WHAT WE HAVE LEARNED
FROM
THE
AIDS EVALUATION OF
STREET OUTREACH PROJECTS
A SUMMARY DOCUMENT
DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
Atlanta, Georgia 30333
CDC
CENTERS FOR DISEASE CONTROL
AND PREVENTION

Copies of this publication can be obtained by
writing Office of Communications, NCHSTP
Centers for Disease Control and Prevention
1600 Clifton Road, N.E., Mailstop E-06
Atlanta, GA 30333
faxing 404–639–8628
or calling NCHSTP Voice Information System
1–888–232–3228
Press 2, 5, 1, and 1 as prompted
and request
What We Have Learned from AESOP.

W
HAT
W
E
H
AVE
L
EARNED
FROM
THE
AIDS E
VALUATION
OF
S
TREET
O
UTREACH
P
ROJECTS
A S
UMMARY
D
OCUMENT
Edited by
Judith B. Greenberg, PhD
Division of STD Prevention
and
Mary S. Neumann, PhD
Division of HIV/AIDS Prevention
National Center for HIV, STD, and TB Prevention
Centers for Disease Control and Prevention
Atlanta, Georgia
1998

S
ITE
C
OLLABORATORS
Agency Principal Investigator
ADAPT, New York Daniel Fernando, PhD
Children’s Hospital Michele Kipke, PhD
of Los Angeles
County of Los Angeles John Schunhoff, PhD
Department of Anna Long, PhD,
Health Services Project Director
Georgia Department Claire Sterk, PhD
of Human Resources
Philadelphia Health Rose Cheney, PhD
Management Corporation
San Francisco Department Alice Gleghorn, PhD
of Public Health
University of Illinois, Chicago Wayne Wiebel, PhD
School of Public Health Bob Nettey, MD,
Project Director
Victim Services Agency, Helene Lauffer
New York Michael Clatts, PhD,
Co-Investigator
CDC Collaborators
John E. Anderson, PhD, Coordinator
Judith Greenberg, PhD, Project Officer
Robin MacGowan, MPH, Project Officer
Jo Valentine, MSW, Project Officer
Other CDC Contributors
Linda Kay, MPH
May Kennedy, PhD
Mary Spink Neumann, PhD
Lloyd Potter, PhD
John Santelli, MD
Kathy Stark, BS
Linda Wright-DeAgüero, PhD
A
CKNOWLEDGMENTS
The editors thank Marie Morgan, from the Division of HIV/AIDS
Prevention, for her hours of collaboration with stylistics, layout,
and proofing of the many iterations of this manuscript. We also
thank Lynda Doll, PhD, and T. Stephen Jones, MD, from the Divi-
sion of HIV/AIDS Prevention–Intervention Research and Support,
for their detailed comments on earlier versions.

C
ONTENTS
Introduction
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 1
Annotated Bibliography
- - - - - - - - - - - - - - - - - - - - - - 9
Articles
A Probability Sampling for Assessing the
Effectiveness of Outreach for Street Youth
- - - - - - - - -17
Michele D. Kipke, Susan O’Connor, Burke Nelson,
and John E. Anderson
A Storytelling Model Using Pictures for HIV
Prevention with Injection Drug Users
- - - - - - - - - - - -29
Anna Long, Judith Greenberg, Gladys Bonilla,
and Ronald Weathers
Elements of an Intensive Outreach Program for
Homeless and Runaway Street Youth in
San Francisco
- - - - - - - - - - - - - - - - - - - - - - - - - - -47
Alice A. Gleghorn, Kristen D. Clements, and
Marc Sabin
Association between Self-Identified Peer-Group
Affiliation and HIV Risk Behaviors among
Street Youth
- - - - - - - - - - - - - - - - - - - - - - - - - - - -61
Michele D. Kipke, Jennifer Unger, Raymond Palmer,
Ellen Iverson, and Susan O’Connor
Enhanced Street Outreach and Condom Use
by High-Risk Populations in Five Cities
- - - - - - - - - - -83
John E. Anderson, Judith Greenberg, and
Robin MacGowan
Products and Contacts for
Intervention Replication
- - - - - - - - - - - - - - - - - - - - 111

1
I
NTRODUCTION
The AIDS Evaluation of Street Outreach Projects (AESOP) was a 5-
year study designed by the Centers for Disease Control and Pre-
vention (CDC) in collaboration with researchers representing
agencies at eight sites. This cooperative study, which included
community-based organizations and health departments, was
conducted from October 1991 through September 1996. Its pur-
pose was to support studies to describe outreach services to injec-
tion drug users (IDUs) and youth in high-risk situations, calculate
the costs of such services, and develop and evaluate enhanced on-
the-street services for these populations. Collaborators at five of
the eight sites (Atlanta, Chicago, Los Angeles, New York, and Phil-
adelphia) focused on outreach to IDUs. At three sites (Los Ange-
les, New York, and San Francisco), the focus was youth.
M
ETHODS
The research was conducted in several phases. During the
forma-
tive phase
of approximately 1 year, the sites conducted the com-
munity assessment process (CAP) to gain maximum information
about the targeted community, including how services were deliv-
ered to these populations, and to develop specific enhancements
to outreach that could be delivered on the street to the same pop-
ulations. To assist the staff at the sites, CDC collaborated with
LTG Associates, Inc., a private contractor, to adapt the community
identification (CID) method. This method included interviews with
groups of persons who interacted with the target population as
well as interviews with members of the population themselves. A
detailed description of CID can be found in Tashima, 1966. Using
the formative research, sites developed interventions plus a design
for evaluating them.
After the formative phase, AESOP entered the
evaluation phase
.
A quasi-experimental design (a study and a comparison area) was
used for each of the eight communities. Each area was to have
adequate numbers of the target group and some ongoing level of
street outreach. Cross-sectional, closed-ended surveys of the target
populations in the control and comparison areas were conducted

AESOP
2
before and after the development and implementation of interven-
tion enhancements. These surveys measured risk behavior, expo-
sure to outreach, and readiness for behavioral change. Staff at
each site conducted at least two preenhancement rounds of inter-
views at intervals of approximately 3 months between January
and August of 1993 and two postenhancement rounds between
1994 and 1995, once the enhancements had been fully imple-
mented for at least 3 months.
Sampling of IDUs and youth was conducted so that it would be as
representative as possible; interviews were conducted at locations
frequented by these populations. Researchers in each city identi-
fied and defined primary sampling units (PSUs) within the study
and comparison areas. The PSUs could be of two types: fixed sites
(shelters, meal programs, drop-in centers) and on-the-street sites
(congregating areas; drug-buying, or "copping," areas; shooting
galleries). The PSUs were observed at multiple times of the day to
determine the relative number of potential respondents at each
site. The number of interviews to be obtained from each PSU was
set to be proportional to this measure of size. If the sample con-
tained fixed sites (e.g., drop-in centers, shelters) and on-the-street
locations, a predetermined percentage of interviews were set for
fixed and on-the-street domains. Interviewing within PSUs was
systematically scheduled by time of day and day of week so that
all relevant times would be represented. Within PSUs, respon-
dents were selected by using systematic methods, such as select-
ing every n
th
potential respondent by predetermined counting.
Once persons were selected, a screening questionnaire was
administered to determine eligibility, and the complete question-
naire was administered to those who were eligible.
E
NHANCEMENTS
AESOP enhancements differed by site because of the diversity of
participating outreach programs, geographic diversity, and the
inclusion of youth and IDUs. Enhancements were focused on the
outreach workers and encompassed a wide range of strategies:
increased training (e.g., training in stages of change, training in
the finger-stick method for HIV testing); additional resources such

I
NTRODUCTION
3
as a storytelling model with pictures for engaging the clients in
risk assessment (see article by Long et al. in this monograph),
referral tracking cards and incentive packages; a mobile van;
improved direct supervision; improvements in recordkeeping of
the delivery of outreach services and referrals; coordination of out-
reach services with other agencies at a particular site; expanded
services, including the addition of specialized staff such as a refer-
ral specialist; a storefront location for more comprehensive ser-
vices to youth (see article by Gleghorn et al. in this monograph);
changes in selection criteria for hiring outreach workers or super-
visors; and social and emotional support to minimize burnout.
Three to seven enhancement strategies were developed at each
site. Quality assurance procedures were developed for on-the-
street monitoring of outreach workers to ensure that enhance-
ments were being delivered as intended.
Eligible IDUs were defined as persons within the geographical
boundaries of the study areas who had injected illegal drugs in the
past 3 years. At three sites with lower numbers of IDUs —Atlanta,
Los Angeles, and Philadelphia—up to 30% of the sample were
allowed to be persons who had used crack cocaine within the past
month. Eligibility for youth was based on age (12 to 23 years) and
lack of permanent residence (recurrently without shelter during
the past year or without permanent shelter during the past 2
months) or use of the street economy for support (drugs, prostitu-
tion, panhandling, crime).
B
EHAVIORAL
E
PIDEMIOLOGY
K
EY
F
INDINGS
1. The initial rounds of survey research indicated that the AESOP
populations engaged in much higher levels of sexual risk
behavior than the levels found in general population surveys.
2. After AESOP enhancements, the percentages of those who had
used condoms during their most recent intercourse ranged
from 57.9% to 71.8% for casual partners. Those percentages
approach the year 2000 health objectives: 50% for unmarried
sexually active persons, 60% for sexually active women aged

AESOP
4
15 to 19 years, 75% for sexually active men aged 15 to 19
years, and 60% for IDUs. Rates for steady, or main, partners
remained low.
3. Among the high-risk populations studied, the highest rate of
condom use was observed for anal sex, followed by vaginal and
oral sex.
4. Outreach workers from a variety of agencies reached a size-
able percentage of IDUs in their communities and supported
them in seeking medical care, especially in seeking counseling
and testing for HIV and treatment for drug use. One third to
two thirds of respondents who had seen an outreach worker
from any program in the preceding 6 months reported having
received referrals for these two services. One third to one half
of respondents reported that they then sought these services.
5. In addition to sexual practices, street youth are at risk
through high rates of drug use that includes sharing of
syringes.
6. Youth in contact with street outreach are much more likely to
have sought health care, HIV counseling and testing, or treat-
ment for a sexually transmitted disease (STD) or for substance
use than are youth who are not in contact with street out-
reach.
7. Among street youth, a history of STD is significantly associated
with current substance use and having multiple sex partners.
8. Homelessness and crack use are associated with lower levels
of stage of change for not sharing needles.
9. IDUs are more likely to report safer drug behavior than safer
sex behavior and tend to be at a higher level of stage of change
for not sharing needles than for condom use.
I
MPLICATIONS
FOR
R
ESEARCHERS
1. Cross-sectional data on street populations do not reveal the
time frame or process by which persons become acculturated
to and integrated into the street economy, which includes
trading of sex and drugs. The degree to which clients are

I
NTRODUCTION
5
acculturated and the length of time they have been on the
street may influence their willingness or ability to change their
behaviors.
2. Research should be planned separately for street populations
of youth and IDUs (e.g., separate goals for interventions, sepa-
rate questionnaires, and separate intervention enhancements).
3. Many factors can affect the delivery of services to street popu-
lations – weather, police activity, riots, changes in laws, urban
relocation because of special events, even the death of a cul-
tural icon, such as Jerry Garcia of the Grateful Dead band.
After Garcia’s death, large numbers of youthful
Deadheads
disappeared from the San Francisco street scene. These fac-
tors should be recorded as they happen, and they should be
considered in data analysis.
4. Surveys of target populations frequently measure only the
elimination of risk behaviors (e.g., ceasing substance use) and
often do not consider reductions in risks (e.g., not injecting in
shooting galleries) or preparations to change (e.g., intention to
buy bleach). Including such gradations of change in surveys
can provide more sensitivity in measuring behavior change at
the community level.
5. The effects of dosage or number of exposures to outreach and
of rates at which innovations diffuse in communities are impor-
tant variables to measure in community-level interventions.
6. Measures of reduced risk can become outmoded during a
study (e.g., guidelines for bleaching needles changed during
AESOP), and research methods should be flexible enough to
allow for this.
7. In studying homeless populations, investigators should in-
clude length of time homeless as a variable.
I
MPLICATIONS
FOR
S
ERVICE
A
GENCIES
1. High percentages of street populations reported contact with
outreach workers, although many reported continued high-
risk behaviors. For many persons, street outreach may not be
sufficient for behavioral change.

AESOP
6
2. Among street youth, substance use and having multiple sex
partners are significantly associated with a history of STD;
therefore, in a clinical setting, an STD diagnosis for a person
from this population may be a marker for other high-risk sex
and drug-using behaviors.
O
UTCOME
E
VALUATION
K
EY
F
INDINGS
1. Theory-based street outreach approaches can be used by
trained indigenous outreach workers.
2. Evaluation of street outreach programs is inherently difficult
and requires multiple approaches.
3. There are several types of street outreach, ranging from brief
contacts to more in-depth encounters between workers and
clients.
4. Street outreach can be an effective mechanism for referring
high-risk persons to treatment.
5. Street outreach distribution programs can affect condom use
by high-risk populations.
a. Having a condom at the time of interview was the strongest
and most consistent predictor of condom use at most recent
intercourse.
b. Obtaining condoms from outreach workers was indirectly
associated with condom use because this factor was
strongly related to carrying a condom.
c. Higher level of stage of change (consideration or intention)
for condom use by persons who do not use condoms is
linked to outreach exposure.
6. Costs of street outreach can be measured: at the AESOP sites,
the costs, relative to the medical costs of AIDS cases, were low.
If 2 of 10,000 contacts reduced their high-risk behavior so as
to avoid HIV transmission, outreach would yield a net benefit.

I
NTRODUCTION
7
7. Among the AESOP sites, the average cost of outreach contact
for high-risk youth was nearly twice that for IDUs. Much of
the increased cost was for facilities (e.g., drop-in centers) and
materials (e.g., food, travel vouchers, hygiene kits).
8. Outreach workers from a variety of agencies reach a sizeable
percentage of IDUs in their communities and support them in
seeking medical services, especially in seeking HIV counseling
and testing and drug treatment.
I
MPLICATIONS
FOR
S
ERVICE
A
GENCIES
1. Street outreach can be expanded to include a variety of ser-
vices, including HIV counseling and testing on the street, the
use of varied theory-based interventions (e.g., staging clients
for risk-reduction messages), even advocacy.
2. Since the interpersonal dynamics of steady and casual sexual
partnerships are different, condom promotion messages
should be tailored to the type of sexual relationship the client
has.
3. After-care referrals, such as support groups and drug coun-
seling services, need to be emphasized to accommodate the
high numbers of IDUs exiting drug treatment.
F
UTURE
R
ESEARCH
Q
UESTIONS
1. Is street outreach more effective with certain types of drug
users (e.g., on the basis of consumption method or drug of
choice)?
2. What types of sex take place at different venues (e.g., vaginal
sex at crack houses, oral sex at adult bookstores, anal sex at
parks)?
3. Which is the antecedent: drug use or prostitution? Does the
antecedent differ by ethnicity, age, or sex?

AESOP
8
Reference
Tashima, N., Crain, C., O’Reilly, K.R., & Sterk-Elifson, C. (1966).
The community identification (CID) process: A discovery
model.
Qualitative Health Research,
6, 23-48.

9
A
NNOTATED
B
IBLIOGRAPHY
B
EHAVIORAL
E
PIDEMIOLOGY
(F
INDINGS
FROM
B
ASELINE
I
NTERVIEW
D
ATA
)
Anderson, J.E., Cheney, R., Clatts, M., Faruque, S., Kipke, M., Long,
A., Mills, S., Toomey, K., & Wiebel, W. (1996). HIV risk
behavior, street outreach and condom use in eight high-risk
populations. AIDS Education and Prevention, 8(3), 191-204.
The populations surveyed engaged in high levels of sexual risk
behavior: 20% to 46% reported two or more sex partners in the
past month. Most of the injection drug users and high-risk
youth were at risk through unprotected sex with main part-
ners; 56% to 75% reported protected vaginal sex with casual
partners. Of this group, 58% to 84% had been tested for HIV
infection, compared with 25% of the national adult population.
Having a condom at time of interview was the most consistent
predictor of condom use during most recent intercourse. A
variable percentage of injection drug users had shared needles
in the past month (10% to 53%). Many respondents had been
in contact with street outreach programs and had received
condoms, bleach, and other materials from workers.
Anderson, J.E., Cheney, R., Faruque, S., Long, A., Toomey, K., &
Wiebel, W. (1996). Stages of change for HIV risk behavior:
Injecting drug users in five cities. Drugs and Society, 9(1/2), 1-17.
Respondents from the street-based samples interviewed at the
five AESOP sites that were focused on injection drug users had
a very high level of risk for HIV, in terms of sex and drug-using
risk behavior. The level of stage of change for condom use was
higher for casual partners than for main partners. Having a
condom at interview was the most consistent predictor of
respondent’s level of stage of change for condom use. Home-
lessness and crack use were associated with lower level of stage
of change for not sharing needles. Program staff need to be
aware of the predominant level of readiness to change in order
to design and implement effective programs.

AESOP
10
CDC. (1993). Assessment of street outreach for HIV prevention—
Selected sites, 1991-1993. MMWR, 42 (45), 873, 879-880.
This report is a description of the first 2 years of the AESOP
project and includes results from the initial round of closed-
end interviews. Results indicated that 17% to 65% of injection
drug users and 23% to 46% of youth in high-risk situations
(YHRS) reported talking with an outreach worker; 14% to 58%
of IDUs and 11% to 26% of YHRS had received HIV prevention
literature; 16% to 58% of IDUs and 22% to 39% of YHRS had
received free condoms; and 13% to 55% of IDUs and 7% to
10% of YHRS had received bleach kits from outreach workers.
These findings suggest that IDUs and YHRS can be identified
and reached through outreach programs; will talk with
outreach workers about HIV prevention; and will accept HIV
prevention literature, materials, and referral services from
outreach workers.
Clatts, M.C., Bresnahan, M., Davis, W.R., Springer, E., & Backes, G.
(1997). The harm reduction model: An alternative approach to
AIDS outreach and prevention for street youth in New York City.
In P. Ericson et al. (Eds.), Harm reduction: A new direction for
drug policies and programs. Toronto: University of Toronto Press.
The authors provide a demographic and behavioral profile of
street youth in New York City and discuss the history of AIDS
prevention services for these young people. A network of
outreach programs developed for AESOP, the Youth At Risk
Cooperative, and the foundation for the network’s training
program for outreach workers in the harm reduction model
are described. Case study material from staff who integrated
the model into case management activities provides a con-
structive demonstration of the potential of the harm reduction
model as a service-delivery strategy for street youth.

ANNOTATED BIBLIOGRAPHY
11
Clements, K., Gleghorn, A., Garcia, D., Katz, M., & Marx, R. (1997).
A risk profile of street youth in northern California: Implications
for gender-specific human immunodeficiency virus prevention.
Journal of Adolescent Health, 20(5), 343-353.
Most of the youth were heterosexual, white, male, and without
stable housing. Of the total, 60% had had vaginal sex in the
past 30 days; only 44% had used a condom during their most
recent sexual encounter. One third of the sample reported
having injected drugs. Compared with males, females were
equally likely to use injection and noninjection drugs but were
more likely to be sexually active, to have been given a
diagnosis of a sexually transmitted disease, and were less
likely to report consistent condom use. Females without
stable housing were less likely to have used condoms during
their most recent vaginal intercourse. These findings suggest
an urgent need for gender-specific prevention efforts and
increased housing options for youth.
Gleghorn, A.A., Marx, R., Vittinghoff, E., & Katz, M. (in press).
Association between drug use patterns and HIV risks among
homeless, runaway, and street youth in Northern California.
Drug and Alcohol Dependence.
The drug use and HIV risk behaviors of homeless, runaway,
and street youth were compared. Youth who were using any
heroin, speed, or cocaine exhibited more sexual risks than did
youth who were not using; primary stimulant users and those
who used a combination of heroin and stimulants showed
greatest sexual risk. Those who injected combinations of
heroin and stimulants engaged in higher levels of risky
injection practices, including frequent injections and back-
loading syringes, than did primary heroin or primary
stimulant injectors. HIV prevention interventions should be
tailored to drug-use patterns, because youth who use
combinations of heroin and stimulants may require more
intensive services.

AESOP
12
Kipke, M.D., O’Connor, S., Palmer, R., & MacKenzie, R.G. (1995).
Street youth in Los Angeles: Profile of a group at high risk for
human immunodeficiency virus infection. Archives of Pediatric
and Adolescent Medicine, 149(May), 513-519.
Of the youths, 70% were sexually active (average of 11.7 sex
partners during past 30 days). High-risk sex and drug-using
behaviors were prevalent and interrelated in this sample of
urban street youth. Substance-using youth were 3.6 times
more likely to use drugs during sex, 2.2 times more likely to
engage in survival sex, and 2.5 times more likely to report a
sexually transmitted disease. Youth with multiple partners
were more likely to report a previous sexually transmitted
disease and survival sex. New and innovative educational
promotions and prevention interventions for this population
are needed.
Kipke, M.D., Palmer, R.F., LaFrance, S., & O’Connor, S. (1997).
Homeless youths’ descriptions of their parents’ childrearing
patterns. Youth and Society, 28, 415-431.
No one parenting style was associated with homelessness
among the sample. An equal percentage of youth reported
having supportive or emotionally available and having
intrusive or emotionally unavailable parents or caretakers.
However, most of the youth enrolled in this study did report
having parents or caretakers who could be described as
intrusive, emotionally unavailable, detached, and who had
problems with substance use or the law. Gaining a better
understanding of family conflict and its relationship to
homelessness and the behaviors of homeless youth is critically
needed to develop effective prevention interventions as well as
appropriate services.

ANNOTATED BIBLIOGRAPHY
13
Kipke, M.D., Unger, J., O’Connor, S., Palmer, R.F., & LaFrance, S.R.
(1997). Street youth, their peer group affiliation and differences
according to residential status, subsistence patterns and use of
services. Adolescence, 32(127), 655-669.
Five street youth groups were identified: punks and
skinheads, druggies, hustlers, gang members, and loners. The
results demonstrated unique patterns with respect to places
where they stayed or slept, their means of support, and use of
services according to peer group affiliation.
Martinez, T.E., Gleghorn, A., Marx, R., Clements K., Boman, M., &
Katz, M.H. (1998). Psychosocial histories, social environment,
and HIV risk behaviors of injection and noninjection drug using
homeless youths. Journal of Psychoactive Drugs, 30 (1), 1-10.
Injection drug use is a common risk behavior for HIV infection
among homeless, runaway, and street youth. Youth who
injected drugs were more likely than youth who did not inject
drugs to report traumatic psychosocial histories, including
parental substance use and forced institutionalization, use of
alcohol and other noninjection drugs, a history of survival sex,
and the use of abandoned buildings as shelter. These findings
underscore the need for multifaceted service and prevention
programs to address the varied needs of these high-risk youth.
E
NHANCEMENTS
Cheney, R., & Merwin, A. (1995). Integrating a theoretical
framework with street outreach services: Issues for successful
training. Public Health Reports, 110(Suppl. 1), 1-5.
The authors discuss three key components necessary to
integrate a behavioral research perspective (in this instance,
the stages-of-change model) into the design of outreach
programs: (a) training for successful service delivery, (b)
training for a theory-guided intervention, and (c) feedback and
evaluation. The third component measures the benefits of
staff training to the outreach workers and to their ability to
apply in the field what they have learned.

AESOP
14
Valentine, J., & Wright-DeAgüero, L. (1996). Defining the
component of street outreach for HIV prevention – The contact
and the encounter. Public Health Reports, 111(Suppl. 1), 69-74.
The discussion suggests techniques for enhancing the
encounter between outreach workers and clients by using the
conceptual framework of the social-work helping relationship.
Five elements of the encounter are defined and developed:
screening, engagement, assessment, service delivery, and
follow-up. The encounter represents an enhancement of the
traditional street outreach interaction and a more systematic
approach to promoting the behavioral change goals of AESOP.
M
ETHODS
Clatts, M.C., Davis, W.R., & Atillasoy, A. (1995). Hitting a moving
target: The use of ethnographic methods in the development of
sampling strategies for the evaluation of AIDS outreach
programs for homeless youth in New York City. In E.Y. Lambert,
R.S. Ashery, & R.H. Needle (Eds.), Qualitative methods in drug
abuse and HIV research (NIDA Research Monograph 157, NIH
Publication No. 95-4025). Rockville, MD: National Institute on
Drug Abuse.
This chapter shows how ethnographic methods that include
participant observation and life history interviews were used
as a sampling strategy and a means of obtaining less
accessible information. Interviews included how youth met
everyday needs and consequently how they participated in the
street economy. In addition to identifying important
geographic and temporal gaps in services, the data provided
useful information about a population of youth about whom
little is known.

