effects on
computerized testing and implications for e. Cruiting. Journal of e.Commerce and Psychology, 1,
25-39.
O'Connor, A. B. (2006). Clinical instruction and evaluation: A teaching resource (2
nd
ed.). Sudbury, MA:
Jones & Bartlett Learning.
Örtenblad, A. (2001). On differences between organizational learning and learning organization. The
Learning Organization, 8(3), 125–133
Park, J. (2007). Factors related to learner dropout in online learning. In Nafukho, F. M., Chermack, T. H., &
Graham, C. M. (Eds.)Proceedings of the 2007 Academy of Human Resource Development Annual
Conference(pp. 25-1–25-8). Indianapolis, IN:AHRD.
Park, J. H., & Wentling, T. (2007). Factors associated with transfer of training in workplace e-learning.
Journal of Workplace Learning, 19(5), 311-329
Park, J.H., & Choi, H.J. (2009). Factors influencing adult learners' decision to drop out or persist in online
learning. Educational Technology & Society, 12(4), 207-217.
Parker, B., & Myrick, F. (2010). Transformative learning as a context for human patient simulation. Journal
of Nursing Education, 49(6), 326-332.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

169
Patterson, B., & McFadden, C. (2009). Attrition in online and campus degree programs. Online Journal of
Distance Learning Administration, 12(2) 1-12.
Patterson, D., & Campbell, R. (2010). Why rape survivors participate in the criminal justice system. Journal
of Community Psychology, 38(2), 191-205.
Patton, M.Q. (2002). Qualitative research and evaluation methods (3
rd
ed). Thousand Oaks, CA: Sage.
Penz, K., D Arcy, C., Stewart, N., Kosteniuk, J., Morgan, D., & Smith, B. (2007). Barriers to participation in
continuing education activities among rural and remote nurses. Journal of Continuing Education in
Nursing, 38(2), 58-66.
Pereira, J. A., Pleguezuelos, E., Meri, A., Molina‐Ros, A., Molina‐Tomás, M. C., & Masdeu, C. (2007).
Effectiveness of using blended learning strategies for teaching and learning human
anatomy. Medical Education, 41(2), 189-195.
Perry, B., Boman, J., Care, W. D., Edwards, M., & Park, C. (2008). Why do students withdraw from online
graduate nursing and health studies education? The Journal of Educators Online, 5(1), 1-17.
Pomales-García, C., & Liu, Y. (2006). Web-based distance learning technology: The impacts of web
module length and format. The American Journal of Distance Education, 20(3), 163-179.
Pong, R. W., & Russell, N. (2003). A review and synthesis of strategies and policy recommendations on the
rural health workforce. Centre for Rural and Northern Health Research: Laurentian University
Retrieved from http://www.cranhr.ca/pdf/TORC_Ruralhealthworkforcesynthesis-finaldraft-May.pdf
Pool, I., Poell, R., & ten Cate, O. (2012). Nurses’ and managers’ perceptions of continuing professional
development for older and younger nurses: a focus group study. International Journal of Nursing
Studies, 50(1), 34-43.
Pratt, J. (2002). E-learning: Is it right for your organization? Home Health Care Management Practice,
14(6), 471-474.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

170
Pugh, C. M., Obadina, E. T., & Aidoo, K. A. (2009). Fear of causing harm: Use of mannequin-based
simulation to decrease student anxiety prior to interacting with female teaching
associates. Teaching and Learning in Medicine, 21(2), 116-120.
R Development Core Team (2012). R: A language and environment for statistical computing. R Foundation
for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0, URL http://www.R-project.org/.
Reeves, T. C. (2000). Alternative assessment approaches for online learning environments in higher
education. Journal of Educational Computing Research, 23(1), 101-111.
Resnick, H., Acierno, R., Holmes, M., Dammeyer, M., & Kilpatrick, D. (2000). Emergency evaluation and
intervention with female victims of rape and other violence. Journal of Clinical Psychology, 56(10),
1317-1333.
Roberge, C.M. (2009). Who Stays in Rural Nursing Practice? An International Review of the Literature on
Factors Influencing Rural Nurse Retention. Online Journal of Rural Nursing and Health Care. 9(1)
82-93.
Roberts, V. W., Brannan, J. D., & White, A. (2005). Outcomes-based research: Evaluating the effectiveness
of an online nurse refresher course. Journal of Continuing Education in Nursing, 36(5), 200-204.
Rowe, M., Frantz, J., & Bozalek, V. (2012). The role of blended learning in the clinical education of
healthcare students: A systematic review. Medical Teacher, 31(4), 216-221.
Ruiz, J. G., Mintzer, M. J., & Leipzig, R. M. (2006). The impact of e-learning in medical
education. Academic Medicine, 81(3), 207-212.
Sadovich, J. M. (2005). Work excitement in nursing: An examination of the relationship between work
excitement and burnout. Nursing Economics, 23(2) 91-96.
Salyers, V. L. (2005). Web-enhanced and face-to-face classroom instructional methods: Effects on course
outcomes and student satisfaction. International Journal of Nursing Education Scholarship, 2(1), 1-
13.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

171
Schneiderman, J., Corbridge, S., & Zerwic, J. J. (2009). Demonstrating the effectiveness of an online,
computer-based learning module for arterial blood gas analysis. Clinical Nurse Specialist, 23(3),
151-155.
Seago, B. L., Ketchum, J. M., & Willett, R. M. (2012). Pelvic examination skills training with genital teaching
associates and a pelvic simulator: Does sequence matter? Simulation in Healthcare, 7(2), 95-101.
Seng, J. S., Sanubol, M., & Johnson County (Iowa) SANE Team. (2004). The first year as sexual assault
nurse examiner: Role transition and role-related stress within a new SANE team. Journal of
Emergency Nursing, 30(2), 126-133.
Shadish, W.R., Cook, T.D., & Campbell, D.T. (2002). Experimental and quasi-experimental designs for
generalized causal inference. Boston, MA: Houghton Mifflin Company.
Shanafelt, T. D. (2009). Enhancing meaning in work: A prescription for preventing physician burnout and
promoting patient centered care. The Journal of the American Medical Association, 302(12), 1338-
1340.
Sievers, V., Murphy, S., & Miller, J. J. (2003). Sexual assault evidence collection more accurate when
completed by sexual assault nurse examiners: Colorado’s experience. Journal of Emergency
Nursing, 29(6), 511-514.
Simms, L. M., Erbin-Roesemann, M., Darga, A., & Coeling, H. (1990). Breaking the burnout barrier:
resurrecting work excitement in nursing. Nursing Economics, 8(3), 177-187.
Sitzmann, T. (2010). Self-regulating online course engagement. Training and Development, 64(3), 26.
Retrieved from www.ilr.cornell.edu/cahrs/news/upload/BellResearch_T-DMarch10.pdf
Sitzmann, T., Kraiger, K., Stewart, D., & Wisher, R. (2006). The comparative effectiveness of web‐based
and classroom instruction: A meta‐analysis. Personnel Psychology, 59(3), 623-664.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

172
Smith, A. M., Ortiguera, S. A., Laskowski, E. R., Hartman, A. D., Mullenbach, D. M., Gaines, K. A., &
Fisher, W. (2001). A preliminary analysis of psychophysiological variables and nursing
performance in situations of increasing criticality. In Mayo Clinic Proceedings, 76(3), 275-284.
Smith, A. R., Silva, C., Covington, D. W., & Joiner Jr, T. E. (2013). An assessment of suicide-related
knowledge and skills among health professionals. Health Psychology. DOI: 10.1037/a0031062
Spohn, C. (2008). The criminal justice system's response to sexual violence. Paper presented at the
National Institute of Justice Sexual Violence Research Workshop. Washington, DC.
Starks, H., & Trinidad, S. B. (2007). Choose your method: A comparison of phenomenology, discourse
analysis, and grounded theory. Qualitative Health Research, 17(10), 1372-1380
Stein, M. B., Kennedy, C. M., & Twamley, E. W. (2002). Neuropsychological function in female victims of
intimate partner violence with and without posttraumatic stress disorder. Biological Psychiatry,
52(11), 1079-1088.
Stefanski, R. R., & Rossler, K. L. (2009). Preparing the novice critical care nurse: A community-wide
collaboration using the benefits of simulation. The Journal of Continuing Education in
Nursing, 40(10), 443-451.
Stewart, A., Inglis, G., Jardine, L., Koorts, P., & Davies, M. W. (2013). A randomised controlled trial of
blended learning to improve the newborn examination skills of medical students. Archives of
Disease in Childhood--Fetal and Neonatal Edition, 98(2), 141-144.
Stone, D. M., Barber, C. W., & Potter, L. (2005). Public health training online: The national center for
suicide prevention training. American Journal of Preventive Medicine, 29(5), 247-251.
Strauss A., & Corbin, J. (1990). Basics of qualitative research: grounded theory procedures and
techniques. Thousand Oaks, CA: Sage.
Stroth, C. (2010). Job embeddedness as a nurse retention strategy for rural hospitals. Journal of Nursing
Administration, 40(1), 32-35.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

173
Sung, Y. H., Kwon, I. G., & Ryu, E. (2008). Blended learning on medication administration for new nurses:
Integration of e-learning and face-to-face instruction in the classroom. Nurse Education
Today, 28(8), 943-952.
Svirko, E. & Mellanby, J. (2008). Attitudes to e-learning, learning style and achievement in learning
neuroanatomy by medical students. Medical Teacher, 30(9-10), 219-227.
Tabachnick, B. G., & Fidell, L. S. (2013). Using Multivariate Statistics (6
th
ed.). Boston, MA: Allyn and
Bacon.
Taylor, P., & Urwin, P. (2001). Age and participation in vocational education and training. Work,
Employment & Society, 15(4), 763-779.
Therneau, T. (2013). A Package for Survival Analysis in S. R package version 2.37-4 [software]. Available
from: http://CRAN.R-project.org/package=survival
Theroux, R., & Pearce, C. (2006). Graduate students’ experiences with standardized patients as adjuncts
for teaching pelvic examinations. Journal of the American Academy of Nurse Practitioners, 18(9),
429-435.
Tjaden, P. G., & Thoennes, N. (2006). Extent, nature, and consequences of rape victimization: Findings
from the National Violence Against Women Survey. Washington, DC: National Institute of Justice.
Retrieved from: https://www.ncjrs.gov/pdffiles1/nij/210346.pdf
Tjaden, P. & Thoennes, N. (1998). Prevalence, incidence, and consequences of violence against women:
Findings from the National Violence against Women Survey. Washington D.C.: Department of
Justice. Retrieved from: https://www.ncjrs.gov/pdffiles/172837.pdf
US Department of Education. (2010). Evaluation of Evidence-Based Practices in Online Learning: A Meta-
Analysis and Review of Online Learning Studies (Washington, DC: SRI International).
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

174
van Gog, T., Sluijsmans, D. M., Joosten-ten Brinke, D., & Prins, F. J. (2010). Formative assessment in an
online learning environment to support flexible on-the-job learning in complex professional
domains. Educational Technology Research and Development, 58(3), 311-324.
Vessey, J. A., & Huss, K. (2002). Using standardized patients in advanced practice nursing
education. Journal of Professional Nursing, 18(1), 29-35.
Walters, C., Raymont, A., Galea, S., & Wheeler, A. (2012). Evaluation of online training for the provision of
opioid substitution treatment by community pharmacists in New Zealand. Drug and Alcohol
Review, 31(7), 903-910.
Weaver, A. (2011). High-fidelity patient simulation in nursing education: An integrative review. Nursing
Education Perspectives, 32(1), 37-40.
Welsh, E. T., Wanberg, C. R., Brown, K. G., & Simmering, M. J. (2003). E‐learning: Emerging uses,
empirical results and future directions. International Journal of Training and Development, 7(4),
245-258.
Wild, R. H., Griggs, K. A., & Downing, T. (2002). A framework for e-learning as a tool for knowledge
management. Industrial Management & Data Systems, 102(7), 371-380.
Willging, P. A., & Johnson, S. D. (2004). Factors that influence students’ decision to dropout of online
courses. Journal of Asynchronous Learning Networks, 8(4), 2-15.
Wolf, Z., Colahan, M., Costello, A., Warwick, F., Ambrose, M., & Giardino, E. (1998). Relationship between
nurse caring and patient satisfaction. Medical Surgical Nursing Journal, 7(2), 99-106.
Woo, M. A., & Kimmick, J. V. (2000). Comparison of internet versus lecture instructional methods for
teaching nursing research. Journal of Professional Nursing, 16(3), 132-139.
Zhang, D., Zhou, L., Briggs, R., & Nunamaker, J. (2006). Instructional video in e-learning: Assessing the
impact of interactive video on learning effectiveness. Information and Management, 43(1), 15-27.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

175
APPENDIX A: PROJECT STAFF
Project staff for NIJ 2010-NE-BX-K260 (in alphabetical order):
Training staff:
Elisabeth Almond, RN, SANE-A
Polly Campbell, RN
Kermit Channell II, Criminalist
Susan Chasson, RN, JD
Kim Day, RN, FNE, SANE-A, SANE-P, SAFEta Coordinator
Carey Goryl, CEO
Tara Henry, FNP, RN, SANE-A, SANE-P
Major Tom Hurley, JD
Kris Karcher, RN
Detective James Markey
Jenifer Markowitz, RN, WHNP, SANE-A
Kim Nash, RN, SANE-A, SANE-P
Danielle Oringer, RN, SANE-A, SANE-P
Rebecca Parsons-Gerstel, RN, SANE-A
Jennifer Pierce-Weeks, RN, SANE-A, SANE-P, Project Director
Matt Redle, JD
Jenny Sanchez, RN, SANE-A
Tom Velardi, JD
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

176
Evaluation staff:
Rebecca Campbell, Ph.D., Consultant
Katie Donoghue, B.A., Student Interview Data Coder/Analyst
Debra Patterson, Ph.D., Principal Investigator
Megan Pennefather, M.S.W., Evaluation Coordinator
Stella Resko, Ph.D., Co-Investigator/Principal Statistician
Mical Roby, B.A., Instructor Interview Data Coder
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
177
APPENDIX B: DISSEMINATION
Patterson, D., & Pierce-Weeks, J. (October, 2013). Evaluation findings of the IAFN’s Online Adult/
Adolescent SAFE Training and Clinical Program. Paper presented at the International Conference
on Forensic Nursing Science & Practice, Anaheim, CA.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
178
APPENDIX C: DATA COLLECTION INSTRUMENTS
APPENDIX C1: Student Pre-Training Online Survey
APPENDIX C-2: Pre-Test/Post-Test Questions
APPENDIX C3: Student Post-Training Online Survey
APPENDIX C-4: Clinical Instructor Interview Protocol
APPENDIX C-5: Student Interview Protocol
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

179
APPENDIX C1: 1 Pre-Training Online Survey
Section I: Training Interest
The survey will begin with questions about your interest in forensic nursing training and your plans after the
training.
2. What made you interested in forensic nursing?
1
3. What made you interested in taking this particular training? (check all that apply)
No cost to me
Most of the training occurs online
IAFN sponsored
The two-day clinical training
Other _______________________________
4. Which best describes your plans following the training?
Apply to work at in an already established SAFE program
Have been offered a position at an already established SAFE program and will begin conducting
exams after the training
Currently conducting exams at an already established SAFE program
Starting a new SAFE program
1
Open-ended survey question was converted into six categorical variables for analysis.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

180
Section II: Computer use
5. The next part of this survey will ask some questions about your feelings about technology and online
learning. Please click on the answer that best reflects your opinion. Remember that there is no right or
wrong answers.
Strongly
Agree
Agree
Neither Agree
or Disagree
Disagree
Strongly
Disagree
a. I usually get very anxious about
using a computer.
1
2
3
4
5
b. I’m not the type to do well with
computers.
1
2
3
4
5
c. I have a lot of self-confidence when it
comes to working with computers.
1
2
3
4
5
d. I like working with computers.
1
2
3
4
5
e. The online course will take less time
than a traditional course in a
classroom.
1
2
3
4
5
f. I have access to good Internet
connectivity.
1
2
3
4
5
6. Have you ever taken an online course before?
O No
O Yes
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

181
Section III: Training Goals
7. The next part of this survey will ask questions about your goals for the training, and current life
responsibilities. Please click on the answer that best reflects your opinion or situation.
Strongly
Agree
Agree
Neither Agree
or Disagree
Disagree
Strongly
Disagree
a. I will try to learn as much as I can from
this course
1
2
3
4
5
b. I am interested in learning the training
material.
1
2
3
4
5
c. My supervisor is supportive of me
attending this training.
1
2
3
4
5
d. I am willing to invest effort to improve
skills and competencies related to
becoming a forensic nurse.
1
2
3
4
5
e. I have time in my schedule to focus on
this course.
1
2
3
4
5
f. I will get more from this training than
most people.
1
2
3
4
5
g. I am motivated to learn the skills needed
to be a forensic nurse examiner.
1
2
3
4
5
h. I have a lot of work responsibilities.
1
2
3
4
5
i. I am willing to exert considerable effort
in this training in order to improve my
skills.
1
2
3
4
5
j. I have a lot of family obligations right
now.
1
2
3
4
5
Part V: Demographics
Finally, we would like to ask you a few questions about yourself so we can have some background
information about the clinicians who participate in the training.
8. What is the highest level of education you have completed?
1=Associate’s degree
2=Bachelor’s degree
3=Some graduate school
4=Graduate school
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
182
9. Are you currently employed?
1= Yes, full-time
2= Yes, part-time
3= No
10. How many hours a week do you work? ___________
11. How many years have you worked as a nurse? ___________
12. How old are you? ___________
13. Which best describes the community where you work?
O Suburban
O Rural
O Urban
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

183
APPENDIX C-2: Pre-Test/Post-Test Questions
Introduction Module: SAFE training introduction.
1. Providing a rape education program in the community is an example of _______________.
A. Tertiary prevention
B. Secondary prevention
C. Primary prevention
D. Initial prevention
2. In which decade was the first SAFE program established:
A. 1960s
B. 1970s
C. 1980s
D. 1990s
3. What is the difference between a SANE and a SAFE?
A. A SANE works in a hospital and a SAFE works in a community-based facility.
B. A SANE is always a nurse whereas a SAFE can be a nurse or any other appropriately trained
health professional, such as a physician.
C. A SANE focuses on the healthcare needs of the patient while a SAFE focuses on the forensic
evidence collection.
D. There is no difference.
4. SAFEs have the ability to serve as expert witnesses for criminal court cases.
A. True
B. False
5. The primary focus of the SAFE should be _________________________.
A. Collecting forensic evidence
B. Determining if the patient is telling the truth
C. Attending to patient healthcare needs
D. Assisting law enforcement in determining the facts of the case
6. Completion of a SAFE training makes you eligible for SAFE certification.
A. True
B. False
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