ANNOTATED BIBLIOGRAPHY
15
O
UTCOME
Gleghorn, A.A., Clements, K.D., Marx, R., Vittinghoff, E., Lee-Chu, P.,
& Katz, M. (1997). The impact of intensive outreach on HIV
prevention activities of homeless, runaway, and street youth in
San Francisco: The AIDS Evaluation of Street Outreach Project
(AESOP). AIDS and Behavior, 1(4), 261-271.
The authors evaluate the impact of an HIV prevention
intervention combining street outreach, storefront prevention
services, and subculture-specific activities for street youth in
intervention and comparison sites before and during
implementation of the intervention. Youth at both types of
sites reported high rates of risky sex and drug-using
behaviors. The intervention did not affect HIV risk behaviors
but was independently associated with increased contact with
outreach workers and increased referrals for services. Higher
levels of contact with outreach workers were associated with
following through with HIV-related referrals and using new
syringes. Youth-oriented needle exchange increased the use of
new syringes.
Greenberg, J., MacGowan, R., Neumann, M.S., Long, A., Fernando,
D., Cheney, R., Sterk, C., & Wiebel, W. (under review). The
relationship between street outreach referrals and accessing
medical services by injecting drug users. Health & Social Work.
This analysis, from 3,237 structured interviews conducted
with injection drug users (IDUs) at five sites between January
1994 and October 1995, examines contact with outreach
workers, the most common medical referrals received and
acted on as a result of this contact, and whether more
frequent contact was associated with increased acting on
medical referrals. Of the IDUs interviewed, 42% to 67% had
talked with an outreach worker in the past 6 months and
reported referrals to a number of medical services, especially
HIV counseling and testing and drug treatment. IDUs with
more than three contacts with outreach workers during the
past 6 months were more likely to seek services. To maximize
the effect of outreach on acting on referrals, training for
outreach workers should address techniques for follow-up
with referred IDUs; identifying and overcoming barriers to

AESOP
16
seeking medical services, especially those for minority clients;
after-care referrals for clients exiting drug treatment
programs; and the importance of treatment for sexually
transmitted diseases in reducing risk for HIV infection.
MacGowan, R.J., Sterk, C.E., Long, A., Cheney, R., Seeman, M., &
Anderson, J.E. (1998). New needle and syringe use and use of
needle exchange programmes by street recruited injection drug
users in 1993. International Journal of Epidemiology, 27, 302-
308.
Street-recruited injection drug users were interviewed in five
U.S. locations in 1993. Most (75% to 95%) reported that it was
easy to get a new syringe. For their most recent injection, 45%
to 77% had used a new syringe, and 2% to 18% had used a
syringe previously used by another injector. The use of needle
exchange programs (NEPs) ranged from 8% to 16% in Chicago,
Philadelphia, and Los Angeles County. Factors associated
with NEP use differed across sites, which suggests that the
dispersion of NEPs and the removal of legal barriers that
restrict access to sterile syringes may be more important to
increasing the use of sterile syringes and NEPs.
Wright-DeAgüero, L.K., Gorsky, R.D., & Seeman, G.M. (1996). Cost
of outreach for HIV prevention among drug users and youth at
risk. Copublished in Drugs and Society, 9 (1/2), 185-197; and
in T. Trotter II (Ed.), Multicultural AIDS prevention programs.
Binghamton, NY: Harrington Park Press.
The authors present the results of a cost analysis at eight sites
that provide outreach services to injection drug users and
street youth. They assessed the potential benefit of HIV
prevention through outreach services by comparing outreach
costs with the costs of treating an HIV-infected person. The
average cost of outreach services was $13.30 per contact.
Costs per contact were 78% higher for street youth than for
drug users. Comparing cost per contact with HIV treatment, if
only 2 in 10,000 outreach contacts reduce their risky behavior
to avoid the transmission of HIV, these programs compare
favorably with other HIV prevention strategies in terms of cost.

17
A PROBABILITY SAMPLING
FOR ASSESSING THE EFFECTIVENESS OF
OUTREACH FOR STREET YOUTH
Michele D. Kipke
*
, Susan O'Connor
*
, Burke Nelson
*
,
and John E. Anderson
†
In 1991, the Division of Adolescent Medicine of Children’s Hospital
Los Angeles received funding from the Centers for Disease Control
and Prevention (CDC) as part of the cooperative agreement for the
AIDS Evaluation of Street Outreach Projects (AESOP) (CDC, 1993).
The purpose of this project was to conduct research to character-
ize street youth and their involvement in HIV risk-related sex and
drug-using behaviors and to develop, implement, and evaluate the
enhancement of street outreach interventions for this population.
Few studies have evaluated the sex and drug-using behaviors of
urban street youths, and no attempt has been made to systemati-
cally evaluate the effectiveness of outreach activities for this popu-
lation. Furthermore, studies have largely relied on convenience
sampling, which may underestimate the degree to which these
youth are engaging in the kinds of behaviors that put them at risk
for HIV infection. For example, runaway or homeless youth have
been recruited from shelters and drop-in centers (Anderson,
Freese & Pennbridge, 1994; Rotheram-Borus & Koopman, 1991;
Rotheram-Borus et al., 1992).
Convenience sampling can identify only the youth who are using
services; thus, the findings from these studies can be generalized
only to youth who are willing to use such services, not the esti-
mated 65% of runaway or homeless youth who are living on the
streets and not using services (Kipke, O’Connor, Palmer &
LaFrance, 1993). Although probability sampling methods have
*Division of Adolescent Medicine, Children’s Hospital of Los Angeles, Los Angeles,
California
†
Division of HIV/AIDS Prevention–Intervention Research and Support, National
Center for HIV, STD, and TB Prevention, Centers for Disease Control and
Prevention, Atlanta, Georgia

AESOP
18
been used to survey homeless adults (Burnam & Koegel, 1988;
Robertson, Westerfelt & Irving, 1991), little effort has been made
to apply these sampling methods to homeless youth. To evaluate
the effectiveness of street outreach activities, it was essential to
develop probability sampling methods that enable researchers to
better describe youth, particularly out-of-school and out-of-home
youth who spend most of their time on the streets.
OBJECTIVES AND OVERVIEW OF SAMPLING DESIGN
Our objective was to recruit a sample representative of the target
population (i.e., to develop a method for selecting homeless youth
such that homeless youth at each site would have an equal or a
known probability of being selected for the sample). Numerous
researchers have relied on shelters for their sampling frame. How-
ever, there are several problems with this practice. First, although
some youth stay in shelters, many others move around frequently
and use shelters infrequently, if at all. Second, it is estimated that
there may be 2,000 homeless youth in Los Angeles County at any
time and that 10,000 homeless youth may be on the streets of Los
Angeles during any one year (United Way Planning Council, 1981).
In Los Angeles, approximately 140 shelter beds are available for
this population. Thus, the size of the population exceeds the size
of that shelter system. Finally, there are other services, such as
drop-in and meal services, that are used by a greater proportion of
the homeless youth population and with greater frequency than
are shelter services. Although shelters and drop-in services have
different biases, adding the latter to a sampling frame would
nevertheless be expected to increase the percentage of the total
population covered.
We understood, however, that constructing a sampling frame that
comprised only shelter and drop-in service locations would pose
similar problems. Perhaps the most important bias is that home-
less youth who do not use services would be excluded. Thus,
street and natural hangout locations would need to be included in
the sampling frame in order to identify the homeless youth who
were not using services. Although it is impossible to establish a
sampling frame that would include every homeless youth, we

A PROBABILITY SAMPLING
19
developed a sampling frame that included both service agency and
street locations in an effort to minimize bias and maximize our
ability to survey a wide spectrum of youth who were representative
of the target population.
SAMPLE POPULATION AND TARGET COMMUNITIES
The target population were youth who were 12 to 23 years of age
and who (a) had been living on the streets without their families
for 2 or more consecutive months or (b) were fully integrated into
the "street economy." By definition, youth integrated into the
street economy meet their subsistence needs through one or more
of the following survival strategies: prostitution or survival sex
(defined as the exchange of sex for money, food, a place to stay,
clothes, or drugs), pornography, panhandling, stealing, selling sto-
len goods, mugging, dealing drugs, or engaging in scams or cons.
A cross-sectional survey was conducted in two communities where
runaway or homeless youth were known to congregate: the Holly-
wood area of Los Angeles (the study community, where the
enhanced outreach interventions were introduced) and the down-
town area of San Diego (the control community). In both com-
munities, comparable sampling frames and recruitment strategies
were used to identify and survey street youth for the purpose of
evaluating the effectiveness of enhanced interventions for street
outreach. In this paper, we focus on the Hollywood sampling
frame and sampling units.
CONSTRUCTION OF SAMPLING
The sampling frames were constructed by using information
obtained during the community assessment process (CAP) and
from systematic field observation. The goal of this phase was to
identify high-volume locations and high-frequency times of the
day and days of the week for surveying the target population.
Information from the community assessment and field observa-
tions yielded (a) lists of street corners where the target population

AESOP
20
is known to hang out, (b) other locations where the target popula-
tion could be found (e.g., parks, alleys, restaurants), and (c) agen-
cies that provide shelter and drop-in services.
All service sites for runaway or homeless youth in Hollywood,
including two shelters and five drop-in centers, were included in
the “fixed” sampling frame. Drop-in centers included agencies
that provide day and night drop-in services to street youth in
Hollywood. During a 2-month period, field staff observed and
recorded the number of youth using these services according to
the day of the week and time of day.
Outreach workers and research interviewers conducted open-
ended interviews with street youth and observed street activity in
order to locate street hangouts with the highest number of home-
less youth and to determine the times and days when the volume
was highest. Along the boulevards of Hollywood, these staff first
identified 104 street corners or alleys, 4 parks, and 3 fast-food res-
taurants as potential sampling sites. Large segments of the main
boulevards were broken into 3-block segments. Thus, the number
of natural sites was reduced to 73 street corners, 4 parks, and 3
fast-food restaurants. Once hangouts were defined, field staff
noted street youth activity at these locations throughout the day.
Additional field observation was conducted, by the field research
team and outreach workers from service agencies for youth, in
order to further refine the street sampling frame. (Sample Street
Observation and Summaries of Service Use are in Appendix A.)
Given our broader definition of street youth (i.e., integrated into
the street economy) and the literature, which has largely relied on
samples recruited from shelter and drop-in centers, we chose to
oversample youth from natural and hangout sites by recruiting
70% of the sample from natural sites (thereby oversampling by
20% from these sites) and 30% from fixed sites.
SAMPLING ASSIGNMENTS
A computer program was developed to randomly select and order
locations for interviewing teams (comprising 2 to 4 members).
This program took into account two important aspects of the sam-

A PROBABILITY SAMPLING
21
pling design. First, with evidence that nearly 65% of street youth
are not using services, the selection was weighted to ensure that a
larger proportion of street locations were chosen (70%), thereby
increasing the probability of recruiting youth who were not using
services. Second, all fixed and natural locations in the pool of
potential sampling sites were proportionally weighted on the basis
of the number of youth that typically congregated at that location.
Thus, locations with a higher volume of youth had a greater prob-
ability of being selected by the computer random selection pro-
gram than had locations with lower volumes. Assignments also
were made according to high-frequency times of the day and days
of the week. Assignments were generated weekly.
SAMPLING UNITS AND SELECTION OF RESPONDENTS
F
IXED
S
ITES
Consistent with probability sampling methods used in surveying
homeless adults (Burnam & Koegel, 1988; Robertson, Westerfelt &
Irving, 1991), the overall sampling design for the fixed sites
involved estimating the relative proportions of the homeless youth
population that passed through the shelters and drop-in centers
in a month. These estimates were used to determine the relative
weighting for each agency. Sampling assignments to fixed sites
were weighted according to the type of service and the estimated
proportion of the study population that used the service in a
month (e.g., 13% of the street youth population are believed to use
sheltering services). Thus, in our study the probability of selection
was proportional to the estimated unduplicated number of youth
who used each service in a month. In Hollywood, three shelters
and five drop-in centers were identified.
For respondent selection at each of the fixed sites, interviewers
first reviewed the agency's sign-in roster to determine how many
youth were in the agency. Interviewers then randomly selected
potential respondents from the agency sign-in sheet. They used a
predetermined random start number and began selecting respon-
dents by using a sampling fraction (i.e., the number of youth to
count off, beginning with the random start-numbered youth on
the agency list). Going down the list, interviewers then selected

AESOP
22
additional youth on the list according to the sampling fraction.
The sampling fraction was determined by dividing the number of
youth signing into the agency by the number of interviewers; the
number of youth selected equaled the number of interviewers (see
the Sampling Fraction Table, Appendix B).
Interviewers then asked the intake worker to introduce them to
the selected respondents. If a potential respondent declined to
participate in the study, a new respondent was selected by choos-
ing the next consecutive youth on the list after the one who
declined. Replacement continued in this manner until all appro-
priate respondents were selected and agreed to be interviewed.
N
ATURAL
S
ITES
During the initial community assessment, teams compiled an
exhaustive list of natural street locations and hangouts along five
boulevards within a 12-square mile area of Hollywood. In select-
ing respondents, interviewer teams first determined the number of
potential respondents at a site specified by the sampling assign-
ment (i.e., in a block segment, on the street corner, in the alley or
park) by counting the number of youth who seemed to be 12 to 24
years of age at the location. They then determined the sampling
fraction by looking at the sampling fraction table and locating the
fraction that corresponded with the total number of youth counted
at that site. For example, if there were two interviewers and 10
potentially eligible youth at the site, the sampling fraction would
be 1/5. Youth were "counted out" (from left to right), starting from
a predetermined random start number and selected according to
the sampling fraction (see Appendix B). If the number of potential
respondents was equal to or fewer than the number of interview-
ers, all youth were approached and asked to complete a screening
instrument. As in sampling in fixed sites, a youth who refused to
participate in the study was replaced by the next consecutive
youth after the one who declined. On the street, this means
selecting the youth nearest and to the right of the refuser. Youth
who entered the sampling site after the initial selections were not
approached for recruitment.

A PROBABILITY SAMPLING
23
DISCUSSION
There are a number of advantages and disadvantages in using a
probability sampling design for street-based epidemiologic
research. Perhaps one of the greatest disadvantages is the cost
associated with developing and implementing such a design. A
community assessment of service agencies is required to estimate
accurately the number of youth who are using services. Extensive,
systematic field observations are required to initially identify natu-
ral sites. Relative weightings are then constructed on the basis of
population estimates. Ongoing observations are then required to
monitor the field to ensure that new hangouts are added and that
low-volume sites are continually dropped from the sampling
frame. Finally, this sampling design requires a greater amount of
time for recruitment and interviewing than would be required by
convenience sampling.
There are, however, clear advantages in using probability sam-
pling. Research involving representative samples of runaway or
homeless youth, particularly youth who are not using services,
has been greatly needed. These results can be generalized to the
larger street youth population of a study area. Probability sam-
pling is perhaps the best method for obtaining samples represen-
tative of the target population, hence for accurately estimating
population characteristics.
ACKNOWLEDGMENTS
This study was supported by the Centers for Disease Control and
Prevention, cooperative agreement U62/CCU907198. The views
expressed are those of the authors, not necessarily the funding
agency. Special thanks go to Judith Greenberg, Steven R.
LaFrance, Richard MacKenzie, Susanne Montgomery, Marjorie
Robertson, and members of the Los Angeles research team
(Michael Cohen, Marcus Kuiland-Nazario, Raymond Palmer, Sara
Parker, Audruin Pittman, German Rodriguez, and Lily Rodriguez).

AESOP
24
References
Anderson, J., Freese, T., & Pennbridge, J. (1994). Sexual risk
behavior and condom use among street youth in Hollywood.
Family Planning Perspectives, 26(1), 22-26.
Burnam, M.A., & Koegel, P. (1988). Methodology for obtaining a
representative sample of homeless persons: The Los Angeles
Skid Row Study. Evaluation Review, 12, 117-152.
CDC. (1993). Assessment of street outreach for HIV prevention—
Selected sites, 1991-1993. MMWR, 42(45), 873, 879-880.
Kipke, M.D., O'Connor, S.L., Palmer, R., & LaFrance, S. (1993,
October). Street youth, outreach and HIV risk: Facing the
challenge in two communities. Presented at American Public
Health Association meeting, San Francisco, CA.
Robertson, M.J., Westerfelt, A., & Irving, P. (1991, November).
Research note: The impact of sampling strategy on estimated
prevalence of major mental disorder among homeless adults in
Alameda County, CA. Presented at American Public Health
Association meeting, Atlanta, GA.
Rotheram-Borus, M.J., & Koopman, C. (1991). Sexual risk beha-
viors, AIDS knowledge, and beliefs about AIDS among run-
aways. American Journal of Public Health, 81, 208-210.
Rotheram-Borus, M.J., Meyer-Bahlburg, H.F.L., Rosario, M.,
Koopman, C., Haignere, C.S., Exner, T.M., Matthieu, M.,
Henderson, R., & Gruen, R.S. (1992). Lifetime sexual beha-
viors among predominantly minority male runaways and gay/
bisexual adolescents in New York City. AIDS Education and
Prevention, (Suppl. Fall), 34-42.
United Way Planning Council. (1981). Runaway youth situation in
Los Angeles County: A general overview. Los Angeles: The
United Way.

APPENDIX A
25
APPENDIX A
SAMPLE STREET OBSERVATION AND
S
UMMARIES OF SERVICE USE
STREET OBSERVATION SUMMARY
Hollywood Boulevard
10:00am
11:00 am
Noon
1:00 pm
2:00 pm
3:00 pm
4:00 pm
5:00 pm
6:00 pm
7:00 pm
Totals
Sycamore 2 2 0103
8
Orange 0 0 2010 3
Orchid 0 4 0320 9
Hillcrest 0 0 0006 6
Highland 3 5 2005 15
McDonald’s 2 4 0354 18
McCadden 0 1 3010 5
Las Palmas 0 7 0018 16
Cherokee 0 0 0047 11
Whitley 1 0 0000 1
Tomy’s 2 0 2313 11
Hudson 0 2 0317 13
Wilcox 0 0 0406 10
Cahuenga 0 0 0003 3
Ivar 2 2 1020 7
Vine 0 5 0003 8
El Centro 0 0 0200 2
Gower 2 2 0010 5
No. Sheets 3 4 0 1323
Totals 14 34 0 10 19 19 55

AESOP
26
HOLLYWOOD DROP-IN CENTERS
SUMMARY OF HIGH-VOLUME TIMES AND DAYS
Gay and Lesbian Community Services Center (GLCSC)
NOTES: I called GSCSC at 1:30 on 10/22, and there were 3 youth in the agency. I
was told that 2 to 5 had been in the agency all day. I suggest that we do not use
GLCSC as a fixed site for interviewing.
9:00 am
10:00 am
11:00 am
Noon
1:00 pm
2:00 pm
3:00 pm
4:00 pm
5:00 pm
Totals
Thu 10/1 220000110 6
Fri 10/2 51202210013
Mon 10/5 34411010014
Tue 10/6 131011100 8
Wed 10/7 31403210014
Thu 10/8 123020000 8
Fri 10/9 23104221015
Mon 10/12 41521010014
Tue 10/13 42205112017
Wed 10/14 41300113013
Thu 10/15 10601221013
Totals 30 20 31 3 20 11 12 8 0

APPENDIX A
27
Los Angeles Youth Network
NOTES: I called LAYN at 2:00 on 10/22, and there were 10 youth in the agency. I
was told that there had been many more earlier in the day but that most had gone
to the YMCA. I suggest that we use LAYN as a fixed site interiew location on Mon-
days and Wednesdays, any time between noon and 4:00pm.
9:00 am
10:00 am
11:00 am
Noon
1:00 pm
2:00 pm
3:00 pm
4:00 pm
5:00 pm
Totals
Thu 10/8 1546453200 39
Fri 10/9 1354323400 34
Mon 10/12 1837226240 44
Tue 10/13 1275231250 37
Wed 10/14 1812642550 43
Thu 10/15 1312362320 32
Totals 89 21 26 20 22 17 18 16 0

AESOP
28
APPENDIX B
SAMPLING FRACTION TABLE
AIDS Evaluation of Street Outreach Project
Children’s Hospital of Los Angeles
Street Locations Agencies
No. of
Youth
No. of
Intercepts Fraction
No. of
Youth
No. of
Intercepts Fraction
1 1 1/1 1 1 1/1
2 2 1/1 2 2 1/1
3 2 1/2 3 3 1/1
4 2 1/2 4 4 1/1
5 2 1/3 5 4 1/2
6 2 1/3 6 4 1/2
7 2 1/4 7 4 1/2
8 2 1/4 8 4 1/2
9 2 1/5 9 4 1/3
10 2 1/5 10 4 1/3
11 2 1/6 11 4 1/3
12 2 1/6 12 4 1/3
13 2 1/7 13 4 1/4
14 2 1/7 14 4 1/4
15 2 1/8 15 4 1/4
16 2 1/8 16 4 1/4
17 2 1/9 17 4 1/5
18 2 1/9 18 4 1/5
19 2 1/10 19 4 1/5
20 2 1/10 20 4 1/5
21 2 1/11 21 4 1/6
22 2 1/11 22 4 1/6
23 2 1/12 23 4 1/6
24 2 1/12 24 4 1/6
25 2 1/13 25 4 1/7

29
A STORYTELLING MODEL
USING PICTURES FOR HIV PREVENTION
WITH INJECTION DRUG USERS
Anna Long
*
, Judith Greenberg
†
, Gladys Bonilla
*
,
and Ronald Weathers
*
The importance of storytelling in the modeling of behavior and
teaching people about their lives has been extensively addressed
by the late Joseph Campbell, a foremost authority on mythology
(most recently, Campbell, 1988). Empirical research in the self-
help community also suggests the importance of personal stories.
Rappaport (1993) compared the personal stories told during meet-
ings of a mutual help group for mentally ill persons with the sto-
ries told by patients receiving professional care for mental illness.
The first group saw themselves as a part of a “caring and sharing”
community and as givers as well as receivers who hoped for posi-
tive change. By contrast, the patients’ stories “often revolve
around learning to see one’s self as sick and dependent on medi-
cation to control behavior.” Similarly, the stories that people tell
about their lives in groups such as Alcoholics Anonymous (AA)
permit the members to take on the ideology of the group as part of
their personal identities. Telling stories of “hitting bottom” and of
recovery serve as testimony to the importance of the AA philoso-
phy of sobriety (Bean, 1975).
Using this storytelling framework, investigators in Los Angeles
County, one of eight AESOP sites, developed a unique outreach
intervention strategy. Injection drug users (IDUs) were encour-
aged to tell their own stories about risk behaviors to outreach
workers after looking at a series of abstract illustrations related to
themes of risk and risk-prevention behaviors for acquiring HIV.
These illustrations were produced by a local Los Angeles artist,
*Office of AIDS Programs and Policy, Los Angeles County Department of Health
Services, Los Angeles, California
†
Division of STD Prevention, National Center for HIV, STD, and TB Prevention,
Centers for Disease Control and Prevention, Atlanta, Georgia

AESOP
30
whose grasp of the street drug culture was translated into draw-
ings that were used to encourage people to discuss risky sex and
drug-using behaviors.
CHOOSING THE STORYTELLING INTERVENTION
F
ORMATIVE
RESEARCH
The AESOP project began with a two-part formative study to guide
the identification of specific risk-reduction needs and correspond-
ing interventions for IDUs in Los Angeles County. Using data from
various sources (research on IDUs conducted in the county, epide-
miologic and drug-use data), we described the IDU population,
reported what was known about their risk behaviors, and specified
the current outreach programs that addressed their HIV risk-
reduction needs.
That initial overview revealed considerable variation in the num-
ber and the demographic characteristics of IDUs in the different
parts of the county. The IDUs were as diverse in their cultural
and ethnic backgrounds as the county’s 4,083 square miles are in
their geographic features. There were also variations in the pro-
grams that community-based organizations had developed to
respond to the needs of IDUs in their particular communities.
The community assessment process (CAP) constituted the second
part of the formative research. These activities focused on develop-
ing more current insight into the IDU population through in-depth
interviews with IDUs themselves; outreach workers; agency repre-
sentatives with knowledge of the IDU community, such as social
service workers and law enforcement officers; and persons who
interact with IDUs but are not part of the formal service delivery
system, such as shopkeepers, taxi drivers, and hotel clerks. The
interviews were focused on IDUs’ knowledge, attitudes, and beliefs
about HIV; sex and drug-using behaviors of IDUs and their risks
for HIV infection; risk-reduction practices of IDUs; assessment of
services used by IDUs; barriers and facilitators to service use; and
ideal intervention strategies.

A STORYTELLING MODEL
31
The CAP revealed the range of risk behaviors of the target popula-
tion. It showed that (a) despite considerable knowledge about HIV,
most IDUs required additional information and strategies that
would help them consistently practice appropriate risk-reduction
behaviors; (b) uniformity was lacking in attitudes toward and
intentions to reduce their risk for HIV; and (c) IDUs would not
change their risk behaviors, regardless of the information they
had about HIV, until they were ready. The notion of readiness
that echoed in many of the CAP interviews was a key factor in our
selecting the stages-of-change model from behavioral theory
(Prochaska & DiClemente, 1986, 1992; Prochaska, DiClemente &
Norcross, 1992) to help us develop the interventions. Finally, out-
reach workers and IDUs indicated a need for materials that would
be suitable for the prevention needs of different groups.
Overall, the formative research revealed that the proposed inter-
ventions should be (a) adaptable to the ethnic, cultural, and lin-
guistic diversity of Los Angeles County IDUs; (b) inexpensive and
reproducible enough to maximize the possibility of adoption by
outreach programs that serve IDUs; (c) comprehensive enough to
address the needs of IDUs across a spectrum of HIV awareness
and risk-reduction practices; (d) accessible enough to facilitate
HIV counseling and testing on-site; and (e) able to provide feed-
back on whether IDUs sought the services to which they were
referred.
Using the formative research, we designed an intervention with
three components: (a) storytelling allowing the outreach worker to
help the IDU recognize personal HIV risk behaviors and learn
about or reinforce intentions to reduce risk behaviors; (b) a referral
tracking system to help outreach workers follow up on the IDUs’
use of the services to which they were referred; and (c) an outreach
worker-administered HIV testing program that facilitated finger-
sticks on the street to enable outreach workers to test a target
population reluctant to seek this service in clinical settings.
R
ATIONALE
FOR
S
TORYTELLING
During the formative research, we routinely observed the setting
in which outreach workers delivered their services to IDUs. One
observation, consistent throughout the county, concerned the use

AESOP
32
of pictures as a common method of communicating ideas in the
communities where outreach was conducted. In many communi-
ties, particularly communities of color, murals, usually painted by
local artists, adorned the walls of public and private buildings,
cinder-block fences, and freeway overpasses. These murals
tended to be colorful, highly complex, and symbolic. Thus, the
use of visual art in the communities where outreach was con-
ducted was viewed as an important consideration in designing the
intervention. The fact that many IDUs mentioned the need for
new materials or for materials that better reflected their communi-
ties also influenced the design and format of the visuals. The need
for HIV interventions with an emphasis on cultural appropriate-
ness has been documented (Stevenson, McKee & Josar, 1995;
Weeks, Schensul, Williams, Singer & Grier, 1995). It was deter-
mined that the required pictures needed to be complex enough to
engage the viewer, to stimulate introspection, and to span the eth-
nic and cultural diversity of Los Angeles County IDUs. We
excluded written messages from the visuals so that the outreach
worker and IDU dyad could work together to develop a story for
each picture.
In contrast to the generic role-model stories used in CDC’s com-
munity demonstration projects for HIV prevention (McAlister,
1997), storytelling allowed the IDUs, assisted by outreach work-
ers, to generate their own stories from a set of illustrations. The
IDUs’ stories often told of specific risk behaviors that the IDU
might have been engaging in, the consequences of these behav-
iors, and risk-reduction strategies to be reinforced by the outreach
worker. The outreach worker would begin by asking the IDU what
was happening in a particular picture. Three key sentences were
used to help the IDU: “Tell me what is happening in the picture.”
“What are the people doing?” “What are they saying?”
R
ELATIONSHIP
OF
THE
S
TORYTELLING
M
ODEL
TO
L
EVEL
OF
S
TAGE
OF
C
HANGE
The storytelling also allowed the project to incorporate the theoret-
ical foundation of the stages-of-change model. Outreach workers
used the storytelling as a prelude to questions that specified each
of the five stages of change through which people typically
progress when changing behaviors: precontemplation, contempla-

A STORYTELLING MODEL
33
tion, ready-for-action, action, or maintenance. (See Fishbein and
Rhodes [1997] for how the stages-of-change model can be applied
in HIV prevention.) Once the clients had been placed in one of the
five stages, a clear and succinct risk-reduction message appropri-
ate for that stage was given.
DEVELOPING THEMES FOR STORYTELLING ILLUSTRATIONS
Because the formative research showed that condoms and bleach
continued to be used inconsistently, we designed the illustrations
to address three specific risk-reducing behaviors: (a) consistent
use of condoms, (b) consistent use of new injection equipment,
and (c) consistent bleaching of shared injection equipment. A
multistage process, drawing on the in-depth interviews with IDUs
in the second part of the formative research, was used to produce
the illustrations: (a) determining the IDUs’ view of the behaviors
that placed them at risk of contracting HIV; (b) identifying themes
in IDUs’ open-ended responses associated with risk-taking behav-
iors; (c) rating these themes for importance and applicability to
IDUs, by a sample of IDUs and outreach workers; (d) selecting
risk-behavior themes on which to focus the illustrations; (e) identi-
fication of an appropriate artist; (f) repeatedly testing sketches
with IDUs and then refining the illustrations; (g) producing final
illustrations; (h) training outreach workers to use the illustrations;
and (i) implementing and evaluating the intervention (see List 1).
Using the information from the CAP in-depth interviews with
IDUs, we selected 40 narrative themes. Many were the verbatim
statements of active IDUs. A convenience sample of 20 IDUs from
two communities closest to where the AESOP research would be
conducted and the outreach staff (10 in all) at two agencies serv-
ing these communities were asked to rate each of the 40 narrative
themes on three scales: (a) the degree to which the theme was
applicable to their community of IDUs; (b) the degree to which the
theme was important to their community; and (c) whether or not
the theme should be included in new materials. Feedback from
outreach workers was important because of their expertise in
working with the target population. On the basis of this review, sex
and drug themes were prioritized for inclusion in the illustrations.

AESOP
34
LIST 1
D
EVELOPING ILLUSTRATIONS FOR INTERVENTION
Characteristics of Ideal Intervention
1. Adaptable to multiple cultures and languages
2. Flexible to address clients’ range of needs and
preparedness
3. Inexpensive and easy to reproduce
Steps in Appropriate Interventions
1. Collect formative information on clients’ needs
and current interventions.
2. Use the comprehensive baseline report of HIV
epidemiology and drug use.
3. Conduct a community assessment of IDUs and
service agencies.
Development of Visuals
1. Survey IDUs to determine their perceived HIV
risk behaviors.
2. Recognize themes from IDUs open-ended responses.
3. Rate IDU themes by IDUs and outreach workers.
4. Select major risk-behavior themes.
5. Select and orient an artist.
6. Repeat field testing and refine illustrations.
7. Produce final illustrations.
8. Train outreach workers.
9. Implement and evaluate.

A STORYTELLING MODEL
35
P
RIORITY
T
HEME
FOR
S
EXUAL
B
EHAVIOR
The sex theme given highest priority by IDUs and outreach work-
ers was "My woman would be offended if I started talking about
condoms." This theme had been a consistent issue not only for
male but also for female IDUs and may have been related to the
lack of condom use during vaginal sex with main partners that
was consistently recorded in the Los Angeles AESOP survey data.
Conversations with IDUs and outreach workers had indicated that
(a) male IDUs were frequently concerned about using condoms
with their main partners because their partners might become
suspicious about their fidelity; (b) female IDUs were not always in
control of the decision to use condoms with main partners,
although they might have more control in using condoms with
casual partners; and (c) both men and women were concerned
about their partner’s possible reaction to their request to use con-
doms. Possibilities for addressing this theme in the storytelling
intervention were (a) increasing men's and women's awareness
that their partners may be equally concerned about the other's
perceptions of suggestions to use condoms and (b) modeling skills
used to discuss and negotiate condom use.
P
RIORITY
T
HEME
FOR
I
NJECTION
B
EHAVIOR
The injection theme that received the highest priority rating from
IDUs and outreach workers was “I use my own outfit [injection
equipment] most of the time.” The baseline survey data supported
this statement. Data indicated that most respondents had used a
brand-new outfit for their most recent injection or one that had
not been used by anyone else. However, 21% reported using a
shared needle "sometimes," "almost every time," or "every time"
they injected. Two of the remaining five priority themes related to
the availability of bleach or new injection equipment were "When
I'm sick, I can't waste time looking for bleach or a new outfit" and
"What do you do when there is no bleach around?"
Providing users with strategies for dealing with the theme of using
one’s own outfit most of the time was an important focus of the
storytelling model. The strategies included (a) reinforcing sole use
of an outfit; (b) reinforcing the desire to avoid situations in which
outfits are used by a group; and (c) examining other situations

AESOP
36
related to sharing, specifically, sharing when experiencing symp-
toms of withdrawal and sharing when one’s outfit is blocked or
otherwise nonfunctional, and developing strategies to avoid inject-
ing in those situations.
PRODUCING ILLUSTRATIONS
S
ELECTING
THE
A
RTIST
The intervention required the services of an artist who could pro-
duce illustrations similar to the indigenous art produced through-
out the county and who could visually represent the complexity of
the messages selected for focus. Once an artist whose work gener-
ated a similar feeling of depth, complexity, and engagement had
been found, the next challenge was to explain to the artist the
need for the materials and the messages to be conveyed.
We took him through a process to increase his understanding of
the risk behaviors that the target population engaged in and of the
barriers to risk reduction that IDUs faced. First, a session was
held to familiarize the artist with the statistics on Los Angeles
County IDUs. This included a discussion of the diversity of the
target population, variation in risk behaviors, and the critical
problems of the IDUs contacted during outreach. Second, written
stories based on the two priority themes were provided to the art-
ist to help him understand the narrative themes.
Several sketches were produced for the "I Don't Share" message.
It was determined that the needle-sharing message would require
three pictures to convey its complexity. The artist, using informa-
tion about risk behaviors and barriers to reduction, developed
three sketches.
I
NVOLVING
THE
T
ARGET
P
OPULATION
AND
F
INE
-T
UNING
THE
I
LLUSTRATIONS
The rough black-and-white sketches were taken into the field for
testing with current IDUs. Two sites afforded a setting amenable
to in-depth interviews with the IDUs. IDUs were shown one

A STORYTELLING MODEL
37
sketch and asked to tell the interviewer what was happening in
the picture. Stories and explanations by the IDUs were analyzed
for content by members of the AESOP staff. The three injection-
related illustrations generated stories that were surprisingly close
to the messages that had been selected for focus. From the pre-
liminary sketches, the artist painted watercolor versions to be
tested in the field.
Testing the watercolors indicated a need to adjust the colors, not
only for emphasis of specific aspects of the illustration but also to
reflect the multicultural setting in Los Angeles. Several flesh
tones were thus used for the people in the pictures. Some figures
were presented as neither male nor female to allow outreach work-
ers to use the illustrations to depict individuals of either sex and
of any ethnicity (see Figures 1, 2, and 3).
Although completing the three illustrations that addressed differ-
ent aspects of the “I don’t share message” was relatively simple, it
proved difficult to make an appropriate illustration to address sex-
related risk behaviors. The initial sketches presented to AESOP
staff members were either too broad or did not focus on HIV. One
sketch presented to the target population, although it addressed
the complexity of sex-related risk behaviors, did not focus suffi-
ciently on HIV. A second sketch, much closer to the original "Not
with my man or woman" story, still did not focus attention on HIV.
Despite the initial intention to exclude text from the visuals, it was
determined that the word HIV needed to be added to the final
sketch. With the addition of HIV, the message became very clear
to the IDUs who tested the illustration (see Figure 4).

Figure 1.
Figure 2.
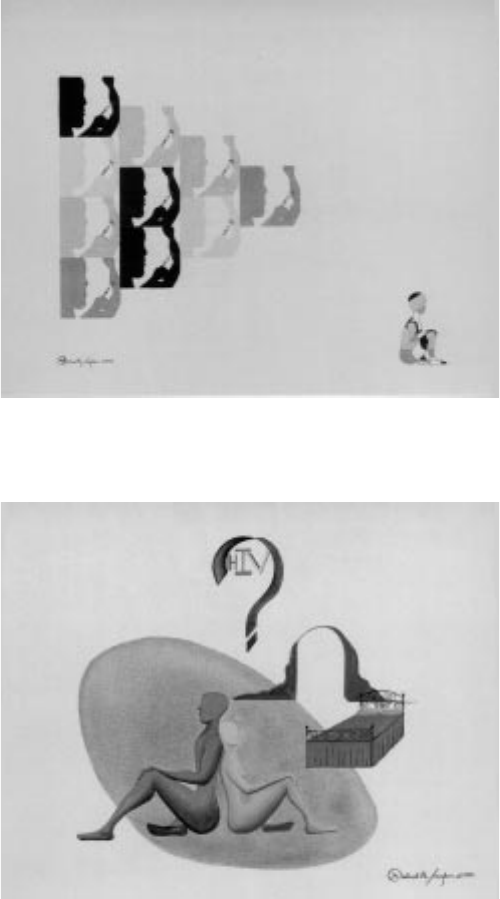
Figure 3.
Figure 4.
Source for illustrations: Michael Taylor, Los Angeles, copyright 1994

AESOP
40
TRAINING OUTREACH WORKERS
TO USE STORYTELLING AND ILLUSTRATIONS
Several factors were considered in designing the outreach worker
training. It was clear from the field observations and formative
research data that some outreach workers were reluctant to use
new methods to reach clients. Many outreach workers had been
in the forefront of responding to the HIV/AIDS crisis early in the
epidemic and considered their background and experience in pro-
viding street outreach services to IDUs more applicable than the
interventions developed by researchers. There was a strong con-
cern that research-based interventions simply "would not work" in
the field. It was clear that the training would need to build upon
workers’ current wealth of knowledge rather than attempting to
supplant their tools and talents with new interventions.
Moreover, to move from the storytelling model to staging clients for
risk-reduction messages, outreach workers required working
knowledge of the theoretical foundation of the interventions. Thus,
outreach workers needed to be trained to use the pictures on the
street, both to elicit risk-behavior information and to teach and
reinforce risk-reduction behaviors. It was decided that two train-
ing sessions would be held—the first on the use of the illustra-
tions and the second on staging clients for readiness to adopt
three risk-reduction behaviors (see List 2).
During the first training session, trainers introduced outreach
workers to the purpose and the use of the illustrations in assess-
ing the client's needs and current risk behaviors and to the
stages-of-change model. They presented drafts of the illustrations
and gave outreach workers the opportunity to practice using the
materials with one another through role playing. The emphasis
during the first session was on outreach workers’ becoming com-
fortable with using the illustrations in a variety of contexts.
During the first training session, some outreach workers, espe-
cially many of the veteran staffers, expressed apprehension about
using the illustrations. Some stated that they would feel "silly" or
"stupid" showing people pictures and asking them "a lot of ques-
tions." Others expressed concern that it would be too time con-
suming to use all four illustrations during every one of their

A STORYTELLING MODEL
41
LIST 2
C
ONTENT OF TRAINING SESSIONS FOR
O
UTREACH WORKERS
Session 1: Teaching and Reinforcing Risk-
Reduction Skills with Illustrations
Purpose of illustrations
Review draft illustrations
Assessing client needs and risk behaviors
Providing risk-reduction messages and strategies
Introduction to stages-of-change model
Using illustrations to get information
Using illustrations as a teaching tool
Role-playing exercise
Questions and discussion
Session 2: AESOP Stages-of-Change Training
Review of illustration-using intervention
Review of stages-of-change model
Review of risk behaviors and risk-reduction behaviors
Steps in staging clients
screening the client
assessing the risk behavior
assessing intentions
Exercises
identifying client’s level of stage of change
obtaining additional information

AESOP
42
outreach contacts and encounters. It was explained that the illus-
trations were designed for intensive work with clients and that not
all illustrations would be used during each encounter. The initial
training session included discussions on selecting specific clients
and situations in which to use the intervention and on selecting
appropriate illustrations to use with specific clients. Outreach
workers were encouraged to practice using the draft illustrations
with one another until the second training session.
The second session focused on formalizing the client staging pro-
cedure. Once the storytelling model had been implemented, out-
reach workers learned to use standard questions and forms to
specify and record clients’ levels of stage of change. Outreach
workers were given an opportunity to practice staging clients with
one another, and their proficiency was assessed.
IMPLEMENTATION
Final, full-color illustrations were printed on 4" 3 5" cards. Before
distributing the cards, AESOP staff members personalized the
cards for each outreach team by adding a label bearing the name,
address, and phone number for the outreach program. The cards
and staging sheets were then delivered to the outreach team.
AESOP staff members accompanied each outreach team as the
outreach teams began using the cards. Staff members observed
outreach workers’ use of the card, judged whether outreach work-
ers had determined the correct stage, and spoke briefly with the
outreach worker’s client. Members of the AESOP staff reviewed
initial interactions with the outreach worker and provided feed-
back to try to maximize outreach workers' effectiveness in imple-
menting the intervention.
As the outreach workers used the cards, it became clear that
much of the initial intent in the planned design of the visual had
been realized. According to extensive observations by the research
team, the storytelling intervention was engaging and held the
attention of target populations longer than standard outreach did.
The illustrations stimulated the IDUs to examine their HIV risk
behaviors, and IDUs began to relate their own stories of risk
behavior to the pictures. Outreach workers became adept at using

A STORYTELLING MODEL
43
the cards to engage clients who were reluctant to discuss their HIV
risk behaviors or to focus the attention of a client on a particular
consequence of that client’s. One unanticipated effect of the visu-
als was the promotion of group discussions in the field. Once one
IDU would become engaged with the picture, peers would become
curious and join in the conversation. At times, three or four cli-
ents engaged in group discussions regarding possible interpreta-
tions of the illustrations, frequently pointing out different aspects
of HIV risk behaviors as well as methods of prevention.
CONCLUSIONS
The cultural and social diversity of the Los Angeles County IDU
population required a strategy that was adaptable, inexpensive,
and portable to sites and segments of the target population
throughout the county. The advantage of the storytelling
approach was that it could be presented in a variety of outreach
settings, could be implemented with persons at various literacy
levels, and could be easily adapted to the cultural needs of each
segment of the target population. It was also a natural lead-in to
staging clients for risk reduction.
The development of any risk-reduction intervention requires care-
ful consideration of the target population’s needs as well as of the
settings in which learning and behavior change take place. Pro-
grams considering the storytelling model are cautioned to work
carefully with the target community, outreach workers, and other
service providers during each step of development and implemen-
tation. It is important to remember that the messages, illustra-
tions, and format of the illustrations must be consistent with the
needs of the target population.

AESOP
44
References
Bean, M. (1975). Alcoholics Anonymous. Psychiatric Annals, 5,
45-61.
Campbell, J., with Moyer B. (1988). The Power of myth (B.S.
Flowers, Ed.). New York: Doubleday.
Fishbein, M., & Rhodes, F. (1997). Using behavioral theory in HIV
prevention (pp. 21-34). In N.H. Corby & R.J. Wolitski (Eds.),
Community HIV prevention: The Long Beach AIDS Community
Demonstration Project. Long Beach California: University
Press, California State University.
McAlister, A. (1997). The diffusion accelerator: Combining media
and interpersonal communication in community-level health
promotion campaigns (pp. 31-43). In N.H. Corby & R.J.
Wolitski (Eds), Community HIV prevention: The Long Beach
AIDS Community Demonstration Project. Long Beach, Cali-
fornia: University Press, California State University.
Prochaska, J.O., & DiClemente, C.C. (1986). Toward a
comprehensive model of change (pp. 3-27). In W.R. Miller & N.
Healther (Eds.), Treating addictive behaviors: Processes of
change. New York: Plenum Press.
Prochaska, J.O., & DiClemente, C.C. (1992). Stages of change in
the modification of problem behaviors (pp. 184-218). In M.
Hersen, P.M. Miller, & R. Eisler (Eds.), Progress in behavior
modification. New York: Wadsworth Publishing.
Prochaska, J.O., DiClemente, C.O., & Norcross, J.C. (1992). In
search of how people change: Application to addictive be-
haviors. American Psychologist, 47, 1102-1114.
Rappaport, J. (1993). Narrative studies, personal stories, and
identity transformation in the mutual help context. Journal of
Applied Behavioral Science, 29(2), 239-256.
Stevenson, H.C., McKee, G.K., & Josar, L. (1995). Culturally
sensitive AIDS education and perceived AIDS risk knowledge:
Reaching the “know-it-all” teenager. AIDS Education and
Prevention, 7(2), 134-144.

A STORYTELLING MODEL
45
Weeks, M.R., Schensul, J.J., Williams, S.S., Singer, M., & Grier, M.
(1995). AIDS prevention for African-American and Latina
women: Culturally and gender-appropriate intervention. AIDS
Education and Prevention, 7(3), 251-264.

47
ELEMENTS OF AN
INTENSIVE OUTREACH PROGRAM
FOR HOMELESS AND RUNAWAY STREET YOUTH IN
SAN FRANCISCO
Alice A. Gleghorn
*
, Kristen D. Clements
*
, and Marc Sabin
†
In 1991, the Centers for Disease Control and Prevention (CDC) ini-
tiated the AIDS Evaluation of Street Outreach Projects (AESOP), a
program designed to evaluate the effectiveness of intensive HIV
prevention outreach programs for high-risk populations. Nation-
ally, AESOP comprised three youth sites and five sites for injection
drug users. Details of the overall AESOP project are provided else-
where (Anderson et al., 1996). The San Francisco Department of
Public Health–AIDS Office contracted with the Haight-Ashbury
Free Medical Clinics to develop ongoing HIV prevention outreach
programs tailored to the youth subcultures and many marginal-
ized youth who congregate in that neighborhood.
Before the implementation of AESOP, no consistent outreach
efforts were specifically targeting youth in the Haight-Ashbury
neighborhood of San Francisco. Therefore, AESOP presented the
opportunity to design a comprehensive HIV prevention program
for homeless and runaway street youth. The result was an inno-
vative set of community-level interventions that developed from
needs and ideas expressed by the youth. We describe the multi-
faceted intervention developed by the Haight-Ashbury Youth Out-
reach Team (HAYOT) and the AESOP staff. Although HAYOT
continues to provide services to youth, the intervention period was
September 1993 through October 1995 (the AESOP study period).
*San Francisco Department of Public Health–AIDS Office, San Francisco, California
†
Haight-Ashbury Free Medical Clinics, Incorporated, San Francisco, California

AESOP
48
THE INTERVENTION
The intervention included traditional street outreach (CDC, 1993),
a youth center developed to provide HIV prevention services, and
youth subculture-specific prevention activities and educational
materials. Although elements of each of these three components
were present throughout the study period, the program focus dif-
fered over time to meet the needs and interests of youth. The ini-
tial emphasis of the intervention was basic street outreach. As
youth attendance at youth center activities increased, staff time
on the streets decreased. Youth involvement in the development
of subculture-specific activities and materials (Schein, Yeager,
Young, Shapiro & Gleghorn, 1996; Slotnick & Daly, 1996)
changed according to youth interest.
S
TREET
O
UTREACH
A
CTIVITIES
Staff outreach. Street outreach was conducted by community
health outreach workers (CHOWs) and peer health educators.
CHOWs went out on the streets to contact youth with another
CHOW or a trained peer. All outreach staff attended outreach
worker training sponsored by the City and the County of San
Francisco. Peers did not go out without a CHOW. During the ini-
tial 3 months of the project, CHOWs typically spent 30 hours per
week doing street outreach; during later phases of the interven-
tion, staff spent approximately 15 hours per week doing outreach
on the streets.
Contact locations. Outreach activities took place in a six-block
area of Haight Street and in two parks that border this area. Sites
where youth frequently congregated included street corners,
parks, and outside local businesses. Sites were specified in pre-
liminary research.
Contact target. CHOWs visually assessed youth in contact loca-
tions to determine which youth might be part of the target popula-
tion of homeless or runaway youth or youth involved in the street
economy. Target youth were typically distinguished by the condi-
tion of their clothing, particularly shoes, and poor hygiene. Youth
who were panhandling were also targeted.