184
Module I: Dynamics
1. People with disabilities are usually sexually assaulted by someone known to them.
A. True
B. False
2. Which of the following groups have the lowest risk of sexual victimization compared to the general
population (check all that apply)?
A. People who are homeless
B. Adolescents
C. Native American/Alaska Native
D. Persons with disabilities
E. Caucasians/European Americans
3. According to the Centers for Disease Control, which of the following is considered an experience of
sexual violence (please check all that apply)?
A. A man is forced to engage in fellatio (mouth on penis) with another man
B. A woman watches pornography after being threatened with bodily harm by her spouse
C. A 20 year old woman has sexual intercourse with a thirteen year old boy
D. A man penetrates his friend’s vagina while she is passed out.
E. All of the above
4. Sexual assault rarely occurs in lesbian/gay intimate relationships.
A. True
B. False
5. Rape has been used as a strategy in several wars and armed conflicts.
A. True
B. False
6. Which of the following statements are true (check all that apply)?
A. Most allegations of rape are false
B. Most rapes are committed by a stranger
C. Most rapes are planned
D. The majority of rape victims endure injuries.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
185
Module II: Forensic science, ethics and self-care
1. In which document is nursing’s relationship to the larger society described as a social contract:
A. ANA’s Scope and Standards of Nursing Practice
B. ANA's Nursing Code of Ethics
C. State Nurse Practice Acts
D. ANA’s Nursing’s Social Policy Statement
2. When faced with ethical choices forensic nurses should use recognized ethical frameworks to guide the
decision making process. These frameworks must take into account all of the following except:
A. Autonomy
B. Non-malfeasance
C. Connectivity
D. Justice
3. The term “forensic” comes the Latin adjective forensis meaning:
A. Of or related to formal science
B. Of or before the forum
C. Of or related to a formal investigation
D. Of or related to force
4. Saakvitne & Pearlman suggest that vicarious trauma can be prevented by paying attention to the
ABCs. When referring to the ABCs, they are referring to:
A. Attention, Balance and Composure
B. Awareness, Balance and Connection
C. Awareness, Benefit and Connection
D. Attention, Benefit and Connection
5. Which of the following statements most accurately describes the term Secondary/Vicarious Trauma as
it relates to sexual assault:
A. It refers to the long term psychosocial impact of sexual assault on the victim of sexual assault.
B. It refers to other, non sexual, injuries resulting from an assault, such as bruises to the arms, legs,
face, etc. which are considered secondary to the sexual trauma.
C. It refers to pervasive changes in the “self” of trauma care workers that results from empathetic
engagement with traumatized individuals over time.
D. None of the above
6. The following term/s have been used to describe the negative effects that can result from working with
traumatized clients over time:
A. Burnout
B. Counter-transference
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
186
C. Compassion Fatigue
D. All of the Above
7. The American Nurses Association first recognized forensic nursing as a specialty in:
A. 1978
B. 1992
C. 1995
D. 2001
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

187
Module III: Patient centered, coordinated team approach.
1. All of the following statements are true regarding privileged communication, except:
A. Privileged communication pertains to both oral and written communications.
B. Laws pertaining to privileged communication vary by state.
C. Conversations between husband and wife are not considered privileged communications.
D. Cases involving child abuse or neglect are exceptions to the rule of privileged communications.
2. If a victim asks an advocate to leave the room, the advocate should:
A. Leave the room, inform other members of the team that the victim does not wish to have an
advocate present and leave the facility.
B. Stay in the room, the victim is in shock and doesn’t really mean what she is saying.
C. Leave the room as requested, but continue to advocate on behalf of the victim with other team
members and/or by providing support to the victim’s family members.
D. Explain to the victim that her job requires her to stay with the victim throughout the examination
process and therefore she cannot leave.
3. Of the following activities, which is NOT a SAFE responsibility:
A. Obtaining feedback from lab personnel to determine if evidence collection methods/systems are
working.
B. Documenting victim injuries, including taking photographs and completing body maps as
necessary.
C. Determining whether or not a sexual assault actually occurred.
D. Knowing what is in the evidence collection kit and why different items are being collected.
4. A woman comes to the local precinct to report that she was raped outside of her apartment complex 3
days ago. The officer on duty should:
A. Ask the victim why she waited so long to report the incident
B. Explain that too much time has passed since the attack and that filing a report would serve little
purpose at this point
C. Record the victim’s story and conduct a follow-up visit to the crime scene to collect evidence.
D. Suggest the victim contact the local rape crisis center for assistance with reporting.
5. The Role of the Detective in a sexual assault case does NOT include:
A. Conduct a comprehensive interview with the victim
B. Direct the investigative response
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

188
C. Screen out cases where prosecution is not justified nor in the public interest
D. Ensure that evidence is collected and the chain of custody is maintained.
E. Package all information regarding the case into a casebook for the prosecution.
6. The acronym CODIS stands for:
A. Collection Data Information System
B. Combined Data Information System
C. Combined DNA Index System
D. Combined DNA Information System
7. The primary role of the sexual assault forensic examiner is to collect evidence that can be used to
prosecute a case.
A. True
B. False
8. The primary concern of the law enforcement first responder arriving at the scene where a sexual
assault has just occurred should be:
A. Ensuring the safety of the victim
B. Finding the perpetrator
C. Conducting an in depth interview with the victim
D. Collecting evidence to assure prosecution
9. Of the following titles, which most accurately describes the primary role of a prosecutor in a sexual
assault case:
A. Trial Advocate
B. Minister of Justice
C. Pre-Trial Manager
D. Policy Shaper
10. The acronym SART stands for:
A. Sexual Assault Rescue Team
B. Sexual Aggression Reaction Team
C. Sexual Assault Response Team
D. Sexual Aggression Response Team
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

189
11. A blood sample that is at least dime-sized is required to conduct the PCR (polymerase chain reaction)
test.
A. True
B. False
12. The prosecutor’s primary responsibility is in representing the interests of the victim.
A. True
B. False
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

190
Module IV: History and physical
1. Which of the following best defines the term ecchymosis:
A. Pinpoint red-purple, hemorrhagic spots on the skin or mucous membranes produced by the rupture
of small capillaries.
B. A hemorrhagic spot or blotch; non-elevated, rounded, or irregular blue or purplish purpuric patch.
C. A discoloration of the soft tissue caused by capillary congestion/dilation due to many causes.
D. Rubbing or scraping away of the superficial skin or mucous membrane from injury or mechanical
means.
2. To be diagnosed with PTSD individuals must experience a stressor that results in intense fear,
helplessness or horror. Additionally, they must meet which of the following criteria (choose all that
apply):
A. 3 avoidant/numbness criteria
B. 2 hyper arousal criteria
C. 2 intrusive recollection criteria
D. 1 month or more in duration
E. Significant impairment in social, occupational or other important areas of functioning.
3. All of the following are characteristics associated with lacerations, EXCEPT:
A. Jagged edges
B. Results from blunt force trauma
C. Bridging of tissue
D. Deeper than it is wide
4. All of the following are examples of an injury resulting from blunt force trauma, EXCEPT:
A. Bruising
B. Laceration
C. Cut
D. Abrasion
E. All of the above
5. In the Mneumonic “BALDSTEP,” which is used as tool to remember physical findings associated with
sexual assault, the letter “B” stands for:
A. Bleeding, bruising & beating
B. Burns, bruising & battering
C. Bleeding, bruising, bite marks & burns
D. Battering, burns, bruising & bite marks
6. When you are evaluating an injury you should:
A. Assess for visible injury
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

191
B. Assess for pain
C. Assess for symptoms
D. All of the above
7. Of the following statements related to strangulation all are true, EXCEPT:
A. The terms choking and strangulation can be used interchangeably by the provider
B. Approximately 50% of strangulation victims have no visible injuries
C. Fatality from strangulation can occur hours to weeks following the event
D. Manual strangulation is the most common form of strangulation seen in cases of domestic violence
8. There are how many essential elements to healthcare communication?
A. 5
B. 3
C. 6
D. 7
9. Tanner Staging is (choose all that apply):
A. A tool used to assess secondary sex characteristic development
B. Divided into 4 phases for males and 5 for females
C. Used to estimate chronological age
D. Divided into 5 phases
E. Based upon developmental changes in Caucasians
10. Burgess and Holstrom found that victims of sexual assault tended to display either one or another of
two types of emotional style:
A. Hysterical or subdued
B. Expressive or controlled
C. Calm or anxious
D. Anxious or controlled
11. Of the following questions, all are relevant to the sexual assault history taking process, EXCEPT:
A. When did the assault occur?
B. Did you know your assailant?
C. What was your assailant wearing?
D. Was there vaginal, anal or oral penetration?
E. What was the gender of your assailant?
12. Having an increased number of adverse childhood experiences makes the following more likely in
adulthood (choose all that apply):
A. Being raped/sexually assaulted
B. Abusing alcohol or drugs
C. Smoking cigarettes
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
192
D. Being a victim of intimate partner violence
E. Hallucinations
F. Attempting suicide
G. Increased mortality
13. The physiological damage that occurs with strangulation can be the result of (choose all that apply):
A. Cardiac arrhythmias
B. Lack of blood flow to the brain
C. Increase of blood in the brain
D. Lack of oxygen to the brain
14. You can determine how many hours have elapsed since a bruise was incurred by evaluating its color,
the crispness of its edges and degree of pain and swelling.
A. True
B. False
15. Sexual assault history taking and forensic interviewing are synonymous.
A. True
B. False
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