ELEMENTS OF AN INTENSIVE OUTREACH PROGRAM
49
Contact restrictions. CHOWs did not approach youth who
seemed to be actively involved in a drug transaction, youth partic-
ipating in a violent action, youth interacting with the police, or
youth involved in any situation that made the CHOW feel unsafe.
Youth who seemed under the influence of drugs or youth with
active psychosis were not approached if the CHOW did not feel
safe. CHOWS offered information on the center’s services to youth
who panhandled in lieu of handouts.
Basic street contact. Basic street contact was defined as a brief
(usually 30 seconds) interaction between the CHOW and target
youth in street locations. Following the model of basic street out-
reach (CDC, 1993), the interactions typically had four elements:
(a) introduction—the CHOW told the youth his or her name and
introduced himself or herself as an outreach worker from the
HAYOT; (b) check-in—the CHOW asked how the youth was doing
and whether the youth needed anything; (c) information—the
CHOW told the youth the location of the youth center and gave the
youth a schedule of services (showers, meals, women’s time); and
(d) distribution of materials—the CHOW gave the youth condoms
and bleach kits. Since the beginning of outreach activities,
CHOWs have distributed information sheets on needle exchange
locations. CHOWs began distributing a referral sheet, a flyer with
information on services for youth in the Haight, in October 1994.
Although condoms were distributed, a basic street contact gener-
ally did not involve discussion of sexual behaviors unless initiated
by the youth. On the basis of the conversation, CHOWs would
encourage a youth who seemed to need more extensive contact to
come to the HAYOT center at the youth’s convenience to talk with
an outreach worker. Occasionally, the CHOW accompanied the
youth to the center for an immediate extended session (described
in later section). Also on rare occasions, the CHOW would give a
youth referral information on the street, without an extended session.
HAYOT Y
OUTH
C
ENTER
A
CTIVITIES
The Youth Center is centrally located in the target area, one level
above the street, in a renovated Victorian house that also houses
other offices. The Youth Center has several offices, a kitchen,
shower facilities, a small room for individual counseling, a larger
room for group discussions, a hall with displays of resource

AESOP
50
materials and youth art, and an outdoor deck and eating area.
The center offers HIV prevention services and limited youth-
support services. The Youth Center, developed to provide out-
reach services for youth for AESOP, is officially a branch of the
Haight-Ashbury Free Medical Clinics, Incorporated. The center is
staffed by a coordinator, two to four CHOWs, and two to three peer
outreach workers. One intern from a local university has also
worked at the center.
Extended sessions. The most common prevention service at the
Youth Center was extended sessions, which were defined as any
discussion of center services or a youth-identified problem
between CHOWs and a youth at the center. These contacts lasted
from 10 minutes to 1½ hours. The issues raised by youth most
commonly involved medical concerns, HIV or sexually transmitted
disease (STD) issues (including testing), housing, drug use and
treatment, and legal problems. Extended sessions were usually
initiated by youth who came to the center for assistance. Approx-
imately 80% of those who came to the center for support services
(described later in this section) and approximately 50% of youth
who had had a basic street contact also had an extended session.
During the extended session, CHOWs typically tried to address the
youth’s immediate needs first (e.g., overdose issues, medical care,
housing, and employment) and then discussed HIV prevention in
terms of sex and drug-using behaviors. If necessary, CHOWs dem-
onstrated how to use a condom or use bleach to clean drug equip-
ment. Such demonstrations were often used to initiate discussion.
Referrals. Approximately 75% of youth were given referrals dur-
ing extended sessions. Referrals were made for services provided
by agencies other than the center. Most commonly, the CHOW
made the appointment for the youth (if appropriate) and wrote the
location, phone number, and appointment time on an appoint-
ment card. Most referrals were for medical services, STD testing
or treatment, obstetrics and gynecology, HIV testing, drug treat-
ment, housing, and employment. All referrals included appoint-
ments unless the agency was closed at the time of the extended
session or the agency had drop-in hours only. Most referrals were
to agencies in close proximity to the Haight neighborhood. Bus
tokens were commonly given to help the youth keep the appoint-
ment; sometimes incentives such as T-shirts were given later if
the youth could prove that he or she had kept the appointment.

ELEMENTS OF AN INTENSIVE OUTREACH PROGRAM
51
Very rarely, the CHOW took a youth to the referral appointment,
but this was not encouraged by HAYOT.
Harm-reduction groups. In October 1994, the center began con-
ducting harm-reduction groups. Youth were offered incentives
(usually pizza) to be part of a small working group that was
responsible for creating educational materials. Youth first listed
the topics that were important to them, and then they chose the
topic that they wanted to work on during a particular session.
Topics have included abscess care, needle exchange, safer shoot-
ing practices, safer sex, alcohol abuse, and overdose. After choos-
ing a topic, youth worked together to come up with the
information that they wanted to include on a harm-reduction edu-
cational card. After the cards were planned, HAYOT staff were
responsible for producing the harm-reduction cards. Staff tried to
have the card ready within 2 days after the harm-reduction group
meeting. Completed cards were placed in the center with the other
educational materials, and CHOWs distributed them on the
streets while doing outreach. CHOWs made a special attempt to
find youth who had participated in the creation of the cards to
show them the end product and get their feedback. If youth were
interested, CHOWs gave them a stack of cards to distribute to
their peers. Twelve harm-reduction cards were developed and dis-
tributed during the study. Every card bore the HAYOT address
and phone number, and youth were encouraged to hold onto as
many cards as possible. Community events were planned at which
youth were given prizes for possessing harm-reduction cards.
Women’s groups. In September 1995, the center began conduct-
ing prevention groups for young women. Female HAYOT staff
recruited young women to develop education-information cards
specifically for their female peers. During the study, four cards
were developed by these groups. The topics included pregnancy
and local prevention services for women. The procedure for the
development and distribution of the women’s cards was the same
as that for the harm-reduction cards.
Educational materials. Two types of educational materials were
available at the center. Informational pamphlets from local agen-
cies offering a variety of services were displayed, and youth could
take these with them. In addition, the 12 harm-reduction cards

AESOP
52
and 2 of the women’s cards created by and for youth were avail-
able at the center.
Educational videos. The center also showed educational videos
when youth were waiting for an extended session or other ser-
vices. If HAYOT staff members believed a youth would benefit
from a particular video, they had that youth watch the video
before or after an extended session. Eight videos dealing with
street life, drug use, or safer sex were available at the center. Also
available was an educational video made for HAYOT by the rock
group, the Grateful Dead, targeting Deadhead youth (described in
Materials for Youth Subcultures). During the rainy season,
HAYOT staff occasionally rented a movie that addressed youth-
relevant topics, such as drug use, and showed it to a larger group
of youth. Discussion groups with staff, which focused on issues
raised by the movie, typically followed the screening.
Drug treatment. Because few youth-oriented drug-treatment
services were available, the center offered limited drug-treatment
services for youth trying to terminate drug use. Services through
the center included discussions with youth about drug use and
drug treatment issues, and a structured, 21-day nonmethadone
medical drug-treatment program conducted in conjunction with
Haight-Ashbury Free Medical Clinics, Inc. If youth were 18 years
of age and interested in a methadone program, they were referred
to another program (Haight-Ashbury Free Clinics does not offer
methadone programs).
Youth interested in the HAYOT drug-treatment program scheduled
an intake appointment with a senior staff member. These intake
appointments took approximately 1½ hours and were limited to
two per week. The intake consisted of information for admission
to the clinic program. After the intake, center staff accompanied
youth to the Haight-Ashbury Free Medical Clinic, where they
received a physical exam, saw a psychiatrist, and were given med-
ication to ease withdrawal symptoms. By seeking drug-treatment
services through HAYOT, youth were able to skip the usual wait-
ing list for treatment. After youth were enrolled in the drug-
treatment program, they checked in at the center at noon each
day. Youth had a brief counseling session at the center before
going to the clinic to pick up their medication. Youth who arrived
more than 15 minutes late were not able to get medications that

ELEMENTS OF AN INTENSIVE OUTREACH PROGRAM
53
day. Youth enrolled in the program could receive center support
and prevention services at any time during center hours. If they
needed more extended counseling, center staff helped them get an
appointment with a psychiatrist at the Haight-Ashbury Free Medi-
cal Clinic.
After 21 days, a youth who was drug-free could continue to come
to the center for counseling and assistance with housing and
employment. Youth who relapsed during the 21-day period could
continue the clinic program throughout the 21-day period. After
21 days, a youth who had relapsed or was still using could not
reenter the program for an additional 30 days. Youth also were
encouraged to attend Alcoholics Anonymous or Narcotics Anony-
mous meetings as well as other counseling. Support groups were
attempted at the center but were discontinued because of a lack of
interested youth and a lack of adequate staff.
General merchant contact. When the project was initiated in
September 1993, general contact was begun. Most of the mer-
chants on Haight between Masonic and Stanyan were contacted in
person by CHOWs and given information about the location and
the services offered to youth through HAYOT. Selected merchants
whose businesses were patronized by youth had ongoing relation-
ships with the project. Twenty merchants allowed the HAYOT to
put HIV posters targeting Deadhead and punk youth in their
stores. Two merchants gave food coupon vouchers to HAYOT,
which distributed them as incentives (e.g., for participation in
harm-reduction groups). Five merchants assisted the project by
distributing condoms supplied by HAYOT in their stores. Two of
these merchants also began supplying bleach to youth as of Janu-
ary 1994. As of August 1995, an estimated 250 bottles of bleach
and 12,000 condoms had been distributed to neighborhood
merchants.
Community events. Six community events took place during the
study period. These events had HIV prevention themes and tar-
geted youth, local merchants, or youth service providers.
Event 1, held in January 1994, targeted youth. The main focus of
the event was the Grateful Dead HIV prevention video that was
developed for the project (described in Materials for Youth Subcul-
tures). Youth were invited to come to the center for a premiere

AESOP
54
showing (60 youth came). A local merchant donated 60 coupons
for free ice cream, and the Grateful Dead donated 12 concert tick-
ets for a raffle that accompanied the event. Food and refreshments
were followed by an introduction to the video and then a showing.
After the video, there was time for comments from the youth.
Event 2, held in July 1994, also targeted youth. Youth were
invited to come to the center for food and to pick up socks (30
came). Youth were separated into different rooms to discuss dif-
ferent issues related to youth services, drug use, and living in
squats. The information was recorded and used in the develop-
ment of a zine (described in Materials for Youth Subcultures) tar-
geting punk or squatter youth.
For Event 3, held in September 1994, merchants were invited to
the center (5 came). Food was offered, and HAYOT staff showed
them the Grateful Dead and punk posters (described in Materials
for Youth Subcultures). Although only 5 merchants came to the
event, 20 merchants in the community agreed to put the posters
in their place of business.
Event 4, also held in September 1994, targeted service providers.
Other community-based organizations that work with youth were
invited to the center for an open house (40 people came). Food
was served, and HAYOT raffled program T-shirts. The main pur-
pose of the event was to network and keep referral relationships
with other agencies strong.
Event 5, held in September 1995, targeted service providers. This
event was similar to Event 4; its primary goal was strengthening
referral networks. Forty providers attended the event, at which
food was served and T-shirts were raffled.
Event 6, also held in September 1995, targeted youth. The pur-
pose of the event was for youth to complete an open-ended survey
to evaluate HAYOT and the services they received there. Fifty
youth attended the event and completed the surveys. Incentives
for youth consisted of T-shirts, food, and socks.

ELEMENTS OF AN INTENSIVE OUTREACH PROGRAM
55
Y
OUTH
S
UPPORT
S
ERVICES
Limited support services were offered at scheduled times during
regular center hours. These services—showers, meals, and
women’s time—were provided, unless otherwise noted, on a first-
come, first-served basis.
Showers. Services, scheduled on separate days for males and
females, included access to the shower and the provision of sham-
poo, soap, and a towel. Showers were offered in 2-hour blocks
four times a week—twice for women, twice for men. The center
can accommodate approximately five youth per hour for showers.
Meals. Meals were provided 2 days per week for 1 hour. They
consisted of food obtained from the food bank that week. In order
to serve as many youth as possible, youth were encouraged to
take portable food (for example, soft drink cans, sandwiches, and
fruit) with them, rather than eating all food on the premises. To
maintain center security, meal admission was limited to 10 youth
inside the center at a time. The center typically served 30 youth
per meal.
Women’s time. To facilitate contact with young women, the cen-
ter initiated a special time for women to visit the center and dis-
cuss their concerns. Women’s time ran for 3 hours once a week
and overlapped with one of the women’s shower times. All women
who came to the center for women’s time were admitted. Two
female staff members (one peer and one CHOW) were available
during women’s time; male staff remained out of sight during
these hours. Services included conversations with staff, snacks,
showers, and OB/GYN information and referrals.
M
ATERIALS
FOR
Y
OUTH
S
UBCULTURES
Preliminary ethnographic research distinguished two predominate
youth subcultures in the study area: hippie or Deadhead youth
and punk or squatter youth. Approximately half of the youth in
AESOP identified with one of these two groups. Each group has
distinctive value system, norms for appearance, artistic and musi-
cal preferences, and acceptance of different types of drug use.
Because of these subcultural differences, HIV prevention materi-

AESOP
56
als were developed for each group. A variety of products were pro-
duced for each subculture. The Grateful Dead band cooperated in
the production of two products for hippie and Deadhead youth: a
video and a condom cover. Posters were developed from focus
groups of youth from each subculture. A core group of punk or
squatter youth developed zines and a referral card oriented to
their peers. We used the following seven steps in developing these
materials:
1. Gained an understanding of the community
2. Focused on a subculture
3. Organized a core group from the subculture
4. Supported the core group’s development and
production of activities or materials
5. Supplied the core group with the necessary resources
6. Evaluated the finished product
7. Developed new products
Deadhead video. AESOP staff collaborated with HAYOT and the
Grateful Dead to produce a 5-minute video promoting condom use
and safe needle hygiene among the band’s followers. The AESOP
coordinator, working with the Grateful Dead’s publicist, secured
an interview with band member Bobby Weir to discuss HIV risk
behaviors and prevention strategies, which would serve as the
centerpiece of the video. Before the interview, AESOP and HAYOT
staff held focus groups with Deadhead youth living on the street to
formulate questions for Mr. Weir. Project staff interviewed Mr.
Weir and then shot footage of Deadhead youth before a Grateful
Dead concert in discussion about their own risk behavior. The
resultant footage was shown to another focus group, and the
youth selected the segments they thought would have the most
effect. The final video integrated concert footage, clips of young
Deadheads talking about their risk for HIV, and Bobby Weir dis-
cussing HIV prevention strategies. A major community event was
held before the premiere of the video at the HAYOT Center, and a
number of tickets to the next Grateful Dead concert (donated by
the Grateful Dead) were raffled to youth. To take part in the raffle,
the youth had to complete a short HIV questionnaire and then dis-

ELEMENTS OF AN INTENSIVE OUTREACH PROGRAM
57
cuss their answers with the outreach workers. The video was also
shown at the center to interested youth. As of November 1995,
150 youth had seen the video.
Deadhead condoms. AESOP worked in coordination with the
Grateful Dead’s publicist to secure the use of their “Steal Your
Face” logo on condom packets. The condom packets bore the logo
and included instructions for condom use and referral numbers
for HAYOT, the California Youth Crisis Line, and the National
AIDS Hotline. A total of 10,000 condom covers were produced. By
the end of the study period, 5,000 condoms had been distributed
by HAYOT.
Posters and T-shirts. Hippie, Deadhead, punk, and squatter
youth worked with community artists and AESOP and HAYOT
staff to produce two HIV prevention education posters. A series of
focus groups were held separately with youth from each subcul-
ture group. In the focus groups, youth actively participated in cre-
ating slogans and designs that would appeal to their peers.
Community artists were recruited to donate their time to design
images. The tentative poster designs were reviewed in youth focus
groups and one-on-one interviews, and suggested changes were
incorporated. Five hundred posters and 200 T-shirts were pro-
duced and distributed to youth and community merchants in
1994 and 1995.
Dope Productions. The zines and referral cards described in the
next two sections were produced by a core group of punk and
squatter youth who organized and named themselves Dope Pro-
ductions. Dope Productions grew out of a series of focus groups
designed to elicit input from youth about materials development.
Youth expressed a desire to continue this type of work and sug-
gested forming an informal production company committed to cre-
ating educational materials by youth for other youth. The name
Dope Productions, agreed upon by a group of 12 street youth,
refers to dope as slang for any type of drug as well as a colloquial-
ism meaning “exceptional.”
Zine. A zine is a type of underground magazine that originated in
the punk subculture. HAYOT and AESOP collaborated with a
group of young injection drug users living in abandoned buildings
to produce, design, write, and distribute a zine specifically for

AESOP
58
their community. Initially, the youth were individually recruited
from the streets and from three squats to take part in a commu-
nity event designed to form a core group committed to writing and
editing the publication. Ice cream vouchers, pizza, and socks were
offered as incentives for participation in the initial meeting. The
core group discussed harm-reduction theory and how it could be
applied to reduce the risks their peers faced. The youth were then
trained in basic computer graphic skills and worked with two
facilitators to organize other youth to produce writing and art.
Articles in the zine addressed the needs, concerns, and beliefs of
the squatting population; topics ranged from prostitution and
squatting ethics to safer shooting techniques. Youth integrated
comprehensive harm-reduction information about needle hygiene,
needle exchange, and condom use, as well as service referrals,
throughout the publication. By the end of the AESOP study, two
issues of the zine had been produced, and 200 copies of each had
been distributed to street youth in San Francisco.
Referral card. Youth from the zine core group worked with an
AESOP organizer to put together a hand-held resource card specif-
ically designed for youth on the street in the Haight. Three youth
discussed the array of services available in the city and then,
working with the organizer, drew up a list of those most important
and accessible to Haight street youth. Then youth reviewed the
services, listing the pros and cons of each. Very short reviews of
11 essential services were fitted into a small accordion-folded
card. The card began with the most basic, practical, and easily
accessible services and moved on to other services. Also described
were the procedures by which youth could easily access that par-
ticular service. The card covered a range of youth outreach ser-
vices: where to shower and snack, free food, nighttime services,
youth shelters, youth needle exchange, medical clinics, women-
specific services, and youth services outside the Haight. Youth
contributed images and helped to design the artwork on the front
cover. By the end of the study, outreach workers had distributed
300 referral cards to youth.
In our evaluation of youth exposure to, and interest in, subcul-
ture-specific HIV prevention materials (Gleghorn, 1997), we found
that these materials may have differential appeal for the various
youth subgroups. In general, targeted subgroups had the highest
exposure rates for materials oriented to their subculture. How-

ELEMENTS OF AN INTENSIVE OUTREACH PROGRAM
59
ever, hippie or Deadhead materials seemed to have broad appeal,
as measured by exposure among the subgroups; hippie and Dead-
head youth had lower exposure to, and higher rejection of, materi-
als designed for punk and squatter youth. Youth who chose not to
identify with a specific subculture also showed moderate levels of
exposure to, and acceptance of, the subculture-specific prevention
materials. Although the use of subculture-specific HIV prevention
materials holds promise for reaching high-risk street youth, future
research should explore factors related to the rejection of materi-
als and whether youth acceptance of outreach materials trans-
lates into participation in HIV prevention activities and decreased
risk behaviors.
SUMMARY
After AESOP ended, HAYOT received other funds to continue their
outreach efforts. By combining street outreach, Youth Center
activities, and subculture-specific materials, the program devel-
oped a comprehensive intervention that increased youth contact
with outreach and prevention services (Gleghorn et al.,1997). Fol-
lowing the seven steps to involve youth in developing HIV preven-
tion activities, innovative, subculture-specific interventions
continue to evolve through the HAYOT. The comprehensiveness of
the program contributed to the program’s success in reaching
high-risk youth.
ACKNOWLEDGMENTS
This study was supported by Centers for Disease Control and Pre-
vention cooperative agreement U62/CCU907200. The interven-
tion in this study was developed by the Haight-Ashbury Youth
Outreach Team (HAYOT) in collaboration with the San Francisco
Department of Public Health–AIDS Office (SFDPHAO). We thank
the following for assistance with this project: Amber Berquist,
David Deery, Amanda Frank, and Julian Proctor, (HAYOT staff);
Matthew Boman, Clare Brown, Ralph Dickinson, Heather Hamil-
ton, Leatha Jones, Tia Elena Martinez, Sue Miller, Henry Padilla,

AESOP
60
Lorna Sumaraga, and Amy Symons (SFDPHAO interviewers); Will-
iam Cann, Arthur DeGuzman, Matthew Dodman, Aida Flandez,
Delia Garcia, Lisa Graybill, Vince Guilin, Jan Gurley, Mitchell
Katz, Tim Kellogg, Ruth Kinney, Priscilla Lee-Chu, David Makof-
sky, Rani Marx, Stephen Mills, Kyle Ranson, Eric Vittinghoff, and
Andy Weisskoff (SFDPHAO staff); Michael Clatts and Michele
Kipke (AESOP youth-site investigators); and John E. Anderson,
Judith Greenberg, and Matthew Seeman (CDC).
References
Anderson, J.E., Cheney, R., Clatts, M., Faruque, S., Kipke, M.,
Long, A., Mills, S., Toomey, K., & Wiebel W. (1996). HIV risk
behavior, street outreach and condom use in eight high risk
populations. AIDS Education and Prevention, 8 (3), 191-204.
CDC. (1993). Assessment of street outreach for HIV prevention —
Selected sites, 1991-1993. Morbidity and Mortality Weekly
Report, 412, 873, 879-880.
Gleghorn, A.A., Clements, K.D., Marx, R., Vittinghoff, E., Lee-Chu,
P., & Katz, M. (1997). The impact of intensive outreach on HIV
prevention activities of homeless, runaway, and street youth
in San Francisco: The AIDS evaluation of street outreach
project (AESOP). AIDS and Behavior, 1(4), 261-271.
Schein, J., Yeager, T., Young, A., Shapiro, R., & Gleghorn, A.
(1996). Straight dope: The making of a community level
intervention [video produced by the San Francisco
Department of Public Health–AIDS Office].
Slotnick, J., & Daly, J.P. (1996). The making of a community
level intervention. In E. Iverson & J.P. Daly (Eds.), The making
of a community level intervention. Los Angeles: Redwood Press.

61
ASSOCIATION BETWEEN SELF-IDENTIFIED
PEER-GROUP AFFILIATION AND
HIV RISK BEHAVIORS
AMONG STREET YOUTH
Michele D. Kipke, Jennifer Unger, Raymond Palmer,
Ellen Iverson, and Susan O’Connor
Well into the second decade of the acquired immunodeficiency
syndrome (AIDS) epidemic, infection with the human immunodefi-
ciency virus (HIV) is the leading cause of death among Americans
aged 25 to 44 years. As of June 1996, 548,102 cases of AIDS had
been reported to the Centers for Disease Control and Prevention
(CDC), and 343,000 deaths had been attributed to AIDS or AIDS-
related causes (CDC, 1996). Clearly, efforts to quell the epidemic
have been unsuccessful. Adolescents are increasingly being rec-
ognized as a segment of the population that is at high risk for HIV
infection (Vermund, 1997). Because of the long latency between
infection and the onset of symptoms (mean, 12 years), many of the
19,997 infected persons in the 20-to-24 age group are likely to
have been infected during their adolescence (Kipke, Futterman &
Hein, 1990).
Inner-city “street” youth have recently been recognized as a seg-
ment of the adolescent population that is at particularly high risk
for HIV infection (Kipke, O’Connor, Palmer & MacKenzie, 1995).
The street youth population comprises youth who are out of
school and unemployed, involved in the juvenile justice system,
runaway or homeless, a member of a gang, undocumented, or
involved in drug dealing and street prostitution. These youth are
believed to be on the streets for myriad reasons, including poverty
in the home that necessitates their working on the streets to sup-
plement the family income, rejection by parents or guardians, vio-
lence in the home, or drug or alcohol use by family members
Division of Adolescent Medicine, Children’s Hospital of Los Angeles, Los Angeles,
California

AESOP
62
(Bond, Mazin & Jiminez, 1992). Although the exact size of this
population is unknown, it is estimated that 750,000 to 1.5 million
youth run away from their homes each year (U.S. Department of
Health and Human Services, 1983). Of these youth, one quarter
are believed to be chronically homeless (i.e., without a family to
return to and without a permanent or stable residence). It is esti-
mated that as many as 4% of the runaway or homeless youth pop-
ulation are currently HIV infected (Rotheram-Borus, Koopman &
Ehrhardt, 1991).
There are a number of reasons why the street youth population
may be at increased risk for HIV infection. First, there is growing
evidence to suggest that an alarming number of these youth abuse
alcohol and use other substances, including drugs that they inject
(Fullilove et al., 1993; Kipke, Montgomery & MacKenzie, 1993;
Robertson, 1989; Yates, Pennbridge, Cohen & MacKenzie, 1988).
Alcohol and other drug use has been highly correlated with HIV
risk-related sexual behaviors among these youth (Kennedy,
Greenberg, Clatts, Kipke & Mills, 1994; Kipke et al., 1995). Sec-
ond, many of these youth are involved in “survival sex” (i.e., the
exchange of sex for food, shelter, clothes, money, drugs, or money
to purchase drugs) (Anderson, Pennbridge & Freese, 1994;
Rotheram-Borus et al., 1992). It is estimated that nearly 45% of
the street youth population engage in survival sex and that con-
dom use is sporadic and inconsistent with “paying partners”
(Anderson et al., 1994; Kipke et al., 1995). Youth involved in sur-
vival sex are therefore likely to be at increased risk for exposure to
HIV through unprotected sexual intercourse with multiple high-
risk sex partners.
A third possible reason, which is just now being explored, is peer-
group affiliation and the influence of peer norms or perceived peer
norms that may further encourage risky sex and drug-using
behaviors and discourage protective, or preventive, behaviors.
This reasoning is consistent with the suggestion that peers influ-
ence adolescents to engage in a variety of problem behaviors
(Brown, Clasen & Eicher, 1986; Elliott, Ageton, Huizinga, Knowles
& Canter, 1983; Jessor & Jessor, 1977). For example, adolescents
who smoke, drink alcohol, and are sexually active usually have
friends who participate in these same behaviors (Biglan et al.,
1990; Dinges & Oetting, 1993; Ennett & Bauman, 1993; Mosbach
& Leventhal, 1988; Newcomb & Bentler, 1989; Oetting & Beau-

PEER-GROUP AFFILIATION AND HIV RISK BEHAVIORS
63
vais, 1986). According to peer cluster theory (Oetting & Beauvais,
1986), peers are a primary influence on the drug-using behaviors
of adolescents. Peers who use drugs together form groups; the
group uses drugs at particular times and places; and the members
of the group share ideas, values, and beliefs about drugs. Peer
groups may consist of crowds or large groups of youth, small
groups of friends, or dyads such as best friends or couples, which
are characterized by the primary activities and attitudes of their
members. Peer clusters are often close, and members have been
found to significantly influence one another; within drug-using
peer clusters, drugs play an important part in defining the group,
shaping typical behaviors, and maintaining the group identity and
structure (Oetting & Beauvais, 1986).
Other research suggests that adolescents tend to identify with dis-
crete groups (Larkin, 1979; Light & Keller, 1979), that youth give
names to the groups with which they identify (Mosbach & Lev-
enthal, 1988; Sussman et al., 1990), and that group membership
is closely tied to behavior (Dolcini & Adler, 1994). Two studies
investigated whether identification with discrete adolescent
groups was predictive of tobacco use. Mosbach and Leventhal
(1988) and Sussman et al. (1990) assessed group identification by
asking adolescents to identify the one peer group that they felt
most a part of. The names were then grouped into five main cate-
gories: hot-shots, regulars, jocks, skaters, and dirts. Hot-shots, or
popular teens, were described as leaders in school activities, such
as academic activities. Regulars were described as resembling the
“normal,” or “typical,” teen. The jocks were described as having a
strong interest in team sports activities. Skaters were described
as placing importance on outdoor skateboarding. Finally, the
dirts were described as exhibiting problem-prone attitudes or
behaviors that included low self-esteem, risk-taking behaviors,
and drug use. Both studies found that youth who identified them-
selves as belonging to the dirts were more likely than other groups
to smoke cigarettes. In a longitudinal study, 7th grade group self-
identification predicted 8th grade cigarette smoking, whereas 7th
grade cigarette smoking did not predict 8th grade group self-iden-
tification (Sussman et al., 1994).
In a recent study conducted with street youth, acculturation to
the streets and integration into the street economy were largely
influenced by associations with other street youth (LaFrance,

AESOP
64
Pennbridge & Casey, 1992). Using qualitative research methods,
the researchers suggested that the street youth population is het-
erogeneous and comprises several street youth subcultural
groups. Although the self-identification of youth “new-to-the-
street” was defined according to their culture of origin (i.e., their
specific ethnic group or community affiliation), fully acculturated
youth were affiliated with one of the street youth subcultural
groups. LaFrance proposed that street-acculturated youth aban-
don the cultural affiliation they leave home with to embrace a new
street identity based on their identification with a subcultural
street group. Most of the street-acculturated youth were affiliated
with one of five street groups: (a) punks or skinheads, character-
ized by their antiestablishment attitudes and opinions and physi-
cal appearance (e.g., multicolored hair or shaved heads, multiple
piercings); (b) hustlers, characterized by their involvement in sur-
vival sex or prostitution; (c) druggies, characterized by their use,
including injecting, dealing, and sharing of drugs; (d) gang mem-
bers, or youth who are members of a gang; and (e) loners, or youth
who reportedly do not affiliate with other groups or are rejected by
groups because of their inability to conform to group norms or
rules. Loners were also described as having more serious mental
health problems. Each street youth group demonstrated its own
unique pattern of survival with respect to places they stayed or
slept, means of financial support and economic subsistence, and
their use of medical and social services. Thus, although the expe-
riences and backgrounds of street youth may be diverse, this
research suggests that most of these youth share a need for accep-
tance and support from other youth who are hanging out or living
on the streets. Youth who are new to the streets may search for
and join other street youth as a means of protection (i.e., there is
safety in numbers). Peers may therefore provide not only compan-
ionship but guidance in how to survive on the streets. Peers may
also influence the development of risk-taking behaviors.
The purpose of this study was to conduct epidemiologic research
to further characterize the street youth population with respect to
these street youth groups and more specifically the effect of self-
identified peer-group affiliation on youths’ use of alcohol and
other drugs and involvement in HIV risk behaviors. A common
methodologic limitation of research conducted with runaway or
homeless youth is the reliance on convenience samples recruited

PEER-GROUP AFFILIATION AND HIV RISK BEHAVIORS
65
from shelter and drop-in centers. These findings cannot be gener-
alized to youth who do not use these services, who may account
for as much as 60% to 70% of this population (Kipke, O’Connor,
Palmer & LaFrance, 1993), or to street youth who are not home-
less but who are otherwise largely “hidden.” To overcome this lim-
itation, we used a stratified probability sampling design to recruit
youth from shelters and drop-in centers as well as from street and
other natural hangout locations.
Our study adds to the literature by (a) assessing street youth, with
whom little research has been conducted, (b) using a representa-
tive sampling design with service and natural hangout sites, (c)
using self-identified peer-group affiliation to define membership,
and (d) using street youths’ own reports to estimate peer drug use
and risk behavior (rather than relying on perceptions of peers’
behavior). We hypothesized that there would be reported differ-
ences with respect to alcohol and other drug use and involvement
in HIV risk-related sex and drug-using behaviors according to
street group affiliation. This research was conducted in the Holly-
wood area of Los Angeles, California, an urban setting with a large
street youth population and an area where runaway and homeless
youth are known to congregate (Kipke et al., 1995).
METHOD
S
ETTING
, S
AMPLING
D
ESIGN
,
AND
R
ECRUITMENT
P
ROCEDURES
Youth were eligible to participate in the research if they were 12 to
23 years of age and (a) living on the streets without their families
for 2 or more consecutive months or (b) fully integrated into the
"street economy." By definition, youth integrated into the street
economy meet their subsistence needs through participation in
one or more of the following survival strategies: prostitution or
survival sex (defined as the exchange of a sexual favor for money,
food, a place to stay, clothes, or drugs), pornography, panhan-
dling, stealing, selling stolen goods, mugging, dealing drugs, or
engaging in “scams” or “cons.”

AESOP
66
An initial field assessment was conducted to estimate the number
of street youth in Hollywood on any given day, the percentage of
youth believed to use shelters and drop-in centers, and to identify
natural hangouts. On the basis of the findings from this assess-
ment, two distinct yet similar sampling frames were developed:
one recruited from 8 "fixed," or service, sites (e.g., shelter, drop-in,
and meal programs) and one from 73 "natural" street or hangouts
(e.g., street corners or highly populated blocks, parks, alleys, bars,
fast-food restaurants). Field research, observation, and service
provider data further suggested that sampling in shelters and
drop-in centers alone would miss a considerable percentage of the
street youth in Hollywood who were disinclined to use these ser-
vices. Given our broader definition of street youth (i.e., integrated
into the street economy) and studies that have relied largely on
samples recruited from shelters and drop-in centers, we con-
structed our sampling design to recruit hard-to-reach subpopula-
tions of street youth, including street youth who were not
homeless and street youth who might not be using the services of
shelters and drop-in centers. This was accomplished by over-
sampling from natural street and hangout sites: we recruited 70%
of the sample from natural sites (thereby oversampling by 20%
from these sites) and 30% from fixed sites.
A Statistical Analysis Software (SAS) computer program (SAS
Institute, Cary, North Carolina) was developed to randomly select
and order locations for interviewing teams (each comprising two to
four members). This program took into account two important
aspects of the sampling design. First, with evidence that nearly
65% of street youth are not using services, the selection was
weighted to ensure that a larger proportion of street locations were
chosen (70%), thereby increasing the probability of recruiting
youth who were not using services. Second, all fixed and natural
locations in the pool of potential sampling sites were proportion-
ally weighted, based on the number of youth who typically congre-
gated at that location during the initial field assessment. Thus,
locations with a higher volume of youth had a greater probability
of being selected by the computer random selection program than
locations with lower volumes. Assignments were also made
according to high-frequency times of day and days of the week.
Assignments were made weekly.

PEER-GROUP AFFILIATION AND HIV RISK BEHAVIORS
67
Youth selected for recruitment were asked 12 questions to deter-
mine eligibility. If eligible, youth were asked to participate in a 15-
to 20-minute structured interview called the AIDS Evaluation of
Street Outreach Projects (AESOP) Street Intercept. A subset of
items was developed to assess peer-group affiliation. These items
were examined relative to other items in the AESOP Street Inter-
cept that assessed youths' involvement in HIV risk-related sex and
drug-using behaviors, their contact with outreach workers, and
their use of shelters and drop-in centers. Youth received $3 in
fast-food vouchers for completing the screening instrument and
$7 in vouchers for completing the Street Intercept. Data were col-
lected by a team of interviewers (aged 21 to 25 years) who had
extensive training and experience in field research techniques (e.g.,
identifying and engaging potential clients, interviewing techniques).
The data reported here were collected by using a subset of items
that assessed respondents’ self-identified peer-group affiliation,
lifetime and recent (past 30 day) use of illicit substances, and
involvement in HIV risk-related sexual behaviors. These data was
obtained from youth enrolled in the study during five 2-month
cross-sectional waves of data collection: January and February
1993 (Wave 1, n = 204), May and June 1993 (Wave 2, n = 205),
November and December 1993 (Wave 3, n = 163), March and April
1994 (Wave 4, n = 177) and October and November 1994 (Wave 5,
n = 211). Data were collected in waves according to a schedule
developed for this CDC-funded cooperative agreement research
project. Across these five waves, 1,455 youth were approached; of
those, 1,163 volunteered to complete the screening instrument.
Of youth who were screened, 154 were ineligible (14%), and 275
(19%) refused to participate. The most common reason for refus-
ing to participate in the study was that the youth were "too busy"
(e.g., hustling, dealing drugs) to complete the survey. These
response rates should be considered a minimum estimate, given
that not all potential respondents were perceived as approachable
(e.g., because an illegal drug transaction was taking place). Pre-
liminary analyses revealed no significant differences in refusal
rates by gender or race. There were, however, significant age dif-
ferences in refusal rates; younger youth aged 12 to 15 years were
least likely to refuse to participate compared with those aged 16 to
18 years (P < .001) who in turn were less likely to refuse to partic-
ipate than were the older youth, aged 19 to 23 years (P < .001).

AESOP
68
Peer-group affiliation was assessed by giving respondents a list of
street youth groups compiled from earlier ethnographic research.
Respondents were asked, “Who would you say you are most like or
spend the most of your time with?” The research received formal
institutional review board approval, and all clients signed an
informed consent form before completing the screening and sur-
vey instruments.
D
ATA
A
NALYSIS
All analyses were performed by using the SAS for personal com-
puters. Demographic variables (age, gender, race) were used to
characterize the street youth groups. Rates of drug use were com-
puted for self-reported recent use (past 30 days) of alcohol and
marijuana (at least once per week), lifetime use of other sub-
stances (i.e., cocaine; crack cocaine; methamphetamine, or
"speed;" heroin; the combination of heroin and cocaine, or "speed-
ball”; opium; D-lysergic acid diethylamide, or LSD; mushrooms;
peyote; and phencyclidine, or PCP), lifetime involvement in injec-
tion drug use, and needle-sharing and needle-cleaning behaviors
during most recent injection. Using a risk-and-dependency spec-
trum (Gable, 1993), we grouped drugs into three broad categories
according to their dependency potential—lethal dose, effective
dose, and acute toxicity: (a) high risk and high dependency
(HRHD), (b) high risk and low dependency (HRLD), and (c) low risk
and low dependency (LRLD). Gable found a differential margin of
safety between drug groups. HRHD drugs (i.e., cocaine, crack
cocaine, methamphetamine, heroin and cocaine in combination,
heroin alone, opium, and alcohol) are described as having a mod-
erate-to-severe risk of fatality and a moderate-to-very-high poten-
tial for dependency. HRLD drugs (i.e., mescaline and ecstasy)
have the same range of fatality risk as HRHD drugs yet have a
decreased potential for dependency. Alternatively, LRLD drugs
(i.e., LSD, mushrooms, peyote, and marijuana) have a low-to-neg-
ligible risk of fatality and a much lower dependency potential than
have HRHD drugs.
Sexual behaviors included number of sex partners, involvement in
sexual intercourse while high on drugs or alcohol, and involve-
ment in survival sex (ever). We defined a sexual encounter as
engaging in vaginal or anal intercourse. Other indices of HIV risk

PEER-GROUP AFFILIATION AND HIV RISK BEHAVIORS
69
assessed included prior infection with sexually transmitted dis-
ease (STD) and perceived risk for infection with an STD or HIV.
Previous research conducted with runaway or homeless youth
suggests the need to distinguish primary and other sex partners
(Anderson et al., 1994). The survey instrument therefore made
this distinction: a primary partner was defined as a "main or
steady sex partner or someone that is important or special” (e.g.,
girl- or boyfriend, or lover), and other partners were defined as
"someone other than your main partners" (e.g., casual or survival
sex partners). Condom use at most recent sexual encounter with
each partner type was computed.
Chi-square analyses were performed to determine significant dif-
ferences across the five waves of data collection. These analyses
revealed that the proportion of youth in each peer group differed
by wave (chi square = 69.9, P < .001). Specifically, youth inter-
viewed in the later waves were more likely to be punks or skin-
heads (51% of Wave 5 vs. 23% in Wave 1), and youth interviewed
in the earlier waves were more likely to be in the “other” affiliation
category (32% in Wave 1 vs. 15% in Wave 5). Therefore, we con-
trolled for wave in all subsequent analyses. It is also important to
note that this research was conducted as part of an evaluation of
street outreach services and that the enhanced interventions were
delivered after the second wave of data collection. By controlling
for wave in later analyses, we also controlled for potential inter-
vention effects on the behaviors of youth within these peer groups.
Next, multiple regression analyses were performed with SAS gen-
eral linear models to determine whether peer-group affiliation was
a significant predictor of alcohol and other drug use and of sex
and drug-using behaviors. The final regression model, which was
significant at P < .05, used Tukey’s honestly significant difference
(HSD) to identify which groups differed on the dependent variables
at the .05 level. Finally, odds ratios were computed in logistic
regression models to calculate the relative risk of engaging in each
behavior for youth in each peer group compared with youth in all
other peer groups.

AESOP
70
RESULTS
S
AMPLE
C
HARACTERISTICS
Youth ranged in age from 13 to 23 years; nearly 80% were aged 16
to 21 years (Table 1). Most of these youth were male (71%), and
the males were significantly older than the females (t = 7.81,
P < .0001). More than half (51%) were Caucasian, and 49% were
members of ethnic minority groups: African American (20%), Lat-
ino (15%), Native American (5%), Asian/Pacific Islanders (2%), or
another ethnic minority group (6%). Of the 752 youth in the
study, 69% reported that at the time of the interview they were liv-
ing on the streets, in a squat or shelter, or in an abandoned build-
ing. Of youth who were living on the streets or without a place of
their own, most had done so for 1 year or more (51%); 14%
reported having been without a place to stay or a place of their
own for 6 months to 1 year; and 35% for less than 6 months. Of
the 31% who had some other place to stay at the time of the inter-
view, 69% had lived in their own house or apartment within the
past 12 months, and 62% had stayed with family or some other
relative. However, most of these youth reported having been pre-
cariously housed at some time during the past 12 months, either
by staying at a friend’s house or apartment (80%), with a boyfriend
or girlfriend or lover (58%), in a foster home or group home (28%),
or at a halfway house or treatment center (10%).
In response to the list of peer groups, 36% responded that they
were most like or identified with punks or skinheads, 14% with
gang members, 12% as loners, 10% as hustlers (most were
involved in the sex trade), and 7% as druggies (most were involved
in drug running or dealing). Of youth who did not identify with one
of these groups, 9% identified with some other specified group
(e.g., surfers, Deadheads [followers of the Grateful Dead rock
band], gay or lesbian youth not involved in the sex trade or sur-
vival sex, drag queens or transgender) although each group
accounted for no more than 2% of the total sample. Twelve per-
cent identified with some other group not listed as a response
option—taggers, squatters, musicians, ravers, or rockers; each of
these groups accounted for no more than one to two youth. Thus,
22% of the sample were included in an “other” affiliation category.

PEER-GROUP AFFILIATION AND HIV RISK BEHAVIORS
71
Between-group comparisons revealed that punks or skinheads
were significantly more likely to be Caucasian (70%) than were
gang members or loners (Table 1). Gang members were signifi-
cantly more likely than all other groups to be African American
(44%), and druggies were significantly more likely to be male than
were hustlers and youth in the “other” category (56%) (Table 1).
With respect to age, hustlers were significantly older than all of
the other groups (mean, 19.2 years), and gang members were the
youngest of the groups (mean, 17.7 years); the mean ages for the
other groups were 19.1 years for the loners, 18.5 years for the
punks or skinheads, and 18.4 years for the druggies.
D
RUG
-U
SING
P
ATTERNS
Rates of alcohol and other drug use were remarkably high among
the youth in this sample (Table 2). Specifically, 75% reported ever
having used a substance in the HRHD drug category: 66%
reported ever having used speed, 52% ever having used cocaine,
41% crack cocaine, and 41% alcohol at least once a week. Thirty-
seven percent reported having used HRLD drugs (32% reported
ever having used ecstasy, 17% reported ever having used mesca-
line) and 88% reported having used an LRLD drug (65% reported
ever having used LSD, 50% ever having used mushrooms, 22%
ever having used peyote, and 45% reported ever having used mari-
juana at least once per week). Of the sample, 37% reported ever
having injected drugs; of those, 58% reported having injected
within the past 30 days, and 45% reported having shared their nee-
dle or equipment at their most recent injection; 82% reported hav-
ing cleaned their needle with bleach at their most recent injection.
Analyses further revealed significant differences between the peer
affiliation groups with respect to alcohol and other drug use (Table
2). Specifically, youth affiliated with the punks or skinheads,
druggies, and hustlers were significantly more likely than all other
groups to report having used a greater number of different drugs
in all three of the drug risk categories. Odds ratios further
revealed that punks or skinheads, as compared with all other
groups, were nearly three times more likely than the other groups
to have used cocaine and speedball, and four times more likely to
have used opium. Both punks or skinheads and druggies, com-
pared with all other groups, were three times more likely to report

AESOP
72
the use of heroin and mushrooms, four and two times (respec-
tively) more likely to have used speed, two times more likely to
report the use of crack cocaine, and four times more likely to use
alcohol at least once per week. In contrast, gang members and
loners were groups least likely to report use of HRHD drugs, par-
ticularly cocaine, speed, speedball, and heroin. Gang members
were, however, four times more likely to have used marijuana at
least once per week compared with all other groups; hustlers and
loners were the least likely to use marijuana with this frequency.
Punks or skinheads were also most likely to report ever having
injected drugs, and gang members were the least likely to report
ever having injected drugs. There were no significant differences
among the groups with respect to needle sharing and cleaning
practices (gang members were not included in this analysis given
the low prevalence of injection drug use).
S
EXUAL
R
ISK
B
EHAVIORS
The study youth had also engaged in a number of HIV risk-related
sexual behaviors, including survival sex (32%), sex with multiple
partners (32%), sexual intercourse while high (51%), and unpro-
tected sexual intercourse with primary (48%) or other (27%) sex
partners during most recent encounter (Table 3). Of the sample,
18% reported having been given a diagnosis of an STD, yet only
47% perceived themselves at risk for an STD; 59% perceived
themselves at risk for HIV infection. As was true for drug use,
there were distinct risk patterns among youth according to peer-
group affiliation, although the patterns were fewer. Specifically,
punks or skinheads were most likely to have been “high” during
their most recent sexual encounter (71%), and hustlers were sig-
nificantly more likely to have engaged in survival sex (81%), to
have had multiple sex partners (72%), and to have been given a
diagnosis of an STD (31%). There were no significant differences
between the groups with respect to use of a condom during the
most recent sexual encounter or the perceived risk for an STD or
HIV infection. Remarkably, 78% of the sample reported having
been tested for antibodies to HIV. There were, however, no signifi-
cant between-group differences with respect to whether youth had
been tested.