193
Module V: Anogenital Exam
1. All of the following descriptions regarding the Labia Majora are accurate, except:
A. Referred to as the “outer lips”
B. Homologous to the male scrotum
C. Composed largely of erectile tissue
D. Has a large arterial and venous network
2. Using the concept of an analog clock to identify genital landmarks, the Fossa Navicularis and Posterior
Fourchette are found at:
A. 3 o'clock
B. 6 o'clock
C. 9 o'clock
D. 12 o'clock
3. A 2004 study of adolescents by Jones et al. found:
A. Adolescents had lower incidents of genital injuries than their adult counterparts.
B. A difference in the pattern of injury between consensual vs. nonconsensual encounters.
C. No difference in the pattern of injury between consensual vs. nonconsensual encounters.
D. Adolescent injury rate, type and site were similar to that found in adults.
5. The medicalization (procedure being performed by professional medical practitioners) of female genital
mutilation is generally considered a positive development.
A. True
B. False
6. The four most common sites of genital injury from most to least are as follows:
C. Perineum, fossa navicularis, & cervix, anus
D. Hymen, perineum, vaginal walls, & anus
E. Posterior Fourchette, labia minora, hymen, & fossa navicularis
F. Vaginal walls, perineum, posterior Fourchette, & cervix
7. Tags, bumps and intravaginal ridges are all examples of:
A. Anatomical abnormalities associated with sexual assault
B. Anatomical abnormalities associated with other disease processes and not necessarily associated
with sexual assault.
C. Normal anatomic variations
D. None of the above
8. Which of the following statements most accurately describes the use of the Toluidine Blue Dye (TBD)
test:
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

194
A. TBD is done to find the existence of injury that can’t be seen by the naked eye or through a
colposcope.
B. TBD is usually applied to the vaginal walls, cervix and rectum.
C. TBD stain may not be absorbed in cases of acute tissue swelling.
D. TBD is considered positive when the stain uptake is diffuse and light blue in color.
9. Long term complications association with Female genital mutilation include (check all that apply):
A. Urinary tract infections
B. Shock
C. Fistulas
D. Incontinence
E. Hemorrhage
F. Abscess
G. HIV/AIDS
10. Which of the following statements related to digital vaginal penetration is true:
A. The most common sites of injury in digital penetration are the hymen & vaginal walls
B. There is less injury associated with digital vaginal penetration than other forms of sexual assault.
C. Studies indicate that as many as 81% of victims of digital vaginal penetration have some type of
injury.
D. The most common type of injury associated with digital vaginal penetration is bruising
11. Genital injury sustained during sexual assault is most commonly seen:
A. Between 3 and 6 o'clock
B. Between 6 and 9 o'clock
C. Between 3 and 9 o'clock
D. At 12 o'clock
12. Studies show a wide variation in the percentage of victims presenting with genital injury. Factors
influencing the presence of or absence of injury include all but:
A. Lack of vaginal penetration
B. Victim alcohol/drug use
C. Known sex partner
D. Delay in reporting
13. Follow up exams are recommended and are useful for:
A. Documenting healing
B. Identifying patient normals
C. Evaluating patient’s ongoing physical and mental status
D. Providing another opportunity for support.
E. All of the above
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

195
14. The Foley catheter technique is used during a sexual assault examination to:
C. Visualize hymenal tissue
D. Facilitate bladder emptying
E. Inflate vaginal walls for visualization
F. Remove vaginal secretions
15. What is the most common type of genital injury seen in female sexual assault cases?
G. Abrasions
H. Lacerations
I. Bruising
J. Tenderness
16. Which of the following exam positions is most conducive for performing the anal exam:
A. Lithotomy
B. Supine knee chest
C. Prone knee chest
D. None of the above
17. All of the following statements related to the hymen are true, except:
A. The hymen separates external genitalia from vagina.
B. An imperforate hymen covers the vaginal opening.
C. A cribriform hymen has multiple small openings and is sometimes likened to looking like Swiss
cheese.
D. Is no longer present after intercourse.
18. When conducting a colposcopic exam, the SAFE should:
A. Document the presence of injury
B. Document the absence of injury
C. Document normal variations
D. All of the above
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
196
Module VI: Photography
1. Exigent evidence refers to:
A. Evidence collected from the external female genitalia.
B. Evidence that, if not obtained immediately, could be lost.
C. Evidence (photos) that are collected and stored in a specific digital format
D. Evidence (photos) that are attached to the patient’s medical records.
2. When assessing the quality of a photo the five factors to consider are:
A. Lighting, focus, pixel size, framing and position
B. Lighting, contrast, focus, size and evidentiary value
C. Lighting, focus, framing, position and evidentiary value
D. Lighting, framing, position, size and focus
3. If a patient is complaining of pain in the shoulder, but there are no visible signs of trauma, you should:
A. Make a note of patient’s complaint in the chart.
B. Since there is no visible sign of trauma, documentation is not necessary.
C. Make a note of patient’s complaint in the chart and take a photo of the area to include in the
records.
D. Ask the patient if they want you to photograph the shoulder.
4. A camera is comprised of 3 elements:
A. Capture element, optical element and mechanical element
B. Optical element, mechanical element, and lighting element
C. Capture element, lighting element and mechanical
D. Optical, lens, and mechanical
5. The higher the resolution the higher the quality of the photo.
A. True
B. False
6. Which of the following statements related to shutter speed is true:
A. The faster the shutter speed the blurrier the picture
B. The faster the shutter speed the slower the aperture
C. The slower the shutter speed the clearer the picture
D. The slower the shutter speed the blurrier the picture
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
197
7. A camera should be positioned:
A. Perpendicular or at 90 degree angle over the injury
B. At a 45 – 60 degree angle from the injury to visualize the edges of an injury.
C. At a 180 angle when trying to capture a protruding injury
D. All of the above
8. It is okay to crop/change a photo if:
A. It’s never okay to alter the original photo.
B. Both the original and the altered photo are labeled appropriately and kept together in the record.
C. You label the cropped photo appropriately (i.e., identify location and type of injury being
photographed) and put it in the medical record. There is no need to keep the original in the medical
record.
D. None of the above.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

198
Module VII: Evidence Collection
1. Of the following statements, which does not adhere to the rules of evidence collection:
A. Gloves should be powder free.
B. Gloves should be changed between the collection of evidence items.
C. Clothing should be dried if possible and stored separately in plastic bags.
D. Foreign objects should be removed using gloves or rubber-tipped forceps.
2. Where (on the body) you swab for evidence is influenced most significantly by:
A. Evidence collection kit directions
B. Patient History
C. Hospital/facility protocol
D. National Protocol for evidence collection
3. Time frames guiding the collection of forensic evidence vary from state to state and currently range
from:
A. 24 – 48 hours
B. 48 – 72 hours
C. 72 – 120 hours
D. 72 hours - 1 week (7 days)
4. During an examination of a suspect you find additional evidence that could be of value to the
investigation, but is not covered in the search warrant, you should:
A. Gather the additional evidence as it is pertinent to the case
B. Only collect what is specified on the search warrant
C. Gather the additional evidence and have the warrant amended after-the-fact
D. Inform the officer of additional evidence and see if he/she can get the search warrant amended.
5. What are the aspects of pharmacokinetics?
A. Liberation, absorption, distribution, metabolism and excretion
B. Distribution, metabolism, and excretion
C. Liberation, absorption, distribution, catabolism and metabolism
D. Absorption, distribution, metabolism and excretion
E. Absorption, distribution and excretion
6. Which of the following statements most accurately describes the transfer of evidence in maintaining the
Chain of Custody?
A. Every transfer of evidence from person to person must be documented
B. Only transfers of evidence which involve movement from facility to facility must be documented
C. Health care workers are involved in collecting evidence, not the transfer of evidence.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
199
D. Maintaining the Chain of Custody is a law enforcement issue and thus does not pertain to health
care workers.
7. During World War I, Edmond Locard advocated for the application of scientific methods to criminal
investigation. His work became the cornerstone of forensic sciences and is commonly referred to as:
A. Locard’s Evidence Principle
B. Locard’s Exchange Principle
C. Locard’s Contact Principle
D. None of the above
8. What are the challenges associated with drug-facilitated sexual assault (DFSA) investigations?
A. Early reporting, under-reporting, evidence collection and laboratory methodologies
B. Delayed reporting, under-reporting, drug dosage, pharmacokinetics, pharmacodynamics, evidence
collection and laboratory methodologies
C. Delayed reporting, over-reporting, drug dosage, pharmacokinetics, evidence collection
D. Early reporting, under-reporting, drug dosage, pharmaceutical formulation, pharmacokinetics,
laboratory methodologies
E. Delayed reporting, over-reporting, drug dosage, Chain of custody.
9. Define pharmacodynamics:
A. What the body does to a drug when it enters our system and the speed at which this takes place.
B. The effects of drugs on the body
C. The speed at which the body processes drugs
D. How the body processes a drug when it enters our system
E. The speed at which we will recognize the effect of drugs on the body
10. Anonymous evidence collection:
A. Allows evidence to be collected and stored for a specified amount of time while the victim decides
whether or not to report the crime.
B. Allows evidence to be collected, stored and used by law enforcement to investigate similar cases in
the future.
C. Refers to evidence collected during a suspect examination.
D. Does not require informed consent prior to collection.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