PEER-GROUP AFFILIATION AND HIV RISK BEHAVIORS
73
DISCUSSION
Despite efforts to reach this very important, yet largely hidden,
population and our efforts to overcome the limitations of earlier
studies (i.e., convenience sampling at service locations), there are
some limitations to this study. First, the findings rely on clients'
self-reported behaviors, which cannot be independently verified.
The levels of use of alcohol and other drugs and the levels of sex
and drug-using behaviors (e.g., survival sex, needle sharing) may
underestimate their prevalence, given that many of these behav-
iors are illegal and socially undesirable and because the data were
collected by an interviewer who was not known to the youth before
the interviews. A second limitation is that the data are cross-
sectional and therefore do not contain information about the tem-
poral relationship between clients' introduction to the streets,
selection of, or affiliation with, a peer group, and involvement in
risky behaviors. Thus, no statements can be made about the
causal relationship between peer-group affiliation, peer norms or
perceived peer norms, and drug-using and HIV risk behaviors.
Finally, although this sample is likely to be representative of the
street youth population in the target geographic area, it is unclear
how generalizable these findings are to street youth populations in
other cities (e.g., Boston, New York, San Francisco). Future
research should continue to use street-based probability sampling
techniques to evaluate similarities and differences among street
youth populations from different geographic areas.
Despite these limitations, this study provides evidence that the
street youth population in Hollywood comprises several groups
that differ with respect to members’ involvement in alcohol and
other drug-using and HIV risk behaviors. These findings are sig-
nificant for a number of reasons. First, they suggest the need to
further define the street youth population and differences with
respect to health problems and risk profiles according to self-
identified peer-group affiliation. Whereas growing evidence sug-
gests that inner-city street youth are at increased risk for the
abuse of alcohol and the use of other substances (Fullilove et al.,
1993) and HIV transmission (Kipke et al., 1995), these findings
suggest that interventions be tailored to meet the specific needs
and risk profile of each segment of the larger street youth popula-
tion. Future research and service delivery efforts should therefore

AESOP
74
begin systematically addressing the diversity of this population.
Future research is also needed to more fully characterize behav-
ioral differences between subcultural groups, particularly with
respect to health and risk profiles. Attempts to replicate these
findings in other urban settings would also be of interest.
Second, these findings suggest that peers may influence street
youth both negatively and positively. For example, our findings
suggest that gang members were at less risk for the use of HRHD
drugs, for involvement in injection drug use, and for sexual inter-
course with multiple partners. Little research has examined the
social networks of street youth, the process by which youth
become affiliated with street peer groups, or the influence of peer-
group pressure, values, norms or perceived norms on youths’
behavior. Research is therefore needed to more fully characterize
the importance of peer relationships among these youth and the
effect of these relationships on street youths’ involvement in risky
as well as preventive behaviors.
Finally, our findings suggest that there is some urgency in the
need to intervene with this population. Designing interventions
that challenge street youth to engage in health-promoting behav-
iors is, at best, a difficult task. Our findings suggest that it may
be beneficial to develop interventions or intervention approaches
that match the different street youth groups. Transitioning them
off the streets or into more stable living circumstances may be the
long-term goal. More information, however, is needed—from
research and service demonstration projects—to guide the devel-
opment of intervention strategies that will identify, engage, and
change the health and risk profiles of these youth. Interventions
may also need to be tailored to address the unique risk profile of
each social peer group.
Street outreach has recently been demonstrated to be an effective
strategy for reaching persons who are not served by traditional
health care programs and who are at risk for HIV transmission
(Wieble et al., 1996). Popular outreach approaches attempt to
engage high-risk persons through the distribution of bleach and
condoms, needle cleaning and condom demonstrations, and role-
playing of safer sex techniques. Other findings suggest that out-
reach and prevention efforts must be delivered in settings where
the target population can be found and must be staffed by people

PEER-GROUP AFFILIATION AND HIV RISK BEHAVIORS
75
who know the community’s values and norms, speak the language
of those whom they are seeking to attract, and are trusted by
members of the target community. A growing literature demon-
strates the effectiveness of peers, both as outreach workers (the
indigenous leader model) and behavior change specialists. Thus,
one promising intervention might use peers to conduct street out-
reach to youth, matching peers to the characteristics, values, and
norms of the different street youth subcultural groups (e.g., hiring
youth who can serve as positive role models, who are or were
homeless, punks or skinheads, formerly involved in survival sex,
former gang members). Outreach workers might be effective inter-
ventionists for changing peer norms and encouraging youth to
seek services, promoting preventive behaviors, and discouraging
risky behaviors.
ACKNOWLEDGMENTS
This study was supported by the Centers for Disease Control and
Prevention, cooperative agreement U62/CCU907198. The views
expressed are those of the authors, not necessarily the funding
agency. Special thanks go to John Anderson and Judith Green-
berg; members of the AESOP field research team (Michael Cohen,
Marcus Kuiland-Nazario, Burke Nelson, Sara Parker, Audruin
Pittman, German Rodriguez, Lily Rodriguez); collaborating youth-
serving agencies (Angel's Flight, Covenant House California, Holly-
wood YMCA, Los Angeles Gay and Lesbian Community Services
Center, Los Angeles Free Clinic, Los Angeles Youth Network, My
Friend's Place, PROTOTYPES, Inc., Teen Canteen, The Way In);
and Eunice Villatoro.

AESOP
76
References
Anderson, J., Pennbridge, J., & Freese, T. (1994). Sexual risk
behavior and condom use among street youth in Hollywood.
Family Planning Perspectives, 26, 22-25.
Biglan, A., Metzler, C.W., Wirt, R., Ary, D., Noell, J., Ocs, L.,
French, C., & Hood, D. (1990). Social and behavioral factors
associated with high-risk sexual behavior among adolescents.
Journal of Behavioral Medicine, 13(3), 253-261.
Bond, L.S., Mazin, R., & Jiminez, M.V. (1992). Street youth and
AIDS. AIDS Education and Prevention, Fall (Suppl.), 14-23.
Brown, B.B., Clasen, D.R., & Eicher, S.A. (1986). Perceptions of
peer pressure, peer conformity dispositions, and self reported
behavior among adolescents. Developmental Psychology,
22(4), 521-530.
CDC. (1996). HIV/AIDS Surveillance Report, 8(No. 1), 1-39.
Dinges, M.M., & Oetting, E.R. (1993). Similarity in drug use
patterns between adolescents and their friends. Adolescence,
28(110), 253-266.
Dolcini, M.M., & Adler, N.E. (1994). Perceived competencies, peer
group affiliation, and risk behavior among early adolescents.
Health Psychology, 13(6), 496-506.
Elliott, D.S., Ageton, S.S., Huizinga, D., Knowles, B.A., & Canter,
R.J. (1983). The prevalence and incidence of delinquent
behavior: 1976-1980. In National estimates of delinquent
behavior by sex, race, social class and other selected variables.
Boulder, CO: Behavioral Research Institute.
Ennett, S.T., & Bauman, K.E. (1993). Peer group structure and
adolescent cigarette smoking: A social network analysis.
Journal of Health and Social Behavior, 34, 226-236.
Fullilove, M.T., Golden, E., Fullilove, R.E., Lennon, R., Porterfield,
D., Schwarcz, S., & Bolan, G. (1993). Crack cocaine use and
high-risk behaviors among sexually active black adolescents.
Journal of Adolescent Health, 14, 295-300.

PEER-GROUP AFFILIATION AND HIV RISK BEHAVIORS
77
Gable, R.S. (1993). Toward a comparative overview of dependence
potential and acute toxicity of psychoactive substances used
nonmedically. American Journal of Drug and Alcohol Abuse,
19, 263-281.
Jessor, R., & Jessor, S.L. (1977). Problem behavior and
psychosocial development: A longitudinal study of youth. New
York: Academic Press.
Kennedy, M.G., Greenberg, J., Clatts, M., Kipke, M.D., & Mills, S.
(1994). Patterns and correlates of high-risk behavior among
street youth. Presented at the annual convention of the
American Public Health Association, Washington, DC.
Kipke, M., Futterman, D., & Hein, K. (1990). HIV infection and
AIDS during adolescence. Medical Clinics of North America,
74(5), 1149-1167.
Kipke, M.D., Montgomery, S.B., & MacKenzie, R.G. (1993).
Substance use among youth seen at a community-based
health clinic. Journal of Adolescent Health, 14, 289-294.
Kipke, M.D., O’Connor, S., Palmer, R., & LaFrance, S. (1993).
Street youth and HIV: Meeting the challenge in two communities.
Presented at the annual conference of the American Public
Health Association, Washington, DC.
Kipke, M.D., O’Connor, S., Palmer, R., & MacKenzie, R.G. (1995).
Street youth in Los Angeles: Profile of a group at high risk for
HIV. Archives of Pediatrics and Adolescent Medicine, 149(5),
513-519.
LaFrance, S.R., Pennbridge, J., & Casey, C.C. (1992). A service
provider’s typology of street youth at risk for HIV in Los
Angeles, California. Report prepared for the Centers for
Disease Control and Prevention.
Larkin, R.W. (1979). Suburban youth in cultural crisis. New York:
Oxford University Press.
Light, D., & Keller, S. (1979). Sociology. New York: Knopf.
Mosbach, P., & Leventhal, H. (1988). Peer-group identification
and smoking: Implications for intervention. Journal of Ab-
normal Psychology, 97, 238-245.

AESOP
78
Newcomb, M.D., & Bentler, P.M. (1989). Substance use and
abuse among children and teenagers. American Psychologist,
44, 242-248.
Oetting, E.R., & Beauvais, F. (1986). Peer cluster theory: Drugs
and the adolescent. Journal of Counseling and Development,
65, 17-22.
Robertson, M.J. (1989). Homeless youth: Patterns of alcohol use.
Berkeley, CA: Alcohol Research Group, School of Public
Health, University of California at Berkeley.
Rotheram-Borus, M.J., Koopman, C., & Ehrhardt, A.A. (1991).
Homeless youths and HIV infection. American Psychologist,
46(11), 1188-1197.
Rotheram-Borus, M.J., Meyer-Bahlburg, H.F., Rosario, M.,
Koopman, C., Haignere, C.S., Exner, T.M., Matthieu, M.,
Henderson, R., & Gruen, R.S. (1992). Lifetime sexual
behavior among predominately minority male runaways and
gay/bisexual adolescents in New York City. AIDS Education
and Prevention, Fall (Suppl.), 34-42.
Sussman, S., Dent, C., McAdams, L., Stacy, A., Burton, D., &
Flay, B. (1994). Group self-identification and adolescent
cigarette smoking: A 1-year prospective study. Journal of
Abnormal Psychology, 103(3), 576-580.
Sussman, S., Dent, C., Stacy, A., Burciaga, C., Raynor, A., Turner,
G.E., Charlin, V., Craig, S., Hansen, W., Burton D., & Flay, B.
(1990). Peer-group association and adolescent tobacco use.
Journal of Abnormal Psychology, 99(4), 349-352.
U.S. Department of Health and Human Services. (1983). Run-
away and homeless youth: National program inspection.
Washington, DC: Office of the Inspector General, Region X.
Vermund, S.H. (1997). Transmission of HIV-1 among adolescents
and adults. In V.T. Devita, S. Hellman & S.A. Rosenberg (Eds.),
AIDS: Etiology, diagnosis, treatment and prevention. Phila-
delphia: Lippincott-Raven.

PEER-GROUP AFFILIATION AND HIV RISK BEHAVIORS
79
Wiebel, W.W., Jimenez, A., Johnson, W., Ouellet, L., Jovanovic, B.,
& Lampinen, T. (1996). Risk behavior and HIV seroincidence
among out-of-treatment injection drug users: A four-year
prospective study. Journal of Acquired Immune Deficiency
Syndromes and Human Retrovirology, 12, 282-289.
Yates, G.L., MacKenzie, R., Pennbridge, J., & Cohen, E. (1988). A
risk profile comparison of runaway and non-runaway youth.
American Journal of Public Health, 81, 208-210.
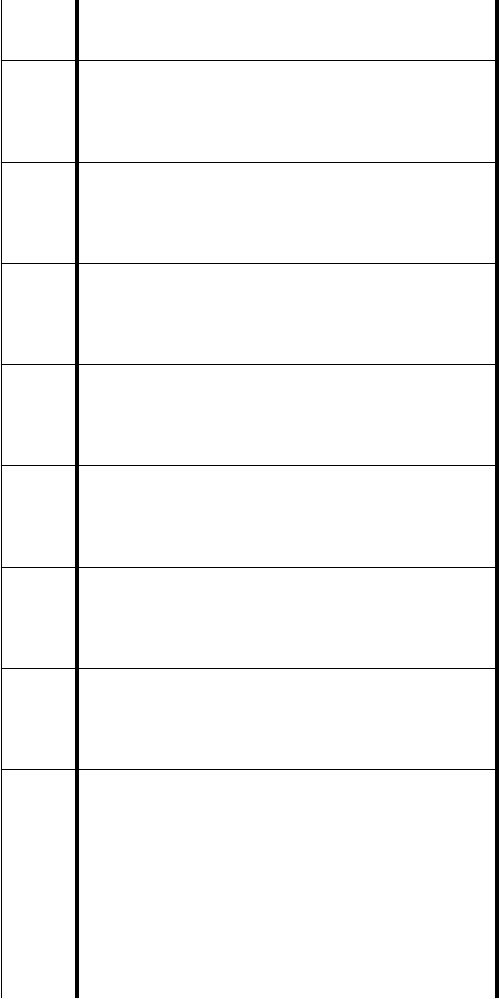
Table 1. Demographic Profile of Study Sample
Risk
Total
N = 750
%
Punks
n = 264
%
Druggies
n = 54
%
Hustlers
n = 72
%
Gang
n = 106
%
Loners
n = 89
%
Other
n = 165
%
HSD
%
Gender
Male 71 64 54 94 61 74 80 18
Female 29 36 44 6 39 26 20 18
Ethnicity
Caucasian 52 70 67 53 23 45 41 19
African American 19 7 20 21 43 24 19 16
Latino 15 11 7 17 22 13 23 15
Asian/Pacific Islander 2 2 0 3 2 3 4 6
Other 11 10 24 7 10 15 8 9
Age (years)
13-15 9 5 9 11 22 4 8 12
16-18 41 49 43 25 40 38 39 20
19-21 39 39 41 46 32 38 41 20
22-23 11 7 7 18 7 19 12 13
HSD — honestly significant difference. A means of comparing columns for minimal percentage difference required for signifi-
cance of P < .05. For example, in the first row, males account for 64% of the punks. The only group outside the 18% HSD
range (i.e., 64% + 18% = 82%) is the hustlers, at 94%.

Table 2. Rates of Lifetime Substance Use for Each Peer Youth Group
Risk
Total
N = 750
%
Punks
n = 264
%
Druggies
n = 54
%
Hustlers
n = 72
%
Gang
n = 106
%
Loners
n = 89
%
Others
n = 165
%
HSD
%
High risk & high dependency 75 92
b
80
bc
86
b
61
d
58
d
63
cd
1 7
Cocaine 52 70
b
59
bc
58
bc
31
d
41
cd
44
cd
2 0
Crack 41 46
bc
52
b
54
b
31
d
38
bc
35
bc
2 0
Speed 66 85
b
74
ac
65
cd
52
d
53
d
53
d
1 9
Speedball 26 41
b
33
bc
18
cd
12
d
23
cd
19
cd
1 8
Heroin 28 46
b
37
ac
21
cd
9
d
23
cd
16
d
1 8
Opium 25 40
b
17
c
16
c
10
c
17
c
14
c
1 7
Alcohol
a
41 59
b
43
bc
33
c
44
bc
25
c
26
c
2 0
High risk & low dependency 37 52
b
30
cd
44
bc
22
d
29
cd
33
bcd
20
Mescaline 17 23
b
13
b
15
b
13
b
15
b
10
b
1 5
Ecstasy 32 45
b
24
cd
41
bc
19
d
22
cd
30
bcd
19
Low risk & low dependency 88 96b 93b 83bc 88bc 79c 77c 14
LSD 65 84
b
76
b
46
c
50
c
52
c
48
c
1 9
Mushrooms 50 68
b
61
b
41
c
28
c
38
c
36
c
2 0
Peyote 22 32
b
20
bc
17
bc
17
bc
17
bc
12
c
1 7
Marijuana
a
45 46
bc
44
bc
35
c
59
b
35
c
30
c
2 0
Ever injected drugs 37 52
b
38
bc
34
bc
13
d
45
b
24
cd
2 1
Shared needle at most
recent injection
45 41
b
53
b
36
b
—58
b
40
b
5 2
Cleaned needle at most
recent injection
82
b
76
b
90
b
——86
b
—61
HSD–honestly significant difference. A means of comparing columns for minimal percentage difference required for significance
of P < .05.
— Percentages were not calculated for cells with fewer than 10 observations.
a
Percentage who use at least once per week.
b, c, d
Percentages with the same letter are not significantly different at P < .05.

Table 3. Risk Behaviors, by Peer Youth Group
Risk
Total
N = 750
%
Punks
n = 264
%
Druggies
n = 54
%
Hustlers
n = 72
%
Gang
n = 106
%
Loners
n = 89
%
Other
n = 165
%
HSD
%
Condom use, most recent sexual
encounter
Main partner 52 50
a
50
a
44
a
62
a
35
a
50
a
38
Casual partner 73 72
a
65
a
73
a
65
a
83
a
81
a
29
Sex while high, most recent encounter 51 71
a
52
ab
39
b
56
ab
33
b
41
ab
31
Survival sex (ever) 32 19
d
41
bc
81
a
19
d
29
cd
48
b
18
Multiple partners, past month 40 34
b
35
b
72
a
31
b
31
b
44
b
20
Prior STD 18 17
ab
24
ab
31
a
18
ab
15
b
15
ab
16
Tested for HIV 78 76
a
72
a
87
a
73
a
81
a
82
a
17
Perceived risk for STD 47 50
ab
34
b
61
a
45
ab
51
ab
47
ab
21
Perceived risk for AIDS 59 65
a
61
a
63
a
51
a
65
a
59
a
21
HSD–honestly significant difference. A means of comparing columns for minimal percentage difference required for significance
of P < .05.
a,b,c
Percentages with the same letter are not significantly different at P < .05.

83
ENHANCED STREET OUTREACH
AND CONDOM USE
BY
HIGH-RISK POPULATIONS IN FIVE CITIES
John E. Anderson
*
, Judith Greenberg
†
,
and Robin MacGowan
*
AESOP was a 5-year, multifaceted evaluation of street outreach
interventions to injection drug users (IDUs) and high-risk youth,
which was conducted in six cities in the United States. We sum-
marize one aspect of the research project: surveys of IDUs and
youth that were conducted as part of a quasi-experimental
research design before and after enhancement of outreach activi-
ties. The objectives of the surveys were threefold: to measure
changes in HIV-related risk behavior, to measure changes in expo-
sure to street outreach workers, and to measure the association
between interaction with street outreach workers and condom use.
METHODS
S
TUDY
D
ESIGN
We used a quasi-experimental research design. Collaborating
research teams in each of six cities selected study and comparison
areas for their high-risk population. The study and comparison
areas were selected for similarity of risk-group characteristics
(age, race/ethnicity) and risk group behavior. Each area also
needed adequate numbers of the group of interest and some level
of street outreach programs in both areas. Researchers in Phila-
delphia, Chicago, and Atlanta focused on IDUs. San Francisco
*Division of HIV/AIDS Prevention - Intervention Research and Support, National
Center for HIV, STD, and TB Prevention, Centers for Disease Control and
Prevention, Atlanta, Georgia
†
Division of STD Prevention, National Center for HIV, STD, and TB Prevention,
Centers for Disease Control and Prevention, Atlanta, Georgia

AESOP
84
researchers focused on youth. In Los Angeles and New York, sepa-
rate teams focused on youth and on IDUs. In some cities, study
and comparison areas included multiple geographic areas, reflect-
ing the spread of IDUs or youth in that geographic area. Street
outreach enhancements targeting sex and drug-using behaviors
were developed and implemented in the study areas only. These
ranged from a “rubber room” in a health clinic, where youth could
obtain condoms and health information, to a mobile van for HIV
counseling and testing and other medical services for IDUs.
Enhancements differed by city (see the Results section). A series
of cross-sectional surveys were conducted both in the study and
comparison areas. Each site conducted a minimum of two pre-
enhancement rounds of interviews approximately every 3 months
from January through August 1993 and two postenhancement
rounds during 1994 and 1995, once the enhancements had been
fully implemented for at least 3 months. In this paper we compare
aggregated data from the two rounds of preenhancement surveys
with two rounds of postenhancement surveys for five sites.
ELIGIBILITY
Eligible IDU respondents were defined as persons within the geo-
graphical boundaries of the intervention or comparison area who
had injected illegal drugs in the past 3 years. (In three cities—
Atlanta, Los Angeles, and Philadelphia—up to 30% of the sample
were allowed to be persons who had used crack cocaine in the
past month but who had not injected in the past 3 years). Eligible
youth respondents were defined as youth aged 12 to 23 years who
had been recurrently without shelter during the past year, without
permanent shelter for 2 months, or derived their livelihood from
the street economy (drugs, prostitution, panhandling, crime). For
each research team, the goal was to complete 200 interviews in
the study area and 200 in the comparison area during each round
of the survey.

ENHANCED STREET OUTREACH AND CONDOM USE
85
SAMPLING
Street outreach takes place in the natural setting of the IDU and
high-risk youth populations; thus, we needed methods by which
to obtain respondents in their communities, not in clinic, shelter,
or other institutional settings. Because the behaviors that defined
these risk groups (e.g., prostitution, panhandling, drug dealing or
injecting illegal drugs or smoking crack) are not common in the
general population and because many group members would not
have been located through phone or residence surveys, standard
survey sampling methods were not possible. Systematic sampling
methods were designed to reduce the sources of bias to a mini-
mum and to produce comparable repeat samples over several
waves of interviewing (Anderson et al., 1996). (See the Methods
section for a detailed description of sampling methods and Kipke,
Unger, Palmer, Iverson, and O’Connor in this monograph for how
these methods were applied at the Los Angeles youth site).
Interviewers were required to keep track of the numbers of refus-
als and eligible clients who did not complete interviews. At all
sites, clients were offered cash or food incentives to participate.
Overall response rates combining nonresponse for refusals before
screening and for noncompletion of the interview by eligible
respondents ranged from 73% to 99% (overall rate, 90%). These
response rates should be considered approximate: it is likely that
not all potential respondents were approached, because they were
not seen or were determined unapproachable (e.g., because an
illegal drug transaction was taking place).
We present data from five groups of researchers who participated
in AESOP: two groups that focused on youth (Children’s Hospital
of Los Angeles and the AIDS Office of the San Francisco City
Health Department) and three groups that focused on IDUs (Uni-
versity of Illinois at Chicago, Los Angeles County AIDS Office, and
Philadelphia Health Management Corporation). These groups had
collected four rounds of data—two before the enhanced interven-
tion and two after the enhancement was in place.

AESOP
86
STATISTICS
Dependent variables. The main dependent behavioral variables
were six measures of condom use during most recent sexual
encounter. Condom use variables were measured separately for
vaginal, anal, and oral sex, and for main and casual partners.
Note that these behaviors were not measured for the entire sam-
ple, but only for those who engaged in this particular activity (e.g.,
anal sex with casual partner). Condom use is a dichotomous mea-
sure of whether condoms were used during the most recent sexual
encounter. The two waves of pre- and postenhancement data were
aggregated to form one set of pre- and one set of postenhancement
scores.
Predictor variables. In addition to location (study area versus
comparison area) and time period (pre- versus postenhancement),
we examined the relationship between risk behavior and predictor
variables that have been associated with condom use: background
factors (age, sex, race/ethnic group, support through street econ-
omy), sex behavior variables (types of partners, number of part-
ners, exchange of sex for needs, sexual orientation, carrying
condoms), and drug-related behavior (injection history, needle
sharing, crack use, drug treatment history). We also examined
exposure to street outreach programs in the past 6 months, meas-
ured by yes-or-no variables (talked with outreach workers;
received condoms, material, or bleach from outreach workers).
Statistical significance between the pre- and postenhancement
rounds was evaluated by using chi-square measures for percentages.
Multivariate modeling. In using the quasi-experimental design
to assess the effect of enhanced street outreach interventions on
condom use, we were looking for the effect of greater condom use
in the study area during the postenhancement period. Logistic
regression models to measure this took the following form:
condom use = study area + postenhancement period +
postenhancement study area
That is, we looked for regression effects of being in the study area,
of being in the postenhancement period, and an interaction term
measuring the effects of being in the postenhancement study area.
A positive coefficient (or odds ratio of greater than 1.0) for the

ENHANCED STREET OUTREACH AND CONDOM USE
87
interaction term is consistent with effectiveness of the enhance-
ment under the assumptions of the quasi-experimental research
design. These three terms were included in every model. The
models were computed in two ways: including only those three
terms and including the three terms plus a series of covariates
measuring respondent characteristics, risk behaviors, and contact
with outreach programs. Stepwise modelling methods were used
to reduce the number of covariates to those that were significant
at the .05 level in the final models.
Some of the predictor variables can be considered intermediate
variables. For this reason, we also looked at logistic regression
analysis to determine the factors associated with getting condoms
from outreach workers and with having condoms at the time of
interview. To the extent that these factors affect condom use and
are in turn associated with enhanced programs, the programs can
be said to have indirect effects on condom use.
RESULTS
C
HILDREN
’
S
H
OSPITAL
OF
L
OS
A
NGELES
This project evaluated street outreach services provided by several
agencies in the Hollywood area. The study and comparison areas
were Hollywood and downtown San Diego. The enhanced inter-
vention centered on the opening of a storefront center (the rubber
room) for the distribution of condoms and the provision of other
services to street youth. The total enhanced outreach program
contained the following elements: (a) interagency outreach coordi-
nation, (b) peer outreach team, (c) rubber room, (d) small print
media, and (e) referral to needle exchange program.
The characteristics of survey respondents in the pre- and posten-
hancement periods were similar in the study and comparison
areas. Even the differences that were statistically significant did
not seem to be meaningful differences. For example, in the post-
enhancement period, 100% of respondents had lived on the street
in the past year compared with 93.7 % in the preenhancement
period—a significant difference, but probably not representative of
a substantive difference between the samples.