200
Module VIII: Documentation
1. When documenting a patient’s behavior it is best to (choose the most accurate statement):
A. Characterize the patient’s behavior (i.e., patient is hysterical)
B. Interpret patient’s behavior (i.e., patient is acting irrationally as a result of trauma)
C. Describe patient’s behavior (i.e., patient is sobbing uncontrollably when describing events).
D. None of the above
2. In documenting body surface injury, the SAFE should be sure to document injury (check all that apply):
A. Type – laceration, abrasion, etc.
B. Location – where on the body
C. Color
D. Age
E. Size
3. All of the following clinical impressions or diagnoses related to sexual assault are considered
acceptable, except:
A. Alleged sexual assault
B. Sexual assault by history
C. Rule out sexual assault
D. No genital trauma on exam
4. According to the World Health Organization professional documentation includes all forms of
documentation recorded by a clinician in the provision of patient care. This can include (please choose
all that apply):
A. Check lists
B. Personal reflections
C. Incident reports
D. Images (photographs and diagrams)
E. Facsimiles
F. E-mails
G. Audio and video tapes
H. Electronic records
I. Written records
5. All of the following statements regarding documentation are true, except:
A. The patient’s name should be included on every page of the chart.
B. The healthcare provider should sign every page of the chart.
C. A Stricken through “O” is not an acceptable abbreviation.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
201
D. It is okay to leave a question blank if it does not apply to the patient’s situation.
6. Contemporaneous documentation refers to:
A. The documentation of events which occurred at the time of the assault, usually completed by first
responder
B. The documentation of current factors affecting patient behavior
C. The documentation of findings as care is given
D. The collaborative documentation of findings by all care givers on the team.
7. Medical records/clinical documentation should reflect the 10 “C’s” of professional documentation and
be:
A. Clear, concise, coded, compliant, contemporary, collaborative, confidential, complete, consensual
and collegiate
B. Clear, concise, complete, contemporary, consecutive, correct, comprehensive, collaborative,
patient centered, and confidential.
C. Clear, confidential, complete, contemporary, contextual, coded, patient centered, collegiate and
conclusive.
D. Clear, complete, confidential, compliant, contextual, compliant, coded, cursory, collaborative and
conclusive.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
202
Module IX: Medical management
1. When it comes to laboratory testing, specificity refers to:
A. The likelihood a test will be positive when disease is present
B. The likelihood a test will be negative when disease is present.
C. The likelihood a test will be negative when disease is not present.
D. The likelihood a test will be positive when disease is not present.
2. If left untreated ________________ is a major cause of pelvic inflammatory disease, tubal infertility,
ectopic pregnancy and chronic pelvic pain.
A. Chlamydia
B. Human papilloma virus
C. Gonorrhea
D. Trichomoniasis
3. The CDC's recommended treatment for uncomplicated Gonorrhea is:
A. Ceftriaxone 125MG IM in a single dose
B. Ceftriaxone 250 MG IM in a single dose
C. Ceftriaxone 125 MG IM plus 400MG Cefixime orally
D. Ceftriaxone 250 MG IM Plus 1GM Azithromycin orally
4. The exact mechanism of action of levonorgestrel emergency contraception is unknown
A. True
B. False
5. The three most common adverse events reported by women who had taken levonorgestrel for
emergency contraception were (choose all that apply):
A. Headache
B. Delayed menses
C. Heavier menstrual bleeding
D. Nausea
E. Lower abdominal pain
6. Routine testing for Syphilis following sexual assault is recommended
A. True
B. False
7. It is estimated that ___ percent of sexually active adults are infected with genital HPV during their
lifetime.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
203
A. 10
B. 25
C. 40
D. 50
8. The percentage of persons seropositive for HSV-2 antibody and have not been diagnosed with genital
herpes.
A. 10%
B. 40%
C. 70%
D. 90%
9. In severe PID, women will present with (choose all that apply):
A. Fever
B. Elevated WBCs
C. Purulent Vaginal discharge
D. Elevated erythrocyte sedimentation rate
10. A major indicator of primary syphilis infection is:
A. Condylomata acuminate
B. Chancre
C. Smooth papules
D. Flat papules
11. The CDC's recommended treatment for uncomplicated Chlamydia is (check all that apply):
A. Azithromycin 1 GM orally in a single dose
B. Ceftriaxone 125MG IM in a single dose
C. Doxycycline 100 MG orally twice a day for 7 days
D. Cipro 1GM orally in a single dose
E. Erythromycin 500 MG orally four times a day for 7 days
12. Routine testing for Hepatitis B following sexual assault is recommended.
A. True
B. False
13. When it comes to laboratory testing, sensitivity refers to:
A. The likelihood a test will be positive when disease is present.
B. The likelihood a test will be negative when disease is present
C. The likelihood a test will be negative when disease is not present.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
204
D. The likelihood a test will be positive when disease is not present.
14. The preferred(gold standard) test used to diagnosis herpes if genital ulcers/lesions are present is:
A. Viral Culture
B. Antigen Detection
C. Cytology
D. Polymerase Chain Reaction (PCR) assays
15. The incubation period preceding symptomatic infection for Syphilis is:
A. 0-14 days
B. 0-30 days
C. 0 days to 3 months
D. 10 days to 3 months
16. An infection of the uterus, fallopian tubes and other reproductive organs that causes lower abdominal
pain is most commonly referred to as:
A. Chlamydia
B. Gonorrhea
C. Trichomoniasis
D. Pelvic Inflammatory Disease
17. According to the CDC, which are the most frequently diagnosed infections among women who have
been sexually assaulted (Choose all that apply):
A. Bacterial vaginosis
B. Chlamydia
C. Gonorrhea
D. Syphilis
E. Trichomoniasis
18. The most common diagnosis associated with symptoms of vaginitis (vaginal discharge, vulvar itching
and irritation, and vaginal odor) is:
A. Vulvovaginal candidiasis
B. Chlamydia
C. Bacterial vaginosis
D. Trichomoniasis
19. The most common pathogens associated with Pelvic Inflammatory Disease are:
A. Trichomoniasis and Bacterial Vaginosis
B. Chlamydia and Gonorrhea
C. Trichomoniasis and Chlamydia
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
205
D. Gonorrhea and Herpes
20. Sexual Assault patient's should be counseled with regard to (check all that apply):
A. Behaviors that contributed to the sexual assault
B. Alcohol use
C. Symptoms of STD's and the need for an exam if they occur
D. Abstinence from sexual intercourse until STD treatment is complete
21. If the female patient complains of lower abdominal pain, the provider should (check all that apply):
A. Check the patient's temperature
B. Check for vaginal or cervical discharge
C. Test for STD's
D. Treat presumptively for PID
22. Treatment of genital warts should be guided by:
A. Patient preference
B. Available Resources
C. Experience of the Health Care Provider
D. B and C
E. All of the Above
23. The incubation period preceding symptomatic infection for Herpes is:
A. 0-5 days
B. 1-14 days
C. 2-12 days
D. 5-28 days
24. What is believed to be the mechanisms of action of levonorgestrel emergency contraception (choose
all that apply);
A. Preventing ovulation
B. Preventing fertilization
C. Inhibiting implantation
D. Aborting an implanted fertilized egg
25. The incubation period preceding symptomatic infection for Chlamydia is:
A. 2-14 days
B. 7-21 days
C. 7-28 days
D. 0-3 months
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
206
26. Preferred testing method for Gonorrhea and Chlamydia are:
A. NAAT (Nucleic Acid Amplification Tests)
B. Gram Stain with Culture and Sensitivity
C. Wet Mount/Wet Prep
D. Serology
27. The CDC's recommended treatment for Trichomoniasis is (choose all that apply):
A. Metronidazole 1 GM orally in a single dose
B. Metronidazole 2 GM orally in a single dose
C. Tinidazole 1 GM orally in a single dose
D. Tinidazole 2 GM orally in a single dose
E. Metronidazole 500 MG orally twice a day for 7 days
28. In consensual sex, the risk for HIV transmission from vaginal intercourse is
A. 0-0.1%
B. 0.1-0.2%
C. 0-1%
D. 1-2%
29. The CDC's recommended treatment for secondary Syphilis is
A. Ceftriaxone 1 GM IM in a single dose
B. Benzathine Penicillin G 2.4 million units IM in a single dose
C. Ceftriaxone 250 MG IM in a single dose
D. Benzathine Procaine Penicillin 2.4 million units IM in a single dose
30. Levonorgestrel is more effective at preventing pregnancy than the Yuzpe method of emergency
contraception.
A. True
B. False
31. The CDC recommends that HIV Post Exposure Prophylaxis be started no later than what time frame
following sexual assault:
A. Within 1 hour
B. Within 24 hours
C. Within 48 hours
D. Within 72 hours
32. HIV Post Exposure therapy was associated with a reduced risk of acquiring HIV in what population
(choose all that apply)
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
207
A. Sexual assault victims
B. Pregnant women
C. Health care workers
D. Animal studies
33. The incubation period preceding symptomatic infection for Gonorrhea is:
A. 1-14 days
B. 7-14 days
C. 7-28 days
D. 0-3 months
34. If HIV Post Exposure Prophylaxis if offered, which of the following should the provider discuss with the
patient (choose all that apply):
A. The unproven benefit and known toxicities of antiretrovirals;
B. The importance of close follow-up;
C. The benefit of adherence to recommended dosing;
D. The necessity of early initiation of Post Exposure Prophylaxis to optimize potential benefits
35. The CDC's recommended treatment for Bacterial Vaginosis is (choose all that apply):
A. Metronidazole 500 MG orally twice a day for 7 days
B. Metronidazole 2 GM orally in a single dose
C. Metronidazole Gel 0.75% intravaginally once daily for 5 days
D. Clindamycin 900 MG orally in a single dose
E. Clindamycin Cream 2% intravaginally at bedtime for 7 days
36. For a sexual assault patient, the CDC recommends:
A. Routine culturing for STD's
B. Culturing for STD's on a case by case basis
C. Culturing for Gonorrhea and Chlamydia only due to prevalence
D. Avoiding culture when possible
37. In consensual sex, the risk for HIV transmission from receptive rectal intercourse is up to:
A. 1%
B. 2%
C. 3%
D. 5%
38. If the patient chooses to receive HIV Post Exposure Prophylaxis, HIV antibody testing should be
conducted at which of the following intervals (choose all that apply):
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
208
A. Initial treatment
B. 6 weeks following start of treatment
C. 3 months following start of treatment
D. 6 months following start of treatment
39. The CDC suggests the following with regard to prophylactic treatment of the sexual assault survivor:
A. Hepatitis B vaccine with HBIG if the patient has never been vaccinated
B. Hepatitis B vaccine without HBIG if the patient has never been vaccinated
C. Hepatitis serology to determine patient's exposure status
40. Routine testing for HIV following sexual assault is recommended.
A. True
B. False
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

209
Module X: Program and operational issues
1. The Emergency Medical Treatment and Labor Act (EMTALA) was passed in 1986 as part of the
Consolidated Omnibus Budget Reconciliation Act (COBRA) and is sometimes referred to as the:
A. Anti-dumping Statute
B. Anti-Labor Statute
C. Do no Harm Statute
D. Emergency Screening Statute
2. All states have a designated SAFE Coordinator who is charged with ensuring that SAFE training is
occurring in conjunction with state recommendations.
A. True
B. False
3. All of the following statements regarding Medical Screening Exams (MSEs) are true, except:
A. MSE’s must rule out an Emergency medical condition
B. All facilities receiving Medicare funding must conduct an MSE
C. Triage Care provided in an emergency care department is equivalent to the MSE
D. MSEs can be conducted by RNs if bylaws and policies addressing this role are in place.
4. A SAFE is covered by his/her facility’s malpractice insurance and should not carry his/her own
malpractice policy.
A. True
B. False
5. Of the following types of research, _________ are considered the most rigorous.
A. Systemic Reviews
B. Randomized Controlled Clinical Trials
C. Meta-Analyses
D. Cohort Studies
6. Evidence-Based Practice (EBP) is the integration of __________ in the clinical decision making
process (choose all that apply):
A. Clinical expertise
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
210
B. Self- evaluation
C. Patient values and preferences
D. Best research evidence
E. Facility policies and procedures
7. Under which of the following circumstances may a registered nurse conduct the medical screening
examination:
A. The registered nurse may not ever conduct a medical screening examination.
B. The registered nurse may conduct a screening examination only when a physician is unavailable.
C. The registered nurse may conduct a medical screening examination under specific circumstances
outlined in policy and institutional bylaws.
D. A medical screening examination is not necessary in sexual assault.
8. Sustainability of SAFE programs are influenced by (check all that apply):
A. Staff transitions
B. Political agendas
C. Social issues
D. Economic issues
E. Scientific breakthroughs
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
211
Module XI: Justice System
1. Defensible practice includes (choose all that apply)
A. Clinical experience
B. Current research
C. Malpractice insurance
D. Accepted practice standards
2. Which of the following should you do to prepare for testimony (choose all that apply)
A. Update your resume/CV
B. Review your record
C. Review your pictures
D. Meet with your attorney
3. Who is considered the Trier of Fact in a criminal case (choose all that apply)
A. The defense attorney
B. The prosecuting attorney
C. The judge
D. The jury
4. In a criminal sexual assault case, who is bringing suit against the accused
A. The accusing victim
B. The victim’s family
C. The government
D. The prosecuting attorney
5. A SAFE may be called as a witness in which of the following circumstances (choose all that apply):
A. A child custody hearing
B. A civil sexual assault suit
C. A criminal sexual assault suit
D. A military court martial
6. It is possible that the victim will not be required to give testimony in a criminal sexual assault case.
A. True
B. False
7. In preparing for testimony, you will want to know (choose all that apply)
A. Who is subpoenaing you
B. What type of case it is (civil vs. criminal)
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
212
C. Where you will need to go for testimony
D. Whether you are testifying as a fact or expert witness
E. What counsel wants from your testimony
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
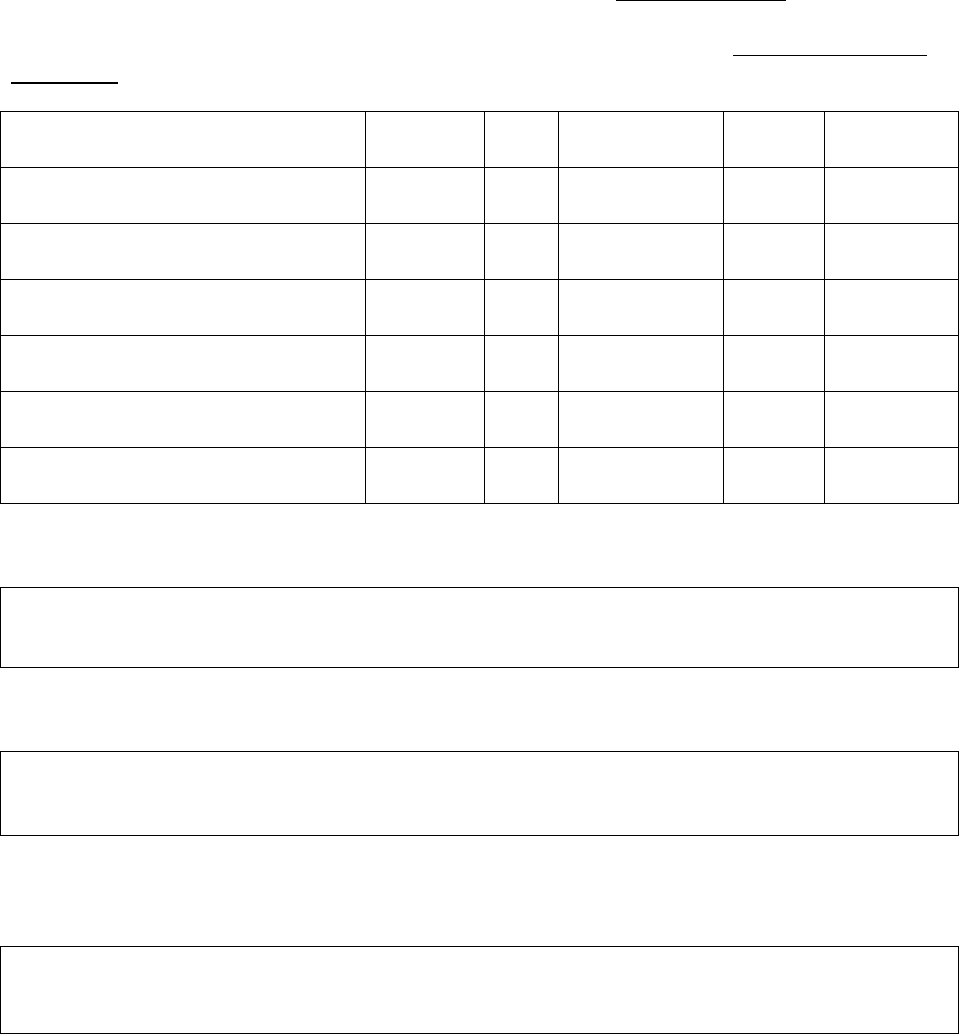
213
APPENDIX C3: Student Post-Training Online Survey
Section I: Feedback on the Online Didactic Component of the Training
The survey will begin with questions to seek your feedback about the online component of the training.
This next part of this survey will ask a few questions about your opinions about the online component of
the training. Please click on the answer that best reflects your opinion.
Strongly
Agree
Agree
Neither Agree
or Disagree
Disagree
Strongly
Disagree
a. There was enough time to learn the
material.
1
2
3
4
5
b. The topics were covered adequately.
1
2
3
4
5
c. The weekly discussion board helped
me understand the material better.
1
2
3
4
5
d. The online training met my
expectations.
1
2
3
4
5
e. I learned a considerable amount
during the online training.
1
2
3
4
5
f. I am satisfied with the amount I have
learned in this course.
1
2
3
4
5
What helped you learn the online course materials?
2
What, if anything, hindered your ability to learn the online course material?
What topics do you wish would have been covered in more detail during the online component of the
training?
2
The open-ended questions in this survey were removed for the quantitative data analysis and therefore do not appear in the
SPSS data file.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

214
It is common for some topics to be more difficult to learn or grasp than others. Which modules did you have
the most difficult time learning or grasping? What do you think made it difficult to learn those particular
modules?
What recommendations would you suggest for improving the online component of the training?
Section II: Training Activities
The next set of questions focus on the activities that you did during the course. Please indicate the extent
to which you agree or disagree with these statements.
All of the
Time
Most of the
Time
Some of the
Time
None of the
Time
a. I read all of the material assigned for the
course.
1
2
3
4
b. I did the recommended homework
assignments.
1
2
3
4
c. I read the postings in the weekly
discussion board.
1
2
3
4
d. I put a good deal of effort into learning
the material.
1
2
3
4
On average, how many hours did you devote to the training each week? ________
It would also be helpful to understand if you sought materials or training that was not a part of the IAFN
training.
Did you read materials that were not part of the assigned readings? Yes No
Did you attend other forensic examiner trainings that were not a part of the IAFN training? Yes No
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