AESOP
88
For the respondents’ reported contact with AIDS-related street
outreach services, there were no statistically significant differ-
ences between the pre- and postenhancement periods. Pre-
enhancement levels of contact were quite high in the intervention
area—64.9% of respondents had spoken with an outreach worker
in the past 6 months, and 54.6% had received condoms. In con-
trast, in the comparison area (downtown San Diego) only 20.7%
had talked with outreach workers in the past 6 months, and
12.9% had received condoms. Differences in exposure to outreach
were controlled in the logistic regression analyses.
Specific survey questions were added to measure contact with the
enhanced street outreach intervention in the study area. Of the
youth, 30% reported having visited the rubber room, and 12%
reported having received condoms there; 29% reported having
received condoms from an outreach worker from AESOP. Regard-
less of pre- or postenhancement, the percentage of respondents
who used condoms during the most recent sexual encounter dif-
fered by the pattern mention earlier: condom use was higher for
casual partners and was highest for anal sex, followed by vaginal
and oral sex.
Logistic regression results indicate that being in the postenhance-
ment study area (the quasi-experimental effect of interest) was not
statistically significantly associated with condom use during most
recent vaginal sex for main or casual partners (Table 1). Getting
condoms from outreach workers was a strong predictor of having
condoms for youth who reported main (odds ratio [OR], 2.5; confi-
dence interval [CI], 1.5–4.2) and casual (OR, 2.4; CI, 1.5–4.0)
partners. With respect to using condoms during most recent vagi-
nal sex, at postenhancement 47.6% of youth reported having used
condoms with main partner, and 71.8% reported having used con-
doms with casual partners. Having a condom at interview was
associated with higher odds of having used condoms during most
recent vaginal sex with main (OR, 2.3; CI, 1.5–3.6) and casual
partners (OR, 2.1; CI, 1.3–3.5).
Many of the high-risk youth interviewed had had contact with
street outreach workers in the pre-and postenhancement periods
in the study area. High levels of preenhancement contact in the
study area probably made large increases in exposure to outreach
in the postenhancement period difficult. No statistically signifi-

ENHANCED STREET OUTREACH AND CONDOM USE
89
cant increases in condom use were noted. However, there was a
strong link between condom use, having condoms, and getting
condoms from outreach workers, which suggests the need to
encourage the carrying of condoms, especially by high-risk youth
in the Hollywood and San Diego areas, for whom spontaneous sex
is probably the norm.
S
AN
F
RANCISCO
C
ITY
H
EALTH
D
EPARTMENT
The study area was the Haight-Asbury District in San Francisco,
where high-risk youth congregate; the comparison area was a
group of outlying areas where street youth with similar character-
istics were to be found (Arcata, Berkeley, Eureka, and Santa
Cruz). The enhanced intervention was the Haight-Ashbury Youth
Center, a storefront operation that was developed especially for
AESOP. The youth center fielded a street outreach team that pro-
vided (in addition to standard outreach services) referrals for med-
ical, drug treatment, and other services. (See Gleghorn et al. in
this monograph for a detailed description.) Community activities
were sponsored at the youth center: discussion groups, women's
shower times, community-designed HIV prevention posters, a
Grateful Dead prevention message video and Grateful Dead logo
condoms, and outpatient drug treatment services.
Survey data indicate that the youth interviewed in the study and
comparison areas were similar. In the study area, there were some
differences of interest between the pre- and postenhancement
periods. Respondents in the later period were less likely to be
male and more likely to inject drugs and use crack cocaine. Con-
tact with outreach programs was higher in Haight-Ashbury than
in the outlying areas for both periods. In the study area, there
were statistically significant increases from pre- to postenhance-
ment in the percentage of high-risk youth who reported having
talked with outreach workers and received materials from them.
High-risk respondents in Haight-Ashbury reported considerable
contact with the Haight-Ashbury outreach center: 60.1% had
heard of the center, and 36.5% had received services there.
In San Francisco, there were no significant differences pre- and
postintervention between study and comparison youth to indicate
a change to safer behavior, defined as condom use during most

AESOP
90
recent sexual encounter by type of partner and type of sex. Multi-
variate logistic regression analysis (Table 2) indicates that being in
the postenhancement study area was not significantly associated
with condom use for main or casual partners. Having a condom
at interview, however, was associated with higher likelihood of use
during most recent vaginal sex with main partners (OR, 2.4; CI,
1.3–4.4). For respondents with main partners, having a condom
at interview was, in turn, strongly associated with having received
condoms from outreach workers (OR, 3.4; CI, 1.8–6.4).
Survey results for San Francisco indicate increased contact with
outreach programs in the study area during the postenhancement
period. The survey also measured a substantial amount of con-
tact with the youth center by youth contacted on the street in the
Haight-Ashbury District. Although no apparent behavior change
was measured through two rounds of postenhancement surveys,
the data do indicate the importance of street outreach programs’
providing condoms to youth and encouraging youth to carry them.
U
NIVERSITY
OF
I
LLINOIS
AT
C
HICAGO
The Chicago project evaluated street outreach to IDUs in inner-
city neighborhoods. The study area was west of the Loop, and the
comparison area was near the Southside. The enhanced interven-
tion centered on services delivered from a mobile van that pro-
vided on-site HIV counseling and testing. Additional enhance-
ments included increasing the number of outreach workers,
escorting clients to referral services, improving client follow-up,
and making community presentations.
Comparisons of the pre- and postenhancement characteristics of
respondents indicate some differences between the two periods.
For example, in the postenhancement period, respondents in both
areas were less likely to exchange sex for needs, less likely to think
of themselves as at risk for HIV, and more likely to have known
someone with HIV infection or AIDS.
Contact with outreach programs increased both in the study and
comparison areas. Outreach contact was at relatively low levels in
the preenhancement period, particularly in the comparison area.
For example, in the study area, ever having talked with an out-

ENHANCED STREET OUTREACH AND CONDOM USE
91
reach worker increased from 32.4% to 57.3% between the pre-
and postenhancement periods; in the comparison area, it
increased from 18.6% to 47.0%. Increased contact in the compar-
ison area was related to programs unrelated to AESOP that were
being developed in this area. In the study area, the percentage
that had received condoms from outreach workers (including the
mobile van) increased from 21.4% to 39.5% and in the comparison
area, from 12.5% to 16.8%.
With regard to condom use during most recent intercourse, there
were statistically significant increases for main partners for vagi-
nal (from 27.1% to 39.0%) and oral sex (from 10.5% to 27.3%) in
the study area. In the comparison area, these percentages
declined for vaginal (from 21.0% to 17.2% and for oral sex (from
16.1% to l1.3%).
Data provided by the outreach programs support the survey
results indicating that many respondents received services from
the mobile van. Quarterly data from the program indicate that
during 1994 (roughly corresponding to the postenhancement
period) nearly 10,000 street outreach contacts were made and
more than 66,000 condoms distributed.
Multiple logistic regression analysis (Table 3) indicates that being
in the postenhancement study area was associated with higher
use of condoms during most recent vaginal sex with main partner
(OR, 1.9; CI, 1.3–2.7). This indicates a quasi-experimental effect
for this variable, consistent with the enhanced intervention’s hav-
ing an effect on change toward safer behavior. Being in the post-
enhancement study area was also associated with a higher odds of
getting condoms from outreach workers (OR, 3.1; CI, 1.3–7.6 )
and having condoms at interview (OR, 2.0; CI, 1.0–4.0). For con-
dom use with casual partners, there were no significant effects of
being in the postenhancement study area. Similar to condom use
for main partners, having condoms is a strong predictor of con-
dom use (OR, 3.0; CI, 1.9–5.0) and is in turn strongly related to
outreach contact (OR, 2.3; CI, 1.3–4.1), indicating a strong indi-
rect relationship between condom use and contact with outreach
programs for persons with casual partners.

AESOP
92
The study and comparison areas for the Chicago site had relatively
low levels of preenhancement outreach activity. Substantial
increases in interaction with outreach workers were reported in
both areas. Survey and program data show the distribution of
condoms and services by mobile van. The surveys measured
aggregate behavior change in the study area consistent with the
effectiveness of enhanced interventions on increased condom use
with main partner. As is true of data from other sites, the survey
data indicated the importance of outreach in supporting condom
use indirectly through supplying condoms.
AIDS P
ROGRAM
, L
OS
A
NGELES
C
OUNTY
This project evaluated street outreach interventions for IDUs,
comparing enhanced street outreach in the central Los Angeles
area (Downtown, South Central, East LA, and Pico Union) with the
comparison area (San Fernando, Pasadena, San Gabriel, Harbor
South, and South LA). The enhanced intervention centered on
additional services provided by the outreach workers, including
the provision of on-the-street HIV counseling and testing, a refer-
ral tracking system, and the use of HIV prevention narratives
based on indigenous artwork on a series of cards. (See Long et al.
in this monograph for a detailed description.)
Characteristics of survey respondents indicate roughly similar
populations in the pre- and postenhancement periods, with some
differences: for example, in the study area, crack use increased;
in the comparison areas, the number of sex partners decreased. A
number of measures of contact with outreach programs increased
between the two periods in both areas. The percentage who had
talked with an outreach worker in the past month, for example,
increased from 52.7% to 59.6% in the study area and from 28.6%
to 38.2% in the comparison area. Neither area had statistically
significant changes in the percentage who used condoms during
most recent sex, for any type of sex or type of partner.
Survey responses indicate exposure to the enhanced intervention.
Almost 16% of respondents in the postenhancement study area
who had talked with outreach workers reported having been
shown the narrative cards. A sizeable percentage reported having
talked about services and having been referred, although a

ENHANCED STREET OUTREACH AND CONDOM USE
93
smaller percentage reported that they went for services. Finally, of
those who talked with outreach workers, 12.9% stated that they
had received an HIV test from the worker, either on the street or in
a nearby mobile van.
Multivariate logistic regression analysis (Table 4) indicates that
having a condom at the time of interview was associated with more
frequent condom use for vaginal sex with main (OR, 2.1; CI, 1.4–
3.2) and casual (OR, 4.1; CI, 2.7–6.1) partners. Having condoms
at the time of interview was in turn strongly associated with out-
reach contact for respondents with main (OR, 2.8; CI, 2.0–3.9)
and casual partners (OR, 2.9; CI, 1.9–4.2), indicating consistent
indirect effects of outreach programs on use of condoms.
Many IDUs interviewed on the street reported contact with street
outreach interventions, including the AESOP enhanced interven-
tions. No statistically significant change in condom use was found
from pre- to postenhancement. Consistent associations between
program contact and having condoms, and between having con-
doms and using them, indicates the importance of outreach pro-
grams in supporting condom use in this population.
P
HILADELPHIA
H
EALTH
M
ANAGEMENT
C
ORPORATION
The Philadelphia site evaluated street outreach for IDUs in two
North Philadelphia areas. The enhanced street outreach interven-
tions centered on providing specialized training to outreach work-
ers related to (a) staging clients into stage-of-change categories, (b)
improved client follow-up, (c) escorting clients to referral services,
(d) use of improved reporting forms, and (e) community presenta-
tions. Outreach workers were added. Learning the stages-of-
change concept enabled workers to stage clients in order to pro-
vide the most appropriate messages and services. Fishbein and
Rhodes (1997) have provided a discussion of how the trans-
theoretical stage model can be applied in HIV prevention.
The populations were similar. There were some differences
between rounds, for example, an increase in crack use in study
and comparison areas. A fairly high proportion of respondents in
both areas had contact with outreach programs in the pre-
enhancement period, and there were no statistically significant

AESOP
94
increases. For example, 60.1% of respondents in the study area
had talked with an outreach worker in the preenhancement period
and 66.7% during the postenhancement period. In the compari-
son area, the figures were 54.2% and 60.9%.
There were no significant increases in the percentage who had
used condoms during their most recent sexual encounter. In the
comparison area, the percentage who had used condoms during
most recent vaginal sex with casual partners decreased from
81.3% to 60.0%. Program data indicate that the enhanced pro-
gram had 4,823 outreach contacts during a 6-month period
corresponding to the postenhancement phase and that 8,715 con-
doms were distributed.
Multivariate analysis did not indicate any effects of being in the
postenhancement study area on condom use with main partners.
For casual partners, being in the postenhancement study area
had a statistically significant effect on condom use (OR, 3.7; CI,
1.4–9.6; Table 5). However, condom use with casual partners
decreased in the comparison area (from 81.3% to 60.0%), and con-
dom use remained the same in the study area (68.0% to 64.5%).
This decrease suggests that the enhancement was effective in
maintaining condom use with casual partners. As was true at
other sites, having a condom at interview was a strong predictor of
condom use with main (OR, 1.8; CI, 1.2–2.6) and casual (OR, 2.2;
CI, 1.3–3.6) partners. Contact with street outreach programs was
a consistent predictor of having condoms at interview for respon-
dents who had main (OR, 3.0; CI, 2.0–4.6) and casual partners
(OR, 2.0; CI, 1.3–3.4).
Outreach contact was relatively high in the preenhancement
period, and the surveys did not indicate significant increases in
outreach contact with IDUs. No increases in condom use with
main partners were observed, but condom use declined for casual
partners in the comparison area. Being in the postenhancement
study area was associated with maintaining condom use for
casual partners. As at other sites, there was consistent associa-
tion between having condoms and using them, and between out-
reach contact and having condoms, indicating the indirect effect of
the programs on condom use.

ENHANCED STREET OUTREACH AND CONDOM USE
95
DISCUSSION
The quasi-experimental design of AESOP—study and comparison
areas and pre- and postenhancement periods—did not identify
many areas in which there was a change in condom use behaviors
associated with enhanced programs. If we define a quasi-experi-
mental effect as a significant association between condom use and
being in the postenhancement study area, these effects were seen
only in Chicago and Los Angeles.
The relative lack of findings indicating behavior change are in part
due to the inherent weaknesses of the quasi-experimental design
(Coyle, Boruch & Turner, 1991). These weaknesses include the
inability to control other factors affecting the behavior of risk
group members, both in the study and comparison areas, and the
difficulty of acquiring equivalent samples over time from the shift-
ing street populations. Further, data collected as part of AESOP
indicated that other changes were occurring in addition to the
AESOP enhancements. These changes included program staffing
changes, environmental changes due to weather and other causes,
and changes in the location of street populations (Kay, 1995). The
relative lack of findings indicating behavior change may be due in
part to lack of contact with outreach workers who delivered the
AESOP enhancement. Although the respondents reported a high
level of contact with outreach workers, many linked their outreach
workers to other outreach programs or could not identify the
agencies of these workers. Because AESOP interventions were not
comparable, data could not be aggregated to examine whether the
respondents exposed to the study intervention changed behavior.
Despite these limitations of the quasi-experimental approach,
other, more powerful evaluation methods such as cohort studies
with random assignment to specific treatments may not be appro-
priate for evaluating street outreach programs. Street outreach
interventions take place in the natural environment of high-risk
groups and necessarily involve interactions with transient clients,
many of whom are not willing or able to participate in ongoing
studies.

AESOP
96
Apart from the quasi-experimental aspects of AESOP, the data
have great value as observational data for evaluating street out-
reach programs. Because street outreach takes place in public
places and sensitive topics are discussed, it is very difficult to col-
lect information on the process. The AESOP data provide some of
the first systematically collected data on street populations that
measure the services received from HIV prevention street outreach
programs, a major component of HIV prevention.
The AESOP survey data also provide information on the preva-
lence of risk behaviors and condom use in the high-risk popula-
tions studied. For example, the percentage who used condoms
during most recent vaginal sex ranged from 21.7% to 47.6% for
main partners and from 57.9% to 71.8% for casual partners.
These percentages can be compared with national HIV prevention
objectives that by the year 2000 the rate of condom use during
most recent intercourse should increase to 50% for unmarried
sexually active persons; and the rate should be 60% among sexu-
ally active women aged 15 to 19 years, 75% among sexually active
men aged 15 to19 years, and 60% among IDUs (U.S. Department
of Health and Human Services, 1990). Higher rates of condom use
with casual or paying partners constitute a pattern that has been
found consistently, including general population surveys (Kost &
Forrest, 1992; Tanfer, Grady, Klepinger & Billy, 1993), studies of
IDUs and their partners (CDC, 1991, 1992; Pivnick, 1993; Rhodes
et al., 1990; Singh et al., 1993), and sexually transmitted disease
clinic patients (CDC, 1990, 1993). In spite of the levels of condom
use reported by AESOP respondents, the data document the
extent to which these populations engage in high-risk behavior in
spite of public health efforts.
Street outreach is designed to reach some of the persons at high-
est risk and some of those most difficult to reach with prevention
messages and services. As such, it is a very important part of HIV
prevention, but at the same time is one of the most difficult. The
collection of data on outreach and for the evaluation of programs
is difficult and costly. The AESOP survey data have shown the
extent to which high-risk populations have contact with outreach
programs and use their services and the extent to which outreach
workers play an important role in dispensing condoms to these
high-risk groups. The AESOP data speak very consistently of the
role of outreach programs in supporting the carrying of condoms

ENHANCED STREET OUTREACH AND CONDOM USE
97
and, indirectly, in condom use by these populations who typically
have spontaneous sex. At every site, having a condom at interview
was associated with higher odds of using condoms. Further, hav-
ing a condom at interview was consistently associated with having
received condoms from outreach workers. At every site, the extent
to which respondents had contact with specific enhanced inter-
ventions was measured. Contact with some enhancements, such
as the van or storefront outreach, were perhaps more easily mea-
sured by interviews with on-the-street populations.
Given that a wide array of customized enhancements to these
established programs had very limited effect on increasing behav-
ioral change over a 6-month period, our data suggest that a cre-
ative focus on condom distribution should be a major goal of
street outreach programs. This focus might include economical
distribution plans to increase availability, such as containers
accessible during evenings and weekends, when outreach workers
are typically not available. Moreover, such containers would be
accessible to the harder-to-reach persons who do not come into
contact with outreach workers. Increasing distribution could be
complemented with an ongoing, community condom promotion
aimed at youth or IDUs, such as Switzerland’s successful STOP
AIDS campaign strategies, in which sexual transmission risks
have taken top billing (Hausser, Zimmerman, Dubois-Arber &
Paccaud, 1991). An increased focus on condoms should also
reduce the acquisition of sexually transmitted diseases, which
have been linked to an increased risk for HIV transmission
(Wasserheit, 1992).

AESOP
98
References
Anderson, J.E., Cheney, R., Clatts, M., Faruque, S., Kipke, M.,
Long, A., Mills, S., Toomey, K., & Wiebel, W. (1996). HIV risk
behavior, street outreach and condom use in 8 high risk popu-
lations. AIDS Education and Prevention, 8(3), 191-204.
CDC. (1990). Heterosexual behaviors and factors that influence
condom use among patients attending a sexually transmitted
disease clinic—San Francisco. Morbidity and Mortality Weekly
Report, 39, 685-689.
CDC. (1991). Drug use and sexual behaviors among sex partners
of injecting-drug users—United States, 1988-1990. Morbidity
and Mortality Weekly Report, 40, 855-860.
CDC. (1992). What have we learned from the AIDS community
demonstration projects? Atlanta, GA: CDC.
CDC. (1993). Distribution of STD clinic patients along a stages-of-
change continuum—Selected sites, 1993. Morbidity and Mor-
tality Weekly Report, 42, 880-883.
Coyle, S.L., Boruch, R.F., & Turner, C.F. (Eds.). (1991). Eval-
uating AIDS prevention programs (expanded ed.). Washington,
DC: National Academy Press.
Fishbein, M., & Rhodes, F. (1997). Using behavioral theory in HIV
prevention (pp. 21-34). In N.H.Corby & R.J. Wolitski (Eds.),
Community HIV prevention: The Long Beach AIDS Community
Demonstration Project. Long Beach California: University Press,
California State University.
Hausser, D., Zimmermann, E., Dubois-Arber, F., & Paccaud, F.
(1991). Evaluation of the AIDS prevention strategy in Switzer-
land. Third assessment report (1989–1990). Lausanne: Institut
universitaire de medecine sociale et preventive.
Kay, L. (1995, November). Possible confounders for interpreting
data from street outreach studies. Paper presented at the
annual meeting of the American Public Health Association,
San Diego.

ENHANCED STREET OUTREACH AND CONDOM USE
99
Kost K., & Forrest, J.D. (1992). American women's sexual behav-
ior and exposure to risk of sexually transmitted diseases.
Family Planning Perspectives, 24, 244-254.
Pivnick, A. (1993). HIV infection and the meaning of condoms.
Culture, Medicine and Psychiatry, 17, 431-453.
Rhodes, F., Corby, N.H., Wolitski, R.J., Tashima, N., Crain, C., &
Yankovich, D.R. (1990). Risk behaviors and perceptions of
AIDS among street injection drug users. Journal of Drug Edu-
cation, 20, 271-288.
Singh, B.K., Koman, J.J., Catan, V.M., Souply, L.L., Birkel, R.C.,
& Golazewski, T.J. (1993). Sexual risk behavior among injec-
tion drug-using human immunodeficiency virus positive
clients. International Journal of the Addictions, 28, 735-747.
Tanfer, K., Grady, W.R., Klepinger, D.H., & Billy, J.O.G. (1993).
Condom use among men. Family Planning Perspectives, 25,
61-66.
U.S. Department of Health and Human Services. (1990). Healthy
people 2000: National health promotion and disease preven-
tion objectives (DHHS Publication No. [PHS] 91-50213). Wash-
ington, DC: U.S. Government Printing Office.
Wasserheit, J.N. (1992). Epidemiological synergy: Interrelation-
ships between human immunodeficiency virus infection and
other sexually transmitted diseases. Sexually Transmitted
Diseases, 19, 61-77.