215
How many pelvic exams have you performed…?
a. prior to the training
none
1-5
6-10
11-15
More than 15
b. since the training ended
none
1-5
6-10
11-15
More than 15
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
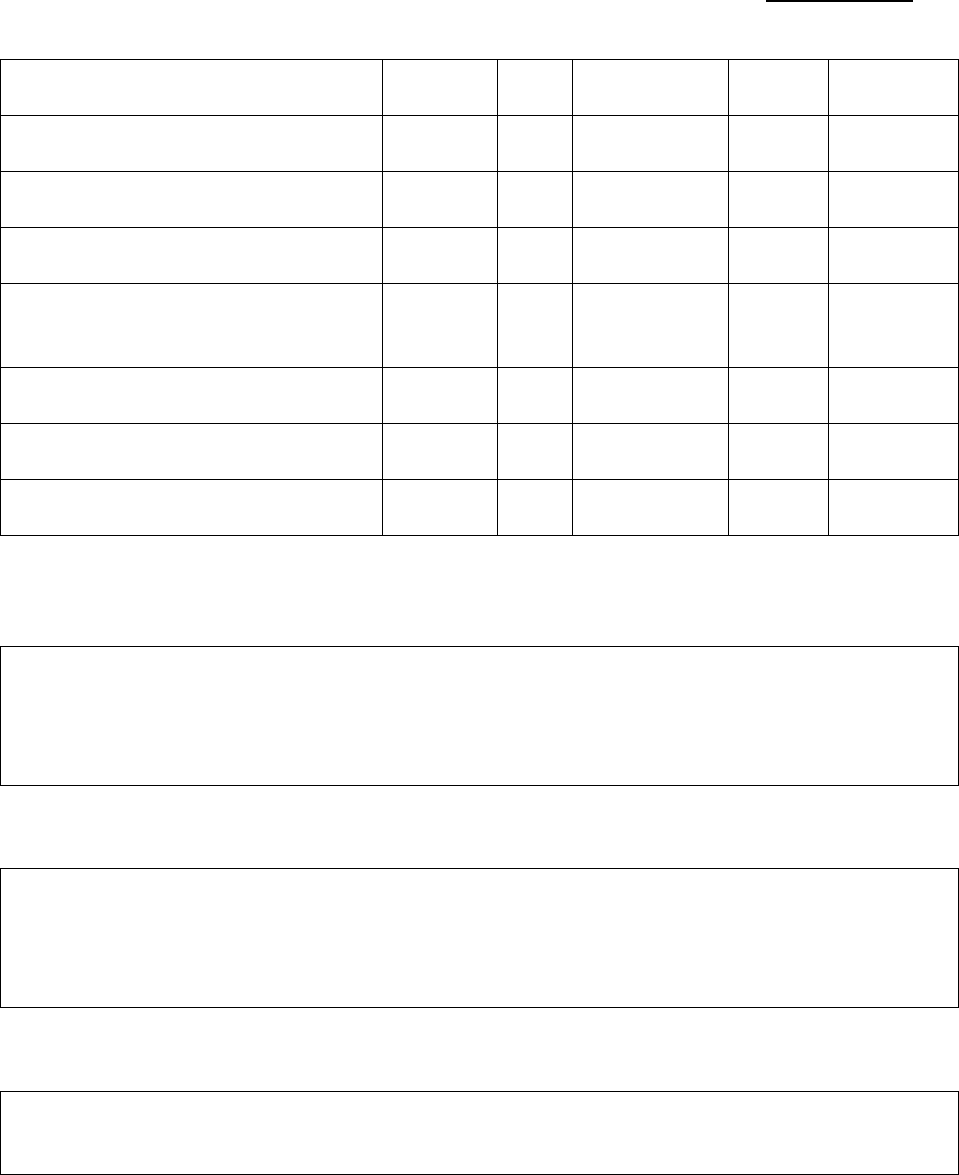
216
Section IV: Feedback on the Two-Day Clinical Training
12. This next part of this survey will ask a few questions about your opinions about the two-day clinical
training. Please click on the answer that best reflects your opinion.
Strongly
Agree
Agree
Neither Agree
or Disagree
Disagree
Strongly
Disagree
a. The pacing of the clinical training was
satisfactory.
1
2
3
4
5
b. The clinical concepts were covered
adequately.
1
2
3
4
5
c. There was enough time to ask
questions during the clinical training.
1
2
3
4
5
d. There was enough time to practice
different components of the medical
forensic exam.
1
2
3
4
5
e. The clinical training met my
expectations.
1
2
3
4
5
f. I learned a considerable amount during
the clinical training.
1
2
3
4
5
g. The clinical training helped me feel
more confident as a forensic examiner.
14. What helped you learn during the clinical training?
15. What, if anything, hindered your ability to learn during the clinical training?
16. What topics do you wish would have been covered in more detail during the clinical training?
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

217
17. It is common for some topics to be more difficult to learn or grasp than others. What topics did you have
the most difficult time learning or grasping during the clinical training? What do you think made it difficult to
learn those particular topics?
18. What recommendations would you suggest for improving the clinical training?
The final section of the survey is a small selection of test questions from the modules. It is important to
understand if you were able to retain the knowledge gained in this training.
Question 19: The primary focus of the SAFE should be __________________.
A. Collecting forensic evidence
B. Determining if the patient is telling the truth
C. Attending to patient healthcare needs
D. Assisting law enforcement in determining the facts of the case
Question 20: People with disabilities are usually sexually assaulted by someone known to them.
A. True
B. False
Question 21: A code of ethics is ________ (check all that apply):
A. Makes explicit the primary goals, values and obligations of the profession
B. Defines the rules under which providers may practice
C. Outlines appropriate provider behavior
D. Is mandatory in all health professions
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

218
Question 22: Warning signs that a trauma exposure response has occurred include (check all that
apply):
A. Helplessness
B. Hypervigilance
C. Reactive Engagement
D. Addictions
E. Complex Disrealism
F. Grandiosity
Question 23: The single most important thing an advocate can do is:
A. Provide support during the exam
B. Assist the victim in regaining a sense of control
C. Prevent law enforcement from bullying the victim
D. Provide transportation when needed
Question 24: If a victim asks an advocate to leave the room, the advocate should:
A. Leave the room, inform other members of the team that the victim does not wish to have an
advocate present and leave the facility.
B. Stay in the room, the victim is in shock and doesn’t really mean what she is saying.
C. Leave the room as requested, but continue to advocate on behalf of the victim with other team
members and/or by providing support to the victim’s family members.
D. Explain to the victim that her job requires her to stay with the victim throughout the examination
process and therefore she cannot leave.
Question 25: The primary concern of the law enforcement first responder arriving at the scene
where a sexual assault has just occurred should be:
A. Ensuring the safety of the victim
B. Finding the perpetrator
C. Conducting an in depth interview with the victim
D. Collecting evidence to assure prosecution
Question 26: The Role of the Detective in a sexual assault case does NOT include:
A. Conduct a comprehensive interview with the victim
B. Direct the investigative response
C. Screen out cases where prosecution is not justified nor in the public interest
D. Ensure that evidence is collected and the chain of custody is maintained.
E. Package all information regarding the case into a casebook for the prosecution.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

219
Question 27: The prosecutor’s primary responsibility is in representing the interests of the victim.
A. True
B. False
Question 28: All of the following are characteristics associated with lacerations, EXCEPT:
A. Jagged edges
B. Results from blunt force trauma
C. Bridging of tissue
D. Deeper than it is wide
Question 29: The physiological damage that occurs with strangulation can be the result of (choose
all that apply):
A. Cardiac arrhythmias
B. Lack of blood flow to the brain
C. Increase of blood in the brain
D. Lack of oxygen to the brain
Question 30: Tanner Staging is (choose all that apply):
A. A tool used to assess secondary sex characteristic development
B. Divided into 4 phases for males and 5 for females
C. Used to estimate chronological age
D. Divided into 5 phases
E. Based upon developmental changes in Caucasians
Question 31: Of the following questions, all are relevant to the sexual assault history taking
process, EXCEPT:
A. When did the assault occur?
B. Did you know your assailant?
C. What was your assailant wearing?
D. Was there vaginal, anal or oral penetration?
E. What was the gender of your assailant?
Question 32: Sexual assault history taking and forensic interviewing are synonymous.
A. True
B. False
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

220
Question 33: Using the concept of an analog clock to identify genital landmarks, the Fossa
Navicularis and Posterior Fourchette are found at:
A. 3 o'clock
B. 6 o'clock
C. 9 o'clock
D. 12 o'clock
Question 34: Genital injury sustained during sexual assault is most commonly seen:
A. Between 3 and 6 o'clock
B. Between 6 and 9 o'clock
C. Between 3 and 9 o'clock
D. At 12 o'clock
Question 35: A camera should be positioned:
A. Perpendicular or at 90 degree angle over the injury
B. At a 45 – 60 degree angle from the injury to visualize the edges of an injury.
C. At a 180 angle when trying to capture a protruding injury
D. All of the above
Question 36: Which of the following statements most accurately describes the transfer of evidence
in maintaining the chain of custody?
A. Every transfer of evidence from person to person must be documented
B. Only transfers of evidence which involve movement from facility to facility must be documented
C. Health care workers are involved in collecting evidence, not the transfer of evidence.
D. Maintaining the Chain of Custody is a law enforcement issue and thus does not pertain to health
care workers.
Question 37: Of the following statements, which does not adhere to the rules of evidence
collection:
A. Gloves should be powder free.
B. Gloves should be changed between the collection of evidence items.
C. Clothing should be dried if possible and stored separately in plastic bags.
D. Foreign objects should be removed using gloves or rubber-tipped forceps.
Question 38: Define pharmacodynamics:
A. What the body does to a drug when it enters our system and the speed at which this takes place.
B. The effects of drugs on the body
C. The speed at which the body processes drugs
D. How the body processes a drug when it enters our system
E. The speed at which we will recognize the effect of drugs on the body
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

221
Question 39: All of the following clinical impressions or diagnoses related to sexual assault are
considered acceptable, except:
A. Alleged sexual assault
B. Sexual assault by history
C. Rule out sexual assault
D. No genital trauma on exam
Question 40: All of the following statements regarding documentation are true, except:
A. The patient’s name should be included on every page of the chart.
B. The healthcare provider should sign every page of the chart.
C. A Stricken through “O” is not an acceptable abbreviation.
D. It is okay to leave a question blank if it does not apply to the patient’s situation.
Question 41: Routine testing for Syphilis following sexual assault is recommended.
A. True
B. False
Question 42: Levonorgestrel is more effective at preventing pregnancy than the Yuzpe method of
emergency contraception.
A. True
B. False
Question 43: The incubation period preceding symptomatic infection for Herpes is:
A. 0-5 days
B. 1-14 days
C. 2-12 days
D. 5-28 days
Question 44: When it comes to laboratory testing, sensitivity refers to:
A. The likelihood a test will be positive when disease is present.
B. The likelihood a test will be negative when disease is present
C. The likelihood a test will be negative when disease is not present.
D. The likelihood a test will be positive when disease is not present.
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
222
Question 45: In consensual sex, the risk for HIV transmission from vaginal intercourse is:
A. 0-0.1%
B. 0.1-0.2%
C. 0-1%
D. 1-2%
Question 46: When it comes to laboratory testing, specificity refers to:
A. The likelihood a test will be positive when disease is present
B. The likelihood a test will be negative when disease is present.
C. The likelihood a test will be negative when disease is not present.
D. The likelihood a test will be positive when disease is not present.
Question 47: Treatment of genital warts should be guided by (choose all that apply):
A. Patient preference
B. Available Resources
C. Experience of the Health Care Provider
D. B and C
E. All of the Above
Question 48: The CDC's recommended treatment for uncomplicated Chlamydia is (check all that
apply):
A. Azithromycin 1 GM orally in a single dose
B. Ceftriaxone 125MG IM in a single dose
C. Doxycycline 100 MG orally twice a day for 7 days
D. Cipro 1GM orally in a single dose
E. Erythromycin 500 MG orally four times a day for 7 days
Question 49: Evidence-Based Practice (EBP) is the integration of __________ in the clinical
decision making process (choose all that apply):
A. Clinical expertise
B. Self- evaluation
C. Patient values and preferences
D. Best research evidence
E. Facility policies and procedures
Question 50: In a criminal sexual assault case, who is bringing suit against the accused
A. The accusing victim
B. The victim’s family
C. The government
D. The prosecuting attorney
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
223
APPENDIX C-4: Clinical Instructor Interview Protocol
Participant ID Number _____________________ Interviewer ID Number_________________
Date Interview Conducted __________________ Length of Interview ___________________
INTRODUCTION AND OVERVIEW
As we talked about before, this interview will take approximately 90 minutes to complete.
The purpose of this interview is to learn more about your experience with implementing the hybrid online
didactic/in-person clinical training and lessons learned. We would also like to hear your thoughts about how
the training program can be improved.
I really appreciate your willingness to talk with me today and share your experiences. The information you
provide will be extremely helpful.
If it’s ok with you, I would like to tape record this interview. It’s going to be hard for me to get everything
down on paper, so the tape can help me later on filling in anything I might have missed. The only other
people who might listen to this tape will be the project supervisors. When the project is done, the tape will
be destroyed. May I tape record our discussion?
Everything we discuss today is private and confidential—your name will not be connected to anything you
say. Your name is not on this interview or the tape.
As we’re going through the interview, if you need to take a break or stop, just let me know. If there are any
questions that you don’t want to answer, just say so, and I will move on to the next section. You do not
have to answer all of the questions in this interview.
Before we get started I need to get your consent to be interviewed (go through procedures to obtain
informed consent).
Do you have any questions before we start?
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

224
Section I: Perceptions of Trainee Success and Challenges
There are two parts to this survey. First, we will focus on the training participants and their successes and
struggles during the training. If you use examples, please do not use anyone’s name.
1. This first question focuses on the retention and attrition of trainees. What do you think influenced
some trainees to drop the training? What do you think influenced trainees to complete the training?
A. What would need to be different to improve retention?
2. What do you think helped the trainees succeed in the training? What do you think led some
trainees to struggle with the training?
A. What did the trainees struggle with?
B. What would need to be different to help with these challenges?
Section II: Perceptions of Training Success and Challenges
In this second part, we will focus on the training itself and discuss the successes and challenges of
implementing a hybrid training.
3. What do you think went well with the development, coordination, and delivery of the didactic
portion of the training?
4. What challenges did you encounter in designing, coordinating, and delivering the didactic portion
of the training?
A. What did you need in order to help with these challenges?
5. What do you think went well with the development, coordination, and delivery of the two-day
clinical training?
6. What challenges did you encounter in designing, coordinating, and delivering the two-day clinical
training?
A. What did you need in order to help with these challenges?
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
225
7. What are the lessons learned from implementing the training?
A. What would you do differently?
8. What recommendations would you suggest for improving the training or overall project?
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
226
APPENDIX C-5: Student Interview Protocol
Participant ID Number _____________________ Interviewer ID Number_________________
Date Interview Conducted __________________ Length of Interview ___________________
INTRODUCTION AND OVERVIEW
As mentioned earlier, this interview will take approximately 60 minutes to complete.
The purpose of this interview is to gain your feedback about the training and your needs since you have
begun working as a sexual assault forensic examiner. We would also like to hear your thoughts about how
the training program can be improved.
I really appreciate your willingness to talk with me today and share your experiences. The information you
provide will be extremely helpful.
If it’s ok with you, I would like to tape record this interview. It’s going to be hard for me to get everything
down on paper, so the tape can help me later on filling in anything I might have missed. The only other
people who might listen to this tape will be the project supervisors. When the project is done, the tape will
be destroyed. May I tape record our discussion?
Everything we discuss today is private and confidential—your name will not be connected to anything you
say. Your name is not on this interview or the tape.
As we’re going through the interview, if you need to take a break or stop, just let me know. If there are any
questions that you don’t want to answer, just say so, and I will move on to the next section. You do not
have to answer all of the questions in this interview.
Before we get started I need to get your consent to be interviewed (go through procedures to obtain
informed consent).
Do you have any questions before we start?
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

227
Background
To help ground the interview, I am going to begin the interview by asking a few questions about your
experiences with sexual assault patients SINCE you have finished the training.
1. Since you have finished the training, have you examined any sexual assault patients? (check all
that apply)
Yes, pediatric
Yes, adolescents
Yes, adults
No
If no: have you had an opportunity to observe another clinician examine a sexual assault
patient? Yes No
2. Are you still working as a sexual assault forensic examiner?
A. Yes, go to Section I
B. No, go to question 3
3. What led to your decision to stop working as a sexual assault forensic examiner?
Section I: Clinical Training
First, we will focus on the clinical training that occurred in Colorado. This is a unique component of SAFE
trainings and we would like to understand its added value.
4. If the IAFN decided to do this training again, would it be important for them to include the two-day
clinical training? Why or why not?
5. If you had taken the online training without the two day clinical training, what would be different
about you? For example, what would be different about your knowledge, skills, or feelings of
preparedness?
6. We would also like feedback about the clinical instructors. What were some of the things they did
that were helpful and some of the things that were not helpful?
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.

228
Section II: Documentation
We are going to switch gears now and discuss the training content focused on documentation. Many
training participants indicated that they would have liked more information about documentation.
7. In thinking about what the training covered on documentation, what was particularly helpful to you?
8. What additional information did you want about documentation or what information would you have
liked covered more in-depth?
9. For those who have examined patients: Have you had a supervisor or colleague review your
documentation? What was their feedback about your documentation?
Section III: Patient Care
Many training participants also indicated that they would have liked more information about interacting with
patients so our final part of the interview will focus on interacting with patients.
10. In thinking about what the training covered about interacting with patients, what was particularly
helpful to you?
11. What additional information did you want about interacting with patients or what information would
you have liked covered more in-depth?
12. Based on what you learned in the training, what do you think is the best way to approach a patient?
What did you learn about how to make the patient more comfortable?
[Ask the next set of questions if the participant has had patients or observed another clinician]:
We only have a few questions left. One way to understand the helpfulness and utility of the training is by
discussing your experiences with sexual assault patients since the training. First, I am going to ask you
about an experience with a patient that went well and how the training did or did not help you with that
patient. Then I am going to ask you about an experience with a patient that did not go as well and how the
training did or did not help you with that patient. Please do not use your patients’ name.
13. Tell me about an experience with a patient that went well
A. What did you learn in the training that helped with this patient or situation?
B. Were there things that you wished that the training covered that could have helped you
with the case?
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
229
14. Tell me about an experience with a patient did not go so well
A. Were there things that you wished that the training covered that could have helped you
with the case?
B. What did you learn in the training that helped with this patient or situation?
15. Now that you are practicing, is there anything that has surprised you about forensic work that you
wished was covered more during the training?
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
230
APPENDIX D: MODULES
This document is a research report submitted to the U.S. Department of Justice. This report has not
been published by the Department. Opinions or points of view expressed are those of the author(s)
and do not necessarily reflect the official position or policies of the U.S. Department of Justice.