AESOP
100
Table 1. Logistic Regression Analysis: Comparison of Two
Pre- and Two Postenhancement Rounds of AESOP Data from
Children’s Hospital, Los Angeles
Vaginal Sex with Main Partners, Past Month
(466 Observations)
Basic Model
Basic Model +
Covariates
Predictors OR 95% CI OR 95% CI
Condom use, most recent vaginal sex
Study area
Postenhancement
Postenhancement study area
African American
STD, ever
Condoms from outreach worker, ever
Have condom now
1.7
0.7
1.2
1.0–2.9
0.4–1.2
0.6–2.5
1.1
0.7
1.3
1.9
0.6
1.9
2.3
0.6– 2.1
0.4– 1.2
0.6– 2.9
1.1– 3.1
0.3– 1.0
1.2– 3.0
1.5– 3.6
Condoms from outreach worker, past mo.
Study area
Postenhancement
Postenhancement study area
Male
Living on the street
Talked with outreach worker, past 6 mos.
3.6
3.0
0.4
1.5–8.6
1.3–7.1
0.1–1.2
1.2
3.1
0.4
2.2
2.3
7.0
0.5– 3.2
1.3– 7.7
0.1– 1.3
1.3– 4.0
1.2– 4.3
3.6–13.5
Have condoms now
Study area
Postenhancement
Postenhancement study area
Condoms from outreach worker, past mo.
3.4
1.3
0.7
1.8–6.5
0.7–2.5
0.3–1.7
3.1
1.1
0.8
2.5
1.6– 5.9
0.6– 2.2
0.3– 1.9
1.5– 4.2

ENHANCED STREET OUTREACH AND CONDOM USE
101
Vaginal Sex with Casual Partners, Past Month
(424 Observations)
Basic Model
Basic Model +
Covariates
Predictors OR 95% CI OR 95% CI
Condom use, most recent vaginal sex
Study area
Postenhancement
Postenhancement study area
3 or more partners, past mo.
Condoms from outreach worker, ever
Have condom now
1.6
0.8
1.2
0.9– 2.9
0.5– 1.4
0.5– 2.6
1.1
0.8
1.0
1.7
2.2
2.1
0.6– 2.1
0.5– 1.4
0.4– 2.4
1.1– 2.6
1.3– 3.8
1.3– 3.5
Condoms from outreach worker, past mo.
Study area
Postenhancement
Postenhancement study area
Hispanic
Talked with outreach worker, past 6 mos.
6.8
3.9
0.4
2.8–16.5
1.6– 9.8
0.1– 1.2
4.5
3.8
0.5
2.2
3.7
1.7–11.6
1.5– 9.7
0.1– 1.4
1.1– 4.1
2.1– 6.4
Have condoms now
Study area
Postenhancement
Postenhancement study area
Condoms from outreach worker, past mo.
1.9
1.2
1.5
1.1– 3.4
0.6– 2.2
0.7– 3.5
1.5
1.0
1.6
2.4
0.8– 2.8
0.6– 2.0
0.7– 3.8
1.5– 4.0

AESOP
102
Table 2. Logistic Regression Analysis: Comparison of Two
Pre- and Two Postenhancement Rounds of AESOP Data from
San Francisco
Vaginal Sex with Main Partners, Past Month
(318 Observations)
Basic Model
Basic Model +
Covariates
Predictors OR 95% CI OR 95% CI
Condom use, most recent vaginal sex
Study area
Postenhancement
Postenhancement study area
African American
Living on the street
Have condom now
Condoms from outreach worker, past mo.
1.7
1.1
0.6
0.9– 3.4
0.5– 2.3
0.2– 1.6
1.7
1.4
0.6
6.8
0.4
2.4
2.0
0.8– 3.6
0.6– 3.0
0.2– 1.6
1.2–38.8
0.2– 0.8
1.3– 4.4
1.1– 3.6
Condoms from outreach worker, past mo.
Study area
Postenhancement
Postenhancement study area
Talked with outreach worker, past 6 mos.
5.4
2.4
0.5
2.1–14.0
0.8– 6.7
0.1– 1.6
5.2
3.2
0.3
4.9
1.9–14.0
1.1– 9.6
0.1– 1.1
2.7– 8.8
Have condoms now
Study area
Postenhancement
Postenhancement study area
STD, ever
Condoms from outreach worker, past mo.
0.1
0.6
1.7
0.5– 2.0
0.3– 1.5
0.6– 5.1
0.7
0.6
1.8
2.4
3.4
0.3– 1.5
0.2– 1.4
0.6– 5.8
1.3– 4.6
1.8– 6.4

ENHANCED STREET OUTREACH AND CONDOM USE
103
Vaginal Sex with Casual Partners, Past Month
(278 Observations)
Basic Model
Basic Model +
Covariates
Predictors OR 95% CI OR 95% CI
Condom use, most recent vaginal sex
Study area
Postenhancement
Postenhancement study area
Somewhat to very likely to get HIV
Have condom now
1.2
0.7
1.7
0.6–2.4
0.3–1.5
0.6–4.5
1.2
0.7
1.7
0.5
1.7
0.6–2.6
0.3–1.5
0.6–4.6
0.3–0.8
1.0–2.9
Condoms from outreach worker, past mo.
Study area
Postenhancement
Postenhancement study area
Used crack, past mo.
Talked with outreach worker, past 6 mos.
3.4
0.8
1.2
1.5–7.7
0.3–2.1
0.4–3.5
2.7
0.7
0.9
2.7
4.4
1.2–6.3
0.3–1.8
0.3–2.9
1.4–5.4
2.4–8.1
Have condoms now
Study area
Postenhancement
Postenhancement study area
Condoms from outreach worker, past mo.
0.8
1.0
2.0
0.4–1.6
0.5–2.2
0.7–5.4
0.6
1.0
2.0
2.5
0.3–1.3
0.5–2.3
0.7–5.6
1.4–4.2

AESOP
104
Table 3. Logistic Regression Analysis: Comparison of Two
Pre- and Two Postenhancement Rounds of AESOP Data from
Chicago
Vaginal Sex with Main Partners, Past Month
(740 Observations)
Basic Model
Basic Model +
Covariates
Predictors OR 95% CI OR 95% CI
Condom use, most recent vaginal sex
Study area
Postenhancement
Postenhancement study area
STD, ever
Have condom now
Condoms from outreach worker, past mo.
1.4
0.8
2.1
0.9–2.3
0.5–1.3
1.2–4.2
1.3
0.8
1.9
0.6
1.8
1.9
0.8– 2.1
0.5– 1.3
1.0– 3.8
0.4– 0.9
1.2– 2.6
1.3– 2.7
Condoms from outreach worker, past mo.
Study area
Postenhancement
Postenhancement study area
Talked with outreach worker, past 6 mos.
Tested for HIV, ever
1.6
1.1
2.2
0.9–2.7
0.6–1.8
1.1–4.5
1.0
0.5
3.1
21.9
3.5
0.5– 2.0
0.2– 0.9
1.3– 7.6
13.7–35.2
1.8– 6.7
Have condoms now
Study area
Postenhancement
Postenhancement study area
STD, ever
Injected, past mo.
Condoms from outreach worker, past mo.
Tested for HIV, since 1993
1.1
0.8
2.4
0.7–1.9
0.5–1.4
1.2–4.7
1.1
0.6
2.0
1.7
1.8
2.4
1.9
0.7– 1.9
0.4– 1.1
1.0– 4.0
1.2– 2.4
1.0– 3.2
1.7– 3.5
1.1– 3.0

ENHANCED STREET OUTREACH AND CONDOM USE
105
Vaginal Sex with Casual Partners, Past Month
(377 Observations)
Basic Model
Basic Model +
Covariates
Predictors OR 95% CI OR 95% CI
Condom use, most recent vaginal sex
Study area
Postenhancement
Postenhancement study area
Male
Have condom now
Condoms from outreach worker, past mo.
1.1
0.7
1.6
0.7-2.0
0.4–1.3
0.7–3.8
1.1
0.7
1.2
0.3
3.0
2.3
0.6– 2.0
0.3– 1.3
0.5– 3.1
0.2– 0.5
1.9– 5.0
1.3– 4.1
Condoms from outreach worker, past mo.
Study area
Postenhancement
Postenhancement study area
Talked with outreach worker, past 6 mos.
1.7
2.0
1.5
0.8–3.6
0.9–4.6
0.5–4.1
1.8
0.8
1.4
25.7
0.7– 4.5
0.3– 2.3
0.4– 5.1
13.3–49.7
Have condoms now
Study area
Postenhancement
Postenhancement study area
STD, ever
Condoms from outreach worker, past mo.
Tested for HIV, since 1993
0.8
1.0
2.3
0.4–1.4
0.5–1.9
0.9–5.7
0.7
0.6
2.3
1.7
2.1
2.1
0.4– 1.2
0.3– 1.3
0.9– 5.8
1.1– 2.8
1.3– 3.5
1.1– 4.1

AESOP
106
Table 4. Logistic Regression Analysis: Comparison of Two
Pre- and Two Postenhancement Rounds of AESOP Data from
Los Angeles County
Vaginal Sex with Main Partners, Past Month
(811 Observations)
Basic Model
Basic Model +
Covariates
Predictors OR 95% CI OR 95% CI
Condom use, most recent vaginal sex
Study area
Postenhancement
Postenhancement study area
African American
Exchange sex for needs, ever
Condoms from outreach worker, ever
Have condom now
1.2
1.0
1.2
0.7– 2.1
0.6– 1.7
0.6– 2.4
0.7
0.8
1.3
1.6
0.4
2.2
2.1
0.4–1.3
0.4–1.4
0.6–2.8
1.0–2.3
0.3–0.7
1.5–3.3
1.4–3.2
Condoms from outreach worker, past mo.
Study area
Postenhancement
Postenhancement study area
African American
Homeless, past year
Somewhat to very likely to get HIV
Drug treatment, past 6 mos.
Bleach from outreach worker
6.3
2.0
0.5
3.9–10.3
1.2– 3.3
0.3– 0.9
5.6
2.2
0.3
1.6
1.7
1.4
0.6
6.6
3.2–9.8
1.2–3.8
0.2–0.7
1.1–2.3
1.2–2.4
1.0–2.0
0.4–1.0
4.6–9.3
Have condoms now
Study area
Postenhancement
Postenhancement study area
Exchange sex for need, ever
3 or more partners, past mo.
Used crack, past mo.
Condoms from outreach worker, past mo.
2.1
1.0
0.9
1.3– 3.2
0.7– 1.7
0.5– 1.6
1.5
0.9
0.9
1.5
2.3
1.4
2.8
0.9–2.5
0.6–1.5
0.5–1.7
1.0–2.1
1.5–3.6
1.0–1.9
2.0–3.9

ENHANCED STREET OUTREACH AND CONDOM USE
107
Vaginal Sex with Casual Partners, Past Month
(526 Observations)
Basic Model
Basic Model +
Covariates
Predictors OR 95% CI OR 95% CI
Condom use, most recent vaginal sex
Study area
Postenhancement
Postenhancement study area
Male
Tested for HIV, ever
Have condom now
1.4
1.4
0.8
0.9– 2.3
0.9– 2.3
0.4– 1.5
1.2
1.1
0.8
0.2
2.1
4.1
0.7– 2.1
0.6– 2.0
0.4– 1.8
0.2– 0.4
1.2– 3.7
2.7– 6.1
Condoms from outreach worker, past mo.
Study area
Postenhancement
Postenhancement study area
Bleach from outreach worker
Talked with outreach worker, past 6 mos.
6.2
2.6
0.3
3.6–10.9
1.5– 4.7
0.2– 0.7
5.6
2.4
0.3
4.4
2.8
2.9–10.6
1.2– 4.6
0.1– 0.6
1.8–10.8
1.1– 6.8
Have condoms now
Study area
Postenhancement
Postenhancement study area
Male
3 or more partners, past mo.
Talked with outreach worker, past 6 mos.
1.7
1.2
1.0
1.0– 2.7
0.8– 2.1
0.5– 1.9
1.2
0.9
1.3
0.5
1.6
2.9
0.7– 2.0
0.6– 1.6
0.6– 2.8
0.3– 0.7
1.1– 2.3
1.9– 4.2

AESOP
108
Table 5. Logistic Regression Analysis: Comparison of Two
Pre- and Two Postenhancement Rounds of AESOP Data from
Philadelphia
Vaginal Sex with Main Partners, Past Month
(692 Observations)
Basic Model
Basic Model +
Covariates
Predictors OR 95% CI OR 95% CI
Condom use, most recent vaginal sex
Study area
Postenhancement
Postenhancement study area
Have condom now
Talked with outreach worker, past 6 mos.
0.9
1.1
1.2
0.5–1.4
0.7–1.7
0.6–2.3
0.8
1.3
1.1
1.8
1.7
0.5–1.3
0.8–2.1
0.6–2.3
1.2–2.6
1.2–2.4
Condoms from outreach worker, past mo.
Study area
Postenhancement
Postenhancement study area
Talked with outreach worker, past 6 mos.
1.0
0.5
1.7
0.6–1.7
0.3–0.9
0.8–3.5
1.0
0.6
1.5
3.5
0.6–1.6
0.3–1.0
0.7–3.2
2.3–5.2
Have condoms now
Study area
Postenhancement
Postenhancement study area
3 or more partners, past mo.
Condoms from outreach worker, ever
Condoms from outreach worker, past mo.
1.3
0.3
1.7
0.8–2.1
0.2–0.5
0.8–3.5
1.3
0.3
1.4
3.9
2.3
3.0
0.8–2.2
0.2–0.5
0.6–3.0
2.5–6.3
1.5–3.4
2.0–4.6

ENHANCED STREET OUTREACH AND CONDOM USE
109
Vaginal Sex with Casual Partners, Past Month
(423 Observations)
Basic Model
Basic Model +
Covariates
Predictors OR 95% CI OR 95% CI
Condom use, most recent vaginal sex
Study area
Postenhancement
Postenhancement study area
Male
Somewhat to very likely to get HIV
Know someone with HIV
Talked with outreach worker, past 6 mos.
Have condom now
0.4
0.3
2.8
0.2–0.9
0.2–0.7
1.2–6.9
0.3
0.3
3.7
0.5
0.5
1.8
1.9
2.2
0.1–0.7
0.1–0.7
1.4–9.6
0.3–0.8
0.3–0.8
1.1–2.9
1.2–3.0
1.3–3.6
Condoms from outreach worker, past mo.
Study area
Postenhancement
Postenhancement study area
Talked with outreach worker, past 6 mos.
1.2
0.9
1.2
0.6–2.6
0.5–1.9
0.5–3.1
1.1
1.0
1.1
2.5
0.5–2.5
0.5–2.2
0.4–3.1
1.5–4.0
Have condoms now
Study area
Postenhancement
Postenhancement study area
Homeless, past year
Tested for HIV, ever
Condoms from outreach worker, past mo.
1.2
0.4
0.8
0.7–2.3
0.2–0.8
0.3–1.8
1.2
0.4
0.7
1.7
1.7
2.0
0.6–2.3
0.2–0.7
0.3–1.7
1.0–2.6
0.9–3.2
1.3–3.4

111
PRODUCTS AND CONTACTS
FOR
INTERVENTION REPLICATION
ASSOCIATION FOR DRUG ABUSE PREVENTION
AND TREATMENT
Title: Doing Street Outreach in the Community:
Helpful Hints to Do a Good Job and Document It
Description: The product is a monograph for administrators and
staff of community-based organizations conducting
or contemplating street outreach. The 50-page
monograph addresses documentation forms, meth-
ods, and procedures to be used in process evalua-
tion, quality assurance, and identifying and meeting
the needs of the target population. Sample forms
are included in the appendix.
Contact: Ms. Naomi Fatt
ADAPT
2230 First Avenue
New York, NY 10029
(212) 289-1957
CHILDREN’S HOSPITAL OF LOS ANGELES
Title: Facing the Challenge: Building Peer Programs for
Street Youth
Description: The product is a study aid and accompanying video
for service providers, educators, community pro-
gram organizers, and policymakers from agencies
that target high-risk youth. The 30-page study aid
addresses how to plan and conduct a peer model
program, recruit participants, and manage the pro-
gram. The 22-minute video presents illustrations of
issues that are key to successful programs.

AESOP
112
Contact: Ms. Ellen Iverson
Division of Adolescent Medicine
Children’s Hospital of Los Angeles
P.O. Box 54700, Mail Stop 2
Los Angeles, CA 90054-0700
(213) 660-2450 ext. 3110
Title: Straight Dope Productions: The Making of a
Community-Level Intervention
Description: The product is a workbook for community-based
organizations that provide HIV-related services to
youth or that would like to extend their current
activities to include services for youth.
Contact: Ms. Ellen Iverson
Division of Adolescent Medicine
Children’s Hospital of Los Angeles
P.O. Box 54700, Mail Stop 2
Los Angeles, CA 90054-0700
(213) 660-2450 ext. 3110
COUNTY OF LOS ANGELES, DEPARTMENT OF
H
EALTH SERVICES, AIDS PROGRAMS
Title: Confidential HIV Antibody Finger Stick
Testing Manual
Description: The product is a manual for administrators and
program coordinators of agencies and organizations
that provide street outreach to injection drug users
and users of other illicit substances. The 35-page
manual contains the development and implementa-
tion of an HIV antibody testing program in which the
finger-stick method is used in a street outreach
setting. The technique is illustrated in the video L.A.
County AIDS Evaluation of Street Outreach Programs.

PRODUCTS AND CONTACTS
113
Contact: Dr. Anna Long, Chief of Staff
Public Health Programs and Services
Los Angeles County Department of Health
313 N. Figueroa Street
Los Angeles, CA 90012
(213) 240-8036
Title: Developing Culture-Specific Media for HIV Risk
Reduction for Injection Drug and Other Substance
Abusers: Lessons from the AIDS Evaluation of Street
Outreach Program
Description: The product is a monograph for agencies and
organizations that have or are contemplating HIV
risk-reduction intervention programs for injection
drug users and users of other illicit substances. The
25-page monograph describes how to develop edu-
cational materials, including determining the need
for such materials and selecting the appropriate
messages, media, and visuals to use.
Contact: Dr. Anna Long, Chief of Staff
Public Health Programs and Services
Los Angeles County Department of Health
313 N. Figueroa Street
Los Angeles, CA 90012
(213) 240-8036

AESOP
114
Title: A Guide to Determining Stages of Change for HIV
Risk Reduction Behaviors: Cessation of Needle
Sharing, Needle Bleaching, and Condom Use
Description: The product is a manual for agencies and organiza-
tions that provide street outreach to injection drug
users and users of other illicit substances. The 50-
page manual covers a method outreach workers can
use to screen clients quickly for specific risk behav-
iors, assess the relative risk of those behaviors, and
determine the clients’ intention to change their
behaviors. The technique is illustrated in the video
L.A. County AIDS Evaluation of Street Outreach Pro-
grams.
Contact: Dr. Anna Long, Chief of Staff
Public Health Programs and Services
Los Angeles County Department of Health
313 N. Figueroa Street
Los Angeles, CA 90012
(213) 240-8036
Title: L.A. County AIDS Evaluation of Street Outreach
Programs
Description: The product is a video for program coordinators and
outreach staff of agencies and organizations that
provide street outreach to injection drug users and
users of other illicit substances. The 45-minute
video covers the background of the program and
illustrates the use of four techniques for street
outreach: stages of change, artwork to engage
clients, finger-stick HIV testing, and referral track-
ing system.
Contact: Dr. Anna Long, Chief of Staff
Public Health Programs and Services
Los Angeles County Department of Health
313 N. Figueroa Street
Los Angeles, CA 90012
(213) 240-8036

PRODUCTS AND CONTACTS
115
Title: Narratives from Illustrations: Development and Use
in the Field
Description: The product is a manual for administrators, pro-
gram coordinators, and outreach staff of agencies
and organizations that provide street outreach to
injection drug users and users of other illicit sub-
stances. The 20-page manual describes an inter-
vention in which narratives and illustrations are
used to engage clients in street outreach settings
and discusses steps for developing and implement-
ing the technique. This technique is illustrated in
the video L.A. County AIDS Evaluation of Street Out-
reach Programs.
Contact: Dr. Anna Long, Chief of Staff
Public Health Programs and Services
Los Angeles County Department of Health
313 N. Figueroa Street
Los Angeles, CA 90012
(213) 240-8036
Title: Outreach Referral Tracking System Manual
Description: The product is a manual for program coordinators
and outreach staff of agencies and organizations
that provide street outreach to injection drug users
and users of other illicit substances. The 30-page
manual covers establishing personal contact with
referral service staff, assessing client readiness to
seek services, and following up client referrals to
services. The technique is illustrated in the video
L.A. County AIDS Evaluation of Street Outreach Pro-
grams.
Contact: Dr. Anna Long, Chief of Staff
Public Health Programs and Services
Los Angeles County Department of Health
313 N. Figueroa Street
Los Angeles, CA 90012
(213) 240-8036

AESOP
116
EMORY UNIVERSITY, THE ROLLINS SCHOOL OF
P
UBLIC HEALTH
Title: Formative Research as Foundation of Intervention
Development: Community Assessment Process (CAP)
Description: The product is a manual for administrators involved
in HIV prevention program development. The 35-
page manual addresses the need for formative
research, the systematic process of conducting it,
and the utilization of findings in the development
and implementation of intervention programs. The
process is illustrated with examples and sample
recording forms.
Contact: Dr. Claire Sterk
The Rollins School of Public Health
Emory University
1518 Clifton Road, NE
Atlanta, GA 30322
(404) 727-9124
Title: Outreach Interventions Based on the Stages of
Change Model
Description: The product is a manual for public health officials,
researchers, and community-based organizations
dealing with HIV who use or plan to use outreach as
a means of providing an intervention. The 20-page
manual covers general training needs for outreach
workers and training needs specific to the stages-of-
change intervention; training exercises are included.
Contact: Dr. Claire Sterk
The Rollins School of Public Health
Emory University
1518 Clifton Road, NE
Atlanta, GA 30322
(404) 727-9124

PRODUCTS AND CONTACTS
117
PHILADELPHIA HEALTH MANAGEMENT CORP.
Title: Hittin’ the Streets: A Handbook for Street
Interviewers and
Hittin’ the Streets: Trainer’s Notes
Description: The product is a handbook and trainer’s notes for
street outreach. The 40-page handbook describes
preparations for conducting street interviews, how
to handle oneself on the street, establishing rapport
in the outreach area, and debriefing. The 10-page
trainer’s notes contain role plays and other exercises
to help outreach workers practice what they learn
from the handbook.
Contact: Philadelphia Health Management Corp.
c/o “Hittin’ the Streets”
260 South Broad Street, 20th Floor
Philadelphia, PA 19102
(215) 985-2524
Title: Making the Change: Helping Your Clients to Help
Themselves
Description: The product is a video with trainer and student
manuals and a video for social service providers,
such as street outreach workers and social workers.
The 55-page manual addresses the stages-of-
change approach and strategies for motivating
clients. It includes tips on how to conduct training
with these materials. The 27-minute video demon–
strates interacting with clients and helping to lead
them to changing their behavior.
Contact: Philadelphia Health Management Corp.
c/o “Making the Change”
260 South Broad Street, 20th Floor
Philadelphia, PA 19102
(215) 985-2524

AESOP
118
UNIVERSITY OF ILLINOIS AT CHICAGO
Title: Evaluation – How to Use an Agency’s Own Data to
Guide Program
Description: The product is a manual for small service-delivery
organizations that have limited resources for evalu-
ation. The 15-page manual covers what evaluation
is, why it should be done, and how to do it. The ap-
pendix contains sample recording forms.
Contact: Dr. Wayne Wiebel
University of Illinois at Chicago
School of Public Health
2121 West Taylor, Room 556
Chicago, IL 60612
(312) 996-4870
Title: Indigenous Leader Outreach Model
Description: The product is a training curriculum for project
leaders and outreach staff interested in applying
peer-based street-outreach techniques. The 100-
page curriculum has two parts: one for trainers and
one for students. The document contains an outline
of the programmatic needs, techniques, and pro-
cesses involved with street outreach.
Contact: Dr. Wayne Wiebel
University of Illinois at Chicago
School of Public Health
2121 West Taylor, Room 556
Chicago, IL 60612
(312) 996-4870

PRODUCTS AND CONTACTS
119
VICTIM SERVICES AGENCY
Title: Coordination of AIDS Outreach and Prevention
Services for Homeless and Runaway Youth
Description: The product is a case study for project directors and
others interested in building service-delivery coali-
tions. The 20-page case study addresses the co-
ordination of street outreach activities among New
York City agencies that serve homeless and runaway
youth. The study discusses why coordination was
attempted, how it was accomplished, and the result-
ing benefits.
Contact: Ms. Helene Lauffer
Victim Services Agency
2 Lafayette Street
New York, NY 10007
(212) 577-3806
Title: Development of Computerized Documentation
Systems for Street Outreach Programs: Case Study
Description: The product is a case study for directors of pro-
grams interested in developing computerized inter-
agency information systems. The 30-page case
study covers the basic idea of creating a wide-area
network and its application to documenting services
and community planning. Some knowledge of com-
puter software would be useful.
Contact: Ms. Helene Lauffer
Victim Services Agency
2 Lafayette Street
New York, NY 10007
(212) 577-3806

AESOP
120
Title: Innovations in AIDS Outreach and Prevention for
Homeless and Runaway Youth: A Training &
Resource Guide for Applications of the Harm
Reduction Model
Description: The product is a manual for service providers who
are interested in integrating this model into their
programs. The 145-page manual covers informa-
tion on homeless and runaway youth and the con-
ceptual foundations and clinical implications of
using the Harm Reduction Model in a client-
centered approach for this population.
Contact: Ms. Helene Lauffer
Victim Services Agency
2 Lafayette Street
New York, NY 10007
(212) 577-3806
